Abstract
Based on the assumption that characterizing the history of a disease will help in improving practice while offering a clue to research, this article aims at reviewing the history of nonalcoholic fatty liver disease (NAFLD) in adults and children. To this end, we address the history of NAFLD histopathology, which begins in 1980 with Ludwig’s seminal studies, although previous studies date back to the 19th century. Moreover, the principal milestones in the definition of genetic NAFLD are summarized. Next, a specific account is given of the evolution, over time, of our understanding of the association of NAFLD with metabolic syndrome, spanning from the outdated concept of “NAFLD as a manifestation of the Metabolic Syndrome”, to the more appropriate consideration that NAFLD has, with metabolic syndrome, a mutual and bi-directional relationship. In addition, we also report on the evolution from first intuitions to more recent studies, supporting NAFLD as an independent risk factor for cardiovascular disease. This association probably has deep roots, going back to ancient Middle Eastern cultures, wherein the liver had a significance similar to that which the heart holds in contemporary society. Conversely, the notions that NAFLD is a forerunner of hepatocellular carcinoma and extra-hepatic cancers is definitely more modern. Interestingly, guidelines issued by hepatological societies have lagged behind the identification of NAFLD by decades. A comparative analysis of these documents defines both shared attitudes (e.g., ultrasonography and lifestyle changes as the first approaches) and diverging key points (e.g., the threshold of alcohol consumption, screening methods, optimal non-invasive assessment of liver fibrosis and drug treatment options). Finally, the principal historical steps in the general, cellular and molecular pathogenesis of NAFLD are reviewed. We conclude that an in-depth understanding of the history of the disease permits us to better comprehend the disease itself, as well as to anticipate the lines of development of future NAFLD research.
1. Background
1.1. Definition
Formerly named nonalcoholic fatty liver disease (NAFLD), the spectrum of fatty liver disorders not resulting from alcohol abuse, viral, autoimmune, drug-induced and genetic etiologies, has recently been renamed metabolic (dysfunction) associated fatty liver disease (MAFLD) [1]. In agreement with a consistent line of opinions, this novel nomenclature correctly points out the “positive” determinants of the disease, namely the close association with metabolic disorders, rather than defining it for what it is not (i.e., nonalcoholic) [2]. Table 1 [1,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] lists some of the definitions that have either been proposed or used to designate NAFLD/MAFLD over time.

Table 1.
Names used in the past to designate NAFLD and MAFLD [1,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21].
1.2. Burden
Obesity is an independent predictor of disease, accounting for the incremental changes in NAFLD over time in the USA [23]. However, NAFLD is not only common in USA and Europe, where it affects roughly one quarter of the general population [24]: in certain areas of the world, such as in South America, urban India and Sri Lanka, Israel and Turkey, prevalence rates of NAFLD range from 30% to 48% [25]. As a result of its epidemic distribution, NAFLD has become a major clinical and public health issue worldwide [26,27,28,29,30,31].
1.3. Aim
Given that the clue to future research is deeply eradicated in NAFLD history [32], and that understanding its historical developments over time will promote optimal practice, a group of researchers worked together to identify the principal steps in the study of NAFLD in adults and children.
The history of NAFLD includes myriads of milestone advances and innumerable major breakthroughs which, collectively, would be virtually impossible to review. Therefore, four major areas of interest have been identified: histopathology; clinical correlates—natural course; guidelines, and general, cellular and molecular pathogenesis. Although these areas are mutually overlapping, this schematic partitioning serves to provide a more legible analysis.
2. History of NAFLD Histopathology
2.1. Before 1980
Addison was the first to describe fatty liver in 1836 [3]. Subsequently, for decades, pathologists pinpointed the similarities of liver histology changes seen in diabetic and morbidly obese individuals with those of alcoholics. In 1838, in autopsy specimens, the pathologist Rokitansky documented hepatic fat accumulation that might be causative of cirrhosis [33]. In 1884, Pepper described fatty infiltration of the liver in a diabetic patient [34]. In 1885, Bartholow reported a potential association between obesity and fatty liver [35]. In 1938, Connor described fatty liver infiltration that might led to the development of cirrhosis in diabetics. He reported on two cases of bleeding esophageal varices (one case was fatal owing to severe hemorrhage) in patients with diabetes and fatty liver. Perilobular fibrosis described in these patients was explained by both mechanical factors and tissue anoxia [4]. In 1958, Westwater and Feiner reported the histological findings of fatty infiltration of the liver in obese patients [36]. In 1962, Thaler added a further clinical and pathological description of the disease [36]. Since then, several reports in the 1950s–1970s pathologically documented the occurrence of fatty liver disease in obese and diabetic subjects [36].
2.2. 1980 and Beyond
In 1980, the term nonalcoholic steatohepatitis (NASH) was coined by Ludwig et al., to describe the progressive form of fatty liver disease histologically resembling alcoholic steatohepatitis though observed in patients who denied any alcohol abuse [7]. The majority of patients were obese women, and many were diabetic. The histopathological changes included lobular hepatitis, inflammatory infiltrates, Mallory bodies and focal necrosis with evidence of fibrosis in most specimens and cirrhosis in three patients [7]. In 1983, Moran et al., extended these findings to obese children in whom steatohepatitis presented with abnormal liver enzymes and non-specific symptoms [37]. Schaffner and Thaler were first to use the name “nonalcoholic fatty liver disease” in 1986 [9].
Over time, several histological scores for disease assessment have been developed and, currently, at least four main semi-quantitative scoring systems for the assessment of the histological features of NAFLD are available. The NAFLD activity score, comprised 14 histological features, 4 of which were evaluated semi-quantitatively: steatosis (0–3), lobular inflammation (0–2), hepatocellular ballooning (0–2), and fibrosis (0–4). Another nine features were recorded as present-or-absent. This score was developed by the NASH Clinical Research Network (NASH-CRN) [38]. The “Fatty Liver Inhibition of Progression (FLIP)” algorithm, which was developed by the FLIP consortium, is based on a scoring system (including steatosis, ballooning and lobular inflammation), the SAF score (steatosis, activity, fibrosis) [39]. The so called “Brunt” system score included ten histological variables to determine the inflammatory grading with a score for staging fibrosis [40]. Finally, the pediatric NAFLD histological score was based on the evaluation of steatosis, ballooning, portal inflammation and lobular inflammation [41].
There is general consensus that a constellation of histological features is required for the histopathological identification of adult NASH, including steatosis, ballooning, lobular inflammation and perisinusoidal fibrosis. In contrast, there is no universal agreement among liver pathologists regarding the essential criteria for the diagnosis of NASH. In addition, compared to other histological features, such as fibrosis, the histological diagnosis of NASH exhibits a large inter- and intra-observer variability and sampling error, which is reflected by the widely ranging prevalence of NASH, from 1.4% to 20% of liver biopsies [42]. This lack of reliability in the assessment of NASH may also affect NASH trials, by introducing patients who do not meet entry criteria, misclassifying fibrosis subgroups, and attenuating apparent treatment effects [43]. For instance, in the sole Phase 3 clinical trial for NAFLD to date that showed significant results, obeticholic acid failed to demonstrate a significant impact on NASH resolution, though it had a significant effect on fibrosis [44,45]. Future studies should identify reliable non-invasive tests for the prediction of NASH.
In this context, a panel of international experts from 22 countries across the globe recently proposed to abandon the simple and inaccurate dichotomous classification into ‘NASH’ versus ‘non-NASH’. These authors, aiming at improving the assessment of severity of disease, argue that the gamut of liver lesions should rather be assessed as a continuous and dynamic variable, such as is done in other diseases, therefore minimizing the negative implication of this conceptually wrong dichotomization [1,46].
Interestingly, steatosis may not persist during the progression of NAFLD, and rather may vanish in advanced cases of NAFLD-cirrhosis. This may lead to the blurring of the distinction between cryptogenic cirrhosis versus burned-out NAFLD-cirrhosis. Recently, various reports have demonstrated that features and the course of the two entities are different [47,48]. Unfortunately, this group of patients is usually excluded from clinical trials, as they lack the key criterion of “presence of steatosis”. The international consensus panel clarified this aspect by proposing that patients with cirrhosis, even in the absence of typical histological features of steatohepatitis, should be considered as MAFLD-related cirrhosis if they meet at least one of the following criteria: past or present evidence of metabolic dysregulation (according to MAFLD criteria), with either documentation of MAFLD in previous biopsy or steatosis by imaging techniques [17,46].
2.3. History of Genetic NAFLD
NAFLD pathobiology has a high level of inheritability, and the genetic determinants of disease development and progression are increasingly recognized. Similar to other complex diseases, the genetic studies of NAFLD have passed through two major stages: the candidate gene approach first, followed by genome-wide association studies (GWAS) [49]. The former approach is driven by hypotheses based on the a priori knowledge of the biological functions regulated by candidate genes. Numerous variants of genes which can govern (therefore candidates) either susceptibility to or progression of NAFLD have been identified using this approach [50]. However, most of these studies were underpowered owing to small size, which has been reflected by the inconsistency of published reports.
The first GWAS in hepatology aimed at investigating the genetic basis of susceptibility to NAFLD dates back to 2008 [51]. Since then, hypothesis-free method-based discoveries, including GWAS, whole-genome and whole-exome sequencing have become the default methodology to determine genotype–phenotype associations. In these tests, correlations are performed between large numbers of single-nucleotide polymorphisms (SNPs), up to hundreds of thousands to over a million across the genome, and a single trait. This has led to an advancement in our understanding of the genetic underpinnings of NAFLD, with at least five variants in different genes having been robustly associated with the susceptibility to development and progression of NAFLD. These include: patatin-like phospholipase domain-containing protein 3 (PNPLA3), transmembrane 6 superfamily member 2 (TM6SF2), glucokinase regulator (GCKR), and hydroxysteroid 17β- dehydrogenase (HSD17B13) [51,52,53,54,55]. In addition, this approach helped in characterizing the genetic basis shared by NAFLD with other liver diseases as well as with other metabolic disorders, by identifying a role for variants in membrane bound O-acyltransferase domain-containing 7 (MBOAT7) [56,57,58], IFNL3/IFNL4 [59,60] and FNDC5 in NAFLD [61]. That said, it remains uncertain whether “genetic NAFLD” is perfectly equivalent to “metabolic NAFLD” as far as, for example, cardiovascular risk is concerned [62].
In the post-GWAS era, we are currently harvesting the benefits of the GWAS discoveries, including the incorporation of genetics in diagnostic and prognostic models [63,64], with an emerging role for polygenic scores [65,66]. In addition, genetic findings are well positioned to lead the path for modernization of the process of drug development, with recent evidence suggesting that a drug target with a genetic link has a double likelihood of success in clinical trials compared to other drugs that lack such a link [67,68]. Finally, the era of phenome-wide association study (PheWAS), moving from investigating a single phenotype to considering multiple phenotypes, is emerging [52].
3. History of Clinical Correlates and Natural Course of NAFLD
3.1. From the Metabolic Syndrome to NAFLD
The history of the metabolic syndrome is intriguing and complex. The first recognition of obesity and visceral adiposity as cardiovascular risk factors probably dates back to almost 2.400–260 years ago, respectively (Table 2 [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98] and Figure 1 [73]).

Table 2.
Principal advances in the history of Metabolic Syndrome [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98].
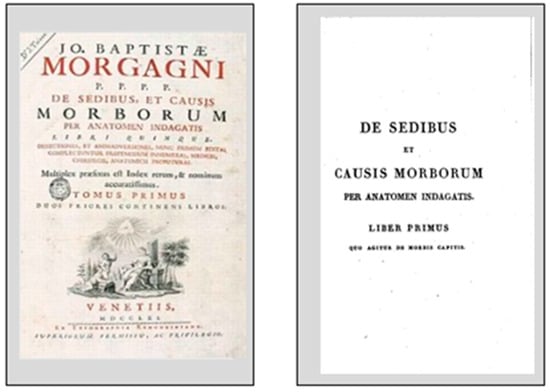
Figure 1.
Joannes Baptista Morgagni’s ‘De Sedibus et Causis Morborum per Anatomen Indagata’.
In 1765, the Italian medical genius, JB Morgagni, lucidly identified the principal features of what we would now define as metabolic syndrome. He reported on the anatomical basis of “android obesity” and associated such pathological findings with hypertension, hyperuricemia, atherosclerosis and obstructive sleep apnea syndrome, long before the modern recognition of this syndrome [73]. This outstanding achievement descended from Morgagni’s mechanistic view of human physiology and pathology. He envisaged health as the result of the well-balanced functioning of the various organs. Conversely, any disease resulted from specific tissue damage, and this is still largely accepted in contemporary medical sciences [73].
However, most contributions belong to the 20th century. During the 1920s, Austrian, Swedish and Spanish authors reported on the association of arterial hypertension, diabetes, obesity, hyperuricemia, and vascular disease [99]. In the same decade, based on insurance data, it was observed that albuminuria/kidney disease, diabetes, cardio-circulatory disease, and high blood pressure clustered in overweight and obese individuals [100]. In 1939, Himsworth identified two different types of diabetes and established an association between insulin resistance and risk of type 2 diabetes [99]. In his seminal studies, conducted for almost 35 years, Vague and his group established a firm association between central distribution of body fat and unfavorable metabolic effects. However, it was not until the early 1980s that, owing to contributions by Kissebah and Bjorntorp, this concept became accepted [76].
The nomenclature of metabolic syndrome has been variable over time, including names such as hypertension–hyperglycaemia–hyperuricaemia syndrome, metabolic trisyndrome, plurimetabolic syndrome, syndrome of affluence, syndrome X, deadly quartet and insulin resistance syndrome [99]. More recent advances in operative definitions of metabolic syndrome are illustrated in Table 2 [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98]. Studies highlighting the association of metabolic syndrome and NAFLD are shown in Table 3 [6,7,11,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122]. Collectively, these studies were deemed to be consistent with the notion that NAFLD was “the hepatic manifestation of the Metabolic Syndrome”, which agrees with the popular motto that “fatty people have fatty livers”.

Table 3.
Principal advances in the history of the association of NAFLD with the Metabolic Syndrome.
3.2. From NAFLD to the Metabolic Syndrome
A more recent line of research, however, has shown that the association of NAFLD with metabolic syndrome is mutual and bi-directional. For example, in the early 2000s, it became clear that surrogate indices of hepatic dysfunction predicted incident T2D and metabolic syndrome [123,124]. Bringing these epidemiological data further, it was possible to conduct theoretical as well as meta-analytic studies, showing that NAFLD was indeed a potential precursor of T2D and metabolic syndrome and that the stage of fibrosis was a strong determinant of such a risk [94,125,126].
3.3. NAFLD and Cardiovascular Risk
The liver was deemed to harbor life and soul in ancient Middle Eastern cultures, thus assuming a significance similar to that which the heart holds in our contemporary Western society [127,128]. On this historical background, a strong link between NAFLD and cardio-metabolic risk has recently been identified [129,130].
In 1995, Lonardo et al. hypothesized that NAFLD could be a clue that is useful in detecting cardiovascular disease [11]. In 2004 and 2005, Targher et al. were first to report that NAFLD was significantly associated with early carotid atherosclerosis in healthy men, and an increased risk of cardiovascular disease in patients with T2D, independent of classical risk factors, and that the occurrence of metabolic syndrome could account for this, to a partial extent [131,132]. Moreover, these authors also identified the stage of liver fibrosis as an independent predictor of carotid intima-media thickness, after the adjustment for potentially confounding factors such as metabolic syndrome [133]. Since 2005, several studies have confirmed that NAFLD is strongly associated not only with subclinical atherosclerosis [134], but also with major cardiovascular events. In 2016, Targher et al., by meta-analyzing 16 unique, observational studies, enrolling a total of 34,043 adult individuals (36.3% had NAFLD), and evaluating nearly 2600 CVD events (>70% of which were CVD deaths) followed-up over a median period of 6.9 years, found that NAFLD patients, compared to controls without NAFLD, exhibited an increased risk of fatal and/or non-fatal CVD events. Moreover, those individuals who had “more severe” NAFLD, defined based on imaging techniques plus either elevated serum gamma-glutamyltransferase concentrations or high NAFLD fibrosis score or high 2-deoxy-2-[fluorine-18]fluoro-D-glucose uptake on positron emission tomography, or by biopsy-proven fibrosis stages, were also more likely to develop fatal and non-fatal events of cardiovascular disease [135]. Therefore, modern studies seemingly confirm the historical notion that the liver is involved in cardiocirculatory physiopathology [127].
3.4. NAFLD and Cancer
By the early 2000s, it had already become clear that NAFLD was associated with both hepatic and extra-hepatic cancers.
3.4.1. Hepatocellular Carcinoma
In 2002, two seminal studies reported on the risk of hepatocellular carcinoma (HCC) developing in the setting of NAFLD.
Bugianesi et al., by retrospectively identifying 44 patients with HCC occurring in the setting of cryptogenic cirrhosis (CC) out of 641 cirrhosis-associated HCCs, observed that hypertriglyceridemia, diabetes, and normal aminotransferases were the risk factors independently associated with HCC arising in CC, suggesting that HCC may represent a late complication of NASH-cirrhosis [136].
Marrero et al., by studying 105 consecutive cases of HCC, reported that either histological or clinical features associated with NAFLD were common among patients with CC; moreover, HCCs manifesting among patients with CC were larger at diagnosis given that they were less likely to have undergone HCC surveillance, and therefore these were less likely to be candidates for surgical or local ablative therapies [137].
Presently, the development of HCC in a subset of individuals is a definite feature of the natural course of NAFLD [129]. A meta-analytic review reported that, compared to other etiologies of liver disease, in non-cirrhotic subjects, those with NASH have a higher risk of HCC [138]. The risk factors for the development of HCC in those with NAFLD include genetics, lifestyle, liver-related and metabolic determinants [139,140].
3.4.2. NAFLD and Extra-Hepatic Cancer
In their pioneer study, Sørensen et al., by using the Danish National Registry of Patients, compared the Danish general population data of 7326 individuals who had received a hospital diagnosis of: alcoholic (ICD-8 _ 571.10), nonalcoholic (ICD-8 _571.11), or unspecified fatty liver (ICD-8 _ 571.19) at least once during the 16-year study period. Data have shown that patients with nonalcoholic/unspecified fatty liver had an increased risk of pancreatic cancer (standardized incidence ratio (SIR) 3.0; 95% CI, 1.3–5.8; vs. SIR 1.5; 95% CI, 0.7–3.0) and kidney cancer (SIR 2.7; 95% CI, 1.1–5.6) [141].
Presently, a variety of extra-hepatic cancers, including colorectal adenoma and carcinoma, are increasingly identified as a systemic manifestation of NAFLD [142,143]. Recent data suggest that NAFLD—more than obesity—is associated with an increased risk of extra-hepatic cancers, such as those of the gastrointestinal tract and uterus [144]. A meta-analytic review of observational studies of asymptomatic individuals submitted to colonoscopy, owing to screening purposes reported that NAFLD was independently associated with a mildly increased risk of incident and prevalent colorectal adenomas and cancer [145]. Various pathogenic mechanisms underlie the association of NAFLD with large bowel carcinogenesis, including sub-clinical systemic inflammation, IR, adipokines, bile acids and liver fibrosis [146,147].
4. History of Guidelines on NAFLD Issued by Scientific Societies
Over time, scientific societies from different geographic areas have issued guidelines focusing on the criteria for diagnosis and management of NAFLD in adults, aimed at regulating clinical decision making. It is notable that a gap of decades separates the first clinico-pathological recognitions of NAFLD from recommendations issued by scientific societies. Probably, this mirrors the initial scarcity of evidence-based data to support strong recommendations. Distinctive features of the wide spectrum of NAFLD include expanding epidemiological trajectories, continuous progress in non-invasive diagnostic tools, as well as findings from basic research and clinical therapeutic trials of novel candidate drug regimens. All these concur in rendering publications and the updating of NAFLD guidelines a formidable multidisciplinary effort and an ongoing challenge for scientific hepatological societies.
The first NAFLD guidelines were released by the Asian Pacific Association Study of the Liver (APASL) in 2007. This document was a summary of proposals by the Asian–Pacific Working Party for NAFLD, and was accompanied by reviews which summarized and annotated evidence and rationale supporting recommendations [148,149]. It was an informative effort directed at clinicians regarding a new globally expanding disease. Interestingly, these authors were able to find some common grounds in NAFLD management, although strong evidence was lacking at that time. This first document proposed by Asian scientific societies paved the way for the publication of clinical practice guidelines for NAFLD in Europe.
In 2010, the European Association for the Study of the Liver (EASL) issued a position statement that summarized the proceedings of the 2009 EASL Special Conference on NAFLD/NASH. This seminal article proposed expert opinion regarding different aspects of the clinical care of NAFLD patients [18].
In 2012, a NAFLD guidelines document was published as a collaborative effort from the three major American hepatological societies: American Association for the Study of Liver Diseases (AASLD), American College of Gastroenterology and American Gastroenterological Association [150]. These comprehensive guidelines included an extensive scientific literature search and followed the standard Grading of Recommendation Assessment, Development and Evaluation (GRADE) methodology [151].
To complete this first set of international NAFLD guidelines, in 2014, The World Gastroenterology Organization published a global NAFLD guidelines document, which is unique in following a resource-sensitive approach, i.e., a hierarchical set of diagnostic, therapeutic, and management options to deal with risk and disease, ranked by the resources available (Cascade) [152].
Between 2007 and 2014, either consensus statements or practice guidelines based on the recommendations of national societies were also issued. These include: the Italian Association for the Study of the Liver (AISF) in 2010 [153], the Chinese Association of The Study of Liver Disease in 2011 [154], the Korean Association for the Study of the Liver in 2013 [155], and the Japanese Society of Gastroenterology and the Japanese Society of Hepatology in 2015 [156].
The abundance and worldwide circulation of international and national guidelines witness that NAFLD is a global challenge. Concurrently, the high number and scientific standard of basic studies, clinical trials and informative review articles collectively attest that NAFLD remains an open and evolving paradigm for clinicians, needing further multidisciplinary approaches aimed at addressing the pathogenic heterogeneity, the multiple metabolic risk factors and the rapid epidemiological diffusion of disease. Major breakthroughs in our understanding of disease and evolving the medical practice fully justify a continuous updating of guidelines. Between 2016 and 2018, EASL, APASL and AASLD published the update of their first set of clinical recommendations. In particular, EASL worked in collaboration with the European Association for the Study of Diabetes and the European Association for the Study of Obesity, in developing the first multidisciplinary clinical practice guidelines on NAFLD in 2016 [157]. The 2016 EASL guidelines pay special attention to NAFLD screening in the population at risk. In 2018, APASL and AASLD published new consensus statements based on the most recent evidence [158,159,160].
Moreover, additional national societies either published novel or updated previous documents or guidelines. This is the case for NICE guidelines in 2016 [161], AISF in 2017 [129] and the Spanish Association for the Study of the Liver in 2018 [162]. Table 4 [18,129,149,150,152,153,154,155,156,157,158,159,160,161,162,163] is a synopsis of all the published guidelines.

Table 4.
Guidelines, ordered by year of publication, published in English by different national and international Scientific Societies on NAFLD in adult population.
The comparative analysis of NAFLD guidelines is an informative academic practice, identifying both shared and diverging key points [164]. The most updated of such comparative studies clearly highlights differences in the definition of alcohol threshold, choice of screening methods, identification of the best non-invasive tool for detecting liver fibrosis and the discussion of different pharmacological approaches [165]. There is general agreement regarding the notion that non-invasive tools such as NAFLD fibrosis score (NFS) and Fibrosis 4 score (FIB-4) and transient elastography or MRI should be used to detect patients with significant liver fibrosis. Moreover, scientific societies also agree that lifestyle changes, including healthy diet, habitual physical activity and weight loss are the mainstay of treatment. However, global management of NAFLD patients still varies across different geographical areas and different national healthcare systems [165,166].
It is expected that translation into clinical practice of those shared recommendations may result in improving homogeneity in NAFLD management, as well as improved outcomes in clinical trials.
Although NAFLD has epidemic proportions in adults, children are not spared either [167]. Additionally, pediatric NAFLD has distinctive histological and pathogenic features, and is an ever escalating cause of chronic liver disease, with the potential of impacting health outcomes in adolescents and young adults [168]. This justifies the publication of NAFLD guidelines from pediatric scientific societies.
In 2017, practice guidelines on this topic were published by the North American Society for Pediatric Gastroenterology, Hepatology, Nutrition (NASPGHAN) and the update of AASLD guidelines on NAFLD included a pediatric section; this is a significant step towards providing diagnostic and therapeutic tools to optimize clinical care in children. The open questions in children are similar to those in adult populations: the identification of risk factors, screening strategies and screening tests, reference standard for the diagnosis, non-invasive biomarkers and imaging; lifestyle modifications as the first-line approach [160,169].
5. History of General, Cellular and Molecular Pathogenesis of NAFLD and NASH
Our understanding of the level of complexity of NAFLD pathogenesis has increased over time. While the earliest view had indicated the mechanistic development of steatohepatitis as a simple “two-hit” phenomenon, i.e., cell insults such as oxidative stress, lipid oxidation and inflammation superimposed on steatosis caused by IR [170], subsequent theories have clearly elucidated a more sophisticated level of complexity. In their seminal paper, Tilg and Moschen proposed that, irrespective of whether inflammation chronologically precedes or follows steatosis, many parallel hits of intestinal and/or adipose tissue origin, endoplasmic reticulum stress, (adipo)cytokines and innate immunity act in concert to regulate the distinctive features of NASH [171]. This “multiple hits hypothesis” continues to maintain its scientific credibility [172].
It would be difficult or even impossible to summarize here all the individual scientific contributions that, over time, have facilitated a more in-depth understanding of NAFLD and NASH pathogenesis. Excellent reviews may be consulted to this end [173,174,175]. That said, however, certain particularly innovative lines of research developed by distinguished groups of authors are acknowledged in Table 5.

Table 5.
Principal advancements in cellular and molecular pathogenesis of NAFLD and NASH.
6. Conclusions
Words of caution have recently been spent by eminent researchers regarding the risks inherent in a premature change of NAFLD nomenclature [216]. NAFLD and MAFLD are not exactly the same disease. A recent study conducted in 13,083 cases extracted from the NHANES III data has clearly documented this notion, by showing that MAFLD is more likely to capture those patients with hepatic steatosis, who exhibit a higher risk of disease progression [217]. Should these findings be confirmed, our understanding of relevant features of NAFLD, such as natural history and treatment response rates to lifestyle changes and experimental drug agents, may likely be in need of reassessment, if the MAFLD definition is accepted.
We have tried to recapitulate the chief historical advancements in NAFLD, spanning histology, pathophysiology, pathogenesis and guidelines. We apologize to all those eminent authors who, inadvertently, are not mentioned here: their contributions have been acknowledged elsewhere [218]. Our review article has shown that there are some unsettled issues in the history of metabolic syndrome: why, for example, were ancient Indo-European physicians apparently aware of its existence (Table 2), whereas ancient Egyptian physicians were not ? [219,220]. Is this a clue to a healthy diet? [219]; or, does this result from North Africans being genetically spared from NAFLD and hence the MetS [24,221]?
An analysis of historical perspectives of disease has also revealed that many lines of current research, such as clinico-pathological correlations, personalized medicine, and sex differences are deeply eradicated in NAFLD history ( Table 2; Table 3). On these grounds, we emphasize that understanding the historical lines of research which have eventually conducted to present views may assist, particularly but not only, younger researchers, toward identifying the most appropriate research strategies to innovate, by giving significance to the past [32]. Stated otherwise, as summarized in this adage attributed to Johann Wolfgang Goethe, “The history of a science is that science itself”.
Author Contributions
A.L. and Y.F. first discussed the idea behind this article and selected co-authors. A.L. wrote the first draft of the manuscript, including Section 1, Section 3, Section 5 and Section 6. Y.F. and K.A.A. wrote the first draft of Section 2. S.L. wrote the first draft of Section 4. All authors jointly reworked the first draft of the manuscript and contributed to retrieving additional references, as well as answering reviewers’ and editors’ comments. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We are indebted to Jacqueline Mole for her careful editing of English.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eslam, M.; Sanyal, A.J.; George, J. MAFLD: A consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 2020. [Google Scholar] [CrossRef]
- Fouad, Y.; Waked, I.; Bollipo, S.; Gomaa, A.; Ajlouni, Y.; Attia, D. What’s in a name? Renaming ‘NAFLD’ to ‘MAFLD’. Liver Int. 2020, 40, 1254–1261. [Google Scholar] [CrossRef]
- Addison, T. Observations on fatty degeneration of the liver. Guys Hosp. Rep. 1836, 1, 485. [Google Scholar]
- Connor, C.L. Fatty infiltration of the liver and the development of cirrhosis in diabetes and chronic alcoholism. Am. J. Pathol. 1938, 14, 347–364. [Google Scholar]
- Dianzani, M.U. Sulla patogenesi dell’accumulo del grasso nella steatosi epatica. Rass. Med. Sarda. 1964, 66, 67–90. [Google Scholar]
- Adler, M.; Schaffner, F. Fatty liver hepatitis and cirrhosis in obese patients. Am. J. Med. 1979, 67, 811–816. [Google Scholar] [CrossRef]
- Ludwig, J.; Viggiano, T.R.; McGill, D.B.; Oh, B.J. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 1980, 55, 434–438. [Google Scholar]
- Batman, P.A.; Scheuer, P.J. Diabetic hepatitis preceding the onset of glucose intolerance. Histopathology 1985, 9, 237–243. [Google Scholar] [CrossRef]
- Schaffner, F.; Thaler, H. Nonalcoholic fatty liver disease. Prog. Liver Dis. 1986, 8, 283–298. [Google Scholar]
- Diehl, A.M.; Goodman, Z.; Ishak, K.G. Alcohollike liver disease in nonalcoholics. A clinical and histologic comparison with alcohol-induced liver injury. Gastroenterology 1988, 95, 1056–1062. [Google Scholar] [CrossRef]
- Lonardo, A.; Bellini, M.; Tondelli, E.; Frazzoni, M.; Grisendi, A.; Pulvirenti, M.; Della Casa, G. Nonalcoholic steatohepatitis and the “bright liver syndrome”: Should a recently expanded clinical entity be further expanded? Am. J. Gastroenterol. 1995, 90, 2072–2074. [Google Scholar]
- Mendler, M.H.; Turlin, B.; Moirand, R.; Jouanolle, A.M.; Sapey, T.; Guyader, D.; le Gall, J.Y.; Brissot, P.; David, V.; Deugnier, Y. Insulin resistance-associated hepatic iron overload. Gastroenterology 1999, 117, 1155–1163. [Google Scholar] [CrossRef]
- Neuschwander-Tetri, B.A.; Caldwell, S.H. Nonalcoholic steatohepatitis: Summary of an AASLD Single Topic Conference. Hepatology 2003, 37, 1202–1219, Correction in 2003, 38, 536. [Google Scholar] [CrossRef]
- Dixon, J.B.; O’Brien, P.E. Bhathal Letter. Gastroenterology 2002, 122, 841–842. [Google Scholar] [CrossRef]
- Farrell, G.C. Non-alcoholic steatohepatitis: What is it, and why is it important in the Asia-Pacific region? J. Gastroenterol. Hepatol. 2003, 18, 124–138. [Google Scholar] [CrossRef]
- Brunt, E.M. Nonalcoholic steatohepatitis. Semin. Liver Dis. 2004, 24, 3–20. [Google Scholar]
- Loria, P.; Lonardo, A.; Carulli, N. Should nonalcoholic fatty liver disease be renamed? Dig. Dis. 2005, 23, 72–82. [Google Scholar] [CrossRef]
- Ratziu, V.; Bellentani, S.; Cortez-Pinto, H.; Day, C.; Marchesini, G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J. Hepatol. 2010, 53, 372–384. [Google Scholar] [CrossRef]
- Brunt, E.M. What’s in a NAme? Hepatology 2009, 50, 663–667. [Google Scholar] [CrossRef]
- Balmer, M.L.; Dufour, J.F. Nicht-alkoholische Steatohepatitis—von NAFLD zu MAFLD. Ther. Umsch. 2011, 68, 183–188. [Google Scholar] [CrossRef]
- Bellentani, S.; Tiribelli, C. Is it time to change NAFLD and NASH nomenclature? Lancet. Gastroenterol. Hepatol. 2017, 2, 547–548. [Google Scholar] [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J. Toward more accurate nomenclature for fatty liver diseases. Gastroenterology 2019, 157, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Stepanova, M.; Afendy, M.; Fang, Y.; Younossi, Y.; Mir, H.; Srishord, M. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin. Gastroenterol. Hepatol. 2011, 9, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef]
- Younossi, Z.M. Non-alcoholic fatty liver disease—A global public health perspective. J. Hepatol. 2019, 70, 531–544. [Google Scholar] [CrossRef]
- Farrell, G.C.; Wong, V.W.; Chitturi, S. NAFLD in Asia—as common and important as in the West. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 307–318. [Google Scholar] [CrossRef]
- Pimpin, L.; Cortez-Pinto, H.; Negro, F.; Corbould, E.; Lazarus, J.V.; Webber, L.; Sheron, N. EASL HEPAHEALTH Steering Committee. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J. Hepatol. 2018, 69, 718–735. [Google Scholar] [CrossRef]
- Zhou, F.; Zhou, J.; Wang, W.; Zhang, X.J.; Ji, Y.X.; Zhang, P.; She, Z.G.; Zhu, L.; Cai, J.; Li, H. Unexpected Rapid Increase in the Burden of NAFLD in China From 2008 to 2018: A Systematic Review and Meta-Analysis. Hepatology 2019, 70, 1119–1133. [Google Scholar] [CrossRef]
- Arshad, T.; Golabi, P.; Henry, L.; Younossi, Z.M. Epidemiology of Non-alcoholic Fatty Liver Disease in North America. Curr. Pharm. Des. 2020, 26, 993–997, published ahead of print in Curr. Pharm. Des. 2020. [Google Scholar] [CrossRef]
- Baumeister, S.E.; Völzke, H.; Marschall, P.; John, U.; Schmidt, C.O.; Flessa, S.; Alte, D. Impact of fatty liver disease on health care utilization and costs in a general population: A 5-year observation. Gastroenterology 2008, 134, 85–94. [Google Scholar] [CrossRef]
- Stepanova, M.; De Avila, L.; Afendy, M.; Younossi, I.; Pham, H.; Cable, R.; Younossi, Z.M. Direct and indirect economic burden of chronic liver disease in the United States. Clin. Gastroenterol. Hepatol. 2017, 15, 759–766. [Google Scholar] [CrossRef] [PubMed]
- Lonardo, A.; Ballestri, S. Perspectives of nonalcoholic fatty liver disease research: A personal point of view. Explor. Med. 2020, 1, 85–107. [Google Scholar] [CrossRef]
- Rokitansky, C.A. Skizze der Größen und Formabweichungen der Leber. Bruchstück Med Jahrb des kaisl, königl Österr Staates 1839. Bd 29 oder neueste Folge Bd 20 Wien: 557.
- Pepper, W. Saccharine diabetes. Med. Rec. 1884, 25, 9–12. [Google Scholar]
- Pepper, W. A System of Practical Medicine by American Authors; Lea Brothers & Co.: Philadelphia, PA, USA, 1885; Volume II, p. 1050. [Google Scholar]
- Brunt, E.M.; Neuschwander-Tetri, B.A.; Burt, A.D. Fatty liver disease: Alcoholic and nonalcoholic. In MacSween’s Pathology of the Liver, 6th ed.; Burt, A.D., Portmann, B., Ferrell, L., Eds.; Elsevier: Amsterdam, The Netherlands, 2011; pp. 293–359. [Google Scholar]
- Moran, J.R.; Ghishan, F.K.; Halter, S.A.; Greene, H.L. Steatohepatitis in obese children: A cause of chronic liver dysfunction. Am. J. Gastroenterol. 1983, 78, 374–377. [Google Scholar] [PubMed]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Bedossa, P.; FLIP Pathology Consortium. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology 2014, 60, 565–575. [Google Scholar] [CrossRef] [PubMed]
- Brunt, E.M.; Janney, C.G.; Di Bisceglie, A.M.; Neuschwander-Tetri, B.A.; Bacon, B.R. Nonalcoholic steatohepatitis: A proposal for grading and staging the histological lesions. Am. J. Gastroenterol. 1999, 94, 2467–2474. [Google Scholar] [CrossRef]
- Alkhouri, N.; De Vito, R.; Alisi, A.; Yerian, L.; Lopez, R.; Feldstein, A.E.; Nobili, V. Development and validation of a new histological score for pediatric non-alcoholic fatty liver disease. J. Hepatol. 2012, 57, 1312–1318. [Google Scholar] [CrossRef]
- Sheka, A.C.; Adeyi, O.; Thompson, J.; Hameed, B.; Crawford, P.A.; Ikramuddin, S. Nonalcoholic Steatohepatitis: A review. JAMA 2020, 323, 1175–1183, Correction in JAMA 2020, 323, 1619. [Google Scholar] [CrossRef]
- Davison, B.A.; Harrison, S.A.; Cotter, G.; Alkhouri, N.; Sanyal, A.; Edwards, C.; Colca, J.R.; Iwashita, J.; Koch, G.G.; Dittrich, H.C. Suboptimal reliability of liver biopsy evaluation has implications for randomized clinical trials. J. Hepatol. 2020. [Google Scholar] [CrossRef]
- Eslam, M.; Alvani, R.; Shiha, G. Obeticholic acid: Towards first approval for NASH. Lancet 2019, 394, 2131–2133. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Ratziu, V.; Loomba, R.; Rinella, M.; Anstee, Q.M.; Goodman, Z.; Bedossa, P.; Geier, A.; Beckebaum, S.; Philip N Newsome, P.N.; et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: Interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 2019, 394, 2184–2196. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.S.; Dufour, J.F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Thuluvath, P.J.; Kantsevoy, S.; Thuluvath, A.J.; Savva, Y. Is cryptogenic cirrhosis different from NASH cirrhosis? J. Hepatol. 2018, 68, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, S.; Marchesini, G. Cryptogenic vs. NASH-cirrhosis: The rose exists well before its name. J. Hepatol. 2018, 68, 391–392. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Valenti, L.; Romeo, S. Genetics and epigenetics of NAFLD and NASH: Clinical impact. J. Hepatol. 2018, 68, 268–279. [Google Scholar] [CrossRef]
- Eslam, M.; George, J. Genetic and epigenetic mechanisms of NASH. Hepatol. Int. 2016, 10, 394–406. [Google Scholar] [CrossRef]
- Romeo, S.; Kozlitina, J.; Xing, C.; Pertsemlidis, A.; Cox, D.; Pennacchio, L.A.; Boerwinkle, E.; Cohen, J.C.; Hobbs, H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008, 40, 1461–1465. [Google Scholar] [CrossRef]
- Eslam, M.; George, J. Genetic contributions to NAFLD: Leveraging shared genetics to uncover systems biology. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 40–52. [Google Scholar] [CrossRef]
- Abul-Husn, N.S.; Cheng, X.; Li, A.H.; Xin, Y.; Schurmann, C.; Stevis, P.; Liu, P.; Kozlitina, Y.; Stender, S.; Wood, G.C.; et al. A protein-truncating HSD17B13 variant and protection from chronic liver disease. N. Engl. J. Med. 2018, 378, 1096–1106. [Google Scholar] [CrossRef]
- Kozlitina, J.; Smagris, E.; Stender, S.; Nordestgaard, B.G.; Zhou, H.H.; Tybjærg-Hansen, A.; Vogt, T.F.; Hobbs, H.H.; Cohen, J.C. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2014, 46, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Mangia, A.; Berg, T.; Lik, H.; Yuen, H.L.; Chan, Y.; Irving, W.L.; Dore, G.J.; Abate, M.L.; Bugianesi, E.; et al. Diverse impacts of the rs58542926 E167K variant in TM6SF2 on viral and metabolic liver disease phenotypes. Hepatology 2016, 64, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Thabet, K.; Asimakopoulos, A.; Shojaei, M.; Romero-Gomez, M.; Mangia, A.; Irving, W.L.; Thomas Berg, T.; Gregory J Dore, G.J.; Grønbæk, H.; Sheridan, D.; et al. MBOAT7 rs641738 increases risk of liver inflammation and transition to fibrosis in chronic hepatitis C. Nat. Commun. 2016, 7, 12757. [Google Scholar] [CrossRef] [PubMed]
- Thabet, K.; Chan, H.L.Y.; Petta, S.; Mangia, A.; Berg, T.; Boonstra, A.; Brouwer, W.P.; Abate, M.L.; Wong, V.W.S.; Nazmy, M.; et al. The membrane-bound O-acyltransferase domain-containing 7 variant rs641738 increases inflammation and fibrosis in chronic hepatitis B. Hepatology 2017, 65, 1840–1850. [Google Scholar] [CrossRef]
- Buch, S.; Stickel, F.; Trépo, E.; Way, M.; Herrmann, A.; Nischalke, H.D.; Brosch, M.; Jonas Rosendahl, J.; Berg, T.; Ridinger, M.; et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat. Genet. 2015, 47, 1443–1448. [Google Scholar] [CrossRef]
- Eslam, M.; Hashem, A.M.; Leung, R.; Romero-Gomez, M.; Berg, T.; Dore, G.; Chan, J.; Irving, H.L.K.; Sheridan, W.L.; Abate, D.M.L.; et al. Interferon-λ rs12979860 genotype and liver fibrosis in viral and non-viral chronic liver disease. Nat. Commun. 2015, 6, 6422. [Google Scholar] [CrossRef]
- Eslam, M.; McLeod, D.; Kelaeng, K.S.; Mangia, A.B.; Thabet, T.; Irving, K.; Dore, W.LG.J.; Sheridan, D.; Grønbæk, H.; Abate, M.L.; et al. IFN-λ3, not IFN-λ4, likely mediates IFNL3-IFNL4 haplotype-dependent hepatic inflammation and fibrosis. Nat. Genet. 2017, 49, 795–800. [Google Scholar] [CrossRef]
- Metwally, M.; Bayoumi, A.; Romero-Gomez, M.; Thabet, K.; John, M.; Adams, L.A.; Huo, X.; Aller, R.; García-Monzón, C.; Arias-Loste, M.T.; et al. A polymorphism in the Irisin-encoding gene (FNDC5) associates with hepatic steatosis by differential miRNA binding to the 3′UTR. J. Hepatol. 2019, 70, 494–500. [Google Scholar] [CrossRef]
- Lonardo, A.; Ballestri, S.; Targher, G. “Not all forms of NAFLD were created equal”. Do metabolic syndrome-related NAFLD and PNPLA3-related NAFLD exert a variable impact on the risk of early carotid atherosclerosis? Atherosclerosis 2017, 257, 253–255. [Google Scholar] [CrossRef]
- Eslam, M.; Hashem, A.M.; Romero-Gomez, M.; Berg, T.D.; Gregory, J.M.; Chan, A.; Irving, H.L.Y.; Sheridan, W.L.; Abate, D.M.L.; et al. FibroGENE: A gene-based model for staging liver fibrosis. J. Hepatol. 2016, 64, 390–398. [Google Scholar] [CrossRef]
- Eslam, M.; George, J. Genome-Wide Association Studies and Hepatitis C: Harvesting the Benefits of the Genomic Revolution. Semin. Liver Dis. 2015, 35, 402–420. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.V.; Chaffin, M.; Aragam, K.G.; Haas, M.E.; Roselli, C.; Choi, S.H.; Natarajan, P.; Lander, E.S.; Lubitz, S.A.; Ellinor, P.T. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat. Genet. 2018, 50, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.R.; Kanai, M.; Kamatani, Y.; Okada, Y.; Neale, B.M.; Daly, M.J. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 2019, 51, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; George, J. Genetic insights for drug development in NAFLD. Trends Pharmacol. Sci. 2019, 40, 506–516. [Google Scholar] [CrossRef]
- Bayoumi, A.; Grønbæk, H.; George, J.; Eslam, M. The Epigenetic Drug Discovery Landscape for Metabolic-associated Fatty Liver Disease. Trends Genet. 2020, 36, 429–441. [Google Scholar] [CrossRef]
- Haslam, D. Diabesty—A historical perspective: Part I. Diabesity Pract. 2012, 1, 141–145. [Google Scholar]
- Haslam, D.; Rigby, N. A long look at obesity. Lancet 2010, 376, 85–86. [Google Scholar] [CrossRef]
- Scholtz, M. Hippocrates’ Aphorisms. Cal. West. Med. 1940, 52, 125–126. [Google Scholar]
- Morgagni, J.B. The Seats and Causes of Diseases Investigated by Anatomy (De Sedibus et Causis Morborum per Anatomen indagata), 2nd ed.; Remondini: Padova, Italy, 1765; Volume 1. [Google Scholar]
- Enzi, G.; Busetto, L.; Inelmen, E.M.; Coin, A.; Sergi, G. Historical Perspective: Visceral Obesity and Related Comorbidity in Joannes Baptista Morgagni’s ‘De Sedibus Et Causis Morborum Per Anatomen Indagata’. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 534–535. [Google Scholar] [CrossRef]
- Haslam, D. Diabesity—A historical perspective: Part II. Diabesity Pract. 2013, 2, 23–28. [Google Scholar]
- Vague, J. La différenciation sexuelle; facteur déterminant des formes de l’obésité. Presse. Med. 1947, 55, 339. [Google Scholar] [PubMed]
- Bray, G.A. Body fat distribution and the distribution and the distribution of scientific knowledge. Obes. Res. 1996, 4, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Vague, J. The degree of masculine differentiation of obesities. A factor determining predisposition to diabetes, atherosclerosis, gout and uric calculous disease. Am. J. Clin. Nutr. 1956, 4, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Avogaro, P.; Crepaldi, G.; Enzi, G.; Tiengo, A. Associazione di iperlipemia, diabete mellito e obesita’ di medio grado. Acta. Diabetol. Lat. 1967, 4, 572–590. [Google Scholar] [CrossRef]
- Feldman, R.; Sender, A.J.; Siegelaub, A.B. Difference in diabetic and nondiabetic fat distribution patterns by skinfold measurements. Diabetes 1969, 18, 478–486. [Google Scholar] [CrossRef]
- Kissebah, A.H.; Vydelingum, N.; Murray, R.; Evans, D.J.J.; Hartz, A.; Kalkhoff, R.K.; Adams, P.W. Relation of body fat distribution to metabolic complications of obesity. J. Clin. Endocrinol. Metab. 1982, 54, 254–260. [Google Scholar] [CrossRef]
- Krotkiewski, M.; Björntorp, P.; Sjöström, L.; Smith, U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J. Clin. Investig. 1983, 72, 1150–1162. [Google Scholar] [CrossRef]
- Larsson, B.; Svärdsudd, K.; Welin, L.; Wilhelmsen, L.; Björntorp, P.; Tibblin, G. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. Br. Med. J. (Clin. Res. Ed.) 1984, 288, 1401–1404. [Google Scholar] [CrossRef]
- Fujioka, S.; Matsuzawa, Y.; Tokunaga, K.; Tarui, S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987, 36, 54–59. [Google Scholar] [CrossRef]
- Reaven, G.M. Role of insulin resistance in human disease. Diabetes 1988, 37, 1595–1607. [Google Scholar] [CrossRef]
- Kaplan, N.M. The deadly quartet. Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch. Intern. Med. 1989, 149, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Ferrannini, E.; Haffner, S.M.; Mitchell, B.D.; Stern, M.P. Hyperinsulinaemia: The key feature of a cardiovascular and metabolic syndrome. Diabetologia 1991, 34, 416–422. [Google Scholar] [CrossRef] [PubMed]
- WHO Alberti and Zimmet Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus Provisional Report of a WHO Consultation. Available online: https://apps.who.int/iris/bitstream/handle/10665/66040/WHO_NCD_NCS_99.2.pdf?sequence=1&isAllowed=y (accessed on 2 July 2020).
- Balkau, B.; Charles, M.A. Comment on the provisional report from the WHO consultation: European Group for the Study of Insulin Resistance (EGIR). Diabet. Med. 1999, 16, 442–443. [Google Scholar] [PubMed]
- Expert Panel on Detection, E. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar]
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among US adults: Findings from the Third National Health and Nutrition Examination Survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Brewer, H.B., Jr.; Cleeman, J.I.; Smith, S.C., Jr.; Lenfant, C. Definition of metabolic syndrome. Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on scientific issues related to definition. Circulation 2004, 109, 433–438. [Google Scholar] [CrossRef]
- Grundy, S.M. Diagnosis and management of the metabolic syndrome: A statement for health care professionals: An American heart association/National heart, lung, and blood institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef]
- Kahn, R.; Buse, J.; Ferrannini, E.; Stern, M. The metabolic syndrome: Time for a critical appraisal. Joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2005, 28, 2289–2304. [Google Scholar] [CrossRef]
- Lonardo, A.; Ballestri, S.; Marchesini, G.; Angulo, P.; Loria, P. Nonalcoholic fatty liver disease: A precursor of the metabolic syndrome. Dig. Liver Dis. 2015, 47, 181–190. [Google Scholar] [CrossRef]
- Reaven, G.M. The Metabolic Syndrome: Requiescat in Pace. Clin. Chem. 2005, 51, 931–938. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C. Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Simmons, R.K.; Alberti, K.G.; Gale, E.A.; Colagiuri, S.; Tuomilehto, J.; Qiao, Q.; Ramachandran, A.; Tajima, N.; Mirchov, I.B.; Ben-Nakhi, A.; et al. The metabolic syndrome: Useful concept or clinical tool? Report of a WHO Expert Consultation. Diabetologia 2010, 53, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Lopes, H.F.; Corrêa-Giannella, M.L.; Consolim-Colombo, F.M.; Egan, B.M. Visceral adiposity syndrome. Diabetol. Metab. Syndr. 2016, 8, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Sarafidis, P.A.; Nilsson, P.M. The metabolic syndrome: A glance at its history. J. Hypertens 2006, 24, 621–626. [Google Scholar] [CrossRef]
- Preble, W.E., Jr. Obesity: Observations on one thousand cases. Boston Med. Surg. J. 1923, 188, 617–621. [Google Scholar] [CrossRef]
- Zelman, S. The liver in obesity. AMA Arch. Intern. Med. 1952, 90, 141–156. [Google Scholar] [CrossRef]
- Beringer, A.; Thaler, H. Relationships between diabetes mellitus and fatty liver. Dtsch. Med. Wochenschr. 1970, 95, 836–838. [Google Scholar] [CrossRef]
- Haller, H. Epidemiology and associated risk factors of hyperlipoproteinemia. Z. Gesamte. Inn. Med. 1977, 32, 124–128. [Google Scholar]
- Itoh, S.; Tsukada, Y.; Motomura, Y.; Ichinoe, A. Five patients with nonalcoholic diabetic cirrhosis. Acta Hepatogastroenterol. 1979, 26, 90–97. [Google Scholar]
- Lee, R.G. Nonalcoholic steatohepatitis: A study of 49 patients. Hum. Pathol. 1989, 20, 594–598. [Google Scholar] [CrossRef]
- Powell, E.E.; Cooksley, W.G.; Hanson, R.; Searle, J.; Halliday, J.W.; Powell, L.W. The natural history of nonalcoholic steatohepatitis: A follow-up study of forty-two patients for up to 21 years. Hepatology 1990, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- Bacon, B.R.; Farahvash, M.J.; Janney, C.G.; Neuschwander-Tetri, B.A. Nonalcoholic steatohepatitis: An expanded clinical entity. Gastroenterology 1994, 107, 1103–1109. [Google Scholar] [CrossRef]
- Cortez-Pinto, H.; Camilo, M.E.; Baptista, A.; De Oliveira, A.G.; De Moura, M.C. Non-alcoholic fatty liver: Another feature of the metabolic syndrome? Clin. Nutr. 1999, 18, 353–358. [Google Scholar] [CrossRef]
- Lonardo, A. Fatty liver and nonalcoholic steatohepatitis. Where do we stand and where are we going? Dig. Dis. 1999, 17, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Marchesini, G.; Brizi, M.; Morselli-Labate, A.M.; Bianchi, G.; Bugianesi, E.; McCullough, A.J.; Forlani, G.; Melchionda, N. Association of nonalcoholic fatty liver disease with insulin resistance. Am. J. Med. 1999, 107, 450–455. [Google Scholar] [CrossRef]
- Marceau, P.; Biron, S.; Hould, F.S.; Marceau, S.; Simard, S.; Thung, S.; Kral, N.J.G. Liver pathology and the metabolic syndrome X in severe obesity. J. Clin. Endocrinol. Metab. 1999, 84, 1513–1517. [Google Scholar] [CrossRef]
- Lonardo, A.; Loria, P.; Leonardi, F.; Borsatti, A.; Neri, P.; Pulvirenti, M.; Verrone, A.M.; Bagni, A.; Bertolotti, M.; Ganazzi, D.; et al. Fasting insulin and uric acid levels but not indices of iron metabolism are independent predictors of non-alcoholic fatty liver disease. A case-control study. Dig. Liver. Dis. 2002, 34, 204–211. [Google Scholar] [CrossRef]
- Donati, G.; Stagni, B.; Piscaglia, F.; Venturoli, N.; Morselli-Labate, A.M.; Rasciti, L.; Bolondi, L. Increased prevalence of fatty liver in arterial hypertensive patients with normal liver enzymes: Role of insulin resistance. Gut 2004, 53, 1020–1023. [Google Scholar] [CrossRef]
- Suzuki, A.; Angulo, P.; Lymp, J.; St Sauver, J.; Muto, A.; Okada, T.; Lindor, K. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology 2005, 41, 64–71. [Google Scholar] [CrossRef]
- Kotronen, A.; Westerbacka, J.; Bergholm, R.; Pietiläinen, K.H.; Yki-Järvinen, H. Liver fat in the metabolic syndrome. J. Clin. Endocrinol. Metab. 2007, 92, 3490–3497. [Google Scholar] [CrossRef]
- Chitturi, S.; Farrell, G.C. Fatty liver now, diabetes and heart attack later? The liver as a barometer of metabolic health. J. Gastroenterol. Hepatol. 2007, 22, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Bo, S.; Uberti, B.; Biroli, G.; Pagano, G.; Cassader, M. Should nonalcoholic fatty liver disease be included in the definition of metabolic syndrome? A cross-sectional comparison with Adult Treatment Panel III criteria in nonobese nondiabetic subjects. Diabetes Care 2008, 31, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Vanni, E.; Bugianesi, E.; Kotronen, A.; De Minicis, S.; Yki-Järvinen, H.; Svegliati-Baroni, G. From the metabolic syndrome to NAFLD or vice versa? Dig. Liver Dis. 2010, 42, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, M.; Takeda, N.; Kojima, T.; Ohbora, A.; Kato, T.; Sarui, H.; Fukui, M.; Nagata, C.; Takeda, J. Identification of individuals with non-alcoholic fatty liver disease by the diagnostic criteria for the metabolic syndrome. World J. Gastroenterol. 2012, 18, 1508–1516. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, T.; Zhang, C.; Tang, F.; Zhong, N.; Li, H.; Song, X.; Lin, H.; Liu, Y.; Xue, F. Identification of reciprocal causality between non-alcoholic fatty liver disease and metabolic syndrome by a simplified Bayesian network in a Chinese population. BMJ Open 2015, 5, e008204. [Google Scholar] [CrossRef]
- Yki-Järvinen, H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet. Diabetes Endocrinol. 2014, 2, 901–910. [Google Scholar] [CrossRef]
- Ma, J.; Hwang, S.J.; Pedley, A.; Massaro, J.M.; Hoffmann; Chung, R.T.; Benjamin, E.J.; Levy, D.; Fox, C.S.; Long, M.T. Bi-directional analysis between fatty liver and cardiovascular disease risk factors. J. Hepatol. 2017, 66, 390–397. [Google Scholar] [CrossRef]
- Hanley, A.J.; Williams, K.; Festa, A.; Wagenknecht, L.E.; D’Agostino, R.B., Jr.; Haffner, S.M. Liver markers and development of the metabolic syndrome: The insulin resistance atherosclerosis study. Diabetes 2005, 54, 3140–3147. [Google Scholar] [CrossRef]
- Nakanishi, N.; Suzuki, K.; Tatara, K. Serum-glutamyltransferase and risk of metabolic syndrome and type 2 diabetes in middle-aged Japanese men. Diabetes Care 2004, 27, 1427–1432. [Google Scholar] [CrossRef]
- Ballestri, S.; Zona, S.; Targher, G.; Romagnoli, D.; Baldelli, E.; Nascimbeni, F.; Roverato, A.; Guaraldi, G.; Lonardo, A. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2016, 31, 936–944. [Google Scholar] [CrossRef]
- Mantovani, A.; Byrne, C.D.; Bonora, E.; Targher, G. Nonalcoholic Fatty Liver Disease and Risk of Incident Type 2 Diabetes: A Meta-analysis. Diabetes Care 2018, 41, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.A.; Riva, E.; Spicci, M.; Strazzabosco, M.; Giovannini, M.; Cesana, G. “The city of Hepar”: Rituals, gastronomy, and politics at the origins of the modern names for the liver. J. Hepatol. 2011, 55, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Lonardo, A.; Targher, G. From a fatty liver to a sugary blood. Dig. Liver Dis. 2018, 50, 378–380. [Google Scholar] [CrossRef] [PubMed]
- Italian Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease (NAFLD): Updates and future directions. Dig. Liver Dis. 2017, 49, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Lonardo, A.; Nascimbeni, F.; Mantovani, A.; Targher, G. Hypertension, diabetes, atherosclerosis and NASH: Cause or consequence? J. Hepatol. 2018, 68, 335–352. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Bertolini, L.; Padovani, R.; Zenari, L.; Zoppini, G.; Falezza, G. Relation of nonalcoholic hepatic steatosis to early carotid atherosclerosis in healthy men: Role of visceral fat accumulation. Diabetes Care 2004, 27, 1498–1500. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Bertolini, L.; Poli, F.; Rodella, S.; Scala, L.; Tessari, R.; Zenari, L.; Falezza, G. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes 2005, 54, 3541–3546. [Google Scholar] [CrossRef]
- Targher, G.; Bertolini, L.; Padovani, R.; Zoppini, G.; Zenari, L.; Falezza, G. Associations between liver histology and carotid intima-media thickness in patients with nonalcoholic fatty liver disease. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 2687–2688. [Google Scholar] [CrossRef]
- Ampuero, J.; Gallego-Durán, R.; Romero-Gómez, M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: Meta-analysis. Rev. Esp. Enferm. Dig. 2015, 107, 10–16. [Google Scholar]
- Targher, G.; Byrne, C.D.; Lonardo, A.; Zoppini, G.; Barbui, C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J. Hepatol. 2016, 65, 589–600. [Google Scholar] [CrossRef]
- Bugianesi, E.; Leone, N.; Vanni, E.; Marchesini, G.; Brunello, F.; Carucci, P.; Musso, A.; De Paolis, P.; Capussotti, L.; Salizzoni, M.; et al. Expanding the natural history of nonalcoholic steatohepatitis: From cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology 2002, 123, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Fontana, R.J.; Su, G.L.; Conjeevaram, H.S.; Emick, D.M.; Lok, A.S. NAFLD may be a common underlying liver disease in patients with hepatocellular carcinoma in the United States. Hepatology 2002, 36, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Stine, J.G.; Wentworth, B.J.; Zimmet, A.; Rinella, ME.; Loomba, R.; Caldwell, S.H.; Argo, C.K. Systematic review with meta-analysis: Risk of hepatocellular carcinoma in non-alcoholic steatohepatitis without cirrhosis compared to other liver diseases. Aliment. Pharmacol. Ther. 2018, 48, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Zoller, H.; Tilg, H. Nonalcoholic fatty liver disease and hepatocellular carcinoma. Metabolism 2016, 65, 1151–1160. [Google Scholar] [CrossRef]
- Younes, R.; Bugianesi, E. Should we undertake surveillance for HCC in patients with NAFLD? J. Hepatol. 2018, 68, 326–334. [Google Scholar] [CrossRef]
- Sørensen, H.T.; Mellemkjaer, L.; Jepsen, P.; Thulstrup, A.M.; Baron, J.; Olsen, J.H.; Vilstrup, H. Risk of cancer in patients hospitalized with fatty liver: A Danish cohort study. J. Clin. Gastroenterol. 2003, 36, 356–359. [Google Scholar] [CrossRef]
- Sanna, C.; Rosso, C.; Marietti, M.; Bugianesi, E. Non-Alcoholic Fatty Liver Disease and Extra-Hepatic Cancers. Int. J. Mol. Sci. 2016, 17, 717. [Google Scholar] [CrossRef]
- Ballestri, S.; Mantovani, A.; Nascimbeni, F.; Lugari, S.; Lonardo, A. Extra-hepatic manifestations and complications of nonalcoholic fatty liver disease. Future Med. Chem. 2019, 11, 2171–2192. [Google Scholar] [CrossRef]
- Allen, A.M.; Hicks, S.B.; Mara, K.C.; Larson, J.J.; Therneau, T.M. The risk of incident extrahepatic cancers is higher in non-alcoholic fatty liver disease than obesity—A longitudinal cohort study. J. Hepatol. 2019, 71, 1229–1236. [Google Scholar] [CrossRef]
- Mantovani, A.; Dauriz, M.; Byrne, C.D.; Lonardo, A.; Zoppini, G.; Bonora, E.; Targher, G. Association between nonalcoholic fatty liver disease and colorectal tumours in asymptomatic adults undergoing screening colonoscopy: A systematic review and meta-analysis. Metabolism 2018, 87, 1–12. [Google Scholar] [CrossRef]
- Kim, M.C.; Park, J.G.; Jang, B.I.; Lee, H.J.; Lee, W.K. Liver fibrosis is associated with risk for colorectal adenoma in patients with nonalcoholic fatty liver disease. Medicine 2019, 98, e14139. [Google Scholar] [CrossRef] [PubMed]
- Lonardo, A.; Roncucci, L. The “obese liver” and gastrointestinal cancer risk. Transl. Gastroenterol. Hepatol. 2020, 5, 44. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; Chitturi, S.; Lau, G.K.; Sollano, J.D. Asia-Pacific Working Party on NAFLD. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: Executive summary. J. Gastroenterol. Hepatol. 2007, 22, 775–777. [Google Scholar] [CrossRef] [PubMed]
- Chitturi, S.; Farrell, G.C.; Hashimoto, E.; Saibara, T.; Lau, G.K.; Sollano, J.D. Non-alcoholic fatty liver disease in the Asia-Pacific region: Definitions and overview of proposed guidelines. J. Gastroenterol. Hepatol. 2007, 22, 778–787. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Diehl, A.M.; Brunt, E.M.; Cusi, K.; Charlton, M.; Sanyal, AJ. The diagnosis and management of non-alcoholic fatty liver disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012, 55, 2005–2023. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Review Team; LaBrecque, D.R.; Abbas, Z.; Anania, F.; Ferenci, P.; Khan, A.G.; Goh, K.L.; Hamid, S.S.; Isakov, V.; Lizarzabal, M.; et al. World Gastroenterology Organisation global guidelines: Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J. Clin. Gastroenterol. 2014, 48, 467–473. [Google Scholar] [CrossRef]
- Loria, P.; Adinolfi, L.E.; Bellentani, S.; Bugianesi, E.; Grieco, A.; Fargion, S.; Gasbarrini, A.; Loguercio, C.; Lonardo, A.; Marchesini, G.; et al. Practice guidelines for the diagnosis and management of nonalcoholic fatty liver disease. A decalogue from the Italian Association for the Study of the Liver (AISF) Expert Committee. Dig. Liver. Dis. 2010, 42, 272–282. [Google Scholar] [CrossRef]
- Fan, J.G.; Jia, J.D.; Li, Y.M.; Wang, B.Y.; Lu, L.G.; Shi, J.P.; Chan, L.Y.; Chinese Association for the Study of Liver Disease. Guidelines for the diagnosis and management of nonalcoholic fatty liver disease. J. Dig. Dis. 2011, 12, 38–44, Update in Chin. J. Hepatol. 2010, 18, 163–166. [Google Scholar] [CrossRef]
- Korean Association for the Study of the Liver. KASL clinical practice guidelines: Management of nonalcoholic fatty liver disease The Korean Association for the Study of the Liver (KASL). Clin. Mol. Hepatol. 2013, 19, 325–348. [Google Scholar] [CrossRef]
- Watanabe, S.; Hashimoto, E.; Ikejima, K.; Uto, H.; Ono, M.; Sumida, Y.; Seike, M.; Takei, Y.; Takehara, T.; Tokushige, K.; et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. J. Gastroenterol. 2015, 50, 364–377. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Chan, W.K.; Chitturi, S.; Chawla, Y.; Dan, Y.Y.; Duseja, A.; Fan, J.; Goh, K.L.; Hamaguchi, M.; Hashimoto, E.; et al. Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-Part 1: Definition, risk factors and assessment. J. Gastroenterol. Hepatol. 2018, 33, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Chitturi, S.; Wong, V.W.; Chan, W.K.; Wong, G.L.; Wong, S.K.; Sollano, J.; Ni, Y.H.; Liu, C.J.; Lin, Y.C.; Lesmana, L.A.; et al. The Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease guidelines 2017-Part 2: Management and special groups. J. Gastroenterol. Hepatol. 2018, 33, 86–98. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (UK) Non-Alcoholic Fatty Liver Disease: Assessment and Management. Available online: https://www.nice.org.uk/guidance/ng49/resources/nonalcoholic-fatty-liver-disease-nafld-assessment-and-management-pdf-1837461227461 (accessed on 2 July 2020).
- Aller, R.; Fernández-Rodríguez, C.; Lo Iacono, O.; Bañares, R.; Abad, J.; Carrión, J.A.; García-Monzón, C.; Caballería, J.; Berenguer, M.; Rodríguez-Perálvarez, M.; et al. Consensus document. Management of non-alcoholic fatty liver disease (NAFLD). Clin. Pract. Guidel. 2018, 41, 328–349, Correction in 2018, 41, 475–476. [Google Scholar]
- Alswat, K.A.; Fallatah, H.I.; Al-Judaibi, B.; Elsiesy, H.A.; Al-Hamoudi, W.K.; Qutub, A.N.; Alturaify, N.; Al-Osaimi, A. Position statement on the diagnosis and management of non-alcoholic fatty liver disease. Saudi. Med. J. 2019, 40, 531–540. [Google Scholar] [CrossRef]
- Nascimbeni, F.; Pais, R.; Bellentani, S.; Day, C.P.; Ratziu, V.; Loria, P.; Lonardo, A. From NAFLD in clinical practice to answers from guidelines. J. Hepatol. 2013, 59, 859–871. [Google Scholar] [CrossRef]
- Leoni, S.; Tovoli, F.; Napoli, L.; Serio, I.; Ferri, S.; Bolondi, L. Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis. World J. Gastroenterol. 2018, 24, 3361–3373. [Google Scholar] [CrossRef]
- Zhu, J.Z.; Hollis-Hansen, K.; Wan, X.Y.; Fei, S.J.; Pang, X.L.; Meng, F.D.; Yu, C.H.; Li, Y.M. Clinical guidelines of non-alcoholic fatty liver disease: A systematic review. World J. Gastroenterol. 2016, 22, 8226–8233. [Google Scholar] [CrossRef]
- Anderson, E.L.; Howe, L.D.; Jones, H.E.; Higgins, J.P.; Lawlor, D.A.; Fraser, A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140908. [Google Scholar] [CrossRef] [PubMed]
- Goldner, D.; Lavine, J.E. Nonalcoholic Fatty Liver Disease in Children: Unique Considerations and Challenges. Gastroenterology 2020, 158, 1967–1983. [Google Scholar] [CrossRef] [PubMed]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar] [PubMed]
- Day, C.P.; James, O.F. Steatohepatitis: A tale of two “hits”? Gastroenterology 1998, 114, 842–845. [Google Scholar] [CrossRef]
- Tilg, H.; Moschen, A.R. Evolution of inflammation in nonalcoholic fatty liver disease: The multiple parallel hits hypothesis. Hepatology 2010, 52, 1836–1846. [Google Scholar] [CrossRef] [PubMed]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef]
- Diehl, A.M.; Day, C. Nonalcoholic Steatohepatitis. N. Engl. J. Med. 2018, 378, 781. [Google Scholar] [CrossRef]
- Sanyal, A.J. Past, present and future perspectives in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 377–386. [Google Scholar] [CrossRef]
- Chakravarthy, M.V.; Neuschwander-Tetri, B.A. The metabolic basis of nonalcoholic steatohepatitis. Endocrinol. Diab. Metab. 2020, 00, e00112. [Google Scholar] [CrossRef]
- Caldwell, S.H.; Swerdlow, R.H.; Khan, E.M.; Iezzoni, J.C.; Hespenheide, E.E.; Parks, J.K.; Parker, W.D., Jr. Mitochondrial abnormalities in non-alcoholic steatohepatitis. J. Hepatol. 1999, 31, 430–434. [Google Scholar] [CrossRef]
- Leclercq, I.A.; Farrell, G.C.; Field, J.; Bell, D.R.; Gonzalez, F.J.; Robertson, G.R. CYP2E1 and CYP4A as microsomal catalysts of lipid peroxides in murine nonalcoholic steatohepatitis. J. Clin. Investig. 2000, 105, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Robertson, G.; Leclercq, I.; Farrell, G.C. Nonalcoholic steatosis and steatohepatitis. II. Cytochrome P-450 enzymes and oxidative stress. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 281, G1135–G1139. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J.; Campbell-Sargent, C.; Mirshahi, F.; Rizzo, W.B.; Contos, M.J.; Sterling, R.K.; Luketic, V.A.; Shiffman, M.L.; Clore, J.N. Nonalcoholic steatohepatitis: Association of insulin resistance and mitochondrial abnormalities. Gastroenterology 2001, 120, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Paradis, V.; Perlemuter, G.; Bonvoust, F.; Dargere, D.; Parfait, B.; Vidaud, M.; Conti, M.; Huet, S.; Ba, N.; Buffet, C.; et al. High glucose and hyperinsulinemia stimulate connective tissue growth factor expression: A potential mechanism involved in progression to fibrosis in nonalcoholic steatohepatitis. Hepatology 2001, 34, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Crespo, J.; Cayón, A.; Fernández-Gil, P.; Hernández-Guerra, M.; Mayorga, M.; Domínguez-Díez, A.; Fernández-Escalante, J.C.; Pons-Romero, F. Gene expression of tumor necrosis factor alpha and TNF-receptors, p55 and p75, in nonalcoholic steatohepatitis patients. Hepatology 2001, 34, 1158–1163. [Google Scholar] [CrossRef]
- Marra, F.; Aleffi, S.; Bertolani, C.; Petrai, I.; Vizzutti, F. Review article: The pathogenesis of fibrosis in non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2005, 22, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, S.H.; de Freitas, L.A.; Park, S.H.; Moreno, M.L.V.; Redick, J.A.; Davis, C.A.; Sisson, B.J.; Patrie, J.T.; Cotrim, H.; Argo, C.K.; et al. Intramitochondrial crystalline inclusions in nonalcoholic steatohepatitis. Hepatology 2009, 49, 1888–1895. [Google Scholar] [CrossRef]
- Targher, G.; Bertolini, L.; Scala, L.; Poli, F.; Zenari, L.; Falezza, G. Decreased plasma adiponectin concentrations are closely associated with nonalcoholic hepatic steatosis in obese individuals. Clin. Endocrinol. 2004, 61, 700–703. [Google Scholar] [CrossRef]
- Kaser, S.; Moschen, A.; Cayon, A.; Kaser, A.; Crespo, J.; Pons-Romero, F.; Ebenbichler, C.-F.; Patsch, J.R.; Tilg, H. Adiponectin and its receptors in non-alcoholic steatohepatitis. Gut 2005, 54, 117–121. [Google Scholar] [CrossRef]
- Pagano, C.; Soardo, G.; Esposito, W.; Fallo, F.; Basan, L.; Donnini, D.; Federspil, G.; Sechi, L.A.; Vettor, R. Plasma adiponectin is decreased in nonalcoholic fatty liver disease. Eur. J. Endocrinol. 2005, 152, 113–118. [Google Scholar] [CrossRef]
- Vuppalanchi, R.; Marri, S.; Kolwankar, D.; Considine, R.V.; Chalasani, N. Is adiponectin involved in the pathogenesis of nonalcoholic steatohepatitis? A preliminary human study. J. Clin. Gastroenterol. 2005, 39, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Bugianesi, E.; Pagotto, U.; Manini, R.; Vanni, E.; Gastaldelli, A.; de Iasio, R.; Gentilcore, E.; Natale, S.; Cassader, M.; Rizzetto, M.; et al. Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J. Clin. Endocrinol. Metab. 2005, 90, 3498–3504. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Bertolini, L.; Rodella, S.; Zoppini, G.; Scala, L.; Zenari, L.; Falezza, G. Associations between plasma adiponectin concentrations and liver histology in patients with nonalcoholic fatty liver disease. Clin. Endocrinol. 2006, 64, 679–683. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Gorreta, F.; Ong, J.P.; Schlauch, K.; Del Giacco, L.; Elariny, H.; Van Meter, A.; Younoszai, A.; Goodman, Z.; Baranova, A.; et al. Hepatic gene expression in patients with obesity-related non-alcoholic steatohepatitis. Liver Int. 2005, 25, 760–771. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Baranova, A.; Ziegler, K.; Del Giacco, L.; Schlauch, K.; Born, T.L.; Elariny, H.; Gorreta, F.; VanMeter, A.; Younoszai, A.; et al. A genomic and proteomic study of the spectrum of nonalcoholic fatty liver disease. Hepatology 2005, 42, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Baffy, G. Uncoupling protein-2 and non-alcoholic fatty liver disease. Front. Biosci. 2005, 10, 2082–2096. [Google Scholar] [CrossRef]
- Puri, P.; Baillie, R.A.; Wiest, M.M.; Mirshahi, F.; Choudhury, J.; Cheung, O.; Sargeant, C.; Contos, M.J.; Sanyal, A.J. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology 2007, 46, 1081–1090. [Google Scholar] [CrossRef]
- Puri, P.; Wiest, M.M.; Cheung, O.; Mirshahi, F.; Sargeant, C.; Min, H.K.; Contos, M.J.; Sterling, R.K.; Fuchs, M.; Zhou, H.; et al. The plasma lipidomic signature of nonalcoholic steatohepatitis. Hepatology 2009, 50, 1827–1838. [Google Scholar] [CrossRef]
- Fon Tacer, K.; Rozman, D. Nonalcoholic Fatty liver disease: Focus on lipoprotein and lipid deregulation. J. Lipids 2011, 2011, 783976. [Google Scholar] [CrossRef]
- Bell, L.N.; Molleston, J.P.; Morton, M.J.; Klipsch, A.; Saxena, R.; Vuppalanchi, R.; Chalasani, N. Hepatic lipid peroxidation and cytochrome P-450 2E1 in pediatric nonalcoholic fatty liver disease and its subtypes. J. Clin. Gastroenterol. 2011, 45, 800–807. [Google Scholar] [CrossRef]
- Feldstein, A.E.; Gores, G.J. Apoptosis in alcoholic and nonalcoholic steatohepatitis. Front. Biosci. 2005, 10, 3093–3099. [Google Scholar] [CrossRef] [PubMed]
- Farrell, G.C.; Larter, C.Z.; Hou, J.Y.; Zhang, R.H.; Yeh, M.H.; Williams, J.; dela Pena, A.; Rona, F.; Osvath, S.R.; Brooling, J.; et al. Apoptosis in experimental NASH is associated with p53 activation and TRAIL receptor expression. J. Gastroenterol. Hepatol. 2009, 24, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Malhi, H.; Gores, G.J. Molecular mechanisms of lipotoxicity in nonalcoholic fatty liver disease. Semin. Liver Dis. 2008, 28, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Gentile, C.L.; Pagliassotti, M.J. The role of fatty acids in the development and progression of nonalcoholic fatty liver disease. J. Nutr. Biochem. 2008, 19, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Kallwitz, E.R.; McLachlan, A.; Cotler, S.J. Role of peroxisome proliferators-activated receptors in the pathogenesis and treatment of nonalcoholic fatty liver disease. World J. Gastroenterol. 2008, 14, 22–28. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Liddle, C. Nonalcoholic fatty liver disease: Pathogenesis and potential for nuclear receptors as therapeutic targets. Mol. Pharm. 2008, 5, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Grønbaek, H.; Thomsen, K.L.; Rungby, J.; Schmitz, O.; Vilstrup, H. Role of nonalcoholic fatty liver disease in the development of insulin resistance and diabetes. Expert Rev. Gastroenterol. Hepatol. 2008, 2, 705–711. [Google Scholar] [CrossRef]
- Kumashiro, N.; Erion, D.M.; Zhang, D.; Kahn, M.; Beddow, S.A.; Chu, X.; Still, C.D.; Gerhard, G.S.; Han, X.; Dziura, J.; et al. Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease. Proc. Natl. Acad. Sci. USA 2011, 108, 16381–16385. [Google Scholar] [CrossRef]
- Baffy, G. Kupffer cells in non-alcoholic fatty liver disease: The emerging view. J. Hepatol. 2009, 51, 212–223. [Google Scholar] [CrossRef]
- Miele, L.; Valenza, V.; La Torre, G.; Montalto, M.; Cammarota, G.; Ricci, R.; Mascianà, R.; Forgione, A.; Gabrieli, M.L.; Perotti, G.; et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 2009, 49, 1877–1887. [Google Scholar] [CrossRef]
- Syn, W.K.; Jung, Y.; Omenetti, A.; Abdelmalek, M.; Guy, C.D.; Yang, L.; Wang, J.; Witek, R.P.; Fearing, C.M.; Pereira, T.A.; et al. Hedgehog-mediated epithelial-to-mesenchymal transition and fibrogenic repair in nonalcoholic fatty liver disease. Gastroenterology 2009, 137, 1478–1488. [Google Scholar] [CrossRef] [PubMed]
- Cheung, O.; Sanyal, A.J. Role of microRNAs in non-alcoholic steatohepatitis. Curr. Pharm. Des. 2010, 16, 1952–1957. [Google Scholar] [CrossRef] [PubMed]
- Van Rooyen, D.M.; Farrell, G.C. SREBP-2: A link between insulin resistance, hepatic cholesterol, and inflammation in NASH. J. Gastroenterol. Hepatol. 2011, 26, 789–792. [Google Scholar] [CrossRef] [PubMed]
- Van Rooyen, D.M.; Larter, C.Z.; Haigh, W.G.; Yeh, M.M.; Ioannou, G.; Kuver, R.; Lee, S.P.; Teoh, N.C.; Farrell, G.C. Hepatic free cholesterol accumulates in obese, diabetic mice and causes nonalcoholic steatohepatitis. Gastroenterology 2011, 141, 1393–1403. [Google Scholar] [CrossRef]
- Van Rooyen, D.M.; Gan, L.T.; Yeh, M.M.; Haigh, W.G.; Larter, C.Z.; Ioannou, G.; Teoh, N.C.; Farrell, G.C. Pharmacological cholesterol lowering reverses fibrotic NASH in obese, diabetic mice with metabolic syndrome. J. Hepatol. 2013, 59, 144–152. [Google Scholar] [CrossRef]
- Pirola, C.J.; Gianotti, T.F.; Burgueño, A.L.; Rey-Funes, M.; Loidl, C.F.; Mallardi, P.; San Martino, J.; Castaño, G.O.; Sookoian., S. Epigenetic modification of liver mitochondrial DNA is associated with histological severity of nonalcoholic fatty liver disease. Gut 2013, 62, 1356–1363. [Google Scholar] [CrossRef]
- Kasumov, T.; Li, L.; Li, M.; Gulshan, K.; Kirwan, J.P.; Liu, X.; Previs, S.; Willard, B.; et al. Ceramide as a mediator of non-alcoholic Fatty liver disease and associated atherosclerosis. PLoS ONE 2015, 10, e0126910. [Google Scholar] [CrossRef]
- Kutlu, O.; Kaleli, H.N.; Ozer, E. Molecular Pathogenesis of Nonalcoholic Steatohepatitis-(NASH-) Related Hepatocellular Carcinoma. Can. J. Gastroenterol. Hepatol. 2018, 2018, 8543763. [Google Scholar] [CrossRef]
- Hernández, A.; Arab, J.P.; Reyes, D.; Lapitz, A.; Moshage, H.; Bañales, J.M.; Arrese, M. Extracellular Vesicles in NAFLD/ALD: From Pathobiology to Therapy. Cells 2020, 9, 817. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Rinella, M.E.; Sanyal, A.; Harrison, S.A.; Brunt, E.; Goodman, Z.; Cohen, D.E.; Loomba, R. From NAFLD to MAFLD: Implications of a premature change in terminology. Hepatology 2020, 10, 1002. [Google Scholar] [CrossRef]
- Lin, S.; Huang, J.; Wang, M.; Kumar, R.; Liu, Y.; Liu, S.; Wu, Y.; Wang, X.; Zhu, Y. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020, 10, 1111, published online ahead of print, 2020. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.S.; Qin, H.L.; Wang, T.; Li, H.T.; Li, H.; Xia, S.H.; Xiang, X.H. Bibliometric analysis of top 100 cited articles in nonalcoholic fatty liver disease research. World J. Hepatol. 2016, 8, 1478–1488. [Google Scholar] [CrossRef] [PubMed]
- David, A.R.; Kershaw, A.; Heagerty, A. The art of medicine. Atherosclerosis and diet in ancient Egyp. Lancet 2010, 375, 718–719. [Google Scholar] [CrossRef]
- Karamanou, M.; Protogerou, A.; Tsoucalas, G.; Androutsos, G.; Poulakou-Rebelakou, E. Milestones in the history of diabetes mellitus: The main contributors. World J. Diabetes 2016, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lim, U.; Monroe, K.R.; Buchthal, S.; Fan, B.; Cheng, I.; Kristal, B.S.; Lampe, J.W.; Hullar, M.A.; Franke, A.A.; Stram, D.O.; et al. Propensity for Intra-abdominal and Hepatic Adiposity Varies Among Ethnic Groups. Gastroenterology 2019, 156, 966–975. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).