Abstract
Recently, non-covalent reactions have emerged as approaches to improve the physicochemical properties of active pharmaceutical ingredients (API), including antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs). This review aimed to present and discuss the non-covalent reaction products of antibiotics, including salt and neutral multi-component solid forms, by framing their substituents and molar ratios, manufacturing techniques, characterization methods, benefits, potency changes, and toxicity, and is completed with an analysis of the development of computational models used in this field. Based on the data, NSAIDs are the most-developed drugs in multi-component system preparations, followed by antibiotics, i.e., antituberculosis and fluoroquinolones. They have reacted with inorganic elements, excipients, nutraceuticals, natural products, and other drugs. However, in terms of treatments for common infections, fluoroquinolones are more frequently used. Generally, NSAIDs are acquired on an over-the-counter basis, causing inappropriate medication. In addition, the pKa differences between the two groups of medicine offer the potential for them to react non-covalently. Hence, this review highlights fluoroquinolone–NSAID multi-component solid systems, which offer some benefits. These systems can increase patient compliance and promote the appropriate monitoring of drug usage; the dual drug multi-component solids have been proven to improve the physicochemical properties of one or both components, especially in terms of solubility and stability. In addition, some reports show an enhancement of the antibiotic activity of the products. However, it is important to consider the possibility of activity changes, interaction, and toxicity when using drug combinations. Hence, these aspects also are discussed in this review. Finally, we present computational modeling, which has been utilized broadly to support multi-component system designs, including coformer screening, preparation methods, and structural modeling, as well as to predict physicochemical properties, potency, and toxicity. This integrated review is expected to be useful for further antibiotic–NSAID multi-component system development.
1. Introduction
Antibiotics have been some of the most used drugs in the last decades. Consequently, microorganism resistance has occurred due to their longtime usage. In addition, antibiotics must target microbes, but should be safe for human cells; hence, their toxicity must also be considered. On the other hand, low solubility and instability are typical problems for some antibiotics, which may cause the drug’s content not to reach the appropriate levels. Next, chemical degradation also may produce toxicity and allergens. Thereafter, efforts have been made to find more selective, potent, safe, and effective antibiotics. However, the complexity of finding new drugs, from modeling and synthesis to clinical testing and formulation, makes the process slow [1].
The development of new drugs requires reagents, i.e., starting chemicals, catalysis, solvent organics, etc. In addition, the synthesis of new drugs requires optimization to obtain a high percentage of yield or purity. Besides, the process may create chemical waste and side products. After its synthesis, a new synthetic drug should be evaluated by more extended pharmacological testing, including toxicity, mutagenicity, clinical testing Phase I, II, and III, etc., before it can be accepted as a suitable active pharmaceutical ingredient. These, often long, steps of drug discovery are costly because they consume a significant amount of resources and time.
In addition to traditional drug development strategies, combining existing drugs with other compounds to create multi-component solids is becoming an increasingly interesting approach to improving drug performance. This technique requires less solvent and is easier to perform than other methods, making it an attractive option. The process involves low-energy, non-covalent reactions that don’t affect the drug–receptor binding, making it ideal for use in the body. By using established drugs to create multi-component systems, certain clinical tests may be avoided, making the solid engineering technique even more desirable. In addition, no reagents are used, high yields are obtained, and almost no waste or residue is yielded. However, it’s important to carefully consider the interaction cases when combining APIs in a multi-component solid.
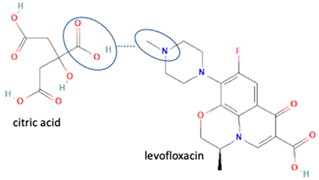
Computational structure–activity relationship modeling has been progressively developed to predict antibiotics’ structure, potency, resistance, mechanism of action, and toxicity [2,3]. One study proved that similar structures tend to show similar physicochemical properties. For example, all fluoroquinolones may have photosensitivity, hygroscopicity, and pH-dependent solubility, confirming the experimental data [4,5]. Hence, many efforts have been performed to overcome those lack of properties. One of the common strategies is reacting antibiotics with inorganic chemicals (metals/halogens) or organic compounds, such as other drugs, excipients, nutraceuticals, etc. Moreover, in addition to improving the solid characteristics, experiments have shown that fluoroquinolone antibiotics can enhance potency by changing the polarity and penetrability of the bacteria’s membrane through non-covalent reactions [6,7].
On the other hand, aside from antibiotics, infected patients usually consume anti-inflammatory agents to overcome inflammation symptoms. NSAIDs (non-steroidal anti-inflammatory drugs), which have relatively few adverse effects, have become first-choice drugs, and are available widely in various dosage forms. However, they generally have low solubility. Furthermore, some are physically unstable, i.e., they show polymorphism and pseudopolymorphism, which change their solid characters. In addition, they may also be chemically unstable. NSAIDs also have exhibited non-covalency with various counterparts in the multi-component solids, which could explain their lack of physicochemical properties. Furthermore, combining both medicines to enhance patient convenience and compliance and improve their physicochemical properties without changing their activity is an exciting prospect. This effort is supported by the fact that many NSAIDs tend to be acidic [8]; inversely, many antibacterial compounds are basic [6,7], or they may be amphoteric [6,7,8]. Hereafter, many antibiotics–NSAID combinations are feasible, resulting in non-covalent interactions and the production of multi-component solid systems.
The first and crucial step in creating multi-component structures is determining the coformer or stoichiometric ratio. Once this is established, appropriate methods can be used to react with the components, including slow evaporation, fast evaporation, neat grinding, liquid-assisted grinding, slurry, and co-precipitation [9,10,11]. Additionally, greener methods are currently available, such as hot melt extrusion (HME) [12], supercritical carbon dioxide [13], sonication slurry technique [14], sublimation [15], and microwaving [16,17]. After this process, reliable analysis methods can be used to confirm the new solid phase formation. Firstly, the thermal analysis may be performed using an electrothermal measurement [6,7], thermogravimetry analysis (TG) [18,19], differential thermal analysis (DTA) [19,20], and differential scanning calorimetry (DSC) [6,7,11,12,21] can be used to identify a new phase. An endothermic curve and the melting point may represent the water released from the hydrate system. Meanwhile, recrystallization is shown by an exothermic curve and degradation, with irregular exothermic curves [6,7,20]. Therefore, a new structure’s thermogram has a different pattern from a single component or physical mixture. Thermal analysis has long been used in pharmaceutical research to identify and detect purity based on phase thermodynamic principles [21,22,23].
However, only powder X-ray diffraction (PXRD) can precisely identify the new solid phase formation based on the diffractogram pattern. The specific distance and intensity represent the unique electron position of the atoms in the new crystal lattice. Hence, different diffractogram patterns from the starting materials indicate the multi-component crystal structure formation. Next, a solid analysis should be conducted to fix the structure and kind of interaction. Various methods can be used, including vibrational spectroscopy techniques such as Fourier transform infrared spectroscopy (FTIR), Raman spectroscopy, and Terahertz spectroscopy, as well as nuclear magnetic resonance (NMR) [24,25].
This review aims to present and discuss various antibiotic multi-component structures and their preparation methods, challenges, and benefits. First, we highlight antituberculosis agents as the first antibiotic multi-component systems. Then, we discuss fluoroquinolone multi-component solids, which are the currently most-reported structures. However, these drugs can be poorly soluble and unstable in light and humid conditions. It has been found that N-methyl-amine-piperazine is responsible for photodegradation and requires protection [26,27,28,29]. On the other side, NSAIDs are insoluble, and some are unstable, such as indomethacin and diclofenac acid [8]. Hence, in another section, we describe combinations with NSAIDs, since they are commonly used to treat infected patients [30,31,32], completing the paper with considerations regarding the activity and toxicity caused by drug–drug interactions [31,32,33].
Finally, the in-silico method has been recognized. It is currently preferred, as a green, efficient, and effective tool for designing new multi-component solids and calculating their physicochemical properties [34,35,36,37,38], as well as for predicting their activity and toxicity [39,40]. This review attempted to provide comprehensive information and is expected to encourage good design and experimental research on developing antibiotic–anti-inflammatory combinations.
2. Antibiotics
Based on their chemical structure and mechanism of action, antibiotics are divided into six groups: (1) cell wall synthesis inhibitors, including the beta-lactam class (e.g., penicillin, cephalosporin, and carbapenem) and dissimilar agents, such as cycloserine, vancomycin, and bacitracin [41]; (2) those that directly work on the cell membrane of the microorganisms, to increase permeability and lead to leakage of intracellular compounds, which include detergents such as polymyxin, and polyene antifungal agents, which bind to cell-wall sterols (e.g., nystatin and amphotericin B) [42]; (3) 30S or 50S ribosomal subunit disruptors, which reversibly inhibit protein synthesis, and commonly work bacteriostatic agents (e.g., chloramphenicol, the tetracyclines, erythromycin, clindamycin, streptogramins, and linezolid) [43]; (4) agents that bind to the 30S ribosomal subunit and alter protein synthesis, which are generally bactericidal (e.g., the aminoglycosides) [44]; (5) agents that affect bacterial nucleic acid metabolism, such as rifamycin, rifampin and rifabutin, and inhibit RNA polymerase [45,46]; the quinolones, which inhibit topoisomerases [47]; (6) antimetabolites, including trimethoprim and the sulfonamides, block essential enzymes of folate metabolism [48].
Meanwhile, based on indications, antibiotics are divided into sulfonamides, trimethoprim, sulfamethoxazole, quinolones (nalidixic acid, ciprofloxacin, delafloxacin, gatifloxacin, levofloxacin, moxifloxacin, norfloxacin, ofloxacin, pefloxacin, sitafloxacin), penicillin, cephalosporins, aminoglycosides, macrolides, clindamycin, quinupristin/dalfopristin, linezolid, vancomycin, teicoplanin, daptomycin, bacitracin, polymyxin, and mupirocin [1,48]. Those antibiotic classes are listed in Table 1. Many new-generation antibiotics are still being developed.

Table 1.
Antibiotics groups summary [1,41,43,44,48,49].
3. Antibiotic Multi-Component Structure Development
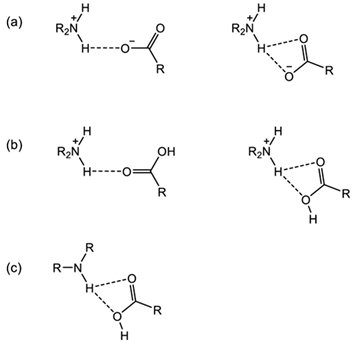
A multi-component crystal is a solid phase consisting of more than one kind of molecule stoichiometrically. This solid phase comprises intermolecular bonds between the components, which are also influenced by their intramolecular chemical bonding. Based on the type of interactions, the multi-component solids are divided into three groups: salts, cocrystals, and hydrate/solvate. The APIs can be an acid, base, or neutral compound, and can combine with another drug, nutraceutical, excipient, or substituent to form a multi-component crystal. Salt or cocrystal formation depends on the “rule of pKa”, which states that components with a pKa value of less than three will produce cocrystals; salt requires a pKa value higher than three. In addition, salt cocrystals can also be produced as a result of the reaction between neutral multi-component systems, acids or Schiff bases, and metal atoms [50].
Multi-component solids may be built by combining a non-soluble component with a water-soluble substituent via hydrogen bonding to attract the water molecules, increasing the solubility. The solid-state arrangement may improve a wide range of APIs’ physicochemical properties, including their solubility, stability, flowability, and permeability. Many also enhance activities and performances, as recently reported [30,51,52,53,54,55]. However, the first benefit is solubility enhancement, which is stated to be the most crucial characteristic of the particles. The solubility increase depends on the starting material’s properties, interaction type, and crystal structure conformation. For example, pymetrozine multi-component systems showed a four-fold improvement in these parameters [54], and nicorandil multi-component crystals showed a 1.9–5.2-fold improvement [55]. Meanwhile, the solubility of NSAIDs after salt formation with fluoroquinolones reaches values tens to hundreds of times higher than their parent compound [30].
Both ionic and non-ionic reactions of the fluoroquinolone group, i.e., ciprofloxacin and levofloxacin, with some substituents increase the solubility of these compounds [6,9], as well as showing increased stability towards humidity and light, which is the main advantage of these systems. For example, the combination of levofloxacin–citric acid [6] and levofloxacin–dihydroxybenzoic acid [7], and ciprofloxacin with cyclodextrin and cucurbit (7)-uril (CB7) improves photostability up to three-fold [27].
3.1. Salt/Ionic Multi-Component Structure
Salt is formed by the different ionic/charge compounds, which transfer hydrogen atoms between acid and base moieties, and may consist of inorganic and organic counterparts to the host molecule. This structural derivation has been applied for a long time, significantly increasing drug solubility and stability, physically and chemically. In addition, the changes observed in antibiotics’ physicochemical properties after salt formation can improve in terms of antibacterial potency, as shown by levofloxacin in combination with antioxidants, citric acid [6], and dihydroxybenzoic acids [7], as well as by ciprofloxacin in combination with NSAIDs [30,31].
3.2. Neutral/Non-Ionic Multi-Component Structure or Cocrystal
Although it was discovered in 1844 and characterized in 1958, the term ‘cocrystal’ was first used in 1963 by Lawton and Lopez. This term refers to a combined system of solid compounds in a crystal lattice, formed due to non-ionic intermolecular bonding with at least a neutral organic counterpart, referred to as a “co-former”. A coformer, particularly non-API, should be pharmacologically neutral, non-toxic, and considered a GRAS (Generally Recognized as Safe) compound. The API and the paired combination must have different polarities to form cocrystals, which then interact in the binding site, known as a “synthon”. Supramolecular synthons may be a homo-synthon (same functional group) or hetero-synthons (various moieties). Drug–drug, drug–nutrient, drug–vitamin, and drug–excipient combinations can cause the formation of a neutral multi-component structure. The cocrystals may involve hydrogen or halogen bonding in two or more different neutral compounds. Furthermore, combining an ionic component with a cocrystal can form an “ionic-cocrystal” with a charge [18,50].
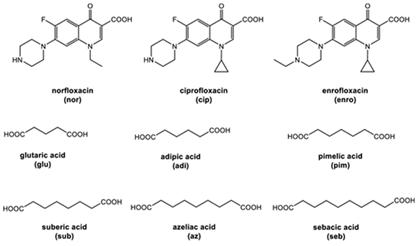
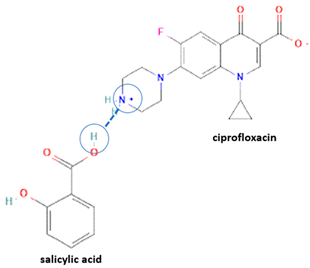
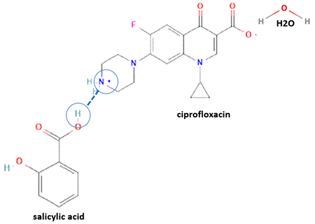
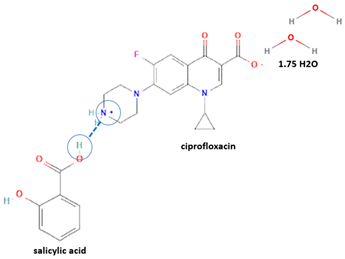
However, antibiotics may also form neutral and ionic multi-component solids, i.e., ciprofloxacin with dicarboxylic acids [9,21] and salicylic acid [31].
3.3. Hydrate and Solvate
Another type of multi-component solid is formed when a molecule compound interacts with an organic solvent or water molecule and builds a stoichiometrically neutral structure, producing a solvate and hydrate, respectively. Solvate and hydrate variations depend on concentration, temperature, humidity, and pressure. Naturally, many antibiotics have hydrate forms, which are commonly more stable than solvates, with different physicochemical properties, such as density, the molecular weight of the crystal, solubility, stability, hygroscopicity, etc. [18,26,56]. More importantly, the solvent or water portion should adjust the dose required, which is often unfixed or unpredictable.
Fluoroquinolones have many sites with the potential to form hydrogen bonds and, often, more than one lattice hydrate forms. For example, levofloxacin and ciprofloxacin may be observed in hemihydrate and monohydrate phases [6,7,19,26,56]. Technically, mainly pseudo-polymorphs are obtained through recrystallization using a solvent. However, as an important note, the degree of conformational flexibility of the molecule is very high, which affects the screening process, and the results of hydrate arrangement are unpredictable [56,57,58,59]. Therefore, an integrative analysis should be performed to determine the true pseudo-polymorphs, including PXRD, thermal analysis, i.e., DSC elaborated with thermogravimetry, and, finally, SCXRD.
3.4. Multi-Component System Preparation Methods
Several methods can be used to create a new solid structure, which can be categorized into three techniques: dissolving, grinding, and heating. The dissolution method commonly produces single crystals and comprises slow evaporation, rapid evaporation, cooling, chemical reactions, spraying, and freeze-drying [8,9]. In this method, active pharmaceutical ingredients (APIs) and a coformer are mixed and entirely dissolved in the solvent, then evaporated to produce salts or neutral combination compounds. Under the solution conditions, the components are mixed accurately, with the solvent facilitating the interaction between them. Next, the solvent evaporates when the solution is supersaturated, and hydrogen bonds or ionic interactions are formed between the molecules. This process goes slowly or quickly, depending on the contact area between the solvent and the atmosphere. In addition, the evaporation process may be accelerated by increasing the temperature and pressure, for example, by storing the solution in an evaporator chamber or using a rotavapor with the appropriate temperature setting. In terms of kinetic energy, the size of the multi-component crystal will be bigger if evaporation runs slowly. Conversely, the multi-component crystal will be smaller if the oration occurs quickly. The evaporation method produces thermodynamically stable crystals but requires a large amount of solvent.
Another evaporation method is a cooling technique at a low temperature to accelerate the saturated condition and produce more crystals spontaneously. Subsequently, the freeze-drying methods involve dispersing an unsaturated solvent into a nozzle using nitrogen gas. These processes aim to remove the unsaturated solution of drugs and co-formers through extreme conditions, such as the use of high pressure and low temperature, to cause the other parts become very saturated; as such, the evaporation process runs faster [8,9].
Next, grinding methods are divided into neat and solvent-assisted grinding. First, neat grinding is done in a mortar to mix and press the component thoroughly, without any solvent. This method produces large numbers of multi-component systems and is quicker than evaporation. However, the homogeneity of this method could be better in large-scale production. The second method is liquid-assisted grinding, using a small amount of solvent in the milling process. The solvent acts as a catalyst without waste production [60]. Other researchers report that a combination of ciprofloxacin–isonicotinic acid can be built by mechano-chemical synthesis, in order to improve stability [61]. This mechanochemical technique is recommended, as it is environmentally friendlier than evaporation due to the reduced usage of organic solvents. However, large-scale production homogeneity is still a challenge.
Heating methods include hot melt extrusion (HME) [12], microwave methods [16,17], and isothermal slurry [1]. High energy activates electrons and accelerates the reaction. Hot melt extrusion uses heat and pressure to melt the mixture in the extruder. The interactions between the drug and the excipient occur as they melt. This method is faster and reduces organic solvent usage. It has been informed that this technique was also tested on ciprofloxacin–isonicotinic acid, as well as the neat grinding method [61]. HME is fast but requires thermo-stable compounds, similar to microwave methods.
Next is the microwave method, which differs from HME in its energy source. HME uses a “stove” apparatus, heat conductance, and pressure; a microwave uses the radio-electromagnetic wave, which vibrates and excites the atoms and molecules. Microwaving accelerates this process and maximizes the multi-component solid yield significantly. For example, the diclofenac-L-proline cocrystal can be produced using a microwave in 30 s [16]. Last, the slurry method is used to suspend the components using water or other solvents, and then heat them, in order to intensify the reaction in wet conditions [11,12]. The powder or crystal yields that can be separated from the solvent make this technique greener than evaporation. This method has been used to synthesize caffeine/maleic acid co-crystals, supported by ultrasonication [12]. This method is restricted only to the undegradable compounds in the solution under hot conditions.
Besides conventional methods, some developed techniques exist, such as the supercritical process [13], sublimation [15], etc. The supercritical method uses a liquid gas, such as carbon dioxide, facilitating intensive contact between the reacting components. Supercritical carbon dioxide acts as a co-solvent and antisolvent, replacing conventional co-crystallization by selecting greener solvents, and may produce fine and uniform particles. The gas antisolvent is the most suitable in the supercritical fluid (SCF) co-crystallization process, possibly due to its similarities to conventional antisolvent methods. It was reported that solvent selection was one of the most critical parameters in producing the appropriate yield, phase purity, and polymorphs, to different extents. In addition, a systematic solubility study was required to optimize the processes [13].
Meanwhile, sublimation is a process that facilitates the formation of multi-component systems by providing the necessary energy to transform a mixture of solid components into a gas and subsequently condensing it into a multi-component solid form. Commonly, an oven is used simply in the hot melt extrusion and sublimation methods. However, this technique has been used to successfully isolate 4-fluorophenol–p-benzoquinone cocrystals, with different polymorphs than those in the conventional method’s yield, showing that sublimation determines the phase space of cocrystals [14].
3.5. Multi-Component Systems Analysis and Characterization Methods
The standard instruments and techniques used to confirm the new solid phase formation are microscopes (binocular/polarized/electron microscope, etc.), thermal analysis (electrothermal, DSC, TGA), vibrational spectrophotometry (FTIR, Raman, Terahertz spectroscopy), NMR, and X-ray diffractometry (PXRD AND SCXRD). Thermal analysis observes the thermal properties of solid compounds. Next, structural analysis methods, such as vibrational spectroscopy (FTIR, Raman, and Terahertz) and NMR, analyze structural changes that occur after a successful reaction. Finally, SCXRD determines the 3D conformation to show the atoms/molecules’ position, distance, and angle position of atoms and molecules.
In this subsequent, we present the solid instrumentations used to characterize the new multi-component phases.
3.5.1. Conventional and Semimanual Thermal Analysis
Every material has a unique energy that is reflected in its physicochemical properties. Thermal analysis, which observes the phase transitions of a substance under heating, such as melting point, recrystallization, oxidation, and degradation, is one of the oldest methods used for material characterization. In the past, conventional apparatuses such as a melting block, Thiele apparatus, or bomb calorimeter have been used to observe those parameters.
A simple thermal method in solid-state observation is thermal microscopy, published by Koffler many years ago [62], but it is still relevant today. An electrothermal microscope is a compact device used to observe the thermal profile of a solid phase, which is heated in order for one to observe phase changes or the transition point, including wetting due to the water release from the hydrate, recrystallization, and fusion, as well as determines a solid material’s melting point, degradation, and a range of other physical and chemical changes that occur during the heating. This method uses electrical energy as a heat source and a heat conductor. The sample only needs to fill a one-sided capillary tube. The starting temperature and the heating rate are set digitally. The components of the electrothermal device are the sample hole, capillary tube, heater, a magnifying lens for observation, and an integrated lamp. A visual hole allows the researcher to observe the solid-state changes. Multi-component systems show a different thermal profile than the single component and may have a lower [18,28] or higher melting point. This method is environmentally friendly as it requires no solvents, is low cost and easy to perform [6,7].
3.5.2. Modern Calorimetry: DSC and DTA/TG
A DSC is a calorimeter that measures the heat flow rate versus the temperature increase. This method is used to observe the thermal characteristics of a solid material in detail, such as the glass transition, water/solvent release from a pseudopolymorphism, fusion/melting point, recrystallization at high temperature, and decomposition, as well as to observe subtle physical changes, such as the glass transition temperature and eutectic point [22,23,63,64]. The DTA measures the temperature difference that occurs during heating and is commonly combined with a TG in one device. Finally, the TG measures the mass decrease resulting from heating and is the primary method used to characterize solvates/hydrates, supporting DSC and DTA data [6,7,18,65].
DSC and DTA thermograms will show endothermic and exothermic curves, representing the energy change during the phase transformation. For example, the glass transition is demonstrated by an endothermic blunt curve, a broad endothermic peak indicates water or solvent molecules release, the melting point shows a sharp endothermic curve, a sharp exothermic curve indicates recrystallization, and oxidation/degradation is indicated by some irregular curves [20,21,22,23]. Currently, almost all the multi-component development reports show the DSC data, indicating that this method is adequate for identifying a new entity with a specific energy.
Depending on their lattice thermodynamics, a multi-component crystal may have a lower or higher melting point/degradation temperature than the starting compounds. One can observe the energetical changes resulting from the interaction energy present in the new multi-component solid phase. For instance, the formation of the levofloxacin–phthalimide cocrystal and levofloxacin–caffeic acid salt led to a reduction in melting point, with values of 172–176 °C and 150–152 °C, respectively, compared to levofloxacin and the coformers, which all have melting points above 200 °C [53]. This indicates significant interaction of energy between the components in the new solid phase. On the other hand, levofloxacin salts, as yielded from reactions with citric acid [6] and dihydroxybenzoic acid [7], have higher melting points than those of the starting materials. In addition, levofloxacin salts are thermolabile and exhibit a degradation profile before melting, which is similar to the single antibiotic but at different temperatures [6,7,21,28].
3.5.3. Vibrational Spectroscopy Analysis
FTIR is commonly used in the characterization and identification of solid states. This method can recognize functional groups involving various bonds, including ionic, covalent, van der Waals, and hydrogen bonds. The working principle of this instrument is to measure the interaction of infrared waves with the bond energy between atoms. The transition of intramolecular vibrational energies (vibrations in the bonds between atoms) will be measured in terms of the amount of radiation contained in the infrared waves emitted by the source. Molecular vibrations are classified into two main groups: stretching and bending. The frequency of infrared waves is expressed in units of wave number (cm−1); the infrared wave spectrum has a wave number region of 14,000 cm−1 to 10 cm−1, but the region used for compound analysis is only the middle region, with a wavelength of 2.5–50 µm or wave number 400–4000 cm−1.
The vibrations in each molecule are unique, so this method is beneficial for identifying a compound. The specific spectrum of each type of bond is called fingerprint vibrations [8]. For example, in the case of hydrate forms, the presence of water molecules can be identified by characteristic peaks in the infrared spectrum, such as the hydrogen bonding stretching vibrations in the range of 2500–3500 cm−1. Next, the interaction between –COO and –NH synthons in a multi-component system is represented at 1500–1900 cm−1, as well as in the fingerprint area of 400–1500 cm−1 [8,60,64,65,66,67]. Hence, FTIR detects multi-component system formation by showing a distinctive spectrum. The salt reaction commonly exhibits a more apparent spectrum [7,9] than cocrystals do [18], reflecting their higher interaction energy [9]. This method is sensitive to moisture, but water molecules in a hydrate lattice have a specific band, which is narrower than the broad spectrum of the entrapped water on the particle’s surface.
Secondly, Raman spectroscopy is a useful tool for analyzing changes in the solid structure, such as hydrate formation, by identifying specific peaks. Raman spectroscopy has also been utilized to detect the presence of water molecules in the crystal lattice [64], for example, by analyzing the unique ciprofloxacin salicylate 1.75 hydrate [65]. Finally, Terahertz spectroscopy also has been used to identify new solid phase construction; for example, it has been previously used to determine pyrazinamide–3-hydroxybenzoic acid [68].
3.5.4. NMR
NMR is an adequate method for analyzing chemical structures two-dimensionally and has been available for measuring liquid and solid samples (solid-state NMR/SSNMR). NMR spectroscopy interacts with the nuclei of atoms with radio electromagnetic (REM) waves, then profiles the resonance frequency yielded. Solid-state NMR may identify and quantify the multi-component solids, of both a crystalline and amorphous nature, by using an irradiation frequency of 500–1000 MHz, with the C and H positions and their bindings represented by the chemical shift in the spectra. Hence, SSNMR deals with solid-structure elucidation, amorphous and crystal characterization, dynamics, and stability. The structure can be solved accurately by reading the exact position of the resonance of the distinct nuclei. NMR has been used in solid-state development to ensure the formation of new interactions. For example, the reaction of levofloxacin with citric acid [6] and dihydroxybenzoic acid [7] was identified by showing distinctive spectra compared to the starting materials. This method is beneficial in determining the structure in the case where an appropriate single crystal cannot be isolated, and when FTIR and SCXRD cannot predict the structure interaction.
3.5.5. X-ray Diffractometry
The X-ray diffractometry observes the change of atomic or molecular order and position, represented by their distance and angle in the lattice structure. X-ray diffraction is an analytical method based on the ability of a crystal to diffract X-rays and produce a characteristic pattern, which allows for an in-depth study of the solid phase structure. This diffraction method utilizes the constructive interference event of monochromatic X-rays. When X-ray radiation reaches atoms in the crystal structure, the high energy of the radiation will cause electrons to move to a higher level. However, this transfer of electrons does not last long because the state is unstable, so the electrons will return to their ground state and release light with identical wavelengths. This phenomenon is known as Rayleigh scattering.
X-ray diffractometry is specific to analyzing crystalline samples because the amorphous forms will not produce a regular diffraction pattern [63,69]. Instead, the diffraction pattern contains information from the contributions of a sample’s micro- and macro-structural features based on peak intensity data, information about the position and distance between atoms, temperature, space, and texture. It also can be used for quantitative phase analysis [69]. For example, PXRD analyzes the multi-component crystal formation mechanism and kinetics of a neutral diclofenac-L-proline multi-component crystal [70]. PXRD has become popular in solid pharmaceutical analysis due to the simplicity of sample preparation and the valuable data obtained regarding the crystalline drug phases [71].
Next, X-ray diffractometry is classified into PXRD (powder X-ray diffraction) and SCXRD (single crystal X-ray diffraction). PXRD differs from SCXRD in terms of sample preparation and instruments. PXRD measures the diffractogram of the powder sample, and SCXRD is used to determine a single crystal system’s new solid structure three-dimensionally. Hence, PXRD analysis is relatively faster than SCXRD, due to its more straightforward sample preparation steps. Practically, isolating single crystals with an appropriate size to be analyzed by SCXRD is challenging. However, PXRD requires a homogenous particle size with a dimension of less than ~10 μm. The small and homogenous crystal’s size can be randomly oriented, but the large variations in the particle size cause the broadening of the diffractogram and complicate structural assignments. In addition, PXRD requires an appropriate number of samples; meanwhile, SCXRD only needs one crystal but should be physically stable, with a size of about 0.1–0.5 mm [69]. SCXRD data collection is the final and crucial step and is used to reflect the reaction site and the non-covalent interactions, such as ionic or ionic neutral bonding.
SCXRD observes single or discrete diffraction peaks and transforms the peak positions into coordinates to recover the underlying crystal lattice dimensions or orientations commonly occurring in powder diffraction. As a result, the interpretation of single crystal diffraction is much less ambiguous than powder diffraction methods. Still, preparing the appropriate single crystal samples is challenging, laborious, and time-consuming. However, even though the crystal structure data are easier to interpret, the spatial properties of a single crystal may not represent the bulk solid, or appropriately describe the bulk properties of interest for a given application [72]. In this case, the structure’s image is commonly supported by software, such as SHELXL, SHELXT, and Mercury, in order to match the structure based on diffraction data, as measured by the goniometer [30,69,70].
Grinding with a mortar and pestle can be used for PXRD sample preparation, but it cannot be used for SCXRD, which requires a clear crystal. Therefore, only solvent-evaporation products are commonly used for SCXRD analysis. However, when using solvent evaporation, some hydrates and solvates may be formed [7,18,69]. Therefore, it is important to conduct an integrative study that combines various analytical methods to achieve the best results in the development of multi-component systems. This includes incorporating data from other solid analysis instruments in addition to PXRD measurements. PXRD measurements have been combined with other experiments under extreme conditions, such as high temperatures and pressures. This method may explore the material behavior changes as a function of these additional variables. For example, PXRD instruments have been integrated with DSC/DTA/TG, which is a widely used technique to investigate solid-state changes under different heating and pressure conditions, such as solvate/hydrate transformation, polymorphism, etc. [73]. PXRD can identify multi-component solids from their different diffractograms, rather than the component’s physical mixture. A diffractogram displays peaks at specific degrees of 2θ (x-axis) with varying intensities (y-axis) to determine crystallinity. Additionally, thermal analysis data, particularly TG, can help identify solvate and hydrate forms by calculating the mass decrease at the predicted water release temperature [18].
After a multi-component structure was obtained, some testing was conducted to evaluate the solid characters and properties, such as solubility, stability, hygroscopicity, etc. Moreover, some pharmacological aspects were checked, including activity, potency, and toxicity, to ensure the drug’s safety and efficacy.
3.6. List of Antibiotic Multi-Component
Antibiotics have been reacted using various counterions/coformers to produce multi-component solid systems and have become the most developed compounds in multi-component solid form after NSAIDs. That fact is probably due to the high feasibility of their structure to react with other compounds. Secondly, there are several issues regarding the lack of physicochemical properties, such as solubility and stability, that need to be addressed. Fluoroquinolones are the second most studied group of antibiotics for multi-component solids after antituberculosis, as shown in Table 2. This table depicts some of the multi-component antibiotics, complete with their structure, stoichiometric proportion, preparation methods, benefits, activity change, and toxicity notes.

Table 2.
Antibiotics Multi-component Solids.
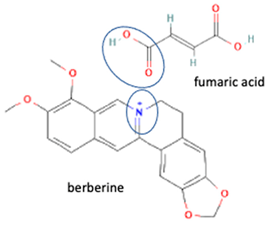
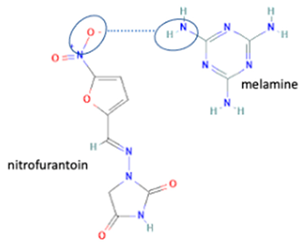
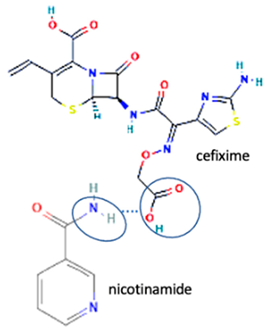
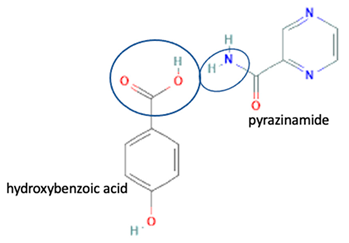
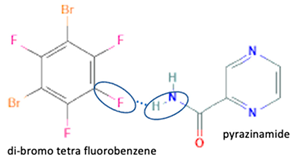
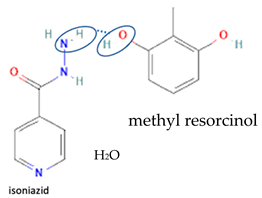
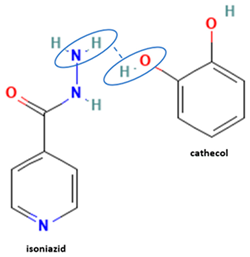
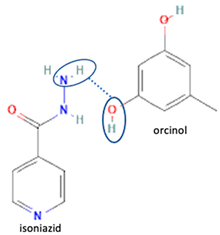
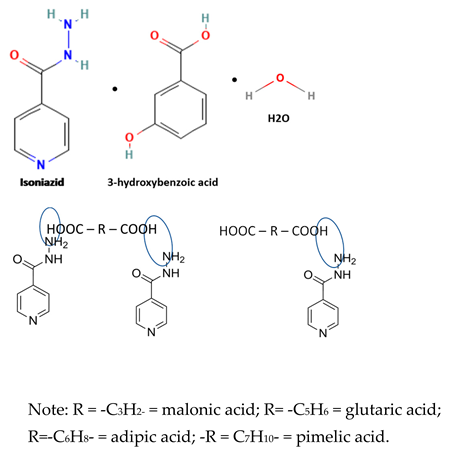
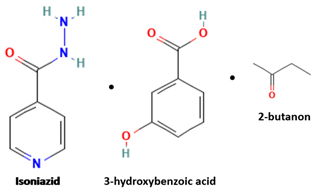
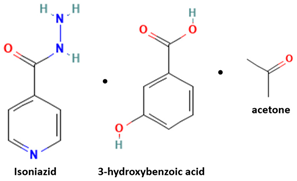
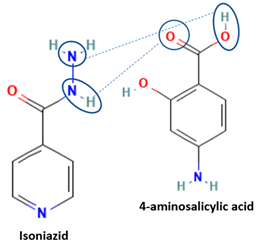
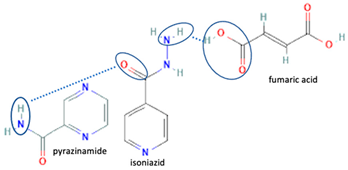
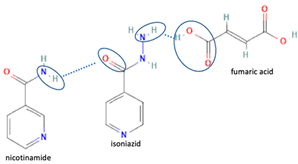
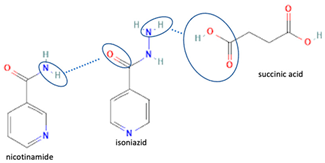
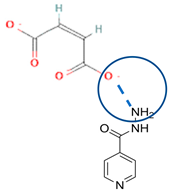
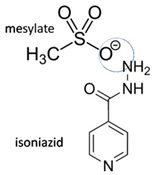
Table 2 shows some antibiotic multi-component crystals. For example, berberine HCl with fumaric acid [74] and nitrofurantoin–melamine [75] have increased stability. Next, researchers built many cocrystals of tuberculosis antibiotics to enhance their solubility and stability. Pyrazinamide and isoniazid are the specific antituberculosis agents developed in the multi-component solid by non-covalent reactions, such as that of the neutral combination of the antibiotic pyrazinamide and the preservative 3-hydroxybenzoic acid. The vibrational spectrometry data showed that the amino group of pyrazinamide forms a hydrogen bond at H11–N12–H13, with the -OH of the carboxylic acid of the conformer; this improved the physicochemical characteristics of the active pharmaceutical ingredient [68].
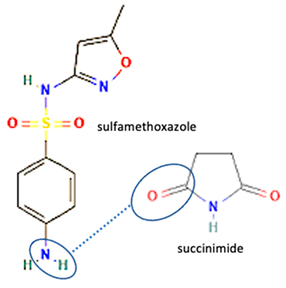
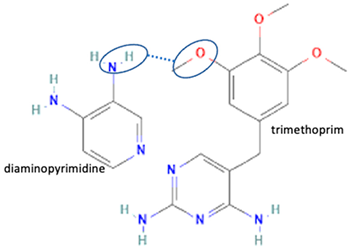
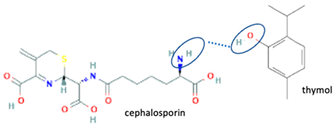
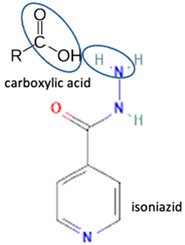
Additionally, from the cephalosporine group, cefixime was combined with nicotinamide to improve its solubility, dissolution, and stability [76]. Next, combining trimethoprim with 2,4-diaminopyrimidines pyrimethamine as a co-former built a crystal system with higher stability [80]. Afterward, sulfamethoxazole and succinimide multi-component solids showed higher stability than the base form [80,82]. In addition, cephalosporin with thymol produced a cocrystal that affected antibiotic activity [81].
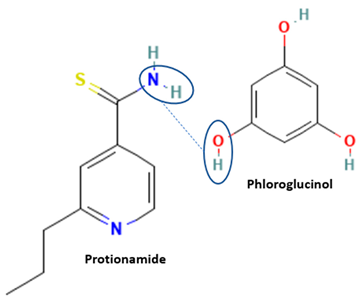
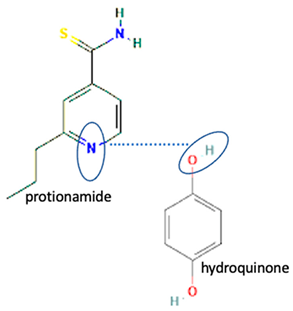
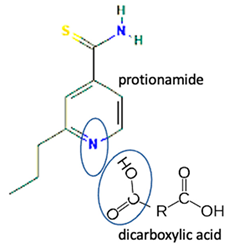
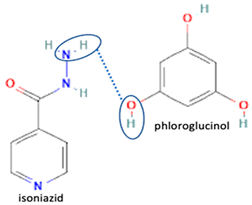
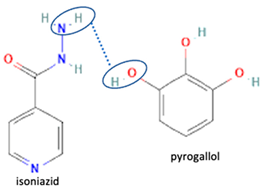
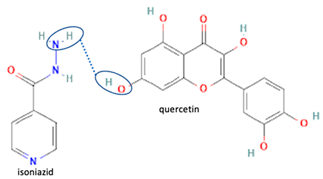
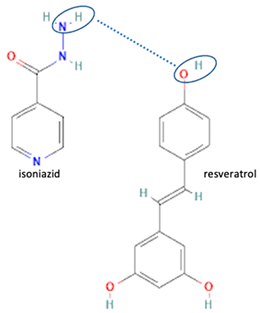
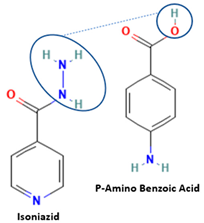
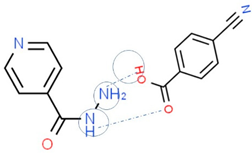
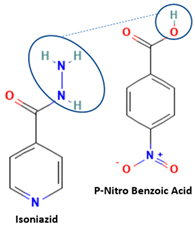
Isoniazid has been combined with some acid substituents (p-aminobenzoic acid, p-cyanobenzoic acid, etc.) and plant metabolites (catechol, quercetin, etc.). This group of acid–coformer agents exhibited better solubility and stability and lower hepatotoxicity than the parent drug and the second group, which was a combination of isoniazid with some base substituents. Afterward, the combinations of prothionamide and phloroglucinol produced a new solid phase [78], which was also achieved with hydroquinone. Among the systems, prothionamide–adipic acid reached the highest concentration in 24 h [79].
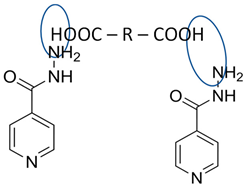
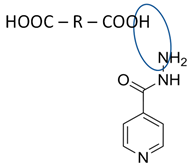
The multi-component systems comprising isoniazid–acid substituents and natural resources were the following: isoniazid combined with cinnamic acid, fumaric acid [74,82,85,86], mandelic acid [82,91], glutaric acid [84], pimelic acid [84], malonic acid [84], hydroxybenzoic acid [86], adipic acid [84,86], gallic acid [86], gentisic acid [82,86], succinic acid and nicotinamide [88], glycolic acid [91], benzoic acid [90], ferulic acid [98], and oleanolic acid [93], etc., which some of them enhancing stability and solubility, and others decreasing those parameters. It has been hypothesized that the carboxylic acid substitution changes isoniazid’s stability and solubility. In addition, the formation of hydrates could decrease the solubility and stability of isoniazid and the natural substitutions.
After the tuberculosis drugs, fluoroquinolones have become the most developed antibiotics, formed by non-covalent interactions with other components. Hereafter, the fluoroquinolone multi-component solid systems will be discussed in the following section, but we will still refer to the listing in Table 2. Moreover, a specific discussion about their combination with NSAIDs will be highlighted, including the possibility of altering their activity and the potential for drug–drug interactions and toxicity.
4. Fluoroquinolones Multi-Component Development
Fluoroquinolones are highlighted in this review because they are currently the most used antibiotics in common infectious bacterial diseases. Various fluoroquinolone derivatives show high effectiveness in killing bacteria. Structurally, their origin compound is nalidixic acid, with fluorine (F) added to the quinolone site, which produces a strong antibacterial effect. Ciprofloxacin, levofloxacin, ofloxacin, norfloxacin, lomefloxacin, moxifloxacin, pefloxacin, and sitafloxacin are the fluoroquinolones used clinically [4]. Those antibiotics are well absorbed and can be administered orally or parenterally [4]. However, this antibiotic group shows more effectiveness orally [23]. Fluoroquinolones act as bactericidal agents against a broad spectrum of bacteria, such as Escherichia, Salmonella, Shigella, Enterobacter, Campylobacter, Neisseria, and Staphylococcus [1]. In addition, fluoroquinolones kill Neisseria gonorrhea sp., which has been resistant to other antibiotics. Moreover, fluoroquinolones are also used to treat resistant Salmonella infections [36].
However, this antibiotic group generally has poor and pH-dependent solubility, besides exhibiting hydrate transformation, and is unstable in light [4,5]. Photo-degradation of these agents was reported to occur quickly, i.e., in one hour under UV lighting exposure. For example, levofloxacin was widely reported to degrade by UV radiation in both aqueous [103,104] and bulk solid form [105,106], as well as in a mixture with paracetamol [107]. The photolysis produced some toxic and allergenic products.
Another report explains that levofloxacin protected from daylight remained stable in 0.9% NaCl, 5% dextrose, and Ringer’s solution [5]. However, a slight decomposition of this antibiotic could still be observed after exposure to daylight, and Ringer’s solution was reported to show the fastest decomposition rate. The degradation product of levofloxacin was its N-oxide structure, from the oxidation of the methyl piperazine site, which is formed regardless of the solvent used. Hereafter, some efforts should be made to protect this compound from direct daylight [5,6,7,26,30].
Next, fluoroquinolone antibiotics are reported to have some hydrate forms, i.e., ciprofloxacin, levofloxacin, and sitafloxacin hydrates. The anhydrous levofloxacin absorbs some water molecules quickly and changes to a hemihydrate (levofloxacin 0.5 H2O) and then to a monohydrate (levofloxacin H2O). Inversely, in particular conditions, the hemihydrate could transform into anhydrous forms with various polymorphs (alpha, beta, gamma), or an amorphous form [19,58]. The different hydrate forms cause variability in physicochemical properties.
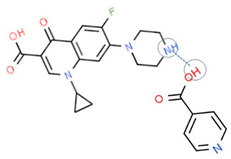
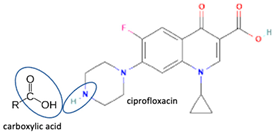
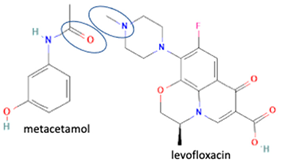
Fortunately, reports indicate that the instability towards light and the occurrence of pseudopolymorphism can be handled by reacting fluoroquinolone on the methyl–piperazine site with another component, with both ionic [6,7,30] and non-ionic interactions [26]. For example, a study combined levofloxacin with the antioxidant citric acid to form a salt, showing better photostability and increased antibiotic activity. In addition, citric acid protects levofloxacin’s N-methyl piperazine moiety from oxidative degradation [6]. Additionally, in other combinations, shown in Table 2, a quinolone derivative compound, berberine chloride, forms a multi-component salt with fumaric acid, which is more stable towards high temperatures and humidity than the starting drugs [74]. Next, the salt formation of levofloxacin with dihydroxybenzoic acids [7] and metacetamol 1:1 [26], as well as the combination of ciprofloxacin with a series of NSAIDs [30], also exhibits higher stability under humid and lit conditions than the fluoroquinolones [26].
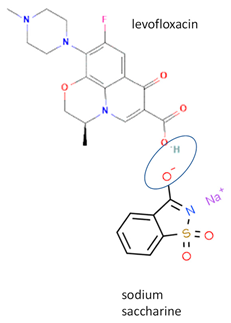
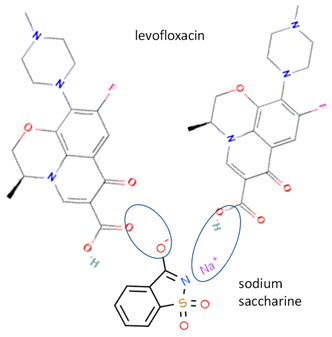
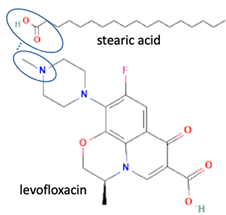
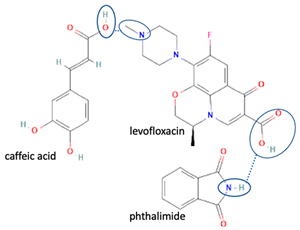
Next, levofloxacin also has been combined with phthalimide and caffeic acid as a promising solid-state molecule, with higher antimicrobial efficiency and stability performance [53]. Other multi-component solids include the combination of ciprofloxacin with dicarboxylic acids, which improves the stability and solubility of the parent antibiotic. Additionally, the study also investigated the multi-component systems of ciprofloxacin with nicotinic acid and isonicotinic acid, in a stoichiometric ratio of 1:1, and the results were added to the data [61]. These systems were prepared using the grinding method and showed better solubility than the original compound [99]. In addition, the combined cocrystals of levofloxacin with stearic acid and sodium saccharin as co-formers also have been reported. In addition to the 1:1 molar ratio, a multi-component system with a 2:1 stoichiometric ratio of sodium levofloxacin–saccharin was also reported. This combination was found to increase the antimicrobial effect while maintaining stability. In addition, the 1:1 levofloxacin–stearic acid can increase the dissolution rate and mask the bitter taste [100].
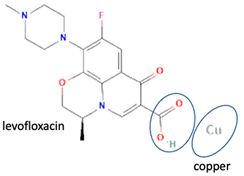
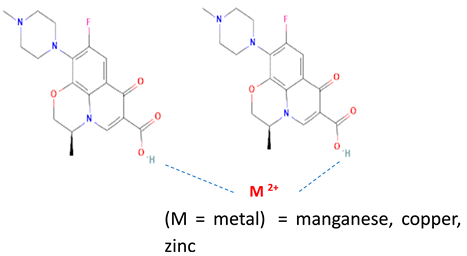
Besides other organic compounds, the ionic reaction was conducted by metal substitution of the antibiotic levofloxacin. It was reported that the complexation of levofloxacin with copper (II) resulted in more stable levofloxacin. The antimicrobial potency test results showed the same activity as free-form levofloxacin [101]. However, it is necessary to continue testing levofloxacin against resistant microbes. Research on the effect of metal complexation of levofloxacin was also carried out on several transition metal ions, namely manganese, cobalt, nickel, copper, and zinc. It was reported that levofloxacin forms complexes with metal ions, forming bidentate ligands. Moreover, it was found that the antibacterial activity of these complex compounds was as good as the free form or better. In addition, those levofloxacin complexes increased the immune system’s activity (immunomodulator) [102].
Another combination system is the three-salt multi-component solid, with various hydrate molecules inserted. Ciprofloxacin (CfH, C17H18FN3O3) crystallizes with 2-thiobarbituric (H2tba) and barbituric acid (H2ba) in the aqueous solution to yield the salt CfH2(Htba)·3H2O, the salt cocrystal CfH2(Hba)(H2ba)·3H2O, and the salt CfH2(Hba)·H2O. These three salts were reported to have a more stable structure than the original compound [51].
Among the solid engineering techniques, solvate and hydrate developments are not good options, because the transformation causes a variation in the physicochemical properties, which is not easy to handle [56,57,58,59]. To enhance physicochemical properties, such as solubility and stability, tailormade salts and cocrystals are preferred [51,54,55]. Moreover, some reports revealed they might enhance antibiotic potency [30,52,53]. Hence, in the next subsequent section, we will explain the primary solid-state engineering of NSAIDs within a multi-component arrangement, including fluoroquinolones.
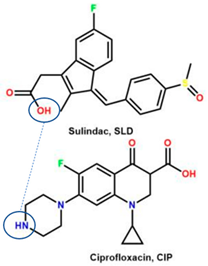
4.1. Fluoroquinolone-NSAID Multi-Components
Like fluoroquinolones, NSAIDs have low solubility but high permeability and are classified in the Class II Biopharmaceutics Classification System (BCS) [8,21,29,30,70,108]. The poor solubility of NSAIDs impacts their’ performance, formulation, and clinical use, and prolongs the onset time. NSAIDs have been reported to form salts and cocrystals, as well as other multi-component systems such as polymorphs, solvates, and hydrates [8,54]. Due to their frequent usage, based on the data, NSAIDs are the most developed drug in solid-state engineering, followed by antibiotics, which have been designed to improve their solubility and stability [109].
Hereafter, next, we focus on fluoroquinolone–NSAID combinations for some reasons. First, it has been known that NSAIDs are essential substituents for clinical purposes, including in treating infectious diseases. Infected patients commonly use antibiotics to kill bacteria, and NSAIDs are used to overcome pain due to inflammation symptoms. Vice versa, inflammation also may trigger microbial infections. These drugs are available over the counter; therefore, NSAID usage is commonly not well-monitored, even though many adverse effects have been reported. Combining antibiotics with NSAIDs in a multi-component system will be better for increasing patient compliance [26,30].
The second supporting reason is structural; fluoroquinolones are amphoteric or tend to form bases [6,7], and are found in the market in their HCl–salt form. Meanwhile, NSAIDs are acidic or amphoteric, including diclofenac acid, which is commonly used in its sodium salt form [8,70]. However, combining them in a multi-component solid system is very challenging in improving the physicochemical properties of both sides, such as increased solubility and stability and the possibility of activity or potency enhancement.
On the other hand, the salt reaction has limitations, because it cannot be applied to compounds that have difficulty forming ions. For example, an ibuprofen derivative, zaltoprofen, used to treat acute pains [110], is a non-ionic compound that cannot form salts. As an NSAID, this drug is poorly soluble and has been formulated as a sustained-release dosage form [111], mixed with a surfactant to increase the solubility [112]. However, this neutral compound can still be combined with nicotinamide via the non-ionic reaction to form a multi-component solid, which has been proven to improve its physicochemical properties [113]. Hence, there are still chances to react with weak base antibiotics.
As mentioned earlier, NSAIDs and antibiotics are frequently used and have been found to react non-covalently with other compounds, which can offer both advantages and challenges [8,109]. A review of multi-component systems involving NSAIDs has been previously reported. On this occasion, we do not present the list of these agents but will continue discussing the possibility of their toxicity if combined with fluoroquinolones.
Comparing drug–excipient combinations, not many multi-component dual drugs, including antibiotic–NSAID combinations, have been developed. This phenomenon is predicted, due to the complex factors affecting the feasibility of host–coformer interactions, safety, dose issue, and toxicity. Additionally, the data show that ciprofloxacin and levofloxacin are the most-developed fluoroquinolones, in the context of creating multi-component solids with NSAIDs. Ciprofloxacin is in the first rank, followed by levofloxacin because they are commonly used to treat broad infection cases and are easy to react with a counterion or coformer. Reports have widely explained that their main advantages comprise enhancing NSAID solubility and improving fluoroquinolone antibiotic stability [26,31].
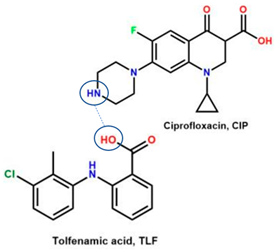
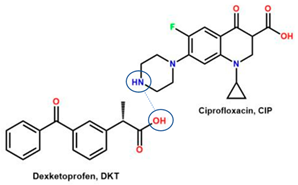
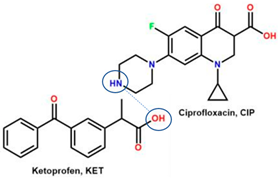
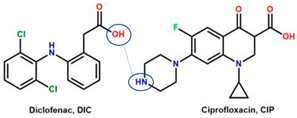
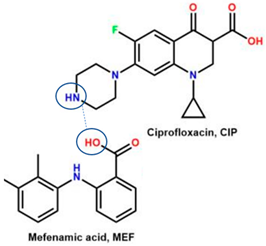
For example, the ciprofloxacin-salicylic acid reaction produced various molar ratios of crystal, solvate, and hydrate forms of muli-component systems [31]. A study described these solid systems with a focus on the polymorphism, formation pathways, and thermodynamic stability of various other multi-component forms, including anhydrous salts, two polymorphic forms of monohydrate salt, methanol, and acetonitrile solvates, and hydrate cocrystal salts. Some of those multi-component systems provide better solubility and stability [31]. An experiment discovered ciprofloxacin–salicylate 1.75 hydrates, which enhanced the solubility of the original compound [65]. Other combinations include ciprofloxacin with mefenamic acid, tolfenamic acid, ketoprofen, dex-ketoprofen, and diclofenac acid, all of which improve the solubility and stability of NSAIDs. However, the ciprofloxacin–diclofenac salt exhibits the most potent antimicrobial effect [30].
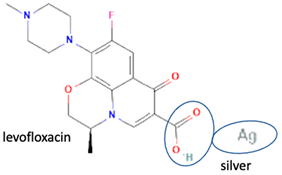
In addition, as shown in Table 2, levofloxacin has been combined with metacetamol [26], citric acid [6], dihydroxybenzoic acid [7], and some inorganic metals, i.e., copper [101], argentum, etc. [102]. Besides, the HCl–salt forms have been used in their most marketed dosage forms. Similar to ciprofloxacin–NSAIDs, levofloxacin–NSAID multi-component solids also increase the anti-inflammatory drug’s solubility and stabilize the fluoroquinolone’s structure by protecting the N-methyl piperazine site, which is responsible for the photodegradation occurrence [26]. Besides the low solubility, instability towards light also becomes the main problem of fluoroquinolones [2,4,5]. Photolysis produces toxic substances immediately after UV exposure, in both liquid [103,104] and solid forms [105,106,107].
Briefly, the multi-component system of fluoroquinolones and NSAIDs has the potential to improve stability and maintain antibiotic potency. In the future, improved potency may also be achieved. However, as a dual drug, multi-component solid, interactions between APIs, mainly NSAIDs, should be considered thoroughly [114,115,116]. Many resistance cases related to the inappropriate use of levofloxacin have occurred widely [117]. The dose calculation and toxicity of the fluoroquinolone–NSAID combination, which has a role in its clinical potential, are crucial to be investigated [118].
4.2. Toxicity Study of NSAIDs and Fluoroquinolones Multi-Component Systems
Referring to other cases, apigenin, a bioflavonoid compound with anti-inflammatory activity against chronic aging diseases, has been combined with 4,4′-bipyridine, enhancing its efficacy and lowering toxicity [119]. In addition, the niflumic acid–pyridine multi-component solid successfully decreased gastrointestinal toxicity by resulting in the No Observed Adverse Effect Level (NOAEL) parameter [120]. However, many reports revealed cases of toxicity resulting from antibiotic–NSAID combinations, which depend on the dosage. High doses may significantly affect targeted cells, especially regarding the use of antibiotics and NSAIDs that have the same activity site, i.e., the neural system [118,121].
After discussing the antibiotic-NSAID multi-component solid, the following sections will focus on toxicity and computational studies. These studies aim to provide insights into selecting the appropriate host–coformer/counterion, preparation methods, structural determination, physicochemical properties, activity, and safety measures. Every drug has certain side effects, including antibiotics and NSAIDs, which may affect the gastrointestinal tract, nervous systems, and elimination organs, such as the liver and kidneys. For example, fluoroquinolones kill microbes by the inhibition of bacterial topoisomerases II and IV, and resistance arises from these target enzymes’ mutations. In addition, they have rare adverse effects, namely tendinopathy and tendon rupture, peripheral neuropathy, and aortic aneurysm [40]. Fluoroquinolones are selective GABA-A receptor inhibitors, preventing GABA binding in the central nervous system. As known, GABA is a primary regulator of the vagus nerve, which controls gastrointestinal (GI) function [3]. Moreover, fluoroquinolones also cause some neuro-system disturbances, such as seizures [121], hallucinations [122], peripheral neuropathy [123], and others [3].
On the other side, fluoroquinolones show many adverse effects on the gastrointestinal tract and the central nervous system, namely, phototoxicity and dermal toxicity, including allergenicity. Levofloxacin has favorable adverse reaction profiles compared to other fluoroquinolones. Among the reported cases of dermal toxicity, there are few reports of toxic epidermal necrosis (TEN) and stomatitis associated with levofloxacin usage. Stomatitis is characterized by pain, inflammation, and ulceration in the oral cavity [124].
There are mild to moderate side effects of fluoroquinolones, as shown when treated with ciprofloxacin, levofloxacin, and sitafloxacin groups. However, reports also reveal the severe side effects of temafloxacin, trovafloxacin, grepafloxacin, and clinafloxacin. For example, temafloxacin causes immune hemolytic anemia, trovafloxacin causes hepatotoxicity, grepafloxacin causes cardiotoxicity, and clinafloxacin causes phototoxicity. Therefore, those compounds are no longer used clinically. Additionally, regulatory agencies such as the FDA have warned about the inappropriate use of fluoroquinolone antibiotics, due to their severe side effects, such as tendon rupture, neuropathy, or heart valve regurgitation. Although the molecular principles underlying these side effects are not yet fully understood, there is evidence that they inhibit human mitochondrial topoisomerase II [3].
Another problem in antibiotic usage is bacterial resistance, which is divided into three categories, namely, multi-drug-resistant (MDR), extensively drug-resistant (XDR), and pan-drug-resistant (PDR) microbes. These categories illustrate the level of global complexity in the issue of antibiotic resistance and the many factors needed to be considered in solving it. Gram-negative bacteria are primarily XDR, followed by PDR and MDR. Recently, a study found resistant Mycobacterium tuberculose, including pre-XDR tuberculosis (TB) and MDR TB, which resist fluoroquinolones and are classically considered risk factors for treatment failure [125]. In these studies, combinations of plant extracts or active compounds have been reported to decrease antibiotic resistance issues. New research has shown that the treatment of extensively drug-resistant tuberculosis (XDR-TB) has been updated to include pre-XDR-TB, which is characterized by multidrug resistance (MDR-TB) with additional resistance to fluoroquinolone antibiotics. This was associated with more capillary lung lesions and bilateral disease, which required more prolonged treatment [125]. Also, more than half of S. aureus strains tested were MDR, showing resistance to fluoroquinolones [126,127,128]. Efforts have been made to improve the fluoroquinolones’ potency, for example, by conjugate biofilm formation, a major virulence factor of Pseudomonas auroginosa that causes antibiotic resistance [129].
On the other hand, side effects and toxicity of NSAIDs have also been reported. Most commonly, severe GI adverse effects increase with NSAID medication, such as ulceration, bleeding, or perforation [130]. The occurrences are more frequent in the elderly. These drugs also exhibit other undesirable effects, including nausea, dyspepsia, loss of appetite, abdominal pain, and diarrhea [131]. Furthermore, COX-1 inhibition reduces cytoprotective effects and causes these disturbances. In addition, NSAID usage may result in severe cardiovascular adverse events, i.e., myocardial infarction and stroke, particularly with the selective COX-2 inhibitor rofecoxib, which was withdrawn from circulation in 2004. These drugs have been found to elevate blood pressure and heart failure by inhibiting natural prostanoid-induced salt excretion and causing changes in renal arteriolar tone. Additionally, renal toxicity, including renal papillary necrosis and interstitial nephritis, also may be exhibited [132].
Aside from the singular NSAIDs, there are concurrent adverse effects related to other drug usage forms. Regarding their pharmacokinetics, NSAIDs may interact with other plasma protein-bound drugs and increase the free serum concentration of these medicines. In addition, NSAIDs decrease renal perfusion and inhibit the glucuronidation process. Therefore, their usage may increase the toxicity of drugs, in terms of renal clearance (such as lithium) or hepatic metabolism [116]. Furthermore, the concurrent use of NSAIDs and antihypertensives, anticoagulants, antiplatelets, selective serotonin receptor inhibitors (SSRIs), and substances that injure the GI mucosa also causes bleeding and severe ulcers due to decreased platelet aggregation. In addition, NSAIDs also interact with alcohol or glucocorticoids, which inhibits the activation of the arachidonic acid precursor phospholipase A2 and increases the risks of adverse effects [115].
The combination of fluoroquinolone with NSAIDs has been reported to increase the risk of seizure disorders, particularly in the central nervous system [32]. However, the mechanisms of toxicity in multi-component systems are still unclear and require further investigation. Due to differences in bonding and interaction, the proposed multi-component system has a unique working mechanism that can potentially impact toxicity. However, there are cases of decreases in toxicity after multi-component system formation. For example, a recent study reported that fluorouracil–phenylalanine cocrystal has different cytotoxicity from their single forms and physical mixture. The cytotoxicity mechanism was investigated in a cell metabolomics study, although it is still unclear [133]. The phytotoxicity of antibiotics and non-steroidal anti-inflammatory drugs to green algae Chlorella sp. and Desmodesmus spinosus also was reported [134]. Another study reported that oxaliplatin, an anticancer-multi-component system with the flavonoids baicalein and naringenin, could reduce toxicity [119]. The nano-cocrystal (NCC) technology of lamivudine and zidovudine was reported to have higher cytotoxicity. It was incorporated with a gel base delivery system, in NCC form [135].
Interestingly, a study reported that NSAIDs might increase the antibiotic’s strength, as shown by azithromycin–paracetamol co-crystal [136]. Next, the antibacterial and antibiofilm activities of four non-steroidal anti-inflammatory drugs (NSAIDs), piroxicam (PXC), diclofenac sodium (DCF), acetylsalicylic acid (ASA), and naproxen sodium (NPX), were evaluated against Escherichia coli and Staphylococcus aureus. Additionally, NSAIDs were combined with kanamycin (KAN) and tetracycline (TET). ASA, DCF, and PXC reduced metabolic activity and culturability. Meanwhile, PXC reduced biofilm mass. Additive interactions were obtained for most of the combinations between NSAIDs and KAN or TET. Hence, A benefit of NSAIDs is the control of biofilms, as they are more effective than conventional antibiotics [137]. In addition, recently, NSAIDs–ciprofloxacin salts, supported by computational and experimental studies, showed that NSAIDs not only maintain ciprofloxacin’s antibiotic activity but improve it by increasing the solubility, which then enhances their diffusion in the culture. This study shows that the reaction with diclofenac lowers ciprofloxacin’s required dose [30], as demonstrated by ciprofloxacin–furosemide combinations [138].
The exploration and investigation of toxicity and activity improvement by combining antibiotics and NSAIDs in a multi-component system is still a challenging task. However, the interactions between the two must be given attention, as they have shown similar adverse effects on the gastrointestinal tract based on available data. Therefore, for the next experiment, observing the possible pharmacokinetics and pharmacodynamic interactions and their impact on the neural, bloodstream, hepatic, and renal systems will be valuable for ensuring the safety and suitability of their multi-component solids. Furthermore, improvements in antibiotic activity and potency can be expected to be related to solubility and penetrability increases.
As well as other synthetic drugs’ development, the relationship between structure and activity has been modeled in many ways, including by studying the activity and toxicity of antibiotic–NSAID multi-component solid systems, which should be confirmed by in vitro and in vivo testing.
5. Computational Approach and Modeling for Multi-Component Solid Development
Computational simulations have become a popular and valuable technique for designing stable chain conformations and packing structures, predicting molecular interaction, etc. The computational approach in developing multi-component systems involves principles and specific calculations of the binding energy between multiple substituents. Molecular dynamics, mechanism, and quantum mechanics are some principles of multi-component solids’ design [29,33,39].
In line with experimental research, multi-component crystal building needs a suitable coformer, solvent, and preparation methods. Using a database, i.e., CSD (Cambridge’s Structural Database)–CCDC (Cambridge’s Crystallographic Data Centre), and mathematical calculation, the thermodynamic pattern of the multi-component system’s interaction can be predicted [139]. Based on these data, a coformer or counterion is selected. Next, computational modeling is used to determine feasible targets for multi-component crystals, predict the physicochemical properties of these systems, and optimize the preparation process.
We have selected several multi-component systems as examples that have been modeled computationally and can be used as a basis for the development of antibiotics-NSAIDs multi-component systems. It is important to note that using in silico modeling is a more environmentally friendly and efficient approach compared to traditional trial-and-error experiments. Firstly, some programs have been used for solvent and coformer screening, such as Mercury, Hyperchem, COSMO-RS, COSMOtherm software, etc. [140].
For example, in the HME process for ciprofloxacin–isonicotinic acid multi-component development, a design of experiment (DoE) was used to evaluate the factors that determined the yield, and researchers found three factors: the effect of temperature, the screw speed, and screw configuration [99]. Furthermore, by analyzing the simulated structure, the activity change and toxicity can also be investigated simultaneously.
A feasibility study was conducted using thermodynamic modeling, regarding the non-covalent reaction process, using perturbed-chain statistical associating fluid theory (PC-SAFT). This method can predict pharmaceutical cocrystal behavior by calculating the single-crystal solubility of any solvent at any temperature. Based on that calculation, the cocrystal’s solubility in other solvents and different temperatures also can be predicted without additional measurements. Using this mathematical approach, the properties of (+)-mandelic acid/(-)-mandelic acid (1:1), caffeine/glutaric acid (1:1), and carbamazepine/nicotinamide (1:1) cocrystal systems were in excellent agreement with the experimental data [140].
Developed in the early 1990s, the liquid phase thermodynamics theory of conductor-like screening model for real solvents (COSMO-RS) has been used in solubility prediction, solvent screening, excipient ranking, pKa prediction, redox potentials calculation, and partitioning coefficients’ determination [141]. In detail, the coformer screening is also based on some parameters: hydrogen bonding propensity, syntonic engineering, and supramolecular compatibility, which are supported by the Cambridge Structure Database (CSD), pKa-based models, Fabian’s method, lattice energy calculation, COSMO-RS, Hansen’s solubility parameter, virtual cocrystal screening (based upon molecular electrostatic potential surfaces (MEPS)), thermal analysis, measuring saturation temperature, Koffler contact method data, and so on [142].
Afterward, COSMO-RS was coupled with the COSMOtherm software to screen common solvents and co-formers for CL-20. The excess enthalpy and solvent cavity volume determined the solvate system’s arrangement. However, the COSMO method was challenging in predicting cocrystal formation, and it still needs entropy and solid-state interactions as the essential data. Meanwhile, solvent selection should maximize entropy. Calculating entropy is a critical factor in predicting cocrystal formation, and an accurate method is essential for screening cocrystal formation. This enables the design of an intelligent approach to multi-component crystal development [143].
Additionally, the supercooling liquid phase can be determined by in silico calculation [30]. A recent integrative study combined ciprofloxacin multi-component solids with a series of NSAIDs, including mefenamic acid, tolfenamic acid, dex-ketoprofen, ketoprofen, diclofenac, and sulindac, which successfully improved the NSAIDs’ solubility, without altering the antibiotic activity of ciprofloxacin. However, ciprofloxacin–DIC enhanced the antimicrobial activity. In the research on ciprofloxacin-NSAIDs multi-component solids, a virtual screening using COSMOQuick was conducted, which relied on thermodynamic calculations to select suitable NSAIDs to be combined with the antibiotic. This was achieved by determining the excess enthalpy of mixing or formation (Hex) of the components in comparison to the single drug in a supercooled liquid phase. A negative Hex value indicated the potential to form multi-component solids [30]. This computational program has also been used to search for new molecular complexes of furosemide–NSAIDs [138].
Next, an antibiotic, linezolid (LIN), was reported to produce many crystals named LIN_II, LIN_III, LIN:BA cocrystal, LIN:PHBA cocrystal hydrate, and LIN:2,6-DHBA cocrystal. Those crystal systems were obtained from some methods, including neat grinding, liquid-assisted grinding, and solvent evaporation, which fits with the in silico study. The virtual cocrystal-screening tools optimized the molecular complementarity, hydrogen bond propensity, and molecular electrostatic potential maps. However, the molecular electrostatic potential maps approach is closer to the experimental results than molecular complementarity and hydrogen bond propensity calculations. This work shows that the contribution of the total energy of the coformer crystal systems determines the cocrystal formation feasibility. Mercury 4.3.1 software provides data to analyze molecular complementarity [141].
Another modeling application in multi-component research is the study of spatial charge descriptors, which can predict cocrystal formation using machine learning algorithms [144]. Two models were developed to predict the density of energetic and general organic cocrystals containing nitro groups, based on the artificial neural network (model I) and surface electrostatic potential correction method (model II), used to predict cocrystal density. This study yielded reliable data, but the first model’s performance is better than model II’s [145].
Modeling software for designing multi-component systems is continuing to grow in number. Recently, Mswahili et al. developed a model to predict cocrystal formation by extracting the descriptor values from the simplified molecular-input line-entry system (SMILES) of compounds. They demonstrated that the calculated values of half of the selected descriptors using feature selection algorithms showed comparable results with experimental data from 1476 instances [35]. Furthermore, a prediction machine has been developed to focus on the L-menthol/thymol eutectic system, combining the data of differential scanning calorimetry (DSC) and powder X-ray diffraction (XRD). However, it was found that not all deep eutectic systems were simple eutectic types. Therefore, integrative experimental methods and thermodynamic modeling are required to determine the simple eutectic mixture [36].
Furthermore, new software prototypes have been developed to arrange multi-component systems by considering both thermodynamic and spatial aspects to fit the host compounds with their counterions/coformers. For example, a multi-component crystal may involve non-covalent bonds with low energy only, including hydrogen, van der Waals, and dipole–dipole bonds, until an ionic reaction, which forms relatively higher-energy salts Still, the space conformation and the environment also should be considered [30,99,143].
Modeling studies have played a significant role in the development of antibiotic multi-component crystals [30,37,99]. Adding to the mentioned studies, the stability modeling of sulfadimidine–4-aminosalicylic acid (4-ASA) cocrystals in two polymorphic forms and crystal habits has also been reported [37]. Next, in an antibiotic study, the use of an in silico method was applied to a multi-component system, 1-{(aryl) [(5-methyl-1,3-thiazol-2-aryl) amino] methyl naphthalene-2-ol, in order to promote some improvement in solubility and stability [38].
Another multi-component computational study was performed, combining antibiotic fluoroquinolone with metal by a dynamic and porin-mimetic approach. The metal–antibiotic system was predicted to improve solubility, which was then confirmed by the wet experiment [29]. Furthermore, fluoroquinolone complexes with Ag/AgCl/Bi2O3/BiFeO3, supported by modeling, showed photocatalytic degradation [102]. In silico approaches have been used to predict the formation of neutral multi-component crystals, such as the combination of quinolone antibiotics and a protein transporter (MexB) [146]. Similar approaches have been applied to other drug multi-component systems, including the prediction of cytotoxicity in fluorouracil–phenylalanine [133] and lamivudine–zidovudine [135] cocrystals. Another modeling study also discovered a new method for producing 5-amino-6-cyano-3-hydroxybenzoic coumarin, which shows antimicrobial activity, using Ni–Cu–Al–CO3 catalyst [147].
Finally, in the present, graphing a molecular structure three-dimensionally is usually assisted by SHELXT, and is refined using SHELXL software, combined with Mercury’s data and modeling [148,149]. All computational modeling approaches can be utilized to screen the coformers or counterions [150], design the preparation method [151], predict the physicochemical properties [152], and observe activity changes, even in the established structure [153]. Computational studies are essential to efficiently, rationally, and integrative develop suitable multi-component systems. In conclusion, in silico studies may produce a more accurate, greener, and comprehensive analysis, as shown by fluoroquinolones’ multi-component systems, regarding their reactions with NSAIDs [26,30,153], metals [29], and furosemide [138]. This modeling approach simplifies the conventional experimental process of selecting the coformer and method, determining the structure, and testing properties, resulting in a more efficient approach [154,155]. Moreover, it also can predict changes in potency, as widely reported in the current decades.
6. Conclusions
Besides resistance cases, antibiotics’ main problem is their lack of physicochemical properties, such as low solubility and stability. Therefore, one of the fruitful approaches in antibiotic development is solid-state engineering, i.e., the formation of multi-component systems composed to improve the stability and solubility of antibiotics. This strategy is growing in popularity and is supported by solid instrument development, straightforward preparation methods, and computational modeling, making it more efficient and environmentally friendlier.
The most developed antibiotics in the multi-component solids are the antituberculosis group (isoniazid and pyrazinamide) and fluoroquinolones (levofloxacin and ciprofloxacin). Multi-component solid systems have several synthons that interact structurally to improve solubility and stability. However, based on the reports, many antituberculosis multi-component systems only result in new crystal structures without affecting stability and solubility. Meanwhile, fluoroquinolones react with their counterion or coformer at their amine piperazine moiety, which protects them from oxidative degradation. Moreover, fluoroquinolones’ multi-component solid systems may also increase their potency by re-arranging the polarity, supporting its capability to pass through the cell membrane of bacteria after the solid rearrangement.
In conclusion, the development of the fluoroquinolone-NSAID multi-component solid system holds great promise and presents a challenging opportunity. This combination has the potential to leverage the advantages of both components and may lead to increased patient compliance. In general, multi-component solids overcome the low solubility and stability issues of NSAIDs. Moreover, some experiments focusing on improving the stability and polarity of these components may push antibiotic potency polarity. However, we also must pay attention to their safety factors by studying the toxicity, which may be assessed simultaneously by computational and laboratory studies.
Author Contributions
Conceptualization, I.N.; method, I.N., M.S.W. and D.H.; resources: I.N. and D.H.; funding acquisition: I.N.; validation, I.N., M.S.W. and D.H.; writing-original draft and editing, I.N. and D.H; visualization: I.N.; supervising, I.N. and M.S.W.; collecting data, I.N. and D.H. All authors have read and agreed to the published version of the manuscript.
Funding
This article publication is funded by the National Research and Innovation Agency—the Directorate-General of Higher Education, Indonesia, with contract number: 083/E5/PG.02.00.PT/2022.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Piper, B.J.; Alinea, A.A.; Wroblewski, J.R.; Graham, S.M.; Chung, D.Y.; McCutcheon, L.R.; Birkett, M.A.; Kheloussi, S.S.; Shah, V.M.; Szarek, J.L.; et al. A Quantitative and Narrative Evaluation of Goodman and Gilman’s Pharmacological Basis of Therapeutics. Pharmacy 2019, 8, 1. [Google Scholar] [CrossRef]
- de Bairros, A.V.; Pereira, D.B.; Everson, W.F.C.; Paim, C.S.; da Silva, F.E.B.S.; Malesuik, M.D.; Paula, F.R. Evaluation of the influence of fluoroquinolone chemical structure on stability: Forced degradation and in silico studies. Braz. J. Pharm. Sci. 2018, 54, e00188. [Google Scholar] [CrossRef]
- Freeman, M.Z.; Cannizzaro, D.N.; Naughton, L.F.; Bove, C. Fluoroquinolones-Associated Disability: It Is Not All in Your Head. Neuro. Sci. 2021, 2, 235–253. [Google Scholar] [CrossRef]
- Ainurofiq, A.; Syahrul, A.; Widayati, A.; Fitriastuti, R.; Herawati, Z. Fluoroquinolone Antibacterial Drugs: Review of Physicochemical Problems; Analysis Techniques; and Solutions. Asia-Pac. J. Sci. Technol. 2022, 27, 10. [Google Scholar]
- Czyrski, A.; Anusiak, K.; Teżyk, A. The degradation of levofloxacin in infusions exposed to daylight with an identification of a degradation product with HPLC-MS. Sci. Rep. 2019, 9, 3621. [Google Scholar] [CrossRef]
- Nugrahani, I.; Laksana, A.N.; Uekusa, H.; Oyama, H. New Organic Salt from Levofloxacin–Citric Acid: What Is the Impact on the Stability and Antibiotic Potency? Molecules 2022, 27, 2166. [Google Scholar] [CrossRef]
- Nugrahani, I.; Sulaiman, M.R.; Eda, C.; Uekusa, H.; Ibrahim, S. Stability and antibiotic potency improvement of levofloxacin by producing new salts with 2,6- and 3,5-dihydroxybenzoic acid and their comprehensive structural study. Pharmaceutics 2023, 15, 124. [Google Scholar] [CrossRef]
- Nugrahani, I.; Parwati, R.D. Challenges and Progress in Nonsteroidal Anti-Inflammatory Drugs Co-crystal Development. Molecules 2021, 26, 4185. [Google Scholar] [CrossRef]
- O’Malley, C.; McArdle, P.; Erxleben, A. Formation of Salts and Molecular Ionic Cocrystals of Fluoroquinolones and α,ω-Dicarboxylic Acids. Cryst. Growth Des. 2022, 22, 3060–3071. [Google Scholar] [CrossRef]
- Bhavani, A.V.S.; Usha, A.L.; Ashritha, K.; Rani, E.R. Review on Pharmaceutical Co-crystal and Design Strategies. Asian J. Pharm. Technol. 2021, 11, 175–180. [Google Scholar] [CrossRef]
- Karimi-Jafari, M.; Padrela, L.; Walker, G.M.; Croker, D.M. Creating cocrystals: A review of pharmaceutical cocrystal preparation routes and applications. Cryst. Growth Des. 2018, 18, 6370–6387. [Google Scholar] [CrossRef]
- Panzade, P.S.; Shendarkar, G.R.; Kulkarni, D.A. Hot Melt Extrusion: An Emerging Green Technique for the Synthesis of High-Quality Pharmaceutical Cocrystals. J. Pharm. Innov. 2022, 17, 283–293. [Google Scholar] [CrossRef]
- MacEachern, L.; Kermanshahi-pour, A.; Mirmehrabi, M. Supercritical Carbon Dioxide for Pharmaceutical Co-Crystal Production. Cryst. Growth Des. 2020, 20, 6226–6244. [Google Scholar] [CrossRef]
- Apshingekar, P.P.; Aher, S.; Kelly, A.L.; Brown, E.C.; Paradkar, A. Synthesis of Caffeine/Maleic Acid Co-crystal by Ultrasound-assisted Slurry Co-crystallization. J. Pharm. Sci. 2017, 106, 66–70. [Google Scholar] [CrossRef]
- Carstens, T.; Haynes, D.A.; Smith, V.J. Cocrystals: Solution, Mechanochemistry, and Sublimation. Cryst. Growth Des. 2020, 20, 1139–1149. [Google Scholar] [CrossRef]
- Nugrahani, I.; Utami, D.; Ayuningtyas, L.; Garmana, A.N.; Oktaviary, R. New Preparation Method Using Microwave, Kinetics, In Vitro Dissolution-Diffusion, and Anti-Inflammatory Study of Diclofenac- Proline Co–Crystal. Chem. Select 2019, 4, 13396–13403. [Google Scholar] [CrossRef]
- Pagire, S.; Korde, R.A.; Deshmukh, S.; Dash, R.C.; Dhumal, A.; Paradkar, A. Microwave assisted synthesis of caffeine/maleic acid co-crystals: The role of the dielectric and physicochemical properties of the solvent. Cryst. Eng. Comm. 2013, 15, 3705–3710. [Google Scholar] [CrossRef]
- Nugrahani, I.; Kumalasari, R.A.; Auli, W.N.; Horikawa, A.; Uekusa, H. Salt cocrystal of diclofenac sodium-L-proline: Structural, pseudopolymorphism, and pharmaceutics performance study. Pharmaceutics 2020, 12, 690. [Google Scholar] [CrossRef]
- Gorman, E.M.; Samas, B.; Munson, E.J. Understanding the Dehydration of Levofloxacin Hemihydrate. J. Pharm. Sci. 2012, 101, 3319–3330. [Google Scholar] [CrossRef]
- Raudino, A.; Sarpietro, M.G.; Pannuzzo, M. Differential scanning calorimetry (DSC): Theoretical fundamentals. In Drug-Biomembrane Interaction Studies; Pignatello, R., Ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 127–168. [Google Scholar]
- Manin, A.N.; Surov, A.O.; Churakov, A.V.; Perlovich, G.L. Crystal structures, thermal analysis, and dissolution behavior of new solid forms of the antiviral drug arbidol with dicarboxylic acids. Crystals 2015, 5, 650–669. [Google Scholar] [CrossRef]
- Feist, M. Thermal analysis: Basics, applications, and benefit. Chem. Texts 2015, 1, 8. [Google Scholar] [CrossRef]
- Monajjemzadeh, F.; Ghaderi, F. Thermal analysis methods in pharmaceutical quality control. J. Mol. Pharm. Org. Process Res. 2015, 3, e121. [Google Scholar]
- Kendall, T.; Stratford, S.; Patterson, A.R.; Lunt, R.A.; Cruickshank, D.; Bonnaud, T.; Scott, C.D. Chapter Five—An industrial perspective on cocrystal: Screening, identification and development of the less utilised solid form in drug discovery and development. Prog. Med. Chem. 2021, 60, 345–442. [Google Scholar]
- Banerjee, M.; Nimkar, K.; Naik, S.; Patravale, V. Unlocking the potential of drug–drug cocrystal—A comprehensive review. J. Control. Release 2022, 348, 456–469. [Google Scholar] [CrossRef]
- Shinozaki, T.; Ono, M.; Higashi, K.; Moribe, K. A Novel Drug-Drug Cocrystal of Levofloxacin and Metacetamol: Reduced Hygroscopicity and Improved Photostability of Levofloxacin. J. Pharm. Sci. 2019, 108, 2383–2390. [Google Scholar] [CrossRef]
- Boraste, D.R.; Chakraborty, G.; Ray, A.K.; Shankarling, G.S.; Pal, H. Supramolecular Host-Guest Interaction of Antibiotic Drug Ciprofloxacin with Cucurbit[7]Uril Macrocycle: Modulations in Photophysical Properties and Enhanced Photostability. J. Photochem. Photobiol. A Chem. 2018, 358, 26–37. [Google Scholar] [CrossRef]
- Hibbard, T.; Nyambura, B.; Scholes, P.; Totolici, M.; Shankland, K.; Al-Obaidi, H. Preparation and physicochemical analysis of novel ciprofloxacin/ dicarboxylic acid salts. J. Pharm. Sci. 2022, 112, 195–203. [Google Scholar] [CrossRef]
- Sousa, C.F.; Coimbra, J.T.; Richter, R.; Morais-Cabral, J.H.; Ramos, M.J.; Lehr, C.M.; Gameiro, P. Exploring the permeation of fluoroquinolone metalloantibiotics across outer membrane porins by combining molecular dynamics simulations and a porin-mimetic in vitro model. Biochim. Biophys. Acta Biomembr. 2022, 1864, 183838. [Google Scholar] [CrossRef]
- Acebedo-martínez, F.J.; Domínguez-martín, A.; Alarcón-payer, C.; Sevillano-páez, A.; Verdugo-escamilla, C.; González-pérez, J.M.; Martínez-Checa, F.; Choquesillo-Lazarte, D. Enhanced NSAIDs Solubility in Drug—Drug Formulations with Ciprofloxacin. Int. J. Mol. Sci. 2023, 24, 3305. [Google Scholar] [CrossRef]
- Surov, A.O.; Vasilev, N.A.; Churakov, A.V.; Stroh, J.; Emmerling, F.; Perlovich, G.L. Solid Forms of Ciprofloxacin Salicylate: Polymorphism, Formation Pathways, and Thermodynamic Stability. Cryst. Growth Des. 2019, 19, 2979–2990. [Google Scholar] [CrossRef]
- Skretkowicz, J.; Gondko, A. Interakcje fluorochinolonów z niesteroidowymi lekami przeciwzapalnymi. Fluoroquinolones interactions with nonsteroidal anti-inflammatory drugs. Pol. Merkur. Lekarski. 2004, 16, 194–195. [Google Scholar]
- Wu, J.; Gygi, F. A simplified implementation of van der Waals density functionals for first-principles molecular dynamics applications. J. Chem. Phys. 2012, 136, 224107. [Google Scholar] [CrossRef]
- Nagarajan, N.; Yapp, E.K.; Le, N.Q.K.; Kamaraj, B.; Al-Subaie, A.M.; Yeh, H.Y. Application of Computational Biology and Artificial Intelligence Technologies in Cancer Precision Drug Discovery. BioMed Res. Int. 2019, 2019, 8427042. [Google Scholar] [CrossRef]
- Mswahili, M.E.; Lee, M.-J.; Martin, G.L.; Kim, J.; Kim, P.; Choi, G.J.; Jeong, Y.-S. Cocrystal Prediction Using Machine Learning Models and Descriptors. Appl. Sci. 2021, 11, 1323. [Google Scholar] [CrossRef]
- Alhadid, A.; Jandl, C.; Mokrushina, L.; Minceva, M. Experimental investigation and modeling of cocrystal formation in l-menthol/thymol eutectic system. Cryst. Growth Des. 2021, 21, 6083–6091. [Google Scholar] [CrossRef]
- Connell, P.O.; Serrano, D.R.; McSweeney, N.; Healy, A.M. Modelling chemical and physical stability of cocrystals, case study: Sulfadimidine: 4-amino salicylic acid cocrystal. In Proceedings of the 8th International Conference and Exhibition on Pharmaceutics & Novel Drug Delivery Systems, Madrid, Spain, 7–9 March 2016. [Google Scholar]
- Lotlikar, O.A.; Dandekar, S.N.; Ramana, M.M.V.; Rathod, S.V. One-Pot Multicomponent Synthesis, Molecular Docking, and In Vitro Antibacterial Activities of 1-{(Aryl)[(5-methyl-1,3-thiazol-2-yl)amino]methyl}naphthalen-2-ol. Russ. J. Org. Chem. 2021, 57, 2024–2030. [Google Scholar] [CrossRef]
- Devogelaer, J.J.; Meekes, H.; Tinnemans, P.; Vlieg, E.; De Gelder, R. Co-crystal Prediction by Artificial Neural Networks. Angew. Chem. 2020, 59, 21711–21718. [Google Scholar] [CrossRef]
- Baggio, D.; Ananda-Rajah, M.R. Fluoroquinolone antibiotics and adverse events. Aust. Prescr. 2021, 44, 161–164. [Google Scholar] [CrossRef]
- Gooi, R.B.; Thatte, S.M. Inhibition of cell wall synthesis: Is this the mechanism of action of penicillins? Med. Hypotheses 1995, 44, 127–131. [Google Scholar] [CrossRef]
- Delcour, A.H. Outer membrane permeability and antibiotic resistance. Biochim. Biophys. Acta 2009, 1794, 808–816. [Google Scholar] [CrossRef]
- Champney, W.S. Antibiotics targeting bacterial ribosomal subunit biogenesis. J. Antimicrob. Chemother. 2020, 75, 787–806. [Google Scholar] [CrossRef]
- Dunckle, J.A.; Vinal, K.; Desai, P.M.; Zelinskaya, N.; Savic, M.; West, D.M.; Comm, G.L.; Dunham, C.M. Molecular recognition and modification of the 30S ribosome by the aminoglycoside-resistance methyltransferase NpmA. Proc. Natl. Acad. Sci. USA 2014, 111, 6275–6280. [Google Scholar] [CrossRef]
- Guillard, C.E. Antimicrobials that affect the synthesis and conformation of nucleic acids. Rev. Sci. Tech. 2012, 31, 77–87. [Google Scholar]
- Bhattacharjee, M.K. Antimetabolites: Antibiotics that inhibit nucleotide synthesis. In Chemistry of Antibiotics and Related Drugs; Springer: Berlin/Heidelberg, Germany, 2016; pp. 95–108. [Google Scholar]
- Basarab, G.S.; Kern, G.H.; McNulty, J.; Mueller, J.P.; Lawrence, K.; Vishwanathan, K.; Alm, R.A.; Barvian, K.; Doig, P.; Galullo, V.; et al. Responding to the challenge of untreatable gonorrhea: ETX0914, a first-in-class agent with a distinct mechanism of action against bacterial Type II topoisomerases. Sci. Rep. 2015, 5, 11827. [Google Scholar] [CrossRef]
- Levison, M.E.; Levison, J.H. Pharmacokinetics and Pharmacodynamics of Antibacterial Agents. Infect. Dis. Clin. N. Am. 2009, 23, 791. [Google Scholar] [CrossRef]
- Michael, J.R. The Pharmacokinetic and Pharmacodynamic Properties of Vancomycin. Clin. Infect. Dis. 2006, 42, S35–S39. [Google Scholar]
- Cruz-Cabeza, A.J. Acid-base crystalline complexes and the pKa rule. Cryst. Eng. Comm. 2012, 14, 6362–6365. [Google Scholar] [CrossRef]
- Golovnev, N.N.; Molokeev, M.S.; Lesnikov, M.K.; Atuchin, V.V. Two salts and the salt cocrystal of ciprofloxacin with thiobarbituric and barbituric acids: The structure and properties. J. Phys. Org. Chem. 2018, 31, e3773. [Google Scholar] [CrossRef]
- Sultana, N.; Arayne, M.S.; Rizvi, S.B.S.; Haroon, U.; Mesaik, M.A. Synthesis, spectroscopic, and biological evaluation of some levofloxacin metal complexes. Med. Chem. Res. 2013, 22, 1371–1377. [Google Scholar] [CrossRef]
- Islam, N.U.; Umar, M.N.; Khan, E.; Al-Joufi, F.A.; Abed, S.N.; Said, M.; Khan, F.A. Levofloxacin Cocrystal/Salt with Phthalimide and Caffeic Acid as Promising Solid-State Approach to Improve Antimicrobial Efficiency. Antibiotics 2022, 11, 797. [Google Scholar] [CrossRef]
- Wu, D.; Li, J.; Xiao, Y.; Ji, X.; Li, C.; Zhang, B.; Hou, B.; Zhou, L.; Xie, C.; Gong, J.; et al. New salts and cocrystals of pymetrozine with improvements on solubility and humidity stability: Experimental and theoretical study. Cryst. Growth Des. 2021, 21, 2371–2388. [Google Scholar] [CrossRef]
- Mannava, M.K.C.; Gunnam, A.; Lodagekar, A.; Shastri, N.R.; Nangia, A.K.; Solomon, K.A. Enhanced solubility, permeability, and tabletability of nicorandil by salt and cocrystal formation. Cryst. Eng. Comm. 2020, 23, 227–237. [Google Scholar] [CrossRef]
- Wei, N.; Jia, L.; Shang, Z.; Gong, J. Polymorphism of levofloxacin: Structure, properties and phase transformation. Cryst. Eng. Comm. 2019, 21, 6196–6207. [Google Scholar] [CrossRef]
- Williams, M.; Sittenauer, J.; Clark, S.; Farthing, J.; Baltezor, M.; McClorey, M. Ciprofloxacin Polymorph and Its Use. U.S. Patent 2019067851A1, 28 September 2018. [Google Scholar]
- Kitaoka, H.; Wada, C.; Moroi, R.; Hakusui, H. Effect of dehydration on the formation of levofloxacin pseudopolymorphs. Chem. Pharm. Bull. 1995, 43, 649–653. [Google Scholar] [CrossRef]
- Thakur, T.S.; Thakuria, R. Crystalline Multicomponent Solids: An Alternative for Addressing the Hygroscopicity Issue in Pharmaceutical Materials. Cryst. Growth Des. 2020, 20, 6245–6265. [Google Scholar] [CrossRef]
- Roy, P.; Pandey, N.; Kumari, N.; Baidya, R.; Mary, Y.S.; Ghosh, A. Development of sulfamethoxazole-succinimide cocrystal by mechanochemical cocrystallization—An insight into spectroscopic, electronic, chemical conformation and physicochemical properties. Chem. Eng. Res. Des. 2022, 185, 446–457. [Google Scholar] [CrossRef]
- de Almeida, A.C.; Torquetti, C.; Ferreira, P.O.; Fernandes, R.P.; dos Santos, E.C.; Kogawa, A.C.; Caires, F.J. Cocrystals of Ciprofloxacin with Nicotinic and Isonicotinic Acids: Mechanochemical Synthesis, Characterization, Thermal and Solubility Study. Thermochim. Acta 2020, 685, 178346. [Google Scholar] [CrossRef]
- Nugrahani, I.; Asyarie, S.; Soewandhi, S.N.; Ibrahim, S. The cold contact methods as a simple drug interaction detection system. Res. Lett. Phys. Chem. 2008, 2008, 169247. [Google Scholar] [CrossRef]
- Cherukuvada, S.; Row, G.T.N. Comprehending the Formation of Eutectics and Cocrystals in Terms of Design and Their Structural Interrelationships. Cryst. Growth Des. 2014, 14, 4187–4198. [Google Scholar] [CrossRef]
- Elbagerma, M.A.; Edwards, H.G.M.; Munshi, T.; Hargreaves, M.D. Characterization of new cocrystals by Raman spectroscopy, powder X-ray diffraction, differential scanning calorimetry, and transmission Raman spectroscopy. Cryst. Growth Des. 2020, 10, 2360–2371. [Google Scholar] [CrossRef]
- Nugrahani, I.; Tjengal, B.; Gusdinar, T.; Horikawa, A.; Uekusa, H. A Comprehensive Study of a New 1.75 Hydrate of Ciprofloxacin Salicylate: SCXRD Structure Determination, Solid Characterization, Water Stability, Solubility, and Dissolution Study. Crystals 2020, 10, 349. [Google Scholar] [CrossRef]
- Budziak-Wieczorek, I.; Maciolek, U. Synthesis and characterization of a (−)-epicathechin and barbituric acid cocrystal: Single-crystal-X-ray diffraction and vibrational spectroscopic studies. ACS Omega 2021, 6, 8199–8209. [Google Scholar] [CrossRef]
- Samsoedin, H.; Bapoo, M.; Doms, T.I. FTIR, dissolution and antiviral activiry of nevirapine co-crystals. Pharm. Anal. Acta 2017, 8, 561. [Google Scholar]
- Wang, Q.; Xue, J.; Hong, Z.; Du, Y. Pharmaceutical Cocrystal Formation of Pyrazinamide with 3-Hydroxybenzoic Acid: A Terahertz and Raman Vibrational Spectroscopies Study. Molecules 2019, 24, 488. [Google Scholar] [CrossRef]
- Bunaciu, A.A.; Udriştioiu, E.; Aboul-enein, H.Y. X-ray Diffraction: Instrumentation and Applications X-Ray Diffraction: Instrumentation and Applications. Crit. Rev. Anal. Chem. 2015, 45, 289–299. [Google Scholar] [CrossRef]
- Nugrahani, I.; Utami, D.; Ibrahim, S.; Nugraha, Y.P.; Uekusa, H. Zwitterionic cocrystal of diclofenac and l-proline: Structure determination, solubility, kinetics of cocrystallization, and stability study. Eur. J. Pharm. Sci. 2018, 117, 168–176. [Google Scholar] [CrossRef]
- Thakral, N.K.; Zanon, R.L.; Kelly, R.C.; Thakral, S. Applications of Powder X-ray Diffraction in Small Molecule Pharmaceuticals: Achievements and Aspirations. J. Pharm. Sci. 2018, 107, 2969–2982. [Google Scholar] [CrossRef]
- Chatterjee, S.K. X-ray Diffraction: Its Theory and Applications; PHI Learning Pvt. Ltd.: Dehli, India, 2010; pp. 103–107. [Google Scholar]
- Hirao, N.; Kawaguchi, S.I.; Hirose, K.; Shimizu, K.; Ohtani, E.; Ohishi, Y. New developments in high-pressure X-ray diffraction beamline for diamond anvil cell at SPring-8. Matter Radiat. Extrem. Condit. 2020, 5, 018403. [Google Scholar] [CrossRef]
- Yang, D.; Cao, J.; Jiao, L.; Yang, S.; Zhang, L.; Lu, Y.; Du, G. Solubility and Stability Advantages of a New Cocrystal of Berberine Chloride with Fumaric Acid. ACS Omega 2020, 5, 8283–8292. [Google Scholar] [CrossRef]
- Zhang, Z.; Cai, Q.; Xue, J.; Qin, J.; Liu, J.; Du, Y. Cocrystal Formation of Antibiotic Nitrofurantoin Drug and Melamine Co-Former Based on a Vibrational Spectroscopic Study. Pharmaceutics 2019, 11, 56. [Google Scholar] [CrossRef]
- Abdullah, A.; Mutmainnah, M.; Wikantyasning, E.R. Cocrystals of Cefixime with Nicotinamide: Improved Solubility, Dissolution, and Permeability. Indones. J. Pharm. 2022, 33, 394–400. [Google Scholar] [CrossRef]
- Choquesillo-Lazarte, D.; Nemecb, V.; Cinčić, D. Halogen bonded cocrystals of active pharmaceutical ingredients: Pyrazinamide, lidocaine and pentoxifylline in combination with haloperfluorinated compounds. Cryst. Eng. Comm. 2017, 19, 5293–5299. [Google Scholar] [CrossRef]
- Dookie, N.; Rambaran, S.; Padayatchi, N.; Mahomed, S.; Naidoo, K. Evolution of drug resistance in Mycobacterium tuberculosis: A review on the molecular determinants of resistance and implications for personalized care. J. Antimicrob. Chemother. 2018, 73, 1138–1151. [Google Scholar] [CrossRef]
- Amrutha, S.; Giri, L.; Lekshmi, S.S.; Varughese, S. Enhanced Aqueous Solubility of the Solid Forms of a BCS Class-II Anti-Tuberculosis Drug, Prothionamide. Cryst. Growth Des. 2020, 20, 5086–5096. [Google Scholar] [CrossRef]
- Refat, L.A.E.; O’Malley, C.; Simmie, J.M.; McArdle, P.; Erxleben, A. Differences in Co-Former Interactions of the 2,4-Diaminopyrimidines Pyrimethamine and Trimethoprim. Cryst. Growth Des. 2022, 22, 3163–3173. [Google Scholar] [CrossRef]
- Fiore, C.; Baraghini, A.; Shemchuk, O.; Sambri, V.; Morotti, M.; Grepioni, F.; Braga, D. Inhibition of the Antibiotic Activity of Cephalosporines by Cocrystallization with Thymol. Cryst. Growth Des. 2022, 22, 1467–1475. [Google Scholar] [CrossRef]
- Mashhadi, S.M.A.; Yufit, D.; Liu, H.; Hodgkinson, P.; Yunus, U. Synthesis and structural characterization of cocrystals of isoniazid and cinnamic acid derivatives. J. Mol. Struc. 2020, 1219, 128621. [Google Scholar] [CrossRef]
- González-González, J.S.; Martínez-Santiago, A.M.M.; Martínez-Martínez, F.J.; Emparán-Legaspi, M.J.; Pineda-Contreras, A.; Flores-Alamo, M.; García-Ortega, H. Cocrystals of Isoniazid with Polyphenols: Mechanochemical Synthesis and Molecular Structure. Crystals 2020, 10, 569. [Google Scholar] [CrossRef]
- Lemmerer, A.; Bernstein, J.; Kahlenberg, V. One-pot covalent and supramolecular synthesis of pharmaceutical cocrystals using the API isoniazid: A potential supramolecular reagent. Cryst. Eng. Comm. 2010, 12, 2856–2864. [Google Scholar] [CrossRef]
- Lemmerer, A.; Bernstein, J.; Kahlenberg, V. Covalent assistance to supramolecular synthesis: Modifying the drug functionality of the antituberculosis API isoniazid in situ during cocrystallization with GRAS and API compounds. Cryst. Eng. Comm. 2012, 14, 2465–2478. [Google Scholar] [CrossRef]
- Mashhadi, S.M.A.; Yunus, U.; Bhatti, M.H.; Tahir, M.N. Isoniazid cocrystals with antioxidant hydroxy benzoic acids. J. Mol. Struc. 2014, 1076, 446–452. [Google Scholar] [CrossRef]
- Drozd, K.V.; Manin, A.N.; Churakov, A.V.; Perlovich, G.L. Drug-drug cocrystals of antituberculous 4-aminosalicylic acid: Screening, crystal structures, thermochemical and solubility studies. Eur. J. Pharm. Sci. 2017, 99, 228–239. [Google Scholar] [CrossRef]
- Aitipamula, S.; Wong, A.B.H.; Chow, P.S.; Tan, R.B.H. Novel solid forms of the anti-tuberculosis drug, Isoniazid: Ternary and polymorphic cocrystals. Cryst. Eng. Comm. 2013, 15, 5877–5887. [Google Scholar] [CrossRef]
- Sarcevica, I.; Orola, L.; Veidis, M.V.; Podjava, A.; Belyakov, S. Crystal and Molecular Structure and Stability of Isoniazid Cocrystals with Selected Carboxylic Acids. Cryst. Growth Des. 2013, 13, 1082–1090. [Google Scholar] [CrossRef]
- Sarcevica, I.; Orola, L.N.; Nartowski, K.P.; Khimyak, Y.Z.; Round, A.N.; Fábián, L. Mechanistic and Kinetic Insight into Spontaneous Cocrystallization of Isoniazid and Benzoic Acid. Mol. Pharm. 2015, 12, 2981–2992. [Google Scholar] [CrossRef]
- Álvarez-Vidaurre, R.; Castiñeiras, A.; Frontera, A.; García-Santos, I.; Gil, D.M.; González-Pérez, J.M.; Niclós-Gutiérrez, J.; Torres-Iglesias, R. Weak Interactions in Cocrystals of Isoniazid with Glycolic and Mandelic Acids. Crystals 2021, 11, 328. [Google Scholar] [CrossRef]
- Mashhadi, S.M.A.; Yunus, U.; Bhatti, M.H.; Ahmed, I. Synthesis, characterization, solubility and stability studies of hydrate cocrystal of antitubercular Isoniazid with antioxidant and anti-bacterial Protocatechuic acid. J. Mol. Sci. 2016, 1117, 17–21. [Google Scholar] [CrossRef]
- Fadipe, V.O.; Haruna, M.S.; Opoku, A.R. Isoniazid-oleanolic acid: A new dual drug cocrystal. In Proceedings of the 17th International Conference and Exhibition on Nanomedicine and Nanotechnology in Healthcare, Brisbane, Australia, 23–24 November 2017; p. 8. [Google Scholar]
- Liu, F.; Wang, L.Y.; Yu, M.C.; Li, Y.T.; Wu, Z.Y.; Yan, C.W. A new cocrystal of isoniazid-quercetin with hepatoprotective effect: The design, structure, and in vitro/in vivo performance evaluation. Eur. J. Pharm. Sci. 2020, 144, 105216. [Google Scholar] [CrossRef]
- Rosa, J.; Machado, T.C.; da Silva, A.K.; Kuminek, G.; Bortolluzzi, A.J.; Caon, T.; Cardoso, S.G. Isoniazid-Resveratrol Cocrystal: A Novel Alternative for Topical Treatment of Cutaneous Tuberculosis. Cryst. Growth Des. 2019, 19, 5029–5036. [Google Scholar] [CrossRef]
- Diniz, L.F.; Souza, M.S.; Carvalho, P.S.; da Silva, C.C.P.; D’Vries, R.F.; Ellena, J. Novel isoniazid cocrystals with aromatic carboxylic acids: Crystal engineering, spectroscopy and thermochemical investigations. J. Mol. Struct. 2018, 1153, 58–68. [Google Scholar] [CrossRef]
- Diniz, L.F.; Souza, M.S.; Carvalho, P.S.; Correa, C.C.; Ellena, J. Modulating the water solubility and thermal stability of the anti-tuberculosis drug Isoniazid via multi-component crystal formation. J. Mol. Struct. 2018, 1171, 223–232. [Google Scholar] [CrossRef]
- Swapna, B.; Maddileti, D.; Nangia, A. Cocrystals of the Tuberculosis Drug Isoniazid: Polymorphism, Isostructurality, and Stability. Cryst. Growth Des. 2014, 14, 5991–6005. [Google Scholar] [CrossRef]
- Karimi-Jafari, M.; Ziaee, A.; O’Reilly, E.; Croker, D.; Walker, G. Formation of Ciprofloxacin-Isonicotinic Acid Cocrystal Using Mechanochemical Synthesis Routes-An Investigation into Critical Process Parameters. Pharmaceutics 2022, 14, 634. [Google Scholar] [CrossRef]
- Bandari, S.; Dronam, V.R.; Eedara, B.B. Development and Preliminary Characterization of Levofloxacin Pharmaceutical Cocrystals for Dissolution Rate Enhancement. J. Pharm. Investig. 2017, 47, 583–591. [Google Scholar] [CrossRef]
- Sousa, I.; Claro, V.; Pereira, J.L.; Amaral, A.L.; Cunha-Silva, L.; De Castro, B.; Gameiro, P. Synthesis, Characterization and Antibacterial Studies of a Copper (II) Levofloxacin Ternary Complex. J. Inorg. Biochem. 2012, 110, 64–71. [Google Scholar] [CrossRef]
- Li, Y.; Yin, W.; Li, M.; Zhang, J.; Chen, L. Multi-component Ag/AgCl/Bi2O3/BiFeO3 for the sunlight-induced photocatalytic degradation. J. Environ. Chem. Eng. 2022, 10, 107280. [Google Scholar] [CrossRef]
- Frackowiak, A.; Kaminski, B.; Urbaniak, B.; Derezinski, P.; Klupczynska, A.; Darul-Duszkiewicz, M.; Kokot, Z.J. A study of ofloxacin and levofloxacin photostability in aqueous solutions. J. Med. Sci. 2016, 85, 238–244. [Google Scholar] [CrossRef]
- Shahnavi, I.A.; Bano, R.; Sheraz, M.A.; Ahmed, S. Photodegradation of levofloxacin in aqueous and organic solvents: A kinetic study. Acta Pharm. 2013, 63, 221–227. [Google Scholar]
- Devi, M.L.; Chandrasekhar, K.B. A validated stability-indicating RP-HPLC method for levofloxacin in the presence of degradation products, its process related impurities and identification of oxidative degradant. J. Pharm. Biomed. Anal. 2009, 50, 710–717. [Google Scholar] [CrossRef]
- Czyrski, A.; Sznura, J. The application of box-Behnken-design in the optimization of HPLC separation of fluoroquinolones. Sci. Rep. 2019, 9, 19458. [Google Scholar] [CrossRef]
- Hai, N.T.T.; Marzouqi, F.A.; Selvaraj, R.; Kim, Y. Rapid photocatalytic degradation of acetaminophen and levofloxacin under solar light irradiation. Mater. Res. Express 2020, 6, 125538. [Google Scholar]
- Khalid, F.; Hassan, S.M.F.; Noor, R.; Zaheer, K.; Hassan, F. Possibility of extending biopharmaceutics classification system based biowaiver to BCS class IIa drug. Pak. J. Pharm. Sci. 2019, 32, 2065–2073. [Google Scholar]
- Wang, X.; Du, S.; Zhang, R.; Jia, X.; Yang, T.; Zhang, X. Drug-drug cocrystals: Opportunities and challenges. Asian J. Pharm. Sci. 2021, 16, 307–317. [Google Scholar] [CrossRef]
- Santenna, C.; Kumar, S.; Balakrishnan, S.; Jhaj, R.; Ahmed, S.N. A comparative experimental study of analgesic activity of a novel non-steroidal anti-inflammatory molecule—Zaltoprofen, and a standard drug—Piroxicam, using murine models. J. Exp. Pharmacol. 2019, 11, 85–91. [Google Scholar] [CrossRef]
- Kiran, H.C.; Venkatesh, D.N.; Kumar, R.R. Formulation and Characterisation of Sustained Release Microbeads Loaded with Zaltoprofen. Int. J. Appl. Pharm. 2019, 11, 173–180. [Google Scholar] [CrossRef]
- Cuong, V.P.; Jong-Suep, B.; Jong-Hun, P.; Sang-Hun, J.; Jong-Seong, K.; Cheong, W.C. A Thorough Analysis of the Effect of Surfactant/s on the Solubility and Pharmacokinetics of (S)-Zaltoprofen. Asian J. Pharm. Sci. 2019, 14, 435–444. [Google Scholar]
- Panzade, P.; Shendarkar, G. Superior Solubility and Dissolution of Zaltoprofen via Pharmaceutical Cocrystals. Turk. J. Pharm. Sci. 2019, 16, 310–316. [Google Scholar] [CrossRef]
- Javed, D.; Zafar, S.; Ahmed, S.; Anwar, K.; Arain, M.I.; Shahnaz, S. Evaluation of drug–drug interactions among dental prescriptions at different clinical settings of Sialkot, Punjab, Pakistan. Prof. Med. J. 2019, 26, 859–864. [Google Scholar] [CrossRef]
- Moore, N.; Pollack, C.; Butkerait, P. Adverse drug reactions and drug–drug interactions with over-the-counter NSAIDs. Ther. Clin. Risk. Manag. 2015, 11, 1061–1075. [Google Scholar]
- Weinblatt, M.E. Drug interactions with non-steroidal anti-inflammatory drugs (NSAIDs). Scand. J. Rheumatol. Suppl. 1989, 83, 7–10. [Google Scholar] [CrossRef]
- Werida, R.H.; El-Okaby, A.M.; El-Khodary, N.M. Evaluation of levofloxacin utilization in intensive care units of tertiary care hospital: A retrospective observational study. Drugs Ther. Perspect. 2020, 36, 33–39. [Google Scholar] [CrossRef]
- Shirasaki, T.; Harata, N.; Nakaye, T.; Akaike, N. Interaction of various non-steroidal anti-inflammatories and quinolone antimicrobials on GABA response in rat dissociated hippocampal pyramidal neurons. Brain Res. 1991, 562, 329–331. [Google Scholar] [CrossRef]
- Ma, X.; Zhuang, C.; Wang, B.; Huang, Y.; Chen, Q.; Lin, N. Cocrystal of apigenin with higher solubility, enhanced oral bioavailability, and anti-inflammatory effect. Cryst. Growth Des. 2019, 19, 5531–5537. [Google Scholar] [CrossRef]
- Kumar, V.; Goswami, P.K.; Tewari, S.; Ramanan, A. Multicomponent solids of niflumic and mefenamic acid based on acid-pyridine synthon. Solid State Chem. 2022, 10, 729608. [Google Scholar] [CrossRef]
- Chui, C.S.L.; Chan, E.W.; Wong, A.Y.S.; Root, A.; Douglas, I.J.; Wong, I.C.K. Association between Oral Fluoroquinolones and Seizures. Neurology 2016, 86, 1708–1715. [Google Scholar] [CrossRef]
- Li, H.; Jiang, Z.; Zhao, Q.; Ding, Y. Adverse Reactions of Fluoroquinolones to Central Nervous System and Rational Drug Use in Nursing Care. Pak. J. Pharm. Sci. 2019, 32, 427–432. [Google Scholar]
- Etminan, M.; Brophy, J.M.; Samii, A. Oral Fluoroquinolone Use and Risk of Peripheral Neuropathy: A Pharmacoepidemiologic Study. Neurology 2014, 83, 1261–1263. [Google Scholar] [CrossRef]
- Hakamifard, A.; Mousavi, S.; Gholipour-Shahraki, T.; Mohaghegh, F. Levofloxacin Induced Stomatitis: A Case Report. J. Pharm. Care 2019, 7, 34–36. [Google Scholar] [CrossRef]
- Kherabi, Y.; Frechet-Jachym, M.; Rioux, C.; Yazdanpanah, Y.; Mechai, F.; Pourcher, V.; Robert, J.; Guglielmetti, L.; MDR TB Management Group. Revised Definitions of Tuberculosis Resistance and Treatment Outcomes, France, 2006–2019. Emerg. Infect. Dis. 2022, 28, 1796–1804. [Google Scholar] [CrossRef]
- Biswas, M.; Biswas, S.; Gupta, B.; Mascellino, M.T.; Rakshit, A.; Chakraborty, B. Changing Paradigms in Antibiotic Resistance in Salmonella Species with Focus on Fluoroquinolone Resistance: A 5-Year Retrospective Study of Enteric Fever in a Tertiary Care Hospital in Kolkata, India. Antibiotics 2022, 11, 1308. [Google Scholar] [CrossRef]
- Moazen, J.; Fatemeh, R.Z.; Behzad, H.A. Characterization of Virulence Genes and Antibiotic Resistance of Methicillin-resistant Staphylococcus aureus (MRSA) and Methicillin-susceptible Staphylococcus aureus (MSSA) Isolates in Intensive Care Unit (ICU) and Non-ICU Wards. Trends Med. Sci. 2022, 2, 129037. [Google Scholar] [CrossRef]
- Vo, T.P.M.; Dinh, T.C.; Phan, H.V.; Cao, T.T.M.; Duong, P.T.; Nguyen, T. Ventilator-Associated Pneumonia Caused by Multidrug-Resistant Gram-Negative Bacteria in Vietnam: Antibiotic Resistance; Treatment Outcomes; and Colistin-Associated Adverse Effects. Healthcare 2022, 10, 1765. [Google Scholar] [CrossRef]
- Meiers, J.; Rox, K.; Titz, A. Lectin-Targeted Prodrugs Activated by Pseudomonas aeruginosa for Self-Destructive Antibiotic Release. J. Med. Chem. 2022, 65, 13988–14014. [Google Scholar] [CrossRef]
- Sostres, C.; Gargallo, C.J.; Arroyo, M.T.; Lanas, A. Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs, aspirin and coxibs) on upper gastrointestinal tract. Best Pract. Res. Clin. Gastroenterol. 2010, 24, 121–132. [Google Scholar] [CrossRef]
- Wongrakpanich, S.; Wongrakpanich, A.; Melhado, K.; Rangaswami, J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 2018, 9, 143–150. [Google Scholar] [CrossRef]
- Varga, Z.; Sabzwari, S.R.A.; Vargova, V. Cardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health Issue. Cureus 2017, 9, e1144. [Google Scholar] [CrossRef]
- Hao, H.; Jia, X.; Ren, T.; Du, Y.; Wang, J. Novel insight into the mechanism underlying synergistic cytotoxicity from two components in 5-Fluorouracil-phenylalanine cocrystal based on cell metabolomics. Eur. J. Pharm. Biopharm. 2022, 180, 181–189. [Google Scholar] [CrossRef]
- Gooma, M.; Elabdeen, A.Z.; Hifney, A.F.; Adam, M.S. Phytotoxicity of antibiotics and non-steroidal anti-inflammatory drugs to green algae Chlorella sp. and Desmodesmus spinosus: Assessment of combined toxicity by box-Behnken experimental design. Environ. Technol. Innov. 2021, 23, 101586. [Google Scholar] [CrossRef]
- Witika, B.A.; Stander, J.C.; Smith, V.J.; Walker, R.B. Nano Cocrystal Embedded Stimuli-Responsive Hydrogels: A Potential Approach to Treat HIV/AIDS. Pharmaceutics 2021, 13, 127. [Google Scholar] [CrossRef]
- Islam, U.I.; Khan, E.; Naveed, U.M.; Shah, A.; Zahoor, M.; Ullah, R.; Bari, A. Enhancing Dissolution Rate and Antibacterial Efficiency of Azithromycin through Drug-Drug Cocrystals with Paracetamol. Antibiotics 2021, 10, 939. [Google Scholar] [CrossRef]
- Leão, C.; Borges, A.; Simões, M. NSAIDs as a Drug Repurposing Strategy for Biofilm Control. Antibiotics 2020, 9, 591. [Google Scholar] [CrossRef]
- Acebedo-Martínez, F.J.; Alarcón-Payer, C.; Rodríguez-Domingo, L.; Domínguez-Martín, A.; Gómez-Morales, J.; Choquesillo-Lazarte, D. Furosemide/Non-Steroidal Anti-Inflammatory Drug-Drug Pharmaceutical Solids: Novel Opportunities in Drug Formulation. Crystals 2021, 11, 1339. [Google Scholar] [CrossRef]
- McArdle, P. Oscail, a Program Package for Small-Molecule Single-Crystal Crystallography with Crystal Morphology Prediction and Molecular Modelling. J. Appl. Crystallogr. 2017, 50, 320–326. [Google Scholar] [CrossRef]
- Lange, L.; Sadowski, G. Thermodynamic Modeling for Efficient Cocrystal Formation. Cryst. Growth Des. 2015, 15, 4406–4416. [Google Scholar] [CrossRef]
- Khalaji, M.; Potrzebowski, M.K.; Dudek, M.K. Virtual Cocrystal Screening Methods as Tools to Understand the Formation of Pharmaceutical Cocrystals—A Case Study of Linezolid, a Wide-Range Antibacterial Drug. Cryst. Growth Des. 2021, 21, 2301–2314. [Google Scholar] [CrossRef]
- Patel, D.J.; Puranik, P.K. Pharmaceutical Cocrystal: An Emerging Technique to Enhance Physicochemical Properties of Drugs. Int. J. ChemTech Res. 2020, 13, 283–309. [Google Scholar] [CrossRef]
- Chapman, C.J.; Groven, L.J. Evaluation of solvate and cocrystal screening methods for CL-20 containing energetic materials. J. Energetic Mater. 2021, 40, 258–272. [Google Scholar] [CrossRef]
- Hao, Y.; Hung, Y.C.; Shimoyama, Y. Investigating Spatial Charge Descriptors for Prediction of Cocrystal Formation Using Machine Learning Algorithms. Cryst. Growth Des. 2022, 22, 6608–6615. [Google Scholar] [CrossRef]
- Zhou, J.H.; Zhao, L.; Shi, L.W.; Luo, P.C. Two models to estimate the density of organic cocrystals. RSC Adv. 2021, 11, 12066–12073. [Google Scholar] [CrossRef]
- Gervasoni, S.; Malloci, G.; Bosin, A.; Vargiu, A.V.; Zgurskaya, H.I.; Ruggerone, P. Recognition of quinolone antibiotics by the multidrug efflux transporter MexB of Pseudomonas aeruginosa. Phys. Chem. Chem. Phys. 2022, 24, 16566–16575. [Google Scholar] [CrossRef]
- Sharma, V.; Mishra, P.; Sharma, A.; Dutt, R.; Shankhwar, V.; Prajapati, P.; Agarwal, D.D. Synthesis, Electrochemical Studies, Molecular Docking, and Biological Evaluation as an Antimicrobial Agent of 5-Amino-6-cyano-3-hydroxybenzo[c]coumarin Using Ni-Cu-Al-CO3 Hydrotalcite as a Catalyst. ACS Omega 2022, 7, 15718–15727. [Google Scholar] [CrossRef]
- Sheldrick, G.M. SHELXT—Integrated space-group and crystal-structure determination. Acta Crystallogr. 2015, 71, 3–8. [Google Scholar] [CrossRef]
- Macrae, C.F.; Sovago, I.; Cottrell, S.J.; Galek, P.T.A.; McCabe, P.; Pidcock, E.; Platings, M.; Shields, G.P.; Stevens, J.S.; Towler, M.; et al. Mercury 4.0: From Visualization to Analysis, Design and Prediction. J. Appl. Crystallogr. 2020, 53, 226–235. [Google Scholar] [CrossRef]
- Fukte, S.R.; Wagh, M.P.; Rawat, S. Coformer Selection: An Important Tool in Co-crystal Formation. Int. J. Pharm. Sci. 2014, 6, 9–14. [Google Scholar]
- Aitipamula, S.; Tan, B.H. Pharmaceutical co-crystals: Crystal engineering and applications. In Multi-Component Crystals: Synthesis, Concepts, Function; Tiekink, E.R., Schpector, J.Z., Eds.; De Gruyter: Berlin, Germany, 2018; pp. 1–27. [Google Scholar]
- Loschen, C.; Klamt, A. Solubility Prediction, Solvate and Cocrystal Screening as Tools for Rational Crystal Engineering. J. Pharm. Pharmacol. 2015, 67, 803–811. [Google Scholar] [CrossRef]
- Duggirala, N.K.; Perry, M.L.; Almarsson, O.; Zaworotko, M.J. Pharmaceutical cocrystals: Along the path to improved medicines. Chem. Commun. 2016, 52, 640–655. [Google Scholar] [CrossRef]
- Nagalapalli, R.; Shankar, Y.G. Synthesis, Crystal Structure, and Hirshfeld Surface Analysis of Ciprofloxacin-Salicylic Acid Molecular Salt. J. Crystallogr. 2014, 2014, 936174. [Google Scholar] [CrossRef]
- Awwadi, F.F.; Dahabiyeh, L.A.; Hamdan, I.I. Trimolecular Co-crystals of Ciprofloxacin, p-Coumaric Acid, and Benzoic Acid or Salicylic Acid. J. Chem. Crystallogr. 2022, 52, 304–314. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).