Abstract
First seen as a fat-storage tissue, the adipose tissue is considered as a critical player in the endocrine system. Precisely, adipose tissue can produce an array of bioactive factors, including cytokines, lipids, and extracellular vesicles, which target various systemic organ systems to regulate metabolism, homeostasis, and immune response. The global effects of adipokines on metabolic events are well defined, but their impacts on brain function and pathology remain poorly defined. Receptors of adipokines are widely expressed in the brain. Mounting evidence has shown that leptin and adiponectin can cross the blood–brain barrier, while evidence for newly identified adipokines is limited. Significantly, adipocyte secretion is liable to nutritional and metabolic states, where defective circuitry, impaired neuroplasticity, and elevated neuroinflammation are symptomatic. Essentially, neurotrophic and anti-inflammatory properties of adipokines underlie their neuroprotective roles in neurodegenerative diseases. Besides, adipocyte-secreted lipids in the bloodstream can act endocrine on the distant organs. In this article, we have reviewed five adipokines (leptin, adiponectin, chemerin, apelin, visfatin) and two lipokines (palmitoleic acid and lysophosphatidic acid) on their roles involving in eating behavior, neurotrophic and neuroprotective factors in the brain. Understanding and regulating these adipokines can lead to novel therapeutic strategies to counteract metabolic associated eating disorders and neurodegenerative diseases, thus promote brain health.
1. Introduction
Adipose tissues are recognized as highly dynamic endocrine tissues exhibiting extensive physiological functions [1]. Adipose tissue is composed of mature adipocytes as well as the stromal vascular fraction, where adipose-derived stem cells, blood cells, fibroblasts, and nerves reside [2]. White and brown adipose tissues are the two fat tissues in mammals. The adipocytes in white and brown adipose tissues are morphologically and functionally distinct. Brown adipose tissues are accountable for thermogenesis by their abundant mitochondria and extensive vascularization [3,4], whereas white adipose tissues are preferably responsible for energy storage in the form of triglycerides. During fasting conditions, insulin inhibits lipolysis in white adipose tissues, where triglycerides are hydrolyzed into fatty acids and glycerol to generate energy [5]. In response to the nutritional states, adipose tissue plays an endocrine role by synthesizing and secreting bioactive compounds termed adipokines. Adipokine secretion is essential to energy and metabolic homeostasis [6]. Adipsin and leptin are the first adipokines identified [7,8]. Since then, many pivotal adipokines, such as adiponectin, resistin, and tumor necrosis factor α (TNF-α), have been extensively studied in metabolism and metabolic syndromes [9]. Novel adipokines, including chemerin, omentin, apelin, and adipocyte fatty acid-binding protein, have been identified by their metabolic functions resembling former adipokines and their alterations afflicted by metabolic diseases in humans [10].
The adipose-brain axis was first established with the discovery of leptin as an endocrine hormone targeting the hypothalamus to regulate energy balance, satiety, metabolism, and body weight [11]. It was later demonstrated that leptin signaling is also involved in hippocampal neuroplasticity [12]. De la Monte et al. have suggested that energy metabolism, glucose utilization, and insulin sensitization are compromised in Alzheimer’s disease (AD) patients, whereas these pathological symptoms may contribute to AD neuropathology [13,14,15,16]. Since AD neuropathology highly resembles the pathology of diabetes mellitus, AD is now recognized as the ‘type 3 diabetes’. Adiponectin promotes insulin sensitivity [17], whereas adiponectin deficiency exacerbates insulin resistance [18] and AD neuropathology [19]. Concerns are raised regarding how metabolic syndromes are linked to neurodegenerative diseases and mood disorders [20,21]. Given that adipose tissue is a major organ to regulate metabolism through adipokines, understanding the central function of adipokines in the brain can illustrate how the adipose-brain crosstalk works to prevent metabolic diseases and to promote brain health.
Metabolic dysfunction could share common molecular mechanisms with neurodegenerative diseases [22]. Therefore, emerging studies aim at investigating how adipose tissue exerts neuroprotective effects and influences neuroplasticity through secreting adipokines. Notably, several adipokines can cross the blood–brain barrier and act on the brain directly [1], while a damaged barrier will hinder adipose-secreting compounds entering the brain [23]. At present, it is noticeable that adipokines can modulate neuroplasticity. Accumulated studies have shown that leptin and adiponectin pathways can regulate cell proliferation [24,25], survival [19,26,27], and synaptic plasticity [12,28] by modulating cellular metabolism [29,30] and suppressing inflammatory response [31,32,33] in the brain. Previous studies focus on the acute action of leptin on synaptic plasticity, whereas recent studies report insulin resistance afflicts circulating leptin levels and affects central neuroplasticity and cognitive functions. Besides, animal studies have demonstrated a possible link between metabolic disorders with aberrant circulating adipokine levels and cognitive behavioral deficits [34,35,36,37,38] or neuropathology [39,40,41].
This review summarizes the emerging evidence on the roles of five adipokines, including leptin, adiponectin, chemerin, apelin, and visfatin, on promoting neuroplasticity. Furthermore, this review will discuss how diet-, obesity-, and diabetes-related conditions alter the adipokine levels and impair neuroplasticity and cognitive function in terms of mood as well as learning and memory.
2. Effects of Conventional and Novel Adipokines on the Brain
The neuroendocrine roles of leptin and adiponectin have been widely studied. Leptin and adiponectin receptors are widely expressed across many brain regions, in particular, the hippocampus, a critical region for spatial learning and memory formation, and emotional regulation [42]. Both leptin and adiponectin are shown to affect synaptic plasticity in the hippocampus. However, the neuroprotective effects of other adipokines, including chemerin, apelin, and visfatin, are mostly unknown.
2.1. Leptin
Leptin is mostly secreted by white adipose tissue to regulate energy homeostasis by suppressing food intake and thereby reducing weight loss [43]. Circulating leptin levels are positively correlated with adiposity [44] and caloric intake [45,46,47,48,49]. In the obese population, increased adiposity is the primary cause of hyperleptinemia, a condition with high circulating leptin levels [44]. Obese subjects are refractory to the anorexigenic effect of leptin due to leptin resistance in the brain and peripheral tissues [50]. Similarly, patients with type 2 diabetes mellitus comorbid with obesity show both insulin-resistance and hyperleptinemia [51]. Multiple studies have demonstrated the effectiveness of exogenous leptin administration on improving insulin resistance in different obese and diabetic rodent models. Mouse models that feature obesity, hyperglycemia, hyperinsulinemia, particularly db/db (leptin-deficient) mice, and Zucker fa/fa (loss-of-function leptin receptor) rats resemble type 2 diabetic conditions in humans. Infusion of recombinant leptin for seven days is sufficient to ameliorate hyperglycemia and hyperinsulinemia in leptin-deficient ob/ob mice [52]. Leptin treatment can also improve insulin resistance, and glucose and lipid imbalances in some type 2 diabetic models [53,54,55,56]. However, mice receiving chronic (>20 weeks) high-fat diet are resistant to leptin even when leptin is directly infused into the cerebral ventricle of the brain [57,58,59,60]. Prominently, leptin also fails to improve diabetes and insulin resistance in type 2 diabetic patients comorbid with obesity [61,62]. These suggest that leptin replacement therapy is feasible when deficient. However, further elevation in the leptin-resistant state will not improve metabolic syndrome.
Adiposity hinges on excessive caloric intake and accumulation, whereas food consumption is a complex behavior integrating energy homeostasis, reward system, and stress. Leptin is an appetite hormone, where leptin receptors are expressed in multiple brain regions [63]. Leptin exerts dual actions to regulate anorexigenic-mediated energy homeostasis [64] as well as to suppress the food-cued reward circuit in the hypothalamus [65,66]. Hypothalamus is the main target of leptin in the brain by eliciting a homeostatic response to energy accumulation in accord with nutritional states. In response to energy accumulation, leptin inhibits orexigenic neurons expressing neuropeptide Y (NPY) and agouti-related peptide (AgRP) as well as activates the anorexigenic proopiomelanocortin (POMC) neurons in the hypothalamic arcuate nucleus (ARC). The inclusive anorexigenic effect prevails during energy accumulation after feeding together with an increased body fat oxidation, and hence suppresses leptin synthesis and secretion in a negative feedback loop [67]. On the other hand, plasma leptin levels are decreased by fasting before fat depletion [68], which in turn, disinhibits orexigenic action and stimulates the appetite.
Hedonic behavior in response to food is mediated by the mesolimbic circuit involving endocannabinoid [69], orexinergic [70], and dopaminergic signaling. The food-induced hedonic circuit can possibly override homeostatic feeding. The lateral hypothalamic (LH) together with the mesolimbic reward circuit, which involves the ventral tegmental area (VTA) and nucleus accumbens (NAc) predominate the hedonic circuit, where leptin elicits anorectic action by inhibiting multiple signaling along the circuit [71,72,73]. Orexin is a neuropeptide that mediates energy sensing, appetite, body weight, and reinforces reward behaviors [74,75,76]. Orexin-expressing neurons located in the LH innervate in the VTA, where leptin receptors are expressed [77]. Leptin can suppress activities of orexin-expressing neurons in the LH, as shown in electrophysiological recordings [77]. Besides, intra-LH leptin infusion abolishes high-fat diet-conditioned place preference mediated by orexin-expressing neurons [77]. Of note, endocannabinoid signaling is in part involved in the leptin inhibitory action on orexin-expressing neurons. Leptin deficiency and high-fat diet could enhance cannabinoid receptor-mediated presynaptic inhibitory control of orexin-expressing neurons in the hypothalamic ARC [69]. These findings taken together suggest the leptin suppresses hedonic behavior in the hypothalamus involving orexigenic and endocannabinoid signaling. In addition, dopamine release in the NAc is an adaptive response to palatable food consumption in association with reward learning and incentive salience [78,79,80]. A recent review has comprehensively addressed the crosstalk of leptin and dopamine signaling in inhibiting the food reward system through the LH-VTA-NAc neural circuit [81]. The LH GABA-ergic projection to the VTA expresses leptin receptors [82]. Leptin promotes GABA release from the LH to VTA is associated with reduced food consumption in leptin-deficient mice [82]. The inhibitory effect of leptin in the reward circuit is further supported by the lentiviral-mediated knockdown of the leptin receptor in the LH [83]. Finally, leptin receptors are also expressed in dopaminergic innervation from the VTA to the NAc. Intra-VTA infusion of leptin suppresses food intake [84]. Inhibition of dopaminergic neuron activity in the VTA neurons [85] and the reduced dopamine levels in the NAc [86] may downregulate the reward system. The underlying molecular signaling for leptin inhibition in the VTA dopaminergic neuron may activate the Janus kinase-signal transducer and activator of transcription proteins JAK/STAT/PI3K/mTOR pathway [84,87]. Significantly, long-term overexpression of leptin in the VTA causes leptin receptor desensitization [88]. Conversely, adenoviral-mediated knockdown of leptin receptor in the VTA promotes food intake and sucrose preference [89], and leptin antagonism or knockout in the VTA increases NAc dopamine levels [90]. The abovementioned studies concertedly suggest the overconsumption behavior and continuous body weight gain regardless of hyperleptinemia in obese subjects [91]. Enlarged adipocyte is the culprit of hyperleptinemia. And potentially, instead of exhibiting a stronger anorexigenic effect or a stronger inhibition of hedonic reward, prolonged hyperleptinemia may desensitize the leptin receptor-mediated signaling [60]. These result in a vicious cycle of hedonic eating and obesity.
Excessive caloric intake and energy accumulation are not the only causes of obesity. Chronic atypical antipsychotic medication is obesogenic in association with severe metabolic disorders, including hyperglycemia, insulin resistance, and hyperleptinemia [92,93,94,95,96,97,98]. In particular, weight gain, increased food consumption, and hyperleptinemia are frequently reported in psychotic patients receiving olanzapine medication [99,100]. Significant elevation of circulating leptin is detected in schizophrenic subjects receiving haloperidol medication (pre, typical antipsychotic treatment) versus risperidone and clozapine medication (post, atypical antipsychotic treatment) [101]. Elevated leptin levels and weight gain in schizophrenic patients treated with atypical antipsychotics may be involved in an adiposity-induced feedback mechanism [102]. Rodent studies further support the fact that the atypical antipsychotics, namely risperidone and olanzapine, are obesogenic as well as induce leptin expression and secretion [103,104,105,106]. Essentially, antipsychotics can act on multiple neuroendocrine pathways. Alongside with serotoninergic antagonism that may underline hedonic feeding behaviors and atypical weight gain [107,108,109], some atypical antipsychotics can contravene energy homeostasis by inhibiting peripheral adrenergic system [97]. β-3 antagonism by atypical antipsychotics can not only disrupt energy homeostasis [110,111] but also induce hyperleptinemia [112]. In sum, atypical antipsychotics are obesogenic by contravening brain anorexigenic and reward circuit as well as disrupting normal adipocyte functioning.
Besides, leptin receptors are found in the hippocampus and neocortex, suggesting their possible roles in the cognitive process [63]. Leptin resistance in obese and diabetic patients can be linked to impaired leptin receptor signaling [64] and leptin insensitivity at the blood–brain barrier [50,113]. Although both leptin mRNA and protein expressions are widely detected in the brain [114,115], circulating leptin can pass through the blood–brain barrier [116] and could function as a neurotrophic factor in modulating neuroplasticity and cognitive functions [117]. db/db mice, which show loss of function in leptin receptor signaling, display neuronal atrophy in the hippocampus, including reduced hippocampal progenitor cell proliferation [118], reduced dendritic branching and dendritic spine [119]. Besides, both db/db mice and Zucker fa/fa rats show spatial memory deficits in the Morris water maze task [118,120,121] and exhibit despair behaviors [122], suggesting that impaired leptin signaling could affect structural plasticity in the hippocampus. HFD-induced diabetic model [123] and db/db mice [124] display hyperleptinemia and leptin resistance. Enhancing leptin levels enhances neuroplasticity and cognitive function in rodents under physiological conditions. For example, intraperitoneal injection with 1 mg/kg recombinant leptin continuously for 14 days promotes hippocampal cell proliferation and survival of newborn neurons in healthy male mice [24]. An in vitro study has demonstrated that leptin promotes dendritic branching and spine maturation in cultured primary neurons [125]. Moreover, leptin elicits a rapid antidepressant effect by reducing depression-like behavior in the forced swim test and tail suspension test [126]. Intrahippocampal infusion with leptin immediately after training improves memory processing in T-maze footshock avoidance and step down passive avoidance tests [127], suggesting that leptin has a direct effect on influencing hippocampal function and enhances behavioral outcome. Notably, previous studies have shown that leptin treatment via systemic injection or intra-hippocampus injection to the dorsal part can improve spatial and context-cued learning and memory. Nonetheless, a study has reported that leptin infusion in the ventral hippocampus, but not in the dorsal hippocampus, impairs memory consolidation for the spatial location of food [128]. A recent review suggests that activating the leptin signaling pathway, specifically in the ventral hippocampus, could suppress spatial working memory [129]. Mechanisms of how leptin affects structural plasticity in the hippocampus are still unclear. Leptin receptors are coupled to JAK/STAT and PI3K/Akt signaling cascades in hippocampal neurons. Activation of the above cascades increases the production of manganese superoxide dismutase (Mn-SOD), an antioxidant enzyme, as well as the anti-apoptotic protein Bcl-xL. The synergistic antioxidant and anti-apoptotic effects may stabilize the mitochondrial membrane potential, and hence lessen mitochondrial oxidative stress to promote neuronal proliferation in the hippocampus [26]. Leptin treatment could increase hippocampal cell proliferation and survival by increasing mitochondrial functioning. In addition, leptin can also promote synaptogenesis via increasing expression of microRNA-132 (miR-132) [119]. Leptin induces long-term potentiation (LTP) by modulating post-synaptic signaling pathway and glutamatergic N-methyl-D-aspartate (NMDA) receptor. LTP is considered as a cellular mechanism of learning and memory formation. The NMDA receptor-dependent LTP in the CA1 region of the hippocampus underlies spatial memory formation [130]. Both db/db mice and Zucker fa/fa rats with defective leptin receptors impair hippocampal LTP formation [120], whereas infusion of 1 µM leptin into the hippocampal dentate gyrus enhances LTP [131]. Ex vivo studies also show that leptin can increase pharmacologically-isolated NMDA receptor-mediated excitatory postsynaptic currents (EPSCs) in the CA1 region in acute rat hippocampal slices [132] (Table 1).

Table 1.
Effects of adipokines on neuroplasticity, neuroprotection, and cognitive behaviors.
Neuroprotective effects of leptin have also been shown in animal models. Eight weeks of systemic infusion with leptin reduces amyloid-β levels in the brain and serum of six-month old CRND8 transgenic mouse model of AD. Leptin treatment also improves object recognition and contextual fear learning [133]. Moreover, intracerebroventricular injection of leptin (1 µg) for ten days improves spatial memory in Y-maze and water maze tasks, as well as restores LTP in the CA1 region in an Aβ-induced AD rat model [134]. The neuroprotective effects of leptin could be linked to a leptin/JAK2/STAT3 signaling pathway [135] or leptin mediated PI3K/Akt/mTOR signaling pathway [136]. In sum, leptin can directly modulate structural and synaptic plasticity, however prolonged elevation in leptin levels could be detrimental to neuroplasticity under hyperleptinemia condition.
2.2. Adiponectin
Adiponectin is secreted by white adipose tissue and exerts anti-inflammatory effects on both endocrine and cardiovascular systems [137,138]. Adiponectin receptors (AdipoRs) express differentially in peripheral tissues. AdipoR1 is highly expressed in skeletal muscle, while AdipoR2 is abundant in the liver [139]. Hypoadiponectinemia, a condition of low circulating adiponectin, is commonly observed in obese and type 2 diabetic patients [140,141,142]. In line with clinical evidence, diabetic and obese mice also have reduced adiponectin expression in adipose tissues as well as the blood [143,144,145,146]. Circulating adiponectin levels are reduced in obesity [140,141,142], whereas the expressions of adiponectin receptors are increased, as evidenced by higher mRNA expressions of AdipoR1 in skeletal muscle in obese subjects [147] and AdipoR2 in insulin-resistant subjects [148]. Recombinant adiponectin treatment can reduce body weight and increase hepatic and muscular insulin sensitivity in an adiponectin-deficient mouse model [149]. Similarly, patients receiving rosiglitazone, an insulin sensitizer targeting the adipose tissue, experience increased plasma adiponectin by approximately two-fold [150]. These findings indicate that upregulating adiponectin expression can improve insulin sensitivity. Adiponectin receptors (AdipoR) are widely expressed in rodent brains, including the hypothalamus, brainstem, prefrontal cortex, and hippocampus, suggesting its role in the CNS in addition to its role in metabolism [27,139,151,152,153,154,155,156,157,158,159]. Overnight fasting by food deprivation for sixteen hours concomitantly downregulates mRNA expression of adiponectin and upregulates mRNA expression levels of AdipoR1 and APPL1 in the hypothalamic ARC [160], a brain area in the mediobasal hypothalamus regulating energy and glucose homeostasis [161].
Adiponectin could enter the blood–brain barrier since the low-molecular weight trimeric form of adiponectin is detectable in cerebrospinal fluid after intravenous injection in adiponectin-deficient mice [25,162]. Prominently, adiponectin is involved in energy homeostasis and appetite in concordance with leptin. A recent investigation shows that adiponectin promotes anorexigenic POMC activity in the hypothalamic ARC [163] possibly through PI3-K signaling [164]. Adiponectin elicits an excitatory effect on POMC neurons in a leptin-receptor dependent manner [163], whereas leptin synergistically potentiates adiponectin excitatory effect on POMC neuronal activity [163]. Simultaneously, adiponectin inhibits the neighboring orexigenic NPY/AgRP neurons, which then disinhibit POMC activity [163]. Further studies show that adiponectin action on the hypothalamic POMC activity may occur in a glucose-dependent reciprocal manner. Adiponectin infusion in the cerebral ventricle exerts an orexigenic effect at high glucose levels but is anorexigenic at low glucose levels [165]. Moreover, adiponectin increases the anorexigenic POMC activity at low glucose levels (2.5–5 mM), mimicking the fasting and physiological states, but decreases the POMC activity at high glucose levels (10 mM), mimicking a fed state [165] in electrophysiological recordings. The state-dependent adiponectin mechanism of action may act differentially on different molecular pathways: Adiponectin inhibits POMC neurons at high glucose via AMPK signaling, while it activates POMC neurons at low glucose via PI3-K signaling [165]. In contrast to the glucose-dependent effect in POMC, adiponectin enhances the activity of inhibitory GABA-ergic NPY neurons in a glucose-independent fashion [166]. Altogether, at low glucose conditions, adiponectin suppresses orexigenic NPY neurons and activates anorexigenic POMC neurons to attenuate appetite and food intake under conditions of fasting or low blood glucose. On the other hand, at high glucose levels, feeding behavior is nullified [165] as adiponectin inhibits both anorexigenic and orexigenic activities. Since leptin resistance and hypoadiponectinemia are symptomatic in obese and type 2 diabetic subjects, disrupted interplay of leptin and adiponectin may collectively impair anorectic actions and thus promote caloric intake and energy accumulation in obese and diabetic conditions. Hypoadiponectinemia is often documented in patients receiving atypical antipsychotics medication, including olanzapine and clozapine, in association with increased adiposity and hyperleptinemia [68,167,168]. Specifically, clozapine medication leads to body weight gain, high triglyceride profile, and hypoadiponectinemia [169,170]. GABA-facilitated orexigenic NPY activation and the subsequent suppression of anorexigenic POMC activity is suggested to be a potential mechanism of olanzapine-induced obesity [171]. The disrupted hypothalamic control of energy homeostasis may, therefore, lead to hyperleptinemia and hypoadiponectinemia. Still, some atypical antipsychotics, including risperidone and quetiapine, do not affect adiponectin levels [168,172,173,174].
AdipoR1 is expressed in dopaminergic neurons in the VTA [175]. The adiponectin receptor expression implicates the crosstalk of adiponectin and dopamine signaling pathways. Hedonic behaviors and affective behaviors are intertwined by dopamine signaling [176,177,178,179]. Recent research dissecting the role of adiponectin receptor in mediating anxiety reveals that intra-VTA infusion of adiponectin or the adiponectin receptor agonist AdipoRon suppresses dopaminergic neuron firing in an AdipoR1-dependent manner [175]. However, impaired adiponectin signaling due to adiponectin haploinsufficiency or AdipoR1 ablation increases dopaminergic activity and anxiety behavior. Adiponectin action shares similarities with the inhibitory action of leptin on the VTA dopaminergic neurons. Importantly, anxiety symptoms are often comorbid with metabolic disorders [180], where hypoadiponectinemia is indicative in obese and type 2 diabetic subjects [140,141,181]. It is speculated that the interplay of leptin and adiponectin may also exist in the VTA dopaminergic neurons to modulate reward and affective behaviors.
Patients with type 2 diabetes or dementia display decreased adiponectin levels [182,183,184]. High fat diet-induced and streptozotocin-induced diabetic conditions reduce AdipoR1 and AdipoR2 expressions in the hippocampus [27]. Adiponectin knockout reduces proliferating cells, differentiating cells, and cell survival in the hippocampus [185]. Adiponectin stimulates the proliferation of hippocampal progenitors through p38MAPK/GSK-3β/β-catenin cascade [157]. Moreover, adiponectin deficiency reduces the dendritic length, branching, and spine density of dentate granule neurons, particularly in early-born granule neurons in the hippocampal dentate gyrus [185]. Low levels of adiponectin are associated with cognitive dysfunction [184]. Chronic adiponectin deficiency impairs spatial memory and learning and induces anxiety-like behavior [19]. Moreover, AdipoR1 knockdown causes metabolic dysfunction and neurodegeneration in an association with the cognitive deficit in Morris water maze [186]. Overexpression of adiponectin in the brain [25] or infusion of recombinant adiponectin into the cerebral ventricle induces antidepressant effects [158,187,188]. The antidepressant effect could be linked to the activation of the AdipoR1/APPL1/AMPK pathway [25]. Rosiglitazone, a blood–brain barrier-impermeable PPARγ-selective agonist, enhances adiponectin levels and elicits antidepressant- and anxiolytic-like effects in wild-type mice, but not adiponectin-deficient mice or mice pretreated with PPARγ-selective antagonist [189].
The pro-cognitive effect of adiponectin in AD could be linked to its anti-inflammatory effect and enhanced effects on synaptic plasticity. Globular adiponectin predominantly binds to AdipoR1 and inhibits nuclear factor-κB (NF-κB) activation in macrophages, which in turn, suppresses its production of pro-inflammatory cytokines [190,191]. Therefore, adiponectin may reduce the extracellular deposition of amyloid-β via its suppressive effect on microglial activation. Moreover, adiponectin attenuates streptozotocin-induced Tau hyperphosphorylation and cognitive deficits through PI3K/Akt/GSK-3β pathway [192]. Activating AMPK can suppress GSK-3β action on Tau phosphorylation, whereas chronic adiponectin deficiency fails to phosphorylate AMPK, which in turn, enables GSK3β action on promoting Tau hyperphosphorylation, and subsequently results in AD-like neuropathology [19]. Nine-month-old adiponectin-deficient, 5×FAD mice show microglia activation together with elevated TNFα and IL-1β levels in the cortex and hippocampus [193]. In accordance with the previous study, an in vivo study illustrates that globular adiponectin exerts anti-inflammatory effects on microglia by reducing IL-1β, IL-6, and TNFα [33]. Pre-treatment with adiponectin can diminish TNFα and IL-1β release in vitro [193]. Adiponectin potentially exerts anti-inflammatory action on microglia via AdipoR1/NF-κB signaling [33,193]. Other studies have further demonstrated that adiponectin exhibits anti-inflammatory response dependent on PPARγ [194] or IL-4/STAT6 signaling pathway [191]. Recently, an ex vivo study has demonstrated that adiponectin exhibits a beneficial effect on hippocampal synaptic plasticity in 5×FAD mice. Acute perfusion for 10-min or 2-h incubation of 2.7 nM adiponectin can induce LTP in the hippocampal CA1 region in five to six months old 5×FAD mice. Acute incubation of adiponectin also increases expressions of AdipoR1 and AdipoR2, increases protein expressions of GluA1, GluN1, GluN2B, and PSD-95 as well as elicits anti-apoptotic and anti-inflammatory effects [195]. These findings suggest that adiponectin inhibits neuronal apoptosis and inflammatory mechanisms and promotes hippocampal long-term potentiation. Taken together, these data have suggested the neuroprotective and neurogenic effects of adiponectin in the hippocampus (Table 1).
2.3. Chemerin
Chemerin is a novel adipokine that acts autocrine, paracrine, and endocrine on different tissues [196] by binding to either chemokine-like receptor 1 [197], chemokine receptor-like receptor 2 [198] or G protein-coupled receptor 1 [199]. Chemerin is highly expressed in white adipose tissue [200] and acts as a pro-inflammatory cytokine [201] and anti-inflammatory cytokine. It promotes adipogenesis [200], angiogenesis [202], and inflammation [203]. Clinical study has shown that change of chemerin levels is linked to obesity because the circulating levels of chemerin is positively correlated with high body-mass index and elevated obesity-related biomarkers [204,205,206]. Similarly, high fat diet-induced obese mice display an increase in plasma chemerin levels, and this increase can be reduced by overnight fasting [207]. Another study has shown that chemerin administration exacerbates the glucose intolerance in obese and diabetic mice by reducing hepatic glucose uptake [208]. Chemerin deficiency results in insulin resistance in adipose tissue and liver, leading to elevated hepatic glucose production and increased blood glucose levels [209]. On the other hand, chemokine-like receptor 1 knockout mice have reduced glucose uptake in adipose tissue and skeletal muscle [210], whereas high-fat diet further exacerbates glucose intolerance, hyperinsulinemia and enhances insulin resistance in these mice [211].
Activation of the chemerin signaling pathway plays a vital role in the neuroendocrine axis by regulating appetite. Chemerin receptors are highly expressed in multiple rodent brain regions, including the prefrontal cortex, hippocampus, and hypothalamus [212]. Continuous intracerebral infusion of chemerin into photoperiodic-sensitive F344 rats can promote food intake [213], whereas chemokine-like receptor 1 deficiency reduces food intake and body weight [210]. Chemerin can also aggravate glucose intolerance [208]. Consistently, clinical data indicate that circulating chemerin levels are increased in patients with obesity, diabetes, and cardiovascular diseases [214].
A recent study has shown that intranasal administration of human recombinant chemerin (rh-chemerin) exerts neuroprotective effects in a rat model of neonatal hypoxia-ischemia brain injury [215]. Intranasal treatment with chemerin significantly reduces infarct volume and attenuates developmental delay 24 h after hypoxic-ischemic encephalopathy. Chemerin treatment significantly improves cognitive and sensorimotor performance in animals with hypoxic-ischemic encephalopathy. Moreover, recombinant chemerin treatment significantly reduces apoptosis and the expressions of pro-apoptotic markers [215], suggesting a neuroprotective role of chemerin. Chemerin signaling is proposed to mediate neuro-inflammatory action in the brain. It is reported that the expression of chemokine like receptor 1 (CMKLR1) is upregulated in AD patients, suggesting the role of central chemerin signaling in the progression of AD [216]. Systemic lipopolysaccharide administration is known to upregulate CMKLR1 expression and promote neuroinflammation [216]. This study has reported that CMKLR1 and Aβ42 are colocalized in hippocampal neurons of APP/PS1 AD mice, and CMKLR1 is involved in Aβ processing and clearance. CMKLR1 is detected in the hippocampus and prefrontal cortex, two critical brain regions involved in the pathology of depression [217]. Intracerebral administration of chemerin elicits antidepressant effects [218]. In the lipopolysaccharide-induced depression mouse model, intracerebral administrations of chemerin receptor agonist: Eicosapentaenoic acid-derived resolvins E1 (1 ng) or E2 (10 ng) produce antidepressant effects depending on ChemR23/mTORC1 pathway in the medial prefrontal cortex and hippocampal dentate gyrus [218] (Table 1), suggesting activating chemerin signaling could be a novel antidepressant target.
2.4. Apelin
Apelin, a peptide hormone secreted by adipocytes, is involved in insulin secretion [219], glucose and lipid metabolism [220], angiogenesis [221], blood pressure regulation [222], and food intake [223]. Apelin has similar properties as physical exercise does in metabolism, and so given entitled it as an exerkine [224]. Apelin can be proteolytically cleaved into several bioactive forms, including apelin-13, -17, and -36, as well as the pyroglutaminated apelin-13 isoform [225]. Apelin receptors are widely distributed in rodent brain and systemic tissues [226].
Apelin is necessary for balancing the fat composition and promoting insulin sensitivity. Apelin-knockout mice exhibit obese and diabetic symptoms, including increased abdominal fat mass, glucose intolerance, hyperinsulinemia, and hypo-adiponectinemia [227]. High-fat diet and high-sucrose consumption aggravate glucose and insulin intolerance in apelin-deficient mice [228]. Clinical study has reported a positive correlation between plasma insulin levels and apelin expression in adipocytes from obese subjects. Given this insulin-sensitizing property, apelin has become a promising therapeutic target for treating obesity and diabetes. Single intravenous injection of 200 pmol/kg Pyr(1)-apelin-13 can improve glucose intolerance in high-fat diet-induced obese and insulin-resistant mice [229]. Chronic apelin treatment (two to four weeks) improves insulin sensitivity, lowers blood glucose levels, and protect the animals from hyperinsulinemia and glucose intolerance in mice with obesity or insulin resistance [228,230]. Apelin treatment can also significantly reduce adiposity and plasma triglycerides [230]. Apelin is involved in lipid metabolism by inhibiting isoproterenol-induced lipolysis in cultured adipocytes [227]. Moreover, exogenous apelin reduces the number of differentiated adipocytes and increases the size of lipid droplets inside the cells, suggesting that apelin might suppress lipolysis [231]. In vitro studies reveal that apelin-13 and [Pyr1]-apelin-13 improve glycemia in an AMPK/eNOS-dependent [229] and PI3K/Akt-dependent [232] pathways respectively. These findings have collectively suggested that apelin treatment could be useful in reducing adiposity, improving insulin sensitivity, and improving diabetic conditions.
Similar to other adipokines, apelin exhibits anti-inflammatory properties [232] and possesses neuroprotective effects [233]. In an ischemia/reperfusion (I/R) stroke rat model, the post-stroke intracerebral injection of apelin-13 can significantly reduce the infarct volume [234]. Similarly, intracerebral infusion of apelin-13 significantly decreases blood–brain barrier permeability and increases vascular endothelial growth factor levels in post-stroke mice [235]. Furthermore, post-stroke treatment with intranasal apelin-13 for three days can reduce infarct volume, reduce neuronal apoptosis, suppress inflammation, and increase angiogenesis [236]. In mice with traumatic brain injury, intracerebral administration of apelin-13 reduces brain damage via suppressing autophagy [237]. Apelin-13 also elicits an anti-inflammatory effect by inhibiting microglia and astrocyte activation and upregulates hippocampal BDNF and TrkB expression in streptozotocin-induced sporadic AD rats. Furthermore, the apelin-13 treatment also promotes learning and memory performance, as evidenced by its effect on improving novel object recognition and spatial recognition through the BDNF/TrkB pathway [238]. In a rat model of depression, apelin-13 treatment elicits antidepressant effect and improves recognition memory via activating phosphatidylinositol 3-kinases (PI3K) and extracellular signal-regulated kinase 1/2 (ERK1/2) signaling pathways. The hippocampus is thought to be the critical brain region mediating the antidepressant-like response of apelin [239,240]. Similarly, intracerebral infusion of apelin-13 can ameliorate depression-like phenotypes in rats subjected to chronic restraint stress. Apelin-13 can also suppress hypothalamic-pituitary-adrenal axis hyperactivity, promote hippocampal BDNF expression, and restore hippocampal glucocorticoid receptor functions in rats with chronic stress [241] (Table 1).
2.5. Visfatin (Nicotinamide phosphoribosyltransferase, NAMPT)
Nicotinamide phosphoribosyltransferase (NAMPT) is an enzyme which catalyzes the biosynthesis of nicotinamide adenine dinucleotide (NAD+) in mammals [242]. There are two isoforms of NAMPT: Intracellular NAMPT (iNAMPT) and extracellular NAMPT (eNAMPT or visfatin) [242]. Growing evidence shows that NAD+/NADH metabolism in adipose tissue is linked to obesity and insulin resistance. In humans, visceral adipose NAMPT expression and serum NAMPT levels are positively correlated with obesity [243]. In mice, adipose NAMPT expression and NAD+ contents are markedly reduced by high-fat diet feeding [244,245], but increased by caloric restriction [246,247]. Adipocyte-specific Nampt knockout mice show severe insulin resistance in multiple organs under a chow-fed condition, which is independent of body weight and adiposity [248]. Loss of Nampt causes adipose tissue inflammation, increases plasma free fatty acid concentrations, and decreases adiponectin. Notably, oral administration with nicotinamide mononucleotide, a key NAD+ intermediate, can restore adipose tissue NAD+ biosynthesis and significantly restore insulin resistance, plasma adiponectin and free fatty acid concentrations in adipocyte-specific Nampt knockout mice. On the other hand, visfatin is secreted from white adipose tissue through sirtuin1 (SIRT1)-mediated deacetylation of iNAMPT [249]. At present, it remains uncertain whether visfatin can cross the blood–brain barrier. However, adipose-secreted visfatin serves as a neuroendocrine factor. Adipose tissue-specific Nampt knockout mice display a significant reduction in circulating visfatin, as well as reduced hypothalamic NAD+ content and SIRT1 activity [249]. On the other hand, adipose-specific Nampt knock-in mice show increases in hypothalamic NAD+ content, SIRT1 activity, and neural activity in response to fasting. Therefore, adipose-secreted visfatin has a strong implication on modulating brain functions.
Visfatin protects neurons against ischemia-induced injury because NAMPT overexpression can reduce infarct volume and improve long-term neurologic outcomes [250]. In a transient global cerebral ischemia model with 20-min carotid arteries occlusion, intracerebral infusion of 100 ng visfatin in the hippocampal CA3 region during cerebral reperfusion can reduce the caspase-3 activation and Bax/Bcl-2 ratio [251]. Visfatin can significantly reduce apoptosis and necrotic cell death in the CA1 region of the hippocampus, with improved memory deficits in I/R rats. The suppressed pro-apoptotic and enhanced anti-apoptotic mechanisms could contribute to the neuroprotective effects of visfatin [250]. In another study, transgenic mice overexpressing NAMPT globally increase NAD+ content and neuronal survival in the hippocampal dentate gyrus [252]. These mice also display better learning and memory performance in the water maze test upon middle cerebral artery occlusion. Post-ischemic intraperitoneal administration with nicotinamide mononucleotide for seven days can improve adult hippocampal neurogenesis [252]. Nicotinamide mononucleotide and NAD+ promotes proliferation and differentiation of neural stem cells in a NAMPT/NAD+/SIRT manner [252]. An in vitro study has concluded that cultured glia, but not neuron, can secrete visfatin under oxygen-glucose deprivation stress. Treatment of wild-type visfatin, but not H247A-mutant enzymatic-dead visfatin, can significantly attenuate oxygen-glucose deprivation-elicited cell death in both cultured mouse neuron and glia. Treatment of neutralizing antibody can, in turn, abolish the protective effect of extracellular visfatin on cell viability [253].
Although the neuroprotective benefits of visfatin towards neurodegenerative diseases require further investigation, growing evidence has indicated that NAD+ administration can improve cellular energetics and extend life span in rodents [254]. The evidence leads to the idea that the administration of NAD+ precursors, including nicotinamide mononucleotide and nicotinamide riboside, is a potential treatment to forestall disease progress in AD by improving brain energetics [255]. In the AD rat model with an intracerebral infusion with Aβ amyloid, intraperitoneal administration of 500 mg/kg nicotinamide mononucleotide improves learning and memory performance in water maze task [256]. Nicotinamide mononucleotide also attenuates Aβ oligomer-induced neuronal cell death, prevents long-term potentiation deficit, restores NAD+ and ATP levels, and eliminates reactive oxygen species in organotypic hippocampal slices [256]. Moreover, nicotinamide riboside treatment exhibits pro-cognitive function by increasing cortical NAD+ content and restoring long-term potentiation deficit in the hippocampal CA1 region of the Tg2576 AD mouse model. This study has suggested that treatment upregulating the NAMPT/NAD+ axis could prevent Aβ accumulation in the brain [257] (Table 1).
3. Novel Adipocyte-Derived Messengers on Brain Health
Lipokine refers to fatty acids that act like hormones and modulate lipid metabolism [258]. Notably, adipose tissue, which is one of the systemic sites with active lipid metabolism, secretes various lipids into the bloodstream to communicate with distant organs. Coincidentally, alterations in lipid metabolism may implicate the onset of brain diseases. For example, apolipoprotein E (ApoE) mediates systemic cholesterol metabolism and acts as a cholesterol carrier to neurons in the central nervous system. Human carriers of mutated apolipoprotein E allele ϵ4 are associated with an increased risk of AD [259]. Moreover, post-mortem studies have shown that AD patients display abnormal levels of ceramides, n-3 polyunsaturated fatty acids (PUFA), and PUFA-derived signaling lipids [260,261,262,263,264].
Lipokines, including monounsaturated palmitoleic acid and lysophosphatidic acid (LPA can exert endocrine effects on systemic tissues and have potential crosstalk with the central nervous system. Palmitoleic acid is a highly abundant fatty acid in the serum. Its circulating levels fluctuate dependent on metabolic states. Obese children and adults exhibit a higher plasma palmitoleic acid content compared to healthy control [265,266]. Besides, the change of palmitoleate could be associated with an increased risk of obesity, dyslipidemia, and insulin resistance [265,266,267,268]. On the other hand, lysophospholipid is a prominent class of lipid signaling molecules, whereas LPA is a crucial member. Circulating LPAs are synthesized by autotaxin, a phosphodiesterase produced by adipocytes [269]. Circulating autotaxin levels increase in obesity and insulin resistance [270,271,272,273,274,275,276], which is positively correlated with an increase in circulating lysophosphatidic acid [277,278]. A high-fat diet can perturb lipid composition in the brain. The altered lipid composition is evidenced by a surge of palmitoleic acid composition in the mouse brain after 14 days of high carbohydrate and high fatty acid diets [279]. Congruently, high-fat diet causes a significant elevation of LPA in mouse cortex after eight weeks of high-fat diet [280]. Importantly, over-nutritious food has detrimental effects on brain plasticity because brain diseases could be linked to dysregulated lipid metabolism [281,282,283,284,285,286]. The effects of palmitoleic acid and lysophosphatidic acid on brain health warrant further investigation.
3.1. Palmitoleic Acid (16:1n7)
Palmitic acid (16:0) is the most common saturated fatty acid in the human body. It can be consumed through diet or synthesized from other fatty acids, carbohydrates, and amino acids endogenously [287]. Under normal physiological conditions, palmitic acid accumulation is prevented by desaturation to palmitoleic acid (16:1n7) or by elongation to stearic acid (18:0), then further desaturation to oleic acid (18:1) [288,289]. Abnormal levels of palmitic acid have been documented in neurodegenerative diseases [290,291,292] that are related to dysregulated palmitic acid biosynthesis. Palmitoleic acid, a monounsaturated fatty acid, primarily originates from stearoyl-CoA desaturase 1-mediated de novo lipogenesis from palmitic acid in humans [287]. Palmitoleic acid is highly abundant in serum and adipose tissues [293]. cis-palmitoleate has been associated with increased insulin sensitivity and decreased lipid accumulation in the liver [258]. Various animal models have illustrated that cis-palmitoleate reduces the expressions of pro-inflammatory cytokines and adipokines in association with metabolic syndromes [258,294,295]. In vitro study also shows that palmitoleic acid increases lipolysis and lipase content in white adipose tissue in a PPARα-dependent manner [296]. Other than adipose tissues, palmitoleic acid can enhance whole-body glucose disposal [297] and improve circulating lipid profiles in both rodents and humans [298]. Therefore, palmitoleic acid is considered a lipokine.
Fatty acid-binding proteins (FABP) are lipid chaperones that regulate lipid trafficking and responses in cells [299,300]. In humans, circulating adipose-derived fatty acid-binding protein (A-FABP) levels are substantially higher than other adipokines, including leptin, resistin, TNF-α, and IL-6 [301,302,303]. Circulating A-FABP is markedly increased in both obese men and women [304], suggesting that A-FABP may involve in modulating insulin sensitivity and lipid metabolism in distant organs. Of note, A-FABP is also considered as an adipokine, which is secreted from adipocyte-derived exosomes by exocytosis [305]. Critically, deficiencies in A-FABP and epidermal fatty acid-binding protein (E-FABP) can activate SCD1 activity, leading to a subsequent elevation in palmitoleate concentration in adipose tissue [306,307]. A-FABP deficient mice exhibit improvement in systemic glucose, lipid metabolism and insulin resistance in association with diet-induced and genetically-disposed obesity [308]. The A-FABP and E-FABP double mutant mice are resistant to diet-induced obesity, insulinemia, type 2 diabetes, dyslipidemia, and fatty liver disease [309,310]. The dysregulated SCD1-mediated de novo synthesis of palmitoleic acid enhances whole-body glucose and fatty acid metabolism [311].
Although it requires more solid evidence to demonstrate the effect of adipocyte-secreted palmitoleic acid and A-FABP on brain health, it is reported that stearoyl-CoA desaturase activity and levels of palmitoleic acid in the brain are associated with AD [312]. Liquid chromatography-mass spectrometry analysis has revealed elevated levels of several monounsaturated fatty acids, including palmitoleic acid, in the mid-frontal cortex, temporal cortex, and hippocampus of AD patients as compared to their age-matched counterparts [312]. This increase is strongly associated with cognitive dysfunction and the increased expression of stearoyl-CoA desaturase in the brain [266,313,314,315,316,317]. Further studies have shown that AD patients have increased expressions of various stearoyl-CoA desaturase isoforms, including SCD-1 [312]. Coherently, stearoyl-CoA desaturase activity is negatively correlated to cognitive measures [312]. Levels of free palmitoleic acid and the desaturation index are decreased in frontal cortices in aged dogs treated with antioxidant, and vice versa [318]. The study implicates that altering stearoyl-CoA desaturase activity and reducing palmitoleic acid levels in the brain may improve cognitive performance [318].
3.2. Lysophosphatidic Acid
Neuroinflammation is commonly associated with type 2 diabetes [319], and obesity [320]. High-fat diet feeding results in profound central and peripheral inflammation [321,322]. Autotaxin is a lysophospholipase that synthesizes lysophosphatidic acid (LPA). Autotaxin is also regarded as an adipokine due to its role in promoting adipocyte differentiation [269]. Evidence suggests that the autotaxin-mediated LPA biosynthesis contributes to the majority of extracellular LPA, in which adipocyte-specific autotaxin contributes to most of the circulating LPA [269,272]. Further investigations suggest that circulating LPA and autotaxin levels are linked to adipocyte differentiation and obesity [269,271]. Autotaxin expression is upregulated in obese patients and obese db/db mice due to the accumulation of triglycerides in the adipocytes [271]. A recent study has reported that adipose-derived autotaxin serves as an inflammatory cytokine of diet-induced obesity [323].
LPA signaling mediates inflammation [324], angiogenesis [325], brain development [326], and neurogenesis [327] in the brain. Specifically, LPA exerts a pleiotropic effect on various brain cell types, including neurons, astrocytes, microglia, and oligodendrocytes that show LPA receptors expression [328]. LPA promotes neuronal differentiation in cortical neural progenitor cells through LPA1 receptor/Gi/o pathway [329], whereas axonal branching is induced in hippocampal cell cultures through LPA3 receptor/Gq/Rho family GTPase 2 (Rnd2) pathway [330]. Mainly, LPA1 is essential in mediating synaptic plasticity and learning. In vitro studies have shown that overexpression of LPA1 increases dendritic spine density and size [331], potentially through protein kinase C (PKC)/Rho and PKC/Rac cascades [332,333]. It is speculated that LPA1 deficiency can cause schizophrenia-like behaviors, including impaired spatial memory retention and increased anxiety-like behavior [334,335,336]. Furthermore, the role of LPA and its receptors in anxiety-like behavior and learning has been confirmed by later studies using LPA1-null mice. These mice show normal survival but display aberrant hippocampal neurogenesis and decreased BDNF levels [327], as well as increased anxiety-like behavior and memory deficits [337]. LPA mediates astrocyte proliferation through the LPA1 receptor [338]. Interestingly, LPA promotes astrocyte-neuronal crosstalk through laminin-mediated EGFR/MAPK signaling to facilitate neuronal differentiation [339]. LPA triggers microglial migration through a Ca2+-dependent K+ channel [340,341], and reduces oxidative stress [342,343]. Moreover, LPA can promote the retraction of oligodendrocyte processes in mature oligodendrocytes [344] as well as promotes the formation of oligodendrocyte processes in differentiating oligodendrocytes [345].
In addition to a metabolic disorder, an altered systemic lipid metabolism may have a neurological impact [346] through autotaxin-LPA signaling. Clinical study has reported that mild cognitive impairment and AD patients have significantly higher levels of autotaxin in cerebrospinal fluid [347]. Furthermore, the autotaxin levels are positively correlated to neuroinflammatory markers, β-amyloid, and tau in the cerebrospinal fluid [347]. In vitro study has shown that LPA could increase Aβ production by upregulating the expression of β-secretase expressions in the N2a neuroblastoma cell line expressing wild-type presenilin 1 and Swedish mutant APP [348]. Potentially, LPA-induced BACE1 promoter activation is mediated by PKCδ/MEK/MAPK/p90RSk/CREB signaling cascades [348,349,350,351,352,353]. Moreover, LPA may be involved in tau hyperphosphorylation and paired helical filaments formation, which are the pathological patterns in AD brains through Gα12/13/RhoA/Rock/GSK-3β pathway [354,355], suggesting potential connection among LPA, microfilament dynamics, and AD pathogenesis.
4. Conclusions
It is an emerging research field to understand the functions of different adipokines in regulating eating behavior, hippocampal plasticity, and neuronal protection. This review has denoted five adipokines (leptin, adiponectin, chemerin, apelin, and visfatin) and two lipokines (palmitoleic acid and lysophosphatidic acid) (Figure 1). The review has summarized the currently available evidence for their novel function in the brain. First, it is evident that the aberrant adipokine production not only renders the susceptibility to metabolic syndromes in genetically deficient rodent models of various adipokines but also the vulnerability to neurodegeneration, especially in models of impaired leptin-signaling. Accumulated evidence has indicated that diet-induced obese or diabetic rodent models show abnormal levels of leptin, adiponectin, chemerin, apelin, and visfatin. Notably, circulating adiponectin and visfatin levels are reduced in diet-induced obesity, with associated impairments in hippocampal plasticity and cognitive behaviors [356]. Due to the multifaceted effect of adipokines on systemic and brain health, dysregulated adipokine secretion could be one of the causes that underlie the comorbidity of metabolic syndromes with neurodegenerative disorders [357,358]. Thus, all these investigations have highlighted the prominent roles of adipokines on brain health. Second, evidence also shows that leptin and adiponectin can elicit their action directly in the brain by crossing the blood–brain barrier. Leptin is not only a satiety regulator through anorexigenic and dopaminergic controls, but ample evidence also supports its role in promoting neuroplasticity in the hippocampus [12]. On the other hand, adiponectin is a chief metabolic regulator in glucose and fatty acid metabolism with insulin-sensitizing ability in both peripheral and central systems. Current findings have suggested the direct effect of adiponectin on synaptic plasticity [195,359] and microglial activation [193]. Both exogenous leptin and adiponectin can exert pro-cognitive effects in mouse models. Besides, leptin and adiponectin signaling pathways are defective in AD brains [360]. Hence, increasing leptin and adiponectin signaling can be a potential therapeutic target for AD [361,362]. Third, emerging literature has also revealed the central function of three novel adipokines: Chemerin, apelin, and visfatin. Inflammatory response and apoptosis are typical in neurodegenerative diseases [363,364] and ischaemic stroke [365,366]. These novel adipokines are potential therapeutic targets, which modulate anti-inflammatory and anti-apoptotic effects in the hippocampus. Finally, this review has highlighted lipokines are a lipid signaling molecule secreted by adipocytes with potential endocrine effect acting on the brain [367]. Still, the potential of lipokines is mostly unknown, future studies will be required to illustrate its properties and function in neuroplasticity and cognitive functions.
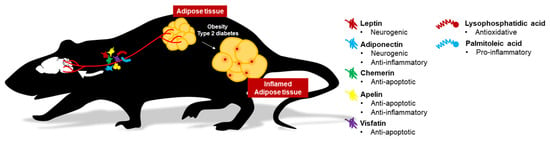
Figure 1.
Potential mechanism of adipokine actions on brain health. Adiponectin and leptin can cross the blood–brain barrier to promote neuroplasticity. Other adipokines and lipokines show profound effects on mediating neurogenic and neuroinflammatory mechanisms.
Overall, adipokines emerge as viable therapeutic targets towards neurodegenerative diseases. Adipokine-based therapeutic approaches could be future pharmaceuticals to obliterate neurodegenerative disorders. More in-depth investigations on the above-mentioned adipokines and its crosstalk with the brain can open up new therapeutic targets to treat neurodegenerative diseases.
Author Contributions
T.H.-y.L. wrote the manuscript. S.-y.Y., K.K.y.C., R.L.-c.H., and P.M.-f.S. revised and edited the manuscript.
Funding
This work is supported by the Hong Kong Research Council Early Career Scheme (project No. 25100217) and National Natural Science Foundation of China (Project No. 81801346) awarded to S.-y.Y.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kershaw, E.E.; Flier, J.S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 2004, 89, 2548–2556. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Sun, H.M.; Hwang, K.C.; Kim, S.W. Adipose-derived stromal vascular fraction cells: Update on clinical utility and efficacy. Crit. Rev. Eukaryot. Gene Expr. 2015, 25, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Warner, A.; Mittag, J. Brown fat and vascular heat dissipation: The new cautionary tail. Adipocyte 2014, 3, 221–223. [Google Scholar] [CrossRef] [PubMed]
- Cedikova, M.; Kripnerova, M.; Dvorakova, J.; Pitule, P.; Grundmanova, M.; Babuska, V.; Mullerova, D.; Kuncova, J. Mitochondria in white, brown, and beige adipocytes. Stem Cells Int. 2016, 2016, 6067349. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.E.; Ahmadian, M.; Jaworski, K.; Sarkadi-Nagy, E.; Sul, H.S. Regulation of lipolysis in adipocytes. Annu. Rev. Nutr. 2007, 27, 79–101. [Google Scholar] [CrossRef] [PubMed]
- Choe, S.S.; Huh, J.Y.; Hwang, I.J.; Kim, J.I.; Kim, J.B. Adipose tissue remodeling: Its role in energy metabolism and metabolic disorders. Front. Endocrinol. 2016, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Cook, K.S.; Min, H.Y.; Johnson, D.; Chaplinsky, R.J.; Flier, J.S.; Hunt, C.R.; Spiegelman, B.M. Adipsin: A circulating serine protease homolog secreted by adipose tissue and sciatic nerve. Science 1987, 237, 402–405. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Proenca, R.; Maffei, M.; Barone, M.; Leopold, L.; Friedman, J.M. Positional cloning of the mouse obese gene and its human homologue. Nature 1994, 372, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Rosen, E.D.; Spiegelman, B.M. What we talk about when we talk about fat. Cell 2014, 156, 20–44. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, K.; Sypniewska, G. Diabetes as a complication of adipose tissue dysfunction. Is there a role for potential new biomarkers? Clin. Chem. Lab. Med. 2013, 51, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Flier, J.S.; Maratos-Flier, E. Lasker lauds leptin. Cell 2010, 143, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Harvey, J.; Solovyova, N.; Irving, A. Leptin and its role in hippocampal synaptic plasticity. Prog. Lipid Res. 2006, 45, 369–378. [Google Scholar] [CrossRef] [PubMed]
- De la Monte, S.M.; Wands, J.R. Review of insulin and insulin-like growth factor expression, signaling, and malfunction in the central nervous system: Relevance to Alzheimer’s disease. J. Alzheimers Dis. 2005, 7, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Steen, E.; Terry, B.M.; Rivera, E.J.; Cannon, J.L.; Neely, T.R.; Tavares, R.; Xu, X.J.; Wands, J.R.; de la Monte, S.M. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease—Is this type 3 diabetes? J. Alzheimers Dis. 2005, 7, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Schioth, H.B.; Craft, S.; Brooks, S.J.; Frey, W.H., 2nd; Benedict, C. Brain insulin signaling and Alzheimer’s disease: Current evidence and future directions. Mol. Neurobiol. 2012, 46, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Craft, S. Alzheimer disease: Insulin resistance and AD—Extending the translational path. Nat. Rev. Neurol. 2012, 8, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Ye, R.; Scherer, P.E. Adiponectin, driver or passenger on the road to insulin sensitivity? Mol. Metab. 2013, 2, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Maeda, N.; Shimomura, I.; Kishida, K.; Nishizawa, H.; Matsuda, M.; Nagaretani, H.; Furuyama, N.; Kondo, H.; Takahashi, M.; Arita, Y.; et al. Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat. Med. 2002, 8, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Ng, R.C.; Cheng, O.Y.; Jian, M.; Kwan, J.S.; Ho, P.W.; Cheng, K.K.; Yeung, P.K.; Zhou, L.L.; Hoo, R.L.; Chung, S.K.; et al. Chronic adiponectin deficiency leads to Alzheimer’s disease-like cognitive impairments and pathologies through AMPK inactivation and cerebral insulin resistance in aged mice. Mol. Neurodegener. 2016, 11, 71. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K. Metabolic syndrome and cognitive decline. Curr. Alzheimer Res. 2007, 4, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Biessels, G.J.; Despa, F. Cognitive decline and dementia in diabetes mellitus: Mechanisms and clinical implications. Nat. Rev. Endocrinol. 2018, 14, 591–604. [Google Scholar] [CrossRef] [PubMed]
- Stoeckel, L.E.; Arvanitakis, Z.; Gandy, S.; Small, D.; Kahn, C.R.; Pascual-Leone, A.; Sherwin, R.; Smith, P. Complex mechanisms linking neurocognitive dysfunction to insulin resistance and other metabolic dysfunction. F1000Research 2016, 5, 353. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, D. Adiposity indices and dementia. Lancet Neurol. 2006, 5, 713–720. [Google Scholar] [CrossRef]
- Garza, J.C.; Guo, M.; Zhang, W.; Lu, X.Y. Leptin increases adult hippocampal neurogenesis in vivo and in vitro. J. Biol. Chem. 2008, 283, 18238–18247. [Google Scholar] [CrossRef] [PubMed]
- Yau, S.Y.; Li, A.; Hoo, R.L.; Ching, Y.P.; Christie, B.R.; Lee, T.M.; Xu, A.; So, K.F. Physical exercise-induced hippocampal neurogenesis and antidepressant effects are mediated by the adipocyte hormone adiponectin. Proc. Natl. Acad. Sci. USA 2014, 111, 15810–15815. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Jiang, H.; Xu, X.; Duan, W.; Mattson, M.P. Leptin-mediated cell survival signaling in hippocampal neurons mediated by JAK STAT3 and mitochondrial stabilization. J. Biol. Chem. 2008, 283, 1754–1763. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Kang, S.M.; Kim, E.; Kim, C.H.; Song, H.T.; Lee, J.E. Adiponectin receptor-mediated signaling ameliorates cerebral cell damage and regulates the neurogenesis of neural stem cells at high glucose concentrations: An in vivo and in vitro study. Cell Death Dis. 2015, 6, e1844. [Google Scholar] [CrossRef] [PubMed]
- Formolo, D.A.; Lee, T.H.; Yau, S.Y. Increasing adiponergic system activity as a potential treatment for depressive disorders. Mol. Neurobiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Wang, Y.; Gan, X.; Fang, D.; Zhong, C.; Wu, L.; Hu, G.; Sosunov, A.A.; McKhann, G.M.; Yu, H.; et al. Drp1-mediated mitochondrial abnormalities link to synaptic injury in diabetes model. Diabetes 2015, 64, 1728–1742. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Guo, H.; Li, X.; Yue, L.; Liu, H.; Zhao, L.; Bai, H.; Liu, X.; Wu, X.; Qu, Y. Adiponectin attenuates oxygen-glucose deprivation-induced mitochondrial oxidative injury and apoptosis in hippocampal HT22 cells via the JAK2/STAT3 pathway. Cell Transpl. 2018, 27, 1731–1743. [Google Scholar] [CrossRef] [PubMed]
- Qiu, G.; Wan, R.; Hu, J.; Mattson, M.P.; Spangler, E.; Liu, S.; Yau, S.Y.; Lee, T.M.; Gleichmann, M.; Ingram, D.K.; et al. Adiponectin protects rat hippocampal neurons against excitotoxicity. Age 2011, 33, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Choi, S.M.; Whitcomb, D.J.; Kim, B.C. Adiponectin controls the apoptosis and the expression of tight junction proteins in brain endothelial cells through AdipoR1 under beta amyloid toxicity. Cell Death Dis. 2017, 8, e3102. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, S.; Cazareth, J.; Zarif, H.; Guyon, A.; Heurteaux, C.; Chabry, J.; Petit-Paitel, A. Globular adiponectin limits microglia pro-inflammatory phenotype through an AdipoR1/NF-kappaB signaling pathway. Front. Cell Neurosci. 2017, 11, 352. [Google Scholar] [CrossRef] [PubMed]
- Zuloaga, K.L.; Johnson, L.A.; Roese, N.E.; Marzulla, T.; Zhang, W.; Nie, X.; Alkayed, F.N.; Hong, C.; Grafe, M.R.; Pike, M.M.; et al. High fat diet-induced diabetes in mice exacerbates cognitive deficit due to chronic hypoperfusion. J. Cereb. Blood Flow Metab. 2016, 36, 1257–1270. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hao, S.; Yin, H.; Gao, J.; Yang, Z. Autophagy ameliorates cognitive impairment through activation of PVT1 and apoptosis in diabetes mice. Behav. Brain Res. 2016, 305, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Du, F.; Wu, L.; Zhang, Z.; Zhong, C.; Yu, Q.; Wang, Y.; Lue, L.F.; Walker, D.G.; Douglas, J.T.; et al. F1F0 ATP synthase-cyclophilin D interaction contributes to diabetes-induced synaptic dysfunction and cognitive decline. Diabetes 2016, 65, 3482–3494. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.J.; Wu, J.H.; Sun, S.Y.; Ma, L.L.; Zhou, J.Q. Liraglutide ameliorates cognitive decline by promoting autophagy via the AMP-activated protein kinase/mammalian target of rapamycin pathway in a streptozotocin-induced mouse model of diabetes. Neuropharmacology 2018, 131, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Song, F.; Xu, K.; Liu, Z.; Han, S.; Li, F.; Sun, Y. Irisin attenuates neuroinflammation and prevents the memory and cognitive deterioration in streptozotocin-induced diabetic mice. Mediators Inflamm. 2019, 2019, 1567179. [Google Scholar] [CrossRef] [PubMed]
- Saravia, F.E.; Beauquis, J.; Revsin, Y.; Homo-Delarche, F.; de Kloet, E.R.; De Nicola, A.F. Hippocampal neuropathology of diabetes mellitus is relieved by estrogen treatment. Cell Mol. Neurobiol. 2006, 26, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Deng, J.; Sheng, W.; Zuo, Z. Metformin attenuates Alzheimer’s disease-like neuropathology in obese, leptin-resistant mice. Pharmacol. Biochem. Behav. 2012, 101, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Hayashi-Park, E.; Ozment, B.N.; Griffith, C.M.; Zhang, H.; Patrylo, P.R.; Rose, G.M. Experimentally induced diabetes worsens neuropathology, but not learning and memory, in middle aged 3xTg mice. Behav. Brain Res. 2017, 322, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Leuner, B.; Gould, E. Structural plasticity and hippocampal function. Annu. Rev. Psychol. 2010, 61, 111–140. [Google Scholar] [CrossRef] [PubMed]
- Brunner, L.; Nick, H.P.; Cumin, F.; Chiesi, M.; Baum, H.P.; Whitebread, S.; Stricker-Krongrad, A.; Levens, N. Leptin is a physiologically important regulator of food intake. Int. J. Obes. Relat. Metab. Disord. 1997, 21, 1152–1160. [Google Scholar] [CrossRef] [PubMed]
- Considine, R.V.; Sinha, M.K.; Heiman, M.L.; Kriauciunas, A.; Stephens, T.W.; Nyce, M.R.; Ohannesian, J.P.; Marco, C.C.; McKee, L.J.; Bauer, T.L.; et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N. Engl. J. Med. 1996, 334, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Licinio, J.; Mantzoros, C.; Negrao, A.B.; Cizza, G.; Wong, M.L.; Bongiorno, P.B.; Chrousos, G.P.; Karp, B.; Allen, C.; Flier, J.S.; et al. Human leptin levels are pulsatile and inversely related to pituitary-adrenal function. Nat. Med. 1997, 3, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Sinha, M.K.; Ohannesian, J.P.; Heiman, M.L.; Kriauciunas, A.; Stephens, T.W.; Magosin, S.; Marco, C.; Caro, J.F. Nocturnal rise of leptin in lean, obese, and non-insulin-dependent diabetes mellitus subjects. J. Clin. Investig. 1996, 97, 1344–1347. [Google Scholar] [CrossRef] [PubMed]
- Boden, G.; Chen, X.; Mozzoli, M.; Ryan, I. Effect of fasting on serum leptin in normal human subjects. J. Clin. Endocrinol. Metab. 1996, 81, 3419–3423. [Google Scholar] [PubMed]
- Chan, J.L.; Heist, K.; DePaoli, A.M.; Veldhuis, J.D.; Mantzoros, C.S. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J. Clin. Investig. 2003, 111, 1409–1421. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.L.; Mantzoros, C.S. Role of leptin in energy-deprivation states: Normal human physiology and clinical implications for hypothalamic amenorrhoea and anorexia nervosa. Lancet 2005, 366, 74–85. [Google Scholar] [CrossRef]
- Myers, M.G.; Cowley, M.A.; Munzberg, H. Mechanisms of leptin action and leptin resistance. Annu. Rev. Physiol. 2008, 70, 537–556. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Hanefeld, M.; Haffner, S.M.; Fusch, C.; Schwanebeck, U.; Kohler, C.; Fucker, K.; Julius, U. Insulin-resistant patients with type 2 diabetes mellitus have higher serum leptin levels independently of body fat mass. Acta Diabetol. 2002, 39, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.B.; Zhou, J.; Redmann, S.M., Jr.; Smagin, G.N.; Smith, S.R.; Rodgers, E.; Zachwieja, J.J. A leptin dose-response study in obese (ob/ob) and lean (+/?) mice. Endocrinology 1998, 139, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Berglund, E.D.; Vianna, C.R.; Donato, J., Jr.; Kim, M.H.; Chuang, J.C.; Lee, C.E.; Lauzon, D.A.; Lin, P.; Brule, L.J.; Scott, M.M.; et al. Direct leptin action on POMC neurons regulates glucose homeostasis and hepatic insulin sensitivity in mice. J. Clin. Investig. 2012, 122, 1000–1009. [Google Scholar] [CrossRef] [PubMed]
- Cummings, B.P.; Bettaieb, A.; Graham, J.L.; Stanhope, K.L.; Dill, R.; Morton, G.J.; Haj, F.G.; Havel, P.J. Subcutaneous administration of leptin normalizes fasting plasma glucose in obese type 2 diabetic UCD-T2DM rats. Proc. Natl. Acad. Sci. USA 2011, 108, 14670–14675. [Google Scholar] [CrossRef] [PubMed]
- Morton, G.J.; Gelling, R.W.; Niswender, K.D.; Morrison, C.D.; Rhodes, C.J.; Schwartz, M.W. Leptin regulates insulin sensitivity via phosphatidylinositol-3-OH kinase signaling in mediobasal hypothalamic neurons. Cell Metab. 2005, 2, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Coppari, R.; Ichinose, M.; Lee, C.E.; Pullen, A.E.; Kenny, C.D.; McGovern, R.A.; Tang, V.; Liu, S.M.; Ludwig, T.; Chua, S.C., Jr.; et al. The hypothalamic arcuate nucleus: A key site for mediating leptin’s effects on glucose homeostasis and locomotor activity. Cell Metab. 2005, 1, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Enriori, P.J.; Evans, A.E.; Sinnayah, P.; Jobst, E.E.; Tonelli-Lemos, L.; Billes, S.K.; Glavas, M.M.; Grayson, B.E.; Perello, M.; Nillni, E.A.; et al. Diet-induced obesity causes severe but reversible leptin resistance in arcuate melanocortin neurons. Cell Metab. 2007, 5, 181–194. [Google Scholar] [CrossRef] [PubMed]
- El-Haschimi, K.; Pierroz, D.D.; Hileman, S.M.; Bjorbaek, C.; Flier, J.S. Two defects contribute to hypothalamic leptin resistance in mice with diet-induced obesity. J. Clin. Investig. 2000, 105, 1827–1832. [Google Scholar] [CrossRef] [PubMed]
- Munzberg, H.; Flier, J.S.; Bjorbaek, C. Region-specific leptin resistance within the hypothalamus of diet-induced obese mice. Endocrinology 2004, 145, 4880–4889. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Thomas, T.C.; Storlien, L.H.; Huang, X.F. Development of high fat diet-induced obesity and leptin resistance in C57Bl/6J mice. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Mittendorfer, B.; Horowitz, J.F.; DePaoli, A.M.; McCamish, M.A.; Patterson, B.W.; Klein, S. Recombinant human leptin treatment does not improve insulin action in obese subjects with type 2 diabetes. Diabetes 2011, 60, 1474–1477. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Matarese, G.; Brennan, A.M.; Chamberland, J.P.; Liu, X.; Fiorenza, C.G.; Mylvaganam, G.H.; Abanni, L.; Carbone, F.; Williams, C.J.; et al. Efficacy of metreleptin in obese patients with type 2 diabetes: Cellular and molecular pathways underlying leptin tolerance. Diabetes 2011, 60, 1647–1656. [Google Scholar] [CrossRef] [PubMed]
- Funahashi, H.; Yada, T.; Suzuki, R.; Shioda, S. Distribution, function, and properties of leptin receptors in the brain. Int. Rev. Cytol. 2003, 224, 1–27. [Google Scholar] [PubMed]
- Zhou, Y.; Rui, L. Leptin signaling and leptin resistance. Front. Med. 2013, 7, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.D. Leptin signaling in brain: A link between nutrition and cognition? Biochim. Biophys. Acta 2009, 1792, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Farr, O.M.; Tsoukas, M.A.; Mantzoros, C.S. Leptin and the brain: Influences on brain development, cognitive functioning and psychiatric disorders. Metabolism 2015, 64, 114–130. [Google Scholar] [CrossRef] [PubMed]
- Coll, A.P.; Farooqi, I.S.; O’Rahilly, S. The hormonal control of food intake. Cell 2007, 129, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Ahima, R.S.; Prabakaran, D.; Mantzoros, C.; Qu, D.; Lowell, B.; Maratos-Flier, E.; Flier, J.S. Role of leptin in the neuroendocrine response to fasting. Nature 1996, 382, 250–252. [Google Scholar] [CrossRef] [PubMed]
- Cristino, L.; Busetto, G.; Imperatore, R.; Ferrandino, I.; Palomba, L.; Silvestri, C.; Petrosino, S.; Orlando, P.; Bentivoglio, M.; Mackie, K.; et al. Obesity-driven synaptic remodeling affects endocannabinoid control of orexinergic neurons. Proc. Natl. Acad. Sci. USA 2013, 110, E2229–E2238. [Google Scholar] [CrossRef] [PubMed]
- Cason, A.M.; Smith, R.J.; Tahsili-Fahadan, P.; Moorman, D.E.; Sartor, G.C.; Aston-Jones, G. Role of orexin/hypocretin in reward-seeking and addiction: Implications for obesity. Physiol. Behav. 2010, 100, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Hay-Schmidt, A.; Helboe, L.; Larsen, P.J. Leptin receptor immunoreactivity is present in ascending serotonergic and catecholaminergic neurons of the rat. Neuroendocrinology 2001, 73, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Figlewicz, D.P.; Evans, S.B.; Murphy, J.; Hoen, M.; Baskin, D.G. Expression of receptors for insulin and leptin in the ventral tegmental area/substantia nigra (VTA/SN) of the rat. Brain Res. 2003, 964, 107–115. [Google Scholar] [CrossRef]
- Balland, E.; Cowley, M.A. New insights in leptin resistance mechanisms in mice. Front. Neuroendocrinol. 2015, 39, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Hara, J.; Beuckmann, C.T.; Nambu, T.; Willie, J.T.; Chemelli, R.M.; Sinton, C.M.; Sugiyama, F.; Yagami, K.; Goto, K.; Yanagisawa, M.; et al. Genetic ablation of orexin neurons in mice results in narcolepsy, hypophagia, and obesity. Neuron 2001, 30, 345–354. [Google Scholar] [CrossRef]
- Harris, G.C.; Wimmer, M.; Aston-Jones, G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature 2005, 437, 556–559. [Google Scholar] [CrossRef] [PubMed]
- Narita, M.; Nagumo, Y.; Hashimoto, S.; Narita, M.; Khotib, J.; Miyatake, M.; Sakurai, T.; Yanagisawa, M.; Nakamachi, T.; Shioda, S.; et al. Direct involvement of orexinergic systems in the activation of the mesolimbic dopamine pathway and related behaviors induced by morphine. J. Neurosci. 2006, 26, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Bello, N.T.; Pang, Z.P. Presynaptic regulation of leptin in a defined lateral hypothalamus-ventral tegmental area neurocircuitry depends on energy state. J. Neurosci. 2017, 37, 11854–11866. [Google Scholar] [CrossRef] [PubMed]
- Salamone, J.D.; Correa, M.; Mingote, S.M.; Weber, S.M. Beyond the reward hypothesis: Alternative functions of nucleus accumbens dopamine. Curr. Opin. Pharmacol. 2005, 5, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Kelley, A.E.; Baldo, B.A.; Pratt, W.E.; Will, M.J. Corticostriatal-hypothalamic circuitry and food motivation: Integration of energy, action and reward. Physiol. Behav. 2005, 86, 773–795. [Google Scholar] [CrossRef] [PubMed]
- Schultz, W. Behavioral dopamine signals. Trends Neurosci. 2007, 30, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Coccurello, R.; Maccarrone, M. Hedonic eating and the “Delicious circle”: From lipid-derived mediators to brain dopamine and back. Front. Neurosci. 2018, 12, 271. [Google Scholar] [CrossRef] [PubMed]
- Leinninger, G.M.; Jo, Y.H.; Leshan, R.L.; Louis, G.W.; Yang, H.; Barrera, J.G.; Wilson, H.; Opland, D.M.; Faouzi, M.A.; Gong, Y.; et al. Leptin acts via leptin receptor-expressing lateral hypothalamic neurons to modulate the mesolimbic dopamine system and suppress feeding. Cell Metab. 2009, 10, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.F.; Choi, D.L.; Schurdak, J.D.; Fitzgerald, M.F.; Clegg, D.J.; Lipton, J.W.; Figlewicz, D.P.; Benoit, S.C. Leptin regulates energy balance and motivation through action at distinct neural circuits. Biol. Psychiatry 2011, 69, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Fulton, S.; Pissios, P.; Manchon, R.P.; Stiles, L.; Frank, L.; Pothos, E.N.; Maratos-Flier, E.; Flier, J.S. Leptin regulation of the mesoaccumbens dopamine pathway. Neuron 2006, 51, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Korotkova, T.M.; Brown, R.E.; Sergeeva, O.A.; Ponomarenko, A.A.; Haas, H.L. Effects of arousal- and feeding-related neuropeptides on dopaminergic and GABAergic neurons in the ventral tegmental area of the rat. Eur. J. Neurosci. 2006, 23, 2677–2685. [Google Scholar] [CrossRef] [PubMed]
- Krugel, U.; Schraft, T.; Kittner, H.; Kiess, W.; Illes, P. Basal and feeding-evoked dopamine release in the rat nucleus accumbens is depressed by leptin. Eur. J. Pharmacol. 2003, 482, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Morton, G.J.; Blevins, J.E.; Kim, F.; Matsen, M.; Figlewicz, D.P. The action of leptin in the ventral tegmental area to decrease food intake is dependent on Jak-2 signaling. Am. J. Physiol. Endocrinol. Metab. 2009, 297, E202–E210. [Google Scholar] [CrossRef] [PubMed]
- Scarpace, P.J.; Matheny, M.; Kirichenko, N.; Gao, Y.X.; Tumer, N.; Zhang, Y. Leptin overexpression in VTA trans-activates the hypothalamus whereas prolonged leptin action in either region cross-desensitizes. Neuropharmacology 2013, 65, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Hommel, J.D.; Trinko, R.; Sears, R.M.; Georgescu, D.; Liu, Z.W.; Gao, X.B.; Thurmon, J.J.; Marinelli, M.; DiLeone, R.J. Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron 2006, 51, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Jiang, C.; Liu, P.; Wang, F.; Ma, L. Mesolimbic leptin signaling negatively regulates cocaine-conditioned reward. Transl. Psychiatry 2016, 6, e972. [Google Scholar] [CrossRef] [PubMed]
- Haass-Koffler, C.L.; Aoun, E.G.; Swift, R.M.; de la Monte, S.M.; Kenna, G.A.; Leggio, L. Leptin levels are reduced by intravenous ghrelin administration and correlated with cue-induced alcohol craving. Transl. Psychiatry 2015, 5, e646. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Bocchio Chiavetto, L.; Bignotti, S.; Battisa Tura, G.; Pioli, R.; Boin, F.; Kenis, G.; Bosmans, E.; de Jongh, R.; Lin, A.; et al. Effects of atypical antipsychotics on the inflammatory response system in schizophrenic patients resistant to treatment with typical neuroleptics. Eur. Neuropsychopharmacol. 2000, 10, 119–124. [Google Scholar] [CrossRef]
- Coccurello, R.; Moles, A. Potential mechanisms of atypical antipsychotic-induced metabolic derangement: Clues for understanding obesity and novel drug design. Pharmacol. Ther. 2010, 127, 210–251. [Google Scholar] [CrossRef] [PubMed]
- Sapra, M.; Lawson, D.; Iranmanesh, A.; Varma, A. Adiposity-independent hypoadiponectinemia as a potential marker of insulin resistance and inflammation in schizophrenia patients treated with second generation antipsychotics. Schizophr. Res. 2016, 174, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Flowers, S.A.; Evans, S.J.; Ward, K.M.; McInnis, M.G.; Ellingrod, V.L. Interaction between atypical antipsychotics and the gut microbiome in a bipolar disease cohort. Pharmacotherapy 2017, 37, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Huang, X.F.; Shao, R.; Chen, C.; Deng, C. Molecular mechanisms of antipsychotic drug-induced diabetes. Front. Neurosci. 2017, 11, 643. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Bansal, Y.; Medhi, B.; Kuhad, A. Antipsychotics-induced metabolic alterations: Recounting the mechanistic insights, therapeutic targets and pharmacological alternatives. Eur. J. Pharmacol. 2019, 844, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhuang, X. Atypical antipsychotics-induced metabolic syndrome and nonalcoholic fatty liver disease: A critical review. Neuropsychiatr. Dis. Treat. 2019, 15, 2087–2099. [Google Scholar] [CrossRef] [PubMed]
- Kraus, T.; Haack, M.; Schuld, A.; Hinze-Selch, D.; Kühn, M.; Uhr, M.; Pollmächer, T. Body weight and leptin plasma levels during treatment with antipsychotic drugs. Am. J. Psychiatry 1999, 156, 312–314. [Google Scholar] [PubMed]
- McIntyre, R.S.; Mancini, D.A.; Basile, V.S.; Srinivasan, J.; Kennedy, S.H. Antipsychotic-induced weight gain: Bipolar disorder and leptin. J. Clin. Psychopharmacol. 2003, 23, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Popovic, V.; Doknic, M.; Maric, N.; Pekic, S.; Damjanovic, A.; Miljic, D.; Popovic, S.; Miljic, N.; Djurovic, M.; Jasovic-Gasic, M.; et al. Changes in neuroendocrine and metabolic hormones induced by atypical antipsychotics in normal-weight patients with schizophrenia. Neuroendocrinology 2007, 85, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Potvin, S.; Zhornitsky, S.; Stip, E. Antipsychotic-induced changes in blood levels of leptin in schizophrenia: A meta-analysis. Can. J. Psychiatry 2015, 60 (Suppl. 2), S26–S34. [Google Scholar]
- Ota, M.; Mori, K.; Nakashima, A.; Kaneko, Y.S.; Fujiwara, K.; Itoh, M.; Nagasaka, A.; Ota, A. Peripheral injection of risperidone, an atypical antipsychotic, alters the bodyweight gain of rats. Clin. Exp. Pharmacol. Physiol. 2002, 29, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Albaugh, V.L.; Henry, C.R.; Bello, N.T.; Hajnal, A.; Lynch, S.L.; Halle, B.; Lynch, C.J. Hormonal and metabolic effects of olanzapine and clozapine related to body weight in rodents. Obesity 2006, 14, 36–51. [Google Scholar] [CrossRef] [PubMed]
- Minet-Ringuet, J.; Even, P.C.; Goubern, M.; Tome, D.; de Beaurepaire, R. Long term treatment with olanzapine mixed with the food in male rats induces body fat deposition with no increase in body weight and no thermogenic alteration. Appetite 2006, 46, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Minet-Ringuet, J.; Even, P.C.; Lacroix, M.; Tome, D.; de Beaurepaire, R. A model for antipsychotic-induced obesity in the male rat. Psychopharmacology 2006, 187, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.C.; Wyler, S.C.; Wan, R.; Castorena, C.M.; Ahmed, N.; Mathew, D.; Lee, S.; Liu, C.; Elmquist, J.K. The atypical antipsychotic olanzapine causes weight gain by targeting serotonin receptor, 2C. J. Clin. Investig. 2017, 127, 3402–3406. [Google Scholar] [CrossRef] [PubMed]
- Kusumi, I.; Boku, S.; Takahashi, Y. Psychopharmacology of atypical antipsychotic drugs: From the receptor binding profile to neuroprotection and neurogenesis. Psychiatry Clin. Neurosci. 2015, 69, 243–258. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.Y. What’s atypical about atypical antipsychotic drugs? Curr. Opin. Pharmacol. 2004, 4, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Basile, V.S.; Masellis, M.; McIntyre, R.S.; Meltzer, H.Y.; Lieberman, J.A.; Kennedy, J.L. Genetic dissection of atypical antipsychotic-induced weight gain: Novel preliminary data on the pharmacogenetic puzzle. J. Clin. Psychiatry 2001, 62 (Suppl. 23), 45–66. [Google Scholar] [PubMed]
- Starrenburg, F.C.; Bogers, J.P. How can antipsychotics cause Diabetes Mellitus? Insights based on receptor-binding profiles, humoral factors and transporter proteins. Eur. Psychiatry 2009, 24, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Gettys, T.W.; Harkness, P.J.; Watson, P.M. The beta 3-adrenergic receptor inhibits insulin-stimulated leptin secretion from isolated rat adipocytes. Endocrinology 1996, 137, 4054–4057. [Google Scholar] [CrossRef] [PubMed]
- Munzberg, H. Differential leptin access into the brain—A hierarchical organization of hypothalamic leptin target sites? Physiol. Behav. 2008, 94, 664–669. [Google Scholar] [CrossRef] [PubMed]
- Morash, B.; Li, A.; Murphy, P.R.; Wilkinson, M.; Ur, E. Leptin gene expression in the brain and pituitary gland. Endocrinology 1999, 140, 5995–5998. [Google Scholar] [CrossRef] [PubMed]
- Ur, E.; Wilkinson, D.A.; Morash, B.A.; Wilkinson, M. Leptin immunoreactivity is localized to neurons in rat brain. Neuroendocrinology 2002, 75, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Banks, W.A.; Clever, C.M.; Farrell, C.L. Partial saturation and regional variation in the blood-to-brain transport of leptin in normal weight mice. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E1158–E1165. [Google Scholar] [CrossRef] [PubMed]
- Van Doorn, C.; Macht, V.A.; Grillo, C.A.; Reagan, L.P. Leptin resistance and hippocampal behavioral deficits. Physiol. Behav. 2017, 176, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Stranahan, A.M.; Arumugam, T.V.; Cutler, R.G.; Lee, K.; Egan, J.M.; Mattson, M.P. Diabetes impairs hippocampal function through glucocorticoid-mediated effects on new and mature neurons. Nat. Neurosci. 2008, 11, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Dhar, M.; Zhu, M.; Impey, S.; Lambert, T.J.; Bland, T.; Karatsoreos, I.N.; Nakazawa, T.; Appleyard, S.M.; Wayman, G.A. Leptin induces hippocampal synaptogenesis via CREB-regulated microRNA-132 suppression of, p.2.5.0.G.A.P. Mol. Endocrinol. 2014, 28, 1073–1087. [Google Scholar] [CrossRef] [PubMed]
- Li, X.L.; Aou, S.; Oomura, Y.; Hori, N.; Fukunaga, K.; Hori, T. Impairment of long-term potentiation and spatial memory in leptin receptor-deficient rodents. Neuroscience 2002, 113, 607–615. [Google Scholar] [CrossRef]
- Gerges, N.Z.; Aleisa, A.M.; Alkadhi, K.A. Impaired long-term potentiation in obese zucker rats: Possible involvement of presynaptic mechanism. Neuroscience 2003, 120, 535–539. [Google Scholar] [CrossRef]
- Guo, M.; Lu, Y.; Garza, J.C.; Li, Y.; Chua, S.C.; Zhang, W.; Lu, B.; Lu, X.Y. Forebrain glutamatergic neurons mediate leptin action on depression-like behaviors and synaptic depression. Transl. Psychiatry 2012, 2, e83. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.E.; Lowe, C.; Pretz, D.; Steger, J.; Williams, L.M.; Tups, A. High-fat diet induces leptin resistance in leptin-deficient mice. J. Neuroendocrinol. 2014, 26, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Chandrasekera, P.C.; Pippin, J.J. Leptin- and leptin receptor-deficient rodent models: Relevance for human type 2 diabetes. Curr. Diabetes Rev. 2014, 10, 131–145. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, D.; MacDonald, N.; Mizielinska, S.; Connolly, C.N.; Irving, A.J.; Harvey, J. Leptin promotes rapid dynamic changes in hippocampal dendritic morphology. Mol. Cell. Neurosci. 2007, 35, 559–572. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Garza, J.C.; Bronner, J.; Kim, C.S.; Zhang, W.; Lu, X.Y. Acute administration of leptin produces anxiolytic-like effects: A comparison with fluoxetine. Psychopharmacology 2010, 207, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Farr, S.A.; Banks, W.A.; Morley, J.E. Effects of leptin on memory processing. Peptides 2006, 27, 1420–1425. [Google Scholar] [CrossRef] [PubMed]
- Kanoski, S.E.; Hayes, M.R.; Greenwald, H.S.; Fortin, S.M.; Gianessi, C.A.; Gilbert, J.R.; Grill, H.J. Hippocampal leptin signaling reduces food intake and modulates food-related memory processing. Neuropsychopharmacology 2011, 36, 1859–1870. [Google Scholar] [CrossRef] [PubMed]
- Suarez, A.N.; Noble, E.E.; Kanoski, S.E. Regulation of memory function by feeding-relevant biological systems: following the breadcrumbs to the hippocampus. Front. Mol. Neurosci. 2019, 12, 101. [Google Scholar] [CrossRef] [PubMed]
- Bliss, T.V.; Collingridge, G.L. A synaptic model of memory: Long-term potentiation in the hippocampus. Nature 1993, 361, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Wayner, M.J.; Armstrong, D.L.; Phelix, C.F.; Oomura, Y. Orexin-A (Hypocretin-1) and leptin enhance LTP in the dentate gyrus of rats in vivo. Peptides 2004, 25, 991–996. [Google Scholar] [CrossRef] [PubMed]
- Malenka, R.C. Postsynaptic factors control the duration of synaptic enhancement in area CA1 of the hippocampus. Neuron 1991, 6, 53–60. [Google Scholar] [CrossRef]
- Greco, S.J.; Bryan, K.J.; Sarkar, S.; Zhu, X.; Smith, M.A.; Ashford, J.W.; Johnston, J.M.; Tezapsidis, N.; Casadesus, G. Leptin reduces pathology and improves memory in a transgenic mouse model of Alzheimer’s disease. J. Alzheimers Dis. 2010, 19, 1155–1167. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.Q.; Zhang, J.; Hao, M.; Yang, J.; Han, Y.F.; Liu, X.J.; Shi, H.; Wu, M.N.; Liu, Q.S.; Qi, J.S. Leptin attenuates the detrimental effects of beta-amyloid on spatial memory and hippocampal later-phase long term potentiation in rats. Horm. Behav. 2015, 73, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, Y.; Liu, J.; Yin, F. Geniposide attenuates the level of Aβ1-42 via enhancing leptin signaling in cellular and APP/PS1 transgenic mice. Arch. Pharmacal Res. 2017, 40, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Tanida, M.; Kasahara, R.; Sobue, K.; Suzuki, K. Leptin inhibits amyloid beta-protein fibrillogenesis by decreasing GM1 gangliosides on the neuronal cell surface through PI3K/Akt/mTOR pathway. J. Neurochem. 2014, 131, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Chandran, M.; Phillips, S.A.; Ciaraldi, T.; Henry, R.R. Adiponectin: More than just another fat cell hormone? Diabetes Care 2003, 26, 2442–2450. [Google Scholar] [CrossRef] [PubMed]
- Kawano, J.; Arora, R. The role of adiponectin in obesity, diabetes, and cardiovascular disease. J. Cardiometab. Syndr. 2009, 4, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, T.; Kamon, J.; Ito, Y.; Tsuchida, A.; Yokomizo, T.; Kita, S.; Sugiyama, T.; Miyagishi, M.; Hara, K.; Tsunoda, M.; et al. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 2003, 423, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Arita, Y.; Kihara, S.; Ouchi, N.; Takahashi, M.; Maeda, K.; Miyagawa, J.; Hotta, K.; Shimomura, I.; Nakamura, T.; Miyaoka, K.; et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem. Biophys. Res. Commun. 1999, 257, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Hotta, K.; Funahashi, T.; Arita, Y.; Takahashi, M.; Matsuda, M.; Okamoto, Y.; Iwahashi, H.; Kuriyama, H.; Ouchi, N.; Maeda, K.; et al. Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Guenther, M.; James, R.; Marks, J.; Zhao, S.; Szabo, A.; Kidambi, S. Adiposity distribution influences circulating adiponectin levels. Transl. Res. 2014, 164, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; van de Wall, E.; Laplante, M.; Azzara, A.; Trujillo, M.E.; Hofmann, S.M.; Schraw, T.; Durand, J.L.; Li, H.; Li, G.; et al. Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J. Clin. Investig. 2007, 117, 2621–2637. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Ricchiuti, V.; Lian, B.Q.; Yao, T.M.; Coutinho, P.; Romero, J.R.; Li, J.; Williams, G.H.; Adler, G.K. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation 2008, 117, 2253–2261. [Google Scholar] [CrossRef] [PubMed]
- Saleh, S.; El-Maraghy, N.; Reda, E.; Barakat, W. Modulation of diabetes and dyslipidemia in diabetic insulin-resistant rats by mangiferin: Role of adiponectin and TNF-alpha. An. Acad. Bras. Cienc. 2014, 86, 1935–1948. [Google Scholar] [CrossRef] [PubMed]
- Croze, M.L.; Geloen, A.; Soulage, C.O. Abnormalities in myo-inositol metabolism associated with type 2 diabetes in mice fed a high-fat diet: Benefits of a dietary myo-inositol supplementation. Br. J. Nutr. 2015, 113, 1862–1875. [Google Scholar] [CrossRef] [PubMed]
- Holmes, R.M.; Yi, Z.; De Filippis, E.; Berria, R.; Shahani, S.; Sathyanarayana, P.; Sherman, V.; Fujiwara, K.; Meyer, C.; Christ-Roberts, C.; et al. Increased abundance of the adaptor protein containing pleckstrin homology domain, phosphotyrosine binding domain and leucine zipper motif (APPL1) in patients with obesity and type 2 diabetes: Evidence for altered adiponectin signalling. Diabetologia 2011, 54, 2122–2131. [Google Scholar] [CrossRef] [PubMed]
- Felder, T.K.; Hahne, P.; Soyal, S.M.; Miller, K.; Hoffinger, H.; Oberkofler, H.; Krempler, F.; Patsch, W. Hepatic adiponectin receptors (ADIPOR) 1 and 2 mRNA and their relation to insulin resistance in obese humans. Int. J. Obes. 2010, 34, 846–851. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Okamoto, Y.; Folco, E.J.; Minami, M.; Wara, A.K.; Feinberg, M.W.; Sukhova, G.K.; Colvin, R.A.; Kihara, S.; Funahashi, T.; Luster, A.D.; et al. Adiponectin inhibits the production of CXC receptor 3 chemokine ligands in macrophages and reduces T-lymphocyte recruitment in atherogenesis. Circ. Res. 2008, 102, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.S.; Jeng, C.Y.; Wu, T.J.; Tanaka, S.; Funahashi, T.; Matsuzawa, Y.; Wang, J.P.; Chen, C.L.; Tai, T.Y.; Chuang, L.M. Synthetic peroxisome proliferator-activated receptor-gamma agonist, rosiglitazone, increases plasma levels of adiponectin in type 2 diabetic patients. Diabetes Care 2002, 25, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Fry, M.; Smith, P.M.; Hoyda, T.D.; Duncan, M.; Ahima, R.S.; Sharkey, K.A.; Ferguson, A.V. Area postrema neurons are modulated by the adipocyte hormone adiponectin. J. Neurosci. 2006, 26, 9695–9702. [Google Scholar] [CrossRef] [PubMed]
- Hoyda, T.D.; Fry, M.; Ahima, R.S.; Ferguson, A.V. Adiponectin selectively inhibits oxytocin neurons of the paraventricular nucleus of the hypothalamus. J. Physiol. 2007, 585, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Neumeier, M.; Weigert, J.; Buettner, R.; Wanninger, J.; Schaffler, A.; Muller, A.M.; Killian, S.; Sauerbruch, S.; Schlachetzki, F.; Steinbrecher, A.; et al. Detection of adiponectin in cerebrospinal fluid in humans. Am. J. Physiol. Endocrinol. Metab. 2007, 293, E965–E969. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Pacheco, F.; Martinez-Fuentes, A.J.; Tovar, S.; Pinilla, L.; Tena-Sempere, M.; Dieguez, C.; Castano, J.P.; Malagon, M.M. Regulation of pituitary cell function by adiponectin. Endocrinology 2007, 148, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Thundyil, J.; Tang, S.C.; Okun, E.; Shah, K.; Karamyan, V.T.; Li, Y.I.; Woodruff, T.M.; Taylor, S.M.; Jo, D.G.; Mattson, M.P.; et al. Evidence that adiponectin receptor 1 activation exacerbates ischemic neuronal death. Exp. Transl. Stroke Med. 2010, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Repunte-Canonigo, V.; Berton, F.; Cottone, P.; Reifel-Miller, A.; Roberts, A.J.; Morales, M.; Francesconi, W.; Sanna, P.P. A potential role for adiponectin receptor 2 (AdipoR2) in the regulation of alcohol intake. Brain Res. 2010, 1339, 11–17. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, D.; Guo, M.; Zhang, W.; Lu, X.Y. Adiponectin stimulates proliferation of adult hippocampal neural stem/progenitor cells through activation of p38 mitogen-activated protein kinase (p38MAPK)/glycogen synthase kinase 3beta (GSK-3beta)/beta-catenin signaling cascade. J. Biol. Chem. 2011, 286, 44913–44920. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Guo, M.; Zhang, D.; Cheng, S.Y.; Liu, M.; Ding, J.; Scherer, P.E.; Liu, F.; Lu, X.Y. Adiponectin is critical in determining susceptibility to depressive behaviors and has antidepressant-like activity. Proc. Natl. Acad. Sci. USA 2012, 109, 12248–12253. [Google Scholar] [CrossRef] [PubMed]
- Varhelyi, Z.P.; Kalman, J.; Olah, Z.; Ivitz, E.V.; Fodor, E.K.; Santha, M.; Datki, Z.L.; Pakaski, M. Adiponectin receptors are less sensitive to stress in a transgenic mouse model of Alzheimer’s disease. Front. Neurosci. 2017, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.E.; Lowe, C.; Legler, K.; Benzler, J.; Boucsein, A.; Bottiger, G.; Grattan, D.R.; Williams, L.M.; Tups, A. Central adiponectin acutely improves glucose tolerance in male mice. Endocrinology 2014, 155, 1806–1816. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Cheng, K.K. Hypothalamic AMPK as a mediator of hormonal regulation of energy balance. Int. J. Mol. Sci. 2018, 19, 3552. [Google Scholar] [CrossRef] [PubMed]
- Kubota, N.; Yano, W.; Kubota, T.; Yamauchi, T.; Itoh, S.; Kumagai, H.; Kozono, H.; Takamoto, I.; Okamoto, S.; Shiuchi, T.; et al. Adiponectin stimulates AMP-activated protein kinase in the hypothalamus and increases food intake. Cell Metab. 2007, 6, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Gao, Y.; Yao, T.; Huang, Y.; He, Z.; Kong, X.; Yu, K.J.; Wang, R.T.; Guo, H.; Yan, J.; et al. Adiponectin potentiates the acute effects of leptin in arcuate Pomc neurons. Mol. Metab. 2016, 5, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.; Takahashi, N.; Hileman, S.M.; Patel, H.R.; Berg, A.H.; Pajvani, U.B.; Scherer, P.E.; Ahima, R.S. Adiponectin acts in the brain to decrease body weight. Nat. Med. 2004, 10, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Suyama, S.; Maekawa, F.; Maejima, Y.; Kubota, N.; Kadowaki, T.; Yada, T. Glucose level determines excitatory or inhibitory effects of adiponectin on arcuate POMC neuron activity and feeding. Sci. Rep. 2016, 6, 30796. [Google Scholar] [CrossRef] [PubMed]
- Suyama, S.; Lei, W.; Kubota, N.; Kadowaki, T.; Yada, T. Adiponectin at physiological level glucose-independently enhances inhibitory postsynaptic current onto NPY neurons in the hypothalamic arcuate nucleus. Neuropeptides 2017, 65, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hanssens, L.; van Winkel, R.; Wampers, M.; Van Eyck, D.; Scheen, A.; Reginster, J.Y.; Collette, J.; Peuskens, J.; De Hert, M. A cross-sectional evaluation of adiponectin plasma levels in patients with schizophrenia and schizoaffective disorder. Schizophr. Res. 2008, 106, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, F.; Crocamo, C.; Clerici, M.; Carra, G. Second-generation antipsychotics and adiponectin levels in schizophrenia: A comparative meta-analysis. Eur. Neuropsychopharmacol. 2015, 25, 1767–1774. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Schreurs, V.; Sweers, K.; Van Eyck, D.; Hanssens, L.; Sinko, S.; Wampers, M.; Scheen, A.; Peuskens, J.; van Winkel, R. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr. Res. 2008, 101, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.M.; Chen, T.T.; Yang, W.S.; Chi, Y.C.; Lin, C.C.; Liou, Y.J.; Wang, Y.C.; Su, T.P.; Chou, P.; Chen, J.Y. Association of adiponectin and metabolic syndrome among patients taking atypical antipsychotics for schizophrenia: A cohort study. Schizophr. Res. 2009, 111, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Weston-Green, K.; Huang, X.F.; Deng, C. Alterations to melanocortinergic, GABAergic and cannabinoid neurotransmission associated with olanzapine-induced weight gain. PLoS ONE 2012, 7, e33548. [Google Scholar] [CrossRef] [PubMed]
- Murashita, M.; Inoue, T.; Kusumi, I.; Nakagawa, S.; Itoh, K.; Tanaka, T.; Izumi, T.; Hosoda, H.; Kangawa, K.; Koyama, T. Glucose and lipid metabolism of long-term risperidone monotherapy in patients with schizophrenia. Psychiatry Clin. Neurosci. 2007, 61, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Wampers, M.; Hanssens, L.; van Winkel, R.; Heald, A.; Collette, J.; Peuskens, J.; Reginster, J.Y.; Scheen, A.; De Hert, M. Differential effects of olanzapine and risperidone on plasma adiponectin levels over time: Results from a 3-month prospective open-label study. Eur. Neuropsychopharmacol. 2012, 22, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, F.; Lax, A.; Crocamo, C.; Clerici, M.; Carra, G. Plasma adiponectin levels in schizophrenia and role of second-generation antipsychotics: A meta-analysis. Psychoneuroendocrinology 2015, 56, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Lei, Y.; You, J.; Li, C.; Sun, L.; Garza, J.; Zhang, D.; Guo, M.; Scherer, P.E.; Lodge, D.; et al. Adiponectin modulates ventral tegmental area dopamine neuron activity and anxiety-related behavior through AdipoR1. Mol. Psychiatry 2019, 24, 126–144. [Google Scholar] [CrossRef] [PubMed]
- Nestler, E.J.; Carlezon, W.A., Jr. The mesolimbic dopamine reward circuit in depression. Biol. Psychiatry 2006, 59, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Coque, L.; Mukherjee, S.; Cao, J.L.; Spencer, S.; Marvin, M.; Falcon, E.; Sidor, M.M.; Birnbaum, S.G.; Graham, A.; Neve, R.L.; et al. Specific role of VTA dopamine neuronal firing rates and morphology in the reversal of anxiety-related, but not depression-related behavior in the ClockDelta19 mouse model of mania. Neuropsychopharmacology 2011, 36, 1478–1488. [Google Scholar] [CrossRef] [PubMed]
- Tye, K.M.; Mirzabekov, J.J.; Warden, M.R.; Ferenczi, E.A.; Tsai, H.C.; Finkelstein, J.; Kim, S.Y.; Adhikari, A.; Thompson, K.R.; Andalman, A.S.; et al. Dopamine neurons modulate neural encoding and expression of depression-related behaviour. Nature 2013, 493, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Chaudhury, D.; Walsh, J.J.; Friedman, A.K.; Juarez, B.; Ku, S.M.; Koo, J.W.; Ferguson, D.; Tsai, H.C.; Pomeranz, L.; Christoffel, D.J.; et al. Rapid regulation of depression-related behaviours by control of midbrain dopamine neurons. Nature 2013, 493, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Kahl, K.G.; Schweiger, U.; Correll, C.; Muller, C.; Busch, M.L.; Bauer, M.; Schwarz, P. Depression, anxiety disorders, and metabolic syndrome in a population at risk for type 2 diabetes mellitus. Brain Behav. 2015, 5, e00306. [Google Scholar] [CrossRef] [PubMed]
- Turer, A.T.; Khera, A.; Ayers, C.R.; Turer, C.B.; Grundy, S.M.; Vega, G.L.; Scherer, P.E. Adipose tissue mass and location affect circulating adiponectin levels. Diabetologia 2011, 54, 2515–2524. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, Y.; Kihara, S.; Funahashi, T.; Matsuzawa, Y.; Libby, P. Adiponectin: A key adipocytokine in metabolic syndrome. Clin. Sci. (Lond.) 2006, 110, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Casares, N.; Garcia-Arnes, J.A.; Rioja, J.; Ariza, M.J.; Gutierrez, A.; Alfaro, F.; Nabrozidis, A.; Gonzalez-Alegre, P.; Gonzalez-Santos, P. Alzheimer’s like brain changes correlate with low adiponectin plasma levels in type 2 diabetic patients. J. Diabetes Complicat. 2016, 30, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, A.L.; Diniz, B.S.; Campos, A.C.; Miranda, A.S.; Rocha, N.P.; Talib, L.L.; Gattaz, W.F.; Forlenza, O.V. Decreased levels of circulating adiponectin in mild cognitive impairment and Alzheimer’s disease. Neuromolecular. Med. 2013, 15, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Wang, X.; Lu, X.Y. Adiponectin Exerts Neurotrophic Effects on Dendritic Arborization, Spinogenesis, and Neurogenesis of the Dentate Gyrus of Male Mice. Endocrinology 2016, 157, 2853–2869. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.W.; Abid, N.B.; Jo, M.H.; Jo, M.G.; Yoon, G.H.; Kim, M.O. Suppression of adiponectin receptor 1 promotes memory dysfunction and Alzheimer’s disease-like pathologies. Sci. Rep. 2017, 7, 12435. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, S.; Veyssiere, J.; Gandin, C.; Zsurger, N.; Pietri, M.; Heurteaux, C.; Glaichenhaus, N.; Petit-Paitel, A.; Chabry, J. Neurogenesis-independent antidepressant-like effects of enriched environment is dependent on adiponectin. Psychoneuroendocrinology 2015, 57, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Chabry, J.; Nicolas, S.; Cazareth, J.; Murris, E.; Guyon, A.; Glaichenhaus, N.; Heurteaux, C.; Petit-Paitel, A. Enriched environment decreases microglia and brain macrophages inflammatory phenotypes through adiponectin-dependent mechanisms: Relevance to depressive-like behavior. Brain Behav. Immun. 2015, 50, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Li, C.; Lei, Y.; Xu, S.; Zhao, D.; Lu, X.Y. Role of the adipose PPARgamma-adiponectin axis in susceptibility to stress and depression/anxiety-related behaviors. Mol. Psychiatry 2017, 22, 1056–1068. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, N.; Argueta, J.G.; Masuhiro, Y.; Kagishita, M.; Nonaka, K.; Saito, T.; Hanazawa, S.; Yamashita, Y. Adiponectin inhibits Toll-like receptor family-induced signaling. FEBS Lett. 2005, 579, 6821–6826. [Google Scholar] [CrossRef] [PubMed]
- Mandal, P.; Pratt, B.T.; Barnes, M.; McMullen, M.R.; Nagy, L.E. Molecular mechanism for adiponectin-dependent M2 macrophage polarization: Link between the metabolic and innate immune activity of full-length adiponectin. J. Biol. Chem. 2011, 286, 13460–13469. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.P.; Gan, G.S.; Liu, Y.M.; Xiao, J.S.; Liu, H.X.; Mei, B.; Zhang, J.J. Adiponectin Attenuates Streptozotocin-Induced Tau Hyperphosphorylation and Cognitive Deficits by Rescuing PI3K/Akt/GSK-3beta Pathway. Neurochem. Res. 2018, 43, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Jian, M.; Kwan, J.S.; Bunting, M.; Ng, R.C.; Chan, K.H. Adiponectin suppresses amyloid-beta oligomer (AbetaO)-induced inflammatory response of microglia via AdipoR1-AMPK-NF-kappaB signaling pathway. J. Neuroinflamm. 2019, 16, 110. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Choi, S.M.; Kim, B.C. Adiponectin Regulates the Polarization and Function of Microglia via PPAR-gamma Signaling Under Amyloid beta Toxicity. Front. Cell Neurosci. 2017, 11, 64. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Jo, J.; Song, J. Adiponectin improves long-term potentiation in the 5XFAD mouse brain. Sci. Rep. 2019, 9, 8918. [Google Scholar] [CrossRef] [PubMed]
- Rourke, J.L.; Dranse, H.J.; Sinal, C.J. Towards an integrative approach to understanding the role of chemerin in human health and disease. Obesity Rev. 2013, 14, 245–262. [Google Scholar] [CrossRef] [PubMed]
- Zabel, B.A.; Silverio, A.M.; Butcher, E.C. Chemokine-like receptor 1 expression and chemerin-directed chemotaxis distinguish plasmacytoid from myeloid dendritic cells in human blood. J. Immunol. 2005, 174, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Zabel, B.A.; Nakae, S.; Zuniga, L.; Kim, J.Y.; Ohyama, T.; Alt, C.; Pan, J.; Suto, H.; Soler, D.; Allen, S.J.; et al. Mast cell-expressed orphan receptor CCRL2 binds chemerin and is required for optimal induction of IgE-mediated passive cutaneous anaphylaxis. J. Exp. Med. 2008, 205, 2207–2220. [Google Scholar] [CrossRef] [PubMed]
- Barnea, G.; Strapps, W.; Herrada, G.; Berman, Y.; Ong, J.; Kloss, B.; Axel, R.; Lee, K.J. The genetic design of signaling cascades to record receptor activation. Proc. Natl. Acad. Sci. USA 2008, 105, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Goralski, K.B.; McCarthy, T.C.; Hanniman, E.A.; Zabel, B.A.; Butcher, E.C.; Parlee, S.D.; Muruganandan, S.; Sinal, C.J. Chemerin, a novel adipokine that regulates adipogenesis and adipocyte metabolism. J. Biol. Chem. 2007, 282, 28175–28188. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, S.; Patel, S.; Jacobe, H.; DiSepio, D.; Ghosn, C.; Malhotra, M.; Teng, M.; Duvic, M.; Chandraratna, R.A. Tazarotene-induced gene 2 (TIG2), a novel retinoid-responsive gene in skin. J. Investig. Dermatol. 1997, 109, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Bozaoglu, K.; Curran, J.E.; Stocker, C.J.; Zaibi, M.S.; Segal, D.; Konstantopoulos, N.; Morrison, S.; Carless, M.; Dyer, T.D.; Cole, S.A.; et al. Chemerin, a novel adipokine in the regulation of angiogenesis. J. Clin. Endocrinol. Metab. 2010, 95, 2476–2485. [Google Scholar] [CrossRef] [PubMed]
- Zabel, B.A.; Allen, S.J.; Kulig, P.; Allen, J.A.; Cichy, J.; Handel, T.M.; Butcher, E.C. Chemerin activation by serine proteases of the coagulation, fibrinolytic, and inflammatory cascades. J. Biol. Chem. 2005, 280, 34661–34666. [Google Scholar] [CrossRef] [PubMed]
- Bozaoglu, K.; Bolton, K.; McMillan, J.; Zimmet, P.; Jowett, J.; Collier, G.; Walder, K.; Segal, D. Chemerin is a novel adipokine associated with obesity and metabolic syndrome. Endocrinology 2007, 148, 4687–4694. [Google Scholar] [CrossRef] [PubMed]
- Sell, H.; Laurencikiene, J.; Taube, A.; Eckardt, K.; Cramer, A.; Horrighs, A.; Arner, P.; Eckel, J. Chemerin is a novel adipocyte-derived factor inducing insulin resistance in primary human skeletal muscle cells. Diabetes 2009, 58, 2731–2740. [Google Scholar] [CrossRef] [PubMed]
- Chakaroun, R.; Raschpichler, M.; Kloting, N.; Oberbach, A.; Flehmig, G.; Kern, M.; Schon, M.R.; Shang, E.; Lohmann, T.; Dressler, M.; et al. Effects of weight loss and exercise on chemerin serum concentrations and adipose tissue expression in human obesity. Metabolism 2012, 61, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Wargent, E.T.; Zaibi, M.S.; O’Dowd, J.F.; Cawthorne, M.A.; Wang, S.J.; Arch, J.R.; Stocker, C.J. Evidence from studies in rodents and in isolated adipocytes that agonists of the chemerin receptor CMKLR1 may be beneficial in the treatment of type 2 diabetes. PeerJ 2015, 3, e753. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.C.; Issa, M.; Goralski, K.B.; Sinal, C.J. Chemerin exacerbates glucose intolerance in mouse models of obesity and diabetes. Endocrinology 2010, 151, 1998–2007. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Okimura, Y.; Iguchi, G.; Nishizawa, H.; Yamamoto, M.; Suda, K.; Kitazawa, R.; Fujimoto, W.; Takahashi, K.; Zolotaryov, F.N.; et al. Chemerin regulates beta-cell function in mice. Sci. Rep. 2011, 1, 123. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.C.; Haidl, I.D.; Zuniga, L.A.; Dranse, H.J.; Rourke, J.L.; Zabel, B.A.; Butcher, E.C.; Sinal, C.J. Disruption of the chemokine-like receptor-1 (CMKLR1) gene is associated with reduced adiposity and glucose intolerance. Endocrinology 2012, 153, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, M.; Ren, L.; Xiang, L.; Chen, J.; Li, M.; Xiao, T.; Ren, P.; Xiong, L.; Zhang, J.V. CMKLR1 deficiency influences glucose tolerance and thermogenesis in mice on high fat diet. Biochem. Biophys. Res. Commun. 2016, 473, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Rourke, J.L.; Muruganandan, S.; Dranse, H.J.; McMullen, N.M.; Sinal, C.J. Gpr1 is an active chemerin receptor influencing glucose homeostasis in obese mice. J. Endocrinol. 2014, 222, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Helfer, G.; Ross, A.W.; Thomson, L.M.; Mayer, C.D.; Stoney, P.N.; McCaffery, P.J.; Morgan, P.J. A neuroendocrine role for chemerin in hypothalamic remodelling and photoperiodic control of energy balance. Sci. Rep. 2016, 6, 26830. [Google Scholar] [CrossRef] [PubMed]
- Perumalsamy, S.; Aqilah Mohd Zin, N.A.; Widodo, R.T.; Wan Ahmad, W.A.; Vethakkan, S.; Huri, H.Z. Chemokine Like Receptor-1 (CMKLR-1) Receptor: A Potential Therapeutic Target in Management of Chemerin Induced Type 2 Diabetes Mellitus and Cancer. Curr. Pharm. Des. 2017, 23, 3689–3698. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xu, N.; Ding, Y.; Doycheva, D.M.; Zhang, Y.; Li, Q.; Flores, J.; Haghighiabyaneh, M.; Tang, J.; Zhang, J.H. Chemerin reverses neurological impairments and ameliorates neuronal apoptosis through ChemR23/CAMKK2/AMPK pathway in neonatal hypoxic-ischemic encephalopathy. Cell Death Dis. 2019, 10, 97. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Yu, Y.; Liu, J.; Li, S.; He, H.; Cheng, N.; Ye, R.D. The chemerin receptor CMKLR1 is a functional receptor for amyloid-beta peptide. J. Alzheimers Dis. 2015, 43, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Fu, Y.; Xu, Y.; Weng, S.; Liu, D.; Cui, D.; Yu, S.; Liu, X.; Jiang, K.; Dong, Y. Chronic mild restraint stress rats decreased CMKLR1 expression in distinct brain region. Neurosci. Lett. 2012, 524, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Deyama, S.; Shimoda, K.; Suzuki, H.; Ishikawa, Y.; Ishimura, K.; Fukuda, H.; Hitora-Imamura, N.; Ide, S.; Satoh, M.; Kaneda, K.; et al. Resolvin E1/E2 ameliorate lipopolysaccharide-induced depression-like behaviors via ChemR23. Psychopharmacology 2018, 235, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Li, Q.; Wang, W.; Yu, P.; Pan, H.; Li, P.; Sun, Y.; Zhang, J. Apelin inhibits insulin secretion in pancreatic beta-cells by activation of PI3-kinase-phosphodiesterase 3B. Endocr Res. 2009, 34, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, C.; Valet, P.; Castan-Laurell, I. Apelin and energy metabolism. Front. Physiol. 2015, 6, 115. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Chen, L.; Li, L. Apelin/APJ system: A novel promising therapy target for pathological angiogenesis. Clin. Chim. Acta 2017, 466, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Yamaleyeva, L.M.; Shaltout, H.A.; Varagic, J. Apelin-13 in blood pressure regulation and cardiovascular disease. Curr. Opin. Nephrol. Hypertens. 2016, 25, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Valle, A.; Hoggard, N.; Adams, A.C.; Roca, P.; Speakman, J.R. Chronic central administration of apelin-13 over 10 days increases food intake, body weight, locomotor activity and body temperature in C57BL/6 mice. J. Neuroendocrinol. 2008, 20, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Vinel, C.; Lukjanenko, L.; Batut, A.; Deleruyelle, S.; Pradere, J.P.; Le Gonidec, S.; Dortignac, A.; Geoffre, N.; Pereira, O.; Karaz, S.; et al. The exerkine apelin reverses age-associated sarcopenia. Nat. Med. 2018, 24, 1360–1371. [Google Scholar] [CrossRef] [PubMed]
- Castan-Laurell, I.; Dray, C.; Knauf, C.; Kunduzova, O.; Valet, P. Apelin, a promising target for type 2 diabetes treatment? Trends Endocrinol. Metab. 2012, 23, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Pope, G.R.; Roberts, E.M.; Lolait, S.J.; O’Carroll, A.M. Central and peripheral apelin receptor distribution in the mouse: Species differences with rat. Peptides 2012, 33, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Yue, P.; Jin, H.; Xu, S.; Aillaud, M.; Deng, A.C.; Azuma, J.; Kundu, R.K.; Reaven, G.M.; Quertermous, T.; Tsao, P.S. Apelin decreases lipolysis via G(q), G(i), and AMPK-Dependent Mechanisms. Endocrinology 2011, 152, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Yue, P.; Jin, H.; Aillaud, M.; Deng, A.C.; Azuma, J.; Asagami, T.; Kundu, R.K.; Reaven, G.M.; Quertermous, T.; Tsao, P.S. Apelin is necessary for the maintenance of insulin sensitivity. Am. J. Physiol. Endocrinol. Metab. 2010, 298, E59–E67. [Google Scholar] [CrossRef] [PubMed]
- Dray, C.; Knauf, C.; Daviaud, D.; Waget, A.; Boucher, J.; Buleon, M.; Cani, P.D.; Attane, C.; Guigne, C.; Carpene, C.; et al. Apelin stimulates glucose utilization in normal and obese insulin-resistant mice. Cell Metab. 2008, 8, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Attane, C.; Foussal, C.; Le Gonidec, S.; Benani, A.; Daviaud, D.; Wanecq, E.; Guzman-Ruiz, R.; Dray, C.; Bezaire, V.; Rancoule, C.; et al. Apelin treatment increases complete Fatty Acid oxidation, mitochondrial oxidative capacity, and biogenesis in muscle of insulin-resistant mice. Diabetes 2012, 61, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Than, A.; Cheng, Y.; Foh, L.C.; Leow, M.K.; Lim, S.C.; Chuah, Y.J.; Kang, Y.; Chen, P. Apelin inhibits adipogenesis and lipolysis through distinct molecular pathways. Mol. Cell Endocrinol. 2012, 362, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Sun, F.; Li, W.; Cao, Y.; Wang, C.; Wang, Y.; Liang, D.; Zhang, R.; Zhang, S.; Wang, H.; et al. Apelin stimulates glucose uptake through the PI3K/Akt pathway and improves insulin resistance in 3T3-L1 adipocytes. Mol. Cell Biochem. 2011, 353, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.; Chen, J.; Bai, B.; Xin, Q. Neuroprotection of apelin and its signaling pathway. Peptides 2012, 37, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Xin, Q.; Cheng, B.; Pan, Y.; Liu, H.; Yang, C.; Chen, J.; Bai, B. Neuroprotective effects of apelin-13 on experimental ischemic stroke through suppression of inflammation. Peptides 2015, 63, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Yang, X.; Huang, C.; Gao, Z.; Tang, Y.; Dong, Q. Apelin-13 Protects against Ischemic Blood-Brain Barrier Damage through the Effects of Aquaporin-4. Cerebrovasc. Dis. 2017, 44, 10–25. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Lee, J.; Gu, X.; Wei, L.; Yu, S.P. Intranasal Delivery of Apelin-13 Is Neuroprotective and Promotes Angiogenesis After Ischemic Stroke in Mice. ASN Neuro 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.J.; Zhang, L.; Han, W.C.; Dai, D.K. Apelin-13 attenuates traumatic brain injury-induced damage by suppressing autophagy. Neurochem. Res. 2015, 40, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Xiang, Y.; Qu, X.; Liu, H.; Liu, C.; Li, G.; Han, L.; Qin, X. Apelin-13 Suppresses Neuroinflammation Against Cognitive Deficit in a Streptozotocin-Induced Rat Model of Alzheimer’s Disease Through Activation of BDNF-TrkB Signaling Pathway. Front. Pharmacol. 2019, 10, 395. [Google Scholar] [CrossRef] [PubMed]
- Li, E.; Deng, H.; Wang, B.; Fu, W.; You, Y.; Tian, S. Apelin-13 exerts antidepressant-like and recognition memory improving activities in stressed rats. Eur. Neuropsychopharmacol. 2016, 26, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.Y.; Wang, B.; Fu, W.; Jin, X.; You, Y.; Tian, S.W.; Kuang, X. The Hippocampus is a Critical Site Mediating Antidepressant-like Activity of Apelin-13 in Rats. Neuroscience 2018, 375, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dai, T.T.; Wang, B.; Xiao, Z.Y.; You, Y.; Tian, S.W. Apelin-13 Upregulates BDNF Against Chronic Stress-induced Depression-like Phenotypes by Ameliorating HPA Axis and Hippocampal Glucocorticoid Receptor Dysfunctions. Neuroscience 2018, 390, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Revollo, J.R.; Grimm, A.A.; Imai, S. The NAD biosynthesis pathway mediated by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J. Biol. Chem. 2004, 279, 50754–50763. [Google Scholar] [CrossRef] [PubMed]
- Garten, A.; Schuster, S.; Penke, M.; Gorski, T.; de Giorgis, T.; Kiess, W. Physiological and pathophysiological roles of NAMPT and NAD metabolism. Nat. Rev. Endocrinol. 2015, 11, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, J.; Mills, K.F.; Yoon, M.J.; Imai, S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab. 2011, 14, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Chalkiadaki, A.; Guarente, L. High-fat diet triggers inflammation-induced cleavage of SIRT1 in adipose tissue to promote metabolic dysfunction. Cell Metab. 2012, 16, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Bruno, J.; Easlon, E.; Lin, S.J.; Cheng, H.L.; Alt, F.W.; Guarente, L. Tissue-specific regulation of SIRT1 by calorie restriction. Genes Dev. 2008, 22, 1753–1757. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Ke, S.F.; Zhou, C.C.; Zhang, S.L.; Guan, Y.F.; Xu, T.Y.; Sheng, C.Q.; Wang, P.; Miao, C.Y. Nicotinamide phosphoribosyltransferase is required for the calorie restriction-mediated improvements in oxidative stress, mitochondrial biogenesis, and metabolic adaptation. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Stromsdorfer, K.L.; Yamaguchi, S.; Yoon, M.J.; Moseley, A.C.; Franczyk, M.P.; Kelly, S.C.; Qi, N.; Imai, S.; Yoshino, J. NAMPT-Mediated NAD(+) Biosynthesis in Adipocytes Regulates Adipose Tissue Function and Multi-organ Insulin Sensitivity in Mice. Cell Rep. 2016, 16, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Yoon, M.J.; Yoshida, M.; Johnson, S.; Takikawa, A.; Usui, I.; Tobe, K.; Nakagawa, T.; Yoshino, J.; Imai, S. SIRT1-Mediated eNAMPT Secretion from Adipose Tissue Regulates Hypothalamic NAD+ and Function in Mice. Cell Metab. 2015, 21, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.; Xing, J.; Chen, X.; Stetler, R.A.; Weng, Z.; Gan, Y.; Zhang, F.; Gao, Y.; Chen, J.; Leak, R.K.; et al. Neuronal NAMPT is released after cerebral ischemia and protects against white matter injury. J. Cereb Blood Flow Metab. 2014, 34, 1613–1621. [Google Scholar] [CrossRef] [PubMed]
- Erfani, S.; Khaksari, M.; Oryan, S.; Shamsaei, N.; Aboutaleb, N.; Nikbakht, F. Nampt/PBEF/visfatin exerts neuroprotective effects against ischemia/reperfusion injury via modulation of Bax/Bcl-2 ratio and prevention of caspase-3 activation. J. Mol. Neurosci. 2015, 56, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Guan, Y.F.; Zhou, X.M.; Li, G.Q.; Li, Z.Y.; Zhou, C.C.; Wang, P.; Miao, C.Y. Regenerative Neurogenesis After Ischemic Stroke Promoted by Nicotinamide Phosphoribosyltransferase-Nicotinamide Adenine Dinucleotide Cascade. Stroke 2015, 46, 1966–1974. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Liu, X.Z.; Tian, W.W.; Guan, Y.F.; Wang, P.; Miao, C.Y. Extracellular visfatin has nicotinamide phosphoribosyltransferase enzymatic activity and is neuroprotective against ischemic injury. CNS Neurosci. Ther. 2014, 20, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Ryu, D.; Wu, Y.; Gariani, K.; Wang, X.; Luan, P.; D’Amico, D.; Ropelle, E.R.; Lutolf, M.P.; Aebersold, R.; et al. NAD(+) repletion improves mitochondrial and stem cell function and enhances life span in mice. Science 2016, 352, 1436–1443. [Google Scholar] [CrossRef] [PubMed]
- Fricker, R.A.; Green, E.L.; Jenkins, S.I.; Griffin, S.M. The Influence of Nicotinamide on Health and Disease in the Central Nervous System. Int. J. Tryptophan Res. 2018, 11, 1178646918776658. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hu, X.; Yang, Y.; Takata, T.; Sakurai, T. Nicotinamide mononucleotide protects against beta-amyloid oligomer-induced cognitive impairment and neuronal death. Brain Res. 2016, 1643, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gong, B.; Pan, Y.; Vempati, P.; Zhao, W.; Knable, L.; Ho, L.; Wang, J.; Sastre, M.; Ono, K.; Sauve, A.A.; et al. Nicotinamide riboside restores cognition through an upregulation of proliferator-activated receptor-gamma coactivator 1alpha regulated beta-secretase 1 degradation and mitochondrial gene expression in Alzheimer’s mouse models. Neurobiol. Aging 2013, 34, 1581–1588. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Gerhold, K.; Mayers, J.R.; Wiest, M.M.; Watkins, S.M.; Hotamisligil, G.S. Identification of a lipokine, a lipid hormone linking adipose tissue to systemic metabolism. Cell 2008, 134, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Saunders, A.M.; Strittmatter, W.J.; Schmechel, D.; George-Hyslop, P.H.; Pericak-Vance, M.A.; Joo, S.H.; Rosi, B.L.; Gusella, J.F.; Crapper-MacLachlan, D.R.; Alberts, M.J.; et al. Association of apolipoprotein E allele epsilon 4 with late-onset familial and sporadic Alzheimer’s disease. Neurology 1993, 43, 1467–1472. [Google Scholar] [CrossRef] [PubMed]
- Cutler, R.G.; Kelly, J.; Storie, K.; Pedersen, W.A.; Tammara, A.; Hatanpaa, K.; Troncoso, J.C.; Mattson, M.P. Involvement of oxidative stress-induced abnormalities in ceramide and cholesterol metabolism in brain aging and Alzheimer’s disease. Proc. Natl. Acad. Sci. USA 2004, 101, 2070–2075. [Google Scholar] [CrossRef] [PubMed]
- Lukiw, W.J.; Pappolla, M.; Pelaez, R.P.; Bazan, N.G. Alzheimer’s disease--a dysfunction in cholesterol and lipid metabolism. Cell Mol. Neurobiol. 2005, 25, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Calon, F.; Julien, C.; Winkler, J.W.; Petasis, N.A.; Lukiw, W.J.; Bazan, N.G. Docosahexaenoic acid-derived neuroprotectin D1 induces neuronal survival via secretase- and PPARgamma-mediated mechanisms in Alzheimer’s disease models. PLoS ONE 2011, 6, e15816. [Google Scholar] [CrossRef]
- Sanchez-Mejia, R.O.; Newman, J.W.; Toh, S.; Yu, G.Q.; Zhou, Y.; Halabisky, B.; Cisse, M.; Scearce-Levie, K.; Cheng, I.H.; Gan, L.; et al. Phospholipase A2 reduction ameliorates cognitive deficits in a mouse model of Alzheimer’s disease. Nat. Neurosci. 2008, 11, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Grimm, M.O.; Grimm, H.S.; Patzold, A.J.; Zinser, E.G.; Halonen, R.; Duering, M.; Tschape, J.A.; De Strooper, B.; Muller, U.; Shen, J.; et al. Regulation of cholesterol and sphingomyelin metabolism by amyloid-beta and presenilin. Nat. Cell Biol. 2005, 7, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Furuhashi, N.; Kuromori, Y.; Miyashita, M.; Iwata, F.; Harada, K. Plasma palmitoleic acid content and obesity in children. Am. J. Clin. Nutr. 2005, 82, 747–750. [Google Scholar] [CrossRef] [PubMed]
- Paillard, F.; Catheline, D.; Duff, F.L.; Bouriel, M.; Deugnier, Y.; Pouchard, M.; Daubert, J.C.; Legrand, P. Plasma palmitoleic acid, a product of stearoyl-coA desaturase activity, is an independent marker of triglyceridemia and abdominal adiposity. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Warensjo, E.; Ohrvall, M.; Vessby, B. Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Cao, H.; King, I.B.; Lemaitre, R.N.; Song, X.; Siscovick, D.S.; Hotamisligil, G.S. Circulating palmitoleic acid and risk of metabolic abnormalities and new-onset diabetes. Am. J. Clin. Nutr. 2010, 92, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Ferry, G.; Tellier, E.; Try, A.; Gres, S.; Naime, I.; Simon, M.F.; Rodriguez, M.; Boucher, J.; Tack, I.; Gesta, S.; et al. Autotaxin is released from adipocytes, catalyzes lysophosphatidic acid synthesis, and activates preadipocyte proliferation. Up-regulated expression with adipocyte differentiation and obesity. J. Biol. Chem. 2003, 278, 18162–18169. [Google Scholar] [CrossRef] [PubMed]
- Gesta, S.; Simon, M.F.; Rey, A.; Sibrac, D.; Girard, A.; Lafontan, M.; Valet, P.; Saulnier-Blache, J.S. Secretion of a lysophospholipase D activity by adipocytes: Involvement in lysophosphatidic acid synthesis. J. Lipid Res. 2002, 43, 904–910. [Google Scholar] [PubMed]
- Boucher, J.; Quilliot, D.; Praderes, J.P.; Simon, M.F.; Gres, S.; Guigne, C.; Prevot, D.; Ferry, G.; Boutin, J.A.; Carpene, C.; et al. Potential involvement of adipocyte insulin resistance in obesity-associated up-regulation of adipocyte lysophospholipase D/autotaxin expression. Diabetologia 2005, 48, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Dusaulcy, R.; Rancoule, C.; Gres, S.; Wanecq, E.; Colom, A.; Guigne, C.; van Meeteren, L.A.; Moolenaar, W.H.; Valet, P.; Saulnier-Blache, J.S. Adipose-specific disruption of autotaxin enhances nutritional fattening and reduces plasma lysophosphatidic acid. J. Lipid Res. 2011, 52, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Rancoule, C.; Dusaulcy, R.; Treguer, K.; Gres, S.; Guigne, C.; Quilliot, D.; Valet, P.; Saulnier-Blache, J.S. Depot-specific regulation of autotaxin with obesity in human adipose tissue. J. Physiol. Biochem. 2012, 68, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Rachakonda, V.P.; Reeves, V.L.; Aljammal, J.; Wills, R.C.; Trybula, J.S.; DeLany, J.P.; Kienesberger, P.C.; Kershaw, E.E. Serum autotaxin is independently associated with hepatic steatosis in women with severe obesity. Obesity (Silver Spring) 2015, 23, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Reeves, V.L.; Trybula, J.S.; Wills, R.C.; Goodpaster, B.H.; Dube, J.J.; Kienesberger, P.C.; Kershaw, E.E. Serum Autotaxin/ENPP2 correlates with insulin resistance in older humans with obesity. Obesity (Silver Spring) 2015, 23, 2371–2376. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, K.; Kane, D.A.; Touaibia, M.; Kershaw, E.E.; Pulinilkunnil, T.; Kienesberger, P.C. Autotaxin Is Regulated by Glucose and Insulin in Adipocytes. Endocrinology 2017, 158, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Rancoule, C.; Attane, C.; Gres, S.; Fournel, A.; Dusaulcy, R.; Bertrand, C.; Vinel, C.; Treguer, K.; Prentki, M.; Valet, P.; et al. Lysophosphatidic acid impairs glucose homeostasis and inhibits insulin secretion in high-fat diet obese mice. Diabetologia 2013, 56, 1394–1402. [Google Scholar] [CrossRef] [PubMed]
- Yung, Y.C.; Stoddard, N.C.; Chun, J. LPA receptor signaling: Pharmacology, physiology, and pathophysiology. J. Lipid Res. 2014, 55, 1192–1214. [Google Scholar] [CrossRef] [PubMed]
- Gimenez da Silva-Santi, L.; Masetto Antunes, M.; Mori, M.A.; Biesdorf de Almeida-Souza, C.; Vergilio Visentainer, J.; Carbonera, F.; Rabello Crisma, A.; Nunes Masi, L.; Massao Hirabara, S.; Curi, R.; et al. Brain Fatty Acid Composition and Inflammation in Mice Fed with High-Carbohydrate Diet or High-Fat Diet. Nutrients 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.C.; Park, S.M.; Kim, I.Y.; Sung, H.; Seong, J.K.; Moon, M.H. High-fat diet-induced lipidome perturbations in the cortex, hippocampus, hypothalamus, and olfactory bulb of mice. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2018, 1863, 980–990. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, R.; Gomez-Pinilla, F. ‘Metabolic syndrome’ in the brain: Deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signalling and cognition. J. Physiol. 2012, 590, 2485–2499. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Zhuang, Y.; Gomez-Pinilla, F. High-fat diet transition reduces brain DHA levels associated with altered brain plasticity and behaviour. Sci. Rep. 2012, 2, 431. [Google Scholar] [CrossRef] [PubMed]
- Sato, N.; Morishita, R. The roles of lipid and glucose metabolism in modulation of beta-amyloid, tau, and neurodegeneration in the pathogenesis of Alzheimer disease. Front. Aging Neurosci. 2015, 7, 199. [Google Scholar] [CrossRef] [PubMed]
- Janssen, C.I.; Jansen, D.; Mutsaers, M.P.; Dederen, P.J.; Geenen, B.; Mulder, M.T.; Kiliaan, A.J. The Effect of a High-Fat Diet on Brain Plasticity, Inflammation and Cognition in Female ApoE4-Knockin and ApoE-Knockout Mice. PLoS ONE 2016, 11, e0155307. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.B.; Zhang, Z.; Luo, P.; Wang, S.S.; Peng, Y.; Chu, S.F.; Chen, N.H. Lipid metabolism in Alzheimer’s disease. Brain Res. Bull. 2019, 144, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Del Olmo, N.; Ruiz-Gayo, M. Influence of High-Fat Diets Consumed During the Juvenile Period on Hippocampal Morphology and Function. Front. Cell Neurosci. 2018, 12, 439. [Google Scholar] [CrossRef] [PubMed]
- Carta, G.; Murru, E.; Banni, S.; Manca, C. Palmitic Acid: Physiological Role, Metabolism and Nutritional Implications. Front. Physiol. 2017, 8, 902. [Google Scholar] [CrossRef] [PubMed]
- Strable, M.S.; Ntambi, J.M. Genetic control of de novo lipogenesis: Role in diet-induced obesity. Crit. Rev. Biochem. Mol. Biol. 2010, 45, 199–214. [Google Scholar] [CrossRef] [PubMed]
- Silbernagel, G.; Kovarova, M.; Cegan, A.; Machann, J.; Schick, F.; Lehmann, R.; Haring, H.U.; Stefan, N.; Schleicher, E.; Fritsche, A.; et al. High hepatic SCD1 activity is associated with low liver fat content in healthy subjects under a lipogenic diet. J. Clin. Endocrinol. Metab. 2012, 97, E2288–E2292. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Balu, D.; Melrose, J.; Chan, C. Brain region-specificity of palmitic acid-induced abnormalities associated with Alzheimer’s disease. BMC Res. Notes 2008, 1, 20. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, Y.H.; Lin, C.I.; Liao, H.; Chen, Y.H.; Lin, S.H. Palmitic acid-induced neuron cell cycle G2/M arrest and endoplasmic reticular stress through protein palmitoylation in SH-SY5Y human neuroblastoma cells. Int. J. Mol. Sci. 2014, 15, 20876–20899. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Melrose, J.; Chan, C. Involvement of astroglial ceramide in palmitic acid-induced Alzheimer-like changes in primary neurons. Eur. J. Neurosci. 2007, 26, 2131–2141. [Google Scholar] [CrossRef] [PubMed]
- Frigolet, M.E.; Gutierrez-Aguilar, R. The Role of the Novel Lipokine Palmitoleic Acid in Health and Disease. Adv. Nutr. 2017, 8, 173S–181S. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Li, H.; Xu, H.; Halim, V.; Zhang, W.; Wang, H.; Ong, K.T.; Woo, S.L.; Walzem, R.L.; Mashek, D.G.; et al. Palmitoleate induces hepatic steatosis but suppresses liver inflammatory response in mice. PLoS ONE 2012, 7, e39286. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Bolsoni-Lopes, A.; Festuccia, W.T.; Farias, T.S.; Chimin, P.; Torres-Leal, F.L.; Derogis, P.B.; de Andrade, P.B.; Miyamoto, S.; Lima, F.B.; Curi, R.; et al. Palmitoleic acid (n-7) increases white adipocyte lipolysis and lipase content in a PPARalpha-dependent manner. Am. J. Physiol. Endocrinol. Metab. 2013, 305, E1093–E1102. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, N.; Watson, M.; Sakamoto, K.; Hundal, H.S. Differential effects of palmitate and palmitoleate on insulin action and glucose utilization in rat L6 skeletal muscle cells. Biochem. J. 2006, 399, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Kuda, O.; Stankova, B.; Tvrzicka, E.; Hensler, M.; Jelenik, T.; Rossmeisl, M.; Flachs, P.; Kopecky, J. Prominent role of liver in elevated plasma palmitoleate levels in response to rosiglitazone in mice fed high-fat diet. J. Physiol. Pharmacol. 2009, 60, 135–140. [Google Scholar] [PubMed]
- Furuhashi, M.; Hotamisligil, G.S. Fatty acid-binding proteins: Role in metabolic diseases and potential as drug targets. Nat. Rev. Drug Discov. 2008, 7, 489–503. [Google Scholar] [CrossRef] [PubMed]
- Furuhashi, M.; Ishimura, S.; Ota, H.; Miura, T. Lipid chaperones and metabolic inflammation. Int. J. Inflam. 2011, 2011, 642612. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.C.; Wat, N.M.; Tam, S.C.; Janus, E.D.; Lam, T.H.; Lam, K.S. C-reactive protein predicts the deterioration of glycemia in chinese subjects with impaired glucose tolerance. Diabetes Care 2003, 26, 2323–2328. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.Y.; Xydakis, A.M.; Hoogeveen, R.C.; Jones, P.H.; Smith, E.O.; Nelson, K.W.; Ballantyne, C.M. Multiplexed analysis of biomarkers related to obesity and the metabolic syndrome in human plasma, using the Luminex-100 system. Clin. Chem. 2005, 51, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Degawa-Yamauchi, M.; Bovenkerk, J.E.; Juliar, B.E.; Watson, W.; Kerr, K.; Jones, R.; Zhu, Q.; Considine, R.V. Serum resistin (FIZZ3) protein is increased in obese humans. J. Clin. Endocrinol. Metab. 2003, 88, 5452–5455. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.; Wang, Y.; Xu, J.Y.; Stejskal, D.; Tam, S.; Zhang, J.; Wat, N.M.; Wong, W.K.; Lam, K.S. Adipocyte fatty acid-binding protein is a plasma biomarker closely associated with obesity and metabolic syndrome. Clin. Chem. 2006, 52, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Kralisch, S.; Ebert, T.; Lossner, U.; Jessnitzer, B.; Stumvoll, M.; Fasshauer, M. Adipocyte fatty acid-binding protein is released from adipocytes by a non-conventional mechanism. Int J. Obes. (Lond.) 2014, 38, 1251–1254. [Google Scholar] [CrossRef] [PubMed]
- Erbay, E.; Babaev, V.R.; Mayers, J.R.; Makowski, L.; Charles, K.N.; Snitow, M.E.; Fazio, S.; Wiest, M.M.; Watkins, S.M.; Linton, M.F.; et al. Reducing endoplasmic reticulum stress through a macrophage lipid chaperone alleviates atherosclerosis. Nat. Med. 2009, 15, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Coleman, S.L.; Park, Y.K.; Lee, J.Y. Unsaturated fatty acids repress the expression of adipocyte fatty acid binding protein via the modulation of histone deacetylation in RAW 264.7 macrophages. Eur. J. Nutr. 2011, 50, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Uysal, K.T.; Scheja, L.; Wiesbrock, S.M.; Bonner-Weir, S.; Hotamisligil, G.S. Improved glucose and lipid metabolism in genetically obese mice lacking aP2. Endocrinology 2000, 141, 3388–3396. [Google Scholar] [CrossRef] [PubMed]
- Maeda, K.; Cao, H.; Kono, K.; Gorgun, C.Z.; Furuhashi, M.; Uysal, K.T.; Cao, Q.; Atsumi, G.; Malone, H.; Krishnan, B.; et al. Adipocyte/macrophage fatty acid binding proteins control integrated metabolic responses in obesity and diabetes. Cell Metab. 2005, 1, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Maeda, K.; Gorgun, C.Z.; Kim, H.J.; Park, S.Y.; Shulman, G.I.; Kim, J.K.; Hotamisligil, G.S. Regulation of metabolic responses by adipocyte/macrophage Fatty Acid-binding proteins in leptin-deficient mice. Diabetes 2006, 55, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Dobrzyn, P.; Jazurek, M.; Dobrzyn, A. Stearoyl-CoA desaturase and insulin signaling--what is the molecular switch? Biochim. Biophys. Acta 2010, 1797, 1189–1194. [Google Scholar] [CrossRef] [PubMed]
- Astarita, G.; Jung, K.M.; Vasilevko, V.; Dipatrizio, N.V.; Martin, S.K.; Cribbs, D.H.; Head, E.; Cotman, C.W.; Piomelli, D. Elevated stearoyl-CoA desaturase in brains of patients with Alzheimer’s disease. PLoS ONE 2011, 6, e24777. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.; Miyazaki, M.; Socci, N.D.; Hagge-Greenberg, A.; Liedtke, W.; Soukas, A.A.; Sharma, R.; Hudgins, L.C.; Ntambi, J.M.; Friedman, J.M. Role for stearoyl-CoA desaturase-1 in leptin-mediated weight loss. Science 2002, 297, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Corpeleijn, E.; Feskens, E.J.; Jansen, E.H.; Mensink, M.; Saris, W.H.; de Bruin, T.W.; Blaak, E.E. Improvements in glucose tolerance and insulin sensitivity after lifestyle intervention are related to changes in serum fatty acid profile and desaturase activities: The SLIM study. Diabetologia 2006, 49, 2392–2401. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Warensjo, E.; Ingelsson, E.; Lundmark, P.; Lannfelt, L.; Syvanen, A.C.; Vessby, B.; Riserus, U. Polymorphisms in the SCD1 gene: Associations with body fat distribution and insulin sensitivity. Obesity (Silver Spring) 2007, 15, 1732–1740. [Google Scholar] [CrossRef] [PubMed]
- Warensjo, E.; Riserus, U.; Vessby, B. Fatty acid composition of serum lipids predicts the development of the metabolic syndrome in men. Diabetologia 2005, 48, 1999–2005. [Google Scholar] [CrossRef] [PubMed]
- Mar-Heyming, R.; Miyazaki, M.; Weissglas-Volkov, D.; Kolaitis, N.A.; Sadaat, N.; Plaisier, C.; Pajukanta, P.; Cantor, R.M.; de Bruin, T.W.; Ntambi, J.M.; et al. Association of stearoyl-CoA desaturase 1 activity with familial combined hyperlipidemia. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 1193–1199. [Google Scholar] [CrossRef] [PubMed]
- Snigdha, S.; Astarita, G.; Piomelli, D.; Cotman, C.W. Effects of diet and behavioral enrichment on free fatty acids in the aged canine brain. Neuroscience 2012, 202, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Srodulski, S.; Sharma, S.; Bachstetter, A.B.; Brelsfoard, J.M.; Pascual, C.; Xie, X.S.; Saatman, K.E.; Van Eldik, L.J.; Despa, F. Neuroinflammation and neurologic deficits in diabetes linked to brain accumulation of amylin. Mol. Neurodegener. 2014, 9, 30. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.A.; Spencer, S.J. Obesity and neuroinflammation: A pathway to cognitive impairment. Brain Behav. Immun. 2014, 42, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Posey, K.A.; Clegg, D.J.; Printz, R.L.; Byun, J.; Morton, G.J.; Vivekanandan-Giri, A.; Pennathur, S.; Baskin, D.G.; Heinecke, J.W.; Woods, S.C.; et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1003–E1012. [Google Scholar] [CrossRef] [PubMed]
- Pistell, P.J.; Morrison, C.D.; Gupta, S.; Knight, A.G.; Keller, J.N.; Ingram, D.K.; Bruce-Keller, A.J. Cognitive impairment following high fat diet consumption is associated with brain inflammation. J. Neuroimmunol. 2010, 219, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Brandon, J.A.; Kraemer, M.; Vandra, J.; Halder, S.; Ubele, M.; Morris, A.J.; Smyth, S.S. Adipose-derived autotaxin regulates inflammation and steatosis associated with diet-induced obesity. PLoS ONE 2019, 14, e0208099. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Natarajan, V. Lysophosphatidic acid (LPA) and its receptors: Role in airway inflammation and remodeling. Biochim. Biophys. Acta 2013, 1831, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ramakrishnan, D.P.; Ren, B. Regulation of angiogenesis by phospholipid lysophosphatidic acid. Front. Biosci. (Landmark Ed.) 2013, 18, 852–861. [Google Scholar] [PubMed]
- Estivill-Torrus, G.; Llebrez-Zayas, P.; Matas-Rico, E.; Santin, L.; Pedraza, C.; De Diego, I.; Del Arco, I.; Fernandez-Llebrez, P.; Chun, J.; De Fonseca, F.R. Absence of LPA1 signaling results in defective cortical development. Cereb. Cortex 2008, 18, 938–950. [Google Scholar] [CrossRef] [PubMed]
- Matas-Rico, E.; Garcia-Diaz, B.; Llebrez-Zayas, P.; Lopez-Barroso, D.; Santin, L.; Pedraza, C.; Smith-Fernandez, A.; Fernandez-Llebrez, P.; Tellez, T.; Redondo, M.; et al. Deletion of lysophosphatidic acid receptor LPA1 reduces neurogenesis in the mouse dentate gyrus. Mol. Cell Neurosci. 2008, 39, 342–355. [Google Scholar] [CrossRef] [PubMed]
- Dubin, A.E.; Herr, D.R.; Chun, J. Diversity of lysophosphatidic acid receptor-mediated intracellular calcium signaling in early cortical neurogenesis. J. Neurosci. 2010, 30, 7300–7309. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, N.; Shano, S.; Moriyama, R.; Chun, J. Lysophosphatidic acid stimulates neuronal differentiation of cortical neuroblasts through the LPA1-G(i/o) pathway. Neurochem. Int. 2007, 50, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Furuta, D.; Yamane, M.; Tsujiuchi, T.; Moriyama, R.; Fukushima, N. Lysophosphatidic acid induces neurite branch formation through LPA3. Mol. Cell Neurosci. 2012, 50, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Pilpel, Y.; Segal, M. The role of LPA1 in formation of synapses among cultured hippocampal neurons. J. Neurochem. 2006, 97, 1379–1392. [Google Scholar] [CrossRef] [PubMed]
- Goldin, M.; Segal, M. Protein kinase C and ERK involvement in dendritic spine plasticity in cultured rodent hippocampal neurons. Eur. J. Neurosci. 2003, 17, 2529–2539. [Google Scholar] [CrossRef] [PubMed]
- Pilpel, Y.; Segal, M. Activation of PKC induces rapid morphological plasticity in dendrites of hippocampal neurons via Rac and Rho-dependent mechanisms. Eur. J. Neurosci. 2004, 19, 3151–3164. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.M.; Reavill, C.; Brown, G.; Brown, J.T.; Cluderay, J.E.; Crook, B.; Davies, C.H.; Dawson, L.A.; Grau, E.; Heidbreder, C.; et al. LPA1 receptor-deficient mice have phenotypic changes observed in psychiatric disease. Mol. Cell Neurosci. 2003, 24, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.; Winter, P.; Shilliam, C.S.; Hughes, Z.A.; Langmead, C.; Maycox, P.R.; Dawson, L.A. Neurochemical changes in LPA1 receptor deficient mice--a putative model of schizophrenia. Neurochem. Res. 2005, 30, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Castilla-Ortega, E.; Sanchez-Lopez, J.; Hoyo-Becerra, C.; Matas-Rico, E.; Zambrana-Infantes, E.; Chun, J.; De Fonseca, F.R.; Pedraza, C.; Estivill-Torrus, G.; Santin, L.J. Exploratory, anxiety and spatial memory impairments are dissociated in mice lacking the LPA1 receptor. Neurobiol. Learn. Mem. 2010, 94, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Santin, L.J.; Bilbao, A.; Pedraza, C.; Matas-Rico, E.; Lopez-Barroso, D.; Castilla-Ortega, E.; Sanchez-Lopez, J.; Riquelme, R.; Varela-Nieto, I.; de la Villa, P.; et al. Behavioral phenotype of maLPA1-null mice: Increased anxiety-like behavior and spatial memory deficits. Genes Brain Behav. 2009, 8, 772–784. [Google Scholar] [CrossRef] [PubMed]
- Shano, S.; Moriyama, R.; Chun, J.; Fukushima, N. Lysophosphatidic acid stimulates astrocyte proliferation through LPA1. Neurochem. Int. 2008, 52, 216–220. [Google Scholar] [CrossRef] [PubMed]
- TC, E.S.; Dezonne, R.S.; Rehen, S.K.; Gomes, F.C. Astrocytes treated by lysophosphatidic acid induce axonal outgrowth of cortical progenitors through extracellular matrix protein and epidermal growth factor signaling pathway. J. Neurochem. 2011, 119, 113–123. [Google Scholar] [CrossRef]
- Schilling, T.; Repp, H.; Richter, H.; Koschinski, A.; Heinemann, U.; Dreyer, F.; Eder, C. Lysophospholipids induce membrane hyperpolarization in microglia by activation of IKCa1 Ca(2+)-dependent K(+) channels. Neuroscience 2002, 109, 827–835. [Google Scholar] [CrossRef]
- Schilling, T.; Stock, C.; Schwab, A.; Eder, C. Functional importance of Ca2+-activated K+ channels for lysophosphatidic acid-induced microglial migration. Eur. J. Neurosci. 2004, 19, 1469–1474. [Google Scholar] [CrossRef] [PubMed]
- Awada, R.; Rondeau, P.; Gres, S.; Saulnier-Blache, J.S.; Lefebvre d’Hellencourt, C.; Bourdon, E. Autotaxin protects microglial cells against oxidative stress. Free Radic. Biol. Med. 2012, 52, 516–526. [Google Scholar] [CrossRef] [PubMed]
- Awada, R.; Saulnier-Blache, J.S.; Gres, S.; Bourdon, E.; Rondeau, P.; Parimisetty, A.; Orihuela, R.; Harry, G.J.; d’Hellencourt, C.L. Autotaxin downregulates LPS-induced microglia activation and pro-inflammatory cytokines production. J. Cell Biochem. 2014, 115, 2123–2132. [Google Scholar] [CrossRef] [PubMed]
- Moller, T.; Musante, D.B.; Ransom, B.R. Lysophosphatidic acid-induced calcium signals in cultured rat oligodendrocytes. Neuroreport 1999, 10, 2929–2932. [Google Scholar] [CrossRef] [PubMed]
- Nogaroli, L.; Yuelling, L.M.; Dennis, J.; Gorse, K.; Payne, S.G.; Fuss, B. Lysophosphatidic acid can support the formation of membranous structures and an increase in MBP mRNA levels in differentiating oligodendrocytes. Neurochem. Res. 2009, 34, 182–193. [Google Scholar] [CrossRef] [PubMed]
- Castanon, N.; Luheshi, G.; Laye, S. Role of neuroinflammation in the emotional and cognitive alterations displayed by animal models of obesity. Front. Neurosci. 2015, 9, 229. [Google Scholar] [CrossRef] [PubMed]
- McLimans, K.E.; Willette, A.A.; Alzheimer’s Disease Neuroimaging, I. Autotaxin is Related to Metabolic Dysfunction and Predicts Alzheimer’s Disease Outcomes. J. Alzheimers Dis. 2017, 56, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Dong, Y.; Cui, M.Z.; Xu, X. Lysophosphatidic acid induces increased BACE1 expression and Abeta formation. Biochim. Biophys. Acta 2013, 1832, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Kinouchi, T.; Sorimachi, H.; Maruyama, K.; Mizuno, K.; Ohno, S.; Ishiura, S.; Suzuki, K. Conventional protein kinase C (PKC)-alpha and novel PKC epsilon, but not -delta, increase the secretion of an N-terminal fragment of Alzheimer’s disease amyloid precursor protein from PKC cDNA transfected 3Y1 fibroblasts. FEBS Lett. 1995, 364, 203–206. [Google Scholar] [PubMed]
- Jolly-Tornetta, C.; Wolf, B.A. Regulation of amyloid precursor protein (APP) secretion by protein kinase calpha in human ntera 2 neurons (NT2N). Biochemistry 2000, 39, 7428–7435. [Google Scholar] [CrossRef] [PubMed]
- Rossner, S.; Mendla, K.; Schliebs, R.; Bigl, V. Protein kinase Calpha and beta1 isoforms are regulators of alpha-secretory proteolytic processing of amyloid precursor protein in vivo. Eur J. Neurosci. 2001, 13, 1644–1648. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.; Wang, D.; Lin, Y.H.; McMahon, T.; Koo, E.H.; Messing, R.O. Protein kinase C epsilon suppresses Abeta production and promotes activation of alpha-secretase. Biochem. Biophys. Res. Commun. 2001, 285, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Blois, J.T.; Mataraza, J.M.; Mecklenbrauker, I.; Tarakhovsky, A.; Chiles, T.C. B cell receptor-induced cAMP-response element-binding protein activation in B lymphocytes requires novel protein kinase Cdelta. J. Biol. Chem. 2004, 279, 30123–30132. [Google Scholar] [CrossRef] [PubMed]
- Sayas, C.L.; Moreno-Flores, M.T.; Avila, J.; Wandosell, F. The neurite retraction induced by lysophosphatidic acid increases Alzheimer’s disease-like Tau phosphorylation. J. Biol. Chem. 1999, 274, 37046–37052. [Google Scholar] [CrossRef] [PubMed]
- Sayas, C.L.; Avila, J.; Wandosell, F. Regulation of neuronal cytoskeleton by lysophosphatidic acid: Role of GSK-3. Biochim. Biophys. Acta 2002, 1582, 144–153. [Google Scholar] [CrossRef]
- Stranahan, A.M. Models and mechanisms for hippocampal dysfunction in obesity and diabetes. Neuroscience 2015, 309, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, X.; Lin, H.; Fu, X.; Lin, W.; Li, M.; Zeng, X.; Gao, Q. Metabolic syndrome and stroke: A meta-analysis of prospective cohort studies. J. Clin. Neurosci. 2017, 40, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, D.A.; Halliwell, B. Oxidative stress, dysfunctional glucose metabolism and Alzheimer disease. Nat. Rev. Neurosci. 2019, 20, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Pousti, F.; Ahmadi, R.; Mirahmadi, F.; Hosseinmardi, N.; Rohampour, K. Adiponectin modulates synaptic plasticity in hippocampal dentate gyrus. Neurosci. Lett. 2018, 662, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Forny-Germano, L.; De Felice, F.G.; Vieira, M. The Role of Leptin and Adiponectin in Obesity-Associated Cognitive Decline and Alzheimer’s Disease. Front. Neurosci. 2018, 12, 1027. [Google Scholar] [CrossRef] [PubMed]
- Irving, A.J.; Harvey, J. Leptin regulation of hippocampal synaptic function in health and disease. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014, 369, 20130155. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.N.; Liu, X.L. Functions of adiponectin signaling in regulating neural plasticity and its application as the therapeutic target to neurological and psychiatric diseases. Rev. Neurosci. 2019, 30, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Ghavami, S.; Shojaei, S.; Yeganeh, B.; Ande, S.R.; Jangamreddy, J.R.; Mehrpour, M.; Christoffersson, J.; Chaabane, W.; Moghadam, A.R.; Kashani, H.H.; et al. Autophagy and apoptosis dysfunction in neurodegenerative disorders. Prog. Neurobiol. 2014, 112, 24–49. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Nutma, E.; van der Valk, P.; Amor, S. Inflammation in CNS neurodegenerative diseases. Immunology 2018, 154, 204–219. [Google Scholar] [CrossRef] [PubMed]
- Radak, D.; Katsiki, N.; Resanovic, I.; Jovanovic, A.; Sudar-Milovanovic, E.; Zafirovic, S.; Mousad, S.A.; Isenovic, E.R. Apoptosis and Acute Brain Ischemia in Ischemic Stroke. Curr. Vasc. Pharmacol. 2017, 15, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Jayaraj, R.L.; Azimullah, S.; Beiram, R.; Jalal, F.Y.; Rosenberg, G.A. Neuroinflammation: Friend and foe for ischemic stroke. J. Neuroinflamm. 2019, 16, 142. [Google Scholar] [CrossRef] [PubMed]
- Parimisetty, A.; Dorsemans, A.C.; Awada, R.; Ravanan, P.; Diotel, N.; Lefebvre d’Hellencourt, C. Secret talk between adipose tissue and central nervous system via secreted factors-an emerging frontier in the neurodegenerative research. J. Neuroinflamm. 2016, 13, 67. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).