Abstract
Antibodies and their derivatives (scFv, Fabs, etc.) represent a unique class of biomolecules that combine selectivity with the ability to target drug delivery. Currently, one of the most promising endeavors in this field is the development of molecular diagnostic tools and antibody-based therapeutic agents, including antibody–drug conjugates (ADCs). To meet this challenge, it is imperative to advance methods for modifying antibodies. A particularly promising strategy involves the introduction of carbonyl groups into the antibody that are amenable to further modification by biorthogonal reactions, namely aliphatic, aromatic, and α-oxo aldehydes, as well as aliphatic and aryl–alkyl ketones. In this review, we summarize the preparation methods and applications of site-specific antibody conjugates that are synthesized using this approach.
1. Introduction
Conjugates of biomolecules [1,2] serve as potent research tools in molecular biology and find applications as therapeutic agents [3]. A variety of reactions from the arsenal of organic chemistry are used to obtain them [1,2,4,5]. The modification of biomolecules should be specific to particular functional groups [2]. The key conjugate assembly reaction should be conducted with high yield in aqueous solutions at physiological temperatures and should not affect other functional groups present in the biomolecule [6,7]. Requirements for such reactions were established at the beginning of the century, leading to the pursuit of new “bioorthogonal” reactions [8] and enhancements of existing methods. The 2022 Nobel Prize in Chemistry was awarded for the development of these reactions, a testament to their significant practical importance [9,10,11,12].
Antibodies [13,14] and their derivatives [14,15,16,17] have long been used for diagnostics [18,19,20] and therapy [21,22]. The chemical modification of antibodies has significantly broadened their scope of application [23]. The primary focus of antibody chemical modification is in the development of therapeutic antibody–drug conjugates (ADCs) (Figure 1) [24].
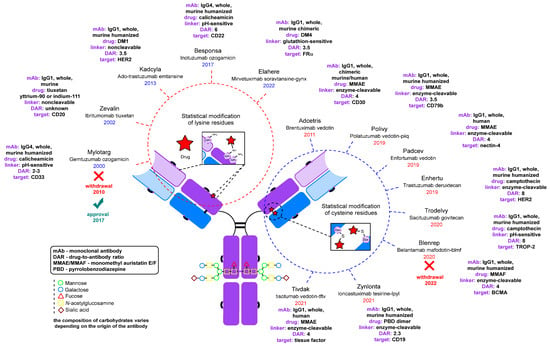
Figure 1.
FDA-approved antibody–drug conjugates and radioimmunoconjugates [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72].
ADCs are a rapidly growing class of drugs for the treatment of oncologic diseases [73,74]. Every year the U.S. Food and Drug Administration (FDA) approves new conjugates for clinical use [75].
There are five classes of mammalian immunoglobulins (Ig): IgA, IgE, IgM, IgG, and IgD [76]. They differ from each other in structure, function, and localization in the body. While some attempts have been made to use IgM [77,78] and other types in conjugation [78] and therapy [79], the IgG class has been by far the most popular for therapeutic purposes as a monoclonal antibody, and, in particular, for the construction of ADCs. The IgG class is the most abundant in mammals and has high stability and a long circulation time in the bloodstream [13]. In this work, we will focus on conjugates involving immunoglobulins of this isotype and their derivatives, such as nanoantibodies.
The IgG class is divided into four subtypes: IgG1, IgG2, IgG3, and IgG4. Of these, the IgG1 subtype remains the most popular subtype for ADC development due to its excellent stability (~21 days circulation time in the bloodstream) and its ability to recruit the complement system for enhanced therapeutic efficacy. IgG2 is less effective in triggering the complement system and is less stable, as this subtype can form covalent dimers leading to subsequent aggregation. IgG3, on the other hand, is less suitable for therapeutic use due to its short plasma half-life (~7 days). IgG4 can form hybrid, bispecific antibodies with non-identical paratopes in their two Fab (fragment antigen-binding) regions by exchanging one pair of light and heavy chains with other IgG4 antibodies [80,81], which hinders the targeting ability of the antibodies of this subtype.
Engineered bispecific antibodies are promising for therapeutic applications as well as for ADC development [82,83]. Bispecific antibodies are the subject of numerous literature reviews [84,85,86,87,88]; however, we will not focus on them here as almost all of them are modified with a genetically introduced [89] or native cysteine residue [90] using maleimide reagents [91], which is outside the scope of this review.
To overcome problems related to the immunogenicity of antibodies [92,93] derived from organisms of different species, recombinant antibodies—chimeric and humanized [94]—are widely used [80,93]. It is worth noting that the majority of antibodies used in FDA-approved ADCs [24] are humanized murine antibodies [13,25].
A fundamental property of antibodies is their ability to recognize and bind to specific antigens [76]. It is important to emphasize that any modification introduced to an IgG molecule should be carefully designed and characterized to prevent any adverse impact on the antibody’s antigen binding ability, specifically on the antigen-binding site [14]. This is particularly important for ADCs, as the precise recognition of the tumor antigen is essential for the targeted delivery of cytotoxic agents [95].
The schematic structure of a typical full-length monoclonal antibody of the IgG class is shown in Figure 2. Immunoglobulin G is a Y-shaped protein molecule with a size of about 10 nm and a mass of about 150 kDa. It is composed of four polypeptide chains. The two larger chains, each consisting of two domains of roughly 110 amino acids, are referred to as heavy chains. These heavy chains are connected by a flexible polypeptide chain rich in cysteine and proline known as the hinge region [76,96]. Within the hinge region, the two heavy chains are linked to each other by disulfide bonds (ranging from 2 to 11, depending on the IgG subtype) that are exposed to the surrounding solvent [97]. In addition, two light chains, each consisting of a single domain, are linked to one domain of a heavy chain by disulfide bonds (one bond between one heavy and one light chain in all IgG subtypes) [97]. This link forms Fab fragments, which are directly responsible for binding to antigens. It is important to note that this structural arrangement provides the antibody molecule with exceptional flexibility. Preserving this structure during the modification process is crucial. The Fab regions can rotate about their axes, move in different directions at significant angles, bend, stretch, and contract to effectively engage with antigens [96,98]. Thus, the angle between the Fab regions modulates the accessibility of the antigen, and perturbations introduced during modification can reduce affinity. The same considerations apply to the Fc (fragment crystallizable) region, but in the context of its effector properties, such as interactions with the immune system. These properties may be less important when obtaining fluorescently labeled or therapeutic antibody–drug conjugates, where the sole function of the antibody is targeted delivery.
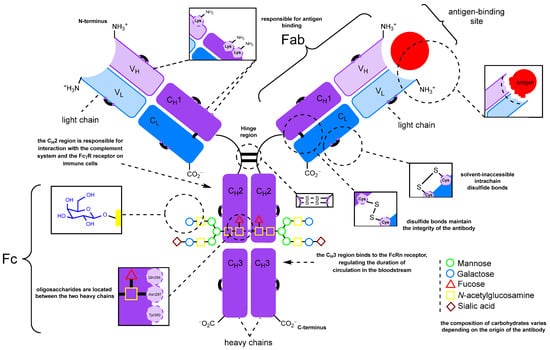
Figure 2.
The structure of immunoglobulin G and the sites available for modification.
Figure 2 also shows the functional groups present in native antibodies that are available for modification. These include N-glycans, side chains of lysine and other amino acids, and disulfide bonds. It is important to note that disulfide bonds can be further categorized into interchain bonds located in the hinge region, which are relatively accessible for modification, and intrachain bonds, of which there are 12 in all IgG subtypes, which are positioned on the surface of the antibody molecule [97,99]. The first FDA-approved ADC, Mylotarg, was synthesized by statistical modification of the lysine side chains. Subsequently, approaches to controlled modification using thiol groups generated by partial chemical reduction [100] of interchain disulfide bonds were developed (Figure 2) [101]. Cysteine labeling has become a widely adopted strategy, with numerous reviews devoted to its characteristics [99,102,103,104]. Notably, among the ADCs that have been reported or are currently in clinical trials, various antibody modification approaches have been explored, including those leveraging genetic engineering techniques [75].
Among the various bioorthogonal reactions available, those involving carbonyl groups are particularly intriguing for several reasons [105]. Carbonyl groups (aldehydes and ketones) (1) are not found in major classes of biopolymers such as proteins, nucleic acids, and polysaccharides; (2) can be site-specifically introduced into biomolecules; and (3) are well suited for bioorthogonal modification reactions, including oxime ligation [106], hydrazone formation [106] or the Pictet–Spengler reaction [105]. Carbonyl groups (aliphatic, aromatic, and α-oxo aldehydes, as well as aliphatic and aryl-alkyl ketones) can be incorporated into immunoglobulin molecules using various methods. This review will focus on the preparation and application of site-specific antibody conjugates, whose synthesis involves the introduction of carbonyl groups into the antibody molecule and their subsequent modification by biorthogonal reactions.
2. Methods for Introducing Carbonyl Groups into Antibodies
There are currently a large number of methods for introducing a carbonyl group into an antibody molecule. Some of these methods have been known for a long time (e.g., periodate oxidation [77,78,107]) and were originally developed for other applications [108], but were later adapted for immunoglobulins and other glycosylated proteins [78]. Some approaches are relatively new (e.g., genetically engineered amino acid introduction [109]) and somewhat complicated. Many of the approaches can be used in conjunction with each other (e.g., glycoengineering methods combined with periodate oxidation), so their division into groups may be tentative. Nonetheless, we have chosen to categorize the approaches into two groups: firstly, the more general approaches that only exploit the natural modification capabilities of antibodies (Figure 3) and secondly, approaches that rely on genetic engineering to alter the structure of the antibody.
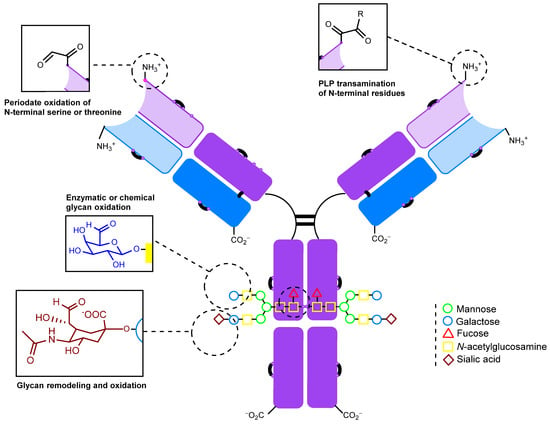
Figure 3.
Sites for modifications that do not require genetic engineering.
2.1. Introduction of the Carbonyl Group into Native Antibodies
2.1.1. Periodate Oxidation of Glycans
IgG molecules typically contain 2–3% carbohydrates by mass. These carbohydrates are present as a branched oligosaccharide chain, conservatively linked to the asparagine-297 residue (Asn297, N297, Figure 2) in the CH2 region of the Fc heavy chain of the immunoglobulin fragment [110]. The localization of carbohydrates on a serine or threonine residue of IgG is rare [111]. As a result, oligosaccharides are consistently located at a significant distance from the antigen-binding center [112]. Numerous reviews have been devoted to the properties and functions of immunoglobulin glycans and their structure [110,111,113,114,115,116,117,118,119,120,121,122,123,124,125]. Hence, the oxidation of oligosaccharide fragments of antibodies to form carbonyl groups appears to be a promising method for initial modification, which can then be followed by the conjugation of the desired molecule [112,126].
The carbohydrate composition is usually limited to fucose, mannose, galactose, N-acetylglucosamine, and sialic acid (Figure 4). The oligosaccharide structures and possible isoforms depend on the antibody producer and can be predicted [127,128]. For example, CHO cells produce antibodies with varying profiles of glycosylation [129,130,131]. However, obtaining antibodies with a homogeneous isoform of glycans in cellular expression systems is challenging. This is due to the various cellular processes, including the activity of enzymes such as glycosidases, glycosyltransferases, and others [111].
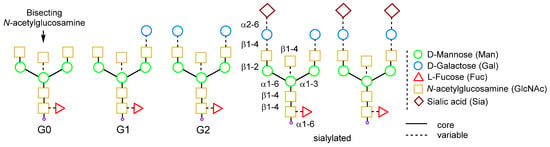
Figure 4.
Human IgG glycoforms [110].
For the oxidation of glycans, the reaction with sodium metaperiodate (NaIO4) is suitable [132]. This reaction has been known since 1928 and was originally developed by Léon Malaprade for the selective oxidation of vicinal alcohols [133] and β-amino alcohols [134].
In the case of glycans, the vicinal diols of sugars undergo oxidation, and cis-diols are oxidized much more readily than trans-diols. Thus, of the sugar residues listed above, only sialic acid, galactose, fucose, and, to a lesser extent, mannose residues can be oxidized. In some reports, mannose did not undergo oxidation under the most favorable conditions (10–20 mM) [135].
Periodate oxidation is influenced by many factors, including the concentration of the oxidant, pH, temperature, and reaction time [136]. Under mild conditions, oxidation may selectively target sialic acid residues, resulting in the generation of an aldehyde group at its exocyclic C-7 atom. Under more forcing conditions, it may affect other carbohydrate residues with vicinal diols, or undesirably oxidize sensitive amino acids such as tryptophan, tyrosine, and methionine [107] (Figure 5).
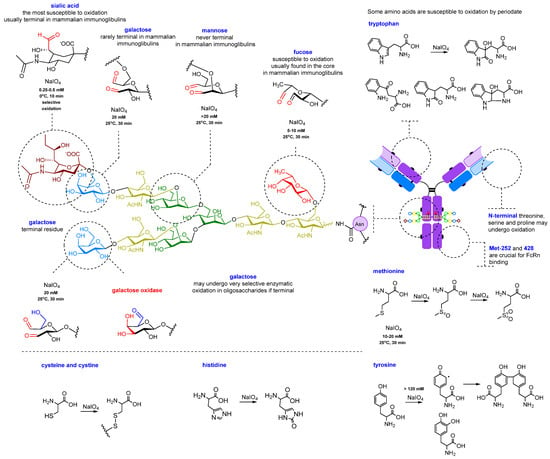
Figure 5.
Glycan oxidation and possible side reactions.
The optimal conditions for selectively oxidizing oligosaccharides alone involve running an oxidation for 30 min with a NaIO4 concentration of 5–20 mM at a temperature of 25 °C in an acetate buffer with a pH of 5–5.5 [135,137,138] (Figure 6). These conditions can be adjusted to achieve a specific level of carbonyl group introduction via the oxidation of other sugar moieties [136,139,140]. Theoretically, a maximum of 24 to 28 aldehyde groups can be generated per antibody through glycan oxidation (Figure 5). However, due to steric factors and side reactions, not all of these groups can be further modified; for instance, hydrazides form cyclic adducts with two neighboring aldehyde groups instead of two individual hydrazones, which reduces the degree of modification. As a result, the degree of labeling usually varies from 2 to 10 molecules per antibody [139].
At high concentrations of periodate (>50 mM), dimers can readily form and there is a possibility of oligomer formation, especially at higher temperatures and more alkaline pH values. This is primarily due to the reaction of aldehyde groups with ε-amino groups of lysine, resulting in the formation of Schiff bases which is favored under basic conditions. In addition, the polymerization of antibodies via the Schiff bases formation can be observed [136,139,141]. If amino acids in the antigen-binding site are involved in dimer formation, this can lead to a significant loss of affinity [139]. Additionally, at concentrations of sodium periodate above 100 mM, a process called overoxidation can occur, in which oligosaccharides are degraded and detached from the antibody [107]. Since one of the functions of oligosaccharides is to increase the solubility of immunoglobulins, antibodies may aggregate after the loss of oligosaccharide chains [139,142,143].
At periodate concentrations above 50 mM, sensitive amino acids also undergo destructive processes, resulting in decreased affinity and an overall loss of immunoglobulin stability [107,135,136,142,144,145,146,147,148,149,150,151,152,153]. It should be noted that some antibodies are more sensitive to oxidation and lose their ability to bind very easily even at low concentrations of sodium periodate (5–10 mM) [136]. This is due to the location of oxidation-sensitive amino acids in the antigen-binding site. For such antibodies, even milder oxidation conditions should be selected, such as less than 0.5 mM sodium periodate, cooling to 0 °C and shorter incubation times [136]. Prolonged incubation can almost completely abolish the affinity [142].
It is important to note that selective oxidation of sialic acid residues with periodate uses much lower concentrations of periodate (0.25–0.5 mM) than conventional oxidation of oligosaccharides [107,136]. These conditions are the most suitable for sensitive amino acids. Oxidation of methionine residues [143,150], including residues Met-252 and Met-428 located on the Fc region of CH3 close to the binding site of the neonatal receptor FcRn (the neonatal fragment crystallizable (Fc) receptor) [154], can affect the efficiency of binding to the latter [143]. This receptor is responsible for the recirculation of the antibody from lysosomes back to the intercellular space, as in the case of nonspecific pinocytosis, and a decrease in the interaction with it significantly reduces the lifetime of the immunoglobulin in the blood [154].
This process occurs in the following way: after nonspecific capture by the cell, the antibody enters the acidic lysosome, where it binds to the neonatal receptor at pH below 6. Subsequently, it is released intact into the intercellular space. There, when the pH is raised to neutral values of about 7.4, the antibody is released from the receptor due to the lack of binding. Importantly, in the process, the antibody is protected from enzymatic degradation in the lysosome by binding to FcRn [154].
Partial oxidation (~40%) of the Met-252 residue has little effect on FcRn, causing a 25% decrease in binding. However, a 60% reduction in binding of the antibody to FcRn results in an 80% reduction in immunoglobulin circulation time. It should be noted that the risk of methionine oxidation increases at acidic pH values. At neutral pH values, the oxidation of Met, Tyr, and Trp is almost nonexistent. Thus, performing the oxidation at a pH of 5.0–5.5 represents a compromise between avoiding the undesired amino acid oxidation and preventing the Schiff base formation [107,137].
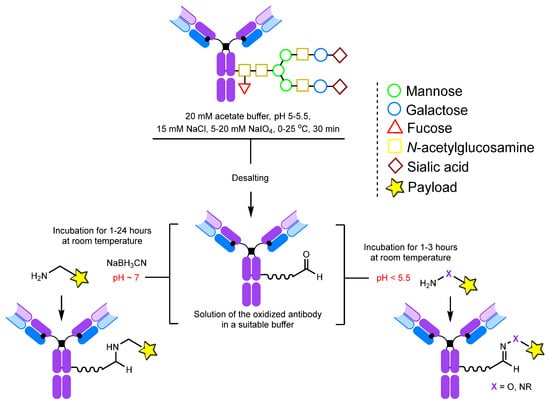
Figure 6.
Conditions for periodate oxidation of glycans and further modification [139,155].
Temperature also greatly affects the oxidation process, but temperature conditions should be selected individually for each antibody. Most sources mention either oxidation at room temperature or cooling to 0–4 °C [136,137,139,142,156].
It should be noted that for some applications, such as affinity chromatography, periodate oxidation is an excellent solution. This is because the immobilization of the antibody on solid support using oxidized Fc fragment oligosaccharides occurs with the correct orientation of the antibody, making the antigen-binding sites accessible to the target. In the case of immobilization using lysine or cysteine residues, however, the orientation of the antibodies is statistical, rendering some antigen-binding sites inaccessible and leading to a reduction in the overall binding efficiency [156,157,158,159].
Despite the fact that glycan modification affects the effector properties of antibodies, in in vivo tests in mice, 125I-tyrosine-labeled radioactive immunoglobulins demonstrated greater efficiency and affinity compared to conjugates that were statistically labeled using lysine or tyrosine residues. While the latter underwent intensive dehalogenation by liver enzymes and subsequent excretion, the glycan-labeled conjugates remained more than 80% intact. This effect is thought to be due to the localization of the glycans in the recess between the two heavy chains of the antibodies, making them inaccessible to enzymes. Similar positive results were obtained for 111In-labeled conjugates [112].
2.1.2. Transamination
Transamination reactions can be used to introduce a carbonyl group at the N-terminus of an antibody of any origin. The reaction involves pyridoxal-5-phosphate (PLP) at 37–50 °C in an aqueous solution (Figure 7) [160,161]. The advantage of this method is its selectivity: it introduces the carbonyl group at the N-terminus without affecting the antigen-binding site. However, a significant disadvantage is that different N-terminal amino acid residues have varying reactivity in the oxidation by pyridoxal-5-phosphate and subsequent modification [162]. For example, alanine, glycine, aspartic acid, glutamic acid, and asparagine form carbonyl products that are easily functionalized by oxime ligation, while the most common N-terminal amino acid, glutamine, is oxidized to a keto derivative that is unreactive toward oxyamines. In addition, some amino acids form adducts with pyridoxal (Figure 8A) [162]. Other disadvantages of this method are the limited number of modification sites (one site per chain, four sites for the whole antibody) and, consequently, a low payload-carrying capacity [160]. In addition, the transamination reaction works best at a temperature of 50 °C, which is undesirable when working with antibodies. Although these limitations hinder the widespread application of this method, it has been successfully applied to create therapeutic drug-loaded Fc antibodies [161].
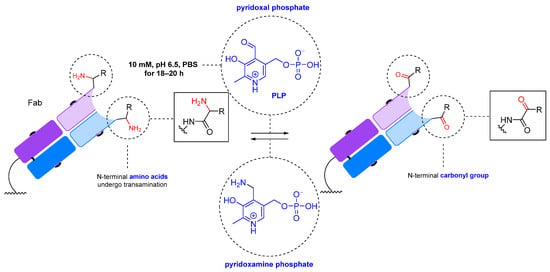
Figure 7.
PLP-mediated N-terminal transamination [160].
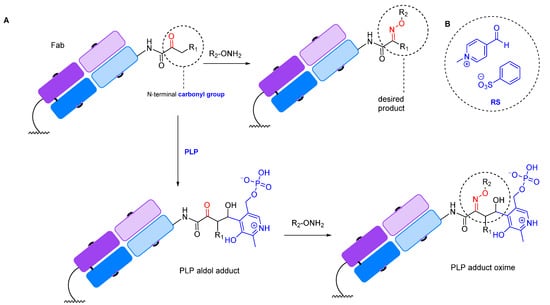
Figure 8.
(A) Some amino acids form adducts with pyridoxal phosphate [162]. (B) N-methylpyridinium-4-carboxaldehyde benzenesulfonate salt (Rapoport’s salt, RS) [163].
These difficulties can be overcome by genetic engineering methods, such as incorporating the desired amino acids at the N-terminus of the antibody. Additionally, there have been attempts to create analogs of pyridoxal phosphate that can effectively oxidize the amino acid residues that are unreactive toward pyridoxal. For the selective oxidation of antibodies with genetically engineered glutamine residues introduced at the N-terminus, a PLP analog with better efficacy has been developed: N-methylpyridinium-4-carboxaldehyde benzenesulfonate salt (Rapoport’s salt, RS, Figure 8B) [163].
2.1.3. Glycan Remodeling
This group of methods is based on the introduction of a carbonyl group into an antibody by enzymatic modification of the composition and structure of glycans without additional genetic engineering.
One such approach to glycan modification relies on the use of galactose oxidase (Figure 9 and Figure 10). The enzyme forms an aldehyde group at the C6 position of the terminal galactose or N-acetylgalactosamine. However, the method has a significant drawback: in mammalian glycoproteins, the terminal residue is often sialic acid, so additional treatment with neuraminidase is required to make the galactose residues available for modification [107].
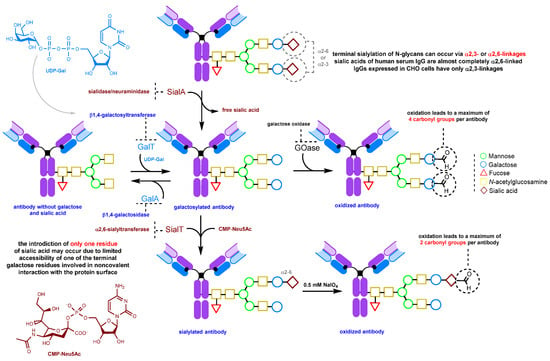
Figure 9.
Enzymatic glycan remodeling [107,125,143,152,164,165,166,167].
Alternatively, terminal sialic acid residues can be enzymatically introduced into the glycan, followed by their mild oxidation using sodium periodate (0.25–0.5 mM) to form carbonyl groups (Figure 9) [143,152]. For trastuzumab, at NaIO4 concentrations below 1 mM, there is no significant loss of binding (less than 15%) to the FcRn receptor due to methionine oxidation. However, at concentrations above 4 mM, a 40% loss of binding occurs due to the oxidation of methionine residues, in particular Met-252 [143].
This method is attractive due to very mild oxidation conditions, requiring less than 0.5 mM of sodium periodate for selective sialic acid oxidation. Under these conditions, there is virtually no undesirable oxidation of amino acids, especially methionine, the integrity of which is important for the long circulation time of the antibody. Antibodies oxidized under mild conditions retain their stability and are not prone to aggregation. For trastuzumab, aggregation was observed under harsher conditions (7.5 mM NaIO4) [143]. If the Fc glycan lacks terminal sialic acid residues and is galactose- and fucose-poor, this method can be used to produce conjugates with good homogeneity [143,152].
2.1.4. Glycoengineering Using Mutant Glycosyltransferases
Engineering of Fc glycosylation is a rational strategy to improve the safety and efficacy of therapeutic IgG antibodies. As mentioned above, glycans significantly influence the effector properties of the antibody, such as ADCC (antibody-dependent cellular cytotoxicity) and CDC (complement-dependent cellular cytotoxicity) [155,168]. Thus, by manipulating glycans, one can induce changes in these properties. In addition to the periodate oxidation of glycans and remodeling using natural enzymes, there are also various post-translational modification methods that employ mutant enzymes, like mutant β1,4-galactosyltransferase [169] and endoglycosidase Endo-S (endo-β-N-acetylglucosaminidase from Streptococcus pyogenes) [152]. These enzymes allow either the modification of the glycan structure followed by periodate oxidation [152], or the introduction of non-natural sugars bearing the target functional group into glycans. While there is a wide range of such groups available, this review will focus only on approaches related to the introduction of carbonyl groups [169].
One such approach is to introduce C2-keto-galactose into the antibody using a mutant β1,4-galactosyltransferase (Figure 10). This method allows for the introduction of a larger number of payload molecules, approximately 4, compared to 1.6 using the sialic acid residue introduction method described above [169].
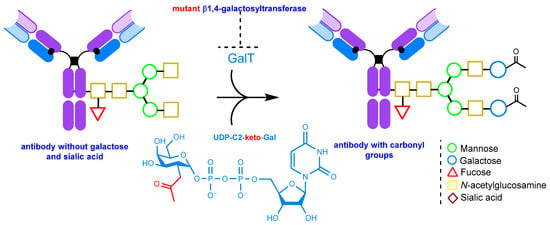
Figure 10.
The introduction of C2-keto-galactose into the glycan chain [152,169].
An alternative method involves the chemoenzymatic synthesis of glycoengineered IgGs, including glycosite-specific antibody–drug conjugates (gsADCs), by almost complete reconstruction of the glycans [152,170,171,172]. This is achieved using the mutant Endo-S D233Q glycosynthase enzyme and pre-synthesized non-natural N-glycan oxazolines serving as substrates. Carbonyl groups can also be introduced via periodate oxidation for subsequent oxime ligation [170]. For a detailed account of N-glycan oxazoline synthesis, please refer to the review [173].
This method uses the hydrolytic activity of the wild-type (WT) endoglycosidase Endo-S to cleave N-glycans from native immunoglobulins [174]. This step is crucial because, as mentioned above, natural IgGs have heterogeneous glycosylation and many glycan isoforms. After this enzymatic process, a single GlcNAc (N-acetylglucosamine) is left on the antibody (Figure 11) If defucosylation is required, fucosidase AlfC from Lactobacillus casei [175] can be added during the deglycosylation step. Next, another enzyme, mutant endoglycosidase (also known as glycosynthase), with high transglycosylation capacity but no hydrolytic activity, is used to attach the pre-synthesized N-glycan oxazoline bearing the requisite functional group (in the context of this review, the carbonyl group or its precursor) to the GlcNAc residue. Notably, this entire enzymatic procedure can be performed in one pot [170].
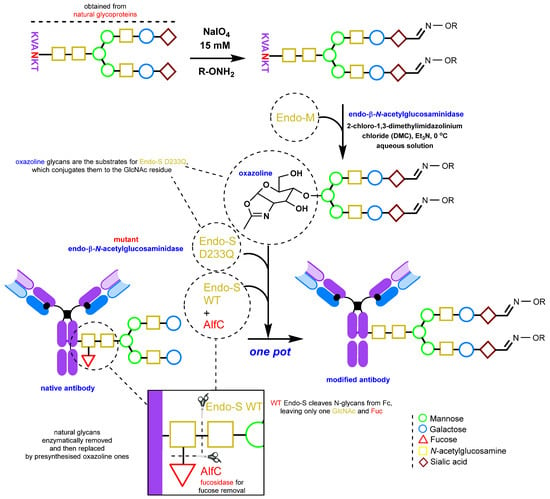
Figure 11.
Enzymatic engineering of glycans [152,169,170,171,176].
Endo-β-N-acetylglucosaminidase from Streptococcus pyogenes (Endo-S) is an endoglycosidase enzyme [174,175,177,178,179,180,181] that recognizes the N-glycans of IgG and has long been used for glycan remodeling of therapeutic antibodies. It accepts a wide range of glycans as substrates. Currently, a large number of mutant variants of the enzyme have been developed that allow mannose-rich and complex glycans to be attached to antibodies. Endo-S2 [171,172] or Endo-S D233Q [170] are two examples of such variants. The method of glycan engineering using mutant glucosaminidase has been the subject of numerous reviews and studies [115,182,183,184,185].
The mutant Endo-S D233Q uses oxazoline glycan derivatives as substrates (Figure 11). These derivatives can be obtained in a one-pot reaction from natural glycopeptides, such as egg yolk sialylglycopeptide (SGP), by using Endo m endoglycosidase from Mucor hiemalis. Following enzymatic glycan cleavage, oxazoline formation proceeds in an aqueous solution in the presence of 2-chloro-1,3-dimethylimidazolinium chloride (DMC) [170].
Incorporation of a carbonyl group into the free glycans can be accomplished by periodate oxidation using 15 mM NaIO4 in a phosphate buffer at pH 7. The subsequent oxime ligation must be performed before oxazoline synthesis [170]. Glycan oxidation and oxime ligation can be carried out in the same manner after glycan conjugation to the antibody, but with a lower concentration of periodate [176].
2.2. Introduction of Carbonyl Groups with Genetic Engineering Tools
2.2.1. Introduction of a Natural Amino Acid as a Precursor of the Carbonyl Group
The production of recombinant monoclonal antibodies [186] is a well-established process [187,188] that has been extensively described in a number of reviews [188,189,190,191,192]. There are additional thorough reviews on bispecific antibodies [193,194,195], nanobodies [196,197], bi-, tri- and tetrabodies [198], and other derivatives [199,200]. This review will not cover these subjects. However, the production of recombinant monoclonal antibodies presents an opportunity to edit the amino acid sequence [201] and insert reactive natural amino acid residues into regions of interest [202,203] within the antibody to allow for further modification (Figure 12).
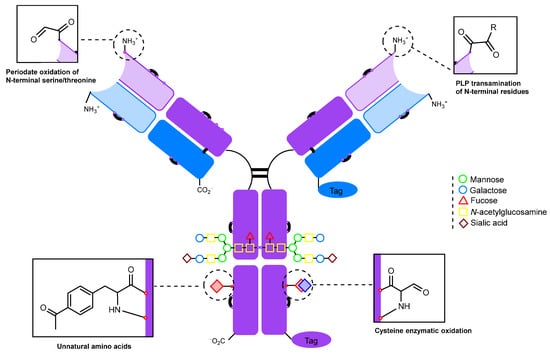
Figure 12.
Potential modification sites of a genetically engineered antibody.
There are two main approaches to amino acid insertion:
- Inserting an amino acid residue of interest outside the complementarity-determining region (CDR) near the N-terminus [204].
- Placing an amino acid residue of interest into the Fc region or Fab region, far from the antigen-binding site [203]. Subsequent to this step, enzymatic or chemical conjugation can be performed.
Commonly inserted amino acids include serine, threonine, proline, selenocysteine [205], and cysteine. The introduction of cysteine residues, in particular, has gained popularity, often referred to under the trademark “THIOMAB” by Genentech [101]. This technology has been used in the development of FDA-approved antibody–drug conjugates such as “Polivy” (polatuzumab vedotin) [206] and the first-in-class antibacterial ADC for targeting Staphilococcus aureus, DSTA4637S [207], which is currently in clinical trials [208,209,210].
The engineered THIOMAB antibody can be modified with a bifunctional maleimide-carbonyl-containing linker, which introduces a carbonyl group to the antibody for subsequent modification (Figure 13) [211]. In this case, the carbonyl group serves as one of the two reactive handles for the synthesis of a dual-drug antibody–drug conjugate [212].
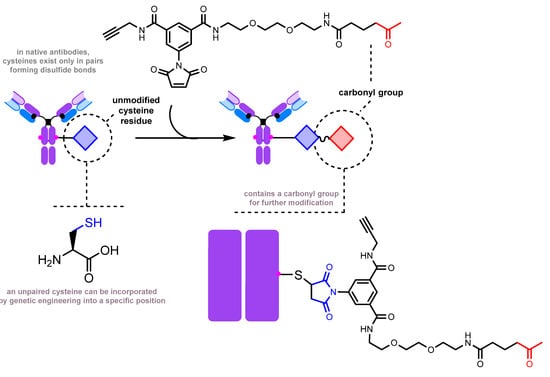
Figure 13.
Ketone group introduction by thiol-maleimide chemistry [211].
Another strategy involves the enzymatic conversion of cysteine residues to formylglycine (Figure 14). It has been employed for modifying antibodies [213,214,215] and Fc fragments [216].
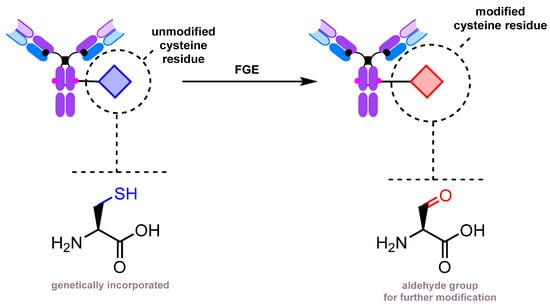
Figure 14.
Enzymatic oxidation of cysteine to formylglycine [213,214].
An interesting example of the vast possibilities of genetic engineering is an approach to glycan remodeling using the mutant Endo-S D233Q and a genetically engineered antibody containing a carbonyl group (Figure 15). The carbonyl group is introduced by enzymatic oxidation by first genetically encoding a cysteine residue in place of N297 and then converting it to formylglycine using FGE (formylglycine-generating enzyme), as described previously [217]. The formylglycine residue is further conjugated with an oxyamino GlcNAc derivative. The Endo-S-mediated conjugation with an N-glycan oxazoline completes the assembly process.
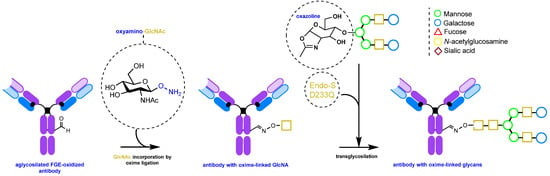
Figure 15.
De novo glycan assembly on an aglycosylated antibody [217].
The N-terminal serine and threonine can be selectively oxidized with sodium periodate to form carbonyl compounds [204] (Figure 16). It should be noted that the rate of oxidation of α-amino alcohols and N-terminal amino acids with an OH group in the side chain is significantly higher (approximately 102–104 times) than the rate of oxidation of diols in sugars [218]. However, the rate of oxidation of amino alcohols is highly dependent on pH values. Under acidic conditions, the oxidation of amino sugars is almost completely suppressed due to the protonation of the amino group. In addition, as mentioned previously, at acidic pH valuesl, there is risk of methionine oxidation, while at neutral pH values, the oxidation of Met, Tyr, and Trp is virtually absent [136]. This makes it possible to selectively oxidize N-terminal residues under neutral conditions. In particular, periodate oxidation of the N-terminal serine of the IgG light chain followed by oxime ligation was used to synthesize a highly homogeneous antibody–drug conjugate with a DAR (drug-to-antibody ratio) of 2 [204].
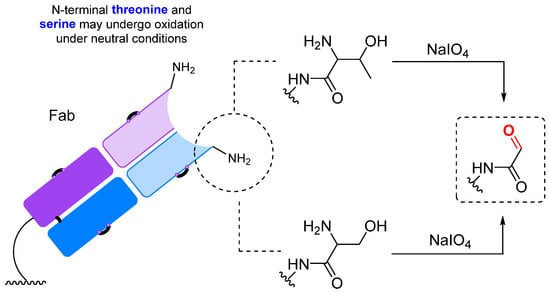
Figure 16.
Periodate oxidation of N-terminal residues [204].
2.2.2. Introduction of a Protein Tag for Subsequent Carbonyl Group Insertion
The method of genetically engineered introduction of an amino acid sequence recognized by a specific enzyme—a tag—has found widespread application [219]. In particular, there are reports on the introduction of a carbonyl group into the antibody using an enzyme tag [220,221].
The approach is based on the introduction of a flexible oligoglycine spacer (G7) and a specific CaaX (Cys-Val-Ile-Met) motif, which is recognized by farnesyltransferase (FTase, EC 2.5.1.58), into the C-terminus of the light chain of the antibody by genetic engineering. This motif is then used to attach geranyl ketone pyrophosphate to the antibody (Figure 17) [220,221]. This method is highly site-specific because prenylation occurs at the exact site recognized by the enzyme. It allows the introduction of two carbonyl-containing fragments into a single antibody molecule. The modification process does not adversely affect the properties of the antibody, and the modification site is located far from the antigen binding site, ensuring that there is no reduction in affinity. In addition, a different geranyl pyrophosphate analog bearing an aromatic aldehyde group was used to introduce a single modification into a DARPin (designed ankyrin repeat protein) for further conjugation with a fluorophore or a drug [222].
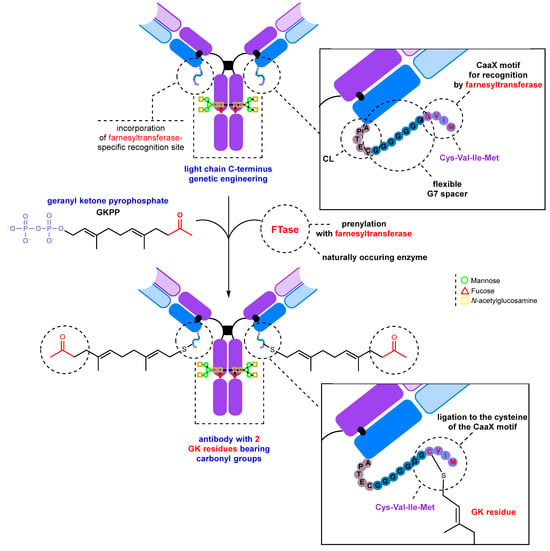
Figure 17.
Introduction of a ketone group into the antibody using farnesyltransferase (FTase) [220,221].
An unconventional approach for the site-specific introduction of an aldehyde group into nanobodies is based on the use of an oligohistidine tag [223]. The conjugation of a diol, which serves as a precursor for aldehyde generation, with a lysine residue is performed by reductive amination. The diol also carries a chelating moiety that, in the presence of Cu2+ ions, comes into close proximity with the histidine tag through complex formation, making the conjugation site-specific. In the next step, the diol is cleaved by 1 mM NaIO4, which simultaneously removes the reaction-directing metal-chelating moiety from the conjugate and generates an aldehyde group that can be used for conjugation to a dye or drug by either hydrazone formation or oxime ligation.
2.2.3. UAAs Containing Carbonyl Groups
A more complex method of introducing a carbonyl group into the antibody involves the use of unnatural amino acids (UAAs) [109]. These UAAs, which contain a carbonyl group, can be incorporated into the antibody at specific positions using genetic engineering [224]. There are two primary approaches to obtaining such genetically engineered antibodies: a cell-based method (Figure 18) and a cell-free method. A number of reviews are devoted to a detailed consideration of the characteristics of the methods [225,226]. In this review, we will only briefly discuss the cell-based method, as it is more commonly used and better developed in practice.
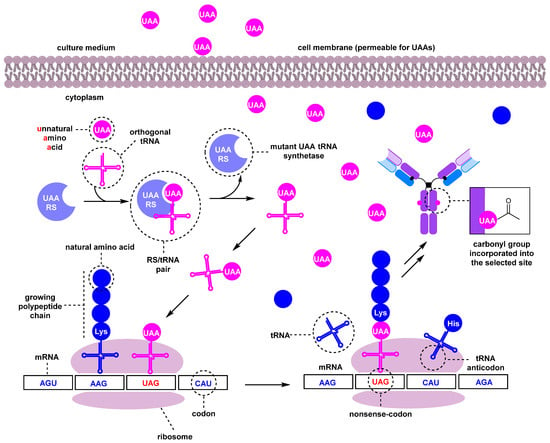
Figure 18.
A simplified scheme of the cell-based UAA incorporation into antibodies [109,225,227].
The incorporation process begins with the recognition of an mRNA codon by a tRNA anticodon in the ribosome. The UAA is typically encoded by a nonsense codon in the mRNA, commonly UAG (amber); the codon choice depends on the host cells [228]. A specialized, orthogonal tRNA charged with the unnatural amino acid is capable of recognizing this codon and incorporating the UAA into the growing polypeptide chain. A mutant tRNA synthetase (RS) selectively acylates only the corresponding orthogonal tRNA with the unnatural amino acid. The selectivity of the tRNA/RS pair must be very high. Mutant RS/tRNA and antibody genes are introduced into E. coli cells with plasmids or into mammalian cells with vectors [225,227,229,230,231]. It is important that the amino acid containing the carbonyl group can cross the cell membrane and accumulate in the cytosol when added to the culture medium. Para-acetyl phenylalanine (pAcF) has been used to introduce the ketone group into antibodies [232], and a number of other carbonyl-bearing amino acids for incorporation into proteins have been reported [233,234,235,236,237] (Figure 19).
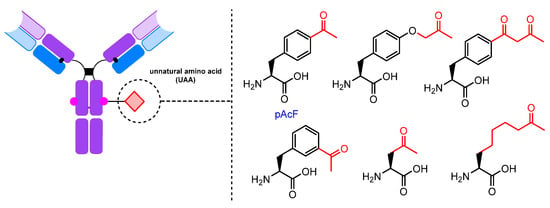
Figure 19.
Carbonyl-containing UAAs.
For example, a mutant anti-Her2 (human epidermal growth factor receptor 2) immunoglobulin containing pAcF was obtained in E. coli with the amber nonsense codon TAG using an orthogonal suppressor aminoacyl-tRNA synthetase/tRNA pair derived from Methanococcus jannaschii [228,232,238,239,240,241,242,243]. This approach has also been employed to generate bispecific antibodies targeting both HER2 and CD30 (TNFRSF8, tumor necrosis factor receptor superfamily member 8) [244], as well as Fab antibody fragments [240,242] and nanobodies [245] bearing a carbonyl group suitable for conjugation.
3. Conjugates: Modification of the Carbonyl Group
The presence of a carbonyl group in the antibody offers several possibilities for modification (Figure 20), including oxime and hydrazone formation [232], the Pictet–Spengler [246] and hydrazino–iso–Pictet–Spengler (HIPS) reactions [214], and the Knoevenagel condensation–Michael addition [247,248]. Several reviews are devoted to the modification of carbonyl-containing proteins and peptides [105,249,250,251].
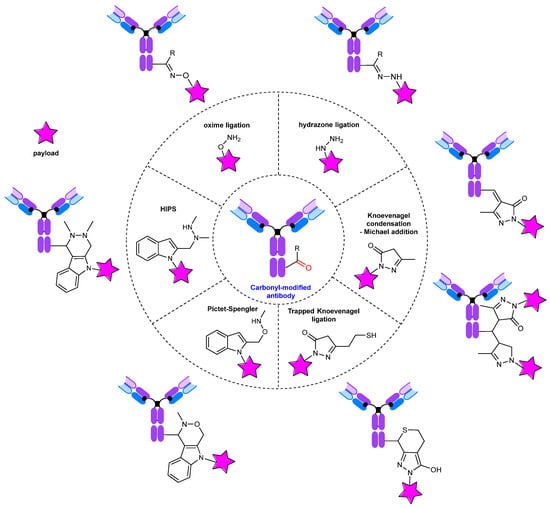
Figure 20.
Modification of carbonyl-containing antibodies.
Oxime ligation is considered to be an effective and reliable approach for protein modification [252]. In an extensive review published in 2017 [106], several aspects of the application of oxime ligation for bioconjugation, particularly those related to mechanism and catalysis, were thoroughly examined.
The most straightforward technique for modifying immunoglobulins via oxime ligation involves conjugation using a long hydrophilic oxyamine linker (Figure 21). This linker can carry functional groups, such as azide [170,244,253,254], cyclooctyne [170,254], alkyne [170], or oxyamine [231], for further biorthogonal modification.
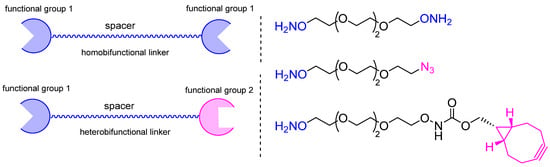
Figure 21.
Examples of bifunctional linkers for oxime ligation.
An alternative approach involves directly conjugating the target molecule with the antibody in one step, eliminating the need for additional procedures (Figure 22).
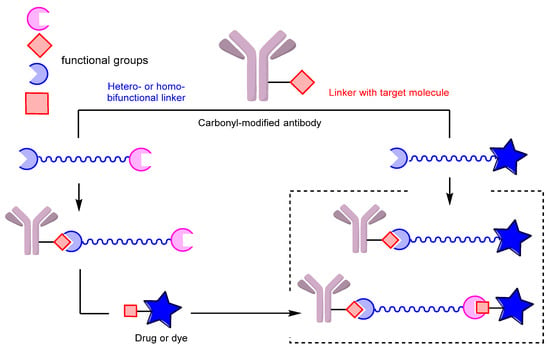
Figure 22.
Two approaches to linker-based conjugation of carbonyl-modified antibodies; left: sequential assembly, right: one-step ligation.
Antibody conjugates with dyes [137,216,232,254,255], cytotoxic drugs such as auristatins [169,221,241,243,256,257] and pyrrolobenzodiazepines [220], folic acid [258], PSMA (prostate-specific membrane antigen) ligands [242], and LXR (liver X receptor) agonists [259] have been generated using this approach. In addition, numerous antibody conjugates with oligonucleotides have been developed, demonstrating the versatility of this method [238,239,240,260] (Figure 23).
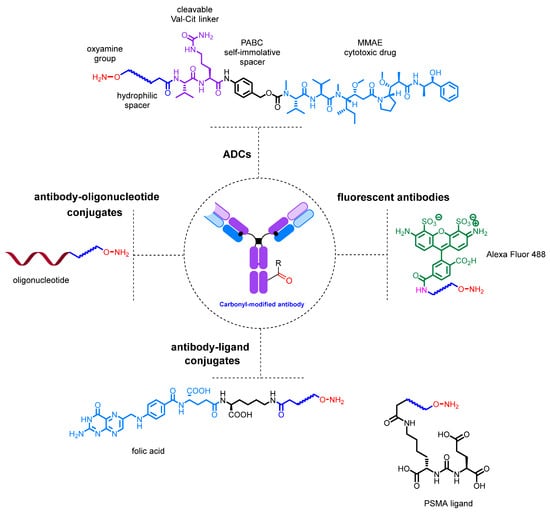
Figure 23.
Examples of conjugates obtained by single-step conjugation.
4. Conclusions
The introduction of a carbonyl group into an antibody is an established method for the production of antibody conjugates. There are a wide variety of approaches, ranging from simple chemical oxidation to the incorporation of noncanonical amino acids requiring specialized expression platforms (Figure 24).

Figure 24.
Methods for introducing carbonyl groups into antibodies and the relationships between them.
Periodate oxidation is the oldest and, arguably, the most versatile method for generating reactive aldehyde moieties from either glycans, synthetic diols or N-terminal amino acids. Although many side reactions, including antibody oligomerization and undesired amino acid oxidation, are possible, they can be limited by careful control of reaction conditions. As a result, NaIO4 remains a suitable reagent choice, especially when combined with modern antibody modification methods for milder oxidation conditions and product homogeneity. Another chemical oxidation method, transamination mediated by PLP and related reagents, despite some drawbacks, represents a convenient strategy provided that the N-terminal residues can be cleanly converted to α-oxo aldehyde moieties. That being said, the N-terminal regions of any antibody can be engineered using standard procedures, so residues suitable for transamination can be introduced, rendering the approach general, albeit, not perfect, as complete homogeneity of the conjugate is hard to achieve due to side reactions.
Enzymatic modification of N-glycans in the Fc fragment can range from simple manipulation of terminal sugar residues using conventional enzymes to radical rebuilding of the entire glycan core using specially designed mutant enzymes with the purpose of introducing new functionality. The complexity of the methods increases with the depth of the oligosaccharide modification, but, in all cases, the exceptional chemoselectivity of the enzymatic reactions allows for the generation of highly homogeneous products. Complete reengineering of the Fc glycan has the added benefit of tailoring antibody effector properties. This can play a role in enhancing the efficacy of glycosite-specific antibody–drug conjugates with ADCC and CDC.
Genetic engineering offers vast possibilities for antibody modification in general and the introduction of reactive carbonyl groups in particular. The more conventional approaches involve the introduction of unpaired cysteines (the THIOMAB technology), which are further converted to formylglycine residues, and the addition of a protein tag for enzymatic or affinity-guided conjugation. A much more laborious but elegant strategy is based on the introduction of unnatural amino acids containing a keto group. Upon further modification of the carbonyl group, all of these methods give rise to site-specific, homogeneous antibody conjugates.
It is important to note that there are links between many of these methods. For instance, enzymatic glycan modification is often followed by periodate oxidation, while glycan remodeling itself may rely on antibody sequence engineering. In another example, engineering the N-terminus can assist in transamination or allow selective periodate oxidation when serine or threonine are introduced.
In recent years, numerous approaches to the introduction of reactive carbonyl groups into antibodies and their derivatives have been proposed. We expect this trend to continue, as carbonyl-based conjugations, particularly hydrazone formation and especially oxime ligation, represent an important tool in the toolbox of biorthogonal reactions. Rivaling the extremely well-developed azide–alkyne cycloadditions in terms of selectivity and reaction rate, oxime ligation is continuously being used to generate antibody conjugates, in particular, ADCs.
In a global sense, antibody–drug conjugate technologies are currently focused on obtaining conjugates that are as site-specific and homogeneous as possible. Equally important is the stability of the conjugate in the bloodstream, which includes the reliability of conjugation of the linker with the cytotoxic agent to the antibody as well as the stability of the linker in the plasma. The homogeneity and site-specificity of the ADC, as well as its stability in plasma, significantly improve its pharmacodynamic properties, efficacy, and reduce the severity of side effects.
It appears that the most effective approach involves incorporating a bioorthogonal functional group into antibodies through the use of natural and genetically engineered amino acids. This approach is well established for antibody conjugates produced by the THIOMAB technology, which consists of introducing an additional unpaired cysteine into the antibody that is suitable for further modification, including the generation of a carbonyl group by FGE. One of the conjugates produced using this technology, Polivy, has already been approved by the FDA for use in patients. Several others, including an antibacterial conjugate, are in clinical trials.
The introduction of unnatural amino acids with a carbonyl group, such as para-acetylphenylalanine, is also a promising approach. However, unlike the introduction of natural amino acids into the antibody sequence, the introduction of unnatural amino acids with biorthogonal functional groups is a very labor-intensive task: it requires obtaining a mutant tRNA/RS pair, which is not trivial in itself, and overcoming difficulties with antibody production in cell culture. This makes the process expensive and makes it difficult to apply the method to the production of conjugates on an industrial scale. Nevertheless, a total of three ADCs currently in clinical trials (ARX788 [261], ARX517 [262], and AGS62P1 [256] are produced by this method with pAcF introduction followed by oxime ligation with an oxyamine-containing auristatin-based payload.
We believe that genetically engineered antibodies will come to the fore in the future as the technology of their production develops. The advantages of the method, in addition to those mentioned above, include the convenience of the conjugation procedure, reproducibility, and the ability to introduce the amino acid residue strictly at the required position on the antibody, since the conjugation site also has a significant influence on the properties of the final conjugate. The use of genetically engineered amino acids is probably the only conjugation method currently available that allows one to choose the site on the antibody where the cytotoxic drug molecule will be introduced.
Another interesting method worth mentioning is glycan remodeling, also known as GlycoConnect. The advantages of this method include the ability to edit glycans of any off-the-shelf antibody. Glycans are known to play an important role in the interaction of antibodies with the immune system, as well as influencing the circulation time of the antibody in the bloodstream. The ability to model antibody glycans and thus modify the properties of the conjugate seems promising. In addition, the method is site-specific since the modification of the antibody is performed strictly on glycans and allows to obtain homogeneous conjugates with a strictly defined loading. Several such conjugates, such as ADCT-601 [263], are currently in clinical trials.
The antibody–drug conjugates currently used in patients are mostly older-generation drugs that were introduced into clinical trials many years ago. In recent years, ADCs based on outdated technologies, particularly statistical labeling of lysines and cysteines, have also entered the market. We expect that the ADC market will continue to be supplied with technologically obsolete examples of therapeutic antibody conjugates for some time to come, as it takes at least ten years from conjugate development to clinical testing and approval. In the future, we expect a number of new site-specific and homogeneous conjugates to enter the market with improved properties and less severe side effects, including those produced by carbonyl-based conjugation.
Author Contributions
Conceptualization, V.A.K. and K.A.S.; methodology, V.A.K. and K.A.S.; writing—original draft preparation, E.L.G., V.A.K. and K.A.S.; writing—review and editing, E.L.G., V.A.A. and K.A.S.; visualization, K.A.S.; supervision, V.A.K.; project administration, V.A.A.; funding acquisition, V.A.K. All figures are original work by K.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
The research was supported by the Ministry of Science and Higher Education of the Russian Federation (Agreement No. 075-15-2021-1049).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Meares, C.F. Bioconjugate Chemistry. In Reference Module in Chemistry, Molecular Sciences and Chemical Engineering; Elsevier: Amsterdam, The Netherlands, 2014; p. B978012409547211087X. ISBN 978-0-12-409547-2. [Google Scholar] [CrossRef]
- Kalia, J.; Raines, R. Advances in Bioconjugation. Curr. Org. Chem. 2010, 14, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Narain, R. (Ed.) Chemistry of Bioconjugates: Synthesis, Characterization, and Biomedical Applications, 1st ed.; Wiley: Hoboken, NJ, USA, 2014; ISBN 978-1-118-35914-3. [Google Scholar] [CrossRef]
- Hermanson, G.T. Bioconjugate Techniques; Elsevier: Amsterdam, The Netherlands, 2013; ISBN 978-0-12-382239-0. [Google Scholar] [CrossRef]
- Algar, W.R.; Dawson, P.; Medintz, I.L. (Eds.) Chemoselective and Bioorthogonal Ligation Reactions; Wiley-VCH: Weinheim, Germany, 2017; Volume 2, ISBN 978-3-527-33436-0. [Google Scholar] [CrossRef]
- Prescher, J.A.; Bertozzi, C.R. Chemistry in Living Systems. Nat. Chem. Biol. 2005, 1, 13–21. [Google Scholar] [CrossRef]
- Best, M.D. Click Chemistry and Bioorthogonal Reactions: Unprecedented Selectivity in the Labeling of Biological Molecules. Biochemistry 2009, 48, 6571–6584. [Google Scholar] [CrossRef] [PubMed]
- Sletten, E.M.; Bertozzi, C.R. Bioorthogonal Chemistry: Fishing for Selectivity in a Sea of Functionality. Angew. Chem. Int. Ed. 2009, 48, 6974–6998. [Google Scholar] [CrossRef]
- Saxon, E.; Bertozzi, C.R. Cell Surface Engineering by a Modified Staudinger Reaction. Science 2000, 287, 2007–2010. [Google Scholar] [CrossRef] [PubMed]
- Prescher, J.A.; Dube, D.H.; Bertozzi, C.R. Chemical Remodelling of Cell Surfaces in Living Animals. Nature 2004, 430, 873–877. [Google Scholar] [CrossRef] [PubMed]
- Vocadlo, D.J.; Hang, H.C.; Kim, E.-J.; Hanover, J.A.; Bertozzi, C.R. A Chemical Approach for Identifying O -GlcNAc-Modified Proteins in Cells. Proc. Natl. Acad. Sci. USA 2003, 100, 9116–9121. [Google Scholar] [CrossRef]
- Hang, H.C.; Yu, C.; Pratt, M.R.; Bertozzi, C.R. Probing Glycosyltransferase Activities with the Staudinger Ligation. J. Am. Chem. Soc. 2004, 126, 6–7. [Google Scholar] [CrossRef]
- Zinn, S.; Vazquez-Lombardi, R.; Zimmermann, C.; Sapra, P.; Jermutus, L.; Christ, D. Advances in Antibody-Based Therapy in Oncology. Nat. Cancer. 2023, 4, 165–180. [Google Scholar] [CrossRef]
- Arlotta, K.J.; Owen, S.C. Antibody and Antibody Derivatives as Cancer Therapeutics. Wiley Interdiscipl. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1556. [Google Scholar] [CrossRef]
- Jin, B.; Odongo, S.; Radwanska, M.; Magez, S. Nanobodies: A Review of Generation, Diagnostics and Therapeutics. Int. J. Mol. Sci. 2023, 24, 5994. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Wang, Z.; Hao, M.; Li, J. Bispecific Antibodies and Their Applications. J. Hematol. Oncol. 2015, 8, 130. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.S.; Khalili, S.; Baradaran, B.; Bidar, N.; Shahbazi, M.-A.; Mosafer, J.; Hashemzaei, M.; Mokhtarzadeh, A.; Hamblin, M.R. Bispecific Monoclonal Antibodies for Targeted Immunotherapy of Solid Tumors: Recent Advances and Clinical Trials. Int. J. Biol. Macromol. 2021, 167, 1030–1047. [Google Scholar] [CrossRef] [PubMed]
- Tetin, S.; Stroupe, S. Antibodies in Diagnostic Applications. Curr. Pharm. Biotechnol. 2004, 5, 9–16. [Google Scholar] [CrossRef]
- Zhang, X.; Soori, G.; Dobleman, T.J.; Xiao, G.G. The Application of Monoclonal Antibodies in Cancer Diagnosis. Expert Rev. Mol. Diagn. 2014, 14, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Dammes, N.; Peer, D. Monoclonal Antibody-Based Molecular Imaging Strategies and Theranostic Opportunities. Theranostics 2020, 10, 938–955. [Google Scholar] [CrossRef]
- Scott, E.C.; Baines, A.C.; Gong, Y.; Moore, R.; Pamuk, G.E.; Saber, H.; Subedee, A.; Thompson, M.D.; Xiao, W.; Pazdur, R.; et al. Trends in the Approval of Cancer Therapies by the FDA in the Twenty-First Century. Nat. Rev. Drug Discov. 2023, 22, 625–640. [Google Scholar] [CrossRef]
- Waldmann, T.A. Monoclonal Antibodies in Diagnosis and Therapy. Science 1991, 252, 1657–1662. [Google Scholar] [CrossRef]
- Fu, Z.; Li, S.; Han, S.; Shi, C.; Zhang, Y. Antibody Drug Conjugate: The “Biological Missile” for Targeted Cancer Therapy. Sign. Transduct. Target Ther. 2022, 7, 93. [Google Scholar] [CrossRef]
- Dumontet, C.; Reichert, J.M.; Senter, P.D.; Lambert, J.M.; Beck, A. Antibody–Drug Conjugates Come of Age in Oncology. Nat. Rev. Drug Discov. 2023, 22, 641–661. [Google Scholar] [CrossRef]
- Gogia, P.; Ashraf, H.; Bhasin, S.; Xu, Y. Antibody–Drug Conjugates: A Review of Approved Drugs and Their Clinical Level of Evidence. Cancers 2023, 15, 3886. [Google Scholar] [CrossRef]
- Ahmadi, S.E.; Shabannezhad, A.; Kahrizi, A.; Akbar, A.; Safdari, S.M.; Hoseinnezhad, T.; Zahedi, M.; Sadeghi, S.; Mojarrad, M.G.; Safa, M. Tissue Factor (Coagulation Factor III): A Potential Double-Edge Molecule to Be Targeted and Re-Targeted toward Cancer. Biomark. Res. 2023, 11, 60. [Google Scholar] [CrossRef]
- Breij, E.C.W.; De Goeij, B.E.C.G.; Verploegen, S.; Schuurhuis, D.H.; Amirkhosravi, A.; Francis, J.; Miller, V.B.; Houtkamp, M.; Bleeker, W.K.; Satijn, D.; et al. An Antibody–Drug Conjugate That Targets Tissue Factor Exhibits Potent Therapeutic Activity against a Broad Range of Solid Tumors. Cancer Res. 2014, 74, 1214–1226. [Google Scholar] [CrossRef]
- Arn, C.R.; Halla, K.J.; Gill, S. Tisotumab Vedotin Safety and Tolerability in Clinical Practice: Managing Adverse Events. J. Adv. Pract. Oncol. 2023, 14, 139–152. [Google Scholar] [CrossRef]
- Markham, A. Tisotumab Vedotin: First Approval. Drugs 2021, 81, 2141–2147. [Google Scholar] [CrossRef]
- Francisco, J.A.; Cerveny, C.G.; Meyer, D.L.; Mixan, B.J.; Klussman, K.; Chace, D.F.; Rejniak, S.X.; Gordon, K.A.; DeBlanc, R.; Toki, B.E.; et al. cAC10-vcMMAE, an Anti-CD30–Monomethyl Auristatin E Conjugate with Potent and Selective Antitumor Activity. Blood 2003, 102, 1458–1465. [Google Scholar] [CrossRef]
- Gualberto, A. Brentuximab Vedotin (SGN-35), an Antibody–Drug Conjugate for the Treatment of CD30-Positive Malignancies. Expert Opin. Investig. Drugs 2012, 21, 205–216. [Google Scholar] [CrossRef]
- Katz, J.; Janik, J.E.; Younes, A. Brentuximab Vedotin (SGN-35). Clin. Cancer Res. 2011, 17, 6428–6436. [Google Scholar] [CrossRef]
- DiJoseph, J.F.; Armellino, D.C.; Boghaert, E.R.; Khandke, K.; Dougher, M.M.; Sridharan, L.; Kunz, A.; Hamann, P.R.; Gorovits, B.; Udata, C.; et al. Antibody-Targeted Chemotherapy with CMC-544: A CD22-Targeted Immunoconjugate of Calicheamicin for the Treatment of B-Lymphoid Malignancies. Blood 2004, 103, 1807–1814. [Google Scholar] [CrossRef]
- Takeshita, A.; Yamakage, N.; Shinjo, K.; Ono, T.; Hirano, I.; Nakamura, S.; Shigeno, K.; Tobita, T.; Maekawa, M.; Kiyoi, H.; et al. CMC-544 (Inotuzumab Ozogamicin), an Anti-CD22 Immuno-Conjugate of Calicheamicin, Alters the Levels of Target Molecules of Malignant B-Cells. Leukemia 2009, 23, 1329–1336. [Google Scholar] [CrossRef]
- Li, X.; Zhou, M.; Qi, J.; Han, Y. Efficacy and Safety of Inotuzumab Ozogamicin (CMC-544) for the Treatment of Relapsed/Refractory Acute Lymphoblastic Leukemia and Non-Hodgkin Lymphoma: A Systematic Review and Meta-Analysis. Clin. Lymphoma Myeloma Leuk. 2021, 21, e227–e247. [Google Scholar] [CrossRef]
- Patel, K.C.; Hageman, K.; Cooper, M.R. Ado-Trastuzumab Emtansine for the Treatment of Human Epidermal Growth Factor Receptor 2-Positive Metastatic Breast Cancer. Am. J. Health Syst. Pharm. 2014, 71, 537–548. [Google Scholar] [CrossRef]
- Peddi, P.F.; Hurvitz, S.A. Ado-Trastuzumab Emtansine (T-DM1) in Human Epidermal Growth Factor Receptor 2 (HER2)-Positive Metastatic Breast Cancer: Latest Evidence and Clinical Potential. Ther. Adv. Med. Oncol. 2014, 6, 202–209. [Google Scholar] [CrossRef]
- Lewis Phillips, G.D.; Li, G.; Dugger, D.L.; Crocker, L.M.; Parsons, K.L.; Mai, E.; Blättler, W.A.; Lambert, J.M.; Chari, R.V.J.; Lutz, R.J.; et al. Targeting HER2-Positive Breast Cancer with Trastuzumab-DM1, an Antibody–Cytotoxic Drug Conjugate. Cancer Res. 2008, 68, 9280–9290. [Google Scholar] [CrossRef]
- Stadtmauer, E.A. Gemtuzumab Ozogamicin in the Treatment of Acute Myeloid Leukemia. Curr. Oncol. Rep. 2002, 4, 375–380. [Google Scholar] [CrossRef]
- Hosono, N.; Ookura, M.; Araie, H.; Morita, M.; Itoh, K.; Matsuda, Y.; Yamauchi, T. Clinical Outcomes of Gemtuzumab Ozogamicin for Relapsed Acute Myeloid Leukemia: Single-Institution Experience. Int. J. Hematol. 2021, 113, 362–369. [Google Scholar] [CrossRef]
- Yu, B.; Liu, D. Gemtuzumab Ozogamicin and Novel Antibody-Drug Conjugates in Clinical Trials for Acute Myeloid Leukemia. Biomark. Res. 2019, 7, 24. [Google Scholar] [CrossRef]
- Takeshita, A. Efficacy and Resistance of Gemtuzumab Ozogamicin for Acute Myeloid Leukemia. Int. J. Hematol. 2013, 97, 703–716. [Google Scholar] [CrossRef]
- Zaro, J.L. Mylotarg: Revisiting Its Clinical Potential Post-Withdrawal. In Antibody-Drug Conjugates; Wang, J., Shen, W.-C., Zaro, J.L., Eds.; AAPS Advances in the Pharmaceutical Sciences Series; Springer International Publishing: Cham, Switzerland, 2015; Volume 17, pp. 179–190. ISBN 978-3-319-13080-4. [Google Scholar] [CrossRef]
- Tennvall, J.; Fischer, M.; Bischof Delaloye, A.; Bombardieri, E.; Bodei, L.; Giammarile, F.; Lassmann, M.; Oyen, W.; Brans, B. EANM Procedure Guideline for Radio-Immunotherapy for B-Cell Lymphoma with 90Y-Radiolabelled Ibritumomab Tiuxetan (Zevalin). Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 616–622. [Google Scholar] [CrossRef]
- Rizzieri, D. Zevalin® (Ibritumomab Tiuxetan): After More than a Decade of Treatment Experience, What Have We Learned? Crit. Rev. Oncol. Hematol. 2016, 105, 5–17. [Google Scholar] [CrossRef]
- Marcus, R. Use of 90Y-Ibritumomab Tiuxetan in Non-Hodgkin’s Lymphoma. Semin. Oncol. 2005, 32, 36–43. [Google Scholar] [CrossRef]
- Witzig, T.E.; Gordon, L.I.; Cabanillas, F.; Czuczman, M.S.; Emmanouilides, C.; Joyce, R.; Pohlman, B.L.; Bartlett, N.L.; Wiseman, G.A.; Padre, N.; et al. Randomized Controlled Trial of Yttrium-90–Labeled Ibritumomab Tiuxetan Radioimmunotherapy versus Rituximab Immunotherapy for Patients with Relapsed or Refractory Low-Grade, Follicular, or Transformed B-Cell Non-Hodgkin’s Lymphoma. J. Clin. Oncol. 2002, 20, 2453–2463. [Google Scholar] [CrossRef]
- Hagenbeek, A. Radioimmunotherapy for NHL: Experience of 90Y-Ibritumomab Tiuxetan in Clinical Practice. Leuk. Lymphoma. 2003, 44, S37–S47. [Google Scholar] [CrossRef]
- Tilly, H.; Morschhauser, F.; Sehn, L.H.; Friedberg, J.W.; Trněný, M.; Sharman, J.P.; Herbaux, C.; Burke, J.M.; Matasar, M.; Rai, S.; et al. Polatuzumab Vedotin in Previously Untreated Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 2022, 386, 351–363. [Google Scholar] [CrossRef]
- Yip, V.; Lee, M.V.; Saad, O.M.; Ma, S.; Khojasteh, S.C.; Shen, B.-Q. Preclinical Characterization of the Distribution, Catabolism, and Elimination of a Polatuzumab Vedotin-Piiq (POLIVY®) Antibody–Drug Conjugate in Sprague Dawley Rats. J. Clin. Med. 2021, 10, 1323. [Google Scholar] [CrossRef]
- Cardillo, T.M.; Govindan, S.V.; Sharkey, R.M.; Trisal, P.; Arrojo, R.; Liu, D.; Rossi, E.A.; Chang, C.-H.; Goldenberg, D.M. Sacituzumab Govitecan (IMMU-132), an Anti-Trop-2/SN-38 Antibody–Drug Conjugate: Characterization and Efficacy in Pancreatic, Gastric, and Other Cancers. Bioconjug. Chem. 2015, 26, 919–931. [Google Scholar] [CrossRef]
- Weiss, J.; Glode, A.; Messersmith, W.A.; Diamond, J. Sacituzumab Govitecan: Breakthrough Targeted Therapy for Triple-Negative Breast Cancer. Expert Rev. Anticancer Ther. 2019, 19, 673–679. [Google Scholar] [CrossRef]
- Ocean, A.J.; Starodub, A.N.; Bardia, A.; Vahdat, L.T.; Isakoff, S.J.; Guarino, M.; Messersmith, W.A.; Picozzi, V.J.; Mayer, I.A.; Wegener, W.A.; et al. Sacituzumab Govitecan (IMMU-132), an anti-Trop-2-SN-38 Antibody-drug Conjugate for the Treatment of Diverse Epithelial Cancers: Safety and Pharmacokinetics. Cancer 2017, 123, 3843–3854. [Google Scholar] [CrossRef]
- Bardia, A.; Messersmith, W.A.; Kio, E.A.; Berlin, J.D.; Vahdat, L.; Masters, G.A.; Moroose, R.; Santin, A.D.; Kalinsky, K.; Picozzi, V.; et al. Sacituzumab Govitecan, a Trop-2-Directed Antibody-Drug Conjugate, for Patients with Epithelial Cancer: Final Safety and Efficacy Results from the Phase I/II IMMU-132-01 Basket Trial. Ann. Oncol. 2021, 32, 746–756. [Google Scholar] [CrossRef]
- Challita-Eid, P.M.; Satpayev, D.; Yang, P.; An, Z.; Morrison, K.; Shostak, Y.; Raitano, A.; Nadell, R.; Liu, W.; Lortie, D.R.; et al. Enfortumab Vedotin Antibody–Drug Conjugate Targeting Nectin-4 Is a Highly Potent Therapeutic Agent in Multiple Preclinical Cancer Models. Cancer Res. 2016, 76, 3003–3013. [Google Scholar] [CrossRef]
- McGregor, B.A.; Sonpavde, G. Enfortumab Vedotin, a Fully Human Monoclonal Antibody against Nectin 4 Conjugated to Monomethyl Auristatin E for Metastatic Urothelial Carcinoma. Expert Opin. Investig. Drugs 2019, 28, 821–826. [Google Scholar] [CrossRef]
- Maas, M.; Stühler, V.; Walz, S.; Stenzl, A.; Bedke, J. Enfortumab Vedotin–next Game-Changer in Urothelial Cancer. Expert Opin. Biol. Ther. 2021, 21, 801–809. [Google Scholar] [CrossRef]
- Spreen, L. Mirvetuximab Soravtansine-Gynx (ElahereTM). Oncol. Times 2023, 45, 6. [Google Scholar] [CrossRef]
- Parvez, S.; Prakash, K.; Soni, D. A Review on Chemistry, Mechanism, Clinical Trials Studies of ELAHERE (Mirvetuximab Soravtansine-Gynx): A Novel FDA Approved Drug to Treat Ovarian Cancer. World J. Pharm. Pharm. Sci. 2023, 12, 891–898. [Google Scholar] [CrossRef]
- Heo, Y.-A. Mirvetuximab Soravtansine: First Approval. Drugs 2023, 83, 265–273. [Google Scholar] [CrossRef]
- Nwabufo, C.K. Mirvetuximab Soravtansine in Ovarian Cancer Therapy: Expert Opinion on Pharmacological Considerations. Cancer Chemother. Pharmacol. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Yam, C.; Rauch, G.M.; Rahman, T.; Karuturi, M.; Ravenberg, E.; White, J.; Clayborn, A.; McCarthy, P.; Abouharb, S.; Lim, B.; et al. A Phase II Study of Mirvetuximab Soravtansine in Triple-Negative Breast Cancer. Investig. New Drugs 2021, 39, 509–515. [Google Scholar] [CrossRef]
- Mosele, F.; Deluche, E.; Lusque, A.; Le Bescond, L.; Filleron, T.; Pradat, Y.; Ducoulombier, A.; Pistilli, B.; Bachelot, T.; Viret, F.; et al. Trastuzumab Deruxtecan in Metastatic Breast Cancer with Variable HER2 Expression: The Phase 2 DAISY Trial. Nat. Med. 2023, 29, 2110–2120. [Google Scholar] [CrossRef]
- Andrikopoulou, A.; Zografos, E.; Liontos, M.; Koutsoukos, K.; Dimopoulos, M.-A.; Zagouri, F. Trastuzumab Deruxtecan (DS-8201a): The Latest Research and Advances in Breast Cancer. Clin. Breast Cancer 2021, 21, e212–e219. [Google Scholar] [CrossRef]
- Ogitani, Y.; Hagihara, K.; Oitate, M.; Naito, H.; Agatsuma, T. Bystander Killing Effect of DS -8201a, a Novel Anti-human Epidermal Growth Factor Receptor 2 Antibody–Drug Conjugate, in Tumors with Human Epidermal Growth Factor Receptor 2 Heterogeneity. Cancer Sci. 2016, 107, 1039–1046. [Google Scholar] [CrossRef]
- Markham, A. Belantamab Mafodotin: First Approval. Drugs 2020, 80, 1607–1613. [Google Scholar] [CrossRef]
- Trudel, S.; Lendvai, N.; Popat, R.; Voorhees, P.M.; Reeves, B.; Libby, E.N.; Richardson, P.G.; Hoos, A.; Gupta, I.; Bragulat, V.; et al. Antibody–Drug Conjugate, GSK2857916, in Relapsed/Refractory Multiple Myeloma: An Update on Safety and Efficacy from Dose Expansion Phase I Study. Blood Cancer J. 2019, 9, 37. [Google Scholar] [CrossRef]
- Calabretta, E.; Hamadani, M.; Carlo-Stella, C. The Antibody-Drug Conjugate Loncastuximab Tesirine for the Treatment of Diffuse Large B-Cell Lymphoma. Blood 2022, 140, 303–308. [Google Scholar] [CrossRef]
- Lee, A. Loncastuximab Tesirine: First Approval. Drugs 2021, 81, 1229–1233. [Google Scholar] [CrossRef]
- Xu, B. Loncastuximab Tesirine: An Effective Therapy for Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Eur. J. Clin. Pharmacol. 2022, 78, 707–719. [Google Scholar] [CrossRef]
- Zammarchi, F.; Corbett, S.; Adams, L.; Tyrer, P.C.; Kiakos, K.; Janghra, N.; Marafioti, T.; Britten, C.E.; Havenith, C.E.G.; Chivers, S.; et al. ADCT-402, a PBD Dimer–Containing Antibody Drug Conjugate Targeting CD19-Expressing Malignancies. Blood 2018, 131, 1094–1105. [Google Scholar] [CrossRef]
- Senter, P.D.; Sievers, E.L. The Discovery and Development of Brentuximab Vedotin for Use in Relapsed Hodgkin Lymphoma and Systemic Anaplastic Large Cell Lymphoma. Nat. Biotechnol. 2012, 30, 631–637. [Google Scholar] [CrossRef]
- Sasso, J.M.; Tenchov, R.; Bird, R.; Iyer, K.A.; Ralhan, K.; Rodriguez, Y.; Zhou, Q.A. The Evolving Landscape of Antibody–Drug Conjugates: In Depth Analysis of Recent Research Progress. Bioconjug. Chem. 2023, 34, 1951–2000. [Google Scholar] [CrossRef]
- Song, C.H.; Jeong, M.; In, H.; Kim, J.H.; Lin, C.-W.; Han, K.H. Trends in the Development of Antibody-Drug Conjugates for Cancer Therapy. Antibodies 2023, 12, 72. [Google Scholar] [CrossRef]
- Kaplon, H.; Crescioli, S.; Chenoweth, A.; Visweswaraiah, J.; Reichert, J.M. Antibodies to Watch in 2023. mAbs 2023, 15, 2153410. [Google Scholar] [CrossRef]
- Murphy, K.M.; Weaver, C.; Berg, L.J.; Janeway, C. Janeway’s Immunobiology, 10th ed.; International Student Edition; W.W. Norton & Company: New York, NY, USA; London, UK, 2022; ISBN 978-0-393-88491-3. [Google Scholar]
- Chua, M.M.; Fan, S.T.; Karush, F. Attachment of Immunoglobulin to Liposomal Membrane via Protein Carbohydrate. Biochim. Biophys. Acta 1984, 800, 291–300. [Google Scholar] [CrossRef]
- Nezlin, R.S.; Sykulev, Y.K. Structural Studies of Immunoglobulins Spin-Labeled at the Carbohydrate Moiety. Mol. Immunol. 1982, 19, 347–356. [Google Scholar] [CrossRef]
- Biswas, S.; Mandal, G.; Anadon, C.M.; Chaurio, R.A.; Lopez-Bailon, L.U.; Nagy, M.Z.; Mine, J.A.; Hänggi, K.; Sprenger, K.B.; Innamarato, P.; et al. Targeting Intracellular Oncoproteins with Dimeric IgA Promotes Expulsion from the Cytoplasm and Immune-Mediated Control of Epithelial Cancers. Immunity 2023, 56, 2570–2583. [Google Scholar] [CrossRef]
- Almagro, J.C.; Daniels-Wells, T.R.; Perez-Tapia, S.M.; Penichet, M.L. Progress and Challenges in the Design and Clinical Development of Antibodies for Cancer Therapy. Front. Immunol. 2018, 8, 1751. [Google Scholar] [CrossRef]
- Vidarsson, G.; Dekkers, G.; Rispens, T. IgG Subclasses and Allotypes: From Structure to Effector Functions. Front. Immunol. 2014, 5, 520. [Google Scholar] [CrossRef]
- Li, T.; Wang, X.; Niu, M.; Wang, M.; Zhou, J.; Wu, K.; Yi, M. Bispecific Antibody Targeting TGF-β and PD-L1 for Synergistic Cancer Immunotherapy. Front. Immunol. 2023, 14, 1196970. [Google Scholar] [CrossRef]
- Beishenaliev, A.; Loke, Y.L.; Goh, S.J.; Geo, H.N.; Mugila, M.; Misran, M.; Chung, L.Y.; Kiew, L.V.; Roffler, S.; Teo, Y.Y. Bispecific Antibodies for Targeted Delivery of Anti-Cancer Therapeutic Agents: A Review. J. Control. Release 2023, 359, 268–286. [Google Scholar] [CrossRef]
- Ma, J.; Mo, Y.; Tang, M.; Shen, J.; Qi, Y.; Zhao, W.; Huang, Y.; Xu, Y.; Qian, C. Bispecific Antibodies: From Research to Clinical Application. Front. Immunol. 2021, 12, 626616. [Google Scholar] [CrossRef]
- Shim, H. Bispecific Antibodies and Antibody–Drug Conjugates for Cancer Therapy: Technological Considerations. Biomolecules 2020, 10, 360. [Google Scholar] [CrossRef]
- Labrijn, A.F.; Janmaat, M.L.; Reichert, J.M.; Parren, P.W.H.I. Bispecific Antibodies: A Mechanistic Review of the Pipeline. Nat. Rev. Drug Discov. 2019, 18, 585–608. [Google Scholar] [CrossRef]
- Szijj, P.; Chudasama, V. The Renaissance of Chemically Generated Bispecific Antibodies. Nat. Rev. Chem. 2021, 5, 78–92. [Google Scholar] [CrossRef]
- Wei, J.; Yang, Y.; Wang, G.; Liu, M. Current Landscape and Future Directions of Bispecific Antibodies in Cancer Immunotherapy. Front. Immunol. 2022, 13, 1035276. [Google Scholar] [CrossRef]
- Dimasi, N.; Fleming, R.; Zhong, H.; Bezabeh, B.; Kinneer, K.; Christie, R.J.; Fazenbaker, C.; Wu, H.; Gao, C. Efficient Preparation of Site-Specific Antibody–Drug Conjugates Using Cysteine Insertion. Mol. Pharm. 2017, 14, 1501–1516. [Google Scholar] [CrossRef]
- Andreev, J.; Thambi, N.; Perez Bay, A.E.; Delfino, F.; Martin, J.; Kelly, M.P.; Kirshner, J.R.; Rafique, A.; Kunz, A.; Nittoli, T.; et al. Bispecific Antibodies and Antibody–Drug Conjugates (ADCs) Bridging HER2 and Prolactin Receptor Improve Efficacy of HER2 ADCs. Mol. Cancer Ther. 2017, 16, 681–693. [Google Scholar] [CrossRef]
- Cal, P.M.S.D.; Bernardes, G.J.L.; Gois, P.M.P. Cysteine-Selective Reactions for Antibody Conjugation. Angew. Chem. Int. Ed. 2014, 53, 10585–10587. [Google Scholar] [CrossRef]
- Harding, F.A.; Stickler, M.M.; Razo, J.; DuBridge, R. The Immunogenicity of Humanized and Fully Human Antibodies: Residual Immunogenicity Resides in the CDR Regions. mAbs 2010, 2, 256–265. [Google Scholar] [CrossRef]
- Doevendans, E.; Schellekens, H. Immunogenicity of Innovative and Biosimilar Monoclonal Antibodies. Antibodies 2019, 8, 21. [Google Scholar] [CrossRef]
- Safdari, Y.; Farajnia, S.; Asgharzadeh, M.; Khalili, M. Antibody Humanization Methods—A Review and Update. Biotechnol. Genet. Eng. Rev. 2013, 29, 175–186. [Google Scholar] [CrossRef]
- Panowski, S.; Bhakta, S.; Raab, H.; Polakis, P.; Junutula, J.R. Site-Specific Antibody Drug Conjugates for Cancer Therapy. mAbs 2014, 6, 34–45. [Google Scholar] [CrossRef]
- Adlersberg, J.B. The Immunoglobulin Hinge (Interdomain) Region. Ric. Clin. Lab. 1976, 6, 191–205. [Google Scholar] [CrossRef]
- Liu, H.; May, K. Disulfide Bond Structures of IgG Molecules: Structural Variations, Chemical Modifications and Possible Impacts to Stability and Biological Function. mAbs 2012, 4, 17–23. [Google Scholar] [CrossRef]
- Deveuve, Q.; Gouilleux-Gruart, V.; Thibault, G.; Lajoie, L. La Région Charnière Des Anticorps Thérapeutiques: L’importance Capitale d’une Courte Séquence. Med. Sci. 2019, 35, 1098–1105. [Google Scholar] [CrossRef]
- Hagihara, Y.; Saerens, D. Engineering Disulfide Bonds within an Antibody. Biochim. Biophys. Acta 2014, 1844, 2016–2023. [Google Scholar] [CrossRef]
- Mthembu, S.N.; Sharma, A.; Albericio, F.; De La Torre, B.G. Breaking a Couple: Disulfide Reducing Agents. ChemBioChem 2020, 21, 1947–1954. [Google Scholar] [CrossRef]
- Junutula, J.R.; Raab, H.; Clark, S.; Bhakta, S.; Leipold, D.D.; Weir, S.; Chen, Y.; Simpson, M.; Tsai, S.P.; Dennis, M.S.; et al. Site-Specific Conjugation of a Cytotoxic Drug to an Antibody Improves the Therapeutic Index. Nat. Biotechnol. 2008, 26, 925–932. [Google Scholar] [CrossRef]
- You, J.; Zhang, J.; Wang, J.; Jin, M. Cysteine-Based Coupling: Challenges and Solutions. Bioconjug. Chem. 2021, 32, 1525–1534. [Google Scholar] [CrossRef]
- Gunnoo, S.B.; Madder, A. Chemical Protein Modification through Cysteine. ChemBioChem 2016, 17, 529–553. [Google Scholar] [CrossRef]
- Akkapeddi, P.; Azizi, S.-A.; Freedy, A.M.; Cal, P.M.S.D.; Gois, P.M.P.; Bernardes, G.J.L. Construction of Homogeneous Antibody–Drug Conjugates Using Site-Selective Protein Chemistry. Chem. Sci. 2016, 7, 2954–2963. [Google Scholar] [CrossRef]
- Spears, R.J.; Fascione, M.A. Site-Selective Incorporation and Ligation of Protein Aldehydes. Org. Biomol. Chem. 2016, 14, 7622–7638. [Google Scholar] [CrossRef]
- Kölmel, D.K.; Kool, E.T. Oximes and Hydrazones in Bioconjugation: Mechanism and Catalysis. Chem. Rev. 2017, 117, 10358–10376. [Google Scholar] [CrossRef]
- O’Shannessy, D.J.; Quarles, R.H. Labeling of the Oligosaccharide Moieties of Immunoglobulins. J. Immunol. Meth. 1987, 99, 153–161. [Google Scholar] [CrossRef]
- Nakane, P.K.; Kawaoi, A. Peroxidase-Labeled Antibody a New Method of Conjugation. J. Histochem Cytochem. 1974, 22, 1084–1091. [Google Scholar] [CrossRef]
- Wang, L.; Brock, A.; Herberich, B.; Schultz, P.G. Expanding the Genetic Code of Escherichia coli. Science 2001, 292, 498–500. [Google Scholar] [CrossRef]
- Liu, S.; Liu, X. IgG N-Glycans. In Advances in Clinical Chemistry; Elsevier: Amsterdam, The Netherlands, 2021; Volume 105, pp. 1–47. ISBN 978-0-12-824627-6. [Google Scholar] [CrossRef]
- Zhong, X.; D’Antona, A.M.; Scarcelli, J.J.; Rouse, J.C. New Opportunities in Glycan Engineering for Therapeutic Proteins. Antibodies 2022, 11, 5. [Google Scholar] [CrossRef]
- Rodwell, J.D.; Alvarez, V.L.; Lee, C.; Lopes, A.D.; Goers, J.W.; King, H.D.; Powsner, H.J.; McKearn, T.J. Site-Specific Covalent Modification of Monoclonal Antibodies: In Vitro and in Vivo Evaluations. Proc. Natl. Acad. Sci. USA 1986, 83, 2632–2636. [Google Scholar] [CrossRef]
- Kaur, H. Characterization of Glycosylation in Monoclonal Antibodies and Its Importance in Therapeutic Antibody Development. Crit. Rev. Biotechnol. 2021, 41, 300–315. [Google Scholar] [CrossRef]
- Zauner, G.; Selman, M.H.J.; Bondt, A.; Rombouts, Y.; Blank, D.; Deelder, A.M.; Wuhrer, M. Glycoproteomic Analysis of Antibodies. Mol. Cell Proteomics. 2013, 12, 856–865. [Google Scholar] [CrossRef]
- Wang, L.-X.; Tong, X.; Li, C.; Giddens, J.P.; Li, T. Glycoengineering of Antibodies for Modulating Functions. Annu. Rev. Biochem. 2019, 88, 433–459. [Google Scholar] [CrossRef]
- Mimura, Y.; Katoh, T.; Saldova, R.; O’Flaherty, R.; Izumi, T.; Mimura-Kimura, Y.; Utsunomiya, T.; Mizukami, Y.; Yamamoto, K.; Matsumoto, T.; et al. Glycosylation Engineering of Therapeutic IgG Antibodies: Challenges for the Safety, Functionality and Efficacy. Protein Cell 2018, 9, 47–62. [Google Scholar] [CrossRef]
- Boune, S.; Hu, P.; Epstein, A.L.; Khawli, L.A. Principles of N-Linked Glycosylation Variations of IgG-Based Therapeutics: Pharmacokinetic and Functional Considerations. Antibodies 2020, 9, 22. [Google Scholar] [CrossRef]
- Sjögren, J.; Lood, R.; Nägeli, A. On Enzymatic Remodeling of IgG Glycosylation; Unique Tools with Broad Applications. Glycobiology 2020, 30, 254–267. [Google Scholar] [CrossRef]
- Golay, J.; Andrea, A.E.; Cattaneo, I. Role of Fc Core Fucosylation in the Effector Function of IgG1 Antibodies. Front. Immunol. 2022, 13, 929895. [Google Scholar] [CrossRef]
- Zhang, L.; Luo, S.; Zhang, B. Glycan Analysis of Therapeutic Glycoproteins. mAbs 2016, 8, 205–215. [Google Scholar] [CrossRef]
- Huhn, C.; Selman, M.H.J.; Ruhaak, L.R.; Deelder, A.M.; Wuhrer, M. IgG Glycosylation Analysis. Proteomics 2009, 9, 882–913. [Google Scholar] [CrossRef]
- Maverakis, E.; Kim, K.; Shimoda, M.; Gershwin, M.E.; Patel, F.; Wilken, R.; Raychaudhuri, S.; Ruhaak, L.R.; Lebrilla, C.B. Glycans in the Immune System and The Altered Glycan Theory of Autoimmunity: A Critical Review. J. Autoimmun. 2015, 57, 1–13. [Google Scholar] [CrossRef]
- Quast, I.; Peschke, B.; Lünemann, J.D. Regulation of Antibody Effector Functions through IgG Fc N-Glycosylation. Cell. Mol. Life Sci. 2017, 74, 837–847. [Google Scholar] [CrossRef]
- Van De Bovenkamp, F.S.; Hafkenscheid, L.; Rispens, T.; Rombouts, Y. The Emerging Importance of IgG Fab Glycosylation in Immunity. J. Immunol. 2016, 196, 1435–1441. [Google Scholar] [CrossRef]
- Vattepu, R.; Sneed, S.L.; Anthony, R.M. Sialylation as an Important Regulator of Antibody Function. Front. Immunol. 2022, 13, 818736. [Google Scholar] [CrossRef]
- O’Shannessy, D.J.; Dobersen, M.J.; Quarles, R.H. A Novel Procedure for Labeling Immunoglobulins by Conjugation to Oligosaccharide Moieties. Immunol. Lett. 1984, 8, 273–277. [Google Scholar] [CrossRef]
- Fan, Y.; Kildegaard, H.F.; Andersen, M.R. Engineer Medium and Feed for Modulating N-Glycosylation of Recombinant Protein Production in CHO Cell Culture. In Heterologous Protein Production in CHO Cells; Meleady, P., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2017; Volume 1603, pp. 209–226. ISBN 978-1-4939-6971-5. [Google Scholar] [CrossRef]
- Sheeley, D.M.; Merrill, B.M.; Taylor, L.C.E. Characterization of Monoclonal Antibody Glycosylation: Comparison of Expression Systems and Identification of Terminal α-Linked Galactose. Anal. Biochem. 1997, 247, 102–110. [Google Scholar] [CrossRef]
- Grainger, R.K.; James, D.C. CHO Cell Line Specific Prediction and Control of Recombinant Monoclonal Antibody N-glycosylation. Biotechnol. Bioeng. 2013, 110, 2970–2983. [Google Scholar] [CrossRef]
- Routier, F.H.; Davies, M.J.; Bergemann, K.; Hounsell, E.F. The Glycosylation Pattern of a Humanized IgGl Antibody (D1.3) Expressed in CHO Cells. Glycoconj. J. 1997, 14, 201–207. [Google Scholar] [CrossRef]
- Kim, W.-D.; Tokunaga, M.; Ozaki, H.; Ishibashi, T.; Honda, K.; Kajiura, H.; Fujiyama, K.; Asano, R.; Kumagai, I.; Omasa, T.; et al. Glycosylation Pattern of Humanized IgG-like Bispecific Antibody Produced by Recombinant CHO Cells. Appl. Microbiol. Biotechnol. 2010, 85, 535–542. [Google Scholar] [CrossRef]
- Rothfus, J.A.; Smith, E.L. Glycopeptides. IV. The Periodate Oxidation of Glycopeptides from Human Gamma-Globulin. J. Biol. Chem. 1963, 238, 1402–1410. [Google Scholar] [CrossRef]
- Malaprade Reaction: (Malaprade Oxidation). In Comprehensive Organic Name Reactions and Reagents; Wiley: Hoboken, NJ, USA, 2010; pp. 1807–1810. ISBN 978-0-471-70450-8. [CrossRef]
- Nicolet, B.H.; Shinn, L.A. The Action of Periodic Acid on α-Amino Alcohols. J. Am. Chem. Soc. 1939, 61, 1615. [Google Scholar] [CrossRef]
- Zuberbühler, K.; Casi, G.; Bernardes, G.J.L.; Neri, D. Fucose-Specific Conjugation of Hydrazide Derivatives to a Vascular-Targeting Monoclonal Antibody in IgG Format. Chem. Commun. 2012, 48, 7100. [Google Scholar] [CrossRef]
- Wolfe, C.A.C.; Hage, D.S. Studies on the Rate and Control of Antibody Oxidation by Periodate. Anal. Biochem. 1995, 231, 123–130. [Google Scholar] [CrossRef]
- Sapozhnikova, K.A.; Gulyak, E.L.; Misyurin, V.A.; Simonova, M.A.; Ryabukhina, E.V.; Alexeeva, A.V.; Tikhonova, N.A.; Lyzhko, N.A.; Popova, G.P.; Misyurin, A.V.; et al. Branched Linkers for Site-Specific Fluorescent Labeling of Antibodies. Molecules 2023, 28, 425. [Google Scholar] [CrossRef]
- Fischer-Durand, N.; Salmain, M.; Vessières, A.; Jaouen, G. A New Bioorthogonal Cross-Linker with Alkyne and Hydrazide End Groups for Chemoselective Ligation. Application to Antibody Labelling. Tetrahedron 2012, 68, 9638–9644. [Google Scholar] [CrossRef]
- Abraham, R.; Moller, D.; Gabel, D.; Senter, P.; Hellström, I.; Hellström, K.E. The Influence of Periodate Oxidation on Monoclonal Antibody Avidity and Immunoreactivity. J. Immunol. Meth. 1991, 144, 77–86. [Google Scholar] [CrossRef]
- Akira, M.; Kohkichi, S.; Tadashi, Y. Modification of Immunoglobulin G Using Specific Reactivity of Sugar Moiety. Immunochemistry 1978, 15, 523–528. [Google Scholar] [CrossRef]
- Kurth, M.; Pelegrin, A.; Rose, K.; Offord, R.E.; Pochon, S.; Mach, J.P.; Buchegger, F. Site-Specific Conjugation of a Radioiodinated Phenethylamine Derivative to a Monoclonal Antibody Results in Increased Radioactivity Localization in Tumor. J. Med. Chem. 1993, 36, 1255–1261. [Google Scholar] [CrossRef]
- Andersen, B.R.; Abele, D.C.; Vannier, W.E. Effects of Mild Periodate Oxidation on Antibodies. J. Immunol. 1966, 97, 913–924. [Google Scholar] [CrossRef]
- Zhou, Q.; Stefano, J.E.; Manning, C.; Kyazike, J.; Chen, B.; Gianolio, D.A.; Park, A.; Busch, M.; Bird, J.; Zheng, X.; et al. Site-Specific Antibody–Drug Conjugation through Glycoengineering. Bioconjug. Chem. 2014, 25, 510–520. [Google Scholar] [CrossRef]
- Inglis, A.S.; Rivett, D.E.; McMahon, D.T.W. The Identification of Tryptophan Residues in Proteins as Oxidised Derivatives during Amino Acid Sequence Determinations. FEBS Lett. 1979, 104, 115–118. [Google Scholar] [CrossRef]
- Clamp, J.; Hough, L. The Periodate Oxidation of Amino Acids with Reference to Studies on Glycoproteins. Biochem. J. 1965, 94, 17–24. [Google Scholar] [CrossRef]
- Robinson, G.M.; Smyth, M.R. Simultaneous Determination of Products and Intermediates of L-Dopa Oxidation Using Capillary Electrophoresis With Diode-Array Detection. Analyst 1997, 122, 797–802. [Google Scholar] [CrossRef]
- Hsuan, J.J. The Cross-Linking of Tyrosine Residues in Apo-Ovotransferrin by Treatment with Periodate Anions. Biochem. J. 1987, 247, 467–473. [Google Scholar] [CrossRef]
- Stadtman, E.R. Role of Oxidized Amino Acids in Protein Breakdown and Stability. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 1995; Volume 258, pp. 379–393. ISBN 978-0-12-182159-3. [Google Scholar] [CrossRef]
- Burzio, L.A.; Waite, J.H. Reactivity of Peptidyl-tyrosine to Hydroxylation and Cross-linking. Protein Sci. 2001, 10, 735–740. [Google Scholar] [CrossRef]
- Yamasaki, R.B.; Osuga, D.T.; Feeney, R.E. Periodate Oxidation of Methionine in Proteins. Anal. Biochem. 1982, 126, 183–189. [Google Scholar] [CrossRef]
- Willan, K.J.; Golding, B.; Givol, D.; Dwek, R.A. Specific Spin Labelling of the Fc Region of Immunoglobulins. FEBS Lett. 1977, 80, 133–136. [Google Scholar] [CrossRef]
- Qasba, P.K. Glycans of Antibodies as a Specific Site for Drug Conjugation Using Glycosyltransferases. Bioconjug. Chem. 2015, 26, 2170–2175. [Google Scholar] [CrossRef]
- Hageman, T.; Wei, H.; Kuehne, P.; Fu, J.; Ludwig, R.; Tao, L.; Leone, A.; Zocher, M.; Das, T.K. Impact of Tryptophan Oxidation in Complementarity-Determining Regions of Two Monoclonal Antibodies on Structure-Function Characterized by Hydrogen-Deuterium Exchange Mass Spectrometry and Surface Plasmon Resonance. Pharm. Res. 2019, 36, 24. [Google Scholar] [CrossRef]
- McDonnell, K.A.; Low, S.C.; Hoehn, T.; Donnelly, R.; Palmieri, H.; Fraley, C.; Sakorafas, P.; Mezo, A.R. Synthesis and Structure−Activity Relationships of Dimeric Peptide Antagonists of the Human Immunoglobulin G−Human Neonatal Fc Receptor (IgG−FcRn) Interaction. J. Med. Chem. 2010, 53, 1587–1596. [Google Scholar] [CrossRef]
- Umaña, P.; Jean–Mairet, J.; Moudry, R.; Amstutz, H.; Bailey, J.E. Engineered Glycoforms of an Antineuroblastoma IgG1 with Optimized Antibody-Dependent Cellular Cytotoxic Activity. Nat. Biotechnol. 1999, 17, 176–180. [Google Scholar] [CrossRef]
- Fleminger, G.; Solomon, B.; Wolf, T.; Hadas, E. Single Step Oxidative Binding of Antibodies to Hydrazide-Modified Eupergit C. Appl. Biochem. Biotechnol. 1990, 26, 231–238. [Google Scholar] [CrossRef]
- O’shannessy, D.J. Hydrazido-Derivatized Supports in Affinity Chromatography. J. Chromatogr. A 1990, 510, 13–21. [Google Scholar] [CrossRef]
- Fleminger, G.; Hadas, E.; Wolf, T.; Solomon, B. Oriented Immobilization of Periodateoxidized Monoclonal Antibodies on Amino and Hydrazide Derivatives of Eupergit C. Appl. Biochem. Biotechnol. 1990, 23, 123–137. [Google Scholar] [CrossRef]
- Hoffman, W.L.; O’Shannessy, D.J. Site-Specific Immobilization of Antibodies by Their Oligosaccharide Moieties to New Hydrazide Derivatized Solid Supports. J. Immunol. Meth. 1988, 112, 113–120. [Google Scholar] [CrossRef]
- Scheck, R.A.; Francis, M.B. Regioselective Labeling of Antibodies through N-Terminal Transamination. ACS Chem. Biol. 2007, 2, 247–251. [Google Scholar] [CrossRef]
- Netirojjanakul, C.; Witus, L.S.; Behrens, C.R.; Weng, C.-H.; Iavarone, A.T.; Francis, M.B. Synthetically Modified Fc Domains as Building Blocks for Immunotherapy Applications. Chem. Sci. 2013, 4, 266–272. [Google Scholar] [CrossRef]
- Witus, L.S.; Francis, M. Site-Specific Protein Bioconjugation via a Pyridoxal 5′-Phosphate-Mediated N-Terminal Transamination Reaction. Curr. Prot. Chem. Biol. 2010, 2, 125–134. [Google Scholar] [CrossRef]
- Witus, L.S.; Netirojjanakul, C.; Palla, K.S.; Muehl, E.M.; Weng, C.-H.; Iavarone, A.T.; Francis, M.B. Site-Specific Protein Transamination Using N -Methylpyridinium-4-Carboxaldehyde. J. Am. Chem. Soc. 2013, 135, 17223–17229. [Google Scholar] [CrossRef]
- Zhang, Z.; Shah, B.; Richardson, J. Impact of Fc N-Glycan Sialylation on IgG Structure. mAbs 2019, 11, 1381–1390. [Google Scholar] [CrossRef]
- Schauer, R. Chemistry, Metabolism, and Biological Functions of Sialic Acids. In Advances in Carbohydrate Chemistry and Biochemistry; Elsevier: Amsterdam, The Netherlands, 1982; Volume 40, pp. 131–234. ISBN 978-0-12-007240-8. [Google Scholar] [CrossRef]
- Cabezas, J.A. Some Questions and Suggestions on the Type References of the Official Nomenclature (IUB) for Sialidase(s) and Endosialidase. Biochem. J. 1991, 278, 311–312. [Google Scholar] [CrossRef]
- Haxho, F.; Neufeld, R.J.; Szewczuk, M.R. Neuraminidase-1: A Novel Therapeutic Target in Multistage Tumorigenesis. Oncotarget 2016, 7, 40860–40881. [Google Scholar] [CrossRef]
- Shields, R.L.; Lai, J.; Keck, R.; O’Connell, L.Y.; Hong, K.; Meng, Y.G.; Weikert, S.H.A.; Presta, L.G. Lack of Fucose on Human IgG1 N-Linked Oligosaccharide Improves Binding to Human FcγRIII and Antibody-Dependent Cellular Toxicity. J. Biol. Chem. 2002, 277, 26733–26740. [Google Scholar] [CrossRef]
- Zhu, Z.; Ramakrishnan, B.; Li, J.; Wang, Y.; Feng, Y.; Prabakaran, P.; Colantonio, S.; Dyba, M.A.; Qasba, P.K.; Dimitrov, D.S. Site-Specific Antibody-Drug Conjugation through an Engineered Glycotransferase and a Chemically Reactive Sugar. mAbs 2014, 6, 1190–1200. [Google Scholar] [CrossRef]
- Tang, F.; Wang, L.-X.; Huang, W. Chemoenzymatic Synthesis of Glycoengineered IgG Antibodies and Glycosite-Specific Antibody–Drug Conjugates. Nat. Protoc. 2017, 12, 1702–1721. [Google Scholar] [CrossRef]
- Li, T.; DiLillo, D.J.; Bournazos, S.; Giddens, J.P.; Ravetch, J.V.; Wang, L.-X. Modulating IgG Effector Function by Fc Glycan Engineering. Proc. Natl. Acad. Sci. USA 2017, 114, 3485–3490. [Google Scholar] [CrossRef]
- Li, T.; Tong, X.; Yang, Q.; Giddens, J.P.; Wang, L.-X. Glycosynthase Mutants of Endoglycosidase S2 Show Potent Transglycosylation Activity and Remarkably Relaxed Substrate Specificity for Antibody Glycosylation Remodeling. J. Biol. Chem. 2016, 291, 16508–16518. [Google Scholar] [CrossRef]
- Fairbanks, A.J. Synthetic and Semi-Synthetic Approaches to Unprotected N -Glycan Oxazolines. Beilstein J. Org. Chem. 2018, 14, 416–429. [Google Scholar] [CrossRef]
- Tong, X.; Li, T.; Orwenyo, J.; Toonstra, C.; Wang, L.-X. One-Pot Enzymatic Glycan Remodeling of a Therapeutic Monoclonal Antibody by Endoglycosidase S (Endo-S) from Streptococcus Pyogenes. Bioorg. Med. Chem. 2018, 26, 1347–1355. [Google Scholar] [CrossRef]
- Giddens, J.P.; Lomino, J.V.; DiLillo, D.J.; Ravetch, J.V.; Wang, L.-X. Site-Selective Chemoenzymatic Glycoengineering of Fab and Fc Glycans of a Therapeutic Antibody. Proc. Natl. Acad. Sci. USA 2018, 115, 12023–12027. [Google Scholar] [CrossRef]
- Faridoon, F.; Shi, W.; Qin, K.; Tang, Y.; Li, M.; Guan, D.; Tian, X.; Jiang, B.; Dong, J.; Tang, F.; et al. New Linker Structures Applied in Glycosite-Specific Antibody Drug Conjugates. Org. Chem. Front. 2019, 6, 3144–3149. [Google Scholar] [CrossRef]
- Kadowaki, S.; Yamamoto, K.; Fujisaki, M.; Izumi, K.; Tochikura, T.; Yokoyama, T. Purification and Characterization of a Novel Fungal Endo-β-N-Acetylglucosaminidase Acting on Complex Oligosaccharides of Glycoproteins. Agric. Biol. Chem. 1990, 54, 97–106. [Google Scholar] [CrossRef]
- Yamamoto, K.J.; Kadowaki, S.; Watanabe, J.; Kumagai, H. Transglycosylation Activity of Mucor Hiemalis Endo-β-N-Acetylglucosaminidase Which Transfers Complex Oligosaccharides to the N-acetylglucosamine Moieties of Peptides. Biochem. Biophys. Res. Commun. 1994, 203, 244–252. [Google Scholar] [CrossRef]
- Haneda, K.; Inazu, T.; Yamamoto, K.; Kumagai, H.; Nakahara, Y.; Kobata, A. Transglycosylation of Intact Sialo Complex-Type Oligosaccharides to the N-acetylglucosamine Moieties of Glycopeptides by Mucor Hiemalis Endo-β-N-Acetylglucosaminidase. Carbohydr. Res. 1996, 292, 61–70. [Google Scholar] [CrossRef]
- Mizuno, M.; Muramoto, I.; Kawakami, T.; Seike, M.; Aimoto, S.; Haneda, K.; Inazu, T. A Synthesis of a Glycopeptide Analogue of Eel Calcitonin. Tetrahedron Lett. 1998, 39, 55–58. [Google Scholar] [CrossRef]
- Yamamoto, K. Chemo-Enzymatic Synthesis of Bioactive Glycopeptide Using Microbial Endoglycosidase. J. Biosci. Bioeng. 2001, 92, 493–501. [Google Scholar] [CrossRef]
- Manabe, S. Attempts to Synthesize Homogeneous Glycan-Conjugated Antibody-Drug Conjugates. Transl. Regul. Sci. 2020, 2, 84–89. [Google Scholar] [CrossRef]
- Le, N.P.L.; Bowden, T.A.; Struwe, W.B.; Crispin, M. Immune Recruitment or Suppression by Glycan Engineering of Endogenous and Therapeutic Antibodies. Biochim. Biophys. Acta 2016, 1860, 1655–1668. [Google Scholar] [CrossRef]
- Griffin, M.E.; Hsieh-Wilson, L.C. Glycan Engineering for Cell and Developmental Biology. Cell Chem. Biol. 2016, 23, 108–121. [Google Scholar] [CrossRef]
- Wang, L.-X.; Lomino, J.V. Emerging Technologies for Making Glycan-Defined Glycoproteins. ACS Chem. Biol. 2012, 7, 110–122. [Google Scholar] [CrossRef]
- Basu, K.; Green, E.M.; Cheng, Y.; Craik, C.S. Why Recombinant Antibodies—Benefits and Applications. Curr. Opin. Biotechnol. 2019, 60, 153–158. [Google Scholar] [CrossRef]
- De St. Groth, S.F.; Scheidegger, D. Production of Monoclonal Antibodies: Strategy and Tactics. J. Immunol. Meth. 1980, 35, 1–21. [Google Scholar] [CrossRef]
- Alejandra, W.-P.; Miriam Irene, J.-P.; Fabio Antonio, G.-S.; Patricia, R.-G.R.; Elizabeth, T.-A.; Aleman-Aguilar, J.P.; Rebeca, G.-V. Production of Monoclonal Antibodies for Therapeutic Purposes: A Review. Int. Immunopharmacol. 2023, 120, 110376. [Google Scholar] [CrossRef]
- Bjerrum, K.B.; Aagaard, J.B.; Soucy, J.A.; Kabiljagic, A.A.; Skjoedt, K.; Graversen, J.H.; Henriksen, M.L.; Hansen, S.W.K. Facile Generation of Monoclonal Antibodies Suitable for Conjugation. J. Immunol. Meth. 2020, 483, 112807. [Google Scholar] [CrossRef]
- Kumar, R.; Parray, H.A.; Shrivastava, T.; Sinha, S.; Luthra, K. Phage Display Antibody Libraries: A Robust Approach for Generation of Recombinant Human Monoclonal Antibodies. Int. J. Biol. Macromol. 2019, 135, 907–918. [Google Scholar] [CrossRef]
- Hentrich, C.; Ylera, F.; Frisch, C.; Ten Haaf, A.; Knappik, A. Monoclonal Antibody Generation by Phage Display. In Handbook of Immunoassay Technologies; Elsevier: Amsterdam, The Netherlands, 2018; pp. 47–80. ISBN 978-0-12-811762-0. [Google Scholar]
- Lembke, W.; Locher, M. Monoclonal Antibodies: Discovery and Protein Engineering. In Regulatory Toxicology; Reichl, F.-X., Schwenk, M., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 83–98. ISBN 978-3-030-57498-7. [Google Scholar] [CrossRef]
- Klein, C.; Schaefer, W.; Regula, J.T.; Dumontet, C.; Brinkmann, U.; Bacac, M.; Umaña, P. Engineering Therapeutic Bispecific Antibodies Using CrossMab Technology. Methods 2019, 154, 21–31. [Google Scholar] [CrossRef]
- Li, H.; Er Saw, P.; Song, E. Challenges and Strategies for Next-Generation Bispecific Antibody-Based Antitumor Therapeutics. Cell Mol. Immunol. 2020, 17, 451–461. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, Y.; Park, J.; Liu, X.; Hu, Y.; Wang, T.; McFarland, K.; Betenbaugh, M.J. Design and Production of Bispecific Antibodies. Antibodies 2019, 8, 43. [Google Scholar] [CrossRef]
- Muyldermans, S. A Guide to: Generation and Design of Nanobodies. FEBS J. 2021, 288, 2084–2102. [Google Scholar] [CrossRef]
- De Marco, A. Recombinant Expression of Nanobodies and Nanobody-Derived Immunoreagents. Protein Expr. Purif. 2020, 172, 105645. [Google Scholar] [CrossRef]
- Todorovska, A.; Roovers, R.C.; Dolezal, O.; Kortt, A.A.; Hoogenboom, H.R.; Hudson, P.J. Design and Application of Diabodies, Triabodies and Tetrabodies for Cancer Targeting. J. Immunol. Meth. 2001, 248, 47–66. [Google Scholar] [CrossRef]
- Vaks, L.; Benhar, I. Production of Stabilized scFv Antibody Fragments in the E. coli Bacterial Cytoplasm. In Human Monoclonal Antibodies; Steinitz, M., Ed.; Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2014; Volume 1060, pp. 171–184. ISBN 978-1-62703-585-9. [Google Scholar] [CrossRef]
- Felices, M.; Lenvik, T.R.; Davis, Z.B.; Miller, J.S.; Vallera, D.A. Generation of BiKEs and TriKEs to Improve NK Cell-Mediated Targeting of Tumor Cells. In Natural Killer Cells; Somanchi, S.S., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2016; Volume 1441, pp. 333–346. ISBN 978-1-4939-3682-3. [Google Scholar] [CrossRef]
- Lyons, A.; King, D.J.; Owens, R.J.; Yarranton, G.T.; Millican, A.; Whittle, N.R.; Adair, J.R. Site-Specific Attachment to Recombinant Antibodies via Introduced Surface Cysteine Residues. Protein Eng. Des. Sel. 1990, 3, 703–708. [Google Scholar] [CrossRef]
- Tumey, L.N.; Li, F.; Rago, B.; Han, X.; Loganzo, F.; Musto, S.; Graziani, E.I.; Puthenveetil, S.; Casavant, J.; Marquette, K.; et al. Site Selection: A Case Study in the Identification of Optimal Cysteine Engineered Antibody Drug Conjugates. AAPS J. 2017, 19, 1123–1135. [Google Scholar] [CrossRef]
- Hofer, T.; Skeffington, L.R.; Chapman, C.M.; Rader, C. Molecularly Defined Antibody Conjugation through a Selenocysteine Interface. Biochemistry 2009, 48, 12047–12057. [Google Scholar] [CrossRef]
- Thompson, P.; Bezabeh, B.; Fleming, R.; Pruitt, M.; Mao, S.; Strout, P.; Chen, C.; Cho, S.; Zhong, H.; Wu, H.; et al. Hydrolytically Stable Site-Specific Conjugation at the N-Terminus of an Engineered Antibody. Bioconjug. Chem. 2015, 26, 2085–2096. [Google Scholar] [CrossRef]
- Li, X.; Nelson, C.G.; Nair, R.R.; Hazlehurst, L.; Moroni, T.; Martinez-Acedo, P.; Nanna, A.R.; Hymel, D.; Burke, T.R.; Rader, C. Stable and Potent Selenomab-Drug Conjugates. Cell Chem. Biol. 2017, 24, 433–442.e6. [Google Scholar] [CrossRef]
- Deeks, E.D. Polatuzumab Vedotin: First Global Approval. Drugs 2019, 79, 1467–1475. [Google Scholar] [CrossRef]
- Lehar, S.M.; Pillow, T.; Xu, M.; Staben, L.; Kajihara, K.K.; Vandlen, R.; DePalatis, L.; Raab, H.; Hazenbos, W.L.; Hiroshi Morisaki, J.; et al. Novel Antibody–Antibiotic Conjugate Eliminates Intracellular S. aureus. Nature 2015, 527, 323–328. [Google Scholar] [CrossRef]
- Zhou, C.; Lehar, S.; Gutierrez, J.; Rosenberger, C.M.; Ljumanovic, N.; Dinoso, J.; Koppada, N.; Hong, K.; Baruch, A.; Carrasco-Triguero, M.; et al. Pharmacokinetics and Pharmacodynamics of DSTA4637A: A Novel THIOMABTM Antibody Antibiotic Conjugate against Staphylococcus aureus in Mice. mAbs 2016, 8, 1612–1619. [Google Scholar] [CrossRef]
- Deng, R.; Zhou, C.; Li, D.; Cai, H.; Sukumaran, S.; Carrasco-Triguero, M.; Saad, O.; Nazzal, D.; Lowe, C.; Ramanujan, S.; et al. Preclinical and Translational Pharmacokinetics of a Novel THIOMABTM Antibody-Antibiotic Conjugate against Staphylococcus aureus. mAbs 2019, 11, 1162–1174. [Google Scholar] [CrossRef]
- Lim, J.; Lewin-Koh, N.; Chu, T.; Rymut, S.M.; Berhanu, A.; Carrasco-Triguero, M.; Rosenberger, C.C.; Hazenbos, W.L.; Miller, L.G.; Fowler, V.G.; et al. 167. A Phase 1b, Randomized, Double-Blind, Placebo-Controlled, Multiple-Ascending Dose Study to Investigate the Safety, Tolerability, and Pharmacokinetics of DSTA4637S in Patients with Staphylococcus Aureus Bacteremia Receiving Standard-of-Care Antibiotics. Open Forum Infect. Dis. 2020, 7, S213. [Google Scholar] [CrossRef]
- Kumar, A.; Kinneer, K.; Masterson, L.; Ezeadi, E.; Howard, P.; Wu, H.; Gao, C.; Dimasi, N. Synthesis of a Heterotrifunctional Linker for the Site-Specific Preparation of Antibody-Drug Conjugates with Two Distinct Warheads. Bioorg. Med. Chem. Lett. 2018, 28, 3617–3621. [Google Scholar] [CrossRef]
- Department of Medicinal Chemistry, University of Utah; Nervig, C.S.; Owen, S.C.; Department of Molecular Pharmaceutics, University of Utah; Department of Biomedical Engineering, University of Utah. Advances in the Development of Dual-Drug Antibody Drug Conjugates. J. Antib. Drug Conjug. 2023. [Google Scholar] [CrossRef]
- Peng, Q.; Zang, B.; Zhao, W.; Li, D.; Ren, J.; Ji, F.; Jia, L. Efficient Continuous-Flow Aldehyde Tag Conversion Using Immobilized Formylglycine Generating Enzyme. Catal. Sci. Technol. 2020, 10, 484–492. [Google Scholar] [CrossRef]
- Drake, P.M.; Albers, A.E.; Baker, J.; Banas, S.; Barfield, R.M.; Bhat, A.S.; De Hart, G.W.; Garofalo, A.W.; Holder, P.; Jones, L.C.; et al. Aldehyde Tag Coupled with HIPS Chemistry Enables the Production of ADCs Conjugated Site-Specifically to Different Antibody Regions with Distinct In Vivo Efficacy and PK Outcomes. Bioconjug. Chem. 2014, 25, 1331–1341. [Google Scholar] [CrossRef]
- Pomplun, S.; Mohamed, M.Y.H.; Oelschlaegel, T.; Wellner, C.; Bergmann, F. Efficient Pictet–Spengler Bioconjugation with N-Substituted Pyrrolyl Alanine Derivatives. Angew. Chem. Int. Ed. 2019, 58, 3542–3547. [Google Scholar] [CrossRef]
- Dickgiesser, S.; Rasche, N.; Nasu, D.; Middel, S.; Hörner, S.; Avrutina, O.; Diederichsen, U.; Kolmar, H. Self-Assembled Hybrid Aptamer-Fc Conjugates for Targeted Delivery: A Modular Chemoenzymatic Approach. ACS Chem. Biol. 2015, 10, 2158–2165. [Google Scholar] [CrossRef]
- Smith, E.L.; Giddens, J.P.; Iavarone, A.T.; Godula, K.; Wang, L.-X.; Bertozzi, C.R. Chemoenzymatic Fc Glycosylation via Engineered Aldehyde Tags. Bioconjug. Chem. 2014, 25, 788–795. [Google Scholar] [CrossRef]
- Dahlgren, G.; Hodsdon, J.M. The Kinetics of the Periodate Oxidation of 2-Aminoethanol. J. Phys. Chem. 1964, 68, 416–418. [Google Scholar] [CrossRef]
- Ta, H.T.; Peter, K.; Hagemeyer, C.E. Enzymatic Antibody Tagging: Toward a Universal Biocompatible Targeting Tool. Tr. Cardiovasc. Med. 2012, 22, 105–111. [Google Scholar] [CrossRef]
- Min, B.; Jin, J.; Kim, H.; Her, N.-G.; Park, C.; Kim, D.; Yang, J.; Hwang, J.; Kim, E.; Choi, M.; et al. cIRCR201-dPBD, a Novel Pyrrolobenzodiazepine Dimer-Containing Site-Specific Antibody–Drug Conjugate Targeting c-Met Overexpression Tumors. ACS Omega 2020, 5, 25798–25809. [Google Scholar] [CrossRef]
- Shin, S.H.; Park, Y.; Park, S.S.; Ju, E.J.; Park, J.; Ko, E.J.; Bae, D.J.; Kim, S.; Chung, C.; Song, H.Y.; et al. An Elaborate New Linker System Significantly Enhances the Efficacy of an HER2-Antibody-Drug Conjugate against Refractory HER2-Positive Cancers. Adv. Sci. 2021, 8, 2102414. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Y.; Uslu, S.; Venkatachalapathy, S.; Rashidian, M.; Schaefer, J.V.; Plückthun, A.; Distefano, M.D. Enzymatic Construction of DARPin-Based Targeted Delivery Systems Using Protein Farnesyltransferase and a Capture and Release Strategy. Int. J. Mol. Sci. 2022, 23, 11537. [Google Scholar] [CrossRef]
- Mortensen, M.R.; Skovsgaard, M.B.; Märcher, A.; Andersen, V.L.; Palmfeldt, J.; Nielsen, T.B.; Tørring, T.; Laursen, N.S.; Andersen, K.R.; Kjems, J.; et al. Introduction of an Aldehyde Handle on Nanobodies by Affinity-Guided Labeling. Bioconjug. Chem. 2020, 31, 1295–1300. [Google Scholar] [CrossRef]
- Wals, K.; Ovaa, H. Unnatural Amino Acid Incorporation in E. coli: Current and Future Applications in the Design of Therapeutic Proteins. Front. Chem. 2014, 2, 15. [Google Scholar] [CrossRef]
- Hallam, T.J.; Smider, V.V. Unnatural Amino Acids in Novel Antibody Conjugates. Future Med. Chem. 2014, 6, 1309–1324. [Google Scholar] [CrossRef]
- Young, D.D.; Schultz, P.G. Playing with the Molecules of Life. ACS Chem. Biol. 2018, 13, 854–870. [Google Scholar] [CrossRef]
- Evans, E.G.B.; Millhauser, G.L. Genetic Incorporation of the Unnatural Amino Acid P-Acetyl Phenylalanine into Proteins for Site-Directed Spin Labeling. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 2015; Volume 563, pp. 503–527. ISBN 978-0-12-802834-6. [Google Scholar] [CrossRef]
- Tharp, J.M.; Vargas-Rodriguez, O.; Schepartz, A.; Söll, D. Genetic Encoding of Three Distinct Noncanonical Amino Acids Using Reprogrammed Initiator and Nonsense Codons. ACS Chem. Biol. 2021, 16, 766–774. [Google Scholar] [CrossRef]
- Palei, S.; Mootz, H.D. Cyclic Peptides Made by Linking Synthetic and Genetically Encoded Fragments. ChemBioChem 2016, 17, 378–382. [Google Scholar] [CrossRef]
- Tian, F.; Lu, Y.; Manibusan, A.; Sellers, A.; Tran, H.; Sun, Y.; Phuong, T.; Barnett, R.; Hehli, B.; Song, F.; et al. A General Approach to Site-Specific Antibody Drug Conjugates. Proc. Natl. Acad. Sci. USA 2014, 111, 1766–1771. [Google Scholar] [CrossRef]
- Costa, S.A.; Mozhdehi, D.; Dzuricky, M.J.; Isaacs, F.J.; Brustad, E.M.; Chilkoti, A. Active Targeting of Cancer Cells by Nanobody Decorated Polypeptide Micelle with Bio-Orthogonally Conjugated Drug. Nano Lett. 2019, 19, 247–254. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, Z.; Wang, Z.; Luo, F.; Guan, M.; Xu, M.; Li, Y.; Zhang, Y.; Wang, Z.; Wang, W. A Simple and Efficient Method to Generate Dual Site-Specific Conjugation ADCs with Cysteine Residue and an Unnatural Amino Acid. Bioconjug. Chem. 2021, 32, 1094–1104. [Google Scholar] [CrossRef]
- Cornish, V.W.; Hahn, K.M.; Schultz, P.G. Site-Specific Protein Modification Using a Ketone Handle. J. Am. Chem. Soc. 1996, 118, 8150–8151. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, Z.; Brock, A.; Schultz, P.G. Addition of the Keto Functional Group to the Genetic Code of Escherichia coli. Proc. Natl. Acad. Sci. USA 2003, 100, 56–61. [Google Scholar] [CrossRef]
- Zhang, Z.; Smith, B.A.C.; Wang, L.; Brock, A.; Cho, C.; Schultz, P.G. A New Strategy for the Site-Specific Modification of Proteins in Vivo. Biochemistry 2003, 42, 6735–6746. [Google Scholar] [CrossRef]
- Zeng, H.; Xie, J.; Schultz, P.G. Genetic Introduction of a Diketone-Containing Amino Acid into Proteins. Bioorg. Med. Chem. Lett. 2006, 16, 5356–5359. [Google Scholar] [CrossRef]
- Huang, Y.; Wan, W.; Russell, W.K.; Pai, P.-J.; Wang, Z.; Russell, D.H.; Liu, W. Genetic Incorporation of an Aliphatic Keto-Containing Amino Acid into Proteins for Their Site-Specific Modifications. Bioorg. Med. Chem. Lett. 2010, 20, 878–880. [Google Scholar] [CrossRef]
- Kazane, S.A.; Sok, D.; Cho, E.H.; Uson, M.L.; Kuhn, P.; Schultz, P.G.; Smider, V.V. Site-Specific DNA-Antibody Conjugates for Specific and Sensitive Immuno-PCR. Proc. Natl. Acad. Sci. USA 2012, 109, 3731–3736. [Google Scholar] [CrossRef]
- Kazane, S.A.; Axup, J.Y.; Kim, C.H.; Ciobanu, M.; Wold, E.D.; Barluenga, S.; Hutchins, B.A.; Schultz, P.G.; Winssinger, N.; Smider, V.V. Self-Assembled Antibody Multimers through Peptide Nucleic Acid Conjugation. J. Am. Chem. Soc. 2013, 135, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Wold, E.D.; McBride, R.; Axup, J.Y.; Kazane, S.A.; Smider, V.V. Antibody Microarrays Utilizing Site-Specific Antibody–Oligonucleotide Conjugates. Bioconjugate Chem. 2015, 26, 807–811. [Google Scholar] [CrossRef]
- Axup, J.Y.; Bajjuri, K.M.; Ritland, M.; Hutchins, B.M.; Kim, C.H.; Kazane, S.A.; Halder, R.; Forsyth, J.S.; Santidrian, A.F.; Stafin, K.; et al. Synthesis of Site-Specific Antibody-Drug Conjugates Using Unnatural Amino Acids. Proc. Natl. Acad. Sci. USA 2012, 109, 16101–16106. [Google Scholar] [CrossRef]
- Kim, C.H.; Axup, J.Y.; Lawson, B.R.; Yun, H.; Tardif, V.; Choi, S.H.; Zhou, Q.; Dubrovska, A.; Biroc, S.L.; Marsden, R.; et al. Bispecific Small Molecule–Antibody Conjugate Targeting Prostate Cancer. Proc. Natl. Acad. Sci. USA 2013, 110, 17796–17801. [Google Scholar] [CrossRef]
- Kularatne, S.A.; Deshmukh, V.; Ma, J.; Tardif, V.; Lim, R.K.V.; Pugh, H.M.; Sun, Y.; Manibusan, A.; Sellers, A.J.; Barnett, R.S.; et al. A CXCR4-Targeted Site-Specific Antibody–Drug Conjugate. Angew. Chem. Int. Ed. 2014, 53, 11863–11867. [Google Scholar] [CrossRef]
- Kim, C.H.; Axup, J.Y.; Dubrovska, A.; Kazane, S.A.; Hutchins, B.A.; Wold, E.D.; Smider, V.V.; Schultz, P.G. Synthesis of Bispecific Antibodies Using Genetically Encoded Unnatural Amino Acids. J. Am. Chem. Soc. 2012, 134, 9918–9921. [Google Scholar] [CrossRef]
- Hutchins, B.M.; Kazane, S.A.; Staflin, K.; Forsyth, J.S.; Felding-Habermann, B.; Schultz, P.G.; Smider, V.V. Site-Specific Coupling and Sterically Controlled Formation of Multimeric Antibody Fab Fragments with Unnatural Amino Acids. J. Mol. Biol. 2011, 406, 595–603. [Google Scholar] [CrossRef]
- Agarwal, P.; Van Der Weijden, J.; Sletten, E.M.; Rabuka, D.; Bertozzi, C.R. A Pictet-Spengler Ligation for Protein Chemical Modification. Proc. Natl. Acad. Sci. USA 2013, 110, 46–51. [Google Scholar] [CrossRef]
- Kudirka, R.A.; Barfield, R.M.; McFarland, J.M.; Drake, P.M.; Carlson, A.; Bañas, S.; Zmolek, W.; Garofalo, A.W.; Rabuka, D. Site-Specific Tandem Knoevenagel Condensation–Michael Addition To Generate Antibody–Drug Conjugates. ACS Med. Chem. Lett. 2016, 7, 994–998. [Google Scholar] [CrossRef]
- Kudirka, R.; Barfield, R.M.; McFarland, J.; Albers, A.E.; de Hart, G.W.; Drake, P.M.; Holder, P.G.; Banas, S.; Jones, L.C.; Garofalo, A.W.; et al. Generating Site-Specifically Modified Proteins via a Versatile and Stable Nucleophilic Carbon Ligation. Chem. Biol. 2015, 22, 293–298. [Google Scholar] [CrossRef]
- Melnyk, O.; Fehrentz, J.-A.; Martinez, J.; Gras-Masse, H. Functionalization of Peptides and Proteins by Aldehyde or Keto Groups. Pept. Sci. 2000, 55, 165–186. [Google Scholar] [CrossRef]
- El-Mahdi, O.; Melnyk, O. α-Oxo Aldehyde or Glyoxylyl Group Chemistry in Peptide Bioconjugation. Bioconjug. Chem. 2013, 24, 735–765. [Google Scholar] [CrossRef] [PubMed]
- Agten, S.M.; Dawson, P.E.; Hackeng, T.M. Oxime Conjugation in Protein Chemistry: From Carbonyl Incorporation to Nucleophilic Catalysis. J. Pept. Sci. 2016, 22, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Kalia, J.; Raines, R.T. Hydrolytic Stability of Hydrazones and Oximes. Angew. Chem. Int. Ed. 2008, 47, 7523–7526. [Google Scholar] [CrossRef]
- Dong, X.; Obermeyer, A.C.; Olsen, B.D. Three-Dimensional Ordered Antibody Arrays Through Self-Assembly of Antibody–Polymer Conjugates. Angew. Chem. Int. Ed. 2017, 56, 1273–1277. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Z.; Kang, L.; Buuh, Z.Y.; Jiang, D.; McGuth, J.C.; Du, J.; Wissler, H.L.; Cai, W.; Wang, R.E. A Switchable Site-Specific Antibody Conjugate. ACS Chem. Biol. 2018, 13, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Sapozhnikova, K.A.; Misyurin, V.A.; Ryazantsev, D.Y.; Kokin, E.A.; Finashutina, Y.P.; Alexeeva, A.V.; Ivanov, I.A.; Kocharovskaya, M.V.; Tikhonova, N.A.; Popova, G.P.; et al. Sensitive Immunofluorescent Detection of the PRAME Antigen Using a Practical Antibody Conjugation Approach. Int. J. Mol. Sci. 2021, 22, 12845. [Google Scholar] [CrossRef] [PubMed]
- Snyder, J.T.; Malinao, M.-C.; Dugal-Tessier, J.; Atkinson, J.E.; Anand, B.S.; Okada, A.; Mendelsohn, B.A. Metabolism of an Oxime-Linked Antibody Drug Conjugate, AGS62P1, and Characterization of Its Identified Metabolite. Mol. Pharm. 2018, 15, 2384–2390. [Google Scholar] [CrossRef]
- Sapozhnikova, K.A.; Gulyak, E.L.; Brylev, V.A.; Misyurin, V.A.; Oreshkov, S.D.; Alexeeva, A.V.; Ryazantsev, D.Y.; Simonova, M.A.; Ryabukhina, E.V.; Popova, G.P.; et al. Aminooxy Click Modification of a Periodate-Oxidized Immunoglobulin G: A General Approach to Antibody–Drug Conjugates with Dye-Mediated Expeditious Stoichiometry Control. Int. J. Mol. Sci. 2023, 24, 5134. [Google Scholar] [CrossRef]
- Kularatne, S.A.; Deshmukh, V.; Gymnopoulos, M.; Biroc, S.L.; Xia, J.; Srinagesh, S.; Sun, Y.; Zou, N.; Shimazu, M.; Pinkstaff, J.; et al. Recruiting Cytotoxic T Cells to Folate-Receptor-Positive Cancer Cells. Angew. Chem. Int. Ed. 2013, 52, 12101–12104. [Google Scholar] [CrossRef]
- Lim, R.K.V.; Yu, S.; Cheng, B.; Li, S.; Kim, N.-J.; Cao, Y.; Chi, V.; Kim, J.Y.; Chatterjee, A.K.; Schultz, P.G.; et al. Targeted Delivery of LXR Agonist Using a Site-Specific Antibody–Drug Conjugate. Bioconjug. Chem. 2015, 26, 2216–2222. [Google Scholar] [CrossRef]
- Dovgan, I.; Koniev, O.; Kolodych, S.; Wagner, A. Antibody–Oligonucleotide Conjugates as Therapeutic, Imaging, and Detection Agents. Bioconjug. Chem. 2019, 30, 2483–2501. [Google Scholar] [CrossRef]
- Zhang, J.; Ji, D.; Shen, W.; Xiao, Q.; Gu, Y.; O’Shaughnessy, J.; Hu, X. Phase I Trial of a Novel Anti-HER2 Antibody–Drug Conjugate, ARX788, for the Treatment of HER2-Positive Metastatic Breast Cancer. Clin. Cancer Res. 2022, 28, 4212–4221. [Google Scholar] [CrossRef]
- Skidmore, L.; Mills, D.; Kim, J.Y.; Shastri, P.; Knudsen, N.A.; Steen, J.; Nelson, J.; Buechler, Y.; Tian, F.; Zhang, S. Abstract 3997: Preclinical Characterization of ARX517, a next-Generation Anti-PSMA Antibody Drug Conjugate for the Treatment of Metastatic Castration-Resistant Prostate Cancer. Cancer Res. 2023, 83, 3997. [Google Scholar] [CrossRef]
- Zammarchi, F.; Havenith, K.E.; Chivers, S.; Hogg, P.; Bertelli, F.; Tyrer, P.; Janghra, N.; Reinert, H.W.; Hartley, J.A.; Van Berkel, P.H. Preclinical Development of ADCT-601, a Novel Pyrrolobenzodiazepine Dimer-Based Antibody–Drug Conjugate Targeting AXL-Expressing Cancers. Mol. Cancer Ther. 2022, 21, 582–593. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).