Molecular-Based Treatment Strategies for Osteoporosis: A Literature Review
Abstract
1. Introduction
2. Calcium
2.1. Mechanism of Action
2.2. Clinical Trials for the Treatment of Osteoporosis
2.3. Adverse Events
3. Vitamin D
3.1. Mechanism of Action
3.2. Clinical Trials for the Treatment of Osteoporosis
3.3. Adverse Events
4. Vitamin K2
4.1. Mechanism of Action
4.2. Clinical Trials for the Treatment of Osteoporosis
4.3. Adverse Events
5. Calcitonin
5.1. Mechanism of Action
5.2. Clinical Trials for the Treatment of Osteoporosis
5.3. Adverse Events
6. Estrogen and Selective Estrogen Receptor Modulators
6.1. Mechanism of Action
6.2. Clinical Trials for the Treatment of Osteoporosis
6.3. Adverse Events
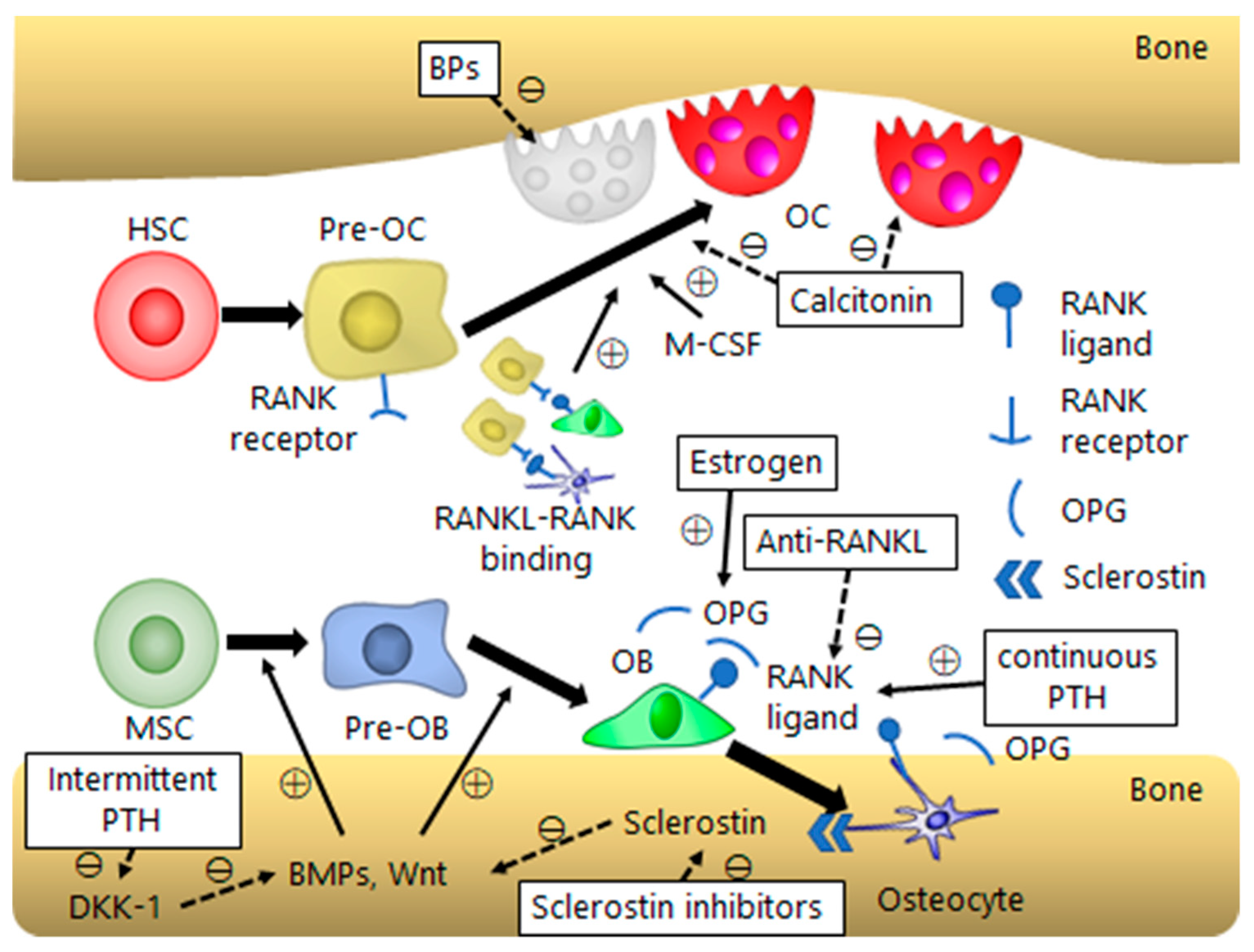
7. Bisphosphonates
7.1. Mechanism of Action
7.2. Clinical Trials for the Treatment of Osteoporosis
7.3. Adverse Events
8. Anti-Receptor Activator of Nuclear Factor κB Ligand Antibody
8.1. Mechanism of Action
8.2. Clinical Trials for the Treatment of Osteoporosis
8.3. Adverse Events
9. Parathyroid Hormone
9.1. Mechanism of Action
9.2. Clinical Trials for the Treatment of Osteoporosis
9.3. Adverse Events
10. Sclerostin Inhibitors
10.1. Mechanism of Action
10.2. Clinical Trials for the Treatment of Osteoporosis
10.3. Adverse Events
11. Combination Therapy
11.1. Mechanism of Action
11.2. Clinical Trials for the Treatment of Osteoporosis
11.2.1. Combination of BPs and Anabolic Agents
11.2.2. Combination of Denosumab and Anabolic Agents
11.2.3. Combination of SERMs and Anabolic Agents
11.3. Adverse Events
12. Stem Cells
12.1. Mechanism of Action
12.2. Clinical Trials for the Treatment of Osteoporosis
12.3. Adverse Events
13. Conclusions and Future Directions
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviations
| AD-MSCs | adipose tissue-derived mesenchymal stem cells |
| ARD | absolute risk difference |
| BMD | bone mineral density |
| BM-MSC | bone marrow-derived mesenchymal stem cell |
| BMP | bone morphogenetic protein |
| BP | bisphosphonate |
| CI | confidence interval |
| DKK | dickkopf |
| ES | embryonic stem |
| FDA | US Food and Drug Administration |
| iPS | induced pluripotent stem |
| iPSC-MSCs | iPS cell-derived MSCs |
| LRP | lipoprotein receptor-related protein |
| MSCs | mesenchymal stem cells |
| OR | odds ratio |
| OPG | osteoprotegerin |
| PTH | parathyroid hormone |
| RCT | randomized controlled trial |
| RR | relative risk |
| Runx2 | runt-related transcription factor 2 |
| RANKL | receptor activator of nuclear factor κB ligand |
| SERM | selective estrogen receptor modulator |
| siRNA | small interfering RNA |
| WMD | weighted mean differences |
References
- Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am. J. Med. 1993, 94, 646–650. [CrossRef]
- Prevention and management of osteoporosis. Available online: https://apps.who.int/iris/handle/10665/42841 (accessed on 22 March 2019).
- Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: Report of a WHO study group. Available online: https://apps.who.int/iris/handle/10665/39142 (accessed on 22 March 2019).
- Lee, R. The outlook for population growth. Science 2011, 333, 569–573. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporosis international. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Raisz, L.G. Pathogenesis of osteoporosis: Concepts, conflicts, and prospects. J. Clin. Investig. 2005, 115, 3318–3325. [Google Scholar] [CrossRef] [PubMed]
- Kawane, T.; Komori, H.; Liu, W.; Moriishi, T.; Miyazaki, T.; Mori, M.; Matsuo, Y.; Takada, Y.; Izumi, S.; Jiang, Q.; et al. Dlx5 and mef2 regulate a novel runx2 enhancer for osteoblast-specific expression. J. Bone Miner. Res. 2014, 29, 1960–1969. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.L.; Hankenson, K.D. Integration of BMP, Wnt, and notch signaling pathways in osteoblast differentiation. J. Cell. Biochem. 2011, 112, 3491–3501. [Google Scholar] [CrossRef]
- Mao, B.; Wu, W.; Davidson, G.; Marhold, J.; Li, M.; Mechler, B.M.; Delius, H.; Hoppe, D.; Stannek, P.; Walter, C.; et al. Kremen proteins are Dickkopf receptors that regulate Wnt/beta-catenin signalling. Nature 2002, 417, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Teitelbaum, S.L. Osteoclasts: New Insights. Bone Res. 2013, 1, 11–26. [Google Scholar]
- Boyle, W.J.; Simonet, W.S.; Lacey, D.L. Osteoclast differentiation and activation. Nature 2003, 423, 337–342. [Google Scholar] [CrossRef]
- Walsh, M.C.; Choi, Y. Biology of the RANKL-RANK-OPG System in Immunity, Bone, and Beyond. Front. Immun. 2014, 5, 511. [Google Scholar] [CrossRef]
- Bonewald, L.F. The amazing osteocyte. J. Bone Miner. Res. 2011, 26, 229–238. [Google Scholar] [CrossRef]
- Shea, B.; Wells, G.; Cranney, A.; Zytaruk, N.; Robinson, V.; Griffith, L.; Ortiz, Z.; Peterson, J.; Adachi, J.; Tugwell, P.; et al. Meta-analyses of therapies for postmenopausal osteoporosis. VII. Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr. Rev. 2002, 23, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Reid, I.R.; Mason, B.; Horne, A.; Ames, R.; Reid, H.E.; Bava, U.; Bolland, M.J.; Gamble, G.D. Randomized controlled trial of calcium in healthy older women. Am. J. Med. 2006, 119, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.M.P.; Eslick, G.D.; Nowson, C.; Smith, C.; Bensoussan, A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: A meta-analysis. Lancet 2007, 370, 657–666. [Google Scholar] [CrossRef]
- Chevalley, T.; Rizzoli, R.; Nydegger, V.; Slosman, D.; Rapin, C.H.; Michel, J.P.; Vasey, H.; Bonjour, J.P. Effects of calcium supplements on femoral bone mineral density and vertebral fracture rate in vitamin-D-replete elderly patients. Osteoporos. Int. 1994, 4, 245–252. [Google Scholar] [CrossRef]
- Hansson, T.; Roos, B. The effect of fluoride and calcium on spinal bone mineral content: A controlled, prospective (3 years) study. Calcif. Tissue Int. 1987, 40, 315–317. [Google Scholar] [CrossRef]
- Recker, R.R.; Hinders, S.; Davies, K.M.; Heaney, R.P.; Stegman, M.R.; Lappe, J.M.; Kimmel, D.B. Correcting calcium nutritional deficiency prevents spine fractures in elderly women. J. Bone Miner. Res. 1996, 11, 1961–1966. [Google Scholar] [CrossRef]
- Reid, I.R.; Ames, R.W.; Evans, M.C.; Gamble, G.D.; Sharpe, S.J. Effect of calcium supplementation on bone loss in postmenopausal women. N. Engl. J. Med. 1993, 328, 460–464. [Google Scholar] [CrossRef]
- Riggs, B.L.; O’Fallon, W.M.; Muhs, J.; O’Connor, M.K.; Kumar, R.; Melton, L.J., 3rd. Long-term effects of calcium supplementation on serum parathyroid hormone level, bone turnover, and bone loss in elderly women. J. Bone Miner. Res. 1998, 13, 168–174. [Google Scholar] [CrossRef]
- Grant, A.M.; Avenell, A.; Campbell, M.K.; McDonald, A.M.; MacLennan, G.S.; McPherson, G.C.; Anderson, F.H.; Cooper, C.; Francis, R.M.; Donaldson, C.; et al. Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): A randomised placebo-controlled trial. Lancet 2005, 365, 1621–1628. [Google Scholar]
- Porthouse, J.; Cockayne, S.; King, C.; Saxon, L.; Steele, E.; Aspray, T.; Baverstock, M.; Birks, Y.; Dumville, J.; Francis, R.; et al. Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ 2005, 330, 1003. [Google Scholar] [CrossRef]
- Prince, R.L.; Devine, A.; Dhaliwal, S.S.; Dick, I.M. Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch. Intern. Med. 2006, 166, 869–875. [Google Scholar] [CrossRef]
- Weaver, C.M.; Alexander, D.D.; Boushey, C.J.; Dawson-Hughes, B.; Lappe, J.M.; LeBoff, M.S.; Liu, S.; Looker, A.C.; Wallace, T.C.; Wang, D.D. Calcium plus vitamin D supplementation and risk of fractures: An updated meta-analysis from the National Osteoporosis Foundation. Osteoporos. Int. 2016, 27, 367–376. [Google Scholar] [CrossRef]
- Kahwati, L.C.; Weber, R.P.; Pan, H.; Gourlay, M.; LeBlanc, E.; Coker-Schwimmer, M.; Viswanathan, M. Vitamin D, Calcium, or Combined Supplementation for the Primary Prevention of Fractures in Community-Dwelling Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2018, 319, 1600–1612. [Google Scholar] [CrossRef]
- Gallagher, J.C.; Rapuri, P.B.; Haynatzki, G.; Detter, J.R. Effect of discontinuation of estrogen, calcitriol, and the combination of both on bone density and bone markers. J. Clin. Endocrinol. Metab. 2002, 87, 4914–4923. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, S.; Moher, D.; Thomas, K.; Hanley, D.A.; Cranney, A. Systematic review of the benefits and harms of calcitriol and alfacalcidol for fractures and falls. J. Bone Miner. Metab. 2008, 26, 531–542. [Google Scholar] [CrossRef]
- Papadimitropoulos, E.; Wells, G.; Shea, B.; Gillespie, W.; Weaver, B.; Zytaruk, N.; Cranney, A.; Adachi, J.; Tugwell, P.; Josse, R.; et al. Meta-analyses of therapies for postmenopausal osteoporosis. VIII: Meta-analysis of the efficacy of vitamin D treatment in preventing osteoporosis in postmenopausal women. Endocr. Rev. 2002, 23, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Richy, F.; Schacht, E.; Bruyere, O.; Ethgen, O.; Gourlay, M.; Reginster, J.Y. Vitamin D analogs versus native vitamin D in preventing bone loss and osteoporosis-related fractures: A comparative meta-analysis. Calcif. Tissue Int. 2005, 76, 176–186. [Google Scholar] [CrossRef]
- Bolland, M.J.; Grey, A.; Avenell, A.; Gamble, G.D.; Reid, I.R. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 2011, 342, d2040. [Google Scholar] [CrossRef] [PubMed]
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; Staehelin, H.B.; Orav, J.E.; Stuck, A.E.; Theiler, R.; Wong, J.B.; Egli, A.; Kiel, D.P.; Henschkowski, J. Fall prevention with supplemental and active forms of vitamin D: A meta-analysis of randomised controlled trials. BMJ 2009, 339, b3692. [Google Scholar] [CrossRef]
- Purwosunu, Y.; Muharram; Rachman, I.A.; Reksoprodjo, S.; Sekizawa, A. Vitamin K2 treatment for postmenopausal osteoporosis in Indonesia. J. Obstet. Gynaecol. Res. 2006, 32, 230–234. [Google Scholar] [CrossRef]
- Shiraki, M.; Shiraki, Y.; Aoki, C.; Miura, M. Vitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosis. J. Bone Miner. Res. 2000, 15, 515–521. [Google Scholar] [CrossRef]
- Ushiroyama, T.; Ikeda, A.; Ueki, M. Effect of continuous combined therapy with vitamin K(2) and vitamin D(3) on bone mineral density and coagulofibrinolysis function in postmenopausal women. Maturitas 2002, 41, 211–221. [Google Scholar] [CrossRef]
- Cockayne, S.; Adamson, J.; Lanham-New, S.; Shearer, M.J.; Gilbody, S.; Torgerson, D.J. Vitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 1256–1261. [Google Scholar] [CrossRef]
- Inoue, T.; Fujita, T.; Kishimoto, H.; Makino, T.; Nakamura, T.; Nakamura, T.; Sato, T.; Yamazaki, K. Randomized controlled study on the prevention of osteoporotic fractures (OF study): A phase IV clinical study of 15-mg menatetrenone capsules. J. Bone Miner. Metab. 2009, 27, 66–75. [Google Scholar] [CrossRef]
- Iwamoto, J. Vitamin K(2) therapy for postmenopausal osteoporosis. Nutrients 2014, 6, 1971–1980. [Google Scholar] [CrossRef]
- Meschia, M.; Brincat, M.; Barbacini, P.; Crossignani, P.G.; Albisetti, W. A clinical trial on the effects of a combination of elcatonin (carbocalcitonin) and conjugated estrogens on vertebral bone mass in early postmenopausal women. Calcif. Tissue Int. 1993, 53, 17–20. [Google Scholar] [CrossRef]
- Ushiroyama, T.; Ikeda, A.; Sakai, M.; Higashiyama, T.; Ueki, M. Effects of the combined use of calcitonin and 1 alpha-hydroxycholecalciferol on vertebral bone loss and bone turnover in women with postmenopausal osteopenia and osteoporosis: A prospective study of long-term and continuous administration with low dose calcitonin. Maturitas 2001, 40, 229–238. [Google Scholar]
- Binkley, N.; Bolognese, M.; Sidorowicz-Bialynicka, A.; Vally, T.; Trout, R.; Miller, C.; Buben, C.E.; Gilligan, J.P.; Krause, D.S.; Oral Calcitonin in Postmenopausal Osteoporosis, I. A phase 3 trial of the efficacy and safety of oral recombinant calcitonin: The Oral Calcitonin in Postmenopausal Osteoporosis (ORACAL) trial. J. Bone Miner. Res. 2012, 27, 1821–1829. [Google Scholar] [CrossRef]
- Ishida, Y.; Kawai, S. Comparative efficacy of hormone replacement therapy, etidronate, calcitonin, alfacalcidol, and vitamin K in postmenopausal women with osteoporosis: The Yamaguchi Osteoporosis Prevention Study. Am. J. Med. 2004, 117, 549–555. [Google Scholar] [CrossRef]
- Rico, H.; Hernandez, E.R.; Revilla, M.; Gomez-Castresana, F. Salmon calcitonin reduces vertebral fracture rate in postmenopausal crush fracture syndrome. Bone Miner. 1992, 16, 131–138. [Google Scholar] [CrossRef]
- Rico, H.; Revilla, M.; Hernandez, E.R.; Villa, L.F.; Alvarez de Buergo, M. Total and regional bone mineral content and fracture rate in postmenopausal osteoporosis treated with salmon calcitonin: A prospective study. Calcif. Tissue Int. 1995, 56, 181–185. [Google Scholar] [CrossRef]
- Knopp-Sihota, J.A.; Newburn-Cook, C.V.; Homik, J.; Cummings, G.G.; Voaklander, D. Calcitonin for treating acute and chronic pain of recent and remote osteoporotic vertebral compression fractures: A systematic review and meta-analysis. Osteoporos. Int. 2012, 23, 17–38. [Google Scholar] [CrossRef]
- Munoz-Torres, M.; Alonso, G.; Raya, M.P. Calcitonin therapy in osteoporosis. Treat. Endocrinol. 2004, 3, 117–132. [Google Scholar] [CrossRef]
- Yoh, K.; Tanaka, K.; Ishikawa, A.; Ishibashi, T.; Uchino, Y.; Sato, Y.; Tobinaga, M.; Hasegawa, N.; Kamae, S.; Yoshizawa, M. Health-related quality of life (HRQOL) in Japanese osteoporotic patients and its improvement by elcatonin treatment. J. Bone Miner. Metab. 2005, 23, 167–173. [Google Scholar] [CrossRef]
- Yoh, K.; Uzawa, T.; Orito, T.; Tanaka, K. Improvement of Quality of Life (QOL) in Osteoporotic Patients by Elcatonin Treatment: A Trial Taking the Participants’ Preference into Account. Jpn. Clin. Med. 2012, 3, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Peichl, P.; Marteau, R.; Griesmacher, A.; Kumpan, W.; Schedl, R.; Prosquil, E.; Fasol, P.; Broll, H. Salmon calcitonin nasal spray treatment for postmenopausal women after hip fracture with total hip arthroplasty. J. Bone Miner. Metab. 2005, 23, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, B.; Black, D.M.; Mitlak, B.H.; Knickerbocker, R.K.; Nickelsen, T.; Genant, H.K.; Christiansen, C.; Delmas, P.D.; Zanchetta, J.R.; Stakkestad, J.; et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 1999, 282, 637–645. [Google Scholar] [CrossRef]
- Zhou, J.; Ma, X.; Wang, T.; Zhai, S. Comparative efficacy of bisphosphonates in short-term fracture prevention for primary osteoporosis: A systematic review with network meta-analyses. Osteoporos. Int. 2016, 27, 3289–3300. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, T.; Zhao, X.; Miller, D.R.; Zhai, S. Comparative Efficacy of Bisphosphonates to Prevent Fracture in Men with Osteoporosis: A Systematic Review with Network Meta-Analyses. Rheumatol. Ther. 2016, 3, 117–128. [Google Scholar] [CrossRef][Green Version]
- Lin, T.; Wang, C.; Cai, X.Z.; Zhao, X.; Shi, M.M.; Ying, Z.M.; Yuan, F.Z.; Guo, C.; Yan, S.G. Comparison of clinical efficacy and safety between denosumab and alendronate in postmenopausal women with osteoporosis: A meta-analysis. Int. J Clin. Pract. 2012, 66, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Matsumoto, T.; Sugimoto, T.; Hosoi, T.; Miki, T.; Gorai, I.; Yoshikawa, H.; Tanaka, Y.; Tanaka, S.; Sone, T.; et al. Clinical Trials Express: fracture risk reduction with denosumab in Japanese postmenopausal women and men with osteoporosis: Denosumab fracture intervention randomized placebo controlled trial (DIRECT). J. Clin. Endocrinol. Metab. 2014, 99, 2599–2607. [Google Scholar] [CrossRef]
- von Keyserlingk, C.; Hopkins, R.; Anastasilakis, A.; Toulis, K.; Goeree, R.; Tarride, J.E.; Xie, F. Clinical efficacy and safety of denosumab in postmenopausal women with low bone mineral density and osteoporosis: A meta-analysis. Semin. Arthritis Rheum. 2011, 41, 178–186. [Google Scholar] [CrossRef]
- Cummings, S.R.; San Martin, J.; McClung, M.R.; Siris, E.S.; Eastell, R.; Reid, I.R.; Delmas, P.; Zoog, H.B.; Austin, M.; Wang, A.; et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N. Engl. J. Med. 2009, 361, 756–765. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhao, J.J.; Mitlak, B.H.; Wang, O.; Genant, H.K.; Eriksen, E.F. Recombinant human parathyroid hormone (1-34) (teriparatide) improves both cortical and cancellous bone structure. J. Bone Miner. Res. 2003, 18, 1932–1941. [Google Scholar] [CrossRef]
- Neer, R.M.; Arnaud, C.D.; Zanchetta, J.R.; Prince, R.; Gaich, G.A.; Reginster, J.Y.; Hodsman, A.B.; Eriksen, E.F.; Ish-Shalom, S.; Genant, H.K.; et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N. Engl. J. Med. 2001, 344, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Leder, B.Z.; O’Dea, L.S.; Zanchetta, J.R.; Kumar, P.; Banks, K.; McKay, K.; Lyttle, C.R.; Hattersley, G. Effects of abaloparatide, a human parathyroid hormone-related peptide analog, on bone mineral density in postmenopausal women with osteoporosis. J. Clin. Endocrinol. Metab. 2015, 100, 697–706. [Google Scholar] [CrossRef]
- Miller, P.D.; Hattersley, G.; Riis, B.J.; Williams, G.C.; Lau, E.; Russo, L.A.; Alexandersen, P.; Zerbini, C.A.; Hu, M.Y.; Harris, A.G.; et al. Effect of Abaloparatide vs Placebo on New Vertebral Fractures in Postmenopausal Women With Osteoporosis: A Randomized Clinical Trial. JAMA 2016, 316, 722–733. [Google Scholar] [CrossRef]
- Cosman, F.; Miller, P.D.; Williams, G.C.; Hattersley, G.; Hu, M.Y.; Valter, I.; Fitzpatrick, L.A.; Riis, B.J.; Christiansen, C.; Bilezikian, J.P.; et al. Eighteen Months of Treatment With Subcutaneous Abaloparatide Followed by 6 Months of Treatment With Alendronate in Postmenopausal Women With Osteoporosis: Results of the ACTIVExtend Trial. Mayo Clin. Proc. 2017, 92, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; Crittenden, D.B.; Adachi, J.D.; Binkley, N.; Czerwinski, E.; Ferrari, S.; Hofbauer, L.C.; Lau, E.; Lewiecki, E.M.; Miyauchi, A.; et al. Romosozumab Treatment in Postmenopausal Women with Osteoporosis. N. Engl. J. Med. 2016, 375, 1532–1543. [Google Scholar] [CrossRef]
- McClung, M.R.; Grauer, A.; Boonen, S.; Bolognese, M.A.; Brown, J.P.; Diez-Perez, A.; Langdahl, B.L.; Reginster, J.Y.; Zanchetta, J.R.; Wasserman, S.M.; et al. Romosozumab in postmenopausal women with low bone mineral density. N. Engl. J. Med. 2014, 370, 412–420. [Google Scholar] [CrossRef]
- Langdahl, B.L.; Libanati, C.; Crittenden, D.B.; Bolognese, M.A.; Brown, J.P.; Daizadeh, N.S.; Dokoupilova, E.; Engelke, K.; Finkelstein, J.S.; Genant, H.K.; et al. Romosozumab (sclerostin monoclonal antibody) versus teriparatide in postmenopausal women with osteoporosis transitioning from oral bisphosphonate therapy: A randomised, open-label, phase 3 trial. Lancet 2017, 390, 1585–1594. [Google Scholar] [CrossRef]
- Saag, K.G.; Petersen, J.; Brandi, M.L.; Karaplis, A.C.; Lorentzon, M.; Thomas, T.; Maddox, J.; Fan, M.; Meisner, P.D.; Grauer, A. Romosozumab or Alendronate for Fracture Prevention in Women with Osteoporosis. N. Engl. J. Med. 2017, 377, 1417–1427. [Google Scholar] [CrossRef]
- Bolland, M.J.; Grey, A.; Reid, I.R. Calcium supplements and cardiovascular risk: 5 years on. Ther. Adv. Drug Saf. 2013, 4, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.R.; Calver, J.; Zhu, K.; Flicker, L.; Prince, R.L. Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.5-year follow-up. J. Bone Miner. Res. 2011, 26, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Bolland, M.J.; Grey, A.; Reid, I.R. Should we prescribe calcium or vitamin D supplements to treat or prevent osteoporosis? Climacteric 2015, 18, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin. Proc. 2006, 81, 353–373. [Google Scholar] [CrossRef]
- Lips, P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: Consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef]
- Sato, Y.; Inose, M.; Higuchi, I.; Higuchi, F.; Kondo, I. Changes in the supporting muscles of the fractured hip in elderly women. Bone 2002, 30, 325–330. [Google Scholar] [CrossRef]
- Okano, T.; Shimomura, Y.; Yamane, M.; Suhara, Y.; Kamao, M.; Sugiura, M.; Nakagawa, K. Conversion of phylloquinone (Vitamin K1) into menaquinone-4 (Vitamin K2) in mice: Two possible routes for menaquinone-4 accumulation in cerebra of mice. J. Biol. Chem. 2008, 283, 11270–11279. [Google Scholar] [CrossRef]
- Shearer, M.J. Vitamin, K. Lancet 1995, 345, 229–234. [Google Scholar] [CrossRef]
- Booth, S.L.; Tucker, K.L.; Chen, H.; Hannan, M.T.; Gagnon, D.R.; Cupples, L.A.; Wilson, P.W.; Ordovas, J.; Schaefer, E.J.; Dawson-Hughes, B.; et al. Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Am. J. Clin. Nutr. 2000, 71, 1201–1208. [Google Scholar] [CrossRef]
- Shiraki, M.; Yamazaki, Y.; Shiraki, Y.; Hosoi, T.; Tsugawa, N.; Okano, T. High level of serum undercarboxylated osteocalcin in patients with incident fractures during bisphosphonate treatment. J. Bone Miner. Metab. 2010, 28, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Shiraki, M.; Itabashi, A. Short-term menatetrenone therapy increases gamma-carboxylation of osteocalcin with a moderate increase of bone turnover in postmenopausal osteoporosis: A randomized prospective study. J. Bone Miner. Metab. 2009, 27, 333–340. [Google Scholar] [CrossRef]
- Asakura, H.; Myou, S.; Ontachi, Y.; Mizutani, T.; Kato, M.; Saito, M.; Morishita, E.; Yamazaki, M.; Nakao, S. Vitamin K administration to elderly patients with osteoporosis induces no hemostatic activation, even in those with suspected vitamin K deficiency. Osteoporos. Int. 2001, 12, 996–1000. [Google Scholar] [CrossRef] [PubMed]
- Ronden, J.E.; Groenen-van Dooren, M.M.; Hornstra, G.; Vermeer, C. Modulation of arterial thrombosis tendency in rats by vitamin K and its side chains. Atherosclerosis 1997, 132, 61–67. [Google Scholar] [CrossRef]
- Felsenfeld, A.J.; Levine, B.S. Calcitonin, the forgotten hormone: Does it deserve to be forgotten? Clin. Kidney J. 2015, 8, 180–187. [Google Scholar] [CrossRef]
- Masi, L.; Brandi, M.L. Calcitonin and calcitonin receptors. Clin. Cases Miner. Bone Metab. 2007, 4, 117–122. [Google Scholar] [PubMed]
- Ikegame, M.; Ejiri, S.; Ozawa, H. Histochemical and autoradiographic studies on elcatonin internalization and intracellular movement in osteoclasts. J. Bone Miner. Res. 1994, 9, 25–37. [Google Scholar] [CrossRef]
- Ito, A.; Kumamoto, E.; Takeda, M.; Shibata, K.; Sagai, H.; Yoshimura, M. Mechanisms for ovariectomy-induced hyperalgesia and its relief by calcitonin: Participation of 5-HT1A-like receptor on C-afferent terminals in substantia gelatinosa of the rat spinal cord. J. Neurosci. 2000, 20, 6302–6308. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Takeda, M.; Yoshimura, T.; Komatsu, T.; Ohno, T.; Kuriyama, H.; Matsuda, A.; Yoshimura, M. Anti-hyperalgesic effects of calcitonin on neuropathic pain interacting with its peripheral receptors. Mol. Pain 2012, 8, 42. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, T.; Ito, A.; Saito, S.Y.; Takeda, M.; Kuriyama, H.; Ishikawa, T. Calcitonin ameliorates enhanced arterial contractility after chronic constriction injury of the sciatic nerve in rats. Fundam. Clin. Pharmacol. 2012, 26, 315–321. [Google Scholar] [CrossRef]
- Overman, R.A.; Borse, M.; Gourlay, M.L. Salmon calcitonin use and associated cancer risk. Ann. Pharmacother. 2013, 47, 1675–1684. [Google Scholar] [CrossRef]
- Sondergaard, B.C.; Catala-Lehnen, P.; Huebner, A.K.; Bay-Jensen, A.C.; Schinke, T.; Henriksen, K.; Schilling, S.; Haberland, M.; Nielsen, R.H.; Amling, M.; et al. Mice over-expressing salmon calcitonin have strongly attenuated osteoarthritic histopathological changes after destabilization of the medial meniscus. Osteoarthritis Cartilage 2012, 20, 136–143. [Google Scholar] [CrossRef]
- Wells, G.; Chernoff, J.; Gilligan, J.P.; Krause, D.S. Does salmon calcitonin cause cancer? A review and meta-analysis. Osteoporos. Int. 2016, 27, 13–19. [Google Scholar] [CrossRef]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R.; National Osteoporosis, F. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef]
- Parfitt, A.M.; Villanueva, A.R.; Foldes, J.; Rao, D.S. Relations between histologic indices of bone formation: Implications for the pathogenesis of spinal osteoporosis. J. Bone Miner. Res. 1995, 10, 466–473. [Google Scholar] [CrossRef]
- Pacifici, R. Estrogen, cytokines, and pathogenesis of postmenopausal osteoporosis. J. Bone Miner. Res. 1996, 11, 1043–1051. [Google Scholar] [CrossRef]
- Almeida, M.; Laurent, M.R.; Dubois, V.; Claessens, F.; O’Brien, C.A.; Bouillon, R.; Vanderschueren, D.; Manolagas, S.C. Estrogens and Androgens in Skeletal Physiology and Pathophysiology. Physiol. Rev. 2017, 97, 135–187. [Google Scholar] [CrossRef]
- Nakamura, T.; Imai, Y.; Matsumoto, T.; Sato, S.; Takeuchi, K.; Igarashi, K.; Harada, Y.; Azuma, Y.; Krust, A.; Yamamoto, Y.; et al. Estrogen prevents bone loss via estrogen receptor alpha and induction of Fas ligand in osteoclasts. Cell 2007, 130, 811–823. [Google Scholar] [CrossRef]
- Almeida, M.; Iyer, S.; Martin-Millan, M.; Bartell, S.M.; Han, L.; Ambrogini, E.; Onal, M.; Xiong, J.; Weinstein, R.S.; Jilka, R.L.; et al. Estrogen receptor-alpha signaling in osteoblast progenitors stimulates cortical bone accrual. J. Clin. Investig. 2013, 123, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Kondoh, S.; Inoue, K.; Igarashi, K.; Sugizaki, H.; Shirode-Fukuda, Y.; Inoue, E.; Yu, T.; Takeuchi, J.K.; Kanno, J.; Bonewald, L.F.; et al. Estrogen receptor alpha in osteocytes regulates trabecular bone formation in female mice. Bone 2014, 60, 68–77. [Google Scholar] [CrossRef]
- Streicher, C.; Heyny, A.; Andrukhova, O.; Haigl, B.; Slavic, S.; Schüler, C.; Kollmann, K.; Kantner, I.; Sexl, V.; Kleiter, M.; et al. Estrogen Regulates Bone Turnover by Targeting RANKL Expression in Bone Lining Cells. Sci. Rep. 2017, 7, 6460. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, J.E.; Anderson, G.L.; Prentice, R.L.; LaCroix, A.Z.; Kooperberg, C.; Stefanick, M.L.; Jackson, R.D.; Beresford, S.A.; Howard, B.V.; Johnson, K.C.; et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results From the Women’s Health Initiative randomized controlled trial. JAMA 2002, 288, 321–333. [Google Scholar]
- Black, D.M.; Delmas, P.D.; Eastell, R.; Reid, I.R.; Boonen, S.; Cauley, J.A.; Cosman, F.; Lakatos, P.; Leung, P.C.; Man, Z.; et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N. Engl. J. Med. 2007, 356, 1809–1822. [Google Scholar] [CrossRef] [PubMed]
- Crandall, C.J.; Newberry, S.J.; Diamant, A.; Lim, Y.W.; Gellad, W.F.; Booth, M.J.; Motala, A.; Shekelle, P.G. Comparative effectiveness of pharmacologic treatments to prevent fractures: An updated systematic review. Ann. Int. Med. 2014, 161, 711–723. [Google Scholar] [CrossRef]
- Cummings, S.R.; Tice, J.A.; Bauer, S.; Browner, W.S.; Cuzick, J.; Ziv, E.; Vogel, V.; Shepherd, J.; Vachon, C.; Smith-Bindman, R.; et al. Prevention of breast cancer in postmenopausal women: Approaches to estimating and reducing risk. J. Natl. Cancer Inst. 2009, 101, 384–398. [Google Scholar] [CrossRef]
- Russell, R.G.; Smith, R.; Preston, C.; Walton, R.J.; Woods, C.G. Diphosphonates in Paget’s disease. Lancet 1974, 1, 894–898. [Google Scholar] [CrossRef]
- Watts, N.B.; Harris, S.T.; Genant, H.K.; Wasnich, R.D.; Miller, P.D.; Jackson, R.D.; Licata, A.A.; Ross, P.; Woodson, G.C., 3rd; Yanover, M.J.; et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N. Engl. J. Med. 1990, 323, 73–79. [Google Scholar] [CrossRef]
- Russell, R.G. Bisphosphonates: The first 40 years. Bone 2011, 49, 2–19. [Google Scholar] [CrossRef]
- Lehenkari, P.P.; Kellinsalmi, M.; Napankangas, J.P.; Ylitalo, K.V.; Monkkonen, J.; Rogers, M.J.; Azhayev, A.; Vaananen, H.K.; Hassinen, I.E. Further insight into mechanism of action of clodronate: Inhibition of mitochondrial ADP/ATP translocase by a nonhydrolyzable, adenine-containing metabolite. Mol. Pharm. 2002, 61, 1255–1262. [Google Scholar] [CrossRef]
- Russell, R.G.; Croucher, P.I.; Rogers, M.J. Bisphosphonates: Pharmacology, mechanisms of action and clinical uses. Osteoporos. Int. 1999, 9, S66–S80. [Google Scholar] [CrossRef]
- Kavanagh, K.L.; Guo, K.; Dunford, J.E.; Wu, X.; Knapp, S.; Ebetino, F.H.; Rogers, M.J.; Russell, R.G.; Oppermann, U. The molecular mechanism of nitrogen-containing bisphosphonates as antiosteoporosis drugs. Proc. Natl. Acad. Sci. USA 2006, 103, 7829–7834. [Google Scholar] [CrossRef]
- Liberman, U.A.; Weiss, S.R.; Broll, J.; Minne, H.W.; Quan, H.; Bell, N.H.; Rodriguez-Portales, J.; Downs, R.W., Jr.; Dequeker, J.; Favus, M. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N. Engl. J. Med. 1995, 333, 1437–1443. [Google Scholar] [CrossRef]
- Tabatabaei-Malazy, O.; Salari, P.; Khashayar, P.; Larijani, B. New horizons in treatment of osteoporosis. Daru 2017, 25, 2. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, E.; Masson, C.; Laffitte, A.; Chappard, D.; Audran, M. Osteomalacia in a patient with Paget’s bone disease treated with long-term etidronate. Morphologie 2012, 96, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Black, D.M.; Rosen, C.J. Postmenopausal Osteoporosis. N. Engl. J. Med. 2016, 374, 2096–2097. [Google Scholar] [CrossRef]
- Khosla, S.; Hofbauer, L.C. Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol. 2017, 5, 898–907. [Google Scholar] [CrossRef]
- Santini, D.; Vincenzi, B.; Avvisati, G.; Dicuonzo, G.; Battistoni, F.; Gavasci, M.; Salerno, A.; Denaro, V.; Tonini, G. Pamidronate induces modifications of circulating angiogenetic factors in cancer patients. Clin. Cancer Res. 2002, 8, 1080–1084. [Google Scholar] [CrossRef]
- Delmas, P.D. Clinical potential of RANKL inhibition for the management of postmenopausal osteoporosis and other metabolic bone diseases. J. Clin. Densitom. 2008, 11, 325–338. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, H.; Shima, N.; Nakagawa, N.; Yamaguchi, K.; Kinosaki, M.; Mochizuki, S.; Tomoyasu, A.; Yano, K.; Goto, M.; Murakami, A.; et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. USA 1998, 95, 3597–3602. [Google Scholar] [CrossRef]
- Burkiewicz, J.S.; Scarpace, S.L.; Bruce, S.P. Denosumab in osteoporosis and oncology. Ann. Pharmacother. 2009, 43, 1445–1455. [Google Scholar] [CrossRef]
- Bone, H.G.; Bolognese, M.A.; Yuen, C.K.; Kendler, D.L.; Miller, P.D.; Yang, Y.C.; Grazette, L.; San Martin, J.; Gallagher, J.C. Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J. Clin. Endocrinol. Metab. 2011, 96, 972–980. [Google Scholar] [CrossRef]
- Selga, J.; Nunez, J.H.; Minguell, J.; Lalanza, M.; Garrido, M. Simultaneous bilateral atypical femoral fracture in a patient receiving denosumab: Case report and literature review. Osteoporos. Int. 2016, 27, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Cernes, R.; Barnea, Z.; Biro, A.; Zandman-Goddard, G.; Katzir, Z. Severe Hypocalcemia Following a Single Denosumab Injection. IMAJ 2017, 19, 719–721. [Google Scholar]
- Yoshimura, H.; Ohba, S.; Yoshida, H.; Saito, K.; Inui, K.; Yasui, R.; Ichikawa, D.; Aiki, M.; Kobayashi, J.; Matsuda, S.; et al. Denosumab-related osteonecrosis of the jaw in a patient with bone metastases of prostate cancer: A case report and literature review. Oncol. Lett. 2017, 14, 127–136. [Google Scholar] [CrossRef]
- Bone, H.G.; Chapurlat, R.; Brandi, M.L.; Brown, J.P.; Czerwinski, E.; Krieg, M.A.; Mellstrom, D.; Radominski, S.C.; Reginster, J.Y.; Resch, H.; et al. The effect of three or six years of denosumab exposure in women with postmenopausal osteoporosis: results from the FREEDOM extension. J. Clin. Endocrinol. Metab. 2013, 98, 4483–4492. [Google Scholar] [CrossRef] [PubMed]
- Hock, J.M.; Gera, I. Effects of continuous and intermittent administration and inhibition of resorption on the anabolic response of bone to parathyroid hormone. J. Bone Miner. Res. 1992, 7, 65–72. [Google Scholar] [CrossRef]
- Rutkovskiy, A.; Stenslokken, K.O.; Vaage, I.J. Osteoblast Differentiation at a Glance. Med. Sci. Monit. Basic Res. 2016, 22, 95–106. [Google Scholar] [CrossRef]
- Osagie-Clouard, L.; Sanghani, A.; Coathup, M.; Briggs, T.; Bostrom, M.; Blunn, G. Parathyroid hormone 1-34 and skeletal anabolic action: The use of parathyroid hormone in bone formation. Bone Joint Res. 2017, 6, 14–21. [Google Scholar] [CrossRef]
- Hattersley, G.; Dean, T.; Corbin, B.A.; Bahar, H.; Gardella, T.J. Binding Selectivity of Abaloparatide for PTH-Type-1-Receptor Conformations and Effects on Downstream Signaling. Endocrinology 2016, 157, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Vahle, J.L.; Long, G.G.; Sandusky, G.; Westmore, M.; Ma, Y.L.; Sato, M. Bone neoplasms in F344 rats given teriparatide (rhPTH(1-34)) are dependent on duration of treatment and dose. Toxic. Pathol. 2004, 32, 426–438. [Google Scholar] [CrossRef]
- Jolette, J.; Attalla, B.; Varela, A.; Long, G.G.; Mellal, N.; Trimm, S.; Smith, S.Y.; Ominsky, M.S.; Hattersley, G. Comparing the incidence of bone tumors in rats chronically exposed to the selective PTH type 1 receptor agonist abaloparatide or PTH(1-34). Regul. Toxic. Pharm. 2017, 86, 356–365. [Google Scholar] [CrossRef] [PubMed]
- Andrews, E.B.; Gilsenan, A.W.; Midkiff, K.; Sherrill, B.; Wu, Y.; Mann, B.H.; Masica, D. The US postmarketing surveillance study of adult osteosarcoma and teriparatide: study design and findings from the first 7 years. J. Bone Miner. Res. 2012, 27, 2429–2437. [Google Scholar] [CrossRef]
- Long, F. Building strong bones: molecular regulation of the osteoblast lineage. Nature reviews. Mol. Cell Biol. 2011, 13, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Ott, S.M. Sclerostin and Wnt signaling--the pathway to bone strength. J. Clin. Endocrinol. Metab. 2005, 90, 6741–6743. [Google Scholar] [CrossRef]
- ten Dijke, P.; Krause, C.; de Gorter, D.J.; Lowik, C.W.; van Bezooijen, R.L. Osteocyte-derived sclerostin inhibits bone formation: Its role in bone morphogenetic protein and Wnt signaling. J. Bone Joint Surg. Am. 2008, 90, 31–35. [Google Scholar] [CrossRef]
- Winkler, D.G.; Sutherland, M.K.; Geoghegan, J.C.; Yu, C.; Hayes, T.; Skonier, J.E.; Shpektor, D.; Jonas, M.; Kovacevich, B.R.; Staehling-Hampton, K.; et al. Osteocyte control of bone formation via sclerostin, a novel BMP antagonist. EMBO 2003, 22, 6267–6276. [Google Scholar] [CrossRef]
- Compton, J.T.; Lee, F.Y. A review of osteocyte function and the emerging importance of sclerostin. J. Bone Joint Surg. Am. 2014, 96, 1659–1668. [Google Scholar] [CrossRef]
- Poole, K.E.; van Bezooijen, R.L.; Loveridge, N.; Hamersma, H.; Papapoulos, S.E.; Lowik, C.W.; Reeve, J. Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB 2005, 19, 1842–1844. [Google Scholar] [CrossRef]
- Weivoda, M.M.; Youssef, S.J.; Oursler, M.J. Sclerostin expression and functions beyond the osteocyte. Bone 2017, 96, 45–50. [Google Scholar] [CrossRef]
- Balemans, W.; Ebeling, M.; Patel, N.; Van Hul, E.; Olson, P.; Dioszegi, M.; Lacza, C.; Wuyts, W.; Van Den Ende, J.; Willems, P.; et al. Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum. Mol. Genet. 2001, 10, 537–543. [Google Scholar] [CrossRef]
- Brunkow, M.E.; Gardner, J.C.; Van Ness, J.; Paeper, B.W.; Kovacevich, B.R.; Proll, S.; Skonier, J.E.; Zhao, L.; Sabo, P.J.; Fu, Y.; et al. Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am. J. Hum. Genet. 2001, 68, 577–589. [Google Scholar] [CrossRef]
- van Bezooijen, R.L.; Deruiter, M.C.; Vilain, N.; Monteiro, R.M.; Visser, A.; van der Wee-Pals, L.; van Munsteren, C.J.; Hogendoorn, P.C.; Aguet, M.; Mummery, C.L.; et al. SOST expression is restricted to the great arteries during embryonic and neonatal cardiovascular development. Dev. Dyn. 2007, 236, 606–612. [Google Scholar] [CrossRef]
- Liu, Y.; Cao, Y.; Zhang, S.; Zhang, W.; Zhang, B.; Tang, Q.; Li, Z.; Wu, J. Romosozumab treatment in postmenopausal women with osteoporosis: A meta-analysis of randomized controlled trials. Climacteric 2018, 1–7. [Google Scholar] [CrossRef] [PubMed]
- McClung, M.R. Sclerostin antibodies in osteoporosis: Latest evidence and therapeutic potential. Ther. Adv. Musculoskelet. Dis. 2017, 9, 263–270. [Google Scholar] [CrossRef]
- Heath, D.J.; Chantry, A.D.; Buckle, C.H.; Coulton, L.; Shaughnessy, J.D., Jr.; Evans, H.R.; Snowden, J.A.; Stover, D.R.; Vanderkerken, K.; Croucher, P.I. Inhibiting Dickkopf-1 (Dkk1) removes suppression of bone formation and prevents the development of osteolytic bone disease in multiple myeloma. J. Bone Miner. Res. 2009, 24, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.P.; Beck, J.T.; Stewart, A.K.; Shah, J.; Kelly, K.R.; Isaacs, R.; Bilic, S.; Sen, S.; Munshi, N.C. A Phase IB multicentre dose-determination study of BHQ880 in combination with anti-myeloma therapy and zoledronic acid in patients with relapsed or refractory multiple myeloma and prior skeletal-related events. Brit. J. Haemat. 2014, 167, 366–375. [Google Scholar] [CrossRef]
- Florio, M.; Gunasekaran, K.; Stolina, M.; Li, X.; Liu, L.; Tipton, B.; Salimi-Moosavi, H.; Asuncion, F.J.; Li, C.; Sun, B.; et al. A bispecific antibody targeting sclerostin and DKK-1 promotes bone mass accrual and fracture repair. Nat. Commun. 2016, 7, 11505. [Google Scholar] [CrossRef]
- McClung, M.R. Using Osteoporosis Therapies in Combination. Curr. Osteoporos. Rep. 2017, 15, 343–352. [Google Scholar] [CrossRef]
- Lou, S.; Lv, H.; Yin, P.; Li, Z.; Tang, P.; Wang, Y. Combination therapy with parathyroid hormone analogs and antiresorptive agents for osteoporosis: A systematic review and meta-analysis of randomized controlled trials. Osteoporos. Int. 2019, 30, 59–70. [Google Scholar] [CrossRef]
- Black, D.M.; Greenspan, S.L.; Ensrud, K.E.; Palermo, L.; McGowan, J.A.; Lang, T.F.; Garnero, P.; Bouxsein, M.L.; Bilezikian, J.P.; Rosen, C.J. The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N. Engl. J. Med. 2003, 349, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.S.; Hayes, A.; Hunzelman, J.L.; Wyland, J.J.; Lee, H.; Neer, R.M. The effects of parathyroid hormone, alendronate, or both in men with osteoporosis. N. Engl. J. Med. 2003, 349, 1216–1226. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.S.; Wyland, J.J.; Lee, H.; Neer, R.M. Effects of teriparatide, alendronate, or both in women with postmenopausal osteoporosis. J. Clin. Endocrinol. Metab. 2010, 95, 1838–1845. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; Eriksen, E.F.; Recknor, C.; Miller, P.D.; Guanabens, N.; Kasperk, C.; Papanastasiou, P.; Readie, A.; Rao, H.; Gasser, J.A.; et al. Effects of intravenous zoledronic acid plus subcutaneous teriparatide (rhPTH(1-34)) in postmenopausal osteoporosis. J. Bone Miner. Res. 2011, 26, 503–511. [Google Scholar] [CrossRef]
- Walker, M.D.; Cusano, N.E.; Sliney, J., Jr.; Romano, M.; Zhang, C.; McMahon, D.J.; Bilezikian, J.P. Combination therapy with risedronate and teriparatide in male osteoporosis. Endocrine 2013, 44, 237–246. [Google Scholar] [CrossRef]
- Furuya, Y.; Mori, K.; Ninomiya, T.; Tomimori, Y.; Tanaka, S.; Takahashi, N.; Udagawa, N.; Uchida, K.; Yasuda, H. Increased bone mass in mice after single injection of anti-receptor activator of nuclear factor-kappaB ligand-neutralizing antibody: Evidence for bone anabolic effect of parathyroid hormone in mice with few osteoclasts. J. Biol. Chem. 2011, 286, 37023–37031. [Google Scholar] [CrossRef]
- Kitaguchi, K.; Kashii, M.; Ebina, K.; Kaito, T.; Okada, R.; Makino, T.; Noguchi, T.; Ishimoto, T.; Nakano, T.; Yoshikawa, H. Effects of single or combination therapy of teriparatide and anti-RANKL monoclonal antibody on bone defect regeneration in mice. Bone 2018, 106, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.N.; Uihlein, A.V.; Lee, H.; Kumbhani, R.; Siwila-Sackman, E.; McKay, E.A.; Burnett-Bowie, S.A.; Neer, R.M.; Leder, B.Z. Teriparatide and denosumab, alone or combined, in women with postmenopausal osteoporosis: The DATA study randomised trial. Lancet 2013, 382, 50–56. [Google Scholar] [CrossRef]
- Leder, B.Z.; Tsai, J.N.; Uihlein, A.V.; Burnett-Bowie, S.A.; Zhu, Y.; Foley, K.; Lee, H.; Neer, R.M. Two years of Denosumab and teriparatide administration in postmenopausal women with osteoporosis (The DATA Extension Study): A randomized controlled trial. J. Clin. Endocrinol. Metab. 2014, 99, 1694–1700. [Google Scholar] [CrossRef]
- Nakamura, Y.; Suzuki, T.; Kamimura, M.; Ikegami, S.; Murakami, K.; Uchiyama, S.; Taguchi, A.; Kato, H. Two-year clinical outcome of denosumab treatment alone and in combination with teriparatide in Japanese treatment-naive postmenopausal osteoporotic women. Bone Res. 2017, 5, 16055. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; Wermers, R.A.; Recknor, C.; Mauck, K.F.; Xie, L.; Glass, E.V.; Krege, J.H. Effects of teriparatide in postmenopausal women with osteoporosis on prior alendronate or raloxifene: Differences between stopping and continuing the antiresorptive agent. J. Clin. Endocrinol. Metab. 2009, 94, 3772–3780. [Google Scholar] [CrossRef]
- Muschitz, C.; Kocijan, R.; Fahrleitner-Pammer, A.; Lung, S.; Resch, H. Antiresorptives overlapping ongoing teriparatide treatment result in additional increases in bone mineral density. J. Bone Miner. Res. 2013, 28, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Tanabe, K.; Ohnuki, M.; Narita, M.; Ichisaka, T.; Tomoda, K.; Yamanaka, S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 2007, 131, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Zhang, P.; Xue, S.; Xu, Y.; Tan, J.; Liu, G. Adipose-derived stem cells alleviate osteoporosis by enhancing osteogenesis and inhibiting adipogenesis in a rabbit model. Cytotherapy 2014, 16, 1643–1655. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Kim, H.; Kim, J.M.; Kim, J.R.; Kim, K.J.; Kim, Y.J.; Park, S.I.; Jeong, J.H.; Moon, Y.M.; Lim, H.S.; et al. Systemic transplantation of human adipose-derived stem cells stimulates bone repair by promoting osteoblast and osteoclast function. J. Cell. Mol. Med. 2011, 15, 2082–2094. [Google Scholar] [CrossRef] [PubMed]
- Aghebati-Maleki, L.; Dolati, S.; Zandi, R.; Fotouhi, A.; Ahmadi, M.; Aghebati, A.; Nouri, M.; Kazem Shakouri, S.; Yousefi, M. Prospect of mesenchymal stem cells in therapy of osteoporosis: A review. J. Cell. Physiol. 2019, 234, 8570–8578. [Google Scholar] [CrossRef]
- Kiernan, J.; Hu, S.; Grynpas, M.D.; Davies, J.E.; Stanford, W.L. Systemic Mesenchymal Stromal Cell Transplantation Prevents Functional Bone Loss in a Mouse Model of Age-Related Osteoporosis. Stem cells Transl. Med. 2016, 5, 683–693. [Google Scholar] [CrossRef]
- An, J.H.; Park, H.; Song, J.A.; Ki, K.H.; Yang, J.Y.; Choi, H.J.; Cho, S.W.; Kim, S.W.; Kim, S.Y.; Yoo, J.J.; et al. Transplantation of human umbilical cord blood-derived mesenchymal stem cells or their conditioned medium prevents bone loss in ovariectomized nude mice. Tissue Engin. Part. A 2013, 19, 685–696. [Google Scholar] [CrossRef]
- Villa-Diaz, L.G.; Brown, S.E.; Liu, Y.; Ross, A.M.; Lahann, J.; Parent, J.M.; Krebsbach, P.H. Derivation of mesenchymal stem cells from human induced pluripotent stem cells cultured on synthetic substrates. Stem Cells 2012, 30, 1174–1181. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Zhang, J.; Yuan, H.; Xu, Z.; Li, Q.; Niu, X.; Hu, B.; Wang, Y.; Li, X. Exosomes Secreted by Human-Induced Pluripotent Stem Cell-Derived Mesenchymal Stem Cells Repair Critical-Sized Bone Defects through Enhanced Angiogenesis and Osteogenesis in Osteoporotic Rats. Int. J. Biol. Sci. 2016, 12, 836–849. [Google Scholar] [CrossRef]
- Lalu, M.M.; McIntyre, L.; Pugliese, C.; Fergusson, D.; Winston, B.W.; Marshall, J.C.; Granton, J.; Stewart, D.J. Safety of cell therapy with mesenchymal stromal cells (SafeCell): A systematic review and meta-analysis of clinical trials. PloS ONE 2012, 7, e47559. [Google Scholar] [CrossRef] [PubMed]
- Antebi, B.; Pelled, G.; Gazit, D. Stem cell therapy for osteoporosis. Curr. Osteoporos. Rep. 2014, 12, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Nishimori, M.; Yakushiji, H.; Mori, M.; Miyamoto, T.; Yaguchi, T.; Ohno, S.; Miyake, Y.; Sakaguchi, T.; Ueda, M.; Ohno, E. Tumorigenesis in cells derived from induced pluripotent stem cells. Hum. Cell 2014, 27, 29–35. [Google Scholar] [CrossRef]
- Phetfong, J.; Sanvoranart, T.; Nartprayut, K.; Nimsanor, N.; Seenprachawong, K.; Prachayasittikul, V.; Supokawej, A. Osteoporosis: The current status of mesenchymal stem cell-based therapy. Cell. Mol. Biol. Lett. 2016, 21, 12. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Grainger, D.W. Developing siRNA therapies to address osteoporosis. Ther. Deliv. 2013, 4, 1239–1246. [Google Scholar] [CrossRef]
| Agents | Mechanism of Action | Effect on Bone Metabolism | Side Effects | Clinical Trials and Meta-Analysis |
|---|---|---|---|---|
| Calcium | Reduction of PTH release | Inhibition of bone resorption | Gastrointestinal disorders Hypercalcemia | [14,15,16,17,18,19,20,21,22,23,24,25,26] |
| Vitamin D | Modulation of the calcium metabolism | Inhibition of bone resorption | Appears to be safe | [27,28,29,30,31,32] |
| Vitamin K2 | Help of the osteocalcin γ-carboxylation | Activation of bone formation | Appears to be safe | [33,34,35,36,37,38] |
| Calcitonin | Regulation of osteoclast function Prevention of osteoclast precursors from maturing | Inhibition of bone resorption | Gastrointestinal disorders Hypocalcemia Weak association between malignant tumor | [39,40,41,42,43,44,45,46,47,48,49] |
| SERMs | Interaction with RANKL/RANK/OPG system | Inhibition of bone resorption | Thromboembolic events Pulmonary embolism Fatal strokes | [50] |
| Bisphosphonates | Induction of osteoclast apoptosis | Inhibition of bone resorption | Gastrointestinal disorders Osteonecrosis of the jaw Atypical femoral fractures Acute renal failure | [51,52] |
| Anti-RANKL antibody | Prevention of the RANKL/RANK system | Inhibition of bone resorption | Osteonecrosis of the jaw Atypical fracture Hypocalcemia | [53,54,55,56] |
| PTH | Stimulation of osteoblast differentiation | Activation of bone formation (intermittent PTH) | Hypercalcemia Increasing risk of osteosarcoma | [57,58,59,60,61] |
| Sclerostin inhibitors | Regulation of BMP and Wnt signaling | Activation of bone formation | Cardiac ischemic event | [62,63,64,65] |
| Stem cells | Differentiate into osteoblasts directly Secretion of various growth factors | Supplementation of cell source for osteoblasts | Appears to be safe | N/A |
| Anabolic Agent | Anti-Resorptive Agent | Main Therapeutic Effect Compared to Effect of Either Therapy | References |
|---|---|---|---|
| PTH (teriparatide) | BP (alendronate, intravenous zoledronic acid) | More rapid BMD increase Greater increase in total hip BMD | [144,145,146,147,148] |
| Anti-RANKL antibody (denosumab) | Greater increase in lumbar spine, femoral neck, total hip BMD | [151,152,153] | |
| SERM (raloxifene) | Greater increase in lumbar spine BMD | [154,155] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ukon, Y.; Makino, T.; Kodama, J.; Tsukazaki, H.; Tateiwa, D.; Yoshikawa, H.; Kaito, T. Molecular-Based Treatment Strategies for Osteoporosis: A Literature Review. Int. J. Mol. Sci. 2019, 20, 2557. https://doi.org/10.3390/ijms20102557
Ukon Y, Makino T, Kodama J, Tsukazaki H, Tateiwa D, Yoshikawa H, Kaito T. Molecular-Based Treatment Strategies for Osteoporosis: A Literature Review. International Journal of Molecular Sciences. 2019; 20(10):2557. https://doi.org/10.3390/ijms20102557
Chicago/Turabian StyleUkon, Yuichiro, Takahiro Makino, Joe Kodama, Hiroyuki Tsukazaki, Daisuke Tateiwa, Hideki Yoshikawa, and Takashi Kaito. 2019. "Molecular-Based Treatment Strategies for Osteoporosis: A Literature Review" International Journal of Molecular Sciences 20, no. 10: 2557. https://doi.org/10.3390/ijms20102557
APA StyleUkon, Y., Makino, T., Kodama, J., Tsukazaki, H., Tateiwa, D., Yoshikawa, H., & Kaito, T. (2019). Molecular-Based Treatment Strategies for Osteoporosis: A Literature Review. International Journal of Molecular Sciences, 20(10), 2557. https://doi.org/10.3390/ijms20102557






