Can the Timed and Targeted Counseling Model Improve the Quality of Maternal and Newborn Health Care? A Process Analysis in the Rural Hoima District in Uganda
Abstract
:1. Background
2. Methods
2.1. Study Design
2.2. Study Area
2.3. Study Population
2.4. Ethics Approval
2.5. Intervention
2.6. Study Instrument and Variables
2.7. Data Management and Analysis
2.8. Relevance of the Study
3. Results
3.1. Social Demographic Characteristics of Participants
3.2. Changes in Key Outcomes
3.3. Quality of Care
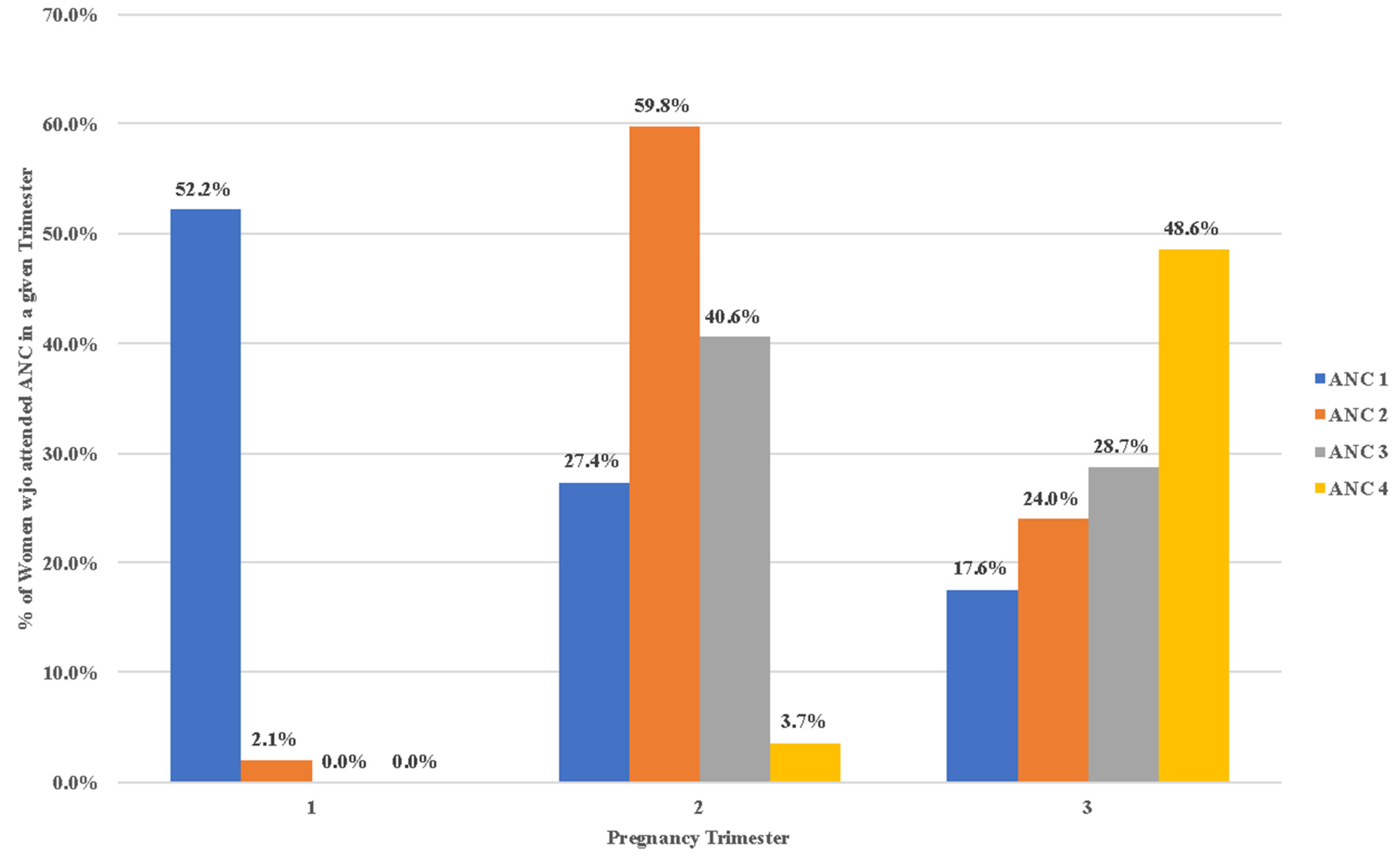
3.4. Timely ANC Visits Recorded by the VHT
3.5. ANC Appropriate Services and Home Practices
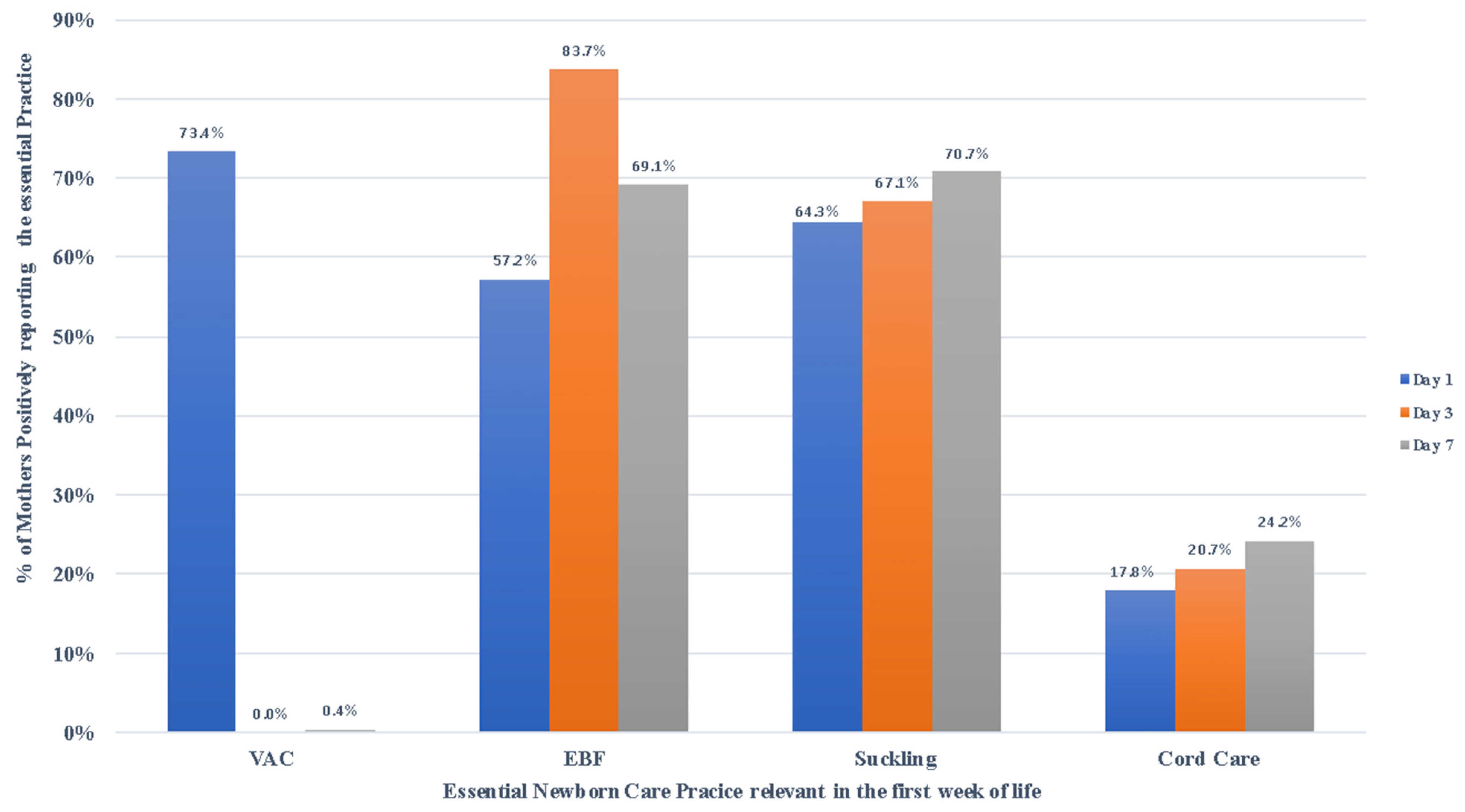
3.6. Essential Newborn Care during the First Week after Childbirth
3.7. Newborn Care at Six Weeks after Childbirth
3.8. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. More Women and Children Survive Today than Ever Before—UN Report; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Stella, K. Childbirth in Uganda: Stories from Women and Health Workers; The Health newborn network: Kampala, Uganda, 2017. [Google Scholar]
- Hodgins, S.; Tielsch, J.; Rankin, K.; Robinson, A.; Kearns, A.; Caglia, J. A New Look at Care in Pregnancy: Simple, Effective Interventions for Neglected Populations. PLoS ONE 2016, 11, e0160562. [Google Scholar] [CrossRef] [Green Version]
- Babughirana, G.; Gerards, S.; Mokori, A.; Nangosha, E.; Kremers, S.; Gubbels, J. Maternal and newborn healthcare practices: Assessment of the uptake of lifesaving services in Hoima District, Uganda. BMC Pregnancy Childbirth 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Ganle, J.K.; Kombet, M.L.; Baatiema, L. Factors influencing the use of supervised delivery services in Garu-Tempane District, Ghana. BMC Pregnancy Childbirth 2019, 19, 141. [Google Scholar] [CrossRef]
- Kate, J.K.; Joseph, E.d.G.-J.; Zulfi, q.A.B.; Pius, O.; Ann, S.; Joy, E.L. The Maternal, Newborn, and Child Health Continuum of Care; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Singh, K.; Story, W.T.; Moran, A.C. Assessing the Continuum of Care Pathway for Maternal Health in South Asia and Sub-Saharan Africa. Matern. Child Health J. 2016, 20, 281–289. [Google Scholar] [CrossRef] [Green Version]
- United Nations International Children’s Emergency Fund. The State of the World’s Children: Maternal and Newborn Health; UNICEF: New York, NY, USA, 2009. [Google Scholar]
- Moller, A.; Patten, J.H.; Hanson, C.; Morgan, A.; Say, L.; Diaz, T.; Moran, A.C. Monitoring maternal and newborn health outcomes globally: A brief history of key events and initiatives. Trop. Med. Int. Health 2019, 24, 1342–1368. [Google Scholar] [CrossRef] [Green Version]
- Bowser, D.; Okunogbe, A.; Oliveras, E.; Subramanian, L.; Morrill, T. A Cost-Effectiveness Analysis of Community Health Workers in Mozambique. J. Prim. Care Community Health 2015, 6, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Kabir, R.; Majumder, A.A.; Arafat, S.Y.; Chodwhury, R.K.; Sultana, S.; Ahmed, S.M.; Monte-Serrat, D.M.; Chowdhury, E.Z. Impact of Intimate Partner violence on ever married women and utilization of antenatal care services in Tanzania. J. Coll. Med. Sci. 2018, 14, 7–13. [Google Scholar] [CrossRef] [Green Version]
- Perry, S.; Fair, C.D.; Burrowes, S.; Holcombe, S.J.; Kalyesubula, R. Outsiders, insiders, and intermediaries: Village health teams’ negotiation of roles to provide high quality sexual, reproductive and HIV care in Nakaseke, Uganda. BMC Health Serv. Res. 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Gogia, S.; Sachdev, H.P.S. Home-based neonatal care by community health workers for preventing mortality in neonates in low- and middle-income countries: A systematic review. J. Perinatol. 2016, 36, S55–S73. [Google Scholar] [CrossRef] [Green Version]
- Guenther, T.; Nsona, H.; Makuluni, R.; Chisema, M.; Jenda, G.; Chimbalanga, E.; Sadruddin, S. Home visits by community health workers for pregnant mothers and newborns: Coverage plateau in Malawi. J. Glob. Health 2019, 9, 010808. [Google Scholar] [CrossRef]
- Namazzi, G.; Waiswa, P.; Nakakeeto, M.; Nakibuuka, V.K.; Namutamba, S.; Najjemba, M.; Namusaabi, R.; Tagoola, A.; Nakate, G.; Ajeani, J.; et al. Strengthening health facilities for maternal and newborn care: Experiences from rural eastern Uganda. Glob. Health Action 2015, 8, 24271. [Google Scholar] [CrossRef] [Green Version]
- Besada, D.; Eagar, D.; Rensburg, R.; Shabangu, G.; Hlahane, S.; Daviaud, E. Resource requirements for community-based care in rural, deep-rural and peri-urban communities in South Africa: A comparative analysis in 2 South African provinces. PLoS ONE 2020, 15, e0218682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michele, G.; Polly, W. Timed and Targeted Counselling for Health and Nutrition (2nd Edition): A Comprehensive Training Course for Community Health Workers; World Vision International: Middlesex, UK, 2015. [Google Scholar]
- Reithinger, R.; Megazzini, K.; Durako, S.J.; Harris, D.R.; Vermund, S.H. Monitoring and evaluation of programmes to prevent mother to child transmission of HIV in Africa. BMJ 2007, 334, 1143–1146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Health & Nutrition Technical Brief: Timed and Targeted Counselling (TTC). A Service Package of the CHW Project Model. 2020. Available online: https://reliefweb.int/report/afghanistan/health-nutrition-technical-brief-timed-and-targeted-counselling-ttc-service (accessed on 6 February 2020).
- Warner, M.E.; Zhang, X. Healthy Places for Children: The Critical Role of Engagement, Common Vision, and Collaboration. Int. J. Environ. Res. Public Health 2020, 17, 9277. [Google Scholar] [CrossRef]
- Uganda Bureau of Statistics. The National Population and Housing Census 2014—Area Specific Profile Series for Hoima District; Uganda Bureau of Statistics: Kampala, Uganda, 2017. [Google Scholar]
- Stephen, B.; Laura, G. Livelihood Mapping and Zoning Exercise: Uganda. A special Report by the Famine Early Warning System Network (Fewsnet); United States Agency for International Development: Washington, DC, USA, 2010. [Google Scholar]
- Kawungezi, P.C.; AkiiBua, D.; Aleni, C.; Chitayi, M.; Niwaha, A.; Kazibwe, A.; Sunya, E.; Mumbere, E.W.; Mutesi, C.; Tukei, C.; et al. Attendance and Utilization of Antenatal Care (ANC) Services: Multi-Center Study in Upcountry Areas of Uganda. Open J. Prev. Med. 2015, 5, 132–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babughirana, G.; Gerards, S.; Mokori, A.; Musasizi, B.; Isabirye, N.; Baigereza, I.C.; Rukanda, G.; Bussaja, E.; Kremers, S.; Gubbels, J. Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Sur-vival in Rural Uganda: Protocol for a Quasi-Experimental Study. Methods Protoc. 2020, 3, 73. [Google Scholar] [CrossRef]
- Ministry of Health Uganda. The Reproductive Health, Maternal, Newborn and Child Health Sharpened Plan; Ministry of Health Uganda: Kampala, Uganda, 2013. [Google Scholar]
- Kaphle, H.P.; Poudel, S.; Gupta, N.; Neupane, N. Maternal Awareness on Child Health Card and Factors Associated with its Retention in Salyan Village Development Committee of Kaski, Nepal. Int. Biol. Biomed. J. 2016, 2. Available online: http://ibbj.org/article-1-75-en.pdf (accessed on 16 March 2016).
- Al–Rabadi, H.S.; Sharif, N.E. Effectiveness of timed and targeted counselling about feeding and caring practices for infants and young children to mothers in West Bank: A randomised controlled trial. Lancet 2017, 390, S23. [Google Scholar] [CrossRef]
- Ministry of Health. Village Health Teams, Strategy and Operational Guidelines; Ministry of Health: Kampla, Uganda, 2010. [Google Scholar]
- World Vision. World Vision’s Time and Targeted Counselling: The World’s most Widespread Family Inclusive Maternal Health Project (28 Countries). 2017. Available online: https://familyincluded.com/world-vision-ttc/ (accessed on 17 February 2010).
- Benova, L.; Dennis, M.L.; Lange, I.L.; Campbell, O.M.R.; Waiswa, P.; Haemmerli, M.; Fernandez, Y.; Kerber, K.; Lawn, J.E.; Santos, A.C.; et al. Two decades of antenatal and delivery care in Uganda: A cross-sectional study using Demographic and Health Surveys. BMC Health Serv. Res. 2018, 18, 1–15. [Google Scholar] [CrossRef] [Green Version]
- McPherson, R.A.; Khadka, N.; Moore, J.M.; Sharma, M. Are Birth-preparedness Programmes Effective? Results from a Field Trial in Siraha District, Nepal. J. Health Popul. Nutr. 2006, 24, 479–488. [Google Scholar]
- Han’a Salim Al, R. Effectiveness of Timed and Targeted Counselling on Maternal, Newborn and Child Health and Nutrition (MNCH/N) Outcomes in Palestine: Assessment of Intervention. 2015. Available online: https://www.mhtf.org/document/effectiveness-of-timed-and-targeted-counselling-on-maternal-newborn-and-child-health-and-nutrition-mnchn-outcomes-in-palestine-assessment-of-intervention/ (accessed on 20 May 2015).
- Monitoring the Situation of Children and Women, Antenatal Care; UNICEF: New York, NY, USA, 2020.
- Genç, M.; Ledger, W.J. Syphilis in pregnancy. Sex. Transm. Infect. 2000, 76, 73–79. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. 20 Avenue Appia; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Kimario, F.F.; Festo, C.; Shabani, J.; Mrisho, M. Determinants of Home Delivery among Women Aged 15–24 Years in Tanzania. Int. J. MCH AIDS (IJMA) 2020, 9, 191–199. [Google Scholar] [CrossRef] [PubMed]
- United Nations Development Programme. Sustainable Development Goal 3. Ensure Healthy Lives and Promote Well-Being for All at All Ages. 2015. Available online: https://sustainabledevelopment.un.org/sdg3 (accessed on 20 January 2015).
- Lema, I.A.; Sando, D.; Magesa, L.; Machumi, L.; Mungure, E.; Sando, M.M.; Geldsetzer, P.; Foster, D.; Kajoka, D.; Naburi, H.; et al. Community Health Workers to Improve Antenatal Care and PMTCT Uptake in Dar es Salaam, Tanzania. JAIDS J. Acquir. Immune Defic. Syndr. 2014, 67, S195–S201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haines, A.; Sanders, D.; Lehmann, U.; Rowe, A.K.; E Lawn, J.; Jan, S.; Walker, D.G.; Bhutta, Z. Achieving child survival goals: Potential contribution of community health workers. Lancet 2007, 369, 2121–2131. [Google Scholar] [CrossRef]
- Venyuy, M.A.; Cumber, S.N.; Nkfusai, C.N.; Bede, F.; Ijang, Y.P.; Wepngong, E.; Bama, S.N.; Tsoka-Gwegweni, J.M.; Tebeu, P.M. Determinants to late antenatal clinic start among pregnant women: The case of Saint Elizabeth General Hospital, Shisong, Cameroon. Pan Afr. Med. J. 2020, 35, 112. [Google Scholar] [CrossRef] [PubMed]
- Cook Children’s Health Care System. Eating during Pregnancy; Cook Children’s Health Care System: Fort Worth, TX, USA, 2020. [Google Scholar]
- Elana Pearl Ben-Joseph. Eating during Pregnancy. 2020. Available online: https://kidshealth.org/en/parents/eating-pregnancy.html (accessed on 3 June 2020).
- Uganda Bureau of Statistics (UBOS); ICF. Uganda Demographic and Health Survey 2016; UBOS: Kampala, Uganda; ICF: Rockville, MD, USA, 2018. [Google Scholar]
- World Health Organization. Newborns: Improving Survival and Well-Being; WHO: New York, NY, USA, 2019. [Google Scholar]
- Charlotte, W.; Pat, D.; Lalla, T.; Pyande, M. Postnatal Care; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Ministry of Health Uganda. A Handbook to Improve Health in Communities; Village Health Team: Kampala, Uganda, 2010. [Google Scholar]
 = baseline values;
= baseline values;  = post-implementation values; ANC = Antenatal care; ENC = Essential Newborn care; EBF = Exclusive Breastfeeding.
= post-implementation values; ANC = Antenatal care; ENC = Essential Newborn care; EBF = Exclusive Breastfeeding.
 = baseline values;
= baseline values;  = post-implementation values; ANC = Antenatal care; ENC = Essential Newborn care; EBF = Exclusive Breastfeeding.
= post-implementation values; ANC = Antenatal care; ENC = Essential Newborn care; EBF = Exclusive Breastfeeding.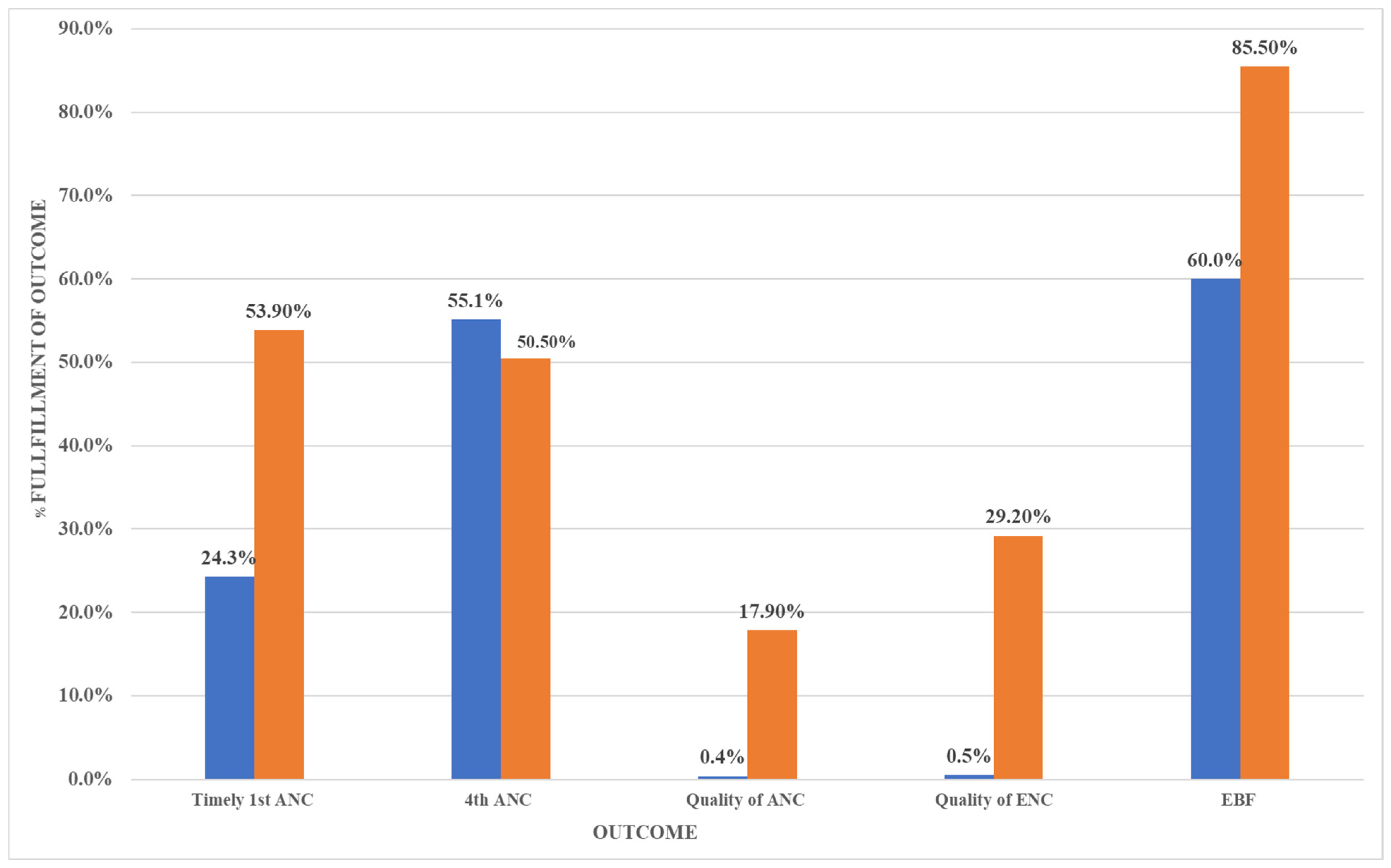
| Visit | Timing | Services Delivered by the VHTs |
|---|---|---|
| 1 | Before or at 3 months of pregnancy | Focuses on suspected pregnant mothers registered as ttC candidates. They are counseled on how to care for themselves during pregnancy, a number of danger signs during pregnancy are explained, and the family is encouraged to notify the VHT in the case of any of these danger signs. Families are counseled on what to do during pregnancy and when giving birth. Women are advised to start ANC before or at three months pregnancy. |
| 2 | 4 months of pregnancy | This visit is to affirm that the pregnant mother went for the first ANC visit and to encourage them to go for the second ANC visit. Pregnant women are educated on the advantages of exclusive breastfeeding of children until 6 months and continuous breastfeeding until they reach the age of 2. In addition, advantages of giving birth in a health facility and hand washing are highlighted. |
| 3 | 6 months of pregnancy | Discussion of the birth plan, timing, and place of the birth, exploring potential challenges faced by expectant mothers in reaching the health facility and ways of overcoming these challenges. Expectant mothers are given information on the different family planning methods and where to go for services, and they are encouraged to utilize one of the methods after delivery. |
| 4 | 8 months of pregnancy | The mother and family are educated about the early signs of true labor, danger signs during labor, and appropriate action to take in the case of these danger signs. The mother is also encouraged to deliver at a health facility and have emergency money available. In addition, the VHTs check whether the mother has a clean birthing kit available (the “Mama Kit”). |
| 5–7 | The newborn period (Days 1, 3, and 7) | This visit is done three times in the first week after birth, on days 1, 3, and 7. The VHT ensures that exclusive breastfeeding and essential maternal and newborn care are understood and practiced. Mothers are educated on the need to seek health care if the neonate develops fever and/or a cough, and the need to go for routine growth monitoring and immunization. |
| 8 | When the baby is 6 weeks old | Malaria prevention is discussed, as well as other illnesses, danger signs in the baby, immunization for the baby, and hygiene practices. The VHT checks whether the child’s growth card has been plotted, gives support for exclusive breastfeeding, checks if the child has had its HIV confirmatory test as part of the prevention of mother-to-child transition of the HIV program, and whether the mother has thought about family planning methods. |
| Variable | Description | Assessed at Baseline (Y/N) a |
|---|---|---|
| Key outcome variables | ||
| Quality of ANC services | The pregnant woman is able to visit a health facility for ANC and receive the eight key services in the goal-oriented ANC recommendations. | Y |
| Quality of ANC care at home | The pregnant woman performs the key four practices at home appropriate for the pregnancy period [34]. These include: woman having adequate rest, extra meal, sleeping LLTIN, and having a hand-washing facility at the home. | N |
| Appropriate childbirth practices | The pregnant woman is supported to practice the four key lifesaving actions prior to or during the time of birth [35]. These include plans to deliver at a health facility, discussion of a birth plan, delivery at the health facility, and provision of a clean birthing kit. | N |
| Timely ANC attendance | The pregnant woman attends ANC visits in a timely manner as recommended by the WHO and the Ugandan goal-oriented ANC [36]. | Y |
| Quality of essential newborn care | Mothers performing the six key essential newborn care practices both at the health facility and at home within the newborn period of 28 days after birth. These include mother was visited by the VHT during the 1st week of birth, baby sleeping under LLTIN, practicing exclusive breastfeeding, suckling well, birth weight of the baby recorded in the CHC, and the baby has been vaccinated. | Y |
| Exclusive breastfeeding | Mother was able to sustain exclusive breastfeeding to the baby up to 6 weeks. | Y |
| Quality of care variables | ||
| Quality of ANC services | ||
| Woman given folic acid during ANC | Pregnant woman is given iron–folic acid tablets at all ANC visits to the health facility. | Y |
| Woman given Fansidar during ANC | Pregnant woman taking a directly observed dose of Fansidar at the health facility during ANC. | Y |
| Woman tested for HIV and results given | Pregnant woman does a routine HIV test at the health facility during the ANC visit. | Y |
| Woman given deworming during pregnancy | Pregnant woman is given a dewormer at the health facility during the ANC visit. | N |
| Woman vaccinated for Tetanus Toxoid (TT) once | The pregnant woman is given at least one dose of TT vaccine during the pregnancy period by the health facility. | N |
| ANC first trimester | Pregnant woman visiting the health facility for her first ANC visit within the first 12 weeks of pregnancy. | Y |
| 4th ANC or more | Pregnant women has attended the health facility for four or more ANC visits. | Y |
| Woman tested for syphilis | Pregnant woman takes a syphilis [26] test at least once during the pregnancy period during ANC and receives the results of the test. | N |
| Quality of ANC care at home | ||
| Woman having adequate rest | The pregnant woman is deliberately taking rest from laborious work during the day, and this is due to the pregnancy condition. | N |
| Woman having an extra meal | The pregnant woman consumes an extra meal on top of her usual meal frequency when not pregnant. | N |
| Woman sleeping in a long-lasting insecticide treated net (LLITN) | The pregnant woman slept under an insecticide-treated bed net the night before the visit made by the VHT. | Y |
| Hand washing facility at the home | There is a visible hand washing facility on the walkway to the latrine of the household. | N |
| Appropriate childbirth practices | ||
| Woman plans to deliver at health facility | The pregnant woman is planning to deliver at the nearest health facility. | N |
| Woman discussed a birth plan | During the 3rd trimester, the pregnant women has discussed a birth plan with the VHT on one of the visits. | Y |
| Delivery at the health facility | The pregnant woman actually delivered at the health facility. | Y |
| Woman has a clean birthing kit | The pregnant woman is given a clean birthing kit by the health facility. | Y |
| Quality of Essential Newborn Care (ENC) | ||
| Mother visited during the 1st week | The VHT performs at least one visit to the household during the 1st newborn week. | N |
| Baby sleeping under an LLITN | During the newborn period visits, the newborn is sleeping under an insecticide-treated bed net. | Y |
| Practicing exclusive breastfeeding | For the 24 hours previous to the household visit, the mother has not given anything to the newborn except for breast milk apart from medication prescribed by medical personnel to the baby. | Y |
| Baby suckling well | The VHT is observing breastfeeding and notices that the baby is suckling well. | N |
| Birth weight record | At discharge from the health facility, the newborn is weighed, and the weight is recorded on the child health card. | N |
| Vaccination | The newborn is given the vaccines appropriate for that time period. | N |
| Infant visited at 6 weeks | ||
| Visitation at 6 weeks | The VHT checked on the 6-week vaccinations, whether the baby was taken for growth monitoring and promotion, and whether the mother knew how to prepare oral rehydration salts in the case of a diarrheal episode. The VHT also checked whether the mother had a discussion at the HF about family planning choices. | N |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babughirana, G.; Gerards, S.; Mokori, A.; Baigereza, I.C.; Mukembo, A.; Rukanda, G.; Kremers, S.P.J.; Gubbels, J. Can the Timed and Targeted Counseling Model Improve the Quality of Maternal and Newborn Health Care? A Process Analysis in the Rural Hoima District in Uganda. Int. J. Environ. Res. Public Health 2021, 18, 4410. https://doi.org/10.3390/ijerph18094410
Babughirana G, Gerards S, Mokori A, Baigereza IC, Mukembo A, Rukanda G, Kremers SPJ, Gubbels J. Can the Timed and Targeted Counseling Model Improve the Quality of Maternal and Newborn Health Care? A Process Analysis in the Rural Hoima District in Uganda. International Journal of Environmental Research and Public Health. 2021; 18(9):4410. https://doi.org/10.3390/ijerph18094410
Chicago/Turabian StyleBabughirana, Geoffrey, Sanne Gerards, Alex Mokori, Isaac Charles Baigereza, Alex Mukembo, Grace Rukanda, Stef P. J. Kremers, and Jessica Gubbels. 2021. "Can the Timed and Targeted Counseling Model Improve the Quality of Maternal and Newborn Health Care? A Process Analysis in the Rural Hoima District in Uganda" International Journal of Environmental Research and Public Health 18, no. 9: 4410. https://doi.org/10.3390/ijerph18094410






