Incentive Mechanism for Online–Offline Dual-Channel Healthcare Services While Considering Spillover Effects
Abstract
1. Introduction
- (1)
- How do public hospitals, online healthcare platforms, and physicians determine their respective optimal decisions in this multi-agent game?
- (2)
- How do non-economic incentives (online reputation) modulate the design of economic incentives and influence physicians’ effort allocation between dual channels?
- (3)
- How do spillover effects impact the setting of incentive intensity across online and offline channels and shape physicians’ effort exertion decisions?
2. Literature
2.1. Healthcare Service System in China
2.2. Principal–Agent Theory
2.3. Motivating Factors for Doctors in Online Healthcare
2.4. Spillover Effects in Supply Chain Channels
3. Modeling and Comparative Analysis
3.1. Problem Description and Model Assumptions
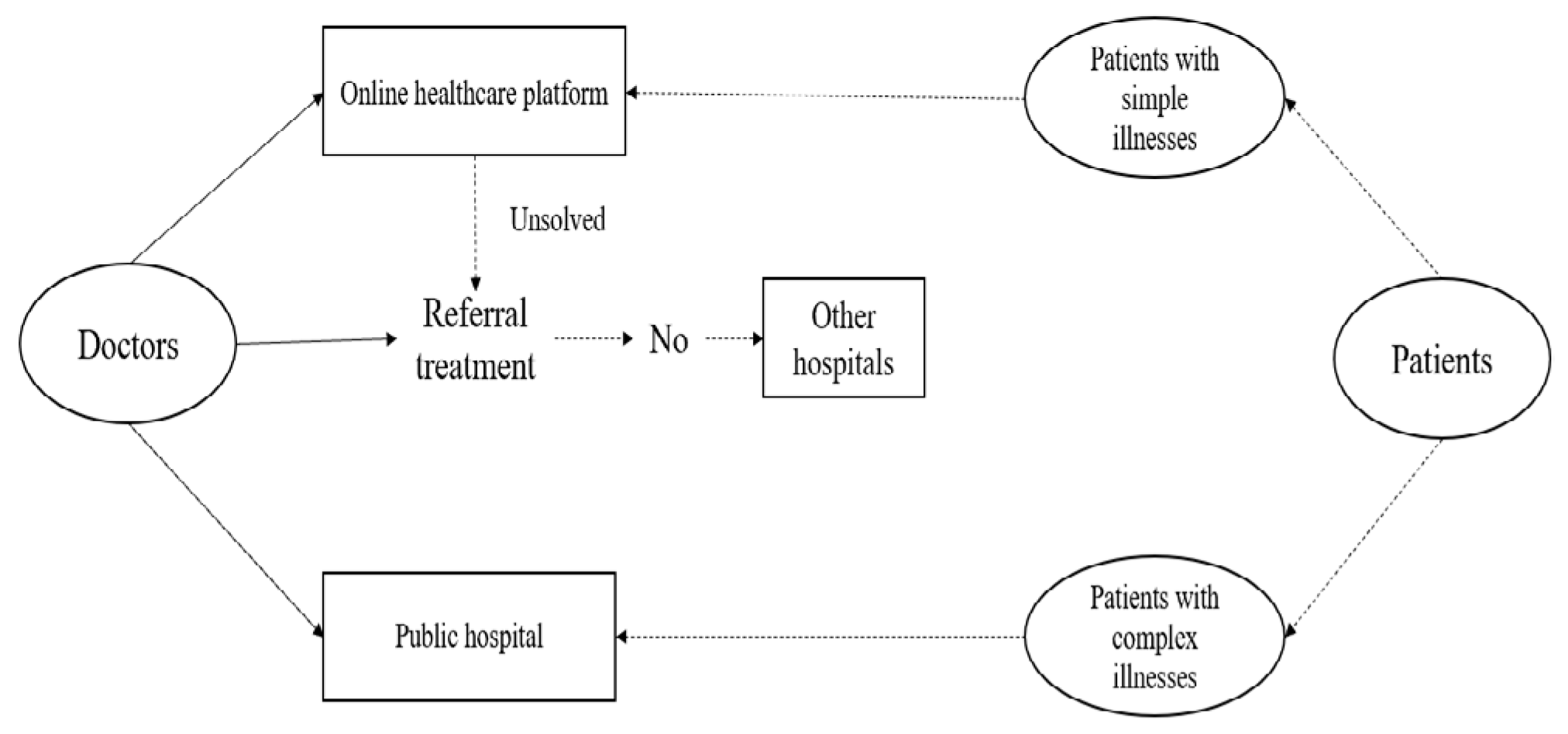
3.2. Dual-Channel Healthcare Service Common Agency Model Without Spillover Effects
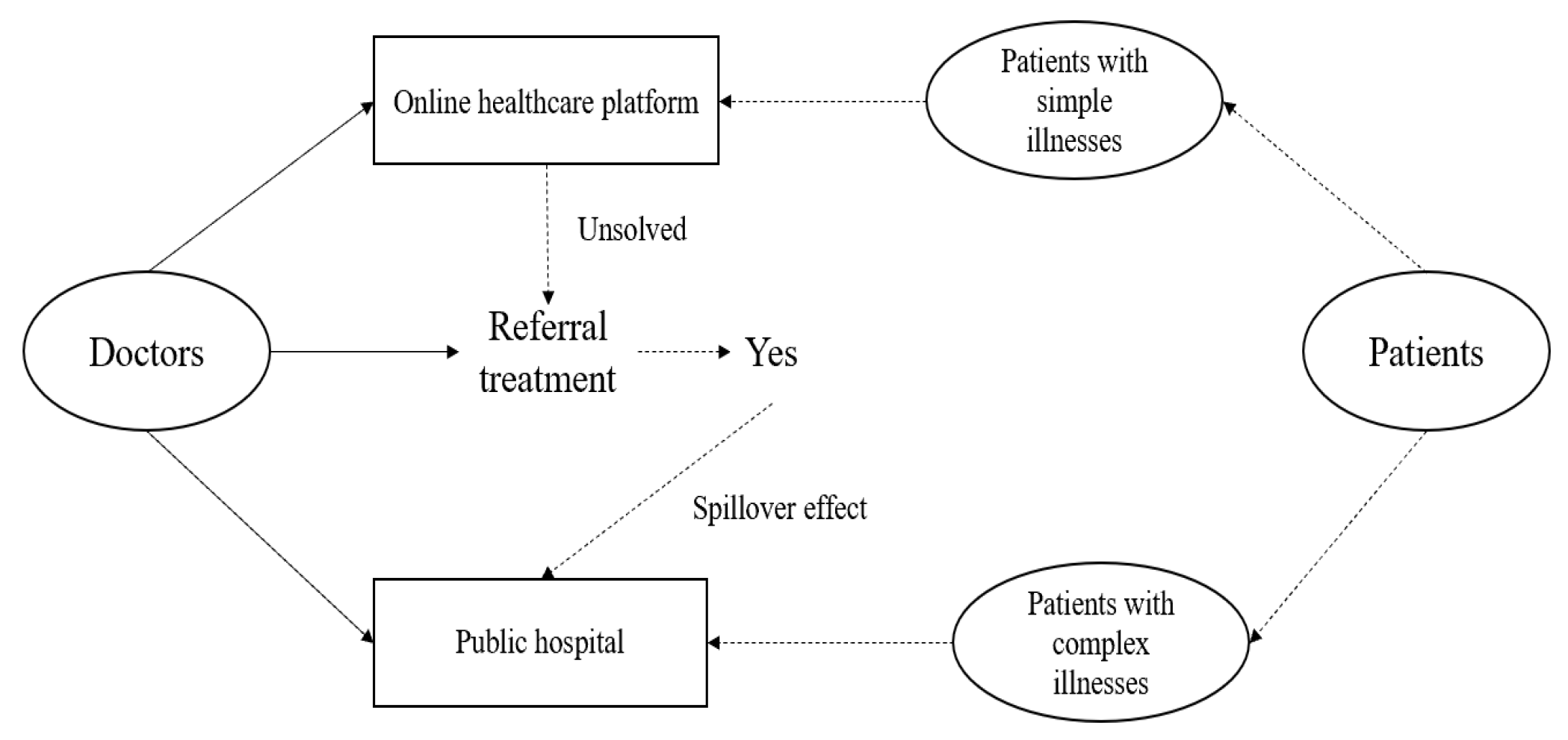
3.3. Common Agency Model of Dual-Channel Healthcare Service with Spillover Effects
3.4. Comparison of Equilibrium Results
4. Numerical Analysis
4.1. The Influence of Online Reputation on Equilibrium Outcomes Without Spillover Effects
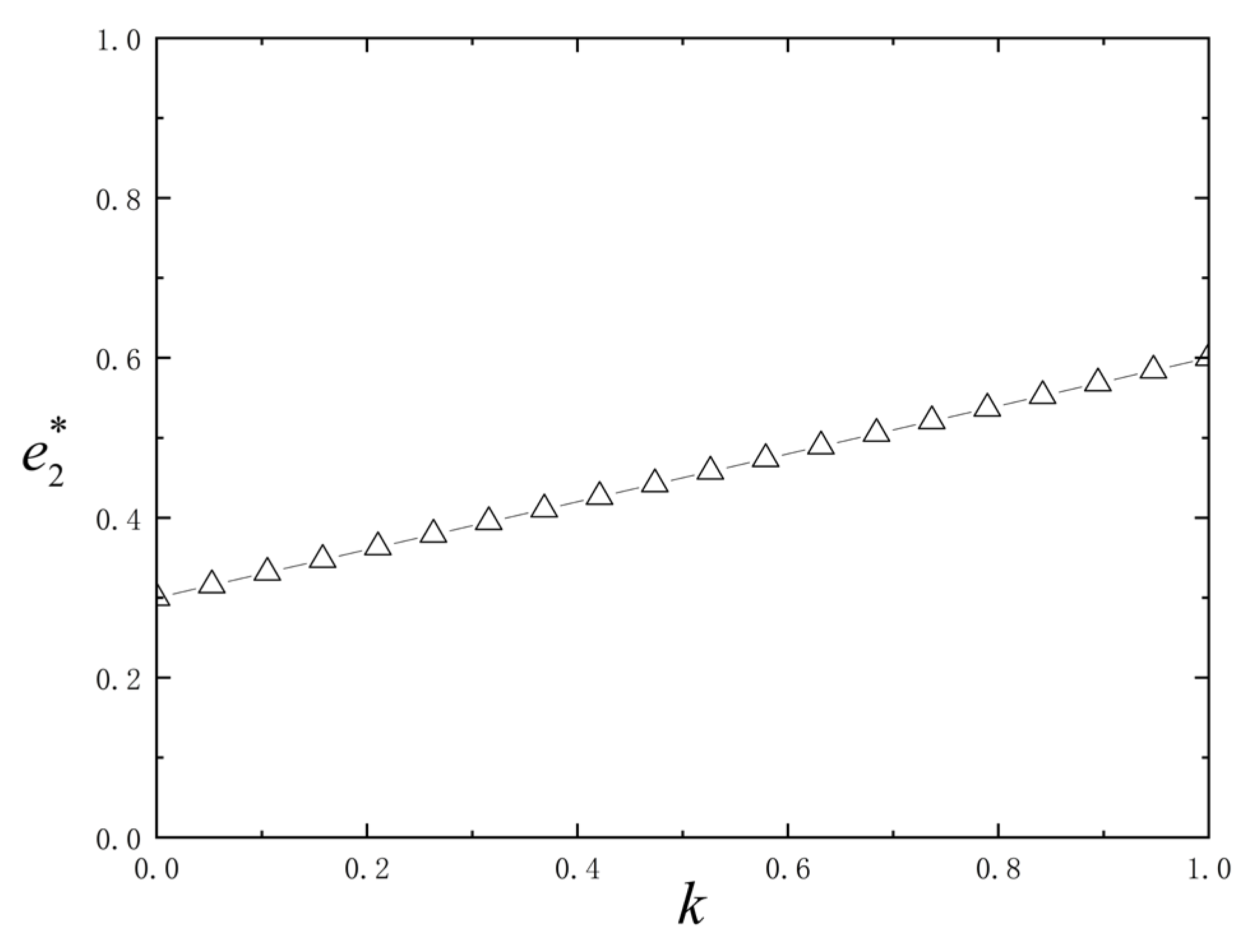
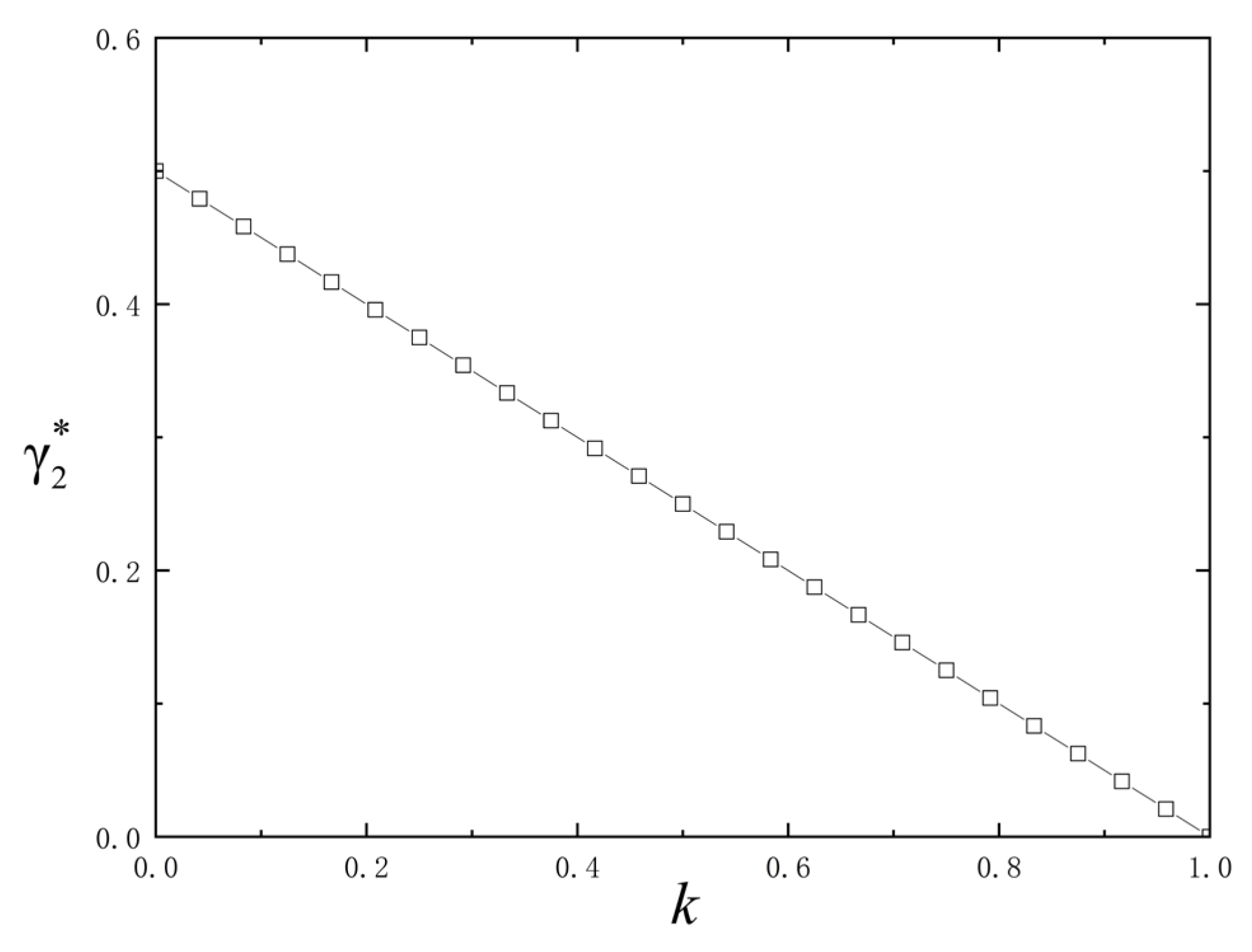
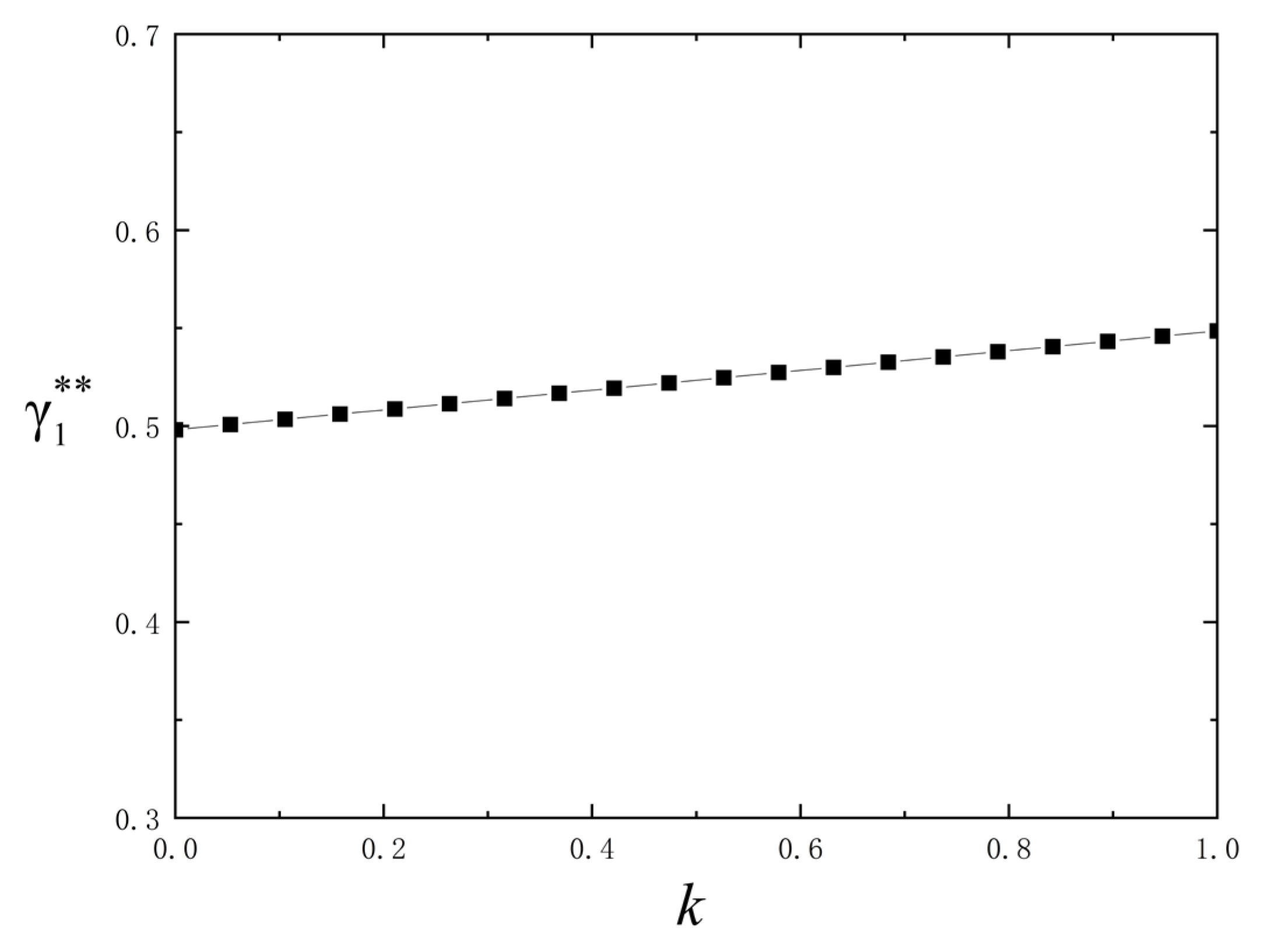
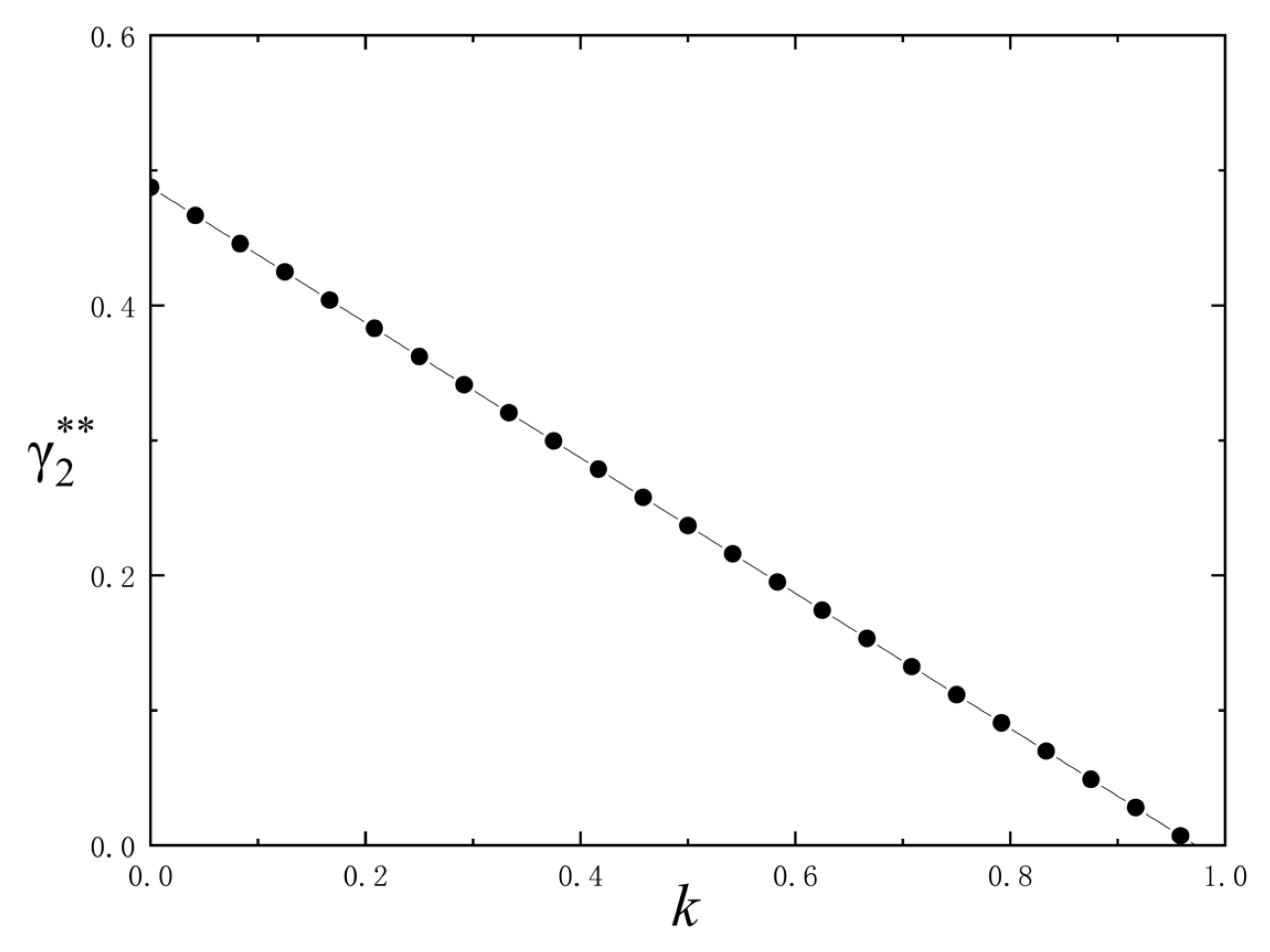
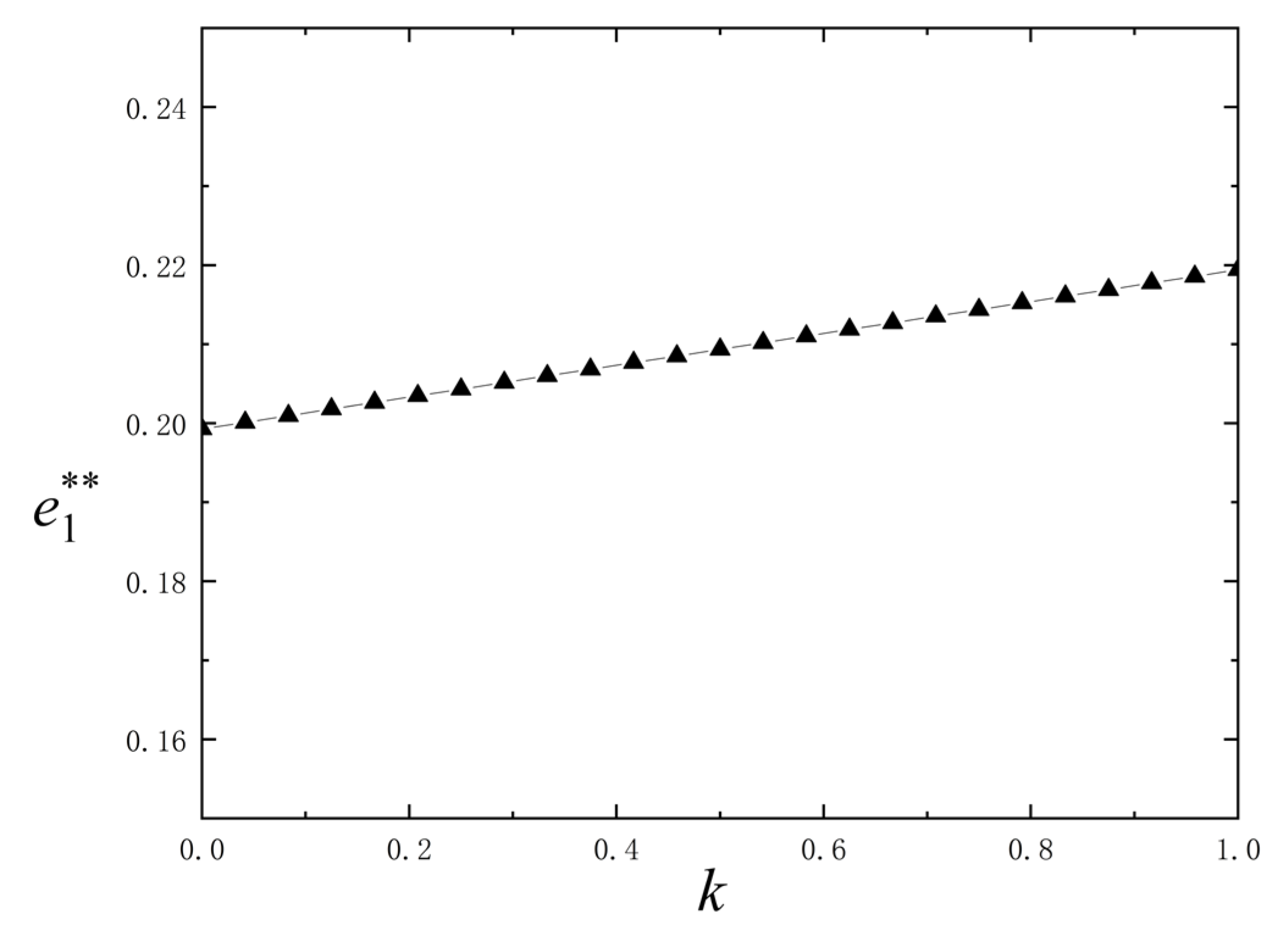
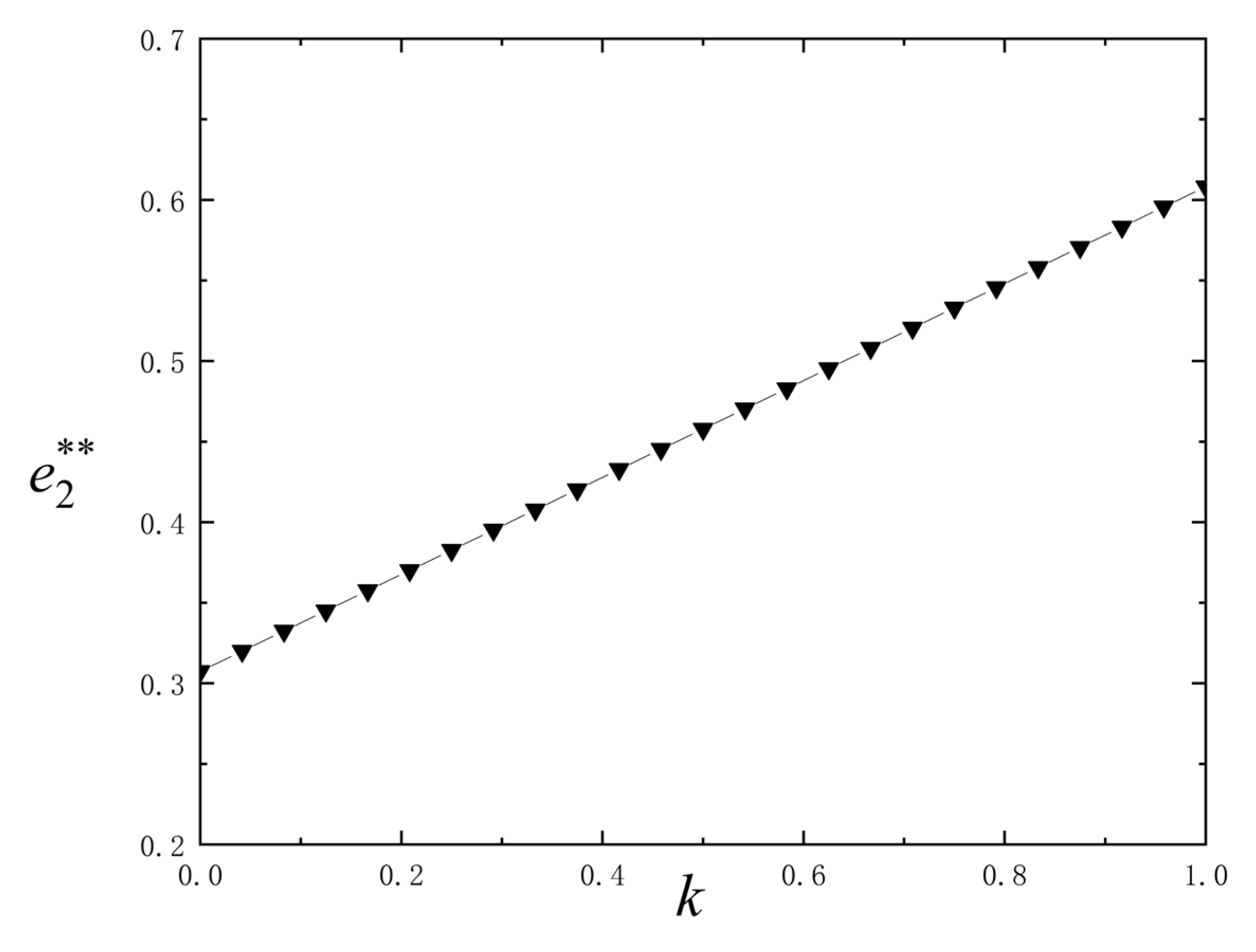
4.2. The Influence of Online Reputation on Several Equilibrium Outcomes with Spillover Effects
5. Managerial Implications
6. Conclusions and Future Research Directions
6.1. Conclusions
- (1)
- In the absence of spillover effects, physicians’ online effort level exhibits a positive correlation with their online reputation, while the economic incentive intensity for online medical services shows a negative correlation with physicians’ online reputation. The positive relationship between online effort and reputation demonstrates a “effort-reputation” positive feedback mechanism in online healthcare services. High-quality services directly enhance patient satisfaction and platform visibility, while accumulated online reputation further motivates physicians to maintain or increase their service engagement. The negative correlation between incentive intensity and online reputation verifies the substitutive role of non-economic factors for traditional economic incentives. Unlike conventional service industries, healthcare is characterized by distinct humanitarian attributes and professional value orientations, where physicians’ decision-making is driven not only by financial rewards but also moderated by non-economic factors such as online reputation and professional fulfillment.
- (2)
- Under spillover effects, as online reputation increases, offline hospitals enhance their incentive intensity for physicians, while online healthcare platforms reduce economic incentives. When significant spillover effects exist, the incentive structure displays clear channel differentiation. Physicians with high online reputation experience “spillover” of their digital influence to offline settings, attracting more patients to seek in-person consultations. Offline hospitals respond by adjusting incentives to balance supply-demand dynamics or recognize physician value. This triggers an “online reputation-offline demand” conversion pathway: high online reputation → conversion of online consultations to offline demand → offline service shortage → adjustment of offline incentives. In the online channel, spillover effects enable high-reputation physicians to attract patients organically, diminishing the marginal utility of economic incentives and prompting platforms to reallocate incentives toward newer physicians. Thus, in dual-channel healthcare environments, spillover effects elevate online reputation from a single-channel incentive factor to a dual-channel determinant.
- (3)
- Compared to scenarios without spillover effects, both offline and online effort levels increase under spillover effects, demonstrating synergistic growth across channels. Typically, heightened offline incentives would prompt physicians to allocate more effort to offline services, while reduced online incentives would discourage online engagement. However, the asymmetric time cost between online lightweight consultations (e.g., 5 min responses) and offline visits (e.g., 30 min appointments) allows physicians to sustain online effort through “fragmented time utilization” even while increasing offline commitments. Consequently, despite the opposing incentive trends described in (2), physicians achieve coordinated effort growth in both channels due to reputation spillovers.
6.2. Limitations and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1
Appendix A.2
Appendix B
Appendix B.1
Appendix B.2
Appendix B.3
Appendix B.4
References
- Cao, X.; Wang, D. The role of online communities in reducing urban-rural health disparities in China. J. Assoc. Inf. Sci. Technol. 2018, 69, 890–899. [Google Scholar] [CrossRef]
- Roettl, J.; Bidmon, S.; Terlutter, R. What predicts patients’ willingness to undergo online treatment and pay for online treatment? Results from a web-based survey to investigate the Changing patient-physician relationship. J. Med. Internet Res. 2016, 18, e32. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.M.; Yan, X.; Shah, S.A.A.; Shah, S.J.; Mamirkulova, G. Exploring the impact of online information signals in leveraging the economic returns of physicians. J. Biomed. Inform. 2019, 98, 103272. [Google Scholar] [CrossRef] [PubMed]
- Goh, J.M.; Gao, G.; Agarwal, R. The creation of social value: Can an online health community reduce rural-urban health disparities? MIS Quart. 2016, 40, 246–263. [Google Scholar] [CrossRef]
- Wang, J.J.; Zhang, X.; Shi, J.J. Hospital dual-channel adoption decisions with telemedicine referral and misdiagnosis. Omega 2023, 119, 102875. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, X.; Lee, P.K.C. Improving the effectiveness of online healthcare platforms: An empirical study with multi-period patient-doctor consultation data. Int. J. Prod. Econ. 2019, 7, 70–80. [Google Scholar] [CrossRef]
- Yang, H.; Du, H.S.; He, W.; Qiao, H. Understanding the motivators affecting doctors’ contributions in online healthcare communities: Professional status as a moderator. Behav. Inf. Technol. 2017, 40, 146–160. [Google Scholar] [CrossRef]
- Wang, L.; Yan, L.; Zhou, T.; Guo, X.; Heim, G.R. Understanding physicians’ online-offline behavior dynamics: An empirical study. Inf. Syst. Res. 2020, 31, 537–555. [Google Scholar] [CrossRef]
- Gao, G.; Greenwood, B.N.; Agarwal, R.; McCullough, J.S. Vocal minority and silent majority: How do online ratings reflect population perceptions of quality. Manag. Inf. Syst. Q. 2015, 39, 565–590. [Google Scholar] [CrossRef]
- Guo, S.; Guo, X.; Fang, Y.; Vogel, D. How doctors gain social and economic returns in online health-care communities: A professional capital perspective. J. Manag. Inf. Syst. 2017, 34, 487–519. [Google Scholar] [CrossRef]
- Zang, Z.; Tan, K.; Yang, X.; Wang, C.; Li, G. Social and economic benefits of doctors on online health-care platforms based on the social capital theory. Nankai Bus. Rev. Int. 2019, 11, 121–140. [Google Scholar] [CrossRef]
- Chang, Y.-W.; Hsu, P.-Y.; Wang, Y.; Chang, P.-Y. Integration of online and offline health services: The role of doctor-patient online interaction. Patient Educ. Couns. 2019, 2, 1905–1910. [Google Scholar] [CrossRef]
- Huang, N.; Yan, Z.; Yin, H. Effects of online-offline service integration on e-healthcare providers: A quasi-natural experiment. Prod. Oper. Manag. 2021, 30, 2359–2378. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. Online written consultation, telephone consultation and offline appointment: An examination of the channel effect in online health communities. Int. J. Med. Inform. 2017, 107, 107–119. [Google Scholar] [CrossRef]
- Chmielewska, M.; Stokwiszewski, J.; Filip, J.; Hermanowski, T. Motivation factors affecting the job attitude of medical doctors and the organizational performance of public hospitals in Warsaw, Poland. BMC Health Serv. Res. 2020, 20, 701. [Google Scholar] [CrossRef]
- Guo, S.; Dang, Y.; Vogel, D.; She, B. The effect of offline medical resource distribution on online physician-patient interaction: Empirical study with online and offline Data. JMIR Form. Res. 2023, 7, e43533. [Google Scholar] [CrossRef]
- Han, X.; Liao, K.; Han, W.; Li, C. The Spillover Effect of Online Medical Consultation Services on Offline Physician–Patient Relationship: Patient Perspective. Health Commun. 2025, 5, 1–16. [Google Scholar] [CrossRef]
- Wang, T.; Sun, Y. Impact of offline experiences on consumer decisions: Balanced vs. unbalanced social exchange in switching to online health services. Digit. Health. 2025, 13, 20552076251326135. [Google Scholar] [CrossRef]
- Wang, M.; Liang, D.; Cao, W.; Fu, Y. Physician recommendation via online and offline social network group decision making with cross-network uncertain trust propagation. Ann. Oper. Res. 2024, 341, 583–619. [Google Scholar] [CrossRef]
- Williams, S.; Barnard, A.; Collis, P.; Sousa, J.C.; Ghimire, S.; Habib, M.; Jelen, T.; Kanniess, F.; Mak, V.; Martins, S. Remote consultations in primary care across low-, middle-and high-income countries: Implications for policy and care delivery. J. Health Serv. Res. Policy 2023, 28, 181–189. [Google Scholar] [CrossRef]
- Wang, W.; Loban, E.; Dionne, E. Public Hospitals in China: Is There a Variation in Patient Experience with Inpatient Care. Int. J. Environ. Res. Public. Health 2019, 16, 193. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, S.; Barnes, S. Understanding congestion in China’s medical market: An incentive structure perspective. Health Policy Plan. 2016, 31, 390–403. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Li, Z.Y.; Zhao, Y. Differentiated health insurance policy for coordinating healthcare referral in hierarchical healthcare systems with an internet diagnosis platform. Socio Econ. Plan. Sci. 2024, 95, 102040. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, Y.; Qiu, Y.; Jin, C. Strategic resource allocation in dual-channel healthcare systems: The role of telemedicine in physician assignment. IEEE Trans. Autom. Sci. Eng. 2025, 22, 13569–13587. [Google Scholar] [CrossRef]
- Jin, H.; Qu, Y. Association between intergenerational support, technology perception and trust, and intention to seek medical care on the internet among Chinese older adults: Cross-sectional questionnaire study. J. Med. Internet Res. 2025, 27, e65065. [Google Scholar] [CrossRef]
- Chen, S.; Lai, K.; Guo, X.; Zhang, X. The influence of digital health technology on the allocation of regional medical resources in China. Health Policy Technol. 2025, 14, 101013. [Google Scholar] [CrossRef]
- Cheng, T.C.; Yip, W. Policies, progress, and prospects for internet telemedicine in China. Health Syst. Reform. 2024, 10, 2389570. [Google Scholar] [CrossRef]
- Chiu, Y.L.; Wang, J.N.; Yu, H.; Hsu, Y.T. Consultation pricing of the online health care service in China: Hierarchical linear regression approach. J. Med. Internet Res. 2021, 23, e29170. [Google Scholar] [CrossRef]
- Dang, Y.; Guo, S.; Song, H.; Li, Y. Setting goal difficulty in monetary incentives to physicians: Evidence from an online health knowledge-sharing platform. Inf. Technol. People. 2024, 37, 605–634. [Google Scholar] [CrossRef]
- Chen, W.; Tang, Y. Optimal investment and pricing strategies of online-offline model for mobile health provider. Electron. Commer. Res. 2023. [Google Scholar] [CrossRef]
- Ye, Q.; Wu, H. Offline to online: The impacts of offline visit experience on online behaviors and service in an Internet hospital. Electron. Mark. 2023, 33, 8. [Google Scholar] [CrossRef]
- Zhao, H.; Cao, X. Who is Facing Higher increased demand after the online-offline channel integration? evidence from public hospitals in China. Risk Manag. Healthc. Policy. 2023, 16, 2635–2648. [Google Scholar] [CrossRef]
- Ross, S.A. The economic theory of agency: The principal’s problem. Am. Econ. Rev. 1973, 63, 134–139. [Google Scholar]
- Bernheim, B.D.; Whinston, M.D. Common marketing agency as a device for facilitating collusion. RAND J. Econ. 1985, 6, 269–281. [Google Scholar] [CrossRef]
- Holmstrom, B.; Milgrom, P. Multitask principal-agent analysis: Incentive contracts asset ownership and job design. J. Law. Econ. Organ. 1991, 7, 24–52. [Google Scholar] [CrossRef]
- Dixit, A.; Grossman, G.M.; Helpman, E. Common agency and coordination: General theory and application to tax policy. J. Polit. Econ. 1997, 105, 752–769. [Google Scholar] [CrossRef]
- Siqueira, K.; Sandler, T.; Cauley, J. Common agency and state-owned enterprise reform. China Econ. Rev. 2009, 20, 208–217. [Google Scholar] [CrossRef]
- Mooney, G.; Ryan, M. Agency in health care: Getting beyond first principles. J. Health Econ. 1993, 12, 125–135. [Google Scholar] [CrossRef]
- Jiang, H.; Pang, Z.; Savin, S. Performance-based contracts for outpatient medical services. Manuf. Serv. Oper. Manag. 2012, 14, 654–669. [Google Scholar] [CrossRef]
- Jacob, J.; Wan, F.; Jin, A. Is telemedicine worth the effort? A study on the impact of effort cost on healthcare platform with heterogeneous preferences. Comput. Ind. Eng. 2024, 188, 109854. [Google Scholar] [CrossRef]
- Alex, B.; González-Chordá, V.M. Error reporting and the performance of nursing management: A game-theoretic study. IMA J. Manag. Math. 2020, 31, 445–468. [Google Scholar] [CrossRef]
- Gouldner, A.W. The norm of reciprocity: A preliminary statement. Am. Sociol. Rev. 1960, 2, 161–178. [Google Scholar] [CrossRef]
- Dur, R.; Roelfsema, H. Social exchange and common agency in organizations. J. Socio-Econ. 2010, 39, 55–63. [Google Scholar] [CrossRef][Green Version]
- Fama, E.F. Agency problems and the theory of the firm. J. Polit. Econ. 1980, 88, 288–307. [Google Scholar] [CrossRef]
- Kreps, D.; Milgrom, P.; Roberts, J.; Wilson, R. Rational cooperation in the finitely repeated prisoners’ dilemma. J. Econ. Theory. 1982, 27, 245–252. [Google Scholar] [CrossRef]
- Abhishek, V.; Jerath, K.; Zhang, Z.J. Agency selling or reselling? Channel structures in electronic retailing. Manag. Sci. 2016, 62, 2259–2280. [Google Scholar] [CrossRef]
- Zhen, X.; Xu, S.; Li, Y.; Shi, D. When and how should a retailer use third-party platform channels? The impact of spillover effects. Eur. J. Oper. Res. 2022, 301, 624–637. [Google Scholar] [CrossRef]
- Yang, W.; Govindan, K.; Zhang, J. Spillover effects of live streaming selling in a dual-channel supply chain. Transp. Res. Part. E 2023, 180, 103298. [Google Scholar] [CrossRef]
- Wu, H.; Deng, Z.; Wang, B.; Wang, H. How online health community participation affects physicians’ performance in hospitals: Empirical evidence from China. Inf. Manag. 2021, 58, 103443. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bi, Y.; Luo, L.; Wu, P. Incentive Mechanism for Online–Offline Dual-Channel Healthcare Services While Considering Spillover Effects. J. Theor. Appl. Electron. Commer. Res. 2025, 20, 210. https://doi.org/10.3390/jtaer20030210
Bi Y, Luo L, Wu P. Incentive Mechanism for Online–Offline Dual-Channel Healthcare Services While Considering Spillover Effects. Journal of Theoretical and Applied Electronic Commerce Research. 2025; 20(3):210. https://doi.org/10.3390/jtaer20030210
Chicago/Turabian StyleBi, Yanlin, Li Luo, and Pengkun Wu. 2025. "Incentive Mechanism for Online–Offline Dual-Channel Healthcare Services While Considering Spillover Effects" Journal of Theoretical and Applied Electronic Commerce Research 20, no. 3: 210. https://doi.org/10.3390/jtaer20030210
APA StyleBi, Y., Luo, L., & Wu, P. (2025). Incentive Mechanism for Online–Offline Dual-Channel Healthcare Services While Considering Spillover Effects. Journal of Theoretical and Applied Electronic Commerce Research, 20(3), 210. https://doi.org/10.3390/jtaer20030210





