Legumain Promotes Atherosclerotic Vascular Remodeling
Abstract
1. Introduction
2. Results
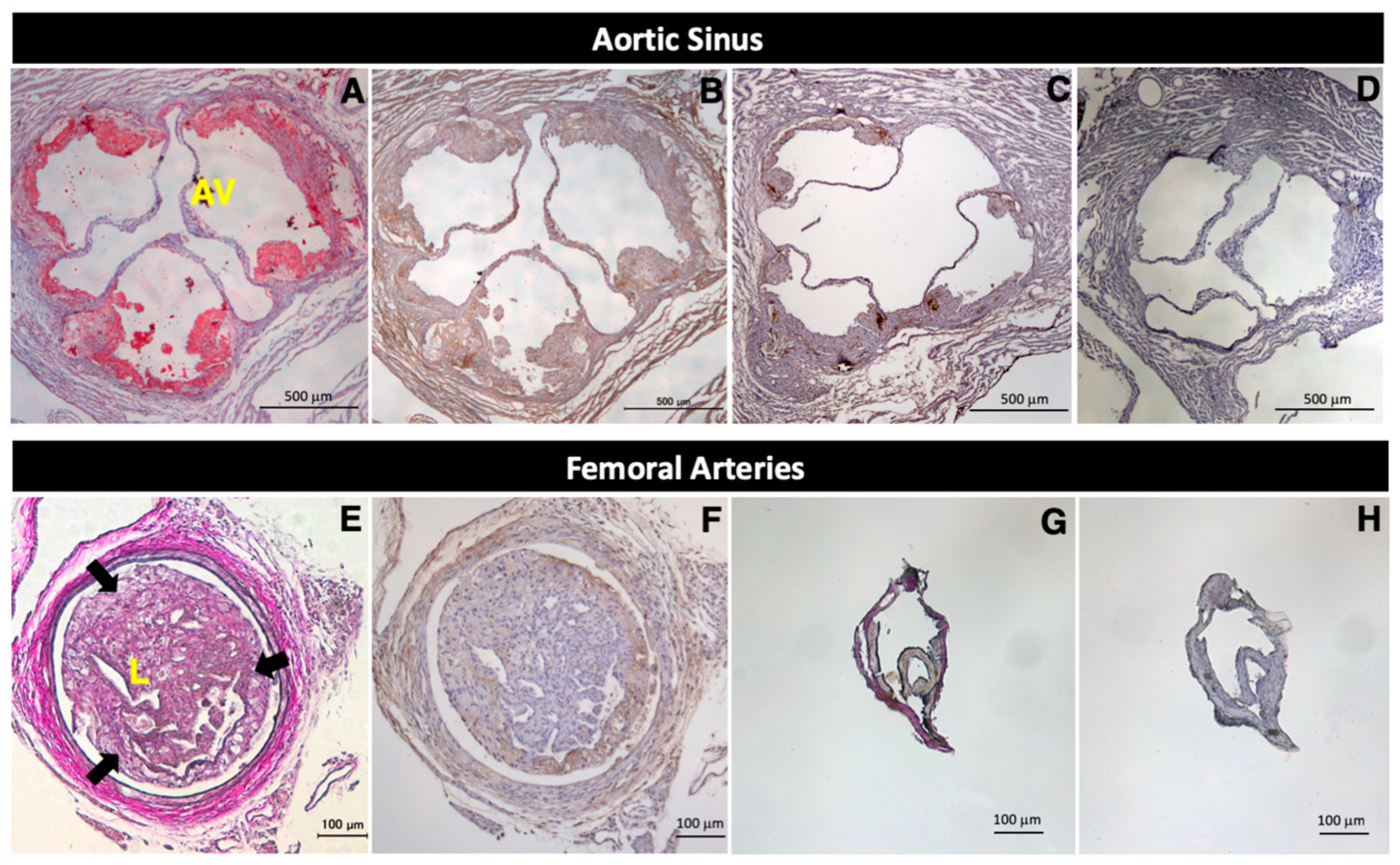
2.1. Expression of Legumain in Mouse Atherosclerotic Lesions
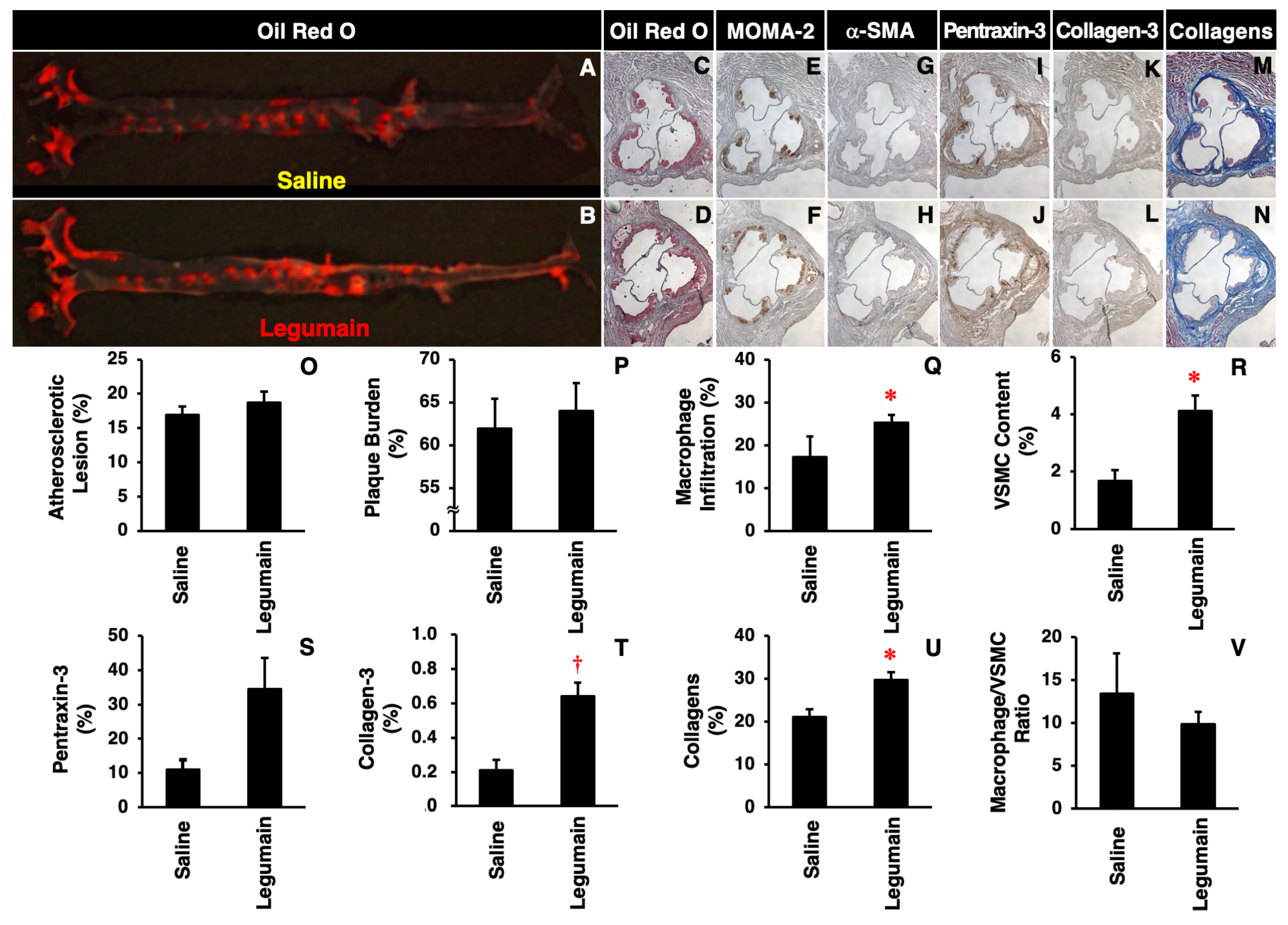
2.2. Effects of Legumain on Atherosclerotic Lesion Development in Apoe−/− Mice
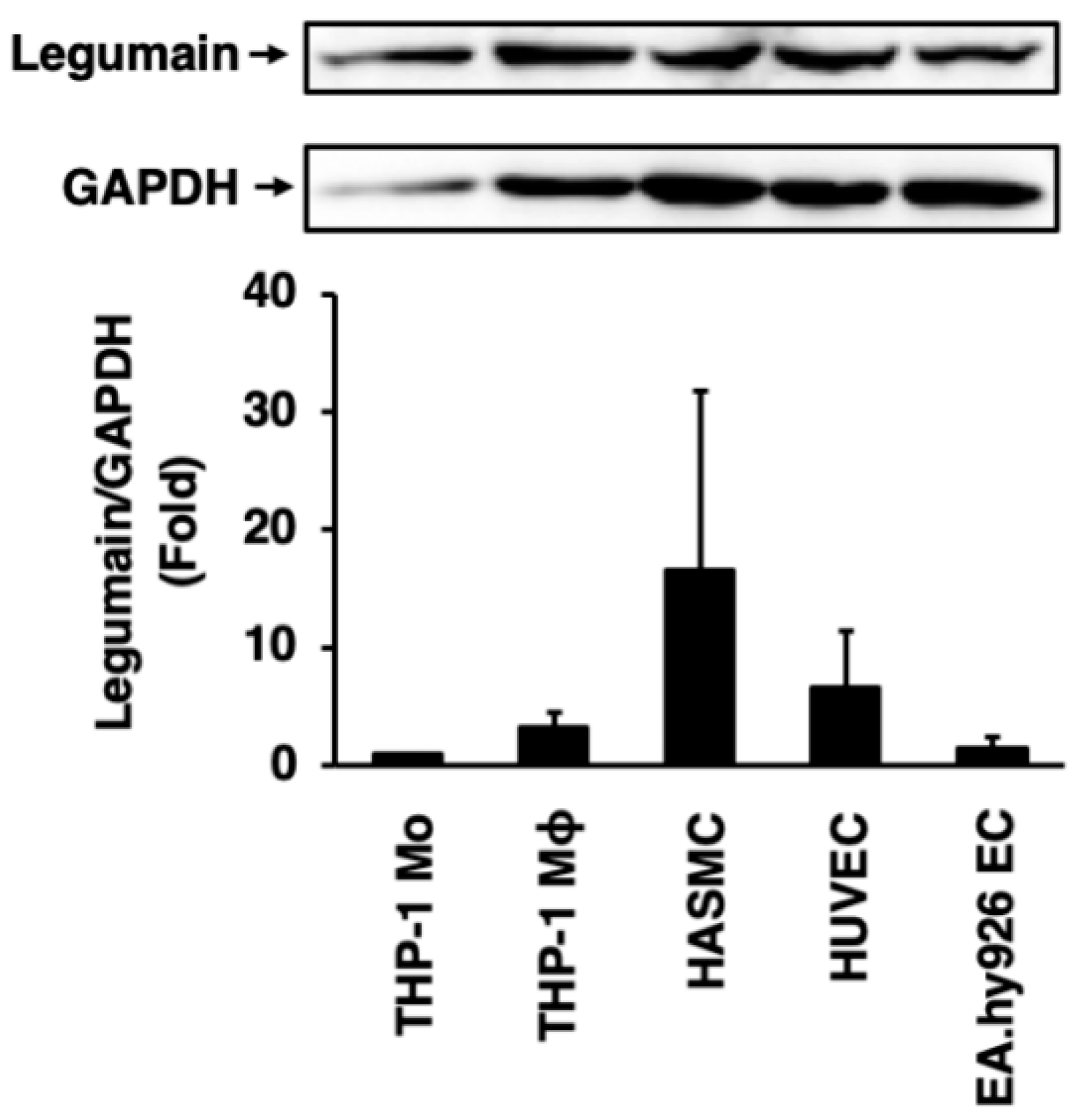
2.3. Expression of Legumain in Human Vascular Cells
2.4. Effects of Legumain on Inflammatory Responses in HUVECs
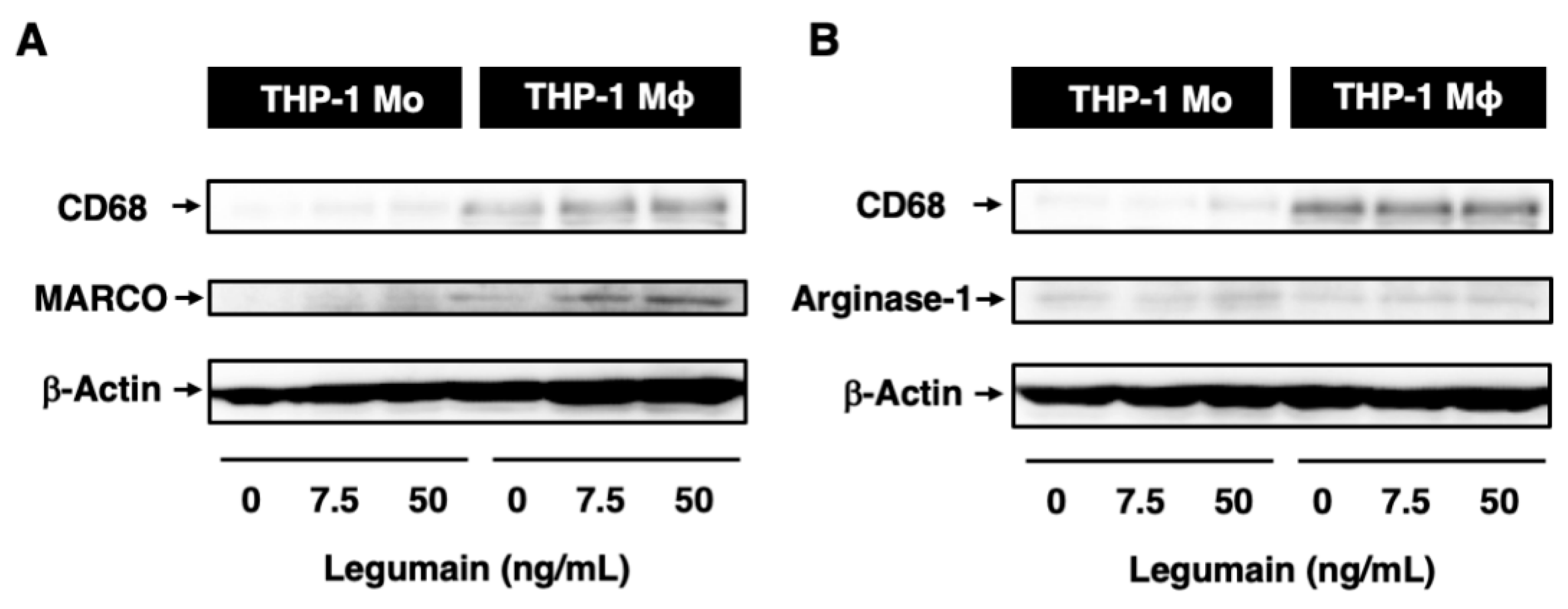
2.5. Effects of Legumain on the Inflammatory Phenotype of Human Macrophages
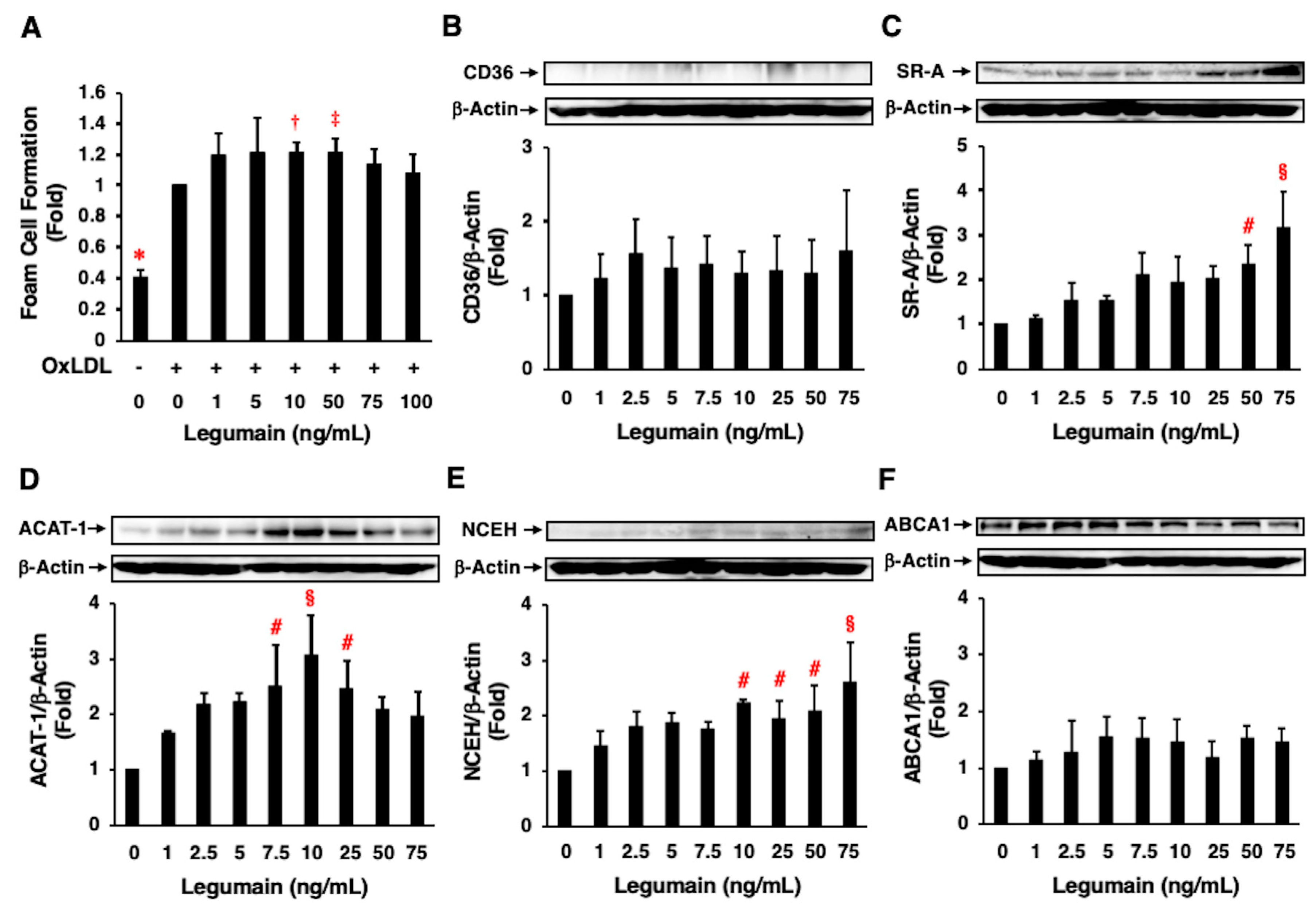
2.6. Effects of Legumain on Foam Cell Formation
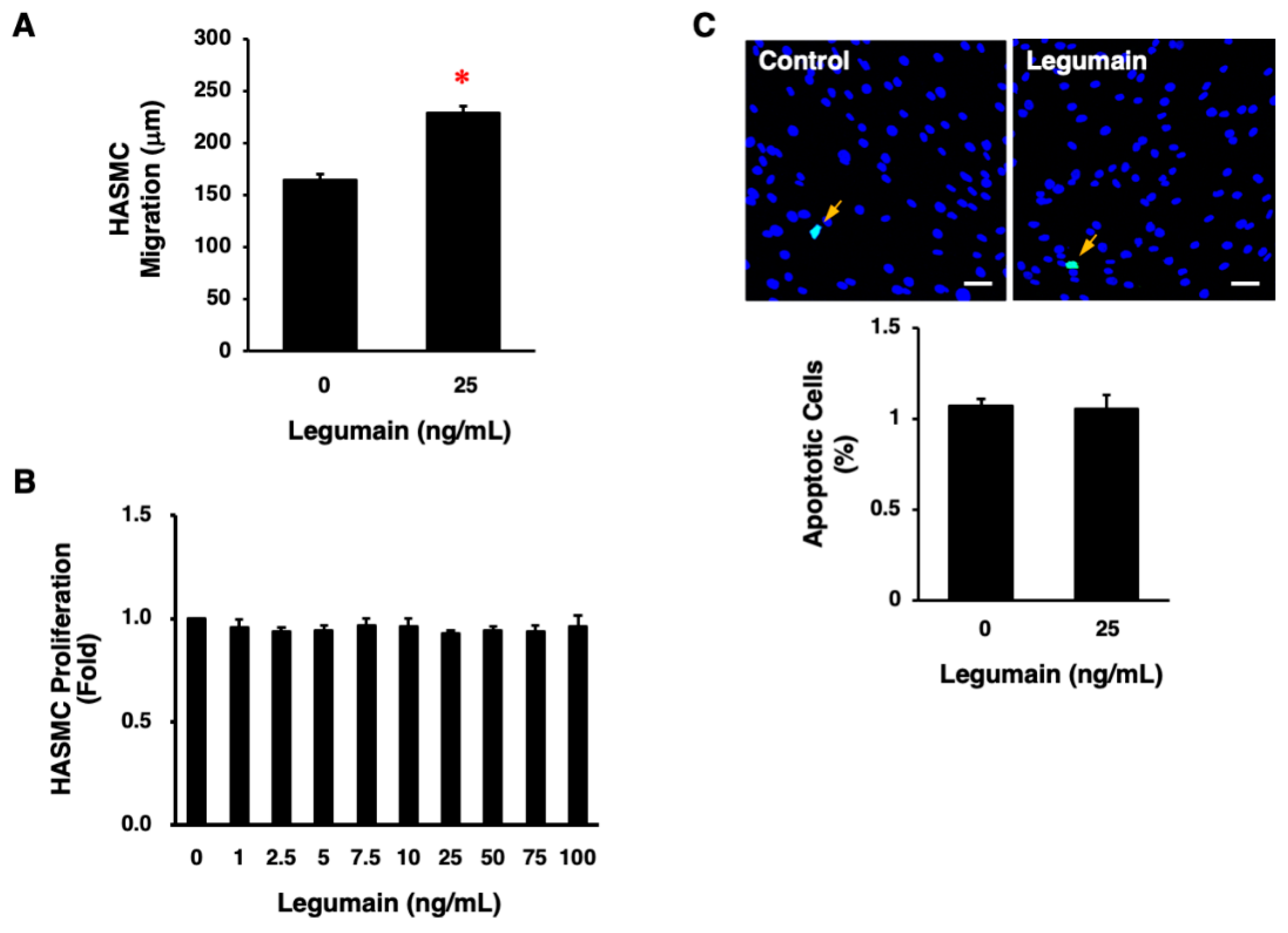
2.7. Effects of Legumain on Migration, Proliferation, and Apoptosis of HASMCs
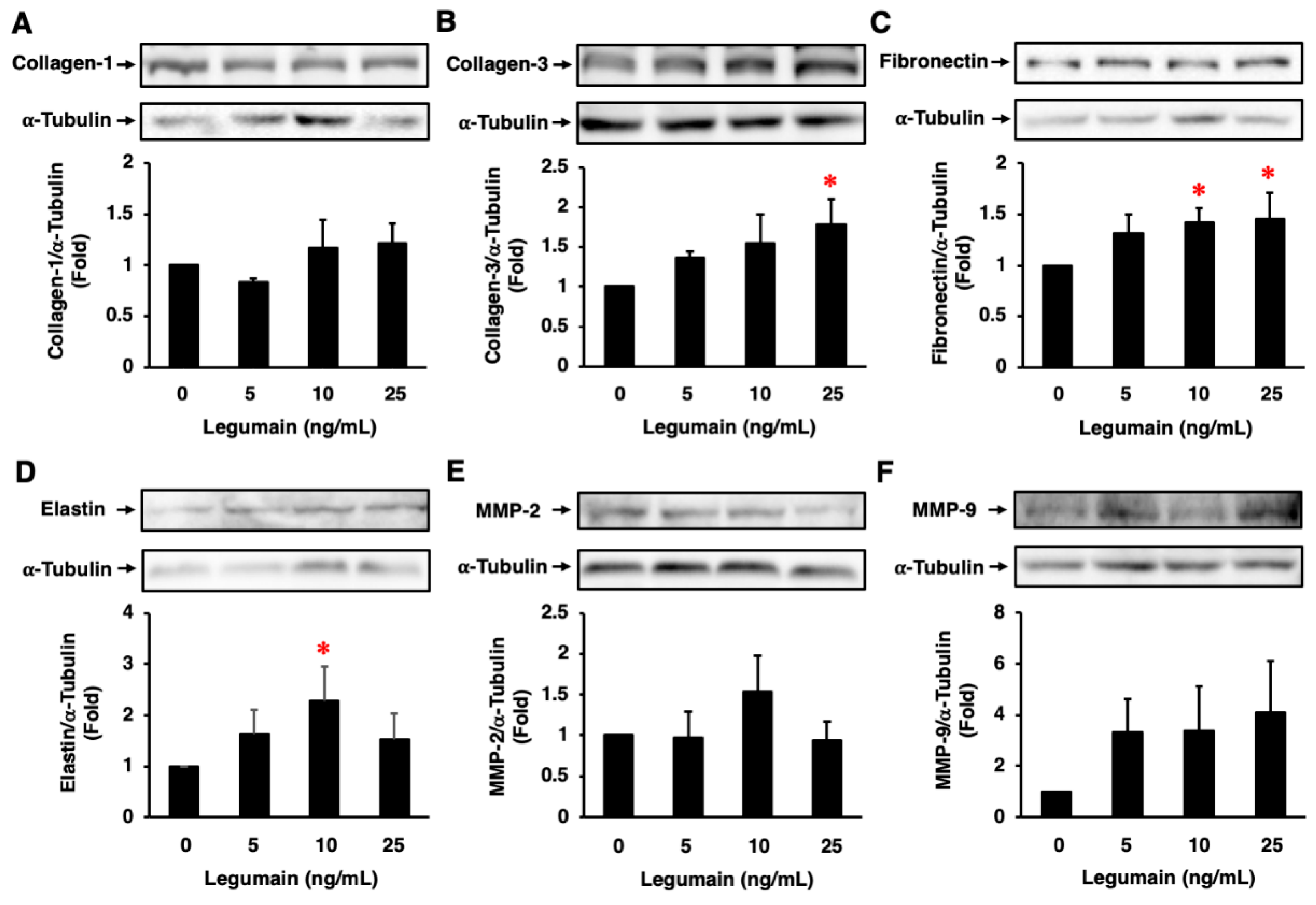
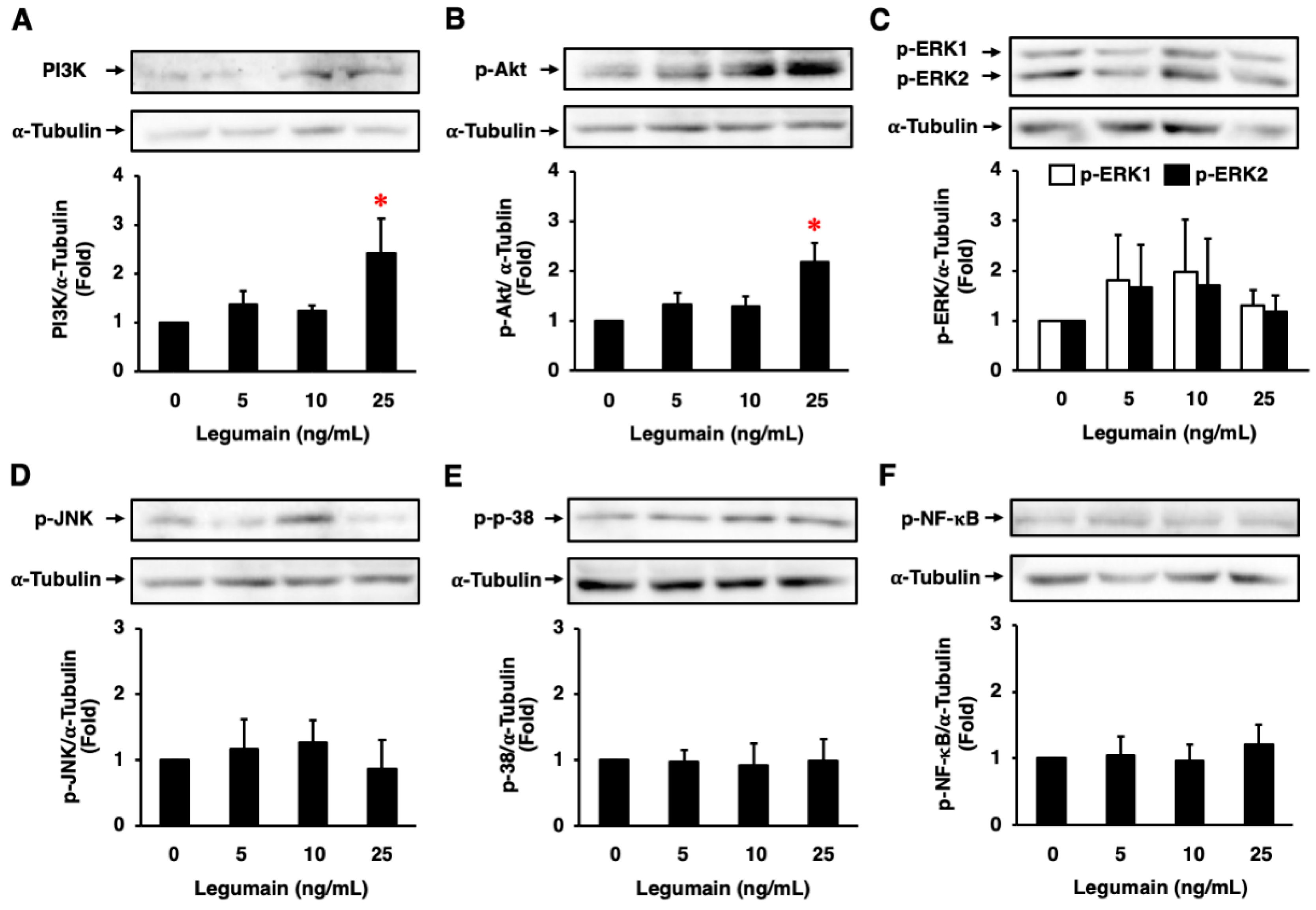
2.8. Effects of Legumain on ECM Protein Expression in HASMCs
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Reverse Transcription-Polymerase Chain Reaction
4.3. Proliferation Assay
4.4. Apoptosis Assay
4.5. Migration Assay
4.6. Foam Cell Formation Assay
4.7. Western Blotting
4.8. Administration of Legumain to Mice
4.9. Animal Measurements
4.10. Assessment of Atherosclerotic Lesions
4.11. Assessment of Legumain Expression in Intimal Lesions following Wire Injury
4.12. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ABCA1 | ATP-binding cassette transporter A1 |
| ACAT-1 | acyl-coenzyme A:cholesterol acyltransferase-1 |
| Apoe−/− mice | apolipoprotein E-deficient mice |
| EC | endothelial cell |
| ECM | extracellular matrix |
| HASMC | human aortic smooth muscle cell |
| HUVEC | human umbilical vein endothelial cell |
| ICAM-1 | intercellular adhesion molecule-1 |
| IL | interleukin |
| LPS | lipopolysaccharide |
| MCM | monocyte/macrophage-conditioned medium |
| MCP-1 | monocyte chemoattractant protein-1 |
| MMP | matrix metalloproteinase |
| NCEH | neutral cholesterol ester hydrolase |
| NF-κB | nuclear factor-κB |
| OxLDL | oxidized low-density lipoprotein |
| SR-A | scavenger receptor class A |
| TNF-α | tumor necrosis factor-α |
| VCAM-1 | vascular cell adhesion molecule-1 |
| VSMC | vascular smooth muscle cell |
References
- Hansson, G.K.; Libby, P. The immune response in atherosclerosis: A double-edged sword. Nat. Rev. Immunol. 2006, 6, 508–519. [Google Scholar] [CrossRef]
- Sato, Y.; Watanabe, R.; Uchiyama, N.; Ozawa, N.; Takahashi, Y.; Shirai, R.; Sato, K.; Mori, Y.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Inhibitory effects of vasostatin-1 against atherogenesis. Clin. Sci. 2019, 132, 2493–2507. [Google Scholar] [CrossRef] [PubMed]
- Gerhardt, T.; Ley, K. Monocyte trafficking across the vessel wall. Cardiovasc. Res. 2015, 107, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Paoli, F.D.; Staels, B.; Chinetti-Gbaguidi, G. Macrophage phenotypes and their modulation in atherosclerosis. Circ. J. 2014, 78, 1775–1781. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Watanabe, R.; Sato, Y.; Ozawa, N.; Kojima, M.; Watanabe-Kominato, K.; Shirai, R.; Sato, K.; Hirano, T.; Watanabe, T. Novel phytopeptide osmotin mimics preventive effects of adiponectin on vascular inflammation and atherosclerosis. Metabolism 2018, 83, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Bories, G.F.P.; Leitinger, N. Macrophage metabolism in atherosclerosis. FEBS Lett. 2017, 591, 3042–3060. [Google Scholar] [CrossRef]
- Watanabe, K.; Watanabe, R.; Konii, H.; Shirai, R.; Sato, K.; Matsuyama, T.; Ishibashi-Ueda, H.; Koba, S.; Kobayashi, Y.; Hirano, T.; et al. Counteractive effects of omentin-1 against atherogenesis. Cardiovasc. Res. 2016, 110, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Rudijanto, A. The role of vascular smooth muscle cells on the pathogenesis of atherosclerosis. Acta Med. Indones 2007, 39, 86–93. [Google Scholar] [PubMed]
- Chistiakov, D.A.; Sobenin, I.A.; Orekhov, A.N. Vascular extracellular matrix in atherosclerosis. Cardiol. Rev. 2013, 21, 270–288. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M.; Ozawa, N.; Mori, Y.; Takahashi, Y.; Watanabe-Kominato, K.; Shirai, R.; Watanabe, R.; Sato, K.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Catestatin prevents macrophage-driven atherosclerosis but not arterial injury-induced neointimal hyperplasia. Thromb. Haemost. 2018, 118, 182–194. [Google Scholar] [CrossRef] [PubMed]
- Takeda, O.; Miura, Y.; Mitta, M.; Matsushita, H.; Kato, I.; Abe, Y.; Yokosawa, H.; Ishii, S. Isolation and analysis of cDNA encoding a precursor of Canavalia ensiformis asparaginyl endopeptidase (legumain). J. Biochem. 1994, 116, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.M.; Dando, P.M.; Rawlings, N.D.; Brown, M.A.; Young, N.E.; Stevens, R.A.; Hewitt, E.; Watts, C.; Barrett, A.J. Cloning, isolation, and characterization of mammalian legumain, an asparaginyl endopeptidase. J. Biol. Chem. 1997, 272, 8090–8098. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Hua, T.; Crowley, C.; Ru, H.; Ni, X.; Shaw, N.; Jiao, L.; Ding, W.; Qu, L.; Hung, L.W.; et al. Structural analysis of asparaginyl endopeptidase reveals the activation mechanism and a reversible intermediate maturation stage. Cell Res. 2014, 24, 344–358. [Google Scholar] [CrossRef] [PubMed]
- Dall, E.; Brandstetter, H. Structure and function of legumain in health and disease. Biochimie 2016, 122, 126–150. [Google Scholar] [CrossRef] [PubMed]
- Freeley, S.; Cardone, J.; Günther, S.C.; West, E.E.; Reinheckel, T.; Watts, C.; Kemper, C.; Kolev, M.V. Asparaginyl endopeptidase (legumain) supports human Th1 induction via cathepsin L-mediated intracellular C3 activation. Front. Immunol. 2018, 9, 2449. [Google Scholar] [CrossRef]
- Chen, J.M.; Dando, P.M.; Stevens, R.A.; Fortunato, M.; Barrett, A.J. Cloning and expression of mouse legumain, a lysosomal endopeptidase. Biochem. J. 1998, 335, 111–117. [Google Scholar] [CrossRef]
- Hashimoto, S.; Suzuki, T.; Dong, H.Y.; Yamazaki, N.; Matsushima, K. Serial analysis of gene expression in human monocytes and macrophages. Blood 1999, 94, 837–844. [Google Scholar]
- Edgington-Mitchell, L.E.; Wartmann, T.; Fleming, A.K.; Gocheva, V.; van der Linden, W.A.; Withana, N.P.; Verdoes, M.; Aurelio, L.; Edgington-Mitchell, D.; Lieu, T.; et al. Legumain is activated in macrophages during pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 311, G548–G560. [Google Scholar] [CrossRef]
- Jafari, A.; Qanie, D.; Andersen, T.L.; Zhang, Y.; Chen, L.; Postert, B.; Parsons, S.; Ditzel, N.; Khosla, S.; Johansen, H.T.; et al. Legumain regulates differentiation fate of human bone marrow stromal cells and is altered in postmenopausal osteoporosis. Stem Cell Rep. 2017, 8, 373–386. [Google Scholar] [CrossRef]
- Park, H.J.; Kim, J.; Saima, F.T.; Rhee, K.J.; Hwang, S.; Kim, M.Y.; Baik, S.K.; Eom, Y.W.; Kim, H.S. Adipose-derived stem cells ameliorate colitis by suppression of inflammasome formation and regulation of M1-macrophage population through prostaglandin E2. Biochem. Biophys. Res. Commun. 2018, 498, 988–995. [Google Scholar] [CrossRef]
- Solberg, R.; Smith, R.; Almlöf, M.; Tewolde, E.; Nilsen, H.; Johansen, H.T. Legumain expression, activity and secretion are increased during monocyte-to-macrophage differentiation and inhibited by atorvastatin. Biol. Chem. 2015, 396, 71–80. [Google Scholar] [CrossRef]
- Lunde, N.N.; Holm, S.; Dahl, T.B.; Elyouncha, I.; Sporsheim, B.; Gregersen, I.; Abbas, A.; Skjelland, M.; Espevik, T.; Solberg, R.; et al. Increased levels of legumain in plasma and plaques from patients with carotid atherosclerosis. Atherosclerosis 2017, 257, 216–223. [Google Scholar] [CrossRef]
- Shen, L.; Li, H.; Shi, Y.; Wang, D.; Gong, J.; Xun, J.; Zhou, S.; Xiang, R.; Tan, X. M2 tumour-associated macrophages contribute to tumor progression via legumain remodeling the extracellular matrix in diffuse large B cell lymphoma. Sci. Rep. 2016, 6, 30347. [Google Scholar] [CrossRef]
- Bai, P.; Lyu, L.; Yu, T.; Zuo, C.; Fu, J.; He, Y.; Wan, Q.; Wan, N.; Jia, D.; Lyu, A. Macrophage-derived legumain promotes pulmonary hypertension by activating the MMP (Matrix Metalloproteinase)-2/TGF (Transforming Growth Factor)-β1 signaling. Arterioscler. Thromb. Vasc. Biol. 2019, 39, e130–e145. [Google Scholar] [CrossRef]
- Sun, W.; Lin, Y.; Chen, L.; Ma, R.; Cao, J.; Yao, J.; Chen, K.; Wan, J. Legumain suppresses OxLDL-induced macrophage apoptosis through enhancement of the autophagy pathway. Gene 2018, 652, 16–24. [Google Scholar] [CrossRef]
- Clerin, V.; Shih, H.H.; Deng, N.; Hebert, G.; Resmini, C.; Shields, K.M.; Feldman, J.L.; Winkler, A.; Albert, L.; Maganti, V.; et al. Expression of the cysteine protease legumain in vascular lesions and functional implications in atherogenesis. Atherosclerosis 2008, 201, 53–66. [Google Scholar] [CrossRef]
- Papaspyridonos, M.; Smith, A.; Burnand, K.G.; Taylor, P.; Padayachee, S.; Suckling, K.E.; James, C.H.; Greaves, D.R.; Patel, L. Novel candidate genes in unstable areas of human atherosclerotic plaques. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 1837–1844. [Google Scholar] [CrossRef]
- Mattock, K.L.; Gough, P.J.; Humphries, J.; Burnand, K.; Patel, L.; Suckling, K.E.; Cuello, F.; Watts, C.; Gautel, M.; Avkiran, M.; et al. Legumain and cathepsin-L expression in human unstable carotid plaque. Atherosclerosis 2010, 208, 83–89. [Google Scholar] [CrossRef]
- Ammirati, E.; Fogacci, F. Clinical relevance of biomarkers for the identification of patients with carotid atherosclerotic plaque: Potential role and limitations of cysteine protease legumain. Atherosclerosis 2017, 257, 248–249. [Google Scholar] [CrossRef]
- Sato, K.; Shirai, R.; Hontani, M.; Shinooka, R.; Hasegawa, A.; Kichise, T.; Yamashita, T.; Yoshizawa, H.; Watanabe, R.; Matsuyama, T.; et al. Potent vasoconstrictor kisspeptin-10 induces atherosclerotic plaque progression and instability: Reversal by its receptor GPR54 antagonist. J. Am. Heart Assoc. 2017, 6, e005790. [Google Scholar] [CrossRef]
- Konii, H.; Sato, K.; Kikuchi, S.; Okiyama, H.; Watanabe, R.; Hasegawa, A.; Yamamoto, K.; Itoh, F.; Hirano, T.; Watanabe, T. Stimulatory effects of cardiotrophin 1 on atherosclerosis. Hypertension 2013, 62, 942–950. [Google Scholar] [CrossRef]
- Morita, Y.; Araki, H.; Sugimoto, T.; Takeuchi, K.; Yamane, T.; Maeda, T.; Yamamoto, Y.; Nishi, K.; Asano, M.; Shirahama-Noda, K.; et al. Legumain/asparaginyl endopeptidase controls extracellular matrix remodeling through the degradation of fibronectin in mouse renal proximal tubular cells. FEBS Lett. 2007, 581, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Xiong, M.; Chen, C.; Du, L.; Liu, Z.; Shi, Y.; Zhang, M.; Gong, J.; Song, X.; Xiang, R.; et al. Legumain, an asparaginyl endopeptidase, mediates the effect of M2 macrophages on attenuating renal interstitial fibrosis in obstructive nephropathy. Kidney Int. 2018, 94, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Dall, E.; Brandstetter, H. Mechanistic and structural studies on legumain explain its zymogenicity, distinct activation pathways, and regulation. Proc. Natl. Acad. Sci. USA 2013, 110, 10940–10945. [Google Scholar] [CrossRef] [PubMed]
- Leosco, D.; Fineschi, M.; Pierli, C.; Fiaschi, A.; Ferrara, N.; Bianco, S.; Longobardi, G.; Pisani, E.; Bravi, A.; Rengo, F. Intracoronary serotonin release after high-pressure coronary stenting. Am. J. Cardiol. 1999, 84, 1317–1322. [Google Scholar] [CrossRef]
- Schuijt, M.P.; van Kats, J.P.; de Zeeuw, S.; Duncker, D.J.; Verdouw, P.D.; Schalekamp, M.A.D.H.; Danser, A.H.J. Cardiac interstitial fluid levels of angiotensin I and II in the pig. J. Hypertens. 1999, 17, 1885–1891. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Obianyo, O.; Du, Y.; Fu, H.; Li, S.; Ye, K. Blockade of asparagine endopeptidase inhibits cancer metastasis. J. Med. Chem. 2017, 60, 7244–7255. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Obianyo, O.; Dall, E.; Du, Y.; Fu, H.; Liu, X.; Kang, S.S.; Song, M.; Yu, S.P.; Cabrele, C.; et al. Inhibition of delta-secretase improves cognitive functions in mouse models of Alzheimer’s disease. Nat. Commun. 2017, 8, 14740. [Google Scholar] [CrossRef]
- Wang, Z.H.; Liu, X.L.; Zhong, M.; Zhang, L.P.; Shang, Y.Y.; Hu, X.Y.; Li, L.; Zhang, Y.; Deng, J.T.; Zhang, W. Pleiotropic effects of atorvastatin on monocytes in atherosclerotic patients. J. Clin. Pharmacol. 2010, 50, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.; Solberg, R.; Jacobsen, L.L.; Voreland, A.L.; Rustan, A.C.; Thoresen, G.H.; Johansen, H.T. Simvastatin inhibits glucose metabolism and legumain activity in human myotubes. PLoS ONE 2014, 9, e85721. [Google Scholar] [CrossRef]
- Naito, C.; Hashimoto, M.; Watanabe, K.; Shirai, R.; Takahashi, Y.; Kojima, M.; Watanabe, R.; Sato, K.; Iso, Y.; Matsuyama, T.; et al. Facilitatory effects of fetuin-A on atherosclerosis. Atherosclerosis 2016, 246, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Watanabe, H.; Takahashi, Y.; Kojima, M.; Konii, H.; Watanabe, K.; Shirai, R.; Sato, K.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Atheroprotective effects of tumor necrosis factor-stimulated gene-6. JACC Basic Transl. Sci. 2016, 6, 494–509. [Google Scholar] [CrossRef] [PubMed]
- Shirai, R.; Sato, K.; Yamashita, T.; Yamaguchi, M.; Okano, T.; Watanabe-Kominato, K.; Watanabe, R.; Matsuyama, T.; Ishibashi-Ueda, H.; Koba, S.; et al. Neopterin counters vascular inflammation and atherosclerosis. J. Am. Heart Assoc. 2018, 7, e007359. [Google Scholar] [CrossRef]
- Sato, K.; Yamashita, T.; Shirai, R.; Shibata, K.; Okano, T.; Yamaguchi, M.; Mori, Y.; Matsuyama, T.; Ishibashi-Ueda, H.; Hirano, T.; et al. Adropin contributes to anti-atherosclerosis by suppressing monocyte-endothelial cell adhesion and smooth muscle cell proliferation. Int. J. Mol. Sci. 2018, 19, 1293. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Shirai, R.; Yamaguchi, M.; Yamashita, T.; Shibata, K.; Okano, T.; Mori, Y.; Matsuyama, T.; Ishibashi-Ueda, H.; Hirano, T.; et al. Anti-atherogenic effects of vaspin on human aortic smooth muscle cell/macrophage responses and hyperlipidemic mouse plaque phenotype. Int. J. Mol. Sci. 2018, 19, 1732. [Google Scholar] [CrossRef] [PubMed]

| Saline (n = 4) | Legumain (n = 8) | p-Value | |
|---|---|---|---|
| Body weight (g) | 29.8 ± 0.8 | 27.9 ± 0.8 | 0.1818 |
| Food intake (g/d) | 3.05 ± 0.20 | 3.05 ± 0.23 | 0.9854 |
| Systolic blood pressure (mm Hg) | 97.0 ± 3.2 | 99.5 ± 2.6 | 0.5750 |
| Diastolic blood pressure (mm Hg) | 72.8 ± 3.5 | 75.4 ± 2.6 | 0.5664 |
| Glucose (mg/dL) | 260.6 ± 35.2 | 216.2 ± 14.8 | 0.1942 |
| Total cholesterol (mg/dL) | 1342.1 ± 41.4 | 1607.7 ± 123.4 | 0.1729 |
| Triglycerides (mg/dL) | 242.9 ± 34.6 | 209.9 ± 19.7 | 0.3907 |
| Free fatty acids (mEq/L) | 2.08 ± 0.25 | 2.18 ± 0.21 | 0.7825 |
| Insulin (ng/mL) | 0.21 ± 0.05 | 0.09 ± 0.04 | 0.0966 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozawa, N.; Sato, Y.; Mori, Y.; Masuda, H.; Yamane, M.; Yamamoto, Y.; Shirai, R.; Watanabe, R.; Sato, K.; Mori, Y.; et al. Legumain Promotes Atherosclerotic Vascular Remodeling. Int. J. Mol. Sci. 2019, 20, 2195. https://doi.org/10.3390/ijms20092195
Ozawa N, Sato Y, Mori Y, Masuda H, Yamane M, Yamamoto Y, Shirai R, Watanabe R, Sato K, Mori Y, et al. Legumain Promotes Atherosclerotic Vascular Remodeling. International Journal of Molecular Sciences. 2019; 20(9):2195. https://doi.org/10.3390/ijms20092195
Chicago/Turabian StyleOzawa, Nana, Yuki Sato, Yukari Mori, Hiroko Masuda, Mao Yamane, Yuka Yamamoto, Remina Shirai, Rena Watanabe, Kengo Sato, Yusaku Mori, and et al. 2019. "Legumain Promotes Atherosclerotic Vascular Remodeling" International Journal of Molecular Sciences 20, no. 9: 2195. https://doi.org/10.3390/ijms20092195
APA StyleOzawa, N., Sato, Y., Mori, Y., Masuda, H., Yamane, M., Yamamoto, Y., Shirai, R., Watanabe, R., Sato, K., Mori, Y., Hirano, T., & Watanabe, T. (2019). Legumain Promotes Atherosclerotic Vascular Remodeling. International Journal of Molecular Sciences, 20(9), 2195. https://doi.org/10.3390/ijms20092195







