NO Exchange for a Water Molecule Favorably Changes Iontophoretic Release of Ruthenium Complexes to the Skin
Abstract
:1. Introduction
2. Results and Discussion
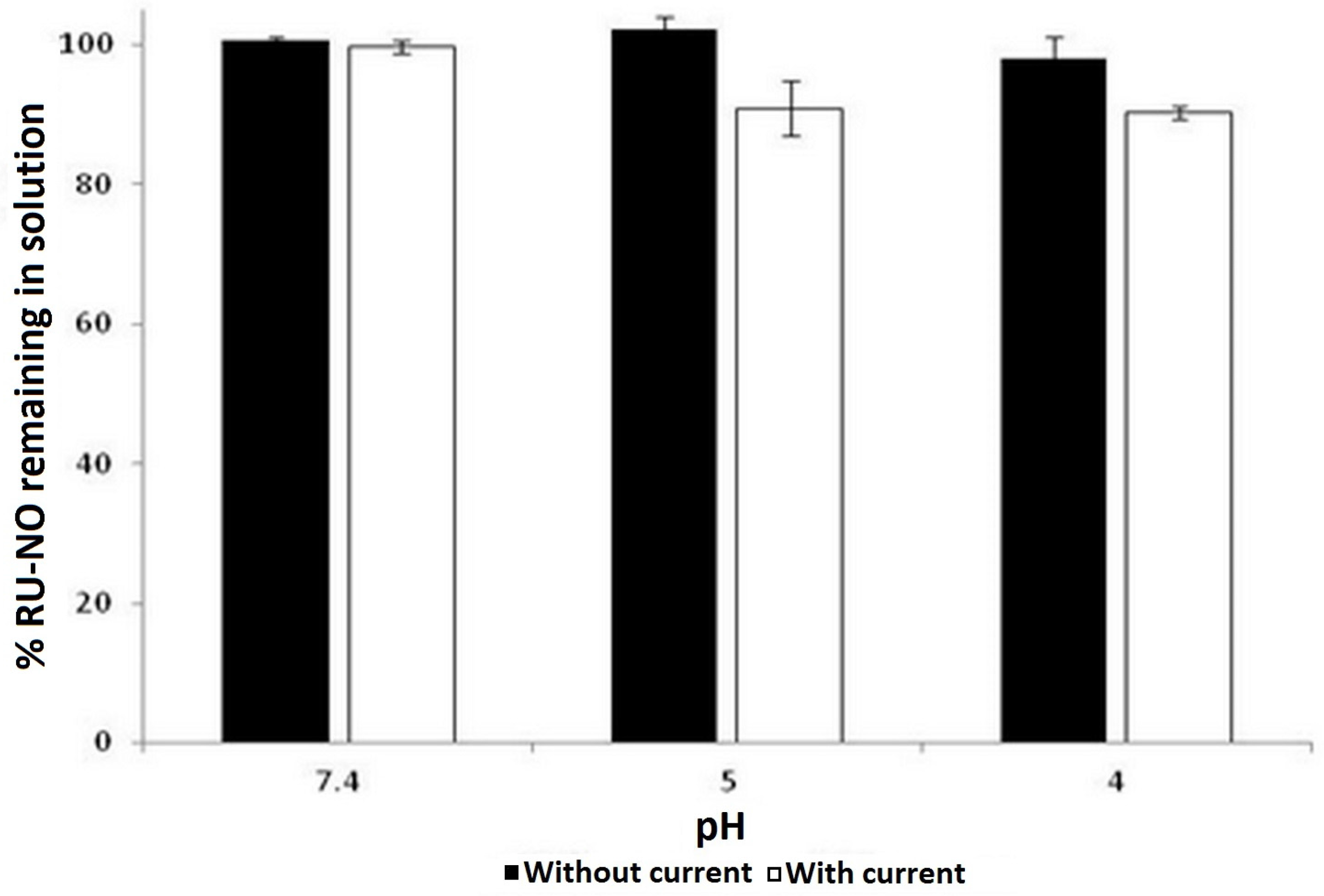
2.1. Ruthenium Complex Stability in Constant Low Intensity Electric Current
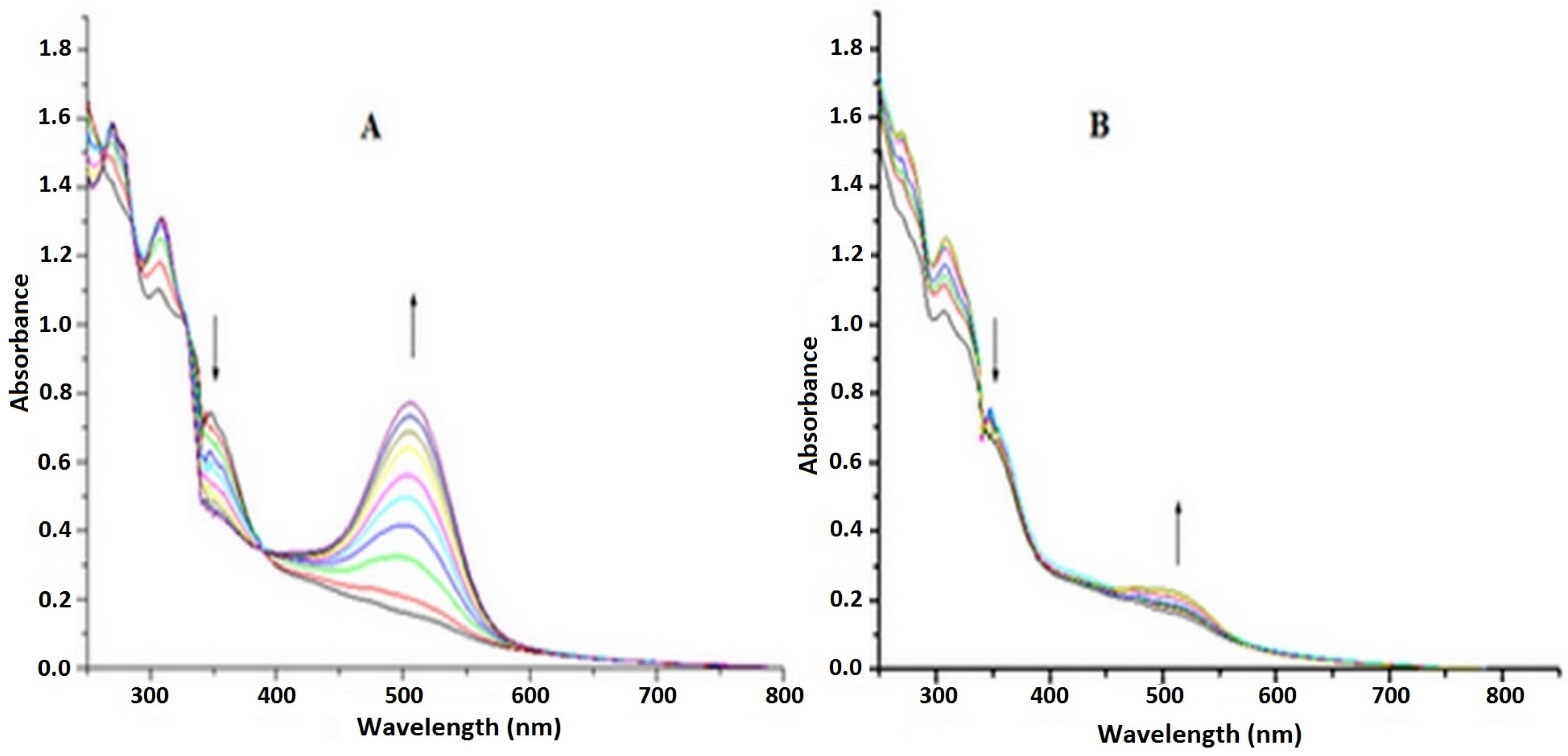
2.2. Irradiation of Ru-NO Complex
2.3. In Vitro Skin Permeation
2.4. NO Release in the Skin
3. Materials and Methods
3.1. Materials
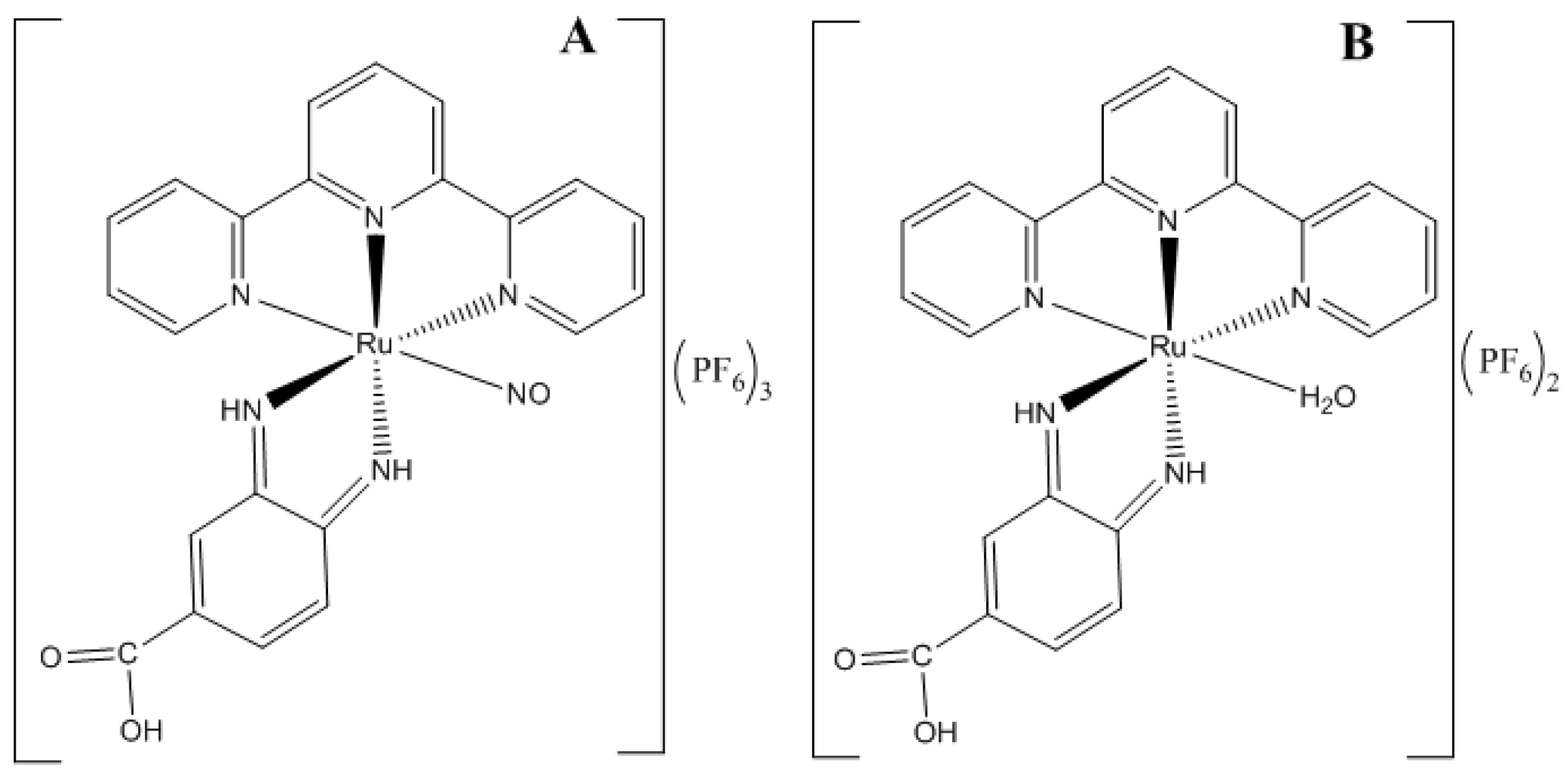
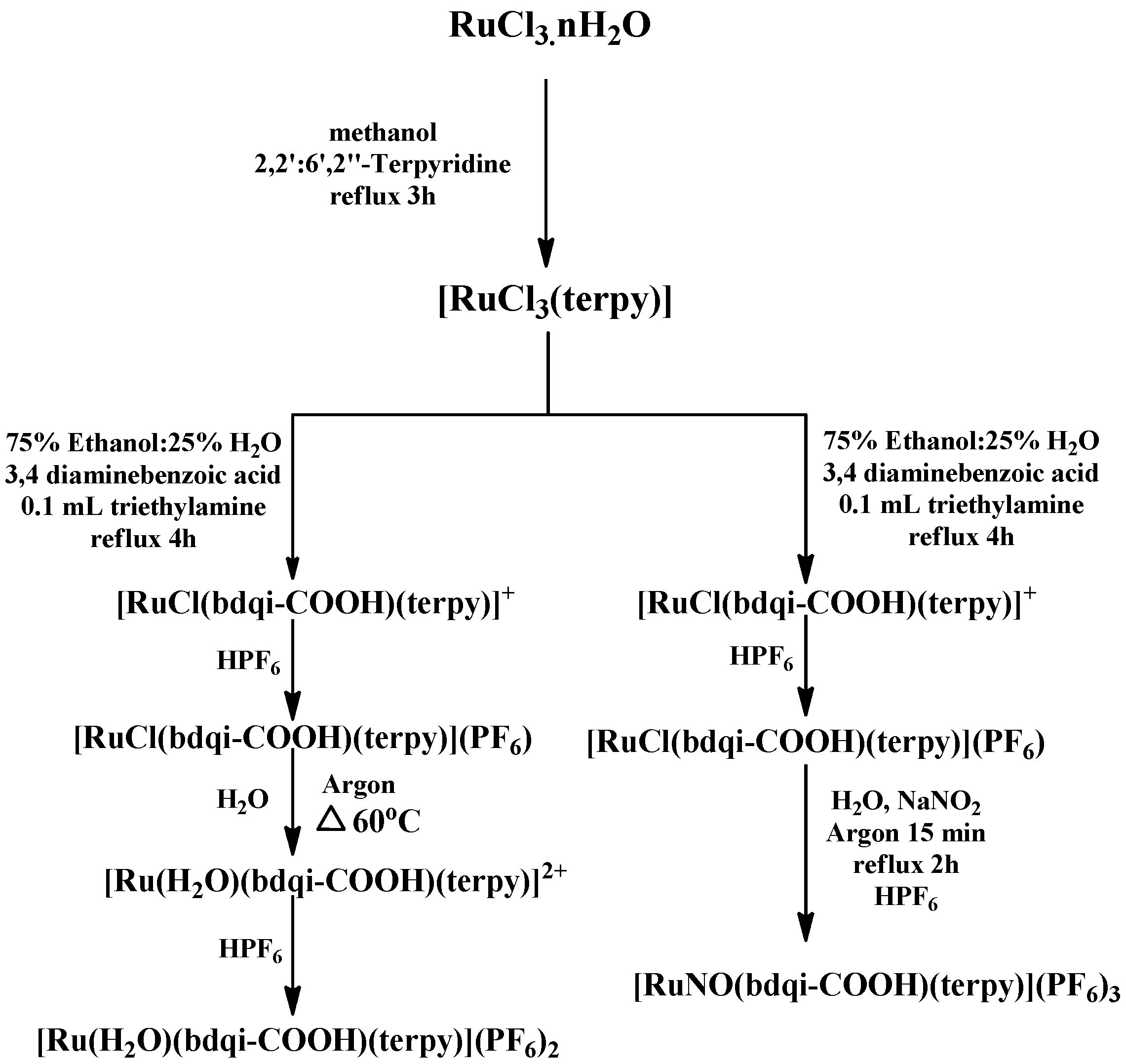
3.2. Synthesis and Characterization of Complexes
3.3. Constant Low Intensity Electric Current: Ruthenium Complex Stability
3.4. Ru-NO Complex Light Irradiation Studies
In Situ Determination of NO Release
3.5. In Vitro Skin Penetration
3.5.1. Skin Integrity Study
3.5.2. Skin Permeation Studies
3.5.3. Skin Retention Studies
3.6. Quantification of Ru-NO and Ru-Aqueous in Skin Penetration Experiments
3.6.1. ICP-MS
3.6.2. Total NO Release
3.7. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ma, D.L.; Ma, V.P.Y.; Chan, D.S.H.; Leung, K.H.; He, H.Z.; Leung, C.H. Recent advances in luminescent heavy metal complexes for sensing. Coord. Chem. Rev. 2012, 256, 3087–3113. [Google Scholar] [CrossRef]
- Li, C.Y.; Su, C.; Wang, H.H.; Kumaresan, P.; Hsu, C.H.; Lee, I.T.; Chang, W.C.; Tingare, Y.S.; Li, T.Y.; Lin, C.F.; et al. Design and development of cyclometalated ruthenium complexes containing thiophenyl-pyridine ligand for dye-sensitized solar cells. Dyes Pigments 2014, 100, 57–65. [Google Scholar] [CrossRef]
- Manikandan, R.; Prakash, G.; Kathirvel, R.; Viswanathamurthi, P. Ruthenium(II) carbonyl complexes bearing quinoline-based NNO tridentate ligands as catalyst for one-pot conversion of aldehydes to amides and o-allylation of phenols. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2013, 116, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.D.C.; Ford, P.C.; da Silva, R.S.; Bendhack, L.M. Ruthenium-nitrite complex as pro-drug releases NO in a tissue and enzyme-dependent way. Nitric Oxide 2011, 24, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Gambino, D.; Otero, L. Perspectives on what ruthenium-based compounds could offer in the development of potential antiparasitic drugs. Inorg. Chim. Acta 2012, 393, 103–114. [Google Scholar] [CrossRef]
- Bergamo, A.; Sava, G. Linking the future of anticancer metal-complexes to the therapy of tumour metastases. Chem. Soc. Rev. 2015, 44, 8818–8835. [Google Scholar] [CrossRef] [PubMed]
- Sava, G.; Gagliardi, R.; Bergamo, A.; Alessio, E.; Mestroni, G. Treatment of metastases of solid mouse tumours by NAMI-A: Comparison with cisplatin, cyclophosphamide and dacarbazine. Anti-Cancer Res. 1999, 19, 969–972. [Google Scholar]
- Sava, G.; Bergamo, A. Ruthenium-based compounds and tumour growth control (Review). Int. J. Oncol. 2000, 17, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Clavel, C.M.; Păunescu, E.; Nowak-Sliwinska, P.; Dyson, P.J. Thermoresponsive organometallic arene ruthenium complexes for tumour targeting. Chem. Sci. 2014, 5, 1097–1101. [Google Scholar] [CrossRef]
- Aitken, J.B.; Antony, S.; Weekley, C.M.; Lai, B.; Spiccia, L.; Harris, H.H. Distinct cellular fates for KP1019 and NAMI-A determined by X-ray fluorescence imaging of single cells. Metallomics 2012, 4, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- Leijen, S.; Burgers, S.A.; Baas, P.; Pluim, D.; Tibben, M.; van Werkhoven, E.; Alessio, E.; Sava, G.; Beijnen, J.H.; Schellens, J.H. Phase I/II study with ruthenium compound NAMI-A and gemcitabine in patients with non-small cell lung cancer after first line therapy. Investig. New Drugs 2015, 33, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Barry, N.P.; Zava, O.; Furrer, J.; Dyson, P.J.; Therrien, B. Anticancer activity of opened arene ruthenium metalla-assemblies. Dalton Trans. 2010, 39, 5272–5277. [Google Scholar] [CrossRef] [PubMed]
- Tfouni, E.; Truzzi, D.R.; Tavares, A.; Gomes, A.J.; Figueiredo, L.E.; Franco, D.W. Biological activity of ruthenium nitrosyl complexes. Nitric Oxide 2012, 26, 38–53. [Google Scholar] [CrossRef] [PubMed]
- Ignarro, L.J.; Buga, G.M.; Wood, K.S.; Byrns, R.E.; Chaudhuri, G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc. Natl. Acad. Sci. USA 1987, 84, 9265–9269. [Google Scholar] [CrossRef] [PubMed]
- Kiss, J.P. Role of nitric oxide in the regulation of monoaminergic neurotransmission. Brain Res. Bull. 2000, 52, 459–466. [Google Scholar] [CrossRef]
- Vallance, P.; Collier, J. Fortnightly review biology and clinical relevance of Nitric Oxide. Br. Med. J. 1994, 309, 453–457. [Google Scholar] [CrossRef]
- Ibiza, S.; Serrador, J.M. The role of nitric oxide in the regulation of adaptive immune responses. Inmunología 2008, 27, 103–117. [Google Scholar] [CrossRef]
- Muntané, J.; Angel, J.; Marín, L.M.; Padillo, F.J. Nitric oxide and cell death in liver cancer cells. Mitochondrion 2013, 13, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Shekhter, A.B.; Serezhenkov, V.A.; Rudenko, T.G.; Pekshev, A.V.; Vanin, A.F. Beneficial effect of gaseous nitric oxide on the healing of skin wounds. Nitric Oxide 2005, 12, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Rommel, S.A.; Sorsche, D.; Schonweiz, S.; Kübel, J.; Rockstroh, N.; Dietzek, B.; Streb, C.; Sven Rau, S. Visible-light sensitized photocatalytic hydrogen generation using a dual emissive heterodinuclear cyclometalated iridium(III)/ ruthenium(II) complex. J. Organomet. Chem. 2016, 821, 163–170. [Google Scholar] [CrossRef]
- Mohan, N.; Muthumari, S.; Ramesh, R. Synthesis, structure and anticancer activity of (η6-benzene) ruthenium(II) complexes containing aroylhydrazone ligands. J. Organomet. Chem. 2016, 807, 45–51. [Google Scholar] [CrossRef]
- Guy, R.H.; Kalia, Y.N.; Delgado-Charro, M.B.; Merino, V.; Lopez, A.; Marro, D. Iontophoresis: Electrorepulsion and electroosmosis. J. Control. Release 2000, 64, 129–132. [Google Scholar] [CrossRef]
- Kalia, Y.N.; Naik, A.; Garrison, J.; Guy, R.H. Iontophoretic drug delivery. Adv. Drug Deliv. Rev. 2004, 56, 619–658. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.N.; de Souza, J.G.; Simão, P.S.; Lopez, R.F.V. Iontophoresis Improved Growth Reduction of Invasive Squamous Cell Carcinoma in Topical Photodynamic Therapy. PLoS ONE 2016, 11, e0145922. [Google Scholar] [CrossRef] [PubMed]
- Huber, L.A.; Pereira, T.A.; Ramos, D.N.; Rezende, L.C.; Emery, F.S.; Sobral, L.M.; Leopoldino, A.M.; Lopez, R.F. Topical Skin Cancer Therapy Using Doxorubicin-Loaded Cationic Lipid Nanoparticles and Iontophoresis. J. Biomed. Nanotechnol. 2015, 11, 1975–1988. [Google Scholar] [CrossRef] [PubMed]
- De Lima, R.G.; Sauaia, M.G.; Bonaventura, D.; Tedesco, A.C.; Bendhack, L.M.; da Silva, R.S. Influence of ancillary ligand L in the nitric oxide photorelease by the [Ru(L)(tpy)NO]3+ complex and its vasodilator activity based on visible light irradiation. Inorg. Chim. Acta 2006, 359, 2543–2549. [Google Scholar] [CrossRef]
- De Santana, D.C.; Pupo, T.T.; Sauaia, M.G.; da Silva, R.S.; Lopez, R.F. Nitric oxide photorelease from hydrogels and from skin containing a nitro-ruthenium complex. Int. J. Pharm. 2010, 391, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Kelland, L. The resurgence of platinum-based cancer chemotherapy. Nat. Rev. Cancer 2007, 7, 573–584. [Google Scholar] [CrossRef] [PubMed]
- De Lima, R.G.; Sauaia, M.G.; Ferezin, C.; Pepe, I.M.; José, N.M.; Bendhack, L.M.; da Rocha, Z.N.; da Silva, R.S. Photochemical and pharmacological aspects of nitric oxide release from some nitrosyl ruthenium complexes entrapped in sol–gel and silicone matrices. Polyhedron 2007, 26, 4620–4624. [Google Scholar] [CrossRef]
- Kudo, S.; Bourassa, J.L.; Boggs, S.E.; Sato, Y.; Ford, P.C. In Situ Nitric Oxide (NO) Measurement by Modified Electrodes: NO Labilized by Photolysis of Metal Nitrosyl Complexes. Anal. Biochem. 1997, 247, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Ford, P.C.; Wink, D.A.; Stanbury, D.M. Autoxidation kinetics of aqueous nitric oxide. FEBS Lett. 1993, 326, 1–3. [Google Scholar] [CrossRef]
- Abla, N.; Naik, A.; Guy, R.H.; Kalia, N.Y. Effect of Charge and Molecular Weight on Transdermal Peptide Delivery by Iontophoresis. Pharm. Res. 2006, 22, 2069–2078. [Google Scholar] [CrossRef] [PubMed]
- Santi, P.; Guy, R.H. Reverse iontophoresis—Parameters determining electroosmotic flow: I. pH and ionic strength. J. Control. Release 1996, 38, 159–165. [Google Scholar] [CrossRef]
- Lopez, R.F.; Bentey, M.V.; Delgado-Charro, M.B.; Guy, R.H. Iontophoretic delivery of 5-aminolevulinic acid (ALA): Effect of pH. Pharm. Res. 2001, 18, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Coneski, P.N.; Schoenfisch, M.H. Nitric oxide release: Part III. Measurement and reporting. Chem. Soc. Rev. 2012, 41, 3753–3758. [Google Scholar] [CrossRef] [PubMed]
- Feelisch, M.; Rassaf, T.; Mnaimneh, S.; Singh, N.; Bryan, N.S.; Jourd’heuil, D.; Kelm, M. Concomitant S-, N-, and heme-nitros (yl) ation in biological tissues and fluids: Implications for the fate of NO in vivo. FASEB J. 2002, 16, 1775–1785. [Google Scholar] [CrossRef] [PubMed]
- Ignarro, L.J. Nitric oxide: A unique endogenous signaling molecule in vascular biology. Biosci. Rep. 1999, 19, 51–71. [Google Scholar] [CrossRef] [PubMed]
- Kolb-Bachofen, V.; Fehsel, K.; Michel, G.; Ruzicka, T. Epidermal keratinocyte expression of inducible nitric oxide synthase in skin lesions of psoriasis vulgaris. Lancet 1994, 344, 139. [Google Scholar] [CrossRef]
- Sauaia, M.G.; de Lima, R.G.; Tedesco, A.C.; da Silva, R.S. Nitric oxide production by visible light irradiation of aqueous solution of nitrosyl ruthenium complexes. Inorg. Chem. 2005, 44, 9946–9951. [Google Scholar] [CrossRef] [PubMed]
- Seto, J.E.; Polat, B.E.; Lopez, R.F.; Blankschtein, D.; Langer, R. Effects of ultrasound and sodium lauryl sulfate on the transdermal delivery of hydrophilic permeants: Comparative in vitro studies with full-thickness and split-thickness pig and human skin. J. Control. Release 2010, 145, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Green, P.G.; Hinz, R.S.; Kim, A.; Szoka, F.C., Jr.; Guy, R.H. Lontophoretic Delivery of a Series of Tripeptides Across the Skin in Vitro. Pharm. Res. 1991, 8, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Gelfuso, G.M.; Barros, M.A.O.; Delgado-Charro, M.B.; Guy, R.H.; Lopez, R.F.V. Iontophoresis of minoxidil sulphate loaded microparticles, a strategy for follicular drug targeting? Colloids Surf. B Biointerfaces 2015, 134, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Nardi, E.P.; Evangelista, F.S.; Tormen, L.; Saint, T.D.; Curtius, A.J.; de Souza, S.S.; Barbosa, F. The use of inductively coupled plasma mass spectrometry (ICP-MS) for the determination of toxic and essential elements in different types of food samples. Food Chem. 2009, 112, 727–732. [Google Scholar] [CrossRef]
- Sample Availability: Samples of the compounds Ru-NO and Ru aqueous are available from the authors.




| Ru Complex | Passive (nmol·L−1·cm−2) | Iontophoresis (nmol·L−1·cm−2) |
|---|---|---|
| Ru-NO | 0.1 ± 0.1 | 1.5 ± 0.2 |
| Ru-aqueous | 0.2 ± 0.0 | 91 ± 33 |
| Donor Solution | Total Concentration of NO * (nmol·L−1·cm−2) | ||
|---|---|---|---|
| SC | VE | RS | |
| Control ** | 4 ± 1 | 15 ± 1 | 4 ± 3 |
| Ru-NO | 18 ± 0 | 18 ± 2 | 4 ± 3 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Santana, D.C.A.S.; Dias, K.; Souza, J.G.; Ogunjimi, A.T.; Souza, M.C.; Silva, R.S.; Lopez, R.F.V. NO Exchange for a Water Molecule Favorably Changes Iontophoretic Release of Ruthenium Complexes to the Skin. Molecules 2017, 22, 104. https://doi.org/10.3390/molecules22010104
De Santana DCAS, Dias K, Souza JG, Ogunjimi AT, Souza MC, Silva RS, Lopez RFV. NO Exchange for a Water Molecule Favorably Changes Iontophoretic Release of Ruthenium Complexes to the Skin. Molecules. 2017; 22(1):104. https://doi.org/10.3390/molecules22010104
Chicago/Turabian StyleDe Santana, Danielle C. A. S., Karina Dias, Joel G. Souza, Abayomi T. Ogunjimi, Marina C. Souza, Roberto S. Silva, and Renata F. V. Lopez. 2017. "NO Exchange for a Water Molecule Favorably Changes Iontophoretic Release of Ruthenium Complexes to the Skin" Molecules 22, no. 1: 104. https://doi.org/10.3390/molecules22010104
APA StyleDe Santana, D. C. A. S., Dias, K., Souza, J. G., Ogunjimi, A. T., Souza, M. C., Silva, R. S., & Lopez, R. F. V. (2017). NO Exchange for a Water Molecule Favorably Changes Iontophoretic Release of Ruthenium Complexes to the Skin. Molecules, 22(1), 104. https://doi.org/10.3390/molecules22010104







