Androgen-Regulated microRNAs (AndroMiRs) as Novel Players in Adipogenesis
Abstract
1. Introduction
2. MicroRNAs in Human Mesenchymal Stem Cell Adipogenesis
3. Androgen-Regulated microRNAs (AndroMiRs)
4. AndroMiRs Putatively Involved in Adipogenesis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Heinlein, C.A.; Chang, C. Androgen Receptor (AR) Coregulators: An Overview. Endocr. Rev. 2002, 23, 175–200. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K.; Chang, C. Molecular communication between androgen receptor and general transcription machinery. J. Steroid Biochem. Mol. Biol. 2003, 84, 41–49. [Google Scholar] [CrossRef]
- Knoll, M.; Lodish, H.F.; Sun, L. Long non-coding RNAs as regulators of the endocrine system. Nat. Rev. Endocrinol. 2015, 11, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Ceder, Y. Non-coding RNAs in Prostate Cancer: From Discovery to Clinical Applications. Adv. Exp. Med. Biol. 2016, 886, 155–170. [Google Scholar]
- Chua, F.Y.; Adams, B.D. Androgen receptor and miR-206 regulation in prostate cancer. Transcription 2017, 8, 313–327. [Google Scholar] [CrossRef]
- Pelletier, G. Localization of androgen and estrogen receptors in rat and primate tissues. Histol. Histopathol. 2000, 15, 1261–1270. [Google Scholar]
- McEwan, I.J. Androgen receptor modulators: A marriage of chemistry and biology. Futur. Med. Chem. 2013, 5, 1109–1120. [Google Scholar] [CrossRef]
- Blouin, K.; Boivin, A.; Tchernof, A. Androgens and body fat distribution. J. Steroid Biochem. Mol. Biol. 2008, 108, 272–280. [Google Scholar] [CrossRef]
- Dieudonné, M.N.; Pecquery, R.; Boumediene, A.; Leneveu, M.C.; Giudicelli, Y. Androgen receptors in human preadipocytes and adipocytes: Regional specificities and regulation by sex steroids. Am. J. Physiol. Content 1998, 274, C1645–C1652. [Google Scholar] [CrossRef]
- Singh, R.; Artaza, J.N.; Taylor, W.E.; Gonzalez-Cadavid, N.F.; Bhasin, S. Androgens Stimulate Myogenic Differentiation and Inhibit Adipogenesis in C3H 10T1/2 Pluripotent Cells through an Androgen Receptor-Mediated Pathway. Endocrinology 2003, 144, 5081–5088. [Google Scholar] [CrossRef]
- Singh, R.; Artaza, J.N.; Taylor, W.E.; Braga, M.; Yuan, X.; Gonzalez-Cadavid, N.F.; Bhasin, S. Testosterone inhibits adipogenic differentiation in 3T3-L1 cells: Nuclear translocation of androgen receptor complex with beta-catenin and T-cell factor 4 may bypass canonical Wnt signaling to down-regulate adipogenic transcription factors. Endocrinology 2006, 147, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Bhasin, S.; Guo, W.; Singh, R.; Miki, R.; Chauhan, P.; Choong, K.; Tchkonia, T.; Lebrasseur, N.K.; Flanagan, J.N.; et al. Effects of dihydrotestosterone on differentiation and proliferation of human mesenchymal stem cells and preadipocytes. Mol. Cell. Endocrinol. 2008, 296, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Benvenuti, S.; Cellai, I.; Luciani, P.; Deledda, C.; Saccardi, R.; Mazzanti, B.; Dal Pozzo, S.; Serio, M.; Peri, A. Androgens and estrogens prevent rosiglitazone-induced adipogenesis in human mesenchymal stem cells. J. Endocrinol. Investig. 2012, 35, 365–371. [Google Scholar]
- Blouin, K.; Nadeau, M.; Perreault, M.; Veilleux, A.; Drolet, R.; Marceau, P.; Mailloux, J.; Luu-The, V.; Tchernof, A. Effects of androgens on adipocyte differentiation and adipose tissue explant metabolism in men and women. Clin. Endocrinol. 2010, 72, 176–188. [Google Scholar] [CrossRef]
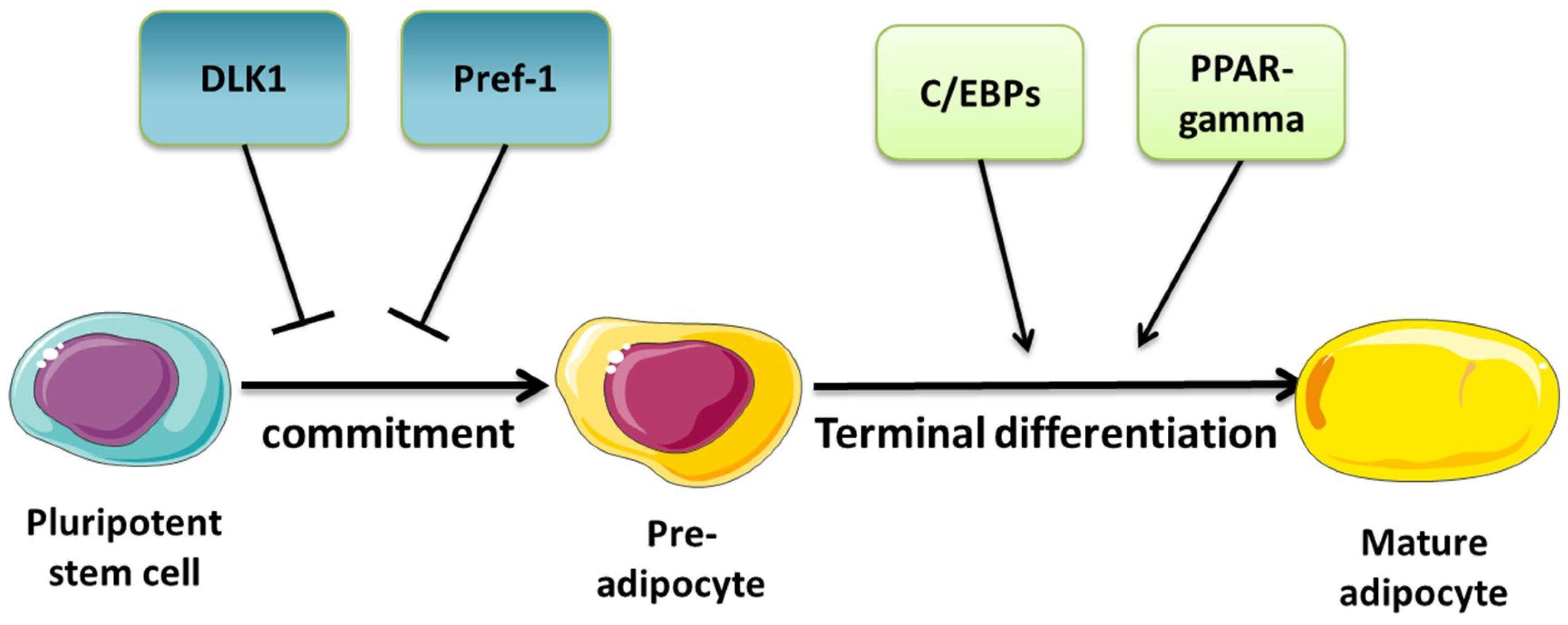
- Lefterova, M.I.; Lazar, M.A. New developments in adipogenesis. Trends Endocrinol. Metab. TEM 2009, 20, 107–114. [Google Scholar] [CrossRef]
- Takada, I.; Kouzmenko, A.P.; Kato, S. Wnt and PPARgamma signaling in osteoblastogenesis and adipogenesis. Nat. Rev. Rheumatol. 2009, 5, 442–447. [Google Scholar] [CrossRef]
- Ross, S.E. Inhibition of Adipogenesis by Wnt Signaling. Science 2000, 289, 950–953. [Google Scholar] [CrossRef]
- Bennett, C.N.; Ross, S.E.; Longo, K.A.; Bajnok, L.; Hemati, N.; Johnson, K.W.; Harrison, S.D.; MacDougald, O. Regulation of Wnt Signaling during Adipogenesis. J. Biol. Chem. 2002, 277, 30998–31004. [Google Scholar] [CrossRef]
- Chen, L.; Hou, J.; Ye, L.; Chen, Y.; Cui, J.; Tian, W.; Li, C.; Liu, L. MicroRNA-143 Regulates Adipogenesis by Modulating the MAP2K5–ERK5 Signaling. Sci. Rep. 2014, 4, 3819. [Google Scholar] [CrossRef]
- Bartel, D.P. MicroRNAs. Cell 2004, 116, 281–297. [Google Scholar] [CrossRef]
- Li, H.; Fan, J.; Fan, L.; Li, T.; Yang, Y.; Xu, H.; Deng, L.; Li, J.; Li, T.; Weng, X.; et al. MiRNA-10b Reciprocally Stimulates Osteogenesis and Inhibits Adipogenesis Partly through the TGF-β/SMAD2 Signaling Pathway. Aging Dis. 2018, 9, 1058–1073. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, T.; Wang, S.; Wei, J.; Fan, J.; Li, J.; Han, Q.; Liao, L.; Shao, C.; Zhao, R.C. miR-17-5p and miR-106a are involved in the balance between osteogenic and adipogenic differentiation of adipose-derived mesenchymal stem cells. Stem Cell Res. 2013, 10, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Mei, Y.; Bian, C.; Li, J.; Du, Z.; Zhou, H.; Yang, Z.; Zhao, R.C. miR-21 modulates the ERK-MAPK signaling pathway by regulating SPRY2 expression during human mesenchymal stem cell differentiation. J. Cell. Biochem. 2013, 114, 1374–1384. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Xu, G.; Ji, C.; Shi, C.; Shen, Y.; Chen, L.; Zhu, L.; Yang, L.; Zhao, Y.; Guo, X. The role of microRNA-26b in human adipocyte differentiation and proliferation. Gene 2014, 533, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Trohatou, O.; Zagoura, D.; Orfanos, N.K.; Pappa, K.I.; Marinos, E.; Anagnou, N.P.; Roubelakis, M.G. miR-26a Mediates Adipogenesis of Amniotic Fluid Mesenchymal Stem/Stromal Cells via PTEN, Cyclin E1, and CDK6. Stem Cells Dev. 2017, 26, 482–494. [Google Scholar] [CrossRef]
- Karbiener, M.; Fischer, C.; Nowitsch, S.; Opriessnig, P.; Papak, C.; Ailhaud, G.; Dani, C.; Amri, E.-Z.; Scheideler, M. microRNA miR-27b impairs human adipocyte differentiation and targets PPARgamma. Biochem. Biophys. Res. Commun. 2009, 390, 247–251. [Google Scholar] [CrossRef]
- Hu, X.; Tang, J.; Hu, X.; Bao, P.; Pan, J.; Chen, Z.; Xian, J. MiR-27b Impairs Adipocyte Differentiation of Human Adipose Tissue-Derived Mesenchymal Stem Cells by Targeting LPL. Cell. Physiol. Biochem. 2018, 47, 545–555. [Google Scholar] [CrossRef]
- Beezhold, K.; Klei, L.R.; Barchowsky, A. Regulation of cyclin D1 by arsenic and microRNA inhibits adipogenesis. Toxicol. letters 2017, 265, 147–155. [Google Scholar] [CrossRef]
- Zhang, X.-M.; Wang, L.-H.; Su, D.-J.; Zhu, D.; Li, Q.-M.; Chi, M.-H. MicroRNA-29b promotes the adipogenic differentiation of human adipose tissue-derived stromal cells. Obesity 2016, 24, 1097–1105. [Google Scholar] [CrossRef]
- Zaragosi, L.-E.; Wdziekonski, B.; Le Brigand, K.; Villageois, P.; Mari, B.; Waldmann, R.; Dani, C.; Barbry, P. Small RNA sequencing reveals miR-642a-3p as a novel adipocyte-specific microRNA and miR-30 as a key regulator of human adipogenesis. Genome Biol. 2011, 12, R64. [Google Scholar] [CrossRef]
- Karbiener, M.; Neuhold, C.; Opriessnig, P.; Prokesch, A.; Bogner-Strauss, J.G.; Scheideler, M. MicroRNA-30c promotes human adipocyte differentiation and co-represses PAI-1 and ALK2. RNA Biol. 2011, 8, 850–860. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, Y.; He, X.; Zhang, S.; Wang, K.; Wu, H.; Chen, L. LncRNA TINCR/miR-31-5p/C/EBP-α feedback loop modulates the adipogenic differentiation process in human adipose tissue-derived mesenchymal stem cells. Stem Cell Res. 2018, 32, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Woeller, C.F.; Flores, E.L.; Pollock, S.J.; Phipps, R.P. Editor’s Highlight: Thy1 (CD90) Expression is Reduced by the Environmental Chemical Tetrabromobisphenol-A to Promote Adipogenesis Through Induction of microRNA-103. Toxicol. Sci. 2017, 157, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Ahonen, M.A.; Haridas, P.N.; Mysore, R.; Wabitsch, M.; Fischer-Posovszky, P.; Olkkonen, V.M. miR-107 inhibits CDK6 expression, differentiation, and lipid storage in human adipocytes. Mol. Cell. Endocrinol. 2019, 479, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Laine, S.K.; Alm, J.J.; Virtanen, S.P.; Aro, H.T.; Laitala-Leinonen, T.K.; Laitala-Leinonen, T.K. MicroRNAs miR-96, miR-124, and miR-199a regulate gene expression in human bone marrow-derived mesenchymal stem cells. J. Cell. Biochem. 2012, 113, 2687–2695. [Google Scholar] [CrossRef]
- Chen, K.; He, H.; Xie, Y.; Zhao, L.; Zhao, S.; Wan, X.; Yang, W.; Mo, Z. miR-125a-3p and miR-483-5p promote adipogenesis via suppressing the RhoA/ROCK1/ERK1/2 pathway in multiple symmetric lipomatosis. Sci. Rep. 2015, 5, 11909. [Google Scholar] [CrossRef]
- Rockstroh, D.; Löffler, D.; Kiess, W.; Landgraf, K.; Körner, A. Regulation of human adipogenesis by miR125b-5p. Adipocyte 2016, 5, 283–297. [Google Scholar] [CrossRef][Green Version]
- Lee, E.K.; Lee, M.J.; Abdelmohsen, K.; Kim, W.; Kim, M.M.; Srikantan, S.; Martindale, J.L.; Hutchison, E.R.; Kim, H.H.; Marasa, B.S.; et al. miR-130 suppresses adipogenesis by inhibiting peroxisome proliferator-activated receptor gamma expression. Mol. Cell. Biol. 2011, 31, 626–638. [Google Scholar] [CrossRef]
- Shin, K.K.; Kim, Y.S.; Kim, J.Y.; Bae, Y.C.; Jung, J.S. miR-137 Controls Proliferation and Differentiation of Human Adipose Tissue Stromal Cells. Cell. Physiol. Biochem. 2014, 33, 758–768. [Google Scholar] [CrossRef]
- Li, Z.; Jin, C.; Chen, S.; Zheng, Y.; Huang, Y.; Jia, L.; Ge, W.; Zhou, Y. Long non-coding RNA MEG3 inhibits adipogenesis and promotes osteogenesis of human adipose-derived mesenchymal stem cells via miR-140-5p. Mol. Cell. Biochem. 2017, 433, 51–60. [Google Scholar] [CrossRef]
- Shi, C.; Zhang, M.; Tong, M.; Yang, L.; Pang, L.; Chen, L.; Xu, G.; Chi, X.; Hong, Q.; Ni, Y.; et al. miR-148a is Associated with Obesity and Modulates Adipocyte Differentiation of Mesenchymal Stem Cells through Wnt Signaling. Sci. Rep. 2015, 5, 9930. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yang, F.; Gao, M.; Gong, R.; Jin, M.; Liu, T.; Sun, Y.; Fu, Y.; Huang, Q.; Zhang, W.; et al. miR-149-3p Regulates the Switch between Adipogenic and Osteogenic Differentiation of BMSCs by Targeting FTO. Mol. Ther.-Nucleic Acids 2019, 17, 590–600. [Google Scholar] [CrossRef] [PubMed]
- Skårn, M.; Namløs, H.M.; Noordhuis, P.; Wang, M.-Y.; Meza-Zepeda, L.A.; Myklebost, O. Adipocyte Differentiation of Human Bone Marrow-Derived Stromal Cells Is Modulated by MicroRNA-155, MicroRNA-221, and MicroRNA-222. Stem Cells Dev. 2012, 21, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Mysore, R.; Zhou, Y.; Sädevirta, S.; Savolainen-Peltonen, H.; Nidhina Haridas, P.A.; Soronen, J.; Leivonen, M.; Sarin, A.-P.; Fischer-Posovszky, P.; Wabitsch, M.; et al. MicroRNA-192* impairs adipocyte triglyceride storage. Biochim. Biophys. Acta 2016, 1861, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Mazzu, Y.Z.; Hu, Y.; Soni, R.K.; Mojica, K.M.; Qin, L.-X.; Agius, P.; Waxman, Z.M.; Mihailovic, A.; Socci, N.D.; Hendrickson, R.C.; et al. miR-193b-Regulated Signaling Networks Serve as Tumor Suppressors in Liposarcoma and Promote Adipogenesis in Adipose-Derived Stem Cells. Cancer Res. 2017, 77, 5728–5740. [Google Scholar] [CrossRef]
- Jeong, B.-C.; Kang, I.-H.; Hwang, Y.-C.; Kim, S.-H.; Koh, J.-T. MicroRNA-194 reciprocally stimulates osteogenesis and inhibits adipogenesis via regulating COUP-TFII expression. Cell Death Dis. 2014, 5, e1532. [Google Scholar] [CrossRef] [PubMed]
- Shuai, Y.; Yang, R.; Mu, R.; Yu, Y.; Rong, L.; Jin, L. MiR-199a-3p mediates the adipogenic differentiation of bone marrow-derived mesenchymal stem cells by regulating KDM6A/WNT signaling. Life Sci. 2019, 220, 84–91. [Google Scholar] [CrossRef]
- He, H.; Chen, K.; Wang, F.; Zhao, L.; Wan, X.; Wang, L.; Mo, Z. miR-204-5p promotes the adipogenic differentiation of human adipose-derived mesenchymal stem cells by modulating DVL3 expression and suppressing Wnt/β-catenin signaling. Int. J. Mol. Med. 2015, 35, 1587–1595. [Google Scholar] [CrossRef]
- Hamam, D.; Ali, D.; Vishnubalaji, R.; Hamam, R.; Al-Nbaheen, M.; Chen, L.; Kassem, M.; Aldahmash, A.; Alajez, N.M. microRNA-320/RUNX2 axis regulates adipocytic differentiation of human mesenchymal (skeletal) stem cells. Cell Death Dis. 2014, 5, e1499. [Google Scholar] [CrossRef]
- Zhu, L.; Chen, L.; Shi, C.-M.; Xu, G.-F.; Xu, L.-L.; Zhu, L.-L.; Guo, X.-R.; Ni, Y.; Cui, Y.; Ji, C. MiR-335, an adipogenesis-related microRNA, is involved in adipose tissue inflammation. Cell Biochem. Biophys. 2014, 68, 283–290. [Google Scholar] [CrossRef]
- Wang, L.; Xu, L.; Xu, M.; Liu, G.; Xing, J.; Sun, C.; Ding, H. Obesity-Associated MiR-342-3p Promotes Adipogenesis of Mesenchymal Stem Cells by Suppressing CtBP2 and Releasing C/EBPα from CtBP2 Binding. Cell. Physiol. Biochem. 2015, 35, 2285–2298. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Cui, J.; Hou, J.; Long, J.; Li, C.; Liu, L. A novel negative regulator of adipogenesis: microRNA-363. Stem Cells 2014, 32, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Bork, S.; Horn, P.; Castoldi, M.; Hellwig, I.; Ho, A.D.; Wagner, W. Adipogenic differentiation of human mesenchymal stromal cells is down-regulated by microRNA-369-5p and up-regulated by microRNA-371. J. Cell. Physiol. 2011, 226, 2226–2234. [Google Scholar] [CrossRef] [PubMed]
- Kraus, M.; Greither, T.; Wenzel, C.; Bräuer-Hartmann, D.; Wabitsch, M.; Behre, H.M. Inhibition of adipogenic differentiation of human SGBS preadipocytes by androgen-regulated microRNA miR-375. Mol. Cell. Endocrinol. 2015, 414, 177–185. [Google Scholar] [CrossRef]
- Li, X.; Yang, Y.; Yan, R.; Xu, X.; Gao, L.; Mei, J.; Liu, J.; Wang, X.; Zhang, J.; Wu, P.; et al. miR-377-3p regulates adipogenic differentiation of human bone marrow mesenchymal stem cells by regulating LIFR. Mol. Cell. Biochem. 2018, 449, 295–303. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, L.; Liu, X.; Hong, T.; Wang, T.; Dong, A.; Li, J.; Xu, X.; Cao, L. miR-431 inhibits adipogenic differentiation of human bone marrow-derived mesenchymal stem cells via targeting insulin receptor substance 2. Stem Cell Res. Ther. 2018, 9, 231. [Google Scholar] [CrossRef]
- Yang, L.; Shi, C.-m.; Chen, L.; Pang, L.-x.; Xu, G.-f.; Gu, N.; Zhu, L.-j.; Guo, X.-r.; Ni, Y.-h.; Ji, C.-b. The biological effects of hsa-miR-1908 in human adipocytes. Mol. Biol. Rep. 2015, 42, 927–935. [Google Scholar] [CrossRef]
- Pang, L.; You, L.; Ji, C.; Shi, C.; Chen, L.; Yang, L.; Huang, F.; Zhou, Y.; Zhang, J.; Chen, X.; et al. miR-1275 inhibits adipogenesis via ELK1 and its expression decreases in obese subjects. J. Mol. Endocrinol. 2016, 57, 33–43. [Google Scholar] [CrossRef]
- Elsafadi, M.; Manikandan, M.; Alajez, N.M.; Hamam, R.; Dawud, R.A.; Aldahmash, A.; Iqbal, Z.; Alfayez, M.; Kassem, M.; Mahmood, A. MicroRNA-4739 regulates osteogenic and adipocytic differentiation of immortalized human bone marrow stromal cells via targeting LRP3. Stem Cell Res. 2017, 20, 94–104. [Google Scholar] [CrossRef]
- Tan, Y.; Gan, M.; Fan, Y.; Li, L.; Zhong, Z.; Li, X.; Bai, L.; Zhao, Y.; Niu, L.; Shang, Y.; et al. miR-10b-5p regulates 3T3-L1 cells differentiation by targeting Apol6. Gene 2019, 687, 39–46. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, A.Y.; Lee, H.W.; Son, Y.H.; Lee, G.Y.; Lee, J.-W.; Lee, Y.S.; Kim, J.B. miR-27a is a negative regulator of adipocyte differentiation via suppressing PPARgamma expression. Biochem. Biophys. Res. Commun. 2010, 392, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Tan, Z.; Du, J.; Shen, L.; Liu, C.; Ma, J.; Bai, L.; Jiang, Y.; Tang, G.; Li, M.; Li, X.; et al. miR-199a-3p affects adipocytes differentiation and fatty acid composition through targeting SCD. Biochem. Biophys. Res. Commun. 2017, 492, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.-B.; Xue, L.; Yang, J.; Ma, A.-H.; Zhao, J.; Xu, M.; Tepper, C.G.; Evans, C.P.; Kung, H.-J.; de Vere White, R.W. An androgen-regulated miRNA suppresses Bak1 expression and induces androgen-independent growth of prostate cancer cells. Proc. Natl. Acad. Sci. USA 2007, 104, 19983–19988. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Bemis, L.; Su, L.-J.; Gao, D.; Flaig, T.W. miR-125b Regulation of Androgen Receptor Signaling Via Modulation of the Receptor Complex Co-Repressor NCOR2. BioRes. Open Access 2012, 1, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Zhang, J.; Zhang, Y.; Wan, X.; Zhang, C.; Huang, X.; Huang, W.; Pu, H.; Pei, C.; Wu, H.; et al. KDM1A triggers androgen-induced miRNA transcription via H3K4me2 demethylation and DNA oxidation. Prostate 2015, 75, 936–946. [Google Scholar] [CrossRef]
- Sun, D.; Layer, R.; Mueller, A.C.; Cichewicz, M.A.; Negishi, M.; Paschal, B.M.; Dutta, A. Regulation of several androgen-induced genes through the repression of the miR-99a/let-7c/miR-125b-2 miRNA cluster in prostate cancer cells. Oncogene 2014, 33, 1448–1457. [Google Scholar] [CrossRef]
- Ahram, M.; Mustafa, E.; Zaza, R.; Abu Hammad, S.; Alhudhud, M.; Bawadi, R.; Zihlif, M. Differential expression and androgen regulation of microRNAs and metalloprotease 13 in breast cancer cells. Cell Biol. Int. 2017, 41, 1345–1355. [Google Scholar] [CrossRef]
- Sen, A.; Prizant, H.; Light, A.; Biswas, A.; Hayes, E.; Lee, H.-J.; Barad, D.; Gleicher, N.; Hammes, S.R. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc. Natl. Acad. Sci. USA 2014, 111, 3008–3013. [Google Scholar] [CrossRef]
- Ribas, J.; Ni, X.; Haffner, M.; Wentzel, E.A.; Salmasi, A.H.; Chowdhury, W.H.; Kudrolli, T.A.; Yegnasubramanian, S.; Luo, J.; Rodriguez, R.; et al. miR-21: An androgen receptor-regulated microRNA that promotes hormone-dependent and hormone-independent prostate cancer growth. Cancer Res. 2009, 69, 7165–7169. [Google Scholar] [CrossRef]
- Ribas, J.; Lupold, S.E. The transcriptional regulation of miR-21, its multiple transcripts, and their implication in prostate cancer. Cell Cycle 2010, 9, 923–929. [Google Scholar] [CrossRef]
- Mishra, S.; Deng, J.J.; Gowda, P.S.; Rao, M.K.; Lin, C.-L.; Chen, C.L.; Huang, T.; Sun, L.-Z. Androgen receptor and microRNA-21 axis downregulates transforming growth factor beta receptor II (TGFBR2) expression in prostate cancer. Oncogene 2014, 33, 4097–4106. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.; Litchfield, L.M.; Ivanova, M.M.; Prough, R.A.; Clark, B.J.; Klinge, C.M. Dehydroepiandrosterone-induces miR-21 transcription in HepG2 cells through estrogen receptor β and androgen receptor. Mol. Cell. Endocrinol. 2014, 392, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Casaburi, I.; Cesario, M.G.; Donà, A.; Rizza, P.; Aquila, S.; Avena, P.; Lanzino, M.; Pellegrino, M.; Vivacqua, A.; Tucci, P.; et al. Androgens downregulate miR-21 expression in breast cancer cells underlining the protective role of androgen receptor. Oncotarget 2016, 7, 12651–12661. [Google Scholar] [CrossRef] [PubMed]
- Cao, P.; Deng, Z.; Wan, M.; Huang, W.; Cramer, S.D.; Xu, J.; Lei, M.; Sui, G. MicroRNA-101 negatively regulates Ezh2 and its expression is modulated by androgen receptor and HIF-1alpha/HIF-1beta. Mol. Cancer 2010, 9, 108. [Google Scholar] [CrossRef]
- Ma, X.; Hayes, E.; Biswas, A.; Seger, C.; Prizant, H.; Hammes, S.R.; Sen, A. Androgens Regulate Ovarian Gene Expression Through Modulation of Ezh2 Expression and Activity. Endocrinology 2017, 158, 2944–2954. [Google Scholar] [CrossRef]
- Li, J.; Xie, M.; Wang, X.; Ouyang, X.; Wan, Y.; Dong, G.; Yang, Z.; Yang, J.; Yue, J. Sex hormones regulate cerebral drug metabolism via brain miRNAs: Down-regulation of brain CYP2D by androgens reduces the analgesic effects of tramadol. Br. J. Pharmacol. 2015, 172, 4639–4654. [Google Scholar] [CrossRef]
- Guo, J.; Huang, X.; Wang, H.; Yang, H. Celastrol Induces Autophagy by Targeting AR/miR-101 in Prostate Cancer Cells. PLoS ONE 2015, 10, 0140745. [Google Scholar] [CrossRef]
- Zheng, C.; Yinghao, S.; Li, J. MiR-221 expression affects invasion potential of human prostate carcinoma cell lines by targeting DVL2. Med. Oncol. 2012, 29, 815–822. [Google Scholar] [CrossRef]
- Gui, B.; Hsieh, C.-L.; Kantoff, P.W.; Kibel, A.S.; Jia, L. Androgen receptor-mediated downregulation of microRNA-221 and -222 in castration-resistant prostate cancer. PLoS ONE 2017, 12, e0184166. [Google Scholar] [CrossRef]
- Sun, T.; Wang, Q.; Balk, S.; Brown, M.; Lee, G.-S.M.; Kantoff, P. The role of microRNA-221 and microRNA-222 in androgen-independent prostate cancer cell lines. Cancer Res. 2009, 69, 3356–3363. [Google Scholar] [CrossRef]
- Sun, T.; Yang, M.; Chen, S.; Balk, S.; Pomerantz, M.; Hsieh, C.-L.; Brown, M.; Lee, G.-S.M.; Kantoff, P.W. The altered expression of MiR-221/-222 and MiR-23b/-27b is associated with the development of human castration resistant prostate cancer. The Prostate 2012, 72, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Wang, X.; He, H.H.; Sweeney, C.J.; Liu, S.X.; Brown, M.; Balk, S.; Lee, G.-S.; Kantoff, P.W. MiR-221 promotes the development of androgen independence in prostate cancer cells via downregulation of HECTD2 and RAB1A. Oncogene 2014, 33, 2790–2800. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Du, S.-Y.; Armenia, J.; Qu, F.; Fan, J.; Wang, X.; Fei, T.; Komura, K.; Liu, S.X.; Lee, G.-S.M.; et al. Expression of lncRNA MIR222HG co-transcribed from the miR-221/222 gene promoter facilitates the development of castration-resistant prostate cancer. Oncogenesis 2018, 7, 30. [Google Scholar] [CrossRef]
- Fletcher, C.E.; Dart, D.A.; Sita-Lumsden, A.; Cheng, H.; Rennie, P.S.; Bevan, C.L. Androgen-regulated processing of the oncomir MiR-27a, which targets Prohibitin in prostate cancer. Hum. Mol. Genet. 2012, 21, 3112–3127. [Google Scholar] [CrossRef] [PubMed]
- Mo, W.; Zhang, J.; Li, X.; Meng, D.; Gao, Y.; Yang, S.; Wan, X.; Zhou, C.; Guo, F.; Huang, Y.; et al. Identification of Novel AR-Targeted MicroRNAs Mediating Androgen Signalling through Critical Pathways to Regulate Cell Viability in Prostate Cancer. PLoS ONE 2013, 8, e56592. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Huang, W.; Yang, S.; Zhang, Y.; Zhang, P.; Kong, Z.; Li, T.; Wu, H.; Jing, F.; Li, Y. Androgen-induced miR-27A acted as a tumor suppressor by targeting MAP2K4 and mediated prostate cancer progression. Int. J. Biochem. Cell Biol. 2016, 79, 249–260. [Google Scholar] [CrossRef]
- B Arroyo, A.; Salloum-Asfar, S.; Pérez-Sánchez, C.; Teruel-Montoya, R.; Navarro, S.; García-Barberá, N.; Luengo-Gil, G.; Roldán, V.; Hansen, J.-B.; López-Pedrera, C.; et al. Regulation of TFPIα expression by miR-27a/b-3p in human endothelial cells under normal conditions and in response to androgens. Sci. Rep. 2017, 7, 43500. [Google Scholar] [CrossRef]
- Wang, M.; Liu, M.; Sun, J.; Jia, L.; Ma, S.; Gao, J.; Xu, Y.; Zhang, H.; Tsang, S.Y.; Li, X. MicroRNA-27a-3p affects estradiol and androgen imbalance by targeting Creb1 in the granulosa cells in mouse polycytic ovary syndrome model. Reprod. Biol. 2017, 17, 295–304. [Google Scholar] [CrossRef]
- Jalava, S.E.; Urbanucci, A.; Latonen, L.; Waltering, K.K.; Sahu, B.; Jänne, O.A.; Seppälä, J.; Lähdesmäki, H.; Tammela, T.L.J.; Visakorpi, T. Androgen-regulated miR-32 targets BTG2 and is overexpressed in castration-resistant prostate cancer. Oncogene 2012, 31, 4460–4471. [Google Scholar] [CrossRef]
- Dang, Q.; Li, L.; Xie, H.; He, D.; Chen, J.; Song, W.; Chang, L.S.; Chang, H.-C.; Yeh, S.; Chang, C. Anti-androgen enzalutamide enhances prostate cancer neuroendocrine (NE) differentiation via altering the infiltrated mast cells → androgen receptor (AR) → miRNA32 signals. Mol. Oncol. 2015, 9, 1241–1251. [Google Scholar] [CrossRef]
- Tang, X.; Tang, X.; Gal, J.; Kyprianou, N.; Zhu, H.; Tang, G. Detection of MicroRNAs in Prostate Cancer Cells by MicroRNA Array. In Advanced Structural Safety Studies; Springer Science and Business Media LLC: Berlin, Germany, 2011; Volume 732, pp. 69–88. [Google Scholar]
- Williams, L.V.; Veliceasa, D.; Vinokour, E.; Volpert, O.V. miR-200b Inhibits Prostate Cancer EMT, Growth and Metastasis. PLoS ONE 2013, 8, e83991. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Nayak, S.; Fernandes, G.; Barai, R.S.; Menon, S.; Chaudhari, U.K.; Kholkute, S.D.; Sachdeva, G. Androgen receptor as a regulator of ZEB2 expression and its implications in epithelial-to-mesenchymal transition in prostate cancer. Endocr. -Relat. Cancer 2014, 21, 473–486. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, Y.-N.; Yin, J.; Barrett, B.; Sheppard-Tillman, H.; Li, D.; Casey, O.M.; Fang, L.; Hynes, P.G.; Ameri, A.H.; Kelly, K. Loss of Androgen-Regulated MicroRNA 1 Activates SRC and Promotes Prostate Cancer Bone Metastasis. Mol. Cell. Biol. 2015, 35, 1940–1951. [Google Scholar] [CrossRef] [PubMed]
- Siu, M.-K.; Suau, F.; Chen, W.-Y.; Tsai, Y.-C.; Tsai, H.-Y.; Yeh, H.-L.; Liu, Y.-N. KLF4 functions as an activator of the androgen receptor through reciprocal feedback. Oncogenesis 2016, 5, e282. [Google Scholar] [CrossRef] [PubMed]
- Siu, M.K.; Chen, W.-Y.; Tsai, H.-Y.; Chen, H.-Y.; Yin, J.J.; Chen, C.-L.; Tsai, Y.-C.; Liu, Y.-N. TCF7 is suppressed by the androgen receptor via microRNA-1-mediated downregulation and is involved in the development of resistance to androgen deprivation in prostate cancer. Prostate Cancer Prostatic Dis. 2017, 20, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.-Y.; Tsai, Y.-C.; Siu, M.K.; Yeh, H.-L.; Chen, C.-L.; Yin, J.J.; Huang, J.; Liu, Y.-N. Inhibition of the androgen receptor induces a novel tumor promoter, ZBTB46, for prostate cancer metastasis. Oncogene 2017, 36, 6213–6224. [Google Scholar] [CrossRef]
- Nguyen, H.C.N.; Xie, W.; Yang, M.; Hsieh, C.-L.; Drouin, S.; Lee, G.-S.M.; Kantoff, P.W. Expression differences of circulating microRNAs in metastatic castration resistant prostate cancer and low-risk, localized prostate cancer. Prostate 2013, 73, 346–354. [Google Scholar] [CrossRef]
- Tiryakioglu, D.; Bilgin, E.; Holdenrieder, S.; Dalay, N.; Gezer, U. miR-141 and miR-375 induction and release are different from PSA mRNA and PCA3 upon androgen stimulation of LNCaP cells. Biomed. Rep. 2013, 1, 802–806. [Google Scholar] [CrossRef]
- Chu, M.; Chang, Y.; Li, P.; Guo, Y.; Zhang, K.; Gao, W. Androgen receptor is negatively correlated with the methylation-mediated transcriptional repression of miR-375 in human prostate cancer cells. Oncol. Rep. 2014, 31, 34–40. [Google Scholar] [CrossRef]
- Lyu, S.; Yu, Q.; Ying, G.; Wang, S.; Wang, Y.; Zhang, J.; Niu, Y. Androgen receptor decreases CMYC and KRAS expression by upregulating let-7a expression in ER-, PR-, AR+ breast cancer. Int. J. Oncol. 2014, 44, 229–237. [Google Scholar] [CrossRef]
- Ramberg, H.; Alshbib, A.; Berge, V.; Svindland, A.; Taskén, K.A. Regulation of PBX3 expression by androgen and Let-7d in prostate cancer. Mol. Cancer 2011, 10, 50. [Google Scholar] [CrossRef] [PubMed]
- Kroiss, A.; Vincent, S.; Decaussin-Petrucci, M.; Meugnier, E.; Viallet, J.; Ruffion, A.; Chalmel, F.; Samarut, J.; Allioli, N. Androgen-regulated microRNA-135a decreases prostate cancer cell migration and invasion through downregulating ROCK1 and ROCK2. Oncogene 2015, 34, 2846–2855. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Pu, H.; Huang, W.; Yang, S.; Zhang, Y.; Kong, Z.; Yang, Z.; Zhao, P.; Li, A.; Li, T.; et al. Androgen-induced miR-135a acts as a tumor suppressor through downregulating RBAK and MMP11, and mediates resistance to androgen deprivation therapy. Oncotarget 2016, 7, 51284–51300. [Google Scholar] [CrossRef] [PubMed]
- Waltering, K.K.; Porkka, K.P.; Jalava, S.E.; Urbanucci, A.; Kohonen, P.J.; Latonen, L.M.; Kallioniemi, O.P.; Jenster, G.; Visakorpi, T. Androgen regulation of micro-RNAs in prostate cancer. Prostate 2011, 71, 604–614. [Google Scholar] [CrossRef]
- Pasqualini, L.; Bu, H.; Puhr, M.; Narisu, N.; Rainer, J.; Schlick, B.; Schäfer, G.; Angelova, M.; Trajanoski, Z.; Börno, S.T.; et al. miR-22 and miR-29a Are Members of the Androgen Receptor Cistrome Modulating LAMC1 and Mcl-1 in Prostate Cancer. Mol. Endocrinol. 2015, 29, 1037–1054. [Google Scholar] [CrossRef]
- Guo, J.; Mei, Y.; Li, K.; Huang, X.; Yang, H. Downregulation of miR-17-92a cluster promotes autophagy induction in response to celastrol treatment in prostate cancer cells. Biochem. Biophys. Res. Commun. 2016, 478, 804–810. [Google Scholar] [CrossRef]
- Chen, P.-J.; Yeh, S.-H.; Liu, W.-H.; Lin, C.-C.; Huang, H.-C.; Chen, C.-L.; Chen, D.-S.; Chen, P.-J. Androgen pathway stimulates MicroRNA-216a transcription to suppress the tumor suppressor in lung cancer-1 gene in early hepatocarcinogenesis. Hepatology 2012, 56, 632–643. [Google Scholar] [CrossRef]
- Miyazaki, T.; Ikeda, K.; Sato, W.; Horie-Inoue, K.; Okamoto, K.; Inoue, S. MicroRNA Library-Based Functional Screening Identified Androgen-Sensitive miR-216a as a Player in Bicalutamide Resistance in Prostate Cancer. J. Clin. Med. 2015, 4, 1853–1865. [Google Scholar] [CrossRef]
- Ma, W.; Hu, S.; Yao, G.; Xie, S.; Ni, M.; Liu, Q.; Gao, X.; Zhang, J.; Huang, X.; Zhang, Y. An androgen receptor-microrna-29a regulatory circuitry in mouse epididymis. J. Biol. Chem. 2013, 288, 29369–29381. [Google Scholar] [CrossRef]
- Takayama, K.-I.; Misawa, A.; Suzuki, T.; Takagi, K.; Hayashizaki, Y.; Fujimura, T.; Homma, Y.; Takahashi, S.; Urano, T.; Inoue, S. TET2 repression by androgen hormone regulates global hydroxymethylation status and prostate cancer progression. Nat. Commun. 2015, 6, 8219. [Google Scholar] [CrossRef]
- Nicholls, P.K.; Harrison, C.A.; Walton, K.L.; McLachlan, R.I.; O’Donnell, L.; Stanton, P.G. Hormonal Regulation of Sertoli Cell Micro-RNAs at Spermiation. Endocrinology 2011, 152, 1670–1683. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.; Liu, Y.; Liu, M.; Wang, Y.; Yan, L.; Wang, H.; Ma, L.; Li, Y.-X.; Zhao, Y.; Wang, Y.-L. Testosterone Represses Estrogen Signaling by Upregulating miR-22: A Mechanism for Imbalanced Steroid Hormone Production in Preeclampsia. Hypertension 2017, 69, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Chu, M.; Chang, Y.; Guo, Y.; Wang, N.; Cui, J.; Gao, W.-Q. Regulation and Methylation of Tumor Suppressor MiR-124 by Androgen Receptor in Prostate Cancer Cells. PLoS ONE 2015, 10, e0116197. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, E.M.; Laursen, K.B.; Whitchurch, J.; McWilliam, A.; Ødum, N.; Persson, J.L.; Heery, D.M.; Gudas, L.J.; Mongan, N.P. MiR137 is an androgen regulated repressor of an extended network of transcriptional coregulators. Oncotarget 2015, 6, 35710–35725. [Google Scholar] [CrossRef]
- Gezer, U.; Tiryakioglu, D.; Bilgin, E.; Dalay, N.; Holdenrieder, S. Androgen Stimulation of PCA3 and miR-141 and Their Release from Prostate Cancer Cells. Cell J. 2015, 16, 488–493. [Google Scholar]
- Chen, Y.; Sun, Y.; Rao, Q.; Xu, H.; Li, L.; Chang, C. Androgen receptor (AR) suppresses miRNA-145 to promote renal cell carcinoma (RCC) progression independent of VHL status. Oncotarget 2015, 6, 31203–31215. [Google Scholar] [CrossRef]
- Murata, T.; Takayama, K.; Katayama, S.; Urano, T.; Horie-Inoue, K.; Ikeda, K.; Takahashi, S.; Kawazu, C.; Hasegawa, A.; Ouchi, Y.; et al. miR-148a is an androgen-responsive microRNA that promotes LNCaP prostate cell growth by repressing its target CAND1 expression. Prostate Cancer Prostatic Dis. 2010, 13, 356–361. [Google Scholar] [CrossRef]
- Yao, J.; Xu, C.; Fang, Z.; Li, Y.; Liu, H.; Wang, Y.; Xu, C.; Sun, Y. Androgen receptor regulated microRNA miR-182-5p promotes prostate cancer progression by targeting the ARRDC3/ITGB4 pathway. Biochem. Biophys. Res. Commun. 2016, 474, 213–219. [Google Scholar] [CrossRef]
- Huang, Q.; Sun, Y.; Ma, X.; Gao, Y.; Li, X.; Niu, Y.; Zhang, X.; Chang, C. Androgen receptor increases hematogenous metastasis yet decreases lymphatic metastasis of renal cell carcinoma. Nat. Commun. 2017, 8, 918. [Google Scholar] [CrossRef]
- Xu, S.; Wang, T.; Song, W.; Jiang, T.; Zhang, F.; Yin, Y.; Jiang, S.-W.; Wu, K.; Yu, Z.; Wang, C.; et al. The inhibitory effects of AR/miR-190a/YB-1 negative feedback loop on prostate cancer and underlying mechanism. Sci. Rep. 2015, 5, 13528. [Google Scholar] [CrossRef]
- Jia, L.; Gui, B.; Zheng, D.; Decker, K.F.; Tinay, I.; Tan, M.; Wang, X.; Kibel, A.S. Androgen receptor-regulated miRNA-193a-3p targets AJUBA to promote prostate cancer cell migration. Prostate 2017, 77, 1000–1011. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Lin, B.; Li, T.; Liu, Y.; Li, Y.; Zhou, X.; Miao, M.; Gu, J.; Pan, H.; Yang, F.; et al. A dual yet opposite growth-regulating function of miR-204 and its target XRN1 in prostate adenocarcinoma cells and neuroendocrine-like prostate cancer cells. Oncotarget 2015, 6, 7686–7700. [Google Scholar] [CrossRef] [PubMed]
- Nakano, K.; Miki, Y.; Hata, S.; Ebata, A.; Takagi, K.; McNamara, K.M.; Sakurai, M.; Masuda, M.; Hirakawa, H.; Ishida, T.; et al. Identification of androgen-responsive microRNAs and androgen-related genes in breast cancer. Anticancer Res. 2013, 33, 4811–4819. [Google Scholar] [PubMed]
- Meng, D.; Yang, S.; Wan, X.; Zhang, Y.; Huang, W.; Zhao, P.; Li, T.; Wang, L.; Huang, Y.; Li, Y. A transcriptional target of androgen receptor, miR-421 regulates proliferation and metabolism of prostate cancer cells. Int. J. Biochem. Cell Biol. 2016, 73, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Panneerdoss, S.; Chang, Y.-F.; Buddavarapu, K.C.; Chen, H.-I.H.; Shetty, G.; Wang, H.; Chen, Y.; Kumar, T.R.; Rao, M.K. Androgen-Responsive MicroRNAs in Mouse Sertoli Cells. PLoS ONE 2012, 7, e41146. [Google Scholar] [CrossRef] [PubMed]
- Panneerdoss, S.; Viswanadhapalli, S.; Abdelfattah, N.; Onyeagucha, B.C.; Timilsina, S.; Mohammad, T.A.; Chen, Y.; Drake, M.; Vuori, K.; Kumar, T.R.; et al. Cross-talk between miR-471-5p and autophagy component proteins regulates LC3-associated phagocytosis (LAP) of apoptotic germ cells. Nat. Commun. 2017, 8, 598. [Google Scholar] [CrossRef]
- Ayub, S.G.; Kaul, D.; Ayub, T. An androgen-regulated miR-2909 modulates TGFβ signalling through AR/miR-2909 axis in prostate cancer. Gene 2017, 631, 1–9. [Google Scholar] [CrossRef]
- Wang, R.-F.; Wang, Z.-F.; Cheng, Q.; Wang, G.-R.; Bai, Z.-M. Androgen receptor suppresses prostate cancer cell invasion via altering the miR-4496/β-catenin signals. Biochem. Biophys. Res. Commun. 2018, 504, 82–88. [Google Scholar] [CrossRef]
- Wang, T.; Li, M.; Guan, J.; Li, P.; Wang, H.; Guo, Y.; Shuai, S.; Li, X. MicroRNAs miR-27a and miR-143 Regulate Porcine Adipocyte Lipid Metabolism. Int. J. Mol. Sci. 2011, 12, 7950–7959. [Google Scholar] [CrossRef]
- Kang, T.; Lu, W.; Xu, W.; Anderson, L.; Bacanamwo, M.; Thompson, W.; Chen, Y.E.; Liu, D. MicroRNA-27 (miR-27) Targets Prohibitin and Impairs Adipocyte Differentiation and Mitochondrial Function in Human Adipose-derived Stem Cells. J. Biol. Chem. 2013, 288, 34394–34402. [Google Scholar] [CrossRef]
- Qadir, A.S.; Woo, K.M.; Ryoo, H.-M.; Baek, J.-H. Insulin suppresses distal-less homeobox 5 expression through the up-regulation of microRNA-124 in 3T3-L1 cells. Exp. Cell Res. 2013, 319, 2125–2134. [Google Scholar] [CrossRef] [PubMed]
- Allan, C.A.; Strauss, B.J.G.; Forbes, E.A.; McLachlan, R.I.; Burger, H.G. Testosterone Therapy Prevents Gain in Visceral Adipose Tissue and Loss of Skeletal Muscle in Nonobese Aging Men. J. Clin. Endocrinol. Metab. 2008, 93, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Behre, H.M.; Tammela, T.L.J.; Arver, S.; Tolrá, J.R.; Bonifacio, V.; Lamche, M.; Kelly, J.; Hiemeyer, F.; Giltay, E.J.; Gooren, L.J. A randomized, double-blind, placebo-controlled trial of testosterone gel on body composition and health-related quality-of-life in men with hypogonadal to low-normal levels of serum testosterone and symptoms of androgen deficiency over 6 months with 12 months open-label follow-up. Aging Male 2012, 15, 198–207. [Google Scholar] [PubMed]

| microRNA | Effect on Adipogenesis | Cell System | Target Gene/ Signaling Pathway | Reference |
|---|---|---|---|---|
| miR-10b | i | hADSC | CEBPα, PPARγ, AP2, | Li et al., 2018 [21] |
| mir-17-5p/106a | p | hADSC | BMP2 | Li et al., 2013 [22] |
| miR-21 | p | hMSC | SPRY2 | Mei et al., 2013 [23] |
| miR-26b | p | hADSC | PTEN | Song et al., 2014 [24]; Trohatou et al., 2017 [25] |
| miR-27b | i | hMSC | PPARγ | Karbiener et al., 2009 [26] |
| miR-27b | i | hADSC | LPL, CEBPα, PPARγ | Hu et al., 2018 [27] |
| miR-29 | i | hMSC | Cyclin D1 | Beezhold et al., 2016 [28] |
| miR-29b | p | hADSC | TNF-α SP-1 | Zhang et al., 2016 [29] |
| miR-30 family | p | hMADS | RUNX2 | Zaragosi et al., 2011 [30] |
| miR-30c | p | hMADS | PAI-1, ALK2 | Karbiener et al., 2011 [31] |
| miR-31 | i | hADSC | CEBPα | Liu et al., 2018 [32] |
| miR-103 | p | hADSC | Thy1 (CD90) | Woeller et al., 2017 [33] |
| miR-107 | i | SGBS | CDK6 | Ahonen et al., 2019 [34] |
| miR-124 | p | hMSC | FABP4, PPARγ, SOX9 | Laine et al., 2012 [35] |
| miR-125a-3p | p | hADSC | RhoA/ROCK1/ERK1/2 | Chen et al., 2015 [36] |
| miR-125b-5p | p/i | SGBS | MMP11 | Rockstroh et al., 2016 [37] |
| miR-130 | i | hMSC | PPARγ | Lee et al., 2011 [38] |
| miR-137 | i | hADSC | CDC42 | Shin et al., 2014 [39] |
| miR-140-5p | i | hMSC | LIFR | Li et al., 2017 [40] |
| miR-148a | p | hMSC | Wnt1 | Shi et al., 2015 [41] |
| miR-149-3p | i | BMSC | FTO | Li et al., 2019 [42] |
| miR-155 | i | hMSC | PPARγ, CEBPα | Skarn et al., 2012 [43] |
| miR-192-3p | i | hADSC | SCD, ALDH3H2 | Mysore et al., 2016 [44] |
| miR-193b | p | hADSC | CRKL, FAK | Mazzu et al., 2017 [45] |
| miR-194 | i | hMSC | COUP-TFII | Jeong et al., 2014 [46] |
| miR-199a-3p | p | BMMSC | KDM6A | Shuai et al., 2019 [47] |
| miR-204-5p | p | hADSC | DVL3 | He et al., 2015 [48] |
| miR-320 fam. | p | hMSC | RUNX2 | Hamam et al., 2014 [49] |
| miR-335 | p | hADSC | MEST | Zhu et al., 2014 [50] |
| miR-342-3p | p | hMSC | CtBP2 | Wang et al., 2015 [51] |
| miR-363 | p | hADSC | E2F3 | Chen et al., 2014 [52] |
| miR-369-5p | i | hMSC | FABP4 | Bork et al., 2011 [53] |
| miR-375 | i | SGBS | ADIPOR2 | Kraus et al., 2015 [54] |
| miR-377-3p | i | hMSC | LIFR | Li et al., 2018 [55] |
| miR-431 | i | BMMSC | IRS2 | Wang et al.,2018 [56] |
| miR-483-5p | p | hADSC | RhoA/ROCK1/ERK1/2 | Chen et al., 2015 [36] |
| miR-1908 | i | hMADS | PPARγ, CEBPα | Yang et al., 2015 [57] |
| miR-1275 | i | hADSC | ELK1 | Pang et al., 2016 [58] |
| miR-4739 | p | hMSC | LRP3 | Elsafadi et al., 2017 [59] |
| microRNA | Androgen Regulation | Tissue | Cell Line | Target Gene/Signaling Pathway | Reference |
|---|---|---|---|---|---|
| let-7a | u | BCA | MCF-7; MDA-MB-231; MDA-MB-453 | KRAS; CMYC | Lyu et al., 2014 [101] |
| let-7c | d | PCA | LNCaP | IGFR1 | Sun et al., 2014 [66] |
| let-7d | u | PCA | LNCaP, C4-2B | PBX3 | Ramberg et al., 2011 [102] |
| miR-1 | u | PCA | LNCaP | SRC | Liu et al., 2015 [94] |
| miR-1 | u | PCA | LNCaP | TCF7 | Siu et al., 2017 [96] |
| miR-1 | u | PCA | LNCaP | ZBTB46 | Chen et al.,2017 [97] |
| miR-17-92 cluster | u | PCA | LNCaP; 22Rv1 | ATG7 | Guo et al., 2016 [107] |
| miR-17-92 cluster | u | PCA | DUCaP; LNCaP | - | Pasqualini et al., 2015 [106] |
| miR-19a | u | PCA | LNCaP | SUZ12; RAB13; SC4MOL; PSAP; ABCA1 | Mo et al., 2013 [85] |
| miR-21 | u | PCA | LNCaP; LAPC-4 | - | Ribas et al., 2009 [69] |
| miR-21 | u | PCA | LNCaP | - | Ribas et al., 2010 [70] |
| miR-21 | u | HCC | HepG2 | PDCD4 | Teng et al., 2014 [72] |
| miR-21 | u | PCA | BPH-1; 22Rv1; PC-3 | TGFBR2 | Mishra et al., 2014 [71] |
| miR-21 | d | BCA | MCF-7 | - | Casaburi et al., 2016 [73] |
| miR-22 | u | placenta | JEG-3 | ESR1 | Shao et al., 2017 [113] |
| miR-22 | u | PCA | DUCaP; LNCaP | LAMC1 | Pasqualini et al., 2015 [106] |
| miR-23b | d | mouse Sertolicells | - | PTEN | Nicholls et al., 2011 [112] |
| miR-27a | u | PCA | LNCaP | PHB | Fletcher et al., 2012 [84] |
| miR-27a | u | PCA | LNCaP | ABCA1; PDS5B | Mo et al., 2013 [85] |
| miR-27a | u | PCA | LNCaP, 22Rv1; Du145; PC3 | MAP2K4 | Wan et al., 2016 [86] |
| miR-27a/b | d | endothelial cell lines | EA.hy926; HUVEC | TFPIα | B Arroyo et al., 2017 [87] |
| miR-29a | u | PCA | DUCaP; LNCaP | Mcl-1 | Pasqualini et al., 2015 [106] |
| miR-29a/b | d | epididymis | PC-1 | AR, IGF1 | Ma et al., 2013 [110] |
| miR-29b | u | PCA | LNCaP; BicR | TET2 | Takayama et al., 2015 [111] |
| miR-30d | d | Sertoli cells | - | - | Nicholls et al., 2011 [112] |
| miR-32 | u | PCA | 22Rv1; LNCaP;RWPE1 | NSE | Dang et al., 2015 [7] |
| miR-32 | u | PCA | LNCaP | BTG2 | Jalava et al., 2012 [89] |
| miR-99a | d | PCA | LNCaP | IGFR1 | Sun et al., 2014 [66] |
| miR-100 | d | BCA | MDA-MB-453 | MMP13 | Ahram et al., 2017 [67] |
| miR-101 | u | PCA | LNCaP | Ezh2 | Cao et al., 2010 [74] |
| miR-101 | u | PCA | LNCaP | - | Guo et al., 2015 [77] |
| miR-101 | u | granulosa cells | primary mouse GCs; KGN | Ezh2 | Ma et al., 2017 [75] |
| miR-101 | u | neuronal cells | SH-SY5Y; U251 | CYP2D6 | Li et al., 2015 [76] |
| miR-124 | u | PCA | PC3; LNCaP | AR | Chu et al., 2015 [114] |
| miR-125b | u | PCA | LNCaP; cds1 | Bak1 | Shi et al., 2007 [63] |
| miR-125b | u | PCA | LNCaP | NCOR2 | Yang et al., 2012 [64] |
| miR-125b | d | PCA | LNCaP | - | Sun et al., 2014 [66] |
| miR-125b | u | PCA | LNCaP | - | Yang et al., 2015 [65] |
| miR-125b | d | BCA | MDA-MB-453 | MMP13 | Ahram et al., 2017 [67] |
| miR-128-2 | u | neuronal cells | SH-SY5Y; U251 | CYP2D6 | Li et al., 2015 [76] |
| miR-133b | u | PCA | LNCaP | CDC2L5; PTPRK; RB1CC1; CPNE3 | Mo et al., 2013 [85] |
| miR-133b | u | PCA | LNCaP | - | Yang et al., 2015 [65] |
| miR-135a | u | PCA | LNCaP; PC-3 | ROCK1, ROCK2 | Kroiss et al., 2015 [84] |
| miR-135a | u | PCA | LNCaP | MMP11, RBAK | Wan et al., 2016 [104] |
| miR-137 | u | PCA | LNCaP | KDM2A, KDM4A; KDM5B; KDM7A; MED1 | Nilsson et al., 2015 [115] |
| miR-141 | u | PCA | LNCaP, VCaP | - | Waltering et al., 2011 [105] |
| miR-141 | u | PCA | LNCaP | - | Tiryakioglu et al., 2013 [99] |
| miR-141 | u | PCA | tissue | - | Nguyen et al., 2013 [98] |
| miR-141 | u | PCA | LNCaP | - | Gezer et al., 2015 [116] |
| miR-145 | d | RCC | ACHN; SCRC-2; SW-839 | HIF2α | Chen et al., 2015 [117] |
| miR-148a | u | PCA | LNCaP | CAND1 | Murata et al., 2011 [118] |
| miR-148a | u | PCA | LNCaP | - | Jalava et al., 2012 [89] |
| miR-182-5p | u | PCA | LNCaP | ARRDC3 | Yao et al., 2016 [119] |
| miR-185-5p | u | RCC | SW839 | VEGF-c; HIF2α | Huang et al., 2017 [120] |
| miR-190a | d | PCA | LNCaP | AR; YB1 | Xu et al., 2015 [121] |
| miR-193a-3p | u | PCA | LNCaP; C4-2B | AJUBA | Jia et al., 2017 [122] |
| miR-200a/b | u | PCA | LNCaP; PC-3; Du145 | ZEB2 | Jacob et al., 2014 [93] |
| miR-200a-c | u | PCA | PC-3-AR | - | Williams et al., 2013 [92] |
| miR-203 | u | PCA | LNCaP; 22Rv1 | SRC | Siu et al., 2016 [95] |
| miR-204 | d | PCA | LNCaP, 22Rv1 | XRN1 | Ding et al., 2015 [123] |
| miR-216a | u | HCC | tissue | TSLC1 | Chen et al., 2012 [108] |
| miR-216a | u | PCA | LNCaP | - | Miyazaki et al., 2015 [109] |
| miR-221/222 | d | PCA | LNCaP; C4-2B | - | Gui et al., 2017 [79] |
| miR-363 | u | BCA | MCF-7 | IQWD1 | Nakano et al., 2013 [124] |
| miR-375 | u | PCA | LNCaP; C4-2; 22Rv1; PC-3; Du145 | - | Chu et al., 2014 [100] |
| miR-375 | d | hMSC | SGBS | ADIPOR2 | Kraus et al., 2015 [54] |
| miR-375 | u | PCA | LNCaP | - | Tiryakioglu et al., 2013 [99] |
| miR-375 | u | PCA | tissue | - | Nguyen et al., 2013 [98] |
| miR-421 | d | PCA | LNCaP; 22Rv1; Du145; PC-3 | NRAS, PRAME, CUL4B, PFKMB2 | Meng et al., 2016 [125] |
| miR-471-5p | u | Sertoli cells | primary cells | LAP | Panneerdoss et al.,2017 [126,127] |
| miR-690 | d | Sertoli cells | - | - | Nicholls et al., 2011 [112] |
| miR-2909 | u | PCA | LNCaP | TGFBR2 | Ayub et al., 2017 [128] |
| miR-4496 | u | PCA | LNCaP | β-Catenin | Wang et al., 2018 [129] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jansen, J.; Greither, T.; Behre, H.M. Androgen-Regulated microRNAs (AndroMiRs) as Novel Players in Adipogenesis. Int. J. Mol. Sci. 2019, 20, 5767. https://doi.org/10.3390/ijms20225767
Jansen J, Greither T, Behre HM. Androgen-Regulated microRNAs (AndroMiRs) as Novel Players in Adipogenesis. International Journal of Molecular Sciences. 2019; 20(22):5767. https://doi.org/10.3390/ijms20225767
Chicago/Turabian StyleJansen, Julia, Thomas Greither, and Hermann M. Behre. 2019. "Androgen-Regulated microRNAs (AndroMiRs) as Novel Players in Adipogenesis" International Journal of Molecular Sciences 20, no. 22: 5767. https://doi.org/10.3390/ijms20225767
APA StyleJansen, J., Greither, T., & Behre, H. M. (2019). Androgen-Regulated microRNAs (AndroMiRs) as Novel Players in Adipogenesis. International Journal of Molecular Sciences, 20(22), 5767. https://doi.org/10.3390/ijms20225767






