Amphetamine-Related Fatalities and Altered Brain Chemicals: A Preliminary Investigation Using the Comparative Toxicogenomic Database
Abstract
1. Introduction
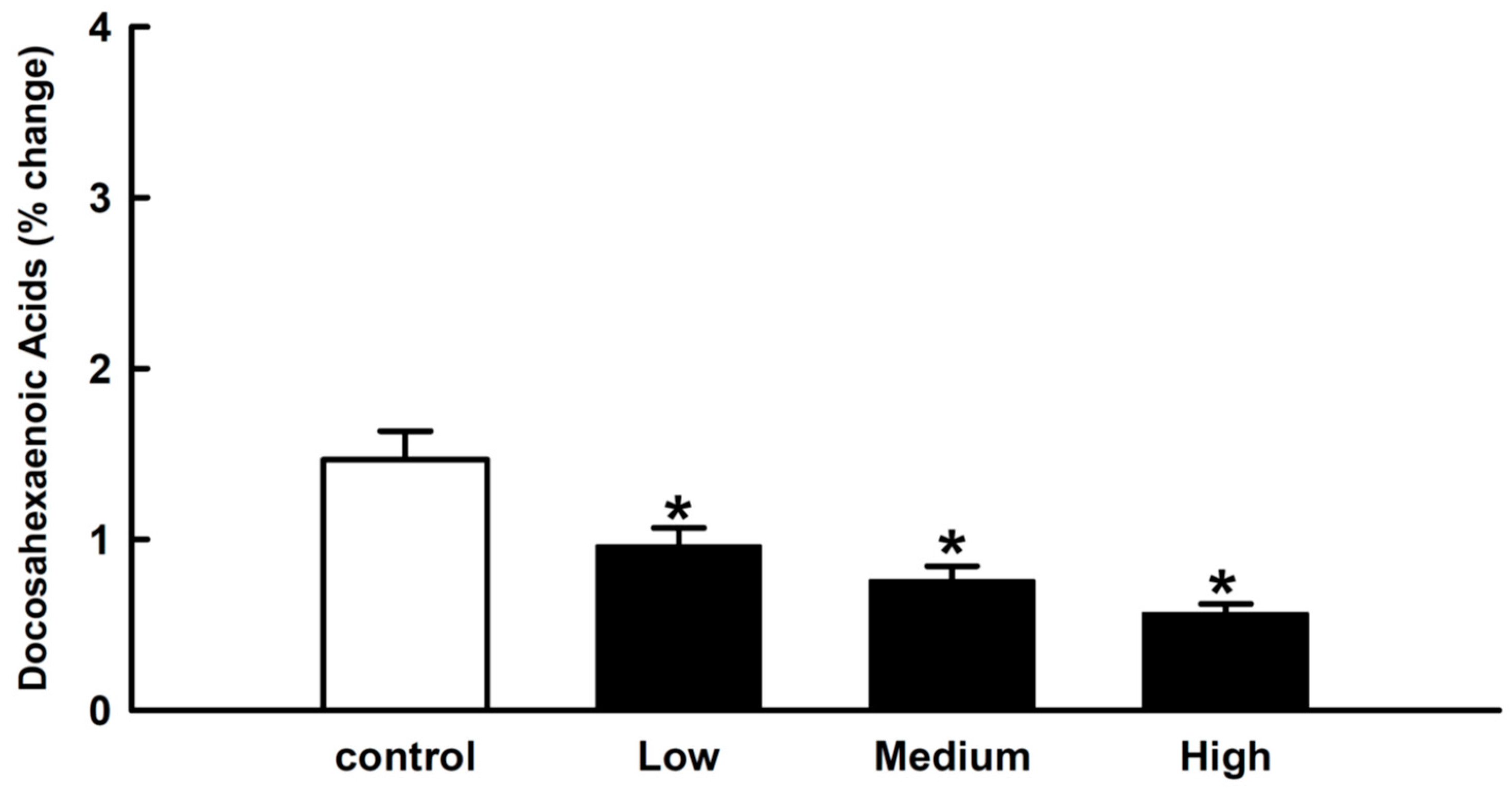
2. Results
3. Discussion
4. Materials and Methods
4.1. Sample Population
4.2. Study Design
4.3. Data Collection
4.4. Bioinformatics Tools and Analysis
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Heal, D.J.; Smith, S.L.; Gosden, J.; Nutt, D.J. Amphetamine, Past and Present—A Pharmacological and Clinical Perspective. J. Psychopharmacol. 2013, 27, 479–496. [Google Scholar] [CrossRef] [PubMed]
- Åhman, A.; Jerkeman, A.; Blomé, M.A.; Björkman, P.; Håkansson, A. Mortality and Causes of Death among People Who Inject Amphetamine: A Long-Term Follow-Up Cohort Study from a Needle Exchange Program in Sweden. Drug Alcohol Depend. 2018, 188, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Al-Haqwi, A.I. Perception among medical students in Riyadh, Saudi Arabia, Regarding Alcohol and Substance Abuse in the Community: A Cross-Sectional Survey. Subst. Abuse Treat. Prev. Policy 2010, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Medhat, B. Substance Use Disorders in Saudi Arabia: Review Article. J. Subst. Use 2013, 18, 450–466. [Google Scholar]
- Attafi, I.M.; Tumayhi, M.M.; Banji, D.; Albeishy, M.Y.; Khardali, I.A.; Korashy, H.M. Analysis of Fatalities Involving Amphetamine in Jazan, Saudi Arabia. Forensic Sci. Int. Rep. 2021, 4, 100237. [Google Scholar] [CrossRef]
- Bramness, J.G.; Gundersen, Ø.H.; Guterstam, J.; Rognli, E.B.; Konstenius, M.; Løberg, E.-M.; Medhus, S.; Tanum, L.; Franck, J. Amphetamine-Induced Psychosis—A Separate Diagnostic Entity or Primary Psychosis Triggered in the Vulnerable? BMC Psychiatry 2012, 12, 221. [Google Scholar] [CrossRef]
- Panenka, W.J.; Procyshyn, R.M.; Lecomte, T.; MacEwan, G.W.; Flynn, S.W.; Honer, W.G.; Barr, A.M. Methamphetamine use: A Comprehensive Review of Molecular, Preclinical and Clinical Findings. Drug Alcohol Depend. 2013, 129, 167–179. [Google Scholar] [CrossRef]
- Metz, V.G.; Segat, H.J.; Dias, V.T.; Barcelos, R.C.S.; Maurer, L.H.; Stiebe, J.; Emanuelli, T.; Burger, M.E.; Pase, C.S. Omega-3 Decreases D1 and D2 Receptors Expression in the Prefrontal Cortex and Prevents Amphetamine-Induced Conditioned Place Preference in Rats. J. Nutr. Biochem. 2019, 67, 182–189. [Google Scholar] [CrossRef]
- Calipari, E.S.; Ferris, M.J. Amphetamine Mechanisms and Actions at the Dopamine Terminal Revisited. J. Neurosci. 2013, 33, 8923–8925. [Google Scholar] [CrossRef]
- Faraone, S.V. The Pharmacology of Amphetamine and Methylphenidate: Relevance to the Neurobiology of Attention-deficit/Hyperactivity Disorder and Other Psychiatric Comorbidities. Neurosci. Biobehav. Rev. 2018, 87, 255–270. [Google Scholar] [CrossRef]
- Robinson, T.E.; Berridge, K.C. The Psychology and Neurobiology of Addiction: An Incentive–Sensitization View. Addiction 2000, 95, 91–117. [Google Scholar]
- Kula, K.; Rojek, S.; Maciów-Głąb, M.; Kopacz, P.; Kłys, M. Medico-Legal Aspect of Amphetamine-Related Deaths. Arch. Med. Sądowej Kryminol./Arch. Forensic Med. Criminol. 2014, 64, 76–101. [Google Scholar] [CrossRef]
- Bowyer, J.F.; Hanig, J.P. Amphetamine-and Methamphetamine-Induced Hyperthermia: Implications of the Effects Produced in Brain Vasculature and Peripheral Organs to Forebrain Neurotoxicity. Temperature 2014, 1, 172–182. [Google Scholar] [CrossRef]
- Song, Y.W.; Lim, Y.; Cho, S.K. 2, 4-Di-Tert-Butylphenol, a Potential HDAC6 Inhibitor, Induces Senescence and Mitotic Catastrophe in Human Gastric Adenocarcinoma AGS cells. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2018, 1865, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, L.; Baxter, A.J.; Lee, Y.Y.; Hall, W.; Sara, G.E.; Johns, N.; Flaxman, A.; Whiteford, H.A.; Vos, T. The Global Epidemiology and Burden of Psychostimulant Dependence: Findings from the Global Burden of Disease Study 2010. Drug Alcohol Depend. 2014, 137, 36–47. [Google Scholar] [CrossRef]
- Bazinet, R.P.; Layé, S. Polyunsaturated Fatty Acids and Their Metabolites in Brain Function and Disease. Nat. Rev. Neurosci. 2014, 15, 771–785. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.K.; Hahn, C.-G.; Jandacek, R.; Rider, T.; Tso, P.; Stanford, K.E.; Richtand, N.M. Selective Deficits in the Omega-3 Fatty Acid Docosahexaenoic Acid in the Postmortem Orbitofrontal Cortex of Patients with Major Depressive Disorder. Biol. Psychiatry 2007, 62, 17–24. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.K.; Jandacek, R.; Rider, T.; Tso, P.; Stanford, K.E.; Hahn, C.-G.; Richtand, N.M. Deficits in Docosahexaenoic Acid and Associated Elevations in the Metabolism of Arachidonic Acid and Saturated Fatty Acids in the Postmortem Orbitofrontal Cortex of Patients with Bipolar Disorder. Psychiatry Res. 2008, 160, 285–299. [Google Scholar] [CrossRef]
- Schneider, M.; Levant, B.; Reichel, M.; Gulbins, E.; Kornhuber, J.; Müller, C.P. Lipids in Psychiatric Disorders and Preventive Medicine. Neurosci. Biobehav. Rev. 2017, 76, 336–362. [Google Scholar] [CrossRef]
- Hamazaki, K.; Hamazaki, T.; Inadera, H. Fatty Acid Composition in the Postmortem Amygdala of Patients with Schizophrenia, Bipolar Disorder, and Major Depressive Disorder. J. Psychiatr. Res. 2012, 46, 1024–1028. [Google Scholar] [CrossRef]
- Marcheselli, V.L.; Hong, S.; Lukiw, W.J.; Tian, X.H.; Gronert, K.; Musto, A.; Hardy, M.; Gimenez, J.M.; Chiang, N.; Serhan, C.N. Novel Docosanoids Inhibit Brain Ischemia-Reperfusion-Mediated Leukocyte Infiltration and Pro-Inflammatory Gene Expression. J. Biol. Chem. 2003, 278, 43807–43817. [Google Scholar] [CrossRef]
- Berman, S.; O’Neill, J.; Fears, S.; Bartzokis, G.; London, E.D. Abuse of Amphetamines and Structural Abnormalities in the Brain. Ann. N. Y. Acad. Sci. 2008, 1141, 195–220. [Google Scholar] [CrossRef] [PubMed]
- Vasan, S.; Olango, G.J. Amphetamine Toxicity. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Heo, H.-J.; Park, Y.-J.; Suh, Y.-M.; Choi, S.-J.; Kim, M.-J.; Cho, H.-Y.; Chang, Y.-J.; Hong, B.; Kim, H.-K.; Kim, E. Effects of Oleamide on Choline Acetyltransferase and Cognitive Activities. Biosci. Biotechnol. Biochem. 2003, 67, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, M.E.; Ng, K.T. Counteractive Effects of Norepinephrine and Amphetamine on Ouabain-Induced Amnesia. Pharmacol. Biochem. Behav. 1977, 6, 533–537. [Google Scholar] [CrossRef] [PubMed]
- Alldredge, B.K.; Lowenstein, D.H.; Simon, R.P. Seizures Associated with Recreational Drug Abuse. Neurology 1989, 39, 1037. [Google Scholar] [CrossRef]
- Wu, C.-F.; Li, C.-L.; Song, H.-R.; Zhang, H.-F.; Yang, J.-Y.; Wang, Y.-L. Selective Effect of Oleamide, an Endogenous Sleepinducing Lipid Amide, on Pentylenetetrazole-Induced Seizures in Mice. J. Pharm. Pharmacol. 2003, 55, 1159–1162. [Google Scholar] [CrossRef]
- Bhattacharjee, A.K.; Chang, L.; Chen, M.; White, L.; Bell, J.M.; Bazinet, R.P.; Rapoport, S.I. Chronic d-Amphetamine Depresses an Imaging Marker of Arachidonic Acid Metabolism in Rat Brain. Int. J. Neuropsychopharmacol. 2008, 11, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Ramkissoon, A.; Wells, P.G. Human Prostaglandin H synthase (hPHS)-1 and hPHS-2 in Amphetamine Analog Bioactivation, DNA Oxidation, and Cytotoxicity. Toxicol. Sci. 2011, 120, 154–162. [Google Scholar] [CrossRef]
- McNamara, R.K. Role of Omega-3 Fatty Acids in the Etiology, Treatment, and Prevention of Depression: Current Status and Future Directions. J. Nutr. Intermed. Metab. 2016, 5, 96–106. [Google Scholar] [CrossRef]
- Yavin, E. Versatile Roles of Docosahexaenoic Acid in the Prenatal Brain: From Pro-and Anti-Oxidant Features to Regulation of Gene Expression. Prostaglandins Leukot. Essent. Fat. Acids 2006, 75, 203–211. [Google Scholar] [CrossRef]
- Jackson, P.A.; Reay, J.L.; Scholey, A.B.; Kennedy, D.O. DHA-Rich Oil Modulates the Cerebral Haemodynamic Response to Cognitive Tasks in Healthy Young Adults: A near IR Spectroscopy Pilot Study. Br. J. Nutr. 2012, 107, 1093–1098. [Google Scholar] [CrossRef]
- Jackson, P.A.; Forster, J.S.; Bell, J.G.; Dick, J.R.; Younger, I.; Kennedy, D.O. DHA Supplementation alone or in Combination with Other Nutrients does not Modulate Cerebral Hemodynamics or Cognitive Function in Healthy Older Adults. Nutrients 2016, 8, 86. [Google Scholar] [CrossRef]
- Yassine, H.N.; Braskie, M.N.; Mack, W.J.; Castor, K.J.; Fonteh, A.N.; Schneider, L.S.; Harrington, M.G.; Chui, H.C. Association of Docosahexaenoic Acid Supplementation with Alzheimer Disease Stage in Apolipoprotein E ε4 Carriers: A review. JAMA Neurol. 2017, 74, 339–347. [Google Scholar] [CrossRef]
- Yanai, H. Effects of N-3 Polyunsaturated Fatty Acids on Dementia. J. Clin. Med. Res. 2017, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Levant, B.; Radel, J.D.; Carlson, S.E. Decreased Brain Docosahexaenoic Acid during Development Alters Dopamine-Related Behaviors in Adult Rats That Are Differentially Affected by Dietary Remediation. Behav. Brain Res. 2004, 152, 49–57. [Google Scholar] [CrossRef]
- Bozzatello, P.; Brignolo, E.; De Grandi, E.; Bellino, S. Supplementation with Omega-3 Fatty Acids in Psychiatric Disorders: A Review of Literature Data. J. Clin. Med. 2016, 5, 67. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.K.; Sullivan, J.; Richtand, N.M.; Jandacek, R.; Rider, T.; Tso, P.; Campbell, N.; Lipton, J. Omega-3 Fatty Acid Deficiency Augments Amphetamine-Induced Behavioral Sensitization in Adult DBA/2J Mice: Relationship with Ventral Striatum Dopamine Concentrations. Synapse 2008, 62, 725–735. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.K.; Sullivan, J.; Richtand, N.M. Omega-3 Fatty Acid Deficiency Augments Amphetamine-Induced Behavioral Sensitization in Adult Mice: Prevention by Chronic Lithium Treatment. J. Psychiatr. Res. 2008, 42, 458–468. [Google Scholar] [CrossRef]
- El-Sisi, A.E.-S.; Sokkar, S.S.; El-Sayad, M.E.-S.; Ramadan, E.S.; Osman, E.Y. Celecoxib and Omega-3 Fatty Acids alone and in Combination with Risperidone Affect the Behavior and Brain Biochemistry in Amphetamine-Induced Model of Schizophrenia. Biomed. Pharmacother. 2016, 82, 425–431. [Google Scholar] [CrossRef]
- Choi, S.J.; Kim, J.K.; Kim, H.K.; Harris, K.; Kim, C.-J.; Park, G.G.; Park, C.-S.; Shin, D.-H. 2, 4-Di-Tert-Butylphenol from Sweet Potato Protects against Oxidative Stress in PC12 Cells and in Mice. J. Med. Food 2013, 16, 977–983. [Google Scholar] [CrossRef]

| Chemicals | Enriched GO (Molecular Function) * | Enriched GO (Biological Process) * |
|---|---|---|
| 1-octadecene, 1-tridecene, 2,4-di-tert-butylphenol, arachidonic acid (AA), docosahexaenoic acid (DHA), eicosane, oleylamide | Protein binding, enzyme binding, ion binding, catalytic activity, oxidoreductase activity | Cellular response to stimulus, cellular process, response to oxygen-containing compound, metabolic process, response to stress |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tumayhi, M.; Banji, D.; Khardali, I.; Banji, O.J.F.; Alshahrani, S.; Alqahtani, S.S.; Muqri, S.; Abdullah, A.; Sherwani, W.; Attafi, I. Amphetamine-Related Fatalities and Altered Brain Chemicals: A Preliminary Investigation Using the Comparative Toxicogenomic Database. Molecules 2023, 28, 4787. https://doi.org/10.3390/molecules28124787
Tumayhi M, Banji D, Khardali I, Banji OJF, Alshahrani S, Alqahtani SS, Muqri S, Abdullah A, Sherwani W, Attafi I. Amphetamine-Related Fatalities and Altered Brain Chemicals: A Preliminary Investigation Using the Comparative Toxicogenomic Database. Molecules. 2023; 28(12):4787. https://doi.org/10.3390/molecules28124787
Chicago/Turabian StyleTumayhi, Murad, David Banji, Ibrahim Khardali, Otilia J. F. Banji, Saeed Alshahrani, Saad S. Alqahtani, Safiah Muqri, Amal Abdullah, Wedad Sherwani, and Ibraheem Attafi. 2023. "Amphetamine-Related Fatalities and Altered Brain Chemicals: A Preliminary Investigation Using the Comparative Toxicogenomic Database" Molecules 28, no. 12: 4787. https://doi.org/10.3390/molecules28124787
APA StyleTumayhi, M., Banji, D., Khardali, I., Banji, O. J. F., Alshahrani, S., Alqahtani, S. S., Muqri, S., Abdullah, A., Sherwani, W., & Attafi, I. (2023). Amphetamine-Related Fatalities and Altered Brain Chemicals: A Preliminary Investigation Using the Comparative Toxicogenomic Database. Molecules, 28(12), 4787. https://doi.org/10.3390/molecules28124787








