Abstract
This study investigates the spillover effects of physicians’ prosocial behavior, specifically knowledge sharing, on the paid consultations of other physicians within the same specialty and offline hospital. Using data from an online healthcare platform, we apply propensity score matching to explore how the sharing of medical knowledge by physicians influences the consultation outcomes of their colleagues. The results reveal significant positive spillover effects, indicating that prosocial behavior benefits other physicians within the same specialty and healthcare institution, thereby enhancing collaboration within the healthcare ecosystem. The spillover effect is stronger within the same offline hospital’s physicians on the online healthcare platform, suggesting that knowledge sharing has a more localized impact within the same healthcare institution. Furthermore, the study examines heterogeneity across both physician-level characteristics (e.g., popularity, title, price, gender) and contextual factors (e.g., specialty type, hospital level, wait time, regional GDP). The findings show that the magnitude and direction of spillover effects differ by subgroup, shaped by professional visibility, authority, and organizational structure. These insights contribute to the understanding of how prosocial behavior can foster collaboration and benefit healthcare networks beyond individual physicians, offering practical implications for healthcare platforms, administrators, and policymakers.
1. Introduction
Online healthcare platforms (OHPs) have developed rapidly in recent years. They pool medical resources from different hospitals at various levels, offering patients the opportunity to access high-level doctors nationwide [1]. The patients can easily consult their desired doctors in terms of a series of paid services, including text-based, video, and voice consultations [2]. Normally, the consultation fee ranges between 10 and 300 yuan per consultation. Aside from the paid services, free services that OHPs provide include knowledge sharing [3]. Such services enable patients to research before deciding on their health. Usually, a patient would go through a doctor’s profile before visiting them; this includes the expertise of such doctors, the ranking of the hospital in that particular field of medicine, and the doctor’s specialty [4].
Knowledge sharing has been one of the most prominent services featured on physicians’ profiles and has also been widely discussed in the literature on OHPs. It is typically offered by physicians, nursing staff, and various other healthcare practitioners who are dedicated to the distribution of medical information [3]. The objective is to establish a virtual community that enables patients to gain a clearer comprehension of their health issues, simultaneously fostering reciprocal learning among healthcare professionals [5]. The exchange of knowledge not only bolsters patient trust but also facilitates informed decision-making concerning healthcare among patients [6]. This boosts engagement on the platform and raises the number of consultations [7]. The literature has already extensively discussed the importance of knowledge sharing in attracting patients and impacting their consulting behavior.
Knowledge sharing is mostly treated as a form of prosocial behavior [8,9]. Prosocial behavior involves both altruistic and egoistic motivations [10]. Altruism refers to acts that mostly benefit other people, while egoism involves acts that benefit the actor and other people [11]. Prior research indicates that knowledge sharing between doctors and patients fosters mutual trust, helps build credibility, and raises the professional profile. All these positive outcomes eventually attract more patients and bring improved financial returns [3,12]. On the other hand, pros for patients in an altruistic sense encompass a better understanding of one’s health condition through medical knowledge gained, empowerment to make informed choices, and lessened asymmetry of information, which prevails between the caregiver and the patients [13]. While previous research has largely focused on the altruistic dimensions of knowledge sharing with patients, there has been a relative neglect of the ways in which physicians’ prosocial behaviors may impact their colleagues within the same medical specialty or institution. This paper tries to fill this gap by bringing to the forefront the altruistic aspects of knowledge sharing and exploring its subsequent effects on other physicians.
Previous spillover effects studies have mainly addressed the domain of consumer behavior, where experiences with one product influenced decisions related to other products within the same brand [14]. Spillover effects, when it comes to competitors, typically explored in consumer behavior, have been mainly focused on the negative impacts, such as how a crisis can affect the financial value of competitors [15,16]. However, in the case of healthcare, spillover effects can extend beyond these negative impacts, potentially fostering a more cooperative environment. In the context of OHPs, the spillover effect goes further than the individual consultations of the doctor; it refers to the potential for one doctor’s knowledge sharing to spill over into the consultations of other doctors within the same specialty or hospital. This phenomenon has not been fully explored in OHPs, especially in prosocial behavior. By investigating the spillover effects of knowledge sharing, this paper extends the scope of prosocial altruism from individual physicians to their colleagues in the broader healthcare ecosystem. Given this background, the current study attempts to answer the following fundamental research questions:
Q1: Does a doctor’s knowledge sharing increase the number of paid consultations for other doctors in the same specialty on OHP?
Q2: Does a doctor’s knowledge sharing increase the number of paid consultations for other doctors in the same offline hospital?
In addition, this study examines how the spillover effects of physicians’ knowledge sharing are conditioned by a range of individual-level and contextual factors. At the individual level, physician characteristics such as online popularity, consultation price, professional title, and gender may influence how patients perceive and process information, thereby moderating the extent to which knowledge sharing leads to spillover effects. At the contextual level, institutional and environmental attributes—including specialty type, hospital level, consultation responsiveness (as proxied by wait time), and the economic development level of the hospital’s province—may also shape the diffusion of trust and information. These dimensions reflect both the personal traits of the physician and the broader structural conditions under which medical knowledge is shared and interpreted.
We therefore explore the following research questions:
Q3: How are these spillover effects moderated by physician-level characteristics, such as popularity, consultation price, professional title, and gender?
Q4: How do contextual and institutional factors—including specialty type, hospital level, consultation responsiveness, and the regional economic environment—condition the magnitude of the spillover effects?
This paper empirically investigates the spillover effects of physicians’ prosocial behavior, specifically knowledge sharing, on online healthcare platforms. Our findings indicate that, besides helping patients, such prosocial behavior exerts a strong influence on the paid consultations of other physicians within the same specialty and offline hospital. More importantly, the magnitude of these spillover effects varies systematically across both physician-level characteristics and contextual factors. Stronger spillover effects are observed among physicians in tertiary hospitals and in specialties such as obstetrics and gynecology, as well as among those with distinct individual traits such as high reputation or junior title—reflecting the complex interplay between organizational position, individual visibility, and contextual receptiveness. These findings highlight the importance of knowledge sharing as a prosocial behavior that can enhance cooperation and mutual learning among healthcare professionals, leading to improved patient outcomes and increased platform engagement.
This study contributes to theory in several ways. First, it extends our understanding of prosocial behavior by examining its indirect effects on the healthcare ecosystem. While previous studies have emphasized the direct benefits of prosocial behavior for either patients or individual physicians, this research highlights its role in creating a reciprocal benefit for other physicians in the same network and thus fills an important gap in the current literature. Second, the study advances the theoretical understanding of spillover effect heterogeneity by jointly analyzing how both physician-level characteristics (e.g., popularity, price, title) and institutional factors (e.g., specialty, hospital level, responsiveness, regional GDP) moderate the strength and direction of these effects. The findings highlight the contextual features of prosocial behavior, which may have very different effects depending on both individual and situational factors. Third, the study contributes to understanding the interdependence between digital and physical healthcare systems, showing that online altruistic behavior can generate tangible benefits within offline hospital environments through increased trust diffusion and brand alignment.
2. Literature Review
2.1. Online Healthcare Platform and Knowledge Sharing
OHPs act as “medical associations”, connecting major hospitals and grassroots medical institutions [17]. Through these platforms, patients gain the opportunity to consult with doctors nationwide from the comfort of their homes [18]. The platforms aggregate doctors from diverse healthcare institutions nationwide, offering a variety of services from top specialists to doctors at different levels and hospitals [19]. Paid services include text-based consultations, video consultations, and voice consultations, with prices typically ranging from 10 to 300 yuan per consultation. Additionally, they provide complimentary services such as knowledge sharing [20]. The diverse array of services attracts an increasing number of patients to utilize OHPs [21,22].
Knowledge sharing is a vital service for doctors to maintain a competitive edge [5]. Beyond merely enhancing doctors’ reputations and increasing demand for their services, knowledge sharing also plays a pivotal role in providing patients with professional disease-related education, thereby benefiting their understanding and well-being [23,24,25]. Before consulting a doctor, patients often visit the relevant doctors’ pages, where they may peruse the complementarily offered knowledge sharing on their respective conditions, offered voluntarily by doctors [9].
Previous literature has widely investigated knowledge sharing in relation to digital health platforms. The benefits and costs framework based on social exchange theory has been used to explore the motivations for knowledge sharing [26]. It has also been found that knowledge sharing by doctors on digital health platforms can be positively influenced by the monetary rewards received from consultations [27]. Furthermore, the act of information sharing has been highlighted to have a significant effect on patient engagement and health outcomes [9]. It is also instrumental in attracting patients to utilize online health services, thus increasing the overall effectiveness of these platforms [28,29].
From the perspective of physicians, therefore, the impact of knowledge sharing on patients’ decisions about consultations directly relates to their income. It is the relational aspect that brings to light the pragmatic effects of sharing knowledge but also resonates with the more general concept of prosocial behavior, which embraces both altruistic and self-serving motivations. Building on this, the next section deals with knowledge sharing as a form of prosocial behavior on OHPs.
2.2. Physicians’ Prosocial Behavior
Prosocial behavior, which refers to actions taken with the altruistic motivation of helping others, spans a broad range of expressions, including helping strangers, engaging in volunteer activities, and making personal donations [30,31,32,33]. Research into prosocial behavior has tended to divide its motivations into two broad categories [11]. The key difference lies in whether the actor derives personal benefits, while the common feature shared by these categories is their essentially altruistic nature [30,31]. The initial classification characterizes prosocial behavior as entirely altruistic, whereby actions are exclusively motivated by the desire to assist others, devoid of any anticipation of personal advantage [34,35]. Conversely, the second classification adopts a more intricate viewpoint, wherein altruistic behaviors exist alongside self-serving intentions. From this perspective, individuals seek a mutually advantageous outcome, facilitating benefits for others while concurrently promoting their own interests [34,36,37,38]. The duality of motives is of vital importance in the context of OHPs.
In the present study, we adopt the latter perspective, according to which prosocial behavior is a construct that comprises both egoistic and altruistic motivations. In the OHP context, altruism has typically been related to the benefits that patients receive. For instance, prosocial behavior by doctors often enhances patients’ understanding of their illness, strengthens their medical knowledge, and empowers them to make informed health-related choices. On the other hand, egoism refers to the personal benefits that physicians can derive from such actions, including increased reputation, greater patient trust, and, ultimately, higher consultation revenue. These altruistic and egoistic motivations often co-exist and drive physicians to perform prosocial behaviors on OHPs [39].
The impact of a doctor’s prosocial behavior on their own consultations has been widely studied. Prior research has shown that doctors’ prosocial behavior can increase patient trust, improve the doctor–patient relationship, and ultimately lead to more paid consultations for the physician sharing knowledge [3,26,40]. While altruism appears as a multifaceted construct in prosocial behavior, most studies under the OHP framework have focused primarily on the direct benefits of physicians’ prosocial behavior for their patients [3,41].
Thus, a gap exists in understanding the consequences of physicians’ prosocial behavior, viewed as altruistic behavior, for other physicians within the same healthcare network. This gap is addressed in the present study, which investigates the altruistic dimensions of prosocial behavior in OHPs, focusing on the impact of physicians’ prosocial behavior on colleagues. In so doing, we extend the understanding of prosocial behavior in digital healthcare platforms to include its effects beyond patients and include other healthcare providers within the network.
2.3. Spillover Effect
The spillover effect refers to the influence of one entity or action on related attributes, extending beyond its immediate impact by altering beliefs or behaviors about attributes not directly addressed, often through inferred associations [42]. The concept has been widely applied in many areas, including consumer behavior and organizational studies, in which the effects of one entity affect others in direct and indirect ways [43,44]. As an example, empirical research has shown that happiness can spill over to online prosocial behavior, hence influencing people’s behavior in a broader social network [45]. The extant literature on spillover effects has so far concentrated on two major fields.
The first one, intra-brand spillover effects, examines how the behavior/attributes of one product influence consumer behavior about other products under the same brand [46]. For instance, a positive experience with a given product can enhance perceptions of other products from the same brand, thereby increasing the brand’s overall equity [47,48]. The second area, inter-brand spillover effects, examines the impact that the behaviors of a specific product or brand have on its competitors [49]. For example, a creative new product development or marketing campaign may siphon off customers from competing products [50,51]. Nevertheless, most of the literature on inter-brand spillover effects is more focused on the negative implications, mainly studying how a brand crisis negatively impacts the financial market values of non-impacted competitors [52,53]. However, research into spillover effects among rivals that help in creating a collaborative environment is relatively limited.
The existing gap in academic research is particularly pertinent when looking at online healthcare, where the spillover effects may take on a more collaborative nature. Specifically, within the context of OHPs, the prosocial actions exhibited by physicians, such as knowledge sharing, may lead to the creation of a cooperative ecosystem that serves to benefit not only the individual physicians but also the broader platform environment [54,55]. Unlike the competitive dynamics typically observed in traditional consumer markets, knowledge sharing within OHPs may create spillover effects that go beyond individual gains and affect not only the physicians’ practices but also those of other physicians within the same platform [56]. By examining the evolution of these dynamics, the current study expands the research canvas to include both digital and traditional healthcare systems, emphasizing the interrelated nature of healthcare ecosystems and the potential for knowledge diffusion to create synergistic benefits in both realms.
3. Research Hypothesis
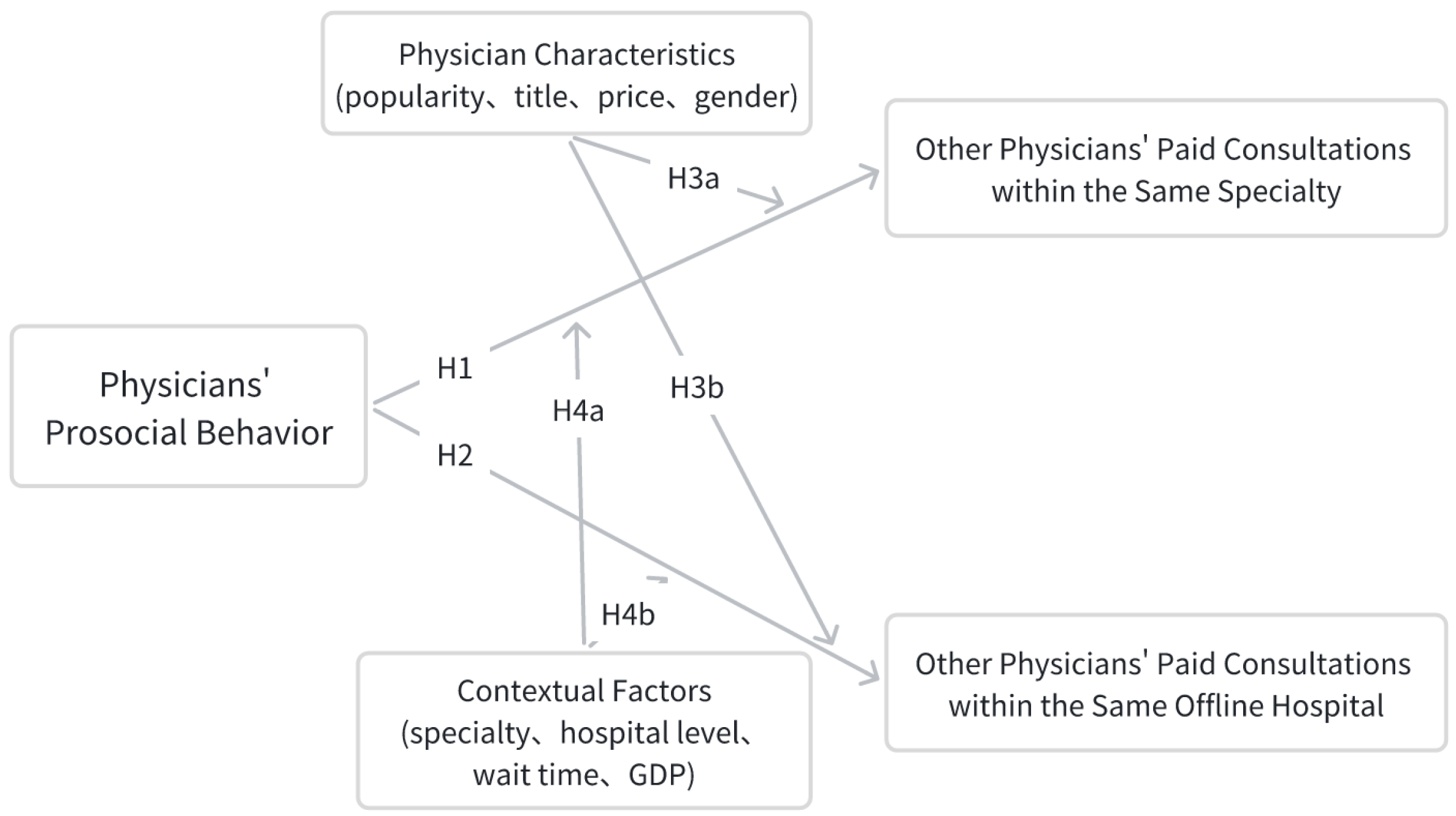
This study examines the impact of physicians’ altruistic behavior, specifically knowledge sharing, on the paid consultations of other physicians in the same specialty group or offline medical facility on online health platforms (OHPs). We focus on how physicians’ prosocial behaviors, such as sharing medical knowledge, influence the paid consultations of other physicians in the same specialties or medical facilities. Furthermore, the extent and direction of these spillover effects may not be uniform. Drawing from the literature on digital reputation, healthcare decision-making, and institutional dynamics, we propose that both individual-level characteristics (e.g., popularity, price, professional title, and gender) and contextual factors (e.g., specialty type, hospital tier, consultation responsiveness, and regional socioeconomic environment) moderate the strength of these effects. Figure 1 presents the conceptual framework guiding our hypotheses.
Figure 1.
Conceptual Structure.
3.1. Impact of a Physician’s Prosocial Behavior on Paid Consultations Within the Same Specialty
Previous studies have shown that physicians’ prosocial behavior, such as sharing medical knowledge, results in more patient trust, which consequently increases consultations for the physician exhibiting this behavior. However, a physician’s prosocial behavior may also have broader effects. In the case of OHPs, prosocial behavior may not only affect the individual physician but also spill over to affect consultations of other physicians in the same specialty. This occurs because those who come into contact with the collective knowledge of a certain doctor may develop a higher level of trust in the specialty in general, leading them to seek the consults of other doctors within the same field.
H1:
Physicians’ prosocial behavior increases the number of paid consultations for other physicians within the same specialty group on OHP.
3.2. Impact of a Physician’s Prosocial Behavior on Paid Consultations Within the Same Offline Hospital
Similarly, knowledge sharing by physicians within an OHP can spill over to affect the consultations of physicians at the same offline hospital. Engaging a physician’s shared knowledge may make the patients more trustful of the whole healthcare institution so as to make them visit other physicians also in the hospital for consultations. This spillover effect occurs as the patients’ perceptions of the hospital’s competence are influenced by the information given by the individual physicians, thus increasing consultations for other physicians within the same institution.
H2:
Physicians’ prosocial behavior leads to increased paid consultations for other physicians within the same offline hospital on OHP.
3.3. Moderating Effect of Physician Characteristics
Individual physician attributes may condition how knowledge-sharing behavior produces spillover effects. Characteristics such as online popularity, consultation price, professional title, and gender influence patient perceptions, information processing, and decision-making. These characteristics can either amplify the reach of knowledge-based trust, constrain its diffusion, or alter the underlying mechanisms through which trust is transferred. Accordingly, the spillover effects of prosocial behavior may vary across physicians within the same specialty group or within the same offline hospital, depending on these individual-level factors.
H3a:
The spillover effect of physicians’ prosocial behavior within the same specialty group is moderated by physician-level characteristics (i.e., popularity, price, title, and gender).
H3b:
The spillover effect of physicians’ prosocial behavior within the same offline hospital is moderated by physician-level characteristics (i.e., popularity, price, title, and gender).
3.4. Moderating Effect of Medical Context and Environment
Beyond individual attributes, contextual and institutional factors such as specialty type, hospital level, consultation responsiveness (proxied by wait time), and regional economic environment may influence how prosocial behavior spreads. These factors shape the structure of medical collaboration, visibility of information, patient expectations, and the perceived credibility of medical collectives.
H4a:
The spillover effect of physicians’ prosocial behavior within the same specialty group is moderated by medical context (i.e., specialty type, hospital level, consultation responsiveness, and regional GDP).
H4b:
The spillover effect of physicians’ prosocial behavior within the same offline hospital is moderated by medical context (i.e., specialty type, hospital level, consultation responsiveness, and regional GDP).
Based on these hypotheses, the present study aims to extend our understanding of the spillover effects of prosocial behavior in the context of OHPs. Specifically, we investigate not only whether physicians’ prosocial behavior generates spillover effects across organizational boundaries—within the same specialty and offline hospital—but also how individual attributes and contextual factors condition the magnitude and direction of these effects. This layered hypothesis framework builds upon existing literature while reflecting the multifaceted heterogeneity inherent in platform-mediated medical interactions.
4. Data and Model
4.1. Data
This study relies on data made available by Haodf, one of the leading platforms in China. The dataset comprises 64,156 physicians who were active on the platform in 2020, spanning a wide range of specialties and offline hospital affiliations. The data are derived from physicians’ digital profiles and patient-facing service records, including structured fields collected by the platform and user interaction metadata.
The dataset captures key physician characteristics—such as professional title, hospital level, gender, and responsiveness—as well as platform-based service attributes, including consultation price diversity, product diversity, and popularity. The core treatment variable is a binary indicator of whether a physician engaged in knowledge sharing, defined by exceeding a threshold number of medical articles posted on their profile. To measure peer effects, the outcome variables are constructed as leave-one-out means of paid consultations among peer groups defined by the same specialty, offline hospital, or R_department, respectively.
Additionally, a set of contextual and lagged control variables were constructed to mitigate confounding, including log-transformed provincial health facility capacity (ln_healthfaci_hosprov) and lagged mean and variance of popularity, response time, and service diversity within organizational peer groups. The full list of variable definitions used in the analysis is provided in Table 1.

Table 1.
Definition of variables for main model.
4.2. Model
We apply propensity score matching (PSM) to estimate the causal effects of physicians’ prosocial behavior on the paid consultations of other physicians in the same specialty group or offline hospital. PSM helps to mitigate selection bias by matching treated and control groups based on observable characteristics, ensuring a more accurate comparison.
In this study, we propose two models to test the spillover effects of knowledge sharing among physicians.
Model 1 investigates how a physician’s knowledge-sharing influences the number of paid consultations of other physicians within the same specialty group. This model controls for a range of physician-level and institutional factors, including popularity, professional title, gender, hospital grade, service responsiveness, price and product diversity, regional healthcare resources, and specialty.
dm_paidᵢ = α + β1·d_knowledgeᵢ + β2·gdp_hospitalprovinceᵢ + β3·titleᵢ + β4·genderᵢ + β5·waittimeᵢ + β6·popularity_lm_wᵢ + β7·popularity_lv_wᵢ + β8·responsetimely_lm_wᵢ + β9·responsetimely_lv_wᵢ + β10·pricediversity_lm_wᵢ + β₁₁·pricediversity_lv_wᵢ + β12·ln_healthfaci_hosprov_lm_wᵢ + β13·ln_healthfaci_hosprov_lv_wᵢ + β14·productdiversity_lm_wᵢ + β15·productdiversity_lv_wᵢ + εᵢ
Model 2 extends this analysis by examining how knowledge sharing affects the paid consultations of other physicians within the same offline hospital. Similar to Model 1, it includes the same set of control variables.
hm_paidᵢ = α + β₁·d_knowledgeᵢ + β₂·gdp_hospitalprovinceᵢ + β₃·titleᵢ + β₄·genderᵢ + β₅·waittimeᵢ + β₆·popularity_lm_wᵢ + β₇·popularity_lv_wᵢ + β₈·responsetimely_lm_wᵢ + β₉·responsetimely_lv_wᵢ + β₁₀·pricediversity_lm_wᵢ + β₁₁·pricediversity_lv_wᵢ + β₁₂·ln_healthfaci_hosprov_lm_wᵢ + β₁₃·ln_healthfaci_hosprov_lv_wᵢ + β₁₄·productdiversity_lm_wᵢ + β₁₅·productdiversity_lv_wᵢ + εᵢ
By utilizing PSM, both models aim to provide a clearer understanding of how prosocial behavior, particularly knowledge sharing, generates spillover effects across healthcare settings.
5. Results
5.1. Analysis
In this study, we apply propensity score matching (PSM) to estimate the causal effects of physicians’ prosocial behavior, specifically knowledge sharing, on the paid consultations of other physicians. PSM helps mitigate selection bias by matching treated and control groups based on observable characteristics, ensuring more accurate comparisons.
Spillover Effects Within Same Specialty Group and Same Offline Hospital (H1 and H2)
The analysis of spillover effects from knowledge sharing on paid consultations within the same specialty group and within the same offline hospital’s physicians on the online healthcare platform (OHP) is presented in Table 2. We focus primarily on the matched sample results, as the unmatched samples may be confounded by unobserved factors, making them unsuitable for causal inference.

Table 2.
Spillover effects of knowledge sharing on paid consultations within same specialty group and offline hospital (Average Treatment Effect on the Treated).
For the dependent variable dm_paid, the results show a positive and statistically significant spillover effect after matching. For the treated group, the Average Treatment Effect on the Treated (ATT) is 923.038, while the control group has 897.378, with a difference of 25.661 (t-stat = 6.040, ***), indicating a positive and statistically significant spillover effect. This finding supports Hypothesis 1, suggesting that knowledge sharing by physicians positively influences paid consultations within the same specialty group.
Similarly, for the dependent variable hm_paid, the matched sample results show a significant spillover effect. For the treated group, the ATT is 991.977, compared with 933.687 in the control group, with a difference of 58.291 (t-stat = 9.160, ***), demonstrating a positive and statistically significant spillover effect on paid consultations within the same offline hospital’s physicians on OHP. This supports Hypothesis 2, confirming that knowledge sharing by physicians extends its effect to consultations among the same offline hospital physicians on OHP.
While the spillover effects observed in the unmatched sample are significant, they are not suitable for causal interpretation due to the potential for confounding factors. Therefore, the findings from the matched samples provide more reliable evidence, such as robustness checks, subgroup heterogeneity analysis, sensitivity tests, and placebo tests, for the hypotheses tested.
The spillover effect for hospital-level consultations (hm_paid, ATT = 58.291) is significantly larger than that for department-level consultations (dm_paid, ATT = 25.661), indicating that physicians’ knowledge sharing has a broader and more pronounced influence on consultations among doctors within the same offline hospital compared with those within the same specialty group. This difference reflects the enhanced scope of influence that arises from hospital-level resource integration and brand synergy, which enable platform complementarity and amplify the diffusion of trust and knowledge across the entire institutional network. Empirical evidence shows that hospitals with strong resource integration capabilities achieve substantially stronger spillover effects than those relying on isolated departmental efforts and that hospital branding further consolidates patient trust and increases the visibility of physicians across departments within the same institution [56].
5.2. Heterogeneity Tests
In this section, we examine the heterogeneity of the spillover effects of physicians’ prosocial behavior across a range of physician-level and contextual-level dimensions. These include doctor popularity, consultation price, professional title, gender, medical specialty, hospital level, consultation wait time, and regional economic development. Table 3 summarizes the categorical variables used in the heterogeneity analysis, including their label names as shown in the results table and corresponding definitions or coding schemes.

Table 3.
Variable descriptions and coding for heterogeneity analysis.
In both Section 5.2.1 and Section 5.2.2, we report the Average Treatment Effect on the Treated (ATT), which represents the average difference in paid consultation outcomes between physicians who engaged in knowledge sharing (treated group) and those who did not (control group) after propensity score matching. This measure isolates the effect of knowledge sharing by comparing each treated physician to statistically similar control physicians across subgroups. A positive and significant ATT indicates that knowledge sharing has a spillover effect on the matched peers’ consultation volumes.
5.2.1. Spillover Effects Within the Same Department (dm_paid)
This subsection provides empirical tests for Hypotheses H3a and H4a, which explore how physician-level attributes and contextual medical environments moderate the spillover effects of prosocial behavior within the same specialty group. To investigate the heterogeneous spillover effects of knowledge sharing at the specialty level, we constructed subgroup variables based on the dimensions outlined in Section 5.2 and grounded in prior literature on peer effects, digital health platforms, and healthcare organizational behavior (see Table 4).

Table 4.
Heterogeneous treatment effects of knowledge sharing on dm_paid (2020, matched ATT results).
The results for Doctor Popularity show consistently significant and positive spillover effects across all groups (ATT = 28.71, 27.11, and 26.41 for low, medium, and high popularity, respectively; all t-values > 3, p < 0.01). Low-popularity physicians generated the strongest effect, indicating that their high-frequency knowledge-sharing helps reduce informational gaps and enhances collective trust in the department [21]. Medium-popularity physicians exhibited slightly weaker effects, likely due to the absence of both reputational authority and algorithmic visibility—an issue known as the “moderate competitiveness trap” [57]. For high-popularity physicians, knowledge sharing tends to reinforce their personal brand rather than facilitate peer trust diffusion, producing a “halo effect” that limits spillover to colleagues [27].
In terms of consultation price, physicians in the mid-price group displayed the highest spillover effect (ATT = 27.19, t = 2.00, **), followed by the lowest-price group (ATT = 25.08, t = 5.14, ***), while high-price segments showed no significant impact. This pattern suggests that within the same specialty, knowledge sharing by low-price physicians may reduce patients’ decision-making risks, encouraging them to seek consultation from other doctors in the department. Mid-price physicians also benefit from informational spillover, although the significance is marginal. Prior research indicates that price-sensitive patients rely more on collective information to assess physician quality, with knowledge sharing expanding trust toward the entire department [58]. By contrast, patients in high-price groups tend to have concentrated preferences and loyalty, making them less susceptible to trust diffusion via knowledge sharing [27,40].
For the physician title, a clear gradient is observed. Junior physicians (Title = 1) exhibited the strongest spillover effect (ATT = 43.23, t = 1.96, **), followed by attending physicians (Title = 2, ATT = 39.74, t = 4.54, ***), associate chief physicians (Title = 3, ATT = 26.43, t = 3.72, ***), and chief physicians (Title = 4, ATT = 19.41, t = 2.83, ***). Although all groups show statistically significant positive effects, there is a general decline in ATT magnitude with higher professional ranks. This suggests that knowledge sharing by junior physicians plays an important role in reducing patient selection barriers [21]. Mid-level physicians often participate in collaborative activities such as case discussions and standard-setting, making their shared knowledge more actionable for peers [19]. In contrast, chief physicians may inadvertently centralize patient trust around themselves due to their authority, reducing the diffusion of trust within the department [27].
Regarding gender, both male (ATT = 23.62, t = 4.67, ***) and female (ATT = 21.33, t = 2.96, ***) physicians demonstrated significant positive spillover effects, with relatively small differences. This suggests that gender does not play a substantial role in moderating spillover effects within the same specialty.
The heterogeneity analysis across specialty types focused on the top five departments by consultation volume: obstetrics and gynecology, pediatrics, traditional Chinese medicine, internal medicine, and surgery. The surgical department was excluded from the analysis due to complete separation issues in the dataset, which prevented convergence of the propensity score matching (PSM) model. Following statistical best practices, departments with severe model violations—such as non-convergence caused by complete separation—were excluded to ensure validity. The analysis of specialty type reveals that pediatrics (ATT = 29.52, t = 1.85, *), traditional Chinese medicine (ATT = 20.42, t = 2.11, **), and obstetrics and gynecology (ATT = 17.01, t = 2.32 **) showed stronger spillover effects than Internal Medicine (ATT = 11.24, t = 2.8, ***). The high effect in pediatrics may stem from the fact that parents tend to rely on the department’s collective expertise rather than on individual physician reputation, and knowledge sharing helps reduce informational asymmetry [40]. In traditional Chinese medicine, the long-term nature of chronic disease management encourages trust accumulation through continuous sharing [23]. For obstetrics and gynecology, knowledge sharing improves transparency and reduces patient concerns in high-sensitivity decisions [59]. Conversely, internal medicine covers a wide range of conditions, and information overload may dilute collective trust diffusion [23].
As for the hospital level, only Level 3 hospitals showed statistically significant spillover effects (ATT = 27.47, t = 6.28, ***), indicating that large, institutionalized hospitals have more structured pathways for horizontal knowledge diffusion. Patients in tertiary hospitals tend to trust the department as a whole, especially when lower-ranking doctors fill information gaps through knowledge sharing [21].
For wait time, which inversely reflects service efficiency, the results suggest a non-linear relationship. Physicians with extremely slow (Level 3, ATT = 38.83, t = 1.86, *) or extremely fast (Level 4: ATT = 59.07, t = 3.41, ***; Level 5: ATT = 22.99, t = 2.77, ***) response times produced significant spillover effects, as did those with no wait time (Level 0: ATT = 20.10, t = 3.53, ***). However, Levels 1 and 2 were not statistically significant. Extremely slow service may enhance trust through compensatory knowledge sharing [12], while fast responses increase patient satisfaction and visibility, forming “efficiency signals” that reinforce departmental credibility [2]. Moderate-efficiency doctors may fall into the “moderate competitiveness trap” [57].
Finally, under Regional GDP, significant spillover effects were observed in low (ATT = 34.90, t = 4.92, ***) and medium-GDP regions (ATT = 33.40, t = 4.29, ***), but not in high-GDP areas. In resource-constrained environments, patients tend to rely more on collective information and knowledge sharing to make informed decisions [21]. Medium-GDP regions, while lacking absolute resource advantages, benefit more from departmental knowledge sharing due to their reliance on collective performance [60]. In contrast, patients in high-GDP regions may prioritize personal branding and physician credentials, limiting the impact of peer knowledge [27].
5.2.2. Spillover Effects Within the Same Hospital (hm_paid)
In alignment with Hypotheses H3b and H4b, this subsection examines whether the spillover effects of knowledge sharing within the same offline hospital vary across physician characteristics and institutional contexts. Using the same subgroup variables as in the specialty-level analysis, we analyze heterogeneous effects at the hospital level to enable direct comparison and deeper insight into how organizational structure and professional profiles shape the diffusion of shared knowledge (see Table 5).

Table 5.
Heterogeneous treatment effects of knowledge sharing on hm_paid (2020, matched ATT results).
The analysis of physician popularity shows a non-linear pattern. High-popularity physicians generated the strongest spillover effect (ATT = 75.83, t = 4.91, ***), followed by low-popularity physicians (ATT = 22.91, t = 2.48 **), while the effect for medium-popularity physicians was not statistically significant. This suggests the coexistence of two mechanisms: for high-popularity physicians, existing reputational capital—such as academic status or favorable patient reviews—acts as a “trust anchor”. Their knowledge-sharing behavior signals hospital-wide competence, leading to trust transfer across colleagues [27]. In contrast, low-popularity physicians may use frequent knowledge sharing to fill information voids, thereby enhancing patient trust in the broader hospital network [21]. Medium-popularity physicians, lacking both reputational authority and algorithmic visibility, are more vulnerable to being overlooked, a phenomenon described as the “moderate competitiveness trap” [57].
For consultation price, the spillover effect was only significant in the lowest-price group (ATT = 44.92, t = 6.03, ***). Similar to the specialty-level findings, this suggests that price-sensitive patients are more likely to make use of publicly available information and exhibit greater responsiveness to knowledge-sharing cues [40]. Conversely, high-price consultations are typically associated with brand loyalty and patient inertia, weakening the collective trust diffusion effect [27,40].
Physician title exhibited a clear upward gradient in spillover strength. Chief physicians (Title = 4) showed the highest effect (ATT = 75.79, t = 7.57, ***), followed by associate chief physicians (Title = 3, ATT = 60.29, t = 5.90, ***), attending physicians (Title = 2, ATT = 43.65, t = 3.24, ***), while junior physicians (Title = 1) did not show a significant effect (ATT = 34.32, t = 1.13). These findings diverge from the specialty-level patterns, where junior physicians generated stronger spillovers. At the hospital level, knowledge sharing by senior doctors appears to drive broader influence, possibly due to their integration into the hospital’s brand and increased algorithmic promotion. In particular, chief physicians are often publicly associated with the hospital’s institutional image, amplifying the reach of their knowledge sharing and leveraging trust across departments [56,61]. Junior physicians, by contrast, may lack the visibility and authority to exert such influence, even when engaging in similar behaviors.
In the case of gender, female physicians demonstrated a stronger spillover effect (ATT = 82.62, t = 7.6, ***) than male physicians (ATT = 49.70, t = 6.51, ***). Prior studies suggest that female physicians may be more effective in emotional communication and cross-disciplinary coordination, which strengthens knowledge flows and facilitates trust-based collaboration within the hospital [60].
For specialty type, notable differences were observed. The surgical department was excluded from the hm_paid analysis, similar to its exclusion in the dm_paid analysis. Obstetrics and gynecology had the strongest spillover effect (ATT = 79.53, t = 3, ***), reflecting its high patient sensitivity and demand for information, which make it conducive to hospital-wide trust transfer via knowledge sharing [56]. In contrast, Pediatrics showed a negative spillover effect (ATT = −36.57, t = −1.75, *), potentially due to internal competition for limited resources, where high-frequency sharing from a few physicians attracts patients disproportionately, thereby reducing demand for others [62,63]. The effects for Traditional Chinese Medicine (ATT = 16.86, t = 0.51) and Internal Medicine (ATT = −0.336, t = −0.02) were not significant, possibly due to the lower relevance of hospital-level branding in these specialties or the dominance of offline, physician-specific care preferences [57,60].
With regard to hospital level, Level 3 hospitals again exhibited the strongest and statistically significant spillover effect (ATT = 54.75, t = 9.11, ***), consistent with the idea of platform-enabled “hospital–star physician” brand integration [56]. In these settings, patient trust tends to extend from high-reputation physicians to the institution itself, reinforcing horizontal knowledge diffusion.
For wait time, physicians with normal (Level 1, ATT = 86.75, t = 4.11, ***), slow (Level 2, ATT = 72.45, t = 2.95, ***), slower (Level 3, ATT = 87.97, t = 2.94, ***), and faster (Level 4, ATT = 75.61, t = 3.31, ***) consultation response times exhibited the strongest spillover effects. These results reflect a trust synergy mechanism, whereby patients associate physicians with moderate efficiency profiles with the hospital’s brand image, forming a “reliable and comprehensive” perception that enhances confidence in the entire institution [64]. In particular, physicians with slightly slower response times often compensate through sustained and in-depth knowledge sharing, which builds long-term trust among patients [65]. By contrast, physicians with no wait time (Level 0, ATT = 53.90, t = 5.71, ***) and the fastest response times (Level 5, ATT = 31.42, t = 2.81, ***) also demonstrated strong and significant spillover effects, though with slightly lower magnitudes. These physicians primarily benefit from efficiency signaling, which boosts algorithmic visibility and attracts more patients through perceived responsiveness. However, due to the limited depth of interaction, patient trust tends to remain at a surface level, which falls short of initiating the multistage process required for substantive trust development [66].
Finally, regional GDP did not significantly moderate the spillover effect at the hospital level—all three categories (low, medium, and high GDP) displayed significant positive effects (e.g., medium GDP: ATT = 57.84, t = 5.08, ***). This indicates that, compared with specialty-based effects, hospitals as higher-order organizational units are better equipped to transcend regional disparities. In particular, medium-GDP regions displayed the strongest spillover, consistent with theories of “latecomer advantage” in digital health infrastructure [40]. Meanwhile, in high-GDP areas, stronger physician networks and faster knowledge dissemination mechanisms help sustain significant spillover, albeit at a slightly lower magnitude [62].
In summary, knowledge sharing generates substantial spillover effects in both intra-specialty and intra-hospital contexts. However, the underlying mechanisms differ. At the specialty level, spillover is shaped by peer networks, trust reallocation among patients, and informational asymmetry. At the hospital level, platform visibility, brand alignment, and institutional routines jointly amplify knowledge diffusion, particularly when high-ranking physicians serve as brand anchors. These findings suggest that platforms should tailor knowledge-sharing incentives to account for organizational structure and physician heterogeneity in order to maximize the value of collective knowledge.
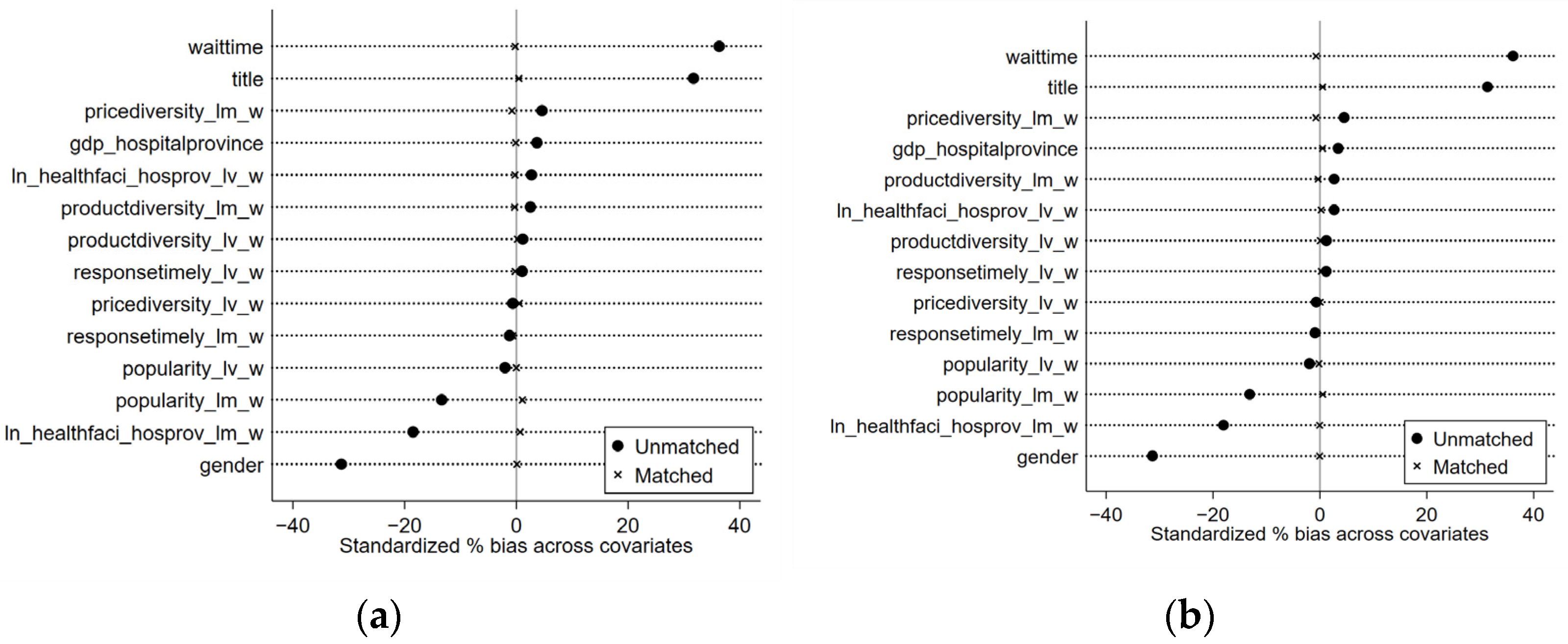
5.3. Matching Effectiveness and Balance Test
The p-test results shown in Figure 2a,b indicate the effectiveness of the matching process in minimizing bias across covariates. After performing the matching process, the standardized percentage bias for each covariate was reduced to below 10%, which is considered an acceptable threshold for achieving balance between the treated and control groups. This suggests that the matching process was successful in reducing bias, leading to a more reliable comparison between groups. The results for both dm_paid and hm_paid show that after matching, the bias in covariates was substantially minimized, confirming that the matching procedure has improved the comparability of the groups in the analysis. This demonstrates that the matching results are robust, and the subsequent analysis can be conducted with reduced confounding effects. Figure 2 displays the results for the main model.
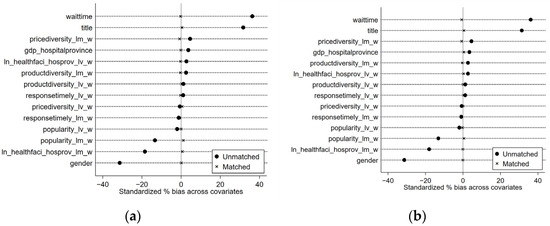
Figure 2.
Standardized mean difference graphs: (a) standardized mean difference graph of dm_paid; (b) standardized mean difference graph of hm_paid.
5.4. Robustness Test
To ensure the reliability of the main findings, we conducted a series of robustness checks across multiple dimensions, including alternative matching parameters, resampled datasets, temporal subgroups, and estimation techniques. These robustness tests are designed to confirm the validity of the causal inferences underlying Hypotheses H1 and H2 and to ensure that the estimated treatment effects are not artifacts of model specification or sampling variation. Specifically, the tests comprised caliper matching using a wider bandwidth (0.25 times the standard deviation), multistage sampling, year-specific subsamples, and inverse probability weighting (IPW) methods for both ATT and ATE estimation.
First, we re-estimated the models using a relaxed caliper of 0.25 standard deviations, as opposed to the default used in the main analysis [67]. The spillover effects of knowledge sharing on both dm_paid (within-specialty consultations) and hm_paid (within-hospital consultations) remained positive and statistically significant (t > 6.0), indicating that the results are not sensitive to the choice of matching threshold (see Table 6).

Table 6.
Robust test (Average Treatment Effect on the Treated).
Second, using a multistage sampled dataset, the estimated ATT for dm_paid was 21.16 (t = 2.70 ***), while hm_paid reached 66.84 (t = 5.94 ***), reaffirming the consistency of the treatment effects even under substantial changes in sample structure (Table 6).
Year-specific robustness checks further support this pattern. For the dm_paid outcome, the ATT was 32.10 (t = 6.77 ***) in 2018 and 29.68 (t = 7.36 ***) in 2019. Correspondingly, for hm_paid, the ATT values were 44.99 (t = 7.12 ***) and 55.68 (t = 10.21 ***) in the respective years, showing temporal stability of the spillover effects across different annual cohorts (Table 6).
In addition, we implemented inverse probability weighting (IPW) to mitigate potential selection bias and offer an alternative identification strategy (see Table 7). Under IPW linear regression, the ATT estimate for dm_paid was 13.32 (t = 3.49 ***), and the ATE was 23.29 (t = 6.18 ***). For hm_paid, the corresponding ATT and ATE were 44.76 (t = 8.20 ***) and 61.64 (t = 11.18 ***), respectively. These results corroborate the causal interpretation of the main findings even after accounting for sample selection mechanisms.

Table 7.
Robust Test Using Inverse Probability Weighting (IPW).
Taken together, the spillover effects of physicians’ knowledge sharing exhibit strong robustness across a wide range of methodological adjustments. The effects are consistently more pronounced at the hospital level (hm_paid), underscoring the broader institutional and network-based transmission of informational externalities in platform-enabled healthcare environments.
5.5. Sensitivity Analysis
To test the robustness of the estimated treatment effects against potential unobserved confounders—such as physician motivation, managerial incentives, or patient selection—we conducted Rosenbaum bounds sensitivity analysis using binary outcomes defined as whether a physician’s spillover effect exceeded the sample mean (i.e., dm_paid_high and hm_paid_high). For the specialty-level outcome (dm_paid_high), the effect remains statistically significant up to Γ = 2.0, implying that an unobserved confounder would need to more than double the odds of knowledge-sharing assignment to nullify the observed result. For the hospital-level outcome (hm_paid_high), the result holds up to Γ = 1.3, indicating that the hospital-level spillover effect is moderately sensitive to hidden bias. Overall, the analysis confirms that the findings are not easily attributable to unobserved heterogeneity and reinforces the credibility of the causal claims underlying Hypotheses H1 and H2 (see Table 8).

Table 8.
Sensitivity analysis using Mantel–Haenszel bounds.
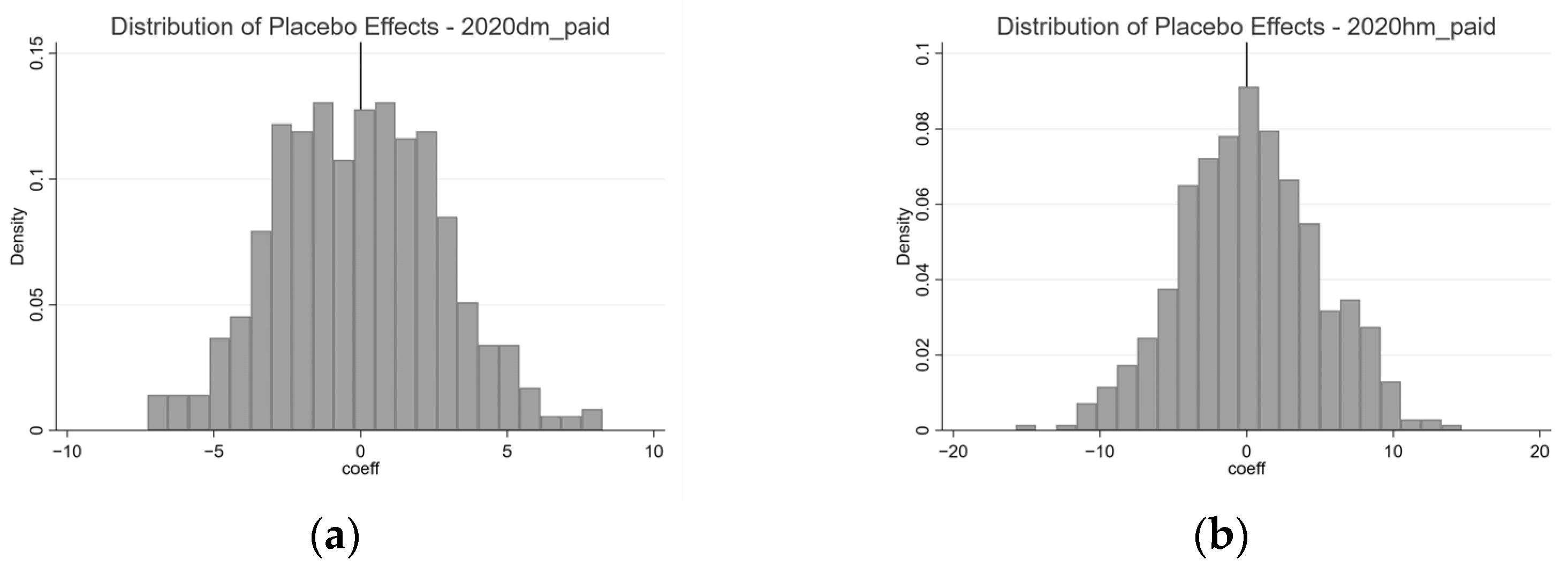
5.6. Placebo Test
To assess the risk of false positives, we conducted placebo tests by randomly reassigning the treatment variable (d_knowledge) 500 times and re-estimating the treatment effect each time. As Table 9 shows, for the specialty-level outcome (dm_paid), the distribution of placebo coefficients is centered around zero (mean = −0.07), and only 3.8% of simulations yielded statistically significant results at the 5% level. For the hospital-level outcome (hm_paid), the placebo distribution also centers near zero (mean = 0.21), with a 4.8% false positive rate. These low rejection rates suggest that the observed spillover effects are unlikely to be driven by random chance, further strengthening the internal validity of the findings and reinforcing support for H1 and H2. Figure 3 displays the distribution of placebo effects.

Table 9.
Placebo test—distribution of simulated treatment effects.
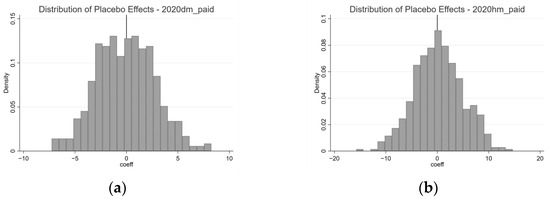
Figure 3.
Distribution of Placebo Effects (a) Distribution of Placebo Effects for dm_paid; (b) Distribution of Placebo Effects for hm_paid.
6. Discussion
6.1. Key Findings
This study investigates the spillover effects of physicians’ prosocial behavior—specifically knowledge sharing—on the paid consultations of their peers within the same specialty group and the same offline hospital on an online healthcare platform (OHP). The findings provide strong empirical support for the presence of positive and statistically significant spillover effects, consistent with Hypotheses 1 and 2. Notably, the spillover effect is substantially larger within offline hospitals compared with within specialty groups. This difference suggests that the influence of knowledge sharing is more pronounced in hospital-level networks, where brand synergy and resource integration amplify patients’ collective trust and facilitate broader diffusion of shared information across departments.
Beyond the confirmation of main effects, this study contributes a systematic investigation of spillover heterogeneity across two dimensions: (1) individual physician attributes (e.g., popularity, price, title, and gender) and (2) contextual/institutional characteristics (e.g., specialty type, hospital level, consultation responsiveness, and regional GDP). These multidimensional subgroup analyses reveal that the pathways and strength of spillover effects vary significantly across different contexts.
At the individual level, physician popularity moderates the direction and magnitude of spillover in distinct ways. Within specialty groups, less popular physicians exhibit stronger spillovers due to their high-frequency sharing behavior that bridges information gaps and enhances departmental trust. In contrast, within hospitals, highly popular physicians produce stronger effects, likely due to their reputational capital acting as a trust anchor that diffuses confidence throughout the institutional brand. Physician title exhibits a reverse pattern: junior physicians generate larger spillovers within specialty groups, while senior physicians dominate at the hospital level. This divergence reflects how visibility, authority, and organizational anchoring condition the influence of knowledge-sharing behavior.
In terms of contextual heterogeneity, spillover effects are stronger in pediatrics, traditional Chinese medicine, and obstetrics and gynecology within specialty groups, highlighting the importance of collective trust and long-term engagement in patient decision-making. Conversely, at the hospital level, the strongest effect emerges in obstetrics and gynecology, while pediatrics exhibits a negative spillover—due to internal resource competition. Hospital level also matters: tertiary hospitals consistently show stronger spillovers, reaffirming the role of platform-enabled brand integration and horizontal collaboration. Additionally, while regional GDP moderates specialty-level spillovers, its influence is less evident at the hospital level, underscoring how institutional structures can mitigate regional disparities in healthcare access and trust formation.
Robustness checks, including alternative caliper widths, multistage sampling, year-specific subsamples, and inverse probability weighting (IPW) models, further support the validity of these findings. Across all methods, knowledge-sharing spillovers remain statistically significant and directionally consistent, with hospital-level effects consistently stronger. These robustness tests affirm the causal interpretation and reliability of the results across diverse empirical specifications. Moreover, the robustness of these findings is further supported by sensitivity and placebo analyses.
6.2. Theoretical Contributions
This study makes several important contributions to the literature. First, it extends the understanding of prosocial behavior by investigating its indirect effects within the ecosystem of healthcare. While prior work has focused almost exclusively on the direct benefits of prosocial behavior for patients or individual physicians [9,57], this study highlights its ability to generate reciprocal benefits for other physicians in the same network, thus filling a key gap in extant research.
The results contribute to the theoretical framework of spillover effect heterogeneity by distinguishing between physician-level and institutional-level moderators. Prior studies have often treated heterogeneity in isolation—focusing on single characteristics such as specialty or title—but this research adopts an integrative approach to jointly analyze how individual attributes and organizational context shape the strength, scope, and direction of spillover effects. The findings reveal that the same physician behavior may operate through different mechanisms depending on the surrounding institutional environment, offering a richer theoretical account of how prosocial actions propagate through complex systems.
This study contributes to the understanding of the interplay between online and traditional healthcare systems. It shows how online prosocial behavior can benefit hospital-wide visibility, trust coordination, and peer collaboration, thus underlining the interdependent nature of modern healthcare ecosystems.
6.3. Practical Implications
The findings offer actionable insights for OHPs, healthcare administrators, and policymakers. First, platforms can actively promote a culture of prosocial behavior by emphasizing its collective benefits. For platforms, promoting knowledge sharing can enhance not only individual physician visibility but also system-wide engagement and patient trust. Importantly, incentive schemes should account for the observed heterogeneity: encouraging junior and less popular physicians to share content can strengthen specialty-level collaboration while leveraging the reputational capital of senior physicians enhances hospital-level diffusion.
Second, hospitals should integrate digital knowledge-sharing practices into their branding and trust-building strategies. Tertiary hospitals, in particular, stand to benefit from supporting high-profile physicians in content production, thereby reinforcing institutional credibility and patient engagement. Additionally, specialties such as obstetrics and gynecology, where spillovers are strong, may be prioritized in campaigns that promote digital outreach.
Lastly, policy frameworks should recognize prosocial behavior as a public good in healthcare ecosystems. By designing policies that reward information sharing and reduce structural barriers to trust diffusion, regulators can foster a more transparent, equitable, and patient-centered care environment.
6.4. Limitations and Future Directions
This study has certain limitations related to the availability of data from OHPs. While we have extended the research on spillover effects to include physicians within the same offline hospital, the inability to access additional offline hospital data for these patients limits the scope of our analysis. For example, data on patients’ offline interactions with other physicians, their referral pathways, or their longitudinal healthcare engagement would provide a more comprehensive understanding of spillover dynamics across online and offline systems.
Future research could replicate this study across different online healthcare platforms or international contexts to test the robustness of the findings in varied institutional environments. Additionally, employing more advanced causal inference techniques—such as instrumental variable approaches or longitudinal panel designs—would allow for a deeper understanding of the long-term effects of prosocial behavior. Further exploration of heterogeneous forms of prosocial engagement, including peer recommendations, interactive Q&A, or multi-physician collaborations, could provide nuanced insights into trust dynamics and platform engagement mechanisms.
Author Contributions
Conceptualization: Y.Z. and J.Z.; Methodology: Y.Z. and J.Z.; Software: Y.Z.; Validation: Y.Z. and J.Z.; Formal Analysis: Y.Z.; Investigation: Y.Z.; Resources: Y.Z. and J.Z.; Data Curation: Y.Z.; Writing—Original Draft Preparation: Y.Z.; Writing—Review and Editing: Y.Z. and J.Z.; Visualization: Y.Z.; Supervision: J.Z.; Project Administration: Y.Z. and J.Z.; Funding Acquisition: J.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (Nos. 72371188, 71971156, 72271082, and 72071063), the Fundamental Research Funds for the Central Universities (No. 22120210241), and the Natural Science Foundation of Anhui Province (No. 2408085J041).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to thank the HaoDaiFu platform for providing the publicly available de-identified dataset used in this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ren, H.; Wang, L.; Wu, J. The faster or richer the response, the better performance? An empirical analysis of online healthcare platforms from a competitive perspective. Decis. Support Syst. 2024, 184, 114274. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, X.; Liu, L.; Lai, K.H. Does voice matter? Investigating patient satisfaction on mobile health consultation. Inf. Process. Manag. 2023, 60, 103362. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Deng, Z.; Chen, X. Knowledge sharing motivations in online health communities: A comparative study of health professionals and normal users. Comput. Hum. Behav. 2017, 75, 797–810. [Google Scholar] [CrossRef]
- Xiong, X.; Luo, L.; Zhou, S.; Li, V.J.; Zhou, Y.; Huo, Z. A profile of patients’ and doctors’ perceptions, acceptance, and utilization of e-health in a deprived region in southwestern China. PLoS Digit. Health 2023, 2, e0000238. [Google Scholar] [CrossRef]
- Hara, N.; Foon Hew, K. Knowledge-sharing in an online community of health-care professionals. Inf. Technol. People 2007, 20, 235–261. [Google Scholar] [CrossRef]
- Oh, S. The characteristics and motivations of health answerers for sharing information, knowledge, and experiences in online environments. J. Am. Soc. Inf. Sci. Technol. 2012, 63, 543–557. [Google Scholar] [CrossRef]
- Han, G.; Kim, I. An Analysis of Factors Influencing Knowledge Sharing in Online Health Communities. J. Inf. Syst. 2024, 33, 51–74. [Google Scholar]
- Kuvaas, B.; Buch, R.; Dysvik, A. Perceived training intensity and knowledge sharing: Sharing for intrinsic and prosocial reasons. Hum. Resour. Manag. 2012, 51, 167–187. [Google Scholar] [CrossRef]
- Wang, J.J.; Liu, H.; Cui, X.; Ye, J.; Chen, H. Impact of a physician’s prosocial behavior on the patient’s choice: An empirical investigation in online health community. Inf. Technol. People 2023, 36, 1703–1725. [Google Scholar] [CrossRef]
- Learning, S. Altruism and prosocial behavior. Personal. Soc. Psychol. 2003, 5, 463. [Google Scholar]
- Pfattheicher, S.; Nielsen, Y.A.; Thielmann, I. Prosocial behavior and altruism: A review of concepts and definitions. Curr. Opin. Psychol. 2022, 44, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.B.; Chandwani, R.; Kumar, M. Factors affecting Web 2.0 adoption: Exploring the knowledge sharing and knowledge seeking aspects in health care professionals. J. Knowl. Manag. 2018, 22, 21–43. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S. Understanding relationship commitment and continuous knowledge sharing in online health communities: A social exchange perspective. J. Knowl. Manag. 2022, 26, 592–614. [Google Scholar] [CrossRef]
- Erdem, T.; Sun, B. An empirical investigation of the spillover effects of advertising and sales promotions in umbrella branding. J. Mark. Res. 2002, 39, 408–420. [Google Scholar] [CrossRef]
- Durnev, A.; Mangen, C. The spillover effects of MD&A disclosures for real investment: The role of industry competition. J. Account. Econ. 2020, 70, 101299. [Google Scholar]
- Liu, D.; Varki, S. The spillover effect of product recalls on competitors’ market value: The role of corporate product reliability. J. Bus. Res. 2021, 137, 452–463. [Google Scholar] [CrossRef]
- Tan, H.; Zhang, X.; Yang, Y. Satisfaction or gratitude? Exploring the disparate effects of physicians’ knowledge sharing on patients’ service evaluation in online medical consultations. Inf. Syst. J. 2023, 33, 1186–1211. [Google Scholar] [CrossRef]
- Ghosh, A.; Gupta, R.; Misra, A. Telemedicine for diabetes care in India during COVID-19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 273–276. [Google Scholar] [CrossRef]
- Guo, S.; Guo, X.; Fang, Y.; Vogel, D. How doctors gain social and economic returns in online health-care communities: A professional capital perspective. J. Manag. Inf. Syst. 2017, 34, 487–519. [Google Scholar] [CrossRef]
- Zhang, Y. Affective-Discursive Practice in Online Medical Consultations in China: Emotional and Empathic Acts, Identity Positions, and Power Relations; Springer Nature: Berlin/Heidelberg, Germany, 2022; Volume 11. [Google Scholar]
- Khurana, S.; Qiu, L.; Kumar, S. When a doctor knows, it shows: An empirical analysis of doctors’ responses in a Q&A forum of an online healthcare portal. Inf. Syst. Res. 2019, 30, 872–891. [Google Scholar]
- Zhao, W.; Gu, D.; Yang, X.; Jia, M.; Liang, C.; Wang, X.; Zolotarev, O. MedT2T: An adaptive pointer constrain generating method for a new medical text-to-table task. Future Gener. Comput. Syst. 2024, 161, 586–600. [Google Scholar] [CrossRef]
- Sabeeh, Z.; Syed Mustapha, S.; Mohamad, R. Healthcare knowledge sharing among a community of specialized physicians. Cogn. Technol. Work. 2018, 20, 105–124. [Google Scholar] [CrossRef]
- Gu, D.; Wang, Q.; Chai, Y.; Yang, X.; Zhao, W.; Li, M.; Zolotarev, O.; Xu, Z.; Zhang, G. Identifying the Risk Factors of Allergic Rhinitis Based on Zhihu Comment Data Using a Topic-Enhanced Word-Embedding Model: Mixed Method Study and Cluster Analysis. J. Med. Internet Res. 2024, 26, e48324. [Google Scholar] [CrossRef]
- Gu, D.; Liu, H.; Zhao, H.; Yang, X.; Li, M.; Liang, C. A deep learning and clustering-based topic consistency modeling framework for matching health information supply and demand. J. Assoc. Inf. Sci. Technol. 2024, 75, 152–166. [Google Scholar] [CrossRef]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Yang, H.; Du, H.S.; He, W.; Qiao, H. Understanding the motivators affecting doctors’ contributions in online healthcare communities: Professional status as a moderator. Behav. Inf. Technol. 2021, 40, 146–160. [Google Scholar] [CrossRef]
- Charband, Y.; Jafari Navimipour, N. Online knowledge sharing mechanisms: A systematic review of the state of the art literature and recommendations for future research. Inf. Syst. Front. 2016, 18, 1131–1151. [Google Scholar] [CrossRef]
- Yang, X.; Xi, N.; Gu, D.; Liang, C.; Liu, H.; Tang, H.; Hamari, J. Medical practice in gamified online communities: Longitudinal effects of gamification on doctor engagement. Inf. Manag. 2024, 61, 103906. [Google Scholar] [CrossRef]
- Schroeder, D.A.; Graziano, W.G. The field of prosocial behavior: An introduction and overview. In The Oxford Handbook of Prosocial Behavior; Oxford University Press: Oxford, UK, 2015; pp. 3–34. [Google Scholar]
- Dovidio, J.F.; Piliavin, J.A.; Schroeder, D.A.; Penner, L.A. The Social Psychology of Prosocial Behavior; Psychology Press: London, UK, 2017. [Google Scholar]
- Aknin, L.B.; Whillans, A.V.; Norton, M.I.; Dunn, E.W. Happiness and prosocial behavior: An evaluation of the evidence. World Happiness Rep. 2019, 2019, 67–86. [Google Scholar]
- Penner, L.A.; Dovidio, J.F.; Piliavin, J.A.; Schroeder, D.A. Prosocial behavior: Multilevel perspectives. Annu. Rev. Psychol. 2005, 56, 365–392. [Google Scholar] [CrossRef]
- Barasch, A.; Levine, E.E.; Berman, J.Z.; Small, D.A. Selfish or selfless? On the signal value of emotion in altruistic behavior. J. Personal. Soc. Psychol. 2014, 107, 393. [Google Scholar] [CrossRef] [PubMed]
- Majdandžić, J.; Amashaufer, S.; Hummer, A.; Windischberger, C.; Lamm, C. The selfless mind: How prefrontal involvement in mentalizing with similar and dissimilar others shapes empathy and prosocial behavior. Cognition 2016, 157, 24–38. [Google Scholar] [CrossRef]
- Berman, J.Z.; Silver, I. Prosocial behavior and reputation: When does doing good lead to looking good? Curr. Opin. Psychol. 2022, 43, 102–107. [Google Scholar] [CrossRef]
- Van Lange, P.A. Does empathy trigger only altruistic motivation? How about selflessness or justice? Emotion 2008, 8, 766. [Google Scholar] [CrossRef] [PubMed]
- Swap, W.C. When prosocial behavior becomes altruistic: An attributional analysis. Curr. Psychol. 1991, 10, 49–64. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, N.; Sun, H. The relationship between moral sense of life and prosocial behavior among medical students: The multiple mediating effects of meaning in life and empathy. Chin. J. Behav. Med. Brain Sci. 2021, 944–948. [Google Scholar]
- Meng, F.; Zhang, X.; Liu, L.; Ren, C. Converting readers to patients? From free to paid knowledge-sharing in online health communities. Inf. Process. Manag. 2021, 58, 102490. [Google Scholar] [CrossRef]
- Meng, F.; Liu, Y.; Zhang, X.; Liu, L. General knowledge-sharing and patient engagement in online health communities: An inverted U-shaped relationship. J. Knowl. Manag. 2024, 28, 763–788. [Google Scholar] [CrossRef]
- Ahluwalia, R.; Unnava, H.R.; Burnkrant, R.E. The moderating role of commitment on the spillover effect of marketing communications. J. Mark. Res. 2001, 38, 458–470. [Google Scholar] [CrossRef]
- Song, W.; Chen, J.; Li, W. Spillover effect of consumer awareness on third parties’ selling strategies and retailers’ platform openness. Inf. Syst. Res. 2020, 32, 172–193. [Google Scholar] [CrossRef]
- Bettels, J.; Wiedmann, K.-P. Brand logo symmetry and product design: The spillover effects on consumer inferences. J. Bus. Res. 2019, 97, 1–9. [Google Scholar] [CrossRef]
- Erreygers, S.; Vandebosch, H.; Vranjes, I.; Baillien, E.; De Witte, H. Feel good, do good online? Spillover and crossover effects of happiness on adolescents’ online prosocial behavior. J. Happiness Stud. 2019, 20, 1241–1258. [Google Scholar] [CrossRef]
- Olson, E.L. The impact of intra-brand platform sharing on brand attractiveness. J. Prod. Brand Manag. 2009, 18, 212–217. [Google Scholar] [CrossRef]
- Smith, D.C.; Park, C.W. The effects of brand extensions on market share and advertising efficiency. J. Mark. Res. 1992, 29, 296–313. [Google Scholar] [CrossRef]
- Balachander, S.; Ghose, S. Reciprocal spillover effects: A strategic benefit of brand extensions. J. Mark. 2003, 67, 4–13. [Google Scholar] [CrossRef]
- Pontes, N.; Pontes, V. Spillover effects of competitive rivalry on brand extensions. J. Brand Manag. 2021, 28, 402–412. [Google Scholar] [CrossRef]
- Tezer, A.; Tofighi, M. CSR spillover effect: The influence of a brand’s corporate social responsibility activity on competing brands. J. Mark. Manag. 2021, 37, 651–670. [Google Scholar] [CrossRef]
- Chae, I.; Stephen, A.T.; Bart, Y.; Yao, D. Spillover effects in seeded word-of-mouth marketing campaigns. Mark. Sci. 2017, 36, 89–104. [Google Scholar] [CrossRef]
- Zou, P.; Li, G. How emerging market investors’ value competitors’ customer equity: Brand crisis spillover in China. J. Bus. Res. 2016, 69, 3765–3771. [Google Scholar] [CrossRef]
- Seo, S.; Jang, S.S. Who spoils the barrel? Negative spillover effect on competitor brands during food crises. Int. J. Hosp. Manag. 2021, 98, 103047. [Google Scholar] [CrossRef]
- Islam, S.; Grigoriadis, C.; Papastergiou, S. Information sharing for creating awareness for securing healthcare ecosystem. In Proceedings of the 2023 19th International Conference on the Design of Reliable Communication Networks (DRCN), Vilanova i la Geltrú, Spain, 22–25 March 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 1–5. [Google Scholar]
- Xu, J.; Jain, H.K.; Gu, D.; Liang, C. Business-Process-Driven Service Composition in a Hybrid Cloud Environment. Inf. Syst. Front. 2025, 27, 259–281. [Google Scholar] [CrossRef]
- Pikkarainen, M.; Kemppainen, L.; Xu, Y.; Jansson, M.; Ahokangas, P.; Koivumäki, T.; Hong Gu, H.; Francis Gomes, J. Resource integration capabilities to enable platform complementarity in healthcare service ecosystem co-creation. Balt. J. Manag. 2022, 17, 688–704. [Google Scholar] [CrossRef]
- Zhou, P.; Xie, Y.; Liang, C.; Zhu, J.; Zhao, S. The effect of prosocial behavior and its intensity on doctors’ performance in an online health community. Humanit. Soc. Sci. Commun. 2024, 11, 874. [Google Scholar] [CrossRef]
- Francetic, I.; Meacock, R.; Elliott, J.; Kristensen, S.R.; Britteon, P.; Lugo-Palacios, D.G.; Wilson, P.; Sutton, M. Framework for identification and measurement of spillover effects in policy implementation: Intended non-intended targeted non-targeted spillovers (INTENTS). Implement. Sci. Commun. 2022, 3, 30. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Tang, J.; Chen, Y.; Ma, J. Collaborative Communication: A Qualitative Study of Roles and Emphases of Health Care Providers in Obstetrics and Gynecology. J. Multidiscip. Healthc. 2024, 17, 1913–1922. [Google Scholar] [CrossRef]
- Deng, Z.; Deng, Z.; Liu, S.; Evans, R. Knowledge transfer between physicians from different geographical regions in China’s online health communities. Inf. Technol. Manag. 2023, 26, 83–100. [Google Scholar] [CrossRef]
- Wu, M.; Brandhorst, H.; Marinescu, M.C.; Lopez, J.M.; Hlava, M.; Busch, J. Automated metadata annotation: What is and is not possible with machine learning. Data Intell. 2023, 5, 122–138. [Google Scholar] [CrossRef]
- Freeman, M.; Savva, N.; Scholtes, S. Economies of scale and scope in hospitals: An empirical study of volume spillovers. Manag. Sci. 2021, 67, 673–697. [Google Scholar] [CrossRef]
- Basajja, M.; Nambobi, M.; Wolstencroft, K. Possibility of enhancing digital health interoperability in Uganda through FAIR data. Data Intell. 2022, 4, 899–916. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, X.; Meng, L.; Lyu, X. More knowledge, more choices? How peer recognition of physicians’ knowledge sharing affect patients’ consultation in online health communities. Front. Public Health 2024, 12, 1376887. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, X.; Xu, X.; Guo, J.; Guo, F. What influences physicians’ online knowledge sharing? A stimulus–response perspective. Front. Psychol. 2022, 12, 808432. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Bai, J.; Zhao, H.; Zhang, X. The effect of “offline-to-online” trust transfer on the utilization of online medical consultation among Chinese rural residents: Experimental study. J. Med. Internet Res. 2023, 25, e43430. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.J. Reducing bias using propensity score matching. J. Nucl. Cardiol. 2018, 25, 404–406. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).