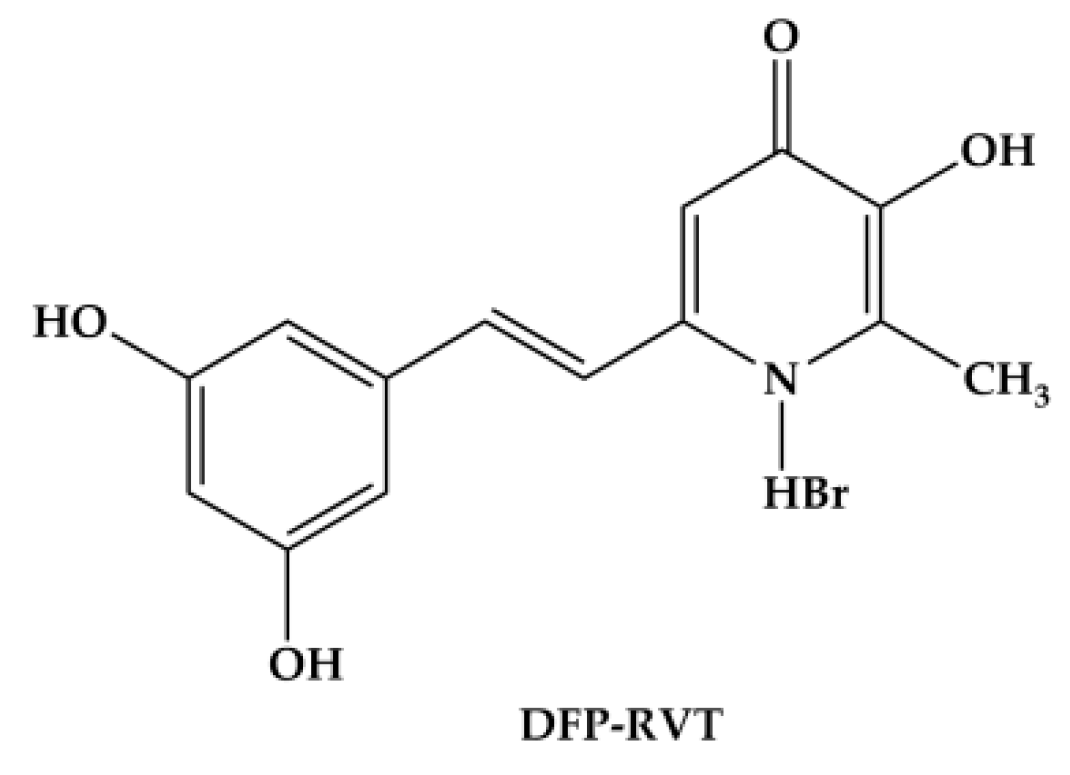
Identifying a Deferiprone–Resveratrol Hybrid as an Effective Lipophilic Anti-Plasmodial Agent
Abstract
1. Introduction
2. Results
2.1. Partition Coefficient
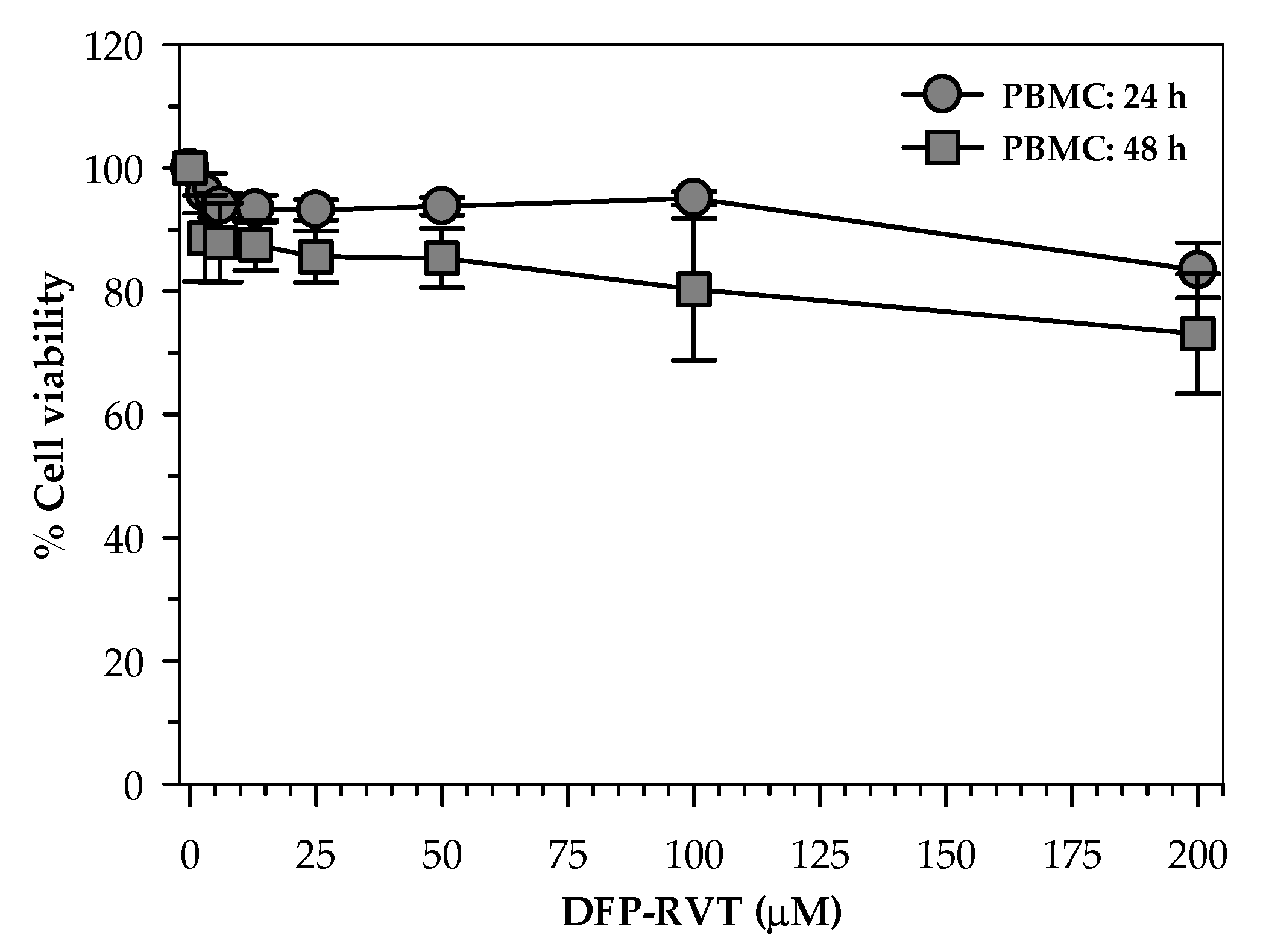
2.2. Toxicity of DFP-RVT in PBMCs
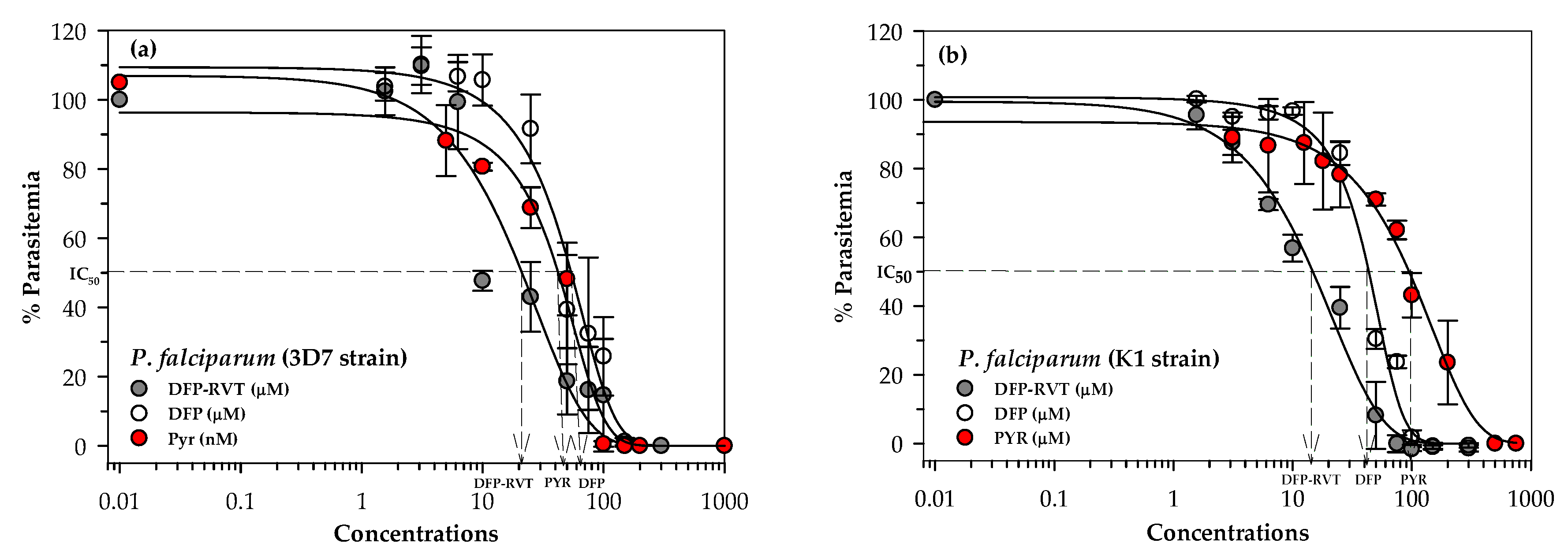
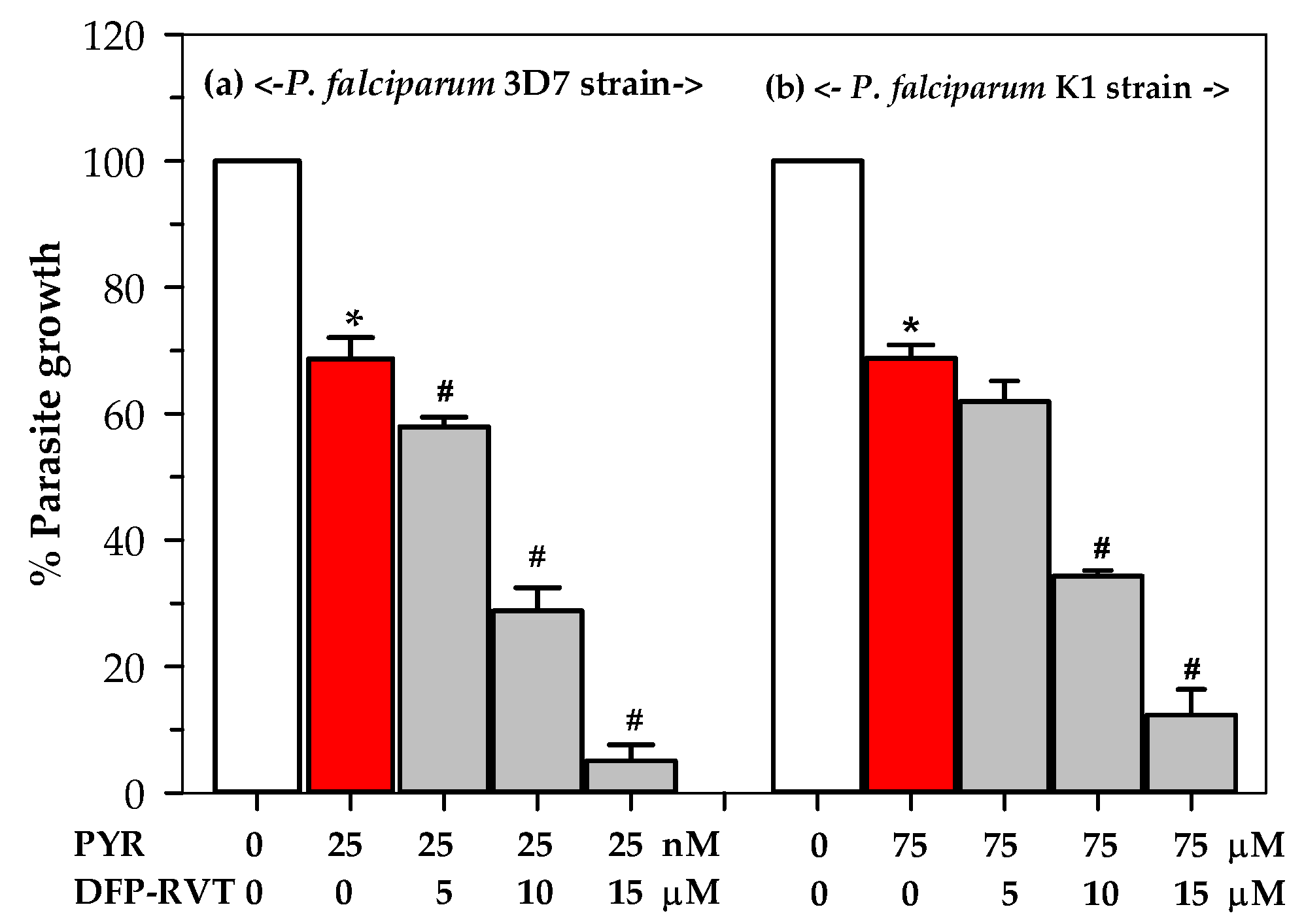
2.3. Inhibitory Effect of DFP-RVT on P. falciparum Growth
2.4. Effect of DFP-RVT Treatment on LIP Levels in PRBCs
3. Discussion
4. Materials and Methods
4.1. Chemicals and Reagents
4.2. Methods
4.2.1. Synthesis of DFP-RVT
4.2.2. Determination of Partition Coefficient
4.2.3. Human Ethics
4.2.4. Toxicity Study in Peripheral Blood Mononuclear Cells
4.2.5. P. falciparum Culture
4.2.6. Sorbitol Synchronization of P. falciparum-Infected RBCs
4.2.7. Drug Sensitivity Test for P. falciparum
4.2.8. Measurement of LIP in P. falciparum-Infected RBC
4.2.9. Statistical Analysis
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Dogovski, C.; Xie, S.C.; Burgio, G.; Bridgford, J.; Mok, S.; McCaw, J.M.; Chotivanich, K.; Kenny, S.; Gnadig, N.; Straimer, J.; et al. Targeting the cell stress response of Plasmodium falciparum to overcome artemisinin resistance. PLoS Biol. 2015, 13, e1002132. [Google Scholar] [CrossRef]
- Mace, K.E.; Lucchi, N.W.; Tan, K.R. Malaria Surveillance—United States, 2017. MMWR Surveill. Summ. 2021, 70, 1–35. [Google Scholar] [CrossRef]
- Ashley, E.A.; Poespoprodjo, J.R. Treatment and prevention of malaria in children. Lancet Child Adolesc. Health 2020, 4, 775–789. [Google Scholar] [CrossRef]
- Gordeuk, V.R.; Loyevsky, M. Antimalarial effect of iron chelators. Adv. Exp. Med. Biol. 2002, 509, 251–272. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.J.; Meremikwu, M. Iron chelating agents for treating malaria. Cochrane Database Syst. Rev. 2003, 2003, CD001474. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, P.M.; Posner, G.H. A medicinal chemistry perspective on artemisinin and related endoperoxides. J. Med. Chem. 2004, 47, 2945–2964. [Google Scholar] [CrossRef]
- Ferrer, P.; Vega-Rodriguez, J.; Tripathi, A.K.; Jacobs-Lorena, M.; Sullivan, D.J., Jr. Antimalarial iron chelator FBS0701 blocks transmission by Plasmodium falciparum gametocyte activation inhibition. Antimicrob. Agents Chemother. 2015, 59, 1418–1426. [Google Scholar] [CrossRef]
- Thuma, P.E.; Olivieri, N.F.; Mabeza, G.F.; Biemba, G.; Parry, D.; Zulu, S.; Fassos, F.F.; McClelland, R.A.; Koren, G.; Brittenham, G.M.; et al. Assessment of the effect of the oral iron chelator deferiprone on asymptomatic Plasmodium falciparum parasitemia in humans. Am. J. Trop. Med. Hyg. 1998, 58, 358–364. [Google Scholar] [CrossRef]
- Iheanacho, E.N.; Samuni, A.; Avramovici-Grisaru, S.; Sarel, S.; Spira, D.T. Inhibition of Plasmodium falciparum growth by a synthetic iron chelator. Trans. R. Soc. Trop. Med. Hyg. 1990, 84, 213–216. [Google Scholar] [CrossRef]
- Ferrer, P.; Tripathi, A.K.; Clark, M.A.; Hand, C.C.; Rienhoff, H.Y., Jr.; Sullivan, D.J., Jr. Antimalarial iron chelator, FBS0701, shows asexual and gametocyte Plasmodium falciparum activity and single oral dose cure in a murine malaria model. PLoS ONE 2012, 7, e37171. [Google Scholar] [CrossRef]
- Thipubon, P.; Uthaipibull, C.; Kamchonwongpaisan, S.; Tipsuwan, W.; Srichairatanakool, S. Inhibitory effect of novel iron chelator, 1-(N-acetyl-6-aminohexyl)-3-hydroxy-2-methylpyridin-4-one (CM1) and green tea extract on growth of Plasmodium falciparum. Malar. J. 2015, 14, 382. [Google Scholar] [CrossRef]
- Fritsch, G.; Treumer, J.; Spira, D.T.; Jung, A. Plasmodium vinckei: Suppression of mouse infections with desferrioxamine B. Exp. Parasitol. 1985, 60, 171–174. [Google Scholar] [CrossRef]
- Scheibel, L.W.; Stanton, G.G. Antimalarial activity of selected aromatic chelators. IV. Cation uptake by Plasmodium falciparum in the presence of oxines and siderochromes. Mol. Pharmacol. 1986, 30, 364–369. [Google Scholar]
- Heppner, D.G.; Hallaway, P.E.; Kontoghiorghes, G.J.; Eaton, J.W. Antimalarial properties of orally active iron chelators. Blood 1988, 72, 358–361. [Google Scholar] [CrossRef]
- Hershko, C.; Theanacho, E.N.; Spira, D.T.; Peter, H.H.; Dobbin, P.; Hider, R.C. The effect of N-alkyl modification on the antimalarial activity of 3-hydroxypyridin-4-one oral iron chelators. Blood 1991, 77, 637–643. [Google Scholar] [CrossRef]
- Shanzer, A.; Libman, J.; Lytton, S.D.; Glickstein, H.; Cabantchik, Z.I. Reversed siderophores act as antimalarial agents. Proc. Natl. Acad. Sci. USA. 1991, 88, 6585–6589. [Google Scholar] [CrossRef] [PubMed]
- Lytton, S.D.; Cabantchik, Z.I.; Libman, J.; Shanzer, A. Reversed siderophores as antimalarial agents. II. Selective scavenging of Fe (III) from parasitized erythrocytes by a fluorescent derivative of desferal. Mol. Pharmacol. 1991, 40, 584–590. [Google Scholar] [PubMed]
- Yang, Y.Z.; Ranz, A.; Pan, H.Z.; Zhang, Z.N.; Lin, X.B.; Meshnick, S.R. Daphnetin: A novel antimalarial agent with in vitro and in vivo activity. Am. J. Trop. Med. Hyg. 1992, 46, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Yinnon, A.M.; Theanacho, E.N.; Grady, R.W.; Spira, D.T.; Hershko, C. Antimalarial effect of HBED and other phenolic and catecholic iron chelators. Blood 1989, 74, 2166–2171. [Google Scholar] [CrossRef]
- Sonnet, P.; Mullie, C. In vitro antimalarial activity of ICL670: A further proof of the correlation between inhibition of beta-hematin formation and of peroxidative degradation of hemin. Exp. Parasitol. 2011, 128, 26–31. [Google Scholar] [CrossRef]
- Mohanty, D.; Ghosh, K.; Pathare, A.V.; Karnad, D. Deferiprone (L1) as an adjuvant therapy for Plasmodium falciparum malaria. Indian J. Med. Res. 2002, 115, 17–21. [Google Scholar]
- Hershko, C.; Gordeuk, V.R.; Thuma, P.E.; Theanacho, E.N.; Spira, D.T.; Hider, R.C.; Peto, T.E.; Brittenham, G.M. The antimalarial effect of iron chelators: Studies in animal models and in humans with mild falciparum malaria. J. Inorg. Biochem. 1992, 47, 267–277. [Google Scholar] [CrossRef]
- Bulbake, U.; Singh, A.; Domb, A.J.; Khan, W. Therapeutic macromolecular iron chelators. Curr. Med. Chem. 2018, 26, 323–334. [Google Scholar] [CrossRef]
- Ellis, G.L.; Amewu, R.; Sabbani, S.; Stocks, P.A.; Shone, A.; Stanford, D.; Gibbons, P.; Davies, J.; Vivas, L.; Charnaud, S.; et al. Two-step synthesis of achiral dispiro-1,2,4,5-tetraoxanes with outstanding antimalarial activity, low toxicity, and high-stability profiles. J. Med. Chem. 2008, 51, 2170–2177. [Google Scholar] [CrossRef]
- Gehrke, S.S.; Pinto, E.G.; Steverding, D.; Pleban, K.; Tempone, A.G.; Hider, R.C.; Wagner, G.K. Conjugation to 4-aminoquinoline improves the anti-trypanosomal activity of Deferiprone-type iron chelators. Bioorg. Med. Chem. 2012, 21, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Zhang, M.; Sheng, R.; Ma, Y. Synthesis and biological evaluation of deferiprone-resveratrol hybrids as antioxidants, Abeta1-42 aggregation inhibitors and metal-chelating agents for Alzheimer’s disease. Eur. J. Med. Chem. 2017, 127, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Gaboriau, F.; Chantrel-Groussard, K.; Rakba, N.; Loyer, P.; Pasdeloup, N.; Hider, R.C.; Brissot, P.; Lescoat, G. Iron mobilization, cytoprotection, and inhibition of cell proliferation in normal and transformed rat hepatocyte cultures by the hydroxypyridinone CP411, compared to CP20: A biological and physicochemical study. Biochem. Pharmacol. 2004, 67, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.Y.; Lu, Z.; Kong, X.L.; Zhou, T.; Bansal, S.; Hider, R. Systematic comparison of the mono-, dimethyl- and trimethyl 3-hydroxy-4(1H)-pyridones - Attempted optimization of the orally active iron chelator, deferiprone. Eur. J. Med. Chem. 2016, 115, 132–140. [Google Scholar] [CrossRef]
- Chen, W.; Yuan, X.; Li, Z.; Lu, Z.; Kong, S.; Jiang, H.; Du, H.; Pan, X.; Nandi, M.; Kong, X.; et al. CN128: A new orally active hydroxypyridinone iron chelator. J. Med. Chem. 2020, 63, 4215–4226. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Mishra, A.P.; Nigam, M.; Sener, B.; Kilic, M.; Sharifi-Rad, M.; Fokou, P.V.; Martins, N.; Sharifi-Rad, J. Resveratrol: A double-edged sword in health benefits. Biomedicines 2018, 6, 91. [Google Scholar] [CrossRef]
- Cabantchik, Z.I.; Glickstein, H.; Golenser, J.; Loyevsky, M.; Tsafack, A. Iron chelators: Mode of action as antimalarials. Acta Haematol. 1996, 95, 70–77. [Google Scholar] [CrossRef]
- Lytton, S.D.; Mester, B.; Dayan, I.; Glickstein, H.; Libman, J.; Shanzer, A.; Cabantchik, Z.I. Mode of action of iron (III) chelators as antimalarials: I. Membrane permeation properties and cytotoxic activity. Blood 1993, 81, 214–221. [Google Scholar] [CrossRef]
- Bendova, P.; Mackova, E.; Haskova, P.; Vavrova, A.; Jirkovsky, E.; Sterba, M.; Popelova, O.; Kalinowski, D.S.; Kovarikova, P.; Vavrova, K.; et al. Comparison of clinically used and experimental iron chelators for protection against oxidative stress-induced cellular injury. Chem. Res. Toxicol. 2010, 23, 1105–1114. [Google Scholar] [CrossRef]
- Scholl, P.F.; Tripathi, A.K.; Sullivan, D.J. Bioavailable iron and heme metabolism in Plasmodium falciparum. Curr. Top. Microbiol. Immunol. 2005, 295, 293–324. [Google Scholar] [CrossRef] [PubMed]
- Pattanapanyasat, K.; Thaithong, S.; Kyle, D.E.; Udomsangpetch, R.; Yongvanitchit, K.; Hider, R.C.; Webster, H.K. Flow cytometric assessment of hydroxypyridinone iron chelators on in vitro growth of drug-resistant malaria. Cytometry 1997, 27, 84–91. [Google Scholar] [CrossRef]
- Raventos-Suarez, C.; Pollack, S.; Nagel, R.L. Plasmodium falciparum: Inhibition of in vitro growth by desferrioxamine. Am. J. Trop. Med. Hyg. 1982, 31, 919–922. [Google Scholar] [CrossRef]
- Yasumoto, E.; Nakano, K.; Nakayachi, T.; Morshed, S.R.; Hashimoto, K.; Kikuchi, H.; Nishikawa, H.; Kawase, M.; Sakagami, H. Cytotoxic activity of deferiprone, maltol and related hydroxyketones against human tumor cell lines. Anticancer Res. 2004, 24, 755–762. [Google Scholar]
- van Zyl, R.L.; Havlik, I.; Monteagudo, F.S. The combined effect of iron chelators and classical antimalarials on the in-vitro growth of Plasmodium falciparum. J. Antimicrob. Chemother. 1992, 30, 273–278. [Google Scholar] [CrossRef]
- van Hensbroek, M.B.; Morris-Jones, S.; Meisner, S.; Jaffar, S.; Bayo, L.; Dackour, R.; Phillips, C.; Greenwood, B.M. Iron, but not folic acid, combined with effective antimalarial therapy promotes haematological recovery in African children after acute falciparum malaria. Trans. R. Soc. Trop. Med. Hyg. 1995, 89, 672–676. [Google Scholar] [CrossRef]
- Nwanyanwu, O.C.; Ziba, C.; Kazembe, P.N.; Gamadzi, G.; Gandwe, J.; Redd, S.C. The effect of oral iron therapy during treatment for Plasmodium falciparum malaria with sulphadoxine-pyrimethamine on Malawian children under 5 years of age. Ann. Trop. Med. Parasitol. 1996, 90, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Pangjit, K.; Banjerdpongchai, R.; Phisalaphong, C.; Fucharoen, S.; Xie, Y.Y.; Lu, Z.D.; Hider, R.C.; Srichairatanakool, S. Characterisation of a novel oral iron chelator: 1-(N-Acetyl-6-aminohexyl)-3-hydroxy-2-methylpyridin-4-one. J. Pharm. Pharmacol. 2015, 67, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Chansiw, N.; Kulprachakarn, K.; Paradee, N.; Prommaban, A.; Srichairatanakool, S. Protection of iron-induced oxidative damage in neuroblastoma (SH-SY5Y) cells by combination of 1-(N-acetyl-6-aminohexyl)-3-hydroxy-2-methylpyridin-4-one and green tea extract. Bioinorg. Chem. Appl. 2021, 2021, 5539666. [Google Scholar] [CrossRef]
- Lafferty, W.E.; Kempf, R.A.; Goodwin, J.S. Suppression of lymphocyte proliferation by human tumor cells grown in short term cultures. J. Clin. Lab. Immunol. 1981, 6, 157–163. [Google Scholar]
- Radfar, A.; Mendez, D.; Moneriz, C.; Linares, M.; Marin-Garcia, P.; Puyet, A.; Diez, A.; Bautista, J.M. Synchronous culture of Plasmodium falciparum at high parasitemia levels. Nat. Protoc. 2009, 4, 1899–1915. [Google Scholar] [CrossRef]
- Smilkstein, M.; Sriwilaijaroen, N.; Kelly, J.X.; Wilairat, P.; Riscoe, M. Simple and inexpensive fluorescence-based technique for high-throughput antimalarial drug screening. Antimicrob. Agents Chemother. 2004, 48, 1803–1806. [Google Scholar] [CrossRef]
- Co, E.M.; Dennull, R.A.; Reinbold, D.D.; Waters, N.C.; Johnson, J.D. Assessment of malaria in vitro drug combination screening and mixed-strain infections using the malaria Sybr green I-based fluorescence assay. Antimicrob. Agents Chemother. 2009, 53, 2557–2563. [Google Scholar] [CrossRef][Green Version]
- Johnson, J.D.; Dennull, R.A.; Gerena, L.; Lopez-Sanchez, M.; Roncal, N.E.; Waters, N.C. Assessment and continued validation of the malaria SYBR green I-based fluorescence assay for use in malaria drug screening. Antimicrob. Agents Chemother. 2007, 51, 1926–1933. [Google Scholar] [CrossRef]
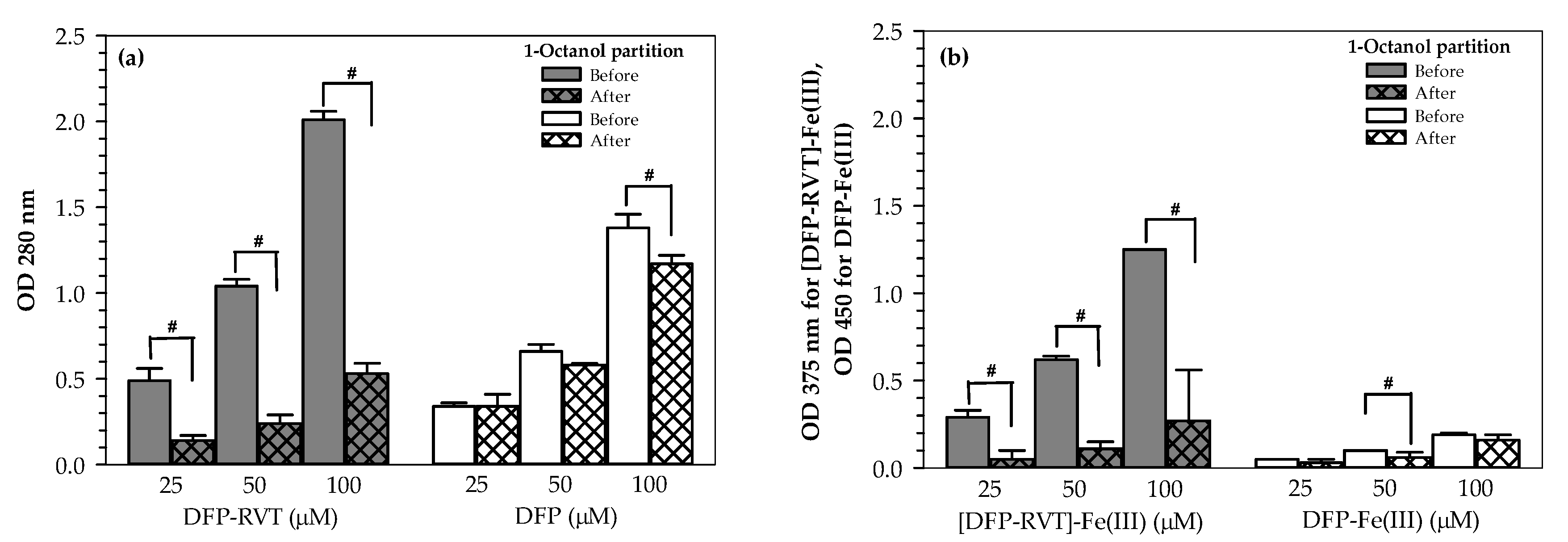

| Compounds | Po/w Values |
|---|---|
| DFP | 0.18 ± 0.06 |
| DFP-iron complex | 0.21 ± 0.11 |
| DFP-RVT | 2.73 ± 0.53 * |
| [DFP-RVT]-iron complex | 4.04 ± 0.01 *,f |
| Compound | Absolute IC50 Value (µM) | |
|---|---|---|
| P. falciparum (3D7 Strain) | P. falciparum (K1 Strain) | |
| DFP-RVT | 16.82 | 13.98 |
| DFP | 47.67 | 42.02 |
| PYR | 0.05 | 105.61 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maneekesorn, S.; Chuljerm, H.; Koonyosying, P.; Uthaipibull, C.; Ma, Y.; Srichairatanakool, S. Identifying a Deferiprone–Resveratrol Hybrid as an Effective Lipophilic Anti-Plasmodial Agent. Molecules 2021, 26, 4074. https://doi.org/10.3390/molecules26134074
Maneekesorn S, Chuljerm H, Koonyosying P, Uthaipibull C, Ma Y, Srichairatanakool S. Identifying a Deferiprone–Resveratrol Hybrid as an Effective Lipophilic Anti-Plasmodial Agent. Molecules. 2021; 26(13):4074. https://doi.org/10.3390/molecules26134074
Chicago/Turabian StyleManeekesorn, Supawadee, Hataichanok Chuljerm, Pimpisid Koonyosying, Chairat Uthaipibull, Yongmin Ma, and Somdet Srichairatanakool. 2021. "Identifying a Deferiprone–Resveratrol Hybrid as an Effective Lipophilic Anti-Plasmodial Agent" Molecules 26, no. 13: 4074. https://doi.org/10.3390/molecules26134074
APA StyleManeekesorn, S., Chuljerm, H., Koonyosying, P., Uthaipibull, C., Ma, Y., & Srichairatanakool, S. (2021). Identifying a Deferiprone–Resveratrol Hybrid as an Effective Lipophilic Anti-Plasmodial Agent. Molecules, 26(13), 4074. https://doi.org/10.3390/molecules26134074






