Development of 111In-Labeled Monoclonal Antibodies Targeting SFTSV Structural Proteins for Molecular Imaging of SFTS Infectious Diseases by SPECT
Abstract
1. Introduction
2. Results and Discussion
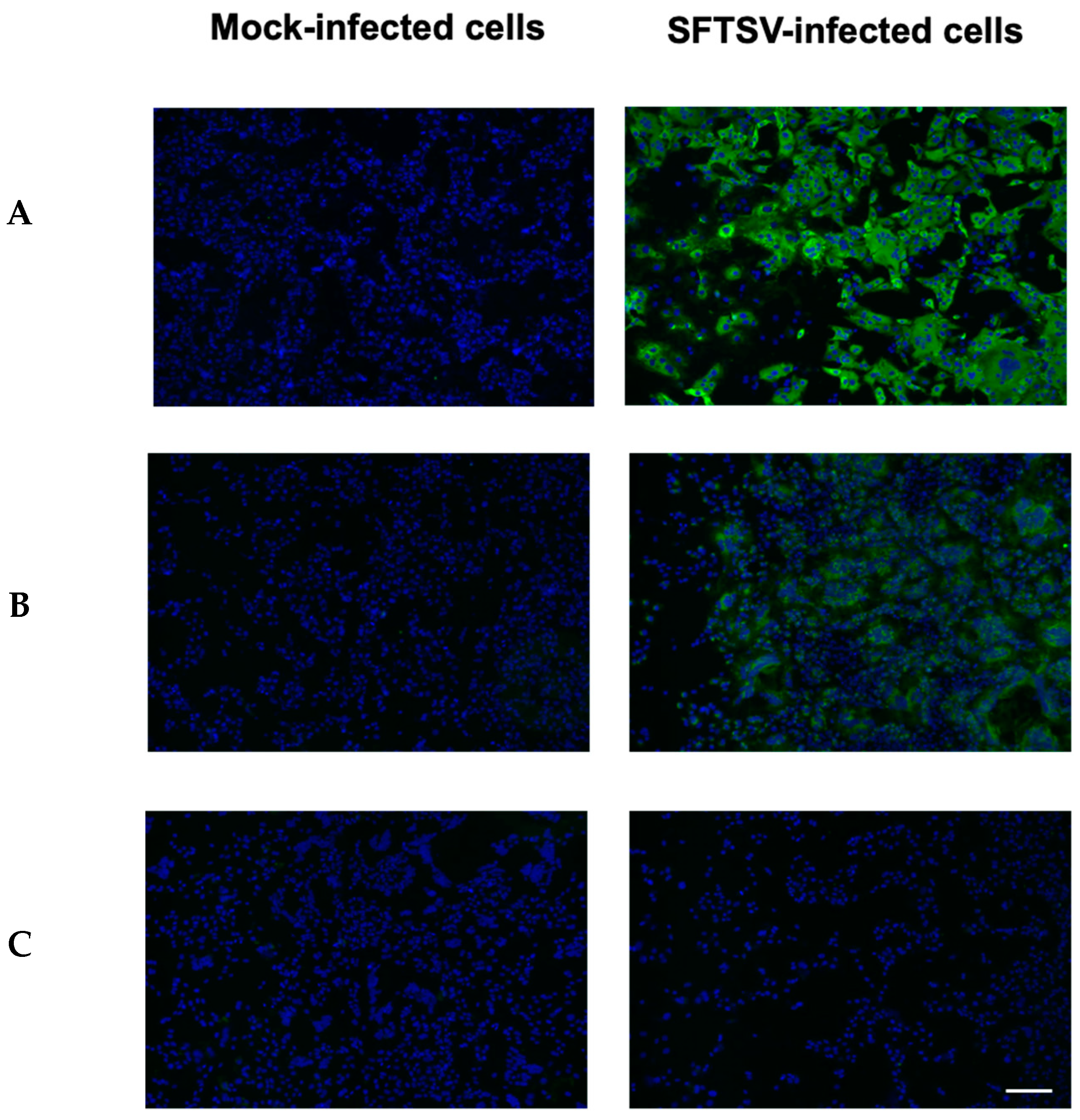
2.1. Screening of SFSV-Targeting Antibodies as Scaffolds for SFTSV Imaging Probes
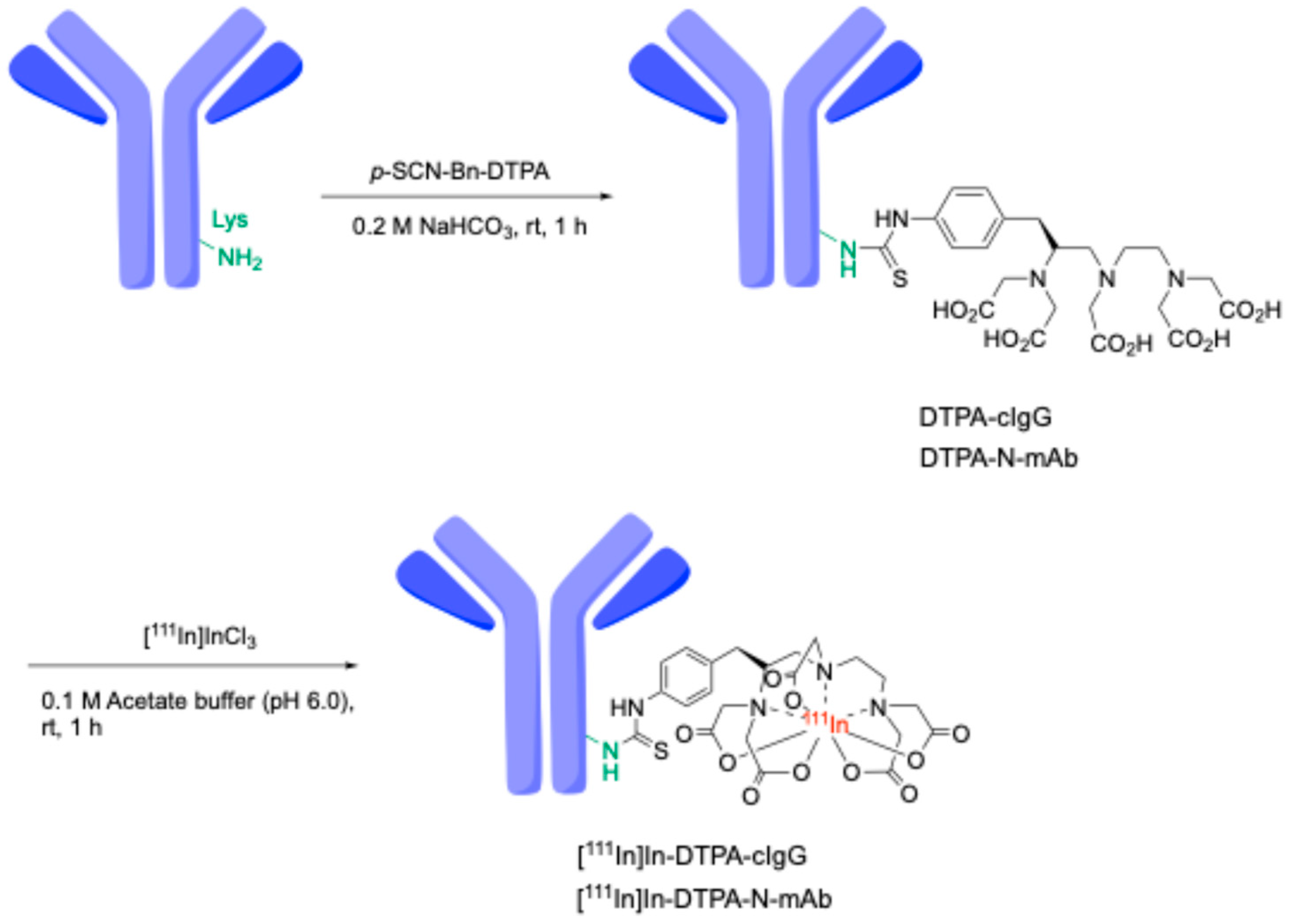
2.2. Radiosynthesis of 111In-Labeled-Diethylenetriaminepentaacetic Acid (DTPA) Antibodies
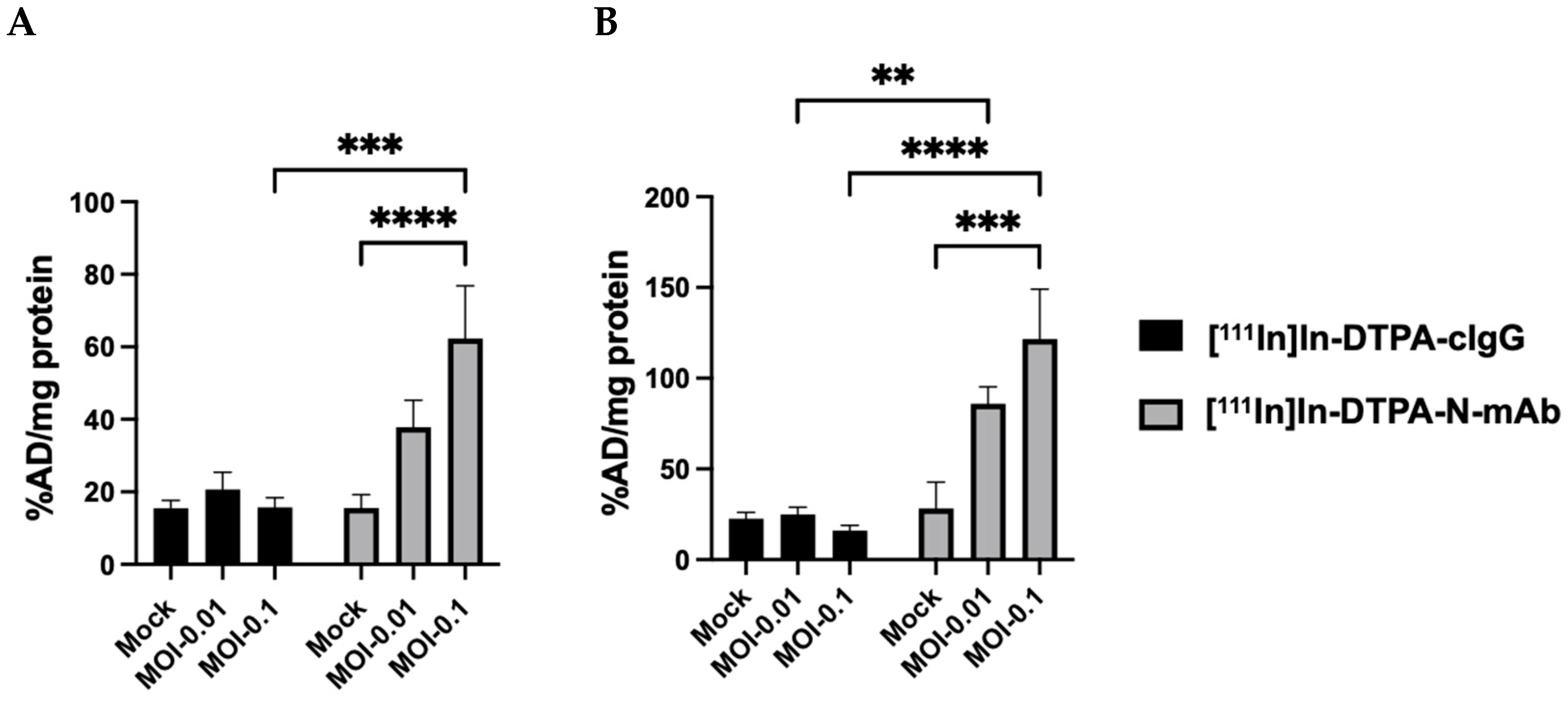
2.3. Cell Binding Assays of 111In-Antibodies to SFTSV-Infected Vero E6 Cells
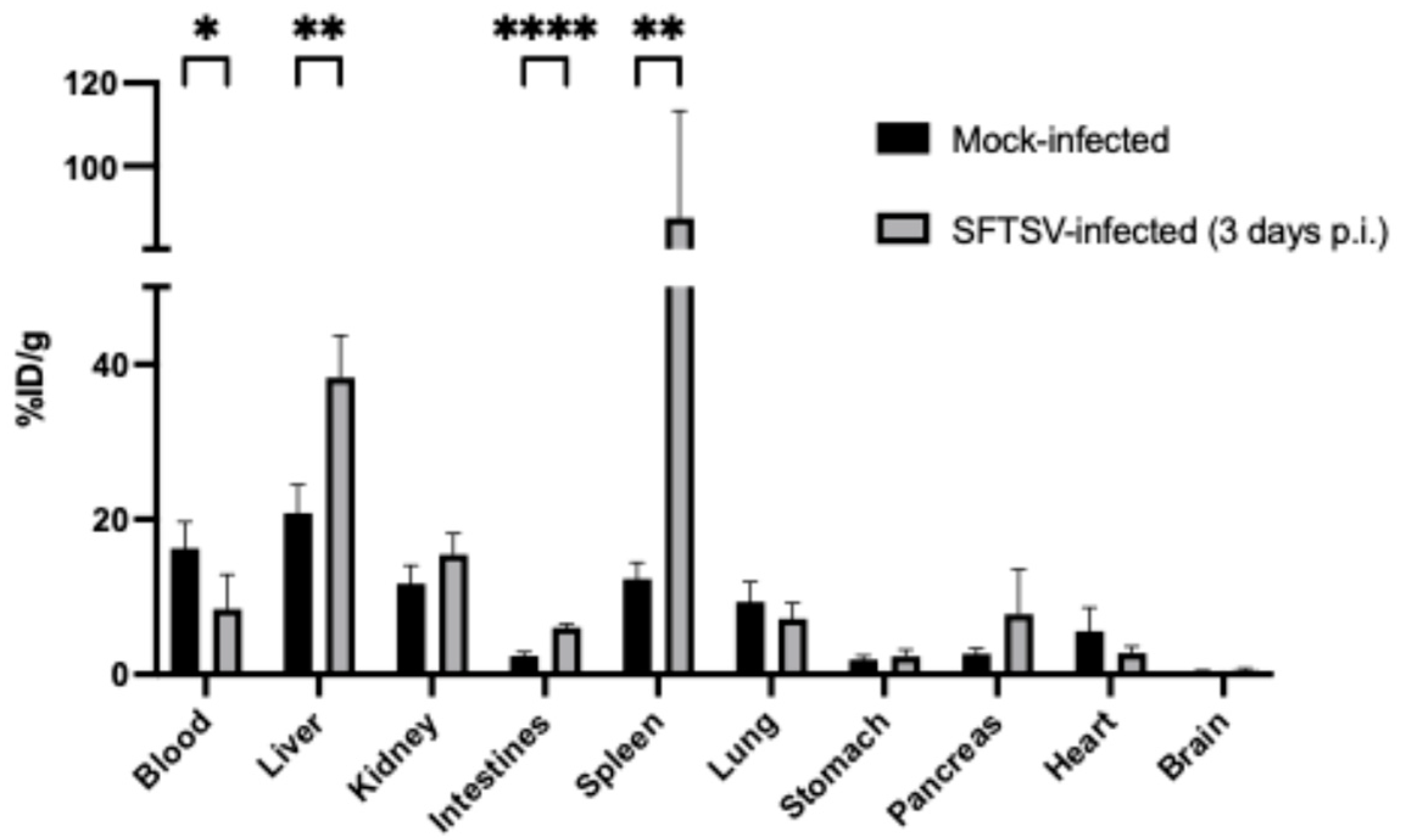
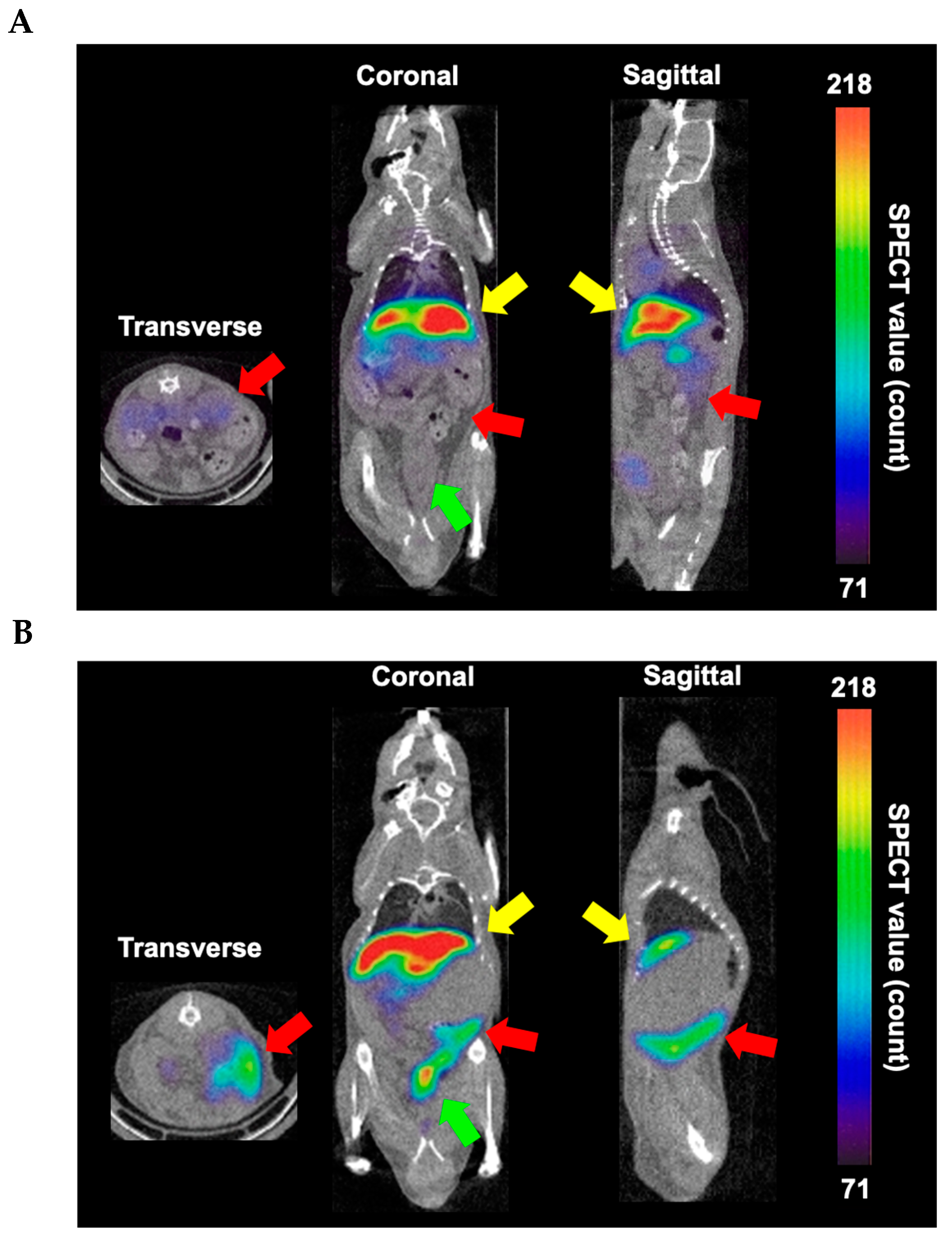
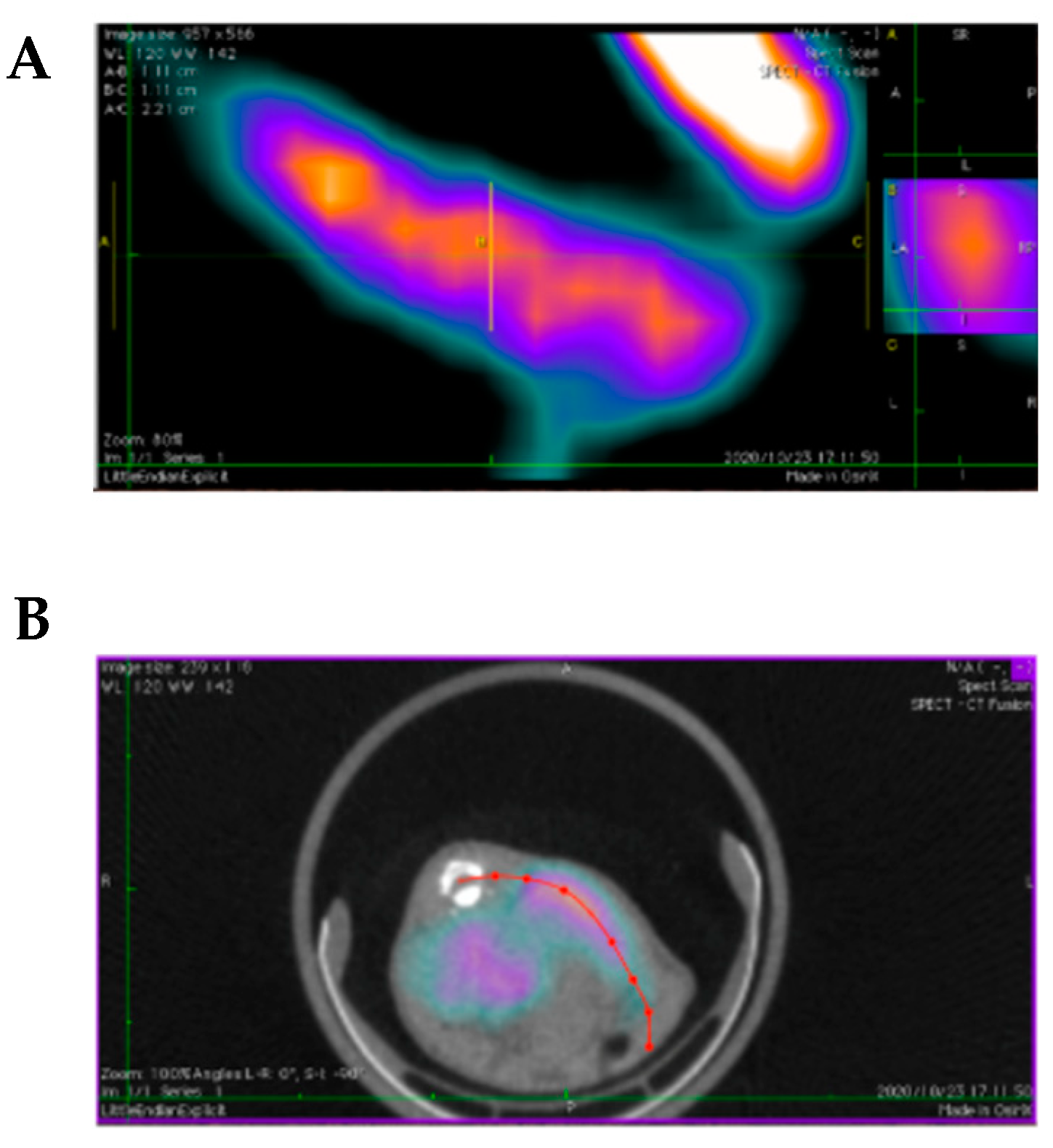
2.4. In Vivo Studies of [111In]In-DTPA-N-mAb in SFTSV- and Mock-Infected Mice
3. Materials and Methods
3.1. Materials
3.2. Preparation of SFTS Virus (SFTSV)-Infected Cells
3.3. Immunofluorescence Staining of SFTSV-Infected Cells
3.4. Synthesis of DTPA-Antibodies
3.5. Radiosynthesis of [111In]In-DTPA Antibodies
3.6. Cellular Binding of [11IIn]In-DTPA Antibody in SFTS-Infected Cells
3.7. Biodistribution of 111In-DTPA-N-mAb in SFTSV-Infected Mice
3.8. Small-Animal SPECT/CT Imaging of SFTSV-Infected Mice
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yu, X.J.; Liang, M.F.; Zhang, S.Y.; Liu, Y.; Li, J.D.; Sun, Y.L.; Zhang, L.; Zhang, Q.F.; Popov, V.L.; Li, C.; et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N. Engl. J. Med. 2011, 364, 1523–1532. [Google Scholar] [CrossRef]
- Kuhn, J.H.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Amarasinghe, G.K.; Anthony, S.J.; Avšič-Županc, T.; Ayllón, M.A.; Bahl, J.; Balkema-Buschmann, A.; et al. 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales. Arch. Virol. 2020, 165, 3023–3072. [Google Scholar] [CrossRef] [PubMed]
- Xing, X.; Guan, X.; Liu, L.; Xu, J.; Li, G.; Zhan, J.; Liu, G.; Jiang, X.; Shen, X.; Jiang, Y.; et al. A Case-control Study of Risk Sources for Severe Fever with Thrombocytopenia Syndrome in Hubei Province, China. Int. J. Infect. Dis. 2017, 55, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.X.; Yang, X.; Leng, Y.; Li, J.C.; Yuan, L.; Wang, Z.; Fan, X.J.; Yuan, C.; Liu, W.; Li, H. Human-to-human transmission of severe fever with thrombocytopenia syndrome virus through potential ocular exposure to infectious blood. Int. J. Infect. Dis. 2022, 123, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Gong, Z.; Gu, S.; Zhang, Y.; Sun, J.; Wu, X.; Ling, F.; Shi, W.; Zhang, P.; Li, D.; Mao, H.; et al. Probable aerosol transmission of severe fever with thrombocytopenia syndrome virus in southeastern China. Clin. Microbiol. Infect. 2015, 21, 1115–1120. [Google Scholar] [CrossRef]
- Li, H.; Lu, Q.B.; Xing, B.; Zhang, S.F.; Liu, K.; Du, J.; Li, X.K.; Cui, N.; Yang, Z.D.; Wang, L.Y.; et al. Epidemiological and clinical features of laboratory-diagnosed severe fever with thrombocytopenia syndrome in China, 2011–2017: A prospective observational study. Lancet Infect. Dis. 2018, 18, 1127–1137. [Google Scholar] [CrossRef]
- Xu, B.; Liu, L.; Huang, X.; Ma, H.; Zhang, Y.; Du, Y.; Wang, P.; Tang, X.; Wang, H.; Kang, K.; et al. Metagenomic analysis of fever, thrombocytopenia and leukopenia syndrome (FTLS) in Henan Province, China: Discovery of a new bunyavirus. PLoS Pathog. 2011, 7, e1002369. [Google Scholar] [CrossRef]
- Takahashi, T.; Maeda, K.; Suzuki, T.; Ishido, A.; Shigeoka, T.; Tominaga, T.; Kamei, T.; Honda, M.; Ninomiya, D.; Sakai, T.; et al. The First Identification and Retrospective Study of Severe Fever with Thrombocytopenia Syndrome in Japan. J. Infect. Dis. 2013, 209, 816–827. [Google Scholar] [CrossRef]
- McMullan, L.K.; Folk, S.M.; Kelly, A.J.; MacNeil, A.; Goldsmith, C.S.; Metcalfe, M.G.; Batten, B.C.; Albariño, C.G.; Zaki, S.R.; Rollin, P.E.; et al. A new phlebovirus associated with severe febrile illness in Missouri. N. Engl. J. Med. 2012, 367, 834–841. [Google Scholar] [CrossRef]
- Chen, Q.L.; Zhu, M.T.; Chen, N.; Yang, D.; Yin, W.W.; Mu, D.; Li, Y.; Zhang, Y.P.; Zainawudong, Y. Epidemiological characteristics of severe fever with thtrombocytopenia syndrome in China, 2011–2021. Zhonghua Liu Xing Bing Xue Za Zhi 2022, 43, 852–859. [Google Scholar]
- Yang, T.; Huang, H.; Jiang, L.; Li, J. Overview of the immunological mechanism underlying severe fever with thrombocytopenia syndrome. Int. J. Mol. Med. 2022, 50, 118. [Google Scholar] [CrossRef]
- Luo, N.; Li, M.; Xu, M.; Shi, C.; Shi, X.; Ni, R.; Chen, Y.; Zheng, L.; Tu, Y.; Hu, D.; et al. Research Progress of Fever with Thrombocytopenia Syndrome. Intensive Care Res. 2023, 3, 172–181. [Google Scholar] [CrossRef]
- Akbar, M.R.; Pranata, R.; Wibowo, A.; Lim, M.A.; Sihite, T.A.; Martha, J.W. The prognostic value of elevated creatine kinase to predict poor outcome in patients with COVID-19—A systematic review and meta-analysis. Diabetes Metab. Syndr. 2021, 15, 529–534. [Google Scholar] [CrossRef]
- Wang, Y.; Song, Z.; Wei, X.; Yuan, H.; Xu, X.; Liang, H.; Wen, H. Clinical laboratory parameters and fatality of Severe fever with thrombocytopenia syndrome patients: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2022, 16, e0010489. [Google Scholar] [CrossRef]
- Wang, F.; Wu, Y.; Jiao, J.; Wang, J.; Ge, Z. Risk Factors and Clinical Characteristics of Severe Fever with Thrombocytopenia Syndrome. Int. J. Gen. Med. 2020, 13, 1661–1667. [Google Scholar] [CrossRef]
- Yan, X.; Luo, C.; Yang, J.; Wang, Z.; Shao, Y.; Wang, P.; Yang, S.; Li, Y.; Dai, Q.; Li, W.; et al. Antiviral Activity of Selective Estrogen Receptor Modulators against Severe Fever with Thrombocytopenia Syndrome Virus In Vitro and In Vivo. Viruses 2024, 16, 1332. [Google Scholar] [CrossRef]
- Li, H.; Zhang, L.K.; Li, S.F.; Zhang, S.F.; Wan, W.W.; Zhang, Y.L.; Xin, Q.L.; Dai, K.; Hu, Y.Y.; Wang, Z.B.; et al. Calcium channel blockers reduce severe fever with thrombocytopenia syndrome virus (SFTSV) related fatality. Cell Res. 2019, 29, 739–753. [Google Scholar] [CrossRef]
- Liu, W.; Lu, Q.B.; Cui, N.; Li, H.; Wang, L.Y.; Liu, K.; Yang, Z.D.; Wang, B.J.; Wang, H.Y.; Zhang, Y.Y.; et al. Case-fatality ratio and effectiveness of ribavirin therapy among hospitalized patients in china who had severe fever with thrombocytopenia syndrome. Clin. Infect. Dis. 2013, 57, 1292–1299. [Google Scholar] [CrossRef]
- Tani, H.; Fukuma, A.; Fukushi, S.; Taniguchi, S.; Yoshikawa, T.; Iwata-Yoshikawa, N.; Sato, Y.; Suzuki, T.; Nagata, N.; Hasegawa, H.; et al. Efficacy of T-705 (Favipiravir) in the Treatment of Infections with Lethal Severe Fever with Thrombocytopenia Syndrome Virus. mSphere 2016, 1, e00061-15. [Google Scholar] [CrossRef]
- Rudin, M.; Weissleder, R. Molecular imaging in drug discovery and development. Nat. Rev. Drug Discov. 2003, 2, 123–131. [Google Scholar] [CrossRef]
- Willmann, J.K.; van Bruggen, N.; Dinkelborg, L.M.; Gambhir, S.S. Molecular imaging in drug development. Nat. Rev. Drug Discov. 2008, 7, 591–607. [Google Scholar] [CrossRef]
- De Winter, F.; Vogelaers, D.; Gemmel, F.; Dierckx, R.A. Promising role of 18-F-fluoro-D-deoxyglucose positron emission tomography in clinical infectious diseases. Eur. J. Clin. Microbiol. Infect. Dis. 2002, 21, 247–257. [Google Scholar] [CrossRef]
- Tzen, K.Y.; Oster, Z.H.; Wagner, H.N., Jr.; Tsan, M.F. Role of iron-binding proteins and enhanced capillary permeability on the accumulation of gallium-67. J. Nucl. Med. 1980, 21, 31–35. [Google Scholar]
- Hayasaka, D.; Nishi, K.; Fuchigami, T.; Shiogama, K.; Onouchi, T.; Shimada, S.; Tsutsumi, Y.; Morita, K. 18F-FDG PET imaging for identifying the dynamics of intestinal disease caused by SFTSV infection in a mouse model. Oncotarget 2016, 7, 140–147. [Google Scholar] [CrossRef]
- Fuchigami, T.; Ono, H.; Oyadomari, K.; Iwatake, M.; Hayasaka, D.; Akbari, M.; Yui, K.; Nishi, K.; Kudo, T.; Yoshida, S.; et al. Development of a 68Ge/68Ga Generator System Using Polysaccharide Polymers and Its Application in PET Imaging of Tropical Infectious Diseases. ACS Omega 2017, 2, 1400–1407. [Google Scholar] [CrossRef]
- Liu, Q.; He, B.; Huang, S.Y.; Wei, F.; Zhu, X.Q. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect. Dis. 2014, 14, 763–772. [Google Scholar] [CrossRef]
- Zhou, H.; Sun, Y.; Wang, Y.; Liu, M.; Liu, C.; Wang, W.; Liu, X.; Li, L.; Deng, F.; Wang, H.; et al. The nucleoprotein of severe fever with thrombocytopenia syndrome virus processes a stable hexameric ring to facilitate RNA encapsidation. Protein Cell 2013, 4, 445–455. [Google Scholar] [CrossRef]
- Magurano, F.; Nicoletti, L. Humoral response in Toscana virus acute neurologic disease investigated by viral-protein-specific immunoassays. Clin. Diagn. Lab. Immunol. 1999, 6, 55–60. [Google Scholar] [CrossRef]
- Martín-Folgar, R.; Lorenzo, G.; Boshra, H.; Iglesias, J.; Mateos, F.; Borrego, B.; Brun, A. Development and characterization of monoclonal antibodies against Rift Valley fever virus nucleocapsid protein generated by DNA immunization. MAbs 2010, 2, 275–284. [Google Scholar] [CrossRef]
- Yu, F.; Du, Y.; Huang, X.; Ma, H.; Xu, B.; Adungo, F.; Hayasaka, D.; Buerano, C.C.; Morita, K. Application of recombinant severe fever with thrombocytopenia syndrome virus nucleocapsid protein for the detection of SFTSV-specific human IgG and IgM antibodies by indirect ELISA. Virol. J. 2015, 12, 117. [Google Scholar] [CrossRef]
- Umeki, K.; Yasuda, A.; Umekita, K.; Megumi, R.; Nomura, H.; Kawaguchi, T.; Matsuda, M.; Takajo, I.; Shimojima, M.; Okayama, A. Detection of anti-SFTSV nuclear protein antibody in the acute phase sera of patients using double-antigen ELISA and immunochromatography. J. Virol. Methods 2020, 285, 113942. [Google Scholar] [CrossRef]
- Nanbo, A.; Watanabe, S.; Halfmann, P.; Kawaoka, Y. The spatio-temporal distribution dynamics of Ebola virus proteins and RNA in infected cells. Sci. Rep. 2013, 3, 1206. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, B.; Paessler, S.; Walker, D.H.; Tesh, R.B.; Yu, X.J. The pathogenesis of severe fever with thrombocytopenia syndrome virus infection in alpha/beta interferon knockout mice: Insights into the pathologic mechanisms of a new viral hemorrhagic fever. J. Virol. 2014, 88, 1781–1786. [Google Scholar] [CrossRef]
- Shimada, S.; Posadas-Herrera, G.; Aoki, K.; Morita, K.; Hayasaka, D. Therapeutic effect of post-exposure treatment with antiserum on severe fever with thrombocytopenia syndrome (SFTS) in a mouse model of SFTS virus infection. Virology 2015, 482, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Verel, I.; Visser, G.W.; Boellaard, R.; Boerman, O.C.; van Eerd, J.; Snow, G.B.; Lammertsma, A.A.; van Dongen, G.A. Quantitative 89Zr immuno-PET for in vivo scouting of 90Y-labeled monoclonal antibodies in xenograft-bearing nude mice. J. Nucl. Med. 2003, 44, 1663–1670. [Google Scholar]
- Suzuki, H.; Matsukawa, M.; Madokoro, R.; Terasaka, Y.; Kannaka, K.; Uehara, T. Reduction of the hepatic radioactivity levels of [111In]In-DOTA-labeled antibodies via cleavage of a linkage metabolized in lysosomes. Nucl. Med. Biol. 2024, 132–133, 108910. [Google Scholar] [CrossRef]
- Cicone, F.; Denoël, T.; Gnesin, S.; Riggi, N.; Irving, M.; Jakka, G.; Schaefer, N.; Viertl, D.; Coukos, G.; Prior, J.O. Preclinical Evaluation and Dosimetry of [111In]CHX-DTPA-scFv78-Fc Targeting Endosialin/Tumor Endothelial Marker 1 (TEM1). Mol. Imaging Biol. 2020, 22, 979–991. [Google Scholar] [CrossRef]
- Alakonya, H.; Koustoulidou, S.; Hopkins, S.L.; Veal, M.; Ajenjo, J.; Sneddon, D.; Dias, G.; Mosley, M.; Baguña Torres, J.; Amoroso, F.; et al. Molecular Imaging of p53 in Mouse Models of Cancer Using a Radiolabeled Antibody TAT Conjugate with SPECT. J. Nucl. Med. 2024, 65, 1626–1632. [Google Scholar] [CrossRef]
- Hiraki, T.; Yoshimitsu, M.; Suzuki, T.; Goto, Y.; Higashi, M.; Yokoyama, S.; Tabuchi, T.; Futatsuki, T.; Nakamura, K.; Hasegawa, H.; et al. Two autopsy cases of severe fever with thrombocytopenia syndrome (SFTS) in Japan: A pathognomonic histological feature and unique complication of SFTS. Pathol. Int. 2014, 64, 569–575. [Google Scholar] [CrossRef]
- Matsuno, K.; Orba, Y.; Maede-White, K.; Scott, D.; Feldmann, F.; Liang, M.; Ebihara, H. Animal Models of Emerging Tick-Borne Phleboviruses: Determining Target Cells in a Lethal Model of SFTSV Infection. Front. Microbiol. 2017, 8, 104. [Google Scholar] [CrossRef]
- Suzuki, T.; Sato, Y.; Sano, K.; Arashiro, T.; Katano, H.; Nakajima, N.; Shimojima, M.; Kataoka, M.; Takahashi, K.; Wada, Y.; et al. Severe fever with thrombocytopenia syndrome virus targets B cells in lethal human infections. J. Clin. Investig. 2020, 130, 799–812. [Google Scholar] [CrossRef] [PubMed]
- Deng, B.; Zhou, B.; Zhang, S.; Zhu, Y.; Han, L.; Geng, Y.; Jin, Z.; Liu, H.; Wang, D.; Zhao, Y.; et al. Clinical features and factors associated with severity and fatality among patients with severe fever with thrombocytopenia syndrome Bunyavirus infection in Northeast China. PLoS ONE 2013, 8, e80802. [Google Scholar] [CrossRef] [PubMed]
- Varghese, J.; De Silva, I.; Millar, D.S. Latest Advances in Arbovirus Diagnostics. Microorganisms 2023, 11, 1159. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Tanaka, M.; Oba, M. Protein transfection study using multicellular tumor spheroids of human hepatoma Huh-7 cells. PLoS ONE 2013, 8, e82876. [Google Scholar] [CrossRef]
- Fuchigami, T.; Chiga, T.; Yoshida, S.; Oba, M.; Fukushima, Y.; Inoue, H.; Matsuura, A.; Toriba, A.; Nakayama, M. Synthesis and Characterization of Radiogallium-Labeled Cationic Amphiphilic Peptides as Tumor Imaging Agents. Cancers 2021, 13, 2388. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuchigami, T.; Ngwe Tun, M.M.; Tanahara, Y.; Nishi, K.; Yoshida, S.; Ogawa, K.; Nakayama, M.; Hayasaka, D. Development of 111In-Labeled Monoclonal Antibodies Targeting SFTSV Structural Proteins for Molecular Imaging of SFTS Infectious Diseases by SPECT. Molecules 2025, 30, 38. https://doi.org/10.3390/molecules30010038
Fuchigami T, Ngwe Tun MM, Tanahara Y, Nishi K, Yoshida S, Ogawa K, Nakayama M, Hayasaka D. Development of 111In-Labeled Monoclonal Antibodies Targeting SFTSV Structural Proteins for Molecular Imaging of SFTS Infectious Diseases by SPECT. Molecules. 2025; 30(1):38. https://doi.org/10.3390/molecules30010038
Chicago/Turabian StyleFuchigami, Takeshi, Mya Myat Ngwe Tun, Yusuke Tanahara, Kodai Nishi, Sakura Yoshida, Kazuma Ogawa, Morio Nakayama, and Daisuke Hayasaka. 2025. "Development of 111In-Labeled Monoclonal Antibodies Targeting SFTSV Structural Proteins for Molecular Imaging of SFTS Infectious Diseases by SPECT" Molecules 30, no. 1: 38. https://doi.org/10.3390/molecules30010038
APA StyleFuchigami, T., Ngwe Tun, M. M., Tanahara, Y., Nishi, K., Yoshida, S., Ogawa, K., Nakayama, M., & Hayasaka, D. (2025). Development of 111In-Labeled Monoclonal Antibodies Targeting SFTSV Structural Proteins for Molecular Imaging of SFTS Infectious Diseases by SPECT. Molecules, 30(1), 38. https://doi.org/10.3390/molecules30010038







