Propolis Extract and Its Bioactive Compounds—From Traditional to Modern Extraction Technologies
Abstract
1. Introduction
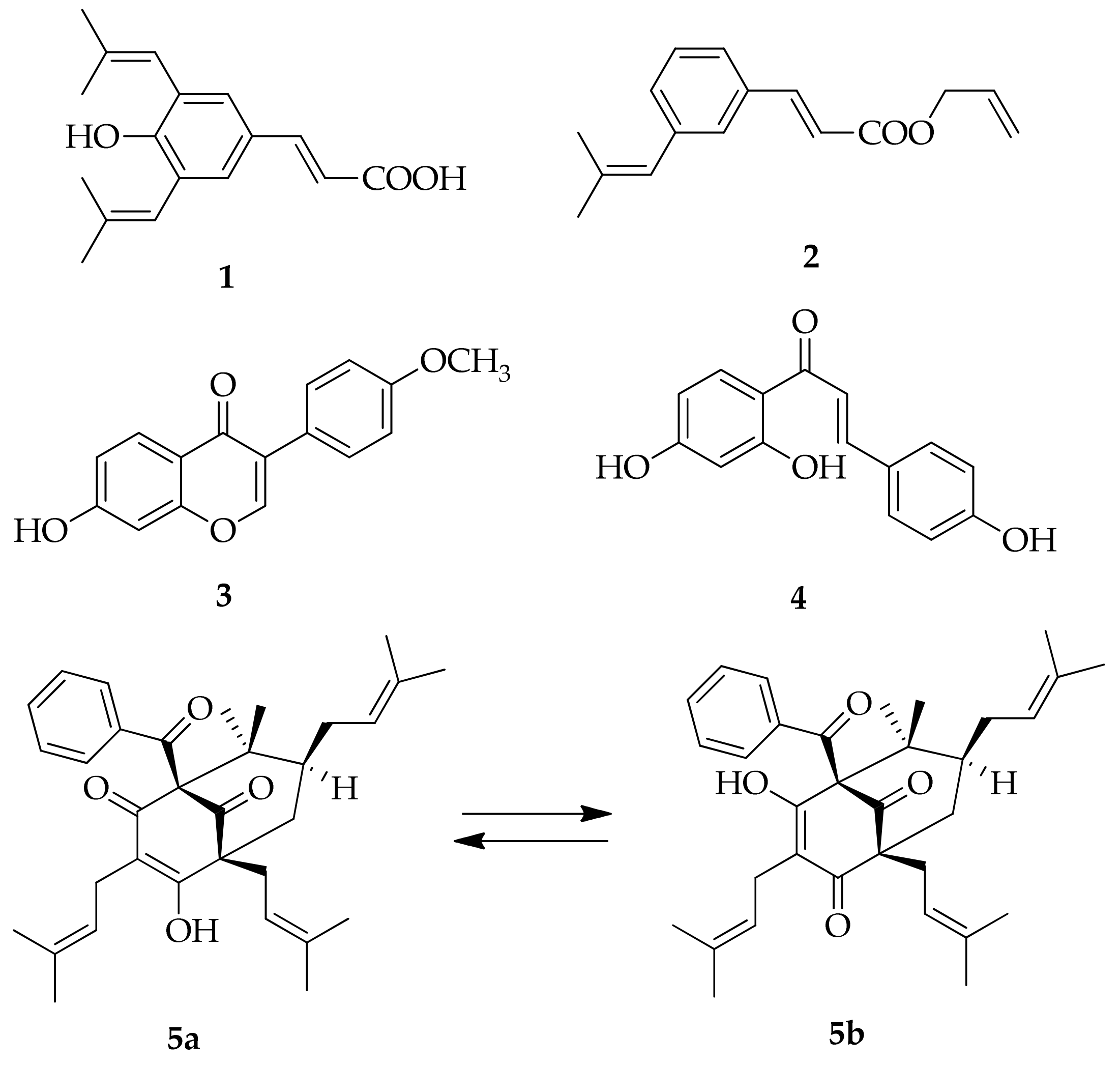
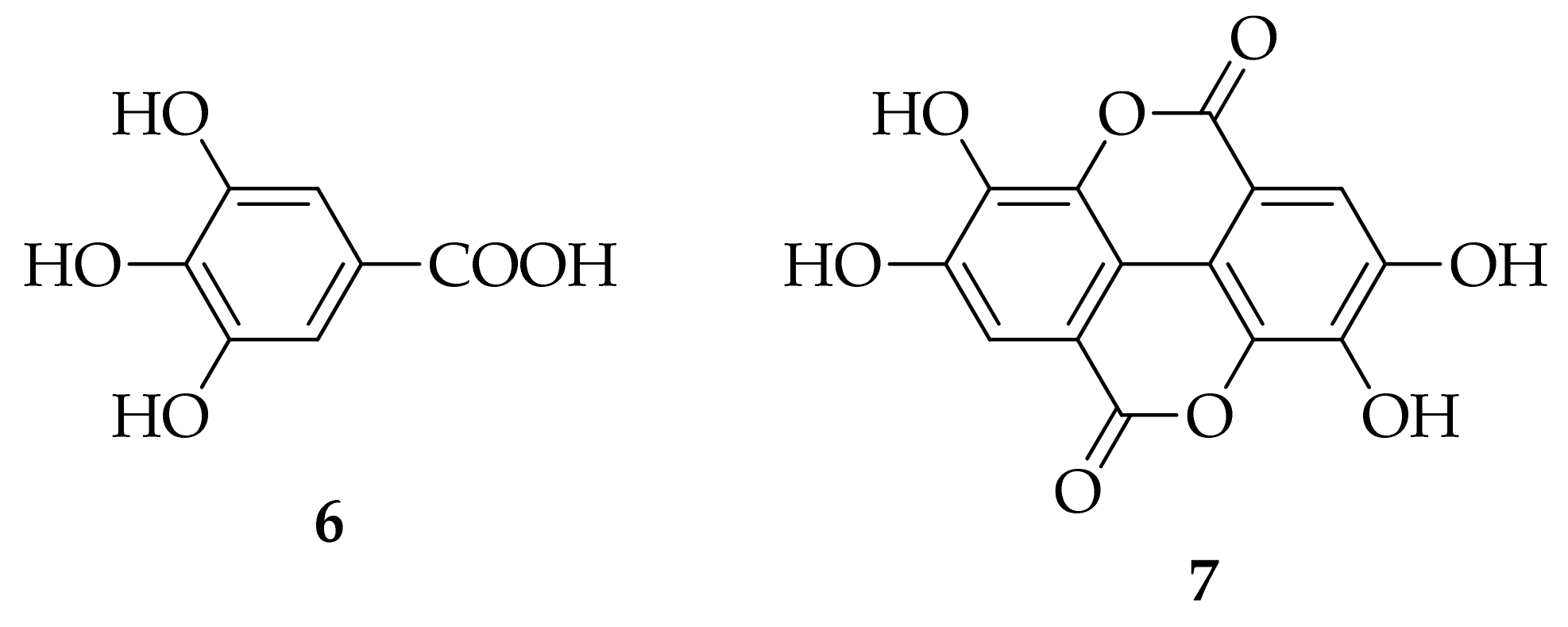
2. Propolis Types, Key Molecules, and Their Biological Activities
2.1. Molecular Mechanisms of Representative Propolis Markers Action
2.2. Chrysin
2.3. Galangin
2.4. Pinocembrin
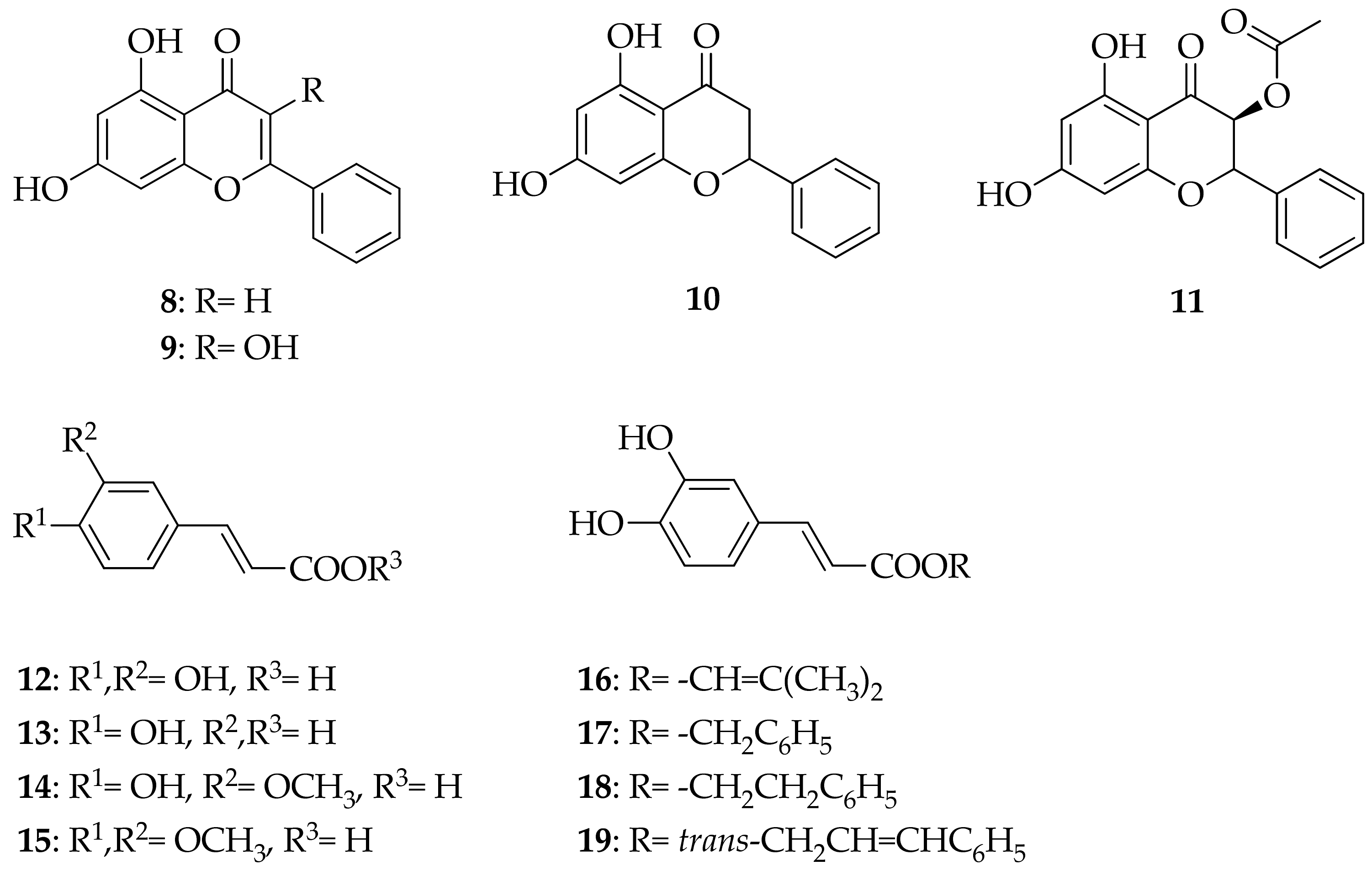
2.5. Nonflavonoids: Phenolic Acids
2.6. Molecular Mechanisms of Propolis Extracts Action
3. Technologies for Propolis Extraction and Types of Propolis Extracts
- (i)
- The presence of a relatively aggressive solvent (EtOH);
- (ii)
- Alcohol-based products are not suitable for children, pregnant and breastfeeding women, and certain patients;
- (iii)
- And relatively high content of beeswax, which causes its separation upon the phase of mixing with water phase, during the manufacturing of pharmaceutical and other products, where such an extract is employed as an API.
- (i)
- The choline chloride (CC):1,2-PG in a molar ratio (n:n) 1:1 or 1:2;
- (ii)
- CC:lactic acid (LA):H2O in 1:2:2 or 1:1:1, n:n:n;
Preparation of Solid Propolis Extracts
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ahangari, Z.; Naseri, M.; Vatandoost, F. Propolis: Chemical Composition and Its Applications in Endodontics. Iran. Endod. J. 2018, 13, 285–292. [Google Scholar] [PubMed]
- Przybyłek, I.; Karpiński, T.M. Antibacterial Properties of Propolis. Molecules 2019, 24, 2047. [Google Scholar] [CrossRef] [PubMed]
- Bankova, V. Chemical diversity of propolis and the problem of standardization. J. Ethnopharmacol. 2005, 100, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Rufatto, L.C.; Luchtenberg, P.; Garcia, C.; Thomassigny, C.; Bouttier, S.; Henriques, J.A.P.; Roesch-Ely, M.; Dumas, F.; Moura, S. Brazilian red propolis: Chemical composition and antibacterial activity determined using bioguided fractionation. Microbiol. Res. 2018, 214, 74–82. [Google Scholar] [CrossRef]
- Do Nascimento, T.G.; dos Santos Arruda, R.E.; da Cruz Almeida, E.T.; dos Santos Oliveira, J.M.; Basílio-Júnior, I.D.; de Moraes Porto, I.C.C.; Sabino, A.R.; Tonholo, J.; Gray, A.; Ebel, R.E.; et al. Comprehensive multivariate correlations between climatic effect, metabolite-profile, antioxidant capacity and antibacterial activity of Brazilian red propolis metabolites during seasonal study. Sci. Rep. 2019, 9, 18293. [Google Scholar] [CrossRef]
- Bankova, V.; Popova, M.; Trusheva, B. Plant Sources of Propolis: An Update from a Chemist’s Point of View. Nat. Prod. Commun. 2006, 1, 1023–1028. [Google Scholar] [CrossRef]
- Souza, Ε.A.; Zaluski, R.; Veiga, N.; Orsi, R.O. Effects of Seasonal Variations and Collection Methods on the Mineral Composition of Propolis from Apis mellifera linnaeus Beehives. Braz. J. Biol. 2016, 76, 396–401. [Google Scholar] [CrossRef]
- Galeotti, F.; Maccari, F.; Fachini, A.; Volpi, N. Chemical Composition and Antioxidant Activity of Propolis Prepared in Different Forms and in Different Solvent Useful for Finished Products. Foods 2018, 7, 41. [Google Scholar] [CrossRef]
- Huang, S.; Zhang, C.-P.; Wang, K.; Li, G.Q.; Hu, F.-L. Recent Advances in the Chemical Composition of Propolis. Molecules 2014, 19, 19610–19632. [Google Scholar] [CrossRef]
- Banskota, A.H.; Tezuka, Y.; Kadota, S. Recent progress in pharmacological research of propolis. Phytother. Res. 2001, 15, 561–571. [Google Scholar] [CrossRef]
- Daleprane, J.B.; Abdalla, D.S. Emerging roles of propolis: Antioxidant, cardioprotective, and antiangiogenic actions. Evid. Based Complement. Altern. Med. 2013, 2013, 1–8. [Google Scholar] [CrossRef]
- Ghisalberti, E.L. Propolis: A Review. Bee World 1979, 60, 59–84. [Google Scholar] [CrossRef]
- Kujumgiev, A.; Tsvetkova, I.; Serkedjieva, Y.; Bankova, V.; Christov, R.; Popov, S. Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J. Ethnopharmacol. 1999, 64, 235–240. [Google Scholar] [CrossRef]
- Sforcin, J.M.; Bankova, V. Propolis: Is there a potential for the development of new drugs? J. Ethnopharmacol. 2011, 133, 253–260. [Google Scholar] [CrossRef]
- Fernandes-Silva, C.C.; Salatino, A.; Salatino, M.L.F.; Breyer, E.D.H.; Negri, G. Chemical profiling of six samples of Brazilian propolis. Química Nova 2013, 36, 237–240. [Google Scholar] [CrossRef]
- Cuesta-Rubio, O.; Frontana-Uribe, B.A.; Ramírez-Apan, T.; Cárdenas, J. Polyisoprenylated benzophenones in Cuban propolis; biological activity of nemorosone. Z. Naturforsch. C J. Biosci. 2002, 57, 372–378. [Google Scholar] [CrossRef]
- Bankova, V.S.; Christov, R.S.; Tejera, A.D. Lignans and other constituents of propolis from the Canary Islands. Phytochemistry 1998, 49, 1411–1415. [Google Scholar] [CrossRef]
- Dos Santos, C.M.; Campos, J.F.; dos Santos, H.F.; Balestieri, J.B.P.; Silva, D.B.; de Picoli Souza, K.; Carollo, C.A.; Estevinho, L.M.; dos Santos, E.L. Chemical Composition and Pharmacological Effects of Geopropolis Produced by Melipona quadrifasciata anthidioides. Oxid. Med. Cell. Longev. 2017, 2017, 8320804. [Google Scholar] [CrossRef]
- Batista, M.C.A.; Abreu, B.V.B.; Dutra, R.P.; Cunha, M.S.; Amaral, F.M.M.; Torres, L.M.B.; Ribeiro, M.N.S. Chemical composition and antioxidant activity of geopropolis produced by Melipona fasciculata (Meliponinae) in flooded fields and cerrado areas of Maranhão State, northeastern Brazil. Acta Amaz. 2016, 46, 315–322. [Google Scholar] [CrossRef]
- Pellati, F.; Prencipe, F.P.; Bertelli, D.; Benvenuti, S. An efficient chemical analysis of phenolic acids and flavonoids in raw propolis by microwave-assisted extraction combined with high-performance liquid chromatography using the fused-core technology. J. Pharm. Biomed. Anal. 2013, 81–82, 126–132. [Google Scholar] [CrossRef]
- Daglia, M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012, 23, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Das, J.; Ramani, R.; Suraju, M.O. Polyphenol compounds and PKC signaling. Biochim. Biophys. Acta 2016, 1860, 2107–2121. [Google Scholar] [CrossRef] [PubMed]
- Ercal, N.; Gurer-Orhanm, H.; Aykin-Burns, N. Toxic metals and oxidative stress part I: Mechanisms involved in metal-induced oxidative damage. Curr. Top. Med. Chem. 2001, 1, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Kasprzak, M.M.; Erxleben, A.; Ochocki, J. Properties and applications of flavonoid metal complexes. RSC Adv. 2015, 5, 45853–45877. [Google Scholar] [CrossRef]
- Xu, Y.; Qian, L.L.; Yang, J.; Han, R.M.; Zhang, J.P.; Skibsted, L.H. Kaempferol Binding to Zinc (II), Efficient Radical Scavenging through Increased Phenol Acidity. J. Phys. Chem. B 2018, 122, 10108–10117. [Google Scholar] [CrossRef] [PubMed]
- Tu, L.-Y.; Pi, J.; Jin, H.; Cai, J.-Y.; Deng, S.-P. Synthesis, characterization and anticancer activity of kaempferol-zinc (II) complex. Bioorg. Med. Chem. Lett. 2016, 26, 2730–2734. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.C.; Tsai, S.H.; Chen, C.S.; Chang, Y.C.; Lee, C.M.; Lai, Z.Y.; Lin, C.M. Structure-activity relationship of coumarin derivatives on xanthine oxidase-inhibiting and free radical-scavenging activities. Biochem. Pharmacol. 2008, 75, 1416–1425. [Google Scholar] [CrossRef]
- Farines, V.; Monje, M.C.; Telo, J.P.; Hnawia, E.; Sauvain, M.; Nepveu, F. Polyphenols as superoxide dismutase modulators and ligands for estrogen receptors. Anal. Chim. Acta 2004, 513, 103–111. [Google Scholar] [CrossRef][Green Version]
- Li, Y.B.; Cao, Z.X.; Zhu, H. Upregulation of endogenous antioxidants and phase 2 enzymes by the red wine polyphenol, resveratrol in cultured aortic smooth muscle cells leads to cytoprotection against oxidative and electrophilic stress. Pharmacol. Res. 2006, 53, 6–15. [Google Scholar] [CrossRef]
- Mirza-Aghazadeh-Attari, M.; Ekrami, E.M.; Aghdas, S.A.M.; Mihanfar, A.; Hallaj, S.; Yousefi, B.; Safa, A.; Majidinia, M. Targeting PI3K/Akt/mTOR signaling pathway by polyphenols: Implication for cancer therapy. Life Sci. 2020, 255, 117481. [Google Scholar] [CrossRef]
- Kim, H.H.; Bae, Y.; Kim, S.H. Galangin attenuates mast cell-mediated allergic inflammation. Food. Chem. Toxicol. 2013, 57, 209–216. [Google Scholar] [CrossRef]
- Yahfoufi, N.; Alsadi, N.; Jambi, M.; Matar, C. The Immunomodulatory and Anti-inflammatory Role of Polyphenols. Nutrients 2018, 10, 1618. [Google Scholar] [CrossRef] [PubMed]
- Mani, R.; Natesan, V. Chrysin: Sources, beneficial pharmacological activities, and molecular mechanism of action. Phytochemistry 2018, 145, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, G.; Szeto, S.S.; Chong, C.M.; Quan, Q.; Huang, C.; Cui, W.; Guo, B.; Wang, Y.; Han, Y.; et al. Examining the neuroprotective effects of protocatechuic acid and chrysin on in vitro and in vivo models of Parkinson disease. Free Radic. Biol. Med. 2015, 84, 33–343. [Google Scholar] [CrossRef][Green Version]
- Hermenean, A.; Mariasiu, T.; Navarro-Gonzalez, I.; Vegara-Meseguer, J.; Miutescu, E.; Chakraborty, S.; Perez-Sanchez, H. Hepatoprotective activity of chrysin is mediated through TNF-α in chemically-induced acute liver damage: An in vivo study and molecular modeling. Exp. Ther. Med. 2017, 13, 1671–1680. [Google Scholar] [CrossRef]
- Zheng, W.; Tao, Z.; Cai, L.; Chen, C.; Zhang, C.; Wang, Q.; Ying, X.; Hu, W.; Chen, H. Chrysin Attenuates IL-1β-Induced Expression of Inflammatory Mediators by Suppressing NF-κB in Human Osteoarthritis Chondrocytes. Inflammation 2017, 40, 1143–1154. [Google Scholar] [CrossRef]
- O’Leary, K.A.; de Pascual-Teresa, S.; Needs, P.W.; Bao, Y.P.; O’Brien, N.M.; Williamson, G. Effect of flavonoids and vitamin E on cyclooxygenase-2 (COX-2) transcription. Mutat. Res. 2004, 551, 245–254. [Google Scholar] [CrossRef]
- Fu, B.; Xue, J.; Li, Z.; Shi, X.; Jiang, B.H.; Fang, J. Chrysin inhibits expression of hypoxia-inducible factor-1a through reducing hypoxia-inducible factor inhibiting its protein synthesis-1a stability inhibiting its protein synthesis. Mol. Cancer Ther. 2007, 6, 220–226. [Google Scholar] [CrossRef]
- Samarghandian, S.; Afshari, J.T.; Davoodi, S. Chrysin reduces proliferation and induces apoptosis in the human prostate cancer cell line pc-3. Clinics 2011, 66, 1073–1079. [Google Scholar] [CrossRef]
- Yu, X.M.; Phan, T.; Patel, P.N.; Jaskula-Sztul, R.; Chen, H. Chrysin activates Notch1 signaling and suppresses tumour growth of anaplastic thyroid carcinoma in vitro and in vivo. Cancer 2013, 119, 774–781. [Google Scholar] [CrossRef]
- Yang, B.; Huang, J.; Xiang, T.; Yin, X.; Luo, X.; Huang, J.; Luo, F.; Li, H.; Li, H.; Ren, G. Chrysin inhibits metastatic potential of human triple-negative breast cancer cells by modulating matrix metalloproteinase-10, epithelial to mesenchymal transition, and PI3K/Akt signaling pathway. J. Appl. Toxicol. 2014, 34, 105–112. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, T.; Du, J.; Cui, S.; Yang, F.; Jin, Q. Anti-Enterovirus 71 Effects of Chrysin and Its Phosphate Ester. PLoS ONE 2014, 9, e89668. [Google Scholar] [CrossRef]
- Li, H.X.; Wang, Z.C.; Qian, Y.M.; Yan, X.Q.; Lu, Y.D.; Zhu, H.L. Design, synthesis, and biological evaluation of chrysin derivatives as potential FabH inhibitors. Chem. Biol. Drug Des. 2017, 89, 136–140. [Google Scholar] [CrossRef]
- Fu, Q.; Gao, Y.; Zhao, H.; Wang, Z.; Wang, J. Galangin protects human rheumatoid arthritis fibroblast like synoviocytes via suppression of the NF κB/NLRP3 pathway. Mol. Med. Rep. 2018, 18, 3619–3624. [Google Scholar] [CrossRef]
- Lu, H.; Yao, H.; Zou, R.; Chen, X.; Xu, H. Galangin Suppresses Renal Inflammation via the Inhibition of NF-κB, PI3K/AKT and NLRP3 in Uric Acid Treated NRK-52E Tubular Epithelial Cells. BioMed Res. Int. 2019, 2019, 3018357. [Google Scholar] [CrossRef]
- Chien, S.T.; Shi, M.D.; Lee, Y.C.; Te, C.C.; Shih, Y.W. Galangin, a novel dietary flavonoid, attenuates metastatic feature via PKC/ERK signaling pathway in TPA-treated liver cancer HepG2 cells. Cancer Cell Int. 2015, 15, 15. [Google Scholar] [CrossRef]
- Lei, D.; Zhang, F.; Yao, D.; Xiong, N.; Jiang, X.; Zhao, H. Galangin increases ERK1/2 phosphorylation to decrease ADAM9 expression and prevents invasion in A172 glioma cells. Mol. Med. Rep. 2018, 17, 667–673. [Google Scholar] [CrossRef]
- Cao, J.; Wang, H.; Chen, F.; Fang, J.; Xu, A.; Xi, W.; Zhang, S.; Wu, G.; Wang, Z. Galangin inhibits cell invasion by suppressing the epithelial-mesenchymal transition and inducing apoptosis in renal cell carcinoma. Mol. Med. Rep. 2016, 13, 4238–4244. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.X.; Wang, B.; Zhao, X.H. In vitro effects and the related molecular mechanism of galangin and quercetin on human gastric cancer cell line (SGC-7901). Pak. J. Pharm. Sci. 2017, 30, 1279–1287. [Google Scholar] [PubMed]
- Pepeljnjak, S.; Kosalec, I. Galangin expresses bactericidal activity against multiple-resistant bacteria: MRSA, Enterococcus spp. and Pseudomonas aeruginosa. FEMS Microbiol. Lett. 2004, 240, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Cushnie, T.P.; Lamb, A.J. Assessment of the antibacterial activity of galangin against 4-quinolone resistant strains of Staphylococcus aureus. Phytomedicine 2006, 13, 187–191. [Google Scholar] [CrossRef]
- Cushnie, T.P.T.; Lamb, A.J. Antimicrobial activity of flavonoids. Int. J. Antimicrob. Agents 2005, 26, 343–356. [Google Scholar] [CrossRef]
- Cushnie, T.P.T.; Hamilton, V.E.S.; Chapman, D.G.; Taylor, P.W.; Lamb, A.J. Aggregation of Staphylococcus aureus following treatment with the antibacterial flavonol galangin. J. Appl. Microbiol. 2007, 103, 1562–1567. [Google Scholar] [CrossRef]
- Ouyang, J.; Sun, F.; Feng, W.; Xie, Y.; Ren, L.; Chen, Y. Antimicrobial Activity of Galangin and Its Effects on Murein Hydrolases of Vancomycin-Intermediate Staphylococcus aureus (VISA) Strain Mu50. Chemotherapy 2018, 63, 20–28. [Google Scholar] [CrossRef]
- Echeverría, J.; Opazo, J.; Mendoza, L.; Urzúa, A.; Wilkens, M. Structure-Activity and Lipophilicity Relationships of Selected Antibacterial Natural Flavones and Flavanones of Chilean Flora. Molecules 2017, 22, 608. [Google Scholar] [CrossRef]
- Rasul, A.; Millimouno, F.M.; Ali Eltayb, W.; Ali, M.; Li, J.; Li, X. Pinocembrin: A novel natural compound with versatile pharmacological and biological activities. BioMed Res. Int. 2013, 2013, 1–9. [Google Scholar] [CrossRef]
- Shen, X.; Liu, Y.; Luo, X.; Yang, Z. Advances in Biosynthesis, Pharmacology, and Pharmacokinetics of Pinocembrin, a Promising Natural Small-Molecule Drug. Molecules 2019, 24, 2323. [Google Scholar] [CrossRef]
- Lan, X.; Wang, W.; Li, Q.; Wang, J. The Natural Flavonoid Pinocembrin: Molecular Targets and Potential Therapeutic Applications. Mol. Neurobiol. 2016, 53, 1794–1801. [Google Scholar] [CrossRef]
- Liu, R.; Gao, M.; Yang, Z.H.; Du, G.H. Pinocembrin protects rat brain against oxidation and apoptosis induced by ischemia-reperfusion both in vivo and in vitro. Brain Res. 2008, 1216, 104–115. [Google Scholar] [CrossRef]
- Wang, W.; Zheng, L.; Xu, L.; Tu, J.; Gu, X. Pinocembrin mitigates depressive-like behaviors induced by chronic unpredictable mild stress through ameliorating neuroinflammation and apoptosis. Mol. Med. 2020, 26, 53. [Google Scholar] [CrossRef]
- Zhou, L.T.; Wang, K.J.; Li, L.; Li, H.; Geng, M. Pinocembrin inhibits lipopolysaccharide-induced inflammatory mediators production in BV2 microglial cells through suppression of PI3K/Akt/NF-κB pathway. Eur. J. Pharmacol. 2015, 761, 211–216. [Google Scholar] [CrossRef]
- De Oliveira, M.R.; Peres, A.; Gama, C.S.; Bosco, S.M.D. Pinocembrin Provides Mitochondrial Protection by the Activation of the Erk1/2-Nrf2 Signaling Pathway in SH-SY5Y Neuroblastoma Cells Exposed to Paraquat. Mol. Neurobiol. 2017, 54, 6018–6031. [Google Scholar] [CrossRef]
- Guang, H.M.; Du, G.H. Protections of pinocembrin on brain mitochondria contribute to cognitive improvement in chronic cerebral hypoperfused rats. Eur. J. Pharmacol. 2006, 542, 77–83. [Google Scholar] [CrossRef]
- Guang, H.M.; Gao, M.; Zhu, S.Y.; He, X.L.; He, G.R.; Zhu, X.M.; Du, G.H. Effect of pinocembrin on Mitochondrial function in Rats with Acute focal Cerebral Ischemia. Chin. Pharm. Bull. 2012, 28, 24–29. [Google Scholar]
- Guo, L.; Chen, X.; Li, L.N.; Tang, W.; Pan, Y.T.; Kong, J.Q. Transcriptome-enabled discovery and functional characterization of enzymes related to (2S)-pinocembrin biosynthesis from Ornithogalum caudatum and their application for metabolic engineering. Microb. Cell Fact. 2016, 15, 27–45. [Google Scholar] [CrossRef]
- Shi, L.L.; Qiang, G.F.; Gao, M.; Zhang, H.A.; Chen, B.N.; Yu, X.Y.; Xuan, Z.H.; Wang, Q.Y.; Du, G.H. Effect of pinocembrin on brain mitochondrial respiratory function. Acta Pharm. Sin. 2011, 46, 642–649. [Google Scholar]
- Liu, R.; Wu, C.X.; Zhou, D.; Yang, F.; Tian, S.; Zhang, L.; Zhang, T.T.; Du, G.H. Pinocembrin protects against β-amyloid-induced toxicity in neurons through inhibiting receptor for advanced glycation end products (RAGE)-independent signaling pathways and regulating mitochondrion-mediated apoptosis. BMC Med. 2012, 10, 105. [Google Scholar] [CrossRef]
- Liu, R.; Li, J.Z.; Song, J.K.; Zhou, D.; Huang, C.; Bai, X.Y.; Xie, T.; Zhang, X.; Li, Y.J.; Wu, C.X.; et al. Pinocembrin improves cognition and protects the neurovascular unit in Alzheimer related deficits. Neurobiol. Aging 2014, 35, 1275–1285. [Google Scholar] [CrossRef]
- Zheng, Y.; Wan, G.; Yang, B.; Gu, X.; Lin, J. Cardioprotective Natural Compound Pinocembrin Attenuates Acute Ischemic Myocardial Injury via Enhancing Glycolysis. Oxid. Med. Cell. Longev. 2020, 2020, 1–13. [Google Scholar] [CrossRef]
- Tundis, R.; Frattaruolo, L.; Carullo, G.; Armentano, B.; Badolato, M.; Loizzo, M.R.; Aiello, F.; Cappello, A.R. An ancient remedial repurposing: Synthesis of new pinocembrin fatty acid acyl derivatives as potential antimicrobial/anti-inflammatory agents. Nat. Prod. Res. 2019, 33, 162–168. [Google Scholar] [CrossRef]
- Nardini, M.; Scaccini, C.; Packer, L.; Virgili, F. In vitro inhibition of the activity of phosphorylase kinase, protein kinase C and protein kinase A by caffeic acid and a procyanidin-rich pine bark (Pinus marittima) extract. Biochim. Biophys. Acta 2000, 1474, 219–225. [Google Scholar] [CrossRef]
- Lin, C.L.; Chen, R.F.; Chen, J.Y.; Chu, Y.C.; Wang, H.M.; Chou, H.L.; Chang, W.C.; Fong, Y.; Chang, W.T.; Wu, C.Y.; et al. Protective effect of caffeic acid on paclitaxel induced anti-proliferation and apoptosis of lung cancer cells involves NF-κB pathway. Int. J. Mol. Sci. 2012, 13, 6236–6245. [Google Scholar] [CrossRef] [PubMed]
- Min, J.; Shen, H.; Xi, W.; Wang, Q.; Yin, L.; Zhang, Y.; Yu, Y.; Yang, Q.; Wang, Z.N. Synergistic Anticancer Activity of Combined Use of Caffeic Acid with Paclitaxel Enhances Apoptosis of Non-Small-Cell Lung Cancer H1299 Cells in Vivo and in Vitro. Cell. Physiol. Biochem. 2018, 48, 1433–1442. [Google Scholar] [CrossRef] [PubMed]
- Olgierd, B.; Kamila, Ż.; Anna, B.; Emilia, M. The Pluripotent Activities of Caffeic Acid Phenethyl Ester. Molecules 2021, 26, 1335. [Google Scholar] [CrossRef]
- Lv, L.; Cui, H.; Ma, Z.; Liu, X.; Yang, L. Recent progresses in the pharmacological activities of caffeic acid phenethyl ester. Naunyn Schmiedebergs Arch. Pharmacol. 2021, 1–13. [Google Scholar] [CrossRef]
- Wang, L.C.; Chu, K.H.; Liang, Y.C.; Lin, Y.L.; Chiang, B.L. Caffeic acid phenethyl ester inhibits nuclear factor-kappaB and protein kinase B signalling pathways and induces caspase-3 expression in primary human CD4+ T cells. Clin. Exp. Immunol. 2010, 160, 223–232. [Google Scholar] [CrossRef]
- Cheng, H.; Zhang, Y.; Lu, W.; Gao, X.; Xu, C.; Bao, H. Caffeic acid phenethyl ester attenuates neuropathic pain by suppressing the p38/NF-κB signal pathway in microglia. J. Pain Res. 2018, 11, 2709–2719. [Google Scholar] [CrossRef]
- Kim, H.; Kim, W.; Yum, S.; Hong, S.; Oh, J.E.; Lee, J.W.; Kwak, M.K.; Park, E.J.; Na, D.H.; Jung, Y. Caffeic acid phenethyl ester activation of Nrf2 pathway is enhanced under oxidative state: Structural analysis and potential as a pathologically targeted therapeutic agent in treatment of colonic inflammation. Free Radic. Biol. Med. 2013, 65, 552–562. [Google Scholar] [CrossRef]
- Sorrenti, V.; Raffaele, M.; Vanella, L.; Acquaviva, R.; Salerno, L.; Pittalà, V.; Intagliata, S.; Di Giacomo, C. Protective Effects of Caffeic Acid Phenethyl Ester (CAPE) and Novel Cape Analogue as Inducers of Heme Oxygenase-1 in Streptozotocin-Induced Type 1 Diabetic Rats. Int. J. Mol. Sci. 2019, 20, 2441. [Google Scholar] [CrossRef]
- Hassan, N.A.; El-Bassossy, H.M.; Mahmoud, M.F.; Fahmy, A. Caffeic acid phenethyl ester, a 5-lipoxygenase enzyme inhibitor, alleviates diabetic atherosclerotic manifestations: Effect on vascular reactivity and stiffness. Chem. Biol. Interact. 2014, 213, 28–36. [Google Scholar] [CrossRef]
- Tsai, C.F.; Kuo, Y.H.; Yeh, W.L.; Wu, C.Y.; Lin, H.Y.; Lai, S.W.; Liu, Y.S.; Wu, L.H.; Lu, J.K.; Lu, D.Y. Regulatory effects of caffeic acid phenethyl ester on neuroinflammation in microglial cells. Int. J. Mol. Sci. 2015, 16, 5572–5589. [Google Scholar] [CrossRef]
- Kurauchi, Y.; Hisatsune, A.; Isohama, Y.; Mishima, S.; Katsuki, H. Caffeic acid phenethyl ester protects nigral dopaminergic neurons via dual mechanisms involving haem oxygenase-1 and brain-derived neurotrophic factor. Br. J. Pharmacol. 2012, 166, 1151–1168. [Google Scholar] [CrossRef]
- Yasui, N.; Nishiyama, E.; Juman, S.; Negishi, H.; Miki, T.; Yamori, Y.; Ikeda, K. Caffeic acid phenethyl ester suppresses oxidative stress in 3T3-L1 adipocytes. J. Asian Nat. Prod. Res. 2013, 15, 1189–1196. [Google Scholar] [CrossRef]
- Vanella, L.; Tibullo, D.; Godos, J.; Pluchinotta, F.R.; Di Giacomo, C.; Sorrenti, V.; Acquaviva, R.; Russo, A.; Li Volti, G.; Barbagallo, I. Caffeic Acid Phenethyl Ester Regulates PPAR’s Levels in Stem Cells-Derived Adipocytes. PPAR Res. 2016, 2016, 1–13. [Google Scholar] [CrossRef]
- Abraham, N.G.; Junge, J.M.; Drummond, G.S. Translational Significance of Heme Oxygenase in Obesity and Metabolic Syndrome. Trends Pharmacol Sci. 2016, 37, 17–36. [Google Scholar] [CrossRef]
- Romana-Souza, B.; Dos Santos, J.S.; Monte-Alto-Costa, A. Caffeic acid phenethyl ester promotes wound healing of mice pressure ulcers affecting NF-κB, NOS2 and NRF2 expression. Life Sci. 2018, 207, 158–165. [Google Scholar] [CrossRef]
- Chung, L.-C.; Chiang, K.-C.; Feng, T.-H.; Chang, K.-S.; Chuang, S.-T.; Chen, Y.-J.; Tsui, K.-H.; Lee, J.-C.; Juang, H.-H. Caffeic acid phenethyl ester upregulates N-myc downstream regulated gene 1 via ERK pathway to inhibit human oral cancer cell growth in vitro and in vivo. Mol. Nutr. Food Res. 2017, 61. [Google Scholar] [CrossRef]
- Chiang, K.C.; Yang, S.W.; Chang, K.P.; Feng, T.H.; Chang, K.S.; Tsui, K.H.; Shin, Y.S.; Chen, C.C.; Chao, M.; Juang, H.H. Caffeic acid phenethyl ester induces N-myc downstream regulated gene 1 to inhibit cell proliferation and invasion of human nasopharyngeal cancer cells. Int. J. Mol. Sci. 2018, 19, 1397. [Google Scholar] [CrossRef]
- Onori, P.; DeMorrow, S.; Gaudio, E.; Franchitto, A.; Mancinelli, R.; Venter, J.; Kopriva, S.; Ueno, Y.; Alvaro, D.; Savage, J.; et al. Caffeic acid phenethyl ester decreases cholangiocarcinoma growth by inhibition of NF-kappaB and induction of apoptosis. Int. J. Cancer 2009, 125, 565–576. [Google Scholar] [CrossRef]
- Liang, Y.; Feng, G.; Wu, L.; Zhong, S.; Gao, X.; Tong, Y.; Cui, W.; Qin, Y.; Xu, W.; Xiao, X.; et al. Caffeic acid phenethyl ester suppressed growth and metastasis of nasopharyngeal carcinoma cells by inactivating the NF-kappaB pathway. Drug Des. Dev. Ther. 2019, 13, 1335–1345. [Google Scholar] [CrossRef]
- Kuo, Y.Y.; Lin, H.P.; Huo, C.; Su, L.C.; Yang, J.; Hsiao, P.H.; Chiang, H.C.; Chung, C.J.; Wang, H.D.; Chang, J.Y.; et al. Caffeic acid phenethyl ester suppresses proliferation and survival of TW2.6 human oral cancer cells via inhibition of Akt signaling. Int. J. Mol. Sci. 2013, 14, 8801–8817. [Google Scholar] [CrossRef]
- Huang, Y.; Jin, M.; Pi, R.; Zhang, J.; Chen, M.; Ouyang, Y.; Liu, A.; Chao, X.; Liu, P.; Liu, J.; et al. Protective effects of caffeic acid and caffeic acid phenethyl ester against acrolein-induced neurotoxicity in HT22 mouse hippocampal cells. Neurosci. Lett. 2013, 535, 146–151. [Google Scholar] [CrossRef]
- Wang, D.; Xiang, D.B.; He, Y.J.; Li, Z.P.; Wu, X.H.; Mou, J.H.; Xiao, H.L.; Zhang, Q.H. Effect of caffeic acid phenethyl ester on proliferation and apoptosis of colorectal cancer cells in vitro. World J. Gastroenterol. 2005, 11, 4008–4012. [Google Scholar] [CrossRef] [PubMed]
- Morroni, F.; Sita, G.; Graziosi, A.; Turrini, E.; Fimognari, C.; Tarozzi, A.; Hrelia, P. Neuroprotective effect of caffeic acid phenethyl ester in a mouse model of Alzheimer’s disease involves Nrf2/HO-1 pathway. Aging Dis. 2018, 9, 605–622. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.M.; Abd El-Twab, S.M. Caffeic acid phenethyl ester protects the brain against hexavalent chromium toxicity by enhancing endogenous antioxidants and modulating the JAK/STAT signaling pathway. Biomed. Pharmacother. 2017, 91, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Breger, J.; Fuchs, B.B.; Aperis, G.; Moy, T.I.; Ausubel, F.M.; Mylonakis, E. Antifungal chemical compounds identified using a C. elegans pathogenicity assay. PLoS Pathog. 2007, 3, e18. [Google Scholar] [CrossRef]
- Sun, L.; Hang, C.; Liao, K. Synergistic effect of caffeic acid phenethyl ester with caspofungin against Candida albicans is mediated by disrupting iron homeostasis. Food. Chem. Toxicol. 2018, 116, 51–58. [Google Scholar] [CrossRef]
- Sun, L.; Liao, K.; Hang, C. Caffeic acid phenethyl ester synergistically enhances the antifungal activity of fluconazole against resistant Candida albicans. Phytomedicine 2018, 40, 55–58. [Google Scholar] [CrossRef]
- Altuntas, A.; Yilmaz, H.R.; Altuntas, A.; Uz, E.; Demir, M.; Gokcimen, A.; Aksu, O.; Bayram, D.S.; Sezer, M.T. Caffeic acid phenethyl ester protects against amphotericin B induced nephrotoxicity in rat model. BioMed Res. Int. 2014, 2014, 1–8. [Google Scholar] [CrossRef]
- Velazquez, C.; Navarro, M.; Acosta, A.; Angulo, A.; Dominguez, Z.; Robles, R.; Robles-Zepeda, R.; Lugo, E.; Goycoolea, F.M.; Velazquez, E.F.; et al. Antibacterial and free-radical scavenging activities of Sonoran propolis. J. Appl. Microbiol. 2007, 103, 1747–1756. [Google Scholar] [CrossRef]
- Collins, W.; Lowen, N.; Blake, D.J. Caffeic acid esters are effective bactericidal compounds against Paenibacillus larvae by altering intracellular oxidant and antioxidant levels. Biomolecules 2019, 9, 312. [Google Scholar] [CrossRef]
- Niu, Y.; Wang, K.; Zheng, S.; Wang, Y.; Ren, Q.; Li, H.; Ding, L.; Li, W.; Zhang, L. Antibacterial effect of caffeic acid phenethyl ester on cariogenic bacteria and Streptococcus mutans biofilms. Antimicrob. Agents. Chemother. 2020, 64, e00251-20. [Google Scholar] [CrossRef]
- Veloz, J.J.; Alvear, M.; Salazar, L.A. Antimicrobial and antibiofilm activity against Streptococcus mutans of individual and mixtures of the main polyphenolic compounds found in Chilean propolis. BioMed Res. Int. 2019, 2019, 1–7. [Google Scholar] [CrossRef]
- Navarro-Navarro, M.; Ruiz-Bustos, P.; Valencia, D.; Robles-Zepeda, R.; Ruiz-Bustos, E.; Virues, C.; Hernandez, J.; Dominguez, Z.; Velazquez, C. Antibacterial activity of Sonoran propolis and some of its constituents against clinically significant Vibrio species. Foodborne Pathog. Dis. 2013, 10, 150–158. [Google Scholar] [CrossRef]
- Lee, H.S.; Lee, S.Y.; Park, S.H.; Lee, J.H.; Ahn, S.K.; Choi, Y.M.; Choi, D.J.; Chang, J.H. Antimicrobial medical sutures with caffeic acid phenethyl ester and their in vitro/in vivo biological assessment. MedChemComm 2013, 4, 777. [Google Scholar] [CrossRef]
- Ho, C.C.; Lin, S.S.; Chou, M.Y.; Chen, F.L.; Hu, C.C.; Chen, C.S.; Lu, G.-Y.; Yang, C.C. Effects of CAPE-like compounds on HIV replication in vitro and modulation of cytokines in vivo. J. Antimicrob. Chemother. 2005, 56, 372–379. [Google Scholar] [CrossRef]
- Shen, H.; Yamashita, A.; Nakakoshi, M.; Yokoe, H.; Sudo, M.; Kasai, H.; Tanaka, T.; Fujimoto, Y.; Ikeda, M.; Kato, N.; et al. Inhibitory effects of caffeic acid phenethyl ester derivatives on replication of hepatitis c virus. PLoS ONE 2013, 8, e82299. [Google Scholar] [CrossRef]
- Kishimoto, N.; Kakino, Y.; Iwai, K.; Mochida, K.; Fujita, T. In vitro antibacterial, antimutagenic and anti-influenza virus activity of caffeic acid phenethyl esters. Biocontrol Sci. 2005, 10, 155–161. [Google Scholar] [CrossRef][Green Version]
- Abamor, E.S. Antileishmanial activities of caffeic acid phenethyl ester loaded PLGA nanoparticles against Leishmania infantum promastigotes and amastigotes in vitro. Asian Pac. J. Trop. Med. 2017, 10, 25–34. [Google Scholar] [CrossRef]
- Zhu, H.; Liang, Q.H.; Xiong, X.G.; Wang, Y.; Zhang, Z.H.; Sun, M.J.; Lu, X.; Wu, D. Anti-Inflammatory Effects of p-Coumaric Acid, a Natural Compound of Oldenlandia diffusa, on Arthritis Model Rats. Evid. Based Complement. Alternat. Med. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Sabitha, R.; Nishi, K.; Gunasekaran, V.P.; Annamalai, G.; Agilan, B.; Ganeshan, M. p-Coumaric acid ameliorates ethanol–induced kidney injury by inhibiting inflammatory cytokine production and NF–κB signaling in rats. Asian Pac. J. Trop. Biomed. 2019, 9, 188–195. [Google Scholar]
- Lampiasi, N.; Montana, G. An in vitro inflammation model to study the Nrf2 and NF-κB crosstalk in presence of ferulic acid as modulator. Immunobiology 2018, 223, 349–355. [Google Scholar] [CrossRef]
- Wink, M. Evolutionary advantage and molecular modes of action of multi-component mixtures used in phytomedicine. Curr. Drug Metab. 2008, 9, 996–1009. [Google Scholar] [CrossRef]
- Búfalo, M.C.; Ferreira, I.; Costa, G.; Francisco, V.; Liberal, J.; Cruz, M.T.; Lopes, M.C.; Batista, M.T.; Sforcin, J.M. Propolis and its constituent caffeic acid suppress LPS-stimulated pro-inflammatory response by blocking NF-κB and MAPK activation in macrophages. J. Ethnopharmacol. 2013, 149, 84–92. [Google Scholar] [CrossRef]
- Claus, R.; Kinscherf, R.; Gehrke, C.; Bonaterra, G.; Basnet, P.; Metz, J.; Deigner, H.P. Antiapoptotic effects of propolis extract and propol on human macrophages exposed to minimally modified low density lipoprotein. Arzneimittelforschung 2000, 50, 373–379. [Google Scholar] [CrossRef]
- Xuan, H.; Yuan, W.; Chang, H.; Liu, M.; Hu, F. Anti-inflammatory effects of Chinese propolis in lipopolysaccharide-stimulated human umbilical vein endothelial cells by suppressing autophagy and MAPK/NF-κB signaling pathway. Inflammopharmacology 2019, 27, 561–571. [Google Scholar] [CrossRef]
- Hotta, S.; Uchiyama, S.; Ichihara, K. Brazilian red propolis extract enhances expression of antioxidant enzyme genes in vitro and in vivo. Biosci. Biotechnol. Biochem. 2020, 84, 1820–1830. [Google Scholar] [CrossRef]
- Zhang, J.; Shen, X.; Wang, K.; Cao, X.; Zhang, C.; Zheng, H.; Hu, F. Antioxidant activities and molecular mechanisms of the ethanol extracts of Baccharis propolis and Eucalyptus propolis in RAW64.7 cells. Pharm. Biol. 2016, 54, 2220–2235. [Google Scholar] [CrossRef]
- Kosalec, I.; Pepeljnjak, S.; Bakmaz, M.; Vladimir-Knezević, S. Flavonoid analysis and antimicrobial activity of commercially available propolis products. Acta Pharm. 2005, 55, 423–430. [Google Scholar]
- Tlak Gajger, I.; Pavlović, I.; Bojić, M.; Kosalec, I.; Srečec, S.; Vlainić, T.; Vlainić, J. The components responsible for the antimicrobial activity of propolis from continental and Mediterranean regions in Croatia. Czech J. Food Sci. 2017, 35, 376–385. [Google Scholar] [CrossRef]
- Vasconcelos, N.G.; Croda, J.; Simionatto, S. Antibacterial mechanisms of cinnamon and its constituents: A review. Microb. Pathog. 2018, 120, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Quan, T.H.; Benjakul, S.; Sae-Ieaw, T.; Balange, A.K.; Maqsood, S. Protein–polyphenol conjugates: Antioxidant property, functionalities and their applications. Trends Food Sci. Technol. 2019, 91, 507–517. [Google Scholar] [CrossRef]
- Manach, C.; Scalbert, A.; Morand, C.; Rémésy, C.; Jiménez, L. Polyphenols: Food sources and bioavailability. Am. J. Clin. Nutr. 2004, 79, 727–747. [Google Scholar] [CrossRef]
- Curti, V.; Zaccaria, V.; Tsetegho Sokeng, A.J.; Dacrema, M.; Masiello, I.; Mascaro, A.; D’Antona, G.; Daglia, M. Bioavailability and In Vivo Antioxidant Activity of a Standardized Polyphenol Mixture Extracted from Brown Propolis. Int. J. Mol. Sci. 2019, 20, 1250. [Google Scholar] [CrossRef]
- Mašek, T.; Perin, N.; Racané, L.; Cindrić, M.; Čipčić Paljetak, H.; Perić, M.; Matijašić, M.; Verbanac, D.; Radić, B.; Šuran, J.; et al. Chemical Composition, Antioxidant and Antibacterial Activity of Different Extracts of Poplar Type Propolis. Croat. Chem. Acta 2018, 91, 81–88. [Google Scholar] [CrossRef]
- Cunha, I.B.S.; Sawaya, A.C.H.F.; Caetano, F.M.; Shimizu, M.T.; Marcucci, M.C.; Drezza, F.T.; Povia, G.S.; de Carlavario, O.P. Factors that Influence the Yield and Composition of Brazilian Propolis Extracts. J. Braz. Chem. Soc. 2004, 15, 964–970. [Google Scholar] [CrossRef]
- Park, Y.K.; Ikegaki, M. Preparation of Water and Ethanolic Extracts of Propolis and Evaluation of the Preparations. Biosci. Biotechnol. Biochem. 1998, 62, 2230–2232. [Google Scholar] [CrossRef]
- Rocha, B.A.; Pires Bueno, P.C.; de Oliviera Lima Leite Vaz, M.M.; Piacezzi Nascimento, A.; Ursoli Ferreira, N.; de Padua Moreno, G.; Rezende Rodrigues, M.; de Mello Costa-Machado, A.R.; Aparecida Barizon, E.; Costa Lima Campos, J.; et al. Evaluation of a Propolis Water Extract Using a Reliable RP-HPLC Methodology and In Vitro and In Vivo Efficacy and Safety Characterisation. Evid. Based Complement. Altern. Med. 2013, 2013. [Google Scholar] [CrossRef]
- Tsukada, T.; Kameda, W.W.; Ide, M. Production of Water-Soluble Propolis Pharmaceutical Preparation. JP Patent 3149208B2, 26 March 2001. [Google Scholar]
- Kwan, H.S. Production of 100% Pure Water-Soluble Propolis by Dissolving Frozen Propolis in Boiling Water. KR Patent 20050004419, 12 May 2005. [Google Scholar]
- Jin, C.S. Rinse Create Matter. KR Patent 20030050938A, 25 June 2003. [Google Scholar]
- Meng, L.; Li, Y. Propolis Natural Reduction Extraction Process Method. CN Patent 102078337A, 1 June 2011. [Google Scholar]
- Ivanovich, S.G. Method for Production of Aqueous Propolis Extract. RU Patent 2402923C1, 10 November 2010. [Google Scholar]
- Sosonowski, Z.M. Method for Extracting Propolis and Water Soluble Dry Propolis Powder. US Patent 4,382,886, 10 May 1983. [Google Scholar]
- Ramanauskienė, K.; Inkėnienė, A.M.; Petrikaitė, V.; Briedis, V. Total Phenolic Content and Antimicrobial Activity of Different Lithuanian Propolis Solution. Evid. Based Complement. Altern. Med. 2013, 2013, 1–5. [Google Scholar] [CrossRef]
- Kubiliene, L.; Jekabsone, A.; Zilius, M.; Trumbeckaite, S.; Simanaviciute, D.; Gerbutaviciene, R.; Majiene, D. Comparison of aqueous, polyethylene glycol-aqueous and ethanolic propolis extracts: Antioxidant and mitochondria modulating properties. BMC Complement. Altern. Med. 2018, 18, 165. [Google Scholar] [CrossRef]
- Savickas, A.; Briedis, V.; Baskevicius, K.G.A.J. Oil Extract of Bee Glue and Process for Preparing the Same. LT Patent 5005B, 27 January 2003. [Google Scholar]
- Keskin, Ş. Orange peel volatile oil: A green solvent for propolis extraction, enhanced α-amilase inhibition activity. Flavour Fragr. J. 2020, 35, 411–416. [Google Scholar] [CrossRef]
- Funari, C.S.; Sutton, A.T.; Lajarim Carneiro, R.; Fraige, K.; Cavalheiro, A.J.; de Silva Bolzani, V.; Hilder, E.F.; Arrua, R.D. Natural deep eutectic solvents and aqueous solutions as an alternative extraction media for propolis. Food Res. Int. 2019, 125, 108559. [Google Scholar] [CrossRef]
- Funari, C.S.; Sutton, A.T.; Lajarim Carneiro, R.; Fraige, K.; Cavalheiro, A.J.; de Silva Bolzani, V.; Hilder, E.F.; Arrua, R.D. Searching for Alternative Solvents for Extracting Green Propolis Type. In Proceedings of the 1st International Congress on Bioactive Compounds and 2nd International Workshop on Bioactive Compounds: Food Design and Health, 22–23 November 2018; Cazarin, C.B.B., Bicas, J.L., Marostica, M.R., Eds.; The Faculty of Food Engineering of the State University of Campinas—FEA/UNICAMP: Campinas, Brasil, 2018; Volume 94196, Available online: https://proceedings.science/icbc-2018/papers/searching-for-alternative-solvents-for-extracting-green-propolis-type (accessed on 20 April 2021).
- Idrus, N.F.M.; Yian, L.N.; Idham, Z.; Aris, N.A.; Rahmana Putra, N.; Aziz, A.H.A.; Yunus, M.A.C. Mini review: Application of supercritical carbon dioxide in extraction of propolis extract. Malays. J. Fund. Appl. Sci. 2018, 14, 387–396. [Google Scholar] [CrossRef]
- Mourtzinos, I.; Koutsianas, N.; Dragani, P.; Patera, A. Extraction and Formation of Inclusion Complexes of Propolis Active Components with Hydroxypropyl-Beta-Cyclodextrin. WO Patent 2012/073051A1, 7 June 2012. [Google Scholar]
- Trusheva, B.; Trunkova, D.; Bankova, V. Different extraction methods of biological active components from propolis: A preliminary study. Chem. Cent. J. 2007, 1, 13. [Google Scholar] [CrossRef] [PubMed]
- Oroian, M.; Dranca, F.; Ursachi, F. Comparative evaluation of maceration, microwave and ultrasonic-assisted extraction of phenolic compounds from propolis. J. Food Sci. Technol. 2020, 57, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Aslam, R.; Makroo, H.A. High pressure extraction and its application in the extraction of bio-active compounds: A review. J. Food Process Eng. 2018, 42, e12896. [Google Scholar] [CrossRef]
- Bankova, V.; Trusheva, B.; Popova, M. Propolis extraction methods: A review. J. Apic. Res. 2021. [Google Scholar] [CrossRef]
- Jun, X. Comparison of Antioxidant Activity of Ethanolic Extracts of Propolis Obtained by Different Extraction Methods. Can. J. Chem. Eng. 2006, 84, 447–451. [Google Scholar] [CrossRef]
- Paradkar, A.; Dhumal, R.; Kelly, A.; Gilda, S. Propolis and Process for the Treatment Thereof and End Products Formed Therefrom. WO Patent 2011092511A1, 4 August 2011. [Google Scholar]
- Radić, S.; Radić, B.; Šuran, J. Liquid Propolis Extract, Its Preparation and Use Thereof. WO Patent 2020169425A1, 27 August 2020. [Google Scholar]
- Lastriyanto, A.; Kartika, A.A. Innovation of Propolis Extraction Machine Based on Vaccum Resistive Heating. J. Phys. Conf. Ser. 2020, 1665, 012012. [Google Scholar] [CrossRef]
- Busch, V.M.; Pereyra-Gonzalez, A.; Segatin, N.; Santagapita, P.R.; Poklar, N.; Buera, M.P. Propolis encapsulation by spray drying: Characterization and stability. LWT Food Sci. Technol. 2017, 75, 227–235. [Google Scholar] [CrossRef]
- Šturm, L.; Gasan Osojnik Črnivec, I.; Istenič, K.; Ota, A.; Megušar, P.; Slukan, A.; Humar, M.; Levic, S.; Nedović, V.; Kopinč, R.; et al. Encapsulation of non-dewaxed propolis by freeze-drying and spray-drying using gum Arabic, maltodextrin and inulin as coating materials. Food Bioprod. Process. 2019, 116, 196–211. [Google Scholar] [CrossRef]
- Sato, T.; Mello, D.; Vasconcellos, L.; Valente, A.J.M.; Borges, A. Chitosan-Based Coacervate Polymers for Propolis Encapsulation: Release and Cytotoxicity Studies. Int. J. Mol. Sci. 2020, 21, 4561. [Google Scholar] [CrossRef]

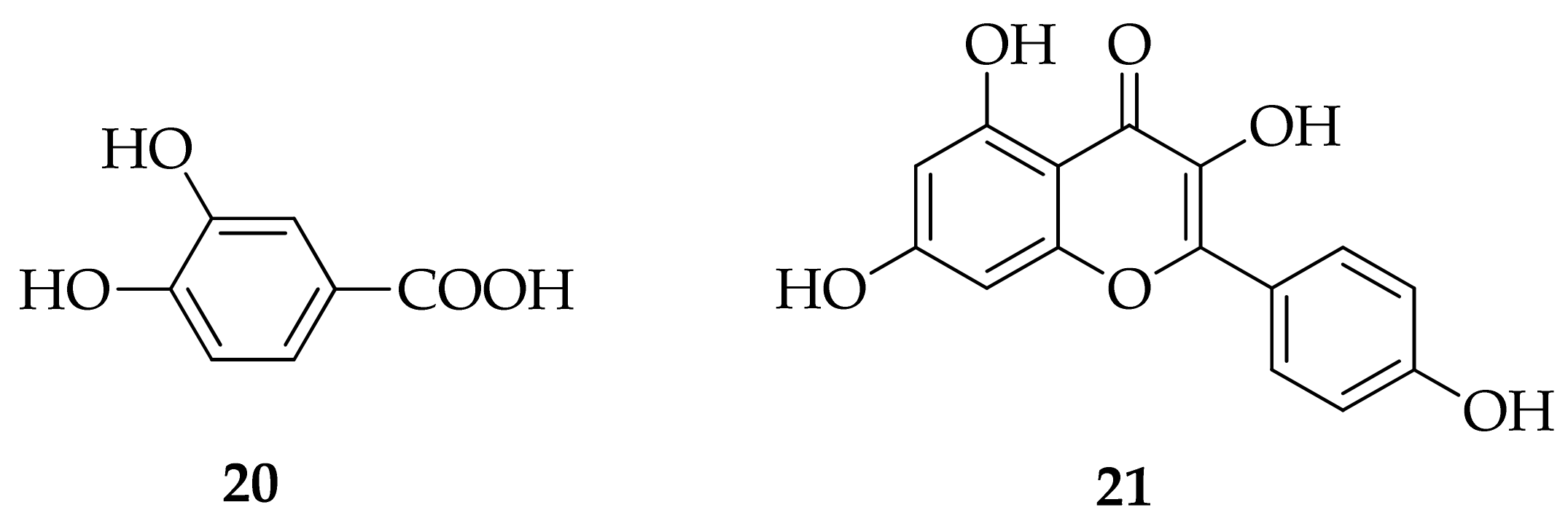
| No | Extraction Solvent (ES) (Special Conditions) | Extraction Type | P:ES Ratio (w/v) | Extraction Temperature | Extraction Duration | Ref. |
|---|---|---|---|---|---|---|
| 1 | EtOH (25–60% v/v)/H2O | M | 1:5 | r.t. | typically 10–30 days | [126] |
| 2 | EtOH (10–95% v/v)/H2O | M + P, SE | 1:12.5 | Δ/70 °C | 30 min | [127,128] |
| 3 | H2O | E | n.r. | Δ/30–50 °C | 6–8 min | [129] |
| 4 | H2O | E | 1:20 | Δ/70–95 °C | 18 h | [130] |
| 5 | H2O (4× repeated with fresh H2O) | M | 1:4 | r.t. | 72 h | [131] |
| 6 | H2O | E | 1:2 | Δ/60 °C | 30 min | [132] |
| 7 | H2O | UAE | 1:10 | Δ/50–60 °C | 2.5 h | [133] |
| 8 | OS: MeOH, n-PrOH, i-PrOH, n-BuOH, s-BuOH, t-BuOH, Et2O, BnOH, 1,2-PG, DMSO, ETG, BnBz, PEG, acetone, HOAc | M | 1:2 | r.t. | 10 days | [134] |
| 9 | 1,2-PG | M/E | 1:10–1:20 | r.t. or Δ/50–60 °C | 10 days 2 h | [135] |
| 10 | H2O/PEG 400 (20% v/v) | M | 1:10 | r.t. | 5 h | [136] |
| 11 | Glycerol (GL) | n.r. | n.r. | n.r. | n.r. | [8] |
| 12 | Glycerol (GL) | E | 1:2 | Δ/90–160 °C | n.r. | [129] |
| 13 | Plant oil | n.r. | n.r. | n.r. | n.r. | [8] |
| 14 | EtOH (96%)/sunflower oil (60:40 w/w) | n.r. | n.r | n.r | n.r | [137] |
| 15 | OPEO (mostly d-limonene) | M | 1:9 | r.t. | 48 h | [138] |
| 16 | CC/1,2-PG (1:1, n/n) | E | 1:20 | Δ/50 °C | 3 h | [139,140] |
| 17 | CC/1,2-PG (1:2, n/n) | E | 1:20 | Δ/50 °C | 3 h | [139,140] |
| 18 | CC/LA/H2O (1:2:2, n/n/n) | E | 1:20 | Δ/50 °C | 3 h | [139,140] |
| 19 | CC/LA/H2O (1:1:1, n/n/n) | E | 1:20 | Δ/50 °C | 3 h | [139,140] |
| 20 | Lys/H2O (1:10, n/n) | E | 1:20 | Δ/50 °C | 3 h | [139,140] |
| 21 | scCO2 | scE | 1:10 | Δ/40–60 °C 10–20 MPa | n.r. | [141] |
| 22 | H2O/GL (3:1)/HP-β-CD (22.5%) or H2O/GL (1:1)/HP-β-CD (11.25%) | CAAE | n.r. | n.r. | n.r. | [142] |
| 23 | EtOH/H2O, 80:20, v/v (UAE; 120 W; closed vessel) | UAE | 1:10 | Δ/70 °C | 1 h | [20] |
| 24 | EtOH/H2O, 80:20, v/v MAE: 300 W/2450 MHz/ closed vessel | MAE | 1:10 | Δ/106 °C | 15 min | [20] |
| 26 | EtOH/H2O, 70:30, v/v UAE: 300 W/20 KHz MAE: 800 W/2450 MHz | UAE MAE | 1:10 or 1:20 | 25 °C | UAE: 30 min MAE: 2 × 10 s | [143] |
| 27 | EtOH/H2O, 70:30, v/v UAE: 20 KHz MAE: 140 W/2450 MHz | UAE MAE | 1:50 | UAE: r.t. MAE: ≈60 °C | UAE: 15 min MAE: 2 × 1 min | [144] |
| 28 | EtOH/H2O, 75:25, v/v HPE: 500 MPa | HPE | 1:35 | r.t. | 1 min | [147] |
| 29 | H2O/EM EM: PS, PECO, LE, MG, PVA, PEO, PAA, cPAA, CMC, GG, XG, cPA | E | typically 1:10 | Δ/40–100 °C | 2–24 h | [148] |
| 30 | PEG200–600/LE (0.1–3.5% w/w) | M/E | 1:2–1:20 | r.t. or 10–150 °C | 5 min to 72 h | [149] |
| 31 | 1. step: H2O/16.6 kPa/100 V 2. step: EtOH/H2O, 70:30, v/v, 16.6 kPa/220 V | VRHE | n.r. | 1. 58 °C 2. 37 °C | 2 × 20 min | [150] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šuran, J.; Cepanec, I.; Mašek, T.; Radić, B.; Radić, S.; Tlak Gajger, I.; Vlainić, J. Propolis Extract and Its Bioactive Compounds—From Traditional to Modern Extraction Technologies. Molecules 2021, 26, 2930. https://doi.org/10.3390/molecules26102930
Šuran J, Cepanec I, Mašek T, Radić B, Radić S, Tlak Gajger I, Vlainić J. Propolis Extract and Its Bioactive Compounds—From Traditional to Modern Extraction Technologies. Molecules. 2021; 26(10):2930. https://doi.org/10.3390/molecules26102930
Chicago/Turabian StyleŠuran, Jelena, Ivica Cepanec, Tomislav Mašek, Božo Radić, Saša Radić, Ivana Tlak Gajger, and Josipa Vlainić. 2021. "Propolis Extract and Its Bioactive Compounds—From Traditional to Modern Extraction Technologies" Molecules 26, no. 10: 2930. https://doi.org/10.3390/molecules26102930
APA StyleŠuran, J., Cepanec, I., Mašek, T., Radić, B., Radić, S., Tlak Gajger, I., & Vlainić, J. (2021). Propolis Extract and Its Bioactive Compounds—From Traditional to Modern Extraction Technologies. Molecules, 26(10), 2930. https://doi.org/10.3390/molecules26102930









