The Use of Poly-d,l-lactic Acid (PDLLA) Devices for Bone Augmentation Techniques: A Systematic Review
Abstract
:1. Introduction
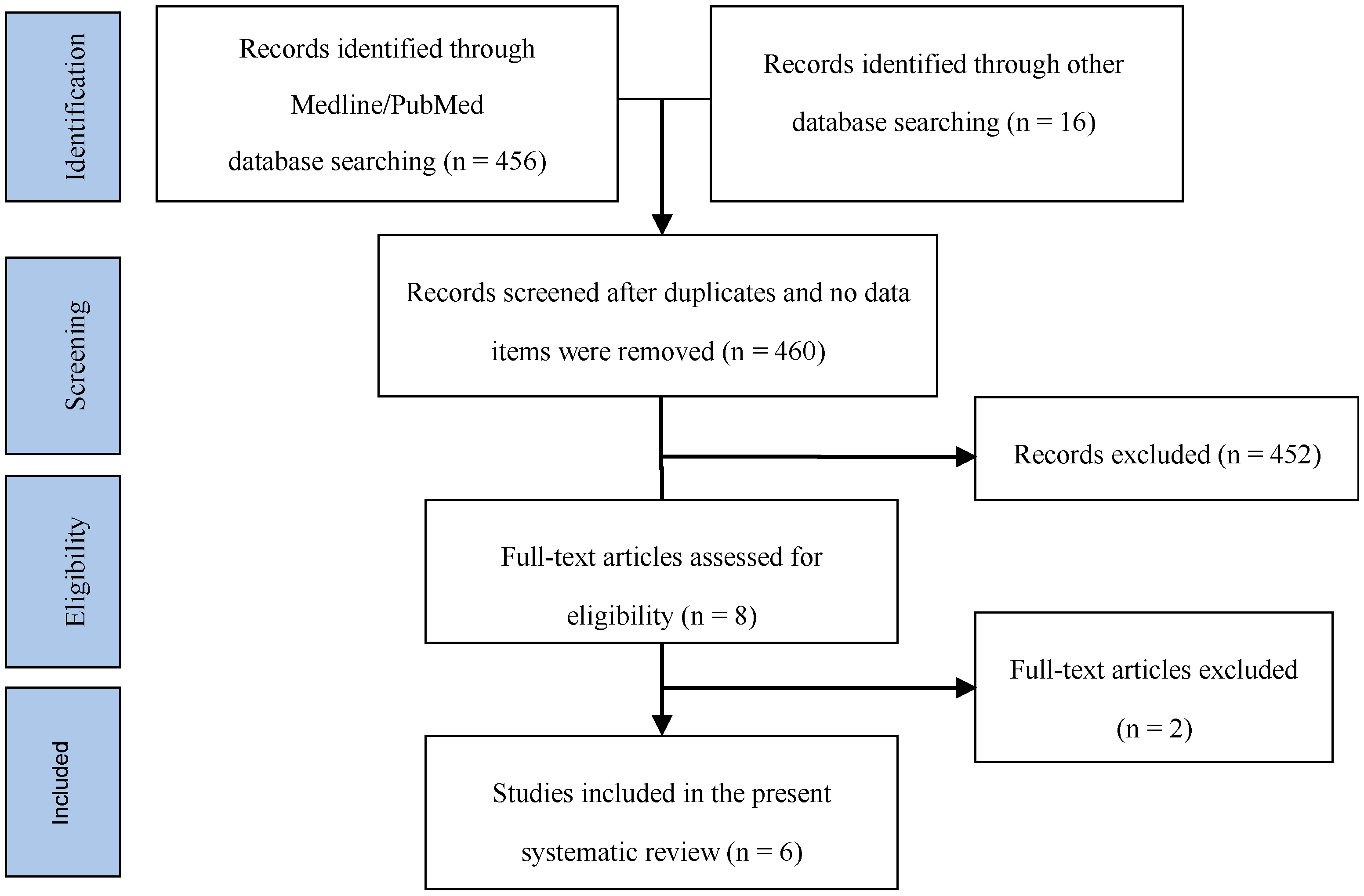
2. Materials and Methods
3. Results
4. Discussion and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.M.D.; Eriksson, A.R. The long term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar] [PubMed]
- Lindquist, L.W.; Carlsson, G.E.; Jemt, T.A. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clin. Oral Implants Res. 1996, 7, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Gunne, J.; Henry, P.; Higuchi, K.; Linden, U.; Bergstrom, C.; van Steenberghe, D. Survival of the Branemark implant in partially edentulous jaws: A 10-year prospective multicenter study. Int. J. Oral Maxillofac. Implants 1999, 14, 639–645. [Google Scholar] [PubMed]
- Ekelund, J.A.; Lindquist, L.W.; Carlsson, G.E.; Jemt, T. Implant treatment in the edentulous mandible: A prospective study on Brånemark system implants over more than 20 years. Int. J. Prosthodont. 2003, 16, 602–608. [Google Scholar] [PubMed]
- Jemt, T.; Johansson, J. Implant treatment in the edentulous maxillae: A 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin. Implant Dent. Relat. Res. 2006, 8, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Zaniboni, M.; Boisco, M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin. Oral Implants Res. 2006, 17, 136–159. [Google Scholar] [CrossRef] [PubMed]
- Donos, N.; Mardas, N.; Chadha, V. Clinical outcomes of implants following lateral bone augmentation: Systematic assessment of available options (barrier membranes, bone grafts, split osteotomy). J. Clin. Periodontol. 2008, 35, 173–202. [Google Scholar] [CrossRef] [PubMed]
- Rocchietta, I.; Fontana, F.; Simion, M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review. J. Clin. Periodontol. 2008, 35, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Hammerle, C.H.; Jung, R.E. Bone augmentation by means of barrier membranes. Periodontology 2000 2003, 33, 36–53. [Google Scholar] [CrossRef] [PubMed]
- Retzepi, M.; Donos, N. Guided bone regeneration: Biological principle and therapeutic applications. Clin. Oral Implants Res. 2010, 21, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Dula, K.; Belser, U.; Hirt, H.P.; Berthold, H. Localized ridge augmentation using guided bone regeneration: I. Surgical procedure in the maxilla. Int. J. Periodont. Restor. Dent. 1993, 13, 29–45. [Google Scholar]
- Buser, D.; Dula, K.; Belser, U.C.; Hirt, H.P.; Berthold, H. Localized ridge augmentation using guided bone regeneration: II. Surgical procedure in the mandible. Int. J. Periodont. Restor. Dent. 1995, 15, 10–29. [Google Scholar]
- Simion, M.; Baldoni, M.; Rossi, P.; Zaffe, D. A comparative study of the effectiveness of e-PTFE membranes with and without early exposure during the healing period. Int. J. Periodont. Restor. Dent. 1994, 14, 166–180. [Google Scholar]
- Machtei, E.E. The effect of membrane exposure on the outcome of regenerative procedures in humans: A meta-analysis. J. Periodontol. 2001, 72, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Hutmacher, D.; Hurzeler, M.B.; Schliephake, H. A review of material properties of biodegradable and bioresorbable polymers and devices for GTR and GBR applications. Int. J. Oral Maxillofac. Implants 1996, 11, 667–678. [Google Scholar] [PubMed]
- Gentile, P.; Chiono, V.; Tonda-Turo, C.; Ferreira, A.M.; Ciardelli, G. Polymeric membranes for guided bone regeneration. Biotechnol. J. 2011, 6, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.H.; Yoon, M.C.; Jeong, C.M.; Jang, J.; Jeong, S.I.; Cho, D.W.; Huh, J.B. Efficacy of rhBMP-2 loaded PCL/PLGA/β-TCP guided bone regeneration membrane fabricated by 3D printing technology for reconstruction of calvaria defects in rabbit. Biomed. Mater. 2014, 9, 065006. [Google Scholar] [CrossRef] [PubMed]
- Miller, N.; Penaud, J.; Foliguet, B.; Membre, H.; Ambrosini, P.; Plombas, M. Resorption rates of 2 commercially available bioresorbable membranes. A histomorphometric study in a rabbit model. J. Clin. Periodontol. 1996, 23, 1051–1059. [Google Scholar] [CrossRef] [PubMed]
- Pina, S.; Ferreira, J.M.F. Bioresorbable Plates and Screws for Clinical Applications: A Review. J. Health Eng. 2012, 3, 243–260. [Google Scholar] [CrossRef]
- Saeidlou, S.; Huneault, M.A.; Li, H.; Park, C.B. Poly(lactic acid) crystallization. Prog. Polym. Sci. 2012, 37, 1657–1677. [Google Scholar] [CrossRef]
- Dorgan, J.R.; Jansen, J.; Clayton, M.P.; Hait, S.B.; Knauss, D.M. Melt rheology of variable L-content poly(lactic acid). J. Rheol. 2005, 49, 607–619. [Google Scholar] [CrossRef]
- Pietrzak, W.S.; Sarver, D.R.; Verstynen, M.L. Bioabsorbable polymer science for the practicing surgeon. J. Craniofac. Surg. 1997, 8, 87–91. [Google Scholar] [CrossRef]
- Vert, M.; Li, S.M.; Garreau, H. Attempts to map the structure and degradation characteristics of aliphatic polyesters derived from lactic and glycolic acids. J. Biomater. Sci. Polym. Ed. 1994, 6, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Bostman, O.; Paivarinta, U.; Partio, E.; Vasenius, J.; Manninen, M.; Rokkanen, P. Degradation and tissue replacement of an absorbable polyglycolide screw in the fixation of rabbit femoral osteotomies. J. Bone Jt. Surg. 1992, 74, 1021–1031. [Google Scholar] [CrossRef]
- Brandt, R.B.; Waters, M.G.; Rispler, M.J.; Kline, E.S. d- and l-lactate catabolism to CO2 in rat tissues. Proc. Soc. Exp. Biol. Med. 1984, 175, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Pilling, E.; Mai, R.; Theissig, F.; Stadlinger, B.; Loukota, R.; Eckelt, U. An experimental in vivo analysis of the resorption to ultrasound activated pins (Sonic weld) and standard biodegradable screws (ResorbX) in sheep. Br. J. Oral Maxillofac. Surg. 2007, 45, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Pilling, E.; Meissner, H.; Jung, R.; Koch, R.; Loukota, R.; Mai, R.; Reitemeier, B.; Richter, G.; Stadlinger, B.; Stelnicki, E.; et al. An experimental study of the biomechanical stability of ultrasound-activated pinned (SonicWeld Rx + Resorb-X) and screwed fixed (Resorb-X) resorbable materials for osteosynthesis in the treatment of simulated craniosynostosis in sheep. Br. J. Oral Maxillofac. Surg. 2007, 45, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Iglhaut, G.; Schwarz, F.; Gründel, M.; Mihatovic, I.; Becker, J.; Schliephake, H. Shell technique using a rigid resorbable barrier system for localized alveolar ridge augmentation. Clin. Oral Implants Res. 2014, 25, e149–e154. [Google Scholar] [CrossRef] [PubMed]
- Marinucci, L.; Lilli, C.; Baroni, T.; Becchetti, E.; Belcastro, S.; Balducci, C.; Locci, P. In Vitro comparison of bioabsorbable and non-resorbable membranes in bone regeneration. J. Periodontol. 2001, 72, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Schmidmaier, G.; Baehr, K.; Mohr, S.; Kretschmar, M.; Beck, S.; Wildemann, B. Biodegradable polylactide membranes for bone defect coverage: Biocompatibility testing, radiological and histological evaluation in a sheep model. Clin. Oral Implants Res. 2006, 17, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Annunziata, M.; Nastri, L.; Borgonovo, A.; Benigni, M.; Poli, P.P. Poly-d-l-lactic acid membranes for bone regeneration. J. Craniofac. Surg. 2015, 26, 1691–1696. [Google Scholar] [CrossRef] [PubMed]
- Buijs, G.J.; van der Houwen, E.B.; Stegenga, B.; Bos, R.R.; Verkerke, G.J. Mechanical strength and stiffness of biodegradable and titanium osteofixation systems. J. Oral Maxillofac. Surg. 2007, 65, 2148–2158. [Google Scholar] [CrossRef] [PubMed]
- Buijs, G.J.; van der Houwen, E.B.; Stegenga, B.; Bos, R.R.; Verkerke, G.J. Torsion strength of biodegradable and titanium screws: A comparison. J. Oral Maxillofac. Surg. 2007, 65, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
- Buijs, G.J.; van der Houwen, E.B.; Stegenga, B.; Verkerke, G.J.; Bos, R.R. Mechanical strength and stiffness of the biodegradable SonicWeld Rx osteofixation system. J. Oral Maxillofac. Surg. 2009, 67, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Rosen, P.S.; Reynolds, M.A. Guided bone regeneration for dehiscence and fenestration defects on implants using an absorbable polymer barrier. J. Periodontol. 2001, 72, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.M.; Liem, R.S.; Bos, R.R.; van der Wal, J.E.; Vissink, A. Resorbable screws for fixation of autologous bone grafts. Clin. Oral Implants Res. 2006, 17, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Chacon, G.E.; Ellis, J.P.; Kalmar, J.R.; McGlumphy, E.A. Using resorbable screws for fixation of cortical onlay bone grafts: An in vivo study in rabbits. J. Oral Maxillofac. Surg. 2004, 62, 1396–1402. [Google Scholar] [CrossRef] [PubMed]
- Santana, R.B.; de Mattos, C.M. Efficacy of vascularized periosteal membranes in providing soft tissue closure at grafted human maxillary extraction sites. Int. J. Oral Maxillofac. Implants 2009, 24, 81–87. [Google Scholar] [PubMed]
- Lekholm, U.; Becker, W.; Dahlin, C.; Becker, B.; Donath, K.; Morrison, E. The role of early versus late removal of GTAM membranes on bone formation at oral implants placed into immediate extraction sockets. An experimental study in dogs. Clin. Oral Implants Res. 1993, 4, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Burger, B.W. Use of ultrasound-activated resorbable poly-d-l-lactide pins (SonicPins) and foil panels (Resorb-X) for horizontal bone augmentation of the maxillary and mandibular alveolar ridges. J. Oral Maxillofac. Surg. 2010, 68, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Lie, N.; Merten, H.A.; Meyns, J.; Lethaus, B.; Wiltfang, J.; Kessler, P. Elevation of the maxillary sinus membrane for de-novo bone formation: First results of a prospective study in humans. J. Cranio-Maxillofac. Surg. 2015, 43, 1670–1677. [Google Scholar] [CrossRef] [PubMed]
- Heidemann, W.; Jeschkeit, S.; Ruffieux, K.; Fischer, J.H.; Wagner, M.; Kruger, G.; Wintermantel, E.; Gerlach, K.L. Degradation of poly(d,l)lactide implants with or without addition of calciumphosphates in vivo. Biomaterials 2001, 22, 2371–2381. [Google Scholar] [CrossRef]
- Gocmen, G.; Atah, O.; Aktop, S.; Sipahi, A.; Gonul, O. Hyaluronic acid versus ultrasonic resorbable pin fixation for space maintenance in non-grafted sinus lifting. J. Oral Maxillofac. Surg. 2016, 74, 497–504. [Google Scholar] [CrossRef] [PubMed]
| Systematic Search Strategy |
|---|
| Search string: (pdlla OR “poly-d,l-lactic acid” OR “poly(l,d-lactide)” OR “poly-d-l-lactide” OR “poly-d,l-lactide” OR “poly(l/d-lactide)” OR “poly(l,d-lactic acid)” OR “poly-d,l-lactide acid” OR “Atrisorb” OR “Resorb-X” OR “SonicWeld” OR “SonicPins”) AND (oral OR dental OR bone) AND (membrane OR shell OR pin OR barrier OR screw OR mesh) Filter: Humans Language: No restrictions Electronic databases: MEDLINE/PubMed, The Cochrane Central Register of Controlled Trials (CENTRAL), ClinicalTrials.gov Inclusion criteria:
Exclusion criteria:
|
| Autor, Year | Design | Patients (Sites) | Groups | Follow-Up | Results | Conclusions |
|---|---|---|---|---|---|---|
| Gocmen et al., 2016 | RCT, Split mouth | 10 (20) |
| 6 months | Significantly higher postoperative mean values of alveolar bone height on both sides compared to the preoperative ones. Significantly greater increase of alveolar bone height and reduction in sinus volume on the test side compared to the control side. 100% implant survival rate at both sides. | There was sufficient bone height to eventually place the implant in both sides of all patients. The two techniques yielded predictable outcomes in implant survival and bone quality. However, the height of alveolar bone and reduction in sinus volume were considerably greater on the PDLLA pin sides. |
| Lie et al., 2015 | RCT, Split mouth. | 5 (10) |
| 6 months | Bone formation revealed by CBCT at both sides, but less radiopacity shown at the test sides. Vital new bone at the histological analysis, although less organized and immature, at the test side and a mixture of autogenous and residual bone substitute at the control side. 100% implant survival rate at both sides. | The PDLLA membrane proved to be a good and reliable technique to create a stable elevation of the sinus membrane and seemed not interfere with the bone forming process. |
| Burger BW, 2010 | CT, Parallel groups | ND |
| ND | About 3 mm increase in bone width measured by computed tomography. No clinical difference in the nature of the grafts and in the bone density between the test and control groups. Unremarkable tissue response. No evidence of prolonged inflammation, swelling, or discomfort. | There are many advantages to using the resorbable PDLLA pins and foil panels for augmenting alveolar ridge defects: the handling and placing the pins and foil is easy and provides excellent support for the underlining mucoperiosteum for particulate bone grafting. |
| Santana & de Mattos, 2009 | CT, split mouth | 22 (56) |
| 6 months | Ridge dimension change showed a small not statistically significant difference in favor of the PDLLA membrane. 7% membrane exposition rate at the test sites. No signs of erythema, edema, swelling, or suppuration in any test or control site. Comparable soft tissue healing at both test or control sites. | Fluid PDLLA membrane may be suitable for alveolar ridge preservation in conjunction with composite bone grafting. Within the limitations of the present study, it was concluded that the vascularized periosteal membrane was an adequate choice for achieving and maintaining complete soft tissue coverage and healing by primary intention of grafted extraction sockets in humans. The procedures allowed for optimal levels of complete coverage of absorbable membranes during healing; however, the use of a fluid PDLLA membrane provided no additional clinical benefits. |
| Raghoebar et al., 2006 | RCT, split mouth | 8 (16) |
| 3–9 months | Comparable increase (about 4 mm) of the alveolar ridge width in both test and control sides. PDLLA material still visible at the histological analysis, not in direct contact with the bone and surrounded by fibrous tissue, thin and immature, with a lot of giant cells; no necrosis, hemorrhage, or significant inflammatory response. 100% implant survival rate at both sides. | Resorbable screws can be used as fixation devices for autologous bone grafts. However, care must be taken when using these screws because of the presence of the polymer (remnants) after nine months, which could interfere in the sequence of the treatment with endosseous implants. |
| Rosen & Reynolds, 2001 | Observational descriptive study (case series) | 9 (11) |
| 4 to 8.5 months | Complete coverage in 10/11 sites (success rate 90.9%). No site had inflammatory reactions or infection. Vital bone, at the histologic evaluation, in close amalgamation with graft particles, without inflammatory infiltrate. | Fluid PDLLA membranes can be used in conjunction with a bone graft to treat peri-implant dehiscences and fenestrations. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Annunziata, M.; Nastri, L.; Cecoro, G.; Guida, L. The Use of Poly-d,l-lactic Acid (PDLLA) Devices for Bone Augmentation Techniques: A Systematic Review. Molecules 2017, 22, 2214. https://doi.org/10.3390/molecules22122214
Annunziata M, Nastri L, Cecoro G, Guida L. The Use of Poly-d,l-lactic Acid (PDLLA) Devices for Bone Augmentation Techniques: A Systematic Review. Molecules. 2017; 22(12):2214. https://doi.org/10.3390/molecules22122214
Chicago/Turabian StyleAnnunziata, Marco, Livia Nastri, Gennaro Cecoro, and Luigi Guida. 2017. "The Use of Poly-d,l-lactic Acid (PDLLA) Devices for Bone Augmentation Techniques: A Systematic Review" Molecules 22, no. 12: 2214. https://doi.org/10.3390/molecules22122214
APA StyleAnnunziata, M., Nastri, L., Cecoro, G., & Guida, L. (2017). The Use of Poly-d,l-lactic Acid (PDLLA) Devices for Bone Augmentation Techniques: A Systematic Review. Molecules, 22(12), 2214. https://doi.org/10.3390/molecules22122214






