Bioactive Glass Applications in Dentistry
Abstract
1. Introduction
2. Compositions of Bioactive Glass
3. Preparations of Bioactive Glass
4. Properties of Bioactive Glass
4.1. Bioactivity of Bioactive Glass
4.2. Antimicrobial Properties
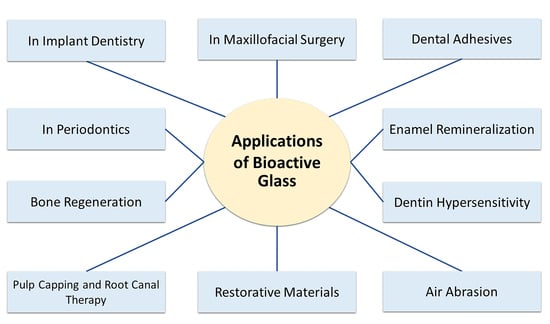
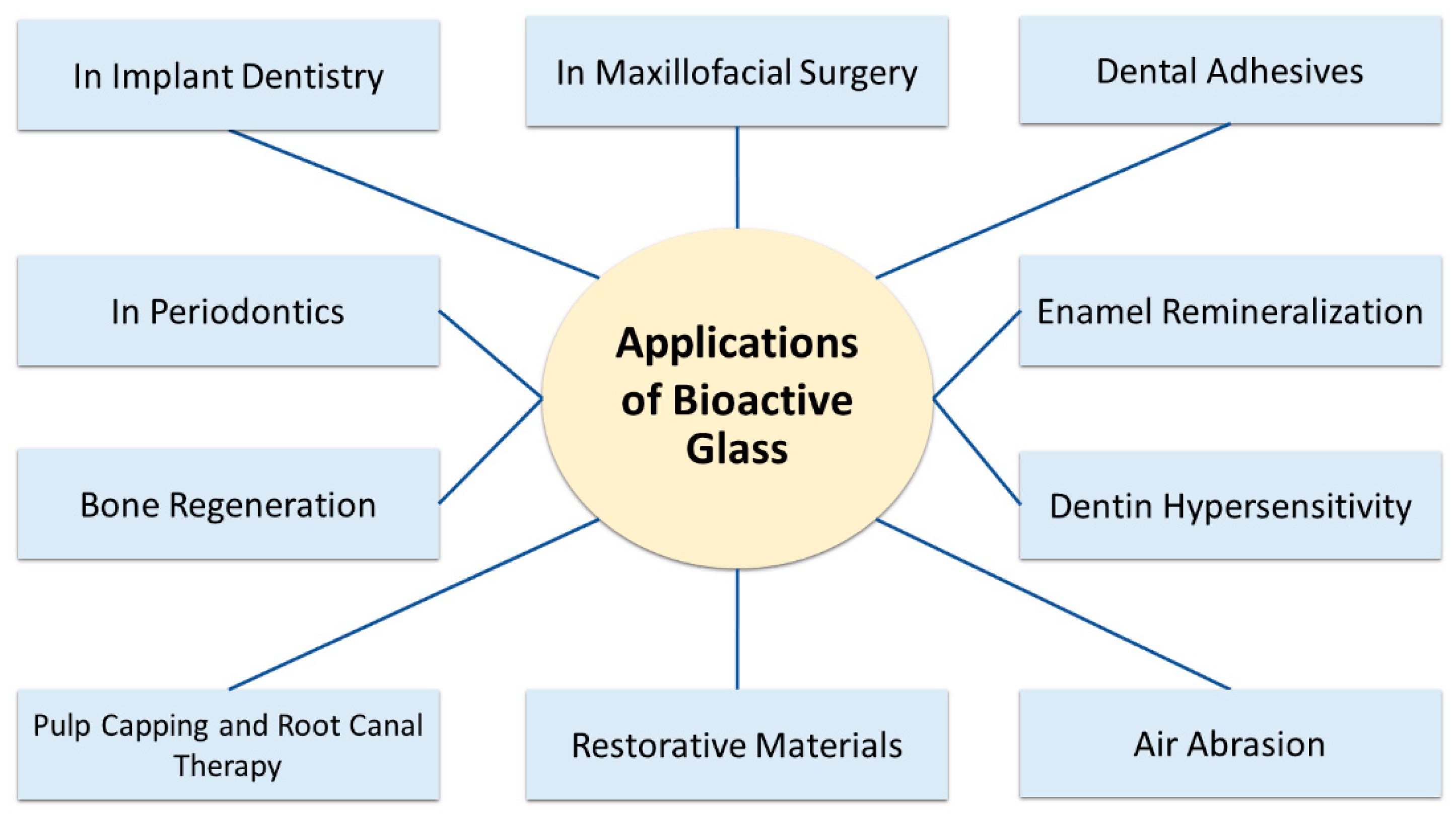
5. Clinical Applications of Bioactive Glasses in Dentistry
5.1. Dental Adhesives
5.2. Enamel Remineralization
5.3. Dentin Hypersensitivity
5.4. Air Abrasion
5.5. Restorative Materials
5.6. Pulp Capping and Root Canal Therapy
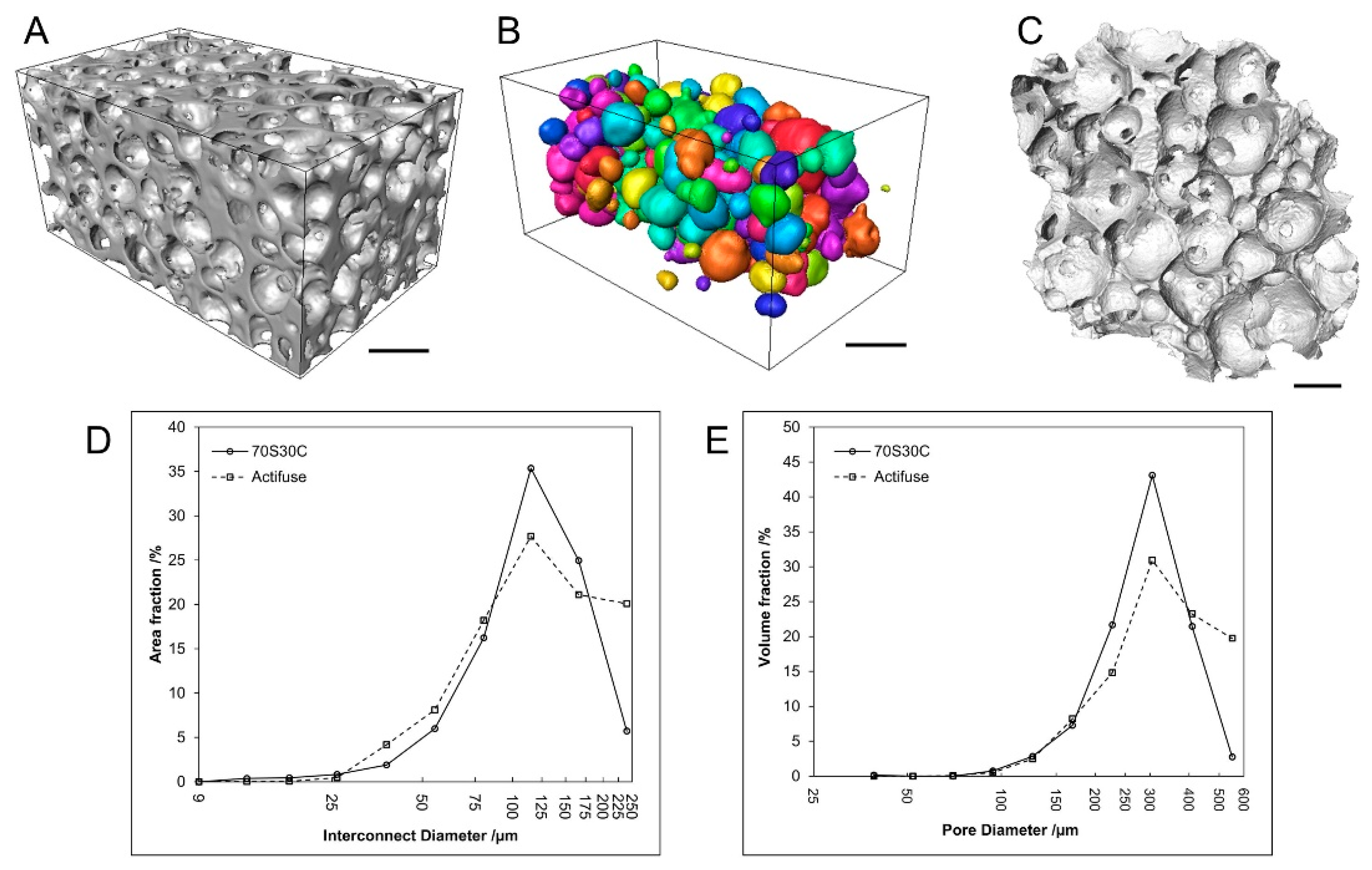
5.7. Bone Regeneration
5.8. In Periodontics
5.9. In Implant Dentistry
5.10. In Maxillofacial Surgery
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fernandes, H.R.; Gaddam, A.; Rebelo, A.; Brazete, D.; Stan, G.E.; Ferreira, J.M.F. Bioactive Glasses and Glass-Ceramics for Healthcare Applications in Bone Regeneration and Tissue Engineering. Materials 2018, 11, 2530. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Khurshid, Z.; Ghabbani, H.; Zafar, M.S.; Sefat, F. 10-Nano glass ionomer cement: Modification for biodental applications. In Advanced Dental Biomaterials; Khurshid, Z., Najeeb, S., Zafar, M.S., Sefat, F., Eds.; Woodhead Publishing: Cambridge, UK, 2019; pp. 217–227. [Google Scholar]
- Najeeb, S.; Khurshid, Z.; Zafar, M.S.; Khan, A.S.; Zohaib, S.; Marti, J.M.; Sauro, S.; Matinlinna, J.P.; Rehman, I.U. Modifications in Glass Ionomer Cements: Nano-Sized Fillers and Bioactive Nanoceramics. Int. J. Mol. Sci. 2016, 17, 1134. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S.; Khurshid, Z.; Almas, K. Oral tissue engineering progress and challenges. J. Tissue Eng. Regen. Med. 2015, 12, 387–397. [Google Scholar] [CrossRef]
- Baino, F.; Hamzehlou, S.; Kargozar, S. Bioactive Glasses: Where Are We and Where Are We Going? J. Funct. Biomater. 2018, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Kolzow, J.; Chen, R.R.; Du, J. Effect of solution condition on hydroxyapatite formation in evaluating bioactivity of B(2)O(3) containing 45S5 bioactive glasses. Bioact. Mater. 2019, 4, 207–214. [Google Scholar] [CrossRef]
- Zafar, M.S.; Farooq, I.; Awais, M.; Najeeb, S.; Khurshid, Z.; Zohaib, S. Chapter 11—Bioactive Surface Coatings for Enhancing Osseointegration of Dental Implants. In Biomedical, Therapeutic and Clinical Applications of Bioactive Glasses; Kaur, G., Ed.; Woodhead Publishing: Cambridge, UK, 2019; pp. 313–329. [Google Scholar]
- Zafar, M.S.; Alnazzawi, A.A.; Alrahabi, M.; Fareed, M.A.; Najeeb, S.; Khurshid, Z. 18—Nanotechnology and nanomaterials in dentistry. In Advanced Dental Biomaterials; Khurshid, Z., Najeeb, S., Zafar, M.S., Sefat, F., Eds.; Woodhead Publishing: Cambridge, UK, 2019; pp. 477–505. [Google Scholar]
- Jones, J.R.; Brauer, D.S.; Hupa, L.; Greenspan, D.C. Bioglass and bioactive glasses and their impact on healthcare. Int. J. Appl. Glass Sci. 2016, 7, 423–434. [Google Scholar] [CrossRef]
- Hench, L.; Hench, J.W.; Greenspan, D. Bioglass: A short history and bibliography. J. Aust. Ceram Soc. 2004, 40, 1–42. [Google Scholar]
- El-Meliegy, E.; Noort, R. Glasses and Glass Ceramics for Medical Applications; Springer: New York, NY, USA, 2012. [Google Scholar]
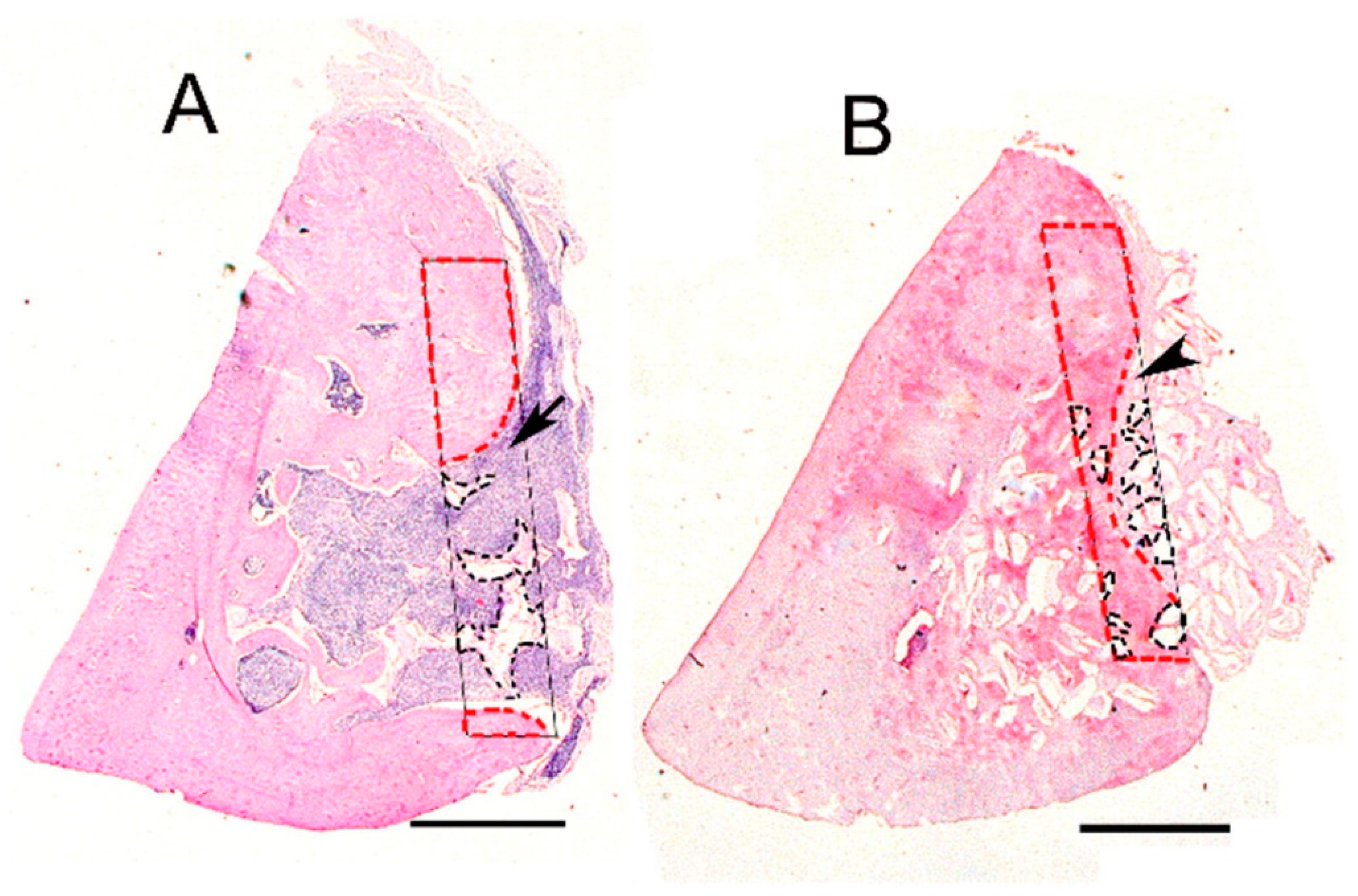
- Ferreira, M.M.; Brito, A.F.; Brazete, D.; Pereira, I.C.; Carrilho, E.; Abrantes, A.M.; Pires, A.S.; Aguiar, M.J.; Carvalho, L.; Botelho, M.F.; et al. Doping β-TCP as a Strategy for Enhancing the Regenerative Potential of Composite β-TCP-Alkali-Free Bioactive Glass Bone Grafts. Experimental Study in Rats. Materials 2018, 12, 4. [Google Scholar] [CrossRef]
- Lowe, B.; Ottensmeyer, M.P.; Xu, C.; He, Y.; Ye, Q.; Troulis, M.J. The Regenerative Applicability of Bioactive Glass and Beta-Tricalcium Phosphate in Bone Tissue Engineering: A Transformation Perspective. J. Funct. Biomater. 2019, 10, 16. [Google Scholar] [CrossRef]
- Rodriguez, O.; Alhalawani, A.; Arshad, S.; Towler, M.R. Rapidly-Dissolving Silver-Containing Bioactive Glasses for Cariostatic Applications. J. Funct. Biomater. 2018, 9, 28. [Google Scholar] [CrossRef]
- Chen, X.; Chen, X.; Brauer, D.S.; Wilson, R.M.; Law, R.V.; Hill, R.G.; Karpukhina, N. Sodium Is Not Essential for High Bioactivity of Glasses. Int. J. Appl. Glass Sci. 2017, 8, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.G.; Brauer, D.S. Predicting the bioactivity of glasses using the network connectivity or split network models. J. Non-Cryst. Solids 2011, 357, 3884–3887. [Google Scholar] [CrossRef]
- Jones, J.; Gentleman, E.; Polak, J. Bioactive Glass Scaffolds for Bone Regeneration. Elements 2007, 3, 393–399. [Google Scholar] [CrossRef]
- Hoppe, A.; Jokic, B.; Janackovic, D.; Fey, T.; Greil, P.; Romeis, S.; Schmidt, J.; Peukert, W.; Lao, J.; Jallot, E.; et al. Cobalt-releasing 1393 bioactive glass-derived scaffolds for bone tissue engineering applications. ACS Appl. Mater. Interfaces 2014, 6, 2865–2877. [Google Scholar] [CrossRef]
- Rokaya, D.; Srimaneepong, V.; Sapkota, J.; Qin, J.; Siraleartmukul, K.; Siriwongrungson, V. Polymeric materials and films in dentistry: An overview. J. Adv. Res. 2018, 14, 25–34. [Google Scholar] [CrossRef]
- Luo, S.H.; Xiao, W.; Wei, X.J.; Jia, W.T.; Zhang, C.Q.; Huang, W.H.; Jin, D.X.; Rahaman, M.N.; Day, D.E. In vitro evaluation of cytotoxicity of silver-containing borate bioactive glass. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 95, 441–448. [Google Scholar] [CrossRef]
- Kapoor, S.; Goel, A.; Tilocca, A.; Dhuna, V.; Bhatia, G.; Dhuna, K.; Ferreira, J.M. Role of glass structure in defining the chemical dissolution behavior, bioactivity and antioxidant properties of zinc and strontium co-doped alkali-free phosphosilicate glasses. Acta Biomater. 2014, 10, 3264–3278. [Google Scholar] [CrossRef]
- Thuy, T.T.; Nakagaki, H.; Kato, K.; Hung, P.A.; Inukai, J.; Tsuboi, S.; Nakagaki, H.; Hirose, M.N.; Igarashi, S.; Robinson, C. Effect of strontium in combination with fluoride on enamel remineralization in vitro. Arch. Oral Biol. 2008, 53, 1017–1022. [Google Scholar] [CrossRef]
- Groh, D.; Döhler, F.; Brauer, D.S. Bioactive glasses with improved processing. Part 1. Thermal properties, ion release and apatite formation. Acta Biomater. 2014, 10, 4465–4473. [Google Scholar] [CrossRef]
- Chen, Q.Z.; Xu, J.L.; Yu, L.G.; Fang, X.Y.; Khor, K.A. Spark plasma sintering of sol–gel derived 45S5 Bioglass®-ceramics: Mechanical properties and biocompatibility evaluation. Mater. Sci. Eng. C 2012, 32, 494–502. [Google Scholar] [CrossRef]
- Filho, O.P.; La Torre, G.P.; Hench, L.L. Effect of crystallization on apatite-layer formation of bioactive glass 45S5. J. Biomed. Mater. Res. 1996, 30, 509–514. [Google Scholar] [CrossRef]
- Prasad, S.; Vyas, V.K.; Ershad, M.; Pyare, R. Crystallization and mechanical properties of (45S5-HA) biocomposite for biomedical implantation. Ceram. Silik 2017, 61, 378–384. [Google Scholar] [CrossRef]
- Wilson, J.; Pigott, G.; Schoen, F.; Hench, L. Toxicology and biocompatibility of bioglasses. J. Biomed. Mater. Res. 1981, 15, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Midha, S.; Kim, T.B.; van den Bergh, W.; Lee, P.D.; Jones, J.R.; Mitchell, C.A. Preconditioned 70S30C bioactive glass foams promote osteogenesis in vivo. Acta Biomater. 2013, 9, 9169–9182. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Fan, W.; Gelinsky, M.; Xiao, Y.; Simon, P.; Schulze, R.; Doert, T.; Luo, Y.; Cuniberti, G. Bioactive SrO-SiO2 glass with well-ordered mesopores: Characterization, physiochemistry and biological properties. Acta Biomater. 2011, 7, 1797–1806. [Google Scholar] [CrossRef] [PubMed]
- Palmer, L.C.; Newcomb, C.J.; Kaltz, S.R.; Spoerke, E.D.; Stupp, S.I. Biomimetic systems for hydroxyapatite mineralization inspired by bone and enamel. Chem. Rev. 2008, 108, 4754–4783. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10, S96–S101. [Google Scholar]
- Vichery, C.; Nedelec, J.M. Bioactive Glass Nanoparticles: From Synthesis to Materials Design for Biomedical Applications. Materials 2016, 9, 288. [Google Scholar] [CrossRef]
- Sepulveda, P.; Jones, J.; Hench, L. In vitro dissolution of melt-derived 45S5 and sol-gel derived 58S bioactive glasses. J. Biomed. Mater. Res. 2002, 61, 301–311. [Google Scholar] [CrossRef]
- Vogel, M.; Voigt, C.; Gross, U.M.; Müller-Mai, C.M. In vivo comparison of bioactive glass particles in rabbits. Biomaterials 2001, 22, 357–362. [Google Scholar] [CrossRef]
- Damen, J.J.; Ten Cate, J.M. Silica-induced precipitation of calcium phosphate in the presence of inhibitors of hydroxyapatite formation. J. Dent. Res. 1992, 71, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Salonen, J.I.; Arjasmaa, M.; Tuominen, U.; Behbehani, M.J.; Zaatar, E. Bioactive glass in dentistry. J. Minim. Interv. Dent. 2009, 2, 208–2018. [Google Scholar]
- Ali, S.; Farooq, I.; Iqbal, K. A review of the effect of various ions on the properties and the clinical applications of novel bioactive glasses in medicine and dentistry. Saudi Dent. J. 2014, 26, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.Z.; Thompson, I.D.; Boccaccini, A.R. 45S5 Bioglass-derived glass-ceramic scaffolds for bone tissue engineering. Biomaterials 2006, 27, 2414–2425. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Baino, F.; Spriano, S.; Pugno, N.M.; Vitale-Brovarone, C. Modelling of the strength–porosity relationship in glass-ceramic foam scaffolds for bone repair. J. Eur. Ceram. Soc. 2014, 34, 2663–2673. [Google Scholar] [CrossRef]
- Zachariasen, W.H. The atomic arrangement in glass. J. Am. Chem. Soc. 1932, 54, 3841–3851. [Google Scholar] [CrossRef]
- Hench, L.L. The story of Bioglass®. J. Mater. Sci. Mater. Med. 2006, 17, 967–978. [Google Scholar] [CrossRef]
- Fu, Q.; Rahaman, M.N.; Fu, H.; Liu, X. Silicate, borosilicate, and borate bioactive glass scaffolds with controllable degradation rate for bone tissue engineering applications. I. Preparation and in vitro degradation. J. Biomed. Mater. Res. 2010, 95, 164–171. [Google Scholar] [CrossRef]
- Gosain, A.K.; Committee, P.S.E.F.D. Bioactive glass for bone replacement in craniomaxillofacial reconstruction. Plast. Reconstr. Surg. 2004, 114, 590–593. [Google Scholar] [CrossRef]
- Ducheyne, P.; Qiu, Q. Bioactive ceramics: The effect of surface reactivity on bone formation and bone cell function. Biomaterials 1999, 20, 2287–2303. [Google Scholar] [CrossRef]
- Amornvit, P.; Bajracharya, S.; Rokaya, D.; Keawcharoen, K.; Supavanich, W. Management of Obstructive Sleep Apnea with Implant Retained Mandibular Advancement Device. World J. Dent. 2014, 5, 184–189. [Google Scholar] [CrossRef]
- Derks, J.; Tomasi, C. Peri-implant health and disease. A systematic review of current epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171. [Google Scholar] [CrossRef]
- Bozic, K.J.; Kurtz, S.M.; Lau, E.; Ong, K.; Chiu, V.; Vail, T.P.; Rubash, H.E.; Berry, D.J. The epidemiology of revision total knee arthroplasty in the United States. Clin. Orthop. Relat. Res. 2010, 468, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Brady, R.A.; Leid, J.G.; Calhoun, J.H.; Costerton, J.W.; Shirtliff, M.E. Osteomyelitis and the role of biofilms in chronic infection. FEMS Immunol. Med. Microbiol. 2008, 52, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Healy, B.; Freedman, A. ABC of wound healing: Infections. BMJ 2006, 332, 838. [Google Scholar] [CrossRef] [PubMed]
- Matos, A.C.; Gonçalves, L.M.; Rijo, P.; Vaz, M.A.; Almeida, A.J.; Bettencourt, A.F. A novel modified acrylic bone cement matrix. A step forward on antibiotic delivery against multiresistant bacteria responsible for prosthetic joint infections. Mater. Sci. Eng. C 2014, 38, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, N.R.; Mechlenburg, I.; Soballe, K.; Lange, J. Patient-reported quality of life and hip function after 2-stage revision of chronic periprosthetic hip joint infection: A cross-sectional study. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2018, 28, 407–414. [Google Scholar] [CrossRef]
- Drago, L.; Vecchi, E.D.; Bortolin, M.; Toscano, M.; Mattina, R.; Romanò, C.L. Antimicrobial activity and resistance selection of different bioglass S53P4 formulations against multidrug resistant strains. Future Microbiol. 2015, 10, 1293–1299. [Google Scholar] [CrossRef]
- Bortolin, M.; De Vecchi, E.; Romanò, C.L.; Toscano, M.; Mattina, R.; Drago, L. Antibiofilm agents against MDR bacterial strains: Is bioactive glass BAG-S53P4 also effective? J. Antimicrob. Chemother. 2015, 71, 123–127. [Google Scholar] [CrossRef]
- Coraca-Huber, D.C.; Fille, M.; Hausdorfer, J.; Putzer, D.; Nogler, M. Efficacy of antibacterial bioactive glass S53P4 against S. aureus biofilms grown on titanium discs in vitro. J. Orthop. Res. 2014, 32, 175–177. [Google Scholar] [CrossRef]
- Galarraga-Vinueza, M.; Mesquita-Guimarães, J.; Magini, R.; Souza, J.; Fredel, M.; Boccaccini, A. Anti-biofilm properties of bioactive glasses embedding organic active compounds. J. Biomed. Mater. Res. 2017, 105, 672–679. [Google Scholar] [CrossRef] [PubMed]
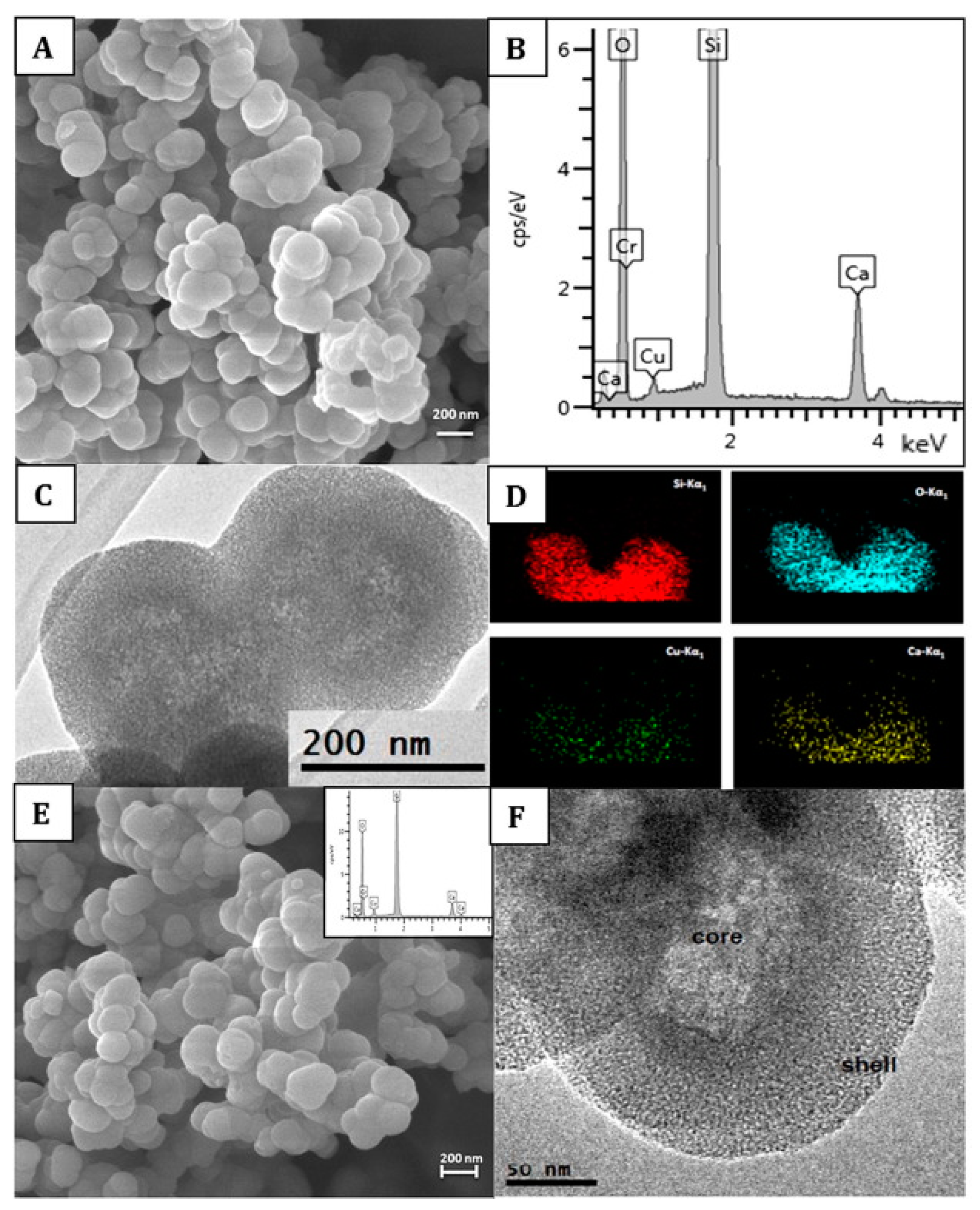
- Bari, A.; Bloise, N.; Fiorilli, S.; Novajra, G.; Vallet-Regí, M.; Bruni, G.; Torres-Pardo, A.; González-Calbet, J.M.; Visai, L.; Vitale-Brovarone, C. Copper-containing mesoporous bioactive glass nanoparticles as multifunctional agent for bone regeneration. Acta Biomater. 2017, 55, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.T.; Wu, Q.; Chen, Y.M.; Smales, R.J.; Shi, S.Y.; Wang, M.T. Antimicrobial effects of a bioactive glass combined with fluoride or triclosan on Streptococcus mutans biofilm. Arch. Oral Biol. 2015, 60, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Lindfors, N.; Hyvönen, P.; Nyyssönen, M.; Kirjavainen, M.; Kankare, J.; Gullichsen, E.; Salo, J. Bioactive glass S53P4 as bone graft substitute in treatment of osteomyelitis. Bone 2010, 47, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Begum, S.; Johnson, W.E.; Worthington, T.; Martin, R.A. The influence of pH and fluid dynamics on the antibacterial efficacy of 45S5 Bioglass. Biomed. Mater. 2016, 11, 015006. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Narhi, T.O.; Hupa, L. Fiber glass-bioactive glass composite for bone replacing and bone anchoring implants. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2015, 31, 371–381. [Google Scholar] [CrossRef]
- Waltimo, T.; Brunner, T.J.; Vollenweider, M.; Stark, W.J.; Zehnder, M. Antimicrobial effect of nanometric bioactive glass 45S5. J. Dent. Res. 2007, 86, 754–757. [Google Scholar] [CrossRef]
- Drago, L.; Vassena, C.; Fenu, S.; Vecchi, E.D.; Signori, V.; Francesco, R.D.; Romanò, C.L. In vitro antibiofilm activity of bioactive glass S53P4. Future Microbiol. 2014, 9, 593–601. [Google Scholar] [CrossRef]
- Rahaman, M.N.; Bal, B.S.; Huang, W. Review: Emerging developments in the use of bioactive glasses for treating infected prosthetic joints. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 41, 224–231. [Google Scholar] [CrossRef]
- Vallittu, P.K. Bioactive glass-containing cranial implants: An overview. J. Mater. Sci. 2017, 52, 8772–8784. [Google Scholar] [CrossRef]
- Stoor, P.; Soderling, E.; Salonen, J.I. Antibacterial effects of a bioactive glass paste on oral microorganisms. Acta Odontol. Scand. 1998, 56, 161–165. [Google Scholar] [CrossRef] [PubMed]
- López-Píriz, R.; Solá-Linares, E.; Rodriguez-Portugal, M.; Malpica, B.; Díaz-Güemes, I.; Enciso, S.; Esteban-Tejeda, L.; Cabal, B.; Granizo, J.J.; Moya, J.S. Evaluation in a dog model of three antimicrobial glassy coatings: Prevention of bone loss around implants and microbial assessments. PLoS ONE 2015, 10, e0140374. [Google Scholar] [CrossRef] [PubMed]
- Abushahba, F.; Söderling, E.; Aalto-Setälä, L.; Sangder, J.; Hupa, L.; Närhi, T.O. Antibacterial properties of bioactive glass particle abraded titanium against Streptococcus mutans. Biomed. Phys. Eng. Express 2018, 4, 045002. [Google Scholar] [CrossRef]
- Bonfim, R.; Chitarra, V.; Gomes, R.; Zacarias, R.; Santos, V.; Vasconcelos, W. Antimicrobial activity of bioactive glass associated to Brazilian red and green propolis. Planta Med. 2009, 75, PJ194. [Google Scholar] [CrossRef]
- Mistry, S.; Roy, R.; Kundu, B.; Datta, S.; Kumar, M.; Chanda, A.; Kundu, D. Clinical Outcome of Hydroxyapatite Coated, Bioactive Glass Coated, and Machined Ti6Al4V Threaded Dental Implant in Human Jaws: A Short-Term Comparative Study. Implant Dent. 2016, 25, 252–260. [Google Scholar] [CrossRef]
- Schepers, E.; Clercq, M.D.; Ducheyne, P.; Kempeneers, R. Bioactive glass particulate material as a filler for bone lesions. J. Oral Rehabil. 1991, 18, 439–452. [Google Scholar] [CrossRef]
- Lovelace, T.B.; Mellonig, J.T.; Meffert, R.M.; Jones, A.A.; Nummikoski, P.V.; Cochran, D.L. Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J. Periodontol. 1998, 69, 1027–1035. [Google Scholar] [CrossRef]
- Gange, P. The evolution of bonding in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 147, S56–S63. [Google Scholar] [CrossRef]
- Tay, F.R.; Pashley, D.H.; Yiu, C.; Cheong, C.; Hashimoto, M.; Itou, K.; Yoshiyama, M.; King, N.M. Nanoleakage types and potential implications: Evidence from unfilled and filled adhesives with the same resin composition. Am. Dent. J. 2004, 17, 182–190. [Google Scholar]
- Hashimoto, M.; Tay, F.R.; Ohno, H.; Sano, H.; Kaga, M.; Yiu, C.; Kumagai, H.; Kudou, Y.; Kubota, M.; Oguchi, H. SEM and TEM analysis of water degradation of human dentinal collagen. J. Biomed. Mater. Res. B 2003, 66, 287–298. [Google Scholar] [CrossRef]
- Mazzoni, A.; Pashley, D.H.; Nishitani, Y.; Breschi, L.; Mannello, F.; Tjäderhane, L.; Toledano, M.; Pashley, E.L.; Tay, F.R. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials 2006, 27, 4470–4476. [Google Scholar] [CrossRef]
- De Munck, J.; Mine, A.; Van den Steen, P.E.; Van Landuyt, K.L.; Poitevin, A.; Opdenakker, G.; Van Meerbeek, B. Enzymatic degradation of adhesive–dentin interfaces produced by mild self-etch adhesives. Eur. J. Oral Sci. 2010, 118, 494–501. [Google Scholar] [CrossRef]
- Osorio, R.; Yamauti, M.; Osorio, E.; Ruiz-Requena, M.E.; Pashley, D.H.; Tay, F.R.; Toledano, M. Zinc reduces collagen degradation in demineralized human dentin explants. J. Dent. 2011, 39, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Sauro, S.; Osorio, R.; Watson, T.F.; Toledano, M. Therapeutic effects of novel resin bonding systems containing bioactive glasses on mineral-depleted areas within the bonded-dentine interface. J. Mater. Sci. Mater. Med. 2012, 23, 1521–1532. [Google Scholar] [CrossRef] [PubMed]
- Tirapelli, C.; Panzeri, H.; Lara, E.H.; Soares, R.G.; Peitl, O.; Zanotto, E.D. The effect of a novel crystallised bioactive glass-ceramic powder on dentine hypersensitivity: A long-term clinical study. J. Oral Rehabil. 2011, 38, 253–262. [Google Scholar] [CrossRef] [PubMed]
- de Morais, R.C.; Silveira, R.E.; Chinelatti, M.A.; Pires-de-Souza, F.D.C.P. Biosilicate as a dentin pretreatment for total-etch and self-etch adhesives: In vitro study. Int. J. Adhes. Adhes. 2016, 70, 271–276. [Google Scholar] [CrossRef]
- de Morais, R.C.; Silveira, R.E.; Chinelatti, M.; Geraldeli, S.; de Carvalho Panzeri Pires-de-Souza, F. Bond strength of adhesive systems to sound and demineralized dentin treated with bioactive glass ceramic suspension. Clin. Oral Investig. 2018, 22, 1923–1931. [Google Scholar] [CrossRef]
- Carneiro, K.K.; Araujo, T.P.; Carvalho, E.M.; Meier, M.M.; Tanaka, A.; Carvalho, C.N.; Bauer, J. Bioactivity and properties of an adhesive system functionalized with an experimental niobium-based glass. J. Mech. Behav. Biomed. Mater. 2018, 78, 188–195. [Google Scholar] [CrossRef]
- Kim, Y.M.; Kim, D.H.; Song, C.W.; Yoon, S.Y.; Kim, S.Y.; Na, H.S.; Chung, J.; Kim, Y.I.; Kwon, Y.H. Antibacterial and remineralization effects of orthodontic bonding agents containing bioactive glass. Korean J. Orthod. 2018, 48, 163–171. [Google Scholar] [CrossRef]
- Mendes, A.; Restrepo, M.; Bussaneli, D.; Zuanon, A. Use of Casein Amorphous Calcium Phosphate (CPP-ACP) on White-spot Lesions: Randomised Clinical Trial. Oral Health Prev. Dent. 2018, 16, 27–31. [Google Scholar]
- Milly, H.; Festy, F.; Watson, T.F.; Thompson, I.; Banerjee, A. Enamel white spot lesions can remineralise using bio-active glass and polyacrylic acid-modified bio-active glass powders. J. Dent. 2014, 42, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Taha, A.A.; Patel, M.P.; Hill, R.G.; Fleming, P.S. The effect of bioactive glasses on enamel remineralization: A systematic review. J. Dent. 2017, 67, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Gjorgievska, E.; Nicholson, J.W. Prevention of enamel demineralization after tooth bleaching by bioactive glass incorporated into toothpaste. Aust. Dent. J. 2011, 56, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Burwell, A.K.; Litkowski, L.J.; Greenspan, D.C. Calcium sodium phosphosilicate (NovaMin): Remineralization potential. Adv. Dent. Res. 2009, 21, 35–39. [Google Scholar] [CrossRef]
- Burwell, A.; Jennings, D.; Muscle, D.; Greenspan, D.C. NovaMin and dentin hypersensitivity--in vitro evidence of efficacy. J. Clin. Dent. 2010, 21, 66–71. [Google Scholar]
- Philip, N. State of the Art Enamel Remineralization Systems: The Next Frontier in Caries Management. Caries Res. 2019, 53, 284–295. [Google Scholar] [CrossRef]
- Gul, H.; Zahid, S.; Zahid, S.; Kaleem, M.; Khan, A.S.; Shah, A.T. Sol-gel derived fluoride-doped bioactive glass powders: Structural and long-term fluoride release/pH analysis. J. Non-Cryst. Solids 2018, 498, 216–222. [Google Scholar] [CrossRef]
- Brauer, D.S.; Karpukhina, N.; O’Donnell, M.D.; Law, R.V.; Hill, R.G. Fluoride-containing bioactive glasses: Effect of glass design and structure on degradation, pH and apatite formation in simulated body fluid. Acta Biomater. 2010, 6, 3275–3282. [Google Scholar] [CrossRef]
- Farooq, I.; Majeed, A.; Alshwaimi, E.; Almas, K. Efficacy of a novel fluoride containing bioactive glass based dentifrice in remineralizing artificially induced demineralization in human enamel. Fluoride 2018, 52, 447–455. [Google Scholar]
- Brannstrom, M. The hydrodynamics of the dentine. Its possible relationship to dentinal pain. Int. Dent. J. 1972, 22, 219–227. [Google Scholar]
- West, N.; Lussi, A.; Seong, J.; Hellwig, E. Dentin hypersensitivity: Pain mechanisms and aetiology of exposed cervical dentin. Clin. Oral Investig. 2013, 17, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Orchardson, R.; Gillam, D.G. The efficacy of potassium salts as agents for treating dentin hypersensitivity. J. Orofac. Pain 2000, 14, 9–19. [Google Scholar] [PubMed]
- Absi, E.G.; Addy, M.; Adams, D. Dentine hypersensitivity. A study of the patency of dentinal tubules in sensitive and non-sensitive cervical dentine. J. Clin. Periodontol. 1987, 14, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Gillam, D.G.; Bulman, J.S.; Eijkman, M.A.; Newman, H.N. Dentists’ perceptions of dentine hypersensitivity and knowledge of its treatment. J. Oral Rehabil. 2002, 29, 219–225. [Google Scholar] [CrossRef]
- Gillam, D.G. Clinical trial designs for testing of products for dentine hypersensitivity—A review. J. West Soc. Periodontol. Periodontal Abstr. 1997, 45, 37–46. [Google Scholar]
- Pradeep, A.R.; Sharma, A. Comparison of clinical efficacy of a dentifrice containing calcium sodium phosphosilicate to a dentifrice containing potassium nitrate and to a placebo on dentinal hypersensitivity: A randomized clinical trial. J. Periodontol. 2010, 81, 1167–1173. [Google Scholar] [CrossRef]
- Montazerian, M.; Zanotto, E.D. A guided walk through Larry Hench’s monumental discoveries. J. Mater. Sci. 2017, 52, 8695–8732. [Google Scholar] [CrossRef]
- Gillam, D.G.; Tang, J.Y.; Mordan, N.J.; Newman, H.N. The effects of a novel Bioglass dentifrice on dentine sensitivity: A scanning electron microscopy investigation. J. Oral Rehabil. 2002, 29, 305–313. [Google Scholar] [CrossRef]
- Gendreau, L.; Barlow, A.P.; Mason, S.C. Overview of the clinical evidence for the use of NovaMin in providing relief from the pain of dentin hypersensitivity. J. Clin. Dent. 2011, 22, 90–95. [Google Scholar]
- Ashwini, S.; Swatika, K.; Kamala, D. Comparative evaluation of desensitizing efficacy of dentifrice containing 5% fluoro calcium phosphosilicate versus 5% calcium sodium phosphosilicate: A randomized controlled clinical trial. Contemp. Clin. Dent. 2018, 9, 330. [Google Scholar]
- Tirapelli, C.; Panzeri, H.; Soares, R.G.; Peitl, O.; Zanotto, E.D. A novel bioactive glass-ceramic for treating dentin hypersensitivity. Braz. Oral Res. 2010, 24, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Orchardson, R.; Gangarosa Sr, L.P.; Holland, G.R.; Pashley, D.H.; Trowbridge, H.O.; Ashley, F.P.; Kleinberg, I.; Zappa, U. Dentine hypersensitivity-into the 21st century. Arch. Oral Biol. 1994, 39, 113S–119S. [Google Scholar] [CrossRef]
- Banerjee, A.; Hajatdoost-Sani, M.; Farrell, S.; Thompson, I. A clinical evaluation and comparison of bioactive glass and sodium bicarbonate air-polishing powders. Int. J. Dent. 2010, 38, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Taha, A.A.; Hill, R.G.; Fleming, P.S.; Patel, M.P. Development of a novel bioactive glass for air-abrasion to selectively remove orthodontic adhesives. Clin. Oral Investig. 2018, 22, 1839–1849. [Google Scholar] [CrossRef]
- Langalia, A. Polymerization shrinkage of composite resins: A review. J. Med. Dent. Sci. Res. 2015, 2, 23–27. [Google Scholar]
- Pereira-Cenci, T.; Cenci, M.S.; Fedorowicz, Z.; Marchesan, M.A. Antibacterial agents in composite restorations for the prevention of dental caries. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef]
- Esteves, C.; Ota-Tsuzuki, C.; Reis, A.; Rodrigues, J. Antibacterial activity of various self-etching adhesive systems against oral streptococci. Oper. Dent. 2010, 35, 448–453. [Google Scholar] [CrossRef]
- Profeta, A.C. Dentine bonding agents comprising calcium-silicates to support proactive dental care: Origins, development and future. Dent. Mater. J. 2014, 33, 443–452. [Google Scholar] [CrossRef]
- Khvostenko, D.; Mitchell, J.C.; Hilton, T.J.; Ferracane, J.L.; Kruzic, J.J. Mechanical performance of novel bioactive glass containing dental restorative composites. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2013, 29, 1139–1148. [Google Scholar] [CrossRef]
- Salehi, S.; Gwinner, F.; Mitchell, J.C.; Pfeifer, C.; Ferracane, J.L. Cytotoxicity of resin composites containing bioactive glass fillers. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2015, 31, 195–203. [Google Scholar] [CrossRef]
- Chatzistavrou, X.; Velamakanni, S.; DiRenzo, K.; Lefkelidou, A.; Fenno, J.C.; Kasuga, T.; Boccaccini, A.R.; Papagerakis, P. Designing dental composites with bioactive and bactericidal properties. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 52, 267–272. [Google Scholar] [CrossRef]
- Tezvergil-Mutluay, A.; Seseogullari-Dirihan, R.; Feitosa, V.P.; Cama, G.; Brauer, D.S.; Sauro, S. Effects of Composites Containing Bioactive Glasses on Demineralized Dentin. J. Dent. Res. 2017, 96, 999–1005. [Google Scholar] [CrossRef]
- Chatzistavrou, X.; Lefkelidou, A.; Papadopoulou, L.; Pavlidou, E.; Paraskevopoulos, K.M.; Fenno, J.C.; Flannagan, S.; Gonzalez-Cabezas, C.; Kotsanos, N.; Papagerakis, P. Bactericidal and Bioactive Dental Composites. Front. Physiol. 2018, 9, 103. [Google Scholar] [CrossRef]
- Par, M.; Tarle, Z.; Hickel, R.; Ilie, N. Dentin Bond Strength of Experimental Composites Containing Bioactive Glass: Changes During Aging for up to 1 Year. J. Adhes. Dent. 2018, 20, 325–334. [Google Scholar]
- Par, M.; Tarle, Z.; Hickel, R.; Ilie, N. Mechanical properties of experimental composites containing bioactive glass after artificial aging in water and ethanol. Clin. Oral Investig. 2018, 26, 2733–2741. [Google Scholar] [CrossRef]
- Yang, S.Y.; Piao, Y.Z.; Kim, S.M.; Lee, Y.K.; Kim, K.N.; Kim, K.M. Acid neutralizing, mechanical and physical properties of pit and fissure sealants containing melt-derived 45S5 bioactive glass. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2013, 29, 1228–1235. [Google Scholar] [CrossRef]
- Nicolae, L.C.; Shelton, R.M.; Cooper, P.R.; Martin, R.A.; Palin, W.M. The Effect of UDMA/TEGDMA Mixtures and Bioglass Incorporation on the Mechanical and Physical Properties of Resin and Resin-Based Composite Materials. In Conference Papers in Science; Hindawi: London, UK, 2014; Volume 2014, pp. 1–5. [Google Scholar]
- Oral, O.; Lassila, L.V.; Kumbuloglu, O.; Vallittu, P.K. Bioactive glass particulate filler composite: Effect of coupling of fillers and filler loading on some physical properties. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2014, 30, 570–577. [Google Scholar] [CrossRef]
- Yli-Urpo, H.; Vallittu, P.K.; Narhi, T.O.; Forsback, A.P.; Vakiparta, M. Release of silica, calcium, phosphorus, and fluoride from glass ionomer cement containing bioactive glass. J. Biomater. Appl. 2004, 19, 5–20. [Google Scholar] [CrossRef]
- Kandaswamy, D.; Rajan, K.J.; Venkateshbabu, N.; Porkodi, I. Shear bond strength evaluation of resin composite bonded to glass-ionomer cement using self-etching bonding agents with different pH: In vitro study. J. Conserv. Dent. 2012, 15, 27–31. [Google Scholar]
- Matsuya, S.; Matsuya, Y.; Ohta, M. Structure of bioactive glass and its application to glass ionomer cement. Dent. Mater. J. 1999, 18, 155–166. [Google Scholar] [CrossRef]
- Khoroushi, M.; Mousavinasab, S.M.; Keshani, F.; Hashemi, S. Effect of resin-modified glass ionomer containing bioactive glass on the flexural strength and morphology of demineralized dentin. Oper. Dent. 2013, 38, E1–E10. [Google Scholar] [CrossRef] [PubMed]
- Yli-Urpo, H.; Narhi, M.; Narhi, T. Compound changes and tooth mineralization effects of glass ionomer cements containing bioactive glass (S53P4), an in vivo study. Biomaterials 2005, 26, 5934–5941. [Google Scholar] [CrossRef] [PubMed]
- Yli-Urpo, H.; Narhi, T.; Soderling, E. Antimicrobial effects of glass ionomer cements containing bioactive glass (S53P4) on oral micro-organisms in vitro. Acta Odontol. Scand. 2003, 61, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Valanezhad, A.; Odatsu, T.; Udoh, K.; Shiraishi, T.; Sawase, T.; Watanabe, I. Modification of resin modified glass ionomer cement by addition of bioactive glass nanoparticles. J. Mater. Sci. Mater. Med. 2016, 27, 3. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, A.R.; Paul, M.J.; Basappa, N. Comparative Evaluation of the Remineralizing Effects and Surface Micro hardness of Glass Ionomer Cements Containing Bioactive Glass (S53P4): An in vitro Study. Int. J. Clin. Pediatr. Dent. 2010, 3, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; Ma, S.; Chen, J.H.; Xu, H.H. Therapeutic polymers for dental adhesives: Loading resins with bio-active components. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2014, 30, 97–104. [Google Scholar] [CrossRef]
- Hilton, T.J. Keys to clinical success with pulp capping: A review of the literature. Oper. Dent. 2009, 34, 615–625. [Google Scholar] [CrossRef]
- Macwan, C.; Deshpande, A. Mineral trioxide aggregate (MTA) in dentistry: A review of literature. J. Oral Res. Rev. 2014, 6, 71–74. [Google Scholar] [CrossRef]
- Gholami, S.; Labbaf, S.; Baharlou Houreh, A.; Ting, H.K.; Jones, J.; Nasr Esfahani, M.H. Long term effects of bioactive glass particulates on dental pulp stem cells in vitro. Biomed. Glasses 2017, 3, 96–103. [Google Scholar] [CrossRef]
- Long, Y.; Liu, S.; Zhu, L.; Liang, Q.; Chen, X.; Dong, Y. Evaluation of Pulp Response to Novel Bioactive Glass Pulp Capping Materials. J. Endod. 2017, 43, 1647–1650. [Google Scholar] [CrossRef]
- Flores-Ledesma, A.; Barcelo Santana, F.; Bucio, L.; Arenas-Alatorre, J.A.; Faraji, M.; Wintergerst, A.M. Bioactive materials improve some physical properties of a MTA-like cement. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 71, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Tay, F.R.; Pashley, D.H. Monoblocks in root canals: A hypothetical or a tangible goal. J. Endod. 2007, 33, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Mandke, L. Importance of coronal seal: Preventing coronal leakage in endodontics. J. Restor. Dent. 2016, 4, 71–75. [Google Scholar] [CrossRef]
- Elzubair, A.; Elias, C.N.; Suarez, J.C.M.; Lopes, H.P.; Vieira, M.V.B. The physical characterization of a thermoplastic polymer for endodontic obturation. J. Dent. 2006, 34, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Mehrvarzfar, P.; Dahi-Taleghani, A.; Saghiri, M.A.; Karamifar, K.; Shababi, B.; Behnia, A. The comparison of MTA, Geristore® and Amalgam with or without Bioglass as a matrix in sealing the furcal perforations (in vitro study). Saudi Dent. J. 2010, 22, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Belladonna, F.G.; Calasans-Maia, M.D.; Novellino Alves, A.T.; de Brito Resende, R.F.; Souza, E.M.; Silva, E.J.; Fidel, S.R.; De-Deus, G. Biocompatibility of a self-adhesive gutta-percha-based material in subcutaneous tissue of mice. J. Endod. 2014, 40, 1869–1873. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.K.; Fan, B.; Wesselink, P.R. Diminished leakage along root canals filled with gutta-percha without sealer over time: A laboratory study. Int. Endod. J. 2000, 33, 121–125. [Google Scholar] [CrossRef]
- Marending, M.; Bubenhofer, S.B.; Sener, B.; De-Deus, G. Primary assessment of a self-adhesive gutta-percha material. Int. Endod. J. 2013, 46, 317–322. [Google Scholar] [CrossRef]
- Mohn, D.; Bruhin, C.; Luechinger, N.A.; Stark, W.J.; Imfeld, T.; Zehnder, M. Composites made of flame-sprayed bioactive glass 45S5 and polymers: Bioactivity and immediate sealing properties. Int. Endod. J. 2010, 43, 1037–1046. [Google Scholar] [CrossRef]
- Gerhardt, L.-C.; Boccaccini, A.R. Bioactive Glass and Glass-Ceramic Scaffolds for Bone Tissue Engineering. Materials 2010, 3, 3867–3910. [Google Scholar] [CrossRef]
- Brydone, A.; Meek, D.; Maclaine, S. Bone grafting, orthopaedic biomaterials, and the clinical need for bone engineering. Proc. Inst. Mech. Eng. Patr H 2010, 224, 1329–1343. [Google Scholar] [CrossRef] [PubMed]
- Janicki, P.; Schmidmaier, G. What should be the characteristics of the ideal bone graft substitute? Combining scaffolds with growth factors and/or stem cells. Injury 2011, 42, S77–S81. [Google Scholar] [CrossRef]
- Arrington, E.D.; Smith, W.J.; Chambers, H.G.; Bucknell, A.L.; Davino, N.A. Complications of iliac crest bone graft harvesting. Clin. Orthop. Relat. Res. 1996, 329, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Banwart, J.C.; Asher, M.A.; Hassanein, R.S. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 1995, 20, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Kinaci, A.; Neuhaus, V.; Ring, D.C. Trends in bone graft use in the United States. Orthopedics 2014, 37, e783–e788. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, L.; Wasserman, B. A Long-Term Survey of Tooth Loss in 600 Treated Periodontal Patients. J. Periodontol. 1978, 49, 225–237. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.A. Peri-implant diseases: Diagnosis and risk indicators. J. Clin. Periodontol. 2008, 35, 292–304. [Google Scholar] [CrossRef]
- Renvert, S.; Persson, G.R. Periodontitis as a potential risk factor for peri-implantitis. J. Clin. Periodontol. 2009, 36, 9–14. [Google Scholar] [CrossRef]
- Reynolds, M.A.; Aichelmann-Reidy, M.E.; Branch-Mays, G.L.; Gunsolley, J.C. The Efficacy of Bone Replacement Grafts in the Treatment of Periodontal Osseous Defects. A Systematic Review. Ann. Periodontol. 2003, 8, 227–265. [Google Scholar] [CrossRef]
- Singh, M.; Mehta, D. Clinical evaluation of Biogran as a graft material in the treatment of periodontal osseous defects. J. Indian Soc. Periodontol. 2000, 3, 69–72. [Google Scholar]
- Profeta, A.C.; Prucher, G.M. Bioactive-glass in periodontal surgery and implant dentistry. Dent. Mater. J. 2015, 34, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Profeta, A.C.; Huppa, C. Bioactive-glass in Oral and Maxillofacial Surgery. Craniomaxillofacial Trauma Reconstr. 2016, 9, 1–14. [Google Scholar]
- Pantchev, A.; Nohlert, E.; Tegelberg, A. Endodontic surgery with and without inserts of bioactive glass PerioGlas--a clinical and radiographic follow-up. Oral Maxillofac. Surg. 2009, 13, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Stanley, H.R.; Hall, M.B.; Clark, A.E.; King, C.J., 3rd; Hench, L.L.; Berte, J.J. Using 45S5 bioglass cones as endosseous ridge maintenance implants to prevent alveolar ridge resorption: A 5-year evaluation. Int. J. Oral Maxillofac. Implants 1997, 12, 95–105. [Google Scholar] [PubMed]
- Sumer, M.; Keles, G.C.; Cetinkaya, B.O.; Balli, U.; Pamuk, F.; Uckan, S. Autogenous cortical bone and bioactive glass grafting for treatment of intraosseous periodontal defects. Eur. J. Dent. 2013, 7, 6–14. [Google Scholar] [PubMed]
- El-Haddad, S.A.E.M.; Abd-El Razzak, M.Y.; Saudi, H.I.; El Ghorab, N.M. Evaluation of bioactive glass and autogenous bone in the treatment of Grade II furcation involvement: A randomized controlled trial. Eur. J. Dent. 2014, 4, 13. [Google Scholar] [CrossRef]
- Sohrabi, K.; Saraiya, V.; Laage, T.A.; Harris, M.; Blieden, M.; Karimbux, N. An evaluation of bioactive glass in the treatment of periodontal defects: A meta-analysis of randomized controlled clinical trials. J. Periodontol. 2012, 83, 453–464. [Google Scholar] [CrossRef]
- Shue, L.; Yufeng, Z.; Mony, U. Biomaterials for periodontal regeneration: A review of ceramics and polymers. Biomatter 2012, 2, 271–277. [Google Scholar] [CrossRef]
- Nevins, M.L.; Camelo, M.; Nevins, M.; King, C.J.; Oringer, R.J.; Schenk, R.K.; Fiorellini, J.P. Human histologic evaluation of bioactive ceramic in the treatment of periodontal osseous defects. Int. J. Periodontics Restor. Dent. 2000, 20, 458–467. [Google Scholar]
- Sculean, A.; Windisch, P.; Keglevich, T.; Gera, I. Clinical and histologic evaluation of an enamel matrix protein derivative combined with a bioactive glass for the treatment of intrabony periodontal defects in humans. Int. J. Periodontics Restor. Dent. 2005, 25, 139–147. [Google Scholar]
- Müller, F.; Wahl, G.; Fuhr, K. Age-related satisfaction with complete dentures, desire for improvement and attitudes to implant treatment. Gerodontology 1994, 11, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Branemark, P.I.; Hansson, H.A.; Lindstrom, J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Odontol. Scand. 1981, 52, 155–170. [Google Scholar]
- Yeo, I.S.; Kim, H.Y.; Li, Y.; Han, J.S. Implant surface factors and bacterial adhesion: A review of the literature. Int. J. Artif. Organs 2012, 35, 762–772. [Google Scholar] [CrossRef] [PubMed]
- Talreja, P.S.; Gayathri, G.; Mehta, D. Treatment of an early failing implant by guided bone regeneration using resorbable collagen membrane and bioactive glass. J. Indian Soc. Periodontol. 2013, 17, 131. [Google Scholar] [CrossRef]
- Kate, M.; Palaskar, S.; Kapoor, P. Implant failure: A dentist’s nightmare. J. Dent. Implant 2016, 6, 51–56. [Google Scholar] [CrossRef]
- Petersen, R.C. Titanium Implant Osseointegration Problems with Alternate Solutions Using Epoxy/Carbon-Fiber-Reinforced Composite. Metals 2014, 4, 549–569. [Google Scholar] [CrossRef]
- Wennerberg, A.; Bougas, K.; Jimbo, R.; Albrektsson, T. Implant coatings: New modalities for increased osseointegration. Am. Dent. J. 2013, 26, 105–112. [Google Scholar]
- MacDonald, D.; Betts, F.; Doty, S.; Boskey, A. A methodological study for the analysis of apatite-coated dental implants retrieved from humans. Ann. Periodontol. 2000, 5, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Civantos, A.; Martinez-Campos, E.; Ramos, V.; Elvira, C.; Gallardo, A.; Abarrategi, A. Titanium coatings and surface modifications: Toward clinically useful bioactive implants. ACS Biomater. Sci. Eng. 2017, 3, 1245–1261. [Google Scholar] [CrossRef]
- Mistry, S.; Kundu, D.; Datta, S.; Basu, D. Comparison of bioactive glass coated and hydroxyapatite coated titanium dental implants in the human jaw bone. Aust. Dent. J. 2011, 56, 68–75. [Google Scholar] [CrossRef]
- Verné, E. Bioactive Glass and Glass-Ceramic Coatings. In Bio-Glasses: An Introduction; John Wiley & Sons, Ltd.: Chichester, UK, 2012; pp. 107–119. [Google Scholar]
- Lopez-Esteban, S.; Saiz, E.; Fujino, S.; Oku, T.; Suganuma, K.; Tomsia, A.P. Bioactive glass coatings for orthopedic metallic implants. J. Eur. Ceram. Soc. 2003, 23, 2921–2930. [Google Scholar] [CrossRef]
- Gomez-Vega, J.; Saiz, E.; Tomsia, A.; Marshall, G.; Marshall, S. Bioactive glass coatings with hydroxyapatite and Bioglass® particles on Ti-based implants. 1. Processing. Biomaterials 2000, 21, 105–111. [Google Scholar] [CrossRef]
- Fujino, S.; Tokunaga, H.; Saiz, E.; Tomsia, A.P. Fabrication and characterization of bioactive glass coatings on Co-Cr implant alloys. Mater. Trans. 2004, 45, 1147–1151. [Google Scholar] [CrossRef]
- Monsalve, M.; Ageorges, H.; Lopez, E.; Vargas, F.; Bolivar, F. Bioactivity and mechanical properties of plasma-sprayed coatings of bioglass powders. Surf. Coat. Technol. 2013, 220, 60–66. [Google Scholar] [CrossRef]
- Calvo, V.L.; Cabedo, M.V.; Bannier, E.; Recacha, E.C.; Boccaccini, A.R.; Arias, L.C.; Vilches, E.S. 45S5 bioactive glass coatings by atmospheric plasma spraying obtained from feedstocks prepared by different routes. J. Mater. Sci. Mater. Med. 2014, 49, 7933–7942. [Google Scholar] [CrossRef]
- Fu, T.; Alajmi, Z.; Shen, Y.; Wang, L.; Yang, S.; Zhang, M. Sol-gel preparation and properties of Ag-containing bioactive glass films on titanium. Int. J. Appl. Ceram. 2017, 14, 1117–1124. [Google Scholar] [CrossRef]
- Hamadouche, M.; Meunier, A.; Greenspan, D.C.; Blanchat, C.; Zhong, J.P.; La Torre, G.P.; Sedel, L. Bioactivity of sol-gel bioactive glass coated alumina implants. J. Biomed. Mater. Res. 2000, 52, 422–429. [Google Scholar] [CrossRef]
- Xue, B.; Guo, L.; Chen, X.; Fan, Y.; Ren, X.; Li, B.; Ling, Y.; Qiang, Y. Electrophoretic deposition and laser cladding of bioglass coating on Ti. J. Alloys Compd. 2017, 710, 663–669. [Google Scholar] [CrossRef]
- Krause, D.; Thomas, B.; Leinenbach, C.; Eifler, D.; Minay, E.J.; Boccaccini, A.R. The electrophoretic deposition of Bioglass® particles on stainless steel and Nitinol substrates. Surf. Coat. Technol. 2006, 200, 4835–4845. [Google Scholar] [CrossRef]
- Popescu, A.; Sima, F.; Duta, L.; Popescu, C.; Mihailescu, I.; Capitanu, D.; Mustata, R.; Sima, L.; Petrescu, S.; Janackovic, D. Biocompatible and bioactive nanostructured glass coatings synthesized by pulsed laser deposition: In vitro biological tests. Appl. Surf. Sci. 2009, 255, 5486–5490. [Google Scholar] [CrossRef]
- D’alessio, L.; Teghil, R.; Zaccagnino, M.; Zaccardo, I.; Ferro, D.; Marotta, V. Pulsed laser ablation and deposition of bioactive glass as coating material for biomedical applications. Appl. Surf. Sci. 1999, 138, 527–532. [Google Scholar] [CrossRef]
- Wang, C.; Chen, Z.; Wang, M. Fabrication and characterization of bioactive glass coatings produced by the ion beam sputter deposition technique. J. Mater. Sci. Mater. Med. 2002, 13, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Popa, A.; Stan, G.; Husanu, M.; Mercioniu, I.; Santos, L.; Fernandes, H.; Ferreira, J. Bioglass implant-coating interactions in synthetic physiological fluids with varying degrees of biomimicry. Int. J. Nanomed. 2017, 12, 683. [Google Scholar] [CrossRef] [PubMed]
- Mardare, C.; Mardare, A.; Fernandes, J.; Joanni, E.; Pina, S.; Fernandes, M.; Correia, R. Deposition of bioactive glass-ceramic thin-films by RF magnetron sputtering. J. Eur. Ceram. Soc. 2003, 23, 1027–1030. [Google Scholar] [CrossRef]
- Stan, G.; Morosanu, C.; Marcov, D.; Pasuk, I.; Miculescu, F.; Reumont, G. Effect of annealing upon the structure and adhesion properties of sputtered bio-glass/titanium coatings. Appl. Surf. Sci. 2009, 255, 9132–9138. [Google Scholar] [CrossRef]
- Šimek, M.; Černák, M.; Kylián, O.; Foest, R.; Hegemann, D.; Martini, R. White paper on the future of plasma science for optics and glass. Plasma Process. Polym. 2019, 16, 1700250. [Google Scholar] [CrossRef]
- Wasa, K.; Kitabatake, M.; Adachi, H. Thin Film Materials Technology: Sputtering of Control Compound Materials; Springer Science & Business Media: Heidelberg, Germany, 2004. [Google Scholar]
- Moritz, N.; Rossi, S.; Vedel, E.; Tirri, T.; Ylänen, H.; Aro, H.; Närhi, T. Implants coated with bioactive glass by CO 2-laser, an in vivo study. J. Mater. Sci. Mater. Med. 2004, 15, 795–802. [Google Scholar] [CrossRef]
- Wheeler, D.; Montfort, M.; McLoughlin, S. Differential healing response of bone adjacent to porous implants coated with hydroxyapatite and 45S5 bioactive glass. J. Biomed. Mater. Res. 2001, 55, 603–612. [Google Scholar] [CrossRef]
- Popa, A.; Stan, G.; Enculescu, M.; Tanase, C.; Tulyaganov, D.; Ferreira, J. Superior biofunctionality of dental implant fixtures uniformly coated with durable bioglass films by magnetron sputtering. J. Mech. Behav. Biomed. Mater. 2015, 51, 313–327. [Google Scholar] [CrossRef]
- Peltola, M.J.; Aitasalo, K.M.; Suonpaa, J.T.; Yli-Urpo, A.; Laippala, P.J.; Forsback, A.P. Frontal sinus and skull bone defect obliteration with three synthetic bioactive materials. A comparative study. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 66, 364–372. [Google Scholar] [CrossRef]
- Tadjoedin, E.S.; De Lange, G.L.; Lyaruu, D.; Kuiper, L.; Burger, E.H. High concentrations of bioactive glass material (BioGran®) vs. autogenous bone for sinus floor elevation: Histomorphometrical observations on three split mouth clinical cases. Clin. Oral Implants Res. 2002, 13, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Peltola, M.; Aitasalo, K.; Suonpää, J.; Varpula, M.; Yli-Urpo, A. Bioactive glass S53P4 in frontal sinus obliteration: A long-term clinical experience. Head Neck 2006, 28, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Fujikura, K.; Karpukhina, N.; Kasuga, T.; Brauer, D.; Hill, R.; Law, R. Influence of Strontium Substitution on Structure and Crystallisation of Bioglass® 45S5. J. Mater. Chem. 2012, 22, 7395–7402. [Google Scholar] [CrossRef]
- Aitasalo, K.M.; Piitulainen, J.M.; Rekola, J.; Vallittu, P.K. Craniofacial bone reconstruction with bioactive fiber-reinforced composite implant. Head Neck 2014, 36, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Peltola, M.J.; Vallittu, P.K.; Vuorinen, V.; Aho, A.A.; Puntala, A.; Aitasalo, K.M. Novel composite implant in craniofacial bone reconstruction. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Hum, J.; Boccaccini, A.R. Bioactive glasses as carriers for bioactive molecules and therapeutic drugs: A review. J. Mater. Sci. Mater. Med. 2012, 23, 2317–2333. [Google Scholar] [CrossRef] [PubMed]
- Vallet-Regi, M.; Balas, F.; Arcos, D. Mesoporous materials for drug delivery. Angew. Chem. 2007, 46, 7548–7558. [Google Scholar] [CrossRef]
- Nandin, M.; El-Fiqi, A.; Khandmaa, D.; Kim, H.W. Feasibility of Defect Tunable Bone Engineering Using Electroblown Bioactive Fibrous Scaffolds with Dental Stem Cells. ACS Biomater. Sci. Eng. 2018, 4, 1019–1028. [Google Scholar]
- Zhao, S.; Zhu, M.; Zhang, J.; Zhang, Y.; Liu, Z.; Zhu, Y.; Zhang, C. Three dimensionally printed mesoporous bioactive glass and poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) composite scaffolds for bone regeneration. J. Mater. Chem. B 2014, 2, 6106–6118. [Google Scholar] [CrossRef]
- Zhu, M.; Li, K.; Zhu, Y.; Zhang, J.; Ye, X. 3D-printed hierarchical scaffold for localized isoniazid/rifampin drug delivery and osteoarticular tuberculosis therapy. Acta Biomater. 2015, 16, 145–155. [Google Scholar] [CrossRef]
- Wu, C.; Zhou, Y.; Chang, J.; Xiao, Y. Delivery of dimethyloxallyl glycine in mesoporous bioactive glass scaffolds to improve angiogenesis and osteogenesis of human bone marrow stromal cells. Acta Biomater. 2013, 9, 9159–9168. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skallevold, H.E.; Rokaya, D.; Khurshid, Z.; Zafar, M.S. Bioactive Glass Applications in Dentistry. Int. J. Mol. Sci. 2019, 20, 5960. https://doi.org/10.3390/ijms20235960
Skallevold HE, Rokaya D, Khurshid Z, Zafar MS. Bioactive Glass Applications in Dentistry. International Journal of Molecular Sciences. 2019; 20(23):5960. https://doi.org/10.3390/ijms20235960
Chicago/Turabian StyleSkallevold, Hans Erling, Dinesh Rokaya, Zohaib Khurshid, and Muhammad Sohail Zafar. 2019. "Bioactive Glass Applications in Dentistry" International Journal of Molecular Sciences 20, no. 23: 5960. https://doi.org/10.3390/ijms20235960
APA StyleSkallevold, H. E., Rokaya, D., Khurshid, Z., & Zafar, M. S. (2019). Bioactive Glass Applications in Dentistry. International Journal of Molecular Sciences, 20(23), 5960. https://doi.org/10.3390/ijms20235960