Bruch’s-Mimetic Nanofibrous Membranes Functionalized with the Integrin-Binding Peptides as a Promising Approach for Human Retinal Pigment Epithelium Cell Transplantation
Abstract
:1. Introduction
2. Results
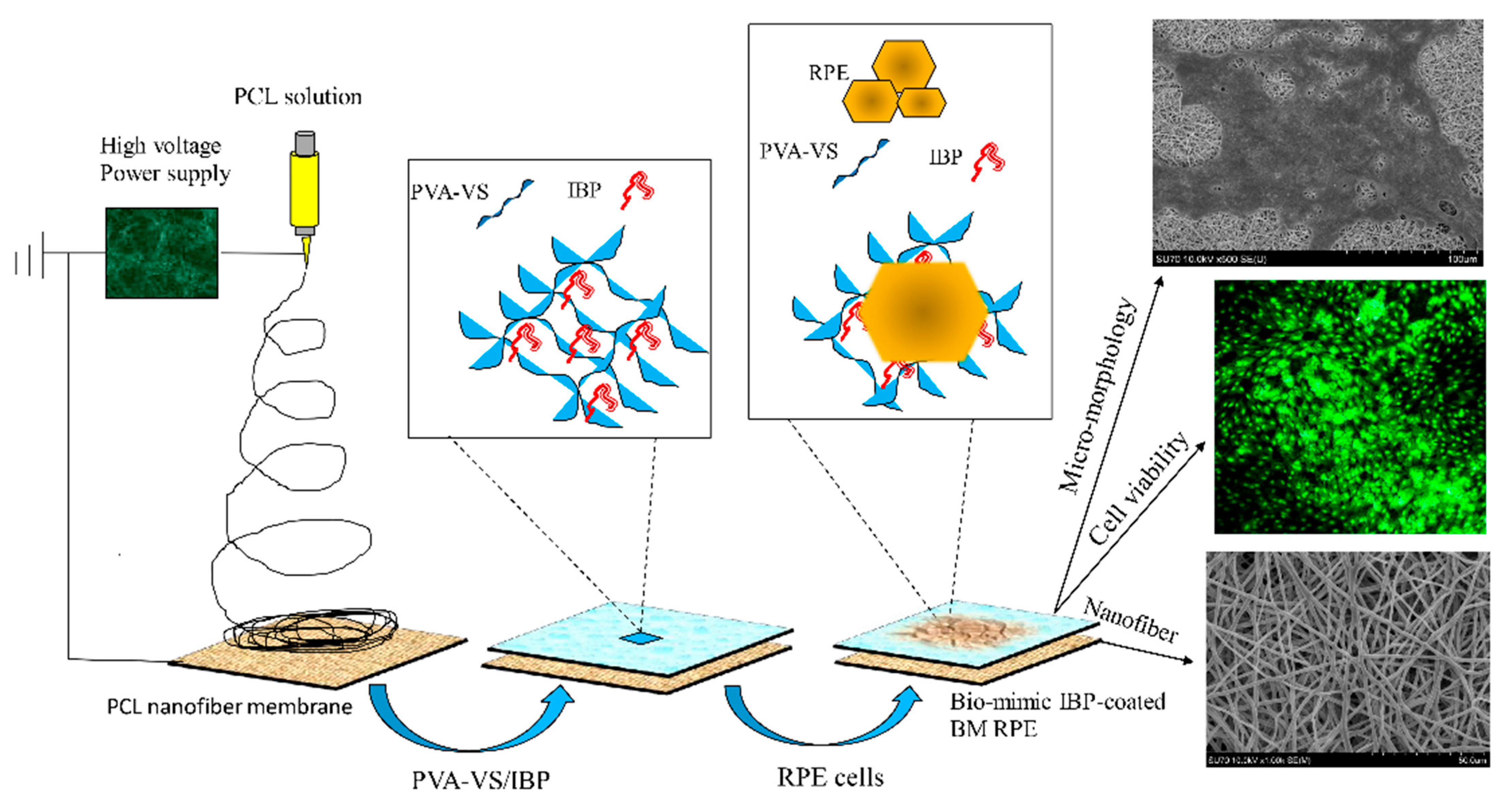
2.1. Characterization of Electrospun Nanofibrous Membranes
2.2. Contact Angle Analysis
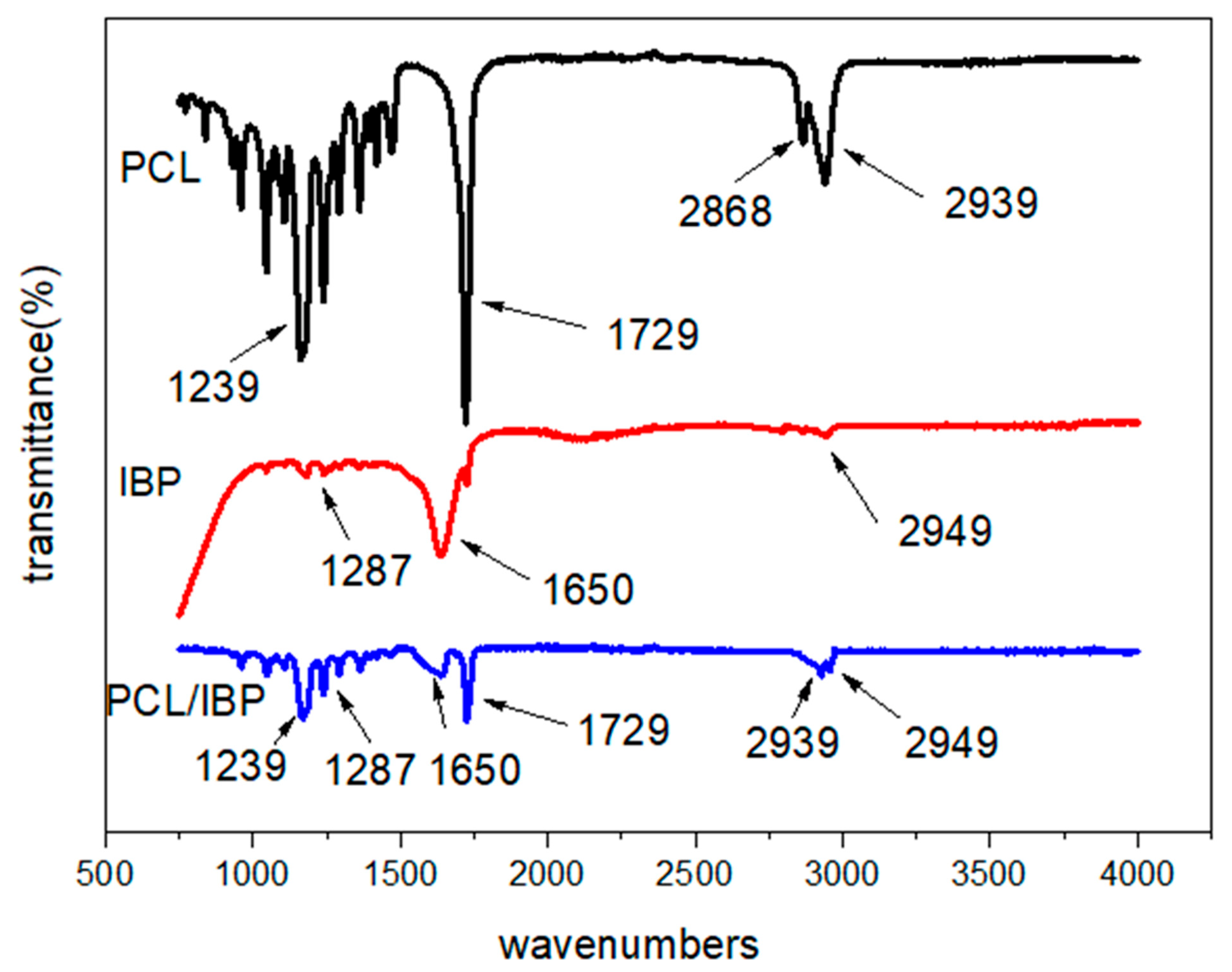
2.3. Chemical Composition of Nanofibrous Membranes
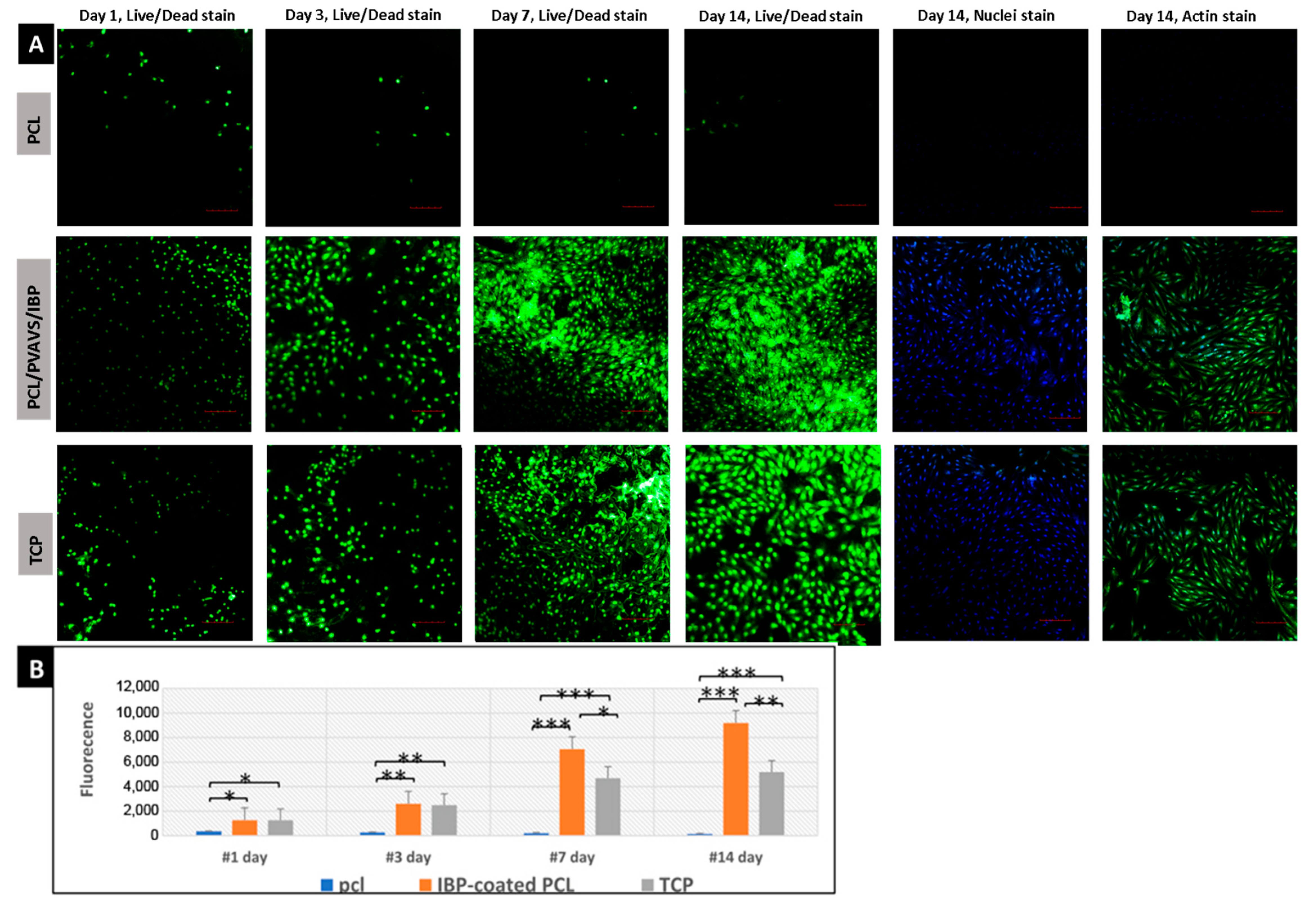
2.4. Biocompatibility Evaluation of Nanofibrous Membranes
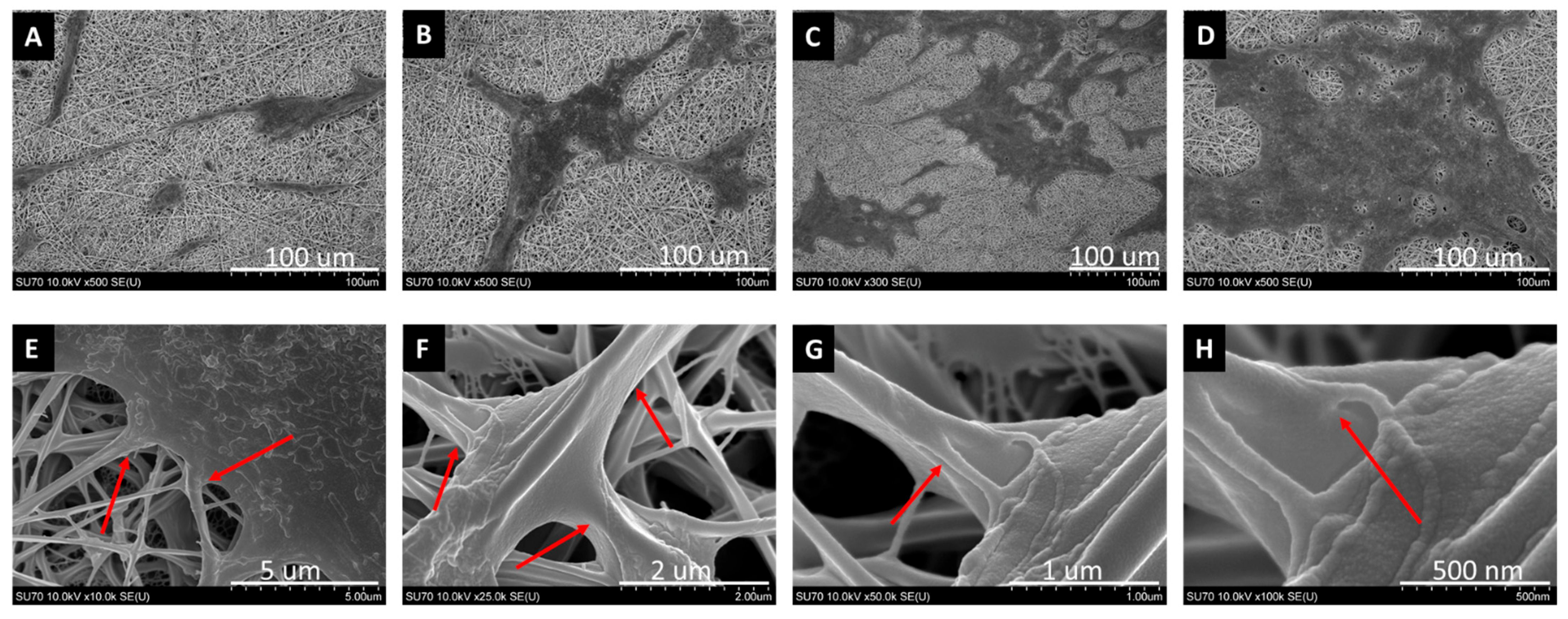
2.5. SEM for Cell Morphology
3. Discussion
4. Materials and Methods
4.1. Materials and Supplies
4.2. Electrospinning of Porous Ultrathin Nanofibrous Membranes
4.3. Modification of Nanofiber Membranes with IBPs
4.4. Surface Morphology Characterization
4.5. Surface Wettability Measurement
4.6. Fourier-Transform Infrared Spectroscopy (FTIR) Analysis
4.7. Cell Culture
4.8. Biocompatibility Test
4.8.1. ARPE-19 Proliferation Assay
4.8.2. Alamar Blue Assay for Cell Viability
4.8.3. Live/Dead Staining
4.8.4. Immunofluorescence Staining
4.8.5. Scanning Electron Microscopic Analysis
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
Abbreviations
| RPE | Retinal pigment epithelial |
| BM | Bruch’s membrane |
| IBP | Integrin-binding peptides |
| AMD | Age-related macular degeneration |
| RP | Retinitis pigmentosa |
| ECM | Extracellular matrix |
| PCL | Poly(ε-caprolactone) |
| PVA-VS | Vinylsulfone functionalized polyvinyl alcohol |
| PEGTA | 4-Arm polyethylene glycol acrylate |
| HFIP | Hexafluoro-2-propanol |
| FE-SEM | Field-emission scanning electron microscopy |
| TCP | Tissue culture polystyrene |
| FTIR | Fourier-transform infrared spectroscopy |
References
- Thomas, C.J.; Mirza, R.G.; Gill, M.K. Age-Related Macular Degeneration. Med. Clin. N. Am. 2021, 105, 473–491. [Google Scholar] [CrossRef] [PubMed]
- Bowes Rickman, C.; LaVail, M.M.; Anderson, E.R.; Grimm, C.; Hollyfield, J.; Ash, J. Retinal Degenerative Diseases: Mechanisms and Experimental Therapy; Springer International Publishing: Cham, Switzerland, 2016; pp. 557–562. [Google Scholar]
- Wong, C.W.; Yanagi, Y.; Lee, W.K.; Ogura, Y.; Yeo, I.; Wong, T.Y.; Cheung, C.M.G. Age-related macular degeneration and polypoidal choroidal vasculopathy in Asians. Prog. Retin. Eye Res. 2016, 53, 107–139. [Google Scholar] [CrossRef] [PubMed]
- Day, S.; Acquah, K.; Lee, P.P.; Mruthyunjaya, P.; Sloan, F.A. Medicare costs for neovascular age-related macular degeneration, 1994–2007. Am. J. Ophthalmol. 2011, 152, 1014–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarbin, M.A. Current concepts in the pathogenesis of age-related macular degeneration. Arch. Ophthalmol. 2004, 122, 598–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, X.; Patel, M.; Chan, C.C. Molecular pathology of age-related macular degeneration. Prog. Retin. Eye Res. 2009, 28, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, M.; Humphries, P. The blood-retina barrier: Tight junctions and barrier modulation. Adv. Exp. Med. Biol. 2012, 763, 70–84. [Google Scholar]
- Qiu, T.G. Transplantation of human embryonic stem cell-derived retinal pigment epithelial cells (MA09-hRPE) in macular degeneration. NPJ Regen. Med. 2019, 4, 19. [Google Scholar] [CrossRef] [Green Version]
- Binder, S.; Stolba, U.; Krebs, I.; Kellner, L.; Jahn, C.; Feichtinger, H.; Povelka, M.; Frohner, U.; Kruger, A.; Hilgers, R.-D.; et al. Transplantation of autologous retinal pigment epithelium in eyes with foveal neovascularization resulting from age-related macular degeneration: A pilot study. Am. J. Ophthalmol. 2002, 133, 215–225. [Google Scholar] [CrossRef]
- Pilotto, E.; Midena, E.; Longhin, E.; Parrozzani, R.; Frisina, R.; Frizziero, L. Müller cells and choriocapillaris in the pathogenesis of geographic atrophy secondary to age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2019, 257, 1159–1167. [Google Scholar] [CrossRef]
- McHugh, K.J.; Tao, S.L.; Saint-Geniez, M. Porous poly(ε-caprolactone) scaffolds for retinal pigment epithelium transplantation. Investig. Ophthalmol. Vis. Sci. 2014, 55, 1754–1762. [Google Scholar] [CrossRef] [Green Version]
- Shirai, H.; Mandai, M.; Matsushita, K.; Kuwahara, A.; Yonemura, S.; Nakano, T.; Assawachananont, J.; Kimura, T.; Saito, K.; Terasaki, H.; et al. Transplantation of human embryonic stem cell-derived retinal tissue in two primate models of retinal degeneration. Proc. Natl. Acad. Sci. USA 2016, 113, E81–E90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curcio, C.A.; Johnson, M. Structure, function, and pathology of Bruch’s membrane. Elastic 2013, 146, 210–213. [Google Scholar]
- Booij, J.C.; Baas, D.C.; Beisekeeva, J.; Gorgels, T.G.; Bergen, A.A. The dynamic nature of Bruch’s membrane. Prog. Retin. Eye Res. 2010, 29, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Treharne, A.J.; Grossel, M.C.; Lotery, A.J.; Thomson, H.A. The chemistry of retinal transplantation: The influence of polymer scaffold properties on retinal cell adhesion and control. Br. J. Ophthalmol. 2011, 95, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yong, T.; Liao, S.; Chan, C.K.; Stevens, M.M.; Ramakrishna, S. Distinctive degradation behaviors of electrospun polyglycolide, poly (DL-lactide-co-glycolide), and poly(L-lactide-co-epsilon-caprolactone) nanofibers cultured with/without porcine smooth muscle cells. Tissue Eng. Part A 2010, 16, 283–298. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, G.R.; Lima, T.H.; Oréfice, R.L.; Fernandes-Cunha, G.M.; Silva-Cunha, A.; Zhao, M.; Behar-Cohen, F. In vitro and in vivo ocular biocompatibility of electrospun poly(ɛ-caprolactone) nanofibers. Eur. J. Pharm. Sci. 2015, 73, 9–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahmoradi, S.; Yazdian, F.; Tabandeh, F.; Soheili, Z.S.; Hatamian Zarami, A.S.; Navaei-Nigjeh, M. Controlled surface morphology and hydrophilicity of polycaprolactone toward human retinal pigment epithelium cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 73, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Fu, K.; Zeng, X.; Chen, N.; Wen, X. Fabrication and Characterization of Composite Meshes Loaded with Antimicrobial Peptides. ACS Appl. Mater. Interfaces 2019, 11, 24609–24617. [Google Scholar] [CrossRef]
- Sun, Y.; Han, F.; Zhang, P.; Zhi, Y.; Yang, J.; Yao, X.; Wang, H.; Lin, C.; Wen, X.; Chen, J.; et al. A synthetic bridging patch of modified co-electrospun dual nano-scaffolds for massive rotator cuff tear. J. Mater. Chem. B 2016, 4, 7259–7269. [Google Scholar] [CrossRef]
- Liu, P.; Chen, N.; Jiang, J.; Wen, X. New surgical meshes with patterned nanofiber mats. RSC Adv. 2019, 9, 17679–17690. [Google Scholar] [CrossRef] [Green Version]
- Huang, D.; Lin, C.; Wen, X.; Gu, S.; Zhao, P. A Potential Nanofiber Membrane Device for Filling Surgical Residual Cavity to Prevent Glioma Recurrence and Improve Local Neural Tissue Reconstruction. PLoS ONE 2016, 11, e0161435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, J.R.; Worthington, K.S.; Green, B.J.; Mullin, N.K.; Jiao, C.; Kaalberg, E.E.; Wiley, L.A.; Han, I.C.; Russell, S.R.; Sohn, E.H.; et al. Two-photon polymerized poly(caprolactone) retinal cell delivery scaffolds and their systemic and retinal biocompatibility. Acta Biomater. 2019, 94, 204–218. [Google Scholar] [CrossRef] [PubMed]
- Beachley, V.; Wen, X. Polymer nanofibrous structures: Fabrication, biofunctionalization, and cell interactions. Prog. Polym. Sci. 2010, 35, 868–892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mousa, S.A.; Lorelli, W.; Campochiaro, P.A. Role of hypoxia and extracellular matrix-integrin binding in the modulation of angiogenic growth factors secretion by retinal pigmented epithelial cells. J. Cell. Biochem. 1999, 74, 135–143. [Google Scholar] [CrossRef]
- Mas-Moruno, C.; Fraioli, R.; Rechenmacher, F.; Neubauer, S.; Kapp, T.; Kessler, H. αvβ3- or α5β1-Integrin-Selective Peptidomimetics for Surface Coating. Angew. Chem. Int. Ed. 2016, 55, 7048–7067. [Google Scholar] [CrossRef]
- Hynes, R. Integrins: Bidirectional, Allosteric Signaling Machines. Cell 2002, 110, 673–687. [Google Scholar] [CrossRef] [Green Version]
- Springer, T.; Dustin, M. Integrin Inside-Out Signalling and the Immunological Synapse. Curr. Opin. Cell Biol. 2011, 24, 107–115. [Google Scholar] [CrossRef] [Green Version]
- Mackay, L.; Khadra, A. The bioenergetics of integrin-based adhesion, from single molecule dynamics to stability of macromolecular complexes. Comput. Struct. Biotechnol. J. 2020, 18, 393–416. [Google Scholar] [CrossRef]
- Aisenbrey, S.; Zhang, M.; Bacher, D.; Yee, J.; Brunken, W.; Hunter, D. Retinal Pigment Epithelial Cells Synthesize Laminins, Including Laminin 5, and Adhere to Them through 3- and 6-Containing Integrins. Investig. Ophthalmol. Vis. Sci. 2007, 47, 5537–5544. [Google Scholar] [CrossRef]
- Afshari, F.; Kwok, J.; Andrews, M.; Blits, B.; Martin, K.; Faissner, A.; Ffrench-Constant, C.; Fawcett, J.W. Integrin activation or alpha9 expression allows retinal pigmented epithelial cell adhesion on Bruch’s membrane in wet age-related macular degeneration. Brain 2010, 133, 448–464. [Google Scholar] [CrossRef] [Green Version]
- Gullapalli, V.; Sugino, I.; Zarbin, M. Culture-induced increase in alpha-integrin subunit expression in retinal pigment epithelium is important for improved resurfacing of aged human Bruch’s membrane. Exp. Eye Res. 2008, 86, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Zarbin, M. Analysis of retinal pigment epithelium integrin expression and adhesion to aged submacular human Bruch’s membrane. Trans. Am. Ophthalmol. Soc. 2003, 101, 499–520. [Google Scholar] [PubMed]
- Oyama, E.; Takahashi, H.; Ishii, K. Effect of amino acids near the RGD sequence on binding activities between alphaIIbbeta3 integrin and fibrinogen in the presence of RGD-containing synthetic peptides from elegantin and angustatin. Peptides 2017, 96, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Zeng, X.; Xue, B.; Campbell, D.; Wang, Y.; Sun, H.; Xu, Y.; Wen, X. Screening of pure synthetic coating substrates for induced pluripotent stem cells and iPSC-derived neuroepithelial progenitors with short peptide based integrin array. Exp. Cell Res. 2019, 380, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Freitas, V.; Vilas Boas, V.; Pimenta, D.; Loureiro, V.; Juliano, M.; Carvalho, M.; Pinheiro, J.J.V.; Camargo, A.C.M.; Moriscot, A.S.; Hoffman, M.P.; et al. SIKVAV, a Laminin α1-Derived Peptide, Interacts with Integrins and Increases Protease Activity of a Human Salivary Gland Adenoid Cystic Carcinoma Cell Line through the ERK 1/2 Signaling Pathway. Am. J. Pathol. 2007, 171, 124–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Liu, X.; Josey, B.; Chou, C.J.; Tan, Y.; Zhang, N.; Wen, X. Short Laminin Peptide for Improved Neural Stem Cell Growth. Stem Cells Transl. Med. 2014, 3, 662–670. [Google Scholar] [CrossRef]
- Seiler, M.; Aramant, R. Cell replacement and visual restoration by retinal sheet transplants. Prog. Retin. Eye Res. 2012, 31, 661–687. [Google Scholar] [CrossRef] [Green Version]
- Lewallen, M.; Xie, T. Cell-based therapies for retinal degenerative diseases: A thousand strategies. J. Glaucoma 2013, 22, S42–S45. [Google Scholar] [CrossRef]
- Cruz, L.; Chen, F.; Ahmado, A.; Greenwood, J.; Coffey, P. RPE transplantation and its role in retinal disease. Prog. Retin. Eye Res. 2007, 26, 598–635. [Google Scholar] [CrossRef]
- Tezel, T.H.; Del Priore, L.V. Reattachment to a substrate prevents apoptosis of human retinal pigment epithelium. Graefes Arch. Clin. Exp. Ophthalmol. 1997, 235, 41–47. [Google Scholar] [CrossRef]
- Tezel, T.H.; Del Priore, L.V. Repopulation of different layers of host human Bruch’s membrane by retinal pigment epithelial cell grafts. Investig. Ophthalmol. Vis. Sci. 1999, 40, 767–774. [Google Scholar]
- Gullapalli, V.; Sugino, I.; Patten, Y.; Shah, S.; Zarbin, M. Impaired RPE survival on aged submacular human Bruch’s membrane. Exp. Eye Res. 2005, 80, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Raudszus, B.; Mulac, D.; Langer, K. A new preparation strategy for surface modified PLA nanoparticles to enhance uptake by endothelial cells. Int. J. Pharm. 2018, 536, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Liao, G.M.; Yang, C.C.; Hu, C.C.; Teng, L.W.; Hsieh, C.H.; Lue, S.J. Optimal loading of quaternized chitosan nanofillers in functionalized polyvinyl alcohol polymer membrane for effective hydroxide ion conduction and suppressed alcohol transport. Polymer 2018, 138, 65–74. [Google Scholar] [CrossRef]
- Nishiyabu, R.; Iizuka, S.; Minegishi, S.; Kitagishi, H.; Kubo, Y. Surface modification of polyvinyl alcohol sponge with functionalized boronic acid to develop porous materials for multicolor emission, chemical sensing and 3D cell culture. Chem. Commun. 2017, 53, 3563–3566. [Google Scholar] [CrossRef]
- Shiohara, A.; Prieto-Simon, B.; Voelcker, N.H. Porous polymeric membranes: Fabrication techniques and biomedical applications. J. Mater. Chem. B 2021, 11, 2129–2154. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.Y.; Kong, J.S.; Lee, H.; Won, J.Y.; Cho, D.W. Development of 3D Printed Bruch’s Membrane-Mimetic Substance for the Maturation of Retinal Pigment Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 1095. [Google Scholar] [CrossRef]
- Karampelas, M.; Sim, D.; Keane, P.; Papastefanou, V.; Sadda, S.; Tufail, A.; Dowler, J. Evaluation of retinal pigment epithelium-Bruch’s membrane complex thickness in dry age-related macular degeneration using optical coherence tomography. Br. J. Ophthalmol. 2013, 97, 1256–1261. [Google Scholar] [CrossRef]
- Andriu, A.; Crockett, J.; Dall’Angelo, S.; Piras, M.; Zanda, M.; Fleming, I.N. Binding of alphavbeta3 integrin-specific radiotracers is modulated by both integrin expression level and activation status. Mol. Imaging Biol. 2018, 20, 27–36. [Google Scholar] [CrossRef] [Green Version]
- Fang, I.M.; Yang, C.H.; Yang, C.M.; Chen, M.S. Overexpression of integrin alpha (6) and beta (4) enhances adhesion and proliferation of human retinal pigment epithelial cells on layers of porcine Bruch’s membrane. Exp. Eye Res. 2008, 88, 12–21. [Google Scholar] [CrossRef]
- Ivins, J.K.; Yurchenco, P.D.; Lander, A.D. Regulation of neurite outgrowth by integrin activation. J. Neurosci. 2000, 20, 6551–6560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arulmoli, J.; Wright, H.J.; Phan, D.T.T.; Sheth, U.; Que, R.A.; Botten, G.A.; Keating, M.; Botvinick, E.L.; Pathak, M.M.; Zarembinski, T.I.; et al. Combination scaffolds of salmon fibrin, hyaluronic acid, and laminin for human neural stem cell and vascular tissue engineering. Acta Biomater. 2016, 43, 122–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, A.; Drinnan, C.T.; Jensen, T.; Finck, C. Production of high purity alveolar-like cells from iPSCs through depletion of uncommitted cells after AFE induction. Differentiation 2017, 96, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.; Yan, Y.; Qi, J.; Deng, L.; Shao, Z.W.; Zhang, K.Q.; Li, B.; Sun, Z.; Li, X. Cooperative Assembly of a Peptide Gelator and Silk Fibroin Afford an Injectable Hydrogel for Tissue Engineering. ACS Appl. Mater. Interfaces 2018, 10, 12474–12484. [Google Scholar] [CrossRef] [PubMed]
- Phelan, M.A.; Kruczek, K.; Wilson, J.H.; Brooks, M.J.; Drinnan, C.T.; Regent, F.; Gerstenhaber, J.A.; Swaroop, A.; Lelkes, P.I.; Li, T. Soy Protein Nanofiber Scaffolds for Uniform Maturation of Human Induced Pluripotent Stem Cell-Derived Retinal Pigment Epithelium. Tissue Eng. Part C Methods 2020, 26, 433–446. [Google Scholar] [CrossRef] [PubMed]
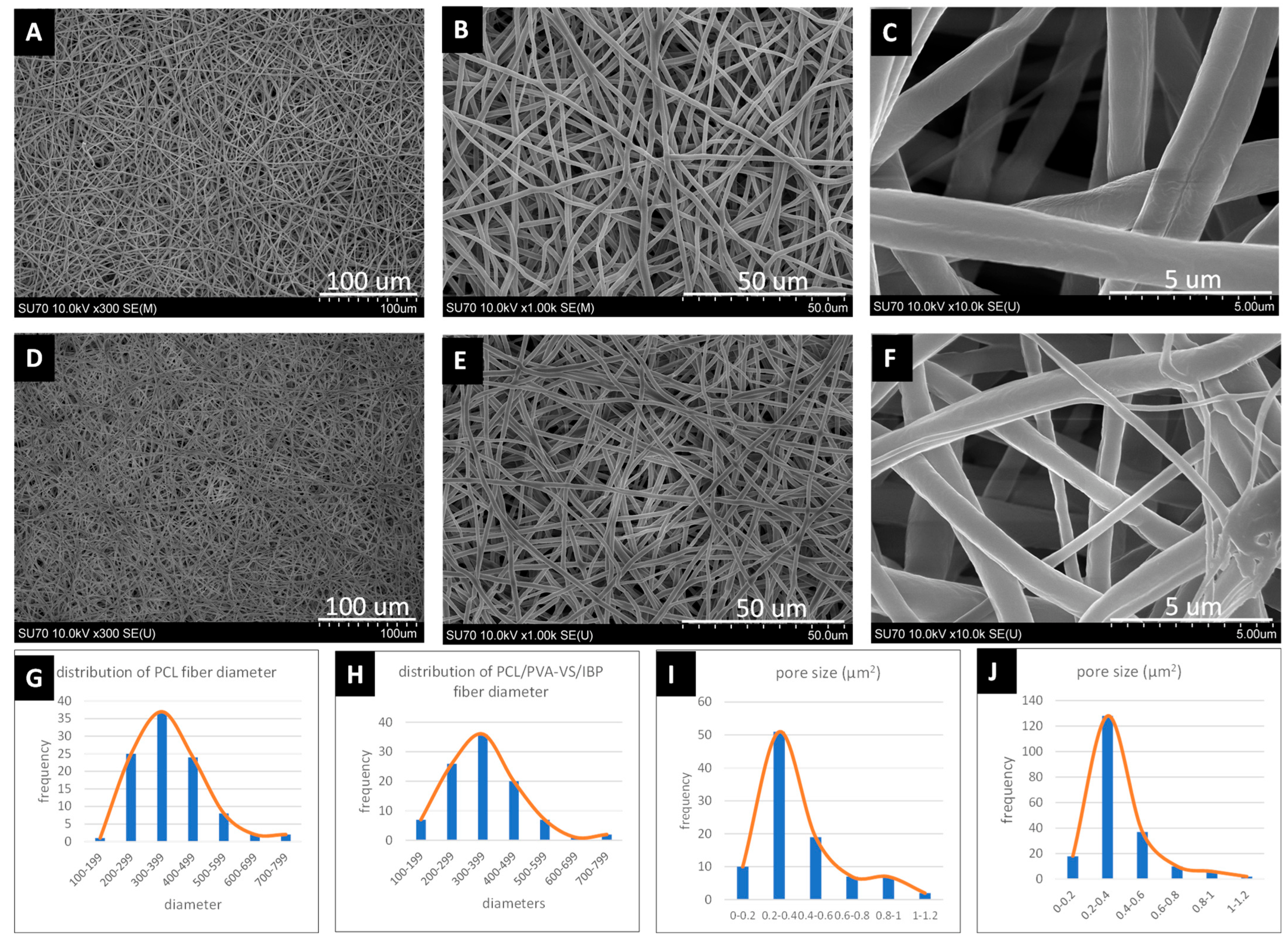

| Nanofibrous Membranes | Fiber Diameter (nm) | Pore Size (μm2) |
|---|---|---|
| PCL | 376.18 ± 79.35 | 0.39 ± 0.21 |
| IBP-coated PCL | 359.04 ± 86.15 | 0.36 ± 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.; Lin, S.; Xue, B.; Wang, C.; Yan, N.; Guan, Y.; Hu, Y.; Wen, X. Bruch’s-Mimetic Nanofibrous Membranes Functionalized with the Integrin-Binding Peptides as a Promising Approach for Human Retinal Pigment Epithelium Cell Transplantation. Molecules 2022, 27, 1429. https://doi.org/10.3390/molecules27041429
Wang S, Lin S, Xue B, Wang C, Yan N, Guan Y, Hu Y, Wen X. Bruch’s-Mimetic Nanofibrous Membranes Functionalized with the Integrin-Binding Peptides as a Promising Approach for Human Retinal Pigment Epithelium Cell Transplantation. Molecules. 2022; 27(4):1429. https://doi.org/10.3390/molecules27041429
Chicago/Turabian StyleWang, Shaocheng, Siyong Lin, Bo Xue, Chenyu Wang, Nana Yan, Yueyan Guan, Yuntao Hu, and Xuejun Wen. 2022. "Bruch’s-Mimetic Nanofibrous Membranes Functionalized with the Integrin-Binding Peptides as a Promising Approach for Human Retinal Pigment Epithelium Cell Transplantation" Molecules 27, no. 4: 1429. https://doi.org/10.3390/molecules27041429
APA StyleWang, S., Lin, S., Xue, B., Wang, C., Yan, N., Guan, Y., Hu, Y., & Wen, X. (2022). Bruch’s-Mimetic Nanofibrous Membranes Functionalized with the Integrin-Binding Peptides as a Promising Approach for Human Retinal Pigment Epithelium Cell Transplantation. Molecules, 27(4), 1429. https://doi.org/10.3390/molecules27041429






