Emerging Roles of Estrogen-Related Receptors in the Brain: Potential Interactions with Estrogen Signaling
Abstract
1. Introduction: Estrogen Receptors (ERs) and Estrogen-Related Receptors (ERRs)
2. ERs and Their Modes of Action
3. ERRs and Their Potential Ligands
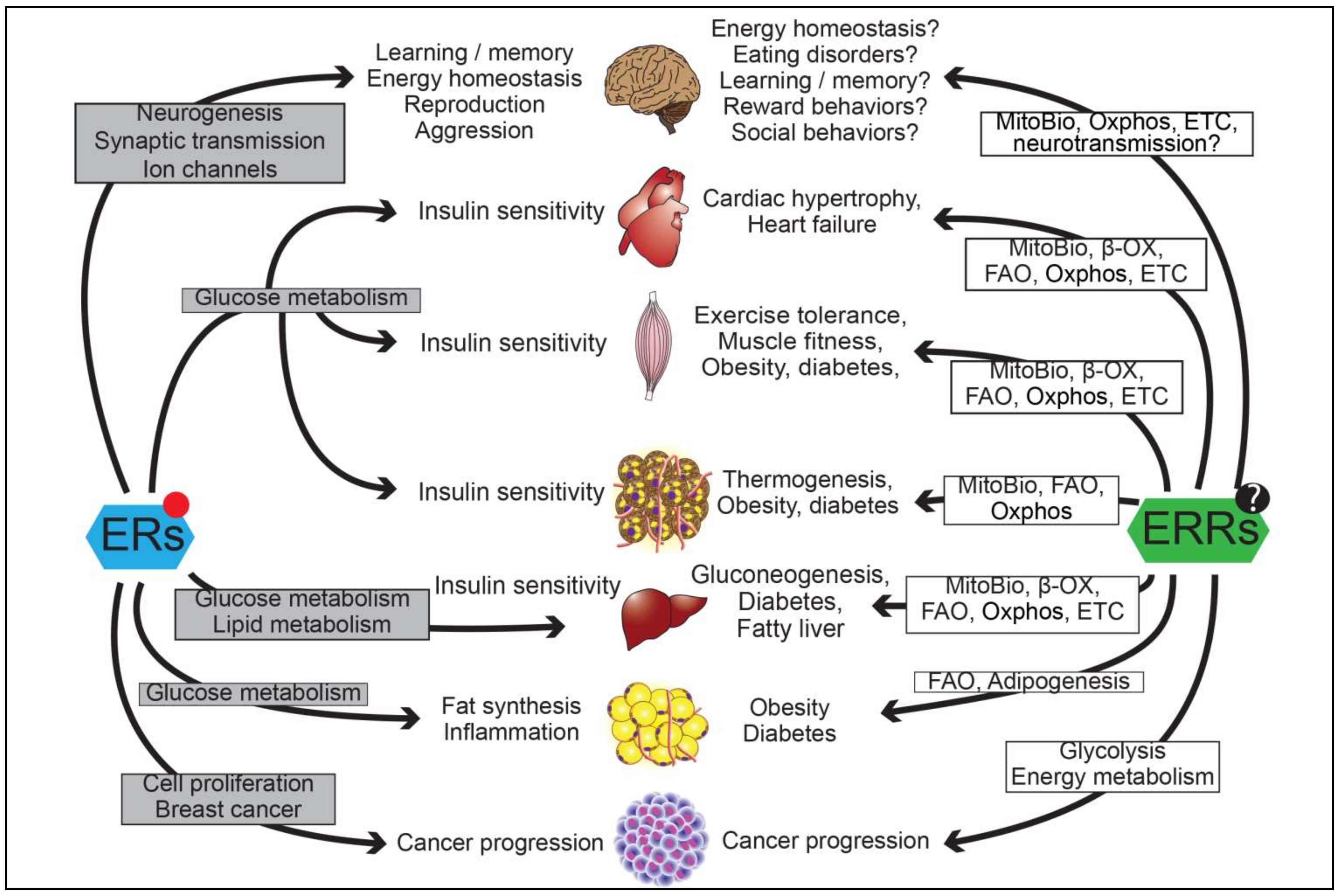
4. Transcriptional Regulations by Both ERs and ERRs
5. Functions of ERs and ERRs in the Brain
5.1. Actions in the Central Regulation of Energy Homeostasis
5.2. Actions in Learning and Memory
5.3. Actions in Social Behaviors
6. Concluding Remark
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| AgRP | Agouti-Related Peptide |
| Akt | Protein Kinase B |
| ARC | Arcuate nucleus Of Hypothalamus |
| BDNF | Brain-Derived Neurotrophic Factor |
| β-OX | β-Oxidation |
| ChIP | Chromatin Immunoprecipitation |
| CYP19 | Aromatase |
| DBD | DNA Binding Domain |
| dmPFC | Dorsomedial Prefrontal Cortex |
| DPN | Diaryl-Propionitrile |
| E2 | 17β-Estradiol |
| ER | Estrogen Receptor |
| ERE | Estrogen Response Element |
| ERR | Estrogen-Related Receptor |
| ERRE | Estrogen-Related Response Element |
| ERK | Extracellular Signal-Regulated Kinase |
| ETC | Electron Transport Chain |
| FAO | Fatty Acid Oxidation |
| FNDC5 | Fibronectin Type III Domain Containing 5 |
| GPER | G protein-Coupled Estrogen Receptor |
| HFD | High Fat Diet |
| IHC | Immunohistochemistry |
| LTP | Long-Term Potenciation |
| MeA | Medial Amygdala |
| MHRE | Multiple-Hormone Response element |
| MitoBio | Mitochondrial Biogenesis |
| NPY | Neuropeptide |
| NTS | Nucleus of Solitary Tract |
| Oxphos | Oxidative Phosphorylation |
| PV | Parvalbumin |
| PGC | Proliferator-Activated Receptor γ Coactivator |
| PI3K | Phosphatidyl Inositide 3-Kinase |
| POMC | Pro-Opiomelanocortin |
| PPT | Propyl-Pyrazole Triol |
| VMH | Ventromedial Nucleus of Hypothalamus |
| VTA | Ventral Tegmental Area |
References
- Klinge, C.M. Estrogen receptor interaction with co-activators and co-repressors. Steroids 2000, 65, 227–251. [Google Scholar] [CrossRef]
- Pettersson, K.; Svensson, K.; Mattsson, R.; Carlsson, B.; Ohlsson, R.; Berkenstam, A. Expression of a novel member of estrogen response element-binding nuclear receptors is restricted to the early stages of chorion formation during mouse embryogenesis. Mech. Dev. 1996, 54, 211–223. [Google Scholar] [CrossRef]
- Giguère, V.; Yang, N.; Segui, P.; Evans, R.M. Identification of a new class of steroid hormone receptors. Nature 1988, 331, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Huss, J.M.; Garbacz, W.G.; Xie, W. Constitutive activities of estrogen-related receptors: Transcriptional regulation of metabolism by the ERR pathways in health and disease. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2015, 1852, 1912–1927. [Google Scholar] [CrossRef] [PubMed]
- Gearhart, M.D.; Holmbeck, S.M.A.; Evans, R.M.; Dyson, H.J.; Wright, P.E. Monomeric complex of human orphan estrogen related receptor-2 with DNA: A pseudo-dimer interface mediates extended half-site recognition. J. Mol. Biol. 2003, 327, 819–832. [Google Scholar] [CrossRef]
- Huppunen, J.; Aarnisalo, P. Dimerization modulates the activity of the orphan nuclear receptor ERRgamma. Biochem. Biophys. Res. Commun. 2004, 314, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Vanacker, J.M.; Pettersson, K.; Gustafsson, J.A.; Laudet, V. Transcriptional targets shared by estrogen receptor-related receptors (ERRs) and estrogen receptor (ER) alpha, but not by ERbeta. EMBO J. 1999, 18, 4270–4279. [Google Scholar] [CrossRef] [PubMed]
- Giguère, V. Transcriptional control of energy homeostasis by the estrogen-related receptors. Endocr. Rev. 2008, 29, 677–696. [Google Scholar] [CrossRef] [PubMed]
- Bookout, A.L.; Jeong, Y.; Downes, M.; Yu, R.T.; Evans, R.M.; Mangelsdorf, D.J. Anatomical profiling of nuclear receptor expression reveals a hierarchical transcriptional network. Cell 2006, 126, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Jakacka, M.; Ito, M.; Martinson, F.; Ishikawa, T.; Lee, E.J.; Jameson, J.L. An Estrogen Receptor (ER)α Deoxyribonucleic Acid-Binding Domain Knock-In Mutation Provides Evidence for Nonclassical ER Pathway Signaling In Vivo. Mol. Endocrinol. 2002, 16, 2188–2201. [Google Scholar] [CrossRef] [PubMed]
- Park, C.J.; Zhao, Z.; Glidewell-Kenney, C.; Lazic, M.; Chambon, P.; Krust, A.; Weiss, J.; Clegg, D.J.; Dunaif, A.; Jameson, J.L.; et al. Genetic rescue of nonclassical ERalpha signaling normalizes energy balance in obese Eralpha-null mutant mice. J. Clin. Investig. 2011, 121, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Malyala, A.; Zhang, C.; Bryant, D.N.; Kelly, M.J.; Rønnekleiv, O.K. PI3K signaling effects in hypothalamic neurons mediated by estrogen. J. Comp. Neurol. 2008, 506, 895–911. [Google Scholar] [CrossRef] [PubMed]
- Micevych, P.E.; Kelly, M.J. Membrane estrogen receptor regulation of hypothalamic function. Neuroendocrinology 2012, 96, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; He, Y.; Yang, Y.; Zhu, L.; Wang, C.; Xu, P.; Hinton, A.O.; Yan, X.; Zhao, J.; Fukuda, M.; et al. PI3K in the ventromedial hypothalamic nucleus mediates estrogenic actions on energy expenditure in female mice. Sci. Rep. 2016, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Xu, P.; Cao, X.; Yang, Y.; Hinton, A.O.; Xia, Y.; Saito, K.; Yan, X.; Zou, F.; Ding, H.; et al. The ERα-PI3K cascade in proopiomelanocortin progenitor neurons regulates feeding and glucose balance in female mice. Endocrinology 2015, 156, 4474–4491. [Google Scholar] [CrossRef] [PubMed]
- Carmeci, C.; Thompson, D.A.; Ring, H.Z.; Francke, U.; Weigel, R.J. Identification of a gene (GPR30) with homology to the G-protein-coupled receptor superfamily associated with estrogen receptor expression in breast cancer. Genomics 1997, 45, 607–617. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, B.F.; Nguyen, T.; Marchese, A.; Cheng, R.; Lynch, K.R.; Heng, H.H.; Kolakowski, L.F.; George, S.R. Discovery of three novel G-protein-coupled receptor genes. Genomics 1998, 47, 310–313. [Google Scholar] [CrossRef] [PubMed]
- Owman, C.; Nilsson, C.; Lolait, S.J. Cloning of cDNA encoding a putative chemoattractant receptor. Genomics 1996, 37, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Takada, Y.; Kato, C.; Kondo, S.; Korenaga, R.; Ando, J. Cloning of cDNAs encoding G protein-coupled receptor expressed in human endothelial cells exposed to fluid shear stress. Biochem. Biophys. Res. Commun. 1997, 240, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.E.; Carstens, E.J.; Irani, B.G.; Gent, L.M.; Hahner, L.M.; Clegg, D.J. Sexually dimorphic role of G protein-coupled estrogen receptor (GPER) in modulating energy homeostasis. Horm. Behav. 2014, 66, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Isensee, J.; Meoli, L.; Zazzu, V.; Nabzdyk, C.; Witt, H.; Soewarto, D.; Effertz, K.; Fuchs, H.; Gailus-Durner, V.; Busch, D.; et al. Expression pattern of G protein-coupled receptor 30 in LacZ reporter mice. Endocrinology 2009, 150, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Kwon, O.; Kang, E.S.; Kim, I.; Shin, S.; Kim, M.; Kwon, S.; Oh, S.R.; Ahn, Y.S.; Kim, C.H. GPR30 mediates anorectic estrogen-induced STAT3 signaling in the hypothalamus. Metab. Clin. Exp. 2014, 63, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Martensson, U.E.A.; Salehi, S.A.; Windahl, S.; Gomez, M.F.; Swärd, K.; Daszkiewicz-Nilsson, J.; Wendt, A.; Andersson, N.; Hellstrand, P.; Grände, P.O.; et al. Deletion of the G protein-coupled receptor 30 impairs glucose tolerance, reduces bone growth, increases blood pressure, and eliminates estradiol-stimulated insulin release in female mice. Endocrinology 2009, 150, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Revankar, C.M. A Transmembrane Intracellular Estrogen Receptor Mediates Rapid Cell Signaling. Science 2005, 307, 1625–1630. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Hu, C.; Brigman, J.L.; Zhu, G.; Hathaway, H.J.; Prossnitz, E.R. GPER deficiency in male mice results in insulin resistance, dyslipidemia, and a proinflammatory state. Endocrinology 2013, 154, 4136–4145. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Dehghani, B.; Magrisso, I.J.; Rick, E.A.; Bonhomme, E.; Cody, D.B.; Elenich, L.A.; Subramanian, S.; Murphy, S.J.; Kelly, M.J.; et al. GPR30 contributes to estrogen-induced thymic atrophy. Mol. Endocrinol. (Baltimore, MD) 2008, 22, 636–648. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.M.; Thompson, L.I.; Patel, P.; Gonzales, A.D.; Ye, H.; Filardo, E.J.; Clegg, D.J.; Gorecka, J.; Akama, K.T.; McEwen, B.S.; et al. G-Protein-Coupled Estrogen Receptor 1 Is Anatomically Positioned to Modulate Synaptic Plasticity in the Mouse Hippocampus. J. Neurosci. 2015, 35, 2384–2397. [Google Scholar] [CrossRef] [PubMed]
- Misawa, A.; Inoue, S. Estrogen-related receptors in breast cancer and prostate cancer. Front. Endocrinol. 2015, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Giguère, V. To ERR in the estrogen pathway. Trends Endocrinol. Metab. TEM 2002, 13, 220–225. [Google Scholar] [CrossRef]
- Hu, P.; Kinyamu, H.K.; Wang, L.; Martin, J.; Archer, T.K.; Teng, C. Estrogen induces estrogen-related receptor α gene expression and chromatin structural changes in estrogen receptor (ER)-positive and ER-negative breast cancer cells. J. Biol. Chem. 2008, 283, 6752–6763. [Google Scholar] [CrossRef] [PubMed]
- Deblois, G.; Giguère, V. Oestrogen-related receptors in breast cancer: Control of cellular metabolism and beyond. Nat. Rev. Cancer 2013, 13, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Michalek, R.D.; Gerriets, V.A.; Nichols, A.G.; Inoue, M.; Kazmin, D.; Chang, C.-Y.; Dwyer, M.A.; Nelson, E.R.; Pollizzi, K.N.; Ilkayeva, O.; et al. Estrogen-related receptor-α is a metabolic regulator of effector T-cell activation and differentiation. Proc. Natl. Acad. Sci. USA 2011, 108, 18348–18353. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Schwaid, A.G.; Wang, X.; Wang, X.; Chen, S.; Chu, Q.; Saghatelian, A.; Wan, Y. Ligand activation of ERRα by cholesterol mediates statin and bisphosphonate effects. Cell Metab. 2016, 23, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Badin, P.-M.; Vila, I.K.; Sopariwala, D.H.; Yadav, V.; Lorca, S.; Louche, K.; Kim, E.R.; Tong, Q.; Song, M.S.; Moro, C.; et al. Exercise-like effects by Estrogen-related receptor-gamma in muscle do not prevent insulin resistance in db/db mice. Sci. Rep. 2016, 6, 26442. [Google Scholar] [CrossRef] [PubMed]
- Gantner, M.L.; Hazen, B.C.; Eury, E.; Brown, E.L.; Kralli, A. Complementary roles of estrogen-related receptors in brown adipocyte thermogenic function. Endocrinology 2016, 157, 4770–4781. [Google Scholar] [CrossRef] [PubMed]
- Handschin, C.; Mootha, V.K. Estrogen-related receptor α (ERRα): A novel target in type 2 diabetes. Drug Discov. Today Ther. Strateg. 2005, 2, 151–156. [Google Scholar] [CrossRef]
- Powelka, A.M.; Seth, A.; Virbasius, J.V.; Kiskinis, E.; Nicoloro, S.M.; Guilherme, A.; Tang, X.; Straubhaar, J.; Cherniack, A.D.; Parker, M.G.; et al. Suppression of oxidative metabolism and mitochondrial biogenesis by the transcriptional corepressor RIP140 in mouse adipocytes. J. Clin. Investig. 2006, 116, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Patch, R.J.; Huang, H.; Patel, S.; Cheung, W.; Xu, G.; Zhao, B.P.; Beauchamp, D.A.; Rentzeperis, D.; Geisler, J.G.; Askari, H.B.; et al. Indazole-based ligands for estrogen-related receptor α as potential anti-diabetic agents. Eur. J. Med. Chem. 2017, 138, 830–853. [Google Scholar] [CrossRef] [PubMed]
- Gibson, D.A.; Saunders, P.T.K. Estrogen dependent signaling in reproductive tissues—A role for estrogen receptors and estrogen related receptors. Mol. Cell. Endocrinol. 2012, 348, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Wrann, C.D.; White, J.P.; Salogiannnis, J.; Laznik-Bogoslavski, D.; Wu, J.; Ma, D.; Lin, J.D.; Greenberg, M.E.; Spiegelman, B.M. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 2013, 18, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Bianco, S.; Lanvin, O.; Tribollet, V.; Macari, C.; North, S.; Vanacker, J.-M. Modulating estrogen receptor-related receptor-alpha activity inhibits cell proliferation. J. Biol. Chem. 2009, 284, 23286–23292. [Google Scholar] [CrossRef] [PubMed]
- Takayanagi, S.; Tokunaga, T.; Liu, X.; Okada, H.; Matsushima, A.; Shimohigashi, Y. Endocrine disruptor bisphenol A strongly binds to human estrogen-related receptor gamma (ERRgamma) with high constitutive activity. Toxicol. Lett. 2006, 167, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.T.; Beames, B.; Alex Merrick, B.; Martin, N.; Romeo, C.; Jetten, A.M. Development of a stable cell line with an intact PGC-1α/ERRα axis for screening environmental chemicals. Biochem. Biophys. Res. Commun. 2014, 444, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.T.; Hsieh, J.-H.; Zhao, J.; Huang, R.; Xia, M.; Martin, N.; Gao, X.; Dixon, D.; Auerbach, S.S.; Witt, K.L.; et al. Development of Novel Cell Lines for High-Throughput Screening to Detect Estrogen-Related Receptor Alpha Modulators. SLAS Discov. Adv. Life Sci. R D 2017, 22, 720–731. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.; Zhao, J.; Huang, R.; Kanaya, N.; Bernal, L.; Hsieh, J.-H.; Auerbach, S.S.; Witt, K.L.; Merrick, B.A.; Chen, S.; et al. Identification of Estrogen-Related Receptor Alpha Agonists in the Tox21 Compound Library. Endocrinology 2017, 159, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Masood, S. Estrogen and progesterone receptors in cytology: A comprehensive review. Diagn. Cytopathol. 1992, 8, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Mohibi, S.; Mirza, S.; Band, H.; Band, V. Mouse models of estrogen receptor-positive breast cancer. J. Carcinog. 2011, 10, 35. [Google Scholar] [PubMed]
- Caldon, C.E.; Sutherland, R.L.; Musgrove, E. Cell cycle proteins in epithelial cell differentiation: Implications for breast cancer. Cell Cycle (Georgetown, TX) 2010, 9, 1918–1928. [Google Scholar] [CrossRef] [PubMed]
- Musgrove, E.A.; Caldon, C.E.; Barraclough, J.; Stone, A.; Sutherland, R.L. Cyclin D as a therapeutic target in cancer. Nat. Rev. Cancer 2011, 11, 558–572. [Google Scholar] [CrossRef] [PubMed]
- Ariazi, E.A.; Clark, G.M.; Mertz, J.E. Estrogen-related receptor alpha and estrogen-related receptor gamma associate with unfavorable and favorable biomarkers, respectively, in human breast cancer. Cancer Res. 2002, 62, 6510–6518. [Google Scholar] [PubMed]
- Suzuki, T.; Miki, Y.; Moriya, T.; Shimada, N.; Ishida, T.; Hirakawa, H.; Ohuchi, N.; Sasano, H. Estrogen-related receptor α in human breast carcinoma as a potent prognostic factor. Cancer Res. 2004, 64, 4670–4676. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhang, Z.; Gladwell, W.; Teng, C.T. Estrogen stimulates estrogen-related receptor alpha gene expression through conserved hormone response elements. Endocrinology 2003, 144, 4894–4904. [Google Scholar] [CrossRef] [PubMed]
- Shigeta, H.; Zuo, W.; Yang, N.; DiAugustine, R.; Teng, C.T. The mouse estrogen receptor-related orphan receptor alpha 1: Molecular cloning and estrogen responsiveness. J. Mol. Endocrinol. 1997, 19, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Deblois, G.; Hall, J.A.; Perry, M.C.; Laganière, J.; Ghahremani, M.; Park, M.; Hallett, M.; Giguère, V. Genome-wide identification of direct target genes implicates estrogen-related receptor α as a determinant of breast cancer heterogeneity. Cancer Res. 2009, 69, 6149–6157. [Google Scholar] [CrossRef] [PubMed]
- Kammerer, M.; Gutzwiller, S.; Stauffer, D.; Delhon, I.; Seltenmeyer, Y.; Fournier, B. Estrogen Receptor α (ERα) and Estrogen Related Receptor α (ERRα) are both transcriptional regulators of the Runx2-I isoform. Mol. Cell. Endocrinol. 2013, 369, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Zhou, D.; Chen, S. Modulation of aromatase expression in the breast tissue by ERR alpha-1 orphan receptor. Cancer Res. 1998, 58, 5695–5700. [Google Scholar] [PubMed]
- Miao, L.; Shi, J.; Wang, C.-Y.; Zhu, Y.; Du, X.; Jiao, H.; Mo, Z.; Klocker, H.; Lee, C.; Zhang, J. Estrogen receptor-related receptor alpha mediates up-regulation of aromatase expression by prostaglandin E2 in prostate stromal cells. Mol. Endocrinol. 2010, 24, 1175–1186. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kumar, P.; Kamat, A.; Mendelson, C.R. Estrogen receptor alpha (ERα) mediates stimulatory effects of estrogen on aromatase (CYP19) gene expression in human placenta. Mol. Endocrinol. 2009, 23, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Tanida, T.; Matsuda, K.I.; Yamada, S.; Hashimoto, T.; Kawata, M. Estrogen-related Receptor β Reduces the Subnuclear Mobility of Estrogen Receptor α and Suppresses Estrogen-dependent Cellular Function. J. Biol. Chem. 2015, 290, 12332–12345. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Cao, X.; He, Y.; Xu, Y. Progress in the molecular understanding of central regulation of body weight by estrogens. Obesity 2015, 23, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Allende-Vigo, M.Z. Women and the metabolic syndrome: An overview of its peculiarities. P. R. Health Sci. J. 2008, 27, 190–195. [Google Scholar] [PubMed]
- Geary, N.; Asarian, L.; Korach, K.S.; Pfaff, D.W.; Ogawa, S. Deficits in E2-dependent control of feeding, weight gain, and cholecystokinin satiation in ER-α null mice. Endocrinology 2001, 142, 4751–4757. [Google Scholar] [CrossRef] [PubMed]
- Roesch, D.M. Effects of selective estrogen receptor agonists on food intake and body weight gain in rats. Physiol. Behav. 2005, 87, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Butera, P.C.; Beikirch, R.J. Central implants of diluted estradiol: Independent effects on ingestive and reproductive behaviors of ovariectomized rats. Brain Res. 1989, 491, 266–273. [Google Scholar] [CrossRef]
- Palmer, K.; Gray, J.M. Central vs peripheral effects of estrogen on food intake and lipoprotein lipase activity in ovariectomized rats. Physiol. Behav. 1986, 37, 187–189. [Google Scholar] [CrossRef]
- Heine, P.A.; Taylor, J.A.; Iwamoto, G.A.; Lubahn, D.B.; Cooke, P.S. Increased adipose tissue in male and female estrogen receptor-alpha knockout mice. Proc. Natl. Acad. Sci. USA 2000, 97, 12729–12734. [Google Scholar] [CrossRef] [PubMed]
- Okura, T.; Koda, M.; Ando, F.; Niino, N.; Ohta, S.; Shimokata, H. Association of polymorphisms in the estrogen receptor alpha gene with body fat distribution. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Nedungadi, T.P.; Zhu, L.; Sobhani, N.; Irani, B.G.; Davis, K.E.; Zhang, X.; Zou, F.; Gent, L.M.; Hahner, L.D.; et al. Distinct hypothalamic neurons mediate estrogenic effects on energy homeostasis and reproduction. Cell Metab. 2011, 14, 453–465. [Google Scholar] [CrossRef] [PubMed]
- Merchenthaler, I.; Lane, M.V.; Numan, S.; Dellovade, T.L. Distribution of estrogen receptor alpha and beta in the mouse central nervous system: In vivo autoradiographic and immunocytochemical analyses. J. Comp. Neurol. 2004, 473, 270–291. [Google Scholar] [CrossRef] [PubMed]
- De Souza, F.S.J.; Nasif, S.; Leal, R.; Levi, D.H.; Low, M.J.; Rubinsten, M. López- The estrogen receptor α colocalizes with proopiomelanocortin in hypothalamic neurons and binds to a conserved motif present in the neuron-specific enhancer nPE2. Eur. J. Pharmacol. 2010, 660, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; He, Y.; Yan, X.; Yang, Y.; Wang, C.; Xu, P.; Hinton, A.O.; Shu, G.; Yu, L.; Tong, Q.; et al. Visualizing estrogen receptor-α-expressing neurons using a new ERα-ZsGreen reporter mouse line. Metabolism 2015, 65, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Slamberova, R.; Hnatczuk, O.C.; Vathy, I. Expression of proopiomelanocortin and proenkephalin mRNA in sexually dimorphic brain regions are altered in adult male and female rats treated prenatally with morphine. J. Pept. Res. 2004, 63, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, S.S.; Belsham, D.D. Estrogen inhibits NPY secretion through membrane-associated estrogen receptor (ER)-α in clonal, immortalized hypothalamic neurons. Int. J. Obes. 2010, 35, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Olofsson, L.E.; Pierce, A.A.; Xu, A.W. Functional requirement of AgRP and NPY neurons in ovarian cycle-dependent regulation of food intake. Proc. Natl. Acad. Sci. USA 2009, 106, 15932–15937. [Google Scholar] [CrossRef] [PubMed]
- Roepke, T.A.; Qiu, J.; Smith, A.W.; Ronnekleiv, O.K.; Kelly, M.J. Fasting and 17beta-estradiol differentially modulate the M-current in neuropeptide Y neurons. J. Neurosci. 2011, 31, 11825–11835. [Google Scholar] [CrossRef] [PubMed]
- Roepke, T.A.; Ronnekleiv, O.K.; Kelly, M.J. Physiological consequences of membrane-initiated estrogen signaling in the brain. Front. Biosci. 2011, 16, 1560–1573. [Google Scholar] [CrossRef]
- Sun, F.; Yu, J. The effect of a special herbal tea on obesity and anovulation in androgen-sterilized rats. Proc. Soc. Exp. Biol. Med. 2000, 223, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Cao, X.; He, Y.; Zhu, L.; Yang, Y.; Saito, K.; Wang, C.; Yan, X.; Hinton, A.O., Jr.; Zou, F.; et al. Estrogen receptor-alpha in medial amygdala neurons regulates body weight. J. Clin. Investig. 2015, 125, 2861–2876. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.E.; Thorburn, A.W.; Britt, K.L.; Hewitt, K.N.; Wreford, N.G.; Proietto, J.; Oz, O.K.; Leury, B.J.; Robertson, K.M.; Yao, S.; et al. Aromatase-deficient (ArKO) mice have a phenotype of increased adiposity. Proc. Natl. Acad. Sci. USA 2000, 97, 12735–12740. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Sladek, R.; Carrier, J.; Bader, J.A.; Richard, D.; Giguere, V. Reduced fat mass in mice lacking orphan nuclear receptor estrogen-related receptor alpha. Mol. Cell. Biol. 2003, 23, 7947–7956. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Lu, Y.; Khan, M.Z.; Anderson, R.M.; McDaniel, L.; Wilson, H.E.; Yin, T.C.; Radley, J.J.; Pieper, A.A.; Lutter, M. Behavioral disturbances in estrogen-related receptor alpha-null mice. Cell Rep. 2015, 11, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Moore, J.; Ashimi, S.S.; Mason, B.L.; Drawbridge, J.N.; Han, S.; Hing, B.; Matthews, A.; McAdams, C.J.; Darbro, B.W.; et al. Eating disorder predisposition is associated with ESRRA and HDAC4 mutations. J. Clin. Investig. 2013, 123, 4706–4713. [Google Scholar] [CrossRef] [PubMed]
- Haber, S.N.; Knutson, B. The reward circuit: Linking primate anatomy and human imaging. Neuropsychopharmacology 2010, 35, 4–26. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Figlewicz, D.P.; Gosnell, B.A.; Levine, A.S.; Pratt, W.E. The contribution of brain reward circuits to the obesity epidemic. Neurosci. Biobehav. Rev. 2013, 37, 2047–2058. [Google Scholar] [CrossRef] [PubMed]
- Alaynick, W.A.; Kondo, R.P.; Xie, W.; He, W.; Dufour, C.R.; Downes, M.; Jonker, J.W.; Giles, W.; Naviaux, R.K.; Giguere, V.; et al. ERRgamma directs and maintains the transition to oxidative metabolism in the postnatal heart. Cell Metab. 2007, 6, 13–24. [Google Scholar] [CrossRef] [PubMed]
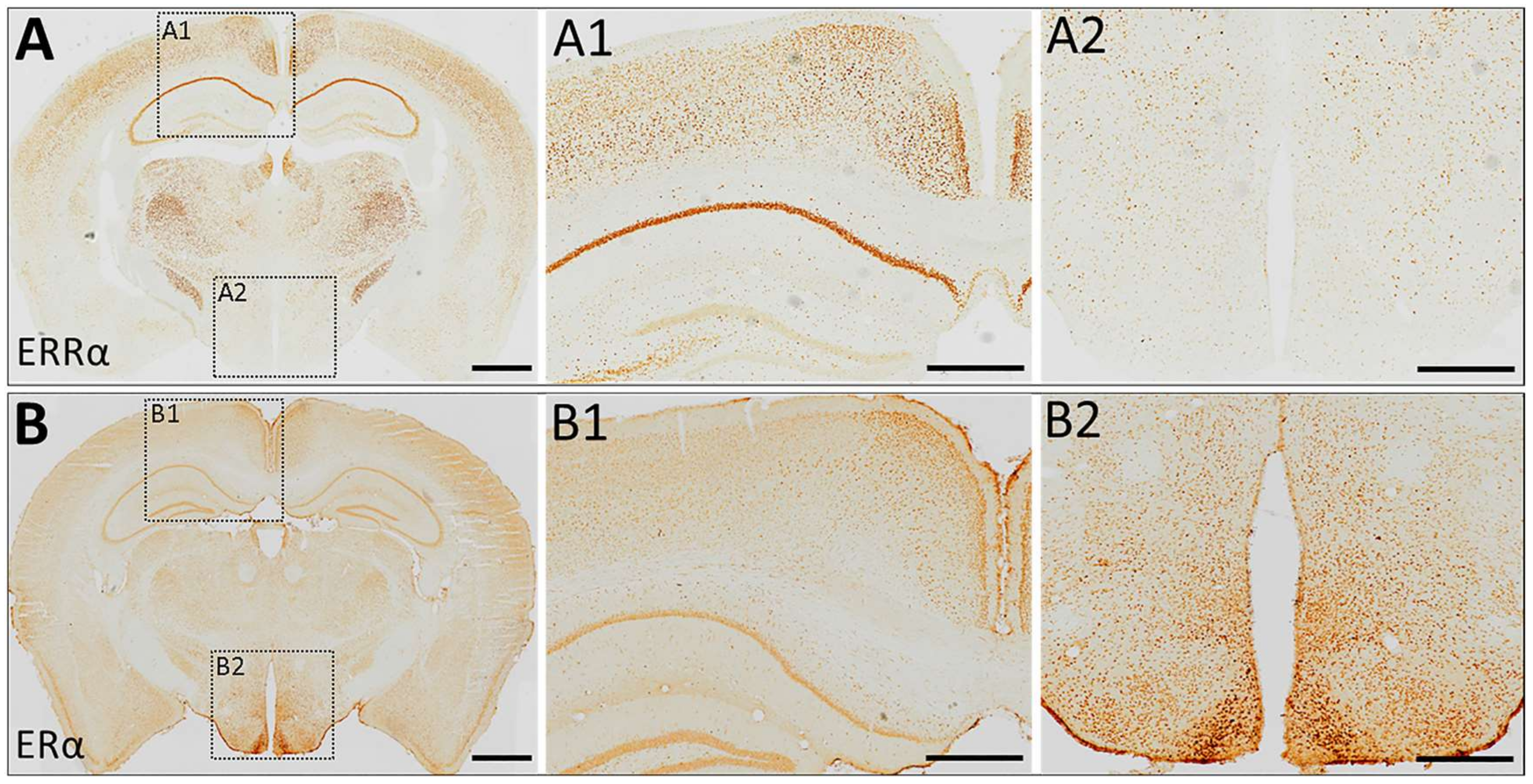
- Tanida, T.; Matsuda, K.I.; Yamada, S.; Kawata, M.; Tanaka, M. Immunohistochemical profiling of estrogen-related receptor gamma in rat brain and colocalization with estrogen receptor α in the preoptic area. Brain Res. 2017, 1659, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Lorke, D.E.; Susens, U.; Borgmeyer, U.; Hermans-Borgmeyer, I. Differential expression of the estrogen receptor-related receptor gamma in the mouse brain. Brain Res. Mol. Brain Res. 2000, 77, 277–280. [Google Scholar] [CrossRef]
- Luo, J.; Sladek, R.; Bader, J.A.; Matthyssen, A.; Rossant, J.; Giguere, V. Placental abnormalities in mouse embryos lacking the orphan nuclear receptor ERR-beta. Nature 1997, 388, 778–782. [Google Scholar] [CrossRef] [PubMed]
- Byerly, M.S.; Swanson, R.D.; Wong, G.W.; Blackshaw, S. Estrogen-related receptor beta deficiency alters body composition and response to restraint stress. BMC Physiol. 2013, 13, 10. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Moss, R.L. Long-term and short-term electrophysiological effects of estrogen on the synaptic properties of hippocampal CA1 neurons. J. Neurosci. 1992, 12, 3217–3225. [Google Scholar] [PubMed]
- Rudick, C.N.; Woolley, C.S. Selective estrogen receptor modulators regulate phasic activation of hippocampal CA1 pyramidal cells by estrogen. Endocrinology 2003, 144, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Kramar, E.A.; Chen, L.Y.; Brandon, N.J.; Rex, C.S.; Liu, F.; Gall, C.M.; Lynch, G. Cytoskeletal changes underlie estrogen’s acute effects on synaptic transmission and plasticity. J. Neurosci. 2009, 29, 12982–12993. [Google Scholar] [CrossRef] [PubMed]
- Milner, T.A.; Ayoola, K.; Drake, C.T.; Herrick, S.P.; Tabori, N.E.; McEwen, B.S.; Warrier, S.; Alves, S.E. Ultrastructural localization of estrogen receptor beta immunoreactivity in the rat hippocampal formation. J. Comp. Neurol. 2005, 491, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Milner, T.A.; McEwen, B.S.; Hayashi, S.; Li, C.J.; Reagan, L.P.; Alves, S.E. Ultrastructural evidence that hippocampal alpha estrogen receptors are located at extranuclear sites. J. Comp. Neurol. 2001, 429, 355–371. [Google Scholar] [CrossRef]
- Smejkalova, T.; Woolley, C.S. Estradiol acutely potentiates hippocampal excitatory synaptic transmission through a presynaptic mechanism. J. Neurosci. 2010, 30, 16137–16148. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.Z.; Woolley, C.S. Estradiol Acutely Suppresses Inhibition in the Hippocampus through a Sex-Specific Endocannabinoid and mGluR-Dependent Mechanism. Neuron 2012, 74, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Phan, A.; Gabor, C.S.; Favaro, K.J.; Kaschack, S.; Armstrong, J.N.; MacLusky, N.J.; Choleris, E. Low doses of 17β-estradiol rapidly improve learning and increase hippocampal dendritic spines. Neuropsychopharmacology 2012, 37, 2299–2309. [Google Scholar] [CrossRef] [PubMed]
- Woolley, C.S. Acute effects of estrogen on neuronal physiology. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 657–680. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.J.; Ronnekleiv, O.K. A selective membrane estrogen receptor agonist maintains autonomic functions in hypoestrogenic states. Brain Res. 2013, 1514, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Korach, K.S.; Moss, R.L. Rapid action of 17beta-estradiol on kainate-induced currents in hippocampal neurons lacking intracellular estrogen receptors. Endocrinology 1999, 140, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Pei, L.; Mu, Y.; Leblanc, M.; Alaynick, W.; Barish, G.D.; Pankratz, M.; Tseng, T.W.; Kaufman, S.; Liddle, C.; Yu, R.T.; et al. Dependence of hippocampal function on ERRγ-regulated mitochondrial metabolism. Cell Metab. 2015, 21, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Villena, J.A.; Kralli, A. ERRα: A metabolic function for the oldest orphan. Trends Endocrinol. Metab. 2008, 19, 269–276. [Google Scholar] [CrossRef] [PubMed]
- De Jesus-Cortes, H.; Lu, Y.; Anderson, R.M.; Khan, M.Z.; Nath, V.; McDaniel, L.; Lutter, M.; Radley, J.J.; Pieper, A.A.; Cui, H. Loss of estrogen-related receptor alpha disrupts ventral-striatal synaptic function in female mice. Neuroscience 2016, 329, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Tetel, M.J.; Pfaff, D.W. Contributions of estrogen receptor-alpha and estrogen receptor-ss to the regulation of behavior. Biochim. Biophys. Acta 2010, 1800, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S.; Washburn, T.F.; Taylor, J.; Lubahn, D.B.; Korach, K.S.; Pfaff, D.W. Modifications of testosterone-dependent behaviors by estrogen receptor-alpha gene disruption in male mice. Endocrinology 1998, 139, 5058–5069. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S.; Lubahn, D.B.; Korach, K.S.; Pfaff, D.W. Behavioral effects of estrogen receptor gene disruption in male mice. Proc. Natl. Acad. Sci. USA 1997, 94, 1476–1481. [Google Scholar] [CrossRef] [PubMed]
- Sano, K.; Tsuda, M.C.; Musatov, S.; Sakamoto, T.; Ogawa, S. Differential effects of site-specific knockdown of estrogen receptor alpha in the medial amygdala, medial pre-optic area, and ventromedial nucleus of the hypothalamus on sexual and aggressive behavior of male mice. Eur. J. Neurosci. 2013, 37, 1308–1319. [Google Scholar] [CrossRef] [PubMed]
- Unger, E.K.; Burke, K.J., Jr.; Yang, C.F.; Bender, K.J.; Fuller, P.M.; Shah, N.M. Medial amygdalar aromatase neurons regulate aggression in both sexes. Cell Rep. 2015, 10, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Ervin, K.S.; Lymer, J.M.; Matta, R.; Clipperton-Allen, A.E.; Kavaliers, M.; Choleris, E. Estrogen involvement in social behavior in rodents: Rapid and long-term actions. Horm. Behav. 2015, 74, 53–76. [Google Scholar] [CrossRef] [PubMed]
- Beach, F.A. Sexual attractivity, proceptivity, and receptivity in female mammals. Horm. Behav. 1976, 7, 105–138. [Google Scholar] [CrossRef]
- Tennent, B.J.; Smith, E.R.; Davidson, J.M. The effects of estrogen and progesterone on female rat proceptive behavior. Horm. Behav. 1980, 14, 65–75. [Google Scholar] [CrossRef]
- Kavaliers, M.; Agmo, A.; Choleris, E.; Gustafsson, J.A.; Korach, K.S.; Muglia, L.J.; Pfaff, D.W.; Ogawa, S. Oxytocin and estrogen receptor alpha and beta knockout mice provide discriminably different odor cues in behavioral assays. Genes Brain Behav. 2004, 3, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, D.W.; Remedios, R.; Anthony, T.E.; Chang, A.; Madisen, L.; Zeng, H.; Anderson, D.J. Scalable control of mounting and attack by Esr1+ neurons in the ventromedial hypothalamus. Nature 2014, 509, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Hashikawa, K.; Hashikawa, Y.; Tremblay, R.; Zhang, J.; Feng, J.E.; Sabol, A.; Piper, W.T.; Lee, H.; Rudy, B.; Lin, D. Esr1(+) cells in the ventromedial hypothalamus control female aggression. Nat. Neurosci. 2017, 20, 1580–1590. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Zhu, H.; Fan, Z.; Wang, F.; Chen, Y.; Liang, H.; Yang, Z.; Zhang, L.; Lin, L.; Zhan, Y.; et al. History of winning remodels thalamo-PFC circuit to reinforce social dominance. Science 2017, 357, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Zhu, J.; Zhu, H.; Zhang, Q.; Lin, Z.; Hu, H. Bidirectional control of social hierarchy by synaptic efficacy in medial prefrontal cortex. Science 2011, 334, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Carus-Cadavieco, M.; Gorbati, M.; Ye, L.; Bender, F.; van der Veldt, S.; Kosse, C.; Borgers, C.; Lee, S.Y.; Ramakrishnan, C.; Hu, Y.; et al. Gamma oscillations organize top-down signalling to hypothalamus and enable food seeking. Nature 2017, 542, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Gan, J.; Jonas, P. Fast-spiking, parvalbumin(+) GABAergic interneurons: From cellular design to microcircuit function. Science 2014, 345, 1255263. [Google Scholar] [CrossRef] [PubMed]
- Cardin, J.A.; Carlen, M.; Meletis, K.; Knoblich, U.; Zhang, F.; Deisseroth, K.; Tsai, L.H.; Moore, C.I. Driving fast-spiking cells induces gamma rhythm and controls sensory responses. Nature 2009, 459, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Sohal, V.S.; Zhang, F.; Yizhar, O.; Deisseroth, K. Parvalbumin neurons and gamma rhythms enhance cortical circuit performance. Nature 2009, 459, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Scarpulla, R.C. Metabolic control of mitochondrial biogenesis through the PGC-1 family regulatory network. Biochim. Biophys. Acta 2011, 1813, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Audet-Walsh, E.; Giguere, V. The multiple universes of estrogen-related receptor alpha and gamma in metabolic control and related diseases. Acta Pharmacol. Sin. 2015, 36, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.C.; Bean, B.P. Sodium entry during action potentials of mammalian neurons: Incomplete inactivation and reduced metabolic efficiency in fast-spiking neurons. Neuron 2009, 64, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.C.; Bean, B.P. Incomplete inactivation and rapid recovery of voltage-dependent sodium channels during high-frequency firing in cerebellar Purkinje neurons. J. Neurophysiol. 2010, 105, 860–871. [Google Scholar] [CrossRef] [PubMed]
- Cowell, R.M.; Blake, K.R.; Russell, J.W. Localization of the transcriptional coactivator PGC-1alpha to GABAergic neurons during maturation of the rat brain. J. Comp. Neurol. 2007, 502, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Lucas, E.K.; Markwardt, S.J.; Gupta, S.; Meador-Woodruff, J.H.; Lin, J.D.; Overstreet-Wadiche, L.; Cowell, R.M. Parvalbumin deficiency and GABAergic dysfunction in mice lacking PGC-1alpha. J. Neurosci. 2010, 30, 7227–7235. [Google Scholar] [CrossRef] [PubMed]
- Lucas, E.K.; Dougherty, S.E.; McMeekin, L.J.; Reid, C.S.; Dobrunz, L.E.; West, A.B.; Hablitz, J.J.; Cowell, R.M. PGC-1alpha provides a transcriptional framework for synchronous neurotransmitter release from parvalbumin-positive interneurons. J. Neurosci. 2014, 34, 14375–14387. [Google Scholar] [CrossRef] [PubMed]
- Saul, M.C.; Seward, C.H.; Troy, J.M.; Zhang, H.; Sloofman, L.G.; Lu, X.; Weisner, P.A.; Caetano-Anolles, D.; Sun, H.; Zhao, S.D.; et al. Transcriptional regulatory dynamics drive coordinated metabolic and neural response to social challenge in mice. Genome Res. 2017, 27, 959–972. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, K.; Cui, H. Emerging Roles of Estrogen-Related Receptors in the Brain: Potential Interactions with Estrogen Signaling. Int. J. Mol. Sci. 2018, 19, 1091. https://doi.org/10.3390/ijms19041091
Saito K, Cui H. Emerging Roles of Estrogen-Related Receptors in the Brain: Potential Interactions with Estrogen Signaling. International Journal of Molecular Sciences. 2018; 19(4):1091. https://doi.org/10.3390/ijms19041091
Chicago/Turabian StyleSaito, Kenji, and Huxing Cui. 2018. "Emerging Roles of Estrogen-Related Receptors in the Brain: Potential Interactions with Estrogen Signaling" International Journal of Molecular Sciences 19, no. 4: 1091. https://doi.org/10.3390/ijms19041091
APA StyleSaito, K., & Cui, H. (2018). Emerging Roles of Estrogen-Related Receptors in the Brain: Potential Interactions with Estrogen Signaling. International Journal of Molecular Sciences, 19(4), 1091. https://doi.org/10.3390/ijms19041091





