Antidepressants as Autophagy Modulators for Cancer Therapy
Abstract
1. Antidepressants in Cancer Therapy
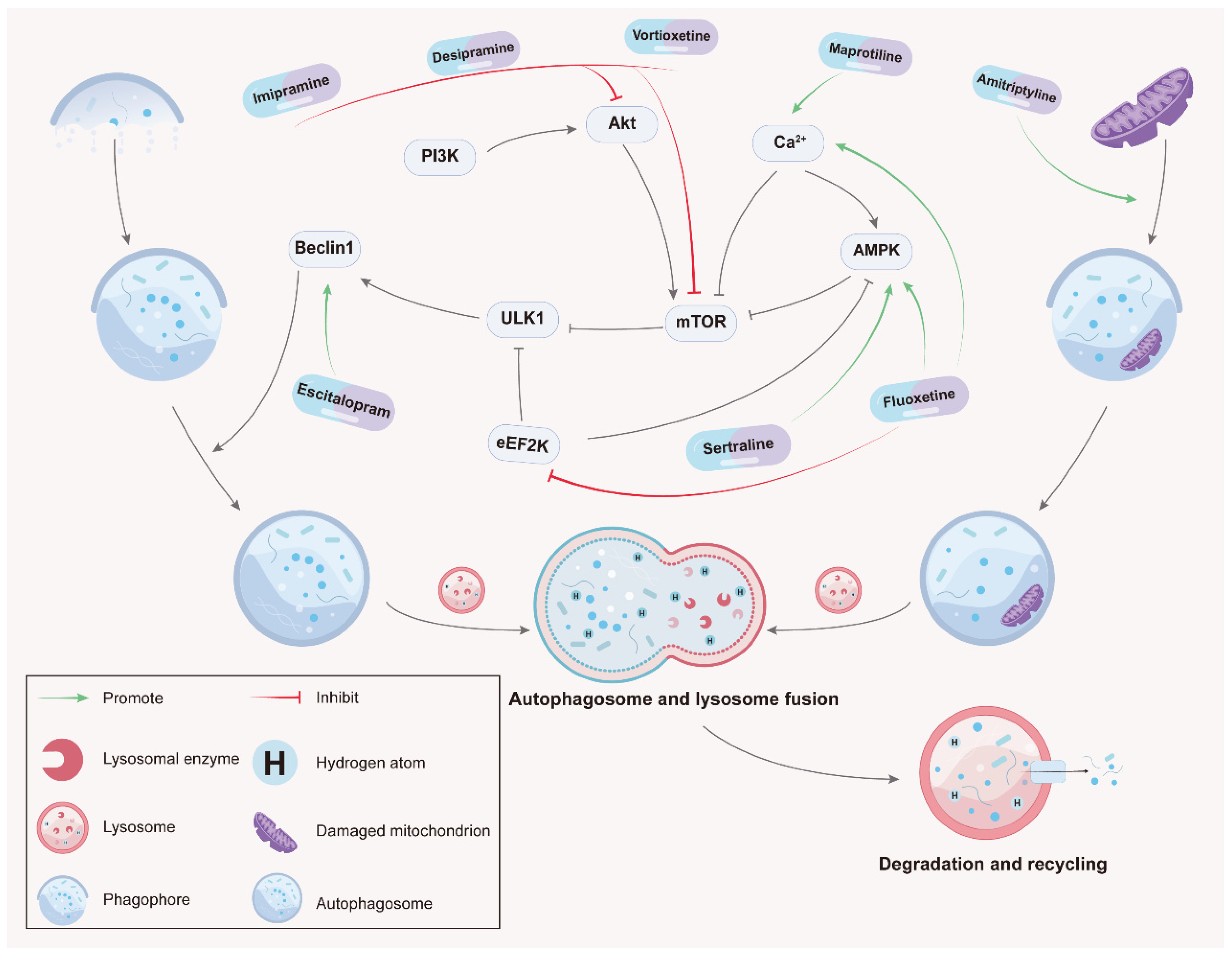
2. Autophagy in Cancer
3. Antidepressants Modulate Autophagy for Tumor Therapy
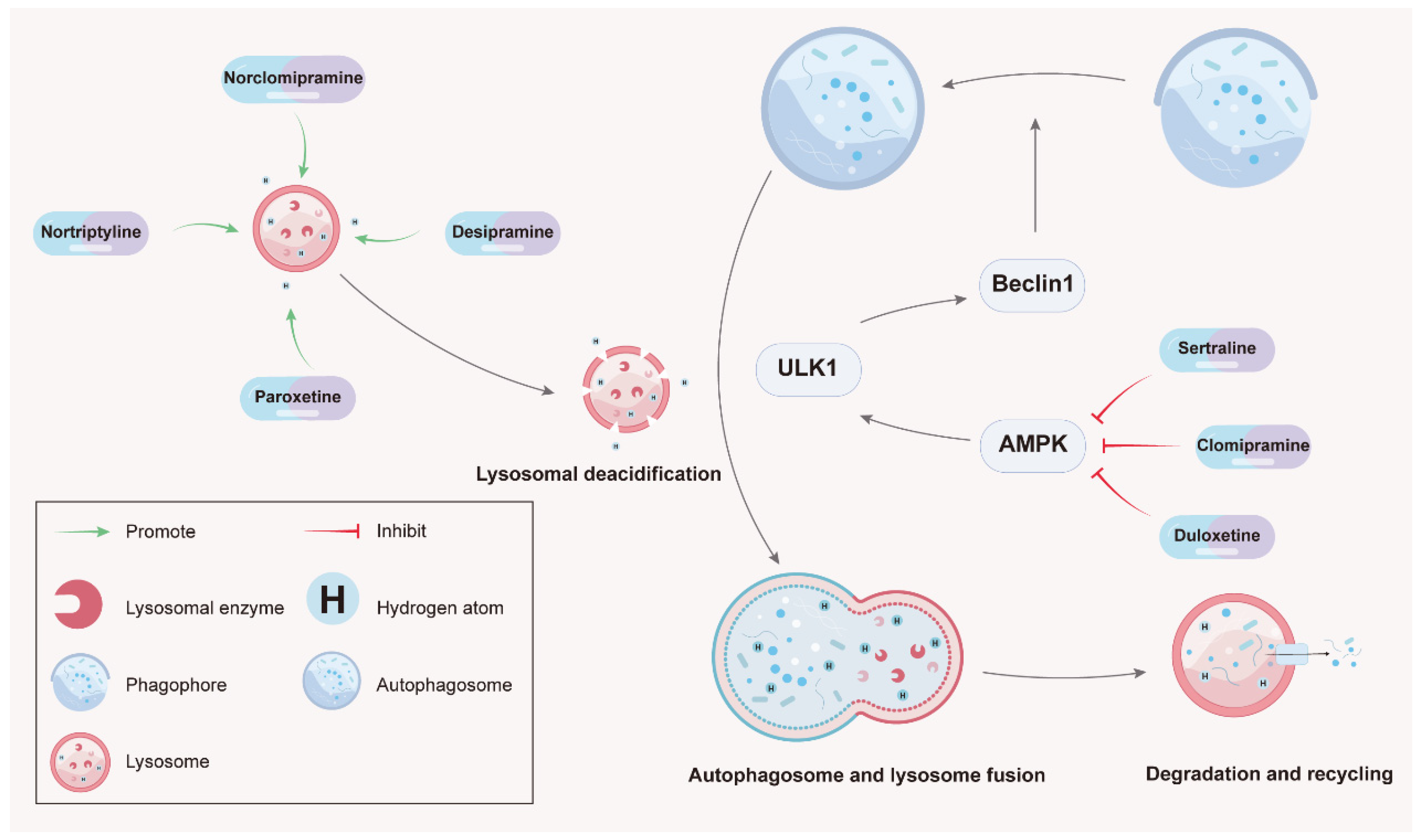
3.1. Tricyclic Antidepressants (TCAs)/Tetracyclic Antidepressants (TeCAs)
3.1.1. Imipramine
3.1.2. Desipramine
3.1.3. Maprotiline
3.1.4. Amitriptyline
3.1.5. Nortriptyline
3.1.6. Clomipramine
3.2. Selective Serotonin Reuptake Inhibitors (SSRIs)
3.2.1. Fluoxetine
3.2.2. Escitalopram
3.2.3. Sertraline
3.2.4. Vortioxetine
3.2.5. Paroxetine
3.3. Serotonin-Norepinephrine Reuptake Inhibitors (SNRsI)
4. Anticancer Antidepressants Investigated for Combinational Treatment and in Clinical Trials
5. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Lutgendorf, S.K.; Andersen, B.L. Biobehavioral approaches to cancer progression and survival: Mechanisms and interventions. Am. Psychol. 2015, 70, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Arrieta, O.; Angulo, L.P.; Nunez-Valencia, C.; Dorantes-Gallareta, Y.; Macedo, E.O.; Martinez-Lopez, D.; Alvarado, S.; Corona-Cruz, J.F.; Onate-Ocana, L.F. Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer. Ann. Surg. Oncol. 2013, 20, 1941–1948. [Google Scholar] [CrossRef] [PubMed]
- Colleoni, M.; Mandala, M.; Peruzzotti, G.; Robertson, C.; Bredart, A.; Goldhirsch, A. Depression and degree of acceptance of adjuvant cytotoxic drugs. Lancet 2000, 356, 1326–1327. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, P.; Lo, C.; Li, M.; Gagliese, L.; Zimmermann, C.; Rodin, G. The relationship between depression and physical symptom burden in advanced cancer. BMJ Support Palliat. Care 2015, 5, 381–388. [Google Scholar] [CrossRef]
- Rodin, G.; Zimmermann, C.; Rydall, A.; Jones, J.; Shepherd, F.A.; Moore, M.; Fruh, M.; Donner, A.; Gagliese, L. The desire for hastened death in patients with metastatic cancer. J. Pain Symptom Manag. 2007, 33, 661–675. [Google Scholar] [CrossRef]
- Satin, J.R.; Linden, W.; Phillips, M.J. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer 2009, 115, 5349–5361. [Google Scholar] [CrossRef]
- Bielecka, A.M.; Obuchowicz, E. Antidepressant drugs as a complementary therapeutic strategy in cancer. Exp. Biol. Med. 2013, 238, 849–858. [Google Scholar] [CrossRef]
- Zheng, Y.; Chang, X.; Huang, Y.; He, D. The application of antidepressant drugs in cancer treatment. Biomed. Pharmacother. 2023, 157, 113985. [Google Scholar] [CrossRef]
- Song, Y.; Yang, X.; Yu, B. Repurposing antidepressants for anticancer drug discovery. Drug Discov. Today 2022, 27, 1924–1935. [Google Scholar] [CrossRef] [PubMed]
- Amaravadi, R.K.; Kimmelman, A.C.; Debnath, J. Targeting Autophagy in Cancer: Recent Advances and Future Directions. Cancer Discov. 2019, 9, 1167–1181. [Google Scholar] [CrossRef] [PubMed]
- Doherty, J.; Baehrecke, E.H. Life, death and autophagy. Nat. Cell Biol. 2018, 20, 1110–1117. [Google Scholar] [CrossRef] [PubMed]
- Xia, H.; Green, D.R.; Zou, W. Autophagy in tumour immunity and therapy. Nat. Rev. Cancer 2021, 21, 281–297. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Green, D.R. Autophagy-Independent Functions of the Autophagy Machinery. Cell 2019, 177, 1682–1699. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.M.M.; Towers, C.G.; Thorburn, A. Targeting autophagy in cancer. Nat. Rev. Cancer 2017, 17, 528–542. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, J.D.; White, E. Autophagy and metabolism. Science 2010, 330, 1344–1348. [Google Scholar] [CrossRef] [PubMed]
- Salimi-Jeda, A.; Ghabeshi, S.; Gol Mohammad Pour, Z.; Jazaeri, E.O.; Araiinejad, M.; Sheikholeslami, F.; Abdoli, M.; Edalat, M.; Abdoli, A. Autophagy Modulation and Cancer Combination Therapy: A Smart Approach in Cancer Therapy. Cancer Treat Res. Commun. 2022, 30, 100512. [Google Scholar] [CrossRef]
- Yun, C.W.; Lee, S.H. The Roles of Autophagy in Cancer. Int. J. Mol. Sci. 2018, 19, 3466. [Google Scholar] [CrossRef]
- Baehrecke, E.H. Autophagy: Dual roles in life and death? Nat. Rev. Mol. Cell Biol. 2005, 6, 505–510. [Google Scholar] [CrossRef]
- Yang, Z.J.; Chee, C.E.; Huang, S.; Sinicrope, F.A. The role of autophagy in cancer: Therapeutic implications. Mol. Cancer Ther. 2011, 10, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Yun, C.W.; Jeon, J.; Go, G.; Lee, J.H.; Lee, S.H. The Dual Role of Autophagy in Cancer Development and a Therapeutic Strategy for Cancer by Targeting Autophagy. Int. J. Mol. Sci. 2020, 22, 179. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.J.; Lei, Y.H.; Yao, N.; Wang, C.R.; Hu, N.; Ye, W.C.; Zhang, D.M.; Chen, Z.S. Autophagy and multidrug resistance in cancer. Chin. J. Cancer 2017, 36, 52. [Google Scholar] [CrossRef] [PubMed]
- Mizushima, N.; Levine, B. Autophagy in Human Diseases. N. Engl. J. Med. 2020, 383, 1564–1576. [Google Scholar] [CrossRef] [PubMed]
- Mowers, E.E.; Sharifi, M.N.; Macleod, K.F. Functions of autophagy in the tumor microenvironment and cancer metastasis. FEBS J. 2018, 285, 1751–1766. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.H.; Kim, S.H.; Kim, Y.; Kim, Y.S.; Lim, Y.; Lee, Y.H.; Shin, S.Y. The tricyclic antidepressant imipramine induces autophagic cell death in U-87MG glioma cells. Biochem. Biophys. Res. Commun. 2011, 413, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Shchors, K.; Massaras, A.; Hanahan, D. Dual Targeting of the Autophagic Regulatory Circuitry in Gliomas with Repurposed Drugs Elicits Cell-Lethal Autophagy and Therapeutic Benefit. Cancer Cell 2015, 28, 456–471. [Google Scholar] [CrossRef]
- Chryplewicz, A.; Scotton, J.; Tichet, M.; Zomer, A.; Shchors, K.; Joyce, J.A.; Homicsko, K.; Hanahan, D. Cancer cell autophagy, reprogrammed macrophages, and remodeled vasculature in glioblastoma triggers tumor immunity. Cancer Cell 2022, 40, 1111–1127.e9. [Google Scholar] [CrossRef]
- Ma, J.; Hou, L.N.; Rong, Z.X.; Liang, P.; Fang, C.; Li, H.F.; Qi, H.; Chen, H.Z. Antidepressant desipramine leads to C6 glioma cell autophagy: Implication for the adjuvant therapy of cancer. Anticancer Agents Med. Chem. 2013, 13, 254–260. [Google Scholar] [CrossRef]
- Cloonan, S.M.; Williams, D.C. The antidepressants maprotiline and fluoxetine induce Type II autophagic cell death in drug-resistant Burkitt’s lymphoma. Int. J. Cancer 2011, 128, 1712–1723. [Google Scholar] [CrossRef]
- Villanueva-Paz, M.; Cordero, M.D.; Pavon, A.D.; Vega, B.C.; Cotan, D.; De la Mata, M.; Oropesa-Avila, M.; Alcocer-Gomez, E.; de Lavera, I.; Garrido-Maraver, J.; et al. Amitriptyline induces mitophagy that precedes apoptosis in human HepG2 cells. Genes Cancer 2016, 7, 260–277. [Google Scholar] [CrossRef] [PubMed]
- Bowie, M.; Pilie, P.; Wulfkuhle, J.; Lem, S.; Hoffman, A.; Desai, S.; Petricoin, E.; Carter, A.; Ambrose, A.; Seewaldt, V.; et al. Fluoxetine induces cytotoxic endoplasmic reticulum stress and autophagy in triple negative breast cancer. World J. Clin. Oncol. 2015, 6, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Zhu, L.; Zhao, Y.; Jiang, Y.; Chen, L.; Yu, Y.; Ouyang, L. Fluoxetine induces autophagic cell death via eEF2K-AMPK-mTOR-ULK complex axis in triple negative breast cancer. Cell. Prolif. 2018, 51, e12402. [Google Scholar] [CrossRef] [PubMed]
- Po, W.W.; Thein, W.; Khin, P.P.; Khing, T.M.; Han, K.W.W.; Park, C.H.; Sohn, U.D. Fluoxetine Simultaneously Induces Both Apoptosis and Autophagy in Human Gastric Adenocarcinoma Cells. Biomol. Ther. 2020, 28, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Zhuang, X.; Zhang, L.; Qiao, T. Antidepressants Fluoxetine Mediates Endoplasmic Reticulum Stress and Autophagy of Non-Small Cell Lung Cancer Cells Through the ATF4-AKT-mTOR Signaling Pathway. Front. Pharmacol. 2022, 13, 904701. [Google Scholar] [CrossRef] [PubMed]
- Chen, V.C.; Hsieh, Y.H.; Chen, L.J.; Hsu, T.C.; Tzang, B.S. Escitalopram oxalate induces apoptosis in U-87MG cells and autophagy in GBM8401 cells. J. Cell Mol. Med. 2018, 22, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.J.; Hsu, T.C.; Chan, H.L.; Lin, C.F.; Huang, J.Y.; Stewart, R.; Tzang, B.S.; Chen, V.C. Protective Effect of Escitalopram on Hepatocellular Carcinoma by Inducing Autophagy. Int. J. Mol. Sci. 2022, 23, 9247. [Google Scholar] [CrossRef] [PubMed]
- Xia, D.; Zhang, Y.T.; Xu, G.P.; Yan, W.W.; Pan, X.R.; Tong, J.H. Sertraline exerts its antitumor functions through both apoptosis and autophagy pathways in acute myeloid leukemia cells. Leuk. Lymphoma 2017, 58, 1–10. [Google Scholar] [CrossRef]
- Chinnapaka, S.; Bakthavachalam, V.; Munirathinam, G. Repurposing antidepressant sertraline as a pharmacological drug to target prostate cancer stem cells: Dual activation of apoptosis and autophagy signaling by deregulating redox balance. Am. J. Cancer Res. 2020, 10, 2043–2065. [Google Scholar]
- Jiang, X.; Lu, W.; Shen, X.; Wang, Q.; Lv, J.; Liu, M.; Cheng, F.; Zhao, Z.; Pang, X. Repurposing sertraline sensitizes non-small cell lung cancer cells to erlotinib by inducing autophagy. JCI Insight 2018, 3, e98921. [Google Scholar] [CrossRef]
- Lv, G.B.; Wang, T.T.; Zhu, H.L.; Wang, H.K.; Sun, W.; Zhao, L.F. Vortioxetine induces apoptosis and autophagy of gastric cancer AGS cells via the PI3K/AKT pathway. FEBS Open Bio 2020, 10, 2157–2165. [Google Scholar] [CrossRef]
- Kuzu, O.F.; Gowda, R.; Noory, M.A.; Robertson, G.P. Modulating cancer cell survival by targeting intracellular cholesterol transport. Br. J. Cancer 2017, 117, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Zinnah, K.M.A.; Park, S.Y. Sensitizing TRAIL-resistant A549 lung cancer cells and enhancing TRAIL-induced apoptosis with the antidepressant amitriptyline. Oncol. Rep. 2021, 46, 144. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.E.D.; Gendoo, D.M.A.; Ghanbari-Azarnier, R.; Liu, J.C.; Jiang, Z.; Tsui, J.; Wang, D.Y.; Xiao, X.; Li, B.; Dubuc, A.; et al. Modeling germline mutations in pineoblastoma uncovers lysosome disruption-based therapy. Nat. Commun. 2020, 11, 1825. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.G.; Yang, J.C.; Kung, H.J.; Shi, X.B.; Tilki, D.; Lara, P.N., Jr.; DeVere White, R.W.; Gao, A.C.; Evans, C.P. Targeting autophagy overcomes Enzalutamide resistance in castration-resistant prostate cancer cells and improves therapeutic response in a xenograft model. Oncogene 2014, 33, 4521–4530. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Munarriz, E.R.; Bartesaghi, S.; Milanese, M.; Dinsdale, D.; Guerra-Martin, M.A.; Bampton, E.T.; Glynn, P.; Bonanno, G.; Knight, R.A.; et al. Desmethylclomipramine induces the accumulation of autophagy markers by blocking autophagic flux. J. Cell Sci. 2009, 122, 3330–3339. [Google Scholar] [CrossRef] [PubMed]
- Zinnah, K.M.A.; Seol, J.W.; Park, S.Y. Inhibition of autophagy flux by sertraline attenuates TRAIL resistance in lung cancer via death receptor 5 upregulation. Int. J. Mol. Med. 2020, 46, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Gong, Q.; Zhan, Y.; Chen, B.; Yin, T.; Lu, Y.; Zhang, Y.; Wang, H.; Ke, J.; Du, B.; et al. Blockage of Autophagic Flux and Induction of Mitochondria Fragmentation by Paroxetine Hydrochloride in Lung Cancer Cells Promotes Apoptosis via the ROS-MAPK Pathway. Front. Cell Dev. Biol. 2019, 7, 397. [Google Scholar] [CrossRef]
- Wang, K.; Chen, B.; Yin, T.; Zhan, Y.; Lu, Y.; Zhang, Y.; Chen, J.; Wu, W.; Zhou, S.; Mao, W.; et al. N-Methylparoxetine Blocked Autophagic Flux and Induced Apoptosis by Activating ROS-MAPK Pathway in Non-Small Cell Lung Cancer Cells. Int. J. Mol. Sci. 2019, 20, 3415. [Google Scholar] [CrossRef]
- Zinnah, K.M.A.; Park, S.Y. Duloxetine Enhances TRAIL-mediated Apoptosis via AMPK-mediated Inhibition of Autophagy Flux in Lung Cancer Cells. Anticancer Res. 2019, 39, 6621–6633. [Google Scholar] [CrossRef]
- Kim, Y.C.; Guan, K.L. mTOR: A pharmacologic target for autophagy regulation. J. Clin. Investig. 2015, 125, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Hua, H.; Kong, Q.; Zhang, H.; Wang, J.; Luo, T.; Jiang, Y. Targeting mTOR for cancer therapy. J. Hematol. Oncol. 2019, 12, 71. [Google Scholar] [CrossRef] [PubMed]
- Justice, M.J.; Bronova, I.; Schweitzer, K.S.; Poirier, C.; Blum, J.S.; Berdyshev, E.V.; Petrache, I. Inhibition of acid sphingomyelinase disrupts LYNUS signaling and triggers autophagy. J. Lipid Res. 2018, 59, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Rozpedek, W.; Pytel, D.; Mucha, B.; Leszczynska, H.; Diehl, J.A.; Majsterek, I. The Role of the PERK/eIF2α/ATF4/CHOP Signaling Pathway in Tumor Progre ssion During Endoplasmic Reticulum Stress. Curr. Mol. Med. 2016, 16, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Rashid, H.-O.; Yadav, R.K.; Kim, H.-R.; Chae, H.-J. ER stress: Autophagy induction, inhibition and selection. Autophagy 2015, 11, 1956–1977. [Google Scholar] [CrossRef] [PubMed]
- Masuda, M.; Miyazaki-Anzai, S.; Levi, M.; Ting, T.C.; Miyazaki, M. PERK-eIF2α-ATF4-CHOP signaling contributes to TNFα-induced vascular ca lcification. J. Am. Heart Assoc. 2013, 2, e000238. [Google Scholar] [CrossRef] [PubMed]
- Eisen, J.N.; Irwin, J.; Quay, J.; Livnat, S. The effect of antidepressants on immune function in mice. Biol. Psychiatry 1989, 26, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Fowler, C.J.; Brannstrom, G. Reduction in beta-adrenoceptor density in cultured rat glioma C6 cells after incubation with antidepressants is dependent upon the culturing conditions used. J. Neurochem. 1990, 55, 245–250. [Google Scholar] [CrossRef]
- Hsu, S.S.; Chen, W.C.; Lo, Y.K.; Cheng, J.S.; Yeh, J.H.; Cheng, H.H.; Chen, J.S.; Chang, H.T.; Jiann, B.P.; Huang, J.K.; et al. Effect of the antidepressant maprotiline on Ca2+ movement and proliferation in human prostate cancer cells. Clin. Exp. Pharmacol. Physiol. 2004, 31, 444–449. [Google Scholar] [CrossRef]
- Von Karstedt, S.; Montinaro, A.; Walczak, H. Exploring the TRAILs less travelled: TRAIL in cancer biology and therapy. Nat. Rev. Cancer 2017, 17, 352–366. [Google Scholar] [CrossRef]
- Chen, M.; He, M.; Song, Y.; Chen, L.; Xiao, P.; Wan, X.; Dai, F.; Shen, P. The cytoprotective role of gemcitabine-induced autophagy associated with apoptosis inhibition in triple-negative MDA-MB-231 breast cancer cells. Int. J. Mol. Med. 2014, 34, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Donohue, E.; Thomas, A.; Maurer, N.; Manisali, I.; Zeisser-Labouebe, M.; Zisman, N.; Anderson, H.J.; Ng, S.S.; Webb, M.; Bally, M.; et al. The autophagy inhibitor verteporfin moderately enhances the antitumor activity of gemcitabine in a pancreatic ductal adenocarcinoma model. J. Cancer 2013, 4, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Pilkington, G.J.; Parker, K.; Murray, S.A. Approaches to mitochondrially mediated cancer therapy. Semin. Cancer Biol. 2008, 18, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Bongiorno-Borbone, L.; Giacobbe, A.; Compagnone, M.; Eramo, A.; De Maria, R.; Peschiaroli, A.; Melino, G. Anti-tumoral effect of desmethylclomipramine in lung cancer stem cells. Oncotarget 2015, 6, 16926–16938. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Rotblat, B.; Ansell, K.; Amelio, I.; Caraglia, M.; Misso, G.; Bernassola, F.; Cavasotto, C.N.; Knight, R.A.; Ciechanover, A.; et al. High throughput screening for inhibitors of the HECT ubiquitin E3 ligase ITCH identifies antidepressant drugs as regulators of autophagy. Cell Death Dis. 2014, 5, e1203. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- White-Gilbertson, S.; Kurtz, D.T.; Voelkel-Johnson, C. The role of protein synthesis in cell cycling and cancer. Mol. Oncol. 2009, 3, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Zhang, Q.; Yang, C.; Xiao, L.; Xue, Z.; Zhu, J. Duloxetine, a Balanced Serotonin-Norepinephrine Reuptake Inhibitor, Improves Painful Chemotherapy-Induced Peripheral Neuropathy by Inhibiting Activation of p38 MAPK and NF-kappaB. Front. Pharmacol. 2019, 10, 365. [Google Scholar] [CrossRef]
- Engelmann, B.J.; Ryan, J.J.; Farrell, N.P. Antidepressants and platinum drugs. Anticancer Res. 2014, 34, 509–516. [Google Scholar]
- Liu, B.H.; Yuan, T.M.; Huang, C.J.; Hsu, D.T.; Chen, S.W.; Hsiao, N.W.; Lin, S.C.; Wu, S.W.; Lin, Y.J.; Chuang, S.M. DNA repair proteins as the targets for paroxetine to induce cytotoxicity in gastric cancer cell AGS. Am. J. Cancer Res. 2022, 12, 1465–1483. [Google Scholar]
- Kabolizadeh, P.; Engelmann, B.J.; Pullen, N.; Stewart, J.K.; Ryan, J.J.; Farrell, N.P. Platinum anticancer agents and antidepressants: Desipramine enhances platinum-based cytotoxicity in human colon cancer cells. J. Biol. Inorg. Chem. 2012, 17, 123–132. [Google Scholar] [CrossRef][Green Version]
- Khing, T.M.; Po, W.W.; Sohn, U.D. Fluoxetine Enhances Anti-tumor Activity of Paclitaxel in Gastric Adenocarcinoma Cells by Triggering Apoptosis and Necroptosis. Anticancer Res. 2019, 39, 6155–6163. [Google Scholar] [CrossRef] [PubMed]
- Duarte, D.; Cardoso, A.; Vale, N. Synergistic Growth Inhibition of HT-29 Colon and MCF-7 Breast Cancer Cells with Simultaneous and Sequential Combinations of Antineoplastics and CNS Drugs. Int. J. Mol. Sci. 2021, 22, 7408. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Duan, J.; Wang, Y.; Chen, X.; Zhou, G.; Wang, R.; Fu, L.; Xu, F. Fluoxetine synergys with anticancer drugs to overcome multidrug resistance in breast cancer cells. Tumour Biol. 2012, 33, 1299–1306. [Google Scholar] [CrossRef]
- Chen, V.C.; Huang, J.Y.; Tzang, B.S.; Hsu, T.C.; McIntyre, R.S. Synergistic Effects of the Combinational Use of Escitalopram Oxalate and 5-Fluorouracil on the Inhibition of Gastric Cancer SNU-1 Cells. Int. J. Mol. Sci. 2022, 23, 16179. [Google Scholar] [CrossRef] [PubMed]
- Drinberg, V.; Bitcover, R.; Rajchenbach, W.; Peer, D. Modulating cancer multidrug resistance by sertraline in combination with a nanomedicine. Cancer Lett. 2014, 354, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Munson, J.M.; Fried, L.; Rowson, S.A.; Bonner, M.Y.; Karumbaiah, L.; Diaz, B.; Courtneidge, S.A.; Knaus, U.G.; Brat, D.J.; Arbiser, J.L.; et al. Anti-invasive adjuvant therapy with imipramine blue enhances chemotherapeutic efficacy against glioma. Sci. Transl. Med. 2012, 4, 127ra136. [Google Scholar] [CrossRef]
- Tatar, O.; Ilhan, N.; Ilhan, N.; Susam, S.; Ozercan, I.H. Is there any potential anticancer effect of raloxifene and fluoxetine on DMBA-induced rat breast cancer? J. Biochem. Mol. Toxicol. 2019, 33, e22371. [Google Scholar] [CrossRef]
- Kabel, A.M.; Elkhoely, A.A. Ameliorative potential of fluoxetine/raloxifene combination on experimentally induced breast cancer. Tissue Cell 2016, 48, 89–95. [Google Scholar] [CrossRef]
- Ma, J.; Yang, Y.R.; Chen, W.; Chen, M.H.; Wang, H.; Wang, X.D.; Sun, L.L.; Wang, F.Z.; Wang, D.C. Fluoxetine synergizes with temozolomide to induce the CHOP-dependent endoplasmic reticulum stress-related apoptosis pathway in glioma cells. Oncol. Rep. 2016, 36, 676–684. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, X.; Wang, X.; Wu, D.; Qi, J.; Zhang, Y.; Wang, K.; Zhou, D.; Meng, Q.M.; Nie, E.; et al. Imipramine impedes glioma progression by inhibiting YAP as a Hippo pathway independent manner and synergizes with temozolomide. J. Cell. Mol. Med. 2021, 25, 9350–9363. [Google Scholar] [CrossRef] [PubMed]
- Ding, R.B.; Chen, P.; Rajendran, B.K.; Lyu, X.; Wang, H.; Bao, J.; Zeng, J.; Hao, W.; Sun, H.; Wong, A.H.; et al. Molecular landscape and subtype-specific therapeutic response of nasopharyngeal carcinoma revealed by integrative pharmacogenomics. Nat. Commun. 2021, 12, 3046. [Google Scholar] [CrossRef] [PubMed]
- Amerio, A.; Gálvez, J.F.; Odone, A.; Dalley, S.A.; Ghaemi, S.N. Carcinogenicity of psychotropic drugs: A systematic review of US Food and Drug Administration-required preclinical in vivo studies. Aust. N. Z. J. Psychiatry 2017, 49, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, G.; Mattioli, F.; Martelli, A. Genotoxic and carcinogenic effects of antipsychotics and antidepressants. Toxicology 2009, 261, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Miguel, C.; Albuquerque, E. Drug interaction in psycho-oncology: Antidepressants and antineoplastics. Pharmacology 2011, 88, 333–339. [Google Scholar] [CrossRef]
- Irarrázaval, O.M.E.; Gaete, G.L. Antidepressants agents in breast cancer patients using tamoxifen: Review of basic and clinical evidence. Rev. Med. Chil. 2016, 144, 1326–1335. [Google Scholar] [CrossRef]
- Stearns, V.; Johnson, M.D.; Rae, J.M.; Morocho, A.; Novielli, A.; Bhargava, P.; Hayes, D.F.; Desta, Z.; Flockhart, D.A. Active tamoxifen metabolite plasma concentrations after coadministrati on of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J. Natl. Cancer Inst. 2003, 95, 1758–1764. [Google Scholar] [CrossRef]
| Antidepressant Types | Cancer Types | Cell Line | Models | Mechanism of Action | Ref. |
|---|---|---|---|---|---|
| Imipramine | Glioma | U-87MG | In vitro | Inhibits Akt/mTOR signaling | [26] |
| Imipramine | Glioma | LN-229; LN-71; LN-443 | In vitro; in vivo | Increases cAMP levels | [27] |
| Imipramine | Glioblastoma | Primary glioblastoma cells | In vitro; in vivo | Induces autophagic flux | [28] |
| Desipramine | Glioma | C6 | In vitro | Inhibits Akt/mTOR signaling; activates PERK-eIF2α-ER stress pathway | [29] |
| Maprotiline | Burkitt’s lymphoma | DG-75 | In vitro | Increases Ca2+ influx | [30] |
| Amitriptyline | Hepatocellular carcinoma | HepG2 | In vitro | Induces Parkin-dependent mitophagy | [31] |
| Fluoxetine | Burkitt’s lymphoma | DG-75 | In vitro | Increases Ca2+ influx | [30] |
| Fluoxetine | Breast cancer | SUM149PT | In vitro | Activates AMPK and inhibits Akt/mTOR signaling; activates PERK-eIF2α-ER stress pathway | [32] |
| Fluoxetine | Breast cancer | MDA-MB-231; MDA-MB-436 | In vitro | Activates AMPK and inhibits mTOR signaling; inhibits eEF2K signaling | [33] |
| Fluoxetine | Gastric cancer | AGS | In vitro | Inhibits Akt/mTOR signaling | [34] |
| Fluoxetine | Lung cancer | H460; A549 | In vitro | Inhibits Akt/mTOR signaling | [35] |
| Escitalopram | Glioblastoma | GBM8401 | In vitro; in vivo | Induces autophagy | [36] |
| Escitalopram | Hepatocellular carcinoma | HepG2; Huh-7 | In vitro; In vivo | Induces autophagy | [37] |
| Sertraline | Acute myeloid leukemia | NB4 | In vitro | Induces autophagy | [38] |
| Sertraline | Prostate cancer | Prostate cancer stem cells | In vitro | Induces autophagy | [39] |
| Sertraline | Lung cancer | A549; H522; PC9/R; H1975 | In vitro; in vivo | Activates AMPK and inhibits mTOR/S6K signaling | [40] |
| Vortioxetine | Gastric cancer | AGS | In vitro | Inhibits AKT/mTOR signaling | [41] |
| Antidepressant Types | Cancer Types | Cell Line | Models | Mechanism of Action | Ref. |
|---|---|---|---|---|---|
| Desipramine | Melanoma | UACC903 | In vitro; in vivo | Inhibits acid sphingomyelinase -mediated intracellular cholesterol transport | [42] |
| Amitriptyline | Lung cancer | A549 | In vitro | Inhibits autophagosome–lysosomal fusion | [43] |
| Nortriptyline | Pineoblastoma | Primary pineoblastoma cells | In vitro; in vivo | Inhibits autophagosome–lysosomal fusion | [44] |
| Clomipramine | Prostate cancer | C4-2B | In vitro; in vivo | Inhibits autophagosome–lysosomal fusion | [45] |
| Norclomipramine | Cervical cancer | HeLa | In vitro | Blocks autophagic cargo degradation | [46] |
| Sertraline | Lung cancer | A549 | In vitro | Inhibits AMPK phosphorylation | [47] |
| Paroxetine | Lung cancer | NCI-H1299; NCI-H1651 | In vitro; in vivo | Inhibits lysosomal acidification | [48] |
| N-methylparoxetine | Lung cancer | NCI-H1299; NCI-H1650 | In vitro | Inhibits lysosomal acidification and lysosomal cathepsins maturation | [49] |
| Duloxetine | Lung cancer | A549 | In vitro | Inhibits AMPK phosphorylation | [50] |
| Drugs | Study Description | Phase | Tumor Types | Start Date | ID |
|---|---|---|---|---|---|
| Imipramine | Imipramine on ER+ and triple-negative breast cancer | I | Breast cancer | July 2019 | NCT03122444 |
| Imipramine | Investigator-initiated study of imipramine hydrochloride and lomustine in recurrent glioblastoma | II | Glioblastoma | May 2022 | NCT04863950 |
| Desipramine | Phase 2a desipramine in small cell lung cancer and other high-grade neuroendocrine tumors | II | Small cell lung cancer; Neuroendocrine tumor | October 2012 | NCT01719861 |
| Maprotiline | A study of maprotiline in combination with tamoxifen and temozolomide for recurrent glioblastoma | I | Glioblastoma | June 2022 | NCT04200066 |
| Nortriptyline | Paclitaxel and nortriptyline hydrochloride in treating patients with relapsed small cell carcinoma | I | Small cell carcinoma | November 2016 | NCT02881125 |
| Fluoxetine | Combination chemotherapy plus fluoxetine in treating patients with advanced or recurrent non-small cell lung cancer | II | Lung cancer | August 2001 | NCT00005850 |
| Fluoxetine | Evaluation of fluoxetine and cytotoxic lysosomal stress in glioma (FLIRT) | I | Brain tumor | August 2023 | NCT05634707 |
| Escitalopram | Escitalopram to placebo in patients with localized pancreatic cancer | II | Pancreatic cancer | August 2022 | NCT05289830 |
| Sertraline | Sertraline and cytosine arabinoside in adults with relapsed and refractory AML | I | Acute myeloid leukemia | August 2016 | NCT02891278 |
| Sertraline | A proof-of-concept clinical trial assessing the safety of the coordinated undermining of survival paths by nine repurposed drugs combined with metronomic temozolomide for recurrent glioblastoma | II | Glioblastoma | November 2016 | NCT02770378 |
| Vortioxetine | Vortioxetine for MDD, cognition, and systemic inflammatory biomarkers | IV | Breast cancer | July 2016 | NCT02637466 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, L.; Fu, Y.; Tian, Y.; Wang, X.; Zhou, X.; Ding, R.-B.; Qi, X.; Bao, J. Antidepressants as Autophagy Modulators for Cancer Therapy. Molecules 2023, 28, 7594. https://doi.org/10.3390/molecules28227594
He L, Fu Y, Tian Y, Wang X, Zhou X, Ding R-B, Qi X, Bao J. Antidepressants as Autophagy Modulators for Cancer Therapy. Molecules. 2023; 28(22):7594. https://doi.org/10.3390/molecules28227594
Chicago/Turabian StyleHe, Leping, Yuanfeng Fu, Yuxi Tian, Xiaofeng Wang, Xuejun Zhou, Ren-Bo Ding, Xingzhu Qi, and Jiaolin Bao. 2023. "Antidepressants as Autophagy Modulators for Cancer Therapy" Molecules 28, no. 22: 7594. https://doi.org/10.3390/molecules28227594
APA StyleHe, L., Fu, Y., Tian, Y., Wang, X., Zhou, X., Ding, R.-B., Qi, X., & Bao, J. (2023). Antidepressants as Autophagy Modulators for Cancer Therapy. Molecules, 28(22), 7594. https://doi.org/10.3390/molecules28227594






