Abstract
Cancer is the second-ranked disease and a cause of death for millions of people around the world despite many kinds of available treatments. Phytochemicals are considered a vital source of cancer-inhibiting drugs and utilize specific mechanisms including carcinogen inactivation, the induction of cell cycle arrest, anti-oxidant stress, apoptosis, and regulation of the immune system. Family Fabaceae is the second most diverse family in the plant kingdom, and species of the family are widely distributed across the world. The species of the Fabaceae family are rich in phytochemicals (flavonoids, lectins, saponins, alkaloids, carotenoids, and phenolic acids), which exhibit a variety of health benefits, especially anti-cancer properties; therefore, exploration of the phytochemicals present in various members of this family is crucial. These phytochemicals of the Fabaceae family have not been explored in a better way yet; therefore, this review is an effort to summarize all the possible information related to the phytochemical status of the Fabaceae family and their anti-cancer properties. Moreover, various research gaps have been identified with directions for future research.
1. Introduction
Cancer is a very dangerous disease and is characterized by the uncontrollable growth of cells. The number of cases and deaths due to cancer is increasing with every passing day (Figure 1). It is difficult to control and has become a major concern for scientists around the world [1]. Many stages (initiation, promotion, and progression) occur in the formation of the cancerous cells [2]. Irregular rates of dietary imbalance, hormonal imbalance, chronic infections, inflammation, and smoking are the major causes of cancer [3]. Despite several treatments to cure cancer, it is still considered the second most devastating cause of death around the world [4,5]. Various methods have been employed to treat cancer, e.g., stem cell transplantation, chemotherapy, radiotherapy, immunotherapy, and surgery. The most effective method to treat cancer is chemotherapy, but various side effects are associated with this method [1,6]. Due to the various side effects of radiotherapy and chemotherapy, alternative treatment methods with no or few side effects are required for the prevention and treatment of cancer [7]. Recently, researchers around the globe have focused their efforts on discovering novel drugs from natural sources such as plants with authentic medicinal importance [8].
Herbal treatment is a natural gift for humans to use to improve their health [9]. Since ancient times, plants and their phytoconstituents have been used as far as medicinal purposes are concerned [10]. Podophyllotoxin was discovered in the 1960s at the same time as when cancer treatments were being searched for from therapeutic plants, which contributed to the discoveries of taxol, vinblastine, camptothecin, and vincristine [11,12,13]. Many plants and their phytochemicals have the potential to control the spread of cancer in the body and continue to attract researchers to examine the anti-cancer activities of various extracted phytochemicals from plant sources [14].
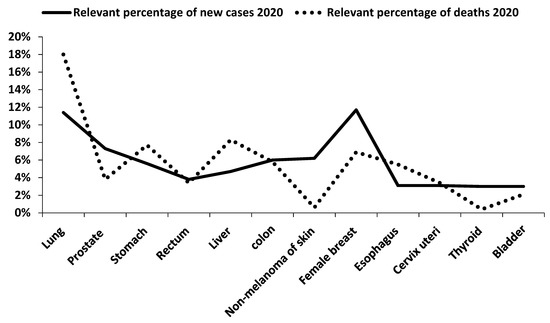
Figure 1.
Relevant percentage of new cases and deaths caused by some major types of cancers in 2020 (Sung et al. [15]).
Kingdom Plantae is characterized by approximately 250,000 plant species; however, the real issue is that only 10% of all plant species have been tested for the treatment of cancer [11,12]. Anti-cancer compounds occur in various plant parts, e.g., leaf, flower, fruits, roots, stigmas, pericarp, embryo, rhizomes, seeds, stem, sprouts, and bark, and these phytochemicals are famous for their role in pharmacology [2]. Different phytochemicals such as flavonoids, alkaloids, saponins, terpenes, lignin, vitamins, minerals, taxanes, gums, biomolecules, glycosides, oils, and various other metabolites are known to show anti-cancer activities [2]. These compounds play a vital role in cancer prevention by activating enzymes and proteins, regulating cellular and signaling events in growth, their anti-inflammatory effect, and anti-oxidant action [12,16].
The Fabaceae family has a diverse fossil record where the late Paleocene period represents the oldest fossil records of the family, which shows the history of the Fabaceae family [17]. Most researchers believe that members of this family have evolved in arid and semiarid regions near the Tethys Sea [18]. These plants have been the main part of meals in these regions since 6000 BC because of their richness in proteins. There is also a history of the use of these plants by humans in Asia, Europe, and North America for medicinal purposes [18,19]. Currently, species of the Fabaceae family occur naturally or are cultivated everywhere around the globe except the poles [18,20]. Different types of beans are used in cuisines due to their richness of proteins and health-promoting activities in the Middle East, Asia, Mexico, and South America [20].
Phytochemicals of this family have industrial and pharmacological importance [21,22]. This family is a big source of phytochemicals, namely, flavonoids, lectins, saponins, alkaloids, carotenoids, and phenolic acids, which have an anti-cancer property, and the use of these phytochemicals is increasing over time [13,23]. However, phytochemicals of this family have not been explored massively for their effect on cancer cell growth. Therefore, more research is needed in the future to explore the potential of phytochemicals of the Fabaceae family against cancer and to discover novel drugs against this disease. Various researchers have worked on anti-cancer aspects of the medicinal plants from the Fabaceae family. This review is the first attempt to explore the potential effects of phytochemicals of the Fabaceae family against cancer cell growth, development, and associated mechanisms. Moreover, research gaps have been explored and future recommendations are given.
2. Development of Cancer and Phytochemical Pathways of Action
Various researches have been conducted over the passing time to understand the exact process of carcinogenesis. Sporn and Liby [24] demonstrated that carcinogenesis is a multistep process, which is divided into three main phases, i.e., initiation, promotion, and finally progression. In most instances, a carcinogen is detoxified within the body as it enters. However, it may be activated through various metabolic pathways. According to Klaunig and Wang [25], carcinogenic agents increase oxidative stress and damage the DNA, and lead to the initiation of carcinogenesis. The proliferation activity of initiated cells starts during the promotion phase and leads to the preneoplastic cells’ accumulation. These preneoplastic cells begin invading and spreading in different parts of the body during the third and the last phase, i.e., the progression phase. The progression phase is irreversible as seen in Figure 2 [26].
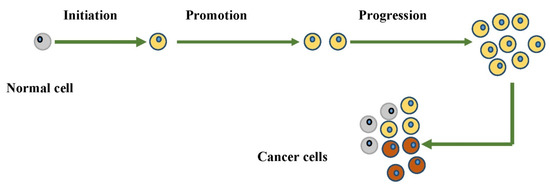
Figure 2.
Diagrammatic representation of carcinogenesis process.
The prevention and treatment of cancer by only one pathway does not turn out to be an effective way due to the involvement of multiple pathways in the occurrence as well as the progression of cancer [27,28]. All the treatment strategies are subjected to a few hindrances, e.g., side effects and drug resistance to chemotherapy [29]. These hindrances have made it difficult for scientists to efficiently develop various treatment strategies related to cancer [30,31]. Chemoprevention is another approach that is widely practiced worldwide, and it is useful during the initiation phase of carcinogenesis, while some have even reported its effectiveness in the promotion and progression phases too [32]. The chemopreventive agents are generally classified into two principal categories, where one group includes blocking agents, while others are suppressive agents majorly sourced from plant phytochemicals [33]. Blocking agents work uniquely; they suppress the carcinogen activation through the metabolic pathway and do not allow carcinogenic agents to interact with the biomolecule. On the other hand, suppressive agents work in another way and suppress the promotion or progression of cancerous cells [34]. The chemopreventive agents usually have an anti-proliferative and anti-oxidant effect or regulate specific enzyme activities and cell cycles. Furthermore, these agents also regulate signal transduction pathways and prevent carcinogenesis [35]. The phytochemicals’ pathway of the anti-cancer effect is presented in Figure 3.
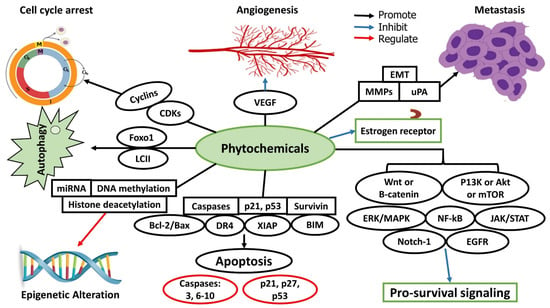
Figure 3.
Phytochemicals’ pathway of anti-cancer effect.
3. Steps Involved in the Development of Phytochemical Drugs from the Medicinal Plants
The quality of active phytochemicals in plants determines their ability to be used as therapeutic agents. Other vital factors, which affect the quality of phytochemicals in plants, are the age of the plants, climate, and season. On the other hand, some plant parts have higher levels of bioactive phytochemicals than others, but more research is needed to improve the knowledge of phytochemicals and how these phytochemicals could be exploited for cancer prevention and treatment (Figure 4). Many techniques can be used to purify the active phytochemical including isolation assays, combinatorial chemistry, and bioassay-guided fractionation [13].
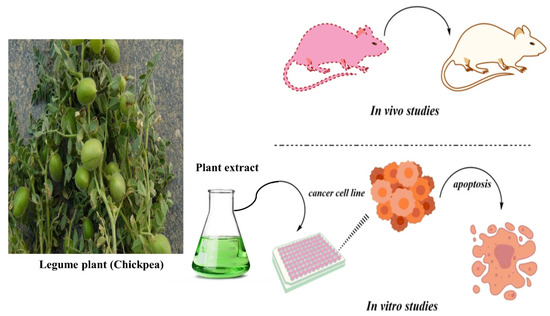
Figure 4.
Assessment of phytochemicals from medicinal plants for anti-cancer activity.
Several analytical techniques can be used for the separation of bioactive compounds from a mixture of compounds in the case of bioassay-guided fractionation. Natural extract tests from the dry or wet plant material serve as the beginning process to evaluate biological activity [13]. For the fractionation of active extract, suitable matrices are utilized, and various analytical techniques, namely, mass spectroscopy, HPLC, TLC, FTIR, and NMR, are used for the separation of active compounds. There is a great variety of solvents that can be used for the separation. For the fractionation, silica, superdex, and other suited matrices can be used. Various dyes can be used to detect the natural bioactive compounds in therapeutic plants. Furthermore, when the purification of these phytochemicals is completed, then these molecules are tested for in vivo or in vitro anti-cancer effects. After achieving anti-cancerous results, other aspects such as pharmacokinetics, metabolic fate, side effects, immunogenicity, pharmacodynamics, dose determination, and drug interaction are focused on for future drug design [4].
4. Major Phytochemical Constituents of the Fabaceae Family
Species of the Fabaceae family are vital sources of phytochemicals, including flavonoids, lectins, saponins, alkaloids, carotenoids, and phenolic acids (Figure 5). These phytochemicals are present in every genus of the Fabaceae family and possess great medicinal values [18,22]. The phytochemicals have gained considerable recognition as far as anti-cancer properties are concerned [13]. However, the phytochemicals of the Fabaceae family have not been explored by various researchers around the world. According to available data, all these phytochemicals have significant anti-cancer values against different forms of cancers in humans (Figure 5). The structures of different phytochemicals found in different members of the Fabaceae family with anti-cancer values are presented in Figure 6.
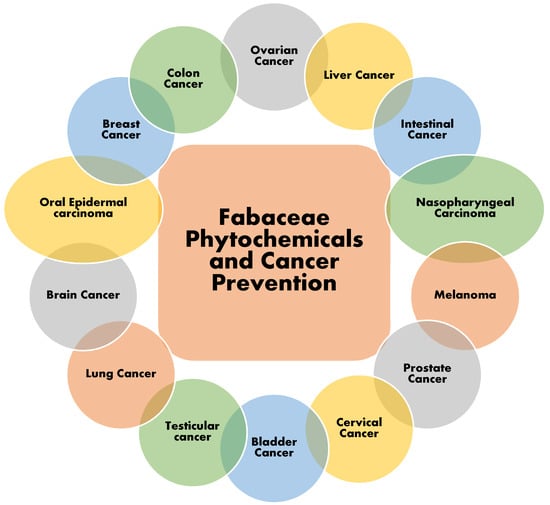
Figure 5.
Reported activity of phytochemicals of family Fabaceae against various types of cancers.
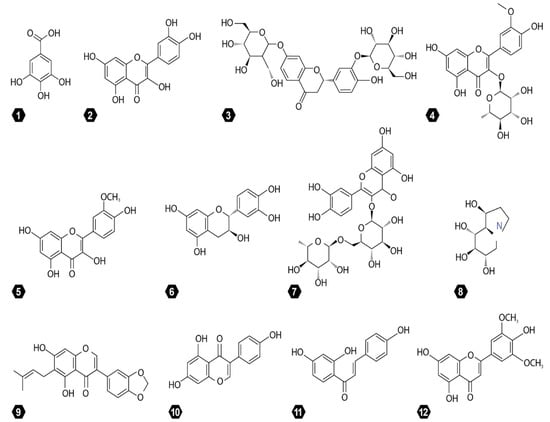
Figure 6.
Structure of main phytochemicals from family Fabaceae. 1. Gallic acid. 2. Quercetin. 3. Butrin. 4. Isorhamnetin-3-O-rhamnoside. 5. Isorhamnetin. 6. Catechin. 7. Rutin. 8. Castanospermine. 9. Derrubone. 10. Genistein. 11. Isoliquiritigenin. 12. Tricin.
Table 1 represents the data of different species of the family Fabaceae that exhibit anti-cancer activities. The major phytochemicals of the family Fabaceae, including alkaloids, flavonoids, carotenoids, lectins, phenolic acid, saponins, and terpenoids, are explored. In total, the anti-cancer activities of the phytochemicals of 71 species are documented in Table 1. The data related to the phytochemicals of the family Fabaceae are scarce as far as anti-cancer activity is concerned. Therefore, the best possible data related to the phytochemical activity of family Fabaceae members against cancer are presented in the table. The details about the importance of each phytochemical are given in the following sections.
4.1. Flavonoids
Flavonoids are considered to be effective anti-oxidants and are known to exhibit anti-angiogenic activity. Various studies have reported that flavonoids inhibit the metabolic activation of carcinogens and stop the further growth of abnormal cells, which may develop into cancerous cells [36]. Flavonoids and their derivatives are considered the vital phytochemical constituents of the Fabaceae family. The most important flavonoids isolated from the various members of the family are chalcone, flavones, flavonol, isoflavones, a flavonol glycoside, prenylated flavonoids, and lavandulyl flavanones [37]. According to Krishna et al. [38], prenylated flavonoids from various members of the Fabaceae family are known to exhibit anti-oxidant and anti-cancer activities.
Earlier, Kleemann et al. [39] reported that flavonoids could be used as a protectant against inflammation, cellular oxidation, and certain cancers. On the other hand, isoflavones extract from legume sprouts had inhibitory properties against breast cancer MCF-7 [13]. Wang et al. [40] also found that the isoflavones extract from Cicer arietinum L. have a repressive effect on MCF-7 breast cancer cells. Flow cytometry results and microscopic observations supported the inhibitory effect on MCF-7 cell lines, and C. arietinum isoflavones with a concentration of 32 µg mL−1 are enough to cause apoptosis of MCF-7.
Clinical studies have confirmed that there is a positive effect of isoflavones on human health by preventing various types of cancer, especially hormone-dependent cancers [41,42]. Eriosema (DC.) Desv. is another important genus in the Fabaceae family with anti-cancer activities. Flavonoids from species such as Eriosema chenense Vogel, E. griseum Baker, and E. robustum Baker have an inhibitory effect against various forms of cancer including lung cancer and oral epidermal carcinoma [43]. Aregueta-Robles et al. [44] found that Phaseolus vulgaris L. extract, as well as its flavonoid contents, have an inhibitory effect on lymphoma in mice both in vivo and in vitro. Flavonoid fraction stopped the production of cancerous cells in a dose-dependent way and, as a result, there was an increase in the cellular population at the S phase after the treatment with flavonoid fraction. Ombra et al. [45] also confirmed that flavonoids from P. vulgaris show considerable anti-cancer properties, and suppress the development of human MCF-7, while flavonoids also showed an inhibitory effect against human epithelial colorectal adenocarcinoma (Caco-3) cells. Moreover, Gatouillat et al. [46] reported the anti-cancer activity from the flavonoids fraction of genus Medicago L. and found that two flavonoids, namely, millepurpan and medicarpin isolated from Medicago sativa L., suppress cancer cells’ proliferation. According to Bora and Sharma [47], millepurpan and medicarpin can be utilized as chemopreventive agents for breast cancer as well as cervical cancer.
Stochmal et al. [48] investigated the role of flavone tricin as a chemopreventive agent sourced from Medicago truncatula Gaertn. It was noticed that tricin in humans caused cell cycle arrest or a growth inhibitory effect on MDA-MB-468 breast cancer. Tricin majorly inhibits the cyclooxygenase enzyme activity; therefore, it regulates the cyclooxygenase-mediated prostaglandin production. Due to this effect, tricin can be exploited as a chemopreventive agent for prostate and intestinal carcinogenesis. Custodio et al. [49] investigated another genus, Ceratonia L., from the Fabaceae family and reported that flavonoids extracted from Ceratonia siliqua L. have an inhibitory effect on tumor cell growth under in vitro conditions. Fu et al. [50] reported a novel flavonoid known as licochalcone-A from the roots of Glycyrrhiza glabra L., and this novel flavonoid leads to late G1 and G2 arrest in androgen-independent PC-3 prostate cancer cells. Choedon et al. [51] determined the effect of butrin extracted from the flowers of Butea monosperma (Lam.) Taub. on liver cancer and found significant results.
4.2. Lectins
Most members of the Fabaceae family are rich in lectin proteins, and communities in various regions use these plants for different diseases due to their anti-cancer and anti-tumor activities [13]. Several studies have confirmed the tumor inhibition mechanisms of lectins in various cell lines including bone, skin, bile duct, and liver cell lines [52,53,54,55,56]. According to De Mejia and Prisecaru [57], various forms of lectins showed anti-cancer properties under in vivo and in vitro conditions. Lectins bind with cancer cell membranes or their receptors resulting in apoptosis and cytotoxicity, and finally suppress the cancer cell growth. Fang et al. [58] assessed the anti-cancer activity of lectin isolated from the Phaseolus vulgaris L. and declared that lectin possesses anti-cancer activities, particularly against MCF-7, nasopharyngeal carcinoma cells (HNE-2, CNE-1, CNE-2), and liver cancer cells (Hep G2). Moreover, P. vulgaris lectin regulates nitric oxide (NO) production through the upregulation of inducible NO synthase known to introduce apoptotic bodies and contribute to the anti-carcinogenic activity. Similar results were confirmed by Lam and Ng [59] while working on the anti-cancer properties of lectin isolated from P. vulgaris.
Ye and Ng [60] demonstrated that lectin from Glycine max (L.) Merr. possesses anti-tumor properties for breast cancer and hepatoma cells. C. arietinum is a rich source of lectin and has a long history of medicinal use in several parts of India as it exhibits strong cancer chemopreventive activity [61]. Une et al. [62] purified the lectin from Canavalia gladiata (Jacq.) DC. using the DEAE-sephacel column and affinity chromatography and confirmed chemopreventive activity. Cavada et al. [63] found that Conyza bonariensis L. contains a considerable amount of lectin, which inhibits the process of carcinogenesis. According to Arteaga et al. [64], the proliferation of colon cancer cells is greatly inhibited by the lectin isolated from Phaseolus acutifolius A. Gray. Gondim et al. [65] evaluated the anti-cancer activity of seed isolated DLasiL lectin of Dioclea lasiocarpa Mart. Ex Benth. The experiments showed that DLasiL lectin was effective against PC-3 prostate cancer, A-2780 ovarian, and MCF-7 breast cancer cell lines.
Lagarda-Diaz et al. [66] stated that legume lectins showed anti-oxidant and anti-cancer activities. Legume lectins inhibit cell proliferation in lung cancer, and the consumption of legume lectins contributes to immunity against different forms of cancer. Korourian et al. [67] used Griffonia simplicifolia (DC.) Baill. lectin-1 (GS 1) to suppress the progression of human breast ductal carcinoma and found significant results.

Table 1.
Phytochemicals of family Fabaceae and suppression of particular cancer types.
Table 1.
Phytochemicals of family Fabaceae and suppression of particular cancer types.
| S. No. | Species | Genus | Phytochemicals | Targeted Cancer | References |
|---|---|---|---|---|---|
| 1 | Acacia nilotica (L.) Willd. eX Del. | Acacia | Gallic acid | Not specified | [68] |
| 2 | Acacia hydaspica R. parker | Acacia | Alkaloids, flavonoids, and saponin | Not specified | [69] |
| 3 | Acacia saligna (Labill.) H.L.Wendl. | Acacia | Flavonoids and saponin | Hep G2 cancer (liver cancer) | [70,71] |
| 4 | Acacia seyal Delile | Acacia | Lectin | Hepatocellular carcinoma, HEP-2 (Larynx Cancer), HCT116 (colon cancer), and MCF-7 (breast cancer) | [72] |
| 5 | Acacia victoriae Benth. | Acacia | Avicins and Fo35 | Breast cancer | [73] |
| 6 | Albizia lebbeck (L.) Benth. | Albizia | Saponins, flavonoids | Liver, larynx, breast, cervical, and colon cancer | [74,75] |
| 7 | Albizia chinensis (Osbeck) Merr. | Albizia | Quercetin (Flavonoid) | Myeloid leukemia | [76,77] |
| 8 | Albizia Julibrissin Baker | Albizia | Alkaloids, saponins, and flavonoids | Leukemia | [78,79,80] |
| 9 | Astragalus ovinus Boiss. | Astragalus | Phenolics, flavonoids | Breast cancer in rats | [81] |
| 10 | Astragalus spinosus (Forssk.) Muschl. | Astragalus | Flavonoids | Not specified | [82] |
| 11 | Astragalus membranaceus (Fisch.) Bunge | Astragalus | Flavonoids, saponins | Breast cancer | [83] |
| 12 | Bauhinia acuminata L. | Bauhinia | Alkaloids, flavonoids | Lung cancer | [84] |
| 13 | Bauhinia variegata (L.) Benth. | Bauhinia | Alkaloids, Kaempferol galactoside, saponins | Liver, lung, breast cancer (both in vitro and in vivo), and human ovarian cancer (in vivo) | [85,86,87] |
| 14 | Bauhinia purpurea L. | Bauhinia | Lectin | MCF-7 (breast cancer) | [88] |
| 15 | Butea monosperma (Lam.) Taub. | Butea | Butrin | Liver cancer | [51] |
| 16 | Caesalpinia bonduc (L.) Roxb | Caesalpinia | Alkaloids | Not specified | [89] |
| 17 | Caesalpinia gilliesii (Hook.) D.Dietr | Caesalpinia | Isorhamnetin, Isorhamnetin-3-O-rhamnoside (flavonoids) | MCF-7 (breast cancer) and HepG2 cancer (liver cancer) | [90] |
| 18 | Caesalpinia pluviosa DC. | Caesalpinia | Caesalpinioflavone | A549 (lung adenocarcinoma), MCF-7, and Hst578T (breast cancer) | [91] |
| 19 | Caesalpinia pulcherrima (L.) Sw. | Caesalpinia | Catechin, Gallic acid, quercetin, Rutin | Breast cancer | [92] |
| 20 | Cajanus cajan (L.) Millsp. | Cajanus | Flavanones | CaCo-2 (colorectal) HeLa (cervical), and MCF-7 (breast cancer) cancer | [93,94,95] |
| 21 | Canavalia gladiata (Jacq.) DC. | Canavalia | Lectin | Not specified | [62] |
| 22 | Cassia occidentalis (L.) Link | Cassia | Alkaloids, flavonoids, saponins | HCT-15, SW-620 (colon cancer), OVCAR-5 (ovarian cancer), SiHa (cervical cancer), PC-3 (prostate cancer, and MCF-7 (breast cancer) | [96,97] |
| 23 | Castanospermum australe A.Cunn. eX mudie | Castanospermum | Castanospermine | Not specified | [98] |
| 24 | Ceratonia siliqua L. (carob) | Ceratonia | Flavonoids | Not specified | [99] |
| 25 | Cicer arietinum L. | Cicer | Isoflavones | Breast cancer | [40] |
| 26 | Conyza bonariensis L. | Conyza | Lectin | Not specified | [63] |
| 27 | Cytisus villosus Pourr. | Cytisus | Flavonols, flavones | Breast and colon cancer | [100] |
| 28 | Derris scandens Roxb. (Benth.) | Derris | Glyurallin, derrubone, derriscandenon B and C (isoflavones) | HT29 (colon cancer) | [95,101] |
| 29 | Dioclea lasiocarpa Mart. eX Benth. | Dioclea | Lectin DLasiL | Breast, prostate, and ovarian cancer | [65] |
| 30 | Eriosema chinense Vogel | Eriosema | Isoflavone, flavonols | Lung cancer and oral epidermal carcinoma | [43] |
| 31 | Eriosema griseum Baker | Eriosema | Flavonols, flavanones | Lung cancer and oral epidermal carcinoma | [43] |
| 32 | Erythrina senegalensis DC | Erythrina | Alkaloids, flavonoids | Breast, cervical, colon, liver, lung cancer, and leukemia | [102] |
| 33 | Gleditsia triacanthos L. | Gleditsia | Flavones | Liver, breast, cervical, larynx, and colon cancer | [103] |
| 34 | Gleditsia caspica Desf. | Gleditsia | Saponins | MCF-7 (breast cancer) | [77] |
| 35 | Gleditsia sinensis Lam. | Gleditsia | Saponins | MCF-7 (breast cancer) | [104] |
| 36 | Glycine max (L.) Merr. | Glycine | Lectin, genistein (Isoflavones), saponins | Breast and liver cancer | [60,67] |
| 37 | Glycyrrhiza uralensis Fisch. eX DC. | Glycyrrhiza | Isoliquiritigenin | Human lung cancer (in vitro) | [105] |
| 38 | Glycyrrhiza glabra L. | Glycyrrhiza | Alkaloids, flavonoids, saponins | Breast, colon, liver, and prostate cancer | [50,106] |
| 39 | Griffonia simplicifolia (DC.) Baill. | Griffonia | Lectin-1 | Breast cancer | [67] |
| 40 | Indigofera tinctoria L. | Indigofera | Flavonoids, phenolic compounds, Saponins | Lung cancer | [107,108,109] |
| 41 | Indigofera cassioides Rottl. Ex. Dc. | Indigofera | Flavonoids, saponins, terpenoids | Breast and colon cancer (in vitro and in vivo) | [110] |
| 42 | Indigofera aspalathoides (Vahl.) | Indigofera | Alkaloids, flavonoids, saponins | Cervical cancer | [111] |
| 43 | Indigofera cordifolia B.Heyne eX Roth | Indigofera | Alkaloids, flavonoids, saponins | Human breast, cervical, liver, and lung cancer | [112] |
| 44 | Indigofera suffruticosa Mill. | Indigofera | Alkaloids, flavonoids, lectin | Not specified | [113] |
| 45 | Laburnum anagyroides Medik. | Laburnum | Cytisine | Lung cancer | [114] |
| 46 | Medicago arabica (L.) Huds. | Medicago | Saponins | HeLa (cervical cancer) | [115] |
| 47 | Medicago Sativa L. | Medicago | Alkaloids, millepurpan, medicarpin (flavonoids), saponins | Breast and cervical cancer | [46,116,117,118] |
| 48 | Medicago truncatula Gaertn. | Medicago | Tricin (flavone) | Breast cancer, intestinal carcinogenesis and prostate cancer | [48] |
| 49 | Melilotus officinalis (Linn.) Pall. | Melilotus | Saponins | Prostate cancer | [119] |
| 50 | Melilotus indicus (L.) All. | Melilotus | Flavonoids | Hepatocellular carcinoma | [120] |
| 51 | Parkia javanica Lam. | Parkia | Alkaloids, flavonoids, saponins | Human liver cancer | [121] |
| 52 | Phaseolus vulgaris L. | Phaseolus | Galic acid, lectin | Breast cancer, colon cancer, Epithelial colorectal adenocarcinoma, liver cancer, and nasopharyngeal carcinoma | [45,58] |
| 53 | Phaseolus Acutifolius A. Gray | Phaseolus | Lectin | Colon cancer | [64] |
| 54 | Physostigma venenosum Balf. | Physostigma | Physostigmine alkaloid or eserine | Not specified | [122] |
| 55 | Prosopis juliflora (Sw.) DC. | Prosopis | Alkaloids | Leukemia | [123,124] |
| 56 | Prosopis cineraria (L.) Druce | Prosopis | Alkaloids, flavonoids, phenolic aicd, saponins | Hepatocellular carcinoma | [125,126] |
| 57 | Pseudarthria hookeri Wight & Arn. | Pseudarthria | Flavanones, flavones, isoflavone | Epithelial colorectal adenocarcinoma (CaCo-2), Leukemia, lung adenocarcinoma (A549), and human ovarian carcinoma (Skov-2) | [127] |
| 58 | Psoralea corylifolia L. | Psoralea | Neobavaisoflavone (flavonoids) | Colon cancer and leukemia | [128] |
| 59 | Senna alexandrina Mill. | Senna | Flavonoids | Liver cancer | [129] |
| 60 | Sesbania grandiflora (L.) poiret | Sesbania | Alkaloids, flavonoids, and saponins | Colon cancer | [130,131] |
| 61 | Sophora tonkinensis Gagnep. | Sophora | Isoflavones | Breast cancer | [132] |
| 62 | Sophora flavescens Aiton | Sophora | Oxymatrine (Alkaloid) | Cervical, colorectal, gastric, human hepatoma carcinoma, lung, pancreatic, and laryngeal cancer | [76,133,134,135,136,137,138,139,140,141] |
| 63 | Spatholobus suberectus Dunn | Spatholobus | Flavonoids, phenolic acid | Not specified | [142] |
| 64 | Tephrosia purpurea L. | Tephrosia | Flavonoids | MCF-7 (breast cancer) | [143] |
| 65 | Trifolium repens L. | Trifolium | Flavonoids, alkaloids | Not specified | [144] |
| 66 | Trifolium spinosa L. | Trifolium | Flavonoids, alkaloids | Not specified | [144] |
| 67 | Trifolium pretense L. | Trifolium | Flavonoids | Breast cancer | [145] |
| 68 | Trigonella foenum-graecum L. | Trigonella | Apigenin, luteolin (flavone) | Breast, colon, esophageal squamous cell carcinoma, lung, and prostate cancer | [146,147] |
| 69 | Vicia faba L. | Vicia | Flavonoids | MCF-7 (breast cancer), HCT 116 | [23] |
| 70 | Wisteria sinensis (Sims) DC. | Wisteria | Flavonoids | Hepatocellular Carcinoma | [148] |
| 71 | Wisteria floribunda (Willd.) DC. | Wisteria | Lectin | MCF-7 (breast cancer) | [88] |
4.3. Saponins
Several members of the Fabaceae family including peanut, soybean, and lentil are rich in saponins and reported to exhibit anti-cancer properties. Various researchers around the globe have confirmed that saponins isolated from members of the Fabaceae family are effective against colon cancer, melanoma cells, and cervical cancer. Saponins can follow various mechanisms to suppress the progression of cancer by cell cycle arrest, the inhibition of cellular invasion, anti-oxidant activity, and the induction of autophagy and apoptosis [149]. Rochfort and Panozzo [150] stated that the intake of legume saponins enhances the immunity against various types of cancer including cervical and colon cancer. Mudryj et al. [151] examined the anti-carcinogenic activity of legume saponins and reported that saponins involve different mechanisms such as immune modulatory effects, acid and neutral sterol metabolism, the normalization of carcinogen-induced cell proliferation, and cytotoxicity of cancerous cells.
Saponins show growth-repressing effects against colon cancer cells by interacting with cholesterol or free sterols that occur in the cell membranes and lead to a change in its permeability [152]. According to Gurfinkel and Rao [153], microorganisms in the colon hydrolyze saponins to sapogenols, which act as a strong chemopreventive agent against colon cancer and delimit further cancer progression. Dai et al. [154] stated that the intake of saponins from Glycine max reduces the risk of and controls breast cancer growth. The effects were more significant, in particular, in the case of premenopausal women. Furthermore, saponins from Glycine max also inhibit prostate cancer; however, more efforts from researchers are required to understand the exact mechanism. Mujoo et al. [73] demonstrated that saponins are present in substantial amounts in Acacia victoriae Benth., which inhibit the proliferation of various tumor cell lines with minimal growth inhibition in immortalized breast epithelial cells, human foreskin fibroblasts, and mouse fibroblasts at a similar concentration. Mujoo et al. [73] also investigated two saponins (avicins and Fo35) from A. victoriae and reported that both cause apoptosis of the Jurket (T-cell leukemia), cell cycles arrest (G1) of the human breast cancer cell line (MDA-MB-453), and apoptosis of cancer cell line (MDA-MB-435).
4.4. Alkaloids
Alkaloids are vital secondary metabolites that are considered a valuable source of novel drugs. Several studies have confirmed that alkaloids have anti-cancer and anti-proliferative properties [155]. Vindesine, vinorelbine, vinblastine, and vincristine are the best examples of alkaloids, which have already been successfully developed as anti-cancer drugs. These are effective against different forms of cancer including testicular cancer, brain cancer, lung cancer, bladder cancer, and melanoma. Over 21,000 different alkaloids have been identified and most of these alkaloids are a great source of medicines, especially exhibiting anti-cancer activities [156].
Steroidal alkaloids are the most promising component of phytochemicals as far as the anti-cancer potential is concerned. Steroidal alkaloids could be used in the discovery of safer drugs for cancer treatment with the aid of more clinical experiments in the future [157]. Matrine alkaloid found in the members of the genus Sophora showed potential anti-cancer effects against lung cancer and liver cancer [158]. Oxymatrine is one of the few important quinolizidine alkaloid compounds extracted majorly from the roots of Sophora flavescens Aiton. Oxymatrine is reported to increase the anti-tumor immunity against lung cancer and can be used to enhance the immunity against various other types of cancer [141]. Cytisine is another alkaloid naturally occurring in two genera of the Fabaceae family including Cytisus and Laburnum [159]. Cytisine is helpful in the suppression of lung cancer through the induction of mitochondria-mediated apoptosis and cell cycle arrest and suggests potential anti-cancer activity [114].
Castanospermine is another alkaloid extracted from Castanospermum australe A. Cunn ex Hook. [98] and is reported to convert protein N-linked high mannose carbohydrates to complex oligosaccharides. Castanospermine serves as an inhibitor of the glycosidases and leads to the suppression of tumor cell proliferation in nude mice [160]. Physostigmine alkaloid, also known as eserine, occurs naturally in Physostigma venenosum Balf. and exhibits anti-tumor activities [122]. Pfitzinger et al. [122] reported that physostigmine treatment significantly suppresses tumor-associated inflammation in mice. However, alkaloids in the Fabaceae family have not been explored in the same way as other family members as far as anti-cancer activities are concerned; therefore, more research is required for the further discovery of potent anti-cancer drugs from alkaloids that occur in the Fabaceae family.
4.5. Carotenoids
Legume leaves are a vital source of carotenoids, which primarily include carotenes, while other carotenoids are lutein, neoxanthin, crocetin, antheraxanthin, violaxanthin, and some others in a very low quantity. On the other hand, legume roots are not as rich in carotenoids as the leaves [161]. Many experimental studies have identified various mechanisms through which carotenoids may control the development of various types of cancer in humans. These mechanisms include anti-oxidant actions, retinol, communication functions, and cell signaling. Therefore, anti-oxidant defense support from the carotenoids reduces cancer risks [162]. Nishino et al. [163] carried out an extensive study and reported that β-carotene, β-cryptoxanthin, lycopene, lutein, and zeaxanthin can be used as chemopreventative agents. Moreover, beta-cryptoxanthin regulates the expression of the RB gene, which is a known anti-oncogene. Horvath et al. [164] stated that the carotenoids extracted from legumes have protective, preventative, and even curative effects against various types of cancer.
Lutein and zeaxanthin are two vital carotenoids that lower the risk of certain cancers [165]. Cancer is associated with the inflammation processes; therefore, the beneficial effects of both lutein and zeaxanthin are due to anti-inflammatory and anti-oxidant properties [164,166], but the exact mechanism of lutein and zeaxanthin action is not clearly understood and needs to be explored in future studies. Beta-carotene markedly inhibits the growth of esophageal cancerous cells in a time- and dose-dependent manner. Another significant fact is that the same concentration of beta-carotene is non-toxic to normal esophageal epithelium Het-lA cells, suggesting β-carotene is a potent anti-cancer agent [167]. PC-SPES is a patented herbal mixture that is utilized in prostate cancer treatment, and this herbal mixture is unique in its composition as it is a combination of eight herbs, two of which belong to the Fabaceae family, including Glycyrrhiza glabra L. and G. uralensis Fisch. ex DC [168]. According to Matus et al. [169], terpenoids are significant inhibitors of the signaling of NF-kB, which is a key regulator in cancer and inflammation. Carotenoids can use a variety of pathways for their anti-cancer activity; however, the induction of apoptosis is considered the most common.
Satia et al. [170] reported that the long-term use of retinol, β-carotene, lutein, and lycopene reduces the risk of lung cancer. Gong et al. [171] stated that legumes are an important source of lutein and significantly inhibit the proliferation of breast cancer cells and enhance the effect of chemopreventive agents through reactive oxygen species (ROS)-mediated mechanisms. Rafi et al. [172] determined the effect of lutein on the proliferation of human prostate cancer cells (PC3) as well as rat prostate carcinoma cells (AT3 cells). The anti-cancer activity of lutein was effective against both rat and human prostate cancer. Kim et al. [173] demonstrated that zeaxanthin in combination with lutein lowers the risk of colorectal cancer through apoptosis of cancerous cells and anti-oxidant functions.
4.6. Phenolic Acids
Phenolic acids are vital phytochemicals present in considerable amounts in the members of the Fabaceae family. Phenolic acids are non-flavonoid phenolic compounds that occur in the free, insoluble-bound, and conjugated soluble forms. On the other hand, these non-flavonoid phenolic compounds are widely distributed in plant species [174]. Natural phenolic acids present in various members of the Fabaceae family are ferulic acid, vanillic acid, caffeic acid, benzoic acid, p-hydroxy acid, 3,4-dihydroxybenzoic acid, sinapinic acid, and syringic acid [175]. Phenolic acids are secondary compounds that have been explored recently against various diseases, particularly cancer. These phenolics reduce the proliferation of cancerous cells, promote apoptosis, and target various aspects of cancer including growth, development, and metastasis [176]. Recently, phenolic acids have been extensively studied due to their anti-inflammatory, anti-tumor, and anti-oxidant activities [177]. Anantharaju et al. [178] demonstrated that the anti-carcinogenic effect of phenolic acids is largely due to five activities: (1) modulation of ROS levels, (2) inducing cell cycle arrest, (3) promoting the suppression of tumor proteins such as p53, (4) suppressing oncogenic signaling cascades controlling apoptosis and angiogenesis as well as proliferation, (5) increasing the ability to differentiate and, finally, transforming into normal cells.
Palko-Labuz et al. [179] stated that phenolic acids exhibit numerous health-related benefits such as anti-oxidant, anti-cancer, and anti-inflammatory activities. Phenolic acids have low bioavailability, which often restricts their possible medical applications; however, conjugation with phospholipids could be helpful to enhance the bioavailability in the biological system. The results showed that conjugates were effective as apoptosis-inducing, anti-proliferative, and cell cycle-affecting agents. Moreover, the same concentration was effective for the majority of metastatic melanoma cell lines and, importantly, did not affect the normal fibroblasts. Salem et al. [68] isolated bioactive gallic acid from the pod extract of Acacia nilotica (L.) Willd. ex Dilile and reported that gallic acid has anti-tumor properties due to anti-oxidant and anti-inflammatory properties.
5. Conclusions and Future Directions
Species of the Fabaceae family are a rich source of phytochemicals including flavonoids, lectins, saponins, alkaloids, carotenoids, and phenolic acids. The consumption of various species of the Fabaceae family lowers the risk of cancer, as the phytochemicals from Fabaceae members are effective in the prevention and treatment of cancer. Some of these phytochemicals have already been utilized against cancer worldwide; however, other phytochemicals are also gaining importance. These phytochemicals use a variety of mechanisms to control cancer including carcinogen inactivation, the induction of cell cycle arrest, anti-oxidant stress, apoptosis, and regulation of the immune system. On the other hand, there is room for more research to be carried out to assess the anti-cancer properties of phytochemicals of the Fabaceae family. More data are needed relating to the phytochemicals of the Fabaceae family for anti-cancer properties, and these data would lead to the discovery of novel drugs from these phytochemicals. Similarly, more studies elucidating the mechanisms behind the anti-cancer properties of phytochemicals are also required in the future. Despite the effectiveness of different phytochemicals in a plant belonging to the Fabaceae family, there is a need to elucidate any synergistic impact of different anti-cancer phytochemicals in a single plant. In the future, any long-term adverse side effects in terms of physiological changes in patients caused by different anti-cancer phytochemicals found in the Fabaceae family also require elucidation. Despite many reports about the efficacy of different anti-cancer phytochemicals, most of these reports are under in vitro or in vivo experiment conditions, and very few clinical trial reports are available. Therefore, more clinical trial reports confirming the efficacy of phytochemicals from Fabaceae members with responsible mechanisms will be indispensable in future studies. To achieve the international standard, significant standardization of prospective phytochemicals in terms of techniques for analyzing their bioavailability, efficacy, safety, quality, composition, manufacturing processes, and regulatory and approval requirements are required.
Author Contributions
Original draft: M.U., A.D. and W.R.K.; review: N.Y., A.D., W.R.K., S.A., G.M. and K.A.K.; figure and tables: A.D., Z.R., M.N.R. and M.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Universiti Putra Malaysia, Grant Number: 5540232.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors are thankful to “Universiti Putra Malaysia” for the provision of financial support.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
References
- Saini, A.; Kumar, M.; Bhatt, S.; Saini, V.; Malik, A. Cancer causes and treatments. Int. J. Pharm Sci. Res. 2020, 11, 3121–3134. [Google Scholar]
- Subramaniam, S.; Selvaduray, K.R.; Radhakrishnan, A.K. Bioactive compounds: Natural defense against cancer? Biomolecules 2019, 9, 758. [Google Scholar] [CrossRef] [PubMed]
- Gezici, S.; Sekeroglu, N. Current perspectives in the application of medicinal plants against cancer: Novel therapeutic agents. Anti-Cancer Agen. Med. Chem. 2019, 19, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, J.; Abbasi, B.A.; Mahmood, T.; Kanwal, S.; Ali, B.; Shah, S.A.; Khalil, A.T. Plant-derived anticancer agents: A green anticancer approach. Asian Pac. J. Trop. Biomed. 2017, 7, 1129–1150. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Current cancer epidemiology. J. Epidemiol. Glob. Health 2019, 9, 217. [Google Scholar] [CrossRef]
- Cid-Gallegos, M.S.; Sánchez-Chino, X.M.; Juárez Chairez, M.F.; Álvarez González, I.; Madrigal-Bujaidar, E.; Jiménez-Martínez, C. Anticarcinogenic activity of phenolic compounds from sprouted legumes. Food Rev. Int. 2020, 2020, 1184058. [Google Scholar] [CrossRef]
- Rizeq, B.; Gupta, I.; Ilesanmi, J.; AlSafran, M.; Rahman, M.M.; Ouhtit, A. The power of phytochemicals combination in cancer chemoprevention. J. Cancer 2020, 11, 4521. [Google Scholar] [CrossRef]
- Harvey, A.L. Natural products in drug discovery. Drug Discov. 2008, 13, 894–901. [Google Scholar] [CrossRef]
- Zhang, J.; Hu, K.; Di, L.; Wang, P.; Liu, Z.; Zhang, J.; Yue, P.; Song, W.; Zhang, J.; Chen, T.; et al. Traditional herbal medicine and nanomedicine: Converging disciplines to improve therapeutic efficacy and human health. Adv. Drug Deliv. Rev. 2021, 178, 113964. [Google Scholar] [CrossRef]
- Usman, M.; Ditta, A.; Ibrahim, F.H.; Murtaza, G.; Rajpar, M.N.; Mehmood, S.; Saleh, M.N.B.; Imtiaz, M.; Akram, S.; Khan, W.R. Quantitative ethnobotanical analysis of medicinal plants of high-temperature areas of Southern Punjab, Pakistan. Plants 2021, 10, 1974. [Google Scholar] [CrossRef]
- Thakore, P.; Mani, R.K.; Kavitha, S.J. A brief review of plants having anti-cancer property. Int. J. Pharm. Res. Dev. 2012, 3, 129–136. [Google Scholar]
- Tariq, A.; Sadia, S.; Pan, K.; Ullah, I.; Mussarat, S.; Sun, F.; Abiodun, O.O.; Batbaatar, A.; Li, Z.; Song, D.; et al. A systematic review on ethnomedicines of anti-cancer plants. Phytother. Res. 2017, 31, 202–264. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, R.; Jaykar, B.; Gomathi, V. Current status of anticancer research in Fabaceae family. Pathways 2020, 6, 7. [Google Scholar]
- Samec, M.; Liskova, A.; Koklesova, L.; Samuel, S.M.; Murin, R.; Zubor, P.; Bujnak, J.; Kwon, T.K.; Büsselberg, D.; Prosecky, R.; et al. The role of plant-derived natural substances as immunomodulatory agents in carcinogenesis. J. Cancer Res. Clin. Oncol. 2020, 146, 3137–3154. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Butler, E.; Macchi, F.; Williams, M. Phytochemicals in cancer prevention and management. Br. J. Med. Pract. 2015, 8, 1–8. [Google Scholar]
- Martinez-Millan, M. Fossil record and age of the Asteridae. Bot. Rev. 2010, 76, 83–135. [Google Scholar] [CrossRef]
- Sharma, A.; Kaur, R.; Katnoria, J.K.; Kaur, R.; Nagpal, A.K. Family Fabaceae: A boon for cancer therapy. In Biotechnology and Production of Anti-Cancer Compounds; Malik, S., Ed.; Springer: Cham, Switzerland, 2017; pp. 157–175. [Google Scholar] [CrossRef]
- Schrire, B. A review of tribe Indigofereae (Leguminosae–Papilionoideae) in Southern Africa (including South Africa, Lesotho, Swaziland & Namibia; excluding Botswana). S. Afr. J. Bot. 2013, 89, 281–283. [Google Scholar]
- Messina, M.J. Legumes and soybeans: Overview of their nutritional profiles and health effects. Am. J. Clin. Nutr. 1999, 70, 439s–450s. [Google Scholar] [CrossRef]
- Pastorino, G.; Cornara, L.; Soares, S.; Rodrigues, F.; Oliveira, M.B.P. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phytother. Res. 2018, 32, 2323–2339. [Google Scholar] [CrossRef] [PubMed]
- Batiha, G.E.S.; Beshbishy, A.M.; El-Mleeh, A.; Abdel-Daim, M.M.; Devkota, H.P. Traditional uses, bioactive chemical constituents, and pharmacological and toxicological activities of Glycyrrhiza glabra L. (Fabaceae). Biomolecules 2020, 10, 352. [Google Scholar] [CrossRef] [PubMed]
- El-Feky, A.M.; Elbatanony, M.M.; Mounier, M.M. Anti-cancer potential of the lipoidal and flavonoidal compounds from Pisum sativum and Vicia faba peels. Egypt. J. Basic Appl. Sci. 2018, 5, 258–264. [Google Scholar] [CrossRef]
- Sporn, M.B.; Liby, K.T. Chemoprevention of Cancer: Past, Present, and Future. In Natural Products for Cancer Chemoprevention; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–18. [Google Scholar]
- Klaunig, J.E.; Wang, Z. Oxidative stress in carcinogenesis. Curr. Opin. Toxicol. 2018, 7, 116–121. [Google Scholar] [CrossRef]
- Klaunig, J.E. Oxidative stress and cancer. Curr. Pharm. Des. 2018, 24, 4771–4778. [Google Scholar] [CrossRef]
- Dandawate, P.; Ahmad, A.; Deshpande, J.; Swamy, K.V.; Khan, E.M.; Khetmalas, M.; Padhye, S.; Sarkar, F. Anticancer phytochemical analogs 37: Synthesis, characterization, molecular docking and cytotoxicity of novel plumbagin hydrazones against breast cancer cells. Bioorganic Med. Chem. Lett. 2014, 24, 2900–2904. [Google Scholar] [CrossRef]
- Ranjan, A.; Ramachandran, S.; Gupta, N.; Kaushik, I.; Wright, S.; Srivastava, S.; Das, H.; Srivastava, S.; Prasad, S.; Srivastava, S.K. Role of phytochemicals in cancer prevention. Int. J. Mol. Sci. 2019, 20, 4981. [Google Scholar] [CrossRef]
- Nedeljkovic, M.; Damjanovic, A. Mechanisms of chemotherapy resistance in triple-negative breast cancer—How we can rise to the challenge. Cells 2019, 8, 957. [Google Scholar] [CrossRef]
- Meguid, R.A.; Hooker, C.M.; Taylor, J.T.; Kleinberg, L.R.; Cattaneo, S.M., II; Sussman, M.S.; Yang, S.C.; Heitmiller, R.F.; Forastiere, A.A.; Brock, M.V. Recurrence after neoadjuvant chemoradiation and surgery for esophageal cancer: Does the pattern of recurrence differ for patients with a complete response and those with partial or no response? J. Thorac. Cardiovasc. Surg. 2009, 138, 1309–1317. [Google Scholar] [CrossRef]
- Chan, C.W.; Law, B.M.; So, W.K.; Chow, K.M.; Waye, M.M. Novel strategies on personalized medicine for breast cancer treatment: An update. Int. J. Mol. Sci. 2017, 18, 2423. [Google Scholar] [CrossRef]
- Koh, Y.C.; Ho, C.T.; Pan, M.H. Recent advances in cancer chemoprevention with phytochemicals. J. Food Drug Anal. 2020, 28, 14–37. [Google Scholar] [CrossRef] [PubMed]
- Dewanjee, S.; Das, S.; Joardar, S.; Bhattacharjee, S.; Chakraborty, P. Carotenoids as Anticancer Agents. In Carotenoids: Structure and Function in the Human Body; Springer: Berlin/Heidelberg, Germany, 2021; p. 475. [Google Scholar]
- Iqbal, J.; Abbasi, B.A.; Ahmad, R.; Batool, R.; Mahmood, T.; Ali, B.; Khalil, A.T.; Kanwal, S.; Shah, S.A.; Alam, M.M.; et al. Potential phytochemicals in the fight against skin cancer: Current landscape and future perspectives. Biomed. Pharmacother. 2019, 109, 1381–1393. [Google Scholar] [CrossRef] [PubMed]
- Steward, W.P.; Brown, K. Cancer chemoprevention: A rapidly evolving field. Br. J. Cancer 2013, 109, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hassan, L.E.A.; Ahamed, M.B.K.; Majid, A.S.A.; Baharetha, H.M.; Muslim, N.S.; Nassar, Z.D.; Majid, A.M.A. Correlation of antiangiogenic, antioxidant, and cytotoxic activities of some Sudanese medicinal plants with phenolic and flavonoid contents. BMC Complement. Med. Ther. 2014, 14, 406. [Google Scholar] [CrossRef] [PubMed]
- Agbo, M.O.; Uzor, P.F.; Nneji, U.N.A.; Odurukwe, C.U.E.; Ogbatue, U.B.; Mbaoji, E.C. Antioxidant, total phenolic and flavonoid content of selected Nigerian medicinal plants. Dhaka Univ. J. Pharm. Sci. 2015, 14, 35–41. [Google Scholar] [CrossRef]
- Krishna, P.M.; KNV, R.; Banji, D. A review on phytochemical, ethnomedical, and pharmacological studies on genus Sophora, Fabaceae. Rev. Bras. Farmacogn. 2012, 22, 1145–1154. [Google Scholar] [CrossRef]
- Kleemann, R.; Verschuren, L.; Morrison, M.; Zadelaar, S.; van Erk, M.J.; Wielinga, P.Y.; Kooistra, T. Anti-inflammatory, anti-proliferative, and anti-atherosclerotic effects of quercetin in human in vitro and in vivo models. Atherosclerosis 2011, 218, 44–52. [Google Scholar] [CrossRef]
- Wang, J.; Yu, H.; Yili, A.; Gao, Y.; Hao, L.; Aisa, H.A.; Liu, S. Identification of hub genes and potential molecular mechanisms of chickpea isoflavones on MCF-7 breast cancer cells by integrated bioinformatics analysis. Ann. Transl. Med. 2020, 8, 86. [Google Scholar] [CrossRef]
- Sarkar, F.H.; Li, Y. Soy isoflavones and cancer prevention: Clinical science review. Cancer Invest. 2003, 21, 744–757. [Google Scholar] [CrossRef]
- Cornwell, T.; Cohick, W.; Raskin, I. Dietary phytoestrogens and health. Phytochemistry 2004, 65, 995–1016. [Google Scholar] [CrossRef]
- Ateba, S.B.; Njamen, D.; Krenn, L. The genus Eriosema (Fabaceae): From the ethnopharmacology to an evidence-based phytotherapeutic perspective? Front. Pharmacol. 2021, 12, 641225. [Google Scholar] [CrossRef] [PubMed]
- Aregueta-Robles, U.; Fajardo-Ramírez, O.R.; Villela, L.; Gutiérrez-Uribe, J.A.; Hernández-Hernández, J.; del Carmen López-Sánchez, R.; Scott, S.P.; Serna-Saldívar, S. Cytotoxic activity of a black bean (Phaseolus vulgaris L.) extract and its flavonoid fraction in both in vitro and in vivo models of lymphoma. Rev. Investig. Clin. 2018, 70, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ombra, M.N.; d’Acierno, A.; Nazzaro, F.; Riccardi, R.; Spigno, P.; Zaccardelli, M.; Pane, C.; Maione, M.; Fratianni, F. Phenolic composition and antioxidant and antiproliferative activities of the extracts of twelve common bean (Phaseolus vulgaris L.) endemic ecotypes of Southern Italy before and after cooking. Oxid. Med. Cell Longev. 2016, 2016, 1398298. [Google Scholar] [CrossRef] [PubMed]
- Gatouillat, G.; Magid, A.A.; Bertin, E.; Morjani, H.; Lavaud, C.; Madoulet, C. Medicarpin and millepurpan, two flavonoids isolated from Medicago sativa, induce apoptosis and overcome multidrug resistance in leukemia P388 cells. Phytomedicine 2015, 22, 1186–1194. [Google Scholar] [CrossRef]
- Bora, K.S.; Sharma, A. Phytochemical and pharmacological potential of Medicago sativa: A review. Pharm. Biol. 2011, 49, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Stochmal, A.; Kowalska, I.; Oleszek, W. Medicago sativa and Medicago truncatula as plant sources of the chemopreventive flavone tricin. Planta Med. 2007, 73, 304. [Google Scholar] [CrossRef]
- Custodio, L.; Fernandes, E.; Escapa, A.L.; López-Avilés, S.; Fajardo, A.; Aligué, R.; Alberício, F.; Romano, A. Antioxidant activity and in vitro inhibition of tumor cell growth by leaf extracts from the carob tree (Ceratonia siliqua). Pharm. Biol. 2009, 47, 721–728. [Google Scholar] [CrossRef]
- Fu, Y.; Hsieh, T.C.; Guo, J.; Kunicki, J.; Lee, M.Y.; Darzynkiewicz, Z.; Wu, J.M. Licochalcone-A, a novel flavonoid isolated from licorice root (Glycyrrhiza glabra), causes G2 and late-G1 arrests in androgen-independent PC-3 prostate cancer cells. Biochem. Biophys. Res. Commun. 2004, 322, 263–270. [Google Scholar] [CrossRef]
- Choedon, T.; Shukla, S.K.; Kumar, V. Chemopreventive and anti-cancer properties of the aqueous extract of flowers of Butea monosperma. J. Ethnopharmacol. 2010, 129, 208–213. [Google Scholar] [CrossRef]
- Fu, L.L.; Zhou, C.C.; Yao, S.; Yu, J.Y.; Liu, B.; Bao, J.K. Plant lectins: Targeting programmed cell death pathways as antitumor agents. Int. J. Biochem. Cell Biol. 2011, 43, 1442–1449. [Google Scholar] [CrossRef]
- Yau, T.; Dan, X.; Ng, C.C.W.; Ng, T.B. Lectins with potential for anti-cancer therapy. Molecules 2015, 20, 3791–3810. [Google Scholar] [CrossRef] [PubMed]
- Gautam, A.K.; Shrivastava, N.; Sharma, B.; Bhagyawant, S.S. Current scenario of legume lectins and their practical applications. J. Crop. Sci. Biotechnol. 2018, 21, 217–227. [Google Scholar] [CrossRef]
- Bhutia, S.K.; Panda, P.K.; Sinha, N.; Praharaj, P.P.; Bhol, C.S.; Panigrahi, D.P.; Mahapatra, K.K.; Saha, S.; Patra, S.; Mishra, S.R.; et al. Plant lectins in cancer therapeutics: Targeting apoptosis and autophagy-dependent cell death. Pharmacol. Res. 2019, 144, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Majeed, M.; Hakeem, K.R.; Rehman, R.U. Mistletoe Lectins: From interconnecting proteins to potential tumor inhibiting agents. Phytomed. Plus 2021, 1, 100039. [Google Scholar] [CrossRef]
- De Mejia, E.G.; Prisecaru, V.I. Lectins as bioactive plant proteins: A potential in cancer treatment. Crit. Rev. Food Sci. Nutr. 2005, 45, 425–445. [Google Scholar] [CrossRef] [PubMed]
- Fang, E.F.; Lin, P.; Wong, J.H.; Tsao, S.W.; Ng, T.B. A lectin with anti-HIV-1 reverse transcriptase, antitumor, and nitric oxide inducing activities from seeds of Phaseolus vulgaris cv. extralong autumn purple bean. J. Agric. Food Chem. 2010, 58, 2221–2229. [Google Scholar] [CrossRef]
- Lam, S.K.; Ng, T.B. Isolation and characterization of a French bean hemagglutinin with antitumor, antifungal, and anti-HIV-1 reverse transcriptase activities and an exceptionally high yield. Phytomedicine 2010, 17, 457–462. [Google Scholar] [CrossRef]
- Ye, X.J.; Ng, T.B. Antitumor and HIV-1 reverse transcriptase inhibitory activities of hemagglutinin and a protease inhibitor from mini-black soybean. Evid.-Based Complement Altern. Med. 2011, 2011, 12. [Google Scholar] [CrossRef]
- Gautam, A.K.; Gupta, N.; Narvekar, D.T.; Bhadkariya, R.; Bhagyawant, S.S. Characterization of chickpea (Cicer arietinum L.) lectin for biological activity. Physiol. Mol. Biol. Plants 2018, 24, 389–397. [Google Scholar] [CrossRef]
- Une, S.; Nonaka, K.; Akiyama, J. Lectin isolated from Japanese red sword beans (Canavalia gladiata) as a potential cancer chemopreventive agent. J. Food Sci. 2018, 83, 837–843. [Google Scholar] [CrossRef]
- Cavada, B.S.; Silva, M.T.L.; Osterne, V.J.S.; Pinto-Junior, V.R.; Nascimento, A.P.M.; Wolin, I.A.V.; Heinrich, I.A.; Nobre, C.A.S.; Moreira, C.G.; Lossio, C.F.; et al. Canavalia bonariensis lectin: Molecular bases of glycoconjugates interaction and antiglioma potential. Int. J. Biol. Macromol. 2017, 106, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Arteaga, I.T.; Guillen, J.C.; Olaya, E.M.; Gasca, T.G.; Zaragoza, M.V.Á.; García-Santoyo, V.; Castillo, J.T.; Aguirre, C.; Phinney, B.; Blanco-Labra, A. Characterization of two non-fetuin-binding lectins from Tepary bean (Phaseolus acutifolius) seeds with differential cytotoxicity on colon cancer cells. J. Glycobiol. 2016, 5, 1–7. [Google Scholar]
- Gondim, A.C.; Romero-Canelon, I.; Sousa, E.H.; Blindauer, C.A.; Butler, J.S.; Romero, M.J.; Sanchez-Cano, C.; Sousa, B.L.; Chaves, R.P.; Nagano, C.S.; et al. The potent anti-cancer activity of Dioclea lasiocarpa lectin. J. Inorg. Biochem. 2017, 175, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Lagarda-Diaz, I.; Guzman-Partida, A.M.; Vazquez-Moreno, L. Legume lectins: Proteins with diverse applications. Int. J. Mol. Sci. 2017, 18, 1242. [Google Scholar] [CrossRef]
- Korourian, S.; Siegel, E.; Kieber-Emmons, T.; Monzavi-Karbassi, B. Expression analysis of carbohydrate antigens in ductal carcinoma in situ of the breast by lectin histochemistry. BMC Cancer 2008, 8, 136. [Google Scholar] [CrossRef]
- Salem, M.M.; Davidorf, F.H.; Abdel-Rahman, M.H. In vitro anti-uveal melanoma activity of phenolic compounds from the Egyptian medicinal plant Acacia nilotica. Fitoterapia 2011, 82, 1279–1284. [Google Scholar] [CrossRef]
- Afsar, T.; Razak, S.; Khan, M.R.; Mawash, S.; Almajwal, A.; Shabir, M.; Haq, I.U. Evaluation of antioxidant, anti-hemolytic and anticancer activity of various solvent extracts of Acacia hydaspica R. Parker aerial parts. BMC Complement. Altern. Med. 2016, 16, 258. [Google Scholar]
- Gedara, S.R.; Galala, A.A. New cytotoxic spirostane saponin and biflavonoid glycoside from the leaves of Acacia saligna (Labill.) HL Wendl. Nat. Prod. Res. 2014, 28, 324–329. [Google Scholar] [CrossRef]
- Elansary, H.O.; Szopa, A.; Kubica, P.; Ekiert, H.; Al-Mana, F.A.; Al-Yafrsi, M.A. Antioxidant and biological activities of Acacia saligna and Lawsonia inermis natural populations. Plants 2020, 9, 908. [Google Scholar] [CrossRef]
- Patel, A.; Hafez, E.; Elsaid, F.; Amanullah, M. Anti-cancer action of a new recombinant lectin produced from Acacia species. Int. J. Med. Sci. 2014, 5, 1–11. [Google Scholar]
- Mujoo, K.; Haridas, V.; Hoffmann, J.J.; Wächter, G.A.; Hutter, L.K.; Lu, Y.; Blake, M.E.; Jayatilake, G.S.; Bailey, D.; Mills, G.B.; et al. Triterpenoid saponins from Acacia victoriae (Bentham) decrease tumor cell proliferation and induce apoptosis. Cancer Res. 2001, 61, 5486–5490. [Google Scholar] [PubMed]
- Desai, T.H.; Joshi, S.V. Anticancer activity of saponin isolated from Albizia lebbeck using various in vitro models. J. Ethnopharmacol. 2019, 231, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Kavitha, C.N.; Raja, K.D.; Rao, S.K. Antitumor activity of Albizia lebbeck L. against Ehrlich ascites carcinoma in vivo and HeLa and A549 cell lines in vitro. J. Cancer Res. Ther. 2021, 17, 491. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Su, B.S.; Chang, L.H.; Gao, Q.; Chen, K.L.; An, P.; Huang, C.; Yang, J.; Li, Z.F. Oxymatrine induces apoptosis in human cervical cancer cells through guanine nucleotide depletion. Anti-Cancer Drugs 2014, 25, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Melek, F.R.; Aly, F.A.; Kassem, I.A.; Abo-Zeid, M.A.; Farghaly, A.A.; Hassan, Z.M. Three further triterpenoid saponins from Gleditsia caspica fruits and protective effect of the total saponin fraction on cyclophosphamide-induced genotoxicity in mice. Z. Naturforsch. C 2015, 70, 31–37. [Google Scholar] [CrossRef]
- Kanadaswami, C.; Lee, L.T.; Lee, P.P.H.; Hwang, J.J.; Ke, F.C.; Huang, Y.T.; Lee, M.T. The antitumor activities of flavonoids. In Vivo 2005, 19, 895–909. [Google Scholar]
- Majewska-Wierzbicka, M.; Czeczot, H. Anticancer activity of flavonoids. Pol. Merkur. Lek. Organ Pol. Tow. Lek. 2012, 33, 364–369. [Google Scholar]
- Kokila, K.; Priyadharshini, S.D.; Sujatha, V. Phytopharmacological properties of Albizia species: A review. Int. J. Pharm. Pharm. Sci. 2013, 5, 70–73. [Google Scholar]
- Mehraban, F.; Mostafazadeh, M.; Sadeghi, H.; Azizi, A.; Toori, M.A.; Gramizadeh, B.; Barati, V.; Sadeghi, H. Anticancer activity of Astragalus ovinus against 7, 12 dimethyl Benz (a) anthracene (DMBA)-induced breast cancer in rats. Avic. J. Phytomed. 2020, 10, 533. [Google Scholar]
- Nayeem, N.; Imran, M.; Asdaq, S.M.B.; Rabbani, S.I.; Alanazi, F.A.; Alamri, A.S.; Sampaio, M.U.; Jochum, M.; Oliva, M.L.V. Total phenolic, flavonoid contents, and biological activities of stem extracts of Astragalus spinosus (Forssk.) Muschl. grown in Northern Border Province, Saudi Arabia. Saudi Sci. J. Biol. Sci. 2022, 29, 1277–1282. [Google Scholar] [CrossRef]
- Zhou, R.; Chen, H.; Chen, J.; Chen, X.; Wen, Y.; Xu, L. Extract from Astragalus membranaceus inhibit breast cancer cells proliferation via PI3K/AKT/mTOR signaling pathway. BMC Complement Altern. Med. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, D.; Shankar, K.G.; Ignacimuthu, S.; Sophy, A.R.; Vidhya, R.; Anusha, J.R. Bauhinia acuminata L. attenuates lung cancer cell proliferation: In vitro, in vivo, and in silico approaches. Phytomed. Plus 2022, 2, 100173. [Google Scholar] [CrossRef]
- Tu, L.Y.; Pi, J.; Jin, H.; Cai, J.Y.; Deng, S.P. Synthesis, characterization, and anticancer activity of kaempferol-zinc (II) complex. Bioorganic Med. Chem. Lett. 2016, 26, 2730–2734. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Yano, T.; Sadzuka, Y.; Sugiyama, T.; Seki, T.; Asano, R. Restoration of connexin 43 by Bowman-Birk protease inhibitor in M5076 bearing mice. Oncol. Rep. 2005, 13, 1247–1250. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Munir, S.; Badshah, S.L.; Khan, N.; Ghani, L.; Poulson, B.G.; Emwas, A.H.; Jaremko, M. Important flavonoids and their role as a therapeutic agent. Molecules 2020, 25, 5243. [Google Scholar] [CrossRef]
- Agrawal, S.B.; Gupta, N.; Bhagyawant, S.S.; Gaikwad, S.M. Anticancer activity of lectins from Bauhinia purpurea and Wisteria floribunda on breast cancer MCF-7 cell lines. Protein Pept. Lett. 2020, 27, 870–877. [Google Scholar] [CrossRef]
- Iheagwam, F.N.; Ogunlana, O.O.; Ogunlana, O.E.; Isewon, I.; Oyelade, J. Potential anti-cancer flavonoids isolated from Caesalpinia bonduc young twigs and leaves: Molecular docking and in silico studies. Bioinform. Biol. Insights 2019, 13, 1177932218821371. [Google Scholar] [CrossRef]
- Osman, S.M.; Khalek, S.M.A.; Koheil, M.A.; El-Haddad, A.E.; Wink, M. A new steroidal compound (β-sitosterol-3-O-butyl) isolated from Caesalpinia gilliesii flowers. Int. J. Appl. Res. Nat. Prod 2015, 8, 14–19. [Google Scholar]
- Zanin, J.L.; Massoni, M.; Santos, M.H.D.; Freitas, G.C.D.; Niero, E.L.; Schefer, R.R.; Lago, J.H.; Ionta, M.; Soares, M.G. Caesalpinioflavone, a new cytotoxic biflavonoid isolated from Caesalpinia pluviosa var. peltophoroides. J. Braz. Chem. Soc. 2015, 26, 804–809. [Google Scholar]
- Sakle, N.S.; More, S.A.; Mokale, S.N. A network pharmacology-based approach to explore potential targets of Caesalpinia pulcherima: An updated prototype in drug discovery. Sci. Rep. 2020, 10, 17217. [Google Scholar] [CrossRef]
- Pal, D.; Mishra, P.; Sachan, N.; Ghosh, A.K. Biological activities and medicinal properties of Cajanus cajan (L) Millsp. J. Adv. Pharm. Technol. Res. 2011, 2, 207. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Tian, R.H.; Cai, J.Z.; Wu, J.H.; Shen, X.L.; Hu, Y.J. Acute and sub-chronic toxicity of Cajanus cajan leaf extracts. Pharm. Biol. 2017, 55, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Ohiagu, F.O.; Chikezie, P.C.; Chikezie, C.M.; Enyoh, C.E. Anticancer activity of Nigerian medicinal plants: A review. Future J. Pharm. Sci. 2021, 7, 70. [Google Scholar] [CrossRef]
- Bhagat, M.; Saxena, A.K. Evaluation of Cassia occidentalis for in vitro cytotoxicity against human cancer cell lines and antibacterial activity. Indian J. Pharmacol. 2010, 42, 234. [Google Scholar] [CrossRef] [PubMed]
- Taiwo, F.O.; Akinpelu, D.A.; Aiyegoro, O.A.; Olabiyi, S.; Adegboye, M.F. The biocidal and phytochemical properties of leaf extract of Cassia occidentalis Linn. Afr. J. Microbiol. Res. 2013, 7, 3435–3441. [Google Scholar]
- Kato, A.; Hirokami, Y.; Kinami, K.; Tsuji, Y.; Miyawaki, S.; Adachi, I.; Hollinshead, J.; Nash, R.J.; Kiappes, J.L.; Zitzmann, N.; et al. Isolation and SAR studies of bicyclic iminosugars from Castanospermum australe as glycosidase inhibitors. Phytochemistry 2015, 111, 124–131. [Google Scholar] [CrossRef]
- Gregoriou, G.; Neophytou, C.M.; Vasincu, A.; Gregoriou, Y.; Hadjipakkou, H.; Pinakoulaki, E.; Christodoulou, M.C.; Ioannou, G.D.; Stavrou, I.J.; Christou, A.; et al. Anti-cancer activity and phenolic content of extracts derived from Cypriot carob (Ceratonia siliqua L.) pods using different solvents. Molecules 2021, 26, 5017. [Google Scholar] [CrossRef]
- Bouziane, A.; Bakchiche, B.; Dias, M.I.; Barros, L.; Ferreira, I.C.; AlSalamat, H.A.; Bardaweel, S.K. Phenolic Compounds and Bioactivity of Cytisus villosus Pourr. Molecules 2018, 23, 1994. [Google Scholar] [CrossRef]
- Ito, C.; Matsui, T.; Miyabe, K.; Hasan, C.M.; Rashid, M.A.; Tokuda, H.; Itoigawa, M. Three isoflavones from Derris scandens (Roxb.) Benth and their cancer chemopreventive activity and in vitro antiproliferative effects. Phytochemistry 2020, 175, 112376. [Google Scholar] [CrossRef]
- Fofana, S.; Ouédraogo, M.; Esposito, R.C.; Ouedraogo, W.P.; Delporte, C.; Van Antwerpen, P.; Mathieu, V.; Guissou, I.P. Systematic Review of Potential Anticancerous Activities of Erythrina senegalensis DC (Fabaceae). Plants 2021, 11, 19. [Google Scholar] [CrossRef]
- Mohammed, R.S.; Abou Zeid, A.H.; El Hawary, S.S.; Sleem, A.A.; Ashour, W.E. Flavonoid constituents, cytotoxic and antioxidant activities of Gleditsia triacanthos L. leaves. Saudi J. Biol. Sci. 2014, 21, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Zhang, C.; Zhan, L.; Cheng, L.; Lu, D.; Wang, X.; Xu, H.; Wang, S.; Wu, D.; Ruan, L. Anticancer effects of Gleditsia sinensis extract in rats transplanted with hepatocellular carcinoma cells. Oncol. Res. 2019, 27, 889. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.K.; Lee, M.H.; Kim, J.E.; Singh, P.; Lee, S.Y.; Jeong, C.H.; Lim, T.G.; Chen, H.; Chi, Y.I.; Kundu, J.K.; et al. Isoliquiritigenin induces apoptosis and inhibits xenograft tumor growth of human lung cancer cells by targeting both wild type and L858R/T790M mutant EGFR. J. Biol. Chem. 2014, 289, 35839–35848. [Google Scholar] [CrossRef]
- Mohamed, K.M.; Salwa, B.E.M.; Nadia, T.S.; Eshak, M.E.H.; Heba, A.B. Study of antioxidants and anticancer activity of licorice [Glycyrrhiza glabra] extracts. Egypt. J. Nutri. 2008, 23, 177–203. [Google Scholar]
- Renukadevi, K.P.; Sultana, S.S. Determination of antibacterial, antioxidant and cytotoxicity effect of Indigofera tinctoria on lung cancer cell line NCI-h69. Int. J. Pharmacol. 2011, 7, 356–362. [Google Scholar] [CrossRef]
- Srinivasan, S.A.; Wankhar, W.A.; Rathinasamy, S.H.; Rajan, R.A. Larvicidal potential of Indigofera tinctoria (Fabaceae) on dengue vector (Aedes aegypti) and its antimicrobial activity against clinical isolates. Asian J. Pharm. Clin. Res. 2015, 8, 316–319. [Google Scholar]
- Vijayan, R.; Joseph, S.; Mathew, B. Indigofera tinctoria leaf extract mediated green synthesis of silver and gold nanoparticles and assessment of their anticancer, antimicrobial, antioxidant, and catalytic properties. Artif. Cells Nanomed. Biotechnol. 2018, 46, 861–871. [Google Scholar] [CrossRef]
- Kumar, R.S.; Rajkapoor, B.; Perumal, P. In vitro and in vivo anticancer activity of Indigofera cassioides Rottl. Ex. DC. Asian Pac. J. Trop. Med. 2011, 4, 379–385. [Google Scholar] [CrossRef]
- Ramya, V.; Madhu-Bala, V.; Prakash-Shyam, K.; Gowdhami, B.; Sathiya-Priya, K.; Vignesh, K.; Vani, B.; Kadalmani, B. Cytotoxic activity of Indigofera aspalathoides (Vahl.) extracts in cervical cancer (HeLa) cells: Ascorbic acid adjuvant treatment enhances the activity. Phytomed. Plus 2021, 1, 100142. [Google Scholar] [CrossRef]
- Thangavel, D.; Govindasamy, J.; Kumar, R.S. In vitro antioxidant and anticancer activities of various extracts of Indigofera cordifolia Roth. J. Pharm. Biol. 2014, 4, 85–93. [Google Scholar]
- Leite, S.P.; Silva, L.L.S.; Catanho, M.T.J.A.; Lima, E.O.; Lima, V.L.M. Anti-inflammatory activity of Indigofera suffruticosa extract. Rebrasa 2003, 7, 47–52. [Google Scholar]
- Xu, W.T.; Li, T.Z.; Li, S.M.; Wang, C.; Wang, H.; Luo, Y.H.; Piao, X.J.; Wang, J.R.; Zhang, Y.; Zhang, T.; et al. Cytisine exerts anti-tumor effects on lung cancer cells by modulating reactive oxygen species-mediated signaling pathways. Artif. Cells Nanomed. Biotechnol. 2020, 48, 84–95. [Google Scholar] [CrossRef]
- Avato, P.; Migoni, D.; Argentieri, M.; Fanizzi, F.P.; Tava, A. Activity of saponins from Medicago species against HeLa and MCF-7 cell lines and their capacity to potentiate cisplatin effect. Anti-Cancer Agents Med. Chem. 2017, 17, 1508–1518. [Google Scholar] [CrossRef] [PubMed]
- Fantini, M.; Benvenuto, M.; Masuelli, L.; Frajese, G.V.; Tresoldi, I.; Modesti, A.; Bei, R. In vitro and in vivo antitumoral effects of combinations of polyphenols, or polyphenols and anticancer drugs: Perspectives on cancer treatment. Int. J. Mol. Sci. 2015, 16, 9236–9282. [Google Scholar] [CrossRef] [PubMed]
- Zagorska-Dziok, M.; Ziemlewska, A.; Nizioł-Łukaszewska, Z.; Bujak, T. Antioxidant activity and cytotoxicity of Medicago sativa L. seeds and herb extract on skin cells. BioRes. Open Access 2020, 9, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Wang, J.; Liu, W.; Nisar, M.F.; El-Esawi, M.A.; Wan, C. Biological Activities and Chemistry of Triterpene Saponins from Medicago Species: An Update Review. Evid.-Based Complement Altern. Med. 2021, 2021, 6617916. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.T.; Gong, P.H.; Xiao, F.Q.; Shao, S.; Zhao, D.Q.; Yan, M.M.; Yang, X.W. Chemical constituents and antioxidant, anti-inflammatory and anti-tumor activities of Melilotus officinalis (Linn.) Pall. Molecules 2018, 23, 271. [Google Scholar] [CrossRef]
- El-Hafeez, A.; Ali, A.; Khalifa, H.O.; Elgawish, R.A.; Shouman, S.A.; El-Twab, A.; Hussein, M.; Kawamoto, S. Melilotus indicus extract induces apoptosis in hepatocellular carcinoma cells via a mechanism involving mitochondria-mediated pathways. Cytotechnology 2018, 70, 831–842. [Google Scholar] [CrossRef]
- Chanu, K.V.; Leishangthem, G.D.; Srivastava, S.K.; Thakuria, D.; Kataria, M.; Telang, A.G. Phytochemical analysis and evaluation of the anticancer activity of Parkia javanica seeds. Pharm. Innov. 2018, 7, 305. [Google Scholar]
- Pfitzinger, P.L.; Fangmann, L.; Wang, K.; Demir, E.; Gürlevik, E.; Fleischmann-Mundt, B.; Brooks, J.; D’Haese, J.G.; Teller, S.; Hecker, A.; et al. Indirect cholinergic activation slows down pancreatic cancer growth and tumor-associated inflammation. J. Exp. Clin. Cancer Res. 2020, 39, 289. [Google Scholar] [CrossRef]
- Raghavendra, M.P.; Satish, S.; Raveesha, K.A. Alkaloids isolated from leaves of Prosopis juliflora against Xanthomonas pathovars. Arch. Phytopathol. Plant. Prot. 2009, 42, 1033–1041. [Google Scholar] [CrossRef]
- Henciya, S.; Seturaman, P.; James, A.R.; Tsai, Y.H.; Nikam, R.; Wu, Y.C.; Dahms, H.U.; Chang, F.R. Biopharmaceutical potentials of Prosopis spp. (Mimosaceae, Leguminosa). J. Food Drug Anal. 2017, 25, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Robertson, S.; Narayanan, N.; Raj Kapoor, B. Antitumor activity of Prosopis cineraria (L.) Druce against Ehrlich ascites carcinoma-induced mice. Nat. Prod. Res. 2011, 25, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Asati, V.; Srivastava, A.; Mukherjee, S.; Sharma, P.K. Comparative analysis of antioxidant and antiproliferative activities of crude and purified flavonoid enriched fractions of pods/seeds of two desert legumes Prosopis cineraria and Cyamopsis tetragonoloba. Heliyon 2021, 7, e07304. [Google Scholar] [CrossRef]
- Dzoyem, J.P.; Tchamgoue, J.; Tchouankeu, J.C.; Kouam, S.F.; Choudhary, M.I.; Bakowsky, U. Antibacterial activity, and cytotoxicity of flavonoids compounds isolated from Pseudarthria hookeri Wight & Arn. (Fabaceae). S. Afr. J. Bot. 2018, 114, 100–103. [Google Scholar]
- Wang, Y.; Hong, C.; Zhou, C.; Xu, D.; Qu, H.B. Screening antitumor compounds psoralen and isopsoralen from Psoralea corylifolia L. seeds. Evid.-Based Complement Altern. Med. 2011, 2011, 363052. [Google Scholar] [CrossRef]
- Al-Dabbagh, B.; Elhaty, I.A.; Al Hrout, A.; Al Sakkaf, R.; El-Awady, R.; Ashraf, S.S.; Amin, A. Antioxidant and anticancer activities of Trigonella foenum-graecum, Cassia acutifolia and Rhazya stricta. BMC Complement Altern. Med. 2018, 18, 240. [Google Scholar] [CrossRef]
- Sreelatha, S.; Padma, P.R.; Umasankari, E. Evaluation of anticancer activity of ethanol extract of Sesbania grandiflora (Agati Sesban) against Ehrlich ascites carcinoma in Swiss albino mice. J. Ethnopharmacol. 2011, 134, 984–987. [Google Scholar] [CrossRef]
- Ponnanikajamideen, M.; Nagalingam, M.; Vanaja, M.; Malarkodi, C.; Rajeshkumar, S. Anticancer activity of different solvent extracts of Sesbania grandiflora against neuroblastoma (imr-32) and colon (ht-29) cell lines. Eur. J. Biomed. Pharm. Sci. 2015, 2, 509–517. [Google Scholar]
- Cai, Y.Z.; Sun, M.; Xing, J.; Luo, Q.; Corke, H. Structure–radical scavenging activity relationships of phenolic compounds from traditional Chinese medicinal plants. Life Sci. 2006, 78, 2872–2888. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, J.; Luo, J.; Lai, F.; Wang, Z.; Tong, H.; Lu, D.; Bu, H.; Zhang, R.; Lin, S. Antiangiogenic effects of oxymatrine on pancreatic cancer by inhibition of the NF-κB-mediated VEGF signaling pathway. Oncol. Rep. 2013, 30, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Zhang, T.; Su, J.; Wang, K.; Li, X. Oxymatrine targets EGFRp-Tyr845 and inhibits EGFR-related signaling pathways to suppress the proliferation and invasion of gastric cancer cells. Cancer Chemother. Pharmacol. 2015, 75, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Huang, W.; Guo, Y.; Xia, P.; Sun, X.; Pan, X.; Hu, W. Oxymatrine inhibits the proliferation of prostate cancer cells in vitro and in vivo. Mol. Med. Rep. 2015, 11, 4129–4134. [Google Scholar] [CrossRef]
- Ying, X.J.; Jin, B.; Chen, X.W.; Xie, J.; Xu, H.M.; Dong, P. Oxymatrine downregulates HPV16E7 expression and inhibits cell proliferation in laryngeal squamous cell carcinoma Hep-2 cells in vitro. Biomed Res. Int. 2015, 2015, 150390. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.; Huang, J. Oxymatrine inhibits epithelial-mesenchymal transition through regulation of NF-κB signaling in colorectal cancer cells. Oncol. Rep 2016, 36, 1333–1338. [Google Scholar] [CrossRef]
- Lin, B.; Li, D.; Zhang, L. Oxymatrine mediates Bax and Bcl-2 expression in human breast cancer MCF-7 cells. Die Pharm. Int. J. Pharm. Sci. 2016, 71, 154–157. [Google Scholar]
- Liu, Y.; Bi, T.; Dai, W.; Wang, G.; Qian, L.; Gao, Q.; Shen, G. RETRACTED: Effects of oxymatrine on the proliferation and apoptosis of human hepatoma carcinoma cells. Technol. Cancer Res. Treat. 2016, 15, 487–497. [Google Scholar] [CrossRef]
- Pei, Z.; Zeng, J.; Gao, Y.; Li, F.; Li, W.; Zhou, H.; Yang, Y.; Wu, R.; Chen, Y.; Liu, J. Oxymatrine inhibits the proliferation of CaSki cells via downregulating HPV16E7 expression. Oncol. Rep. 2016, 36, 291–298. [Google Scholar] [CrossRef]
- Ye, J.; Zou, M.M.; Li, P.; Lin, X.J.; Jiang, Q.W.; Yang, Y.; Huang, J.R.; Yuan, M.L.; Xing, Z.H.; Wei, M.N.; et al. Oxymatrine and cisplatin synergistically enhance the anti-tumor immunity of CD8+ T cells in non-small cell lung cancer. Front. Oncol. 2018, 8, 631. [Google Scholar] [CrossRef]
- Zhang, L.; Khoo, C.; Koyyalamudi, S.R.; Pedro, N.D.; Reddy, N. Antioxidant, anti-inflammatory, and anticancer activities of ethanol-soluble organics from water extracts of selected medicinal herbs and their relation with flavonoid and phenolic contents. Pharmacologia 2017, 8, 59–72. [Google Scholar]
- Gulecha, V.; Sivakuma, T. Anticancer activity of Tephrosia purpurea and Ficus religiosa using MCF 7 cell lines. Asian Pac. J. Trop. Med. 2011, 4, 526–529. [Google Scholar] [CrossRef]
- Lellau, T.F.; Liebezeit, G. Cytotoxic and antitumor activities of ethanolic extracts of salt Marsh plants from the Lower Saxonian Wadden Sea, Southern North Sea. Pharm. Biol. 2003, 41, 293–300. [Google Scholar] [CrossRef]
- Khazaei, M.; Pazhouhi, M. Antiproliferative effect of Trifolium pratens L. extracts in human breast cancer cells. Nutr. Cancer 2019, 71, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Dong, A.; Gao, C.; Tan, C.; Xie, Z.; Zu, X.; Qu, L.; Jiang, Y. New synthetic flavone derivatives induce apoptosis of hepatocarcinoma cells. Bioorganic Med. Chem. 2010, 18, 6322–6328. [Google Scholar] [CrossRef]
- Khan, A.U.; Dagur, H.S.; Khan, M.; Malik, N.; Alam, M.; Mushtaque, M. Therapeutic role of flavonoids and flavones in cancer prevention: Current trends and future perspectives. Eur. J. Med. Chem. Rep. 2021, 3, 100010. [Google Scholar] [CrossRef]
- Mohamed, M.A.; Hamed, M.M.; Abdou, A.M.; Ahmed, W.S.; Saad, A.M. Antioxidant and cytotoxic constituents from Wisteria sinensis. Molecules 2011, 16, 4020–4030. [Google Scholar] [CrossRef]
- Elekofehinti, O.O.; Iwaloye, O.; Olawale, F.; Ariyo, E.O. Saponins in Cancer Treatment: Current Progress and Future Prospects. Pathophysiology 2021, 28, 250–272. [Google Scholar] [CrossRef]
- Rochfort, S.; Panozzo, J. Phytochemicals for health, the role of pulses. J. Agric. Food Chem. 2007, 55, 7981–7994. [Google Scholar] [CrossRef]
- Mudryj, A.N.; Yu, N.; Aukema, H.M. Nutritional and health benefits of pulses. Appl. Physiol. Nutr. Metab. 2014, 39, 1197–1204. [Google Scholar] [CrossRef]
- Singh, B.; Singh, J.P.; Singh, N.; Kaur, A. Saponins in pulses and their health-promoting activities: A review. Food Chem. 2017, 233, 540–549. [Google Scholar] [CrossRef]
- Gurfinkel, D.M.; Rao, A.V. Soyasaponins: The relationship between chemical structure and colon anticarcinogenic activity. Nutr. Cancer 2003, 47, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Dai, Q.; Franke, A.A.; Jin, F.; Shu, X.O.; Hebert, J.R.; Custer, L.J.; Cheng, J.; Gao, Y.T.; Zheng, W. Urinary excretion of phytoestrogens and risk of breast cancer among Chinese women in Shanghai. Cancer Epidemiol. Biomark. Prev. 2002, 11, 815–821. [Google Scholar]
- Najjaa, H.; Abdelkarim, B.A.; Doria, E.; Boubakri, A.; Trabelsi, N.; Falleh, H.; Tlili, H.; Neffati, M. Phenolic composition of some Tunisian medicinal plants associated with an anti-proliferative effect on human breast cancer MCF-7 cells. Eurobiotech J. 2020, 4, 104–112. [Google Scholar] [CrossRef]
- Mondal, A.; Gandhi, A.; Fimognari, C.; Atanasov, A.G.; Bishayee, A. Alkaloids for cancer prevention and therapy: Current progress and future perspectives. Eur. J. Pharmacol. 2019, 858, 172472. [Google Scholar] [CrossRef] [PubMed]
- Dey, P.; Kundu, A.; Chakraborty, H.J.; Kar, B.; Choi, W.S.; Lee, B.M.; Bhakta, T.; Atanasov, A.G.; Kim, H.S. Therapeutic value of steroidal alkaloids in cancer: Current trends and future perspectives. Int. J. Cancer 2019, 145, 1731–1744. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, H.; Yu, P.; Liu, Q.; Liu, K.; Duan, H.; Luan, G.; Yagasaki, K.; Zhang, G. Effects of matrine against the growth of human lung cancer and hepatoma cells as well as lung cancer cell migration. Cytotechnology 2009, 59, 191–200. [Google Scholar] [CrossRef]
- Zhu, X.M.; Du, L.D.; Du, G.H. Cytisine. In Natural Small Molecule Drugs from Plants; Springer: Berlin/Heidelberg, Germany, 2018; pp. 685–689. [Google Scholar]
- Wojtowicz, K.; Januchowski, R.; Sosińska, P.; Nowicki, M.; Zabel, M. Effect of brefeldin A and castanospermine on resistant cell lines as supplements in anticancer therapy. Oncol. Rep. 2016, 35, 2896–2906. [Google Scholar] [CrossRef]
- Sri, K.S.; Erdman, J.W., Jr. Legume carotenoids. Crit. Rev. Food Sci. Nutr. 1987, 26, 137. [Google Scholar]
- Fiedor, J.; Burda, K. Potential role of carotenoids as antioxidants in human health and disease. Nutrients 2014, 6, 466–488. [Google Scholar] [CrossRef]
- Nishino, H.; Tokuda, H.; Murakoshi, M.; Satomi, Y.; Masuda, M.; Onozuka, M.; Yamaguchi, S.; Takayasu, J.; Tsuruta, J.; Okuda, M.; et al. Cancer prevention by natural carotenoids. Biofactors 2000, 13, 89–94. [Google Scholar] [CrossRef]
- Horvath, G.; Csikós, E.; Andres, E.V.; Bencsik, T.; Takátsy, A.; Gulyás-Fekete, G.; Turcsi, E.; Deli, J.; Szőke, É.; Kemény, Á.; et al. Analyzing the Carotenoid Composition of Melilot (Melilotus officinalis (L.) Pall.) Extracts and the Effects of Isolated (All-E)-lutein-5, 6-epoxide on Primary Sensory Neurons and Macrophages. Molecules 2021, 26, 503. [Google Scholar] [CrossRef] [PubMed]
- Krinsky, N.I.; Johnson, E.J. Carotenoid actions and their relation to health and disease. Mol. Asp. Med. 2005, 26, 459–516. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L. Anti-inflammatory agents, and antioxidants as a possible “third great wave” in cardiovascular secondary prevention. Am. J. Cardiol. 2008, 101, S4–S13. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Zhang, Y.; Li, Q.; Yang, L.; Zhang, N.; Ma, S.; Zhang, K.; Song, J.; Guan, F. β-Carotene Induces Apoptosis in Human Esophageal Squamous Cell Carcinoma Cell Lines via the Cav-1/AKT/NF-κB Signaling Pathway. J. Biochem. Mol. Toxicol. 2016, 30, 148–157. [Google Scholar] [CrossRef] [PubMed]
- El Gaafary, M.; Büchele, B.; Syrovets, T.; Agnolet, S.; Schneider, B.; Schmidt, C.Q.; Simmet, T. An α-acetoxy-tirucallic acid isomer inhibits Akt/mTOR signaling and induces oxidative stress in prostate cancer cells. J. Pharmacol. Exp. Ther. 2015, 352, 33–42. [Google Scholar] [CrossRef]
- Matus, M.F.; Jorquera-Román, M.; Zúñiga-Hernández, J. Anti-proliferative effect of terpenes on human prostate cancer cells: Natural sources and their potential role as chemopreventive agents. Rev. Chil. Nutr. 2017, 44, 371–382. [Google Scholar] [CrossRef]
- Satia, J.A.; Littman, A.; Slatore, C.G.; Galanko, J.A.; White, E. Long-term use of β-carotene, retinol, lycopene, and lutein supplements and lung cancer risk: Results from the Vitamins and Lifestyle (VITAL) study. Am. J. Epidemiol. 2009, 169, 815–828. [Google Scholar] [CrossRef]
- Gong, X.; Smith, J.R.; Swanson, H.M.; Rubin, L.P. Carotenoid lutein selectively inhibits breast cancer cell growth and potentiates the effect of chemotherapeutic agents through ROS-mediated mechanisms. Molecules 2018, 23, 905. [Google Scholar] [CrossRef]
- Rafi, M.M.; Kanakasabai, S.; Gokarn, S.V.; Krueger, E.G.; Bright, J.J. Dietary lutein modulates growth and survival genes in prostate cancer cells. J. Med. Food 2015, 18, 173–181. [Google Scholar] [CrossRef]
- Kim, J.; Lee, J.; Oh, J.H.; Chang, H.J.; Sohn, D.K.; Kwon, O.; Shin, A.; Kim, J. Dietary lutein plus zeaxanthin intake and DICER1 rs3742330 A > G polymorphism relative to colorectal cancer risk. Sci. Rep. 2019, 9, 3406. [Google Scholar] [CrossRef]
- Kumar, N.; Goel, N. Phenolic acids: Natural versatile molecules with promising therapeutic applications. Biotechnol. Rep. 2019, 24, e00370. [Google Scholar] [CrossRef]
- Behbahani, M.; Abolhasani, J.; Amini, M.M.; Sadeghi, O.; Omidi, F.; Bagheri, A.; Salarian, M. Application of mercapto ordered carbohydrate-derived porous carbons for trace detection of cadmium and copper ions in agricultural products. Food Chem. 2015, 173, 1207–1212. [Google Scholar] [CrossRef] [PubMed]
- Rashmi, H.B.; Negi, P.S. Phenolic acids from vegetables: A review on processing stability and health benefits. Food Res. Int. 2020, 136, 109298. [Google Scholar] [CrossRef]
- Al Jitan, S.; Alkhoori, S.A.; Yousef, L.F. Phenolic acids from plants: Extraction and application to human health. Stud. Nat. Prod. Chem. 2018, 58, 389–417. [Google Scholar]
- Anantharaju, P.G.; Gowda, P.C.; Vimalambike, M.G.; Madhunapantula, S.V. An overview on the role of dietary phenolics for the treatment of cancers. Nutr. J. 2016, 15, 99. [Google Scholar] [CrossRef] [PubMed]
- Palko-Labuz, A.; Gliszczyńska, A.; Skonieczna, M.; Poła, A.; Wesołowska, O.; Środa-Pomianek, K. Conjugation with phospholipids as a modification increasing anticancer activity of phenolic acids in metastatic melanoma–In vitro and in silico studies. Int. J. Mol. Sci. 2021, 22, 8397. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).