The Role of Exosomal MicroRNAs in the Tumor Microenvironment of Breast Cancer
Abstract
1. Introduction
1.1. Breast Cancer
1.2. Tumor Microenvironment (TME)
1.3. Exosomes
1.4. MicroRNAs
2. The Role of miRNAs in Exosomes in the Intercellular Crosstalk
2.1. Exosomes from Cancer Cells Can Provide MicroRNAs to Modify the Stromal Cells in the Tumor Microenvironment for Their Own Advantage (Table 2)
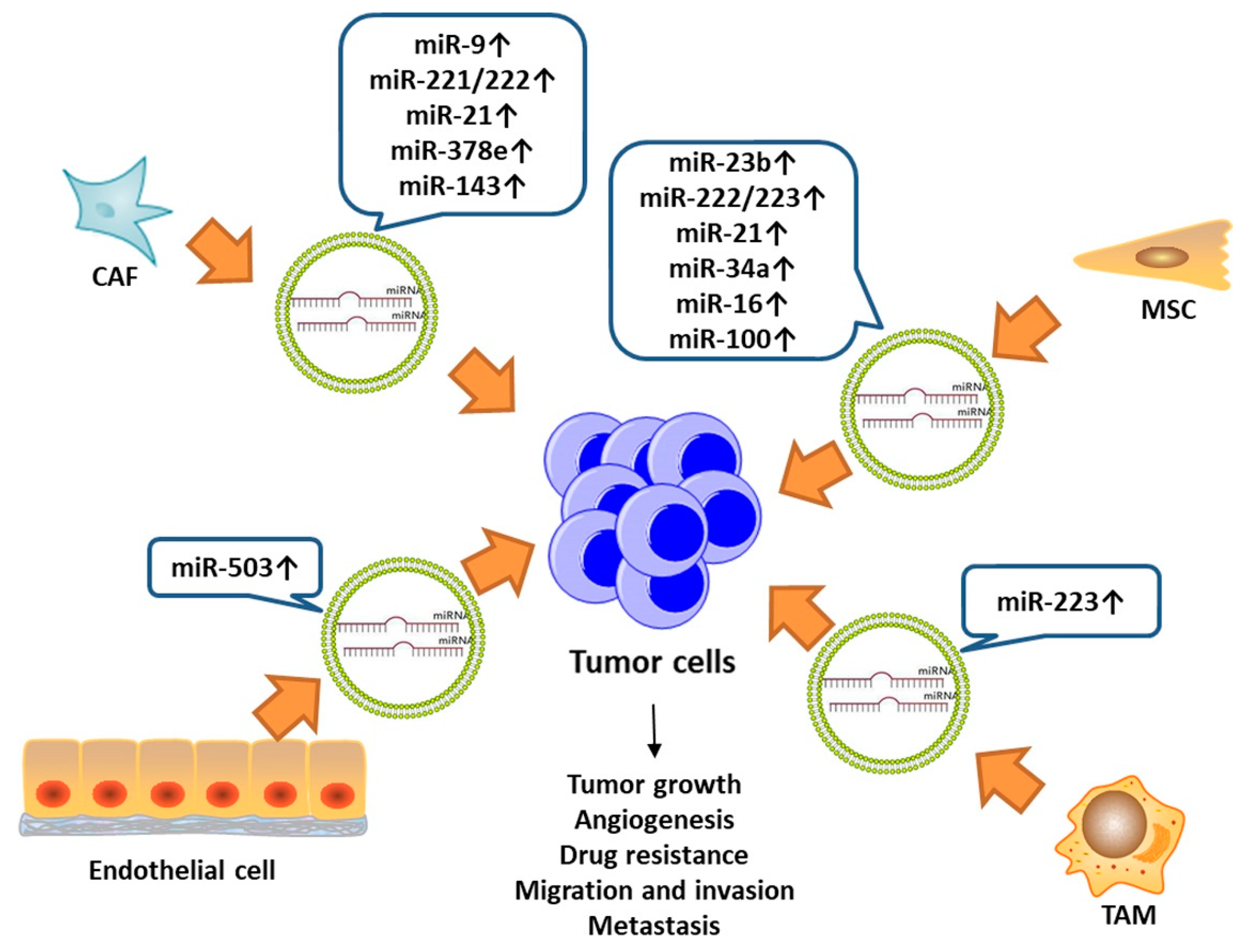
2.2. Exosomes from Stromal Cells Can Transfer miRNAs to Cancer Cells and Contribute to Cancer Progression (Table 3)
2.3. Circulating MicroRNAs in Exosomes Imply Their Potential Biomarker Value
3. Therapeutic Method Targeting at the Exosomal microRNAs
4. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Cancer Genome Atlas, N. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- DeSantis, C.E.; Ma, J.; Goding Sauer, A.; Newman, L.A.; Jemal, A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J. Clin. 2017, 67, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Aleskandarany, M.A.; Vandenberghe, M.E.; Marchio, C.; Ellis, I.O.; Sapino, A.; Rakha, E.A. Tumour Heterogeneity of Breast Cancer: From Morphology to Personalised Medicine. Pathobiology 2018, 85, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Burstein, H.J.; P Winer, E.; Gnant, M.; Dubsky, P.; Loibl, S.; Colleoni, M.; Regan, M.M.; Piccart-Gebhart, M.; Senn, H.J.; et al. De-escalating and escalating treatments for early-stage breast cancer: The St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer. Ann. Oncol. 2017, 28, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.S.; Winer, E.P.; Goldhirsch, A.; Gelber, R.D.; Gnant, M.; Piccart-Gebhart, M.; Thurlimann, B.; Senn, H.J.; Panel, M. Tailoring therapies—Improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer. Ann. Oncol. 2015, 26, 1533–1546. [Google Scholar] [CrossRef] [PubMed]
- Kurozumi, S.; Yamaguchi, Y.; Kurosumi, M.; Ohira, M.; Matsumoto, H.; Horiguchi, J. Recent trends in microRNA research into breast cancer with particular focus on the associations between microRNAs and intrinsic subtypes. J. Hum. Genet. 2017, 62, 15–24. [Google Scholar] [CrossRef]
- Elston, C.W.; Ellis, I.O.; Pinder, S.E. Pathological prognostic factors in breast cancer. Crit. Rev.Oncol. Hematol. 1999, 31, 209–223. [Google Scholar] [CrossRef]
- Langley, R.R.; Fidler, I.J. The seed and soil hypothesis revisited—The role of tumor-stroma interactions in metastasis to different organs. Int. J. Cancer 2011, 128, 2527–2535. [Google Scholar] [CrossRef]
- Ribatti, D.; Mangialardi, G.; Vacca, A. Stephen Paget and the ‘seed and soil’ theory of metastatic dissemination. Clin. Exp. Med. 2006, 6, 145–149. [Google Scholar] [CrossRef]
- Paget, S.J.T.L. The distribution of secondary growths in cancer of the breast. Lancet 1889, 133, 571–573. [Google Scholar] [CrossRef]
- Soysal, S.D.; Tzankov, A.; Muenst, S.E. Role of the Tumor Microenvironment in Breast Cancer. Pathobiology 2015, 82, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.I.; Katsura, A.; Matsuyama, H.; Miyazono, K. MicroRNA regulons in tumor microenvironment. Oncogene 2015, 34, 3085–3094. [Google Scholar] [CrossRef] [PubMed]
- Hui, L.; Chen, Y. Tumor microenvironment: Sanctuary of the devil. Cancer Lett. 2015, 368, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, R.; Zeisberg, M. Fibroblasts in cancer. Nat. Rev. Cancer 2006, 6, 392–401. [Google Scholar] [CrossRef]
- Kalluri, R. The biology and function of fibroblasts in cancer. Nat. Rev. Cancer 2016, 16, 582–598. [Google Scholar] [CrossRef]
- Liao, Z.; Tan, Z.W.; Zhu, P.; Tan, N.S. Cancer-associated fibroblasts in tumor microenvironment—Accomplices in tumor malignancy. Cell. Immunol. 2018. [Google Scholar] [CrossRef]
- Shiga, K.; Hara, M.; Nagasaki, T.; Sato, T.; Takahashi, H.; Takeyama, H. Cancer-Associated Fibroblasts: Their Characteristics and Their Roles in Tumor Growth. Cancers 2015, 7, 2443–2458. [Google Scholar] [CrossRef]
- Weber, C.E.; Kothari, A.N.; Wai, P.Y.; Li, N.Y.; Driver, J.; Zapf, M.A.; Franzen, C.A.; Gupta, G.N.; Osipo, C.; Zlobin, A.; et al. Osteopontin mediates an MZF1-TGF-beta1-dependent transformation of mesenchymal stem cells into cancer-associated fibroblasts in breast cancer. Oncogene 2015, 34, 4821–4833. [Google Scholar] [CrossRef]
- McDonald, L.T.; LaRue, A.C. Hematopoietic stem cell derived carcinoma-associated fibroblasts: A novel origin. Int. J. Clin. Exp. Pathol. 2012, 5, 863. [Google Scholar]
- Orimo, A.; Gupta, P.B.; Sgroi, D.C.; Arenzana-Seisdedos, F.; Delaunay, T.; Naeem, R.; Carey, V.J.; Richardson, A.L.; Weinberg, R.A. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell 2005, 121, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Nagasaki, T.; Hara, M.; Nakanishi, H.; Takahashi, H.; Sato, M.; Takeyama, H. Interleukin-6 released by colon cancer-associated fibroblasts is critical for tumour angiogenesis: Anti-interleukin-6 receptor antibody suppressed angiogenesis and inhibited tumour-stroma interaction. Br. J. Cancer 2014, 110, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Giulianelli, S.; Cerliani, J.P.; Lamb, C.A.; Fabris, V.T.; Bottino, M.C.; Gorostiaga, M.A.; Novaro, V.; Gongora, A.; Baldi, A.; Molinolo, A.; et al. Carcinoma-associated fibroblasts activate progesterone receptors and induce hormone independent mammary tumor growth: A role for the FGF-2/FGFR-2 axis. Int. J. Cancer 2008, 123, 2518–2531. [Google Scholar] [CrossRef] [PubMed]
- Radisky, E.S.; Radisky, D.C. Stromal induction of breast cancer: Inflammation and invasion. Rev. Endocr. Metab. Disord. 2007, 8, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Kohlhapp, F.J.; Mitra, A.K.; Lengyel, E.; Peter, M.E. MicroRNAs as mediators and communicators between cancer cells and the tumor microenvironment. Oncogene 2015, 34, 5857–5868. [Google Scholar] [CrossRef] [PubMed]
- Balkwill, F.R.; Capasso, M.; Hagemann, T. The tumor microenvironment at a glance. J. Cell Sci. 2012, 125, 5591–5596. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Marchesi, F.; Malesci, A.; Laghi, L.; Allavena, P. Tumour-associated macrophages as treatment targets in oncology. Nat. Rev. Clin. Oncol. 2017, 14, 399–416. [Google Scholar] [CrossRef] [PubMed]
- Noy, R.; Pollard, J.W. Tumor-associated macrophages: From mechanisms to therapy. Immunity 2014, 41, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.B.; Yeh, E.S.; Soloff, A.C. Tumor-associated macrophages: Unwitting accomplices in breast cancer malignancy. NPJ Breast Cancer 2016, 2. [Google Scholar] [CrossRef]
- Lim, B.; Woodward, W.A.; Wang, X.; Reuben, J.M.; Ueno, N.T. Inflammatory breast cancer biology: The tumour microenvironment is key. Nat. Rev. Cancer 2018, 18, 485–499. [Google Scholar] [CrossRef]
- Green, T.M.; Alpaugh, M.L.; Barsky, S.H.; Rappa, G.; Lorico, A. Breast Cancer-Derived Extracellular Vesicles: Characterization and Contribution to the Metastatic Phenotype. BioMed Res. Int. 2015, 2015, 634865. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Yu, F.; Ding, H.; Wang, Y.; Li, P.; Wang, K. Emerging Function and Clinical Values of Exosomal MicroRNAs in Cancer. Mol. Ther. Nucleic. Acids 2019, 16, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Sempere, L.F.; Keto, J.; Fabbri, M. Exosomal MicroRNAs in Breast Cancer towards Diagnostic and Therapeutic Applications. Cancers 2017, 9, 71. [Google Scholar] [CrossRef] [PubMed]
- Kharaziha, P.; Ceder, S.; Li, Q.; Panaretakis, T. Tumor cell-derived exosomes: A message in a bottle. Biochim. Biophys. Acta 2012, 1826, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Hannafon, B.N.; Ding, W.Q. Intercellular communication by exosome-derived microRNAs in cancer. Int. J. Mol. Sci. 2013, 14, 14240–14269. [Google Scholar] [CrossRef]
- Xu, R.; Rai, A.; Chen, M.; Suwakulsiri, W.; Greening, D.W.; Simpson, R.J. Extracellular vesicles in cancer—Implications for future improvements in cancer care. Nat. Rev. Clin. Oncol. 2018, 15, 617–638. [Google Scholar] [CrossRef] [PubMed]
- Mulcahy, L.A.; Pink, R.C.; Carter, D.R. Routes and mechanisms of extracellular vesicle uptake. J. Extracell. Vesicles 2014, 3, 24641. [Google Scholar] [CrossRef]
- Meng, Y.; Sun, J.; Wang, X.; Hu, T.; Ma, Y.; Kong, C.; Piao, H.; Yu, T.; Zhang, G. Exosomes: A Promising Avenue for the Diagnosis of Breast Cancer. Technol. Cancer Res. Treat. 2019, 18, 1533033818821421. [Google Scholar] [CrossRef]
- Bahrami, A.; Aledavood, A.; Anvari, K.; Hassanian, S.M.; Maftouh, M.; Yaghobzade, A.; Salarzaee, O.; ShahidSales, S.; Avan, A. The prognostic and therapeutic application of microRNAs in breast cancer: Tissue and circulating microRNAs. J. Cell. Physiol. 2018, 233, 774–786. [Google Scholar] [CrossRef]
- Record, M. Intercellular communication by exosomes in placenta: A possible role in cell fusion? Placenta 2014, 35, 297–302. [Google Scholar] [CrossRef]
- Teng, X.; Chen, L.; Chen, W.; Yang, J.; Yang, Z.; Shen, Z. Mesenchymal Stem Cell-Derived Exosomes Improve the Microenvironment of Infarcted Myocardium Contributing to Angiogenesis and Anti-Inflammation. Cell. Physiol. Biochem. 2015, 37, 2415–2424. [Google Scholar] [CrossRef] [PubMed]
- Greening, D.W.; Nguyen, H.P.; Elgass, K.; Simpson, R.J.; Salamonsen, L.A. Human Endometrial Exosomes Contain Hormone-Specific Cargo Modulating Trophoblast Adhesive Capacity: Insights into Endometrial-Embryo Interactions. Biol. Reprod. 2016, 94, 38. [Google Scholar] [CrossRef] [PubMed]
- Di Ieva, A.; Butz, H.; Niamah, M.; Rotondo, F.; De Rosa, S.; Sav, A.; Yousef, G.M.; Kovacs, K.; Cusimano, M.D. MicroRNAs as biomarkers in pituitary tumors. Neurosurgery 2014, 75, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.C.; Feinbaum, R.L.; Ambros, V.J. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell 1993, 1993, 843–854. [Google Scholar] [CrossRef]
- Berindan-Neagoe, I.; Monroig Pdel, C.; Pasculli, B.; Calin, G.A. MicroRNAome genome: A treasure for cancer diagnosis and therapy. CA Cancer J. Clin. 2014, 64, 311–336. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Rana, T.M. Therapeutic targeting of microRNAs: Current status and future challenges. Nat. Rev. Drug Discov. 2014, 13, 622–638. [Google Scholar] [CrossRef]
- Challagundla, K.B.; Fanini, F.; Vannini, I.; Wise, P.; Murtadha, M.; Malinconico, L.; Cimmino, A.; Fabbri, M. microRNAs in the tumor microenvironment: Solving the riddle for a better diagnostics. Expert Rev. Mol. Diagn. 2014, 14, 565–574. [Google Scholar] [CrossRef]
- Zhang, H.; Li, Y.; Lai, M. The microRNA network and tumor metastasis. Oncogene 2010, 29, 937–948. [Google Scholar] [CrossRef]
- Huang, Q.; Gumireddy, K.; Schrier, M.; le Sage, C.; Nagel, R.; Nair, S.; Egan, D.A.; Li, A.; Huang, G.; Klein-Szanto, A.J.; et al. The microRNAs miR-373 and miR-520c promote tumour invasion and metastasis. Nat. Cell Biol. 2008, 10, 202–210. [Google Scholar] [CrossRef]
- Zhong, S.; Chen, X.; Wang, D.; Zhang, X.; Shen, H.; Yang, S.; Lv, M.; Tang, J.; Zhao, J. MicroRNA expression profiles of drug-resistance breast cancer cells and their exosomes. Oncotarget 2016, 7, 19601–19609. [Google Scholar] [CrossRef]
- Chen, W.X.; Xu, L.Y.; Qian, Q.; He, X.; Peng, W.T.; Zhu, Y.L.; Cheng, L. Analysis of miRNA signature differentially expressed in exosomes from adriamycin-resistant and parental human breast cancer cells. Biosci. Rep. 2018, 38. [Google Scholar] [CrossRef] [PubMed]
- Guzman, N.; Agarwal, K.; Asthagiri, D.; Yu, L.; Saji, M.; Ringel, M.D.; Paulaitis, M.E. Breast Cancer-Specific miR Signature Unique to Extracellular Vesicles Includes “microRNA-like” tRNA Fragments. Mol. Cancer Res. MCR 2015, 13, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Kruger, S.; Abd Elmageed, Z.Y.; Hawke, D.H.; Worner, P.M.; Jansen, D.A.; Abdel-Mageed, A.B.; Alt, E.U.; Izadpanah, R. Molecular characterization of exosome-like vesicles from breast cancer cells. BMC Cancer 2014, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Stevic, I.; Muller, V.; Weber, K.; Fasching, P.A.; Karn, T.; Marme, F.; Schem, C.; Stickeler, E.; Denkert, C.; van Mackelenbergh, M.; et al. Specific microRNA signatures in exosomes of triple-negative and HER2-positive breast cancer patients undergoing neoadjuvant therapy within the GeparSixto trial. BMC Med. 2018, 16, 179. [Google Scholar] [CrossRef] [PubMed]
- Fish, E.J.; Irizarry, K.J.; DeInnocentes, P.; Ellis, C.J.; Prasad, N.; Moss, A.G.; Curt Bird, R. Malignant canine mammary epithelial cells shed exosomes containing differentially expressed microRNA that regulate oncogenic networks. BMC Cancer 2018, 18, 832. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhang, Q.; Zhang, J.; Li, C.; Miao, Y.R.; Lei, Q.; Li, Q.; Guo, A.Y. EVmiRNA: A database of miRNA profiling in extracellular vesicles. Nucleic Acids Res. 2019, 47, D89–D93. [Google Scholar] [CrossRef] [PubMed]
- Melo, S.A.; Sugimoto, H.; O’Connell, J.T.; Kato, N.; Villanueva, A.; Vidal, A.; Qiu, L.; Vitkin, E.; Perelman, L.T.; Melo, C.A.; et al. Cancer exosomes perform cell-independent microRNA biogenesis and promote tumorigenesis. Cancer Cell 2014, 26, 707–721. [Google Scholar] [CrossRef] [PubMed]
- Kosaka, N.; Iguchi, H.; Hagiwara, K.; Yoshioka, Y.; Takeshita, F.; Ochiya, T. Neutral sphingomyelinase 2 (nSMase2)-dependent exosomal transfer of angiogenic microRNAs regulate cancer cell metastasis. J. Biol. Chem. 2013, 288, 10849–10859. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Pochampally, R.; Watabe, K.; Lu, Z.; Mo, Y.Y. Exosome-mediated transfer of miR-10b promotes cell invasion in breast cancer. Mol. Cancer 2014, 13, 256. [Google Scholar] [CrossRef]
- Ma, L.; Teruya-Feldstein, J.; Weinberg, R.A. Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature 2007, 449, 682–688. [Google Scholar] [CrossRef]
- Li, X.J.; Ren, Z.J.; Tang, J.H.; Yu, Q. Exosomal MicroRNA MiR-1246 Promotes Cell Proliferation, Invasion and Drug Resistance by Targeting CCNG2 in Breast Cancer. Cell. Physiol. Biochem. 2017, 44, 1741–1748. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Lai, X.; Yu, S.; Chen, S.; Ma, Y.; Zhang, Y.; Li, H.; Zhu, X.; Yao, L.; Zhang, J. Exosomal miR-221/222 enhances tamoxifen resistance in recipient ER-positive breast cancer cells. Breast Cancer Res. Treat. 2014, 147, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.D.; Wu, Y.; Zhang, X.H.; Lv, M.M.; Chen, W.X.; Chen, X.; Yang, S.J.; Shen, H.; Zhong, S.L.; Tang, J.H.; et al. Exosomes from adriamycin-resistant breast cancer cells transmit drug resistance partly by delivering miR-222. Tumour Biol. 2016, 37, 3227–3235. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.X.; Cai, Y.Q.; Lv, M.M.; Chen, L.; Zhong, S.L.; Ma, T.F.; Zhao, J.H.; Tang, J.H. Exosomes from docetaxel-resistant breast cancer cells alter chemosensitivity by delivering microRNAs. Tumour Biol. 2014, 35, 9649–9659. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.X.; Liu, X.M.; Lv, M.M.; Chen, L.; Zhao, J.H.; Zhong, S.L.; Ji, M.H.; Hu, Q.; Luo, Z.; Wu, J.Z.; et al. Exosomes from drug-resistant breast cancer cells transmit chemoresistance by a horizontal transfer of microRNAs. PLoS ONE 2014, 9, e95240. [Google Scholar] [CrossRef] [PubMed]
- Mao, L.; Li, J.; Chen, W.X.; Cai, Y.Q.; Yu, D.D.; Zhong, S.L.; Zhao, J.H.; Zhou, J.W.; Tang, J.H. Exosomes decrease sensitivity of breast cancer cells to adriamycin by delivering microRNAs. Tumour Biol. 2016, 37, 5247–5256. [Google Scholar] [CrossRef] [PubMed]
- Kia, V.; Paryan, M.; Mortazavi, Y.; Biglari, A.; Mohammadi-Yeganeh, S. Evaluation of exosomal miR-9 and miR-155 targeting PTEN and DUSP14 in highly metastatic breast cancer and their effect on low metastatic cells. J. Cell. Biochem. 2019, 120, 5666–5676. [Google Scholar] [CrossRef]
- Kia, V.; Mortazavi, Y.; Paryan, M.; Biglari, A.; Mohammadi-Yeganeh, S. Exosomal miRNAs from highly metastatic cells can induce metastasis in non-metastatic cells. Life Sci. 2019, 220, 162–168. [Google Scholar] [CrossRef]
- Mihelich, B.L.; Dambal, S.; Lin, S.; Nonn, L. miR-182, of the miR-183 cluster family, is packaged in exosomes and is detected in human exosomes from serum, breast cells and prostate cells. Oncol. Lett. 2016, 12, 1197–1203. [Google Scholar] [CrossRef]
- O’Brien, K.; Lowry, M.C.; Corcoran, C.; Martinez, V.G.; Daly, M.; Rani, S.; Gallagher, W.M.; Radomski, M.W.; MacLeod, R.A.; O’Driscoll, L. miR-134 in extracellular vesicles reduces triple-negative breast cancer aggression and increases drug sensitivity. Oncotarget 2015, 6, 32774–32789. [Google Scholar] [CrossRef]
- Zhou, W.; Fong, M.Y.; Min, Y.; Somlo, G.; Liu, L.; Palomares, M.R.; Yu, Y.; Chow, A.; O’Connor, S.T.; Chin, A.R.; et al. Cancer-secreted miR-105 destroys vascular endothelial barriers to promote metastasis. Cancer Cell 2014, 25, 501–515. [Google Scholar] [CrossRef] [PubMed]
- Di Modica, M.; Regondi, V.; Sandri, M.; Iorio, M.V.; Zanetti, A.; Tagliabue, E.; Casalini, P.; Triulzi, T. Breast cancer-secreted miR-939 downregulates VE-cadherin and destroys the barrier function of endothelial monolayers. Cancer Lett. 2017, 384, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Wu, X.; Zhou, W.; Fong, M.Y.; Cao, M.; Liu, J.; Liu, X.; Chen, C.H.; Fadare, O.; Pizzo, D.P.; et al. Cancer-cell-secreted exosomal miR-105 promotes tumour growth through the MYC-dependent metabolic reprogramming of stromal cells. Nat. Cell Biol. 2018, 20, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Fong, M.Y.; Zhou, W.; Liu, L.; Alontaga, A.Y.; Chandra, M.; Ashby, J.; Chow, A.; O’Connor, S.T.; Li, S.; Chin, A.R.; et al. Breast-cancer-secreted miR-122 reprograms glucose metabolism in premetastatic niche to promote metastasis. Nat. Cell Biol. 2015, 17, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Ochi, H.; Sunamura, S.; Kosaka, N.; Mabuchi, Y.; Fukuda, T.; Yao, K.; Kanda, H.; Ae, K.; Okawa, A.; et al. Cancer-secreted hsa-miR-940 induces an osteoblastic phenotype in the bone metastatic microenvironment via targeting ARHGAP1 and FAM134A. Proc. Natl. Acad. Sci. USA 2018, 115, 2204–2209. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liang, Y.; Sang, Y.; Song, X.; Zhang, H.; Liu, Y.; Jiang, L.; Yang, Q. MiR-770 suppresses the chemo-resistance and metastasis of triple negative breast cancer via direct targeting of STMN. Cell Death Dis. 2018, 9, 14. [Google Scholar] [CrossRef] [PubMed]
- Vaupel, P.; Mayer, A. Hypoxia in cancer: Significance and impact on clinical outcome. Cancer Metastasis Rev. 2007, 26, 225–239. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.O.; Youn, H.; Lee, C.H.; Kang, K.W.; Chung, J.K. Visualization of exosome-mediated miR-210 transfer from hypoxic tumor cells. Oncotarget 2017, 8, 9899–9910. [Google Scholar] [CrossRef] [PubMed]
- King, H.W.; Michael, M.Z.; Gleadle, J.M. Hypoxic enhancement of exosome release by breast cancer cells. BMC Cancer 2012, 12, 421. [Google Scholar] [CrossRef] [PubMed]
- Baroni, S.; Romero-Cordoba, S.; Plantamura, I.; Dugo, M.; D’Ippolito, E.; Cataldo, A.; Cosentino, G.; Angeloni, V.; Rossini, A.; Daidone, M.G.; et al. Exosome-mediated delivery of miR-9 induces cancer-associated fibroblast-like properties in human breast fibroblasts. Cell Death Dis. 2016, 7, e2312. [Google Scholar] [CrossRef] [PubMed]
- Dioufa, N.; Clark, A.M.; Ma, B.; Beckwitt, C.H.; Wells, A. Bi-directional exosome-driven intercommunication between the hepatic niche and cancer cells. Mol. Cancer 2017, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Kosaka, N.; Tominaga, N.; Yoshioka, Y.; Takeshita, F.; Takahashi, R.U.; Yoshida, M.; Tsuda, H.; Tamura, K.; Ochiya, T. Exosomes from bone marrow mesenchymal stem cells contain a microRNA that promotes dormancy in metastatic breast cancer cells. Sci. Signal. 2014, 7, ra63. [Google Scholar] [CrossRef] [PubMed]
- Uen, Y.; Wang, J.W.; Wang, C.; Jhang, Y.; Chung, J.Y.; Tseng, T.; Sheu, M.; Lee, S. Mining of potential microRNAs with clinical correlation—Regulation of syndecan-1 expression by miR-122-5p altered mobility of breast cancer cells and possible correlation with liver injury. Oncotarget 2018, 9, 28165–28175. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.C.; Lima, N.D.S.; Sarian, L.O.; Matheu, A.; Ribeiro, M.L.; Derchain, S.F.M. Exosome-mediated breast cancer chemoresistance via miR-155 transfer. Sci. Rep. 2018, 8, 829. [Google Scholar] [CrossRef] [PubMed]
- Bliss, S.A.; Sinha, G.; Sandiford, O.A.; Williams, L.M.; Engelberth, D.J.; Guiro, K.; Isenalumhe, L.L.; Greco, S.J.; Ayer, S.; Bryan, M.; et al. Mesenchymal Stem Cell-Derived Exosomes Stimulate Cycling Quiescence and Early Breast Cancer Dormancy in Bone Marrow. Cancer Res. 2016, 76, 5832–5844. [Google Scholar] [CrossRef] [PubMed]
- Lim, P.K.; Bliss, S.A.; Patel, S.A.; Taborga, M.; Dave, M.A.; Gregory, L.A.; Greco, S.J.; Bryan, M.; Patel, P.S.; Rameshwar, P. Gap junction-mediated import of microRNA from bone marrow stromal cells can elicit cell cycle quiescence in breast cancer cells. Cancer Res. 2011, 71, 1550–1560. [Google Scholar] [CrossRef]
- Vallabhaneni, K.C.; Penfornis, P.; Dhule, S.; Guillonneau, F.; Adams, K.V.; Mo, Y.Y.; Xu, R.; Liu, Y.; Watabe, K.; Vemuri, M.C.; et al. Extracellular vesicles from bone marrow mesenchymal stem/stromal cells transport tumor regulatory microRNA, proteins, and metabolites. Oncotarget 2015, 6, 4953–4967. [Google Scholar] [CrossRef]
- Deng, Z.; Rong, Y.; Teng, Y.; Zhuang, X.; Samykutty, A.; Mu, J.; Zhang, L.; Cao, P.; Yan, J.; Miller, D.; et al. Exosomes miR-126a released from MDSC induced by DOX treatment promotes lung metastasis. Oncogene 2017, 36, 639–651. [Google Scholar] [CrossRef]
- Shah, S.H.; Miller, P.; Garcia-Contreras, M.; Ao, Z.; Machlin, L.; Issa, E.; El-Ashry, D. Hierarchical paracrine interaction of breast cancer associated fibroblasts with cancer cells via hMAPK-microRNAs to drive ER-negative breast cancer phenotype. Cancer Biol. Ther. 2015, 16, 1671–1681. [Google Scholar] [CrossRef]
- Donnarumma, E.; Fiore, D.; Nappa, M.; Roscigno, G.; Adamo, A.; Iaboni, M.; Russo, V.; Affinito, A.; Puoti, I.; Quintavalle, C.; et al. Cancer-associated fibroblasts release exosomal microRNAs that dictate an aggressive phenotype in breast cancer. Oncotarget 2017, 8, 19592–19608. [Google Scholar] [CrossRef]
- Yang, M.; Chen, J.; Su, F.; Yu, B.; Su, F.; Lin, L.; Liu, Y.; Huang, J.D.; Song, E. Microvesicles secreted by macrophages shuttle invasion-potentiating microRNAs into breast cancer cells. Mol. Cancer 2011, 10, 117. [Google Scholar] [CrossRef]
- Lee, J.K.; Park, S.R.; Jung, B.K.; Jeon, Y.K.; Lee, Y.S.; Kim, M.K.; Kim, Y.G.; Jang, J.Y.; Kim, C.W. Exosomes derived from mesenchymal stem cells suppress angiogenesis by down-regulating VEGF expression in breast cancer cells. PLoS ONE 2013, 8, e84256. [Google Scholar] [CrossRef] [PubMed]
- Pakravan, K.; Babashah, S.; Sadeghizadeh, M.; Mowla, S.J.; Mossahebi-Mohammadi, M.; Ataei, F.; Dana, N.; Javan, M. MicroRNA-100 shuttled by mesenchymal stem cell-derived exosomes suppresses in vitro angiogenesis through modulating the mTOR/HIF-1alpha/VEGF signaling axis in breast cancer cells. Cell. Oncol. 2017, 40, 457–470. [Google Scholar] [CrossRef] [PubMed]
- Bovy, N.; Blomme, B.; Freres, P.; Dederen, S.; Nivelles, O.; Lion, M.; Carnet, O.; Martial, J.A.; Noel, A.; Thiry, M.; et al. Endothelial exosomes contribute to the antitumor response during breast cancer neoadjuvant chemotherapy via microRNA transfer. Oncotarget 2015, 6, 10253–10266. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zhou, Y.; Xia, T.; Zhou, X.; Huang, Z.; Zhang, H.; Zhu, W.; Ding, Q.; Wang, S. Circulating microRNAs from the miR-106a-363 cluster on chromosome X as novel diagnostic biomarkers for breast cancer. Breast Cancer Res. Treat. 2018, 170, 257–270. [Google Scholar] [CrossRef] [PubMed]
- Hannafon, B.N.; Trigoso, Y.D.; Calloway, C.L.; Zhao, Y.D.; Lum, D.H.; Welm, A.L.; Zhao, Z.J.; Blick, K.E.; Dooley, W.C.; Ding, W.Q. Plasma exosome microRNAs are indicative of breast cancer. Breast Cancer Res. BCR 2016, 18, 90. [Google Scholar] [CrossRef] [PubMed]
- Eichelser, C.; Stuckrath, I.; Muller, V.; Milde-Langosch, K.; Wikman, H.; Pantel, K.; Schwarzenbach, H. Increased serum levels of circulating exosomal microRNA-373 in receptor-negative breast cancer patients. Oncotarget 2014, 5, 9650–9663. [Google Scholar] [CrossRef]
- Gao, S.; Wang, Y.; Wang, M.; Li, Z.; Zhao, Z.; Wang, R.X.; Wu, R.; Yuan, Z.; Cui, R.; Jiao, K.; et al. MicroRNA-155, induced by FOXP3 through transcriptional repression of BRCA1, is associated with tumor initiation in human breast cancer. Oncotarget 2017, 8, 41451–41464. [Google Scholar] [CrossRef]
- Kong, X.; Zhang, J.; Li, J.; Shao, J.; Fang, L. MiR-130a-3p inhibits migration and invasion by regulating RAB5B in human breast cancer stem cell-like cells. Biochem. Biophys. Res. Commun. 2018, 501, 486–493. [Google Scholar] [CrossRef]
- Ni, Q.; Stevic, I.; Pan, C.; Muller, V.; Oliviera-Ferrer, L.; Pantel, K.; Schwarzenbach, H. Different signatures of miR-16, miR-30b and miR-93 in exosomes from breast cancer and DCIS patients. Sci. Rep. 2018, 8, 12974. [Google Scholar] [CrossRef]
- Zhang, G.; Zhang, W.; Li, B.; Stringer-Reasor, E.; Chu, C.; Sun, L.; Bae, S.; Chen, D.; Wei, S.; Jiao, K.; et al. MicroRNA-200c and microRNA-141 are regulated by a FOXP3-KAT2B axis and associated with tumor metastasis in breast cancer. Breast Cancer Res. BCR 2017, 19, 73. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, M.; Iinuma, H.; Umemoto, Y.; Yanagisawa, T.; Matsumoto, A.; Jinno, H. Exosome-encapsulated microRNA-223-3p as a minimally invasive biomarker for the early detection of invasive breast cancer. Oncol. Lett. 2018, 15, 9584–9592. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Martinez, A.; de Miguel-Perez, D.; Ortega, F.G.; Garcia-Puche, J.L.; Robles-Fernandez, I.; Exposito, J.; Martorell-Marugan, J.; Carmona-Saez, P.; Garrido-Navas, M.D.C.; Rolfo, C.; et al. Exosomal miRNA profile as complementary tool in the diagnostic and prediction of treatment response in localized breast cancer under neoadjuvant chemotherapy. Breast Cancer Res. BCR 2019, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Sueta, A.; Yamamoto, Y.; Tomiguchi, M.; Takeshita, T.; Yamamoto-Ibusuki, M.; Iwase, H. Differential expression of exosomal miRNAs between breast cancer patients with and without recurrence. Oncotarget 2017, 8, 69934–69944. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Deng, S.; Wang, G.; Liu, C.; Meng, L.; Qiao, S.; Shen, L.; Zhang, Y.; Lu, J.; Li, W.; et al. A direct quantification method for measuring plasma MicroRNAs identified potential biomarkers for detecting metastatic breast cancer. Oncotarget 2016, 7, 21865–21874. [Google Scholar] [CrossRef] [PubMed]
- Zhai, L.Y.; Li, M.X.; Pan, W.L.; Chen, Y.; Li, M.M.; Pang, J.X.; Zheng, L.; Chen, J.X.; Duan, W.J. In Situ Detection of Plasma Exosomal MicroRNA-1246 for Breast Cancer Diagnostics by a Au Nanoflare Probe. ACS Appl. Mater. Interfaces 2018, 10, 39478–39486. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, L.L.; Hou, M.F.; Xia, Y.K.; He, W.H.; Yan, A.; Weng, Y.P.; Zeng, L.P.; Chen, J.H. A ratiometric electrochemical biosensor for the exosomal microRNAs detection based on bipedal DNA walkers propelled by locked nucleic acid modified toehold mediate strand displacement reaction. Biosens. Bioelectron. 2018, 102, 33–40. [Google Scholar] [CrossRef]
- Sina, A.A.; Vaidyanathan, R.; Wuethrich, A.; Carrascosa, L.G.; Trau, M. Label-free detection of exosomes using a surface plasmon resonance biosensor. Anal. Bioanal. Chem. 2019, 411, 1311–1318. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, J.A.; Kwon, M.H.; Kang, J.Y.; Rhee, W.J. In Situ single step detection of exosome microRNA using molecular beacon. Biomaterials 2015, 54, 116–125. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, J.A.; Jeong, S.; Rhee, W.J. Simultaneous and multiplexed detection of exosome microRNAs using molecular beacons. Biosens. Bioelectron. 2016, 86, 202–210. [Google Scholar] [CrossRef]
- Shao, G.; Ji, S.; Wu, A.; Liu, C.; Wang, M.; Zhang, P.; Jiao, Q.; Kang, Y. DNAzyme-based probe for circulating microRNA detection in peripheral blood. Drug Des. Dev. Ther. 2015, 9, 6109–6117. [Google Scholar] [CrossRef][Green Version]
- Koumangoye, R.B.; Sakwe, A.M.; Goodwin, J.S.; Patel, T.; Ochieng, J. Detachment of breast tumor cells induces rapid secretion of exosomes which subsequently mediate cellular adhesion and spreading. PLoS ONE 2011, 6, e24234. [Google Scholar] [CrossRef] [PubMed]
- Manri, C.; Yokoi, T.; Nishida, H. Size-Selective Harvesting of Extracellular Vesicles for Strategic Analyses Towards Tumor Diagnoses. Appl. Biochem. Biotechnol. 2017, 182, 609–623. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.X.; Cheng, L.; Pan, M.; Qian, Q.; Zhu, Y.L.; Xu, L.Y.; Ding, Q. D Rhamnose beta-Hederin against human breast cancer by reducing tumor-derived exosomes. Oncol. Lett. 2018, 16, 5172–5178. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Li, M.; Cui, S.; Wang, D.; Zhang, C.Y.; Zen, K.; Li, L. Shikonin Inhibits the Proliferation of Human Breast Cancer Cells by Reducing Tumor-Derived Exosomes. Molecules 2016, 21, 777. [Google Scholar] [CrossRef] [PubMed]
- Gernapudi, R.; Yao, Y.; Zhang, Y.; Wolfson, B.; Roy, S.; Duru, N.; Eades, G.; Yang, P.; Zhou, Q. Targeting exosomes from preadipocytes inhibits preadipocyte to cancer stem cell signaling in early-stage breast cancer. Breast Cancer Res. Treat. 2015, 150, 685–695. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.Y.; Lee, J.K.; Jeon, Y.K.; Kim, C.W. Exosome derived from epigallocatechin gallate treated breast cancer cells suppresses tumor growth by inhibiting tumor-associated macrophage infiltration and M2 polarization. BMC Cancer 2013, 13, 421. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, H.D.; Yao, Y.F.; Zhong, S.L.; Zhao, J.H.; Tang, J.H. beta-Elemene Reverses Chemoresistance of Breast Cancer Cells by Reducing Resistance Transmission via Exosomes. Cell. Physiol. Biochem. 2015, 36, 2274–2286. [Google Scholar] [CrossRef]
- Hannafon, B.N.; Carpenter, K.J.; Berry, W.L.; Janknecht, R.; Dooley, W.C.; Ding, W.Q. Exosome-mediated microRNA signaling from breast cancer cells is altered by the anti-angiogenesis agent docosahexaenoic acid (DHA). Mol. Cancer 2015, 14, 133. [Google Scholar] [CrossRef]
- Ohno, S.; Takanashi, M.; Sudo, K.; Ueda, S.; Ishikawa, A.; Matsuyama, N.; Fujita, K.; Mizutani, T.; Ohgi, T.; Ochiya, T.; et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol. Ther. 2013, 21, 185–191. [Google Scholar] [CrossRef]
- O’Brien, K.P.; Khan, S.; Gilligan, K.E.; Zafar, H.; Lalor, P.; Glynn, C.; O’Flatharta, C.; Ingoldsby, H.; Dockery, P.; De Bhulbh, A.; et al. Employing mesenchymal stem cells to support tumor-targeted delivery of extracellular vesicle (EV)-encapsulated microRNA-379. Oncogene 2018, 37, 2137–2149. [Google Scholar] [CrossRef] [PubMed]
- Taghikhani, A.; Hassan, Z.M.; Ebrahimi, M.; Moazzeni, S.M. microRNA modified tumor-derived exosomes as novel tools for maturation of dendritic cells. J. Cell. Physiol. 2018, 234, 9417–9427. [Google Scholar] [CrossRef] [PubMed]
- Lamichhane, T.N.; Jeyaram, A.; Patel, D.B.; Parajuli, B.; Livingston, N.K.; Arumugasaamy, N.; Schardt, J.S.; Jay, S.M. Oncogene Knockdown via Active Loading of Small RNAs into Extracellular Vesicles by Sonication. Cell. Mol. Bioeng. 2016, 9, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Roma-Rodrigues, C.; Pereira, F.; Alves de Matos, A.P.; Fernandes, M.; Baptista, P.V.; Fernandes, A.R. Smuggling gold nanoparticles across cell types—A new role for exosomes in gene silencing. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1389–1398. [Google Scholar] [CrossRef] [PubMed]
- Naseri, Z.; Oskuee, R.K.; Jaafari, M.R.; Forouzandeh Moghadam, M. Exosome-mediated delivery of functionally active miRNA-142-3p inhibitor reduces tumorigenicity of breast cancer in vitro and in vivo. Int. J. Nanomed. 2018, 13, 7727–7747. [Google Scholar] [CrossRef] [PubMed]

| Subtypes | Classification | HER2 | HR |
|---|---|---|---|
| Triple negative | TNBC 1 | (−) | ER 2 (−), PgR 3 (−) |
| HR (−) and HER2 (+) | HER2-positive | (+) | ER (−), PgR (−) |
| HR (+) and HER2 (+) | (+) | ER and/or PgR (+) | |
| HR (+) and HER2 (−) | Luminal-A like | (−) | ER and/or PgR (+); Multi-parameter molecular marker ‘good’ if available; High ER/PR; clearly low Ki-67 (low proliferation [7]); low grade (well-differentiated [8]) |
| Intermediate | (−) | Multi-parameter molecular marker ‘intermediate’ if available. | |
| Luminal-B like | (−) | ER and/or PgR (+); Multi-parameter molecular marker ‘bad’ if available; Lower ER/PR; clearly high Ki-67 (high proliferation [7]); histological grade 3 (poorly differentiated [8]) |
| Stimulant | Cargo-microRNAs | Donor Cells | Recipient Cells | Gene Targets | Biological Activities | Major Findings | Refs |
|---|---|---|---|---|---|---|---|
| miR-10a, 10b, 21, 27a, 155, 373 (↑) | Cancer cell (MDA-MB-231, MCF-7, 67NR, 4T1) | Epithelial cells (MCF-10A, NMuMG) | HOXD10 (miR-10b), PTEN (miR-21) | Tumorigenesis (in a Dicer-dependent manner) | Pre-miRNAs, Dicer (CD43-mediated accumulation), AGO2, and TRBP are present in exosomes of cancer cells to generate mature miRNAs. | [57] | |
| miR-210 (↑) | Cancer cell (4T1, MCF-7, MDA-MB-231-D3H1, MDA-MB-231-D3H2LN) | Endothelial cells (HUVECs) | ephrin-A3 | Angiogenesis; metastasis | nSMase2 is important to regulate exosomal miRNAs, which will transfer to endothelial cells to promote metastatic initiation efficiency. | [58] | |
| Twist | miR-10b (↑) | Cancer cell (MDA-MB-231, MCF-7) | Epithelial cells (MCF-10A, HMLE) | HOXD10 (inhibit the expression of the pro-metastatic gene, RHOC), KLF44 | Invasion | nSMase2 or ceramide promotes the exosome-mediated miR-10b secretion. | [59,60] |
| miR-1246 (↑) | Cancer cell (MDA-MB-231, MCF-7) | Epithelial cells (MCF-10A, HMLE) | CCNG2 (tightly regulated through the cell cycle) | Cell proliferation; invasion; drug resistance | Exosomal miR-1246 functions in regulating breast tumor progression and has the potential for applications in miRNA-based therapeutics. | [61] | |
| miR-221/222 (↑) | Cancer cell [MCF-7/Tam] | Cancer cell [MCF-7/WT (tamoxifen sensitive)] | ERα, p27 (cell cycle arrest, autophagy, and angiogenesis) | Drug resistance (tamoxifen) | EV-secreted miR-221/222 serves as signaling molecules to mediate the communication of tamoxifen resistance. | [62] | |
| miR-222 (↑) | Cancer cell (MCF-7/Adr) | Cancer cell (MCF-7/sensitive) | Drug resistance (adriamycin) | Exosomes are effective in transmitting drug resistance and the delivery of miR-222 via exosomes may be a mechanism. | [63] | ||
| miR-23a, 29a, 1246, 222, 452 (↑) | Cancer cell (MCF-7/Doc) | Cancer cell (MCF-7/sensitive) | Sprouty2 [regulate invasion and metastasis] (miR-23a), PTEN (miR-222), APC4 (miR-452) | Drug resistance (docetaxel) | Abundant miRNAs of Doc/exo in pathways implicated in therapy failure. | [64] | |
| miR-100, 222, 30a (↑) | Cancer cell (MCF-7/Doc, MCF-7/Adr) | Cancer cell (MCF-7/sensitive) | PTEN (miR-222) | Drug resistance (docetaxel, adriamycin) | The involvement of miRNAs in pathways implicated in cancer pathogenesis, membrane vesiculation, and therapy failure. | [65] | |
| miR-23a, 24, 149, 222 (↑) | Cancer cell (MCF-7/Adr) | Cancer cell (MCF-7/sensitive) | Sprouty2 (miR-23a), PTEN p27 (miR-24), (miR-222) | Drug resistance (adriamycin) | Adr/exo loaded miRNAs for its production, release and which were associated with Wnt signaling pathway. Adr/exo was able to increase the overall resistance and regulate gene levels. | [66] | |
| miR-9, miR-155 (↑) | Cancer cell (MDA-MB-231) | Cancer cells (MCF-7) | PTEN (miR-9), DUSP14 (miR-155) | Tumor growth | Exosomal miRNAs can transfer from highly metastatic cancer cells to other low metastatic cancer cells and can suppress target genes in the recipient cells. | [67,68] | |
| miR-182 (↑) | Cancer cell (miR-182 transfected MDA-MB-231) | Cancer cell (naïve MDA-MB-231 cells) | Tumorigenesis | MiR-182 is packaged in exosomes, detectable in exosomes from cell culture supernatant and human serum, which may be transferred between cells via a microvesicle-dependent mechanism. | [69] | ||
| miR-134 (↓) | Cancer cell (miR-134-transfected Hs578T, a TNBC cell line; isogenic sub-clone cells) | Cancer cells (Hs578Ts(i)8 parent cells) | STAT5B (control Hsp90) | Cellular proliferation; migration and invasion; drug resistance (cisplatin, anti-Hsp90 drug) | (1) The direct transfection or EV delivery transport route of miRNA achieved different effects. (2) MiR-134 had clinical relevance in breast tumors. | [70] | |
| miR-105 (↑) | Cancer cell (MDA-MB-231, MCF-10A as the control group) | Endothelial cells (HMVECs) | ZO-1 (also called tight junctions protein 1, migration-related gene) | Metastasis | Exosome-mediated transfer of cancer cell-secreted miR-105 efficiently destroys tight junctions and the integrity of these natural barriers against metastasis. | [71] | |
| miR-939 (↑) | Cancer cell (MDA-MB-231-GFP cells) | Endothelial cells (HUVECs) | VE-cadherin (a component of adherens junction involved in vessel permeability) | Migration and invasion | MiR-939 could (1) increase HUVECs monolayer permeability; (2) favor trans-endothelial migration by the disruption of the endothelial barrier. | [72] | |
| MYC (oncogene) | miR-105 (↑) | Cancer cell (MDA-MB-231, MCF-10A as the control group) | CAFs (patient-derived primary fibroblasts CAF265922; fetal lung fibroblast cell line WI-38; mouse embryonic fibroblast cell line NIH3T3) | MXI1 | Tumor growth | Reprogrammed CAFs would ultimately promote tumor growth by leading different metabolic pathways under the circumstances of efficient or insufficient nutrition. | [73] |
| miR-122 (↑) | Cancer cell (MDA-MB-361, MDA-MB-468, MDA-MB-231, MDA-MB-231-HM, SKBR3, BT4, MCF-10A as the control group) | Lung fibroblast, brain astrocytes, neurons | PKM2, GLUT1 | Reprogram glucose metabolism; cancer cell proliferation; metastasis | Exosomal miR-122 inhibited the glucose uptake by niche cells and increased glucose availability to cancer cells, while inhibition of miR-122 decreases the incidence of metastasis in vivo. | [74] | |
| miR-940 (↑) | Cancer cell (MDA-MB-231) | Human mesenchymal stem cells (MSC, UCB408E6E7TERT-33) | ARHGAP1, FAM134A | Bone metastasis | miR-940 facilitates the osteogenic differentiation of human MSCs. | [75] | |
| miR-770 (↓) | Cancer cell (MDA-MB-231, MDA-MB-468) | TAMs (THP-1 cell) | STMN1 | Drug resistance (doxorubicin); metastasis | miR-770 could (i) influence the polarization of macrophages which promote M1 phenotype and inhibit M2 phenotype, (ii) suppress the doxorubicin-resistance and metastasis of TNBC cells | [76] | |
| HIF-1α | miR-210 (↑) | Cancer cell (MDA-MB-231, 4T1) | Endothelial cells (SVEC), macrophages (Raw264.7), stem cells (MBs-MSC), fibroblasts (3T3), and dendritic cells (JAWS2). | Ephrin A3, PTP1B (vascular remodeling related genes) | Angiogenesis | A miR-210 specific reporter system to realize in vitro and in vivo visualization. | [78] |
| HIF-1α | miR-210 (↑) | Cancer cell (MDA-MB-231, SKBR3, MCF-7) | TME | Hypoxic cancer cells may release more exosomes into their microenvironment to promote their own survival and invasion | [79] | ||
| miR-9 (↑) | Cancer cell (MDA-MB-231, MDA-MB-468) | Normal fibroblasts (isolated from specimens belonging to patients) | mainly involved in cell motility and ECM remodeling pathways | Tumor growth; migration and invasion | (1) Enhance cell motility; (2) enhance the switch to CAF phenotype | [80] |
| Stimulant | Cargo-microRNAs | Donor Cells | Recipient Cells | Gene Targets | Biological Activities | Major Findings | Refs |
|---|---|---|---|---|---|---|---|
| miR-9 (↑) | CAFs | Cancer cell (MDA-MB-231, MDA-MB-468); Normal Fibroblasts | E-cadherin | Migration, invasion, cell proliferation | MiR-9 was an important player in the crosstalk between cancer cells and stroma. | [80] | |
| miR-186, 23a, -205 (↑) | The hepatic niche (HepN) | Cancer cell (MDA-MB-231) | Regulate E-cadherin transcription and MErT induction | MErT | The normal tissue/HepN derived exosomes in enabling seeding and entry into the dormancy of the cancer cells at the metastatic site. | [81] | |
| miR-23b (↑) | Bone marrow mesenchymal stem cells (BM-MSC) | Cancer cell (BM2 cell, MDA-MB-231) | MARCKS (encode a protein that promotes cell cycling and motility) | Dormancy; drug resistance (docetaxel) | (1) They generated a bone marrow-metastatic human breast cancer cell line (BM2); (2) Exosomal transfer of miRNAs from the bone marrow may promote breast cancer cell dormancy in a metastatic niche. | [82] | |
| miR-122-5p (↑) | Human hepatoma cells (Huh-7, Hep3B) | Cancer cells (MCF-7) | syndecan-1 (SDC1) | Metastasis | Metastasis or mobility of breast cancer cells might be affected by circulating miR-122-5p and not directly correlated with the progression of breast cancer. | [83] | |
| miR-155 (↑) | Breast CSC; DOX-/PTX-resistant MCF-7 cell line | Cancer cell (MCF-7 cell, MDA-MB-231) | TGF-β, C/EBP-β and FOXO3a | EMT; migration; chemoresistance | Exosomes may intermediate resistance, and migration capacity to sensitive cells partly through exosome transfer of miR-155. | [84] | |
| miR-222/223 (↑) | MSC (naive MSC; T47D, MDA-MB-231-primed MSCs) | Cancer cell (MDA-MB-231, T47D) | Cycle quiescence; dormancy; drug resistance (carboplatin) | Breast cancer cells prime MSC to release exosomal miR-222/223, which in turn promotes quiescence in a subset of cancer cells and confers drug resistance. | [85] | ||
| miR-127, 197, 222, 223 (↑) | BM stromal cells (prepared from BM aspirates of healthy donors) | Cancer cell (MDA-MB-231, T47D) | CXCL12 (chemokine family) | Cycle quiescence; dormancy | (1) The transfer of miRNAs from BM stroma to BC cells might play a role in the dormancy of BM metastases. (2) Gap-junction maybe another way of the transfer of miRNAs. | [86] | |
| miR-21, 34a (↑) | Human MSC | Cancer cell (MCF-7, osteosarcoma cell) | Cell proliferation | First comprehensive-omics based study that characterized the complex cargo of extracellular vesicles secreted by hMSCs and their role in supporting breast cancers. | [87] | ||
| IL-13 | miR-126a (↑) | MDSC | Cancer cell (4T1, MDA-MB-231); IL-13+Th2 cell | S100A9 | Lung metastasis; angiogenesis | Doxorubicin treatment led to an enhancement of IL-33 in breast cancer cells, IL-13 receptor and miR-126a in MDSCs in a positive feedback loop manner. | [88] |
| miR-221/222 (↑) | CAFs | Cancer cell (MCF-7 cell line long-term conditioned for growth in estrogen depleted conditions) | ER (estrogen receptor) | ER-negative phenotype | CAF-secreted microRNAs are directly involved in ER-repression and may contribute to the MAPK-induced ER-repression in breast cancer cells. | [89] | |
| miR-21, -378e, -143 (↑) | CAFs; Normal fibroblasts with overexpressed miRs | Cancer cell (BT549, MDA-MB-231, T47D) | Cell growth; stemness; EMT | CAFs strongly promote the development of an aggressive breast cancer cell phenotype. | [90] | ||
| IL-4 | miR-223 (↑) | TAMs (isolated from the peripheral blood and activated by adding IL-4) | Cancer cell (SKBR3, MDA-MB-231) | Mef2c (inhibit proliferation and granulocyte function) | Invasion | MiR-223 may target at the Mef2c-β-catenin pathway to mediate breast cancer cell invasion. | [91] |
| miR-16 (↑) | MSC | Cancer cell (4T1); Mouse endothelial cell line (SVEC) | VEGF | Angiogenesis | MiR-16 was partially responsible for the antiangiogenic effect of MSC-derived exosomes. | [92] | |
| miR-100 (↑) | MSC | Cancer cell (MDA-MB-231, MCF-7, T47D); Endothelial cells (HUVECs) | mTOR | Angiogenesis | MSC-derived exosomes induce a decrease in the expression and secretion of VEGF through modulating the mTOR/HIF-1α signaling axis in breast cancer-derived cells. | [93] | |
| miR-503 (↑) | Endothelial cells (HUVECs) | Cancer cell (A549, HCT116, MDA-MB-231, U87) | CCND2, CCND3 | Cell proliferation; invasion | Increased plasmatic miR-503 in breast cancer patients after neoadjuvant chemotherapy, which could be partly due to increased miRNA secretion | [94] |
| Cargo | Patient Cohorts | Exosome Source (Isolation Method) | Assay Used | Outcome and Utility | Refs |
|---|---|---|---|---|---|
| miR-106a-3p, 106a-5p, 20b-5p, 92a-2-5p (plasma miRNAs); miR-106a-5p, 19b-3p, 20b-5p, 92a-3p (serum miRNAs) | 400 plasma samples (from 200 BC patients and 200 healthy controls (HCs)), 406 serum samples (from 204 BC patients and 202 HCs), | plasma (from 32 BC patients and 32 HCs), serum (from 32 BC patients and 32 HCs) | qRT-PCR | Except for the expression of miR-20b-5p, the expression patterns of exosomal miRNAs were concordant between plasma and serum, indicating the potential use of exosomal miRNAs as biomarkers. | [95] |
| miR-21, 1246 (↑) | exosomes from the conditioned media of human breast cancer cell lines, mouse plasma of patient-derived orthotopic xenograft models (PDX), and human plasma samples from 16 patients | plasma (ultracentrifugation, ExoQuick) | next-generation small RNA sequencing; qRT-PCR | The combination of plasma exosome miR-1246 and miR-21 is a better indicator of breast cancer than their individual levels. | [96] |
| miR-373 (↑) | 168 patients with invasive breast cancer, 19 patients with benign breast diseases and 28 healthy women | serum (ExoQuick) | RT-PCR | Serum levels of exosomal miR-373 are linked to triple-negative and more aggressive breast carcinomas. | [97] |
| miR-155 (↑) | 259 participants, including patients with breast cancer or benign breast tumors, members of breast cancer families, and matched healthy female controls. | plasma (ultracentrifugation) | nest-qPCR | For patients with early stage or localized breast cancer, there were high levels of miR-155 in both plasma and blood cells. | [98] |
| miR-130a-3p (↓) | 40 pairs of breast cancer and adjacent normal tissues, 40 pairs of blood samples from patients with breast cancer and healthy controls (confirmed as invasive ductal breast cancer, and no patient had received any chemotherapy or radiotherapy ahead of surgery.) | circulating blood (ExoQuick Exosomal Extraction Kit) | Lower levels of exosome-derived miR-130a-3p are associated with lymph node metastasis (p = 0.0019) and advanced TNM stage (p = 0.0014). | [99] | |
| miR-16 (↑), 30b (↓), 93 (↑) | 111 BC patients, 42 DCIS patients and 39 healthy women | plasma | TaqMan real-time PCR | (1) The levels of exosomal miR-16 were higher in plasma of BC (p = 0.034) and DCIS (p = 0.047) patients than healthy women and were associated with estrogen (p = 0.004) and progesterone (p = 0.008) receptor status. (2) In estrogen-positive patients miR-16 was significantly enriched in exosomes (p = 0.0001). (3) Lower levels of exosomal miR-30b were associated with recurrence (p = 0.034). (4) Exosomal miR-93 was upregulated in DCIS patients (p = 0.001). | [100] |
| miR-200c (↑), -141 (↑) | 259 human subjects, including 114 patients with breast cancer, 30 patients with benign breast tumors, 21 women with a family history of breast cancer, and 94 healthy women | plasma (ultracentrifugation) | nest-qPCR | Circulating levels of miR-200c and miR-141 are potential biomarkers for early detection of breast cancer metastases. | [101] |
| miR-223-3p (↑) | 185 breast cancer patients, 20 healthy volunteers | plasma (ultracentrifugation) | microRNA (miRNA) microarray; RT-qPCR | (1) identify the invasive lesions of DCIS patients diagnosed by biopsy; (2) significantly associated with the malignancy of breast cancer. | [102] |
| miR-21(↑), 105(↑), 155(↑) | 53 breast cancer women (6 of them were diagnosed as metastatic patients) and 8 healthy donors | serum | qPCR | During neoadjuvant treatment, exosomal miRNA-21 expression levels directly correlated with tumor size (p = 0.039) and inversely with Ki67 expression (p = 0.031). | [103] |
| miR-340-5p (↑), 17-5p (↓), 130a-3p (↓), 93-5p (↓) | 16 patients with primary breast cancer with recurrence and 16 without recurrence; 35 breast cancer patients with and 39 without recurrence | serum (ExoQuick) | qRT-PCR | There are different expression patterns of miRNAs between tumor tissues and serum | [104] |
| Therapeutic Cargo | EV Source | Recipient Cells | Target Gene | Drug Loading Techniques/POSSIBLE Drugs | Biological Activities | Key Findings | Refs |
|---|---|---|---|---|---|---|---|
| antagomiR-222/223 | MSCs | Cancer cell (MDA-MB-231, T47D) | Co-transfection (Lipofectamine RNAiMAX Reagent) | cycle quiescence; dormancy; drug resistance (carboplatin) | A novel therapeutic strategy to target dormant breast cancer cells. | [85] | |
| miR-130a, 425 (↓) | MCF-7 | associated with the mTOR, ErbB, MAPK and TGF-β signaling pathways | DRβ-H | cell proliferation | DRβ-H inhibited MCF-7/S cell growth through reducing exosome release. | [114] | |
| miR-128 (↓) | Cancer cell (MCF-7) | Cancer cell (MCF-7) | Bax | Shikonin (SK) | cell proliferation | shikonin inhibits the proliferation of MCF-7 cells by reducing tumor-derived exosomal miR-128. | [115] |
| miR-140 (↑) | Mouse preadipocyte (3T3L1, MBA-1) | MCF10DCIS cells | SOX9 | Shikonin (SK) | tumorigenesis; regulating differentiation, stemness, and migration | (1) MiR-140/SOX2/SOX9 axis can regulate differentiation, stemness, and migration. (2) SK-treated preadipocytes secrete exosomes with high levels of miR-140, which can inhibit nearby DCIS cells by targeting SOX9 signaling | [116] |
| miR-16 (↑) | Cancer cell (4T1) | TAMs (RAW264.7) | EGCG | TME | EGCG up-regulates miR-16 in tumor cells, which can be transferred to TAM via exosomes and inhibits TAM infiltration and M2 polarization | [117] | |
| miR-34a (↑), 452 (↓) | Cancer cell (MCF-7/Doc, MCF-7/Adr) | Cancer cell | β-elemene | reverse drug resistance (docetaxel, adriamycin) | β-elemene effectively sensitizes drug-resistant BCA cells to Doc and Adr through a signaling pathway that involves miRNA and gene regulation | [118] | |
| miR-23b, 320b (↑) | Cancer cell (MDA-MB-231, MCF-7, ZR751 and BT20) | Epithelial cells (MCF-10A, EA.hy926) | PLAU, AMOTL1 (miR-23b); NRP1, ETS2 (miR-320b) | DHA | angiogenesis | the microRNAs transferred by exosomes mediate DHA’s anti-angiogenic action. | [119] |
| let-7a | Donor cells (express the transmembrane domain of PDGF fused to the GE11 peptide) | EGFR-expressing breast cancer cells | Modified exosomes with the GE11 peptide or EGF on their surfaces | (1) Modified exosomes with the GE11 peptide or EGF on their surfaces delivered miRNA to EGFR-expressing cancer tissues; (2) intravenously injected exosomes targeting EGFR delivered let-7a specifically to xenograft breast cancer cells in RAG2−/−mice. | [120] | ||
| miR-379 (↑) | Engineered MSCs | Cancer cells (T47D, HCC-1954) | COX-2 | lentiviral transduction | Exploiting the tumor-homing capacity of MSCs while engineering the cells to secrete EVs enriched with miR-379 holds exciting potential as an innovative therapy for metastatic breast cancer. | [121] | |
| miR-155, -142, and let-7i (↑) | Cancer cells (4T1) | Dendritic cells | IL-6, IL-17, IL-1b, TGF-β, SOCS1, KLRK1, IFN-γ, and TLR4 | electroporation | The modified exosomes would be a hopeful cell-free vaccine for cancer treatment. | [122] | |
| anti-miR-142-3p oligonucleotides | MSCs | Cancer cell (4T1 and TUBO) | APC (miR-142-3p); P2 × 7R (miR-150) | LNA (locked nucleic acid)-modified | MSCs-derived exosomes could be used as a feasible nano-vehicle to deliver drug molecules like LNA-anti-miR-142-3p in both in vitro and in vivo studies. | [125] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Q.; Peng, F.; Chen, J. The Role of Exosomal MicroRNAs in the Tumor Microenvironment of Breast Cancer. Int. J. Mol. Sci. 2019, 20, 3884. https://doi.org/10.3390/ijms20163884
Liu Q, Peng F, Chen J. The Role of Exosomal MicroRNAs in the Tumor Microenvironment of Breast Cancer. International Journal of Molecular Sciences. 2019; 20(16):3884. https://doi.org/10.3390/ijms20163884
Chicago/Turabian StyleLiu, Qingqing, Fu Peng, and Jianping Chen. 2019. "The Role of Exosomal MicroRNAs in the Tumor Microenvironment of Breast Cancer" International Journal of Molecular Sciences 20, no. 16: 3884. https://doi.org/10.3390/ijms20163884
APA StyleLiu, Q., Peng, F., & Chen, J. (2019). The Role of Exosomal MicroRNAs in the Tumor Microenvironment of Breast Cancer. International Journal of Molecular Sciences, 20(16), 3884. https://doi.org/10.3390/ijms20163884





