Abstract
In Chronic Kidney Disease (CKD) patients, elevated blood pressure (BP) is a frequent finding and is traditionally considered a direct consequence of their sodium sensitivity. Indeed, sodium and fluid retention, causing hypervolemia, leads to the development of hypertension in CKD. On the other hand, in non-dialysis CKD patients, salt restriction reduces BP levels and enhances anti-proteinuric effect of renin–angiotensin–aldosterone system inhibitors in non-dialysis CKD patients. However, studies on the long-term effect of low salt diet (LSD) on cardio-renal prognosis showed controversial findings. The negative results might be the consequence of measurement bias (spot urine and/or single measurement), reverse epidemiology, as well as poor adherence to diet. In end-stage kidney disease (ESKD), dialysis remains the only effective means to remove dietary sodium intake. The mismatch between intake and removal of sodium leads to fluid overload, hypertension and left ventricular hypertrophy, therefore worsening the prognosis of ESKD patients. This imposes the implementation of a LSD in these patients, irrespective of the lack of trials proving the efficacy of this measure in these patients. LSD is, therefore, a rational and basic tool to correct fluid overload and hypertension in all CKD stages. The implementation of LSD should be personalized, similarly to diuretic treatment, keeping into account the volume status and true burden of hypertension evaluated by ambulatory BP monitoring.
1. Introduction
Sodium is not only considered an important mineral in maintaining the balance of body fluid, but it has also played an important role in the history of the world for its economical, religious, and symbolic importance. The concept that salt is a beneficial substance was so ingrained that although the earlier studies on the relationship between low sodium intake and reduction of blood pressure (BP) date back to 1948 [1], it was only after nearly forty years that the international community has recognized the role of salt intake in the pathophysiology of hypertension [2]. According to the World Health Organization, the restriction of sodium intake to less than 2.3 g/day of sodium corresponding to 5.8 g of salt (or 100 mmol) is one of the most cost-effective measures to improve public health [3]. Cumulating evidence highlights that higher sodium consumption contributes to higher BP [4], thus increasing the risk of cardiovascular disease (CVD) [5,6]. However, recent studies have raised some concerns about the real benefit of a low salt diet in the healthy general population [7,8,9,10]. In particular, in a large cohort study in over 100,000 patients from 18 countries the role of higher salt consumption was associated with increased BP levels [7], and poor CV outcomes [8]. At the same time, it emerged that sodium intake of <3 g forecasted a higher CV risk, drawing a U-shaped mortality curve [8]. Although these findings have also been obtained by other investigators [8,9,10], these studies are methodologically flawed by reverse causality (e.g., patients eat less salt because they are sicker and/or more malnourished), collinearity (e.g., a low sodium intake may be associated with a low protein-energy intake) and biased methods used to assess individual salt intake (e.g., single spot urine sample) [11].
In Chronic Kidney Disease (CKD) patients, high BP is a frequent finding, which is traditionally considered as a direct consequence of sodium sensitivity. Hence, a low salt diet (LSD) is widely considered a cornerstone in the treatment of hypertension in CKD.
In this review, we address the importance of the kidney in sodium regulation, the relationship of sodium intake with hypertension from earlier CKD stages to end-stage kidney disease (ESKD), and the available evidence on the benefit of salt restriction in non-dialysis CKD and in the ESKD population.
2. Adherence to Low-Salt Diet: Definition and Assessment in CKD Patients
The terms sodium and salt (generally sodium chloride) are used interchangeably, generating confusion about sodium intake. Table 1 illustrates formulas to convert sodium in salt (sodium chloride) and vice versa, according to the units of measurement.

Table 1.
Formulas to convert sodium in salt (sodium chloride) and vice versa, according to units of measurement.
The first concern in the evaluation of adherence to LSD is the method used for evaluation of sodium intake. Accordingly, the measurement of sodium excretion by 24 h urine sample collection (UNaV) is considered as the gold standard. However, UNaV may be cumbersome for the patient, and, therefore, estimation from spot urine samples using the Nerbass, Kawasaki, Tanaka, and INTERSALT formulas have been proposed to evaluate sodium intake. The rationale arises from the assumption that spot urine excretion would be proportionate to UNaV corrected for creatinine excretion. However, a cross-sectional study in CKD patients showed that these formulas might provide an inaccurate estimate of sodium intake, irrespective of severity of CKD and use of diuretics [12].
Another issue is the evaluation of salt intake by a single measurement, which is not generally considered sufficient to evaluate an individual’s usual salt intake because of the wide day-to-day variability in salt consumption and urinary excretion [13].
Among CKD cohorts, the Chronic Renal Insufficiency Cohort (CRIC) study reported that only about one out of four patients had a sodium intake <100 mmol/24 h, evaluated by three measurements [14]. As reported in Table 2, these findings are consistent with the prevalence of LSD reported in secondary analyses of trials [15,16,17,18,19], and also when CKD patients were regularly followed in nephrology clinics (<25% had a salt intake below 6 g/day) [20].

Table 2.
Studies evaluating the effect of urinary sodium excretion (UNaV) on end-stage kidney disease (ESKD) and cardiovascular (CV) outcomes in patients with or without Chronic Kidney Disease (CKD).
Novel methods for self-monitoring of salt intake have been developed to improve the adherence to the LSD; these are based on urine chloride strips, given that urinary chloride excretion is very tightly correlated with urinary sodium excretion. The potential benefit of self-monitoring is the ability to immediately achieve an adequate estimate of sodium intake immediately (75.5% sensitivity and 82.6% specificity to correctly classify patients with UNaV >100 mmol/24 h) in order to make proper dietary adjustments aimed at achieving recommended intake [23]. However, any benefit on the achievement of the BP goal with use of chloride strips has still to be proved with use of chloride strips. To answer this question, one randomized clinical trial, the SALUTE-CKD (SALt lowering by Urine sodium self-measurement Trial in Chronic Kidney DiseasE) has advanced to the final stage of development and results are expected in the next few months.
Furthermore, a recent trial performed in 99 patients has evaluated the efficacy of a web-based self-management program for dietary sodium restriction compared with routine care. After 3 months in intervention group a significant reduction of sodium intake (−40 mmol/day) and systolic BP (−8 mmHg) was registered in the intervention group, whereas no significant difference was found in control group. Surprisingly, in the following maintenance phase, no difference in sodium intake was detected between the two groups, due to the inadvertent adoption of the intervention by the control group. Notably, the largest effect was reported in the first 3 months, when participants actively used the web-based self-management program [24].
In ESKD patients, sodium intake can be estimated with a dietary questionnaire, though several factors, such as high dialysate sodium concentration and sodium plasma concentration, can affect thirsty and water intake in these patients, irrespective of their sodium intake [25].
Finally, in ESKD patients, residual kidney function must be carefully evaluated: in this subgroup of patients, dialysis is started with an incremental approach, corresponding to a low dose of dialysis (peritoneal or hemodialysis) integrated into the conservative management [26,27]. In these patients, the assessment of sodium intake by UNaV may be misleading, because of the aliquot of sodium intake removed by dialysis.
3. Hypertension and Salt in CKD
Hypertension and CKD are common chronic noncommunicable diseases strictly inter-related with each other; indeed, elevated BP is not only a frequent complication of CKD [28], but it can also act as the cause of CKD [29]. A recent meta-analysis showed that hypertensive patients have a 75% greater risk than normotensive individuals of development of de novo CKD (GFR <60 mL/min/1.73 m2), estimating a 10% increase of CKD onset for each increase of 10 mmHg of either BP component. Notably, even pre-hypertension (Systolic BP of 120–139 mm Hg and/or Diastolic BP of 80–89 mm Hg) was associated with a 25% higher risk of developing low GFR [29].
Furthermore, the prognostic role of lowering BP assumes greater importance in CKD patients if we bear in mind at least three basic points: (1) higher prevalence of hypertension in CKD than in the general population, which increases progressively from 65% to 95% as GFR falls from 85 to 15 mL/min/1.73 m2 [29]; (2) hypertension is the main known risk factor for CKD progression and for CV mortality [30]; (3) Hypertension is often resistant to the treatment in CKD patients, resulting in worsening CV prognosis [31,32].
Salt and water retention play a key role for development of hypertension in CKD. In fact, according to the classical model, under normal conditions, high salt intake temporarily increases plasma sodium level, which is soon buffered by movement of water from the intracellular to the extracellular compartment. Thus, increased plasma sodium concentration also stimulates the thirst center, leading to an increase in water intake and secretion of antidiuretic hormone, which restores plasma sodium concentration to a normal level while increasing and maintaining extracellular fluid volume. On the other hand, high salt intake suppresses the renin-angiotensin-aldosterone system (RAAS), which consequently reduces sodium tubular reabsorption, thus contributing to re-establishing sodium and water homeostasis [33].
In CKD patients, external sodium balance is preserved by expansion of the extracellular volume (ECV), which however causes the persistence of high BP levels. Therefore, hypertension in CKD is an early manifestation of ECV expansion and, at the same time, a maladaptive mechanism aimed at limiting ECV expansion that corresponds to approximately 5% to 10% of body weight, generally without peripheral edema, when cardiac and hepatic function is normal and the transcapillary Starling forces are not disrupted [34]. In spite of ECV expansion, RAAS is inappropriately activated in CKD, leading to vasoconstriction and sodium retention, which contribute significantly to the raising of BP levels [35].
As reported in a classic experiment [36], the BP response to sodium load is amplified in CKD patients. In particular, increasing sodium intake was increased from 20 to 120 mmol/day in patients with advanced renal failure, this caused a significant acute increase of BP (+12.2 ± 1.4 mmHg). On the other hand, the same increase in sodium intake in healthy people was not associated with any BP change and, even greater elevation of sodium intake up to 1120 mmol/day, did not produce any effect on BP values. This experiment is the proof of concept of the sodium sensitivity of BP in CKD. Notably, sodium sensitivity may be already detectable in the earlier CKD stages, as reported in a study comparing patients with glomerular disease vs healthy controls, which showed a significant BP reduction in response to lowering salt intake, whereas BP did not change in controls [37].
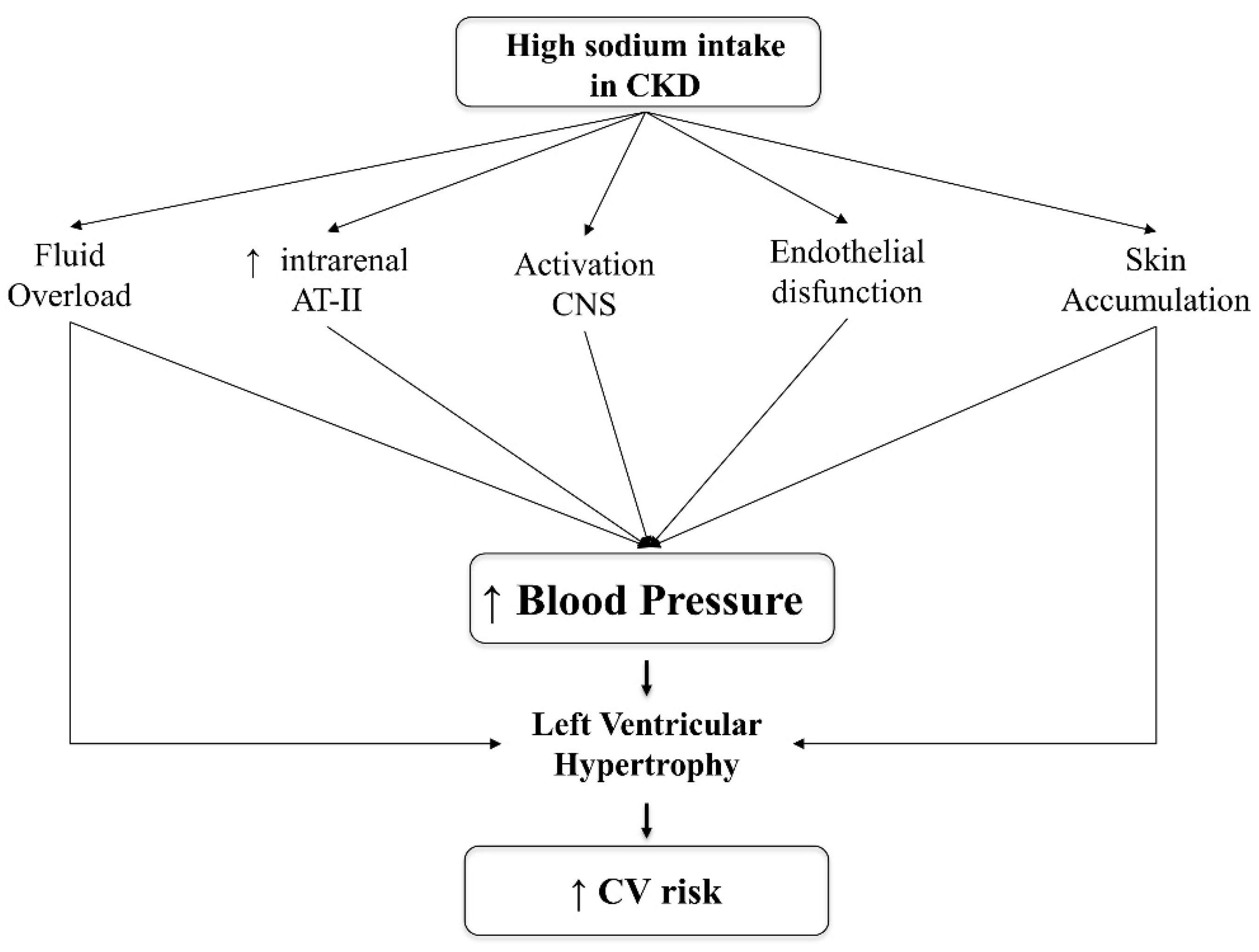
Moreover, experimental studies showed that high salt intake induces intrarenal production of Angiotensin-II [38], stimulates the synthesis of pro-inflammatory cytokines [39] and increases oxidative stress [40], as well as triggering sympathetic activity [41], whose activation is already increased in CKD, as a result of increased arterial stiffness and/or endothelial dysfunction [42].
4. Alternative Mechanism of Sodium Toxicity
Recent experimental findings suggest that skin could work as a reservoir of sodium, escaping from renal control [43]. In particular, high salt intake might cause sodium accumulation in the skin, which is detected by cells of the Monocytes Phagocytes System (MPS) located in the skin interstitium, which act as osmoreceptors by expression of the tonicity enhancer-binding protein (Ton-EBP). This transcription factor leads to Vascular Endothelial Growth Factor (VEGF) production that increases sodium clearance by the lymphatic network [44,45]. Moreover, high sodium levels in the CKD condition would promote the expression of pro-inflammatory factors, such as Interleukin-6, VEGF, and Monocyte Chemoattractant Protein-1 (MCP-1), via Ton-EBP pathway, leading to local inflammation and vascular proliferation in peritoneal, heart, and vascular tissue [46].
Figure 1 summarizes the potential mechanisms underlying the increase of BP levels and dependent CV risk associated with high salt intake in CKD.
Figure 1.
Potential pathogenic mechanisms of hypertension in CKD due to high salt intake. Abbreviations: CKD: Chronic Kidney Disease; AT-II: Angiotensin-II; CNS; Central Nervous System; CV: cardiovascular.
The concept that sodium balance is regulated by additional extra-renal mechanisms was first reported by Herr et al., whose study showed that high salt intake increased total sodium content, whereas total body water and body weight did not change [47]. More recently, a space flight simulation study has reported that in healthy subjects under controlled sodium intake, UNaV changes periodically (every 6 days), independently from BP levels and total body water [48].
The recent availability of 23Na Magnetic Resonance Imaging (MRI) in humans has allowed detection and quantification of sodium storage in the skin [49]. In particular, a higher tissue sodium content was detected in patients affected by hyperaldosteronism. Interestingly, surgical and/or medical correction of hyperaldosteronism was associated with a significant reduction in tissue sodium content; whereas body weight did not change [50]. Recently, in a cross-sectional analysis of 99 CKD patients, skin sodium content was strongly associated with left ventricular mass independently from BP levels and volume status [51]. Finally, sodium stored into the skin is modifiable in CKD patients, as reported by a recent study showing a significant reduction of skin sodium content, after a single hemodialysis session, though the mechanism by which sodium is removed from skin remains still unclear [52].
5. Clinical Effects of Low Salt Diet in Non-Dialysis CKD
We have recently completed a metanalysis comparing low versus high salt diet in 738 CKD patients [53]. Analysis included nine trials [54,55,56,57,58,59,60,61,62]. This meta-analysis showed that a moderate salt restriction of 4.4 g/day (from 179 mEq/day to 104 mEq/day) was associated with a significant lowering of 4.9 mmHg [95% C.I.: 6.8/3.1 mmHg; p < 0.001] in systolic BP and of 2.3 mmHg [95% C.I.: 6.8/3.1 mmHg; p < 0.001] in diastolic BP measured by traditional method [53]. A similar effect was found in the five out of eleven studies [57,60,61,63,64] evaluating the effect of LSD on Ambulatory BP (ABP). In particular, we found that salt restriction reduces systolic and diastolic ABP of 5.9 mmHg (95% C.I.: 2.3/9.5 mmHg; p < 0.001) and 3.0 mmHg (95% C.I.: 1.7/4.7 mmHg; p < 0.001), respectively [53].
As regards ABP studies, it is worth mentioning that in CKD cohorts, sodium sensitivity has been associated with a higher prevalence of altered circadian rhythm and nocturnal hypertension [65,66], which are predictors of poor cardio-renal prognosis [67].
Moreover, in seven out of eleven studies [54,55,56,57,58,59] reporting the effect of salt restriction on proteinuria, pooled analysis showed a significant improvement of 0.4 g/day (95% C.I.: 0.2–0.6 g/day) associated with lower salt intake [53]. These findings are in agreement with a previous meta-analysis reporting that in patients following a lower salt diet, there was an augmented antiproteinuric effect of RAAS blockers [68]. The synergic effect of LSD and RAAS inhibition may be correlated to the finding that high salt intake enhances angiotensin-converting enzyme (ACE) activity in renal tissues, in spite of decreased plasma renin and angiotensinogen concentrations, which could reduce the effect of RAAS blockers in tissues [38].
Although these effects of LSD on BP and proteinuria suggest an improvement of prognosis in CKD patients, few studies [14,15,16,17,18,19] have evaluated the long-term effect of salt restriction on the cardio-renal outcomes (Table 2).
In the CRIC study, a large observational study carried out in 3757 CKD patients followed for almost seven years, the group of patients with a UnaV of >195 mmol/day was associated with a higher risk of CKD progression [14]. Among participants of this study, 804 composite CV events (575 heart failure, 305 myocardial infarctions, and 148 strokes) occurred during a median of 6.8 years of follow-up, drawing a linear relation between higher sodium intake and higher CV risk [22]. Similarly, a post-hoc analysis of the Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan (RENAAL) and Irbesartan Diabetic Nephropathy Trial (IDNT) trials in a subgroup of 1177 patients with available 24 h urinary sodium measurements, showed that the beneficial effects of RAAS blockers on renal and cardiovascular outcomes were greater in patients with lower sodium intake [18]. Furthermore, in Autosomal Dominant Polycystic Kidney Disease (ADPKD) patients, fast progressors irrespective of intensive CKD management [69,70], a recent post-hoc analysis of the HALT-PKD trial has shown that a moderate salt restriction reduces CKD progression [21].
On the other hand, other studies have not confirmed these results, finding no association between low salt intake and improvement of the renal prognosis, in CKD patients [15,16,17]. In particular, secondary analysis of the first and second Ramipril Efficacy in Nephropathy (REIN) trials showed that low salt intake was associated with a lower risk of ESKD, but this association disappeared after adjustment for basal proteinuria [15]. In the longitudinal follow up of the Modification of Diet in Renal Disease (MDRD) Study, no association of single baseline 24 h urinary sodium excretion with kidney failure and a composite outcome of kidney failure or all-cause mortality was found [16]. Similarly, post-hoc analysis of the ongoing telmisartan alone and in combination with ramipril global endpoint trial (ONTARGET) and telmisartan randomized assessment study in ACE intolerant subjects with cardiovascular disease (TRANSCEND) studies trials showed no association between UNaV (though estimated by morning spot urine) and renal endpoints (30% decline of eGFR or ESKD) in patients with or without CKD at baseline [17]. Surprisingly, in diabetic non-CKD patients, UNaV was inversely associated with a cumulative incidence of ESKD, and in fact, patients with the lowest sodium excretion had the highest cumulative incidence of ESKD [19].
Of note, the negative studies are post hoc analyses of clinical trials designed to test the efficacy of RAAS inhibitors rather than of low-sodium intervention, confounding thus a possible association [15,16,17,18]. Furthermore, in some of these studies, UNaV was measured by a single 24 h urine [19] or spot urine sample [17]. On the other hand, we cannot exclude that other factors might play a role: a renal hemodynamic response to an acute reduction of sodium intake was impaired by aging, especially when atherosclerotic damage coexists [71]. This may expose patients to acute kidney injury and hypotension [72]. Furthermore, patients with CKD have a higher prevalence of white coat effect [73,74], exposing CKD patients to “inappropriate” antihypertensive treatment, which may potentially cause renal hypoperfusion [75]. Therefore, particular attention must be paid in the management of CKD patients, personalizing salt intake on the basis of “true” hypertensive status measured by ABPM and volemic status, and monitoring the adherence and anti-hypertensive effect LSD over time.
6. Sodium Intake in End-Stage Kidney Disease
In ESKD patients, similarly to early CKD stages (Figure 1), the deleterious effects of high salt intake are mainly related to the fluid overload, resulting in high BP levels, left ventricular hypertrophy, and increased CV mortality [76,77,78,79,80]. Therefore, sodium restriction is a major therapeutic goal in these patients. Indeed, it has been estimated that, in ESKD patients with no residual diuresis, a salt intake of <6 g should cause patients to gain no more than 0.8 kg/day in interdialytic weight.
A recent metanalysis of four trials (3 in HD/1 in PD) showed that ESKD patients with lower salt intake (N = 67) had a significant improvement of both systolic [−8.4 (−12.0; −4,8) mmHg] and diastolic BP [−4.4 (−6.6; −4.2) mmHg] levels compared with the higher salt intake group (N = 64) [81]. Moreover, a post-hoc analysis of the HEMO study revealed that low sodium intake, evaluated by a 24 h food questionnaire, allowed to decrease the need for ultrafiltration, even if it was not associated with pre-dialysis systolic BP levels [82].
Similarly, hypervolemia is prevalent in Peritoneal Dialysis (PD) patients, because of the common mismatch between intake and removal of sodium and fluid [83,84,85]. In a recent study performed in a cohort of 1054 incident PD patients, overhydration was evident in over 50% of patients starting PD [83]. This finding is relevant because persistence of volume overload heralds a 60% higher mortality risk [84]. Interestingly, recent experimental findings have reported that high sodium intake is related to direct toxicity on the peritoneal membrane, leading to chronic inflammation, fibrosis, and hypervascularization, increasing, in turn, peritoneal permeability [86].
Surprisingly, few studies have addressed the relationship between sodium intake and mortality in ESKD patients (Table 3). In hemodialysis, secondary analysis of HEMO study showed that higher dietary sodium correlated with mortality rate independently from patients’ nutritional status [82]. A retrospective study on 305 Chinese PD patients has reported that sodium intake, assessed by a 3-day diet questionnaire, was inversely associated with all-cause and cardiovascular mortality. It is noteworthy that patients with lower sodium intake also had lower serum albumin levels and reduced lean body mass, as well as lower energy and protein intake, when compared with patients with higher sodium intake, suggesting that patients with a lower dietary sodium intake were more malnourished and with reduced appetite. Moreover, the group of patients with highest salt intake had mean sodium intake of 2.5 g/day, which is lower than the mean intake reported in the general population, suggesting a possible measurement bias. This study, moreover, was flawed by methodological issues (small sample size, monocentric, few events, and overfitted cox models), further reducing the generalizability of the results [87].

Table 3.
Studies evaluating the effect of urinary sodium excretion (UNaV) on mortality in ESKD patients.
Therefore, salt restriction remains the basic approach to achieve volume control in PD patients, keeping in mind that sodium removal is lower in PD patients treated with cycler (Automated PD, APD), because of greater sodium sieving as compared with Continuous Ambulatory PD (CAPD). In these patients, high salt intake may not be counterbalanced by sodium removal, consequently leading to hypervolemia and hypertension [88].
7. Conclusions
The negative effects of sodium on BP values are amplified in CKD patients, as a result of fluid overload and of direct toxicity on the heart, the vascular system, and kidney. In non-dialysis CKD patients, LSD is beneficial for hypertension control, irrespective of BP levels, to lower proteinuria by enhancing the antiproteinuric effect of RAAS inhibition. Whether these effects can improve cardio-renal prognosis still remains unclear. Nonetheless, salt restriction assumes a greater importance in ESKD because of the common mismatch between intake and removal of sodium, which leads to hypertension, LVH, and higher CV risk. Therefore, reducing salt intake is crucial for hypertensive CKD patients from earlier stages to ESKD. However, it remains insufficiently and/or inadequately applied. More studies are therefore needed to improve adherence to LSD in the long term.
Author Contributions
S.B.: Data curation, Writing—original draft; M.P.: Data curation, Funding acquisition, Writing—original draft; I.G.: Funding acquisition Writing—review & editing; A.M. and M.A.: Funding acquisition Writing—review & editing; M.E.L., L.D.N., C.G. and G.C.: Supervision Writing—review & editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kempner, W. Some Effects of the Rice Diet Treatment of Kidney Disease and Hypertension. Bull. N. Y. Acad. Med. 1946, 22, 358–370. [Google Scholar]
- Kotchen, T.A.; Cowley AWJr Frohlich, E.D. Salt in health and disease—A delicate balance. N. Engl. J. Med. 2013, 368, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012; pp. 1–46. [Google Scholar]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomized trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; MacGregor, G.A. Salt reduction lowers cardiovascular risk: Meta-analysis of outcome trials. Lancet 2011, 378, 380–382. [Google Scholar] [CrossRef]
- Strazzullo, P.; D’Elia, L.; Kandala, N.B.; Cappuccio, F.P. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 2009, 339, b4567. [Google Scholar] [CrossRef]
- Mente, A.; O’Donnell, M.J.; Rangarajan, S.; McQueen, M.J.; Poirier, P.; Wielgosz, A.; Morrison, H.; Li, W.; Wang, X.; Di, C.; et al. Association of urinary sodium and potassium excretion with blood pressure. N. Engl. J. Med. 2014, 371, 601–611. [Google Scholar] [CrossRef]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef]
- Graudal, N.; Jürgens, G.; Baslund, B.; Alderman, M.H. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: A meta-analysis. Am. J. Hypertens. 2014, 27, 1129–1137. [Google Scholar] [CrossRef]
- Stolarz-Skrzypek, K.; Kuznetsova, T.; Thijs, L.; Tikhonoff, V.; Seidlerová, J.; Richart, T.; Jin, Y.; Olszanecka, A.; Malyutina, S.; Casiglia, E.; et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA 2011, 305, 1777–1785. [Google Scholar] [CrossRef]
- Whelton, P.K.; Appel, L.J.; Sacco, R.L.; Anderson, C.A.; Antman, E.M.; Campbell, N.; Dunbar, S.B.; Frohlich, E.D.; Hall, J.E.; Jessup, M.; et al. Sodium, blood pressure, and cardiovascular disease: Further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 2012, 126, 2880–2889. [Google Scholar] [CrossRef]
- Dougher, C.E.; Rifkin, D.E.; Anderson, C.A.; Smits, G.; Persky, M.S.; Block, G.A.; Ix, J.H. Spot urine sodium measurements do not accurately estimate dietary sodium intake in chronic kidney disease. Am. J. Clin. Nutr. 2016, 104, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Olde Engberink, R.H.G.; van den Hoek, T.C.; van Noordenne, N.D.; van den Born, B.H.; Peters-Sengers, H.; Vogt, L. Use of a Single Baseline Versus Multiyear 24-Hour Urine Collection for Estimation of Long-Term Sodium Intake and Associated Cardiovascular and Renal Risk. Circulation 2017, 136, 917–926. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Mills, K.T.; Appel, L.J.; Yang, W.; Chen, J.; Lee, B.T.; Rosas, S.E.; Porter, A.; Makos, G.; Weir, M.R.; et al. Urinary Sodium and Potassium Excretion and CKD Progression. J. Am. Soc. Nephrol. 2016, 27, 1202–1212. [Google Scholar] [CrossRef] [PubMed]
- Vegter, S.; Perna, A.; Postma, M.J.; Navis, G.; Remuzzi, G.; Ruggenenti, P. Sodium intake, ACE inhibition, and progression to ESRD. J. Am. Soc. Nephrol. 2012, 23, 165–173. [Google Scholar] [CrossRef]
- Fan, L.; Tighiouart, H.; Levey, A.S.; Beck, G.J.; Sarnak, M.J. Urinary sodium excretion and kidney failure in nondiabetic chronic kidney disease. Kidney Int. 2014, 86, 582–588. [Google Scholar] [CrossRef]
- Smyth, A.; Dunkler, D.; Gao, P.; Teo, K.K.; Yusuf, S.; O’Donnell, M.J.; Mann, J.F.; Clase, C.M. ONTARGET and TRANSCEND investigators. The relationship between estimated sodium and potassium excretion and subsequent renal outcomes. Kidney Int. 2014, 86, 1205–1212. [Google Scholar] [CrossRef]
- Lambers Heerspink, H.J.; Holtkamp, F.A.; Parving, H.H.; Navis, G.J.; Lewis, J.B.; Ritz, E.; de Graeff, P.A.; de Zeeuw, D. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int. 2012, 82, 330–337. [Google Scholar] [CrossRef]
- Thomas, M.C.; Moran, J.; Forsblom, C.; Harjutsalo, V.; Thorn, L.; Ahola, A.; Wadén, J.; Tolonen, N.; Saraheimo, M.; Gordin, D.; et al. The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Diabetes Care 2011, 34, 861–866. [Google Scholar] [CrossRef]
- De Nicola, L.; Chiodini, P.; Zoccali, C.; Borrelli, S.; Cianciaruso, B.; Di Iorio, B.; Santoro, D.; Giancaspro, V.; Abaterusso, C.; Gallo, C.; et al. Prognosis of CKD patients receiving outpatient nephrology care in Italy. Clin. J. Am. Soc. Nephrol. 2011, 6, 2421–2428. [Google Scholar] [CrossRef]
- Torres, V.E.; Abebe, K.Z.; Schrier, R.W.; Perrone, R.D.; Chapman, A.B.; Yu, A.S.; Braun, W.E.; Steinman, T.I.; Brosnahan, G.; Hogan, M.C.; et al. Dietary salt restriction is beneficial to the management of autosomal dominant polycystic kidney disease. Kidney Int. 2017, 91, 493–500. [Google Scholar] [CrossRef]
- Mills, K.T.; Chen, J.; Yang, W.; Appel, L.J.; Kusek, J.W.; Alper, A.; Delafontaine, P.; Keane, M.G.; Mohler, E.; Ojo, A.; et al. Sodium Excretion and the Risk of Cardiovascular Disease in Patients With Chronic Kidney Disease. JAMA 2016, 315, 2200–2210. [Google Scholar] [CrossRef] [PubMed]
- Panuccio, V.; Pizzini, P.; Parlongo, G.; Caridi, G.; Tripepi, R.; Mafrica, A.; Cutrupi, S.; D’Arrigo, G.; Porto, G.; Garofalo, C.; et al. Urine chloride self-measurement to monitor sodium chloride intake in patients with chronic kidney disease. Clin. Chem. Lab. Med. 2019, 57, 1162–1168. [Google Scholar] [CrossRef] [PubMed]
- Humalda, J.K.; Klaassen, G.; de Vries, H.; Meuleman, Y.; Verschuur, L.C.; Straathof, E.J.M.; Laverman, G.D.; Bos, W.J.W.; van der Boog, P.J.M.; Vermeulen, K.M.; et al. A Self-management Approach for Dietary Sodium Restriction in Patients With CKD: A Randomized Controlled Trial. Am. J. Kidney Dis. 2020, 75, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Lindley, E.J. Reducing sodium intake in hemodialysis patients. Semin. Dial. 2009, 22, 260–263. [Google Scholar] [CrossRef]
- Garofalo, C.; Borrelli, S.; De Stefano, T.; Provenzano, M.; Andreucci, M.; Cabiddu, G.; La Milia, V.; Vizzardi, V.; Sandrini, M.; Cancarini, G.; et al. Incremental dialysis in ESRD: Systematic review and meta-analysis. J. Nephrol. 2019, 32, 823–836. [Google Scholar] [CrossRef]
- Bellizzi, V.; Conte, G.; Borrelli, S.; Cupisti, A.; De Nicola, L.; Di Iorio, B.R.; Cabiddu, G.; Mandreoli, M.; Paoletti, E.; Piccoli, G.B.; et al. Controversial issues in CKD clinical practice: Position statement of the CKD-treatment working group of the Italian Society of Nephrology. J. Nephrol. 2017, 30, 159–170. [Google Scholar] [CrossRef]
- Klag, M.J.; Whelton, P.K.; Randall, B.L.; Neaton, J.D.; Brancati, F.L.; Ford, C.E.; Shulman, N.B.; Stamler, J. Blood pressure and end-stage renal disease in men. N. Engl. J. Med. 1996, 334, 13–18. [Google Scholar] [CrossRef]
- Garofalo, C.; Borrelli, S.; Pacilio, M.; Minutolo, R.; Chiodini, P.; De Nicola, L.; Conte, G. Hypertension and Prehypertension and Prediction of Development of Decreased Estimated GFR in the General Population: A Meta-analysis of Cohort Studies. Am. J. Kidney Dis. 2016, 67, 89–97. [Google Scholar] [CrossRef]
- Chang, A.R.; Lóser, M.; Malhotra, R.; Appel, L.J. Blood Pressure Goals in Patients with CKD: A Review of Evidence and Guidelines. Clin. J. Am. Soc. Nephrol. 2019, 14, 161–169. [Google Scholar] [CrossRef]
- Borrelli, S.; De Nicola, L.; Stanzione, G.; Conte, G.; Minutolo, R. Resistant hypertension in nondialysis chronic kidney disease. Int. J. Hypertens. 2013, 2013, 929183. [Google Scholar] [CrossRef]
- De Nicola, L.; Gabbai, F.B.; Agarwal, R.; Chiodini, P.; Borrelli, S.; Bellizzi, V.; Nappi, F.; Conte, G.; Minutolo, R. Prevalence and prognostic role of resistant hypertension in chronic kidney disease patients. J. Am. Coll. Cardiol. 2013, 61, 2461–2467. [Google Scholar] [CrossRef] [PubMed]
- Guyton, A.C. Kidneys and fluids in pressure regulation. Small volume but large pressure changes. Hypertension 1992, 19 (Suppl. 1), I2. [Google Scholar] [CrossRef] [PubMed]
- De Nicola, L.; Minutolo, R.; Bellizzi, V.; Zoccali, C.; Cianciaruso, B.; Andreucci, V.E.; Fuiano, G.; Conte, G.; Investigators of the TArget Blood Pressure LEvels in Chronic Kidney Disease (TABLE in CKD) Study Group. Achievement of target blood pressure levels in chronic kidney disease: A salty question? Am. J. Kidney Dis. 2004, 43, 782–795. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Boutouyrie, P. The structural factor of hypertension: Large and small artery alterations. Circ. Res. 2015, 116, 1007–1021. [Google Scholar] [CrossRef] [PubMed]
- Koomans, H.A.; Roos, J.C.; Dorhout Mees, E.J.; Delawi, I.M. Sodium balance in renal failure. A comparison of patients with normal subjects under extremes of sodium intake. Hypertension 1985, 7, 714–721. [Google Scholar] [CrossRef]
- Cianciaruso, B.; Bellizzi, V.; Minutolo, R.; Colucci, G.; Bisesti, V.; Russo, D.; Conte, G.; De Nicola, L. Renal adaptation to dietary sodium restriction in moderate renal failure resulting from chronic glomerular disease. J. Am. Soc. Nephrol. 1996, 7, 306–313. [Google Scholar]
- Kobori, H.; Nishiyama, A.; Abe, Y.; Navar, L.G. Enhancement of intrarenal angiotensinogen in Dahl salt-sensitive rats on high salt diet. Hypertension 2003, 41, 592–597. [Google Scholar] [CrossRef]
- Ying, W.Z.; Sanders, P.W. Dietary salt modulates renal production of transforming growth factor-beta in rats. Am. J. Physiol. 1998, 274, F635–F641. [Google Scholar] [CrossRef]
- Meng, S.; Roberts, L.J., II; Cason, G.W.; Curry, T.S.; Manning, R.D., Jr. Superoxide dismutase and oxidative stress in Dahl salt-sensitive and -resistant rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002, 283, R732–R738. [Google Scholar] [CrossRef]
- Guild, S.J.; McBryde, F.D.; Malpas, S.C.; Barrett, C.J. High dietary salt and angiotensin II chronically increase renal sympathetic nerve activity: A direct telemetric study. Hypertension 2012, 59, 614–620. [Google Scholar] [CrossRef]
- Chesterton, L.J.; Sigrist, M.K.; Bennett, T.; Taal, M.W.; McIntyre, C.W. Reduced baroreflex sensitivity is associated with increased vascular calcification and arterial stiffness. Nephrol. Dial. Transpl. 2005, 20, 1140–1147. [Google Scholar] [CrossRef]
- Titze, J.; Dahlmann, A.; Lerchl, K.; Kopp, C.; Rakova, N.; Schröder, A.; Luft, F.C. Spooky sodium balance. Kidney Int. 2014, 85, 759–767. [Google Scholar] [CrossRef]
- Machnik, A.; Neuhofer, W.; Jantsch, J.; Dahlmann, A.; Tammela, T.; Machura, K.; Park, J.K.; Beck, F.X.; Müller, D.N.; Derer, W.; et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat. Med. 2009, 15, 545–552. [Google Scholar] [CrossRef]
- Machnik, A.; Dahlmann, A.; Kopp, C.; Goss, J.; Wagner, H.; van Rooijen, N.; Eckardt, K.U.; Müller, D.N.; Park, J.K.; Luft, F.C.; et al. Mononuclear phagocyte system depletion blocks interstitial tonicity-responsive enhancer binding protein/vascular endothelial growth factor C expression and induces salt-sensitive hypertension in rats. Hypertension 2010, 55, 755–761. [Google Scholar] [CrossRef]
- Wiig, H.; Schröder, A.; Neuhofer, W.; Jantsch, J.; Kopp, C.; Karlsen, T.V.; Boschmann, M.; Goss, J.; Bry, M.; Rakova, N.; et al. Immune cells control skin lymphatic electrolyte homeostasis and blood pressure. J. Clin. Investig. 2013, 123, 2803–2815. [Google Scholar] [CrossRef]
- Heer, M.; Baisch, F.; Kropp, J.; Gerzer, R.; Drummer, C. High dietary sodium chloride consumption may not induce body fluid retention in humans. Am. J. Physiol. Renal. Physiol. 2000, 278, F585–F595. [Google Scholar] [CrossRef]
- Rakova, N.; Jüttner, K.; Dahlmann, A.; Schröder, A.; Linz, P.; Kopp, C.; Rauh, M.; Goller, U.; Beck, L.; Agureev, A.; et al. Long-term space flight simulation reveals infradian rhythmicity in human Na(+) balance. Cell Metab. 2013, 17, 125–131. [Google Scholar] [CrossRef]
- Kopp, C.; Linz, P.; Wachsmuth, L.; Dahlmann, A.; Horbach, T.; Schöfl, C.; Renz, W.; Santoro, D.; Niendorf, T.; Müller, D.N.; et al. (23)Na magnetic resonance imaging of tissue sodium. Hypertension 2012, 59, 167–172. [Google Scholar] [CrossRef]
- Kopp, C.; Linz, P.; Dahlmann, A.; Hammon, M.; Jantsch, J.; Müller, D.N.; Schmieder, R.E.; Cavallaro, A.; Eckardt, K.U.; Uder, M.; et al. 23Na magnetic resonance imaging-determined tissue sodium in healthy subjects and hypertensive patients. Hypertension 2013, 61, 635–640. [Google Scholar] [CrossRef]
- Schneider, M.P.; Raff, U.; Kopp, C.; Scheppach, J.B.; Toncar, S.; Wanner, C.; Schlieper, G.; Saritas, T.; Floege, J.; Schmid, M.; et al. Skin Sodium Concentration Correlates with Left Ventricular Hypertrophy in CKD. J. Am. Soc. Nephrol. 2017, 28, 1867–1876. [Google Scholar] [CrossRef]
- Dahlmann, A.; Dörfelt, K.; Eicher, F.; Linz, P.; Kopp, C.; Mössinger, I.; Horn, S.; Büschges-Seraphin, B.; Wabel, P.; Hammon, M.; et al. Magnetic resonance-determined sodium removal from tissue stores in hemodialysis patients. Kidney Int. 2015, 87, 434–441. [Google Scholar] [CrossRef]
- Garofalo, C.; Borrelli, S.; Provenzano, M.; De Stefano, T.; Vita, C.; Chiodini, P.; Minutolo, R.; De Nicola, L.; Conte, G. Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical Trials. Nutrients 2018, 10, 732. [Google Scholar] [CrossRef] [PubMed]
- Slagman, M.C.; Waanders, F.; Hemmelder, M.H.; Woittiez, A.J.; Janssen, W.M.; Lambers Heerspink, H.J.; Navis, G.; Laverman, G.D. HOlland NEphrology STudy Group. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: Randomised controlled trial. BMJ 2011, 343, d4366. [Google Scholar] [CrossRef]
- Vogt, L.; Waanders, F.; Boomsma, F.; de Zeeuw, D.; Navis, G. Effects of dietary sodium and hydrochlorothiazide on the antiproteinuric efficacy of losartan. J. Am. Soc. Nephrol. 2008, 19, 999–1007. [Google Scholar] [CrossRef]
- Kwakernaak, A.J.; Krikken, J.A.; Binnenmars, S.H.; Visser, F.W.; Hemmelder, M.H.; Woittiez, A.J.; Groen, H.; Laverman, G.D.; Navis, G.; Holland Nephrology Study (HONEST) Group. Effects of sodium restriction and hydrochlorothiazide on RAAS blockade efficacy in diabetic nephropathy: A randomised clinical trial. Lancet Diabetes Endocrinol. 2014, 2, 385–395. [Google Scholar] [CrossRef]
- McMahon, E.J.; Bauer, J.D.; Hawley, C.M.; Isbel, N.M.; Stowasser, M.; Johnson, D.W.; Campbell, K.L. A randomized trial of dietary sodium restriction in CKD. J. Am. Soc. Nephrol. 2013, 24, 2096–2103. [Google Scholar] [CrossRef] [PubMed]
- Konishi, Y.; Okada, N.; Okamura, M.; Morikawa, T.; Okumura, M.; Yoshioka, K.; Imanishi, M. Sodium sensitivity of blood pressure appearing before hypertension and related to histological damage in immunoglobulin a nephropathy. Hypertension 2001, 38, 81–85. [Google Scholar] [CrossRef]
- Keyzer, C.A.; van Breda, G.F.; Vervloet, M.G.; de Jong, M.A.; Laverman, G.D.; Hemmelder, M.H.; Janssen, W.M.; Lambers Heerspink, H.J.; Kwakernaak, A.J.; Bakker, S.J.; et al. Effects of Vitamin D Receptor Activation and Dietary Sodium Restriction on Residual Albuminuria in CKD: The ViRTUE-CKD Trial. J. Am. Soc. Nephrol. 2017, 28, 1296–1305. [Google Scholar] [CrossRef]
- Meuleman, Y.; Hoekstra, T.; Dekker, F.W.; Navis, G.; Vogt, L.; van der Boog, P.J.M.; Bos, W.J.W.; van Montfrans, G.A.; van Dijk, S.; ESMO Study Group. Sodium Restriction in Patients With CKD: A Randomized Controlled Trial of Self-management Support. Am. J. Kidney Dis. 2017, 69, 576–586. [Google Scholar] [CrossRef]
- Ruilope, L.M.; Casal, M.C.; Guerrero, L.; Alcázar, J.M.; Férnandez, M.L.; Lahera, V.; Rodicio, J.L. Sodium intake does not influence the effect of verapamil in hypertensive patients with mild renal insufficiency. Drugs 1992, 44 (Suppl. 1), 94–98. [Google Scholar] [CrossRef]
- Hwang, J.H.; Chin, H.J.; Kim, S.; Kim, D.K.; Kim, S.; Park, J.H.; Shin, S.J.; Lee, S.H.; Choi, B.S.; Lim, C.S. Effects of intensive low-salt diet education on albuminuria among nondiabetic patients with hypertension treated with olmesartan: A single-blinded randomized, controlled trial. Clin. J. Am. Soc. Nephrol. 2014, 9, 2059–2069. [Google Scholar] [CrossRef] [PubMed]
- de Brito-Ashurst, I.; Perry, L.; Sanders, T.A.; Thomas, J.E.; Dobbie, H.; Varagunam, M.; Yaqoob, M.M. The role of salt intake and salt sensitivity in the management of hypertension in South Asian people with chronic kidney disease: A randomised controlled trial. Heart 2013, 99, 1256–1260. [Google Scholar] [CrossRef] [PubMed]
- Saran, R.; Padilla, R.L.; Gillespie, B.W.; Heung, M.; Hummel, S.L.; Derebail, V.K.; Pitt, B.; Levin, N.W.; Zhu, F.; Abbas, S.R.; et al. A Randomized Crossover Trial of Dietary Sodium Restriction in Stage 3-4 CKD. Clin. J. Am. Soc. Nephrol. 2017, 12, 399–407. [Google Scholar] [CrossRef]
- Minutolo, R.; Borrelli, S.; Chiodini, P.; Scigliano, R.; Bellizzi, V.; Cianciaruso, B.; Nappi, F.; Zamboli, P.; Catapano, F.; Conte, G.; et al. Effects of age on hypertensive status in patients with chronic kidney disease. J. Hypertens. 2007, 25, 2325–2333. [Google Scholar] [CrossRef]
- Kimura, G.; Dohi, Y.; Fukuda, M. Salt sensitivity and circadian rhythm of blood pressure: The keys to connect CKD with cardiovascular events. Hypertens. Res. 2010, 33, 515–520. [Google Scholar] [CrossRef]
- Minutolo, R.; Agarwal, R.; Borrelli, S.; Chiodini, P.; Bellizzi, V.; Nappi, F.; Cianciaruso, B.; Zamboli, P.; Conte, G.; Gabbai, F.B.; et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch. Intern. Med. 2011, 171, 1090–1098. [Google Scholar] [CrossRef]
- D’Elia, L.; Rossi, G.; Schiano di Cola, M.; Savino, I.; Galletti, F.; Strazzullo, P. Meta-Analysis of the Effect of Dietary Sodium Restriction with or without Concomitant Renin-Angiotensin-Aldosterone System-Inhibiting Treatment on Albuminuria. Clin. J. Am. Soc. Nephrol. 2015, 10, 1542–1552. [Google Scholar] [CrossRef]
- Borrelli, S.; Leonardis, D.; Minutolo, R.; Chiodini, P.; De Nicola, L.; Esposito, C.; Mallamaci, F.; Zoccali, C.; Conte, G. Epidemiology of CKD Regression in Patients under Nephrology Care. PLoS ONE 2015, 10, e0140138. [Google Scholar] [CrossRef]
- De Nicola, L.; Provenzano, M.; Chiodini, P.; Borrelli, S.; Garofalo, C.; Pacilio, M.; Liberti, M.E.; Sagliocca, A.; Conte, G.; Minutolo, R. Independent Role of Underlying Kidney Disease on Renal Prognosis of Patients with Chronic Kidney Disease under Nephrology Care. PLoS ONE 2015, 10, e0127071. [Google Scholar] [CrossRef]
- Simeoni, M.; Borrelli, S.; Garofalo, C.; Fuiano, G.; Esposito, C.; Comi, A.; Provenzano, M. Atherosclerotic-nephropathy: An updated narrative review. J. Nephrol. 2020. [Google Scholar] [CrossRef]
- Abuelo, J.G. Normotensive ischemic acute renal failure. N. Engl. J. Med. 2007, 357, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Minutolo, R.; Borrelli, S.; Scigliano, R.; Bellizzi, V.; Chiodini, P.; Cianciaruso, B.; Nappi, F.; Zamboli, P.; Conte, G.; De Nicola, L. Prevalence and clinical correlates of white coat hypertension in chronic kidney disease. Nephrol. Dial. Transpl. 2007, 22, 2217–2223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Minutolo, R.; Gabbai, F.B.; Agarwal, R.; Chiodini, P.; Borrelli, S.; Bellizzi, V.; Nappi, F.; Stanzione, G.; Conte, G.; De Nicola, L. Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: A multicenter prospective cohort study. Am. J. Kidney Dis. 2014, 64, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Fagard, R.H.; Staessen, J.A.; Thijs, L.; Gasowski, J.; Bulpitt, C.J.; Clement, D.; de Leeuw, P.W.; Dobovisek, J.; Jääskivi, M.; Leonetti, G.; et al. Response to antihypertensive therapy in older patients with sustained and nonsustained systolic hypertension. Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Circulation 2000, 102, 1139–1144. [Google Scholar] [CrossRef] [PubMed]
- Merchant, A.; Wald, R.; Goldstein, M.B.; Yuen, D.; Kirpalani, A.; Dacouris, N.; Ray, J.G.; Kiaii, M.; Leipsic, J.; Kotha, V.; et al. Relationship between different blood pressure measurements and left ventricular mass by cardiac magnetic resonance imaging in end-stage renal disease. J. Am. Soc. Hypertens. 2015, 9, 275–284. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Regidor, D.L.; Kovesdy, C.P.; Van Wyck, D.; Bunnapradist, S.; Horwich, T.B.; Fonarow, G.C. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation 2009, 119, 671–679. [Google Scholar] [CrossRef]
- Agarwal, R. Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension 2010, 56, 512–517. [Google Scholar] [CrossRef]
- Ok, E.; Asci, G.; Chazot, C.; Ozkahya, M.; Mees, E.J. Controversies and problems of volume control and hypertension in haemodialysis. Lancet 2016, 388, 285–293. [Google Scholar] [CrossRef]
- Zoccali, C.; Moissl, U.; Chazot, C.; Mallamaci, F.; Tripepi, G.; Arkossy, O.; Wabel, P.; Stuard, S. Chronic Fluid Overload and Mortality in ESRD. J. Am. Soc. Nephrol. 2017, 28, 2491–2497. [Google Scholar] [CrossRef]
- Cole, N.I.; Swift, P.A.; He, F.J.; MacGregor, G.A.; Suckling, R.J. The effect of dietary salt on blood pressure in individuals receiving chronic dialysis: A systematic review and meta-analysis of randomised controlled trials. J. Hum. Hypertens. 2019, 33, 319–326. [Google Scholar] [CrossRef]
- Mc Causland, F.R.; Waikar, S.S.; Brunelli, S.M. Increased dietary sodium is independently associated with greater mortality among prevalent hemodialysis patients. Kidney Int. 2012, 82, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Van Biesen, W.; Verger, C.; Heaf, J.; IPOD-PD Study Group. Evolution Over Time of Volume Status and PD-Related Practice Patterns in an Incident Peritoneal Dialysis Cohort. Clin. J. Am. Soc. Nephrol. 2019, 14, 882–893. [Google Scholar] [CrossRef]
- Ronco, C.; Verger, C.; Crepaldi, C.; IPOD-PD Study Group. Baseline hydration status in incident peritoneal dialysis patients: The initiative of patient outcomes in dialysis (IPOD-PD study). Nephrol. Dial. Transpl. 2015, 30, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, S.; De Nicola, L.; Minutolo, R.; Perna, A.; Provenzano, M.; Argentino, G.; Cabiddu, G.; Russo, R.; La Milia, V.; De Stefano, T.; et al. Sodium toxicity in peritoneal dialysis: Mechanisms and “solutions”. J. Nephrol. 2020, 33, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Sakata, F.; Ishii, T.; Tawada, M.; Suzuki, Y.; Kinashi, H.; Katsuno, T.; Takei, Y.; Maruyama, S.; Mizuno, M.; et al. Excessive salt intake increases peritoneal solute transport rate via local tonicity-responsive enhancer binding protein in subtotal nephrectomized mice. Nephrol. Dial. Transpl. 2019, 34, 2031–2042. [Google Scholar] [CrossRef]
- Dong, J.; Li, Y.; Yang, Z.; Luo, J. Low dietary sodium intake increases the death risk in peritoneal dialysis. Clin. J. Am. Soc. Nephrol. 2010, 5, 240–247. [Google Scholar] [CrossRef]
- Borrelli, S.; La Milia, V.; De Nicola, L.; Cabiddu, G.; Russo, R.; Provenzano, M.; Minutolo, R.; Conte, G.; Garofalo, C.; Study Group Peritoneal Dialysis of Italian Society of Nephrology. Sodium removal by peritoneal dialysis: A systematic review and meta-analysis. J. Nephrol. 2019, 32, 231–239. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).