Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Master Cast Preparation
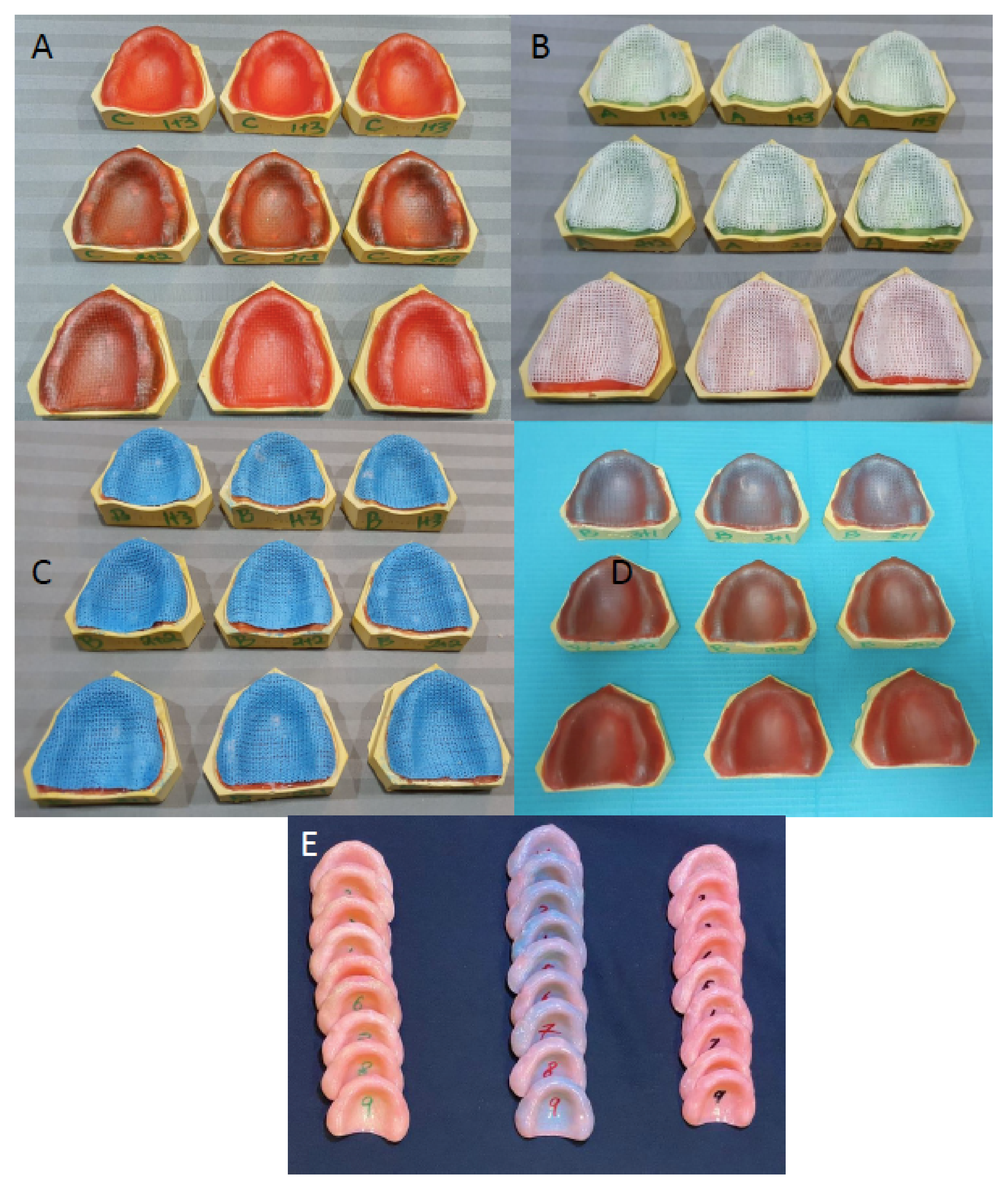
2.2. Acrylic Denture Base Fabrication
2.3. Processing of Denture Plates
2.4. Fatigue Load Application
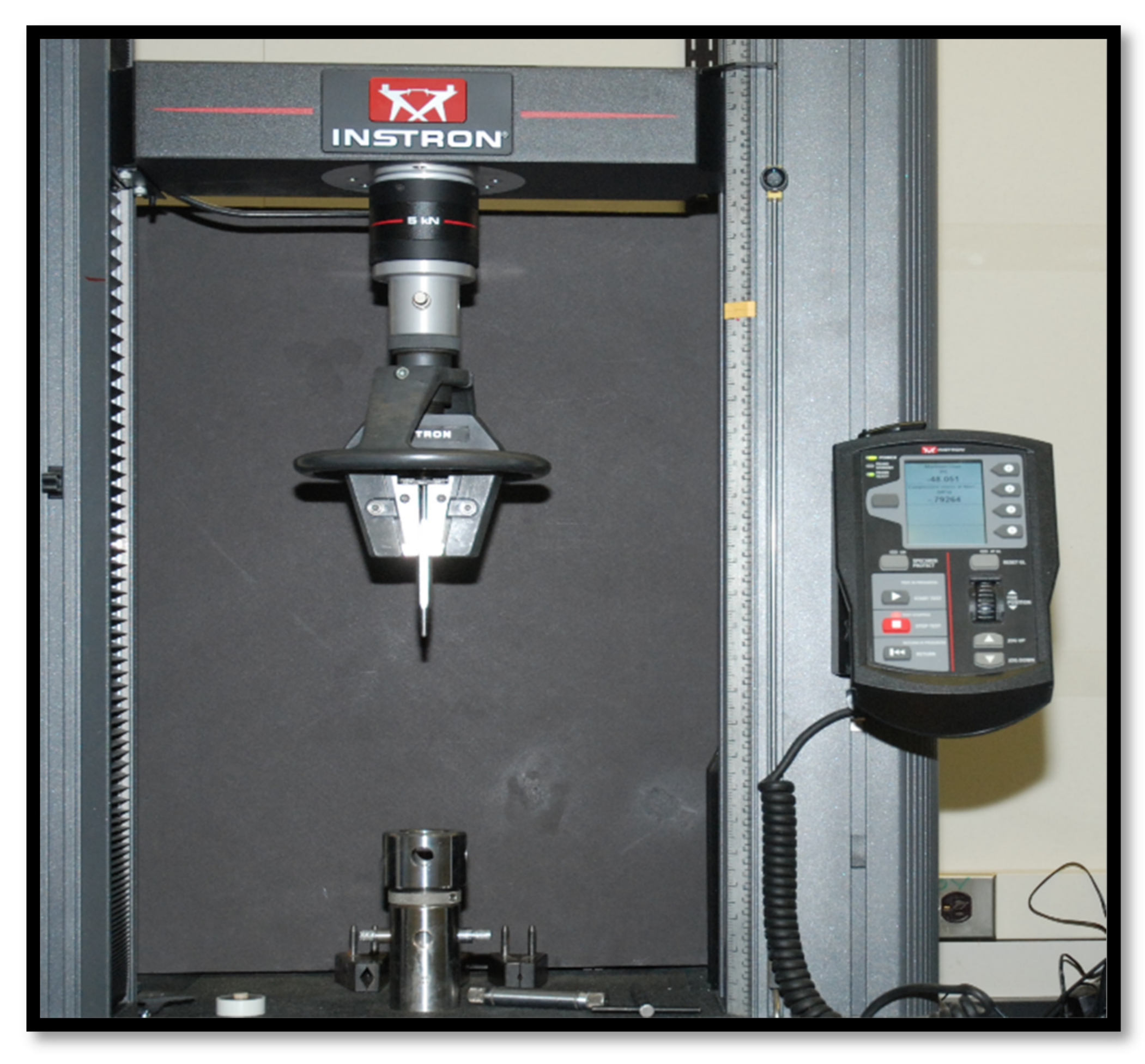
2.5. Fracture Testing
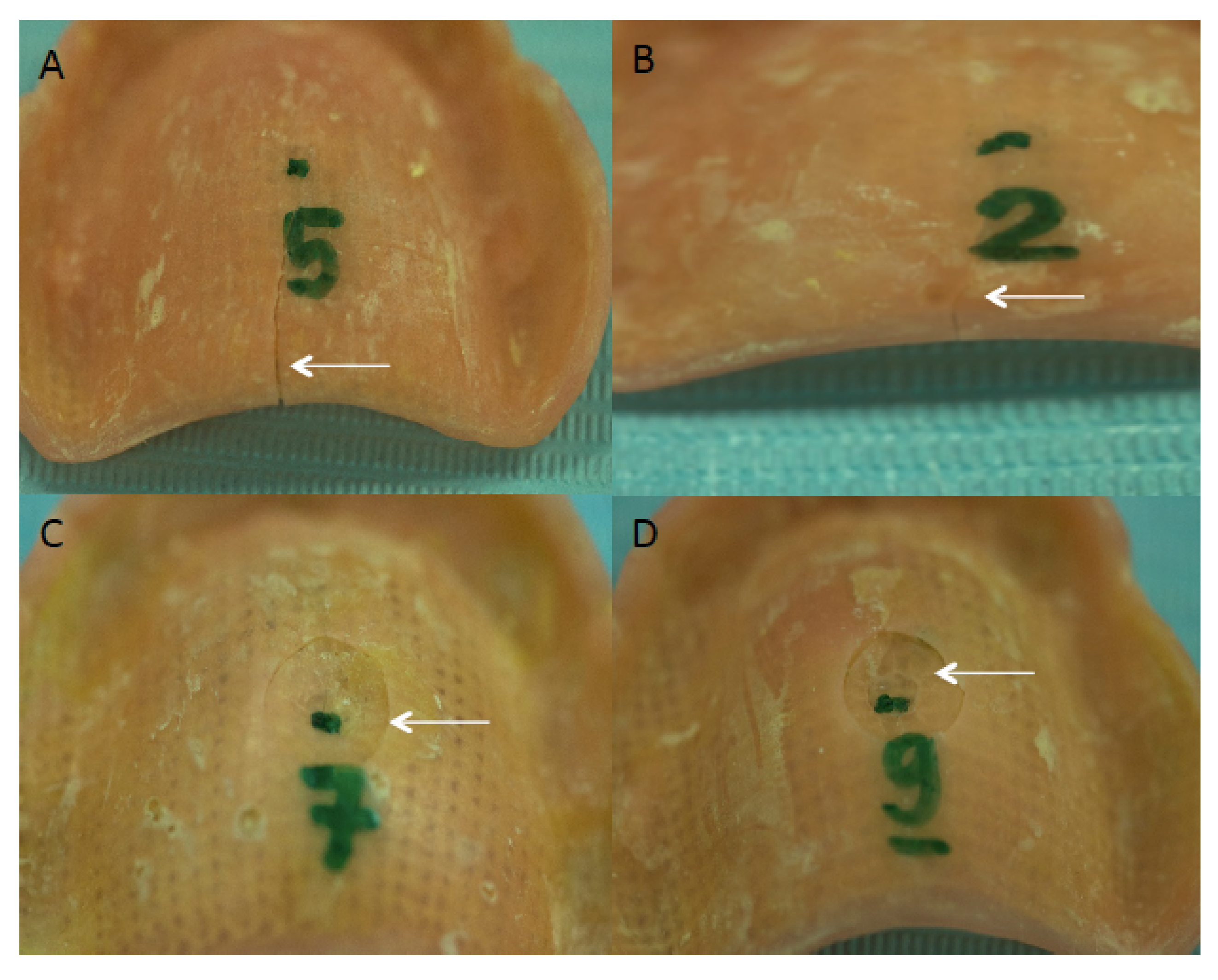
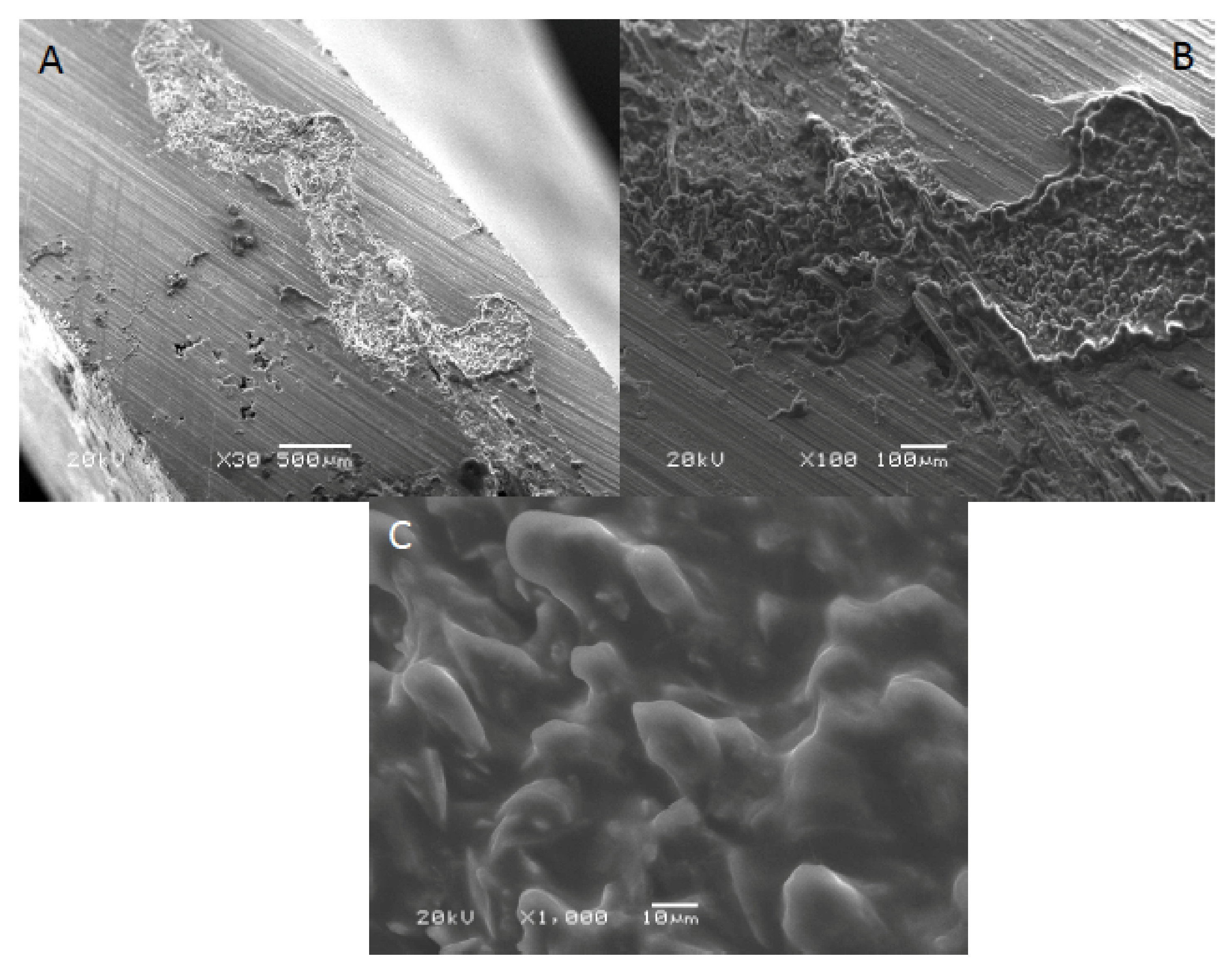
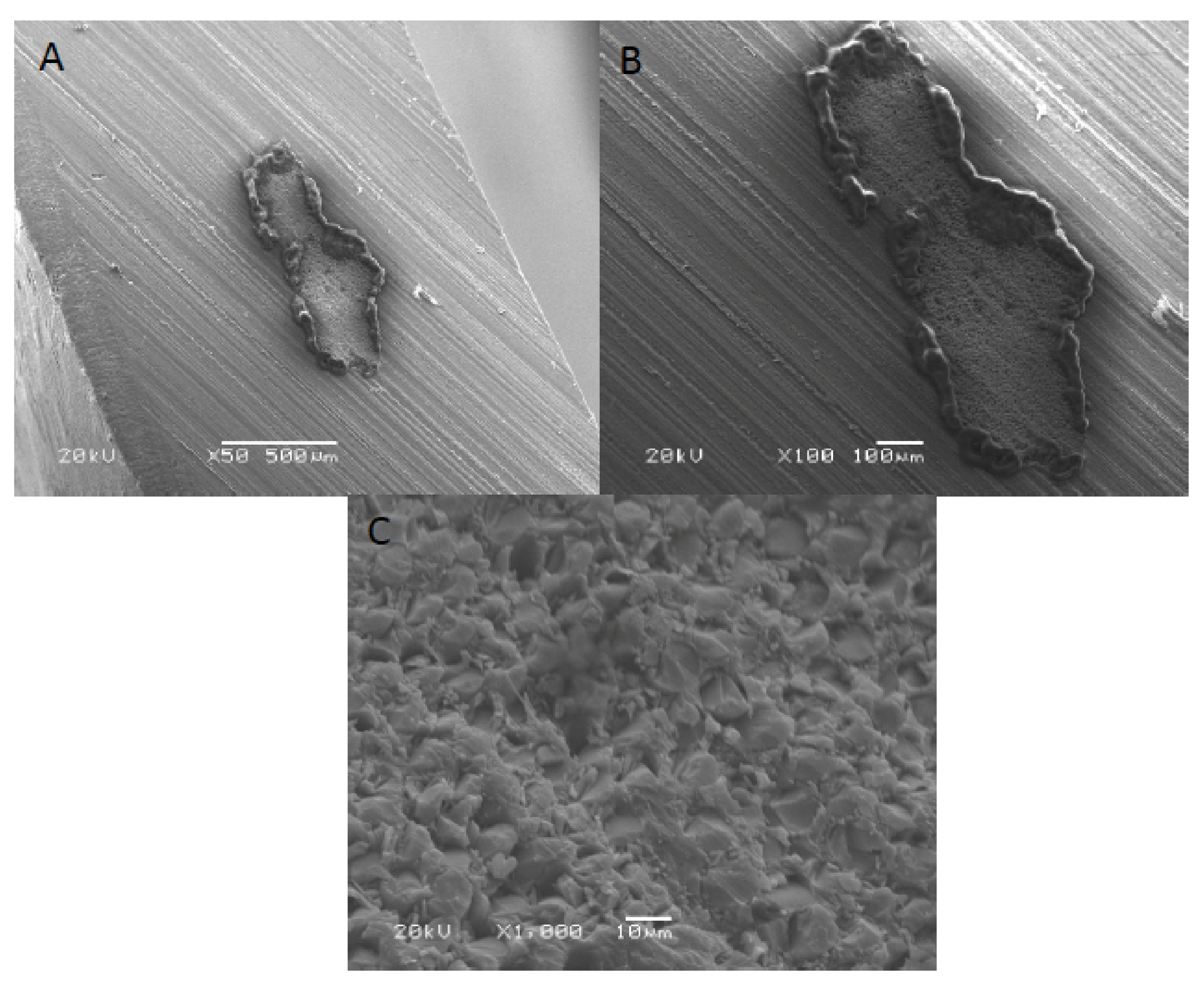
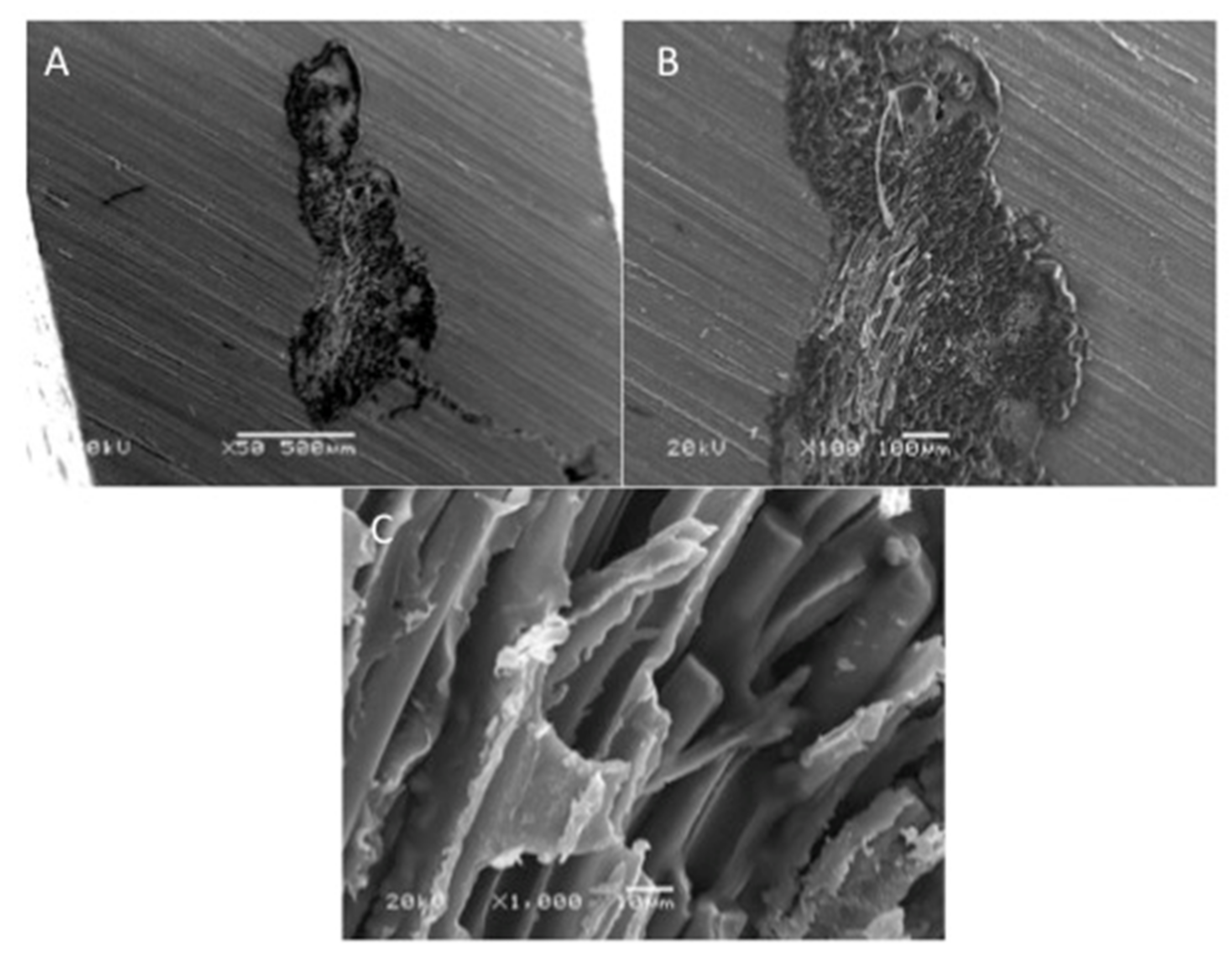
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Karci, M.; Demir, N.; Yazman, S. Evaluation of Flexural Strength of Different Denture Base Materials Reinforced with Different Nanoparticles. J. Prosthodont. 2019, 28, 572–579. [Google Scholar] [CrossRef]
- Zafar, M.S. Prosthodontic applications of polymethyl methacrylate (PMMA): An update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Rahal, J.S.; Mesquita, M.F.; Henriques, G.E.P.; Nóbilo, M.A.A. Surface roughness of acrylic resins submitted to mechanical and chemical polishing. J. Oral Rehabil. 2004, 31, 1075–1079. [Google Scholar] [CrossRef] [PubMed]
- Phoenix, R.D. Denture base materials. Dent. Clin. N. Am. 1996, 40, 113–120. [Google Scholar] [PubMed]
- Gul, H.; Aslam, A.; Nayyer, M.; Kaleem, M. Possible errors in acrylic denture fabrication leading to teeth-denture base interface failure. Pak. Oral Dent. J. 2017, 37, 510–515. [Google Scholar]
- Johnston, E.P.; Nicholls, J.I.; Smith, D.E. Flexure fatigue of 10 commonly used denture base resins. J. Prosthet. Dent. 1981, 46, 478–483. [Google Scholar] [CrossRef]
- Han, S.Y.; Moon, Y.H.; Lee, J. Shear bond strength between CAD/CAM denture base resin and denture artificial teeth when bonded with resin cement. J. Adv. Prosthodont. 2020, 12, 251–258. [Google Scholar] [CrossRef]
- Prajwala, N.; Ravi Kumar, C.; Sujesh, M.; Chalapathi Rao, D.; Pavani, L. Denture base reinforcing materials—A review. IP Ann. Prosthodont. Restor. Dent. 2020, 6, 52–59. [Google Scholar] [CrossRef]
- Teraoka, F.; Nakagawa, M.; Takahashi, J. Adaptation of acrylic dentures reinforced with metal wire. J. Oral Rehabil. 2001, 28, 937–942. [Google Scholar] [CrossRef]
- Transverse Strength of Reinforced Denture Base Resin with Metal Wire and E-Glass Fibers. Available online: https://www.researchgate.net/publication/228357826_Transverse_Strength_of_Reinforced_Denture_Base_Resin_with_Metal_Wire_and_E-Glass_Fibers (accessed on 21 June 2021).
- Kanie, T.; Arikawa, H.; Fujii, K.; Ban, S. Color change in acrylic denture base resin reinforced with wire mesh and glass cloth. Dent. Mater. J. 2003, 22, 425–435. [Google Scholar] [CrossRef] [Green Version]
- Somani, M.V.; Khandelwal, M.; Punia, V.; Sharma, V. The effect of incorporating various reinforcement materials on flexural strength and impact strength of polymethylmethacrylate: A meta-analysis. J. Indian Prosthodont. Soc. 2019, 19, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Alla, R.K.; Sajjan, S.; Alluri, V.R.; Ginjupalli, K.; Upadhya, N. Influence of Fiber Reinforcement on the Properties of Denture Base Resins. Biomater. Nanobiotechnol. 2013, 4, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef] [Green Version]
- Goguaţǎ, L.M.; Bratu, D.; Jivǎnescu, A.; Erimescu, R.; Mǎrcǎuaţeanu, C. Glass fibre reinforced acrylic resin complete dentures: A 5-year clinical study. Gerodontology 2012, 29, 64–69. [Google Scholar] [CrossRef]
- Larson, W.R.; Dixon, D.L.; Aquilino, S.A.; Clancy, J.M.S. The effect of carbon graphite fiber reinforcentent on the strength of provisional crown and fixed partial denture resins. J. Prosthet. Dent. 1991, 66, 816–820. [Google Scholar] [CrossRef]
- John, J.; Gangadhar, S.A.; Shah, I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J. Prosthet. Dent. 2001, 86, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.H.; Cho, H.W.; Oh, S.; Bae, J.M. Effects of glass fiber mesh with different fiber content and structures on the compressive properties of complete dentures. J. Prosthet. Dent. 2015, 113, 636–644. [Google Scholar] [CrossRef]
- Heintze, S.D.; Eser, A.; Monreal, D.; Rousson, V. Using a chewing simulator for fatigue testing of metal ceramic crowns. J. Mech. Behav. Biomed. Mater. 2017, 65, 770–780. [Google Scholar] [CrossRef]
- AlHelal, A.; AlRumaih, H.S.; Kattadiyil, M.T.; Baba, N.Z.; Goodacre, C.J. Comparison of retention between maxillary milled and conventional denture bases: A clinical study. J. Prosthet. Dent. 2017, 117, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.D.; Darvell, B.W. The evolution of the complete denture base. Theories of complete denture retention—A review. Part 1. Aust. Dent. J. 1993, 38, 216–219. [Google Scholar] [CrossRef]
- Cunningham, J.L.; Benington, I.C. An investigation of the variables which may affect the bond between plastic teeth and denture base resin. J. Dent. 1999, 27, 129–135. [Google Scholar] [CrossRef]
- Chen, J.C.; Lacefield, W.R.; Castleberry, D.J. Effect of denture thickness and curing cycle on the dimensional stability of acrylic resin denture bases. Dent. Mater. 1988, 4, 20–24. [Google Scholar] [CrossRef]
- Sarikaya, I.; Hayran, Y. Effects of dynamic aging on the wear and fracture strength of monolithic zirconia restorations. BMC Oral Health 2018, 18, 146. [Google Scholar] [CrossRef]
- Jagger, D.C.; Harrison, A.; Jandt, K.D. The reinforcement of dentures. J. Oral Rehabil. 1999, 26, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven glass fibers. J. Prosthet. Dent. 1999, 81, 318–326. [Google Scholar] [CrossRef]
- Vallittu, P.K. Glass fiber reinforcement in repaired acrylic resin removable dentures: Preliminary results of a clinical study. Quintessence Int. 1997, 28, 39–44. [Google Scholar] [PubMed]
- Narva, K.K.; Vallittu, P.K.; Helenius, H.; Yli-Urpo, A. Clinical Survey of Acrylic Resin Removable Denture Repairs with Glass-Fiber Reinforcement. Int. J. Prosthodont. 2001, 14, 219–224. [Google Scholar]
- Stipho, H.D. Repair of acrylic resin denture base reinforced with glass fiber. J. Prosthet. Dent. 1998, 80, 546–550. [Google Scholar] [CrossRef]
- Vijay, A.; Prabhu, N.; Balakrishnan, D.; Narayan, A.I. Comparative study of the flexural strength of high impact denture base resins reinforced by silver nanoparticles and e-glass fibres: An in-vitro study. J. Clin. Diagn. Res. 2018, 12, 22–26. [Google Scholar] [CrossRef]
- Kim, S.H.; Watts, D.C. The effect of reinforcement with woven E-glass fibers on the impact strength of complete dentures fabricated with high-impact acrylic resin. J. Prosthet. Dent. 2004, 91, 274–280. [Google Scholar] [CrossRef]
- Glass Fiber Reinforced Polymer (GFRP)—Technology in Architecture. Available online: https://technologyinarchitecture.wordpress.com/2018/06/30/glass-fiber-reinforced-polymer-gfrp/ (accessed on 22 June 2021).
- Sekinishi, T.; Inukai, S.; Murakami, N.; Wakabayashi, N. Influence of denture tooth thickness on fracture mode of thin acrylic resin bases: An experimental and finite element analysis. J. Prosthet. Dent. 2015, 114, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Acharya, V.; Berg, R.W.; Marotta, J.; Green, C.C.; Barbizam, J.V.; White, S.N. Resinous denture base fracture loads: Effects of thickness and teeth. Int. J. Prosthodont. 2012, 25, 53–59. [Google Scholar] [PubMed]
- Żmudzki, J.; Chladek, G.; Kasperski, J. Biomechanical factors related to occlusal load transfer in removable complete dentures. Biomech. Model. Mechanobiol. 2015, 14, 679–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study Groups | Materials for Reinforcement |
|---|---|
| Group 1 | Dental fiberglass framework, Group Z: SES Mesh, Inno dental Co. Ltd., Seoul, Korea |
| Group 2 | Orthopedic casting tape, Delta Lite Plus, BSN medical GMBH., Frankfurt, Germany |
| Group 3 | Orthopedic casting tape 2, Shanghai Nineluck Co. Ltd., Beijing, China |
| Group 4 (control) | Heat Cure acrylic no reinforcements Meliodent Heat Cure, Kulzer GmbH., Frankfurt, Germany |
| Group | Mean (N) | SD (N) | ANOVA p-Value | Kruskal-Wallis p-Value | Group Comparison | Z-Value | Adjusted p-Value |
|---|---|---|---|---|---|---|---|
| 1 | 692.33 | 75.41 | <0.001 | <0.001 | 2 vs. 3 | −2.27 | 0.03 |
| 2 vs. 4 | 2.59 | 0.02 | |||||
| 2 | 487.40 | 51.72 | 3 vs. 4 | 4.86 | 0.00 | ||
| 3 | 486.94 | 52.39 | 1 vs. 2 | 0.02 | 0.99 | ||
| 1 vs. 3 | −2.26 | 0.03 | |||||
| 4 | 281.41 | 30.51 | 1 vs. 4 | 2.61 | 0.03 |
| Variable | Pearson CC | Pearson p-Value | Spearma CC | Spearman p-Value |
|---|---|---|---|---|
| Thickness | 0.751 | <0.001 | 0.822 | <0.001 |
| Weight | 0.812 | <0.001 | 0.862 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rana, M.H.; Shaik, S.; Hameed, M.S.; Al-Saleh, S.; AlHamdan, E.M.; Alshahrani, A.; Alqahtani, A.; Albaqawi, A.H.; Vohra, F.; Abduljabbar, T. Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin. Polymers 2021, 13, 2793. https://doi.org/10.3390/polym13162793
Rana MH, Shaik S, Hameed MS, Al-Saleh S, AlHamdan EM, Alshahrani A, Alqahtani A, Albaqawi AH, Vohra F, Abduljabbar T. Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin. Polymers. 2021; 13(16):2793. https://doi.org/10.3390/polym13162793
Chicago/Turabian StyleRana, Muhammad H., Sharaz Shaik, Mohammad S. Hameed, Samar Al-Saleh, Eman M. AlHamdan, Abdullah Alshahrani, Abdulaziz Alqahtani, Ahmed Heji Albaqawi, Fahim Vohra, and Tariq Abduljabbar. 2021. "Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin" Polymers 13, no. 16: 2793. https://doi.org/10.3390/polym13162793
APA StyleRana, M. H., Shaik, S., Hameed, M. S., Al-Saleh, S., AlHamdan, E. M., Alshahrani, A., Alqahtani, A., Albaqawi, A. H., Vohra, F., & Abduljabbar, T. (2021). Influence of Dental Glass Fibers and Orthopedic Mesh on the Failure Loads of Polymethyl Methacrylate Denture Base Resin. Polymers, 13(16), 2793. https://doi.org/10.3390/polym13162793






