Cutaneous Metastasis after Surgery, Injury, Lymphadenopathy, and Peritonitis: Possible Mechanisms
Abstract
1. Introduction
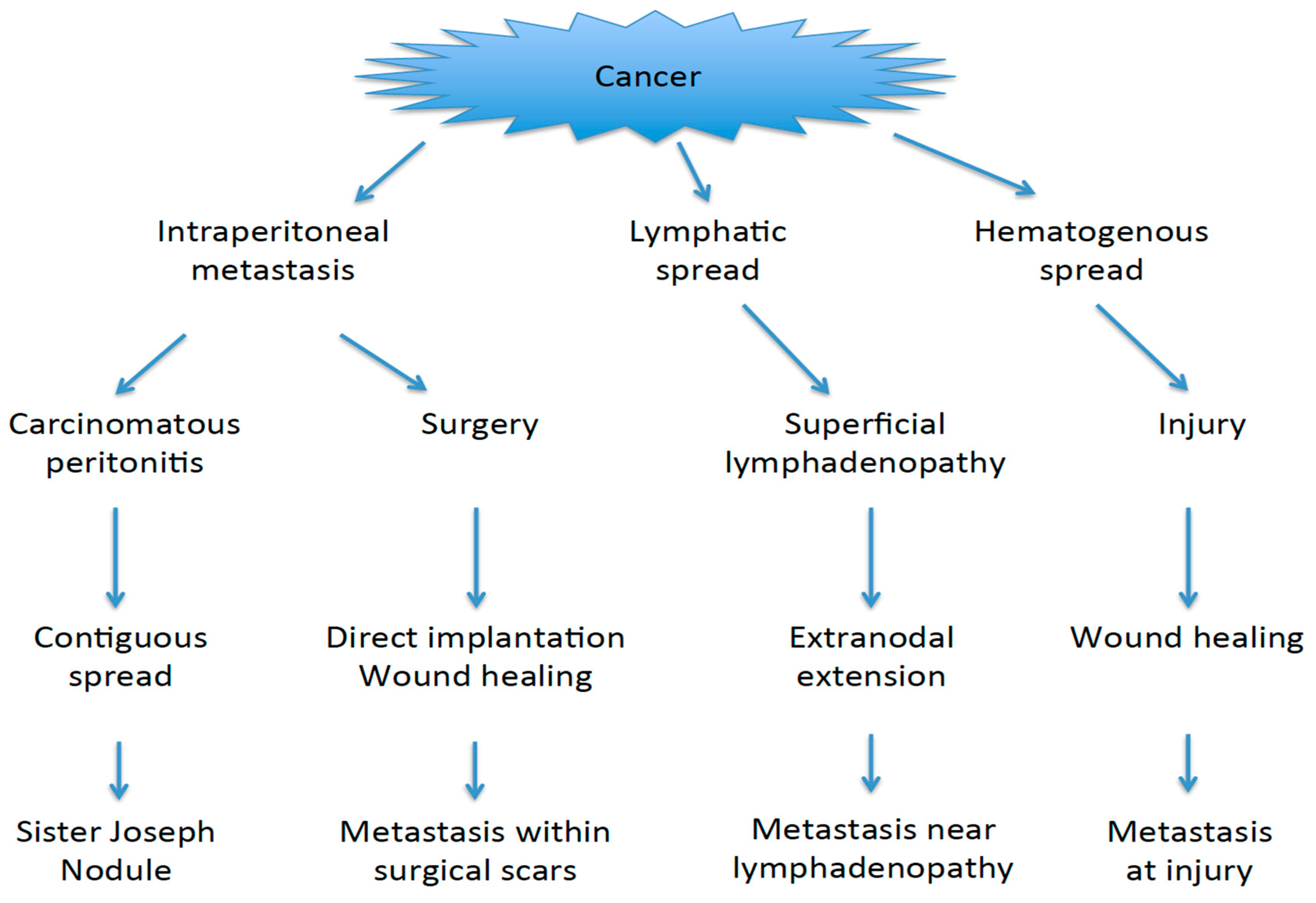
2. Patterns of Skin Metastases
2.1. SJN
2.2. Non-SJN Metastasis after Surgery
2.3. Non-SJN Metastasis after Injury
2.4. Non-SJN Metastasis after Lymphadenopathy
3. Possible Mechanisms of Skin Metastases
3.1. Mode of Spread
3.1.1. Several Routes to the Umbilicus
3.1.2. Direct Implantation
3.1.3. Hematogenous Metastasis
3.1.4. Extranodal Extension
3.2. Mechanisms of Tumor Growth
3.2.1. Wound Healing and Inflammation
3.2.2. Adipose Tissue
3.3. Modifying Factors
3.3.1. Host Factors
3.3.2. Tumor Factors
3.3.3. Treatment Factors
4. Clinical Treatments
5. Concluding Remarks
Funding
Conflicts of Interest
References
- Takeo, M.; Lee, W.; Ito, M. Wound Healing and Skin Regeneration. Cold Spring Harb. Perspect. Med. 2015, 5, a023267. [Google Scholar] [CrossRef] [PubMed]
- Lookingbill, D.P.; Spangler, N.; Sexton, F.M. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J. Am. Acad. Dermatol. 1990, 22, 19–26. [Google Scholar] [CrossRef]
- Hu, S.C.S.; Hen, G.S.; Wu, C.S.; Chai, C.Y.; Chen, W.T.; Lan, C.C.E. Rates of cutaneous metastases from different internal malignancies: Experience from a Taiwanese medical center. J. Am. Acad. Dermatol. 2009, 60, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, I.; Matsuura, T. Skin metastases in epithelial ovarian and fallopian tube carcinoma. Medicine 2017, 96, e7798. [Google Scholar] [CrossRef] [PubMed]
- Cormio, G.; Capotorto, M.; Di Vagno, G.; Cazzolla, A.; Carriero, C.; Selvaggi, L. Skin metastases in ovarian carcinoma: A report of nine cases and a review of the literature. Gynecol. Oncol. 2003, 90, 682–685. [Google Scholar] [CrossRef]
- Powell, F.C.; Cooper, A.J.; Massa, M.C.; Goellner, J.R.; Su, W.P. Sister Mary Joseph’s nodule: A clinical and histologic study. J. Am. Acad. Dermatol. 1984, 10, 610–615. [Google Scholar] [CrossRef]
- Majmudar, B.; Wiskind, A.K.; Croft, B.N.; Dudley, A.G. The Sister (Mary) Joseph nodule: Its significance in gynecology. Gynecol. Oncol. 1991, 40, 152–159. [Google Scholar] [CrossRef]
- Girijala, R.R.; Riahi, R.R.; Cohen, P.R. Sister Mary Joseph Nodule as a Cutaneous Manifestation of Metastatic Appendiceal Adenocarcinoma: Case Report and Literature Review. Cureus 2018, 20, e2244. [Google Scholar] [CrossRef]
- Mimura, T.; Yagi, Y.; Asami, Y.; Miyamoto, S.; Iitsuka, C.; Onuki, M.; Ishikawa, T.; Kushima, M.; Matsumoto, K.; Sekizawa, A. Sister Mary Joseph nodule in ovarian cancer: A case report and literature review. Kanto J. Obstet. Gynaecol. 2018, 55, 479–484. (In Japanese) [Google Scholar]
- Hori, T.; Okada, N.; Nakauchi, M.; Hiramoto, S.; Kikuchi-Mizota, A.; Kyogoku, M.; Oike, F.; Sugimoto, H.; Tanaka, J.; Morikami, Y.; et al. Hematogenous umbilical metastasis from colon cancer treated by palliative single-incision laparoscopic surgery. World J. Gastrointest. Surg. 2013, 27, 272–277. [Google Scholar] [CrossRef]
- Pearlman, A.W. Breast cancer—Influence of growth rate on prognosis and treatment evaluation: A study based on mastectomy scar recurrences. Cancer 1976, 38, 1826–1833. [Google Scholar] [CrossRef]
- Fortner, J.G.; Lawrence, W. Implantation of gastric cancer in abdominal wounds. Ann. Surg. 1960, 152, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Curtis, M.G.; Hopkins, M.P.; Cross, B.; Tantri, M.D.; Jexison, E.L.; Rehmus, E. Wound seeding associated with endometrial cancer. Gynecol. Oncol. 1994, 52, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Bogani, G.; Dowdy, S.C.; Cliby, W.A.; Gostout, B.S.; Kumar, S.; Ghezzi, F.; Multinu, F.; Mariani, A. Incisional recurrences after endometrial cancer surgery. Anticancer Res. 2015, 35, 6097–6104. [Google Scholar] [PubMed]
- Oosterling, S.J.; van der Bij, G.J.; van Egmond, M.; van der Sijp, J.R. Surgical trauma and peritoneal recurrence of colorectal carcinoma. Eur. J. Surg. Oncol. 2005, 31, 29–37. [Google Scholar] [CrossRef]
- Dhall, R.; Grant, K.A. Cervical adenocarcinoma metastasizing to the skin incision: A case report. Asia-Ocean. J. Obstet. Gynaecol. 1991, 17, 261–263. [Google Scholar] [CrossRef]
- Gordon, A.N.; Jensen, R.; Jones, H.W., 3rd. Squamous carcinoma of the cervix complicating pregnancy: Recurrence in episiotomy after vaginal delivery. Obstet. Gynecol. 1989, 73, 850–852. [Google Scholar]
- Schmitz, H.E.; Grossbard, P. Endometriosis of episiotomy scar. Am. J. Obstet. Gynecol. 1948, 55, 880–882. [Google Scholar] [CrossRef]
- Seydel, A.S.; Sickel, J.Z.; Warner, E.D.; Sax, H.C. Extrapelvic endometriosis: Diagnosis and treatment. Am. J. Surg. 1996, 171, 239–241. [Google Scholar] [CrossRef]
- Sataline, L.; Pellicia, O. Inflammatory oncotaxis. JAMA 1978, 240, 2434. [Google Scholar]
- Martinez, A.; Querleu, D.; Leblac, E.; Narducci, F.; Ferron, G. Low incidence of port-site metastases after laparoscopic staging of uterine cancer. Gynecol. Oncol. 2010, 118, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; Marquette, S.; Amant, F.; Berteloot, P.; Neven, P. Port-site metastases after open laparoscopy: A study in 173 patients with advanced ovarian carcinoma. Int. J. Gynecol. Cancer 2005, 15, 776–779. [Google Scholar] [CrossRef] [PubMed]
- Hsiu, J.G.; Given, F.T., Jr.; Kemp, G.M. Tumor implantation after diagnostic laparoscopic biopsy of serous ovarian tumors of low malignant potential. Obstet. Gynecol. 1986, 68, 90S–93S. [Google Scholar] [PubMed]
- Denton, G.W.; Schofield, J.B.; Gallagher, P. Uncommon complications of laparoscopic sterilisation. Ann. R. Coll. Surg. Engl. 1990, 72, 210–211. [Google Scholar] [PubMed]
- Siriwardevia, A.; Samarji, W. Cutaneous tumour seeding from a previously undiagnosed pancreatic carcinoma after laparoscopic cholecystectomy. Ann. R. Coll. Surg. Engl. 1993, 75, 199–200. [Google Scholar]
- Ugarte, F. Laparoscopic cholecystectomy port seeding from a colon carcinoma. Am. Surg. 1995, 61, 820–821. [Google Scholar] [PubMed]
- Lane, T.M.; Cook, A.J. Port-site metastasis after laparoscopic cholecystectomy for benign disease. J. Laparoendosc. Adv. Surg. Tech. 1999, 9, 283–284. [Google Scholar] [CrossRef]
- Carlson, N.L.; Krivak, T.C.; Winter, W.E., III; Macri, C.I. Port Site Metastasis of Ovarian Carcinoma Remote from Laparoscopic Surgery for Benign Disease. Gynecol. Oncol. 2002, 85, 529–531. [Google Scholar] [CrossRef]
- Rieger, N.; McIntosh, N. Port site metastasis from synchronous primaries of the colon and ovary following laparoscopic cholecystectomy. Eur. J. Surg. Oncol. 1998, 24, 44–54. [Google Scholar] [CrossRef]
- Nevler, A.; Gluck, I.; Balint-Labat, N.; Rosin, D. Recurrent Metastatic Spread to a Percutaneous Gastrostomy Site in a Patient with Squamous Cell Carcinoma of the Tongue: A Case Report and Review of the Literature. J. Oral. Maxillofac. Surg. 2014, 72, 829–832. [Google Scholar] [CrossRef]
- Magillligan, D.J., Jr.; Isshak, G. Carcinoma of the Breast in a Pacemaker Pocket—Simple Recurrence or Oncotaxis? Pacing Clin. Electrophysiol. 1980, 3, 220–223. [Google Scholar] [CrossRef]
- Behtash, N.; Ghaemmaghami, F.; Yarandi, F.; Ardalan, F.A. Cutaneous metastasis from carcinoma of the cervix at the drain site. Gynecol. Oncol. 2002, 85, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Walansky, H.; Lischner, H.W. Needle track implantation of tumor after percutaneous lung biopsy. Ann. Intern. Med. 1969, 71, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Shine, T.; Wallack, M.K. Inflammatory oncotaxis after testing the skin of the cancer patient. Cancer 1981, 47, 1325–1328. [Google Scholar] [CrossRef]
- Mbaeri, T.U.; Orakwe, J.C.; Ezejifor, O.I. Unsuspected Skin Metastasis of Adenocarcinoma of the Prostate in a Patient on Goserelin. Niger. J. Surg. 2018, 24, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Pertzborn, S.; Buekers, T.E.; Sood, A.K. Hematogenous skin metastases from cervical cancer at primary presentation. Gynecol. Oncol. 2000, 76, 416–417. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.; Seagle, B.L.L.; Bautista, E.; Hansra, B.S.; Samuelson, R.; Shahabi, S. Vulvar Metastasis of an Early-Stage Well-Differentiated Endometrial Cancer After Minimally Invasive Surgery. J. Minim. Invasive Gynecol. 2014, 21, 708–711. [Google Scholar] [CrossRef] [PubMed]
- Cohen, H.J.; Laszlo, J. Influence of trauma on the unusual distribution of metastases from carcinoma of the larynx. Cancer 1972, 29, 466–471. [Google Scholar] [CrossRef]
- Palaia, I.; Angioli, R.; Cutillo, G.; Manci, N.; Benedetti Panici, P. Skin relapse from cervical cancer. Gynecol. Oncol. 2002, 87, 155–156. [Google Scholar] [CrossRef]
- Rattanasirivilai, A.; Kurban, A.; Lenzy, Y.M.; Yaar, R. Cutaneous metastasis of prostatic adenocarcinoma: A cautionary tale. J. Cutan Pathol. 2011, 38, 521–524. [Google Scholar] [CrossRef]
- Yilmaz, Z.; Bese, T.; Demirkiran, F.; Ilvan, S.; Sanioglu, C.; Arvas, M.; Kosebay, D. Skin metastasis in ovarian carcinoma. Int. J. Gynecol. Cancer 2006, 16, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Yau, A.; Magliocco, A.; Chu, P. Cutaneous metastatic disease in cervical cancer: A case report. J. Obstet. Gynaecol. Can. 2010, 32, 467–472. [Google Scholar] [CrossRef]
- Diehl, L.F.; Hurwitz, M.A.; Johnson, S.A.; Butler, W.M.; Taylor, H.G. Skin metastases confined to a field of previous irradiation; report of two cases and review of the literature. Cancer 1984, 53, 1864–1868. [Google Scholar] [CrossRef]
- Kayikcioglu, F.; Boran, N.; Ayhan, A.; Güler, N. Inflammatory Breast Metastases of Ovarian Cancer: A Case Report. Gynecol. Oncol. 2001, 83, 613–616. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.I.; Lee, M.C.; Kuo, T.T.; Hong, H.S. Cellulitis-like cutaneous metastasis of uterine cervical carcinoma. J. Am. Acad. Dermatol. 2007, 56, S26–S28. [Google Scholar] [CrossRef] [PubMed]
- Antonio, A.M.; Alves, J.V.; Goulao, J.; Bartolo, E. Ovarian carcinoma presenting as cutaneous nasal metastasis. An. Bras. Dermatol. 2016, 91, 101–104. [Google Scholar] [CrossRef]
- Schwartz, R.A. Cutaneous metastatic disease. J. Am. Acad. Dermatol. 1995, 33, 161–185. [Google Scholar] [CrossRef]
- Galvan, V.G. Sister Mary Joseph’s nodule. Ann. Intern. Med. 1998, 128, 410. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Wolf, J.K.; Levenback, C. Laparoscopic port-site metastases: Etiology and prevention. Gynecol. Oncol. 2003, 91, 179–189. [Google Scholar] [CrossRef]
- Sugarbaker, P.H. Sister Mary Joseph’s sign. J. Am. Coll. Surg. 2001, 193, 339–340. [Google Scholar] [CrossRef]
- DerHagopian, R.P. Inflammatory Oncotaxis. JAMA 1979, 241, 2264. [Google Scholar] [CrossRef] [PubMed]
- Rousset-Jablonski, C.; Alifano, M.; Pli-Bureau, G.; Camilleri-Broet, S.; Rousset, P.; Regnard, J.F.; Gompel, A. Catamenial pneumothorax and endometriosis-related pneumothorax: Clinical features and risk factors. Hum. Reprod. 2011, 26, 2322–2329. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.C.; Doyle, G.V.; Terstappen, L.W.M.M. Significance of Circulating Tumor Cells Detected by the CellSearch System in Patients with Metastatic Breast Colorectal and Prostate Cancer. J. Oncol. 2010, 2010, 617421. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Riethdorf, S.; Wu, G.; Wang, T.; Yang, K.; Peng, G.; Liu, J.; Pantel, K. Meta-analysis of the prognostic value of circulating tumor cells in breast cancer. Clin. Cancer Res. 2012, 18, 5701–5710. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Aigner, M.; Thorlund, K.; Mollberg, N.; Motschall, E.; Jensen, K.; Diener, M.K.; Büchler, M.W.; Koch, M.; Weitz, J. Meta-analysis shows that detection of circulating tumor cells indicates poor prognosis in patients with colorectal cancer. Gastroenterology 2010, 138, 1714–1726. [Google Scholar] [CrossRef] [PubMed]
- De Bono, J.S.; Scher, H.I.; Montgomery, R.B.; Parker, C.; Miller, M.C.; Tissing, H.; Doyle, G.V.; Terstappen, L.W.W.M.; Pienta, K.J.; Raghavan, D. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 2008, 14, 6302–6309. [Google Scholar] [CrossRef]
- Hou, J.M.; Krebs, M.G.; Lancashire, L.; Sloane, R.; Backen, A.; Swain, R.K.; Priest, L.J.; Greystoke, A.; Zhou, C.; Morris, K.; et al. Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J. Clin. Oncol. 2012, 30, 525–532. [Google Scholar] [CrossRef]
- Romero-Laorden, N.; Olmos, D.; Fehm, T.; Garcia-Donas, J.; Diaz-Padilla, I. Circulating and disseminated tumor cells in ovarian cancer: A systematic review. Gynecol. Oncol. 2014, 133, 632–639. [Google Scholar] [CrossRef]
- Pantel, K.; Brakenhoff, R.H. Dissecting the metastatic cascade. Nat. Rev. Cancer 2004, 4, 448–456. [Google Scholar] [CrossRef]
- Choi, A.H.; Blount, S.; Perez, M.N.; Chavez de Paz, C.E.; Rodriguez, S.A.; Surrusco, M.; Garberoglio, C.A.; Lum, S.S.; Senthil, M. Size of Extranodal Extension on Sentinel Lymph Node Dissection in the American College of Surgeons Oncology Group Z0011 Trial Era. JAMA Surg. 2015, 150, 1141–1148. [Google Scholar] [CrossRef]
- Aziz, S.; Wik, E.; Knutsvik, G.; Klingen, T.A.; Chen, Y.; Davidsen, B.; Aas, H.; Aas, T.; Akslen, L.A. Extra-nodal extension is a significant prognostic factor in lymph node positive breast cancer. PLoS ONE 2017, 12, e0171853. [Google Scholar] [CrossRef] [PubMed]
- Luchini, C.; Fleischmann, A.; Boormans, J.L.; Fassan, M.; Nottegar, A.; Lucato, P.; Stubbs, B.; Solmi, M.; Porcaro, A.; Vernose, N.; et al. Extranodal extension of lymph node metastasis influences recurrence in prostate cancer: A systematic review and metaanalysis. Sci. Rep. 2017, 7, 2374. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, F.; Mori, T.; Matsumura, S.; Matsumoto, Y.; Fukasawa, M.; Teshima, M.; Kobayashi, K.; Yoshimoto, S. Prognostic significance of surgical extranodal extension in head and neck squamous cell carcinoma patients. Jpn. J. Clin. Oncol. 2017, 47, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, G.M.; Quah, S.; Sampath, P. Cancer: The dark side of wound healing. FEBS J. 2018, 285, 4516–4534. [Google Scholar] [CrossRef] [PubMed]
- Ceelen, W.; Pattyn, P.; Mareel, M. Surgery, wound healing, and metastasis: Recent insights and clinical implications. Crit. Rev. Oncol. Hematol. 2014, 89, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Qian, B.Z. Inflammation fires up cancer metastasis. Semin. Cancer Biol. 2017, 47, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Savant, S.S.; Sriramkumar, S.; O’Hagan, H.M. The Role of Inflammation and Inflammatory Mediators in the Development, Progression, Metastasis, and Chemoresistance of Epithelial Ovarian Cancer. Cancers 2018, 10, 251. [Google Scholar] [CrossRef]
- Medzhitov, R. Origin and physiological roles of inflammation. Nature 2008, 454, 428–435. [Google Scholar] [CrossRef]
- Mantovani, A.; Marchesi, F.; Malesci, A.; Laghi, L.; Allavena, P. Tumor-Associated Macrophages as Treatment Targets in Oncology. Nat. Rev. Clin. Oncol. 2017, 14, 399–416. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, Y. Tumor-associated macrophages: From basic research to clinical application. J. Hematol. Oncol. 2017, 10, 58. [Google Scholar] [CrossRef]
- Chanmee, T.; Ontong, P.; Konno, K.; Itano, N. Tumor-Associated Macrophages as Major Players in the Tumor Microenvironment. Cancers 2014, 6, 1670–1680. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.O.; Gordon, S. The M1 and M2 paradigm of macrophage activation: Time for reassessment. F1000 Prime Rep. 2014, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.D.; Rice, P.L.; Redente, E.F.; Kauvar, E.F.; Lemond, L.; Aly, T.; Wanebo, K.; Chan, E.D. Wound Healing after Trauma May Predispose to Lung Cancer Metastasis. Review of Potential Mechanisms. Am. J. Respir. Cell Mol. Biol. 2011, 44, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Qian, B.; Deng, Y.; Im, J.H.; Muschel, R.J.; Zou, Y.; Li, J.; Lang, R.A.; Pollard, J.W. A distinct macrophage population mediates metastatic breast cancer cell extravasation, establishment and growth. PLoS ONE 2009, 4, e6562. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, M.; Zannoni, G.F.; Martinelli, E.; Anchora, L.P.; Ferrandina, G.; Torpeano, G.; Faagottei, A.; Scambia, G. Polarisation of Tumor-Associated Macrophages toward M2 Phenotype Correlates with Poor Response to Chemoradiation and Reduced Survival in Patients with Locally Advanced Cervical Cancer. PLoS ONE 2015, 10, e0136654. [Google Scholar] [CrossRef] [PubMed]
- Cho, U.; Kim, B.; Kim, S.; Han, Y.; Song, Y.S. Pro-inflammatory M1 macrophage enhances metastatic potential of ovarian cancer cells through NF-κB activation. Mol. Carcinog. 2018, 57, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Menter, D.G.; Kopetz, S.; Hawk, E.; Sood, A.K.; Loree, J.M.; Gresele, P.; Honn, K.V. Platelet “first responders” in wound response, cancer, and metastasis. Cancer Metastasis Rev. 2017, 36, 199–213. [Google Scholar] [CrossRef]
- Li, N. Platelets in cancer metastasis: To help the “villain” to do evil. Int. J. Cancer 2016, 138, 2078–2087. [Google Scholar] [CrossRef]
- Wu, L.; Saxena, S.; Awaji, M.; Singh, R.K. Tumor-Associated Neutrophils in Cancer: Going Pro. Cancers 2019, 11, 564. [Google Scholar] [CrossRef]
- Powell, D.R.; Huttenlocher, A. Neutrophils in the tumor microenvironment. Trends Immunol. 2016, 37, 41–52. [Google Scholar] [CrossRef]
- Hurt, B.; Schlick, R.; Edil, B.; El Kasmi, K.C.; Barnett, C., Jr. Cancer-promoting mechanisms of tumor-associated neutrophils. Am. J. Surg. 2017, 214, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Singel, K.L.; Segal, B.H. Neutrophils in the tumor microenvironment: Trying to heal the wound that cannot heal. Immunol. Rev. 2016, 273, 329–343. [Google Scholar] [CrossRef] [PubMed]
- Mabuchi, S.; Yokoi, E.; Komura, N.; Kimura, T. Myeloid-derived suppressor cells and their role in gynecological malignancies. Tumor Biol. 2018, 40, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sprouse, M.L.; Welte, T.; Boral, D.; Liu, H.N.; Yin, W.; Vishnoi, M.; Goswami-Sewell, D.; Li, L.; Pei, G.; Jia, P.; et al. PMN-MDSCs Enhance CTC Metastatic Properties through Reciprocal Interactions via ROS/Notch/Nodal Signaling. Int. J. Mol. Sci. 2019, 20, 1916. [Google Scholar] [CrossRef] [PubMed]
- Safarzadeh, E.; Orangi, M.; Mohammad, H.; Babaie, F.; Baradaran, B. Myeloid-derived suppressor cells: Important contributors to tumor progression and metastasis. J. Cell. Physiol. 2018, 233, 3024–3036. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Nefedova, Y.; Lei, A.; Gabrilovich, D. Neutrophils and PMN-MDSC: Their biological role and interaction with stromal cells. Semin. Immunol. 2018, 35, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Keskin, D.; Kim, J.; Cooke, V.G.; Wu, C.C.; Sugimoto, H.; Gu, C.; De Palma, M.; Kalluri, R.; LeBleu, V.S. Targeting vascular pericytes in hypoxic tumors increases lung metastasis via angiopoietin-2. Cell Rep. 2015, 10, 1066–1081. [Google Scholar] [CrossRef]
- Browning, L.; Patel, M.R.; Horvath, E.B.; Tawara, K.; Jorcyk, C.L. IL-6 and ovarian cancer: Inflammatory cytokines in promotion of metastasis. Cancer Manag. Res. 2018, 10, 6685–6693. [Google Scholar] [CrossRef]
- Paez-Ribes, M.; Allen, E.; Hudock, J.; Takeda, T.; Okuyama, H.; Vinals, F.; Inoue, M.; Bergers, G.; Hanahan, D.; Casanovas, O. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell 2009, 15, 220–224. [Google Scholar] [CrossRef]
- Bai, W.K.; Zhang, W.; Hu, B. Vascular endothelial growth factor suppresses dendritic cells function of human prostate cancer. OncoTargets Ther. 2018, 11, 1267–1274. [Google Scholar] [CrossRef]
- Terme, M.; Pernot, S.; Marcheteau, E.; Sandoval, F.; Benhamouda, N.; Colussi, O.; Dubreuil, O.; Carpentier, A.F.; Tartour, E.; Taieb, J. VEGFA-VEGFR Pathway Blockade Inhibits Tumor-Induced Regulatory T-cell Proliferation in Colorectal Cancer. Cancer Res. 2013, 73, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.A.; Kang, Y. The metastasis-promoting roles of tumor-associated immune cells. J. Mol. Med. 2013, 91, 411–429. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, R. The biology and function of fibroblasts in cancer. Nat. Rev. Cancer 2016, 16, 582–598. [Google Scholar] [CrossRef] [PubMed]
- Kuzet, S.E.; Gaggioli, C. Fibroblast activation in cancer: When seed fertilizes soil. Cell Tissue Res. 2016, 365, 607–619. [Google Scholar] [CrossRef] [PubMed]
- Shiga, K.; Hara, M.; Nagasaki, T.; Takahashi, H.; Takayama, H. Cancer-Associated Fibroblasts: Their Characteristics and Their Roles in Tumor Growth. Cancers 2015, 7, 2443–2458. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Chen, J.; Yao, H.; Liu, J.; Yu, S.; Lao, L.; Wang, M.; Luo, M.; Xing, Y.; Chen, F.; et al. CD10+GPR77+ cancer-associated fibroblasts promote cancer formation and chemoresistance by sustaining cancer stemness. Cell 2018, 172, 841–856. [Google Scholar] [CrossRef] [PubMed]
- Nieman, K.M.; Romero, I.L.; Van Houten, B.; Lengyel, E. Adipose tissue and adipocytes supports tumorigenesis and metastasis. Biochim. Biophys. Acta 2013, 181, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Duong, M.N.; Geneste, A.; Fallone, F.; Li, X.; Dumontet, C.; Mller, C. The fat and the bad: Mature adipocytes, key actors in tumor progression and resistance. Oncotarget 2017, 8, 57622. [Google Scholar] [CrossRef] [PubMed]
- Varricchi, G.; Ganata, F.; Loffredo, S.; Genovese, A.; Maone, G. Angiogenesis and lymphangiogenesis in inflammatory skin disorders. J. Am. Acad. Dermatol. 2015, 73, 144–153. [Google Scholar] [CrossRef]
- Salminen, A.; Kaarniranta, K.; Kauppinen, A. Immunosenescence: The potential role of myeloid-derived suppressor cells (MDSC) in age-related immune deficiency. Cell. Mol. Life Sci. 2019, 76, 1901–1908. [Google Scholar] [CrossRef]
- Jackaman, C.; Tomay, F.; Duong, L.; Razak, N.B.A.; Pixley, F.J.; Metharom, P.; Nelson, D.J. Aging and cancer: The role of macrophages and neutrophils. Ageing Res. Rev. 2017, 36, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Weyand, C.M.; Goronzy, J.J. Aging of the Immune System. Mechanisms and Therapeutic Targets. Ann. Am. Thorac. Soc. 2016, 13, S422–S428. [Google Scholar] [CrossRef] [PubMed]
- Kolb, R.; Sutterwala, F.S.; Zhang, W. Obesity and cancer: Inflammation bridges the two. Curr. Opin. Pharmacol. 2016, 29, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, N.M.; Gucalp, A.; Dammenberg, A.J.; Hudis, C.A. Obesity and Cancer Mechanisms: Tumor Microenvironment and Inflammation. J. Clin. Oncol. 2016, 34, 4270–4276. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Zhang, H.; Jiang, X.; Qian, C.; Liu, Z.; Luo, D. Factors involved in cancer metastasis: A better understanding to “seed and soil” hypothesis. Mol. Cancer 2017, 16, 176. [Google Scholar] [CrossRef] [PubMed]
- De Groot, A.E.; Roy, S.; Brown, J.S.; Pienta, K.J.; Amend, S.R. Revisiting Seed and Soil: Examining the Primary Tumor and Cancer Cell Foraging in Metastasis. Mol. Cancer Res. 2017, 15, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Bardia, A.; Wittner, B.S.; Stott, S.L.; Smas, M.E.; Ting, D.T.; Isakoff, S.J.; Ciciliano, J.C.; Wells, M.N.; Shah, A.M.; et al. Circulating Breast Tumor Cells Exhibit Dynamic Changes in Epithelial and Mesenchymal Composition. Science 2013, 339, 580–584. [Google Scholar] [CrossRef]
- Paolucci, V.; Schaeff, B.; Schneider, M.; Gutt, C. Tumor seeding following laparoscopy: International survey. World J. Surg. 1999, 23, 989–997. [Google Scholar] [CrossRef]
- Kadar, N. Port-site recurrences following laparoscopic operations for gynaecological malignancies. Br. J. Obstet. Gynaecol. 1997, 104, 1308–1313. [Google Scholar] [CrossRef]
- Van Dam, P.A.; DeCloedt, J.; Tjalma, W.A.A.; Buytaert, P.; Becquart, D.; Vergote, I.B. Trocar implantation metastasis after laparoscopy in patients with advanced ovarian cancer: Can the risk be reduced? Am. J. Obstet. Gynecol. 1999, 181, 536–541. [Google Scholar] [CrossRef]
- Pavlidis, E.T.; Pavlidis, T.E. Role of bevacizumab in colorectal cancer growth and its adverse effects: A review. World J. Gastroenterol. 2013, 19, 5051–5060. [Google Scholar] [CrossRef] [PubMed]
- Dalton, H.J.; Pradeep, S.; McGuire, M.; Hailemichael, Y.; Shaolin, M.A.; Lyons, Y.; Armaiz-Pena, G.N.; Previs, R.A.; Hansen, J.M.; Rupaimoole, R.; et al. Macrophages Facilitate Resistance to Anti-VEGF Therapy by Altered VEGFR Expression. Clin. Cancer Res. 2017, 23, 7034–7046. [Google Scholar] [CrossRef] [PubMed]
- Diakos, C.I.; Charles, K.A.; McMillan, D.C.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, e493–e503. [Google Scholar] [CrossRef]
- Ries, C.H.; Cannarile, M.A.; Hoves, S.; Benz, J.; Wartha, K.; Runza, V.; Rey-Giraud, F.; Pradel, L.P.; Feuerhake, F.; Klaman, I.; et al. Targeting Tumor-Associated Macrophages with Anti-CSF-1R Antibody Reveals a Strategy for Cancer Therapy. Cancer Cell 2014, 25, 846–859. [Google Scholar] [CrossRef] [PubMed]
- Gabrilovich, D.I. Myeloid-Derived Suppressor Cells. Cancer Immunol. Res. 2016, 5, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Shou, D.; Wen, L.; Song, Z.; Yin, J.; Sun, Q.; Gong, W. Suppressive role of myeloid-derived suppressor cells (MDSCs) in the microenvironment of breast cancer and targeted immunotherapies. Oncotarget 2016, 7, 64505–64511. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Donthireddy, L.; Marbel, D.; Condamine, T.; Wang, F.; Lavilla-Alonso, S.; Hashimoto, A.; Vonteddu, P.; Behera, R.; Goins, M.A.; et al. Cancer-Associated Fibroblasts Neutralize the Anti-tumor Effect of CSF1 Receptor Blockade by Inducing PMN-MDSC Infiltration of Tumors. Cancer Cell 2017, 32, 654–668. [Google Scholar] [CrossRef]
- Davis, A.N.; Afshar-Kharghan, V.; Sood, A.K. Platelet Effects on Ovarian Cancer. Semin. Oncol. 2014, 41, 378–384. [Google Scholar] [CrossRef]
- Topalian, S.L.; Drake, C.G.; Pardoll, D.M. Immune Checkpoint Blockade: A Common Denominator Approach to Cancer Therapy. Cancer Cell 2015, 27, 450–461. [Google Scholar] [CrossRef]
- Wei, S.C.; Duffy, C.R.; Allison, J.P. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 2018, 8, 1069–1086. [Google Scholar] [CrossRef]
- Tong, B.; Wang, M. CD47 is a novel potent immunotherapy target in human malignancies: Current studies and future promises. Future Oncol. 2018, 14, 2179–2188. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Sakaguchi, S. Regulatory T cells in cancer immunotherapy. Cell Res. 2017, 27, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Arnold, K.M.; Opdenaker, L.M.; Flynn, D.; Sims-Mourtada, J. Wound Healing and Cancer Stem Cells: Inflammation as a Driver of Treatment Resistance in Breast Cancer. Cancer Growth Metastasis 2015, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Gao, F.; Li, H.; Liu, H.; Zhang, Y.; Zheng, R.; Zhang, Y.; Chen, J.; Li, X.; Liu, G.; et al. CD47: A potential immunotherapy target for eliminating cancer cells. Clin. Transl. Oncol. 2016, 18, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Cioffi, M.; Trabulo, S.; Hidalgo, M.; Costello, E.; Greenhalf, W.; Erkan, M.; Kleeff, J.; Sainz, B., Jr.; Heeschen, C. Inhibition of CD47 effectively targets pancreatic cancer stem cells via dual mechanisms. Clin. Cancer Res. 2015, 21, 2325–2337. [Google Scholar] [CrossRef] [PubMed]
- Matlung, H.L.; Szilagyi, K.; Barclay, N.A.; van den Berg, T.K. The CD47-SIRPα signaling axis as an innate immune checkpoint in cancer. Immunol. Rev. 2017, 276, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Murata, Y.; Saito, Y.; Kotani, T.; Matozaki, T. CD47-signal regulatory protein α signaling system and its application to cancer immunotherapy. Cancer Sci. 2018, 109, 2349–2357. [Google Scholar] [CrossRef] [PubMed]
- Pawelec, G. Does patient age influence anti-cancer immunity? Semin. Immunopathol. 2019, 41, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Hurez, V.; Padron, A.S.; Svatek, R.S.; Curiel, T.J. Considerations for successful cancer immunotherapy in aged hosts. Clin. Exp. Immunol. 2017, 187, 53–63. [Google Scholar] [CrossRef]
- Manser, A.R.; Uhrberg, M. Age-related changes in natural killer cell repertoires: Impact on NK cell function and immune surveillance. Cancer Immunol. Immunother. 2016, 65, 417–426. [Google Scholar] [CrossRef]
- Muppala, S.; Konduru, S.K.P.; Merchant, N.; Ramsoondar, J.; Rampersad, C.K.; Rajitha, B.; Mukund, V.; Kancherla, J.; Hammond, A.; Barik, T.K.; et al. Adiponectin: Its role in obesity-associated colon and prostate cancers. Crit. Rev. Oncol. Hematol. 2017, 116, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Paget, S. The distribution of secondary growths in cancer of the breast. Lancet 1889, 133, 571–573. [Google Scholar] [CrossRef]
- Skipper, D.; Jeffrey, M.J.; Cooper, A.J.; Taylor, I.; Alexander, P. Preferential growth of bloodborne cancer cells in colonic anastomoses. Br. J. Cancer 1988, 57, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Murthy, S.M.; Goldschmidt, R.A.; Rao, L.N.; Ammirati, M.; Buchmann, T.; Scanlon, E.F. The influence of surgical trauma on experimental metastases. Cancer 1989, 64, 2035–2044. [Google Scholar] [CrossRef]
- Hutchinson, C.M.A.; Hameed, K.; Zaitoun, A.; Madhusudan, S. Inflammatory oncotaxis in cholangiocarcinoma. Grand Rounds 2013, 13, 57–62. [Google Scholar] [CrossRef]
| Preceding Condition or Procedure | Site of Cutaneous Metastasis | Mode of Tumor Spread | Primary Site of Tumors | Age | Ref. |
|---|---|---|---|---|---|
| Umbilical Metastasis (Sister Joseph Nodule, SJN) | |||||
| Carcinomatous peritonitis | Umbilicus | Direct invasion, Hematogenous, (Lymphatic) | Colon, Ovary, Stomach, Endometrium, Pancreas, Vulva, Appendix | 32–95y | [4,5,6,7,8] |
| Inguinal node met | Umbilicus | Lymphatic, Hematogenous | Ovary, Colon | 47, 83y | [9,10] |
| Non-SJN Metastasis after Surgery | |||||
| Surgical incision | Incision of tumor removal | Implant, (Hematogenous) | Breast, Ovary, Stomach, Colon, Cervix, Endometrium | 25–68y | [4,5,11,12,13,14,15,16] |
| Episiotomy for delivery | Implant | Cervix, Normal Endometrium | 24–33y | [17,18] | |
| Incision of cesarean section | Implant | Normal Endometrium | 21–40y | [19] | |
| Old scar before tumor removal | Implant, Hematogenous | Ovary | 44y | [20] | |
| Laparoscopy | Port site of tumor removal | Implant, Hematogenous | Ovary, Colon, Cervix, Endometrium, Gall Bladder | 24–72y | [5,21,22] |
| Implant | Borderline ovarian tumor, Endometriosis | 28–37y | [23,24] | ||
| Old scar before tumor removal | Hematogenous, Implant | Pancreas, Colon, Ovary | 69–85y | [25,26,27,28,29] | |
| PEG | Abdomen | Hematogenous | Head and Neck | 50–72y | [30] |
| Pacemaker implantation | Breast | Hematogenous | Breast, Lung sarcoma | 82, 89y | [31] |
| Drainage | Abdomen | Implant | Cervix, Ovary | 37, 44y | [5,32] |
| Paracentesis | Abdomen | Implant, Hematogenous | Ovary | 36–67y | [5] |
| Non-SJN Metastasis after Injury | |||||
| Needle biopsy | Chest wall | Implant, Hematogenous | Lung | 79y | [33] |
| Injection | Arm, Abdomen | Hematogenous | Colon, Prostate | 70, 74y | [34,35] |
| Puncture | Hand | Hematogenous | Cervix | 54y | [36] |
| Abrasion | Vulva | Implant | Endometrium (after MIS) | 87y | [37] |
| Body spica cast | Axilla | Hematogenous | Larynx | 58y | [38] |
| Non-SJN Metastasis after Lymphadenopathy | |||||
| Inguinal node met | Lower abdomen, Inguinal area, Thigh | Lymphatic | Cervix, Prostate, Ovary | 47–78y | [39,40,41,42] |
| Axillary node met | Chest wall | Lymphatic | Breast, Ovary | 35–46y | [43,44] |
| Cervical node met | Chest wall, Face | Lymphatic | Cervix | 41y | [45] |
| Other Metastasis | |||||
| Undifferentiated carcinoma | Nasal ala | Hematogenous | Ovary | 58y | [46] |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otsuka, I. Cutaneous Metastasis after Surgery, Injury, Lymphadenopathy, and Peritonitis: Possible Mechanisms. Int. J. Mol. Sci. 2019, 20, 3286. https://doi.org/10.3390/ijms20133286
Otsuka I. Cutaneous Metastasis after Surgery, Injury, Lymphadenopathy, and Peritonitis: Possible Mechanisms. International Journal of Molecular Sciences. 2019; 20(13):3286. https://doi.org/10.3390/ijms20133286
Chicago/Turabian StyleOtsuka, Isao. 2019. "Cutaneous Metastasis after Surgery, Injury, Lymphadenopathy, and Peritonitis: Possible Mechanisms" International Journal of Molecular Sciences 20, no. 13: 3286. https://doi.org/10.3390/ijms20133286
APA StyleOtsuka, I. (2019). Cutaneous Metastasis after Surgery, Injury, Lymphadenopathy, and Peritonitis: Possible Mechanisms. International Journal of Molecular Sciences, 20(13), 3286. https://doi.org/10.3390/ijms20133286





