Pharmacokinetics and Tissue Distribution of Anwuligan in Rats after Intravenous and Intragastric Administration by Liquid Chromatography-Mass Spectrometry
Abstract
1. Introduction
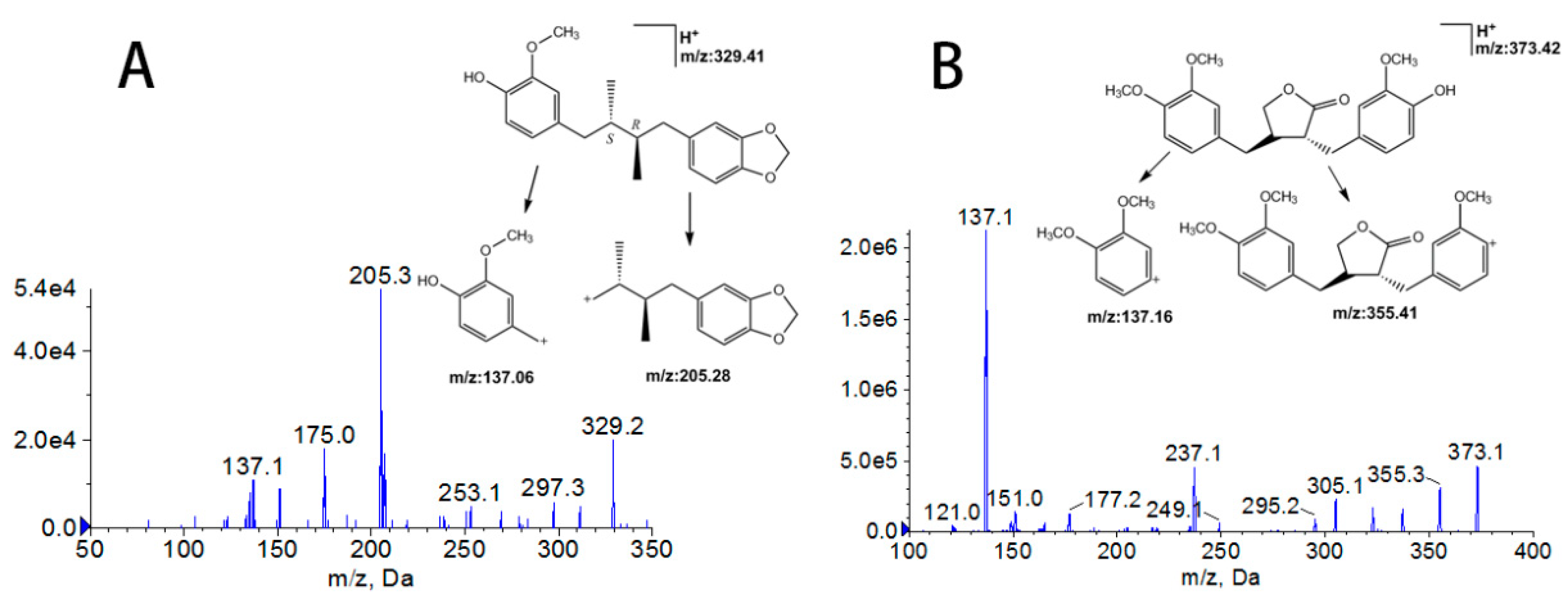
2. Results
2.1. Method Validation
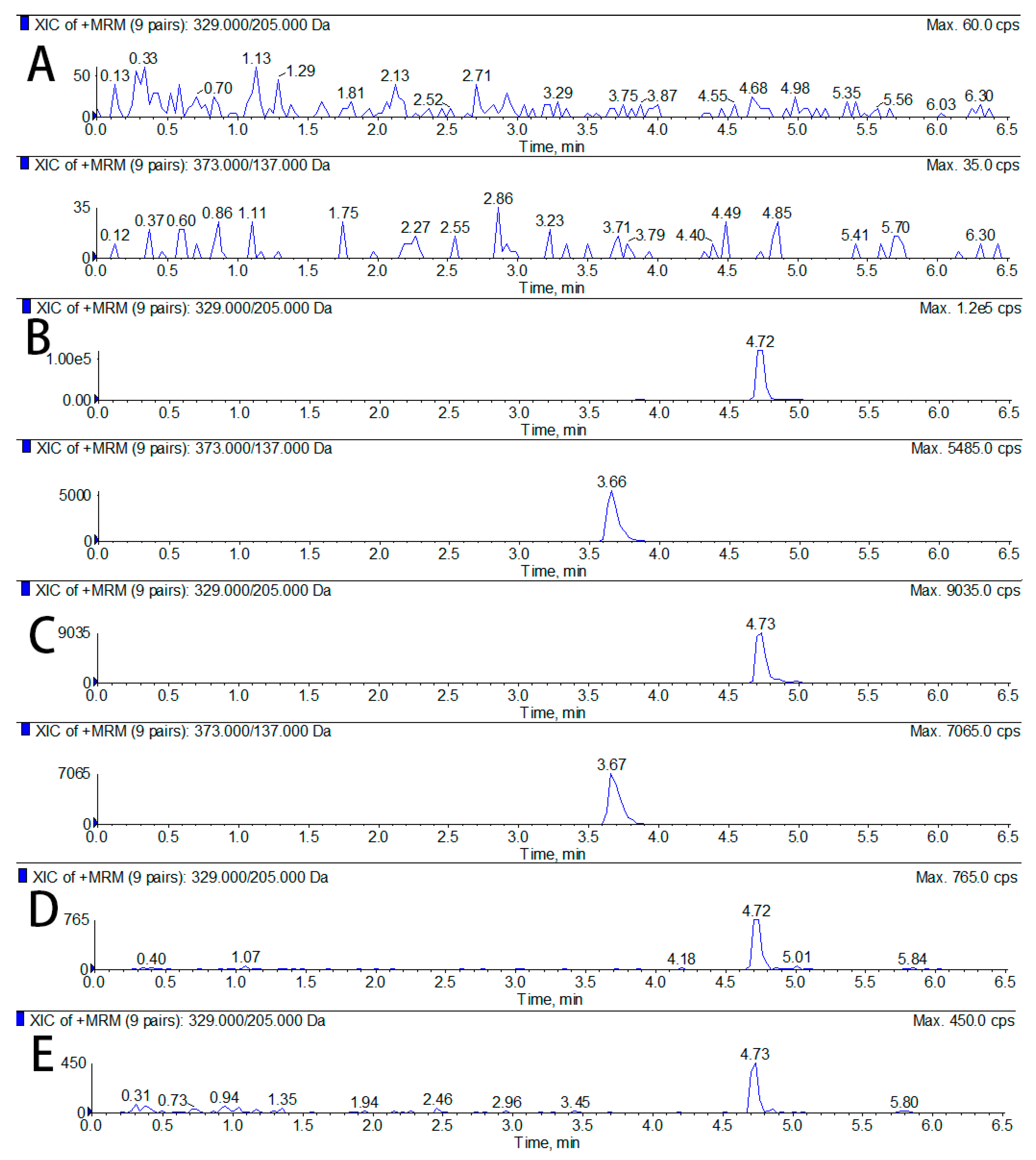
2.1.1. Specificity
2.1.2. Calibration Curve and LLOQ
2.1.3. Precision and Accuracy
2.1.4. Extraction Recovery and Matrix Effect
2.1.5. Stability
2.1.6. Dilution Intergrity
2.2. Dose Selection
2.3. Pharmacokinetic Study
2.3.1. Intravenous Administration PKs
2.3.2. Intragastric Administration PKs
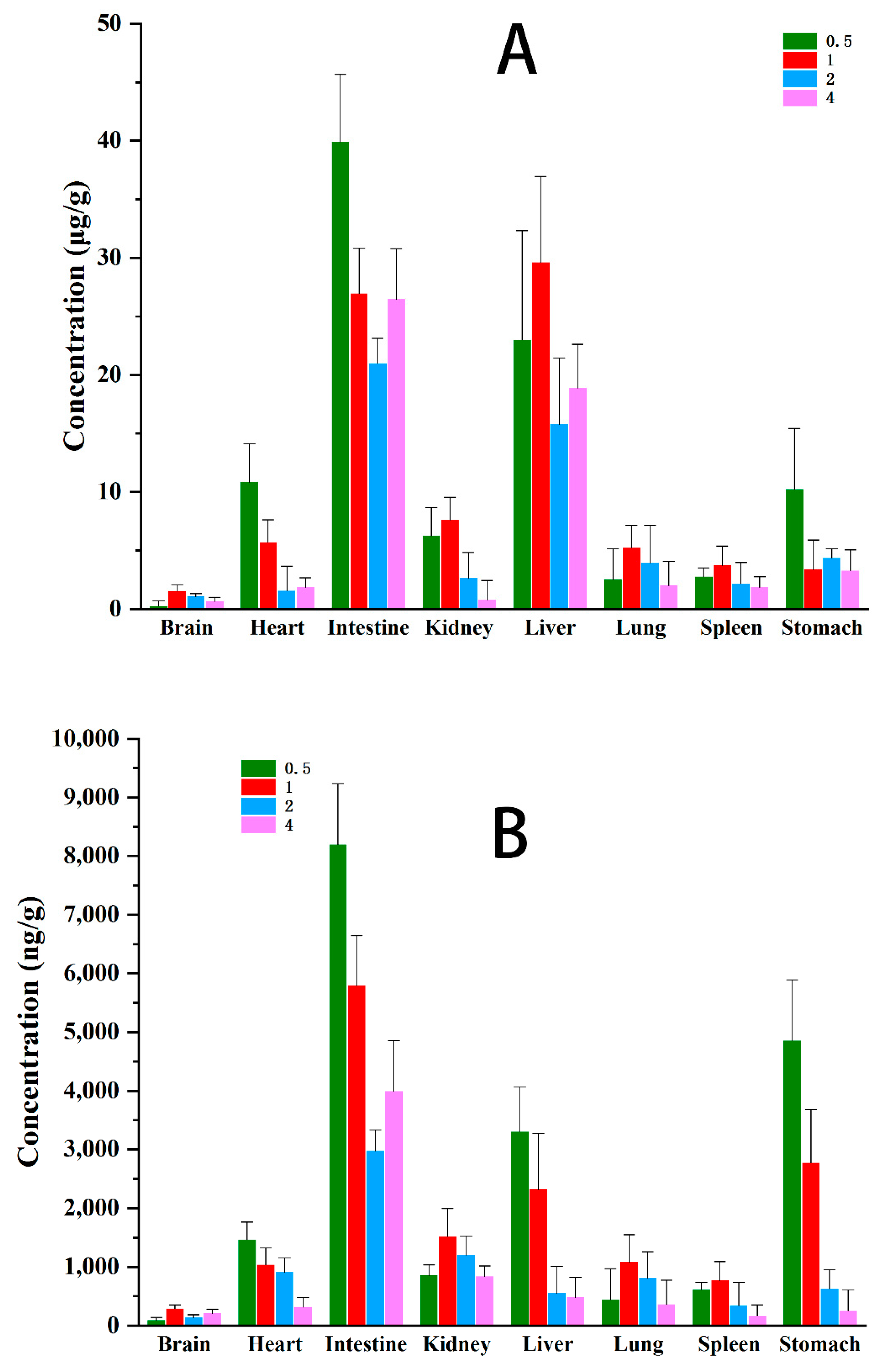
2.4. Tissue Distribution
2.4.1. Intravenous Administration Tissue Distribution
2.4.2. Intragastric Administration Tissue Distribution
3. Materials and Methods
3.1. Reagents and Materials
3.2. Animals
3.3. LC-MS/MS Conditions
3.4. Preparation of Calibration Standards and Quality Control (QC) Samples
3.5. Sample Preparation
3.5.1. Plasma Samples
3.5.2. Tissue Samples
3.6. Method Validation
3.6.1. Specificity
3.6.2. Calibration Curve and LLOQ
3.6.3. Precision and Accuracy
3.6.4. Extraction Recovery and Matrix Effect
3.6.5. Stability
3.6.6. Dilution Integrity
3.7. PKs and Tissue Distribution Study Protocols
3.8. Data Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sohn, J.H.; Han, K.L.; Choo, J.H.; Hwang, J.K. Macelignan protects HepG2 cells against tert-butylhydroperoxide-induced oxidative damage. BioFactors 2007, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.W.; Shin, K.H.; Wagner, H.; Lotter, H. The structure of macelignan from Myristica fragrans. Phytochemistry 1987, 26, 1542–1543. [Google Scholar] [CrossRef]
- Orabi, Y.K.; Mossa, J.S.; El-Feraly, F.S. Isolation and characterization of two antimicrobial agents from mace (Myristica fragrans). J. Nat. Prod. 1991, 54, 856–859. [Google Scholar] [CrossRef] [PubMed]
- Rukayadi, Y.; Lee, K.; Han, S.; Kim, S.; Hwang, J.K. Antibacterial and Sporicidal Activity of Macelignan Isolated from Nutmeg (Myristica fragrans Houtt.) against Bacillus cereus. Food Sci. Biotechnol. 2009, 18, 1301–1304. [Google Scholar]
- Chung, J.Y.; Choo, J.H.; Lee, M.H.; Hwang, J.K. Anticariogenic activity of macelignan isolated from Myristica fragrans (nutmeg) against Streptococcus mutans. Phytomedicine 2006, 13, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Rukayadi, Y.; Kim, K.H.; Hwang, J.K. In Vitro Anti-biofilm Activity of Macelignan isolated from Myristica fragrans Houtt. against Oral Primary Colonizer Bacteria. Phytother. Res. 2008, 22, 308–312. [Google Scholar]
- Park, B.Y.; Min, B.S.; Kwon, O.K.; Oh, S.R.; Ahn, K.S.; Kim, T.J.; Kim, D.Y.; Bae, K.; Lee, H.K. Increase of caspase-3 activity by lignans from Machilus thunbergii in HL-60 cells. Biol. Pharm. Bull. 2004, 27, 1305–1307. [Google Scholar] [CrossRef]
- Qiang, F.; Lee, B.; Ha, I.; Kang, K.W.; Woo, E.; Han, H. Effect of maceligan on the systemic exposure of paclitaxel: In vitro and in vivo evaluation. Eur. J. Pharm. Sci. 2010, 41, 226–231. [Google Scholar] [CrossRef]
- Zhang, C.; Qi, X.; Shi, Y.; Sun, Y.; Li, S.; Gao, X.; Yu, H. Estimation of Trace Elements in Mace (Myristica fragrans Houtt) and Their Effect on Uterine Cervix Cancer Induced by Methylcholanthrene. Biol. Trace Elem. Res. 2012, 149, 431–434. [Google Scholar] [CrossRef]
- Im, Y.B.; Ha, I.; Kang, K.W.; Lee, M.; Han, H. Macelignan: A New Modulator of P-Glycoprotein in Multidrug-Resistant Cancer Cells. Nutr. Cancer 2009, 61, 538–543. [Google Scholar] [CrossRef]
- Shin, S.H.; Woo, W.S.; Lee, J.Y.; Han, Y.B. Effects of Lignans on Hepatic Drug-Metabolizing Enzymes. Arch. Pharmacal. Res. 1990, 13, 265–268. [Google Scholar] [CrossRef]
- Sohn, J.H.; Han, K.L.; Kim, J.H.; Rukayadi, Y.; Hwang, J.K. Protective Effects of macelignan on cisplatin-induced hepatotoxicity is associated with JNK activation. Biol. Pharm. Bull. 2008, 31, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.B.; Ghadyale, V.A.; Taklikar, S.S.; Kulkarni, C.R.; Arvindekar, A.U. Insulin Secretagogue, Alpha-glucosidase and Antioxidant Activity of Some Selected Spices in Streptozotocin-induced Diabetic Rats. Plant Foods Hum. Nutr. 2011, 66, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Staels, B.; Fruchart, J.C. Original Article Therapeutic Roles of Peroxisome Proliferator- Activated Receptor Agonists. Diabetes 2005, 54, 2460–2470. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Kim, K.H.; Shim, J.S.; Hwang, J.K. Inhibitory effects of macelignan isolated from Myristica fragrans HOUTT. On melanin biosynthesis. Biol. Pharm. Bull. 2008, 31, 986–989. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.J.; Kang, Y.G.; Kim, J.; Hwang, J.K. Macelignan inhibits melanosome transfer mediated by protease-activated receptor-2 in keratinocytes. Biol. Pharm. Bull. 2011, 34, 748–754. [Google Scholar] [CrossRef]
- Checker, R.; Chatterjee, S.; Sharma, D.; Gupta, S.; Variyar, P.; Sharma, A.; Poduval, T.B. Immunomodulatory and radioprotective effects of lignans derived from fresh nutmeg mace (Myristica fragrans) in mammalian splenocytes. Int. Immunopharmacol. 2008, 8, 661–669. [Google Scholar] [CrossRef]
- Han, K.L.; Choi, J.S.; Lee, J.Y.; Song, J.; Joe, M.K.; Jung, M.H.; Hwang, J. Therapeutic Potential of Peroxisome Proliferators-Activated Receptor-α/γ Dual Agonist With Alleviation of Endoplasmic Reticulum Stress for the Treatment of Diabetes. Diabetes 2008, 57, 737–745. [Google Scholar] [CrossRef]
- Han, Y.S.; Kim, M.; Hwang, J. Macelignan Inhibits Histamine Release and Inflammatory Mediator Production in Activated Rat Basophilic Leukemia Mast Cells. Inflammation 2012, 35, 1723–1731. [Google Scholar] [CrossRef]
- Jin, D.; Lim, C.S.; Hwang, J.K.; Ha, I.; Han, J. Anti-oxidant and anti-inflammatory activities of macelignan in murine hippocampal cell line and primary culture of rat microglial cells. Biochem. Biophys. Res. Commun. 2005, 331, 1264–1269. [Google Scholar] [CrossRef]
- Cui, C.; Jin, D.; Hwang, Y.K.; Lee, I.; Hwang, J.K.; Ha, I.; Han, J. Macelignan attenuates LPS-induced inflammation and reduces LPS-induced spatial learning impairments in rats. Neurosci. Lett. 2008, 448, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Lu, Y.; Chen, D. Authentication of Schisandra chinensis and Schisandra sphenanthera in Chinese patent medicines. J. Pharm. Biomed. Anal. 2016, 131, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Sun, L.; Tai, Z.; Gao, S.; Xu, W.; Chen, W. A simple and sensitive HPLC method for the simultaneous determination of eight bioactive components and fingerprint analysis of Schisandra sphenanthera. Anal. Chim. Acta 2010, 662, 97–104. [Google Scholar] [CrossRef]
- Chen, Q. Research Methods in Pharmacology of Chinese Materia Medica, 3rd ed.; People’s Medical Publishing House: Beijing, China, 2011. [Google Scholar]
- Sharma, D.R.; Sunkaria, A.; Bal, A.; Bhutia, Y.D.; Vijayaraghavan, R.; Flora, S.J.; Gill, K.D. Neurobehavioral impairments, generation of oxidative stress and release of pro-apoptotic factors after chronic exposure to sulphur mustard in mouse brain. Toxicol. Appl. Pharm. 2009, 15, 208–218. [Google Scholar] [CrossRef]
- Tao, X.; Cush, J.J.; Garret, M.; Lipsky, P.E. A phase I study of ethyl acetate extract of the chinese antirheumatic herb Tripterygium wilfordii hook F in rheumatoid arthritis. J. Rheumatol. 2005, 10, 2160–2167. [Google Scholar]
- Mukker, J.K.; Kotlyarova, V.; Singh, R.S.P.; Alcorn, J. HPLC method with fluorescence detection for the quantitative determination of flaxseed lignans. J. Chromatogr. B 2010, 878, 3076–3082. [Google Scholar] [CrossRef]
- Mukker, J.K.; Singh, R.S.P.; Muir, A.D.; Krol, E.S.; Alcorn, J. Comparative pharmacokinetics of purified flaxseed and associated mammalian lignans in male Wistar rats. Br. J. Nutr. 2015, 113, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Yang, X. Quantification of myrislignan in rat plasma by solid-phase extraction and reversed-phase high-performance liquid chromatography. Biomed. Chromatogr. 2008, 22, 601–605. [Google Scholar] [CrossRef]
- Bioanalytical Method Validation Guidance for Industry 2018. Available online: https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf (accessed on 2 November 2019).
- Drug Analysis System [CP/DK]. Available online: http://www.drugchina.net/# (accessed on 2 November 2019).
Sample Availability: Samples of the anwuligan and arctigenin are available from the authors. |

| Samples | Calibration Curves | Correlation Coefficients (r) | SES * | SEI # | Linear Ranges (ng/mL) | LLOQs (ng/mL) |
|---|---|---|---|---|---|---|
| Plasma | Y = 0.00929 + 0. 000157x | 0.996–0.997 | 6.3 × 10−4 | 0.22 | 0.5–2000 | 0.5 |
| Intestine | Y = 0.00378 + 0. 0030x | 0.996–0.998 | 9.6 × 10−4 | 0.37 | 0.5–2000 | 0.5 |
| Heart | Y = 0.000419 + 0.0491x | 0.995–0.997 | 8.7 × 10−4 | 0.19 | 0.5–2000 | 0.5 |
| Liver | Y = 0.00587 + 0.000116x | 0.997–0.999 | 4.1 × 10−5 | 0.13 | 0.5–2000 | 0.5 |
| Spleen | Y = 0.0000987 + 0.0011x | 0.994–0.996 | 7.9 × 10−4 | 0.28 | 0.5–2000 | 0.5 |
| Lung | Y = 0.00689 + 0.000892x | 0.995–0.997 | 9.0 × 10−4 | 0.39 | 0.5–2000 | 0.5 |
| Kidney | Y = –0.000326 + 0.000131x | 0.996–0.998 | 7.7 × 10−5 | 0.27 | 0.5–2000 | 0.5 |
| Stomach | Y = –0.0045 + 0.00088x | 0.996–0.997 | 6.9 × 10−4 | 0.34 | 0.5–2000 | 0.5 |
| Brain | Y = –0.0068 + 0.00017x | 0.996–0.998 | 8.2 × 10−4 | 0.26 | 0.5–2000 | 0.5 |
| Samples | QC Conc. (ng/mL) | Intra−Day | Inter−Day | ||
|---|---|---|---|---|---|
| Precision (RSD, %) | Accuracy (Mean, %) | Precision (RSD, %) | Accuracy (Mean, %) | ||
| Plasma | 0.5 | 11.3 | −6.7 | 7.2 | 5.3 |
| 5 | 9.6 | −5.3 | 8.3 | 6.5 | |
| 100 | 5.3 | 3.5 | 4.5 | −5.2 | |
| 1600 | 8.4 | 4.9 | 3.8 | 5.7 | |
| Heart | 0.5 | 7.5 | 9.5 | 6.0 | 10.6 |
| 5 | 5.4 | −7.0 | 4.0 | −9.2 | |
| 100 | 8.5 | 7.3 | 7.0 | 6.7 | |
| 1600 | 8.7 | −3.4 | 4.1 | −4.4 | |
| Liver | 0.5 | 4.5 | −4.7 | 9.7 | −5.5 |
| 5 | 8.6 | 6.4 | 8.8 | 9.3 | |
| 100 | 7.1 | −5.4 | 3.9 | 5.9 | |
| 1600 | 5.3 | 3.2 | 6.3 | −7.4 | |
| Spleen | 0.5 | 8.7 | −7.9 | 9.0 | −8.9 |
| 5 | 4.2 | 4.0 | 9.3 | −4.7 | |
| 100 | 7.1 | −4.4 | 5.7 | −7.1 | |
| 1600 | 6.6 | 6.9 | 8.8 | 3.6 | |
| Lung | 0.5 | 6.0 | 7.5 | 8.0 | 6.9 |
| 5 | 4.9 | 4.4 | 5.7 | −5.0 | |
| 100 | 4.7 | −7.1 | 3.2 | 3.8 | |
| 1600 | 6.4 | −7.2 | 6.9 | 6.6 | |
| Kidney | 0.5 | 10.9 | −11.5 | 10.6 | −12.6 |
| 5 | 8.4 | −4.3 | 4.9 | −5.1 | |
| 100 | 8.5 | 5.5 | 9.0 | 7.6 | |
| 1600 | 5.4 | 6.7 | 5.9 | −6.8 | |
| Brain | 0.5 | 7.0 | −9.3 | 11.3 | −8.7 |
| 5 | 6.3 | −5.1 | 9.7 | −5.5 | |
| 100 | 5.5 | −4.4 | 5.3 | 3.9 | |
| 1600 | 3.9 | 3.6 | 4.2 | 3.4 | |
| Intestine | 0.5 | 6.6 | 8.6 | 5.9 | 8.6 |
| 5 | 4.6 | 4.3 | 3.2 | 7.2 | |
| 100 | 4.0 | 6.8 | 8.1 | 7.6 | |
| 1600 | 8.3 | 5.4 | 4.8 | 3.1 | |
| Stomach | 0.5 | 8.7 | 6.1 | 6.9 | −8.3 |
| 5 | 7.8 | 6.6 | 6.4 | −4.0 | |
| 100 | 5.9 | −6.2 | 4.3 | 3.9 | |
| 1600 | 7.7 | −6.2 | 7.5 | −4.4 | |
| Samples | QC Conc.(ng/mL) | Matrix Effect | Extract Recovery | ||
|---|---|---|---|---|---|
| Mean ± SD (%) | RSD (%) | Mean ± SD (%) | RSD (%) | ||
| Plasma | 0.5 | 90.7 ± 2.3 | 2.6 | 85.1 ± 2.4 | 2.9 |
| 5 | 89.5 ± 7.6 | 8.6 | 95.5 ± 5 | 5.3 | |
| 100 | 96.2 ± 6.3 | 6.6 | 109.4 ± 8.5 | 7.8 | |
| 1600 | 93.1 ± 7.5 | 8.1 | 106.4 ± 9.5 | 8.9 | |
| Heart | 0.5 | 90.9 ± 8.8 | 9.7 | 86.2 ± 5 | 5.9 |
| 5 | 96.6 ± 9.3 | 9.7 | 103 ± 2.2 | 2.1 | |
| 100 | 90.8 ± 4.1 | 4.6 | 96.6 ± 9.9 | 10.3 | |
| 1600 | 84.6 ± 6.3 | 7.5 | 84 ± 3.9 | 4.7 | |
| Liver | 0.5 | 93.3 ± 8.3 | 9.0 | 109.8 ± 2.4 | 2.3 |
| 5 | 89.6 ± 7.2 | 8.1 | 106.3 ± 6.4 | 6.1 | |
| 100 | 85.1 ± 6.0 | 7.1 | 114 ± 2.8 | 2.5 | |
| 1600 | 84.5 ± 9.2 | 11.0 | 96.9 ± 9.6 | 9.9 | |
| Spleen | 0.5 | 89.2 ± 6.5 | 7.3 | 104.6 ± 4.9 | 4.7 |
| 5 | 91.9 ± 4.2 | 4.6 | 108.8 ± 3.9 | 3.6 | |
| 100 | 86.3 ± 7.3 | 8.5 | 111.3 ± 2.3 | 2.1 | |
| 1600 | 96.8 ± 6.5 | 6.7 | 90.7 ± 8.8 | 9.7 | |
| Lung | 0.5 | 87.5 ± 5.8 | 6.7 | 94.1 ± 3.9 | 4.2 |
| 5 | 93.8 ± 2.2 | 2.4 | 93.3 ± 8.1 | 8.8 | |
| 100 | 95.0 ± 9.0 | 9.5 | 101.9 ± 9.9 | 9.7 | |
| 1600 | 88.3 ± 9.8 | 11.1 | 102.2 ± 2.8 | 2.7 | |
| Kidney | 0.5 | 86.7 ± 3.9 | 4.6 | 95.9 ± 2.4 | 2.6 |
| 5 | 87.2 ± 8.7 | 10.1 | 114.5 ± 8.4 | 7.4 | |
| 100 | 87.4 ± 9.8 | 11.2 | 105.2 ± 5 | 4.8 | |
| 1600 | 90.5 ± 4.3 | 4.8 | 84.5 ± 4.5 | 5.4 | |
| Brain | 0.5 | 88.5 ± 3.7 | 4.2 | 102.5 ± 5.8 | 5.7 |
| 5 | 95.8 ± 4.5 | 4.7 | 84.8 ± 4.9 | 5.8 | |
| 100 | 95.1 ± 7.0 | 7.4 | 103.6 ± 5.4 | 5.3 | |
| 1600 | 85.5 ± 5.7 | 6.7 | 106.9 ± 6.4 | 6.0 | |
| Intestine | 0.5 | 85.8 ± 3.9 | 4.6 | 93 ± 4.7 | 5.1 |
| 5 | 86.0 ± 2.8 | 3.4 | 104.9 ± 5.4 | 5.2 | |
| 100 | 84.6 ± 8.7 | 10.3 | 102 ± 9.8 | 9.6 | |
| 1600 | 92.8 ± 8.1 | 8.8 | 92.8 ± 7.1 | 7.6 | |
| Stomach | 0.5 | 91.8 ± 6.9 | 7.5 | 114.5 ± 8.1 | 7.1 |
| 5 | 88.0 ± 2.4 | 2.8 | 96.7 ± 2.8 | 2.9 | |
| 100 | 87.8 ± 9.0 | 10.3 | 93.8 ± 9 | 9.6 | |
| 1600 | 91.7 ± 3.7 | 4.0 | 102 ± 3.4 | 3.4 | |
| Samples | QC Conc.(ng/mL) | Short-Term (at Room Temperature for 4 h) | Autosampler 4 °C for 24 h | Three Freeze-Thraw Cycles | Storage at −80 °C for 30 d |
|---|---|---|---|---|---|
| Plasma | 5 | 110.4 ± 3.2 | 114.4 ± 10.7 | 110.0 ± 4.7 | 106.7 ± 3.3 |
| 1600 | 94.2 ± 10.4 | 85.2 ± 5.9 | 86.0 ± 4.3 | 99.0 ± 5.6 | |
| Heart | 5 | 95.0 ± 10.4 | 90.3 ± 10.6 | 107.1 ± 4.5 | 85.2 ± 4.5 |
| 1600 | 94.8 ± 5.2 | 102.6 ± 7.8 | 111.8 ± 7.3 | 96.0 ± 3.3 | |
| Liver | 5 | 97.3 ± 4.8 | 91.6 ± 8.0 | 105.6 ± 9.1 | 103.2 ± 7.7 |
| 1600 | 87.1 ± 8.9 | 87.0 ± 7.5 | 106.7 ± 9.5 | 86.4 ± 6.3 | |
| Spleen | 5 | 98.5 ± 10.2 | 100.9 ± 5.3 | 98.6 ± 10.5 | 110.0 ± 8.2 |
| 1600 | 105.6 ± 5.3 | 87.6 ± 5.1 | 102.6 ± 7.7 | 114.9 ± 6.2 | |
| Lung | 5 | 112.4 ± 3.7 | 97.2 ± 3.5 | 88.6 ± 7.6 | 111.1 ± 4.8 |
| 1600 | 87.2 ± 9.7 | 93.6 ± 4.0 | 112.9 ± 9.7 | 92.8 ± 7.5 | |
| Kidney | 5 | 95.7 ± 9.9 | 95.2 ± 6.3 | 88.7 ± 6.4 | 86.4 ± 8.4 |
| 1600 | 99.8 ± 9.1 | 97.1 ± 6.2 | 104.3 ± 9.3 | 112.2 ± 6.3 | |
| Brain | 5 | 93.2 ± 7.4 | 104.5 ± 4.2 | 90.0 ± 5.0 | 112.8 ± 7.7 |
| 1600 | 104.1 ± 4.0 | 106.2 ± 3.3 | 106.9 ± 8.7 | 112.5 ± 7.1 | |
| Intestine | 5 | 103.8 ± 4.9 | 95.5 ± 6.6 | 87.1 ± 4.1 | 95.1 ± 9.6 |
| 1600 | 111.6 ± 10.1 | 110.3 ± 7.1 | 108.3 ± 7.4 | 113.9 ± 4.9 | |
| Stomach | 5 | 90.2 ± 8.0 | 99.9 ± 3.2 | 88.8 ± 4.3 | 105.9 ± 7.5 |
| 1600 | 104.0 ± 10.1 | 109.4 ± 9.8 | 107.2 ± 9.4 | 89.3 ± 8.7 |
| Pharmacokinetic Parameters | Intravenous | Intragastric |
|---|---|---|
| Cmax (ng/mL) | 8310 ± 910 | 810 ± 190 |
| t1/2 (h) | 3.20 ± 1.09 | 5.17 ± 1.82 |
| AUC0–t (ng/mL∙h) | 16,700 ± 7700 | 10,700 ± 2800 |
| AUC0–∞ (ng/mL∙h) | 16,800 ± 8500 | 11,400 ± 3600 |
| MRT0–∞ (h) | 3.71 ± 0.96 | 10.02 ± 2.04 |
| CL (L/h/kg) | 0.89 ± 0.32 | 5.26 ± 1.39 |
| Vd (L/kg) | 4.1 ± 1.1 | 39.3 ± 12.6 |
| F (bioavailability, %) | - | 16.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, Y.; Zhang, Y.; Duan, X.-Y.; Cui, D.-W.; Qiu, X.; Bian, Y.; Wang, K.-F.; Feng, X.-S. Pharmacokinetics and Tissue Distribution of Anwuligan in Rats after Intravenous and Intragastric Administration by Liquid Chromatography-Mass Spectrometry. Molecules 2020, 25, 39. https://doi.org/10.3390/molecules25010039
Song Y, Zhang Y, Duan X-Y, Cui D-W, Qiu X, Bian Y, Wang K-F, Feng X-S. Pharmacokinetics and Tissue Distribution of Anwuligan in Rats after Intravenous and Intragastric Administration by Liquid Chromatography-Mass Spectrometry. Molecules. 2020; 25(1):39. https://doi.org/10.3390/molecules25010039
Chicago/Turabian StyleSong, Yang, Yuan Zhang, Xiao-Yi Duan, Dong-Wei Cui, Xin Qiu, Yu Bian, Ke-Fei Wang, and Xue-Song Feng. 2020. "Pharmacokinetics and Tissue Distribution of Anwuligan in Rats after Intravenous and Intragastric Administration by Liquid Chromatography-Mass Spectrometry" Molecules 25, no. 1: 39. https://doi.org/10.3390/molecules25010039
APA StyleSong, Y., Zhang, Y., Duan, X.-Y., Cui, D.-W., Qiu, X., Bian, Y., Wang, K.-F., & Feng, X.-S. (2020). Pharmacokinetics and Tissue Distribution of Anwuligan in Rats after Intravenous and Intragastric Administration by Liquid Chromatography-Mass Spectrometry. Molecules, 25(1), 39. https://doi.org/10.3390/molecules25010039






