The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Registration of Patellar and Achilles Tendinopathy
2.3. Measures of Burden
2.3.1. Prevalence Measures
2.3.2. Time to Tendinopathy Onset
2.3.3. Symptoms Duration and Severity
2.4. Potential Risk Factors
2.5. Statistical Analysis
3. Results
3.1. Player Characteristics
3.2. Response Rate
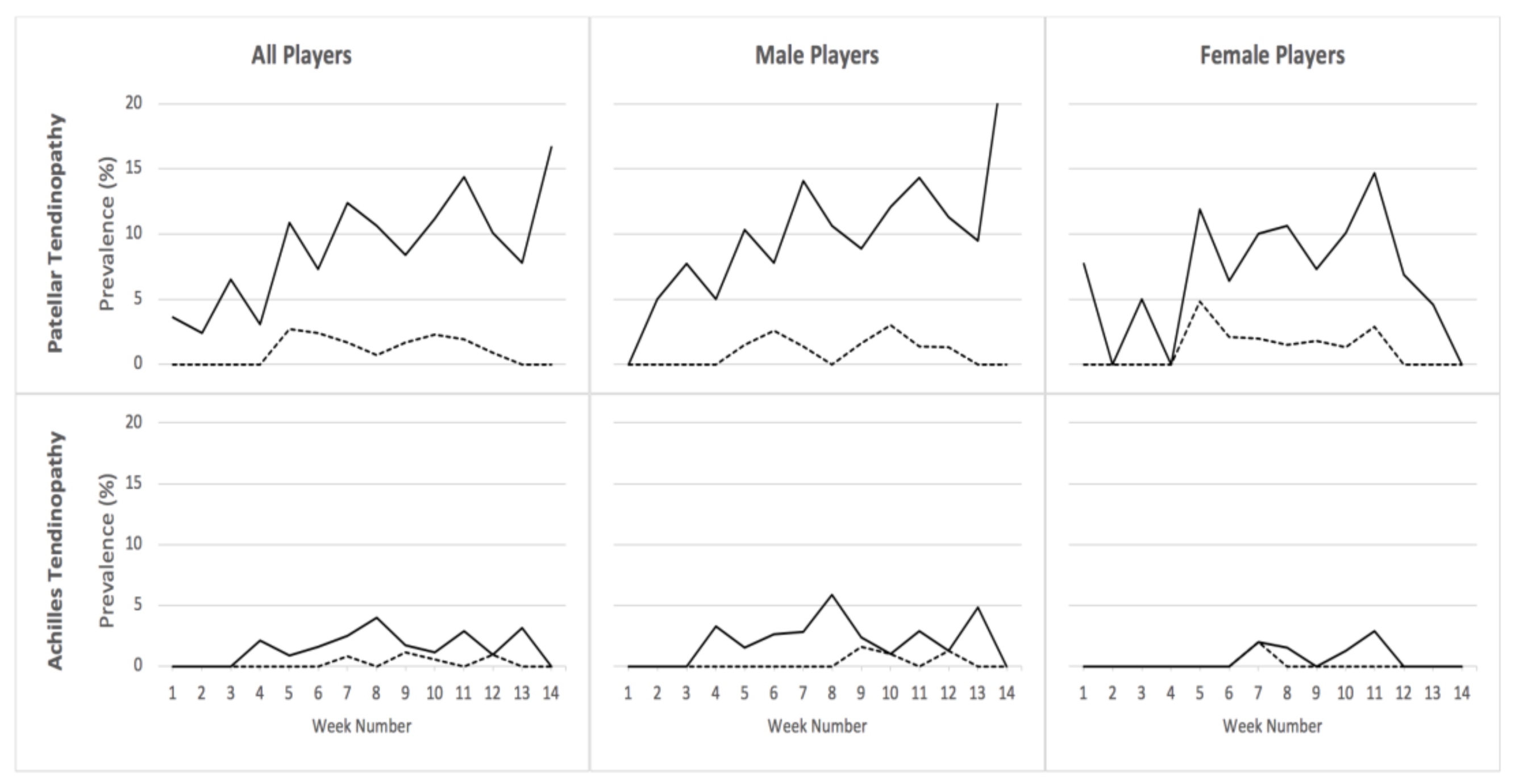
3.3. Prevalence of Patellar and Achilles Tendinopathy
3.4. Time to Tendinopathy Onset
3.5. Symptoms’ Duration and Severity
3.6. Multivariable Analysis of Risk Factors
4. Discussion
4.1. Prevalence of Patellar and Achilles Tendinopathy
4.2. Time to Tendinopathy, Symptoms’ Duration and Severity Score
4.3. Risk Factors of Patellar and Achilles Tendinopathy
4.4. Methodological Considerations
4.5. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lian, O.B.; Engebretsen, L.; Bahr, R. Prevalence of jumper’s knee among elite athletes from different sports: A cross-sectional study. Am. J. Sports Med. 2005, 33, 561–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amin, N.H.; Old, A.B.; Tabb, L.P.; Garg, R.; Toossi, N.; Cerynik, D.L. Performance outcomes after repair of complete achilles tendon ruptures in National Basketball Association players. Am. J. Sports Med. 2013, 41, 1864–1868. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.; Backman, L.J.; Speed, C. Tendinopathy: Update on Pathophysiology. J. Orthop. Sports Phys. Ther. 2015, 45, 833–841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, J.L.; Rio, E.; Purdam, C.R.; Docking, S.I. Revisiting the continuum model of tendon pathology: What is its merit in clinical practice and research? Br. J. Sports Med. 2016, 50, 1187–1191. [Google Scholar] [CrossRef]
- Rosso, F.; Bonasia, D.E.; Cottino, U.; Dettoni, F.; Bruzzone, M.; Rossi, R. Patellar tendon: From tendinopathy to rupture. Asia-Pac. J. Sport Med. Arthrosc. Rehabil. Technol. 2015, 2, 99–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ackermann, P.W.; Renström, P. Tendinopathy in sport. Sports Health 2012, 4, 193–201. [Google Scholar] [CrossRef]
- Simpson, M.; Rio, E.; Cook, J. At What Age Do Children and Adolescents Develop Lower Limb Tendon Pathology or Tendinopathy? A Systematic Review and Meta-analysis. Sport Med. 2015, 46, 545–557. [Google Scholar] [CrossRef]
- Cook, J.L.; Khan, K.M.; Kiss, Z.S.; Griffiths, L. Patellar tendinopathy in junior basketball players: A controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14–18 years. Scand. J. Med. Sci. Sports 2000, 10, 216–220. [Google Scholar] [CrossRef]
- Bahr, R.; Clarsen, B.; Ekstrand, J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br. J. Sports Med. 2018, 52, 1018–1021. [Google Scholar] [CrossRef]
- Sprague, A.L.; Smith, A.H.; Knox, P.; Pohlig, R.T.; Grävare Silbernagel, K. Modifiable risk factors for patellar tendinopathy in athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1575–1585. [Google Scholar] [CrossRef]
- Bahr, R. No injuries, but plenty of pain? On the methodology for recording overuse symptoms in sports. Br. J. Sports Med. 2009, 43, 966–972. [Google Scholar] [CrossRef]
- Clarsen, B.; Myklebust, G.; Bahr, R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: The Oslo Sports Trauma Research Centre (OSTRC) overuse injury questionnaire. Br. J. Sports Med. 2013, 47, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Owoeye, O.B.A.; Wiley, J.P.; Walker, R.E.A.; Palacios-Derflingher, L.; Emery, C.A. Diagnostic accuracy of a self-report measure of patellar tendinopathy in youth basketball. J. Orthop. Sports Phys. Ther. 2018, 48, 758–766. [Google Scholar] [CrossRef]
- Khan, K.; Cook, J.; Maffulli, N. Patellar Tendinopathy and Patellar Tendon Rupture. In Tendon Injuries; Maffulli, N., Renström, P., Leadbetter, W., Eds.; Springer: Berlin, Germany, 2005; pp. 166–177. [Google Scholar]
- Cook, J.L.; Purdam, C.R. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br. J. Sports Med. 2009, 43, 409–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, J.L.; Purdam, C.R. The challenge of managing tendinopathy in competing athletes. Br. J. Sports Med. 2013, 48, 506–509. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strobe Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar] [CrossRef] [PubMed]
- Clarsen, B.; Rønsen, O.; Myklebust, G.; Flørenes, T.W.; Bahr, R. The Oslo Sports Trauma Research Center questionnaire on health problems: A new approach to prospective monitoring of illness and injury in elite athletes. Br. J. Sports Med. 2014, 48, 754–760. [Google Scholar] [CrossRef] [Green Version]
- Van der Worp, H.; van Ark, M.; Roerink, S.; Pepping, G.-J.; van den Akker-Scheek, I.; Zwerver, J. Risk factors for patellar tendinopathy: A systematic review of the literature. Br. J. Sports Med. 2011, 45, 446–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Buuren, S.; Boshuizen, H.C.; Knook, D.L. Multiple imputation of missing blood pressure covariates in survival analysis. Stat. Med. 1999, 18, 681–694. [Google Scholar] [CrossRef]
- Azur, M.J.; Stuart, E.A.; Frangakis, C.; Leaf, P.J. Multiple imputation by chained equations: What is it and how does it work? Int. J. Methods Psychiatr. Res. 2011, 20, 40–49. [Google Scholar] [CrossRef]
- Owoeye, O.B.A.; Ghali, B.; Befus, K.; Stilling, C.; Hogg, A.; Choi, J.; Palacios-Derflingher, L.; Pasanen, K.; Emery, C.A. Epidemiology of all-complaint injuries in youth basketball. Scand. J. Med. Sci. Sports 2020, 30, 2466–2476. [Google Scholar] [CrossRef] [PubMed]
- Harøy, J.; Clarsen, B.; Thorborg, K.; Hölmich, P.; Bahr, R.; Andersen, T.E. Groin Problems in Male Soccer Players Are More Common Than Previously Reported. Am. J. Sports Med. 2017, 45, 1304–1308. [Google Scholar] [CrossRef] [PubMed]
- DiFiori, J.P.; Güllich, A.; Brenner, J.S.; Côté, J.; Hainline, B.; Ryan, E.; Malina, R.M. The NBA and Youth Basketball: Recommendations for Promoting a Healthy and Positive Experience. Sport Med. 2018, 48, 2053–2065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassel, M.; Baur, H.; Hirschmüller, A.; Carlsohn, A.; Fröhlich, K.; Mayer, F. Prevalence of Achilles and patellar tendinopathy and their association to intratendinous changes in adolescent athletes. Scand. J. Med. Sci. Sports 2015, 25, e310–e318. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, A.S.; Sayres, L.C.; McCurdy, M.L.; Collado, H.; Sainani, K.L.; Fredericson, M. Overuse Injuries in High School Runners: Lifetime Prevalence and Prevention Strategies. Pm&r 2011, 3, 125–131. [Google Scholar]
- Emerson, C.; Morrissey, D.; Perry, M.; Jalan, R. Ultrasonographically detected changes in Achilles tendons and self reported symptoms in elite gymnasts compared with controls—An observational study. Man. Ther. 2010, 15, 37–42. [Google Scholar] [CrossRef]
- De Vries, A.J.; van der Worp, H.; Diercks, R.L.; van den Akker-Scheek, I.; Zwerver, J. Risk factors for patellar tendinopathy in volleyball and basketball players: A survey-based prospective cohort study. Scand. J. Med. Sci. Sports 2015, 25, 678–684. [Google Scholar] [CrossRef]
- Cook, J.L.; Bass, S.L.; Black, J.E. Hormone therapy is associated with smaller Achilles tendon diameter in active post-menopausal women. Scand. J. Med. Sci. Sports 2007, 17, 128–132. [Google Scholar] [CrossRef]
- Clarsen, B.; Bahr, R.; Heymans, M.W.; Engedahl, M.; Midtsundstad, G.; Rosenlund, L.; Thorsen, G.; Myklebust, G. The prevalence and impact of overuse injuries in five Norwegian sports: Application of a new surveillance method. Scand. J. Med. Sci. Sports 2015, 25, 323–330. [Google Scholar] [CrossRef]
- Andersen, C.A.; Clarsen, B.; Johansen, T.V.; Engebretsen, L. High prevalence of overuse injury among iron-distance triathletes. Br. J. Sports Med. 2013, 47, 857–861. [Google Scholar] [CrossRef] [Green Version]
- Leppänen, M.; Pasanen, K.; Clarsen, B.; Kannus, P.; Bahr, R.; Parkkari, J.; Haapasalo, H.; Vasankari, T. Overuse injuries are prevalent in children’s competitive football: A prospective study using the OSTRC Overuse Injury Questionnaire. Br. J. Sports Med. 2018, 53, 165–171. [Google Scholar] [CrossRef]
- Meeuwisse, W.H.; Tyreman, H.; Hagel, B.; Emery, C. A dynamic model of etiology in sport injury: The recursive nature of risk and causation. Clin. J. Sport Med. 2007, 17, 215–219. [Google Scholar] [CrossRef]
- Ghali, B.M.; Owoeye, O.B.A.; Stilling, C.; Palacios-Derflingher, L.; Jordan, M.; Pasanen, K.; Emery, C.A. Internal and External Workload in Youth Basketball Players Who Are Symptomatic and Asymptomatic for Patellar Tendinopathy. J. Orthop. Sports Phys. Ther. 2019, 50, 402–408. [Google Scholar] [CrossRef]
- Owoeye, O.B.A.; VanderWey, M.J.; Pike, I. Reducing Injuries in Soccer (Football): An Umbrella Review of Best Evidence Across the Epidemiological Framework for Prevention. Sports Med.-Open 2020, 6, 46. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, R.O.; Bertelsen, M.L.; Møller, M.; Hulme, A.; Windt, J.; Verhagen, E.; Mansournia, M.A.; Casals, M.; Parner, E.T. Training load and structure-specific load: Applications for sport injury causality and data analyses. Br. J. Sports Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition—Narrative review and new concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owoeye, O.B.A. Digging Deep into the Etiology of Basketball Injuries: A Complex Systems Approach for Risk Mitigation. In The Basketball Sports Medicine and Science Book; Lavar, L., Kocaoglu, B., Bytomski, J., Cole, B., Arundale, A.A.N., Eds.; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Breda, S.J.; Oei, E.H.G.; Zwerver, J.; Visser, E.; Waarsing, E.; Krestin, G.P.; de Vos, R.J. Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: A randomised clinical trial. Br. J. Sports Med. 2021, 55, 501–509. [Google Scholar] [CrossRef]
- Clifford, C.; Challoumas, D.; Paul, L.; Syme, G.; Millar, N.L. Effectiveness of isometric exercise in the management of tendinopathy: A systematic review and meta-analysis of randomised trials. BMJ Open Sport Exerc. Med. 2020, 6, e000760. [Google Scholar] [CrossRef]
- Everhart, J.S.; Cole, D.; Sojka, J.H.; Higgins, J.D.; Magnussen, R.A.; Schmitt, L.C.; Flanigan, D.C. Treatment Options for Patellar Tendinopathy: A Systematic Review. Arthroscopy 2017, 33, 861–872. [Google Scholar] [CrossRef]
- Malliaras, P.; Cook, J.; Purdam, C.; Rio, E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J. Orthop. Sports Phys. Ther. 2015, 45, 1–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Males n = 315 | Females n = 200 | |
|---|---|---|
| Age (years) | ||
| Median (range) | 16 (11–18) | 16 (13–18) |
| Missing, n (%) | 59 (19) | 31 (16) |
| Height (cm) | ||
| Median (range) | 179 (110–201) | 168 (152–193) |
| Missing, n (%) | 32 (10) | 14 (7) |
| Weight (kg) | ||
| Median (range) | 67 (38–132) | 60 (41–141) |
| Missing, n (%) | 30 (10) | 15 (8) |
| Previous Knee Injury (1 Year), n (%) | ||
| Yes | 216 (69.6) | 152 (76.0) |
| No | 30 (9.5) | 30 (15.0) |
| Missing | 69 (21.9) | 18 (9.0) |
| Previous Anterior Knee Pain (3 months) n (%) | ||
| Yes | 90 (28.6) | 53 (26.5) |
| No | 141 (44.7) | 116 (58.0) |
| Missing | 84 (26.7) | 31 (15.5) |
| Previous Achilles Tendon Pain (3 months) n (%) | ||
| Yes | 191 (60.6) | 150 (75.0) |
| No | 38 (12.1) | 14 (7.0) |
| Missing | 86 (27.3) | 36 (18.0) |
| Player Position, n (%) | ||
| Guard | 136 (43.2) | 89 (44.5) |
| Post | 50 (15.9) | 45 (22.5) |
| Combo | 81 (25.7) | 52 (26.0) |
| Missing | 48 (15.2) | 14 (7.0) |
| Single Sport Baskeball Participation, n (%) | ||
| Yes | 101 (32.1) | 70 (35.0) |
| No | 161 (51.1) | 99 (49.5) |
| Missing | 53 (16.8) | 31 (15.5) |
| Variable | OR | 95% CI | p-Value |
|---|---|---|---|
| Sex | |||
| Female (Referent) | - | - | - |
| Male | 2.23 | 1.10–4.69 | 0.026 * |
| Previous Anterior Knee Pain | |||
| No (Referent) | - | - | - |
| Yes | 8.79 | 4.58–16.89 | <0.001 * |
| League Setting | |||
| Club (Referent) | - | - | - |
| School | 0.76 | 0.39–1.51 | 0.436 |
| Weight | 0.98 | 0.96–1.01 | 0.156 |
| Age | 1.27 | 0.96–1.67 | 0.090 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Owoeye, O.B.A.; Palacios-Derflingher, L.; Pasanen, K.; HubkaRao, T.; Wiley, P.; Emery, C.A. The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 9480. https://doi.org/10.3390/ijerph18189480
Owoeye OBA, Palacios-Derflingher L, Pasanen K, HubkaRao T, Wiley P, Emery CA. The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9480. https://doi.org/10.3390/ijerph18189480
Chicago/Turabian StyleOwoeye, Oluwatoyosi B. A., Luz Palacios-Derflingher, Kati Pasanen, Tate HubkaRao, Preston Wiley, and Carolyn A. Emery. 2021. "The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study" International Journal of Environmental Research and Public Health 18, no. 18: 9480. https://doi.org/10.3390/ijerph18189480
APA StyleOwoeye, O. B. A., Palacios-Derflingher, L., Pasanen, K., HubkaRao, T., Wiley, P., & Emery, C. A. (2021). The Burden and Risk Factors of Patellar and Achilles Tendinopathy in Youth Basketball: A Cohort Study. International Journal of Environmental Research and Public Health, 18(18), 9480. https://doi.org/10.3390/ijerph18189480






