Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain
Abstract
1. Introduction
2. Results
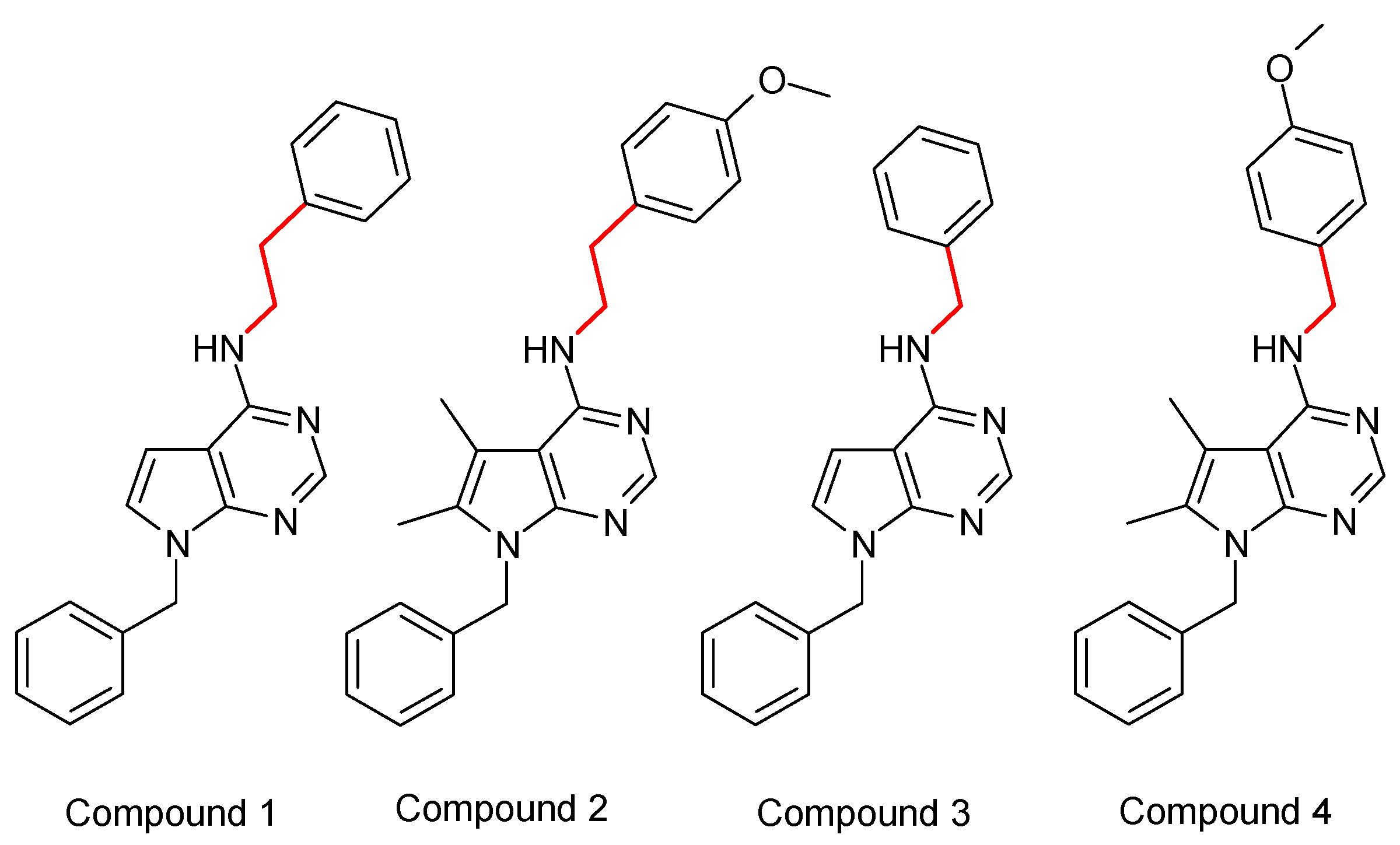
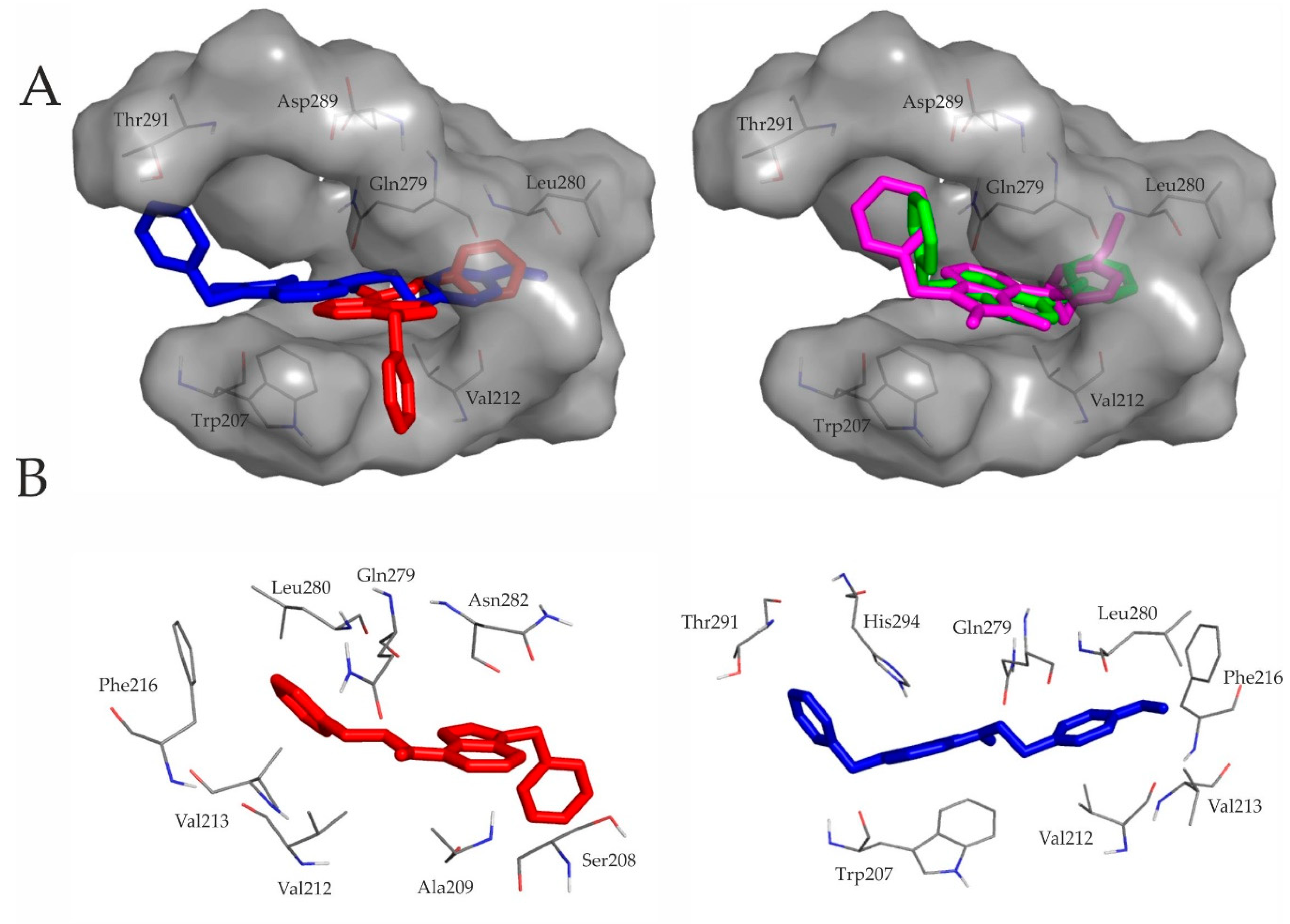
2.1. Binding of the Novel Pyrrolo-Pyrimidine Compounds to the sst4 Target In Silico: Structural Calculations
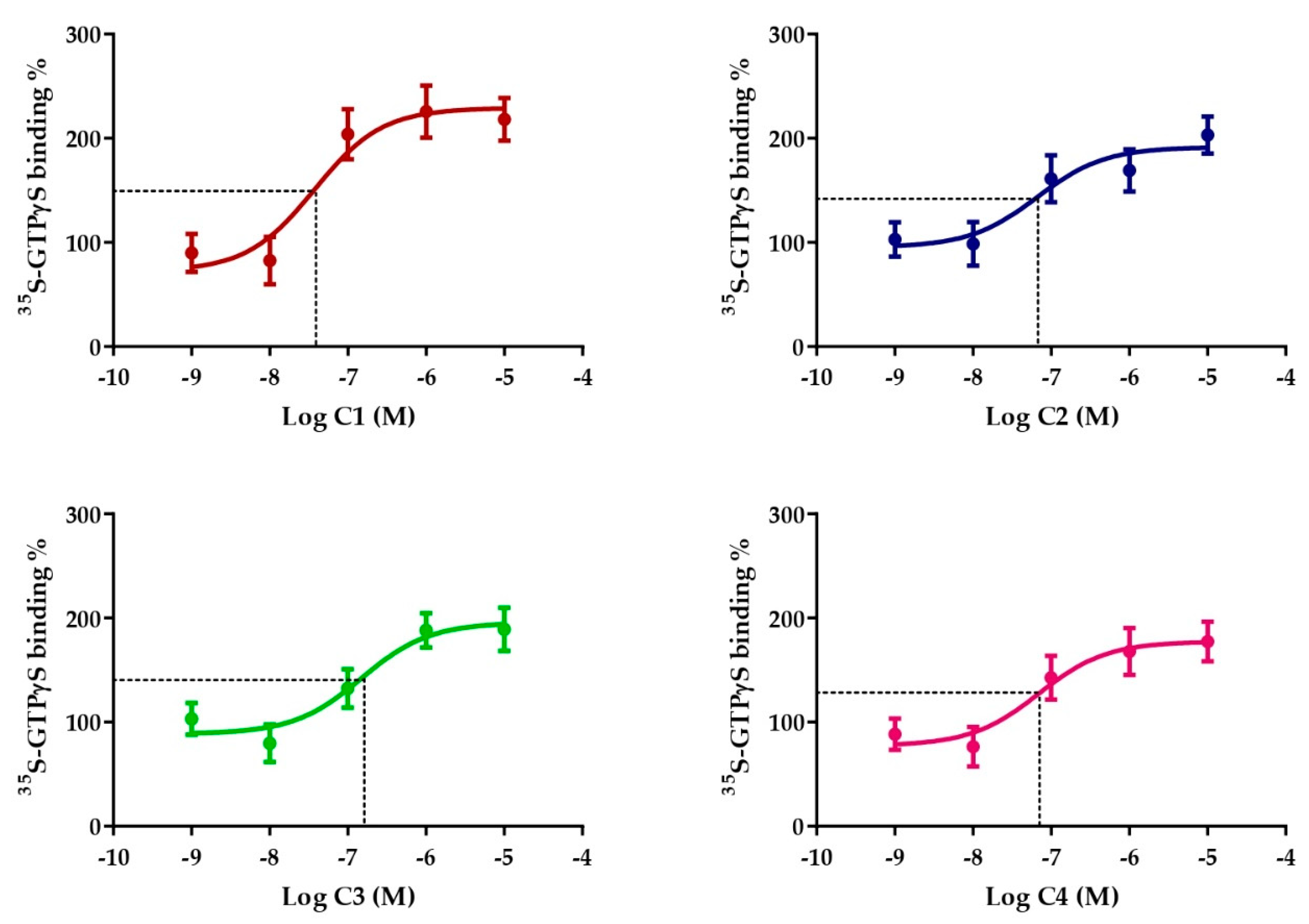
2.2. Somatostatin-Receptor-4-Linked G-Protein Activation by the Novel Pyrrolo-Pyrimidine Compounds on Stable Receptor-Expressing Cells
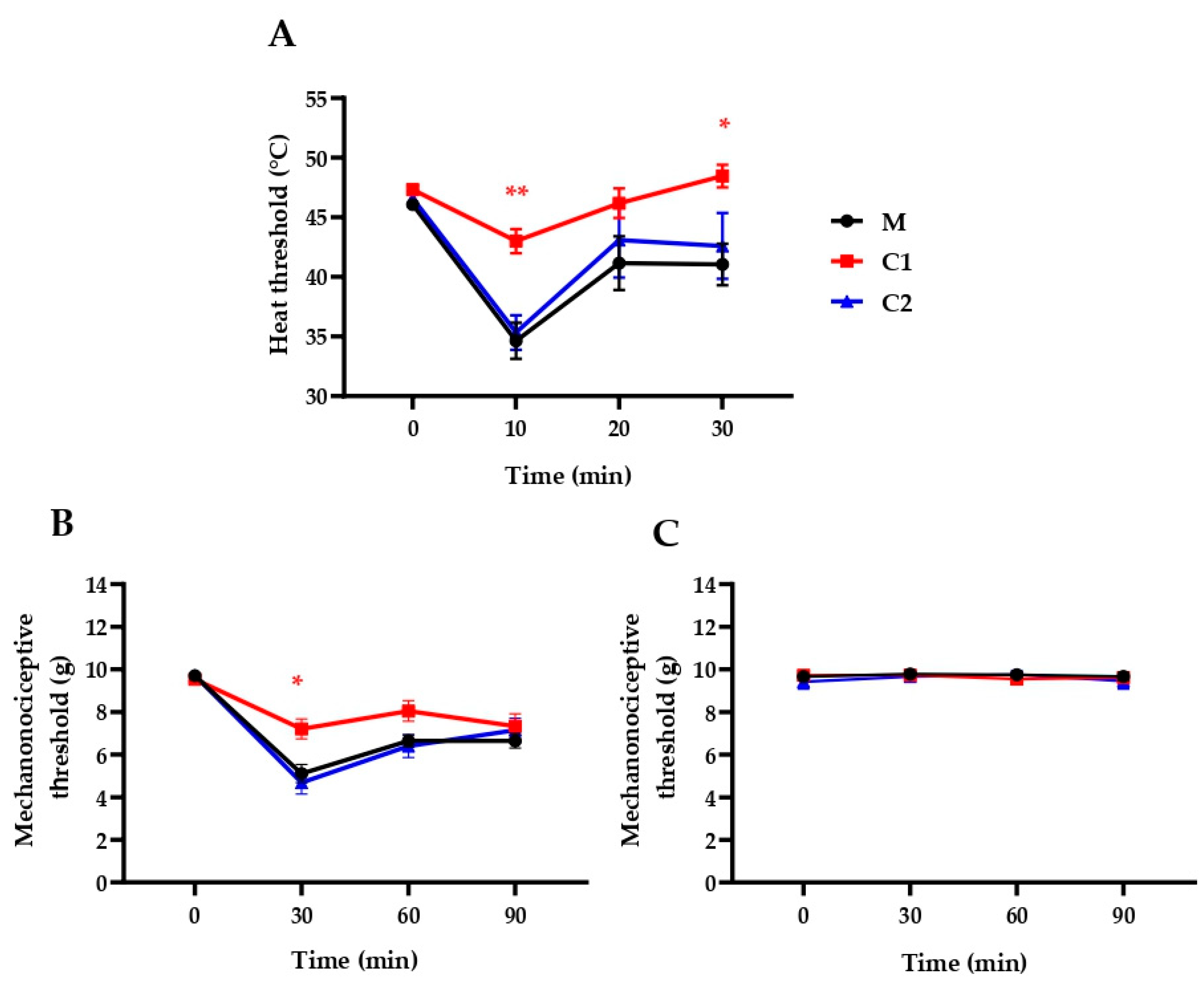
2.3. C1 Compound Decreases RTX-Induced Inflammatory Thermal Allodynia and Mechanical Hyperalgesia
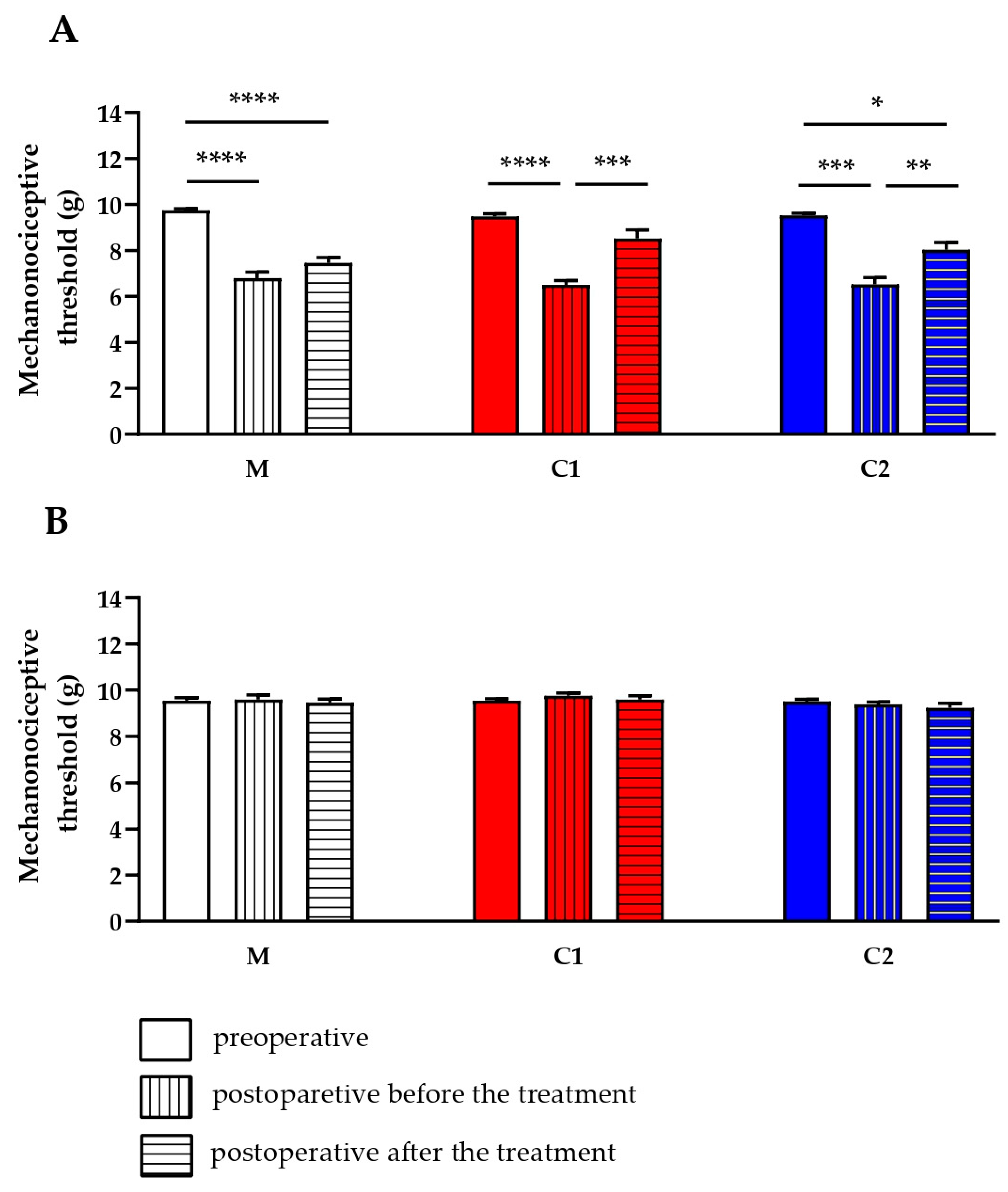
2.4. C1 and C2 Compounds Reduce Chronic Neuropathic Mechanical Hyperalgesia
2.5. Selectivity Profile of Compound 1
3. Discussion
4. Materials and Methods
4.1. In Silico Molecula Modeling Studies (Structural Calculations)
4.1.1. Preparation of Ligand and Target Structures.
4.1.2. Grid Calculation and Docking.
4.2. Somatostatin-Receptor-4-Linked G-Protein Activation Assay
4.3. Acute Neurogenic Inflammatory Thermal Allodynia and Mechanical Hyperalgesia
4.4. Chronic Traumatic Neuropathic Pain Model
4.5. Selectivity Profile Determination
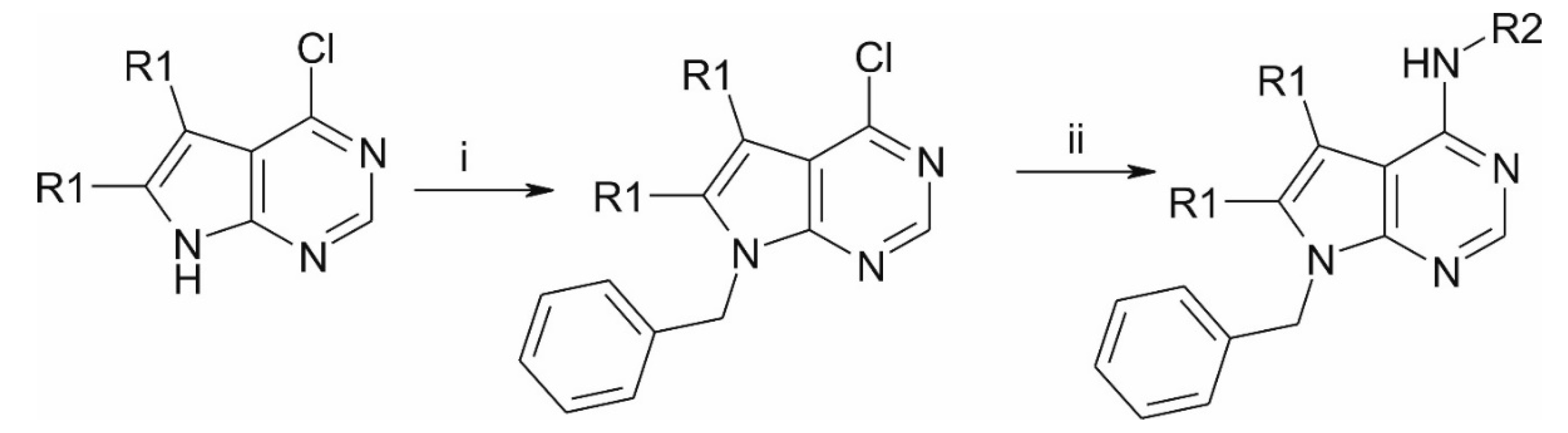
4.6. Synthesis of the Compounds
4.7. Solution Preparation
4.8. Animals and Ethics
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| GPCR | G-protein coupled receptor |
| TMD | transmembrane domain |
| SRIF1 | somatotropin release-inhibiting factor |
| RO5 | Lipinksi’s rule of five |
| MW | molecular weight |
| mlogP | logarithm of octanol/water partition coefficient according to Morigucchi |
| RTX | resiniferatoxin |
| TRPV1 | transient receptor potential vanilloid 1 |
| PDB | Protein Databank |
| RMSD | root mean square deviation |
| GTP | guanosine triphosphate |
| GDP | guanosine diphosphate |
| DPA | dynamic plantar aesthesiometer |
| DMSO | dimethyl sulfoxide |
| MC | methylcellulose |
References
- Szolcsányi, J.; Helyes, Z.; Oroszi, G.; Németh, J.; Pintér, E. Release of somatostatin and its role in the mediation of the anti-inflammatory effect induced by antidromic stimulation of sensory fibres of rat sciatic nerve. Br. J. Pharm. 1998, 123, 936–942. [Google Scholar] [CrossRef] [PubMed]
- Pintér, E.; Helyes, Z.; Szolcsányi, J. Inhibitory effect of somatostatin on inflammation and nociception. Pharmacol. Ther. 2006, 112, 440–456. [Google Scholar] [CrossRef] [PubMed]
- Szolcsányi, J.; Pintér, E.; Helyes, Z.; Oroszi, G.; Németh, J. Systemic anti-inflammatory effect induced by counter-irritation through a local release of somatostatin from nociceptors. Br. J. Pharmacol. 1998, 125, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Szolcsányi, J. Forty years in capsaicin research for sensory pharmacology and physiology. Neuropeptides 2004, 38, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Larouche, V.; Akirov, A.; Alshehri, S.; Ezzat, S. Management of Small Bowel Neuroendocrine Tumors. Cancers 2019, 11, 1395. [Google Scholar] [CrossRef] [PubMed]
- Riedemann, T. Diversity and Function of Somatostatin-Expressing Interneurons in the Cerebral Cortex. Int. J. Mol. Sci. 2019, 20, 2952. [Google Scholar] [CrossRef]
- Lambert, G.A.; Zagami, A.S. Does somatostatin have a role to play in migraine headache? Neuropeptides 2018, 69, 1–8. [Google Scholar] [CrossRef]
- Stengel, A.; Taché, Y. Central somatostatin signaling and regulation of food intake. Ann. N. Y. Acad. Sci. 2019, 1455, 98–104. [Google Scholar] [CrossRef]
- Günther, T.; Tulipano, G.; Dournaud, P.; Bousquet, C.; Csaba, Z.; Kreienkamp, H.-J.; Lupp, A.; Korbonits, M.; Castaño, J.P.; Wester, H.-J.; et al. International Union of Basic and Clinical Pharmacology. CV. Somatostatin Receptors: Structure, Function, Ligands, and New Nomenclature. Pharmacol. Rev. 2018, 70, 763–835. [Google Scholar] [CrossRef]
- Hoyer, D.; Bell, G.I.; Berelowitz, M.; Epelbaum, J.; Feniuk, W.; Humphrey, P.P.; O’Carroll, A.M.; Patel, Y.C.; Schonbrunn, A.; Taylor, J.E. Classification and nomenclature of somatostatin receptors. Trends Pharmacol. Sci. 1995, 16, 86–88. [Google Scholar] [CrossRef]
- Patel, Y.C. Somatostatin and its receptor family. Front. Neuroendocr. 1999, 20, 157–198. [Google Scholar] [CrossRef] [PubMed]
- Somvanshi, R.K.; Kumar, U. δ-Opioid Receptor and Somatostatin Receptor-4 Heterodimerization: Possible Implications in Modulation of Pain Associated Signaling. PLoS ONE 2014, 9, e85193. [Google Scholar] [CrossRef] [PubMed]
- Szolcsányi, J.; Pintér, E.; Helyes, Z.; Petho, G. Inhibition of the function of TRPV1-expressing nociceptive sensory neurons by somatostatin 4 receptor agonism: Mechanism and therapeutical implications. Curr. Top. Med. Chem. 2011, 11, 2253–2263. [Google Scholar] [CrossRef] [PubMed]
- Helyes, Z.; Thán, M.; Oroszi, G.; Pintér, E.; Németh, J.; Kéri, G.; Szolcsányi, J. Anti-nociceptive effect induced by somatostatin released from sensory nerve terminals and by synthetic somatostatin analogues in the rat. Neurosci. Lett. 2000, 278, 185–188. [Google Scholar] [CrossRef]
- Sándor, K.; Elekes, K.; Szabó, A.; Pintér, E.; Engström, M.; Wurster, S.; Szolcsányi, J.; Helyes, Z. Analgesic effects of the somatostatin sst4 receptor selective agonist J-2156 in acute and chronic pain models. Eur. J. Pharmacol. 2006, 539, 71–75. [Google Scholar] [CrossRef]
- Helyes, Z.; Pintér, E.; Sándor, K.; Elekes, K.; Bánvölgyi, A.; Keszthelyi, D.; Szoke, E.; Tóth, D.M.; Sándor, Z.; Kereskai, L.; et al. Impaired defense mechanism against inflammation, hyperalgesia, and airway hyperreactivity in somatostatin 4 receptor gene-deleted mice. Proc. Natl. Acad. Sci. USA 2009, 106, 13088–13093. [Google Scholar] [CrossRef]
- Thán, M.; Németh, J.; Szilvássy, Z.; Pintér, E.; Helyes, Z.; Szolcsányi, J. Systemic anti-inflammatory effect of somatostatin released from capsaicin-sensitive vagal and sciatic sensory fibres of the rat and guinea-pig. Eur. J. Pharmacol. 2000, 399, 251–258. [Google Scholar] [CrossRef]
- Lilly Clinical Development Pipeline. Available online: https://www.lilly.com/discovery/pipeline (accessed on 27 September 2019).
- Hannon, J.P.; Nunn, C.; Stolz, B.; Bruns, C.; Weckbecker, G.; Lewis, I.; Troxler, T.; Hurth, K.; Hoyer, D. Drug Design at Peptide Receptors. JMN 2002, 18, 15–28. [Google Scholar] [CrossRef]
- Feytens, D.; Cescato, R.; Reubi, J.C.; Tourwé, D. New sst4/5-selective somatostatin peptidomimetics based on a constrained tryptophan scaffold. J. Med. Chem. 2007, 50, 3397–3401. [Google Scholar] [CrossRef]
- Rivier, J.; Erchegyi, J.; Hoeger, C.; Miller, C.; Low, W.; Wenger, S.; Waser, B.; Schaer, J.-C.; Reubi, J.C. Novel sst4-Selective Somatostatin (SRIF) Agonists. 1. Lead Identification Using a Betide Scan. J. Med. Chem. 2003, 46, 5579–5586. [Google Scholar] [CrossRef]
- Gademann, K.; Kimmerlin, T.; Hoyer, D.; Seebach, D. Peptide Folding Induces High and Selective Affinity of a Linear and Small β-Peptide to the Human Somatostatin Receptor 4. J. Med. Chem. 2001, 44, 2460–2468. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Birzin, E.T.; McVaugh, C.T.; van Rijn, R.D.; Rohrer, S.P.; Chicchi, G.; Underwood, D.J.; Thornton, E.R.; Smith, A.B.; Hirschmann, R. Effects of Heterocyclic Aromatic Substituents on Binding Affinities at Two Distinct Sites of Somatostatin Receptors. Correlation with the Electrostatic Potential of the Substituents. J. Med. Chem. 2003, 46, 1858–1869. [Google Scholar] [CrossRef] [PubMed]
- Kéri, G.; Erchegyi, J.; Horváth, A.; Mezõ, I.; Idei, M.; Vántus, T.; Balogh, A.; Vadász, Z.; Bökönyi, G.; Seprõdi, J.; et al. A tumor-selective somatostatin analog (TT-232) with strong in vitro and in vivo antitumor activity. Proc. Natl. Acad. Sci. USA 1996, 93, 12513–12518. [Google Scholar] [CrossRef] [PubMed]
- Michael Crider, A.; Witt, K. Somatostatin sst4 Ligands: Chemistry and Pharmacology. MRMC 2007, 7, 213–220. [Google Scholar] [CrossRef]
- Helyes, Z.; Pintér, E.; Németh, J.; Kéri, G.; Thán, M.; Oroszi, G.; Horváth, A.; Szolcsányi, J. Anti-inflammatory effect of synthetic somatostatin analogues in the rat. Br. J. Pharmacol. 2001, 134, 1571–1579. [Google Scholar] [CrossRef]
- Pintér, E.; Helyes, Z.; Németh, J.; Pórszász, R.; Pethö, G.; Thán, M.; Kéri, G.; Horváth, A.; Jakab, B.; Szolcsányi, J. Pharmacological characterisation of the somatostatin analogue TT-232: Effects on neurogenic and non-neurogenic inflammation and neuropathic hyperalgesia. Naunyn Schmiedebergs Arch. Pharm. 2002, 366, 142–150. [Google Scholar] [CrossRef]
- Elekes, K.; Helyes, Z.; Kereskai, L.; Sándor, K.; Pintér, E.; Pozsgai, G.; Tékus, V.; Bánvölgyi, Á.; Németh, J.; Szűts, T.; et al. Inhibitory effects of synthetic somatostatin receptor subtype 4 agonists on acute and chronic airway inflammation and hyperreactivity in the mouse. Eur. J. Pharmacol. 2008, 578, 313–322. [Google Scholar] [CrossRef]
- Helyes, Z.; Szabó, Á.; Németh, J.; Jakab, B.; Pintér, E.; Bánvölgyi, Á.; Kereskai, L.; Kéri, G.; Szolcsányi, J. Antiinflammatory and analgesic effects of somatostatin released from capsaicin-sensitive sensory nerve terminals in a Freund’s adjuvant–induced chronic arthritis model in the rat. Arthritis Rheum 2004, 50, 1677–1685. [Google Scholar] [CrossRef]
- Weckbecker, G.; Lewis, I.; Albert, R.; Schmid, H.A.; Hoyer, D.; Bruns, C. Opportunities in somatostatin research: Biological, chemical and therapeutic aspects. Nat. Rev. Drug Discov. 2003, 2, 999–1017. [Google Scholar] [CrossRef]
- Engström, M.; Tomperi, J.; El-Darwish, K.; Åhman, M.; Savola, J.-M.; Wurster, S. Superagonism at the Human Somatostatin Receptor Subtype 4. J. Pharm. Exp. Ther. 2005, 312, 332–338. [Google Scholar] [CrossRef]
- Scheich, B.; Gaszner, B.; Kormos, V.; László, K.; Ádori, C.; Borbély, É.; Hajna, Z.; Tékus, V.; Bölcskei, K.; Ábrahám, I.; et al. Somatostatin receptor subtype 4 activation is involved in anxiety and depression-like behavior in mouse models. Neuropharmacology 2016, 101, 204–215. [Google Scholar] [CrossRef]
- Schuelert, N.; Just, S.; Kuelzer, R.; Corradini, L.; Gorham, L.C.J.; Doods, H. The somatostatin receptor 4 agonist J-2156 reduces mechanosensitivity of peripheral nerve afferents and spinal neurons in an inflammatory pain model. Eur. J. Pharmacol. 2015, 746, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Park, T.S.W.; Khan, N.; Kuo, A.; Nicholson, J.R.; Corradini, L.; Smith, M.T. J-2156, a somatostatin receptor type 4 agonist, alleviates mechanical hyperalgesia in a rat model of chronic low back pain. Biomed. Pharmacother. 2019, 117, 109056. [Google Scholar] [CrossRef] [PubMed]
- Gorham, L.; Just, S.; Doods, H. Somatostatin 4 receptor activation modulates TPRV1 currents in dorsal root ganglion neurons. Neurosci. Lett. 2014, 573, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Tang, C.; Ho, B.; Ankersen, M.; Stidsen, C.E.; Crider, A.M. Nonpeptide somatostatin agonists with sst4 selectivity: Synthesis and structure-activity relationships of thioureas. J. Med. Chem. 1998, 41, 4693–4705. [Google Scholar] [CrossRef] [PubMed]
- Rohrer, S.P.; Birzin, E.T.; Mosley, R.T.; Berk, S.C.; Hutchins, S.M.; Shen, D.-M.; Xiong, Y.; Hayes, E.C.; Parmar, R.M.; Foor, F.; et al. Rapid Identification of Subtype-Selective Agonists of the Somatostatin Receptor Through Combinatorial Chemistry. Science 1998, 282, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, K.E.; Witt, K.A.; Crider, A.M.; Kontoyianni, M. Somatostatin Receptor-4 Agonists as Candidates for Treatment of Alzheimer’s Disease. In Drug Design and Discovery in Alzheimer’s Disease; Elsevier: Amsterdam, The Netherlands, 2014; pp. 566–597. ISBN 978-0-12-803959-5. [Google Scholar]
- Qiu, C.; Zeyda, T.; Johnson, B.; Hochgeschwender, U.; de Lecea, L.; Tallent, M.K. Somatostatin Receptor Subtype 4 Couples to the M-Current to Regulate Seizures. J. Neurosci. 2008, 28, 3567–3576. [Google Scholar] [CrossRef]
- Szolcsányi, J.; Pintér, E.; Helyes, Z.; Szőke, É.; Wáczek, F.; Őrfi, L.; Kéri, G.; Szűts, T. New agents for treating neurogenic inflammation and neuropathic hyperalgesia related disorders 2016. U.S. Patent 10,344,032, 9 July 2019. [Google Scholar]
- Moriguchi, I.; Hirono, S.; Liu, Q.; Nakagome, I.; Matsushita, Y. Simple Method of Calculating Octanol/Water Partition Coefficient. Chem. Pharm. Bull. 1992, 40, 127–130. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings1PII of original article: S0169-409X(96)00423-1. The article was originally published in Advanced Drug Delivery Reviews 23 (1997) 3–25.1. Adv. Drug Deliv. Rev. 2001, 46, 3–26. [Google Scholar]
- García-Sosa, A.T.; Oja, M.; Hetényi, C.; Maran, U. Disease-Specific Differentiation Between Drugs and Non-Drugs Using Principal Component Analysis of Their Molecular Descriptor Space. Mol. Inf. 2012, 31, 369–383. [Google Scholar] [CrossRef]
- Liu, Z.; Crider, A.M.; Ansbro, D.; Hayes, C.; Kontoyianni, M. A structure-based approach to understanding somatostatin receptor-4 agonism (sst4). J. Chem. Inf. Model 2012, 52, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Engström, M.; Savola, J.-M.; Wurster, S. Differential Efficacies of Somatostatin Receptor Agonists for G-Protein Activation and Desensitization of Somatostatin Receptor Subtype 4-Mediated Responses. J. Pharm. Exp. 2006, 316, 1262–1268. [Google Scholar] [CrossRef] [PubMed]
- Szőke, É.; Bálint, M.; Hetényi, C.; Markovics, A.; Elekes, K.; Pozsgai, G.; Szűts, T.; Kéri, G.; Őrfi, L.; Sándor, Z.; et al. Small molecule somatostatin receptor subtype 4 (sst4) agonists are novel anti-inflammatory and analgesic drug candidates. Neuropharmacology 2019. submitted. [Google Scholar]
- Almási, R.; Pethö, G.; Bölcskei, K.; Szolcsányi, J. Effect of resiniferatoxin on the noxious heat threshold temperature in the rat: A novel heat allodynia model sensitive to analgesics. Br. J. Pharmacol. 2003, 139, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Sugiura, T.; Tominaga, M.; Katsuya, H.; Mizumura, K. Bradykinin Lowers the Threshold Temperature for Heat Activation of Vanilloid Receptor 1. J. Neurophysiol. 2002, 88, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, T.; Higashi, T.; Togashi, K.; Iida, T.; Segi, E.; Sugimoto, Y.; Tominaga, T.; Narumiya, S.; Tominaga, M. Sensitization of TRPV1 by EP1 and IP reveals peripheral nociceptive mechanism of prostaglandins. Mol. Pain 2005, 1, 3. [Google Scholar] [CrossRef]
- Tékus, V.; Bölcskei, K.; Kis-Varga, Á.; Dézsi, L.; Szentirmay, É.; Visegrády, A.; Horváth, C.; Szolcsányi, J.; Pethő, G. Effect of transient receptor potential vanilloid 1 (TRPV1) receptor antagonist compounds SB705498, BCTC and AMG9810 in rat models of thermal hyperalgesia measured with an increasing-temperature water bath. Eur. J. Pharmacol. 2010, 641, 135–141. [Google Scholar] [CrossRef]
- Meyer, R.; Campbell, J. Myelinated nociceptive afferents account for the hyperalgesia that follows a burn to the hand. Science 1981, 213, 1527–1529. [Google Scholar] [CrossRef]
- Szolcsányi, J.; Bölcskei, K.; Szabó, Á.; Pintér, E.; Pethő, G.; Elekes, K.; Börzsei, R.; Almási, R.; Szűts, T.; Kéri, G.; et al. Analgesic effect of TT-232, a heptapeptide somatostatin analogue, in acute pain models of the rat and the mouse and in streptozotocin-induced diabetic mechanical allodynia. Eur. J. Pharmacol. 2004, 498, 103–109. [Google Scholar] [CrossRef]
- Selmer, I.-S.; Schindler, M.; Humphrey, P.P.A.; Waldvogel, H.J.; Faull, R.L.M.; Emson, P.C. First localisation of somatostatin sst4 receptor protein in selected human brain areas: An immunohistochemical study. Mol. Brain Res. 2000, 82, 114–125. [Google Scholar] [CrossRef]
- Selmer, I.-S.; Schindler, M.; Humphrey, P.P.A.; Emson, P.C. Immunohistochemical localization of the somatostatin sst4 receptor in rat brain. Neuroscience 2000, 98, 523–533. [Google Scholar] [CrossRef]
- Seltzer, Z.; Dubner, R.; Shir, Y. A novel behavioral model of neuropathic pain disorders produced in rats by partial sciatic nerve injury. Pain 1990, 43, 205–218. [Google Scholar] [CrossRef]
- Botz, B.; Imreh, A.; Sándor, K.; Elekes, K.; Szolcsányi, J.; Reglődi, D.; Quinn, J.P.; Stewart, J.; Zimmer, A.; Hashimoto, H.; et al. Role of Pituitary Adenylate-Cyclase Activating Polypeptide and Tac1 gene derived tachykinins in sensory, motor and vascular functions under normal and neuropathic conditions. Peptides 2013, 43, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Basbaum, A.I. Distinct neurochemical features of acute and persistent pain. Proc. Natl. Acad. Sci. USA 1999, 96, 7739–7743. [Google Scholar] [CrossRef]
- Dellemijn, P. Are opioids effective in relieving neuropathic pain? Pain 1999, 80, 453–462. [Google Scholar] [CrossRef]
- Suzuki, R.; Dickenson, A.H. Neuropathic pain: Nerves bursting with excitement. NeuroReport 2000, 11, R17–R21. [Google Scholar] [CrossRef]
- Botz, B.; Bölcskei, K.; Helyes, Z. Challenges to develop novel anti-inflammatory and analgesic drugs. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017, 9, e1427. [Google Scholar] [CrossRef]
- Schrödinger Release 2017–4: Maestro; Schrödinger, LLC: New York, NY, USA, 2017.
- Stewart, J.J.P. Stewart Computational Chemistry. MOPAC: Colorado Springs, CO, USA, 2016. Available online: http://OpenMOPAC.net (accessed on 12 October 2019).
- Stewart, J.J.P. Optimization of parameters for semiempirical methods VI: More modifications to the NDDO approximations and re-optimization of parameters. J. Mol. Model. 2013, 19, 1–32. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. GROMACS: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX 2015, 1–2, 19–25. [Google Scholar] [CrossRef]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated Docking with Selective Receptor Flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [PubMed]
- Markovics, A.; Szőke, É.; Sándor, K.; Börzsei, R.; Bagoly, T.; Kemény, Á.; Elekes, K.; Pintér, E.; Szolcsányi, J.; Helyes, Z. Comparison of the Anti-inflammatory and Anti-nociceptive Effects of Cortistatin-14 and Somatostatin-14 in Distinct In Vitro and In Vivo Model Systems. J. Mol. Neurosci. 2012, 46, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.-L.; Khan, G.M.; Alloway, K.D.; Chen, S.-R. Resiniferatoxin Induces Paradoxical Changes in Thermal and Mechanical Sensitivities in Rats: Mechanism of Action. J. Neurosci. 2003, 23, 2911–2919. [Google Scholar] [CrossRef] [PubMed]
- Hunyady, Á.; Hajna, Z.; Gubányi, T.; Scheich, B.; Kemény, Á.; Gaszner, B.; Borbély, É.; Helyes, Z. Hemokinin-1 is an important mediator of pain in mouse models of neuropathic and inflammatory mechanisms. Brain Res. Bull. 2019, 147, 165–173. [Google Scholar] [CrossRef]
- Horváth, Á.; Tékus, V.; Bencze, N.; Szentes, N.; Scheich, B.; Bölcskei, K.; Szőke, É.; Mócsai, A.; Tóth-Sarudy, É.; Mátyus, P.; et al. Analgesic effects of the novel semicarbazide-sensitive amine oxidase inhibitor SZV 1287 in mouse pain models with neuropathic mechanisms: Involvement of transient receptor potential vanilloid 1 and ankyrin 1 receptors. Pharmacol. Res. 2018, 131, 231–243. [Google Scholar] [CrossRef]
- Wang, J.-B.; Johnson, P.S.; Persico, A.M.; Hawkins, A.L.; Griffin, C.A.; Uhl, G.R. Human μ opiate receptor: cDNA and genomic clones, pharmacologic characterization and chromosomal assignment. FEBS Lett. 1994, 338, 217–222. [Google Scholar] [CrossRef]
- Simonin, F.; Gaveriaux-Ruff, C.; Befort, K.; Matthes, H.; Lannes, B.; Micheletti, G.; Mattei, M.G.; Charron, G.; Bloch, B.; Kieffer, B. kappa-Opioid receptor in humans: cDNA and genomic cloning, chromosomal assignment, functional expression, pharmacology, and expression pattern in the central nervous system. Proc. Natl. Acad. Sci. USA 1995, 92, 7006–7010. [Google Scholar] [CrossRef]
- Weyler, W.; Salach, J.I. Purification and properties of mitochondrial monoamine oxidase type A from human placenta. J. Biol. Chem. 1985, 260, 13199–13207. [Google Scholar]
- Zhou, Q.-Y.; Grandy, D.K.; Thambi, L.; Kushner, J.A.; Tol, H.H.M.V.; Cone, R.; Pribnow, D.; Salon, J.; Bunzow, J.R.; Civelli, O. Cloning and expression of human and rat Dt dopamine receptors. Nature 1990, 347, 76–80. [Google Scholar] [CrossRef]
- Felder, C.C.; Joyce, K.E.; Briley, E.M.; Mansouri, J.; Mackie, K.; Blond, O.; Lai, Y.; Ma, A.L.; Mitchell, R.L. Comparison of the pharmacology and signal transduction of the human cannabinoid CB1 and CB2 receptors. Mol. Pharmacol. 1995, 48, 443–450. [Google Scholar]
- Payne, S.L.; Johansson, A.M.; Strange, P.G. Mechanisms of ligand binding and efficacy at the human D2(short) dopamine receptor: D2 dopamine receptor mechanisms. J. Neurochem. 2004, 82, 1106–1117. [Google Scholar] [CrossRef] [PubMed]
- Gould, R.J.; Murphy, K.M.; Snyder, S.H. [3H]nitrendipine-labeled calcium channels discriminate inorganic calcium agonists and antagonists. Proc. Natl. Acad. Sci. USA 1982, 79, 3656–3660. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.-P.; Mangano, T.; Hufeisen, S.; Setola, V.; Roth, B.L. Identification of Human Ether-à-go-go Related Gene Modulators by Three Screening Platforms in an Academic Drug-Discovery Setting. ASSAY Drug Dev. Technol. 2010, 8, 727–742. [Google Scholar] [CrossRef] [PubMed]
| Residues | Compound 1 | Compound 2 | Compound 3 | Compound 4 |
|---|---|---|---|---|
| Trp207 | x | x | x | |
| Ser208 | x | x | ||
| Ala209 | x | x | ||
| Val212 | x | x | x | x |
| Val213 | x | x | x | |
| Phe216 | x | x | x | x |
| Tyr276 | x | |||
| Gln277 | x | x | x | x |
| Lue280 | x | x | x | |
| Asn282 | x | x | x | |
| Leu283 | x | x | x | x |
| Asp289 | x | x | ||
| Ala290 | x | |||
| Thr291 | x | x | ||
| His294 | x | x | x |
| Compound 1 | Compound 2 | Compound 3 | Compound 4 | |
|---|---|---|---|---|
| Einter (kcal/mol) | −8.54 | −7.64 | −8.31 | −8.46 |
| MW | 328.4 | 386.5 | 314.4 | 372.5 |
| mlogP | 3.60 | 3.68 | 3.38 | 3.47 |
| NH-donor | 1 | 1 | 1 | 1 |
| NH-acceptor | 2 | 3 | 2 | 3 |
| Target | Specific Binding (%) | Enzymatic Activity (%) | Agonist/Antagonist Effect (%) |
|---|---|---|---|
| K+ channel hERG | 23.6 | ||
| Ca2+ channel | 19.4 | ||
| COX-2 | −10.4 | ||
| PDE3A | −15.0 | ||
| PDE4D2 | −0.6 | ||
| MAOA | 2.7 | ||
| CB1 | 30.8/−1.5 | ||
| CB2 | 58.9/7.7 | ||
| D1 | 3.3/−10 | ||
| D2S | 17.2/−11.5 | ||
| Delta (DOP) | −0.3/−1.4 | ||
| Kappa (KOP) | −1.5/23.6 | ||
| Mu (MOP) | 5.5/20.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kántás, B.; Börzsei, R.; Szőke, É.; Bánhegyi, P.; Horváth, Á.; Hunyady, Á.; Borbély, É.; Hetényi, C.; Pintér, E.; Helyes, Z. Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain. Int. J. Mol. Sci. 2019, 20, 6245. https://doi.org/10.3390/ijms20246245
Kántás B, Börzsei R, Szőke É, Bánhegyi P, Horváth Á, Hunyady Á, Borbély É, Hetényi C, Pintér E, Helyes Z. Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain. International Journal of Molecular Sciences. 2019; 20(24):6245. https://doi.org/10.3390/ijms20246245
Chicago/Turabian StyleKántás, Boglárka, Rita Börzsei, Éva Szőke, Péter Bánhegyi, Ádám Horváth, Ágnes Hunyady, Éva Borbély, Csaba Hetényi, Erika Pintér, and Zsuzsanna Helyes. 2019. "Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain" International Journal of Molecular Sciences 20, no. 24: 6245. https://doi.org/10.3390/ijms20246245
APA StyleKántás, B., Börzsei, R., Szőke, É., Bánhegyi, P., Horváth, Á., Hunyady, Á., Borbély, É., Hetényi, C., Pintér, E., & Helyes, Z. (2019). Novel Drug-Like Somatostatin Receptor 4 Agonists are Potential Analgesics for Neuropathic Pain. International Journal of Molecular Sciences, 20(24), 6245. https://doi.org/10.3390/ijms20246245






