Dental Luting Cements: An Updated Comprehensive Review
Abstract
1. Introduction
2. Selection of Luting Agents
| Luting Agent | Film Thickness (I *: Low) | Working/ Setting Time (min) (I *: Long/ Short) | Compressive/ Tensile Strength (MPa) (I *: High/High) | Elastic Modules (GPa) (I *: Dentine = 13.7; Enamel = 84–130) | Pulp Irritation (I *: Low) | Solubility (I *: Minimal) | Microleakage (I *: Very Low) | Color Stability and Aesthetics (I *: High) |
|---|---|---|---|---|---|---|---|---|
| Zinc phosphate | ≤25 | 1.5–5/5–14 | 48–133/0.65–4.5 | 19.8 | Moderate | High | High | Low |
| Zinc polycarboxylate | <25 | 1.75–2.5/5–9 | 57–99/1.4–6.3 | 16.1–19.5 | Low | High | High to very high | Low |
| Conventional GIC F | <25 | 2.3–5/6–9 | 93–226/2.36–5.3 | 11.2 | Moderate | Low | Low | Low |
| RMGIC F | >25 | 2–4/2–4 | 85–126/2.53–24 | 6.8 | Moderate to high | Very low | Very low | Moderate |
| Resin cement | >25 | 1–5/1–7 | 52–224/5.07–41 | 11.8–16.5 | Moderate to high | Very low | Very low | High |
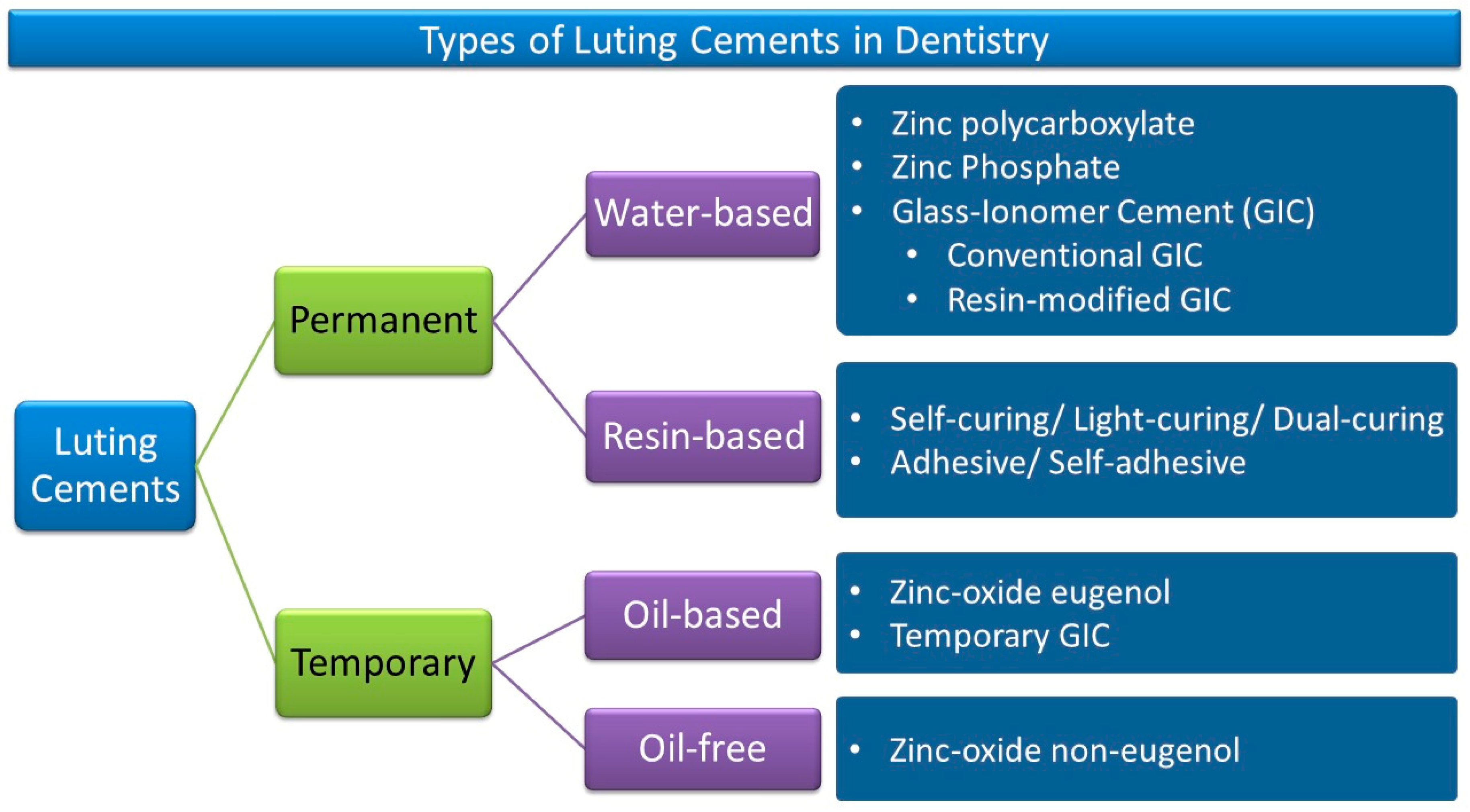
3. Long-Term Luting Cements
3.1. Zinc Phosphate Cement
3.2. Zinc Polycarboxylate Cement
3.3. Glass-Ionomer Cement
3.4. Hybrid Ionomer Cements or Resin-Modified Glass-Ionomer Cements
3.5. Resin Cements
4. Provisional Luting Cements
- Easy to handle and spread;
- Sufficient strength to retain indirect restorations for a short-term period;
- Easy to remove and clean from the substrate and restoration;
- Optimal working and curing times;
- Sufficiently viscous and easy to apply;
- Biocompatible without damaging the soft tissues and the prepared tooth;
- Removed without releasing subproducts;
- Inert to the adhesive properties of the long-term cement.
5. Substrate and Restoration Surface Treatments before Cementation
6. Optical Properties of Luting Cements
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pameijer, C.H. A review of luting agents. Int. J. Dent. 2012, 2012, 752861. [Google Scholar]
- Bagheri, R. Film thickness and flow properties of resin-based cements at different temperatures. J. Dent. 2013, 14, 57–63. [Google Scholar]
- Kious, A.R.; Myers, M.L.; Brackett, W.W.; Haywood, V.B. Film thickness of crown disclosing material and its relevance to cementation. J. Prosthet. Dent. 2014, 112, 1246–1249. [Google Scholar] [CrossRef]
- Aker Sagen, M.; Dahl, J.E.; Matinlinna, J.P.; Tibballs, J.E.; Rønold, H.J. The influence of the resin-based cement layer on ceramic-dentin bond strength. Eur. J. Oral Sci. 2021, 129, e12791. [Google Scholar] [CrossRef] [PubMed]
- Wingo, K. A review of dental cements. J. Vet. Dent. 2018, 35, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Xiong, Y.; Lu, Z.; Zhang, W.; Wu, J.; Wei, R.; Li, X. Evaluation of flushing ability of cementing flushing fluids. ACS Omega 2021, 6, 28955–28966. [Google Scholar] [CrossRef]
- Zaniboni, J.F.; Silva, A.M.; Fernández, E.; de Melo Alencar, C.; Morais, J.M.P.; de Campos, E.A.; Kuga, M.C. Temporary cement residues affect the bond strength and dentin penetration of self-adhesive resin cement in fiberglass post cementation. Microsc. Res. Tech. 2021, 84, 2351–2360. [Google Scholar] [CrossRef]
- Fiori-Júnior, M.; Matsumoto, W.; Silva, R.A.; Porto-Neto, S.T.; Silva, J.M. Effect of temporary cements on the shear bond strength of luting cements. J. Appl. Oral Sci. 2010, 18, 30–36. [Google Scholar] [CrossRef]
- Garcia, I.M.; Leitune, V.C.B.; Ibrahim, M.S.; Melo, M.A.S.; Faus Matoses, V.; Sauro, S.; Collares, F.M. Determining the effects of eugenol on the bond strength of resin-based restorative materials to dentin: A meta-analysis of the literature. Appl. Sci. 2020, 10, 1070. [Google Scholar] [CrossRef]
- Chiluka, L.; Shastry, Y.M.; Gupta, N.; Reddy, K.M.; Prashanth, N.B.; Sravanthi, K. An in vitro study to evaluate the effect of eugenol-free and eugenol-containing temporary cements on the bond strength of resin cement and considering time as a factor. J. Int. Soc. Prev. Community Dent. 2017, 7, 202–207. [Google Scholar]
- Ganss, C.; Jung, M. Effect of eugenol-containing temporary cements on bond strength of composite to dentin. Oper. Dent. 1998, 23, 55–62. [Google Scholar] [PubMed]
- Sokolowski, G.; Szczesio, A.; Bociong, K.; Kaluzinska, K.; Lapinska, B.; Sokolowski, J.; Domarecka, M.; Lukomska-Szymanska, M. Dental resin cements-the influence of water sorption on contraction stress changes and hydroscopic expansion. Materials 2018, 11, 973. [Google Scholar] [PubMed]
- Hiraishi, N.; Kitasako, Y.; Nikaido, T.; Foxton, R.M.; Tagami, J.; Nomura, S. Acidity of conventional luting cements and their diffusion through bovine dentine. Int. Endod. J. 2003, 36, 622–628. [Google Scholar] [CrossRef]
- Ghodsi, S.; Arzani, S.; Shekarian, M.; Aghamohseni, M. Cement selection criteria for full coverage restorations: A comprehensive review of literature. J. Clin. Exp. Dent. 2021, 13, e1154–e1161. [Google Scholar]
- Radovic, I.; Monticelli, F.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Self-adhesive resin cements: A literature review. J. Adhes. Dent. 2008, 10, 251–258. [Google Scholar] [PubMed]
- Leung, G.K.-H.; Wong, A.W.-Y.; Chu, C.-H.; Yu, O.Y. Update on Dental Luting Materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef]
- Ladha, K.; Verma, M. Conventional and contemporary luting cements: An overview. J. Indian Prosthodont. Soc. 2010, 10, 79–88. [Google Scholar]
- Oilo, G. Luting cements: A review and comparison. Int. Dent. J. 1991, 41, 81–88. [Google Scholar]
- Hattar, S.; Hatamleh, M.M.; Sawair, F.; Al-Rabab’ah, M. Bond strength of self-adhesive resin cements to tooth structure. Saudi Dent. J. 2015, 27, 70–74. [Google Scholar] [CrossRef]
- Dos Santos, V.H.; Griza, S.; de Moraes, R.R.; Faria, E.S.A.L. Bond strength of self-adhesive resin cements to composite submitted to different surface pretreatments. Restor. Dent. Endod. 2014, 39, 12–16. [Google Scholar] [CrossRef]
- Perdigão, J.; Araujo, E.; Ramos, R.Q.; Gomes, G.; Pizzolotto, L. Adhesive dentistry: Current concepts and clinical considerations. J. Esthet. Restor. Dent. 2021, 33, 51–68. [Google Scholar] [CrossRef]
- Rosenstiel, S.F.; Land, M.F.; Crispin, B.J. Dental luting agents: A review of the current literature. J. Prosthet. Dent. 1998, 80, 280–301. [Google Scholar]
- Heboyan, A.G. Marginal and internal fit of fixed prosthodontic constructions: A literature review. Int. J. Dent. Res. Rev. 2019, 2, 19. [Google Scholar]
- Srimaneepong, V.; Heboyan, A.; Zafar, M.S.; Khurshid, Z.; Marya, A.; Fernandes, G.V.O.; Rokaya, D. Fixed prosthetic restorations and periodontal health: A narrative review. J. Funct. Biomater. 2022, 13, 15. [Google Scholar] [CrossRef]
- Heboyan, A.; Manrikyan, M.; Zafar, M.S.; Rokaya, D.; Nushikyan, R.; Vardanyan, I.; Vardanyan, A.; Khurshid, Z. Bacteriological evaluation of gingival crevicular fluid in teeth restored using fixed dental prostheses: An in vivo study. Int. J. Mol. Sci. 2021, 22, 5463. [Google Scholar] [CrossRef]
- Avetisyan, A.; Markaryan, M.; Rokaya, D.; Tovani-Palone, M.R.; Zafar, M.S.; Khurshid, Z.; Vardanyan, A.; Heboyan, A. Characteristics of periodontal tissues in prosthetic treatment with fixed dental prostheses. Molecules 2021, 26, 1331. [Google Scholar]
- Sakaguchi, R.; Ferracane, J.; Powers, J. Restorative Dental Materials, 14th ed.; Mosby: St. Louis, MO, USA, 2019. [Google Scholar]
- Mehl, C.; Harder, S.; Steiner, M.; Vollrath, O.; Kern, M. Influence of cement film thickness on the retention of implant-retained crowns. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2013, 22, 618–625. [Google Scholar]
- Tribst, J.P.M.; Dos Santos, A.F.C.; da Cruz Santos, G.; da Silva Leite, L.S.; Lozada, J.C.; Silva-Concílio, L.R.; Baroudi, K.; Amaral, M. Effect of cement layer thickness on the immediate and long-term bond strength and residual stress between lithium disilicate glass-ceramic and human dentin. Materials 2021, 14, 5153. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.E.; Lott, J. A clinically focused discussion of luting materials. Aust. Dent. J. 2011, 56 (Suppl. 1), 67–76. [Google Scholar]
- Game, R.; Darveniza, M. Zinc phosphate cement and retention. Aust. Dent. J. 1988, 33, 154. [Google Scholar]
- Masaka, N.; Yoneda, S.; Masaka, K. An up to 43-year longitudinal study of fixed prosthetic restorations retained with 4-meta/mma-tbb resin cement or zinc phosphate cement. J. Prosthet. Dent. 2021, S0022–S3913, 00212. [Google Scholar] [CrossRef] [PubMed]
- Fakiha, Z.; Al-Aujan, A.; Al-Shamrani, S. Retention of cast posts cemented with zinc phosphate cement using different cementing techniques. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2001, 10, 37–41. [Google Scholar]
- Shetty, H.; Shetty, S.; Kakade, A.; Shetty, A.; Karobari, M.I.; Pawar, A.M.; Marya, A.; Heboyan, A.; Venugopal, A.; Nguyen, T.H.; et al. Three-dimensional semi-automated volumetric assessment of the pulp space of teeth following regenerative dental procedures. Sci. Rep. 2021, 11, 21914. [Google Scholar] [CrossRef]
- Wilson, A.D. The nature of the zinc polycarboxylate cement matrix. J. Biomed. Mater. Res. 1982, 16, 549–557. [Google Scholar]
- Ali, M.N.; Edwards, M.; Nicholson, J.W. Zinc polycarboxylate dental cement for the controlled release of an active organic substance: Proof of concept. J. Mater. Sci. Mater. Med. 2010, 21, 1249–1253. [Google Scholar]
- Akinmade, A.O.; Nicholson, J.W. Effect of adhesive layer thickness on the bond strength of a zinc polycarboxylate dental cement. Biomaterials 1995, 16, 149–154. [Google Scholar] [CrossRef]
- Branco, R.; Hegdahl, T. Physical properties of some zinc phosphate and polycarboxylate cements. Acta Odontol. Scand. 1983, 41, 349–353. [Google Scholar] [CrossRef]
- Handa, M.; Marya, P.; Gupta, V.; Chopra, S. Comparative evaluation of microleakage of metallic copings luted with three different commercially available luting cements: An in vitro study. J. Indian Prosthodont Soc. 2021, 21, 57–65. [Google Scholar]
- Heboyan, A.; Marya, A.; Syed, A.U.Y.; Khurshid, Z.; Zafar, M.S.; Rokaya, D.; Anastasyan, M. In vitro microscopic evaluation ofmetal- and zirconium-oxide-based crowns’ marginal fit. Pesqui. Bras. Odontopediatria Clín. Integr. 2022, 22, e210144. [Google Scholar]
- Kreulen, C.M.; Wolke, J.G.; de Baat, C.; Creugers, N.H. [attaching single- and multi-unit fixed dental prostheses]. Ned. Tijdschr. Tandheelkd. 2013, 120, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Sathyanarayan, S.; Balavadivel, T.; Guru, R.C.; Sande, A.R.; Rajendran, V.; Sengottaiyan, A.K. Retention of various luting agents used with implant-supported crowns. J. Pharm. Bioallied Sci. 2021, 13, S1206–S1209. [Google Scholar]
- Aladag, A.; Sahan, M.H.; Akkus, N.O.; Aktas, R. Retention of luting agents used for implant-supported restorations: A comparative in-vitro study. Niger. J. Clin. Pract. 2020, 23, 1073–1078. [Google Scholar] [PubMed]
- Ramzan, M.; Karobari, M.I.; Heboyan, A.; Mohamed, R.N.; Mustafa, M.; Basheer, S.N.; Desai, V.; Batool, S.; Ahmed, N.; Zeshan, B. Synthesis of silver nanoparticles from extracts of wild ginger (zingiber zerumbet) with antibacterial activity against selective multidrug resistant oral bacteria. Molecules 2022, 27, 2007. [Google Scholar] [CrossRef]
- Francisconi, L.F.; Scaffa, P.M.; de Barros, V.R.; Coutinho, M.; Francisconi, P.A. Glass ionomer cements and their role in the restoration of non-carious cervical lesions. J. Appl. Oral Sci. 2009, 17, 364–369. [Google Scholar]
- Krämer, N.; Schmidt, M.; Lücker, S.; Domann, E.; Frankenberger, R. Glass ionomer cement inhibits secondary caries in an in vitro biofilm model. Clin. Oral Investig. 2018, 22, 1019–1031. [Google Scholar] [CrossRef] [PubMed]
- Abhay, S.S.; Ganapathy, D.; Veeraiyan, D.N.; Ariga, P.; Heboyan, A.; Amornvit, P.; Rokaya, D.; Srimaneepong, V. Wear resistance, color stability and displacement resistance of milled peek crowns compared to zirconia crowns under stimulated chewing and high-performance aging. Polymers 2021, 13, 3761. [Google Scholar]
- Kakkad, N.; Yadav, N.S.; Hazari, P.; Narwani, S.; Somkuwar, K.; Basha, S.; Verma, V.; Arora, S.; Aldowah, O.; Heboyan, A.; et al. Comparative evaluation of tensile bond strength of poly ether ether ketone (peek) and zirconia copings using resin cement with or without adhesive: An in vitro study. Materials 2022, 15, 4167. [Google Scholar] [CrossRef] [PubMed]
- Perera, D.; Yu, S.C.H.; Zeng, H.; Meyers, I.A.; Walsh, L.J. Acid resistance of glass ionomer cement restorative materials. Bioengineering 2020, 7, 150. [Google Scholar] [PubMed]
- Bahsi, E.; Sagmak, S.; Dayi, B.; Cellik, O.; Akkus, Z. The evaluation of microleakage and fluoride release of different types of glass ionomer cements. Niger. J. Clin. Pract. 2019, 22, 961–970. [Google Scholar] [CrossRef]
- Brito, C.R.; Velasco, L.G.; Bonini, G.A.; Imparato, J.C.; Raggio, D.P. Glass ionomer cement hardness after different materials for surface protection. J. Biomed. Mater. Res. A 2010, 93, 243–246. [Google Scholar]
- Wan Jusoh, W.N.; Matori, K.A.; Mohd Zaid, M.H.; Zainuddin, N.; Ahmad Khiri, M.Z.; Abdul Rahman, N.A.; Abdul Jalil, R.; Kul, E. Incorporation of hydroxyapatite into glass ionomer cement (gic) formulated based on alumino-silicate-fluoride glass ceramics from waste materials. Materials 2021, 14, 954. [Google Scholar] [CrossRef]
- Liu, R.; Wang, E.; Guo, Y.; Zhou, Q.; Zheng, Y.; Zhai, J.; Zhang, K.; Zhang, B. Enhanced antibacterial properties and promoted cell proliferation in glass ionomer cement by modified with fluorinated graphene-doped. J. Appl. Biomater. Funct. Mater. 2021, 19, 22808000211037487. [Google Scholar] [CrossRef] [PubMed]
- Francois, P.; Fouquet, V.; Attal, J.P.; Dursun, E. Commercially available fluoride-releasing restorative materials: A review and a proposal for classification. Materials 2020, 13, 2313. [Google Scholar]
- Malhotra, S.; Bhullar, K.K.; Kaur, S.; Malhotra, M.; Kaur, R.; Handa, A. Comparative evaluation of compressive strength and flexural strength of gc gold hybrid, gic conventional and resin-modified glass-ionomer cement. J. Pharm. Bioallied. Sci. 2022, 14, S214–S216. [Google Scholar]
- Kielbassa, A.M.; Oehme, E.P.; Shakavets, N.; Wolgin, M. In vitro wear of (resin-coated) high-viscosity glass ionomer cements and glass hybrid restorative systems. J. Dent. 2021, 105, 103554. [Google Scholar] [CrossRef]
- Mickenautsch, S.; Tyas, M.J.; Yengopal, V.; Oliveira, L.B.; Bönecker, M. Absence of carious lesions at margins of glass-ionomer cement (gic) and resin-modified gic restorations: A systematic review. Eur. J. Prosthodont. Restor. Dent. 2010, 18, 139–145. [Google Scholar] [PubMed]
- Yengopal, V.; Mickenautsch, S. Caries-preventive effect of resin-modified glass-ionomer cement (rm-gic) versus composite resin: A quantitative systematic review. Eur. Arch Paediatr. Dent. 2011, 12, 5–14. [Google Scholar]
- Bezerra, I.M.; Brito, A.C.M.; de Sousa, S.A.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.F.D. Glass ionomer cements compared with composite resin in restoration of noncarious cervical lesions: A systematic review and meta-analysis. Heliyon 2020, 6, e03969. [Google Scholar]
- Brenes-Alvarado, A.; Cury, J.A. Fluoride release from glass ionomer cement and resin-modified glass ionomer cement materials under conditions mimicking the caries process. Oper. Dent. 2021, 46, 457–466. [Google Scholar] [CrossRef]
- Heboyan, A.; Avetisyan, A.; Karobari, M.I.; Marya, A.; Khurshid, Z.; Rokaya, D.; Zafar, M.S.; Fernandes, G.V.O. Tooth root resorption: A review. Sci. Prog. 2022, 105, 368504221109217. [Google Scholar]
- Tanweer, N.; Qazi, F.U.; Das, G.; Bilgrami, A.; Basha, S.; Ahmed, N.; Bahammam, H.A.; Bahammam, S.A.; Basheer, S.N.; Assiry, A.A.; et al. Effect of erosive agents on surface characteristics of nano-fluorapatite ceramic: An in-vitro study. Molecules 2022, 27, 4691. [Google Scholar]
- Zeller, D.K.; Fischer, J.; Rohr, N. Viscous behavior of resin composite cements. Dent. Mater. J. 2021, 40, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Goulart, M.; Borges Veleda, B.; Damin, D.; Bovi Ambrosano, G.M.; Coelho de Souza, F.H.; Erhardt, M.C.G. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int. J. Esthet. Dent. 2018, 13, 86–97. [Google Scholar] [PubMed]
- Gürdal, I.; Atay, A.; Eichberger, M.; Cal, E.; Üsümez, A.; Stawarczyk, B. Color change of cad-cam materials and composite resin cements after thermocycling. J. Prosthet. Dent. 2018, 120, 546–552. [Google Scholar] [CrossRef]
- Karkera, R.; Raj, A.P.; Isaac, L.; Mustafa, M.; Reddy, R.N.; Thomas, M. Comparison of the solubility of conventional luting cements with that of the polyacid modified composite luting cement and resin-modified glass lonomer cement. J. Contemp. Dent. Pract. 2016, 17, 1016–1021. [Google Scholar]
- Nakabayashi, N.; Watanabe, A.; Gendusa, N.J. Dentin adhesion of "modified" 4-meta/mma-tbb resin: Function of hema. Dent. Mater. 1992, 8, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Nakabayashi, N.; Takarada, K. Effect of hema on bonding to dentin. Dent. Mater. 1992, 8, 125–130. [Google Scholar]
- Heboyan, A.; Zafar, M.S.; Karobari, M.I.; Tribst, J.P.M. Insights into polymeric materials for prosthodontics and dental implantology. Materials 2022, 15, 5383. [Google Scholar]
- Zimmerli, B.; Strub, M.; Jeger, F.; Stadler, O.; Lussi, A. Composite materials: Composition, properties and clinical applications. A literature review. Schweiz. Monatsschr. Zahnmed. 2010, 120, 972–986. [Google Scholar]
- Shinkai, K.; Taira, Y.; Suzuki, S.; Kawashima, S.; Suzuki, M. Effect of filler size and filler loading on wear of experimental flowable resin composites. J. Appl. Oral Sci. 2018, 26, e201060652. [Google Scholar]
- El-Deeb, H.A.; Mobarak, E.H. Repair bond strength of high-viscosity glass-ionomer cements using resin composite bonded with light- and self-cured adhesive systems. Oper. Dent. 2021, 46, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Akehashi, S.; Takahashi, R.; Nikaido, T.; Burrow, M.F.; Tagami, J. Enhancement of dentin bond strength of resin cement using new resin coating materials. Dent. Mater. J. 2019, 38, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Wiedenmann, F.; Becker, F.; Eichberger, M.; Stawarczyk, B. Measuring the polymerization stress of self-adhesive resin composite cements by crack propagation. Clin. Oral Investig. 2021, 25, 1011–1018. [Google Scholar] [CrossRef] [PubMed]
- Eltoukhy, R.I.; Elkaffas, A.A.; Ali, A.I.; Mahmoud, S.H. Indirect resin composite inlays cemented with a self-adhesive, self-etch or a conventional resin cement luting agent: A 5 years prospective clinical evaluation. J. Dent. 2021, 112, 103740. [Google Scholar]
- Al-Saleh, M.; El-Mowafy, O.; Tam, L.; Fenton, A. Microleakage of posterior composite restorations lined with self-adhesive resin cements. Oper. Dent. 2010, 35, 556–563. [Google Scholar]
- Vasconcelos, E.C.J.; Polido, M.; Brito, J.; Gonçalves, L.L. Dentin bonding and sem analysis of a new experimental universal adhesive system containing a dendrimer. Polymers 2020, 12, 461. [Google Scholar]
- Inukai, T.; Abe, T.; Ito, Y.; Pilecki, P.; Wilson, R.F.; Watson, T.F.; Foxton, R.M. Adhesion of indirect mod resin composite inlays luted with self-adhesive and self-etching resin cements. Oper. Dent. 2012, 37, 474–484. [Google Scholar]
- Favarão, J.; Oliveira, D.; Zanini, M.M.; Rocha, M.G.; Correr-Sobrinho, L.; Sinhoreti, M. Effect of curing-light attenuation on color stability and physical and chemical properties of resin cements containing different photoinitiators. J. Mech. Behav. Biomed. Mater. 2021, 113, 104110. [Google Scholar] [CrossRef]
- Farah, C.S.; Orton, V.G.; Collard, S.M. Shear bond strength of chemical and light-cured glass ionomer cements bonded to resin composites. Aust. Dent. J. 1998, 43, 81–86. [Google Scholar] [CrossRef]
- Olmos-Olmos, G.; Teutle-Coyotecatl, B.; Román-Mendez, C.D.; Carrasco-Gutiérrez, R.; González-Torres, M.; Contreras-Bulnes, R.; Rodríguez-Vilchis, L.E.; de Los Angeles Moyaho-Bernal, M. The influence of light-curing time on fluoride release, surface topography, and bacterial adhesion in resin-modified glass ionomer cements: Afm and sem in vitro study. Microsc. Res. Tech. 2021, 84, 1628–1637. [Google Scholar]
- Bragança, G.F.; Vianna, A.S.; Neves, F.D.; Price, R.B.; Soares, C.J. Effect of exposure time and moving the curing light on the degree of conversion and knoop microhardness of light-cured resin cements. Dent. Mater. 2020, 36, e340–e351. [Google Scholar] [CrossRef] [PubMed]
- Aldhafyan, M.; Silikas, N.; Watts, D.C. Influence of curing modes on thermal stability, hardness development and network integrity of dual-cure resin cements. Dent. Mater. 2021, 37, 1854–1864. [Google Scholar] [CrossRef] [PubMed]
- Mazzitelli, C.; Maravic, T.; Mancuso, E.; Josic, U.; Generali, L.; Comba, A.; Mazzoni, A.; Breschi, L. Influence of the activation mode on long-term bond strength and endogenous enzymatic activity of dual-cure resin cements. Clin. Oral. Investig. 2022, 26, 1683–1694. [Google Scholar] [CrossRef] [PubMed]
- Gultekin, P.; Pak Tunc, E.; Ongul, D.; Turp, V.; Bultan, O.; Karataslı, B. Curing efficiency of dual-cure resin cement under zirconia with two different light curing units. J. Istanb. Univ. Fac. Dent. 2015, 49, 8–16. [Google Scholar]
- Turkoglu, P.; Sen, D. Evaluation of dual-cure resin cement polymerization under different types and thicknesses of monolithic zirconia. Biomed. Res. Int. 2019, 2019, 4567854. [Google Scholar] [PubMed]
- Yoshikawa, T.; Sadr, A.; Tagami, J. µct-3d visualization analysis of resin composite polymerization and dye penetration test of composite adaptation. Dent. Mater. J. 2018, 37, 71–77. [Google Scholar] [CrossRef]
- Yoshikawa, T.; Morigami, M.; Sadr, A.; Tagami, J. Effects of light curing method and resin composite composition on composite adaptation to the cavity wall. Dent. Mater. J. 2014, 33, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.A.; Coutinho, M.; Cardozo, P.I.; Silva, L.A.; Zorzatto, J.R. Conventional dual-cure versus self-adhesive resin cements in dentin bond integrity. J. Appl. Oral Sci. 2011, 19, 355–362. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Naranjo, B.; Valdiviezo, P. Adhesive systems used in indirect restorations cementation: Review of the literature. Dent. J. 2019, 7, 71. [Google Scholar]
- Nagamine, M.; Itota, T.; Torii, Y.; Irie, M.; Staninec, M.; Inoue, K. Effect of resin-modified glass ionomer cements on secondary caries. Am. J. Dent. 1997, 10, 173–178. [Google Scholar]
- Tam, L.E.; Chan, G.P.; Yim, D. In vitro caries inhibition effects by conventional and resin-modified glass-ionomer restorations. Oper. Dent. 1997, 22, 4–14. [Google Scholar] [PubMed]
- Nicholson, J.W.; Czarnecka, B. The biocompatibility of resin-modified glass-ionomer cements for dentistry. Dent. Mater. 2008, 24, 1702–1708. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca Roberti Garcia, L.; Pontes, E.C.; Basso, F.G.; Hebling, J.; de Souza Costa, C.A.; Soares, D.G. Transdentinal cytotoxicity of resin-based luting cements to pulp cells. Clin. Oral. Investig. 2016, 20, 1559–1566. [Google Scholar] [PubMed]
- Pontes, E.C.; Soares, D.G.; Hebling, J.; Costa, C.A. Cytotoxicity of resin-based luting cements to pulp cells. Am. J. Dent. 2014, 27, 237–244. [Google Scholar] [PubMed]
- da Silva, D.C.; Vaz, L.G.; Tavares, W.L.F.; Vieira, L.Q.; de Oliveira, R.R.; Sobrinho, A.P.R. Cytotoxicity of two self-adhesive resin cements and their interference in the phagocytic activity of murine macrophages. Restor. Dent. Endod. 2022, 47, e31. [Google Scholar] [PubMed]
- Ahsan, A.; Ashley, M. Hypersensitivity to dental composites and resin-bonding agents. Dent. Update 2016, 43, 836–838; 841–842. [Google Scholar]
- Bourbia, M.; Finer, Y. Biochemical stability and interactions of dental resin composites and adhesives with host and bacteria in the oral cavity: A review. J. Can. Dent. Assoc. 2018, 84, i1. [Google Scholar]
- Mounajjed, R.; Salinas, T.J.; Ingr, T.; Azar, B. Effect of different resin luting cements on the marginal fit of lithium disilicate pressed crowns. J. Prosthet. Dent. 2018, 119, 975–980. [Google Scholar] [CrossRef]
- Elbishari, H.; Elsubeihi, E.S.; Alkhoujah, T.; Elsubeihi, H.E. Substantial in-vitro and emerging clinical evidence supporting immediate dentin sealing. Jpn. Dent. Sci. Rev. 2021, 57, 101–110. [Google Scholar] [CrossRef]
- Heboyan, A.; Syed, A.U.Y.; Rokaya, D.; Cooper, P.R.; Manrikyan, M.; Markaryan, M. Cytomorphometric analysis of inflammation dynamics in the periodontium following the use of fixed dental prostheses. Molecules 2020, 25, 4650. [Google Scholar] [CrossRef]
- Heboyan, A.G.; Movsisyan, N.M.; Khachatryan, V.A. Provisional restorations in restorative dentistry. World Sci. 2019, 3, 11–17. [Google Scholar]
- Heboyan, A.; Manrikyan, M.; Markaryan, M.; Vardanyan, I. Changes in the parameters of gingival crevicular fluid in masticatory function restoration by various prosthodontic constructions. Int. J. Pharm. Res. 2020, 12, 2088–2093. [Google Scholar]
- Bezerra, C.P.; Campos, C.F.; Leite, J.; Fernandes, M.S.; Coury Saraceni, C.H.; Rodrigues, F.P.; Dutra-Correa, M. On the understanding of zinc-oxide eugenol cement use prior to etch-rinse bonding strategies. Indian J. Dent. Res. 2019, 30, 424–427. [Google Scholar] [PubMed]
- Dragland, I.S.; Wellendorf, H.; Kopperud, H.; Stenhagen, I.; Valen, H. Investigation on the antimicrobial activity of chitosan-modified zinc oxide-eugenol cement. Biomater. Investig. Dent. 2019, 6, 99–106. [Google Scholar] [PubMed]
- Durairaj, R.B.; Sivasaravanan, S.; Sharma, D.K.; Ramachandran, S.; Heboyan, A. Investigations on mechanical properties of titanium reinforced glass ionomer cement (gic)—Ceramic composites suitable for dental implant applications. Dig. J. Nanomater. Biostructures 2021, 16, 161–167. [Google Scholar] [CrossRef]
- Lewinstein, I.; Block, J.; Melamed, G.; Dolev, E.; Matalon, S.; Ormianer, Z. Fluoride ion release and solubility of fluoride enriched interim cements. J. Prosthet. Dent. 2014, 112, 188–193. [Google Scholar]
- Billington, R.W.; Hadley, P.C.; Williams, J.A.; Pearson, G.J. Kinetics of fluoride release from zinc oxide-based cements. Biomaterials 2001, 22, 2507–2513. [Google Scholar] [CrossRef]
- Martins, J.D.; Moura, D.; Lima, C.M.; de Carvalho, R.; Leite, F.; Souza, R. Surface treatment and cementation of lithium silicate ceramics containing zro2. Oper. Dent. 2022, 47, 202–213. [Google Scholar] [CrossRef]
- Blanchet, I.; Camoin, A.; Tardieu, C.; Jacquot, B. Microabrasion in the management of enamel discolorations in paediatric dentistry: A systematic review. J. Clin. Pediatr. Dent. 2022, 47, 17–26. [Google Scholar]
- Kang, L.L.; Chuang, S.F.; Li, C.L.; Lin, J.C.; Lai, T.W.; Wang, C.C. Enhancing resin cement adhesion to zirconia by oxygen plasma-aided silicatization. Materials 2022, 15, 5568. [Google Scholar] [CrossRef]
- Campos, F.; Almeida, C.S.; Rippe, M.P.; de Melo, R.M.; Valandro, L.F.; Bottino, M.A. Resin bonding to a hybrid ceramic: Effects of surface treatments and aging. Oper. Dent. 2016, 41, 171–178. [Google Scholar]
- Guarda, G.B.; Correr, A.B.; Gonçalves, L.S.; Costa, A.R.; Borges, G.A.; Sinhoreti, M.A.; Correr-Sobrinho, L. Effects of surface treatments, thermocycling, and cyclic loading on the bond strength of a resin cement bonded to a lithium disilicate glass ceramic. Oper. Dent. 2013, 38, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.P.; Anami, L.C.; Melo, R.M.; Valandro, L.F.; Bottino, M.A. Effects of surface treatments on the bond strength between resin cement and a new zirconia-reinforced lithium silicate ceramic. Oper. Dent. 2016, 41, 284–292. [Google Scholar]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Effect of different surface treatments on resin-matrix cad/cam ceramics bonding to dentin: In vitro study. BMC Oral Health 2022, 22, 635. [Google Scholar]
- Eder, A.; Wickens, J. Surface treatment of gold alloys for resin adhesion. Quintessence Int. 1996, 27, 35–40. [Google Scholar]
- Vichi, A.; Ferrari, M.; Davidson, C.L. Influence of ceramic and cement thickness on the masking of various types of opaque posts. J. Prosthet. Dent. 2000, 83, 412–417. [Google Scholar]
- Bacchi, A.; Caldas, R.A.; Cesar, P.F.; Pfeifer, C.S. Optical properties and colorimetric evaluation of resin cements formulated with thio-urethane oligomers. J. Esthet. Restor. Dent. 2019, 31, 153–159. [Google Scholar]
- Chang, J.; Da Silva, J.D.; Sakai, M.; Kristiansen, J.; Ishikawa-Nagai, S. The optical effect of composite luting cement on all ceramic crowns. J. Dent. 2009, 37, 937–943. [Google Scholar]
- Turgut, S.; Bagis, B. Effect of resin cement and ceramic thickness on final color of laminate veneers: An in vitro study. J. Prosthet. Dent. 2013, 109, 179–186. [Google Scholar] [CrossRef]
- Alarcón-Sánchez, M.A.; Heboyan, A.; Fernandes, G.V.d.O.; Castro-Alarcón, N.; Romero-Castro, N.S. Potential Impact of Prosthetic Biomaterials on the Periodontium: A Comprehensive Review. Molecules 2023, 28, 1075. [Google Scholar] [CrossRef]
- Menezes-Silva, R.; Cabral, R.N.; Pascotto, R.C.; Borges, A.F.S.; Martins, C.C.; Navarro, M.F.L.; Sidhu, S.K.; Leal, S.C. Mechanical and optical properties of conventional restorative glass-ionomer cements—A systematic review. J. Appl. Oral Sci. 2019, 27, e2018357. [Google Scholar] [CrossRef] [PubMed]

| Non-Adhesive Cements | Adhesive Cements |
|---|---|
|
|
| Luting Agents | Indications | Adhesion | Excess Removal (I *: Easy) | Retention (I *: High) | Advantages | Disadvantages | Precautions |
|---|---|---|---|---|---|---|---|
| Zinc phosphate | 1,3,6,9,10 | Chemical | Easy | Moderate | History of use | Solubility, leakage | Use for “traditional” cast restorations |
| Zinc polycarboxylate | 1,3,4,6 | Chemical | Medium | Low/moderate | Biocompatibility | Low strength, solubility | Do not reduce powder/liquid ratio |
| Glass-ionomer F | 1,3,6,9,10,12 | Chemical | Medium | Moderate to high | Translucency | Solubility, leakage | Avoid early moisture exposure |
| RMGIC F | 1,3,9,10 | Micro-mechanical | Medium | High | Low solubility, low microleakage | Water sorption, history of use | Avoid with ceramic restorations |
| Resin cement | 1–3, 5–12 | Mechanical | Medium to difficult | High | Adhesive, low solubility | Film thickness, history of use | Moisture control |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heboyan, A.; Vardanyan, A.; Karobari, M.I.; Marya, A.; Avagyan, T.; Tebyaniyan, H.; Mustafa, M.; Rokaya, D.; Avetisyan, A. Dental Luting Cements: An Updated Comprehensive Review. Molecules 2023, 28, 1619. https://doi.org/10.3390/molecules28041619
Heboyan A, Vardanyan A, Karobari MI, Marya A, Avagyan T, Tebyaniyan H, Mustafa M, Rokaya D, Avetisyan A. Dental Luting Cements: An Updated Comprehensive Review. Molecules. 2023; 28(4):1619. https://doi.org/10.3390/molecules28041619
Chicago/Turabian StyleHeboyan, Artak, Anna Vardanyan, Mohmed Isaqali Karobari, Anand Marya, Tatevik Avagyan, Hamid Tebyaniyan, Mohammed Mustafa, Dinesh Rokaya, and Anna Avetisyan. 2023. "Dental Luting Cements: An Updated Comprehensive Review" Molecules 28, no. 4: 1619. https://doi.org/10.3390/molecules28041619
APA StyleHeboyan, A., Vardanyan, A., Karobari, M. I., Marya, A., Avagyan, T., Tebyaniyan, H., Mustafa, M., Rokaya, D., & Avetisyan, A. (2023). Dental Luting Cements: An Updated Comprehensive Review. Molecules, 28(4), 1619. https://doi.org/10.3390/molecules28041619












