Obstacles against the Marketing of Curcumin as a Drug
Abstract
1. Introduction and History
2. Disease Targets of Curcumin: From Cell Lines to Clinical Trials Studies
2.1. Antimicrobial Effect of Curcumin
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcuminoids | Concentration 0.1–1 mg/mL | Anti-parasitic Nematocidal activity of mixed Curcuminoids | In vitro | Kiuchi F et al. 1993 [18] |
| Curcumin Curcumin + boric acid + oxalic acid dihydrate (boron complex) | Curcumin: IC50: 100 µM boron complex: IC50: 6 µM | Anti-viral inhibitor of the HIV-l | In vitro | Sui Z et al. 1993 [19] |
| Curcumin essential oil extracted | Concentration of 0.1% in the medium | Anti-fungal aflatoxin synthesis by Aspergillus parasiticus | In vitro | Tantaoui-Elaraki A et al. 1994 [20] |
| Curcumin | 2.5 g which was repeated 7 days later | Anti-viral inhibitor of the HIV-1 | Clinical Trial (3 Subjects) | Jordan W.C et al. 1996 [21] |
| Turmeric extract | antifungal activity against Candida albicans at 1 µg/mL | Anti-fungal Candida albicans | In vitro | Roth GN et al. 1998 [22] |
| Turmeric oil | Anti-bacterial activity in 50–200 ppm | Anti-bacterial | In vitro | Negi P.S et al.1999 [23] |
| Curcumin | cytotoxicity against leishmania in vitro. The LD50 = 37.6 µM | Anti-parasitic against leishmania | In vitro | Koide T et al. 2002 [24] |
| Curcumin extract | Anti-fungal at 50–500 mg/L | Anti-fungal | In vitro | Kim MK et al. 2003 [25] |
| Curcumin | In vitro: IC50: 5 µM Animal: once daily for 5 days at a dose of 100 mg/kg | Anti-malarial | In vitro & Animal model | Reddy RC et al. 2005 [26] |
| Curcumin | at 30 and 100 μM | Anti-parasitic Giardia lamblia trophozoites | In vitro | Pérez-Arriaga L et al. 2006 [27] |
| Curcumin | 30 mg every 12 h for 7 days | Anti-bacterial | Clinical trial (25 Subjects) | Di Mario F et al. 2007 [28] |
| Curcumin extract quercitin and curcumin (FlogMEV) extracts | In patients with prostatitis quercitin (100 mg) and curcumin (200 mg) for 14 days | Anti-bacterial | Clinical trial (284 Subjects) | Cai T et al. 2009 [29] |
| Curcumin nanoparticle | Concentration of 260 μM | Anti-bacterial | In/vitro | Trigo Gutierrez JK et al. 2017 [30] |
| Curcumin nanoparticle | 0.1 and 0.2 mg per well concentration | Anti-bacterial | In vitro | Fakhrullina G et al. 2019 [31] |
| Curcumin nanoparticle curcumin-silver nanoparticles | Minimum inhibitory concentration 20 mg/L | Anti-bacterial | In vitro | Jaiswal S et al. 2018 [32] |
| Iodinated curcumin | Minimum inhibitory concentration 150 and 120 µg/mL | Anti-bacterial | In vitro | Manchanda G et al. 2018 [33] |
2.2. Gastrointestinal Effect of Curcumin
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin | Concentrations 5–30μM | Liver protective through inhibiting hepatic stellate cells activation | In vitro | Tang Y et al. 2010 [46] |
| Curcumin | Dose: 25 μg daily for 10 weeks, intraperitoneal | Liver protective: effectively limits the development and progression of fibrosis | Animal model | Vizzutti F et al. 2010 [47] |
| Curcumin | 300 mg/kg, by gavage daily for 12 weeks | Liver protective: inhibited the development of liver cirrhosis mainly due to its anti-inflammatory activities and not by a direct anti-fibrotic effect | Animal model | Bruck R et al. 2007 [48] |
| Curcumin | 1 g after the evening meal for 6 months | Ameliorate ulcerative colitis remission in patients with ulcerative colitis | Clinical trial (89 Subjects) | Hanai H et al. 2006 [39] |
| Curcumin | 550 mg of curcumin twice daily for 1 month and then 550 mg three times daily for another month. | Reductions in concomitant medications Crohn’s disease | Clinical trial (5 Subjects) | Holt PRet al. 2005 [49] |
| Curcumin | Concentrations 10–30 μM | Ameliorate Inflammatory bowel disease: dose-dependent suppression of metalloproteinase-3 in colonic myofibroblasts from children and adults with active IBD | In vitro | Epstein J et al. 2010 [50] |
| Curcumin | Dose: 75 mg/kg/day orally daily for 6 weeks | Liver protective: prevents chronic alcohol-induced liver disease involving decreasing ROS generation and enhancing antioxidative capacity | Animal model | Rong S et al. 2012 [51] |
| Curcumin | Dose: 150 mg/kg, orally daily for 6 weeks | Liver protective: by inhibition of oxidative stress via mitogen-activated protein kinase/nuclear factor E2-related factor 2 | Animal model | Xiong ZE et al. 2015 [52] |
| Curcumin | Dose: 150 mg/kg, orally daily for 8 weeks | Liver protective: prevention of the oxidative stress induced by chronic alcohol | Animal model | Varatharajalu R et al. 2016 [53] |
| Curcumin | Dose: 70 mg/kg, orally daily for 8 weeks | Liver protective: improvement of different features of Non-alcoholic fatty liver disease after a short-term supplementation | Clinical trial (80 Subjects) | Rahmani S et al. 2016 [54] |
| Curcumin | Curcumin (2%) diet from 4 to 18 weeks of age | Intestine protective: beneficial effects of dietary curcumin on intestinal tumorigenesis in rodent models of colon cancer. | Animal model | Murphy E.A et al. 2011 [55] |
| Curcumin | Dose: 50 mg/kg, orally daily for 10 | Inflammatory bowel disease: beneficial effects in experimental colitis and may, therefore, be useful in the treatment of IBD. | Animal model | Ukil A et al. 2003 [56] |
| Curcumin | Curcumin (2%) diet from 9 days | ulcerative colitis: dietary curcumin may be of different value for Crohn’s disease and ulcerative colitis. | Animal model | Billerey-Larmonier C et al. 2008 [57] |
2.3. Cardiovascular Protective Effect of Curcumin
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin | Dose: 25–50–100–200 mg/kg, orally daily for 10 days | Cardioprotective: curcumin (50 mg/kg) with piperine (20 mg/kg) exhibited profound cardioprotection compared to curcumin (200 mg/kg) alone-treated group. | Animal model | Chakraborty M et al. 2017 [67] |
| Curcumin | Dose: 120 mg/kg, orally daily for 67 days | Cardioprotective: through direct antioxidant effects and indirect strategies that could be related to protein kinase C-activated downstream signaling. | Animal model | Correa F et al. 2013 [68] |
| Curcumin | Dose: 200 mg/kg, orally daily for 4 weeks | Cardioprotective: cardioprotective effect could be attributed to antioxidant. | Animal model | Swamy AV et al. 2012 [69] |
| Curcumin | Dose: curcumin (100 mg/kg) plus piperine (5 mg/kg) orally daily for 4 weeks | Anti-hypercholesterolemia: co-administration of curcumin plus piperine increasing the activity and gene expression of ApoAI, CYP7A1, LCAT, and LDLR, providing a promising combination for the treatment of hyperlipidemia. | Animal model | Tu Y et al. 2014 [70] |
| Curcumin | Dose: curcumin 100 mg/kg orally daily for 6 weeks | Cardioprotective: concomitant co-administration of curcumin and metformin revealed more protection than metformin alone through Inhibition of JAK/STAT pathway and activation of Nrf2/HO-1 pathway | Animal model | Abdelsamia E.M et al. 2019 [71] |
| Curcumin nanoparticle: curcumin and nisin based poly lactic acid nanoparticle (CurNisNp) | Dose: 10 and 21 mg/kg injection daily for 7 days | Cardioprotective: curcumin nanoparticle confers a significant level of cardioprotection in the guinea pig and is nontoxic. | Animal model | Nabofa W.E.E et al. 2018 [72] |
| Curcumin | Dose: curcumin 100 mg/kg orally daily for 24 days | Cardioprotective: Curcumin improve the heart function and structural changes in doxorubicin-treated rats | Animal model | Jafarinezhad Z et al. 2019 [73] |
| Curcumin nanoparticle | Dose: 100–150 mg/kg orally daily for 15 days | Cardioprotective: curcumin nanoparticles exert better antioxidative effects on MI compared to conventional curcumin, thus improving myocardial function more effectively and limiting the extension of heart damage. | Animal model | Boarescu PM, et al. 2019 [74] |
| Curcumin | Dose: 100 mg/kg orally daily for 7 days | Cardioprotective: protects against myocardial infarction-induced cardiac fibrosis via SIRT1 activation | In vitro and in vivo | Xiao J et al. 2016 [75] |
| Curcuminoids | Dose: 4 g orally daily for 8 days | Cardioprotective: significantly decreased MI associated with coronary artery bypass grafting through the antioxidant and anti-inflammatory effects | Clinical trial (121 Subjects) | Wongcharoen W et al. 2014 [76] |
| Curcumin | Concentration: 5 μmol/L | Vascular protective: effectively reverses the endothelial dysfunction induced by homocysteine | In vitro | Ramaswami G et al. 2004 [77] |
| Curcumin | Curcumin (0.05-g/100-g diet) for 10 weeks | Anti-hyperlipidemia: curcumin exhibits an obvious hypolipidemic effect by increasing plasma paraoxonase activity, ratios of high-density lipoprotein cholesterol to total cholesterol and of apo A-I to apo B, and hepatic fatty acid oxidation activity with simultaneous inhibition of hepatic fatty acid and cholesterol biosynthesis in high-fat–fed hamsters. | Animal model | Jang EM et al. 2008 [78] |
| Curcumin | Curcumin (0.02% w/w diet) for 18 weeks | Anti-atherogenic: Long-term curcumin treatment lowers plasma and hepatic cholesterol and suppresses early atherosclerotic lesions comparable to the protective effects of lovastatin. | Animal model | Shin S.K et al. 2011 [79] |
| Curcumin extract: hydro-alcoholic extract of rhyzome of C. longa containing ∼10 mg of curcumin | Dose: 20 mg orally daily for 30 days | Anti-hyperlipidemia: decreases significantly the LDL and apo B and increases the HDL and apo A of healthy subjects | Clinical trial (30 Subjects) | Ramírez-Boscá A et al. 2000 [80] |
2.4. Anti-Cancer Effect of Curcumin
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin | Concentration 15 µM | Prostate cancer. chronic inflammation can induce a metastasis prone phenotype in prostate cancer cells: Curcumin disrupts this feedback loop by the inhibition of NFκB signaling | In vitro | Killian PH et al. 2012 [89] |
| Curcumin | Concentration 50 µM for 1–4 h | Colon cancer: curcumin is an activator of PTPN1 and can reduce cell motility in colon cancer via dephosphorylation of pTyr(421)-CTTN, which could be exploited for novel therapeutic approaches in colon cancer | In vitro | Radhakrishnan VM et al. 2014 [90] |
| Curcumin or tetrahydrocurcumin (THC) | Curcumin: 300 mg/kg THC: 3000 mg/kg for 21 days | Anti-cancer: anti-angiogenic properties of Curcumin and THC represent a common potential mechanism for their anti-cancer actions. | Animal model | Yoysungnoen P et al. 2008 [91] |
| Curcumin | Concentration 0–20 μM | Breast cancer: curcumin suppresses chemokine-like ECM-associated protein osteopontin-induced VEGF expression and tumor angiogenesis | In vitro | Chakraborty G et al. 2008 [92] |
| Curcumin | Concentration 3.12–50 µM | ovarian and endometrial cancers: curcumin suppresses JAK-STAT signaling via activation of PIAS-3, thus attenuating STAT-3 phosphorylation and tumor cell growth. | In vitro | Saydmohammed M et al. 2010 [93] |
| Curcumin | Concentration 20–40 µM | Liver cancer: suppresses migration and proliferation of Hep3B hepatocarcinoma cells through inhibition of the Wnt signaling pathway | In vitro | Kim HJ et al. 2013 [94] |
| Curcumin | Concentration (2, 20, and 50 μM) for 4 h | Burkitt’s lymphoma: curcumin might play an important role in radiotherapy of high-grade non-Hodgkin’s lymphoma through inhibition of the PI3K/AKT-dependent NF-κB pathway. | In vitro | Qiao Q et al. 2013 [95] |
| Curcumin | Concentration 0–20 μg/mL for 24 h | Osteosarcoma: curcumin caused death of HOS cells by blocking cells successively in G(1)/S and G(2)/M phases and activating the caspase-3 pathway | In vitro | Lee DS et al. 2009 [96] |
| Curcumin | Concentration 4–10 µM for 24 h | Glioma: curcumin exerts inhibitory action on glioma cell growth and proliferation through induction of cell cycle arrest | In vitro | Liu E et al. 2007 [97] |
| Curcumin | Concentration 10, 25 µM for 24 h | Breast cancer: Curcumin induces apoptosis in human breast cancer cells through p53-dependent Bax induction | In vitro | Choudhuri T et al. 2002 [98] |
| Curcumin | Concentration 0 to 20 μM for 24 h | Gastric carcinoma: curcumin inhibited the growth of the AGS cells and induced apoptosis | In vitro | Cao AL et al. 2015 [99] |
| Curcumin | Concentration 0 to 100 μM for 72 h | Adenocarcinoma: curcumin-induced growth inhibition through G2/M arrest in Ras-driven cells and by apoptosis induction in Src-driven cells, | In vitro | Ono M et al. 2013 [100] |
| Curcumin | Concentration 0 to 40 μM for 24–72 h | Colon cancer: Curcumin suppresses proliferation of colon cancer cells by targeting Cyclin-dependent kinase 2 | In vitro | Lim TG et al. 2014 [101] |
| Curcumin micelles | Concentration 0 to 100 μg/mL for 24 h | Lung cancer: mixed micelles of PF127 and GL44 significant improvement in curcumin oral bioavailability. | In vitro | Patil S et al. 2015 [102] |
| Curcuminoids | Dose: 8 caplets daily for 8 weeks. Each caplet contains 1 g curcuminoids (900 mg curcumin, 80 mg desmethoxycurcumin, and 20 mg bisdesmethoxycurcumin) | Pancreatic cancer: Oral curcumin has biological activity in some patients with pancreatic cancer. | Clinical trial (25 cases) | Dhillon N et al. 2008 [86] |
| Curcumin | Dose: 0.45 and 3.6 g daily for up to 4 months. | Colorectal cancer: a daily dose of 3.6 g of curcumin are suitable for its evaluation in the prevention of malignancies at sites other than the gastrointestinal tract. | Clinical trial (15 cases) phase I | Sharma RA et al. 2004 [85] |
2.5. Effect of Curcumin on Skin Diseases
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin | Dose: 40 mg/kg orally daily for 20 days | Psoriasis: all psoriasis indexes including ear redness, weight, thickness and lymph node weight were significantly improved | Animal model | Kang D et al. 2016 [111] |
| Turmeric tonic | Topical tonic Twice a day for 9 weeks | Psoriasis: turmeric tonic significantly reduced the erythema, scaling and induration of lesions (PASI score), and also improved the patients’ quality of life | Clinical trial (40 subjects) | Bahraini P et al. 2018 [112] |
| Curcumin nano-fiber chrysin-curcumin nano-fiber | Topical 5–7.5–10% w/w for 5, 10, 15 days | Wound healing: chrysin-curcumin-loaded nanofibers have anti-inflammatory properties in several stages of the wound-healing process by affecting the IL-6, MMP-2, TIMP-1, TIMP-2, and iNOS gene expression. | Animal model | Mohammadi Z et al. 2019 [113] |
| Curcumin nanocapsule | Dose: 6 mg/kg, intra-peritoneally, twice a week for 21 days | Skin cancer: curcumin caused significant reduction of cell viability in a concentration- and time-dependent manner. | Animal model | Mazzarino L et al. 2011 [114] |
| Curcumin | Concentration 0 to 20 μM for 6, 12 h | Skin cancer, melanoma: curcumin-induced cell death and apoptosis | In vitro | Yu T et al. 2010 [115] |
2.6. Neuroprotective Effect of Curcumin
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin a natural dietary supplement (NDS), containing extracts from Curcuma longa, silymarin, guggul, chlorogenic acid, and inulin | Dose: daily administration of NDS (0.9 mg/mouse) for 16 weeks | Neuroprotective: NDS exerts neuroprotective effects in high fat diet-fed mice by reducing brain fat accumulation, oxidative stress and inflammation, and improving brain insulin resistance. | Animal model | Nuzzo D et al. 2018 [128] |
| Curcuminoids | Concentration 0.1–30 μM few minutes before addition to artificial cerebrospinal fluid for the perfusion | Neuroprotective: curcuminoids can restore susceptibility for plastic changes in CA1 excitability that is injured by exposure to Aβ peptide and rescue sinking PS LTP in A β-peptide-exposed hippocampal CA1 neurons. | In vitro | Ahmed Tet al. 2011 [129] |
| Curcumin | Concentration 0–8 μM | Alzheimer’s Disease: curcumin effectively disaggregates Abeta as well as prevents fibril and oligomer formation | Animal model | Yang F et al. 2005 [130] |
| Curcuminoids | Concentration 10 μM | Alzheimer’s Disease: curcumin binds to Aβ oligomers and to Aβ fibrils | In vitro | Yanagisawa D et al. 2011 [131] |
| Curcumin | Concentration 0–30 μM | Alzheimer’s Disease: curcumin significantly attenuated β amyloid-induced radical oxygen species production and β-sheet structure formation. | In vitro | Shimmyo Y et al. 2008 [132] |
| Curcumin | Concentration 0–10 μM | Alzheimer’s Disease: curcumin downregulated the expression of amyloid precursor protein and amyloid-β in swAPP695-HEK293 cells, which was through miR-15b-5p | In vitro | Liu HY et al. 2019 [133] |
| Curcuminoids | Dose: 3–30 mg/kg | Alzheimer’s Disease: increased PSD-95, synaptophysin and camkIV expression levels in the hippocampus in the rat AD model | Animal model | Ahmed T et al. 2010 [134] |
| Ethanolic extract of turmeric | Dose: 80 mg/kg orally, daily for three weeks | Alzheimer’s Disease: effectively prevented cognitive deficits | Animal model | Ishrat T et al. 2009 [135] |
| Curcumin C3 Complex(®) an extract derived from the rhizomes (roots) of the plant Curcuma longa | Dose: 2, 4 g/day, orally for 24 weeks. | Alzheimer’s Disease: Results were unable to demonstrate clinical or biochemical evidence of efficacy of this formulation. | Clinical trial (36 Subjects) | Ringman JM et al. 2012 [136] |
| Tumeric powder capsules | Dose: 764 mg/day turmeric (100 mg/day curcumin) orally for 12 weeks | Alzheimer’s Disease: a significant improvement of the behavioral symptoms in the AD with the turmeric treatment, | Clinical trial (3 Subjects) | Hishikawa N et al. 2012 [137] |
| Curcumin | Concentration 0–1 μM | Parkinson’s Disease: Curcumin protected brain mitochondria against peroxynitrite by direct detoxification and inhibition of 3-nitrotyrosine formation and by elevation of total cellular glutathione levels in vivo | In vitro | Mythri RB et al. 2007 [138] |
| Curcumin nanoparticle polymeric nanoparticle encapsulated curcumin | In vitro: (1, 10, 50, 100, 500 nM, 1, 5 μM) In vivo: 25 mg/kg intraperitoneally twice daily for 4 weeks | Alzheimer’s Disease: NanoCurc™ ameliorated ROS-mediated damage in both cell culture and in animal models | Animal model/In vitro | Ray B et al. 2011 [139] |
| Curcumin | Concentration 0–10 μM for 24 h | Neuroprotection: curcumin enhanced neuronal survival against NMDA toxicity | In vitro | Lin MS et al. 2011 [140] |
| Curcumin | diet of 500 ppm curcumin for 4 weeks | Traumatic brain injury (TBI): curcumin reduced oxidative damage, normalized levels of BDNF, synapsin I, and CREB and counteracted the cognitive impairment caused by TBI. | Animal model | Wu A et al. 2006 [141] |
| Curcumin | Dose: 1.25, 2.5, 5, 10 mg/kg, intraperitoneally daily single dose | Depression: exerts antidepressant-like effects through the central monoaminergic neurotransmitter systems. | Animal model | Xu Y et al. 2005 [142] |
| Curcumin | Dose: 200 mg/kg, intraperitoneally daily for 7 days. | Brain ischemia: curcumin attenuated forebrain ischemia-induced neuronal injury and oxidative stress in hippocampal tissue. | Animal model | Al-Omar FA et al. 2006 [143] |
| Curcumin | Dose: 100, 200, 300 mg/kg, Orally, single dose | Epilepsy: Curcumin (300 mg/kg) significantly increased the latency to myoclonic jerks, clonic seizures as well as generalized tonic–clonic seizures and reduced oxidative stress and cognitive impairment | Animal model | Mehla J et al. 2010 [144] |
| Curcumin | Dose: 50 mg/kg, Orally, daily for 4 days | Parkinson’s Disease: curcumin protects the tyrosine hydroxylase-positive cells in the substantia nigra and dopamine levels in the striatum through its antioxidant capabilities | Animal model | Zbarsky V et al. 2005 [145] |
| Curcumin | Concentration 0–25 μM for 24 h | Parkinson’s Disease: these protective effects are attributed to the antioxidative properties also modulation of nuclear factor kappaB translocation. | In vitro | Wang J et al. 2009 [146] |
| Curcumin/its metabolite | Dose: 80 mg/kg, intraperitoneally, daily for 7 days | Parkinson’s Disease: curcumin and tetrahydrocurcumin reversed the MPTP induced depletion of dopamine and DOPAC through inhibition of MAO-B activity. | Animal model | Rajeswari A et al. 2008 [147] |
| Curcumin | Concentration 4 μM for 48 h | Parkinson’s Disease: curcumin could alleviate α-synuclein-induced toxicity, decreased ROS levels and protected cells against apoptosis. | In vitro | Wang MS et al. 2010 [148] |
| Curcumin | Concentration 0–1 μM for 2 times changing in 6 days treatment | Parkinson’s Disease: curcumin protects cells against A53T mutant α-synuclein-induced cell death through prevention of oxidative stress and the mitochondrial rescue | In vitro | Liu Zet al. 2011 [123] |
| Manganese complexes of curcumin | In vitro: 0–5 μg/mL for 3 h In vivo: 3 times (50 mg/kg × 3) at time points 1, 3, and 7 h post first MPTP sc injection, intraperitoneally | Neuroprotection: treatment with this complex attenuated MPTP-induced striatal dopamine depletion significantly | Animal model/In vitro | Vajragupta O et al. 2003 [149] |
2.7. Protective Effect of Curcumin in Eye Diseases
3. Cellular and Molecular Targets of Curcumin
4. Curcumin Metabolism and Degradation
5. Curcumin Toxicity
6. Pharmacokinetic Deficiency of Curcumin and Current Attempts
| Product | Species | Route of Administration | Dose | Plasma/Tissue Level (Cmax) | Time to Maximum Concentration (Tmax) min | Ref. |
|---|---|---|---|---|---|---|
| Curcuminoids | Rat | Oral | 500 mg/kg | 0.06 µg/mL | 41.7 | [234] |
| Curcumin | Rat | Oral | 200 mg/kg | 1.2 µg/mL | no | [235] |
| Curcumin & Curcumin phospholipid complex (Meriva) | Rat | Oral | 340 mg/kg | 6.5 nM & 33.4 nM | 30 & 15 | [236] |
| Curcuminoids | Human | Oral | 450–3600 mg | 10 nM/g tissue | No data | [237] |
| Curcumin | Human | Oral | 3600 mg | 12.7 nmol/g tissue | No data | [238] |
| Curcuminoids | Rat | Oral | 100 mg/kg | trace | 60 | [239] |
| Curcumin | Rat | Oral | 400 mg | trace | No data | [209] |
| Curcumin | Mouse | Intraperitoneal | 100 mg/kg | trace | No data | [240] |
| Curcumin | Human | Oral | 3600 mg | 10 nM | No data | [85] |
| Curcumin | Human | Oral | 1200 mg | 51 ng/mL | No data | [196] |
| Curcumin | In vitro | Exposure | 5–75 µg/mL | 3% in tissue | No data | [241] |
| Curcumin | Rat | Oral | 10, 80, 400 mg | 65–66% | No data | [242] |
| Curcuma extract | Human | Oral | 440 and 2200 mg/day | 175 to 310 μg/L | No data | [199] |
| Phospholipid formulation | Human | Oral | 200−300 mg | 50 ng/mL | 240 | [225] |
| Solid lipid curcumin particle | Human | Oral | 650 mg | 22.43 ng/mL | 160 | [227] |
| Curcumin-impregnated soluble dietary fiber dispersions | Human | Oral | 600 mg | 0.37 μg/g tissue | 60 | [243] |
| Micronized formulation | Human | Oral | 500 mg | 0.60 μg/mL | No data | [229] |
| Micronized formulation | Human | Oral | 500 mg | 50.6 nM | 460 | [232] |
| Liquid micelles formulation | Human | Oral | 500 mg | 3701 nM | 66 | [232] |
| Curcumin/piperine co-administration | Rat | Oral | Curcumin 2 g/kg piperine 20 mg/kg | 1.55 µg/mL | 120 | [231] |
| Lipophilic matrix | Human | Oral | 376 mg | 18 ng/mL | 60 | [244] |
| γ-cyclodextrin complex | Human | Oral | 376 mg | 87 ng/mL | 60 | [244] |
| Colloidal nanoparticle | Human | Oral | 30 mg | 29.5 ng/mL | 60 | [233] |
| Curcumin | Rat | Intravenous | 40 mg/kg | No data | No data | [245] |
| BCM-95® CG A patent formulation | Human | Oral | 2000 mg | 456.88 ng/g tissue | 206 | [246] |
7. Conclusions and Future Prospects
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AH R | Aryl hydrocarbon receptor |
| AD | Alzheimer’s disease |
| AP-1 | Activator protein 1 |
| Bax | Bcl-2-associated X protein |
| BDNF | Brain-derived neurotrophic factor |
| CDPK | Calcium-dependent protein kinases |
| CRDB | Curcumin Resource Database |
| CREB | cAMP response element-binding protein |
| COX-2 | Cyclooxygenase-2 |
| CT | Clinical Trial |
| CXCR 4 | C-X-C Motif Chemokine Receptor 4 |
| EGF | Epidermal growth factor |
| ER-alfa | Estrogen receptor alfa |
| ERK | Extracellular signal-regulated kinases |
| FADD | Fas Associated via death domain |
| FAK | Focal adhesion kinase |
| FAS | Fas cell surface death receptor |
| FGF | Fibroblast growth factors |
| GST | Glutathione-S-transferase |
| HAT | Histone acetylase |
| H2 R | Histamine H2 receptor |
| HDAC | Histone deacetylase |
| HGF | Hepatocyte growth factor |
| HMG-CoA-R | 3-hydroxy-3-methyl-glutaryl-CoA reductase |
| HSP-70 | Heat shock protein 70 |
| IBD | Intestinal inflammatory diseases |
| ICAMs | Intercellular cell adhesion molecules |
| IL | Interleukin |
| iNOS | Inducible nitric oxide synthase |
| JAK | Janus kinase |
| JNK | c-Jun N-terminal kinases |
| LDL R | Low-Density Lipoprotein Receptor |
| MCP-1 | Monocyte chemoattractant protein-1 |
| MIP-1α | Macrophage inflammatory proteins |
| MMP | Matrix metallopeptidases |
| MRP | Multidrug resistance-associated protein |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| NFκB | Nuclear Factor kappa-light-chain-enhancer of ctivated B cells |
| NGF | Nerve growth factor |
| Nrf2 | Nuclear factor erythroid 2–related factor 2 |
| NuBACS | Nutraceutical Bioavailability Classification cheme |
| P38-MAPK | P38 mitogen-activated protein kinases |
| PD | Parkinson’s disease |
| PDGF | Platelet-derived growth factor |
| P-gp | P-glycoprotein |
| PhK | Phosphorylase kinase |
| PKA | Protein kinase A |
| PLA2 | Phospholipase A2 |
| PPAR-gamma | Peroxisome proliferator-activated receptor amma |
| ROS | Reactive oxygen species |
| RNS | Reactive nitrogen species |
| SLP | Solid lipid particle |
| STAT | Signal transducer and activator of transcription |
| SyK | Spleen tyrosine kinase |
| TF | Tissue factor |
| TGF-α | Transforming growth factor alpha |
| TGF-β | Transforming growth factor beta |
| TLR | Toll-like receptors |
| TNF-α | Tumor necrosis factor alpha |
| UGT | Uridine diphosphate-glucuronosyltransferase |
| VCAM | Vascular cell adhesion molecule |
| XO | Xanthine oxidase |
| 5-LOX | 5-Lipoxygenase |
References
- Aggarwal, B.B.; Sundaram, C.; Malani, N.; Ichikawa, H. Curcumin: The Indian solid gold. Adv. Exp. Med. Biol. 2007, 595, 1–75. [Google Scholar] [CrossRef] [PubMed]
- Bigford, G.E.; Del Rossi, G. Supplemental substances derived from foods as adjunctive therapeutic agents for treatment of neurodegenerative diseases and disorders. Adv. Nutr. 2014, 5, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Lampe, V.; Milobedzka, J. Studien über Curcumin. Berichte Dtsch. Chem. Ges. 1913, 46, 2235–2240. [Google Scholar] [CrossRef]
- Kunnumakkara, A.B.; Bordoloi, D.; Padmavathi, G.; Monisha, J.; Roy, N.K.; Prasad, S.; Aggarwal, B.B. Curcumin, the golden nutraceutical: Multitargeting for multiple chronic diseases. Br. J. Pharmacol. 2017, 174, 1325–1348. [Google Scholar] [CrossRef]
- Daybe, F.V. Uber Curcumin. Den Farbstoff der Curcumawurzzel Ber 1870, 3, 609. [Google Scholar]
- Govindarajan, V.S. Turmeric—Chemistry, technology, and quality. Crit. Rev. Food Sci. Nutr. 1980, 12, 199–301. [Google Scholar] [CrossRef]
- Kumar, A.; Chetia, H.; Sharma, S.; Kabiraj, D.; Talukdar, N.C.; Bora, U. Curcumin Resource Database. Database J. Biol. Databases Curation 2015, 2015, bav070. [Google Scholar] [CrossRef][Green Version]
- Mishra, B.; Priyadarsini, K.I.; Bhide, M.K.; Kadam, R.M.; Mohan, H. Reactions of superoxide radicals with curcumin: Probable mechanisms by optical spectroscopy and EPR. Free Radic. Res. 2004, 38, 355–362. [Google Scholar] [CrossRef]
- Trujillo, J.; Chirino, Y.I.; Molina-Jijón, E.; Andérica-Romero, A.C.; Tapia, E.; Pedraza-Chaverrí, J. Renoprotective effect of the antioxidant curcumin: Recent findings. Redox Biol. 2013, 1, 448–456. [Google Scholar] [CrossRef]
- Liu, Z.-J.; Liu, H.-Q.; Xiao, C.; Fan, H.-Z.; Huang, Q.; Liu, Y.-H.; Wang, Y. Curcumin protects neurons against oxygen-glucose deprivation/reoxygenation-induced injury through activation of peroxisome proliferator-activated receptor-γ function. J. Neurosci. Res. 2014, 92, 1549–1559. [Google Scholar] [CrossRef]
- Reddy, P.H.; Manczak, M.; Yin, X.; Grady, M.C.; Mitchell, A.; Kandimalla, R.; Kuruva, C.S. Protective effects of a natural product, curcumin, against amyloid β induced mitochondrial and synaptic toxicities in Alzheimer’s disease. J. Investig. Med. 2016, 64, 1220–1234. [Google Scholar] [CrossRef] [PubMed]
- Motaghinejad, M.; Motevalian, M.; Fatima, S.; Hashemi, H.; Gholami, M. Curcumin confers neuroprotection against alcohol-induced hippocampal neurodegeneration via CREB-BDNF pathway in rats. Biomed. Pharmacother. Biomed. Pharmacother. 2017, 87, 721–740. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Sun, A.Y.; Simonyi, A.; Jensen, M.D.; Shelat, P.B.; Rottinghaus, G.E.; MacDonald, R.S.; Miller, D.K.; Lubahn, D.E.; Weisman, G.A.; et al. Neuroprotective mechanisms of curcumin against cerebral ischemia-induced neuronal apoptosis and behavioral deficits. J. Neurosci. Res. 2005, 82, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Tang, X.Q.; Zhi, J.L.; Cui, Y.; Yu, H.M.; Tang, E.H.; Sun, S.N.; Feng, J.Q.; Chen, P.X. Curcumin protects PC12 cells against 1-methyl-4-phenylpyridinium ion-induced apoptosis by bcl-2-mitochondria-ROS-iNOS pathway. Apoptosis Int. J. Program. Cell Death 2006, 11, 943–953. [Google Scholar] [CrossRef]
- Zorofchian Moghadamtousi, S.; Abdul Kadir, H.; Hassandarvish, P.; Tajik, H.; Abubakar, S.; Zandi, K. A Review on Antibacterial, Antiviral, and Antifungal Activity of Curcumin. Available online: https://www.hindawi.com/journals/bmri/2014/186864/ (accessed on 13 April 2020).
- Mathew, D.; Hsu, W.-L. Antiviral potential of curcumin. J. Funct. Foods 2018, 40, 692–699. [Google Scholar] [CrossRef]
- Shlar, I.; Droby, S.; Choudhary, R.; Rodov, V. The mode of antimicrobial action of curcumin depends on the delivery system: Monolithic nanoparticles vs. supramolecular inclusion complex. RSC Adv. 2017, 7, 42559–42569. [Google Scholar] [CrossRef]
- Kiuchi, F.; Goto, Y.; Sugimoto, N.; Akao, N.; Kondo, K.; Tsuda, Y. Nematocidal activity of turmeric: Synergistic action of curcuminoids. Chem. Pharm. Bull. 1993, 41, 1640–1643. [Google Scholar] [CrossRef] [PubMed]
- Sui, Z.; Salto, R.; Li, J.; Craik, C.; Ortiz de Montellano, P.R. Inhibition of the HIV-1 and HIV-2 proteases by curcumin and curcumin boron complexes. Bioorg. Med. Chem. 1993, 1, 415–422. [Google Scholar] [CrossRef]
- Tantaoui-Elaraki, A.; Beraoud, L. Inhibition of growth and aflatoxin production in Aspergillus parasiticus by essential oils of selected plant materials. J. Environ. Pathol. Toxicol. Oncol. Off. Organ Int. Soc. Environ. Toxicol. Cancer 1994, 13, 67–72. [Google Scholar]
- Jordan, W.C.; Drew, C.R. Curcumin—A natural herb with anti-HIV activity. J. Natl. Med. Assoc. 1996, 88, 333. [Google Scholar]
- Roth, G.N.; Chandra, A.; Nair, M.G. Novel bioactivities of Curcuma longa constituents. J. Nat. Prod. 1998, 61, 542–545. [Google Scholar] [CrossRef]
- Negi, P.S.; Jayaprakasha, G.K.; Jagan Mohan Rao, L.; Sakariah, K.K. Antibacterial activity of turmeric oil: A byproduct from curcumin manufacture. J. Agric. Food Chem. 1999, 47, 4297–4300. [Google Scholar] [CrossRef] [PubMed]
- Koide, T.; Nose, M.; Ogihara, Y.; Yabu, Y.; Ohta, N. Leishmanicidal effect of curcumin in vitro. Biol. Pharm. Bull. 2002, 25, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-K.; Choi, G.-J.; Lee, H.-S. Fungicidal property of Curcuma longa L. rhizome-derived curcumin against phytopathogenic fungi in a greenhouse. J. Agric. Food Chem. 2003, 51, 1578–1581. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.C.; Vatsala, P.G.; Keshamouni, V.G.; Padmanaban, G.; Rangarajan, P.N. Curcumin for malaria therapy. Biochem. Biophys. Res. Commun. 2005, 326, 472–474. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Arriaga, L.; Mendoza-Magaña, M.L.; Cortés-Zárate, R.; Corona-Rivera, A.; Bobadilla-Morales, L.; Troyo-Sanromán, R.; Ramírez-Herrera, M.A. Cytotoxic effect of curcumin on Giardia lamblia trophozoites. Acta Trop. 2006, 98, 152–161. [Google Scholar] [CrossRef]
- Di Mario, F.; Cavallaro, L.G.; Nouvenne, A.; Stefani, N.; Cavestro, G.M.; Iori, V.; Maino, M.; Comparato, G.; Fanigliulo, L.; Morana, E.; et al. A curcumin-based 1-week triple therapy for eradication of Helicobacter pylori infection: Something to learn from failure? Helicobacter 2007, 12, 238–243. [Google Scholar] [CrossRef]
- Cai, T.; Mazzoli, S.; Bechi, A.; Addonisio, P.; Mondaini, N.; Pagliai, R.C.; Bartoletti, R. Serenoa repens associated with Urtica dioica (ProstaMEV) and curcumin and quercitin (FlogMEV) extracts are able to improve the efficacy of prulifloxacin in bacterial prostatitis patients: Results from a prospective randomised study. Int. J. Antimicrob. Agents 2009, 33, 549–553. [Google Scholar] [CrossRef]
- Trigo Gutierrez, J.K.; Zanatta, G.C.; Ortega, A.L.M.; Balastegui, M.I.C.; Sanitá, P.V.; Pavarina, A.C.; Barbugli, P.A.; de Mima, E.G.O. Encapsulation of curcumin in polymeric nanoparticles for antimicrobial Photodynamic Therapy. PLoS ONE 2017, 12, e0187418. [Google Scholar] [CrossRef]
- Fakhrullina, G.; Khakimova, E.; Akhatova, F.; Lazzara, G.; Parisi, F.; Fakhrullin, R. Selective Antimicrobial Effects of Curcumin@Halloysite Nanoformulation: A Caenorhabditis elegans Study. ACS Appl. Mater. Interfaces 2019, 11, 23050–23064. [Google Scholar] [CrossRef]
- Jaiswal, S.; Mishra, P. Antimicrobial and antibiofilm activity of curcumin-silver nanoparticles with improved stability and selective toxicity to bacteria over mammalian cells. Med. Microbiol. Immunol. 2018, 207, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, G.; Sodhi, R.K.; Jain, U.K.; Chandra, R.; Madan, J. Iodinated curcumin bearing dermal cream augmented drug delivery, antimicrobial and antioxidant activities. J. Microencapsul. 2018, 35, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L. The Problem of Curcumin and Its Bioavailability: Could Its Gastrointestinal Influence Contribute to Its Overall Health-Enhancing Effects? Adv. Nutr. 2018, 9, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Farzaei, M.H.; Zobeiri, M.; Parvizi, F.; El-Senduny, F.F.; Marmouzi, I.; Coy-Barrera, E.; Naseri, R.; Nabavi, S.M.; Rahimi, R.; Abdollahi, M. Curcumin in Liver Diseases: A Systematic Review of the Cellular Mechanisms of Oxidative Stress and Clinical Perspective. Nutrients 2018, 10, 855. [Google Scholar] [CrossRef] [PubMed]
- Villegas, I.; Sánchez-Fidalgo, S.; de la Lastra, C.A. Chemopreventive effect of dietary curcumin on inflammation-induced colorectal carcinogenesis in mice. Mol. Nutr. Food Res. 2011, 55, 259–267. [Google Scholar] [CrossRef]
- Larmonier, C.B.; Uno, J.K.; Lee, K.-M.; Karrasch, T.; Laubitz, D.; Thurston, R.; Midura-Kiela, M.T.; Ghishan, F.K.; Sartor, R.B.; Jobin, C.; et al. Limited effects of dietary curcumin on Th-1 driven colitis in IL-10 deficient mice suggest an IL-10-dependent mechanism of protection. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 295, G1079–G1091. [Google Scholar] [CrossRef]
- Larmonier, C.B.; Midura-Kiela, M.T.; Ramalingam, R.; Laubitz, D.; Janikashvili, N.; Larmonier, N.; Ghishan, F.K.; Kiela, P.R. Modulation of neutrophil motility by curcuminImplications for inflammatory bowel disease. Inflamm. Bowel Dis. 2011, 17, 503–515. [Google Scholar] [CrossRef]
- Hanai, H.; Iida, T.; Takeuchi, K.; Watanabe, F.; Maruyama, Y.; Andoh, A.; Tsujikawa, T.; Fujiyama, Y.; Mitsuyama, K.; Sata, M.; et al. Curcumin maintenance therapy for ulcerative colitis: Randomized, multicenter, double-blind, placebo-controlled trial. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2006, 4, 1502–1506. [Google Scholar] [CrossRef]
- Durgaprasad, S.; Pai, C.G.; Vasanthkumar, N.; Alvres, J.F.; Namitha, S. A pilot study of the antioxidant effect of curcumin in tropical pancreatitis. Indian J. Med. Res. 2005, 122, 315–318. [Google Scholar]
- Burge, K.; Gunasekaran, A.; Eckert, J.; Chaaban, H. Curcumin and Intestinal Inflammatory Diseases: Molecular Mechanisms of Protection. Int. J. Mol. Sci. 2019, 20, 1912. [Google Scholar] [CrossRef]
- Shen, L.; Liu, L.; Ji, H.-F. Regulative effects of curcumin spice administration on gut microbiota and its pharmacological implications. Food Nutr. Res. 2017, 61, 1361780. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Wang, H.; Zhang, P.; Gao, C.; Tao, J.; Ge, Z.; Zhu, D.; Bi, Y. Modulation of gut microbiota contributes to curcumin-mediated attenuation of hepatic steatosis in rats. Biochim. Biophys. Acta Gen. Subj. 2017, 1861, 1801–1812. [Google Scholar] [CrossRef] [PubMed]
- Maslowski, K.M.; Vieira, A.T.; Ng, A.; Kranich, J.; Sierro, F.; Yu, D.; Schilter, H.C.; Rolph, M.S.; Mackay, F.; Artis, D.; et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 2009, 461, 1282–1286. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, C.; Cavalieri, D.; Di Paola, M.; Ramazzotti, M.; Poullet, J.B.; Massart, S.; Collini, S.; Pieraccini, G.; Lionetti, P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 2010, 107, 14691–14696. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Chen, A. Curcumin protects hepatic stellate cells against leptin-induced activation in vitro by accumulating intracellular lipids. Endocrinology 2010, 151, 4168–4177. [Google Scholar] [CrossRef]
- Vizzutti, F.; Provenzano, A.; Galastri, S.; Milani, S.; Delogu, W.; Novo, E.; Caligiuri, A.; Zamara, E.; Arena, U.; Laffi, G.; et al. Curcumin limits the fibrogenic evolution of experimental steatohepatitis. Lab. Investig. J. Tech. Methods Pathol. 2010, 90, 104–115. [Google Scholar] [CrossRef]
- Bruck, R.; Ashkenazi, M.; Weiss, S.; Goldiner, I.; Shapiro, H.; Aeed, H.; Genina, O.; Helpern, Z.; Pines, M. Prevention of liver cirrhosis in rats by curcumin. Liver Int. Off. J. Int. Assoc. Study Liver 2007, 27, 373–383. [Google Scholar] [CrossRef]
- Holt, P.R.; Katz, S.; Kirshoff, R. Curcumin therapy in inflammatory bowel disease: A pilot study. Dig. Dis. Sci. 2005, 50, 2191–2193. [Google Scholar] [CrossRef]
- Epstein, J.; Docena, G.; MacDonald, T.T.; Sanderson, I.R. Curcumin suppresses p38 mitogen-activated protein kinase activation, reduces IL-1beta and matrix metalloproteinase-3 and enhances IL-10 in the mucosa of children and adults with inflammatory bowel disease. Br. J. Nutr. 2010, 103, 824–832. [Google Scholar] [CrossRef]
- Rong, S.; Zhao, Y.; Bao, W.; Xiao, X.; Wang, D.; Nussler, A.K.; Yan, H.; Yao, P.; Liu, L. Curcumin prevents chronic alcohol-induced liver disease involving decreasing ROS generation and enhancing antioxidative capacity. Phytomed. Int. J. Phytother. Phytopharm. 2012, 19, 545–550. [Google Scholar] [CrossRef]
- Xiong, Z.E.; Dong, W.G.; Wang, B.Y.; Tong, Q.Y.; Li, Z.Y. Curcumin attenuates chronic ethanol-induced liver injury by inhibition of oxidative stress via mitogen-activated protein kinase/nuclear factor E2-related factor 2 pathway in mice. Pharmacogn. Mag. 2015, 11, 707–715. [Google Scholar] [CrossRef]
- Varatharajalu, R.; Garige, M.; Leckey, L.C.; Reyes-Gordillo, K.; Shah, R.; Lakshman, M.R. Protective Role of Dietary Curcumin in the Prevention of the Oxidative Stress Induced by Chronic Alcohol with respect to Hepatic Injury and Antiatherogenic Markers. Oxid. Med. Cell. Longev. 2016, 2016, 5017460. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, S.; Asgary, S.; Askari, G.; Keshvari, M.; Hatamipour, M.; Feizi, A.; Sahebkar, A. Treatment of Non-alcoholic Fatty Liver Disease with Curcumin: A Randomized Placebo-controlled Trial. Phytother. Res. PTR 2016, 30, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.A.; Davis, J.M.; McClellan, J.L.; Gordon, B.T.; Carmichael, M.D. Curcumin’s Effect on Intestinal Inflammation and Tumorigenesis in the ApcMin/+ Mouse. J. Interferon Cytokine Res. 2011, 31, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Ukil, A.; Maity, S.; Karmakar, S.; Datta, N.; Vedasiromoni, J.R.; Das, P.K. Curcumin, the major component of food flavour turmeric, reduces mucosal injury in trinitrobenzene sulphonic acid-induced colitis. Br. J. Pharmacol. 2003, 139, 209–218. [Google Scholar] [CrossRef]
- Billerey-Larmonier, C.; Uno, J.K.; Larmonier, N.; Midura, A.J.; Timmermann, B.; Ghishan, F.K.; Kiela, P.R. Protective effects of dietary curcumin in mouse model of chemically induced colitis are strain dependent. Inflamm. Bowel Dis. 2008, 14, 780–793. [Google Scholar] [CrossRef]
- Wongcharoen, W.; Phrommintikul, A. The protective role of curcumin in cardiovascular diseases. Int. J. Cardiol. 2009, 133, 145–151. [Google Scholar] [CrossRef]
- Brouet, I.; Ohshima, H. Curcumin, an Anti-tumor Promoter and Anti-inflammatory Agent, Inhibits Induction of Nitric Oxide Synthase in Activated Macrophages. Biochem. Biophys. Res. Commun. 1995, 206, 533–540. [Google Scholar] [CrossRef]
- Farhangkhoee, H.; Khan, Z.A.; Chen, S.; Chakrabarti, S. Differential effects of curcumin on vasoactive factors in the diabetic rat heart. Nutr. Metab. 2006, 3, 27. [Google Scholar] [CrossRef]
- Frey, N.; Olson, E.N. Cardiac Hypertrophy: The Good, the Bad, and the Ugly. Annu. Rev. Physiol. 2003, 65, 45–79. [Google Scholar] [CrossRef]
- Backs, J.; Olson, E.N. Control of Cardiac Growth by Histone Acetylation/Deacetylation. Circ. Res. 2006, 98, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Marcu, M.G.; Jung, Y.-J.; Lee, S.; Chung, E.-J.; Lee, M.-J.; Trepel, J.; Neckers, L. Curcumin is an Inhibitor of p300 Histone Acetylatransferase. Available online: https://www.ingentaconnect.com/content/ben/mc/2006/00000002/00000002/art00006 (accessed on 14 April 2020).
- Morimoto, T.; Sunagawa, Y.; Kawamura, T.; Takaya, T.; Wada, H.; Nagasawa, A.; Komeda, M.; Fujita, M.; Shimatsu, A.; Kita, T.; et al. The dietary compound curcumin inhibits p300 histone acetyltransferase activity and prevents heart failure in rats. J. Clin. Investig. 2008, 118, 868–878. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.-A.; Lee, S.Y.; Han, S.H.; Hong, J.; Na, J.-R.; Lee, J.Y.; Kim, Y.; Kim, S. Hypocholesterolemic effects of Curcuma longa L. with Nelumbo nucifera leaf in an in vitro model and a high cholesterol diet-induced hypercholesterolemic mouse model. Anim. Cells Syst. 2015, 19, 133–143. [Google Scholar] [CrossRef]
- Soliman, G. Effect of Curcumin, Mixture of Curcumin and Piperine and Curcum (Turmeric) on Lipid Profile of Normal and Hyperlipidemic Rats. Egypt. J. Hosp. Med. 2005, 21, 145–161. [Google Scholar] [CrossRef]
- Chakraborty, M.; Bhattacharjee, A.; Kamath, J.V. Cardioprotective effect of curcumin and piperine combination against cyclophosphamide-induced cardiotoxicity. Indian J. Pharmacol. 2017, 49, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Correa, F.; Buelna-Chontal, M.; Hernández-Reséndiz, S.; García-Niño, W.R.; Roldán, F.J.; Soto, V.; Silva-Palacios, A.; Amador, A.; Pedraza-Chaverrí, J.; Tapia, E.; et al. Curcumin maintains cardiac and mitochondrial function in chronic kidney disease. Free Radic. Biol. Med. 2013, 61, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Swamy, A.V.; Gulliaya, S.; Thippeswamy, A.; Koti, B.C.; Manjula, D.V. Cardioprotective effect of curcumin against doxorubicin-induced myocardial toxicity in albino rats. Indian J. Pharmacol. 2012, 44, 73–77. [Google Scholar] [CrossRef]
- Tu, Y.; Sun, D.; Zeng, X.; Yao, N.; Huang, X.; Huang, D.; Chen, Y. Piperine potentiates the hypocholesterolemic effect of curcumin in rats fed on a high fat diet. Exp. Ther. Med. 2014, 8, 260–266. [Google Scholar] [CrossRef]
- Abdelsamia, E.M.; Khaleel, S.A.; Balah, A.; Abdel Baky, N.A. Curcumin augments the cardioprotective effect of metformin in an experimental model of type I diabetes mellitus; Impact of Nrf2/HO-1 and JAK/STAT pathways. Biomed. Pharmacother. 2019, 109, 2136–2144. [Google Scholar] [CrossRef]
- Nabofa, W.E.E.; Alashe, O.O.; Oyeyemi, O.T.; Attah, A.F.; Oyagbemi, A.A.; Omobowale, T.O.; Adedapo, A.A.; Alada, A.R.A. Cardioprotective Effects of Curcumin-Nisin Based Poly Lactic Acid Nanoparticle on Myocardial Infarction in Guinea Pigs. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jafarinezhad, Z.; Rafati, A.; Ketabchi, F.; Noorafshan, A.; Karbalay-Doust, S. Cardioprotective effects of curcumin and carvacrol in doxorubicin-treated rats: Stereological study. Food Sci. Nutr. 2019, 7, 3581–3588. [Google Scholar] [CrossRef] [PubMed]
- Boarescu, P.-M.; Chirilă, I.; Bulboacă, A.E.; Bocșan, I.C.; Pop, R.M.; Gheban, D.; Bolboacă, S.D. Effects of Curcumin Nanoparticles in Isoproterenol-Induced Myocardial Infarction. Available online: https://www.hindawi.com/journals/omcl/2019/7847142/ (accessed on 20 December 2019).
- Xiao, J.; Sheng, X.; Zhang, X.; Guo, M.; Ji, X. Curcumin protects against myocardial infarction-induced cardiac fibrosis via SIRT1 activation in vivo and in vitro. Drug Des. Devel. Ther. 2016, 10, 1267–1277. [Google Scholar] [CrossRef] [PubMed]
- Wongcharoen, W.; Jai-aue, S.; Phrommintikul, A.; Nawarawong, W.; Woragidpoonpol, S.; Tepsuwan, T.; Sukonthasarn, A.; Apaijai, N.; Chattipakorn, N. Effects of Curcuminoids on Frequency of Acute Myocardial Infarction After Coronary Artery Bypass Grafting. Am. J. Cardiol. 2012, 110, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Ramaswami, G.; Chai, H.; Yao, Q.; Lin, P.H.; Lumsden, A.B.; Chen, C. Curcumin blocks homocysteine-induced endothelial dysfunction in porcine coronary arteries. J. Vasc. Surg. 2004, 40, 1216–1222. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.-M.; Choi, M.-S.; Jung, U.J.; Kim, M.-J.; Kim, H.-J.; Jeon, S.-M.; Shin, S.-K.; Seong, C.-N.; Lee, M.-K. Beneficial effects of curcumin on hyperlipidemia and insulin resistance in high-fat–fed hamsters. Metabolism 2008, 57, 1576–1583. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.-K.; Ha, T.-Y.; McGregor, R.A.; Choi, M.-S. Long-term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol. Nutr. Food Res. 2011, 55, 1829–1840. [Google Scholar] [CrossRef]
- Ramírez-Boscá, A.; Soler, A.; Carrión, M.A.; Díaz-Alperi, J.; Bernd, A.; Quintanilla, C.; Quintanilla, A.E.; Miquel, J. An hydroalcoholic extract of Curcuma longa lowers the apo B/apo A ratio: Implications for atherogenesis prevention. Mech. Ageing Dev. 2000, 119, 41–47. [Google Scholar] [CrossRef]
- Block, K.I.; Gyllenhaal, C.; Lowe, L.; Amedei, A.; Amin, A.R.; Amin, A.; Aquilano, K.; Arbiser, J.; Arreola, A.; Arzumanyan, A.; et al. A Broad-Spectrum Integrative Design for Cancer Prevention and Therapy. Semin. Cancer Biol. 2015, 35, S276–S304. [Google Scholar] [CrossRef]
- Mantovani, A. Molecular pathways linking inflammation and cancer. Curr. Mol. Med. 2010, 10, 369–373. [Google Scholar] [CrossRef]
- Catanzaro, M.; Corsini, E.; Rosini, M.; Racchi, M.; Lanni, C. Immunomodulators Inspired by Nature: A Review on Curcumin and Echinacea. Molecules 2018, 23, 2778. [Google Scholar] [CrossRef]
- Mohamed, S.I.A.; Jantan, I.; Haque, M.A. Naturally occurring immunomodulators with antitumor activity: An insight on their mechanisms of action. Int. Immunopharmacol. 2017, 50, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.A.; Euden, S.A.; Platton, S.L.; Cooke, D.N.; Shafayat, A.; Hewitt, H.R.; Marczylo, T.H.; Morgan, B.; Hemingway, D.; Plummer, S.M.; et al. Phase I clinical trial of oral curcumin: Biomarkers of systemic activity and compliance. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004, 10, 6847–6854. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, N.; Aggarwal, B.B.; Newman, R.A.; Wolff, R.A.; Kunnumakkara, A.B.; Abbruzzese, J.L.; Ng, C.S.; Badmaev, V.; Kurzrock, R. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 4491–4499. [Google Scholar] [CrossRef] [PubMed]
- Ghalaut, V.S.; Sangwan, L.; Dahiya, K.; Ghalaut, P.S.; Dhankhar, R.; Saharan, R. Effect of imatinib therapy with and without turmeric powder on nitric oxide levels in chronic myeloid leukemia. J. Oncol. Pharm. Pract. Off. Publ. Int. Soc. Oncol. Pharm. Pract. 2012, 18, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Capalbo, C.; Belardinilli, F.; Filetti, M.; Parisi, C.; Petroni, M.; Colicchia, V.; Tessitore, A.; Santoni, M.; Coppa, A.; Giannini, G.; et al. Effective treatment of a platinum-resistant cutaneous squamous cell carcinoma case by EGFR pathway inhibition. Mol. Clin. Oncol. 2018, 9, 30–34. [Google Scholar] [CrossRef]
- Killian, P.H.; Kronski, E.; Michalik, K.M.; Barbieri, O.; Astigiano, S.; Sommerhoff, C.P.; Pfeffer, U.; Nerlich, A.G.; Bachmeier, B.E. Curcumin inhibits prostate cancer metastasis in vivo by targeting the inflammatory cytokines CXCL1 and -2. Carcinogenesis 2012, 33, 2507–2519. [Google Scholar] [CrossRef]
- Radhakrishnan, V.M.; Kojs, P.; Young, G.; Ramalingam, R.; Jagadish, B.; Mash, E.A.; Martinez, J.D.; Ghishan, F.K.; Kiela, P.R. pTyr421 cortactin is overexpressed in colon cancer and is dephosphorylated by curcumin: Involvement of non-receptor type 1 protein tyrosine phosphatase (PTPN1). PLoS ONE 2014, 9, e85796. [Google Scholar] [CrossRef]
- Yoysungnoen, P.; Wirachwong, P.; Changtam, C.; Suksamrarn, A.; Patumraj, S. Anti-cancer and anti-angiogenic effects of curcumin and tetrahydrocurcumin on implanted hepatocellular carcinoma in nude mice. World J. Gastroenterol. 2008, 14, 2003–2009. [Google Scholar] [CrossRef]
- Chakraborty, G.; Jain, S.; Kale, S.; Raja, R.; Kumar, S.; Mishra, R.; Kundu, G.C. Curcumin suppresses breast tumor angiogenesis by abrogating osteopontin-induced VEGF expression. Mol. Med. Rep. 2008, 1, 641–646. [Google Scholar] [CrossRef]
- Saydmohammed, M.; Joseph, D.; Syed, V. Curcumin suppresses constitutive activation of STAT-3 by up-regulating protein inhibitor of activated STAT-3 (PIAS-3) in ovarian and endometrial cancer cells. J. Cell. Biochem. 2010, 110, 447–456. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, S.Y.; Park, O.J.; Kim, Y.-M. Curcumin suppresses migration and proliferation of Hep3B hepatocarcinoma cells through inhibition of the Wnt signaling pathway. Mol. Med. Rep. 2013, 8, 282–286. [Google Scholar] [CrossRef]
- Qiao, Q.; Jiang, Y.; Li, G. Inhibition of the PI3K/AKT-NF-κB pathway with curcumin enhanced radiation-induced apoptosis in human Burkitt’s lymphoma. J. Pharmacol. Sci. 2013, 121, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.S.; Lee, M.K.; Kim, J.H. Curcumin induces cell cycle arrest and apoptosis in human osteosarcoma (HOS) cells. Anticancer Res. 2009, 29, 5039–5044. [Google Scholar] [PubMed]
- Liu, E.; Wu, J.; Cao, W.; Zhang, J.; Liu, W.; Jiang, X.; Zhang, X. Curcumin induces G2/M cell cycle arrest in a p53-dependent manner and upregulates ING4 expression in human glioma. J. Neurooncol. 2007, 85, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Choudhuri, T.; Pal, S.; Agwarwal, M.L.; Das, T.; Sa, G. Curcumin induces apoptosis in human breast cancer cells through p53-dependent Bax induction. FEBS Lett. 2002, 512, 334–340. [Google Scholar] [CrossRef]
- Cao, A.-L.; Tang, Q.-F.; Zhou, W.-C.; Qiu, Y.-Y.; Hu, S.-J.; Yin, P.-H. Ras/ERK signaling pathway is involved in curcumin-induced cell cycle arrest and apoptosis in human gastric carcinoma AGS cells. J. Asian Nat. Prod. Res. 2015, 17, 56–63. [Google Scholar] [CrossRef]
- Ono, M.; Higuchi, T.; Takeshima, M.; Chen, C.; Nakano, S. Differential anti-tumor activities of curcumin against Ras- and Src-activated human adenocarcinoma cells. Biochem. Biophys. Res. Commun. 2013, 436, 186–191. [Google Scholar] [CrossRef]
- Lim, T.-G.; Lee, S.-Y.; Huang, Z.; Lim, D.Y.; Chen, H.; Jung, S.K.; Bode, A.M.; Lee, K.W.; Dong, Z. Curcumin suppresses proliferation of colon cancer cells by targeting CDK2. Cancer Prev. Res. Phila. PA 2014, 7, 466–474. [Google Scholar] [CrossRef]
- Patil, S.; Choudhary, B.; Rathore, A.; Roy, K.; Mahadik, K. Enhanced oral bioavailability and anticancer activity of novel curcumin loaded mixed micelles in human lung cancer cells. Phytomed. Int. J. Phytother. Phytopharm. 2015, 22, 1103–1111. [Google Scholar] [CrossRef]
- Vollono, L.; Falconi, M.; Gaziano, R.; Iacovelli, F.; Dika, E.; Terracciano, C.; Bianchi, L.; Campione, E. Potential of Curcumin in Skin Disorders. Nutrients 2019, 11, 2169. [Google Scholar] [CrossRef]
- Dai, M.; Zheng, X.; Xu, X.; Kong, X.; Li, X.; Guo, G.; Luo, F.; Zhao, X.; Wei, Y.Q.; Qian, Z. Chitosan-alginate sponge: Preparation and application in curcumin delivery for dermal wound healing in rat. J. Biomed. Biotechnol. 2009, 2009, 595126. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, C.; Das, M.; Sahoo, S.K. Sustained wound healing activity of curcumin loaded oleic acid based polymeric bandage in a rat model. Mol. Pharm. 2012, 9, 2801–2811. [Google Scholar] [CrossRef] [PubMed]
- Hegge, A.B.; Andersen, T.; Melvik, J.E.; Bruzell, E.; Kristensen, S.; Tønnesen, H.H. Formulation and bacterial phototoxicity of curcumin loaded alginate foams for wound treatment applications: Studies on curcumin and curcuminoides XLII. J. Pharm. Sci. 2011, 100, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, D.; Ahmed, M.R.; Gomathi, K.; Chitra, K.; Sehgal, P.K.; Jayakumar, R. Dermal wound healing processes with curcumin incorporated collagen films. Biomaterials 2004, 25, 1911–1917. [Google Scholar] [CrossRef]
- Gong, C.; Wu, Q.; Wang, Y.; Zhang, D.; Luo, F.; Zhao, X.; Wei, Y.; Qian, Z. A biodegradable hydrogel system containing curcumin encapsulated in micelles for cutaneous wound healing. Biomaterials 2013, 34, 6377–6387. [Google Scholar] [CrossRef]
- Mohanty, C.; Sahoo, S.K. Curcumin and its topical formulations for wound healing applications. Drug Discov. Today 2017, 22, 1582–1592. [Google Scholar] [CrossRef]
- Rachmawati, H.; Edityaningrum, C.A.; Mauludin, R. Molecular inclusion complex of curcumin-β-cyclodextrin nanoparticle to enhance curcumin skin permeability from hydrophilic matrix gel. AAPS PharmSciTech 2013, 14, 1303–1312. [Google Scholar] [CrossRef]
- Kang, D.; Li, B.; Luo, L.; Jiang, W.; Lu, Q.; Rong, M.; Lai, R. Curcumin shows excellent therapeutic effect on psoriasis in mouse model. Biochimie 2016, 123, 73–80. [Google Scholar] [CrossRef]
- Bahraini, P.; Rajabi, M.; Mansouri, P.; Sarafian, G.; Chalangari, R.; Azizian, Z. Turmeric tonic as a treatment in scalp psoriasis: A randomized placebo-control clinical trial. J. Cosmet. Dermatol. 2018, 17, 461–466. [Google Scholar] [CrossRef]
- Mohammadi, Z.; Sharif Zak, M.; Majdi, H.; Mostafavi, E.; Barati, M.; Lotfimehr, H.; Ghaseminasab, K.; Pazoki-Toroudi, H.; Webster, T.J.; Akbarzadeh, A. The effect of chrysin-curcumin-loaded nanofibres on the wound-healing process in male rats. Artif. Cells Nanomed. Biotechnol. 2019, 47, 1642–1652. [Google Scholar] [CrossRef]
- Mazzarino, L.; Silva, L.F.C.; Curta, J.C.; Licínio, M.A.; Costa, A.; Pacheco, L.K.; Siqueira, J.M.; Montanari, J.; Romero, E.; Assreuy, J.; et al. Curcumin-loaded lipid and polymeric nanocapsules stabilized by nonionic surfactants: An in vitro and In vivo antitumor activity on B16-F10 melanoma and macrophage uptake comparative study. J. Biomed. Nanotechnol. 2011, 7, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Li, J.; Sun, H. C6 ceramide potentiates curcumin-induced cell death and apoptosis in melanoma cell lines in vitro. Cancer Chemother. Pharmacol. 2010, 66, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Cole, G.M.; Yang, F.; Lim, G.P.; Cummings, J.L.; Frautschy, D.L.M. A Rationale for Curcuminoids for the Prevention or Treatment of Alzheimers Disease. Available online: http://www.eurekaselect.com/91646/article (accessed on 21 April 2020).
- Ringman, J.M.; Frautschy, S.A.; Cole, G.M.; Masterman, D.L.; Cummings, J.L. A potential role of the curry spice curcumin in Alzheimer’s disease. Curr. Alzheimer Res. 2005, 2, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Cole, G.M.; Teter, B.; Frautschy, S.A. Neuroprotective effects of curcumin. Adv. Exp. Med. Biol. 2007, 595, 197–212. [Google Scholar] [CrossRef]
- Brookmeyer, R.; Gray, S.; Kawas, C. Projections of Alzheimer’s disease in the United States and the public health impact of delaying disease onset. Am. J. Public Health 1998, 88, 1337–1342. [Google Scholar] [CrossRef]
- Lim, G.P.; Chu, T.; Yang, F.; Beech, W.; Frautschy, S.A.; Cole, G.M. The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. J. Neurosci. Off. J. Soc. Neurosci. 2001, 21, 8370–8377. [Google Scholar] [CrossRef]
- Frautschy, S.A.; Hu, W.; Kim, P.; Miller, S.A.; Chu, T.; Harris-White, M.E.; Cole, G.M. Phenolic anti-inflammatory antioxidant reversal of Abeta-induced cognitive deficits and neuropathology. Neurobiol. Aging 2001, 22, 993–1005. [Google Scholar] [CrossRef]
- Santacruz, K.; Lewis, J.; Spires, T.; Paulson, J.; Kotilinek, L.; Ingelsson, M.; Guimaraes, A.; DeTure, M.; Ramsden, M.; McGowan, E.; et al. Tau suppression in a neurodegenerative mouse model improves memory function. Science 2005, 309, 476–481. [Google Scholar] [CrossRef]
- Liu, Z.; Yu, Y.; Li, X.; Ross, C.A.; Smith, W.W. Curcumin protects against A53T alpha-synuclein-induced toxicity in a PC12 inducible cell model for Parkinsonism. Pharmacol. Res. 2011, 63, 439–444. [Google Scholar] [CrossRef]
- Cui, Q.; Sun, S. Curcumin Antagonizes Rotenone-induced Injury of PC12 Cells by Antioxidant Activity. Acta Med. Univ. Sci. Technol. Huazhong 2010, 39, 37–41, 46. [Google Scholar]
- Buratta, S.; Chiaradia, E.; Tognoloni, A.; Gambelunghe, A.; Meschini, C.; Palmieri, L.; Muzi, G.; Urbanelli, L.; Emiliani, C.; Tancini, B. Effect of Curcumin on Protein Damage Induced by Rotenone in Dopaminergic PC12 Cells. Int. J. Mol. Sci. 2020, 21, 2761. [Google Scholar] [CrossRef]
- Buccarello, L.; Dragotto, J.; Iorio, F.; Hassanzadeh, K.; Corbo, M.; Feligioni, M. The pivotal role of SUMO-1-JNK-Tau axis in an in vitro model of oxidative stress counteracted by the protective effect of curcumin. Biochem. Pharmacol. 2020, 114066. [Google Scholar] [CrossRef] [PubMed]
- Jagatha, B.; Mythri, R.B.; Vali, S.; Bharath, M.M.S. Curcumin treatment alleviates the effects of glutathione depletion in vitro and in vivo: Therapeutic implications for Parkinson’s disease explained via in silico studies. Free Radic. Biol. Med. 2008, 44, 907–917. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, D.; Amato, A.; Picone, P.; Terzo, S.; Galizzi, G.; Bonina, F.P.; Mulè, F.; Di Carlo, M. A Natural Dietary Supplement with a Combination of Nutrients Prevents Neurodegeneration Induced by a High Fat Diet in Mice. Nutrients 2018, 10, 1130. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Gilani, A.-H.; Hosseinmardi, N.; Semnanian, S.; Enam, S.A.; Fathollahi, Y. Curcuminoids rescue long-term potentiation impaired by amyloid peptide in rat hippocampal slices. Synap 2011, 65, 572–582. [Google Scholar] [CrossRef]
- Yang, F.; Lim, G.P.; Begum, A.N.; Ubeda, O.J.; Simmons, M.R.; Ambegaokar, S.S.; Chen, P.P.; Kayed, R.; Glabe, C.G.; Frautschy, S.A.; et al. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J. Biol. Chem. 2005, 280, 5892–5901. [Google Scholar] [CrossRef]
- Yanagisawa, D.; Taguchi, H.; Yamamoto, A.; Shirai, N.; Hirao, K.; Tooyama, I. Curcuminoid binds to amyloid-β1-42 oligomer and fibril. J. Alzheimers Dis. JAD 2011, 24 (Suppl. 2), 33–42. [Google Scholar] [CrossRef]
- Shimmyo, Y.; Kihara, T.; Akaike, A.; Niidome, T.; Sugimoto, H. Epigallocatechin-3-gallate and curcumin suppress amyloid beta-induced beta-site APP cleaving enzyme-1 upregulation. Neuroreport 2008, 19, 1329–1333. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Fu, X.; Li, Y.-F.; Li, X.-L.; Ma, Z.-Y.; Zhang, Y.; Gao, Q.-C. miR-15b-5p targeting amyloid precursor protein is involved in the anti-amyloid eflect of curcumin in swAPP695-HEK293 cells. Neural Regen. Res. 2019, 14, 1603–1609. [Google Scholar] [CrossRef]
- Ahmed, T.; Enam, S.A.; Gilani, A.H. Curcuminoids enhance memory in an amyloid-infused rat model of Alzheimer’s disease. Neuroscience 2010, 169, 1296–1306. [Google Scholar] [CrossRef]
- Ishrat, T.; Hoda, M.N.; Khan, M.B.; Yousuf, S.; Ahmad, M.; Khan, M.M.; Ahmad, A.; Islam, F. Amelioration of cognitive deficits and neurodegeneration by curcumin in rat model of sporadic dementia of Alzheimer’s type (SDAT). Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2009, 19, 636–647. [Google Scholar] [CrossRef] [PubMed]
- Ringman, J.M.; Frautschy, S.A.; Teng, E.; Begum, A.N.; Bardens, J.; Beigi, M.; Gylys, K.H.; Badmaev, V.; Heath, D.D.; Apostolova, L.G.; et al. Oral curcumin for Alzheimer’s disease: Tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimers Res. Ther. 2012, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Hishikawa, N.; Takahashi, Y.; Amakusa, Y.; Tanno, Y.; Tuji, Y.; Niwa, H.; Murakami, N.; Krishna, U.K. Effects of turmeric on Alzheimer’s disease with behavioral and psychological symptoms of dementia. Ayu 2012, 33, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Mythri, R.B.; Jagatha, B.; Pradhan, N.; Andersen, J.; Bharath, M.M.S. Mitochondrial complex I inhibition in Parkinson’s disease: How can curcumin protect mitochondria? Antioxid. Redox Signal. 2007, 9, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Ray, B.; Bisht, S.; Maitra, A.; Maitra, A.; Lahiri, D.K. Neuroprotective and neurorescue effects of a novel polymeric nanoparticle formulation of curcumin (NanoCurc™) in the neuronal cell culture and animal model: Implications for Alzheimer’s disease. J. Alzheimers Dis. JAD 2011, 23, 61–77. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-S.; Hung, K.-S.; Chiu, W.-T.; Sun, Y.-Y.; Tsai, S.-H.; Lin, J.-W.; Lee, Y.-H. Curcumin enhances neuronal survival in N-methyl-d-aspartic acid toxicity by inducing RANTES expression in astrocytes via PI-3K and MAPK signaling pathways. Prog. Neuropsychopharmacol. Biol. Psychiatry 2011, 35, 931–938. [Google Scholar] [CrossRef]
- Wu, A.; Ying, Z.; Gomez-Pinilla, F. Dietary curcumin counteracts the outcome of traumatic brain injury on oxidative stress, synaptic plasticity, and cognition. Exp. Neurol. 2006, 197, 309–317. [Google Scholar] [CrossRef]
- Xu, Y.; Ku, B.-S.; Yao, H.-Y.; Lin, Y.-H.; Ma, X.; Zhang, Y.-H.; Li, X.-J. The effects of curcumin on depressive-like behaviors in mice. Eur. J. Pharmacol. 2005, 518, 40–46. [Google Scholar] [CrossRef]
- Al-Omar, F.A.; Nagi, M.N.; Abdulgadir, M.M.; Al Joni, K.S.; Al-Majed, A.A. Immediate and delayed treatments with curcumin prevents forebrain ischemia-induced neuronal damage and oxidative insult in the rat hippocampus. Neurochem. Res. 2006, 31, 611–618. [Google Scholar] [CrossRef]
- Mehla, J.; Reeta, K.H.; Gupta, P.; Gupta, Y.K. Protective effect of curcumin against seizures and cognitive impairment in a pentylenetetrazole-kindled epileptic rat model. Life Sci. 2010, 87, 596–603. [Google Scholar] [CrossRef]
- Zbarsky, V.; Datla, K.P.; Parkar, S.; Rai, D.K.; Aruoma, O.I.; Dexter, D.T. Neuroprotective properties of the natural phenolic antioxidants curcumin and naringenin but not quercetin and fisetin in a 6-OHDA model of Parkinson’s disease. Free Radic. Res. 2005, 39, 1119–1125. [Google Scholar] [CrossRef]
- Wang, J.; Du, X.-X.; Jiang, H.; Xie, J.-X. Curcumin attenuates 6-hydroxydopamine-induced cytotoxicity by anti-oxidation and nuclear factor-kappa B modulation in MES23.5 cells. Biochem. Pharmacol. 2009, 78, 178–183. [Google Scholar] [CrossRef]
- Rajeswari, A.; Sabesan, M. Inhibition of monoamine oxidase-B by the polyphenolic compound, curcumin and its metabolite tetrahydrocurcumin, in a model of Parkinson’s disease induced by MPTP neurodegeneration in mice. Inflammopharmacology 2008, 16, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.S.; Boddapati, S.; Emadi, S.; Sierks, M.R. Curcumin reduces alpha-synuclein induced cytotoxicity in Parkinson’s disease cell model. BMC Neurosci. 2010, 11, 57. [Google Scholar] [CrossRef] [PubMed]
- Vajragupta, O.; Boonchoong, P.; Watanabe, H.; Tohda, M.; Kummasud, N.; Sumanont, Y. Manganese complexes of curcumin and its derivatives: Evaluation for the radical scavenging ability and neuroprotective activity. Free Radic. Biol. Med. 2003, 35, 1632–1644. [Google Scholar] [CrossRef] [PubMed]
- Radomska-Leśniewska, D.M.; Osiecka-Iwan, A.; Hyc, A.; Góźdź, A.; Dąbrowska, A.M.; Skopiński, P. Therapeutic potential of curcumin in eye diseases. Cent. Eur. J. Immunol. 2019, 44, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.-K.; Mo, B.; Zhao, J.; Yu, Y.-J.; Liu, L.; Yue, C.-L.; Liu, W. Neuroprotective effect of curcumin against oxidative damage in BV-2 microglia and high intraocular pressure animal model. J. Ocul. Pharmacol. Ther. Off. J. Assoc. Ocul. Pharmacol. Ther. 2014, 30, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, C.; Guo, H.; Kern, T.S.; Huang, K.; Zheng, L. Curcumin Inhibits Neuronal and Vascular Degeneration in Retina after Ischemia and Reperfusion Injury. PLoS ONE 2011, 6, e23194. [Google Scholar] [CrossRef]
- Zhu, W.; Wu, Y.; Meng, Y.-F.; Wang, J.-Y.; Xu, M.; Tao, J.-J.; Lu, J. Effect of curcumin on aging retinal pigment epithelial cells. Drug Des. Devel. Ther. 2015, 9, 5337–5344. [Google Scholar] [CrossRef][Green Version]
- Gupta, S.K.; Kumar, B.; Nag, T.C.; Agrawal, S.S.; Agrawal, R.; Agrawal, P.; Saxena, R.; Srivastava, S. Curcumin prevents experimental diabetic retinopathy in rats through its hypoglycemic, antioxidant, and anti-inflammatory mechanisms. J. Ocul. Pharmacol. Ther. Off. J. Assoc. Ocul. Pharmacol. Ther. 2011, 27, 123–130. [Google Scholar] [CrossRef]
- Manikandan, R.; Thiagarajan, R.; Beulaja, S.; Chindhu, S.; Mariammal, K.; Sudhandiran, G.; Arumugam, M. Anti-cataractogenic effect of curcumin and aminoguanidine against selenium-induced oxidative stress in the eye lens of Wistar rat pups: An in vitro study using isolated lens. Chem. Biol. Interact. 2009, 181, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Suryanarayana, P.; Saraswat, M.; Mrudula, T.; Krishna, T.P.; Krishnaswamy, K.; Reddy, G.B. Curcumin and turmeric delay streptozotocin-induced diabetic cataract in rats. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2092–2099. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, N.; Guha, R.; Chowdhury, S.; Nandi, S.; Konar, A.; Hazra, S. Curcumin nanoparticles inhibit corneal neovascularization. J. Mol. Med. Berl. Ger. 2015, 93, 1095–1106. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Hu, D.-N.; Pan, Z.; Lu, C.-W.; Xue, C.-Y.; Aass, I. Curcumin protects against hyperosmoticity-induced IL-1beta elevation in human corneal epithelial cell via MAPK pathways. Exp. Eye Res. 2010, 90, 437–443. [Google Scholar] [CrossRef]
- Chung, S.-H.; Choi, S.H.; Choi, J.A.; Chuck, R.S.; Joo, C.-K. Curcumin suppresses ovalbumin-induced allergic conjunctivitis. Mol. Vis. 2012, 18, 1966–1972. [Google Scholar] [PubMed]
- Burugula, B.; Ganesh, B.S.; Chintala, S.K. Curcumin Attenuates Staurosporine-Mediated Death of Retinal Ganglion Cells. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4263–4273. [Google Scholar] [CrossRef]
- Davis, B.M.; Pahlitzsch, M.; Guo, L.; Balendra, S.; Shah, P.; Ravindran, N.; Malaguarnera, G.; Sisa, C.; Shamsher, E.; Hamze, H.; et al. Topical Curcumin Nanocarriers are Neuroprotective in Eye Disease. Sci. Rep. 2018, 8, 11066. [Google Scholar] [CrossRef]
- Kasi, P.D.; Tamilselvam, R.; Skalicka-Woźniak, K.; Nabavi, S.F.; Daglia, M.; Bishayee, A.; Pazoki-Toroudi, H.; Nabavi, S.M. Molecular targets of curcumin for cancer therapy: An updated review. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016, 37, 13017–13028. [Google Scholar] [CrossRef]
- Zhou, H.; Beevers, C.S.; Huang, S. The targets of curcumin. Curr. Drug Targets 2011, 12, 332–347. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Surh, Y.-J.; Shishodia, S. (Eds.) The Molecular Targets and Therapeutic Uses of Curcumin in Health and Disease; Advances in Experimental Medicine and Biology; Springer: New York, NY, USA, 2007; ISBN 978-0-387-46400-8. [Google Scholar]
- Song, X.; Zhang, M.; Dai, E.; Luo, Y. Molecular targets of curcumin in breast cancer (Review). Mol. Med. Rep. 2019, 19, 23–29. [Google Scholar] [CrossRef]
- Hsu, H.-Y.; Wen, M.-H. Lipopolysaccharide-mediated reactive oxygen species and signal transduction in the regulation of interleukin-1 gene expression. J. Biol. Chem. 2002, 277, 22131–22139. [Google Scholar] [CrossRef] [PubMed]
- Nanji, A.A.; Jokelainen, K.; Tipoe, G.L.; Rahemtulla, A.; Thomas, P.; Dannenberg, A.J. Curcumin prevents alcohol-induced liver disease in rats by inhibiting the expression of NF-kappa B-dependent genes. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 284, G321–G327. [Google Scholar] [CrossRef]
- Rahimi, K.; Ahmadi, A.; Hassanzadeh, K.; Soleimani, Z.; Sathyapalan, T.; Mohammadi, A.; Sahebkar, A. Targeting the balance of T helper cell responses by curcumin in inflammatory and autoimmune states. Autoimmun. Rev. 2019, 18, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.; Kong, P.-J.; Yuh, Y.-J.; Lim, S.-Y.; Yim, S.-V.; Chun, W.; Kim, S.-S. Curcumin suppresses lipopolysaccharide-induced cyclooxygenase-2 expression by inhibiting activator protein 1 and nuclear factor kappab bindings in BV2 microglial cells. J. Pharmacol. Sci. 2004, 94, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Rahman, I.; Marwick, J.; Kirkham, P. Redox modulation of chromatin remodeling: Impact on histone acetylation and deacetylation, NF-kappaB and pro-inflammatory gene expression. Biochem. Pharmacol. 2004, 68, 1255–1267. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Lu, J.; Holmgren, A. Thioredoxin reductase is irreversibly modified by curcumin: A novel molecular mechanism for its anticancer activity. J. Biol. Chem. 2005, 280, 25284–25290. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Qiu, F. Curcuminoid Metabolism and its Contribution to the Pharmacological Effects. Curr. Drug Metab. 2013, 14, 791–806. [Google Scholar] [CrossRef]
- Yu, Q.; Liu, Y.; Wu, Y.; Chen, Y. Dihydrocurcumin ameliorates the lipid accumulation, oxidative stress and insulin resistance in oleic acid-induced L02 and HepG2 cells. Biomed. Pharmacother. 2018, 103, 1327–1336. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Deb, L.; Prasad, S. Curcumin Differs from Tetrahydrocurcumin for Molecular Targets, Signaling Pathways and Cellular Responses. Molecules 2015, 20, 185–205. [Google Scholar] [CrossRef]
- Wu, J.-C.; Tsai, M.-L.; Lai, C.-S.; Wang, Y.-J.; Ho, C.-T.; Pan, M.-H. Chemopreventative effects of tetrahydrocurcumin on human diseases. Food Funct. 2014, 5, 12–17. [Google Scholar] [CrossRef]
- Naito, M.; Wu, X.; Nomura, H.; Kodama, M.; Kato, Y.; Kato, Y.; Osawa, T. The Protective Effects of Tetrahydrocurcumin on Oxidative Stress in Cholesterol-fed Rabbits. J. Atheroscler. Thromb. 2002, 9, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Murugan, P.; Pari, L. Effect of Tetrahydrocurcumin on Lipid Peroxidation and Lipids in Streptozotocin-Nicotinamide-Induced Diabetic Rats. Basic Clin. Pharmacol. Toxicol. 2006, 99, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Pari, L.; Murugan, P. Antihyperlipidemic Effect of Curcumin and Tetrahydrocurcumin in Experimental Type 2 Diabetic Rats. Ren. Fail. 2007, 29, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Li, J.; Wu, L.; Zhou, C.; Wang, Q.; Li, X.; Zhou, M.; Wang, H. Tetrahydrocurcumin provides neuroprotection in rats after traumatic brain injury: Autophagy and the PI3K/AKT pathways as a potential mechanism. J. Surg. Res. 2016, 206, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Thomas, S.G.; Kunnumakkara, A.B.; Sundaram, C.; Harikumar, K.B.; Sung, B.; Tharakan, S.T.; Misra, K.; Priyadarsini, I.K.; Rajasekharan, K.N.; et al. Biological activities of curcumin and its analogues (Congeners) made by man and Mother Nature. Biochem. Pharmacol. 2008, 76, 1590–1611. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, E.; Hoehle, S.I.; Walch, S.G.; Riess, A.; Sólyom, A.M.; Metzler, M. Curcuminoids Form Reactive Glucuronides In Vitro. J. Agric. Food Chem. 2007, 55, 538–544. [Google Scholar] [CrossRef]
- Vijaya Saradhi, U.V.R.; Ling, Y.; Wang, J.; Chiu, M.; Schwartz, E.B.; Fuchs, J.R.; Chan, K.K.; Liu, Z. A liquid chromatography–tandem mass spectrometric method for quantification of curcuminoids in cell medium and mouse plasma. J. Chromatogr. B 2010, 878, 3045–3051. [Google Scholar] [CrossRef]
- Zhu, J.; Sanidad, K.Z.; Sukamtoh, E.; Zhang, G. Potential roles of chemical degradation in the biological activities of curcumin. Food Funct. 2017, 8, 907–914. [Google Scholar] [CrossRef]
- Wang, Y.-J.; Pan, M.-H.; Cheng, A.-L.; Lin, L.-I.; Ho, Y.-S.; Hsieh, C.-Y.; Lin, J.-K. Stability of curcumin in buffer solutions and characterization of its degradation products. J. Pharm. Biomed. Anal. 1997, 15, 1867–1876. [Google Scholar] [CrossRef]
- Gordon, O.N.; Luis, P.B.; Sintim, H.O.; Schneider, C. Unraveling curcumin degradation: Autoxidation proceeds through spiroepoxide and vinylether intermediates en route to the main bicyclopentadione. J. Biol. Chem. 2015, 290, 4817–4828. [Google Scholar] [CrossRef]
- Zhang, G.; Nitteranon, V.; Chan, L.Y.; Parkin, K.L. Glutathione conjugation attenuates biological activities of 6-dehydroshogaol from ginger. Food Chem. 2013, 140, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schramm, A.; Jähne, E.A.; Baburin, I.; Hering, S.; Hamburger, M. Natural products as potential human ether-a-go-go-related gene channel inhibitors—Outcomes from a screening of widely used herbal medicines and edible plants. Planta Med. 2014, 80, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.-W.; Sheng, Y.; Zhang, Q.; Liu, H.-B.; Xie, X.; Ma, W.-C.; Huo, R.; Dong, D.-L. Curcumin inhibits hERG potassium channels in vitro. Toxicol. Lett. 2012, 208, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhou, Y.; Yang, J.; Zhang, H.H.; Zhao, S.L.; Zhang, T.; Huo, J.; Zheng, P. Curcumin induces apoptosis and protective autophagy in human gastric cancer cells with different degree of differentiation. Zhonghua Zhong Liu Za Zhi 2017, 39, 490–496. [Google Scholar] [CrossRef]
- Kuttan, R.; Bhanumathy, P.; Nirmala, K.; George, M.C. Potential anticancer activity of turmeric (Curcuma longa). Cancer Lett. 1985, 29, 197–202. [Google Scholar] [CrossRef]
- Nelson, K.M.; Dahlin, J.L.; Bisson, J.; Graham, J.; Pauli, G.F.; Walters, M.A. The Essential Medicinal Chemistry of Curcumin. J. Med. Chem. 2017, 60, 1620–1637. [Google Scholar] [CrossRef]
- Cheng, A.L.; Hsu, C.H.; Lin, J.K.; Hsu, M.M.; Ho, Y.F.; Shen, T.S.; Ko, J.Y.; Lin, J.T.; Lin, B.R.; Ming-Shiang, W.; et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001, 21, 2895–2900. [Google Scholar]
- Prasad, S.; Gupta, S.C.; Tyagi, A.K.; Aggarwal, B.B. Curcumin, a component of golden spice: From bedside to bench and back. Biotechnol. Adv. 2014, 32, 1053–1064. [Google Scholar] [CrossRef]
- Rahimnia, A.-R.; Panahi, Y.; Alishiri, G.; Sharafi, M.; Sahebkar, A. Impact of Supplementation with Curcuminoids on Systemic Inflammation in Patients with Knee Osteoarthritis: Findings from a Randomized Double-Blind Placebo-Controlled Trial. Drug Res. 2015, 65, 521–525. [Google Scholar] [CrossRef]
- Kocaadam, B.; Şanlier, N. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit. Rev. Food Sci. Nutr. 2017, 57, 2889–2895. [Google Scholar] [CrossRef]
- Lao, C.D.; Ruffin, M.T.; Normolle, D.; Heath, D.D.; Murray, S.I.; Bailey, J.M.; Boggs, M.E.; Crowell, J.; Rock, C.L.; Brenner, D.E. Dose escalation of a curcuminoid formulation. BMC Complement. Altern. Med. 2006, 6, 10. [Google Scholar] [CrossRef] [PubMed]
- Chainani, W.N. Safety and anti-inflammatory activity of curcumin: A component of tumeric (Curcuma longa). J. Altern. Complement. Med. 2003, 9, 161–168. [Google Scholar] [CrossRef]
- Qin, S.; Huang, L.; Gong, J.; Shen, S.; Huang, J.; Ren, H.; Hu, H. Efficacy and safety of turmeric and curcumin in lowering blood lipid levels in patients with cardiovascular risk factors: A meta-analysis of randomized controlled trials. Nutr. J. 2017, 16, 68. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.A.; McLelland, H.R.; Hill, K.A.; Ireson, C.R.; Euden, S.A.; Manson, M.M.; Pirmohamed, M.; Marnett, L.J.; Gescher, A.J.; Steward, W.P. Pharmacodynamic and pharmacokinetic study of oral Curcuma extract in patients with colorectal cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2001, 7, 1894–1900. [Google Scholar]
- Ryan, J.L.; Heckler, C.E.; Ling, M.; Katz, A.; Williams, J.P.; Pentland, A.P.; Morrow, G.R. Curcumin for radiation dermatitis: A randomized, double-blind, placebo-controlled clinical trial of thirty breast cancer patients. Radiat. Res. 2013, 180, 34–43. [Google Scholar] [CrossRef]
- Epelbaum, R.; Schaffer, M.; Vizel, B.; Badmaev, V.; Bar-Sela, G. Curcumin and gemcitabine in patients with advanced pancreatic cancer. Nutr. Cancer 2010, 62, 1137–1141. [Google Scholar] [CrossRef]
- Eaton, J.E.; Nelson, K.M.; Gossard, A.A.; Carey, E.J.; Tabibian, J.H.; Lindor, K.D.; LaRusso, N.F. Efficacy and safety of curcumin in primary sclerosing cholangitis: An open label pilot study. Scand. J. Gastroenterol. 2019, 54, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Lukefahr, A.L.; McEvoy, S.; Alfafara, C.; Funk, J.L. Drug-induced autoimmune hepatitis associated with turmeric dietary supplement use. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef]
- Storka, A.; Vcelar, B.; Klickovic, U.; Gouya, G.; Weisshaar, S.; Aschauer, S.; Bolger, G.; Helson, L.; Wolzt, M. Safety, tolerability and pharmacokinetics of liposomal curcumin in healthy humans. Int. J. Clin. Pharmacol. Ther. 2015, 53, 54–65. [Google Scholar] [CrossRef]
- Greil, R.; Greil-Ressler, S.; Weiss, L.; Schönlieb, C.; Magnes, T.; Radl, B.; Bolger, G.T.; Vcelar, B.; Sordillo, P.P. A phase 1 dose-escalation study on the safety, tolerability and activity of liposomal curcumin (Lipocurc™) in patients with locally advanced or metastatic cancer. Cancer Chemother. Pharmacol. 2018, 82, 695–706. [Google Scholar] [CrossRef]
- Sun, J.; Bi, C.; Chan, H.M.; Sun, S.; Zhang, Q.; Zheng, Y. Curcumin-loaded solid lipid nanoparticles have prolonged in vitro antitumour activity, cellular uptake and improved in vivo bioavailability. Colloids Surf. B Biointerfaces 2013, 111, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Lasoff, D.R.; Cantrell, F.L.; Ly, B.T. Death associated with intravenous turmeric (Curcumin) preparation. Clin. Toxicol. 2018, 56, 384–385. [Google Scholar] [CrossRef] [PubMed]
- Priyadarsini, K.I. The Chemistry of Curcumin: From Extraction to Therapeutic Agent. Molecules 2014, 19, 20091–20112. [Google Scholar] [CrossRef]
- Ravindranath, V.; Chandrasekhara, N. Absorption and tissue distribution of curcumin in rats. Toxicology 1980, 16, 259–265. [Google Scholar] [CrossRef]
- Nabavi, S.M.; Russo, G.L.; Tedesco, I.; Daglia, M.; Orhan, I.E.; Nabavi, S.F.; Bishayee, A.; Nagulapalli Venkata, K.C.; Abdollahi, M.; Hajheydari, Z. Curcumin and Melanoma: From Chemistry to Medicine. Nutr. Cancer 2018, 70, 164–175. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Sung, B. Pharmacological basis for the role of curcumin in chronic diseases: An age-old spice with modern targets. Trends Pharmacol. Sci. 2009, 30, 85–94. [Google Scholar] [CrossRef]
- Xie, X.; Tao, Q.; Zou, Y.; Zhang, F.; Guo, M.; Wang, Y.; Wang, H.; Zhou, Q.; Yu, S. PLGA Nanoparticles Improve the Oral Bioavailability of Curcumin in Rats: Characterizations and Mechanisms. J. Agric. Food Chem. 2011, 59, 9280–9289. [Google Scholar] [CrossRef]
- Yang, C.; Su, X.; Liu, A.; Zhang, L.; Yu, A.; Xi, Y.; Zhai, G. Advances in clinical study of curcumin. Curr. Pharm. Des. 2013, 19, 1966–1973. [Google Scholar]
- Prasad, S.; Tyagi, A.K.; Aggarwal, B.B. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: The golden pigment from golden spice. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2014, 46, 2–18. [Google Scholar] [CrossRef]
- Hou, Y.; Wang, H.; Zhang, F.; Sun, F.; Xin, M.; Li, M.; Li, J.; Wu, X. Novel self-nanomicellizing solid dispersion based on rebaudioside A: A potential nanoplatform for oral delivery of curcumin. Int. J. Nanomed. 2019, 14, 557–571. [Google Scholar] [CrossRef]
- Sunagawa, Y.; Hirano, S.; Katanasaka, Y.; Miyazaki, Y.; Funamoto, M.; Okamura, N.; Hojo, Y.; Suzuki, H.; Doi, O.; Yokoji, T.; et al. Colloidal submicron-particle curcumin exhibits high absorption efficiency-a double-blind, 3-way crossover study. J. Nutr. Sci. Vitaminol. 2015, 61, 37–44. [Google Scholar] [CrossRef]
- Patel, S.S.; Acharya, A.; Ray, R.S.; Agrawal, R.; Raghuwanshi, R.; Jain, P. Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Crit. Rev. Food Sci. Nutr. 2020, 60, 887–939. [Google Scholar] [CrossRef] [PubMed]
- McClements, D.J.; Li, F.; Xiao, H. The Nutraceutical Bioavailability Classification Scheme: Classifying Nutraceuticals According to Factors Limiting their Oral Bioavailability. Annu. Rev. Food Sci. Technol. 2015, 6, 299–327. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhu, W.; Yang, C.; Guo, H.; Yu, A.; Ji, J.; Gao, Y.; Sun, M.; Zhai, G. A novel folate-modified self-microemulsifying drug delivery system of curcumin for colon targeting. Int. J. Nanomed. 2012, 7, 151–162. [Google Scholar] [CrossRef]
- Liu, W.; Zhai, Y.; Heng, X.; Che, F.Y.; Chen, W.; Sun, D.; Zhai, G. Oral bioavailability of curcumin: Problems and advancements. J. Drug Target. 2016, 24, 694–702. [Google Scholar] [CrossRef]
- Tønnesen, H.H.; Karlsen, J. Studies on curcumin and curcuminoids. VI. Kinetics of curcumin degradation in aqueous solution. Z. Lebensm. Unters. Forsch. 1985, 180, 402–404. [Google Scholar] [CrossRef]
- Hoehle, S.I.; Pfeiffer, E.; Sólyom, A.M.; Metzler, M. Metabolism of curcuminoids in tissue slices and subcellular fractions from rat liver. J. Agric. Food Chem. 2006, 54, 756–764. [Google Scholar] [CrossRef]
- Ireson, C.R.; Jones, D.J.L.; Orr, S.; Coughtrie, M.W.H.; Boocock, D.J.; Williams, M.L.; Farmer, P.B.; Steward, W.P.; Gescher, A.J. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2002, 11, 105–111. [Google Scholar]
- Hassaninasab, A.; Hashimoto, Y.; Tomita-Yokotani, K.; Kobayashi, M. Discovery of the curcumin metabolic pathway involving a unique enzyme in an intestinal microorganism. Proc. Natl. Acad. Sci. USA 2011, 108, 6615–6620. [Google Scholar] [CrossRef]
- Cuomo, J.; Appendino, G.; Dern, A.S.; Schneider, E.; McKinnon, T.P.; Brown, M.J.; Togni, S.; Dixon, B.M. Comparative absorption of a standardized curcuminoid mixture and its lecithin formulation. J. Nat. Prod. 2011, 74, 664–669. [Google Scholar] [CrossRef]
- Semalty, A.; Semalty, M.; Rawat, M.S.M.; Franceschi, F. Supramolecular phospholipids-polyphenolics interactions: The PHYTOSOME strategy to improve the bioavailability of phytochemicals. Fitoterapia 2010, 81, 306–314. [Google Scholar] [CrossRef]
- Gota, V.S.; Maru, G.B.; Soni, T.G.; Gandhi, T.R.; Kochar, N.; Agarwal, M.G. Safety and pharmacokinetics of a solid lipid curcumin particle formulation in osteosarcoma patients and healthy volunteers. J. Agric. Food Chem. 2010, 58, 2095–2099. [Google Scholar] [CrossRef]
- Rasenack, N.; Müller, B.W. Dissolution rate enhancement by in situ micronization of poorly water-soluble drugs. Pharm. Res. 2002, 19, 1894–1900. [Google Scholar] [CrossRef]
- Madhavi, D.; Kagan, D. Bioavailability of a Sustained Release Formulation of Curcumin. Integr. Med. Encinitas Calif. 2014, 13, 24–30. [Google Scholar]
- Bhardwaj, R.K.; Glaeser, H.; Becquemont, L.; Klotz, U.; Gupta, S.K.; Fromm, M.F. Piperine, a major constituent of black pepper, inhibits human P-glycoprotein and CYP3A4. J. Pharmacol. Exp. Ther. 2002, 302, 645–650. [Google Scholar] [CrossRef]
- Shoba, G.; Joy, D.; Joseph, T.; Majeed, M.; Rajendran, R.; Srinivas, P.S. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998, 64, 353–356. [Google Scholar] [CrossRef]
- Schiborr, C.; Kocher, A.; Behnam, D.; Jandasek, J.; Toelstede, S.; Frank, J. The oral bioavailability of curcumin from micronized powder and liquid micelles is significantly increased in healthy humans and differs between sexes. Mol. Nutr. Food Res. 2014, 58, 516–527. [Google Scholar] [CrossRef]
- Sasaki, H.; Sunagawa, Y.; Takahashi, K.; Imaizumi, A.; Fukuda, H.; Hashimoto, T.; Wada, H.; Katanasaka, Y.; Kakeya, H.; Fujita, M.; et al. Innovative preparation of curcumin for improved oral bioavailability. Biol. Pharm. Bull. 2011, 34, 660–665. [Google Scholar] [CrossRef]
- Yang, K.-Y.; Lin, L.-C.; Tseng, T.-Y.; Wang, S.-C.; Tsai, T.-H. Oral bioavailability of curcumin in rat and the herbal analysis from Curcuma longa by LC-MS/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life. Sci. 2007, 853, 183–189. [Google Scholar] [CrossRef]
- Maiti, K.; Mukherjee, K.; Gantait, A.; Saha, B.P.; Mukherjee, P.K. Curcumin–phospholipid complex: Preparation, therapeutic evaluation and pharmacokinetic study in rats. Int. J. Pharm. 2007, 330, 155–163. [Google Scholar] [CrossRef]
- Marczylo, T.H.; Verschoyle, R.D.; Cooke, D.N.; Morazzoni, P.; Steward, W.P.; Gescher, A.J. Comparison of systemic availability of curcumin with that of curcumin formulated with phosphatidylcholine. Cancer Chemother. Pharmacol. 2007, 60, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Garcea, G.; Jones, D.J.L.; Singh, R.; Dennison, A.R.; Farmer, P.B.; Sharma, R.A.; Steward, W.P.; Gescher, A.J.; Berry, D.P. Detection of curcumin and its metabolites in hepatic tissue and portal blood of patients following oral administration. Br. J. Cancer 2004, 90, 1011–1015. [Google Scholar] [CrossRef] [PubMed]
- Garcea, G.; Berry, D.P.; Jones, D.J.L.; Singh, R.; Dennison, A.R.; Farmer, P.B.; Sharma, R.A.; Steward, W.P.; Gescher, A.J. Consumption of the putative chemopreventive agent curcumin by cancer patients: Assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2005, 14, 120–125. [Google Scholar]
- Asai, A.; Miyazawa, T. Occurrence of orally administered curcuminoid as glucuronide and glucuronide/sulfate conjugates in rat plasma. Life Sci. 2000, 67, 2785–2793. [Google Scholar] [CrossRef]
- Perkins, S.; Verschoyle, R.D.; Hill, K.; Parveen, I.; Threadgill, M.D.; Sharma, R.A.; Williams, M.L.; Steward, W.P.; Gescher, A.J. Chemopreventive efficacy and pharmacokinetics of curcumin in the min/+ mouse, a model of familial adenomatous polyposis. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2002, 11, 535–540. [Google Scholar]
- Ravindranath, V.; Chandrasekhara, N. In vitro studies on the intestinal absorption of curcumin in rats. Toxicology 1981, 20, 251–257. [Google Scholar] [CrossRef]
- Ravindranath, V.; Chandrasekhara, N. Metabolism of curcumin—Studies with [3H]curcumin. Toxicology 1981, 22, 337–344. [Google Scholar] [CrossRef]
- Im, K.; Ravi, A.; Kumar, D.; Kuttan, R.; Maliakel, B. An enhanced bioavailable formulation of curcumin using fenugreek-derived soluble dietary fibre. J. Funct. Foods 2012, 4, 348–357. [Google Scholar] [CrossRef]
- Purpura, M.; Lowery, R.P.; Wilson, J.M.; Mannan, H.; Münch, G.; Razmovski-Naumovski, V. Analysis of different innovative formulations of curcumin for improved relative oral bioavailability in human subjects. Eur. J. Nutr. 2018, 57, 929–938. [Google Scholar] [CrossRef]
- Boyanapalli, S.S.S.; Huang, Y.; Su, Z.; Cheng, D.; Zhang, C.; Guo, Y.; Rao, R.; Androulakis, I.P.; Kong, A.-N. Pharmacokinetics and Pharmacodynamics of Curcumin in regulating anti-inflammatory and epigenetic gene expression. Biopharm. Drug Dispos. 2018, 39, 289–297. [Google Scholar] [CrossRef]
- Antony, B.; Merina, B.; Iyer, V.S.; Judy, N.; Lennertz, K.; Joyal, S. A Pilot Cross-Over Study to Evaluate Human Oral Bioavailability of BCM-95CG (Biocurcumax), A Novel Bioenhanced Preparation of Curcumin. Indian J. Pharm. Sci. 2008, 70, 445–449. [Google Scholar] [CrossRef]

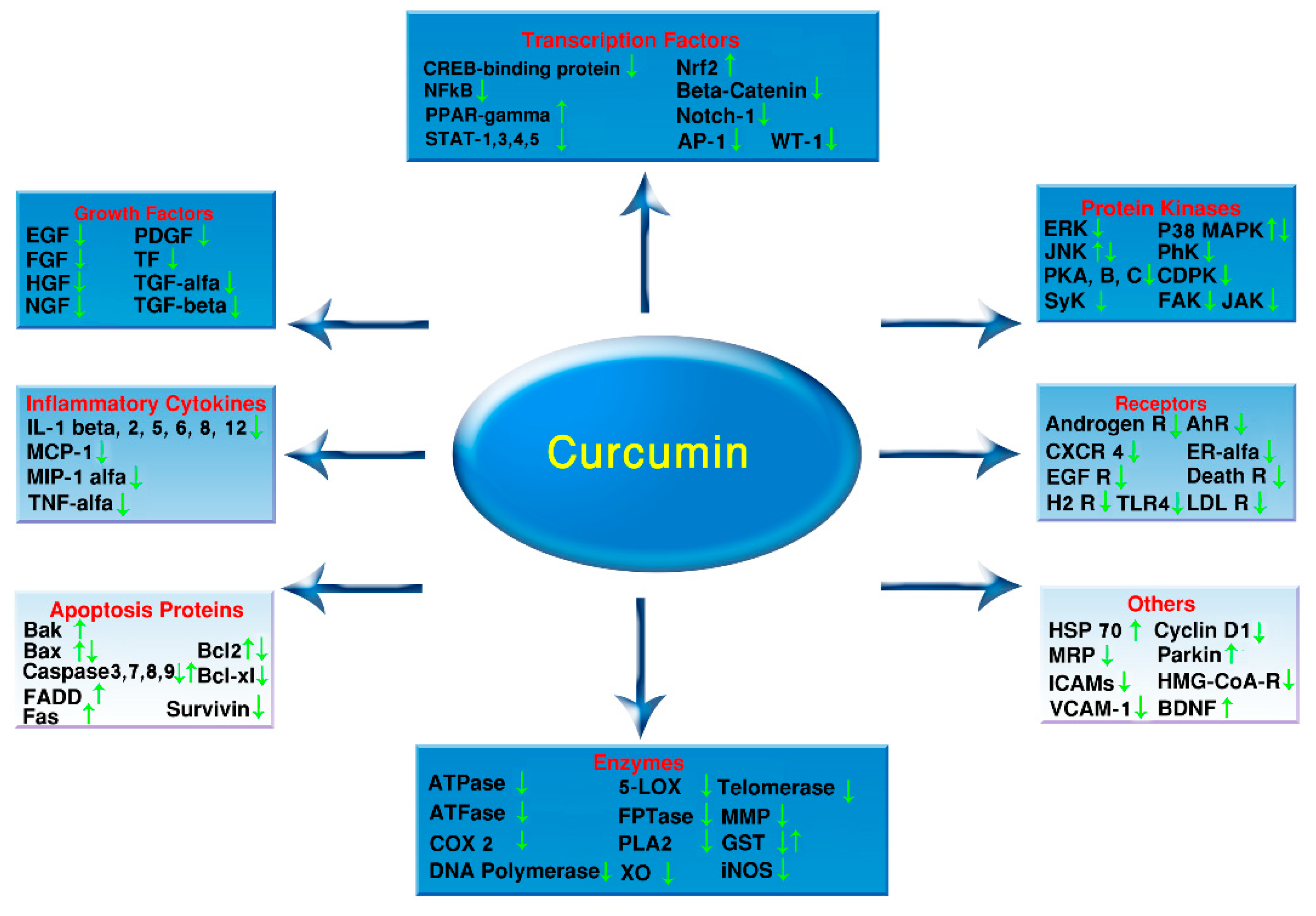
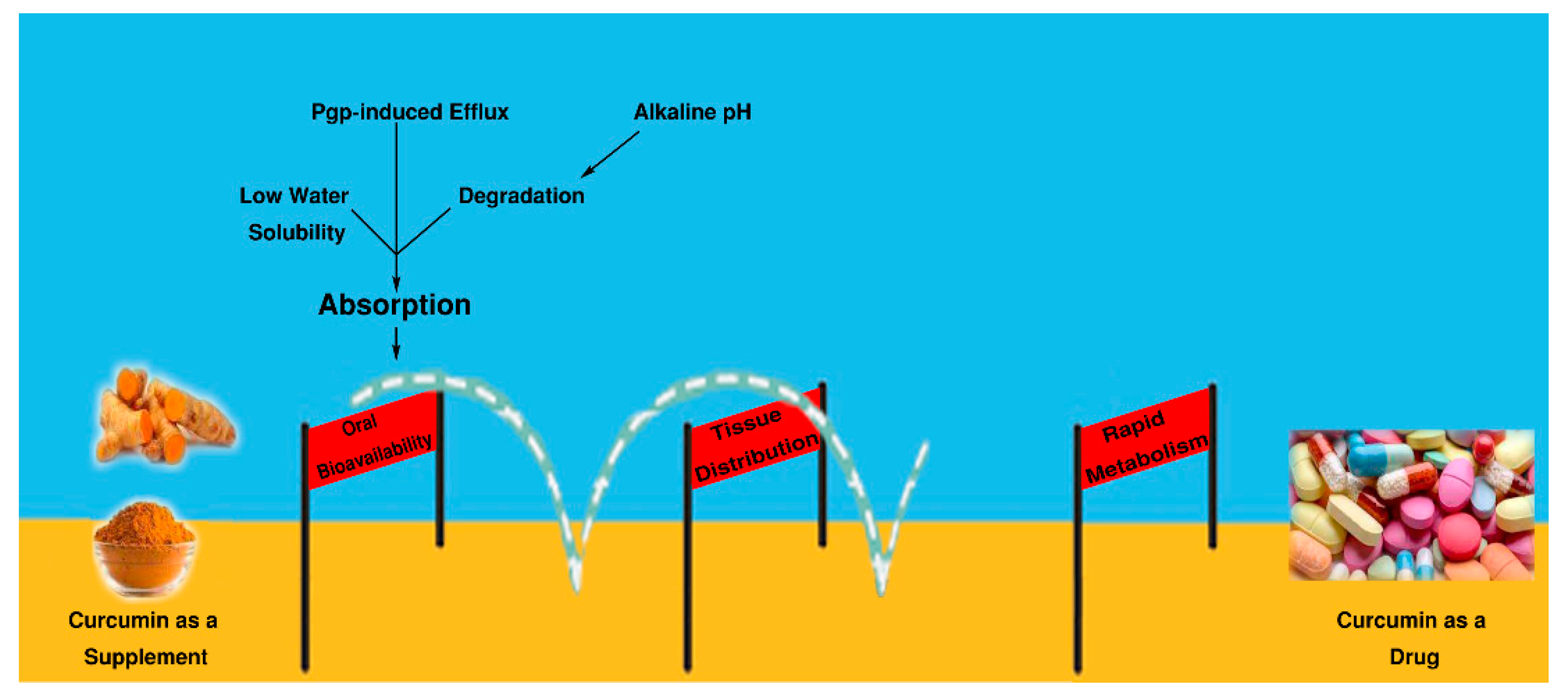
| Product | Dose or Concentration Used | Effect and Findings | Type of Study | Studied by |
|---|---|---|---|---|
| Curcumin | In vitro: 0.1, 1, 10 μM for 2 for 1 h In vivo: 10 mg/kg orally daily for 6 weeks | Glaucoma: curcumin, increased the cell viability and decreased intracellular ROS and apoptosis significantly. In vivo study, curcumin protected rat BV-2 microglia from death significantly | In vitro/Animal model | Yue YK et al. 2014 [151] |
| Curcumin | Curcumin (0.01%, 0.05% and 0.25%, which are equivalent to 100, 500 and 2500 ppm in diets) for 2 days before the injury | Glaucoma: Curcumin protected retinal neurons and microvessels against Ischemia/Reperfusion injury through inhibition of injury-induced activation of NF-κB and STAT3, and on over-expression of MCP-1. | Animal model | Wang L et al. 2011 [152] |
| Curcumin | Concentration 0–100 μM for 24 h | Age-related macular degeneration: Curcumin improved cell viability and reduced apoptosis and oxidative stress and had a significant influence on expression of apoptosis-associated proteins and oxidative stress biomarkers. | In vitro | Zhu W et al. 2015 [153] |
| Curcumin | Dose: 1 g/kg orally, daily for 16 weeks | Diabetic retinopathy: curcumin positively controlled the antioxidant system, pro-inflammatory cytokines, tumor necrosis factor-α and vascular endothelial growth factor in the diabetic retinae | Animal model | Gupta SK et al. 2011 [154] |
| Curcumin + sodium selenite | Concentrations Curcumin 100, 200 μM sodium selenite 100 μM | Cataract: Curcumin suppressed selenium-induced oxidative stress and cataract formation through preventing depletion of antioxidants, and inhibiting generation of free radicals, and by inhibiting iNOS expression | In vitro | Manikandan R et al. 2009 [155] |
| Curcumin and Turmeric extract | 0.002%–0.01% curcumin and 0.5% turmeric in diet | Cataract: turmeric and curcumin were effective against the diabetic cataract development in rats. | Animal model | Suryanarayana P et al. 2005 [156] |
| Curcumin nanoparticles (NP) | In vitro: curcumin 5–20 μM for 24 h In vivo: 20-μL solution containing 80 μg curcumin for 14 days | Corneal neovascularization: NP increased the retention of curcumin in the cornea and suppressed the expression of VEGF, inflammatory cytokines, and MMP so prevented corneal neovascularization through suppressing the NFκB pathway. | In vitro/Animal model | Pradhan N et al. 2015 [157] |
| Curcumin | Concentrations 1–30 μM for 24 h | Dry eye disease: Curcumin has the potential for dry eye disease. It prevented the hyperosmoticity-induced increase of NF-κB and IL-1β production | In vitro | Chen M et al. 2010 [158] |
| Curcumin | Dose:10, 20 mg/kg intraperitoneally twice on days 14 and 17, beginning 1 h before the challenge in the conjunctival sac | Conjunctivitis: curcumin suppressed the allergic conjunctival inflammation in an experimental model. | Animal model | Chung SH et al. 2012 [159] |
| Curcumin | Dose: 2.5 and 10 μM) injected into the vitreous of C57BL/6 mice. | Retinal degeneration: curcumin attenuated retinal ganglion cell and amacrine cell death by restoring NF-κB expression. | Animal model | Burugula B et al. 2011 [160] |
| Curcumin Nanoparticle | In vitro: curcumin 0–20 μM for 24 h In vivo: topical eye drop daily for 21 days | Neuroprotective in eye disease: Curcumin-loaded nanocarriers protected a retinal cell line against glutamate and hypoxia-induced injury | In vitro/Animal model | Davis BM et al. 2018 [161] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassanzadeh, K.; Buccarello, L.; Dragotto, J.; Mohammadi, A.; Corbo, M.; Feligioni, M. Obstacles against the Marketing of Curcumin as a Drug. Int. J. Mol. Sci. 2020, 21, 6619. https://doi.org/10.3390/ijms21186619
Hassanzadeh K, Buccarello L, Dragotto J, Mohammadi A, Corbo M, Feligioni M. Obstacles against the Marketing of Curcumin as a Drug. International Journal of Molecular Sciences. 2020; 21(18):6619. https://doi.org/10.3390/ijms21186619
Chicago/Turabian StyleHassanzadeh, Kambiz, Lucia Buccarello, Jessica Dragotto, Asadollah Mohammadi, Massimo Corbo, and Marco Feligioni. 2020. "Obstacles against the Marketing of Curcumin as a Drug" International Journal of Molecular Sciences 21, no. 18: 6619. https://doi.org/10.3390/ijms21186619
APA StyleHassanzadeh, K., Buccarello, L., Dragotto, J., Mohammadi, A., Corbo, M., & Feligioni, M. (2020). Obstacles against the Marketing of Curcumin as a Drug. International Journal of Molecular Sciences, 21(18), 6619. https://doi.org/10.3390/ijms21186619





