Ex Vivo Lung Perfusion with K(ATP) Channel Modulators Antagonize Ischemia Reperfusion Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Surgical Techniques for Procurment of Donation after Circulatory Death Donor Lung and EVLP Model
2.3. EVLP Procedure with K(ATP) Channel Modulators and Physiological Variables
2.4. Clinical Biochemistry Parameters
2.5. MTT Viability Assay with a Rat Epithelial Cell Line for Non-Toxic Dosage of K(ATP) Modulator Concentrations
2.6. Cytokines, Chemokines and Mediator of Wound Healing
2.7. Estimates of ATP Content, Myeloperoxidase Activity and Carbonyl Protein Content in Lung Tissues
2.8. TUNEL Staining and Analysis
2.9. Statistical Method
3. Results
3.1. An In Vitro Assay Determined the Non-Toxic Concentrations of K(ATP) Modulators for Use during EVLP
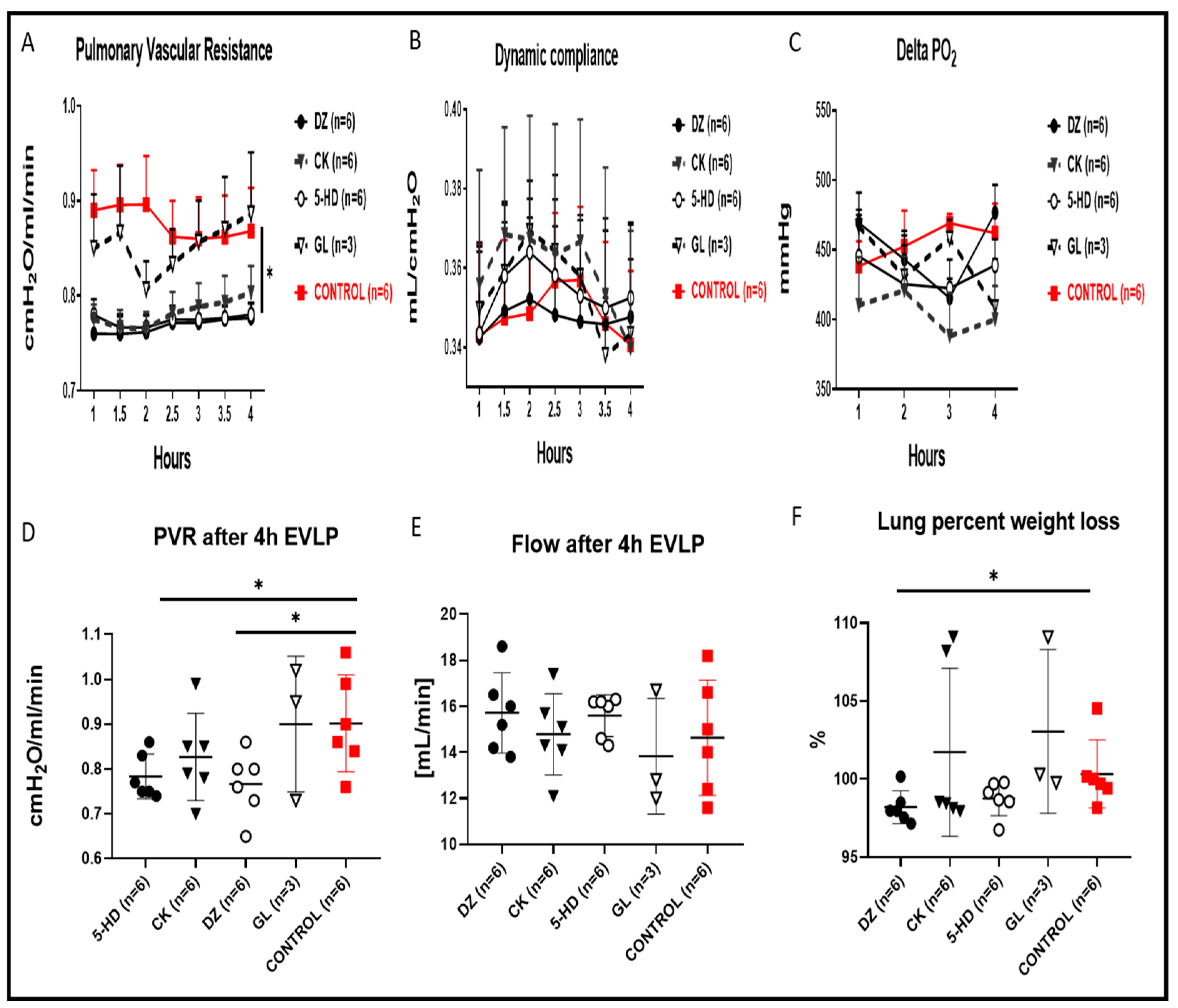
3.2. Lung Physiology during EVLP
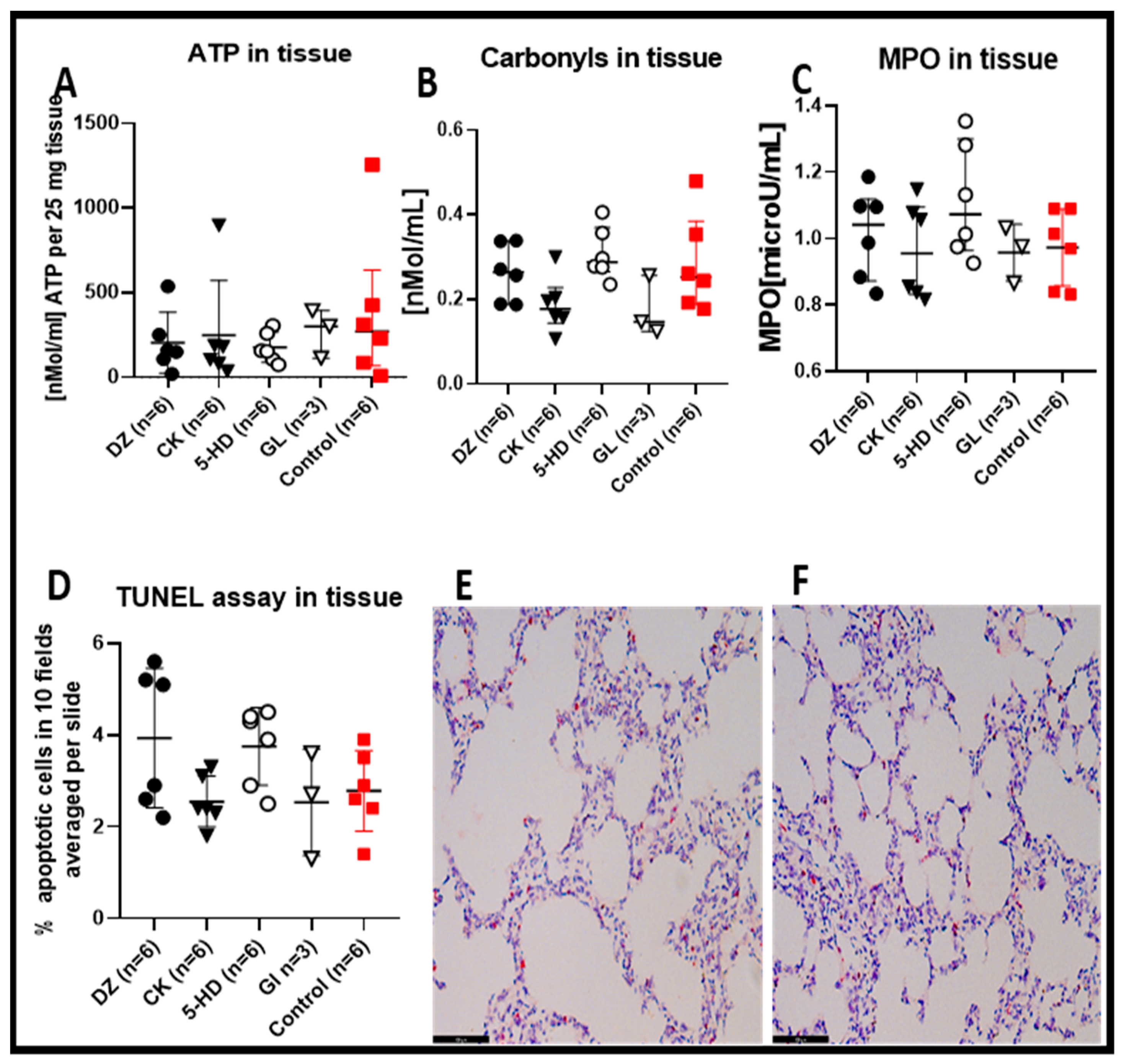
3.3. Lung Tissue Biochemical Measurements
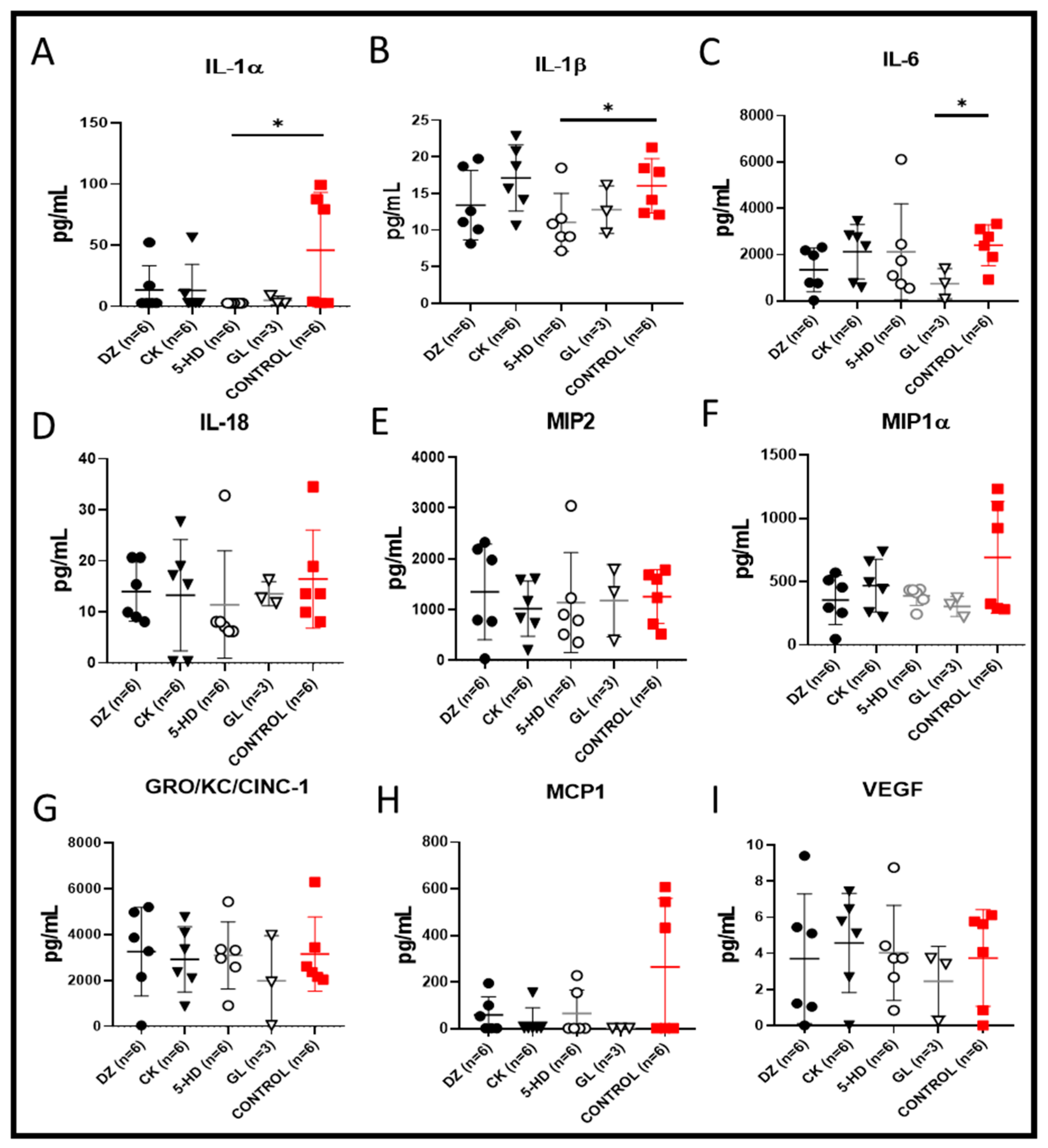
3.4. Perfusate Cytokines, Chemokines and Mediator of Wound Healing
3.5. Correlations among Perfusate Cytokines and Tissue Carbonylated Proteins with the Four K(ATP) Channel Modulators or the Control
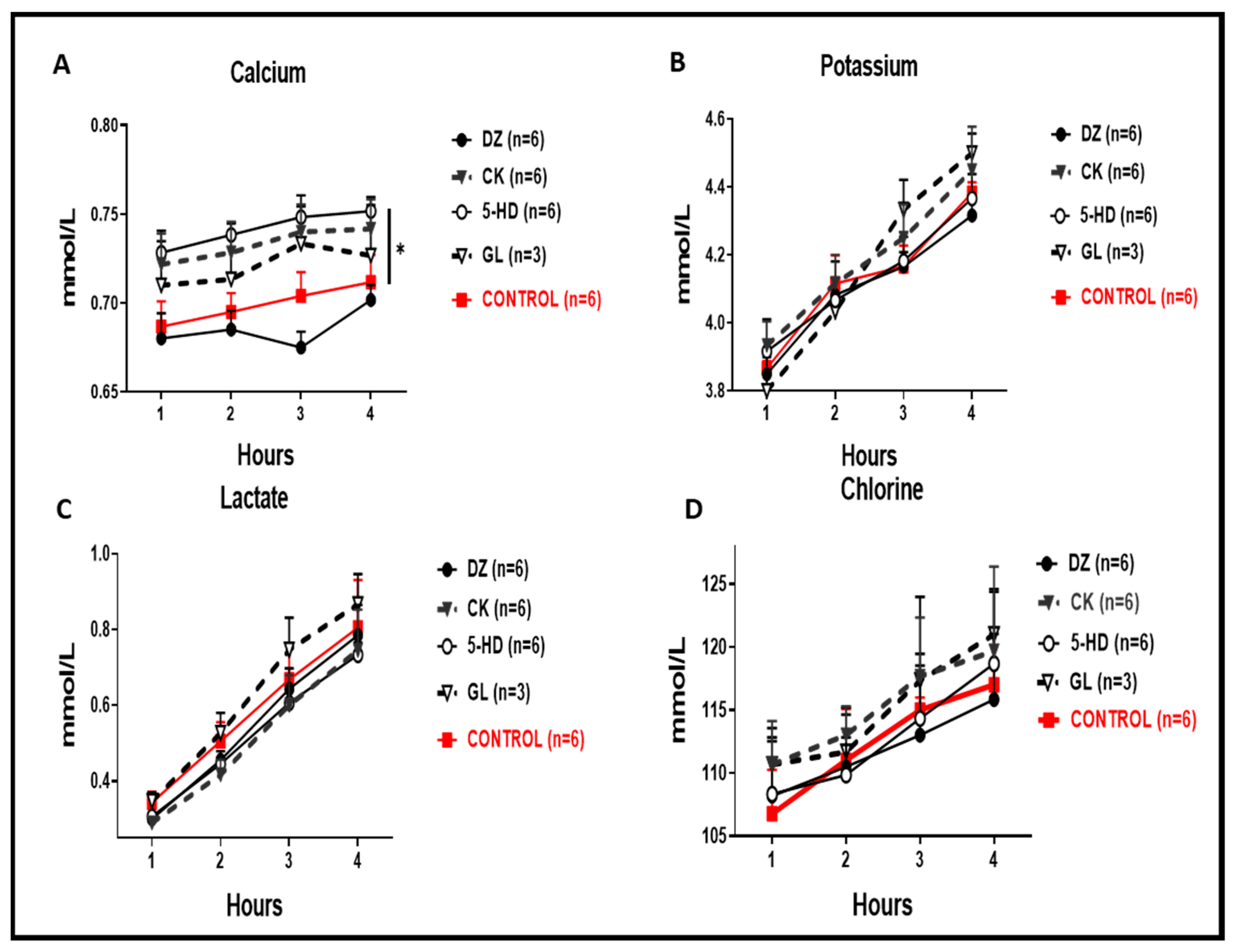
3.6. Biochemical Measurements in the Perfusate during EVLP
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 5-HD | 5-hydroxydecanoic acid. |
| K(ATP) | ATP sensitive potassium channel |
| Cdyn | Dynamic compliance |
| CK | cromakalim |
| DMSO | dimethyl sulfoxide |
| DCD | donation after circulatory death |
| DZ | diazoxide |
| EVLP | ex vivo lung perfusion |
| FiO2 | inspired oxygen fraction |
| GL | glybenclamide |
| I/R | ischemia-reperfusion |
| MPO | myeloperoxidase |
| MTT | 3-(4,5-dethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide |
| PAP | pulmonary arterial pressure |
| PVR | pulmonary vascular resistance |
| ROS | reactive oxygen species |
| TUNEL | terminal deoxynucleotidyl transferase dUTP nick end labelling |
References
- Weill, D. Lung transplantation: Indications and contraindications. J. Thorac. Dis. 2018, 10, 4574–4587. [Google Scholar] [CrossRef] [PubMed]
- Valapour, M.; Lehr, C.J.; Skeans, M.A.; Smith, J.M.; Uccellini, K.; Goff, R.; Foutz, J.; Israni, A.K.; Snyder, J.J.; Kasiske, B.L. OPTN/SRTR 2018 annual data report: Lung. Am. J. Transpl. 2020, 20 (Suppl. S1), 427–508. [Google Scholar] [CrossRef]
- Diamond, J.M.; Lee, J.C.; Kawut, S.M.; Shah, R.J.; Localio, A.R.; Bellamy, S.L.; Lederer, D.J.; Cantu, E.; Kohl, B.A.; Lama, V.N.; et al. Clinical risk factors for primary graft dysfunction after lung transplantation. Am. J. Respir. Crit. Care Med. 2013, 187, 527–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talaie, T.; Di Chiacchio, L.; Prasad, N.K.; Pasrija, C.; Julliard, W.; Kaczorowski, D.J.; Zhao, Y.; Lau, C.L. Ischemia-reperfusion injury in the transplanted lung: A literature review. Transplant. Direct. 2021, 7, e652. [Google Scholar] [CrossRef]
- Inci, I. Donors after cardiocirculatory death and lung transplantation. J. Thorac. Dis. 2017, 9, 2660–2669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sommer, W.; Kuhn, C.; Tudorache, I.; Avsar, M.; Gottlieb, J.; Boethig, D.; Haverich, A.; Warnecke, G. Extended criteria donor lungs and clinical outcome: Results of an alternative allocation algorithm. J. Heart Lung Transpl. 2013, 32, 1065–1072. [Google Scholar] [CrossRef]
- Cypel, M.; Yeung, J.C.; Hirayama, S.; Rubacha, M.; Fischer, S.; Anraku, M.; Sato, M.; Harwood, S.; Pierre, A.; Waddell, T.K.; et al. Technique for prolonged normothermic ex vivo lung perfusion. J. Heart Lung Transpl. 2008, 27, 1319–1325. [Google Scholar] [CrossRef]
- Weiss, S.; Kotsch, K.; Francuski, M.; Reutzel-Selke, A.; Mantouvalou, L.; Klemz, R.; Kuecuek, O.; Jonas, S.; Wesslau, C.; Ulrich, F.; et al. Brain death activates donor organs and is associated with a worse I/R injury after liver transplantation. Am. J. Transpl. 2007, 7, 1584–1593. [Google Scholar] [CrossRef]
- Gourishankar, S.; Jhangri, G.S.; Cockfield, S.M.; Halloran, P.F. Donor tissue characteristics influence cadaver kidney transplant function and graft survival but not rejection. J. Am. Soc. Nephrol. 2003, 14, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Chatterjee, S.; Nieman, G.F.; Christie, J.D.; Fisher, A.B. Shear stress-related mechanosignaling with lung ischemia: Lessons from basic research can inform lung transplantation. Am. J. Physiol. Lung Cell Mol. Physiol. 2014, 307, L668–L680. [Google Scholar] [CrossRef] [Green Version]
- Tano, J.Y.; Gollasch, M. Calcium-activated potassium channels in ischemia reperfusion: A brief update. Front. Physiol. 2014, 5, 381. [Google Scholar] [CrossRef] [Green Version]
- Honda, H.M.; Korge, P.; Weiss, J.N. Mitochondria and ischemia/reperfusion injury. Ann. N. Y. Acad. Sci. 2005, 1047, 248–258. [Google Scholar] [CrossRef]
- Chatterjee, S.; Fujiwara, K.; Perez, N.G.; Ushio-Fukai, M.; Fisher, A.B. Mechanosignaling in the vasculature: Emerging concepts in sensing, transduction and physiological responses. Am. J. Physiol. Heart Circ. Physiol. 2015, 308, H1451–H1462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weigt, S.S.; Palchevskiy, V.; Belperio, J.A. Inflammasomes and IL-1 biology in the pathogenesis of allograft dysfunction. J. Clin. Investig. 2017, 127, 2022–2029. [Google Scholar] [CrossRef]
- Lamkanfi, M.; Mueller, J.L.; Vitari, A.C.; Misaghi, S.; Fedorova, A.; Deshayes, K.; Lee, W.P.; Hoffman, H.M.; Dixit, V.M. Glyburide inhibits the Cryopyrin/Nalp3 inflammasome. J. Cell Biol. 2009, 187, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Q.; Matsuzaki, I.; Chatterjee, S.; Fisher, A.B. Activation of endothelial NADPH oxidase during normoxic lung ischemia is KATP channel dependent. Am. J. Physiol. Lung Cell Mol. Physiol. 2005, 289, L954–L961. [Google Scholar] [CrossRef] [Green Version]
- Pompermayer, K.; Amaral, F.A.; Fagundes, C.T.; Vieira, A.T.; Cunha, F.Q.; Teixeira, M.M.; Souza, D.G. Effects of the treatment with glibenclamide, an ATP-sensitive potassium channel blocker, on intestinal ischemia and reperfusion injury. Eur. J. Pharmacol. 2007, 556, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Council, N.R. Guide for the Care and Use of Laboratory Animals, 8th ed.; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar] [CrossRef]
- Motoyama, H.; Chen, F.; Hijiya, K.; Kondo, T.; Ohsumi, A.; Yamada, T.; Sato, M.; Aoyama, A.; Bando, T.; Date, H. Plasmin administration during ex vivo lung perfusion ameliorates lung ischemia-reperfusion injury. J. Heart Lung Transpl. 2014, 33, 1093–1099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- De Perrot, M.; Liu, M.; Waddell, T.K.; Keshavjee, S. Ischemia-reperfusion-induced lung injury. Am. J. Respir. Crit. Care Med. 2003, 167, 490–511. [Google Scholar] [CrossRef] [PubMed]
- Mykytenko, J.; Reeves, J.G.; Kin, H.; Wang, N.P.; Zatta, A.J.; Jiang, R.; Guyton, R.A.; Vinten-Johansen, J.; Zhao, Z.Q. Persistent beneficial effect of postconditioning against infarct size: Role of mitochondrial K(ATP) channels during reperfusion. Basic Res. Cardiol. 2008, 103, 472–484. [Google Scholar] [CrossRef]
- Wu, Q.; Tang, C.; Zhang, Y.J.; Jiang, Y.; Li, X.W.; Wang, S.G.; Bie, P. Diazoxide suppresses hepatic ischemia/reperfusion injury after mouse liver transplantation by a BCL-2-dependent mechanism. J. Surg. Res. 2011, 169, e155–e166. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, S.; Harvat, T.; Kinzer, K.; Zhang, L.; Feng, F.; Qi, M.; Oberholzer, J. Diazoxide, a K(ATP) channel opener, prevents ischemia-reperfusion injury in rodent pancreatic islets. Cell Transpl. 2015, 24, 25–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimizu, S.; Oikawa, R.; Tsounapi, P.; Inoue, K.; Shimizu, T.; Tanaka, K.; Martin, D.T.; Honda, M.; Sejima, T.; Tomita, S.; et al. Blocking of the ATP sensitive potassium channel ameliorates the ischaemia-reperfusion injury in the rat testis. Andrology 2014, 2, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Ge, D.; Wang, Q.; Xu, S.; Xue, L.; Lu, C.; Tan, L. Diazoxide decreases ischemia-reperfusion injury in a rat model of lung transplantation. Transpl. Proc. 2011, 43, 2510–2516. [Google Scholar] [CrossRef]
- Yamashita, M.; Schmid, R.A.; Fujino, S.; Cooper, J.D.; Patterson, G.A. Nicorandil, a potent adenosine triphosphate-sensitive potassium-channel opener, ameliorates lung allograft reperfusion injury. J. Thorac. Cardiovasc. Surg. 1996, 112, 1307–1314. [Google Scholar] [CrossRef] [Green Version]
- Chouchani, E.T.; Pell, V.R.; James, A.M.; Work, L.M.; Saeb-Parsy, K.; Frezza, C.; Krieg, T.; Murphy, M.P. A unifying mechanism for mitochondrial superoxide production during ischemia-reperfusion injury. Cell Metab. 2016, 23, 254–263. [Google Scholar] [CrossRef] [Green Version]
- Ponnalagu, D.; Singh, H. Insights into the role of mitochondrial ion channels in inflammatory response. Front. Physiol. 2020, 11, 258. [Google Scholar] [CrossRef] [PubMed]
- Pompermayer, K.; Souza, D.G.; Lara, G.G.; Silveira, K.D.; Cassali, G.D.; Andrade, A.A.; Bonjardim, C.A.; Passaglio, K.T.; Assreuy, J.; Cunha, F.Q.; et al. The ATP-sensitive potassium channel blocker glibenclamide prevents renal ischemia/reperfusion injury in rats. Kidney Int. 2005, 67, 1785–1796. [Google Scholar] [CrossRef] [Green Version]
- Figura, M.; Chilton, L.; Liacini, A.; Viskovic, M.M.; Phan, V.; Knight, D.; Millar, T.M.; Patel, K.; Kubes, P.; Giles, W.R.; et al. Blockade of K(ATP) channels reduces endothelial hyperpolarization and leukocyte recruitment upon reperfusion after hypoxia. Am. J. Transplant. 2009, 9, 687–696. [Google Scholar] [CrossRef]
- Shimizu, S.; Saito, M.; Kinoshita, Y.; Ohmasa, F.; Dimitriadis, F.; Shomori, K.; Hayashi, A.; Satoh, K. Nicorandil ameliorates ischaemia-reperfusion injury in the rat kidney. Br. J. Pharmacol. 2011, 163, 272–282. [Google Scholar] [CrossRef] [Green Version]
- Kandilci, H.B.; Gumusel, B.; Demiryurek, A.T.; Lippton, H. Preconditioning modulates pulmonary endothelial dysfunction following ischemia-reperfusion injury in the rat lung: Role of potassium channels. Life Sci. 2006, 79, 2172–2178. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Guo, Z.; Liu, H.; Shi, Y.; Ge, S. Influence of levosimendan postconditioning on apoptosis of rat lung cells in a model of ischemia-reperfusion injury. PLoS ONE 2015, 10, e0114963. [Google Scholar] [CrossRef] [Green Version]
- Nilakantan, V.; Liang, H.; Mortensen, J.; Taylor, E.; Johnson, C.P. Variable effects of the mitoK(ATP) channel modulators diazoxide and 5-HD in ATP-depleted renal epithelial cells. Mol. Cell Biochem. 2010, 335, 211–222. [Google Scholar] [CrossRef]
- Hanley, P.J.; Mickel, M.; Loffler, M.; Brandt, U.; Daut, J. K(ATP) channel-independent targets of diazoxide and 5-hydroxydecanoate in the heart. J. Physiol. 2002, 542, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Akopova, O.V. Direct and off-target effects of atp-sensitive potassium channels opener diazoxide. J. Drug Metab. Toxicol. 2017, 8, 227. [Google Scholar] [CrossRef] [Green Version]
- Hanley, P.J.; Drose, S.; Brandt, U.; Lareau, R.A.; Banerjee, A.L.; Srivastava, D.K.; Banaszak, L.J.; Barycki, J.J.; Van Veldhoven, P.P.; Daut, J. 5-Hydroxydecanoate is metabolised in mitochondria and creates a rate-limiting bottleneck for beta-oxidation of fatty acids. J. Physiol. 2005, 562, 307–318. [Google Scholar] [CrossRef]
- Li, X.; Rapedius, M.; Baukrowitz, T.; Liu, G.X.; Srivastava, D.K.; Daut, J.; Hanley, P.J. 5-Hydroxydecanoate and coenzyme A are inhibitors of native sarcolemmal KATP channels in inside-out patches. Biochim. Biophys. Acta 2010, 1800, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Montoya-Perez, R.; Saavedra-Molina, A.; Trujillo, X.; Huerta, M.; Andrade, F.; Sanchez-Pastor, E.; Ortiz, M. Inhibition of oxygen consumption in skeletal muscle-derived mitochondria by pinacidil, diazoxide, and glibenclamide, but not by 5-hydroxydecanoate. J. Bioenerg. Biomembr. 2010, 42, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Botha, P.; MacGowan, G.A.; Dark, J.H. Sildenafil citrate augments myocardial protection in heart transplantation. Transplantation 2010, 89, 169–177. [Google Scholar] [CrossRef]
- Cocks, T.M.; King, S.J.; Angus, J.A. Glibenclamide is a competitive antagonist of the thromboxane A2 receptor in dog coronary artery in vitro. Br. J. Pharm. 1990, 100, 375–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Gable, M.E.; Garlid, K.D.; Askari, A. Interactions of K+ATP channel blockers with Na+/K+-ATPase. Mol. Cell Biochem. 2007, 306, 231–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Conditions | DZ | CK | 5-HD | GL | Control |
|---|---|---|---|---|---|
| r | r | r | r | r | |
| (p) | (p) | (p) | (p) | (p) | |
| IL-1α | −0.02857 | −0.4286 | −0.4285 | 0.5 | 0.0285 |
| (1) | (0.4194) | (0.4194) | (1) | (1) | |
| IL-1β | −0.7728 | −0.0857 | −0.2029 | 0.5 | 0.0285 |
| (0.1028) | (0.9194) | (0.7139) | (1) | (1) | |
| IL-6 | −0.2571 | −0.3143 | 0.2571 | 0.5 | 0.4286 |
| (0.6583) | (0.5639) | (0.6583) | (1) | (0.4194) | |
| IL-18 | −0.4928 | −0.0289 | −0.5296 | −0.7697 | −0.0289 |
| (0.3556) | (1) | (0.2972) | (0.4408) | (1) | |
| MIP2 | −0.7714 | 0.2571 | −01429 | 0.5 | −0.2 |
| (0.1028) | (0.6583) | (0.8028) | (1) | (0.7139) | |
| MIP-1α | 0.0285 | −0.4286 | 0.6571 | 0.5 | −0.0857 |
| (1) | (0.4194) | (0.1750) | (1) | (0.9194) | |
| GRO/KC | −0.4286 | 0.3143 | −0.4286 | 0.5 | 0.0285 |
| (0.4194) | (0.5639) | (0.4194) | (1) | (1) | |
| MCP-1 | 0.0285 | 0.2571 | 0.3339 | 0.5 | −0.08571 |
| (1) | (0.6583) | (0.4972) | (1) | (0.9194) | |
| VEGF | 0.08571 | −0.1429 | −0.2029 | 1 | 0.2571 |
| (0.9194) | (0.8028) | (0.7139) | (0.3333) | (0.6584) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arni, S.; Maeyashiki, T.; Latshang, T.; Opitz, I.; Inci, I. Ex Vivo Lung Perfusion with K(ATP) Channel Modulators Antagonize Ischemia Reperfusion Injury. Cells 2021, 10, 2296. https://doi.org/10.3390/cells10092296
Arni S, Maeyashiki T, Latshang T, Opitz I, Inci I. Ex Vivo Lung Perfusion with K(ATP) Channel Modulators Antagonize Ischemia Reperfusion Injury. Cells. 2021; 10(9):2296. https://doi.org/10.3390/cells10092296
Chicago/Turabian StyleArni, Stephan, Tatsuo Maeyashiki, Tsogyal Latshang, Isabelle Opitz, and Ilhan Inci. 2021. "Ex Vivo Lung Perfusion with K(ATP) Channel Modulators Antagonize Ischemia Reperfusion Injury" Cells 10, no. 9: 2296. https://doi.org/10.3390/cells10092296







