Transdermal Drug Delivery Enhancement by Compounds of Natural Origin
Abstract
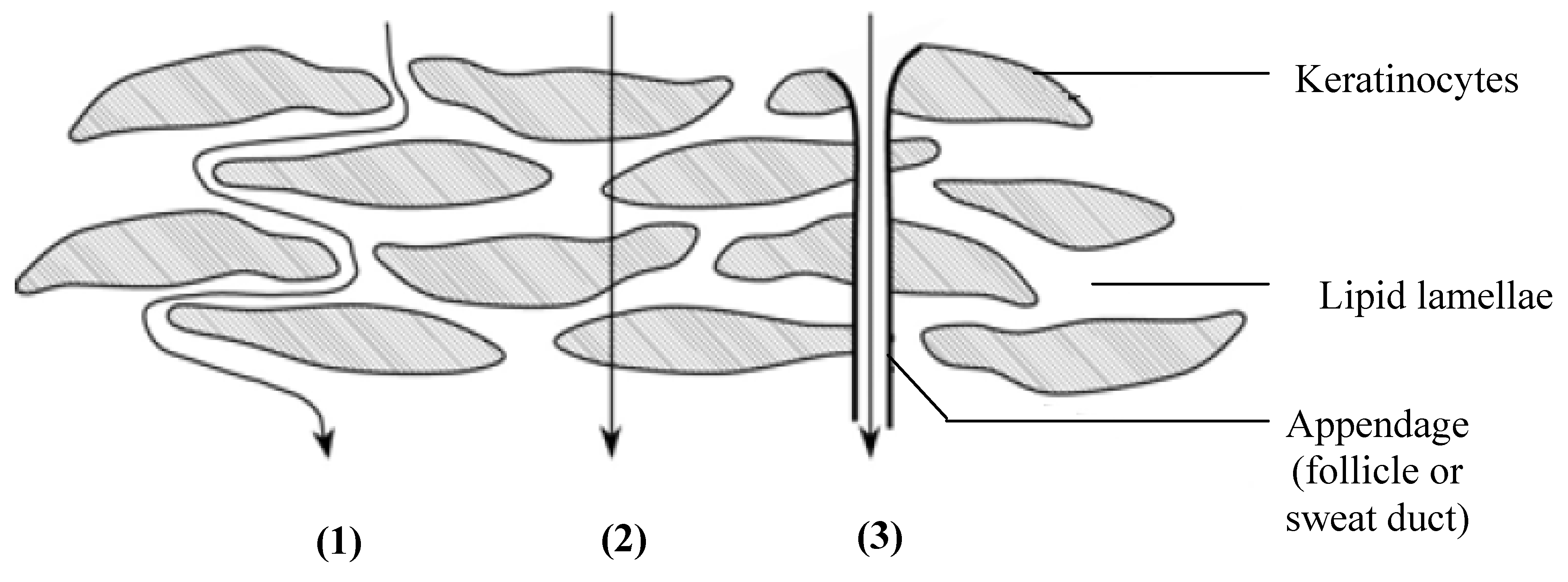
:1. Introduction
2. Essential Oils
| Essential oils | Fixed oils/Fatty acids |
|---|---|
| Distilled from different plant parts | Pressed from seeds |
| Very important to the plant’s life processes, although not involved in seed germination and early growth | Not so important for the plant’s life processes, although it is needed for seeds to germinate and sprout |
| Relatively small molecules built from rings and short chains | Relatively large molecules with large molecular sizes built from long carbohydrate chains |
| Volatile and aromatic | Non-volatile and non-aromatic |
| Circulate all through the plants and can diffuse through tissues, cell walls and membranes | Do not circulate in plants, diffuse through tissues or cell walls and membranes |
| Does not rot or go stale | Can rot and go stale |
| Can be anti-septic, anti-parasitic, anti-viral, anti-fungal and anti-bacterial | No anti-septic, anti-parasitic, anti-viral, |anti-fungal and anti-bacterial functions |
- – nitrogen- and sulphur-containing compounds (e.g., allyl isothiocyanate found in mustard oil);
- – aromatic compounds, which are benzene derivatives (e.g., eugenol which is the main constituent of clove oil);
- – terpenes (e.g., 1,8-cineole in eucalyptus oil) and terpenoids; and
- – miscellaneous compounds (includes long-chain unbranched substances).
2.1. Niaouli Oil
2.2. Eucalyptus Oil
| Source of eucalyptus essential oil | Key constituents |
|---|---|
| Eucalyptus citriodora | Citronellal (75–85%) |
| Neo-isopulegol and isopulegol (0–10%) | |
| Eucalyptus dives | α- and β-Phellandrene (23–30%) |
| Piperitone (35–45%) | |
| p-Cymene (6–10%) | |
| α-Thujene (2–6%) | |
| Terpinene-4-ol (3–6%) | |
| Eucalyptus globules | 1,8-Cineole (58–80%) |
| α-Pinene (10–22%) | |
| Limonene (1–8%) | |
| p-Cymene (1–5%) | |
| trans-Pinocarveol (1–5%) | |
| Aromadendrene (1–5%) | |
| Globulol (0.5–1.5%) | |
| Eucalyptus polybractea | 1,8-Cineole (60–80%) |
| l-Limonene (1–5%) | |
| p-Cymene (1–2%) | |
| α-Pinene (1–2%) | |
| Eucalyptus radiata | Eucalyptol (60–75%) |
| α-Terpineol (5–10%) | |
| l-Limonene (4–8%) | |
| α-Pinene (8–12%) |
2.3. Alpinia oxyphylla Oil
2.4. Turpentine Oil
2.5. Sweet Basil and Tulsi Oil
2.6. Cardamom Oil
2.7. Peppermint Oil
2.8. Fennel Oil
2.9. Black Cumin Oil
3. Terpenes
| Number of isoprene units | Number of carbon atoms | |
|---|---|---|
| Monoterpenes | 2 | C10 |
| Sesquiterpenes | 3 | C15 |
| Diterpenes | 4 | C20 |
| Sesterterpenes | 5 | C25 |
| Triterpenes | 6 | C30 |
| Tetraterpenes | 8 | C40 |
| Polyterpenes | >8 | >C40 |
| Class | Example(s) of terpene | Source |
|---|---|---|
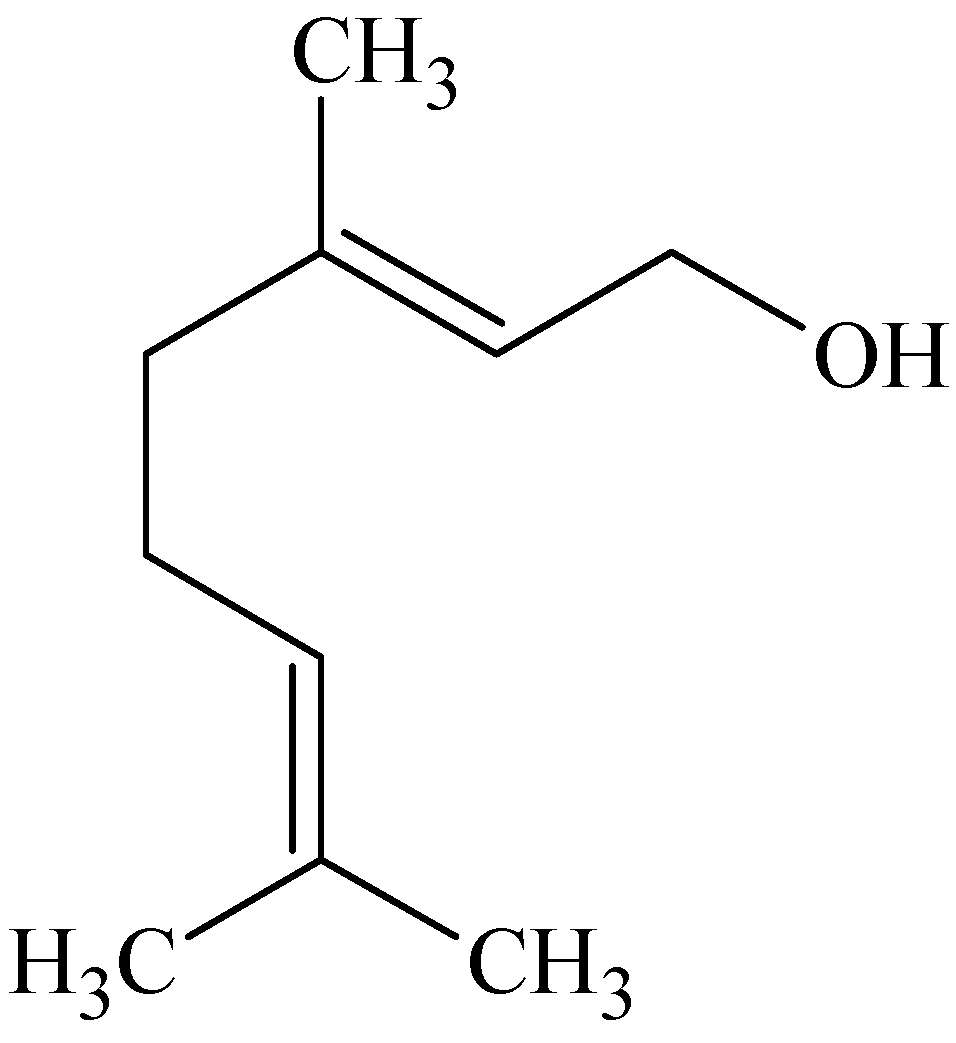
| ACYCLIC MONOTERPENES (Alcohols) | Geraniol and nerol | Geraniol is an unsaturated primary alcohol found in geranium and other essential oils. It is found as esters and as a glucoside, but mainly occurs in the free form. Nerol is the isomeric alcohol and is found in various essential oils, primarily in neroli and bergamot oils [22,41]. Palmarosa oil contains more geraniol than any other oil and for nerol it is catnip and rose oil [23]. |
| Linalol | Linalol is found as (+)- and (−)-forms in the oil of Linaloe (a plant found in Central America), but can also be found free and as esters in numerous other essential oils [22]. Rosewood oil contains more linalol than any other oil [23]. | |
| MONOCYCLIC MONOTERPENES (Hydrocarbons) | Limonene | The optically active limonene is widespread in nature and is found in its (+)- and (−)-forms in various essential oils such as bergamot, caraway, lemon and orange oils [22,41]. The signature oils for d-limonene and l-limonene is grapefruit and fleabane, respectively [23]. |
| MONOCYCLIC MONOTERPENES (Alcohols) Alcohols related to α-terpineol | α-Terpineol | Found in many essential oils such as camphor, neroli and petitgrain oil [22]. The signature oil is lemon eucalyptus [23]. |
| β-Terpineol | Isomeric with α-terpineol, but is not isolated from natural sources. Found in commercial terpineol [22]. | |
| γ-Terpineol | Second isomer of α-terpineol and is found in at least one essential oil and commercial terpineol [22]. | |
| MONOCYCLIC MONOTERPENES (Alcohols) Alcohols derived from thymol | Menthol | Menthol is a constituent of numerous peppermint oils and is found as its (−)-form [22,23]. |
| MONOCYCLIC MONOTERPENES (Alcohols) Alcohols derived from carvacrol | Carveol | Carveol is found in caraway oil [22,23]. |
| MONOCYCLIC MONOTERPENES (Ketones) Ketones related to menthone | Menthone | (−)-form is found in numerous peppermint oils, (+)-form also occurs naturally [22,41]. |
| Pulegone | Found in pennyroyal and many other essential oils as its (+)-form [22]. | |
| iso-Pulegone | Often an accompaniment of pulegone in essential oils [22]. | |
| Piperitone | Occurs in numerous eucalyptus oils as (+)- and (−)-forms [22]. | |
| MONOCYCLIC MONOTERPENES (Ketones) Ketones related to carvomenthone | Carvomenthone | Isomeric with menthone and is a saturated ketone. (−)-Form is found in numerous essential oils [22]. |
| Carvone Unsaturated ketone | Occurs in its (+)-, (−)- and (±)-forms and is the main constituent of caraway and dill oils [22]. It can also be found in spearmint oil [41]. | |
| MONOCYCLIC MONOTERPENES (Oxides) | 1,8-Cineole | Widespread in essential oils, particularly in eucalyptus and wormseed oil [22,41]. |
| BICYCLIC MONOTERPENES (Hydrocarbons) | α-Thujene | Found in numerous essential oils [22]. |
| BICYCLIC MONOTERPENES (Hydrocarbons) | Car-3-ene | Found in several turpentine oils [22]. |
| BICYCLIC MONOTERPENES (Hydrocarbons) | α-Pinene | Widespread in nature, found in most essential oils of Coniferae. It is the main constituent of turpentine oil. Secreted by conifers, turpentine oil consists of resinous material dissolved in turpentine oil [22]. |
| β-Pinene (Nopinene) | Isomeric with α-pinene [22]. Its signature oil is galbanum [23]. | |
| BICYCLIC MONOTERPENES (Oxygenated derivatives) | Verbenol, verbenone and verbanone | Verbenol and verbenone has been found in nature, with the latter being found in verbena oil [22]. The signature oil for verbenone is rosemary verbenone [23]. |
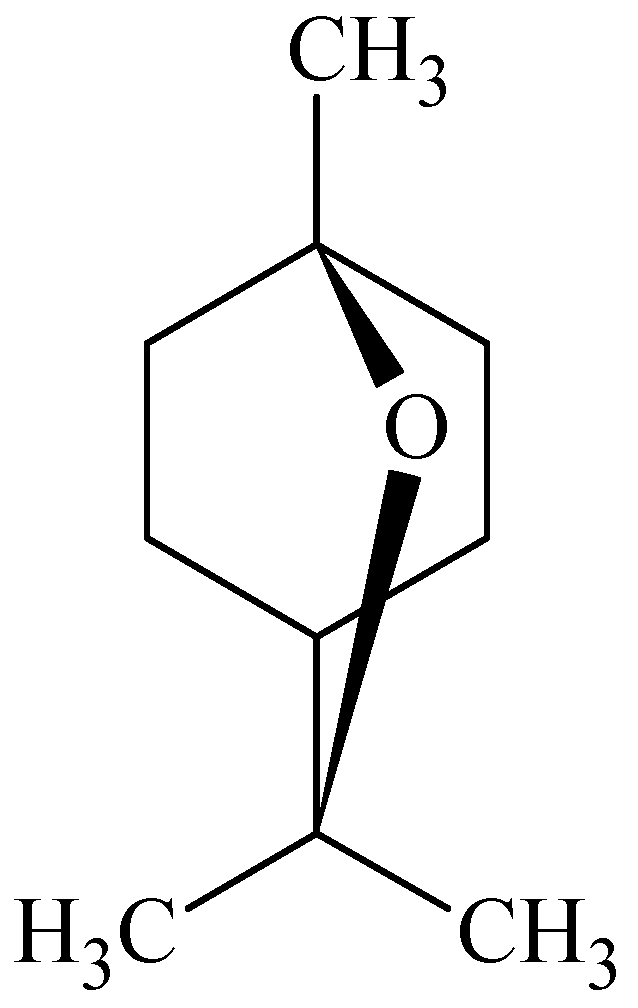
| BICYCLIC MONOTERPENES (Ketones – camphane group) | Camphor | Not widely distributed in nature, is the major constituent of camphor oil, obtained from the leaves and wood of the camphor tree (Cinnamomum camphora) [22]. |
| BICYCLIC MONOTERPENES (Ketones – fenchane group | Fenchone | Occurs as the optically active forms in fennel, thuja and cedar leaf oils [22,23]. |
| SESQUITERPENES (Alcohol) | Farnesol | Widely distributed in flower oils, in particular those of the acacia, cyclamen and the rose [22]. |
| Nerolidol | Isomeric with farnesol and found in neroli oil [22]. | |
| (−)-Guaiol | A crystalline alcohol found in guaiacum wood oil [22]. | |
| (+)-Cedrol | Cedarwood oil [45]. | |
| (−)-α-Bisabolol | Camomile oil [45]. | |
| SESQUITERPENES (Hydrocarbon) | Bisabolene | Widespread in nature, found in bergamot and myrrh oils. Also in many other essential oils [22]. |
| The Azulenes | All hydrocarbons are derived from azulene (C10H8), a parent hydrocarbon. Most of those attained from natural origin have the molecular formula C15H18. Azulenes is responsible for the blue color of certain essential oils, or when essential oils become blue/violet when undergoing processes which might result in dehydrogenation [22]. | |
| (Unsaturated hydrocarbons) | ||
| (+)-Longifolene | Tricyclic sesquiterpene found in the essential oil of Pinus longifolia [22]. | |
| β-Caryophyllene | Main hydrocarbon constituent of clove oil [22]. | |
| (+)-Aromadendrene | Eucalyptus oil [45]. | |
| (+)-β-Cedrene | Cedarwood oil [45]. | |
| ACYCLIC DITERPENES (Alcohol) | Phytol | Found in rosemary oil [22,23]. |
| ACYCLIC TRITERPENES (Hydrocarbon) | Squalene | It is found in the unsaponifiable fraction of shark liver oil and in several plant sources such as vegetable oils and several fungi [22]. Jasmine is the signature oil [23]. |
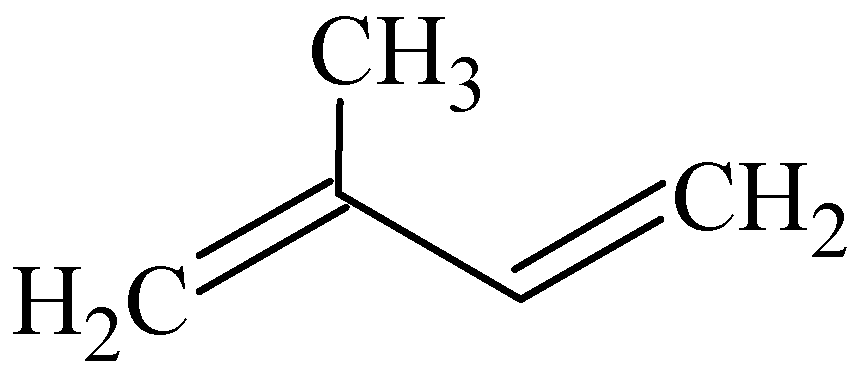
3.1. Limonene
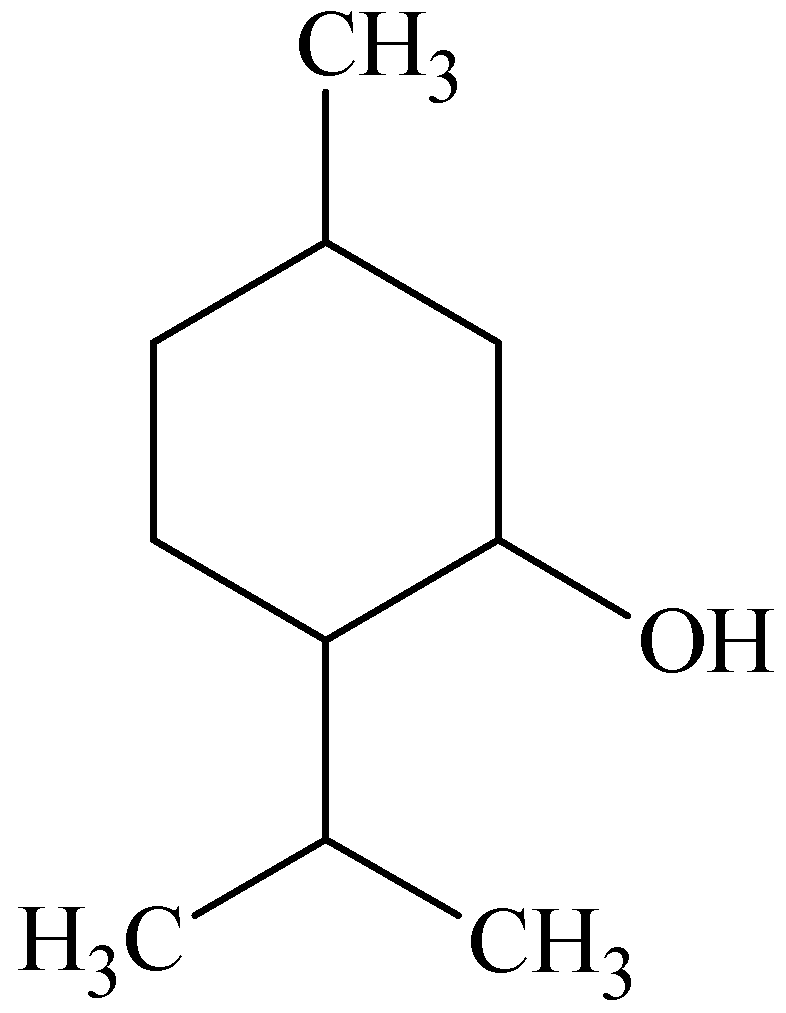
3.2. Menthol

3.3. 1-8-Cineole
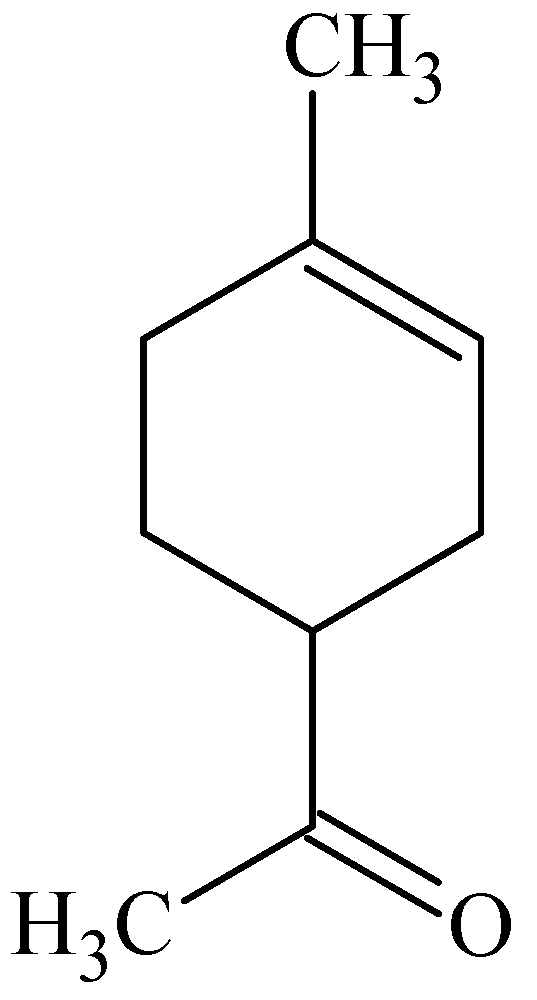
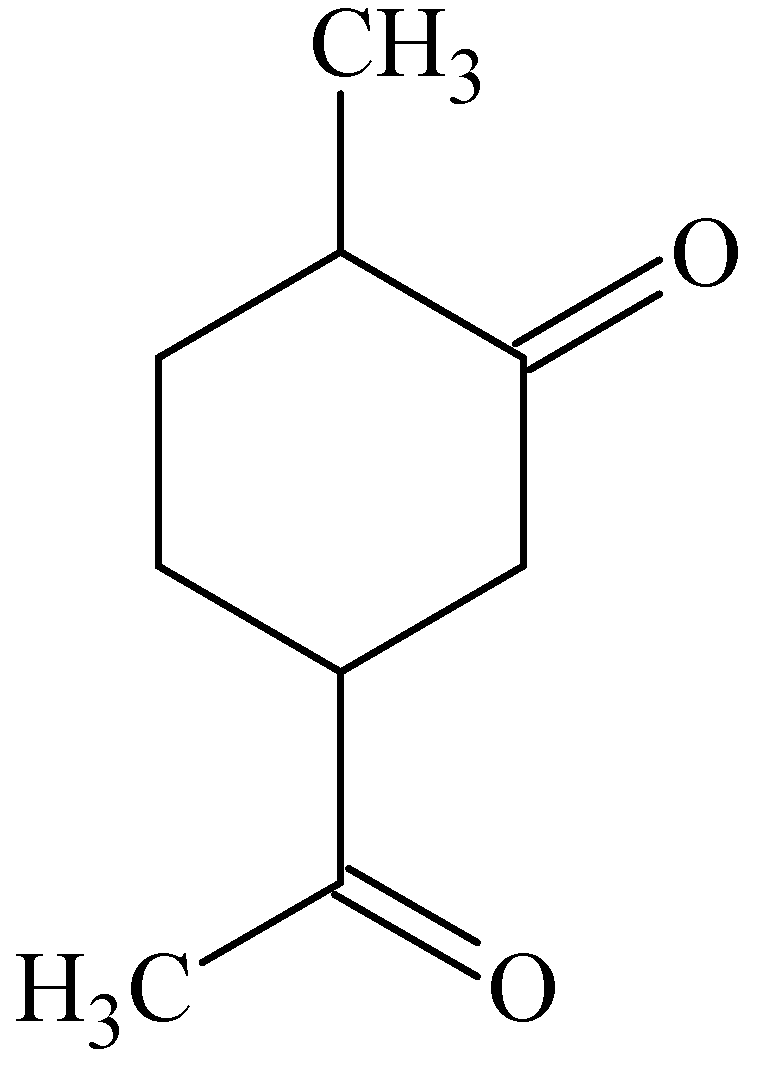
3.4. Carvone
3.5. Geraniol
3.6. Sesquiterpenes
- – Hydrocarbons: (+)-longifolene, β-caryophyllene, (+)-aromadendrene and (+)-β-cedrene;
- – Alcohols: (−)-isolongifolol (synthetic derivative), (−)-guaiol, (+)-cedrol, (−)-α-bisabolol, farnesol and nerolidol;
- – Others/miscellaneous: β-caryophyllene oxide and (+)-cedryl acetate which are both synthetic derivatives.
4. Fixed Oils/Fatty Acids
4.1. Fish Oil
4.2. Fatty Acids from Algae
4.3. Phospholipids
4.4. Vesicular Carriers
5. Polysaccharides
5.1. Chitosan and Derivatives
5.2. Aloe vera Gel/Juice
6. Miscellaneous
6.1. Capsaicin

6.2. Vitamin E
7. Conclusions
Acknowledgements
References
- Mezei, M. Liposomes as penetration promoters and localizers of topically applied drugs. In Drug Permeation Enhancement: Theory and Applications; Hsieh, D.S., Ed.; Marcel Dekker: New York, NY, USA, 1994; pp. 171–198. [Google Scholar]
- Ghafourian, T.; Samaras, E.G.; Brooks, J.D.; Riviere, J.E. Validated models for predicting skin penetration from different vehicles. Eur. J. Pharm. Sci. 2010, 41, 612–616. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Leu, Y.-L.; Hwang, T.-L.; Chen, H.-C.; Hung, C.-F. Development of sesquiterpenes from alpinia oxyphylla as novel skin permeation enhancers. Eur. J. Pharm. Sci. 2003, 19, 253–262. [Google Scholar] [CrossRef]
- Shah, V.P. Skin penetration enhancers: Scientific perspectives. In Drug Permeation Enhancement: Theory and Applications; Hsieh, D.S., Ed.; Marcel Dekker: New York, NY, USA, 1994; pp. 19–23. [Google Scholar]
- Cornwell, P.A.; Barry, B.W.; Bouwstra, J.A.; Gooris, G.S. odes of action of terpene penetration enhancers in human skin; Differential scanning calorimetry, small-angle X-ray diffraction and enhancer uptake studies. Int. J. Pharm. 1996, 127, 9–26. [Google Scholar] [CrossRef]
- Hadgraft, J. Skin deep. Eur. J. Pharm. Biopharm. 2004, 58, 291–299. [Google Scholar] [CrossRef]
- Hadgraft, J. Skin, the final frontier. Int. J. Pharm. 2001, 224, 1–18. [Google Scholar] [CrossRef]
- Hsieh, D.S. Understanding permeation enhancement technologies. In Drug Permeation Enhancement: Theory and Applications; Hsieh, D.S., Ed.; Marcel Dekker: New York, NY, USA, 1994; pp. 3–17. [Google Scholar]
- Law, S.; Wertz, P.W.; Swartzendruber, D.C.; Squier, C.A. Regional variation in content, composition and organisation of porcine epithelial barrier lipids revealed by thin-layer chromatography and transmission electron microscopy. Arch. Oral Biol. 1995, 40, 1085–1091. [Google Scholar] [CrossRef]
- Chen, H.-C.; Mendelsohn, R.; Rerek, M.E.; Moore, D.J. Fourier transform infrared spectroscopy and differential scanning calorimetry studies of fatty acid homogeneous ceramide 2. Biochim. Biophys. Acta 2000, 1468, 293–303. [Google Scholar] [CrossRef]
- Moore, D.J.; Rerek, M.E. Insights into the molecular organisation of lipids in the skin barrier from infrared spectroscopy studies of stratum corneum lipid models. Acta Derm. Venereol. 2000, 298, 16–22. [Google Scholar] [CrossRef]
- Ho, C.K. Probabilistic modeling of percutaneous absorption for risk-based exposure assessments and transdermal drug delivery. Stat. Methodol. 2004, 1, 47–69. [Google Scholar] [CrossRef]
- Roy, S.D. Preformulation aspects of transdermal drug delivery systems. In Transdermal and Topical Drug Delivery Systems; Ghosh, T.K., Pfister, W.R., Yum, S.I., Eds.; Interpharm Press: Buffalo Grove, IL, USA, 1997; pp. 139–166. [Google Scholar]
- Naik, A.; Kalia, Y.N.; Guy, R.H. Transdermal drug delivery: Overcoming the skin’s barrier function. Pharm. Sci. Tech. Today 2000, 3, 318–325. [Google Scholar] [CrossRef]
- Behl, C.R.; Char, H.; Patel, S.B.; Mehta, D.B.; Piemontese, D.; Malick, A.W. In vivo and in vitro skin uptake and permeation studies: Critical considerations and factors which affect them. In Topical Drug Bioavailability, Bioequivalence, and Penetration; Shah, V.P., Maibach, H.I., Eds.; Plenum Press: New York, NY, USA, 1993; pp. 225–259. [Google Scholar]
- Hadgraft, J.; Williams, D.G.; Allan, G. Azone®: Mechanisms of action and clinical effect. In Pharmaceutical Skin Penetration Enhancement; Walters, K.A., Hadgraft, J., Eds.; Marcel Dekker: New York, NY, USA, 1993; pp. 175–197. [Google Scholar]
- Charoo, N.A.; Shamsher, A.A.A.; Kohli, K.; Pillai, K.; Rahman, K. Improvement in bioavailability of transdermally applied flurbiprofen using tulsi (ocinum sanctum) and turpentine oil. Colloid. Surface. B 2008, 65, 300–307. [Google Scholar] [CrossRef]
- Walker, R.B.; Smith, E.W. The role of percutaneous penetration enhancers. Adv. Drug Deliver. Rev. 1996, 18, 295–301. [Google Scholar] [CrossRef]
- Thomas, B.J.; Finnin, B.C. The transdermal revolution. Drug Discov. Today 2004, 9, 697–703. [Google Scholar] [CrossRef]
- Foldvari, M. Non-invasive administration of drugs through the skin: challenges in delivery system design. Pharm. Sci. Technol. Today 2000, 3, 417–425. [Google Scholar] [CrossRef]
- Barry, B.W. Lipid-protein-partitioning theory of skin penetration enhancement. J. Control. Release 1991, 15, 237–248. [Google Scholar] [CrossRef]
- Pinder, A.R. The Chemistry of the Terpenes; Wiley: New York, NY, USA, 1960; pp. 1–223. [Google Scholar]
- Stewart, D. The Chemistry of Essential Oils Made Simple: God’s Love Manifest in Molecules; Care Publications: Marble Hill, MO, USA, 2005; pp. 55–591. [Google Scholar]
- Essential Science Publishing, Essential Oils: Desk Reference, 3rd ed; Essential Science Publishing: Orem, UT, USA, 2006; pp. 1–75.
- Betts, T.J. Chemical characterisation of the different types of volatile oil constituents by various solute retention ratios with the use of conventional and novel commercial gas chromatographic stationary phases. J. Chromatog. A 2001, 936, 33–46. [Google Scholar] [CrossRef]
- Dudareva, N.; Pichersky, E.; Gershenzon, J. Biochemistry of plant volatiles. Plant Physiol. 2004, 135, 1893–1902. [Google Scholar] [CrossRef]
- Monti, D.; Chetoni, P.; Burgalassi, S.; Najarro, M.; Fabrizio Saettone, M.; Boldrini, E. Effect of different terpene-containing essential oils on permeation of estradiol through hairless mouse skin. Int. J. Pharm. 2002, 237, 209–214. [Google Scholar] [CrossRef]
- Monti, D.; Tampucci, S.; Chetoni, S.; Burgalassi, S.; Bertoli, A.; Pistelli, L. Niaouli oils from different sources: Analysis and influence on cutaneous permeation of estradiol in vitro. Drug Deliv. 2009, 16, 237–242. [Google Scholar] [CrossRef]
- Williams, A.C.; Barry, B.W. Essential oils as novel human skin penetration enhancers. Int. J. Pharm. 1989, 57, R7–R9. [Google Scholar] [CrossRef]
- Williams, A.C.; Barry, B.W. Terpenes and the lipid-protein-partitioning theory of skin penetration enhancement. Pharmaceut. Res. 1991, 8, 17–24. [Google Scholar] [CrossRef]
- Karpanen, T.J.; Conway, B.R.; Worthington, T.; Hilton, A.C.; Elliott, T.S.J.; Lambert, P.A. Enhanced chlorhexidine skin penetration with eucalyptus oil. BMC Infect. Dis. 2010, 10, 278. [Google Scholar] [CrossRef]
- Lee, E.; Park, K.-K.; Lee, J.-M.; Chun, K.-S.; Kang, J.-Y.; Lee, S.-S.; Surh, Y.-J. Suppression of mouse tumor promotion and induction of apoptosis in HL-60 cells by Alpinia oxyphylla Miquel (Zingiberaceae). Carcinogenesis 1998, 19, 1377–1381. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Leu, Y.-L.; Hwang, T.-L.; Cheng, H.-C. Essential oils from sweet basil (ocimum basilicum) as novel enhancers to accelerate transdermal drug delivery. Biol. Pharm. Bull. 2004, 27, 1819–1825. [Google Scholar] [CrossRef]
- Jain, R.; Aqil, M.; Ahad, A.; Ali, A.; Khar, R.K. Basil oil is a promising skin penetration enhancer for transdermal delivery of labetolol hydrochloride. Drug Dev. Ind. Pharm. 2008, 34, 384–389. [Google Scholar] [CrossRef]
- Yamahara, J.; Kashiwa, H.; Kishi, K.; Fujimura, H. Dermal penetration enhancement by crude drugs: In vitro skin permeation of prednisolone enhanced by active constituents in cardamom seed. Chem. Pharm. Bull. 1989, 37, 855–856. [Google Scholar] [CrossRef]
- Huang, Y.-B.; Wu, P.-C.; Ko, H.-M.; Tsai, Y.-H. Cardamom oil as a skin permeation enhancer for indomethacin, piroxicam and diclofenac. Int. J. Pharm. 1995, 126, 111–117. [Google Scholar] [CrossRef]
- Huang, Y.-B.; Wu, P.-C.; Ko, H.-M.; Tsai, Y.-H. Effect of pretreatment by cardamom oil on in vivo percutaneous absorption of piroxicam gel: Pharmacokinetic analysis in rabbits. Int. J. Pharm. 1996, 134, 183–191. [Google Scholar] [CrossRef]
- Nielsen, J.B. Natural oils affect the human skin integrity and percutaneous penetration of benzoic acid dose-dependently. Basic Clin. Pharmacol. Toxicol. 2006, 98, 575–581. [Google Scholar] [CrossRef]
- Das, M.K.; Bhattacharya, A.; Ghosal, S.K. Effect of different terpene-containing essential oils on percutaneous absorption of trazodone hydrochloride through mouse epidermis. Drug Deliv. 2006, 13, 425–431. [Google Scholar] [CrossRef]
- Amin, S.; Kohli, K.; Khar, R.K.; Mir, S.R.; Pillai, K.K. Mechanism of in vitro percutaneous absorption enhancement of carvedilol by penetration enhancers. Pharm. Dev. Technol. 2008, 13, 533–539. [Google Scholar] [CrossRef]
- Thakur, R.A.; Wang, Y.; Michniak, B.B. Essential oils and terpenes. In Percutaneous Penetration Enhancers, 2nd; Smith, E.W., Maibach, H.I., Eds.; CRC Press: Boca Raton, FL, USA, 2006; pp. 159–173. [Google Scholar]
- Cornwell, P.A.; Barry, B.W. The routes of penetration of ions and 5-fluorouracil across human skin and the mechanisms of action of terpene skin penetration enhancers. Int. J. Pharm. 1993, 94, 189–194. [Google Scholar] [CrossRef]
- Gao, S.; Singh, J. In vitro percutaneous absorption enhancement of a lipophilic drug tamoxifen by terpenes. J. Control. Release 1998, 51, 193–199. [Google Scholar] [CrossRef]
- Torssell, K.B.G. Natural Product Chemistry: A Mechanistic and Biosynthetic Approach to Secondary Metabolism; Wiley: Chichester, UK, 1983; pp. 167–225, Chapter 5. [Google Scholar]
- Cornwell, P.A.; Barry, B.W. Sesquiterpene components of volatile oils as skin penetration enhancers for the hydrophilic permeant 5-fluorouracil. J. Pharm. Pharmacol. 1994, 46, 261–269. [Google Scholar] [CrossRef]
- Lim, P.-F.-C.; Liu, X.-Y.; Kang, L.; Ho, P.-C.-L.; Chan, Y.-W.; Chan, S.-Y. Limonene GP1/PG organogel as a vehicle in transdermal delivery of haloperidol. Int. J. Pharm. 2006, 311, 157–164. [Google Scholar] [CrossRef]
- Clarys, P.; Alewaeters, K.; Jadoul, A.; Barel, A.; Manadas, R.U.; Préat, V. In vitro percutaneous penetration through hairless rat skin: Influence of temperature, vehicle and penetration enhancers. Eur. J. Pharm. Biopharm. 1998, 46, 279–283. [Google Scholar] [CrossRef]
- Femenía-Font, A.; Balaguer-Fernández, C.; Merino, V.; Rodilla, V.; López-Castellano, A. Effect of chemical enhancers on the in vitro percutaneous absorption of sumatriptan succinate. Eur. J. Pharm. Biopharm. 2005, 61, 50–55. [Google Scholar] [CrossRef]
- Moghimi, H.R.; Makhmalzadeh, B.S.; Manafi, A. Enhancement effect of terpenes on silver sulphadiazine permeation through third-degree burn eschar. Burns 2009, 35, 1165–1170. [Google Scholar] [CrossRef]
- Krishnaiah, Y.S.R.; Satyanarayana, V.; Bhaskar, P. Influence of limonene on the bioavailability of nicardipine hydrochloride from membrane-moderated transdermal therapeutic systems in human volunteers. Int. J. Pharm. 2002, 247, 91–102. [Google Scholar] [CrossRef]
- Jain, A.K.; Thomas, N.S.; Panchagnula, R. Transdermal drug delivery of imipramine hydrochloride.: I. Effect of terpenes. J. Control. Release 2002, 79, 93–101. [Google Scholar] [CrossRef]
- Kararli, T.T.; Kirchoff, C.F.; Penzotti, S.C., Jr. Enhancement of transdermal transport of azidothymidine (AZT) with novel terpene and terpene-like enhancers: In vivo-in vitro correlations. J. Control. Release 1995, 34, 43–51. [Google Scholar] [CrossRef]
- Amnuaikit, C.; Ikeuchi, I.; Ogawar, K.; Higaki, K.; Kimura, T. Skin permeation of propranolol from polymeric film containing terpene enhancers for transdermal use. Int. J. Pharm. 2005, 289, 167–178. [Google Scholar] [CrossRef]
- Krishnaiah, Y.S.R.; Satyanarayana, V.; Bhaskar, P. Formulation and in vivo evaluation of membrane-moderated transdermal therapeutic systems of nicardipine hydrochloride using carvone as a penetration enhancer. Drug Deliv. 2003, 10, 101–109. [Google Scholar] [CrossRef]
- Hanif, R.M.; Qineng, P.; Zhan, G. Penetration enhancing effect of tetrahydrogeraniol on the percutaneous absorption of 5-fluorouracil from gels in excised rat skin. J. Control. Release 1998, 55, 297–302. [Google Scholar] [CrossRef]
- Arellano, A.; Santoyo, S.; Martín, C.; Ygartua, P. Enhancing effect of terpenes on the in vitro percutaneous absorption of diclofenac sodium. Int. J. Pharm. 1996, 130, 141–145. [Google Scholar] [CrossRef]
- Godwin, D.A.; Michniak, B.B. Influence of drug lipophilicity on terpenes as transdermal penetration enhancers. Drug Dev. Ind. Pharm. 1999, 25, 905–915. [Google Scholar] [CrossRef]
- El-Kattan, A.F.; Asbill, C.S.; Kim, N.; Michniak, B.B. The effects of terpene enhancers on the percutaneous permeation of drugs with different lipophilicities. Int. J. Pharm. 2001, 215, 229–240. [Google Scholar] [CrossRef]
- Babu, R.J.; Singh, M.; Kanikkannan, N. Fatty alcohols and fatty acids. In Percutaneous Penetration Enhancers, 2nd; Smith, E.W., Maibach, H.I., Eds.; CRC Press: Boca Raton, FL, USA, 2006; pp. 137–158. [Google Scholar]
- Hjaltason, B. New frontiers in the processing and utilization of fish oil. In Nutritional Impact of Food Processing. Bibl. Nutr. Dieta; Somogyi, J.C., Müller, H.R., Eds.; Karger Publishing: Basel, Switzerland, 1989; pp. 96–106. [Google Scholar]
- Loftsson, T.; Guđmundsdóttir, T.K.; Friđriksdótter, H.; Sugurđardóttir, A.M.; Thorkelsson, J.; Guđmundsson, G.; Hjaltason, B. Fatty acids from cod-liver oil as skin penetration enhancers. Pharmazie 1995, 50, 188–190. [Google Scholar]
- Loftsson, T.; Thormar, H.; Ólafsson, J.H.; Gunnarsdóttir, T.M.; Hjaltsason, B.; Gudmundsson, G. Fatty acid extract from cod-liver oil: Activity against herpes simplex virus and enhancement of transdermal delivery of acyclovir in vitro. Pharm. Pharmacol. Commun. 1998, 4, 287–291. [Google Scholar]
- Prescott, G.W. The Algae: A Review; Nelson: London, UK, 1969; pp. 3–35, Chapter 1. [Google Scholar]
- Lee, R.E. Phycology, 3rd ed; Cambridge University Press: Cambridge, UK, 1999; pp. 3–177. [Google Scholar]
- Fang, J.-Y.; Chiu, H.-C.; Wu, J.-T.; Chiang, Y.-R.; Hsu, S.-H. Fatty acids in Botryococcus braunii accelerate topical delivery of flurbiprofen into and across skin. Int. J. Pharm. 2004, 276, 163–173. [Google Scholar] [CrossRef]
- Garrett, R.H.; Grisham, C.M. Principles of Biochemistry: With a Human Focus, 1st ed; Brooks/Cole: Pacific Grove, CA, USA, 2001; pp. 158–633. [Google Scholar]
- Yokomizo, Y.; Sagitani, H. Effects of phospholipids on the in vitro percutaneous penetration of prednisolone and analysis of mechanism by using attenuated total reflectance-fourier transform infrared spectroscopy. J. Pharm. Sci. 1996, 85, 1220–1226. [Google Scholar] [CrossRef]
- Valjakka-Koskela, R.; Kirjavainen, M.; Mönkkönen, J.; Urtti, A.; Kiesvaara, J. Enhancement of percutaneous absorption of naproxen by phospholipids. Int. J. Pharm. 1998, 175, 225–230. [Google Scholar] [CrossRef]
- Yokomizo, Y.; Sagitani, H. Effects of phospholipids on the percutaneous penetration of indomethacin through the dorsal skin of guinea pigs in vitro. J. Control. Release 1996, 38, 267–274. [Google Scholar] [CrossRef]
- Yokomizo, Y.; Sagitani, H. The effects of phospholipids on the percutaneous penetration of indomethacin through the dorsal skin of guinea pig in vitro. 2. The effects of the hydrophobic group in phospholipids and a comparison with general enhancers. J. Control. Release 1996, 42, 37–46. [Google Scholar] [CrossRef]
- Nashihata, T.; Kotera, K.; Nakano, Y.; Yamazaki, M. Rat percutaneous transport of diclofenac and influence of hydrogenated soya phospholipids. Chem. Pharm. Bull. 1987, 35, 3807–3812. [Google Scholar] [CrossRef]
- Kato, A.; Ishibashi, Y.; Miyake, Y. Effect of egg yolk lecithin on transdermal delivery of bunazosin hydrochloride. J. Pharm. Pharmacol. 1987, 39, 399–400. [Google Scholar]
- Kimura, T.; Nagahara, N.; Hirabayashi, K.; Kurosaki, Y.; Nakayama, T. Enhanced percutaneous penetration of flufenamic acid using lipid disperse systems containing glycosylceramides. Chem. Pharm. Bull. 1989, 37, 454–457. [Google Scholar] [CrossRef]
- Kirjavainen, M.; Urtti, A.; Valjakka-Koskela, R.; Kiesvaara, J.; Mönkkönen, J. Liposome-skin interactions and their effects on the skin permeation of drugs. Eur. J. Pharm. Sci. 1999, 7, 279–286. [Google Scholar] [CrossRef]
- Mura, S.; Manconi, M.; Sinico, C.; Valenti, D.; Fadda, A.M. Penetration enhancer-containing vesicles (PEVs) as carriers for cutaneous delivery of minoxidil. J. Control. Release 2009, 380, 72–79. [Google Scholar]
- Dragicevic-Curic, N.; Scheglmann, D.; Albrecht, V.; Fahr, A. Temoporfin-loaded invasomes: Development, characterization and in vitro skin penetration studies. J. Control. Release 2008, 127, 59–69. [Google Scholar] [CrossRef]
- Touitou, E.; Dayan, N.; Bergelson, L.; Godin, B.; Eliaz, M. Ethosomes-Novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J. Control. Release 2000, 65, 403–418. [Google Scholar] [CrossRef]
- Burrows, F.; Louime, C.; Abazinge, M.; Onokpise, O. Extraction and evaluation of chitosan from crab exoskeleton as a seed fungicide and plant growth enhancer. Am. Eurasian J. Agric. Environ. Sci. 2007, 2, 103–111. [Google Scholar]
- He, W.; Guo, X.; Xiao, L.; Feng, M. Study on the mechanisms of chitosan and its derivatives used as transdermal penetration enhancers. Int. J. Pharm. 2009, 382, 234–243. [Google Scholar] [CrossRef]
- He, W.; Guo, X.; Zhang, M. Transdermal permeation enhancement of N-trimethyl chitosan for testosterone. Int. J. Pharm. 2008, 356, 82–87. [Google Scholar] [CrossRef]
- Taveira, S.F.; Nomizo, A.; Lopez, R.F.V. Effect of the ionthophoresis of chitosan gel on doxorubicin skin penetration and cytotoxicity. J. Control. Release 2009, 134, 35–40. [Google Scholar] [CrossRef]
- Lv, H.-X.; Zhang, Z.-H.; Wang, X.-P.; Cheng, Q.-Q.; Wang, W.; Huang, X.-H.; Zhou, J.-P.; Zhang, Q.; Hou, L-L.; Huo, W. A biomimetic chitosan derivates: Preparation, characterisation and transdermal enhancement studies of N-Arginine chitosan. Molecules 2011, 16, 6778–6790. [Google Scholar]
- Morton, J.F. Folk uses and commercial exploitation of Aloe leaf pulp. Econ. Bot. 1961, 15, 311–319. [Google Scholar] [CrossRef]
- Kim, Y.S. Carbohydrates. In New Perspectives on Aloe; Park, Y.I., Lee, S.K., Eds.; Springer Science: New York, NY, USA, 2006; pp. 57–62. [Google Scholar]
- Loots, D.; Van der Westhuizen, F.H.; Botes, L. Aloe ferox leaf gel phytochemical content, antioxidant capacity and possible health benefits. J. Agric. Food Chem. 2007, 55, 6891–6896. [Google Scholar] [CrossRef]
- Cole, L.; Heard, C. Skin permeation enhancement potention of Aloe vera and a proposed mechanism of action based upon size exclusion and pull effect. Int. J. Pharm. 2007, 333, 10–16. [Google Scholar] [CrossRef]
- Ballam, L.; Heard, C.M. Pre-treatment with Aloe vera juice does not enhance the in vitro permeation of ketoprofen across skin. Skin Pharmacol. Physiol. 2010, 23, 113–116. [Google Scholar] [CrossRef]
- McGaw, D.R.; Holder, R.; Commissiong, E.; Maxwell, A. Extraction of Volatile and Fixed Oil Products from Hot Peppers. In Proceedings of the 6th International Symposium on Supercritical Fluids, International Society for Advancement of Supercritical Fluids, Versailles, France, 28-30 April 2003.
- Fox, L.P.; Merk, H.F.; Bickers, D.R. Dermatological pharmacology. In Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, 11th; Brunton, L.L., Lazo, J.S., Parker, K.L., Eds.; McGraw-Hill: New York, NY, USA, 2006; pp. 1679–1706. [Google Scholar]
- Degim, I.T.; Uslu, A.; Hadgraft, J.; Atay, T.; Akay, C.; Cevheroglu, S. The effects of Azone® and capsaicin on the permeation of naproxen through human skin. Int. J. Pharm. 1999, 179, 21–25. [Google Scholar] [CrossRef]
- Trivedi, J.S.; Krill, S.L.; Fort, J.J. Vitamin E as a human skin penetration enhancer. Eur. J. Pharm. Sci. 1995, 3, 241–243. [Google Scholar] [CrossRef]
© 2011 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Fox, L.T.; Gerber, M.; Plessis, J.D.; Hamman, J.H. Transdermal Drug Delivery Enhancement by Compounds of Natural Origin. Molecules 2011, 16, 10507-10540. https://doi.org/10.3390/molecules161210507
Fox LT, Gerber M, Plessis JD, Hamman JH. Transdermal Drug Delivery Enhancement by Compounds of Natural Origin. Molecules. 2011; 16(12):10507-10540. https://doi.org/10.3390/molecules161210507
Chicago/Turabian StyleFox, Lizelle T., Minja Gerber, Jeanetta Du Plessis, and Josias H. Hamman. 2011. "Transdermal Drug Delivery Enhancement by Compounds of Natural Origin" Molecules 16, no. 12: 10507-10540. https://doi.org/10.3390/molecules161210507
APA StyleFox, L. T., Gerber, M., Plessis, J. D., & Hamman, J. H. (2011). Transdermal Drug Delivery Enhancement by Compounds of Natural Origin. Molecules, 16(12), 10507-10540. https://doi.org/10.3390/molecules161210507







