Evaluation of 2-Thioxoimadazolidin-4-one Derivatives as Potent Anti-Cancer Agents through Apoptosis Induction and Antioxidant Activation: In Vitro and In Vivo Approaches
Abstract
1. Introduction
2. Results
2.1. Cytotoxic Activity
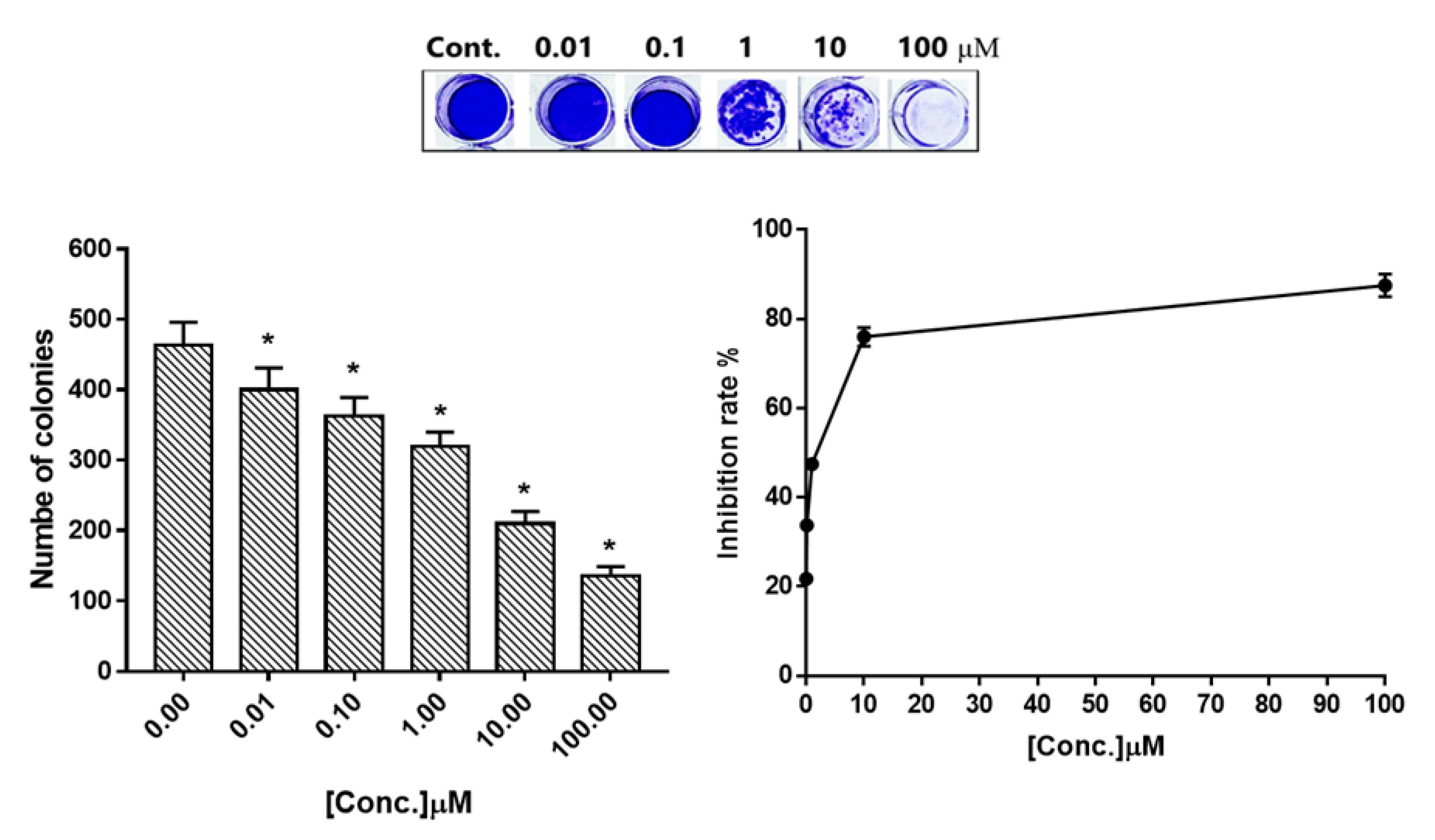
2.2. Colony Forming Assay
2.3. Apoptotic Investigation
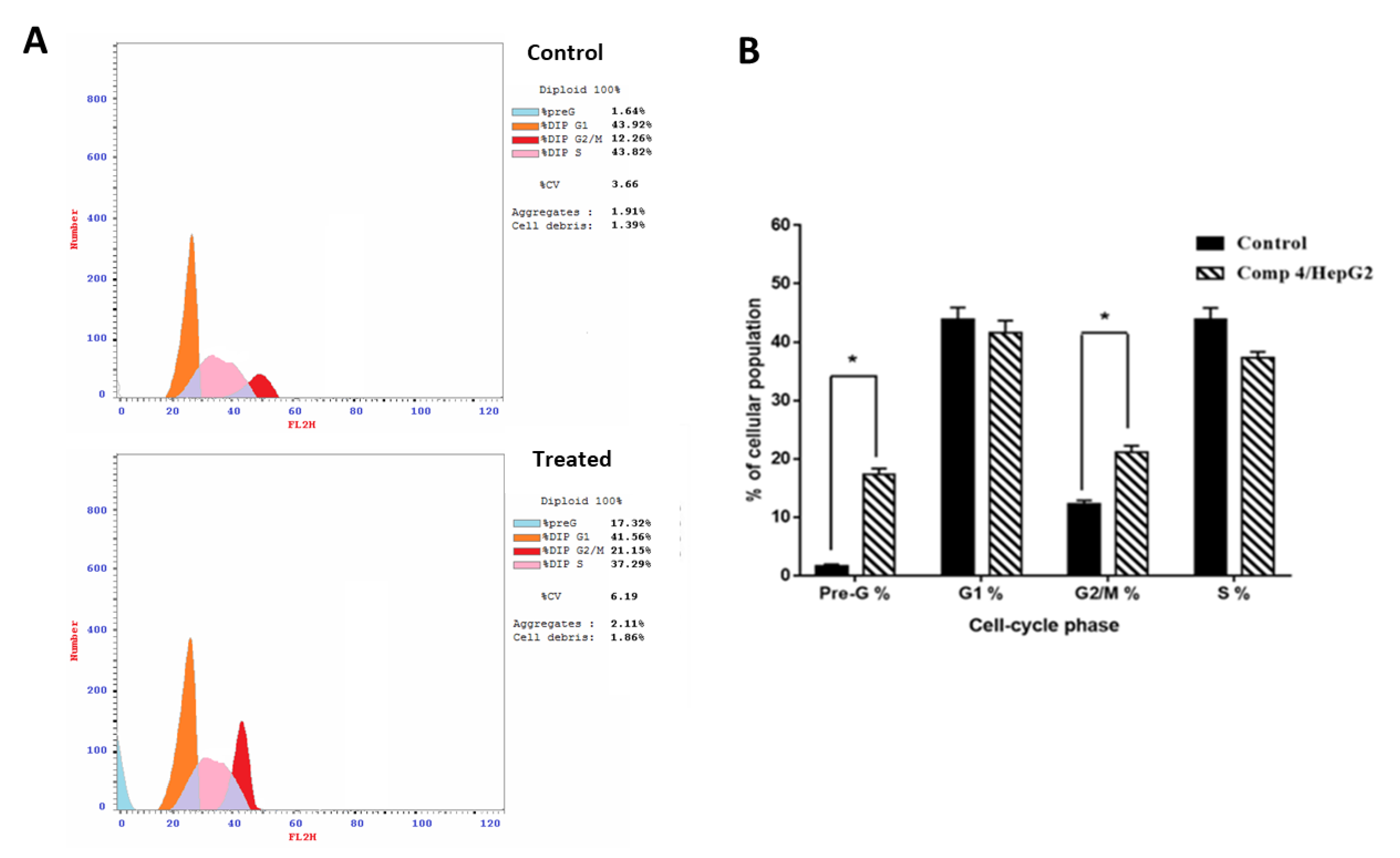
2.3.1. Compound 4 Induces Cell Cycle Arrest in G2/M Phase in HepG2 Cells
2.3.2. Compound 4 Treatment Induced Apoptosis in HepG2 Cells
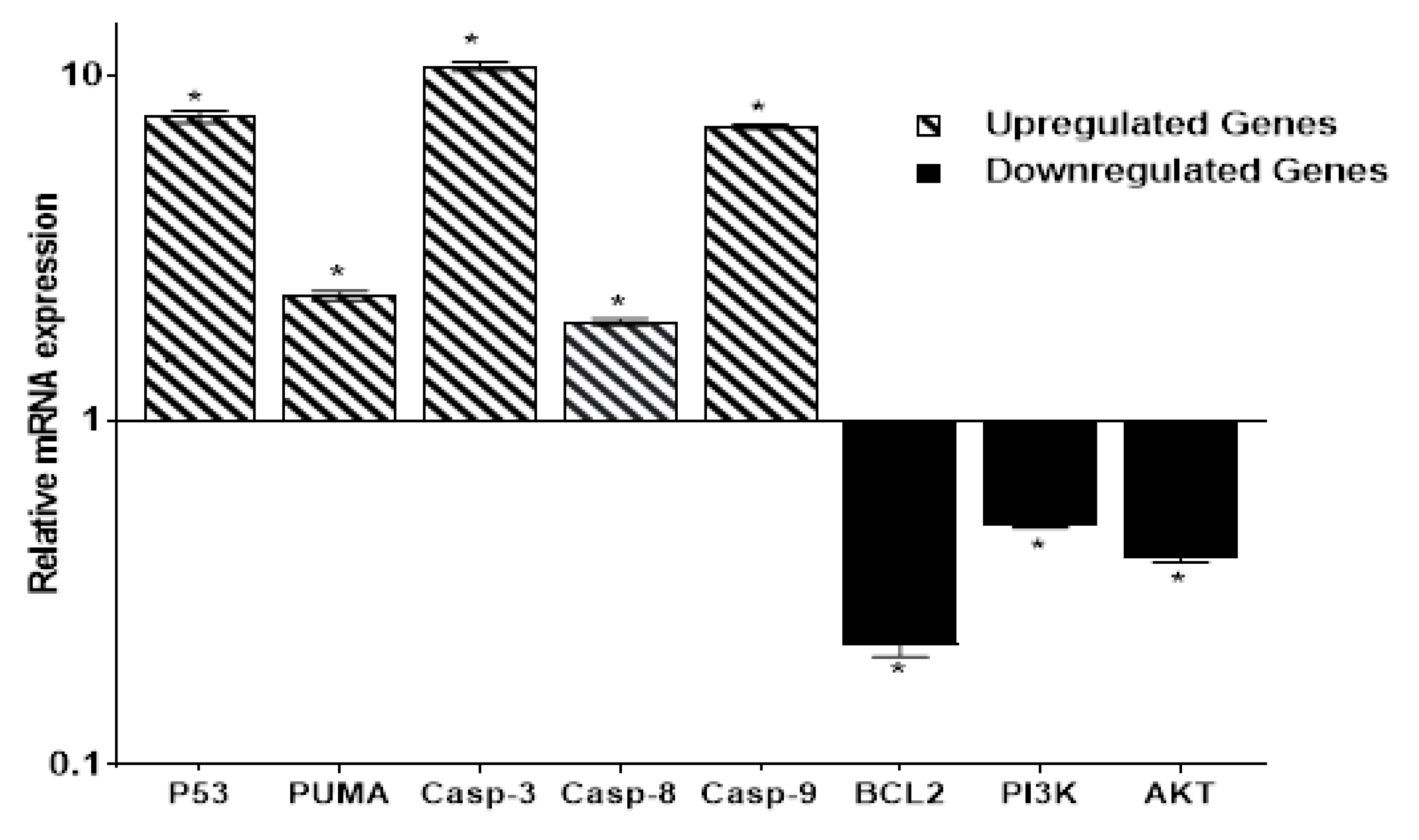
2.3.3. Compound 4 Treatment Induced Up and Downregulation of Apoptosis-Related Genes in HepG2 Cells
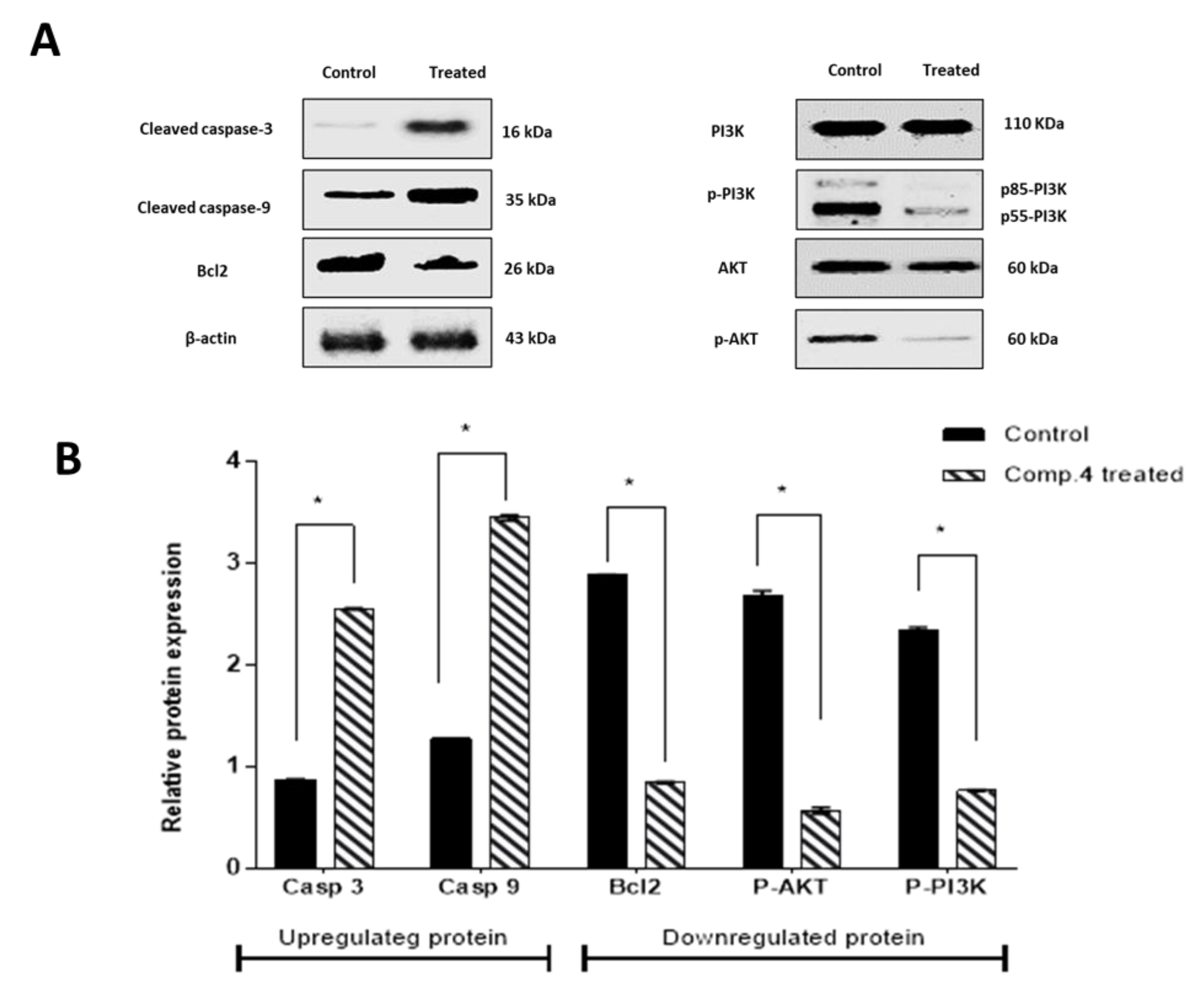
2.3.4. Compound 4 Induced Up and Downregulation of Target Proteins in HepG2 Cells
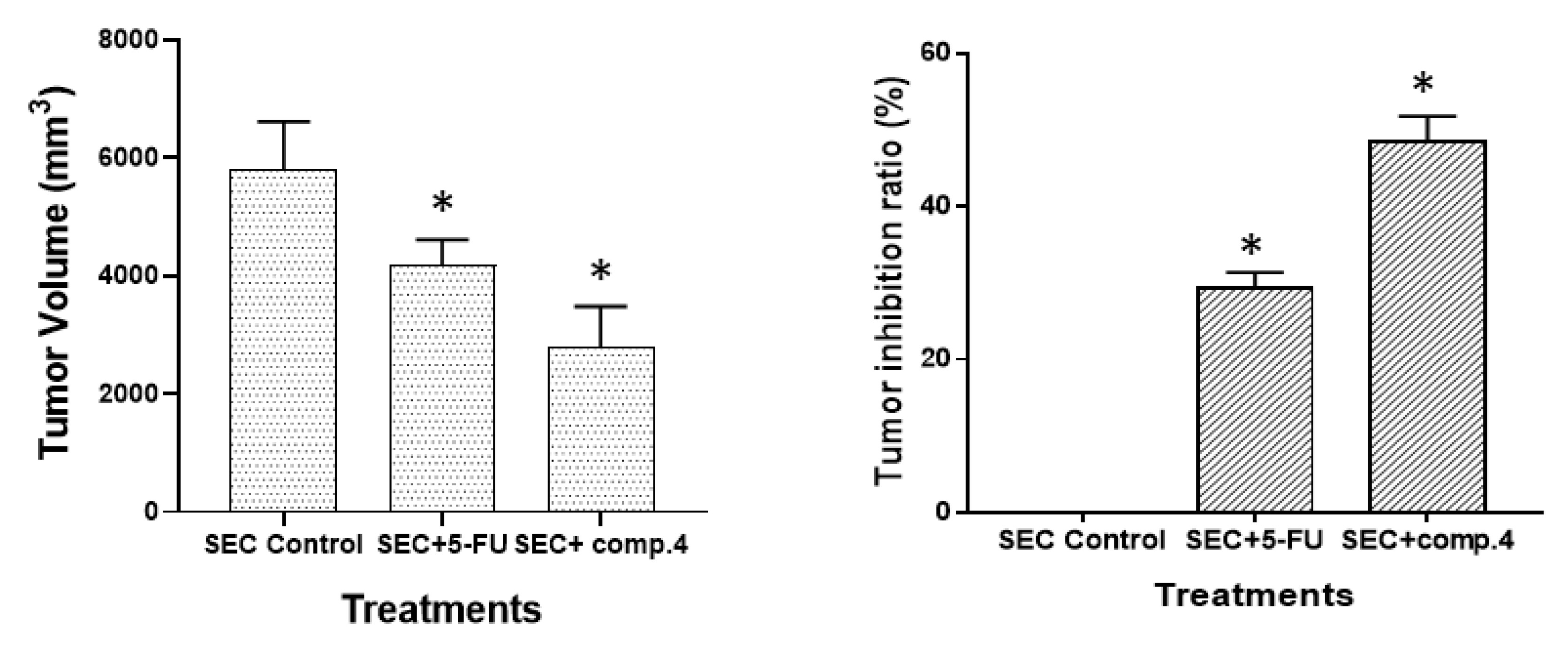
2.4. In Vivo Study
2.4.1. Anti-Tumor Potentiality
2.4.2. Hematological Parameters
2.4.3. Biochemical Parameters
2.4.4. Compound 4 Treatment Induced Antioxidant Activation
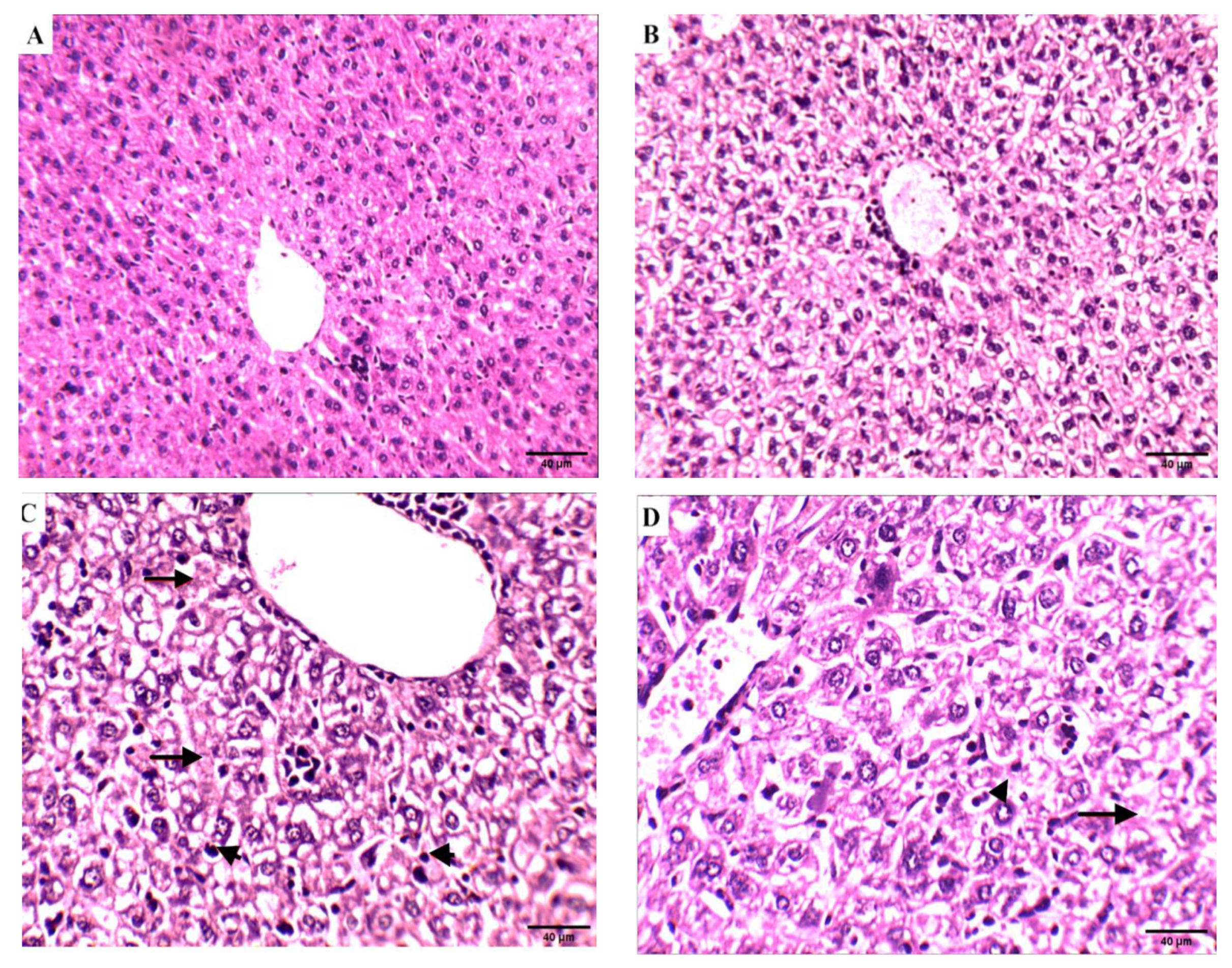
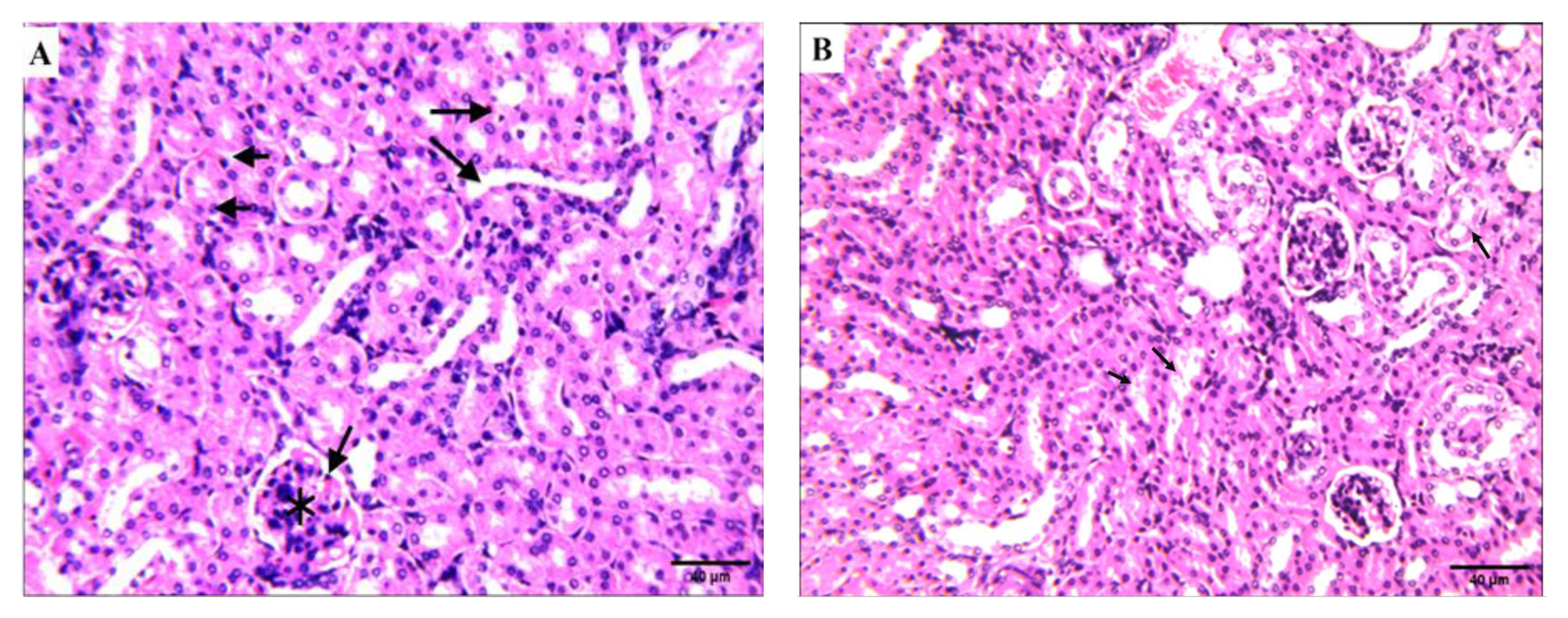
2.4.5. Histopathological Examinations
Effect of Compound 4 on the Liver Tissue of SEC-Bearing Mice
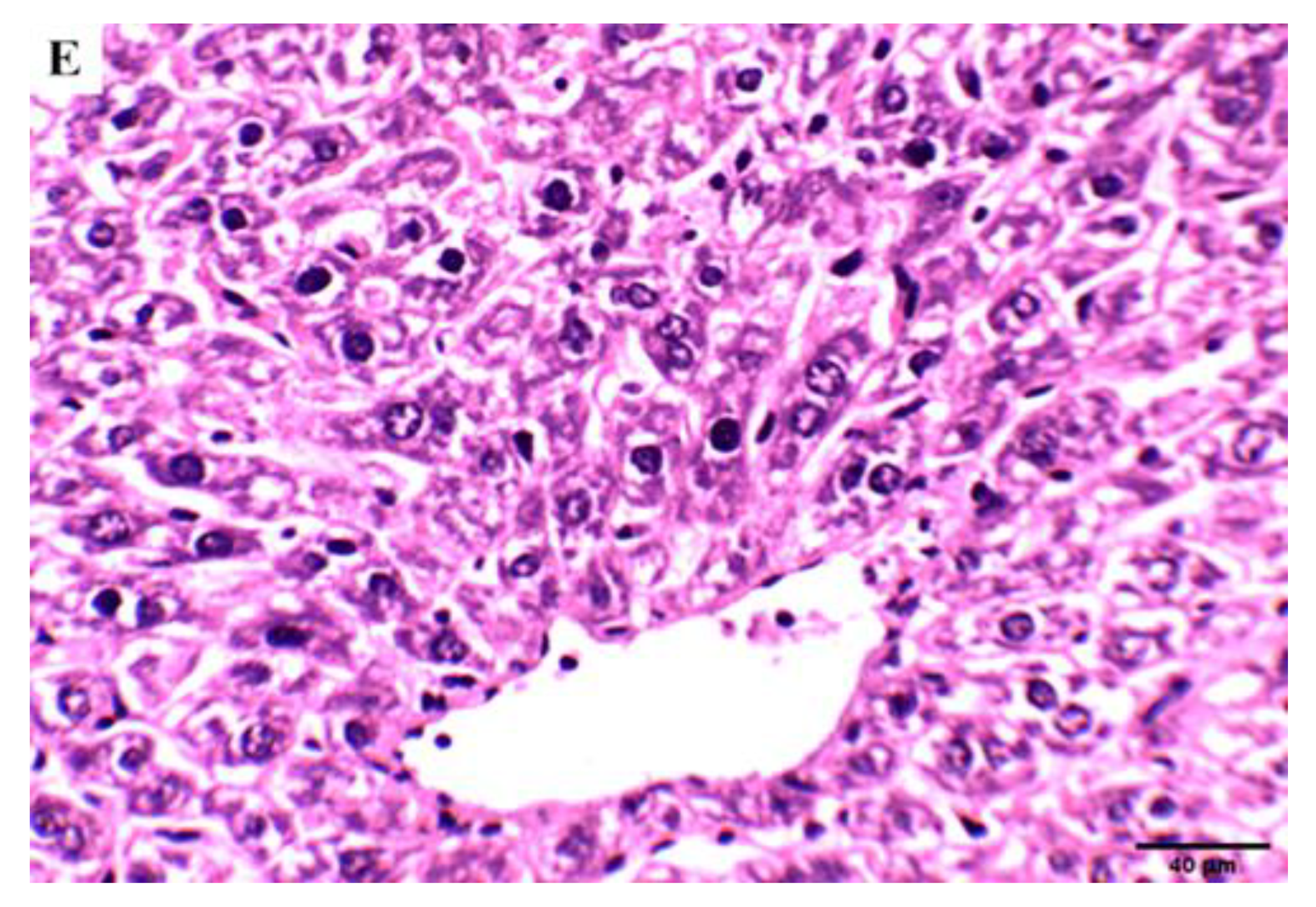
Effect of Compound 4 on the Kidney Tissue of SEC-Bearing Mice
2.5. In Silico Studies
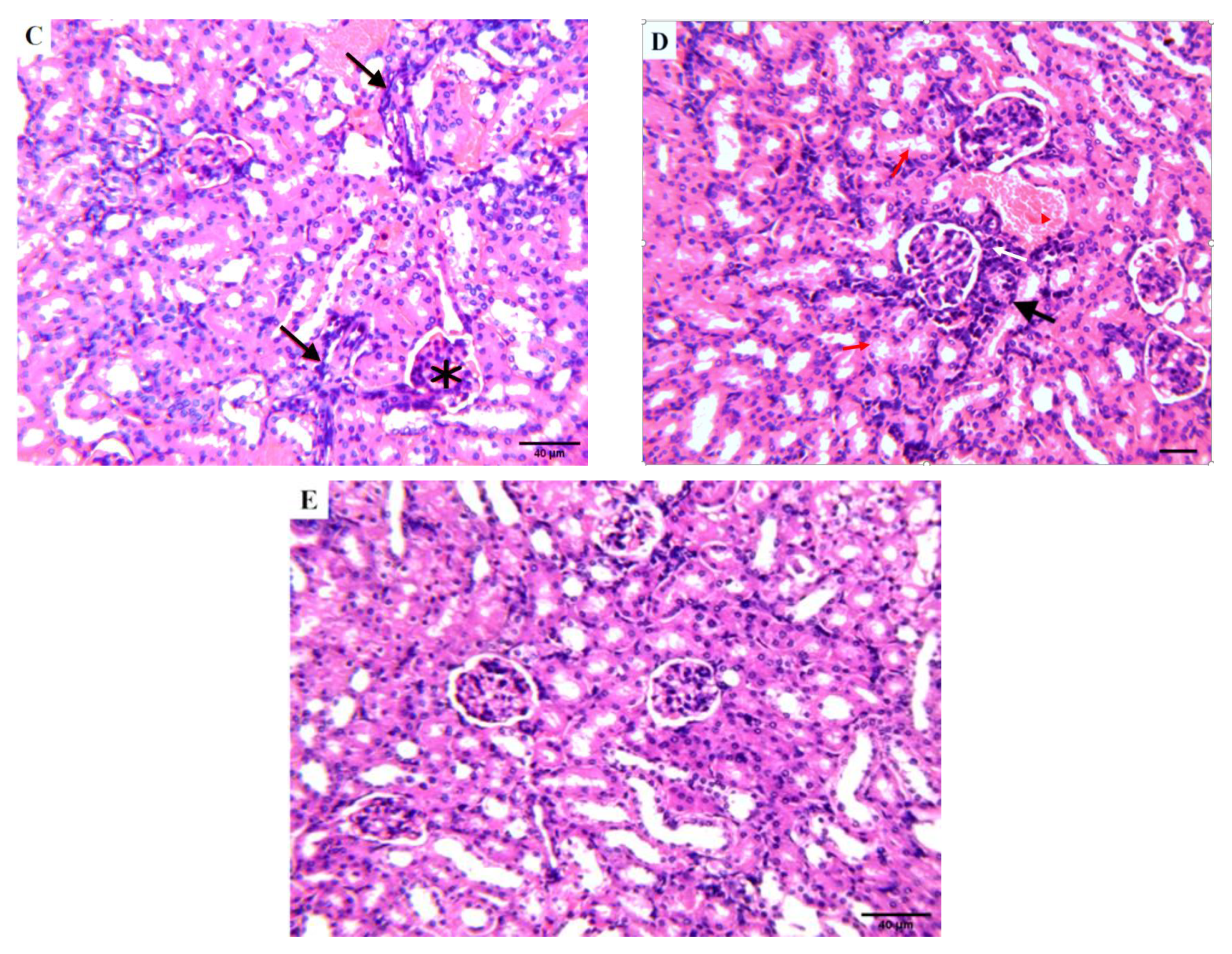
2.5.1. Molecular Docking
2.5.2. ADME Pharmacokinetics
3. Discussion
4. Materials and Methods
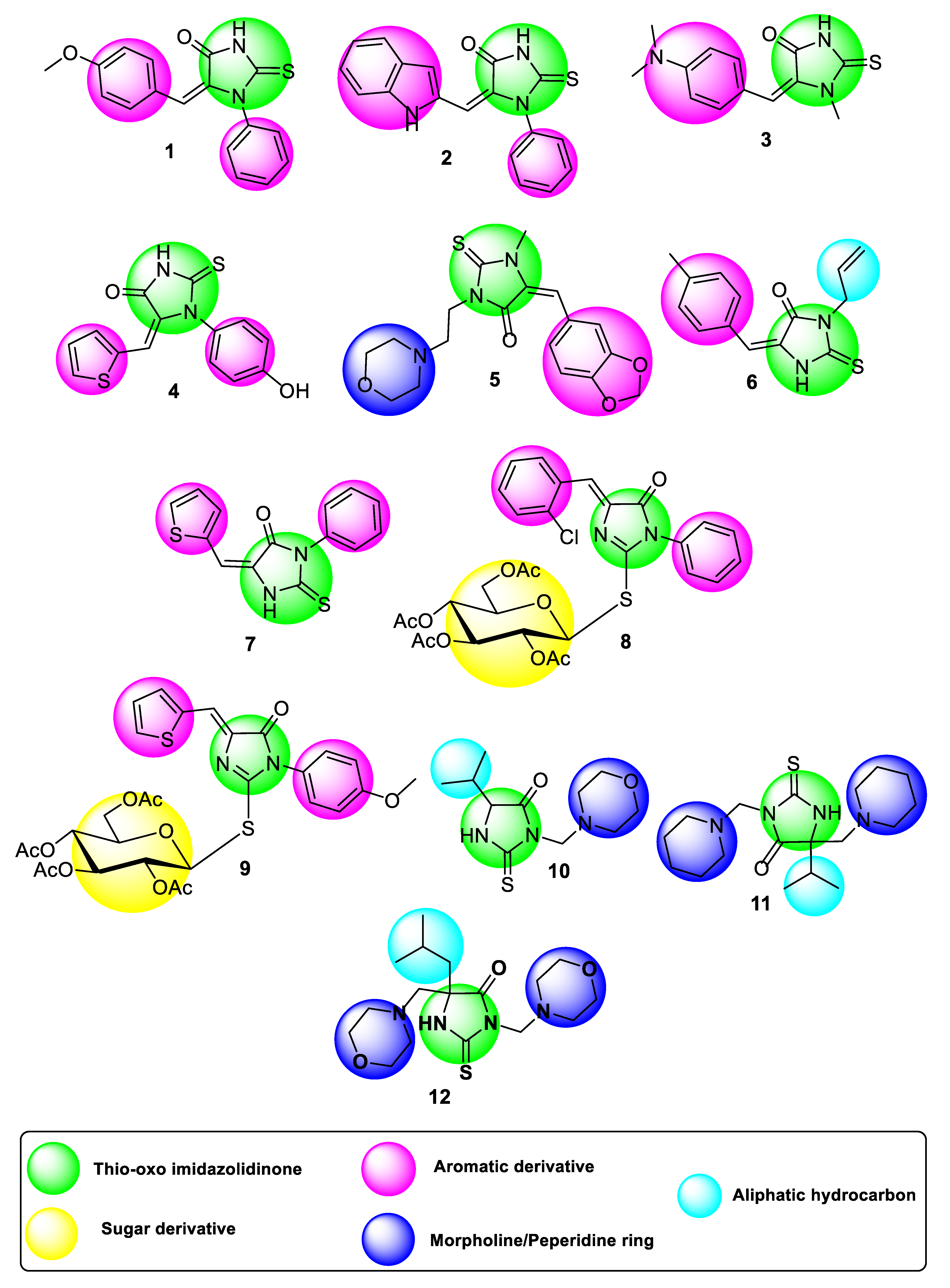
4.1. Chemistry of Compounds 1–12
4.2. MTT Assay for Cytotoxic Screening
4.3. Colony Forming Assay
4.4. Apoptosis Investigation Assays
4.4.1. Flow Cytometric Analysis
4.4.2. Gene Expression (RT-PCR) Analysis
4.4.3. Western Blot
4.5. In Vivo Assay
4.5.1. Animals
4.5.2. Median Lethal Dose (LD50)
4.5.3. Tumor Cell Line and Transplantation
4.5.4. Experimental Design
4.5.5. Tumor Volume and Tumor Inhibition Ratio (TIR%)
4.5.6. Hematological Assays
4.5.7. Serum Biochemical Parameters
4.5.8. Oxidant and Antioxidant Assessment
4.5.9. Histopathological Study
4.6. In Silico Studies
4.6.1. Molecular Docking
4.6.2. ADME Pharmacokinetics
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Senwar, K.R.; Reddy, T.S.; Thummuri, D.; Sharma, P.; Naidu, V.G.M.; Srinivasulu, G.; Shankaraiah, N. Design, synthesis and apoptosis inducing effect of novel (Z)-3-(3′-methoxy-4′-(2-amino-2-oxoethoxy)-benzylidene) indolin-2-ones as potential antitumor agents. Eur. J. Med. Chem. 2016, 118, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Subramanian, S.; Boggu, P.R.; Yun, J.; Jung, S.-H. Identification of N-arylsulfonylpyrimidones as anticancer agents. Arch. Pharmacal Res. A Publ. PSK 2018, 41, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Avendano, C.; Menendez, J.C. Med Chem Anticancer Agents; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Varmus, H. The New Era in Cancer Research. Science 2006, 312, 1162–1165. [Google Scholar] [CrossRef]
- Eckhardt, B.S.P.S. Recent Progress in the Development of Anticancer Agents. CMCACA 2002, 2, 419–439. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aziz, A.A.-M.; El-Azab, A.S.; Abou-Zeid, L.A.; ElTahir, K.E.H.; Abdel-Aziz, N.I.; Ayyad, R.R.; Al-Obaid, A.M. Synthesis, anti-inflammatory, analgesic and COX-1/2 inhibition activities of anilides based on 5,5-diphenylimidazolidine-2,4-dione scaffold: Molecular docking studies. Eur. J. Med. Chem. 2016, 115, 121–131. [Google Scholar] [CrossRef]
- Vasir, J.K.; Labhasetwar, V. Targeted Drug Delivery in Cancer Therapy. Technol. Cancer Res. Treat. 2005, 4, 363–374. [Google Scholar] [CrossRef]
- Lipinski, C.A. Lead and drug-like compounds: The rule-of-five revolution. Drug Discov. Technol. 2004, 1, 337–341. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 2001, 46, 3–26. [Google Scholar] [CrossRef]
- Tompkins, J.E. 5,5-Diaryl-2-thiohydantoins and 5,5-diaryl N3- substituted 2-thiohydantoins as potential hypolipidemic agents. J. Med. Chem. 1986, 29, 855–864. [Google Scholar] [CrossRef]
- Khodair, A.I.; El-subbagh, H.I.; Al-Obaid, A.M. Phosphorus Sulfur Silicon. Relat. Elem. 1998, 140, 159. [Google Scholar] [CrossRef]
- Takahashi, A.; Matsuoka, H.; Ozawa, Y.; Uda, Y. Antimutagenic Properties of 3,5-Disubstituted 2-Thiohydantoins. J. Agric. Food Chem. 1998, 46, 5037–5041. [Google Scholar] [CrossRef]
- Froelich, E.; Fruehan, A.; Jackman, M.; Kirchner, F.K.; Alexander, E.J.; Archer, S. 5-heptyl-2-thiohydantion, a new antitubercular agent. J. Am. Chem. Soc. 1954, 76, 3099–4105. [Google Scholar] [CrossRef]
- Marx, J.V.; Richert, D.A.; Westerfeld, W.W. Peripheral inhibition of thyroxine by thiohydantoins derived from amino acids. J. Med. Chem. 1970, 13, 1179–1181. [Google Scholar]
- El-Barbary, A.A.; Khodair, A.I.; Pedersen, E.B.; Nielsen, C. SGlucosylated hydantoins as new antiviral agents. J. Med. Chem. 1994, 37, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, G.; Bascou, J.P.; Perez, J.; Gadras, A. Fungicidal Optically Active 1-(mono-or Substituted Amino)-2-substituted-4,4- disubstituted-2-imidazolin-5-ones and 5- thiones Corresponding. U.S. Patent 6,018,052, 5 February 2002. [Google Scholar]
- Lacroix, G.; Bascou, J.-P.; Perez, J.; Gadras, A. Optically Active 5,5-disubstituted-3-(mono- or Disubstituted Amino)-2-thiohydantoin Intermediates to Fungicidal 2-imidazolin-5-ones. U.S. Patent 5,650,519, 22 July 1997. [Google Scholar]
- Živković, M.B.; Matić, I.Z.; Rodić, M.V.; Novaković, I.T.; Sladić, D.M.; Krstić, N.M. Synthesis, characterization and in vitro cytotoxic activities of new steroidal thiosemicarbazones and thiadiazolines. RSC Adv. 2016, 6, 34312–34333. [Google Scholar] [CrossRef]
- Vengurlekar, R.S.S. A Study on the Biological Activity of 2-thioxo-imidazolidin-4-ones. Lett. Drug. Des. Discov. 2012, 9, 549–555. [Google Scholar] [CrossRef]
- Jiheel1, M.; Al-Rekaabi, A.; Alqurashy, N.; Deresawi, M.A. The Effect of 2-Thioxo Imidazolidin-4-Ones (2- Thiohydantion) on Anticancer Activity: An in Vitro Study. Indian J. Forensic Med. Toxicol. 2020, 14, 3201–3206. [Google Scholar] [CrossRef]
- Koff, J.L.; Ramachandiran, S.; Bernal-Mizrachi, L.A. Time to kill: Targeting apoptosis in cancer. Int. J. Mol. Sci. 2015, 16, 2942–2955. [Google Scholar] [CrossRef]
- Pistritto, G.; Trisciuoglio, D.; Ceci, C.; Garufi, A.; D’Orazi, G. Apoptosis as anticancer mechanism: Function and dysfunction of its modulators and targeted therapeutic strategies. Aging 2016, 8, 603–619. [Google Scholar] [CrossRef]
- Elhady, H.A.; El-Sayed, R.; Al-nathali, H.S. Design, synthesis and evaluation of anticancer activity of novel 2-thioxoimidazolidin-4-one derivatives bearing pyrazole, triazole and benzoxazole moieties. Chem. Cent. J. 2018, 12, 51. [Google Scholar] [CrossRef]
- Lopez, J.; Tait, S.W. Mitochondrial apoptosis: Killing cancer using the enemy within. Br. J. Cancer 2015, 112, 957–962. [Google Scholar] [CrossRef]
- Zhang, J.H.; Xu, M. DNA fragmentation in apoptosis. Cell Res. 2000, 10, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Xu, F.; Shuai, W.; Sun, H.; Yao, H.; Ma, C.; Xu, S.; Yao, H.; Zhu, Z.; Yang, D.-H.; et al. Discovery of Novel Quinoline–Chalcone Derivatives as Potent Anti-tumor Agents with Microtubule Polymerization Inhibitory Activity. J. Med. Chem. 2019, 62, 993–1013. [Google Scholar] [CrossRef] [PubMed]
- Klaunig, J.E. Oxidative stress and cancer. Curr. Pharm. Des. 2018, 24, 4771–4778. [Google Scholar] [CrossRef] [PubMed]
- El-Osta, H.; Circu, M.L. Mitochondrial ROS and apoptosis. In Mitochondrial Mechanisms of Degeneration and Repair in Parkinson’s Disease; Buhlman, L., Ed.; Springer: Cham, Germany, 2016; pp. 1–23. [Google Scholar]
- Çomu, F.M.; Kılıç, Y.; Ozer, A.; Kirişçi, M.; Dursun, A.D.; Tatar, T.; Zor, M.H.; Kartal, H.; Küçük, A.; Boyunaga, H.; et al. Effect of picroside II on erythrocyte deformability and lipid peroxidation in rats subjected to hind limb ischemia reperfusion injury. Drug Des. Devel. Ther. 2016, 10, 927–931. [Google Scholar] [PubMed]
- Baig, S.; Seevasant, I.; Mohamad, J.; Mukheem, A.; Huri, H.Z.; Kamarul, T. Potential of apoptotic pathway-targeted cancer therapeutic research: Where do we stand? Cell Death Dis. 2016, 7, e2058. [Google Scholar] [CrossRef]
- Fulda, S. Therapeutic opportunities based on caspase modulation. Semin. Cell Dev. Biol. 2018, 82, 150–157. [Google Scholar] [CrossRef]
- Brockmann, A.; Bluwstein, A.; Kögel, A.; May, S.; Marx, A.; Tschan, M.P.; Brunner, T. Thiazolides promote apoptosis in colorectal tumor cells via MAP kinase-induced Bim and Puma activation. Cell Death Dis. 2015, 6, e1778. [Google Scholar] [CrossRef][Green Version]
- Faes, S.; Dormond, O. PI3K and AKT: Unfaithful Partners in Cancer. Int. J. Mol. Sci. 2015, 16, 21138–21152. [Google Scholar] [CrossRef]
- Kattan, S.W.; Nafie, M.S.; Elmgeed, G.A.; Alelwani, W.; Badar, M.; Tantawy, M.A. Molecular docking, antiproliferative activity and induction of apoptosis in human liver cancer cells treated with androstane derivatives: Implication of PI3K/AKT/mTOR pathway. J. Steroid. Biochem. Mol. Biol. 2020, 198, 105604. [Google Scholar] [CrossRef]
- Sarhan, A.A.M.; Boraei, A.T.A.; Barakat, A.; Nafie, M.S. Discovery of hydrazide-based pyridazino[4,5-b]indole scaffold as a new phosphoinositide 3-kinase (PI3K) inhibitor for breast cancer therapy. RSC Adv. 2020, 10, 19534–19541. [Google Scholar] [CrossRef]
- IMayer, A.; Arteaga, C.L. The PI3K/AKT Pathway as a Target for Cancer Treatment. Annu. Rev. Med. 2016, 67, 11–28. [Google Scholar] [CrossRef]
- Sabbah, D.A.; Brattain, M.G.; Zhong, H. Dual Inhibitors of PI3K/mTOR or mTOR-Selective Inhibitors: Which Way Shall We Go? CMC 2011, 18, 5528–5544. [Google Scholar] [CrossRef]
- Tarantelli, C.; Lupia, A.; Stathis, A.; Bertoni, F. Is There a Role for Dual PI3K/mTOR Inhibitors for Patients Affected with Lymphoma? IJMS 2020, 21, 1060. [Google Scholar] [CrossRef]
- Alapati, V.; Noolvi, M.N.; Manjula, S.N.; Pallavi, K.J.; Patel, H.M.; Tippeswamy, B.S.; Satyanarayana, S.V. In vivo anti-tumour activity of novel Quinazoline derivatives. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1753–1764. [Google Scholar] [PubMed]
- Amakiri, A.O.; Owen, O.J.; Ngodigha, E.M.; Jack, D.O. Effect of Refined Petroleum Product (Kerosene) Flame and Fumes on Serum Enzyme Characteristics of Broiler Chickens. Int. J. Poult. Sci. 2008, 7, 1039–1041. [Google Scholar] [CrossRef]
- Marslin, G.; Sheeba, C.J.; Kalaichelvan, V.K.; Manavalan, R.; Reddy, P.N.; Franklin, G. Poly (D,L-lactic-co-glycolic acid) Nanoencapsulation Reduces Erlotinib-Induced Subacute Toxicity in Rat. J. Biomed. Nanotechnol. 2009, 5, 464–471. [Google Scholar] [CrossRef]
- Sidorov, K.K. About harmonization of domestic and international classifications of acute toxicity of chemicals. Toxicol. Vestn. 2004, 6, 2–3. [Google Scholar]
- Khodair, A.I.; El-barbary, A.A.; Abbas, Y.A.; Imam, D.R. Synthesis, Reactions and Conformational Analysis of 5-Arylidene-2-Thiohydantoins as Potential Antiviral Agents, Phosphorus. Phosphorus. Sulfur. Silicon. Relat. Elem. 2001, 170, 261–278. [Google Scholar] [CrossRef]
- Khodair, A.I. Glycosylation of 2-thiohydantoin derivatives. Synthesis of some novel S-alkylated and S-glucosylated hydantoins. Carbohydr. Res. 2001, 331, 445–453. [Google Scholar] [CrossRef]
- Khodair, A.I.; Gesson, J.-P. Sulfur Glycosylation Reactions Involving 3-Allyl-2-Thiohydantoin Nucleoside Bases as Potential Antiviral and Anti-tumor Agents. Phosphorus. Sulfur. Silicon. Relat. Elem. 1998, 142, 167–190. [Google Scholar] [CrossRef]
- Khodair, A.I. Synthesis of 2-Thiohydantoins and Their S-Glucosylated Derivatives as Potential Antiviral and Anti-tumor Agents. Nucleos. Nucleot. Nucl. 2001, 20, 1735–1750. [Google Scholar] [CrossRef]
- Khodair, A.I.; Bakare, S.B.; Awad, M.K.; Nafie, M.S. Design, synthesis, DFT, molecular modelling studies and biological evaluation of novel 3-substituted (E)-5-(arylidene)-1-methyl-2-thioxoimidazolidin-4-ones with potent cytotoxic activities against breast MCF-7, liver HepG2, and lung A549. J. Mol. Struct. 2020, 129805. [Google Scholar] [CrossRef]
- Elbadawi, M.M.; Khodair, A.I.; Awad, M.K.; Kassab, S.E.; Elsaady, M.T.; Abdellatif, K.R.A. Design, Synthesis and Biological Evaluation of Novel Thiohydantoin Derivatives as Antiproliferative Agents: A Combined Experimental and Theoretical Assessments. J. Mol. Struct. 2022, 1249, 131574. [Google Scholar] [CrossRef]
- Khodair, A.I.A.; El Ashry, E.S.H.; Al-Masoudi, N.A.L. Thiohydantoin nucleosides. synthesis approaches. Monch. Für Chemi. 2004, 135, 1061–1079. [Google Scholar]
- Khodair, A.I.; Nielsen, J. Synthesis of 3-Substituted 5-Arylidene-1-methyl-2-thiohydantoins under Microwave Irradiation. Heterocycles 2002, 57, 1017–1032. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Freshney, R.I. Culture of Tumor Cells, Culture of Animal Cells; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2010; pp. 463–479. [Google Scholar] [CrossRef]
- Tantawy, E.S.; Amer, A.M.; Mohamed, E.K.; Alla, M.M.A.; Nafie, M.S. Synthesis, characterization of some pyrazine derivatives as anticancer agents: In vitro and in Silico approaches. J. Mol. Struct. 2020, 1210, 128013. [Google Scholar] [CrossRef]
- Nafie, M.S.; Amer, A.M.; Mohamed, A.K.; Tantawy, E.S. Discovery of novel pyrazolo[3,4-b] pyridine scaffold-based derivatives as potential PIM-1 kinase inhibitors in breast cancer MCF-7 cells. Bioorg. Med. Chem. 2020, 28, 115828. [Google Scholar] [CrossRef]
- Katz, D.; Ito, E.; Lau, K.S.; Mocanu, J.D.; Bastianutto, C.; Schimmer, A.D.; Liu, F.-F. Increased efficiency for performing colony formation assays in 96-well plates: Novel applications to combination therapies and high-throughput screening. Biotechniques 2008, 44, ix–xiv. [Google Scholar] [CrossRef] [PubMed]
- Nafie, M.S.; Arafa, K.; Sedky, N.K.; Alakhdar, A.A.; Arafa, R.K. Triaryl dicationic DNA minor-groove binders with antioxidant activity display cytotoxicity and induce apoptosis in breast cancer. Chem. -Biol. Interact. 2020, 324, 109087. [Google Scholar] [CrossRef] [PubMed]
- Nafie, M.S.; Mahgoub, S.; Amer, A.M. Antimicrobial and antiproliferative activities of novel synthesized 6-(quinolin-2-ylthio) pyridine derivatives with molecular docking study as multi-targeted JAK2/STAT3 inhibitors. Chem. Biol. Drug. Des. 2020, 97, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Finney, D. Statistical Method in Biological Assay, 3rd ed.; Charles Griffin &Company Ltd.: Glasgow, Scotland, 1978. [Google Scholar]
- Gad, E.M.; Nafie, M.S.; Eltamany, E.H.; Hammad, M.S.A.G.; Barakat, A.; Boraei, A.T.A. Discovery of New Apoptosis-Inducing Agents for Breast Cancer Based on Ethyl 2-Amino-4,5,6,7-Tetra Hydrobenzo[b]Thiophene-3-Carboxylate: Synthesis, In Vitro, and In Vivo Activity Evaluation. Molecules 2020, 25, 2523. [Google Scholar] [CrossRef] [PubMed]
- Youssef, E.; El-Moneim, M.A.; Fathalla, W.; Nafie, M.S. Design, synthesis and antiproliferative activity of new amine, amino acid and dipeptide-coupled benzamides as potential sigma-1 receptor. J. Iran. Chem. Soc. 2020. [Google Scholar] [CrossRef]

| Compounds | IC50 *,# ± SE (µM) | |
|---|---|---|
| HepG2 Liver Cancer Cells | THLE-2 Normal Liver Cells | |
| 1 | 27.82 ± 0.94 | - |
| 2 | 0.18 ± 0.03 | 16.87 ± 1.11 |
| 3 | 8.93 ± 0.75 | - |
| 4 | 0.017 ± 0.004 | 56.55 ± 1.5 |
| 5 | 1.94 ± 0.09 | - |
| 6 | 0.61 ± 0.08 | 35.14 ± 1.33 |
| 7 | 0.41 ± 0.009 | 15.36 ± 0.74 |
| 8 | 0.79 ± 0.04 | 14.10 ± 0.58 |
| 9 | NA | - |
| 10 | 64.78 ± 1.63 | - |
| 11 | 1.14 ± 0.05 | - |
| 12 | 1.13 ± 0.066 | - |
| # Staurosporine | 5.07 ± 0.22 | 17.6 ± 0.94 |
| 5-FU | 5.18 ± 0.53 | 42.98 ± 1.29 |
| Parameters | Treatments | p-Value | ||||
|---|---|---|---|---|---|---|
| Normal Control | Normal + Compound 4 (6 mg/Kg BW) | SEC Control | SEC + Compound 4 (6 mg/Kg BW) | SEC + 5-FU | ||
| Hemoglobin (g/dL) | 13.3 ± 0.7 | 12.6 ± 0.5 | 11.8 ± 0.8 | 13.3 ± 0.7 | 10.6 ± 1.1 | 0.18 |
| RBC’s count (×106/µL) | 8.8 ± 0.3 | 8.7 ± 0.4 | 7.52 ± 0.5 | 9.3 ± 0.4 | 7.5 ± 0.8 | 0.12 |
| WBC’s count (×103/µL) | 9.4 ± 1.2 | 9.42 ± 1.3 | 16.5 ± 3.4 | 9.5 ± 1.9 | 13.1 ± 4.1 | 0.009 * |
| Parameters | Treatments | p-Value | ||||
|---|---|---|---|---|---|---|
| Normal Control | Normal + Compound 4 (6 mg/Kg BW) | SEC Control | SEC + Compound 4 (6 mg/Kg BW) | SEC + 5-FU | ||
| Urea (mg/dL) | 27.8 ± 2.6 | 28.13 ± 2.7 | 25.2 ± 2.3 | 27 ± 1.5 | 26.1 ± 2.7 | 0.38 |
| Creatinine (mg/dL) | 1.6 ± 0.2 | 1.1 ± 0.2 | 0.7 ± 01 | 1.0 ± 0.1 | 0.8 ± 0.1 | 0.16 |
| ALT (U/L) | 35.3 ± 3.8 | 43.25 ± 7.4 | 50 ± 2.7 | 37.4 ± 10.4 | 39.1 ± 3.6 | 0.22 |
| AST (U/L) | 37.4 ± 2.8 | 44.9 ± 10.8 | 48.9 ± 5.5 | 37.8 ± 8.4 | 38 ± 4.6 | 0.42 |
| Total Protein (g/dL) | 6.9 ± 0.4 | 6.9 ± 1.5 | 6.6 ± 0.4 | 7.4 ± 0.2 | 7.2 ± 0.4 | 0.39 |
| Albumin (g/dL) | 4.4 ± 0.4 | 4.4 ± 0.8 | 4.01 ± 0.4 | 3.43 ± 0.1 | 4.1 ± 0.3 | 0.35 |
| Treatments | Oxidative Stress | Antioxidants | |||
|---|---|---|---|---|---|
| MDA (nmol/g Tissue) | NO (U/g Tissue) | GSH (mg/g Tissue) | CAT (U/g Tissue) | SOD (U/g Tissue) | |
| Normal control | 61.38 ± 2.07 | 36.58 ± 1. 7 | 47.23 ± 2.08 | 53.35 ± 2.01 | 46.39 ± 2.08 |
| SEC control | 98.39 * ± 2.04 | 79.69 * ± 2.58 | 18.23 * ± 1.09 | 21.69 * ± 0.87 | 27.36 * ± 1.27 |
| SEC+ Compound 4 (6 mg/kg BW) | 73.36 # ± 2.15 | 42.38 # ± 1.08 | 39.27 # ± 1.38 | 46.9 # ± 1.87 | 48.69 # ± 0.95 |
| Compound | PI3k (1E8Z) * | AKT (3QKK) * | ||||
|---|---|---|---|---|---|---|
| Binding Energy | HB Interaction | Other Interactions | Binding Energy | HB Interaction | Other Interactions | |
| 4 | −18.58 Kcal/mol | 1 Hydrogen bond with Val 882 | Arene–arene interactions with Tyr 867 and arene-cation with Lys 890 | −10.97 Kcal/mol | 1 Hydrogen bond with Asp 292 | - |
| # | Molinspiration 2018.10 | MolSoft | Swiss ADME | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MWt (D) | MV (A3) | PSA (A2) | Log P | Nrotb | Nviolations | HBA | HBD | Solubility (mg/L) | Drug Likeness (Lipinski Pfizer Filter) | |
| 1 | 310.38 | 269.60 | 47.03 | 2.48 | 3 | 0 | 3 | 1 | 52.40 | “Yes, drug-like” MW ≤ 500, Log P ≤ 4.15, HBA ≤ 10 and HDD ≤ 5 |
| 2 | 319.39 | 273.04 | 53.59 | 2.88 | 2 | 0 | 2 | 2 | 38.07 | |
| 3 | 261.35 | 235.12 | 41.03 | 1.25 | 2 | 0 | 2 | 1 | 303.25 | |
| 4 | 302.38 | 242.79 | 58.02 | 1.84 | 2 | 0 | 4 | 2 | 450.13 | |
| 5 | 375.45 | 325.26 | 57.88 | 0.98 | 4 | 0 | 6 | 0 | 2413.05 | |
| 6 | 258.35 | 233.74 | 37.08 | 2.24 | 3 | 0 | 2 | 1 | 68.95 | |
| 7 | 286.38 | 234.77 | 37.80 | 2.32 | 2 | 0 | 3 | 1 | 138.71 | |
| 10 | 257.36 | 235.54 | 44.81 | 0.69 | 3 | 0 | 4 | 1 | 3509.58 | |
| 11 | 352.55 | 345.78 | 38.81 | 2.76 | 5 | 0 | 4 | 1 | 165.26 | |
| 12 | 369.53 | 351.00 | 54.04 | 2.50 | 6 | 0 | 5 | 1 | 355.76 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nafie, M.S.; Khodair, A.I.; Hassan, H.A.Y.; El-Fadeal, N.M.A.; Bogari, H.A.; Elhady, S.S.; Ahmed, S.A. Evaluation of 2-Thioxoimadazolidin-4-one Derivatives as Potent Anti-Cancer Agents through Apoptosis Induction and Antioxidant Activation: In Vitro and In Vivo Approaches. Molecules 2022, 27, 83. https://doi.org/10.3390/molecules27010083
Nafie MS, Khodair AI, Hassan HAY, El-Fadeal NMA, Bogari HA, Elhady SS, Ahmed SA. Evaluation of 2-Thioxoimadazolidin-4-one Derivatives as Potent Anti-Cancer Agents through Apoptosis Induction and Antioxidant Activation: In Vitro and In Vivo Approaches. Molecules. 2022; 27(1):83. https://doi.org/10.3390/molecules27010083
Chicago/Turabian StyleNafie, Mohamed S., Ahmed I. Khodair, Hebat Allah Y. Hassan, Noha M. Abd El-Fadeal, Hanin A. Bogari, Sameh S. Elhady, and Safwat A. Ahmed. 2022. "Evaluation of 2-Thioxoimadazolidin-4-one Derivatives as Potent Anti-Cancer Agents through Apoptosis Induction and Antioxidant Activation: In Vitro and In Vivo Approaches" Molecules 27, no. 1: 83. https://doi.org/10.3390/molecules27010083
APA StyleNafie, M. S., Khodair, A. I., Hassan, H. A. Y., El-Fadeal, N. M. A., Bogari, H. A., Elhady, S. S., & Ahmed, S. A. (2022). Evaluation of 2-Thioxoimadazolidin-4-one Derivatives as Potent Anti-Cancer Agents through Apoptosis Induction and Antioxidant Activation: In Vitro and In Vivo Approaches. Molecules, 27(1), 83. https://doi.org/10.3390/molecules27010083









