Small Molecule Soluble Epoxide Hydrolase Inhibitors in Multitarget and Combination Therapies for Inflammation and Cancer
Abstract
1. Arachidonic Acid Pathway and Epoxyeicosatrienoic Acids (EETs)
2. Soluble Epoxide Hydrolase (sEH)
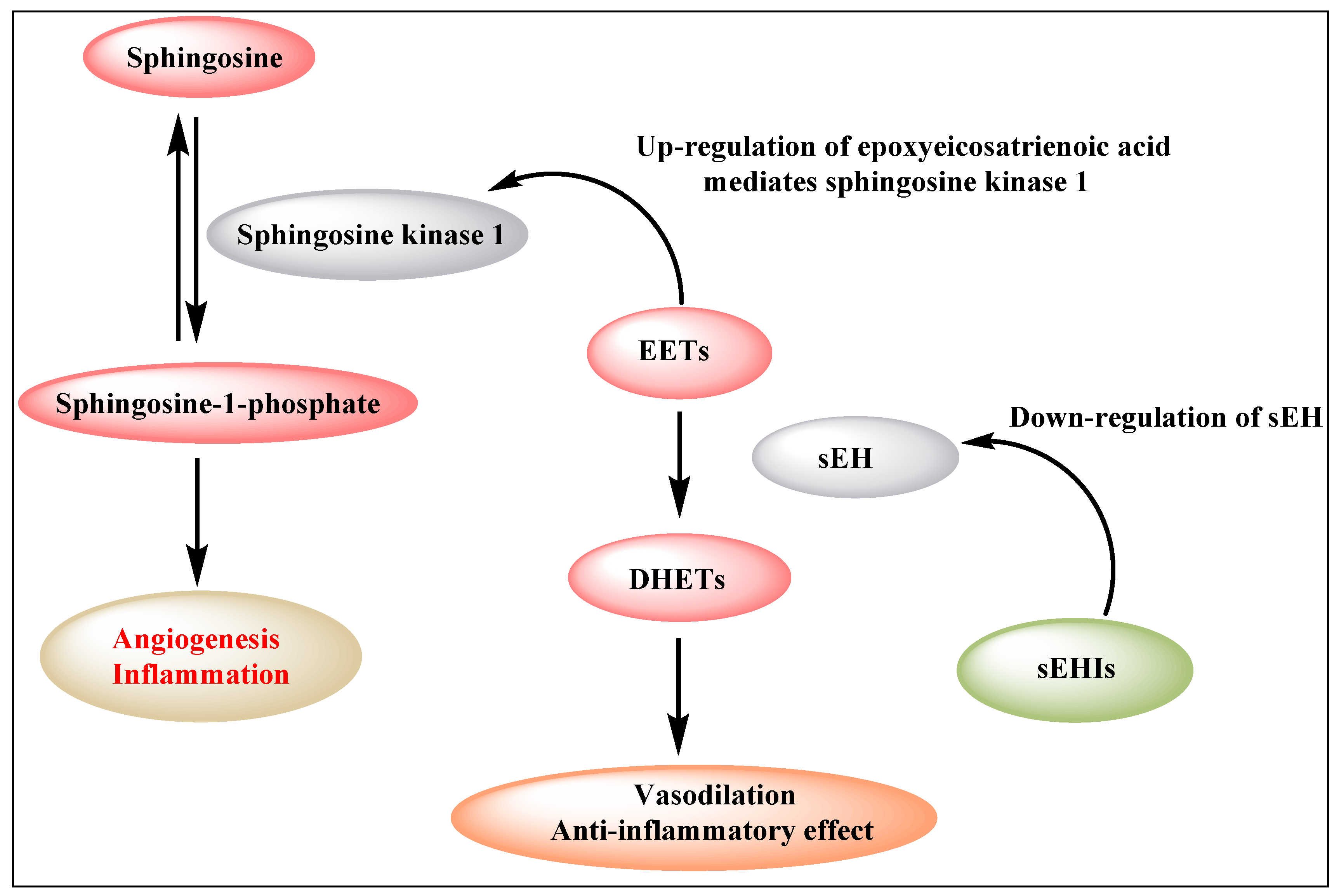
3. Role of EETs in Angiogenesis and Inflammation
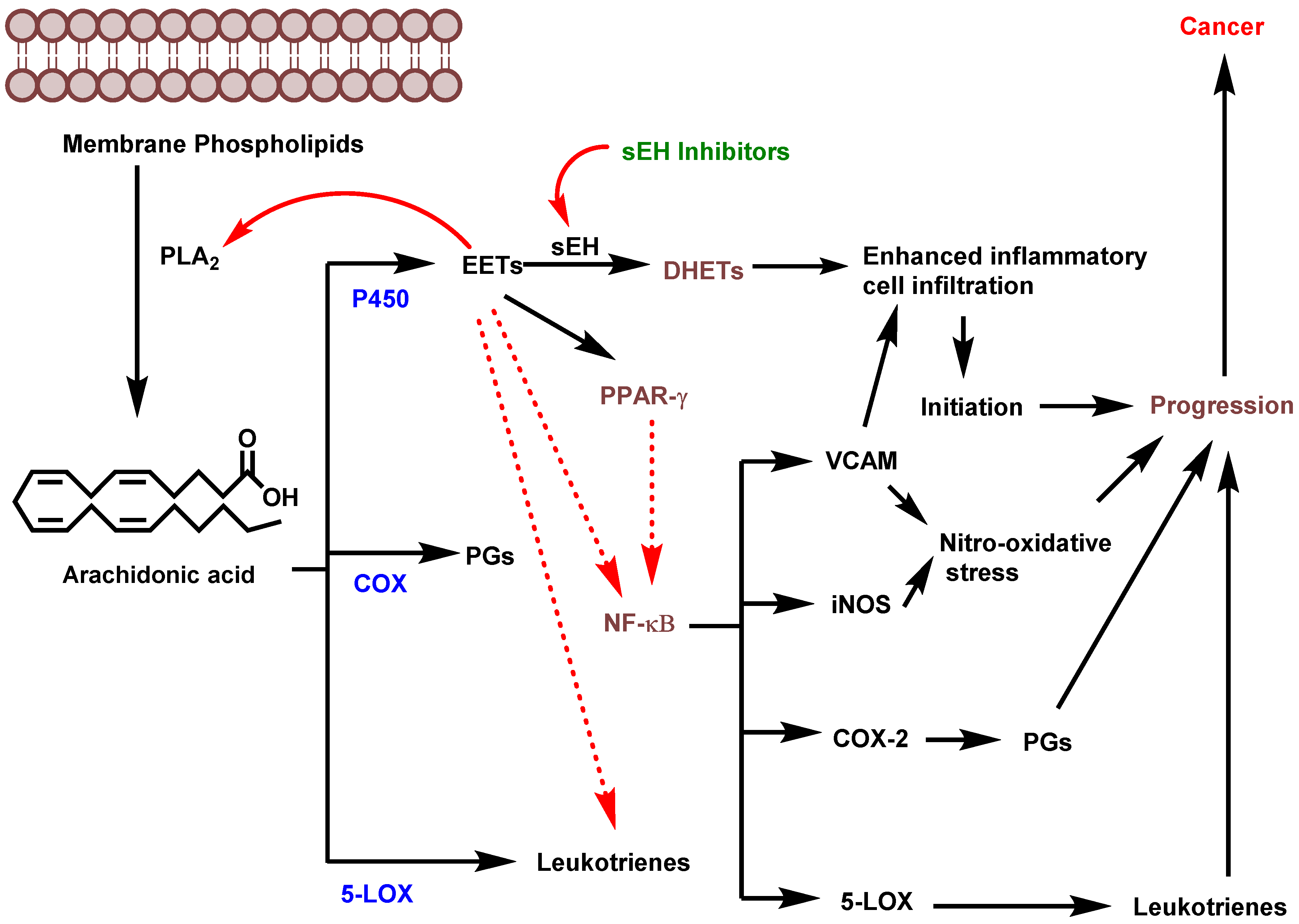
4. sEH in Inflammation-Driven Carcinogenesis
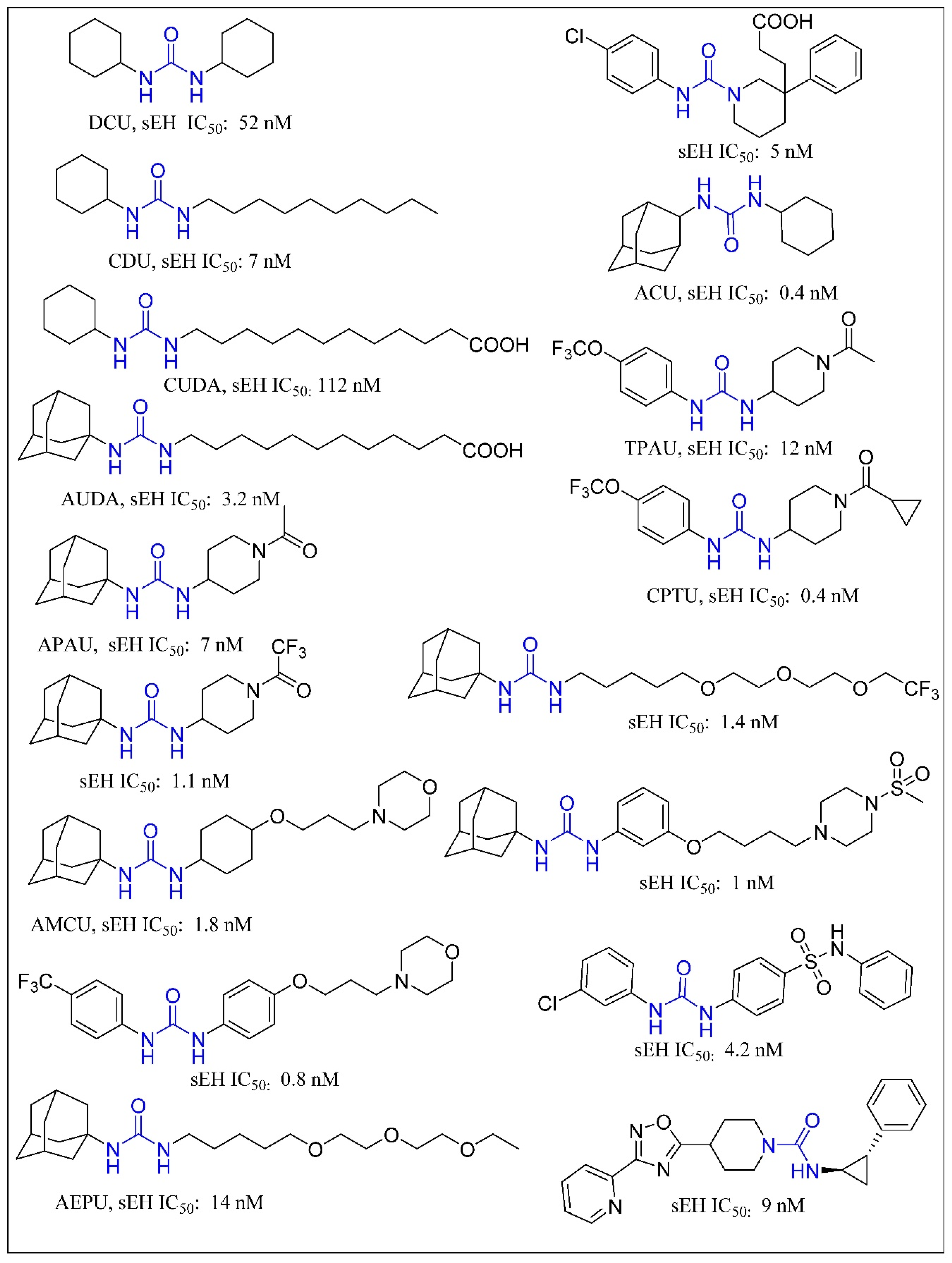
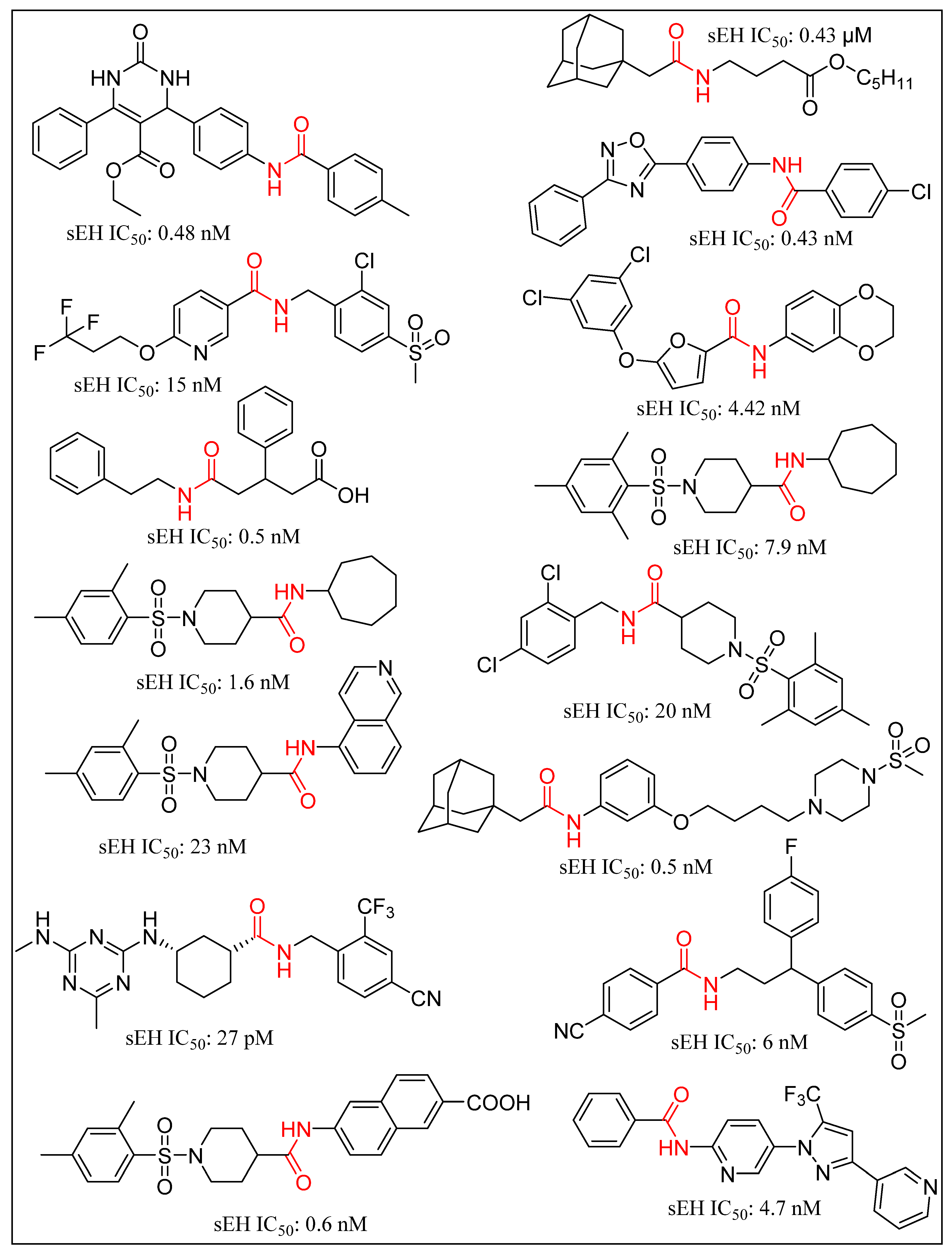
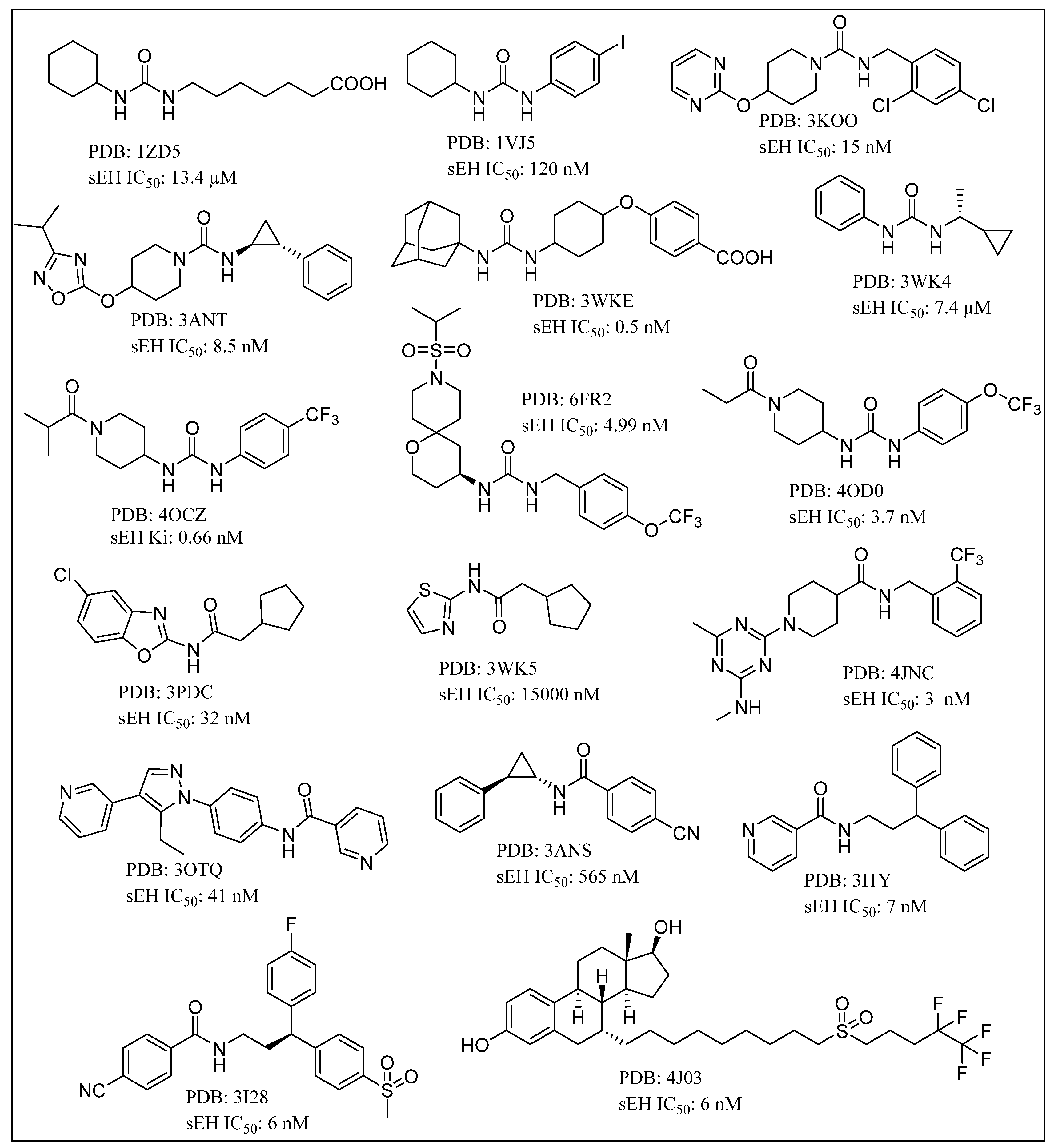
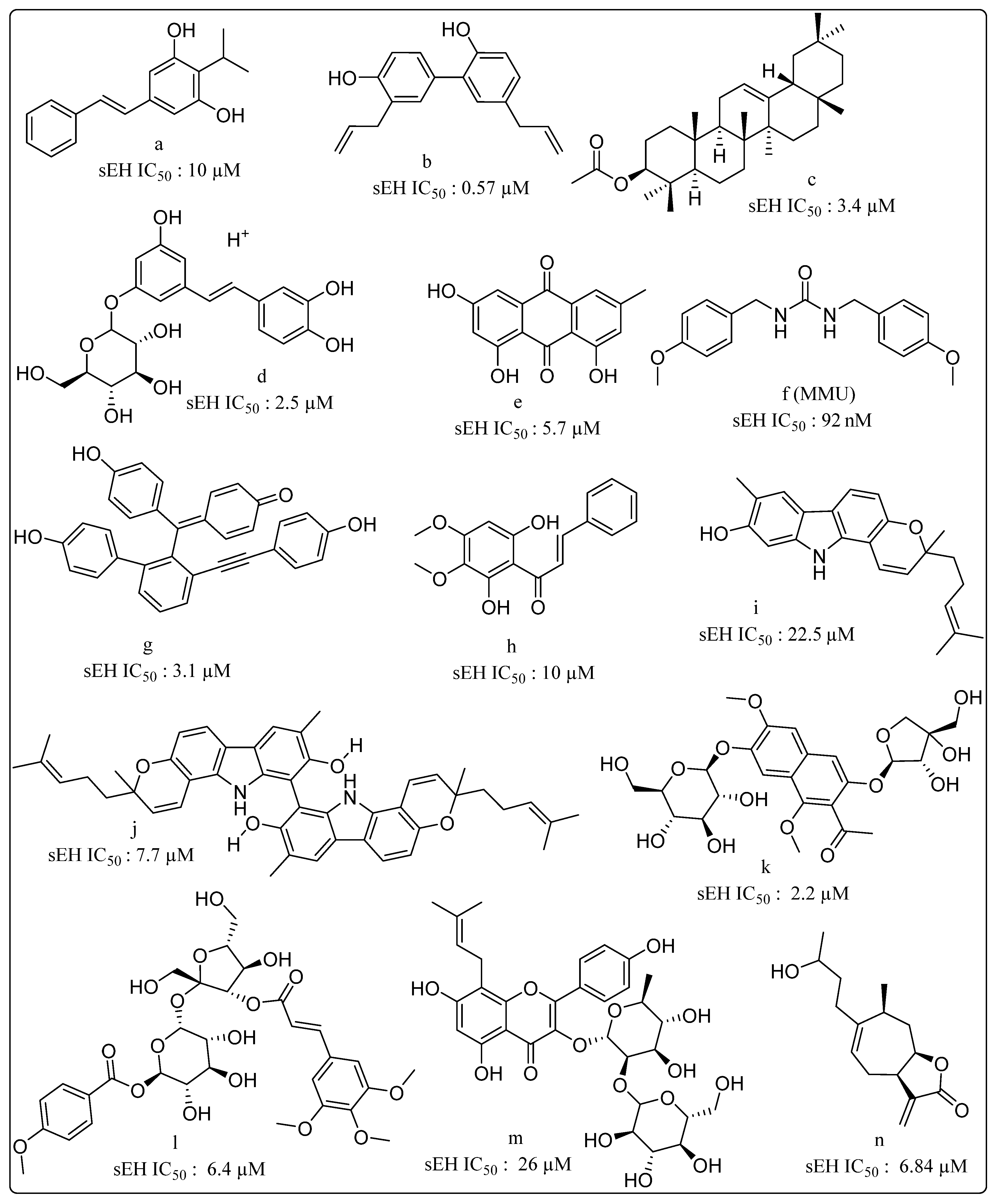
5. Soluble Epoxide Hydrolase Inhibitors (sEHIs)
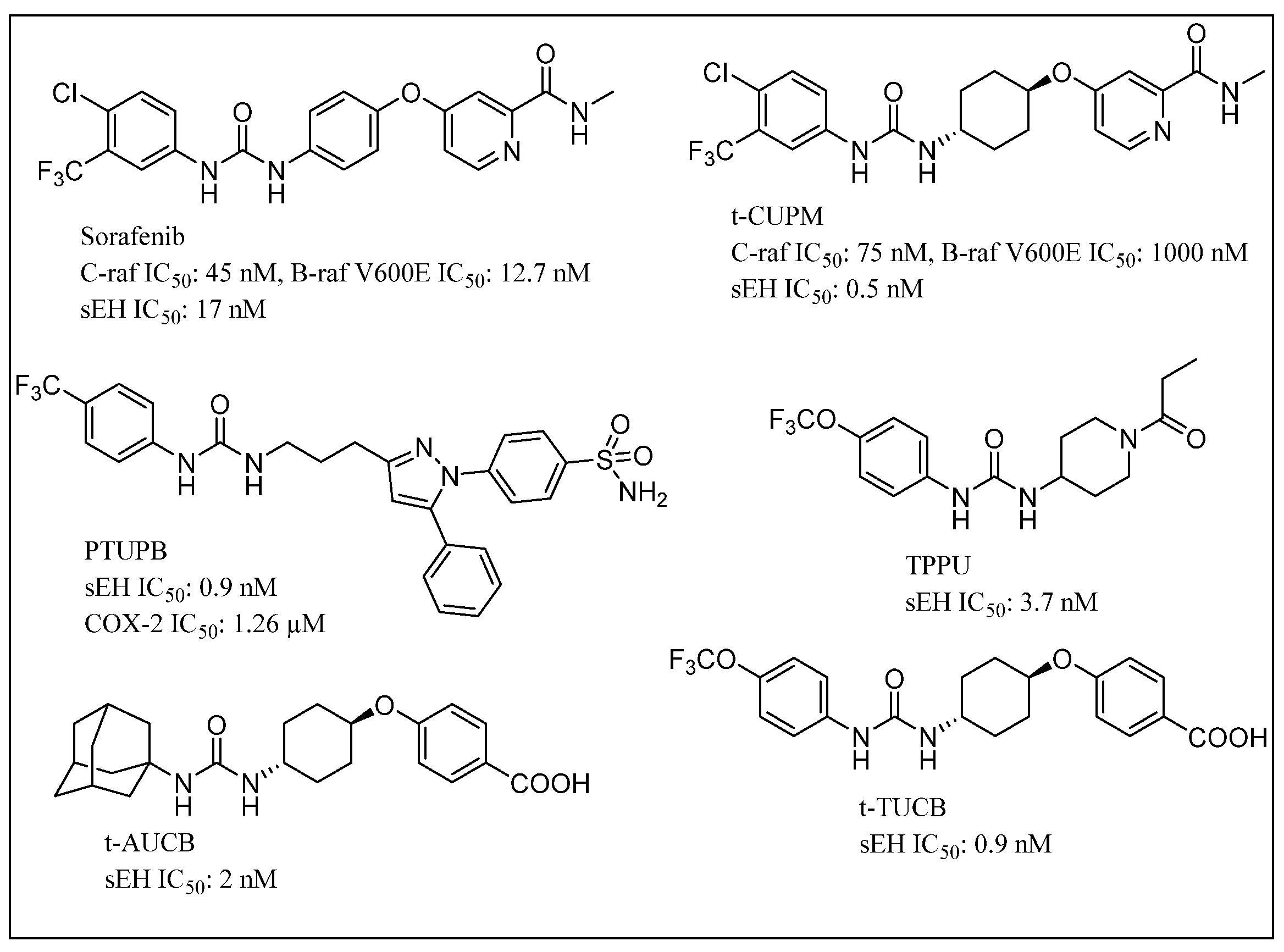
6. Dual Inhibition/Modulation of sEH as Part of Anti-Inflammatory Therapeutics
7. Dual Inhibition of sEH in Combination Chemotherapy
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| sEH | soluble epoxy hydrolase |
| EET | epoxyeicosatrienoic acid |
| ARA | arachidonic acid |
| COX | cyclooxygenase |
| LOX | lipoxygenase |
| 5-LO | 5-lipoxygenase |
| CYP | cytochrome P450 |
| HETEs | hydroxyeicosatetraenoic acids |
| LTA4 | leukotriene A4 |
| hsEH | human soluble epoxy hydrolase |
| DHETs | dihydroxyeicosatrienoic acid |
| Sphk1 | Sphingosine kinase 1 |
| FLAP | 5-lipoxygenase-activating protein |
| KRAS | Ki-ras2 Kirsten rat sarcoma viral oncogene homolog |
| sEHIs | soluble epoxy hydrolase inhibitors |
| DCU | 1,3-Dicyclohexylurea |
| CDU | 1-cyclohexyl-3-dodecyl-urea |
| AUDA | 12-(3-adamantan-1-yl-ureido) dodecanoic acid |
| AEPU | 1-adamantanyl-3-(5-(2-(2-ethoxyethoxy)ethoxy)pentyl)urea |
| APAU | 1-(1-Acetypiperidin-4-yl)-3-adamantanylurea |
| TPPU | 1-(1-propanoylpiperidin-4-yl)-3-[4-(trifluoromethoxy)phenyl]urea |
| PTUPB | 4-(5-phenyl-3-(3-[3-(4-trifluoromethyl-phenyl)-ureido]-propyl)S-pyrazol-1-yl) benzenesulfonamide |
| t-AUCB | trans-4-[4-(3-Adamantan-1-yl-ureido)-cyclohexyloxy]-benzoic acid |
| t-TUCB | trans-4-[4-[3-(4-Trifluoromethoxy-phenyl)-ureido]-cyclohexyloxy]-benzoic acid |
| CPTU | 1-(1-(cyclopropanecarbonyl)piperidin-4-yl)-3-(4 (trifluoromethoxy)phenyl)urea |
| TPAU | (1-trifluoromethoxyphenyl-3-(1-acetylpiperidin-4-yl)urea |
| ACU | 1-adamantyl-3-cyclohexylurea |
| AMAU | N-((1-acetylpiperidin-4-yl)methyl)-N’-(adamant-1-yl)urea |
| CUPM | 5-[4-[3-(4-chloro-3-trifluoromethyl-phenyl)-ureido]-cyclohexyloxy]-pyridine-2-carboxylic acid methylamide |
References
- Needleman, P.; Truk, J.; Jakschik, B.A.; Morrison, A.R.; Lefkowith, J.B. Arachidonic acid metabolism. Annu. Rev. Biochem. 1986, 55, 69–102. [Google Scholar] [CrossRef] [PubMed]
- Imig, J.D. Epoxides and soluble epoxide hydrolase in cardiovascular physiology. Physiol. Rev. 2012, 92, 101–130. [Google Scholar] [CrossRef] [PubMed]
- Kulmatycki, K.M.; Jamali, F. Drug disease interactions: Role of inflammatory mediators in disease and variability in drug response. Inflammation 2005, 23, 24. [Google Scholar]
- Zhang, W.; Liao, J.; Li, H.; Dong, H.; Bai, H.; Yang, A.; Hammock, B.D.; Yang, G.Y. Reduction of inflammatory bowel disease-induced tumor development in IL-10 knockout mice with soluble epoxide hydrolase gene deficiency. Mol. Carcinog. 2013, 52, 726–738. [Google Scholar] [CrossRef]
- Norwood, S.; Liao, J.; Hammock, B.D.; Yang, G.Y. Epoxyeicosatrienoic acids and soluble epoxide hydrolase: Potential therapeutic targets for inflammation and its induced carcinogenesis. Am. J. Transl. Res. 2010, 2, 447. [Google Scholar]
- Spector, A.A.; Fang, X.; Snyder, G.D.; Weintraub, N.L. Epoxyeicosatrienoic acids (EETs): Metabolism and biochemical function. Prog. Lipid Res. 2004, 43, 55–90. [Google Scholar] [CrossRef]
- Wei, X.; Zhang, D.; Dou, X.; Niu, N.; Huang, W.; Bai, J.; Zhang, G. Elevated 14, 15-epoxyeicosatrienoic acid by increasing of cytochrome P450 2C8, 2C9 and 2J2 and decreasing of soluble epoxide hydrolase associated with aggressiveness of human breast cancer. BMC Cancer 2014, 14, 841. [Google Scholar] [CrossRef][Green Version]
- Panigrahy, D.; Edin, M.L.; Lee, C.R.; Huang, S.; Bielenberg, D.R.; Butterfield, C.E.; Barnes, C.M.; Mammoto, A.; Mammoto, T.; Luria, A.; et al. Epoxyeicosanoids stimulate multiorgan metastasis and tumor dormancy escape in mice. J. Clin. Investig. 2012, 122, 178–191. [Google Scholar] [CrossRef]
- Yang, S.; Lin, L.; Chen, J.-X.; Lee, C.R.; Seubert, J.M.; Wang, Y.; Wang, H.; Chao, Z.-R.; Tao, D.-D.; Gong, J.-P.; et al. Cytochrome P-450 epoxygenases protect endothelial cells from apoptosis induced by tumor necrosis factor-alpha via MAPK and PI3K/Akt signaling pathways. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H142–H151. [Google Scholar] [CrossRef]
- Jiang, J.-G.; Chen, C.-L.; Card, J.W.; Yang, S.; Chen, J.-X.; Fu, X.-N.; Ning, Y.-G.; Xiao, X.; Zeldin, D.C.; Wang, D.W. Cytochrome P450 2J2 promotes the neoplastic phenotype of carcinoma cells and is up-regulated in human tumors. Cancer Res. 2005, 65, 4707–4715. [Google Scholar] [CrossRef]
- Newman, J.W.; Morisseau, C.; Hammock, B.D. Epoxide hydrolases: Their roles and interactions with lipid metabolism. Prog. Lipid Res. 2005, 44, 1–51. [Google Scholar] [CrossRef] [PubMed]
- Hammock, B.D.; Grant, D.; Storms, D. Epoxide hydrolases. Compr. Toxicol. 1997, 3, 283–305. [Google Scholar]
- Fretland, A.J.; Omiecinski, C.J. Epoxide hydrolases: Biochemistry and molecular biology. Chem. Biol. Interact. 2000, 129, 41–59. [Google Scholar] [CrossRef]
- Shen, H.C.; Hammock, B.D. Discovery of inhibitors of soluble epoxide hydrolase: A target with multiple potential therapeutic indications. J. Med. Chem. 2012, 55, 1789–1808. [Google Scholar] [CrossRef]
- Gomez, G.A.; Morisseau, C.; Hammock, B.D.; Christianson, D.W. Structure of human epoxide hydrolase reveals inferences on bifunctional catalysis in epoxide and phosphate ester hydrolysis. Biochemistry 2004, 43, 4716–4723. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Xu, F.; Huse, L.M.; Morisseau, C.; Draper, A.J.; Newman, J.W.; Parker, C.; Graham, L.; Engler, M.M.; Hammock, B.D.; et al. Soluble epoxide hydrolase regulates hydrolysis of vasoactive epoxyeicosatrienoic acids. Circ. Res. 2000, 87, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Borhan, B.; Jones, A.D.; Pinot, F.; Grant, D.F.; Kurth, M.J.; Hammock, B.D. Mechanism of Soluble Epoxide Hydrolase formation of an α-hydroxy ester-enzyme intermediate through Asp-333. J. Biol. Chem. 1995, 270, 26923–26930. [Google Scholar] [CrossRef]
- Argiriadi, M.A.; Morisseau, C.; Hammock, B.D.; Christianson, D.W. Detoxification of environmental mutagens and carcinogens: Structure, mechanism, and evolution of liver epoxide hydrolase. Proc. Natl. Acad. Sci. USA 1999, 96, 10637–10642. [Google Scholar] [CrossRef]
- Yamada, T.; Morisseau, C.; Maxwell, J.E.; Argiriadi, M.A.; Christianson, D.W.; Hammock, B.D. Biochemical evidence for the involvement of tyrosine in epoxide activation during the catalytic cycle of epoxide hydrolase. J. Biol. Chem. 2000, 275, 23082–23088. [Google Scholar] [CrossRef]
- Morisseau, C.; Hammock, B.D. Epoxide hydrolases: Mechanisms, inhibitor designs, and biological roles. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 311–333. [Google Scholar] [CrossRef]
- Schiøtt, B.; Bruice, T.C. Reaction mechanism of soluble epoxide hydrolase: Insights from molecular dynamics simulations. J. Am. Chem. Soc. 2002, 124, 14558–14570. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.W.; Subrahmanyam, R.M.; Summers, S.A.; Xiao, X.; Alkayed, N.J. Soluble epoxide hydrolase dimerization is required for hydrolase activity. J. Biol. Chem. 2013, 288, 7697–7703. [Google Scholar] [CrossRef] [PubMed]
- Node, K.; Huo, Y.; Ruan, X.; Yang, B.; Spiecker, M.; Ley, K.; Zeldin, D.C.; Liao, J.K. Anti-inflammatory properties of cytochrome P450 epoxygenase-derived eicosanoids. Science 1999, 285, 1276–1279. [Google Scholar] [CrossRef] [PubMed]
- Spector, A.A.; Norris, A.W. Action of epoxyeicosatrienoic acids on cellular function. Am. J. Physiol. Cell Physiol. 2007, 292, C996–C1012. [Google Scholar] [CrossRef] [PubMed]
- Panigrahy, D.; Greene, E.R.; Pozzi, A.; Wang, D.W.; Zeldin, D.C. EET signaling in cancer. Cancer Metastasis Rev. 2011, 30, 525–540. [Google Scholar] [CrossRef]
- Fleming, I.; Busse, R. Endothelium-derived epoxyeicosatrienoic acids and vascular function. Hypertension 2006, 47, 629–633. [Google Scholar] [CrossRef]
- Lu, T.; Hoshi, T.; Weintraub, N.L.; Spector, A.A.; Lee, H.C. Activation of ATP-sensitive K+ channels by epoxyeicosatrienoic acids in rat cardiac ventricular myocytes. J. Physiol. 2001, 53, 811–827. [Google Scholar] [CrossRef]
- Michaelis, U.R.; Fisslthaler, B.; Barbosa-Sicard, E.; Falck, J.R.; Fleming, I.; Busse, R. Cytochrome P450 epoxygenases 2C8 and 2C9 are implicated in hypoxia-induced endothelial cell migration and angiogenesis. J. Cell Sci. 2005, 118, 5489–5498. [Google Scholar] [CrossRef]
- Michaelis, U.R.; Fleming, I. From endothelium-derived hyperpolarizing factor (EDHF) to angiogenesis: Epoxyeicosatrienoic acids (EETs) and cell signaling. Pharmacol. Ther. 2006, 111, 584–595. [Google Scholar] [CrossRef]
- Michaelis, U.R.; Falck, J.R.; Schmidt, R.; Busse, R.; Fleming, I. Cytochrome P4502C9-derived epoxyeicosatrienoic acids induce the expression of cyclooxygenase-2 in endothelial cells. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 321–326. [Google Scholar] [CrossRef]
- Pozzi, A.; Macias-Perez, I.; Abair, T.; Wei, S.; Su, Y.; Zent, R.; Falck, J.R.; Capdevila, J.H. Characterization of 5, 6-and 8, 9-epoxyeicosatrienoic acids (5, 6-and 8, 9-EET) as potent in vivo angiogenic lipids. J. Biol. Chem. 2005, 280, 27138–27146. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.; Liu, Y.; Xie, L.; Wu, X.; Qiu, L.; Di, W. Sphingosine kinase 1/sphingosine-1-phosphate (S1P)/S1P receptor axis is involved in ovarian cancer angiogenesis. Oncotarget 2017, 8, 74947. [Google Scholar] [CrossRef] [PubMed]
- Pyne, N.J.; Pyne, S. Sphingosine-1-phosphate and cancer. Nat. Rev. Cancer 2010, 10, 489–503. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Chen, S.; You, B.; Sun, J. Activation of sphingosine kinase-1 mediates induction of endothelial cell proliferation and angiogenesis by epoxyeicosatrienoic acids. Cardiovasc. Res. 2008, 78, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Su, K.H.; Lee, K.I.; Shyue, S.K.; Chen, H.Y.; Wei, J.; Lee, T.S. Implication of transient receptor potential vanilloid type 1 in 14, 15-epoxyeicosatrienoic acid-induced angiogenesis. Int. J. Biol. Sci. 2014, 10, 990. [Google Scholar] [CrossRef] [PubMed]
- Lou, C.; Zhang, L.; Wang, X.; Ma, X.; Qin, C.; Li, W.; Jia, T.; Nan, Q.; Qiang, R. Soluble epoxide hydrolase: Potential target for inflammation and inflammation-driven cancer. J. Carcinog. Mutagen. 2017, 8, 1000294. [Google Scholar] [CrossRef]
- Imig, J.D.; Zhao, X.; Capdevila, J.H.; Morisseau, C.; Hammock, B.D. Soluble epoxide hydrolase inhibition lowers arterial blood pressure in angiotensin II hypertension. Hypertension 2002, 39, 690–694. [Google Scholar] [CrossRef]
- Chiamvimonvat, N.; Ho, C.M.; Tsai, H.J.; Hammock, B.D. The soluble epoxide hydrolase as a pharmaceutical target for hypertension. J. Cardiovasc. Pharmacol. 2007, 50, 225–237. [Google Scholar] [CrossRef]
- Li, J.; Carroll, M.A.; Chander, P.N.; Falck, J.R.; Sangras, B.; Stier, C.T. Soluble epoxide hydrolase inhibitor, AUDA, prevents early salt-sensitive hypertension. Front. Biosci. 2008, 13, 3480–3487. [Google Scholar] [CrossRef][Green Version]
- Liu, J.Y.; Park, S.H.; Morisseau, C.; Hwang, S.H.; Hammock, B.D.; Weiss, R.H. Sorafenib has soluble epoxide hydrolase inhibitory activity, which contributes to its effect profile In Vivo. Mol. Cancer Ther. 2009, 8, 2193–2203. [Google Scholar] [CrossRef]
- Zhang, L.N.; Vincelette, J.; Cheng, Y.; Mehra, U.; Chen, D.; Anandan, S.K.; Gless, R.; Webb, H.K.; Wang, Y.X. Inhibition of soluble epoxide hydrolase attenuated atherosclerosis, abdominal aortic aneurysm formation, and dyslipidemia. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Inceoglu, B.; Jinks, S.L.; Schmelzer, K.R.; Waite, T.; Kim, I.H.; Hammock, B.D. Inhibition of soluble epoxide hydrolase reduces LPS-induced thermal hyperalgesia and mechanical allodynia in a rat model of inflammatory pain. Life Sci. 2006, 79, 2311–2319. [Google Scholar] [CrossRef] [PubMed]
- Inceoglu, B.; Jinks, S.L.; Ulu, A.; Hegedus, C.M.; Georgi, K.; Schmelzer, K.R.; Wagner, K.; Jones, P.D.; Morisseau, C.; Hammock, B.D. Soluble epoxide hydrolase and epoxyeicosatrienoic acids modulate two distinct analgesic pathways. Proc. Natl. Acad. Sci. USA 2008, 105, 18901–18906. [Google Scholar] [CrossRef] [PubMed]
- Rose, T.E.; Morisseau, C.; Liu, J.Y.; Inceoglu, B.; Jones, P.D.; Sanborn, J.R.; Hammock, B.D. 1-Aryl-3-(1-acylpiperidin-4-yl) urea inhibitors of human and murine soluble epoxide hydrolase: Structure-Activity relationships, pharmacokinetics, and reduction of inflammatory pain. J. Med. Chem. 2010, 53, 7067–7075. [Google Scholar] [CrossRef]
- Wagner, K.M.; McReynolds, C.B.; Schmidt, W.K.; Hammock, B.D. Soluble epoxide hydrolase as a therapeutic target for pain, inflammatory and neurodegenerative diseases. Pharmacol. Ther. 2017, 180, 62–76. [Google Scholar] [CrossRef]
- Wagner, K.; Inceoglu, B.; Gill, S.S.; Hammock, B.D. Epoxygenated fatty acids and soluble epoxide hydrolase inhibition: Novel mediators of pain reduction. J. Agric. Food Chem. 2011, 59, 2816–2824. [Google Scholar] [CrossRef][Green Version]
- Ma, M.; Ren, Q.; Yang, J.; Zhang, K.; Xiong, Z.; Ishima, T.; Pu, Y.; Hwang, S.H.; Toyoshima, M.; Iwayama, Y.; et al. Key role of soluble epoxide hydrolase in the neurodevelopmental disorders of offspring after maternal immune activation. Proc. Natl. Acad. Sci. USA 2019, 116, 7083–7088. [Google Scholar] [CrossRef]
- Ren, Q.; Ma, M.; Yang, J.; Nonaka, R.; Yamaguchi, A.; Ishikawa, K.I.; Kobayashi, K.; Murayama, S.; Hwang, S.H.; Saiki, S.; et al. Soluble epoxide hydrolase plays a key role in the pathogenesis of Parkinson’s disease. Proc. Natl. Acad. Sci. USA 2018, 115, E5815–E5823. [Google Scholar] [CrossRef]
- Hashimoto, K. Role of soluble epoxide hydrolase in metabolism of PUFAs in psychiatric and neurological disorders. Front. Pharmacol. 2019, 10, 36. [Google Scholar] [CrossRef]
- Zarriello, S.; Tuazon, J.P.; Corey, S.; Schimmel, S.; Rajani, M.; Gorsky, A.; Incontri, D.; Hammock, B.D.; Borlongan, C.V. Humble beginnings with big goals: Small molecule soluble epoxide hydrolase inhibitors for treating CNS disorders. Prog. Neurobiol. 2019, 172, 23–39. [Google Scholar] [CrossRef]
- Wu, J.; Zhao, Y.; Fan, Z.; Chen, Q.; Chen, J.; Sun, Y.; Jiang, X.; Xiao, Q. Soluble epoxide hydrolase inhibitor protects against blood-brain barrier dysfunction in a mouse model of type 2 diabetes via the AMPK/HO-1 pathway. Biochem. Biophys. Res. Commun. 2020, 524. [Google Scholar] [CrossRef] [PubMed]
- Savina, Y.; Duflot, T.; Bounoure, F.; Kotzki, S.; Thiébaut, P.A.; Serreau, P.A.; Skiba, M.; Picquenot, J.M.; Cornic, M.; Morisseau, C.; et al. Impact of the acute local inhibition of soluble epoxide hydrolase on diabetic skin microcirculatory dysfunction. Diabetes Vasc. Dis. Res. 2019, 16, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Minaz, N.; Razdan, R.; Hammock, B.D.; Mujwar, S.; Goswami, S.K. Impact of diabetes on male sexual function in streptozotocin-induced diabetic rats: Protective role of soluble epoxide hydrolase inhibitor. Biomed. Pharmacother. 2019, 115, 108897. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Dziumbla, S.; Lin, J.; Bibli, S.I.; Zukunft, S.; De Mos, J.; Awwad, K.; Frömel, T.; Jungmann, A.; Devraj, K.; et al. Inhibition of soluble epoxide hydrolase prevents diabetic retinopathy. Nature 2017, 552, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Corson, T.W. Soluble epoxide hydrolase inhibition for ocular diseases: Vision for the future. Front. Pharmacol. 2019, 10, 95. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, R.S.; Park, B.; Sheik Pran Babu, S.P.; Si, Y.; Kharwadkar, R.; Mitter, S.K.; Lee, B.; Sun, W.; Qi, X.; Boulton, M.E.; et al. Chemical proteomics reveals soluble epoxide hydrolase as a therapeutic target for ocular neovascularization. ACS Chem. Biol. 2018, 13, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.H.; Park, Y.K.; Hammock, B.D.; Nishi, K. Structure-Activity relationships of cycloalkylamide derivatives as inhibitors of the soluble epoxide hydrolase. J. Med. Chem. 2011, 54, 1752–1761. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gomez, G.A.; Morisseau, C.; Hammock, B.D.; Christianson, D.W. Human soluble epoxide hydrolase: Structural basis of inhibition by 4-(3-cyclohexylureido)-carboxylic acids. Protein Sci. 2006, 15, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Eldrup, A.B.; Soleymanzadeh, F.; Taylor, S.J.; Muegge, I.; Farrow, N.A.; Joseph, D.; McKellop, K.; Man, C.C.; Kukulka, A.; De Lombaert, S. Structure-Based optimization of arylamides as inhibitors of soluble epoxide hydrolase. J. Med. Chem. 2009, 52, 5880–5895. [Google Scholar] [CrossRef] [PubMed]
- Argiriadi, M.A.; Morisseau, C.; Goodrow, M.H.; Dowdy, D.L.; Hammock, B.D.; Christianson, D.W. Binding of alkylurea inhibitors to epoxide hydrolase implicates active site tyrosines in substrate activation. J. Biol. Chem. 2000, 275, 15265–15270. [Google Scholar] [CrossRef]
- Xing, L.; McDonald, J.J.; Kolodziej, S.A.; Kurumbail, R.G.; Williams, J.M.; Warren, C.J.; O’Neal, J.M.; Skepner, J.E.; Roberds, S.L. Discovery of potent inhibitors of soluble epoxide hydrolase by combinatorial library design and structure-based virtual screening. J. Med. Chem. 2011, 54, 1211–1222. [Google Scholar] [CrossRef] [PubMed]
- Morisseau, C.; Pakhomova, S.; Hwang, S.H.; Newcomer, M.E.; Hammock, B.D. Inhibition of soluble epoxide hydrolase by fulvestrant and sulfoxides. Bioorg. Med. Chem. Lett. 2013, 23, 3818–3821. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dietze, E.C.; Kuwano, E.; Casas, J.; Hammock, B.D. Inhibition of cytosolic epoxide hydrolase by trans-3-phenylglycidols. Biochem. Pharmacol. 1991, 42, 1163–1175. [Google Scholar] [CrossRef]
- Morisseau, C.; Du, G.; Newman, J.W.; Hammock, B.D. Mechanism of mammalian soluble epoxide hydrolase inhibition by chalcone oxide derivatives. Arch. Biochem. Biophys. 1998, 356, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Asokkumar, K.; Prathyusha, L.T.; Umamaheshwari, M.; Sivashanmugam, T.; Subhadradevi, V.; Jagannath, P.; Madeswaran, A.; Salesheir, F. Design, ADMET and docking studies on some novel chalcone derivatives as soluble epoxide hydrolase enzyme inhibitors. J. Chil. Chem. Soc. 2012, 57, 1442–1446. [Google Scholar] [CrossRef][Green Version]
- Huang, S.-X.; Cao, B.; Morisseau, C.; Jin, Y.; Hammock, B.D.; Long, Y.-Q. Structure-based optimization of the piperazino-containing 1,3-disubstituted ureas affording sub-nanomolar inhibitors of soluble epoxide hydrolase. Med. Chem. Commun. 2012, 3, 379–384. [Google Scholar] [CrossRef][Green Version]
- Jones, P.D.; Hsing-Ju, T.; Zung, N.D.; Morisseau, C.; Hammock, B.D. Synthesis and SAR of conformationally restricted inhibitors of soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2006, 16, 5212–5216. [Google Scholar] [CrossRef][Green Version]
- Jones, P.D.; Wolf, N.M.; Morisseau, C.; Whetstone, P.; Hock, B.; Hammock, B.D. Fluorescent substrates for soluble epoxide hydrolase and application to inhibition studies. Anal. Biochem. 2005, 343, 66–75. [Google Scholar] [CrossRef]
- Morisseau, C.; Goodrow, M.H.; Newman, J.W.; Wheelock, C.E.; Dowdy, D.L.; Hammock, B.D. Structural refinement of inhibitors of urea-based soluble epoxide hydrolases. Biochem. Pharmacol. 2002, 63, 1599–1608. [Google Scholar] [CrossRef]
- Ulu, A.; Appt, S.; Morisseau, C.; Hwang, S.H.; Jones, P.D.; Rose, T.E.; Dong, H.; Lango, J.; Yang, J.; Tsai, H.J.; et al. Pharmacokinetics and in vivo potency of soluble epoxide hydrolase inhibitors in cynomolgus monkeys. Br. J. Pharmacol. 2012, 165, 1401–1412. [Google Scholar] [CrossRef]
- Watanabe, T.; Morisseau, C.; Newman, J.W.; Hammock, B.D. In Vitro metabolism of the mammalian soluble epoxide hydrolase inhibitor, 1-cyclohexyl-3-dodecyl-urea. Drug Metab. Dispos. 2003, 31, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Olearczyk, J.J.; Field, M.B.; Kim, I.H.; Morisseau, C.; Hammock, B.D.; Imig, J.D. Substituted adamantyl-urea inhibitors of the soluble epoxide hydrolase dilate mesenteric resistance vessels. J. Pharmacol. Exp. Ther. 2006, 318, 1307–1314. [Google Scholar] [CrossRef]
- Kim, I.H.; Morisseau, C.; Watanabe, T.; Hammock, B.D. Design, synthesis, and biological activity of 1, 3-disubstituted ureas as potent inhibitors of the soluble epoxide hydrolase of increased water solubility. J. Med. Chem. 2004, 47, 2110–2122. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.J.; Hwang, S.H.; Morisseau, C.; Yang, J.; Jones, P.D.; Kasagami, T.; Kim, I.H.; Hammock, B.D. Pharmacokinetic screening of soluble epoxide hydrolase inhibitors in dogs. Eur. J. Pharm. Sci. 2010, 40, 222–238. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wan, D.; Yang, J.; McReynolds, C.B.; Barnych, B.; Wagner, K.M.; Morisseau, C.; Hwang, S.H.; Sun, J.; Blöcher, R.; Hammock, B.D. In vitro and in vivo metabolism of a potent inhibitor of soluble epoxide hydrolase, 1-(1-propionylpiperidin-4-yl)-3-(4-(trifluoromethoxy) phenyl) urea. Front. Pharmacol. 2019, 10, 464. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Whitcomb, R.; MacIntyre, E.; Tran, V.; Do, Z.N.; Sabry, J.; Patel, D.V.; Anandan, S.K.; Gless, R.; Webb, H.K. Pharmacokinetics and pharmacodynamics of AR9281, an inhibitor of soluble epoxide hydrolase, in single- and multiple-dose studies in healthy human subjects. J. Clin. Pharmacol. 2012, 52, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Sun, G.Y.; Liu, T.; Duan, J.X.; Zhou, H.F.; Lee, K.S.; Hammock, B.D.; Fang, X.; Jiang, J.X.; Guan, C.X. Soluble epoxide hydrolase inhibitor 1-trifluoromethoxyphenyl-3-(1-propionylpiperidin-4-yl) urea attenuates bleomycin-induced pulmonary fibrosis in mice. Cell Tissue Res. 2016, 363, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Eldrup, A.B.; Soleymanzadeh, F.; Farrow, N.A.; Kukulka, A.; De Lombaert, S. Optimization of piperidyl-ureas as inhibitors of soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2010, 20, 571–575. [Google Scholar] [CrossRef]
- Shen, H.C.; Ding, F.X.; Wang, S.; Deng, Q.; Zhang, X.; Chen, Y.; Zhou, G.; Xu, S.; Chen, H.S.; Tong, X.; et al. Discovery of a highly potent, selective, and bioavailable soluble epoxide hydrolase inhibitor with excellent ex vivo target engagement. J. Med. Chem. 2009, 52, 5009–5012. [Google Scholar] [CrossRef]
- Shen, H.C.; Ding, F.X.; Wang, S.; Xu, S.; Chen, H.S.; Tong, X.; Tong, V.; Mitra, K.; Kumar, S.; Zhang, X.; et al. Discovery of spirocyclic secondary amine-derived tertiary ureas as highly potent, selective and bioavailable soluble epoxide hydrolase inhibitors. Bioorg. Med. Chem. Lett. 2009, 19, 3398–3404. [Google Scholar] [CrossRef]
- Burmistrov, V.V.; Butov, G.M. Synthesis and properties of N-[R-adamantan-1 (2)-yl]-N′-(2-fluorophenyl) ureas—Target-Oriented soluble epoxide hydrolase inhibitors. Russ. J. Org. Chem. 2018, 54, 1307–1312. [Google Scholar] [CrossRef]
- Burmistrov, V.V.; Morisseau, C.; Karlov, D.; Pitushkin, D.; Vernigora, A.; Rasskazova, E.; Butov, G.M.; Hammock, B.D. Bioisosteric substitution of adamantane with bicyclic lipophilic groups improves water solubility of human soluble epoxide hydrolase inhibitors. Bioorg. Med. Chem. Lett. 2020, 30, 127430. [Google Scholar] [CrossRef] [PubMed]
- Codony, S.; Pujol, E.; Pizarro, J.; Feixas, F.; Valverde, E.; Loza, M.I.; Brea, J.M.; Saez, E.; Oyarzabal, J.; Pineda-Lucena, A.; et al. 2-Oxaadamant-1-yl Ureas as soluble epoxide hydrolase inhibitors: In Vivo evaluation in a murine model of acute pancreatitis. J. Med. Chem. 2020, 63, 9237–9257. [Google Scholar] [CrossRef] [PubMed]
- Waltenberger, B.; Garscha, U.; Temml, V.; Liers, J.; Werz, O.; Schuster, D.; Stuppner, H. Discovery of potent soluble epoxide hydrolase (sEH) inhibitors by pharmacophore-based virtual screening. J. Chem. Inf. Model. 2016, 56, 747–762. [Google Scholar] [CrossRef] [PubMed]
- Rezaee, E.; Hedayati, M.; Rad, L.H.; Shahhosseini, S.; Faizi, M.; Tabatabai, S.A. Novel soluble epoxide hydrolase inhibitors with a dihydropyrimidinone scaffold: Design, synthesis and biological evaluation. Med. Chem. Commun. 2016, 7, 2128–2135. [Google Scholar] [CrossRef]
- Lazaar, A.L.; Yang, L.; Boardley, R.L.; Goyal, N.S.; Robertson, J.; Baldwin, S.J.; Newby, D.E.; Wilkinson, I.B.; Tal-Singer, R.; Mayer, R.J.; et al. Pharmacokinetics, pharmacodynamics and adverse event profile of GSK2256294, a novel soluble epoxide hydrolase inhibitor. Br. J. Clin. Pharmacol. 2016, 81, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, N.; Paliwal, S.; Sharma, S.; Verma, K.; Gururani, R.; Tiwari, A.; Verma, A.; Chauhan, M.; Singh, A.; Kumar, D.; et al. Discovery of novel soluble epoxide hydrolase inhibitors as potent vasodilators. Sci. Rep. 2018, 8, 14604. [Google Scholar] [CrossRef]
- Batchu, S.N.; Lee, S.B.; Samokhvalov, V.; Chaudhary, K.R.; El-Sikhry, H.; Weldon, S.M.; Seubert, J.M. Novel soluble epoxide hydrolase inhibitor protects mitochondrial function following stress. Can. J. Physiol. Pharmacol. 2012, 90, 811–823. [Google Scholar] [CrossRef]
- Kim, I.H.; Heirtzler, F.R.; Morisseau, C.; Nishi, K.; Tsai, H.J.; Hammock, B.D. Optimization of amide-based inhibitors of soluble epoxide hydrolase with improved water solubility. J. Med. Chem. 2005, 48, 3621–3629. [Google Scholar] [CrossRef]
- Anandan, S.K.; Webb, H.K.; Do, Z.N.; Gless, R.D. Unsymmetrical non-adamantyl N, N′-diaryl urea and amide inhibitors of soluble expoxide hydrolase. Bioorg. Med. Chem. Lett. 2009, 19, 4259–4263. [Google Scholar] [CrossRef]
- Rezaee, E.; Amrolah, S.M.; Nazari, M.; Tabatabi, S.A. Novel amide derivatives of 3-phenylglutaric acid as potent soluble epoxide hydrolase inhibitors. Mol. Divers. 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pecic, S.; Deng, S.-X.; Morisseau, C.; Hammock, B.D.; Landry, D.W. Design, synthesis and evaluation of non-urea inhibitors of soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2012, 22, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Liu, Y.; Gong, G.; Smith, D.H.; Yan, F.; Rinderspacher, A.; Feng, Y.; Zhu, Z.; Li, X.; Deng, S.X.; et al. Discovery of potent non-urea inhibitors of soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2009, 19, 2354–2359. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pecic, S.; Pakhomova, S.; Newcomer, M.E.; Morisseau, C.; Hammock, B.D.; Zhu, Z.; Rinderspacher, A.; Deng, S.-X. Synthesis and structure-activity relationship of piperidine-derived non-urea soluble epoxide hydrolase inhibitors. Bioorg. Med. Chem. Lett. 2013, 23, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.C.; Ding, F.X.; Deng, Q.; Xu, S.; Tong, X.; Zhang, X.; Chen, Y.; Zhou, G.; Pai, L.Y.; Alonso-Galicia, M.; et al. A strategy of employing aminoheterocycles as amide mimics to identify novel, potent and bioavailable soluble epoxide hydrolase inhibitors. Bioorg. Med. Chem. Lett. 2009, 19, 5716–5721. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Ma, W.H.; Ma, Y.L.; Ban, S.R.; Feng, X.E.; Li, Q.S. Synthesis and biological activity of 4-substituted benzoxazolone derivatives as a new class of sEH inhibitors with high anti-inflammatory activity in vivo. Bioorg. Med. Chem. Lett. 2013, 23, 2380–2383. [Google Scholar] [CrossRef]
- Schmelzer, K.R.; Kubala, L.; Newman, J.W.; Kim, I.H.; Eiserich, J.P.; Hammock, B.D. Soluble epoxide hydrolase is a therapeutic target for acute inflammation. Proc. Natl. Acad. Sci. USA 2005, 102, 9772–9777. [Google Scholar] [CrossRef]
- Burmistrov, V.V.; Morisseau, C.; Pitushkin, D.; Karlov, D.; Fayzullin, R.R.; Butov, G.M.; Hammock, B.D. Adamantyl thioureas as soluble epoxide hydrolase inhibitors. Bioorg. Med. Chem. Lett. 2018, 28, 2302–2313. [Google Scholar] [CrossRef]
- Bhagwati, S.; Siddiqui, M.I. Identification of potential soluble epoxide hydrolase (sEH) inhibitors by ligand-based pharmacophore model and biological evaluation. J. Biomol. Struct. Dyn. 2019, 38, 4956–4966. [Google Scholar] [CrossRef]
- Tanaka, D.; Tsuda, Y.; Shiyama, T.; Nishimura, T.; Chiyo, N.; Tominaga, Y.; Sawada, N.; Mimoto, T.; Kusunose, N. A practical use of ligand efficiency indices out of the fragment-based approach: Ligand efficiency-guided lead identification of soluble epoxide hydrolase inhibitors. J. Med. Chem. 2011, 54, 851–857. [Google Scholar] [CrossRef]
- Amano, Y.; Yamaguchi, T.; Tanabe, E. Structural insights into binding of inhibitors to soluble epoxide hydrolase gained by fragment screening and X-ray crystallography. Bioorg. Med. Chem. 2014, 22, 2427–2434. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.S.; Liu, J.-Y.; Wagner, K.M.; Pakhomova, S.; Dong, H.; Morisseau, C.; Fu, S.H.; Yang, J.; Wang, P.; Ulu, A.; et al. Optimized Inhibitors of soluble epoxide hydrolase improve in vitro target residence time and in vivo efficacy. J. Med. Chem. 2014, 57, 7016–7030. [Google Scholar] [CrossRef] [PubMed]
- Lukin, A.; Kramer, J.; Hartmann, M.; Weizel, L.; Hernandez-Olmos, V.; Falahati, K.; Burghardt, I.; Kalinchenkova, N.; Bagnyukova, D.; Zhurilo, N.; et al. Discovery of polar spirocyclic orally bioavailable urea inhibitors of soluble epoxide hydrolase. Bioorg. Chem. 2018, 80, 655–667. [Google Scholar] [CrossRef] [PubMed]
- Thalji, R.K.; McAtee, J.J.; Belyanskaya, S.; Brandt, M.; Brown, G.D.; Costell, M.H.; Ding, Y.; Dodson, J.W.; Eisennagel, S.H.; Fries, R.E.; et al. Discovery of 1-(1, 3, 5-triazin-2-yl) piperidine-4-carboxamides as inhibitors of soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2013, 23, 3584–3588. [Google Scholar] [CrossRef]
- Lo, H.Y.; Man, C.C.; Fleck, R.W.; Farrow, N.A.; Ingraham, R.H.; Kukulka, A.; Proudfoot, J.R.; Betageri, R.; Kirrane, T.; Patel, U.; et al. Substituted pyrazoles as novel sEH antagonist: Investigation of key binding interactions within the catalytic domain. Bioorg. Med. Chem. Lett. 2010, 20, 6379–6383. [Google Scholar] [CrossRef]
- Scholz, M.S.; Wingen, L.M.; Brunst, S.; Wittman, S.; Cardoso, I.L.A.; Weizel, L.; Proschak, E. Soluble epoxide hydrolase inhibitors with carboranes as non-natural 3-D pharmacophores. Eur. J. Med. Chem. 2020, 185, 111766. [Google Scholar] [CrossRef]
- Vinh, L.B.; Kim, J.H.; Lee, J.S.; Nguyet, N.T.M.; Yang, S.Y.; Ma, J.Y.; Kim, Y.H. Soluble epoxide hydrolase inhibitory activity of phenolic glycosides from Polygala tenuifolia and in silico approach. Med. Chem. Res. 2018, 27, 726–734. [Google Scholar] [CrossRef]
- Liu, J.Y.; Morisseau, C.; Huang, H.; Hammock, B.D. Screening of soluble epoxide hydrolase inhibitory ingredients from traditional Chinese medicines for anti-inflammatory use. J. Ethnopharmacol. 2016, 194, 475–482. [Google Scholar] [CrossRef]
- Kitamura, S.; Morisseau, C.; Inceoglu, B.; Kamita, S.G.; De Nicola, G.R.; Nyegue, M.; Hammock, B.D. Potent natural soluble epoxide hydrolase inhibitors from Pentadiplandra brazzeana Baillon: Synthesis, quantification, and measurement of biological activities in vitro and in vivo. PLoS ONE 2015, 10, e0117438. [Google Scholar] [CrossRef]
- Thao, N.P.; Kim, J.H.; Luyen, B.T.T.; Dat, N.T.; Kim, Y.H. In silico investigation of cycloartane triterpene derivatives from Cimicifuga dahurica (Turcz.) Maxim. roots for the development of potent soluble epoxide hydrolase inhibitors. Int. J. Biol. Macromol. 2017, 98, 526–534. [Google Scholar] [CrossRef]
- Buscató, E.L.; Büttner, D.; Brüggerhoff, A.; Klingler, F.M.; Weber, J.; Scholz, B.; Živković, A.; Marschalek, R.; Stark, H.; Steinhilber, D.; et al. From a multipotent stilbene to soluble epoxide hydrolase inhibitors with antiproliferative properties. ChemMedChem 2013, 8, 919–923. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, I.S.; Ryu, J.; Lee, J.S.; Kang, J.S.; Kang, S.Y.; Kim, Y.H. In vitro and in silico investigation of anthocyanin derivatives as soluble epoxide hydrolase inhibitors. Int. J. Biol. Macromol. 2018, 112, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.H.; Oh, S.J.; Lee, S.Y.; Lee, Y.-J.; Ma, J.Y.; Kim, Y.H.; Kim, S.K. Discovery of soluble epoxide hydrolase inhibitors from natural products. Food Chem. Toxicol. 2014, 64, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.Y.; Kim, J.H.; Choi, S.-K.; Kim, Y.H. Constituents of the seeds of Cassia tora with inhibitory activity on soluble epoxide hydrolase. Bioorg. Med. Chem. Lett. 2015, 25, 5097–5101. [Google Scholar] [CrossRef] [PubMed]
- Jo, A.R.; Kim, J.H.; Yan, X.-T.; Yang, S.Y.; Kim, Y.H. Soluble epoxide hydrolase inhibitory components from Rheum undulatum and in silico approach. J. Enzym. Inhib. Med. Chem. 2016, 31, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Cho, C.W.; Tai, B.H.; Yang, S.Y.; Choi, G.-S.; Kang, J.S.; Kim, Y.H. Soluble epoxide hydrolase inhibitory activity of selaginellin derivatives from Selaginella tamariscina. Molecules 2015, 20, 21405–21414. [Google Scholar] [CrossRef]
- Kim, J.H.; Morgan, A.M.A.; Tai, B.H.; Van, D.T.; Cuong, N.M.; Kim, Y.H. Inhibition of soluble epoxide hydrolase activity by compounds isolated from the aerial parts of Glycosmis stenocarpa. J. Enzym. Inhib. Med. Chem. 2016, 31, 640–644. [Google Scholar] [CrossRef]
- He, X.; Zhao, W.-Y.; Shao, B.; Zhang, B.-J.; Liu, T.-T.; Sun, C.-P.; Huang, H.-L.; Wu, J.-R.; Liang, J.-H.; Ma, X.-C. Natural soluble epoxide hydrolase inhibitors from Inula helenium and their interactions with soluble epoxide hydrolase. Int. J. Biol. Macromol. 2020, 158, 1362–1368. [Google Scholar] [CrossRef]
- Su, X.D.; Li, W.; Kim, J.E.; Yang, S.Y.; Ma, J.Y.; Kim, Y.H. Prenyl-flavonoids from Epimedium koreanum Nakai and their soluble epoxide hydrolase and tyrosinase inhibitory activities. Med. Chem. Res. 2017, 26, 2761–2767. [Google Scholar]
- Li, H.X.; Heo, M.; Go, Y.; Kim, Y.S.; Kim, Y.H.; Yang, S.Y.; Li, W. Coumarin and moracin derivatives from mulberry leaves (Morus alba L.) with soluble epoxide hydrolase inhibitory activity. Molecules 2020, 25, 3967. [Google Scholar] [CrossRef]
- Sun, C.-P.; Zhang, J.; Zhao, W.-Y.; Yi, J.; Yan, J.-K.; Wang, Y.-L.; Morisseau, C.; Liu, Z.-B.; Hammock, B.D.; Ma, X.-C. Protostane-Type triterpenoids as natural soluble epoxide hydrolase inhibitors: Inhibition potentials and molecular dynamics. Bioorg. Chem. 2020, 96, 103637. [Google Scholar] [CrossRef] [PubMed]
- Falck, J.R.; Kodela, R.; Manne, R.; Atcha, K.R.; Puli, N.; Dubasi, N.; Manthati, V.L.; Capdevila, J.H.; Yi, X.Y.; Goldman, D.H.; et al. 14,15-Epoxyeicosa-5,8,11-trienoic acid (14,15-EET) surrogates containing epoxide bioisosteres: Influence upon vascular relaxation and soluble epoxide hydrolase inhibition. J. Med. Chem. 2009, 52, 5069–5075. [Google Scholar] [CrossRef]
- Falck, J.R.; Koduru, S.R.; Mohapatra, S.; Manne, R.; Atcha, R.; Manthati, V.L.; Capdevila, J.H.; Christian, S.; Imig, J.D.; Campbell, W.B. 14,15-Epoxyeicosa-5,8,11-trienoic acid (14,15-EET) surrogates: Carboxylate modifications. J. Med. Chem. 2014, 57, 6965–6972. [Google Scholar] [CrossRef] [PubMed]
- Litovchick, A.; Dumelin, C.E.; Habeshian, S.; Gikunju, D.; Guie, M.A.; Centrella, P.; Zhang, Y.; Sigel, E.A.; Cuozzo, J.W.; Keefe, A.D.; et al. Encoded library synthesis using chemical ligation and the discovery of sEH inhibitors from a 334-million member library. Sci. Rep. 2015, 5, 10916. [Google Scholar] [CrossRef] [PubMed]
- Belyanskaya, S.L.; Ding, Y.; Callahan, J.F.; Lazaar, A.L.; Israel, D.I. Discovering drugs with DNA-encoded library technology: From concept to clinic with an inhibitor of soluble epoxide hydrolase. ChemBioChem 2017, 18, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Abis, G.; Charles, R.L.; Kopec, J.; Yue, W.W.; Atkinson, R.A.; Bui, T.T.; Lynham, S.; Popova, S.; Sun, Y.B.; Fraternali, F.; et al. 15-deoxy-Δ 12, 14-Prostaglandin J 2 inhibits human soluble epoxide hydrolase by a dual orthosteric and allosteric mechanism. Commun. Biol. 2019, 2, 188. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Panigrahy, D.; Hwang, S.H.; Yang, J.; Mahakian, L.M.; Wettersten, H.I.; Liu, J.Y.; Wang, Y.; Ingham, E.S.; Tam, S.; et al. Dual inhibition of cyclooxygenase-2 and soluble epoxide hydrolase synergistically suppresses primary tumor growth and metastasis. Proc. Natl. Acad. Sci. USA 2014, 111, 11127–11132. [Google Scholar] [CrossRef]
- Jones, R.D.; Liao, J.; Tong, X.; Xu, D.; Sun, L.; Li, H.; Yang, G.Y. Epoxy-Oxylipins and soluble epoxide hydrolase metabolic pathway as targets for NSAID-induced gastroenteropathy and inflammation-associated carcinogenesis. Front. Pharmacol. 2019, 10, 731. [Google Scholar] [CrossRef]
- Schmelzer, K.R.; Inceoglu, B.; Kubala, L.; Kim, I.H.; Jinks, S.L.; Eiserich, J.P.; Hammock, B.D. Enhancement of antinociception by coadministration of nonsteroidal anti-inflammatory drugs and soluble epoxide hydrolase inhibitors. Proc. Natl. Acad. Sci. USA 2006, 103, 13646–13651. [Google Scholar] [CrossRef]
- Wagner, K.; Inceoglu, B.; Hammock, B.D. Soluble epoxide hydrolase inhibition, epoxygenated fatty acids and nociception. Prostaglandins Other Lipid Mediat. 2011, 96, 76–83. [Google Scholar] [CrossRef]
- Goswami, S.K.; Wan, D.; Yang, J.; Da Silva, C.A.T.; Morisseau, C.; Kodani, S.D.; Yang, G.Y.; Inceoglu, B.; Hammock, B.D. Anti-Ulcer efficacy of soluble epoxide hydrolase inhibitor TPPU on diclofenac-induced intestinal ulcers. J. Pharmacol. Exp. Ther. 2016, 357, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Wagner, K.M.; Morisseau, C.; Liu, J.Y.; Dong, H.; Wecksler, A.T.; Hammock, B.D. Synthesis and structure-activity relationship studies of urea-containing pyrazoles as dual inhibitors of cyclooxygenase-2 and soluble epoxide hydrolase. J. Med. Chem. 2011, 54, 3037–3050. [Google Scholar] [CrossRef] [PubMed]
- Abdelazeem, A.H.; Safi El-Din, A.G.; Abdel-Fattah, M.M.; Amin, N.H.; El-Moghazy, S.M.; El-Saadi, M.T. Discovery of novel urea-diarylpyrazole hybrids as dual COX-2/sEH inhibitors with improved anti-inflammatory activity and highly reduced cardiovascular risks. Eur. J. Med. Chem. 2020, 205, 112662. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.-Y.; Yang, J.; Inceoglu, B.; Qiu, H.; Ulu, A.; Hwang, S.-H.; Chiamvimonvat, N.; Hammock, B.D. Inhibition of soluble epoxide hydrolase enhances the anti-inflammatory effects of aspirin and 5-lipoxygenase activation protein inhibitor in a murine model. Biochem. Pharmacol. 2010, 79, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Garscha, U.; Romp, E.; Pace, S.; Rossi, A.; Temml, V.; Schuster, D.; Konig, S.; Gerstmeier, J.; Liening, S.; Werner, M.; et al. Pharmacological profile and efficiency in vivo of diflapolin, the first dual inhibitor of 5-lipoxygenase-activating protein and soluble epoxide hydrolase. Sci. Rep. 2017, 7, 9398. [Google Scholar] [CrossRef]
- Temml, V.; Garscha, U.; Romp, E.; Schubert, G.; Gerstmeier, J.; Kutil, Z.; Matuszczak, B.; Waltenberger, B.; Stuppner, H.; Werz, O.; et al. Discovery of the first dual inhibitor of the 5-lipoxygenase-activating protein and soluble epoxide hydrolase using pharmacophore-based virtual screening. Sci. Rep. 2017, 7, 42751. [Google Scholar] [CrossRef]
- Hiesinger, K.; Schott, A.; Kramer, J.S.; Blocher, R.; Witt, F.; Wittman, S.K.; Steinhilber, D.; Pogoryelov, D.; Gerstmeier, J.; Werz, O.; et al. Design of dual inhibitors of soluble epoxide hydrolase and LTA4 hydrolase. ACS Med. Chem. Lett. 2020, 11, 298–302. [Google Scholar] [CrossRef]
- Hefke, L.; Hiesinger, K.; Zhu, W.F.; Kramer, J.S.; Proschak, E. Computer-Aided fragment growing strategies to design dual inhibitors of soluble epoxide hydrolase and LTA4 hydrolase. ACS Med. Chem. Lett. 2020, 11, 1244–1249. [Google Scholar] [CrossRef]
- Moser, D.; Wisniewska, J.M.; Hahn, S.; Achenback, J.; Buscato, E.; Klingler, F.-M.; Hofmann, B.; Steinhilber, D.; Proschak, E. Dual-Target virtual screening by pharmacophore elucidation and molecular shape filtering. ACS Med. Chem. Lett. 2012, 3, 155–158. [Google Scholar] [CrossRef]
- Nandha, B.; Ramareddy, S.A.; Hazra, K. Synthesis of substituted fluorobenzimidazoles as inhibitors of 5-lipoxygenase and soluble epoxide hydrolase for anti-inflammatory activity. Arch. Pharm. 2018, 351, 1800030. [Google Scholar] [CrossRef]
- Meirer, K.; Rodl, C.B.; Wisniewska, J.M.; George, S.; Hafner, A.-K.; Buscato, E.; Klingler, F.-M.; Hahn, S.; Berressem, D.; Wittmann, S.K.; et al. Synthesis and structure-activity relationship studies of novel dual inhibitors of soluble epoxide hydrolase and 5-lipoxygenase. J. Med. Chem. 2013, 56, 1777–1781. [Google Scholar] [CrossRef] [PubMed]
- Achenback, J.; Klingler, F.-M.; Blocher, R.; Moser, D.; Hafner, A.K.; Rodl, C.B.; Kretschmer, S.; Kruger, B.; Lohr, F.; Stark, H.; et al. Exploring the chemical space of multitarget ligands using self-organizing maps. ACS Med. Chem. Lett. 2013, 4, 1169–1172. [Google Scholar] [CrossRef] [PubMed]
- Meirer, K.; Glatzel, D.; Kretschmer, S.; Wittmann, S.K.; Hartmann, M.; Blocher, R.; Angioni, C.; Geisslinger, G.; Steinhilber, D.; Hofmann, B.; et al. Design, synthesis and cellular characterization of a dual inhibitor of 5-lipoxygenase and soluble epoxide hydrolase. Molecules 2017, 22, 45. [Google Scholar] [CrossRef] [PubMed]
- Kodani, S.D.; Bhakta, S.; Hwang, S.H.; Pakhomova, S.; Newcomer, M.E.; Morisseau, C.; Hammock, B.D. Identification and optimization of soluble epoxide hydrolase inhibitors with dual potency towards fatty acid amide hydrolase. Bioorg. Med. Chem. Lett. 2018, 28, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Kodani, S.D.; Wan, D.; Wagner, K.M.; Hwang, S.H.; Morisseau, C.; Hammock, B.D. Design and potency of dual soluble epoxide hydrolase/fatty acid amide hydrolase inhibitors. ACS Omega 2018, 3, 14076–14086. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Zhang, B.; Xu, M.; Morisseau, C.; Hwang, S.H.; Hammock, B.D.; Li, Q.X. 1-Trifluoromethoxyphenyl-2-(1-propionylpiperidin-4-yl) urea, a selective and potent dual inhibitor of soluble epoxide hydrolase and p38 kinase intervenes in Alzheimer’s signaling in human nerve cells. ACS Chem. Neurosci. 2019, 10, 4018–4030. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.; Rotter, M.; Weiser, T.; Wittmann, S.; Weizel, L.; Kaiser, A.; Heering, J.; Goebel, T.; Angioni, C.; Wurglics, M.; et al. A dual modulator of farnesoid X receptor and soluble epoxide hydrolase to counter nonalcoholic steatohepatitis. J. Med. Chem. 2017, 60, 7703–7724. [Google Scholar] [CrossRef] [PubMed]
- Schierle, S.; Helmstadter, M.; Schmidt, J.; Hartmann, M.; Horz, M.; Kaiser, A.; Weizel, L.; Heitel, P.; Proschak, A.; Hernandez-Olmos, V.; et al. Dual farnesoid X receptor/soluble epoxide hydrolase modulators derived from Zafirlukast. ChemMedChem 2020, 15, 50–67. [Google Scholar] [CrossRef]
- Inceoglu, B.; Wagner, K.; Schebb, N.H.; Morisseau, C.; Jinks, S.L.; Ulu, A.; Hegedus, C.; Rose, T.; Brosnan, R.; Hammock, B.D. Analgesia mediated by soluble epoxide hydrolase inhibitors is dependent on cAMP. Proc. Natl. Acad. Sci. USA 2011, 108, 5093–5097. [Google Scholar] [CrossRef]
- Blocher, R.; Wagner, K.M.; Gopireddy, R.R.; Harris, T.R.; Wu, H.; Barnych, B.; Hwang, S.H.; Xiang, Y.K.; Proschak, E.; Morisseau, C.; et al. Orally available soluble epoxide hydrolase/phosphodiesterase 4 dual inhibitor treats inflammatory pain. J. Med. Chem. 2018, 26, 3541–3550. [Google Scholar] [CrossRef]
- Roca, H.; Jones, J.D.; Purica, M.C.; Weidner, S.; Koh, A.J.; Kuo, R.; Wilkinson, J.E.; Wang, Y.; Daignault-Newton, S.; Pienta, K.J.; et al. Apoptosis-induced CXCL5 accelerates inflammation and growth of prostate tumor metastases in bone. J. Clin. Investig. 2018, 128, 248–266. [Google Scholar] [CrossRef] [PubMed]
- Stanford, J.C.; Young, C.; Hicks, D.; Owens, P.; Williams, A.; Vaught, D.B.; Morrison, M.M.; Lim, J.; Williams, M.; Brantley-Sieders, D.M.; et al. Efferocytosis produces a prometastatic landscape during postpartum mammary gland involution. J. Clin. Investig. 2014, 124, 4737–4752. [Google Scholar] [CrossRef] [PubMed]
- Park, S.I.; Liao, J.; Berry, J.E.; Li, X.; Koh, A.J.; Michalski, M.E.; Eber, M.R.; Soki, F.N.; Sadler, D.; Sud, S.; et al. Cyclophosphamide creates a receptive microenvironment for prostate cancer skeletal metastasis. Cancer Res. 2012, 72, 2522–2532. [Google Scholar] [CrossRef] [PubMed]
- Gartung, A.; Yang, J.; Sukhatme, V.P.; Bielenberg, D.R.; Fernandes, D.; Chang, J.; Schmidt, B.A.; Hwang, S.H.; Zurakowski, D.; Huang, S.; et al. Suppression of chemotherapy-induced cytokine/lipid mediator surge and ovarian cancer by a dual COX-2/sEH inhibitor. Proc. Natl. Acad. Sci. USA 2019, 116, 1698–1703. [Google Scholar] [CrossRef]
- Ho, G.Y.; Woodward, N.; Coward, J.I. Cisplatin versus carboplatin: Comparative review of therapeutic management in solid malignancies. Crit. Rev. Oncol. Hematol. 2016, 102, 37–46. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, H.; Ma, A.H.; Yu, W.; Zimmermann, M.; Yang, J.; Hwang, S.H.; Zhu, D.; Lin, T.Y.; Malfatti, M.; et al. COX-2/sEH dual inhibitor PTUPB potentiates the antitumor efficacy of cisplatin. Mol. Cancer Ther. 2018, 17, 474–483. [Google Scholar] [CrossRef]
- Ghosh, N.; Chaki, R.; Mandal, V.; Mandal, S.C. COX-2 as a target for cancer chemotherapy. Pharmacol. Rep. 2010, 62, 233–244. [Google Scholar] [CrossRef]
- Gridelli, C.; Gallo, C.; Ceribelli, A.; Gebbia, V.; Gamucci, T.; Ciardiello, F.; Carozza, F.; Favaretto, A.; Daniele, B.; Galetta, D.; et al. Factorial phase III randomised trial of rofecoxib and prolonged constant infusion of gemcitabine in advanced non-small-cell lung cancer: The GEmcitabine-COxib in NSCLC (GECO) study. Lancet Oncol. 2007, 8, 500–512. [Google Scholar] [CrossRef]
- Pan, C.X.; Loehrer, P.; Seitz, D.; Helft, P.; Juliar, B.; Ansari, R.; Pletcher, W.; Vinson, J.; Cheng, L.; Sweeney, C. A phase II trial of irinotecan, 5-fluorouracil and leucovorin combined with celecoxib and glutamine as first-line therapy for advanced colorectal cancer. Oncology 2005, 69, 63–70. [Google Scholar] [CrossRef]
- Lowenfels, A.B.; Maisonneuve, P.; Cavallini, G.; Ammann, R.W.; Lankisch, P.G.; Andersen, J.R.; Dimagno, E.P.; Andren-Sandberg, A.; Domellof, L.; Group, I.P.S. Pancreatitis and the risk of pancreatic cancer. N. Engl. J. Med. 1993, 328, 1433–1437. [Google Scholar] [CrossRef]
- Hingorani, S.R.; Wang, L.; Multani, A.S.; Combs, C.; Deramaudt, T.B.; Hruban, R.H.; Rustgi, A.K.; Chang, S.; Tuveson, D.A. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 2005, 7, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Pylayeva-Gupta, Y.; Grabocka, E.; Bar-Sagi, D. RAS oncogenes: Weaving a tumorigenic web. Nat. Rev. Cancer 2011, 11, 761–774. [Google Scholar] [CrossRef] [PubMed]
- Blasco, R.B.; Francoz, S.; Santamaría, D.; Cañamero, M.; Dubus, P.; Charron, J.; Baccarini, M.; Barbacid, M. C-Raf, but not B-Raf, is essential for development of K-Ras oncogene-driven non-small cell lung carcinoma. Cancer Cell 2011, 19, 652–663. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Hwang, S.H.; Li, H.; Liu, J.Y.; Hammock, B.D.; Yang, G.Y. Inhibition of chronic pancreatitis and murine pancreatic intraepithelial neoplasia by a dual inhibitor of c-RAF and soluble epoxide hydrolase in LSL-KrasG12D/Pdx-1-Cre mice. Anticancer Res. 2016, 36, 27–37. [Google Scholar]
- Zhang, G.; Panigrahy, D.; Mahakian, L.M.; Yang, J.; Liu, J.Y.; Lee, K.S.S.; Wettersten, H.I.; Ulu, A.; Hu, X.; Tam, S.; et al. Epoxy metabolites of docosahexaenoic acid (DHA) inhibit angiogenesis, tumor growth, and metastasis. Proc. Natl. Acad. Sci. USA 2013, 110, 6530–6535. [Google Scholar] [CrossRef]
- Morin, C.; Sirois, M.; Échavé, V.; Albadine, R.; Rousseau, E. 17, 18-Epoxyeicosatetraenoic acid targets PPARγ and p38 mitogen-activated protein kinase to mediate its anti-inflammatory effects in the lung: Role of soluble epoxide hydrolase. Am. J. Respir. Cell Mol. Biol. 2010, 43, 564–575. [Google Scholar] [CrossRef]
- Kubota, T.; Arita, M.; Isobe, Y.; Iwamoto, R.; Goto, T.; Yoshioka, T.; Urabe, D.; Inoue, M.; Arai, H. Eicosapentaenoic acid is converted via ω-3 epoxygenation to the anti-inflammatory metabolite 12-hydroxy-17, 18-epoxyeicosatetraenoic acid. FASEB J. 2014, 28, 586–593. [Google Scholar] [CrossRef]
- Xia, R.; Sun, L.; Liao, J.; Li, H.; You, X.; Xu, D.; Yang, J.; Hwang, S.H.; Jones, R.D.; Hammock, B.; et al. Inhibition of pancreatic carcinoma growth through enhancing ω-3 Epoxy polyunsaturated fatty acid profile by inhibition of soluble epoxide hydrolase. Anticancer Res. 2019, 39, 3651–3660. [Google Scholar] [CrossRef]
- Freitas, R.D.; Campos, M.M. Protective effects of omega-3 fatty acids in cancer-related complications. Nutrients 2019, 11, 945. [Google Scholar] [CrossRef]
- Dong, X.W.; Jia, Y.L.; Jiang, B.; Jiang, J.X.; Shen, J.; Jin, Y.C.; Guan, Y.; Sun, Y.; Xie, Q.M. Soluble epoxide hydrolase inhibitor AUDA decreases bleomycin-induced pulmonary toxicity in mice by inhibiting the p38/Smad3 pathways. Toxicology 2017, 389, 31–41. [Google Scholar] [CrossRef]
- Li, J.; Liu, H.; Xing, B.; Yu, Y.; Wang, H.; Chen, G.; Gu, B.; Zhang, G.; Wei, D.; Gu, P.; et al. t-AUCB, an improved sEH inhibitor, suppresses human glioblastoma cell growth by activating NF-κB-p65. J. Neuro Oncol. 2012, 108, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; DuBois, R.N. Eicosanoids and cancer. Nat. Rev. Cancer 2010, 10, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Yang, J.; Zhang, J.; Wang, Y.; Hwang, S.H.; Qi, W.; Wan, D.; Kim, D.; Sun, J.; Sanidad, K.Z.; et al. Lipidomic profiling reveals soluble epoxide hydrolase as a therapeutic target of obesity-induced colonic inflammation. Proc. Natl. Acad. Sci. USA 2018, 115, 5283–5288. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Wecksler, A.T.; Zhang, G.; Morisseau, C.; Nguyen, L.V.; Fu, S.H.; Hammock, B.D. Synthesis and biological evaluation of sorafenib-and regorafenib-like sEH inhibitors. Bioorg. Med. Chem. Lett. 2013, 23, 3732–3737. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das Mahapatra, A.; Choubey, R.; Datta, B. Small Molecule Soluble Epoxide Hydrolase Inhibitors in Multitarget and Combination Therapies for Inflammation and Cancer. Molecules 2020, 25, 5488. https://doi.org/10.3390/molecules25235488
Das Mahapatra A, Choubey R, Datta B. Small Molecule Soluble Epoxide Hydrolase Inhibitors in Multitarget and Combination Therapies for Inflammation and Cancer. Molecules. 2020; 25(23):5488. https://doi.org/10.3390/molecules25235488
Chicago/Turabian StyleDas Mahapatra, Amarjyoti, Rinku Choubey, and Bhaskar Datta. 2020. "Small Molecule Soluble Epoxide Hydrolase Inhibitors in Multitarget and Combination Therapies for Inflammation and Cancer" Molecules 25, no. 23: 5488. https://doi.org/10.3390/molecules25235488
APA StyleDas Mahapatra, A., Choubey, R., & Datta, B. (2020). Small Molecule Soluble Epoxide Hydrolase Inhibitors in Multitarget and Combination Therapies for Inflammation and Cancer. Molecules, 25(23), 5488. https://doi.org/10.3390/molecules25235488




