Body Surface Area-Based Dosing of Mycophenolate Mofetil in Pediatric Hematopoietic Stem Cell Transplant Recipients: A Prospective Population Pharmacokinetic Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Mycophenolate Mofetil Dosing, Blood Sampling, and Data Collection
2.3. Pharmacokinetic Analysis
2.3.1. Non-Compartmental Analysis (NCA)
2.3.2. Population Pharmacokinetic Analysis
2.4. Model Evaluation
2.5. Model Simulation
3. Results
3.1. Population Characteristics
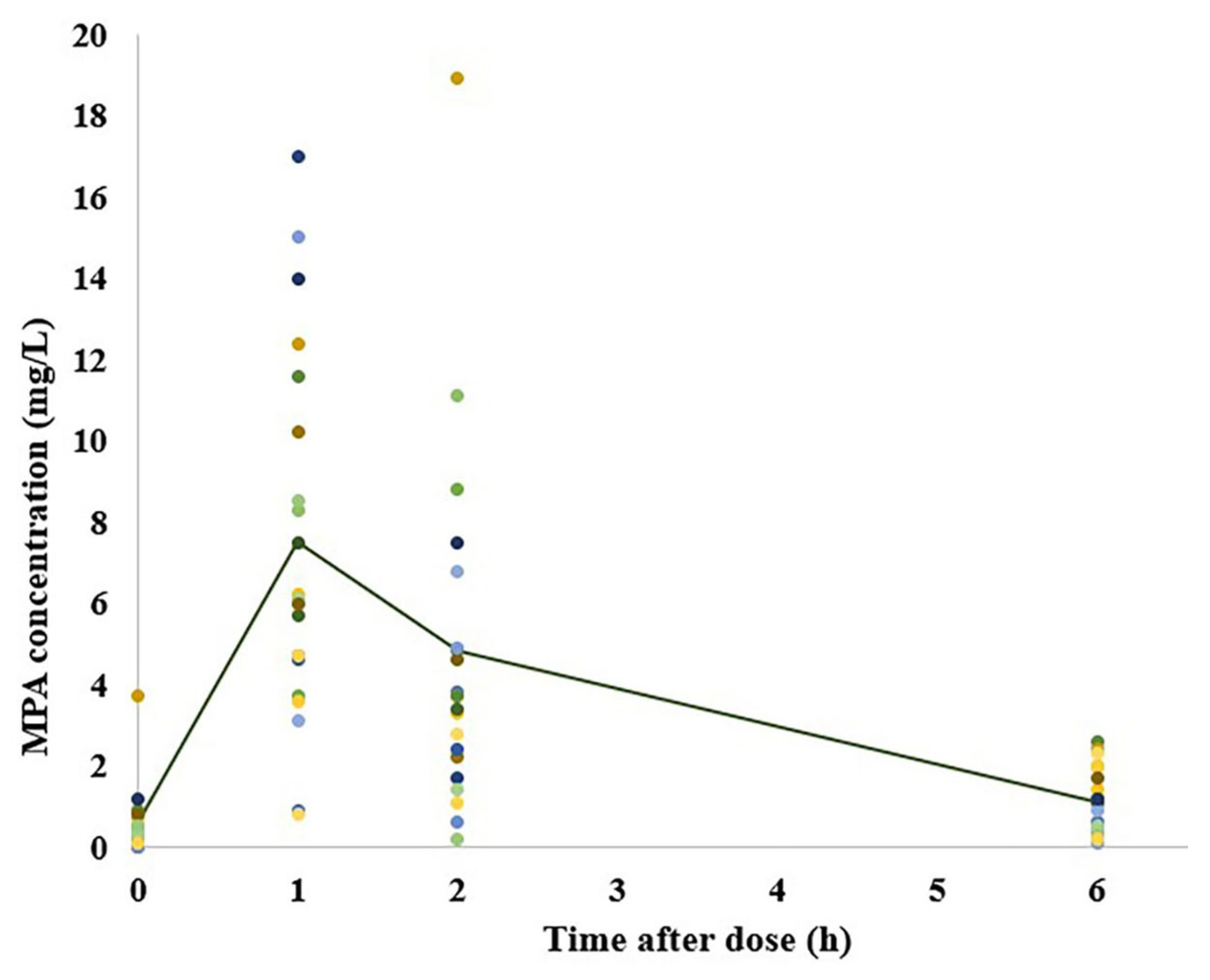
3.2. Pharmacokinetic Analysis
3.2.1. NCA Results and the Relationship between MMF PK and aGVHD Prophylaxis
3.2.2. Population Pharmacokinetic Analysis
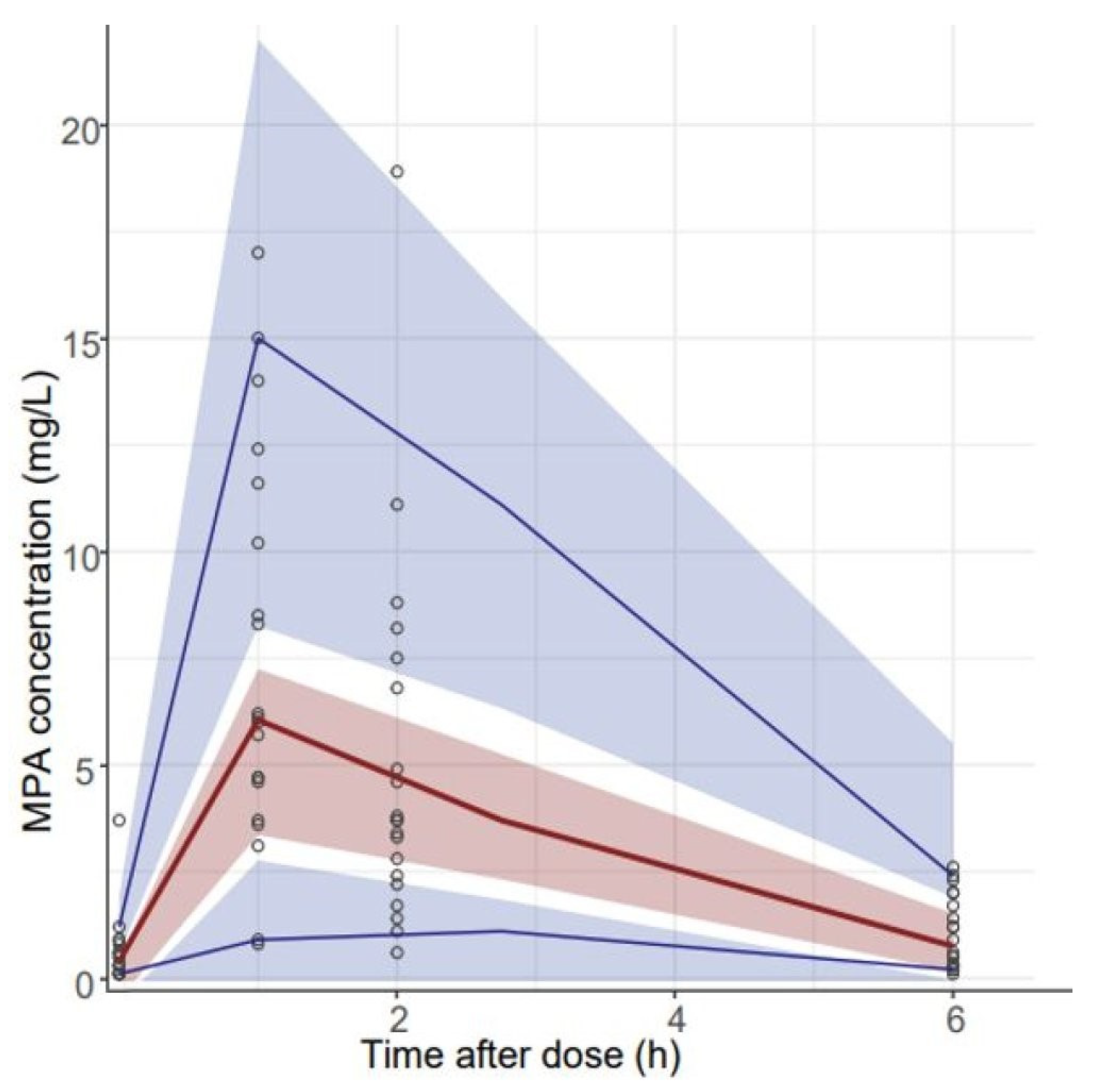
3.3. Model Evaluation
3.4. Model Simulation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacobsohn, D.A. Acute graft-versus-host disease in children. Bone Marrow Transpl. 2008, 41, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Jagasia, M.; Arora, M.; Flowers, M.E.; Chao, N.J.; McCarthy, P.L.; Cutler, C.S.; Urbano-Ispizua, A.; Pavletic, S.Z.; Haagenson, M.D.; Zhang, M.-J.; et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood 2012, 119, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Malard, F.; Holler, E.; Sandmaier, B.M.; Huang, H.; Mohty, M. Acute graft-versus-host disease. Nat. Rev. Dis. Prim. 2023, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Zeiser, R.; Blazar, B.R. Acute Graft-versus-Host Disease—Biologic Process, Prevention, and Therapy. N. Engl. J. Med. 2017, 377, 2167–2179. [Google Scholar] [CrossRef] [PubMed]
- Jamani, K.; Russell, J.A.; Daly, A.; Stewart, D.; Savoie, L.; Duggan, P.; Storek, J. Prognosis of grade 3-4 acute GVHD continues to be dismal. Bone Marrow Transpl. 2013, 48, 1359–1361. [Google Scholar] [CrossRef] [PubMed]
- El-Jawahri, A.; Li, S.; Antin, J.H.; Spitzer, T.R.; Armand, P.A.; Koreth, J.; Nikiforow, S.; Ballen, K.K.; Ho, V.T.; Alyea, E.P.; et al. Improved Treatment-Related Mortality and Overall Survival of Patients with Grade IV Acute GVHD in the Modern Years. Biol. Blood Marrow Transpl. 2016, 22, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Holtan, S.G.; Yu, J.; Choe, H.K.; Paranagama, D.; Tang, J.; Naim, A.; Galvin, J.; Deeg, H.J. Disease progression, treatments, hospitalization, and clinical outcomes in acute GVHD: A multicenter chart review. Bone Marrow Transpl. 2022, 57, 1581–1585. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Hematopoietic Cell Transplantation (HCT) (Version 3.2023). 2023. Available online: https://www.nccn.org/professionals/physician_gls/pdf/hct.pdf (accessed on 10 October 2023).
- Kawashima, N.; Iida, M.; Suzuki, R.; Fukuda, T.; Atsuta, Y.; Hashii, Y.; Inoue, M.; Kobayashi, M.; Yabe, H.; Okada, K.; et al. Prophylaxis and treatment with mycophenolate mofetil in children with graft-versus-host disease undergoing allogeneic hematopoietic stem cell transplantation: A nationwide survey in Japan. Int. J. Hematol. 2019, 109, 491–498. [Google Scholar] [CrossRef]
- Inagaki, J.; Kodama, Y.; Fukano, R.; Noguchi, M.; Okamura, J. Mycophenolate mofetil for treatment of steroid-refractory acute graft-versus-host disease after pediatric hematopoietic stem cell transplantation. Pediatr. Transpl. 2015, 19, 652–658. [Google Scholar] [CrossRef]
- Carlone, G.; Simeone, R.; Baraldo, M.; Maestro, A.; Zanon, D.; Barbi, E.; Maximova, N. Area-under-the-Curve-Based Mycophenolate Mofetil Dosage May Contribute to Decrease the Incidence of Graft-versus-Host Disease after Allogeneic Hematopoietic Cell Transplantation in Pediatric Patients. J. Clin. Med. 2021, 10, 406. [Google Scholar] [CrossRef]
- Penack, O.; Marchetti, M.; Ruutu, T.; Aljurf, M.; Bacigalupo, A.; Bonifazi, F.; Ciceri, F.; Cornelissen, J.; Malladi, R.; Duarte, R.F.; et al. Prophylaxis and management of graft versus host disease after stem-cell transplantation for haematological malignancies: Updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2020, 7, e157–e167. [Google Scholar] [CrossRef]
- Zeiser, R. Prevention of Graft-Versus-Host Disease; Rosmarin, A.G., Ed.; UpToDate: Waltham, MA, USA; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2022. [Google Scholar]
- Wei, Y.; Wu, D.; Chen, Y.; Dong, C.; Qi, J.; Wu, Y.; Cai, R.; Zhou, S.; Li, C.; Niu, L.; et al. Population pharmacokinetics of mycophenolate mofetil in pediatric patients early after liver transplantation. Front. Pharmacol. 2022, 13, 1002628. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Ye, Q.; Huang, Y.; Xu, H.; Li, Z. Population Pharmacokinetics of Enteric-Coated Mycophenolate Sodium in Children after Renal Transplantation and Initial Dosage Recommendation Based on Body Surface Area. Comput. Math. Methods Med. 2022, 2022, 1881176. [Google Scholar] [CrossRef] [PubMed]
- Barau, C.; Furlan, V.; Debray, D.; Taburet, A.M.; Barrail-Tran, A. Population pharmacokinetics of mycophenolic acid and dose optimization with limited sampling strategy in liver transplant children. Br. J. Clin. Pharmacol. 2012, 74, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Long-Boyle, J.; Rydholm, N.; Orchard, P.J.; Tolar, J.; Smith, A.R.; Jacobson, P.; Brundage, R. Population pharmacokinetics of unbound mycophenolic acid in pediatric and young adult patients undergoing allogeneic hematopoietic cell transplantation. J. Clin. Pharmacol. 2012, 52, 1665–1675. [Google Scholar] [CrossRef] [PubMed]
- Premaud, A.; Weber, L.T.; Tonshoff, B.; Armstrong, V.W.; Oellerich, M.; Urien, S.; Marquet, P.; Rousseau, A. Population pharmacokinetics of mycophenolic acid in pediatric renal transplant patients using parametric and nonparametric approaches. Pharmacol. Res. 2011, 63, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Blair, E.Y.; Nath, C.E.; Shaw, P.J.; Earl, J.W.; Stephen, K.; Montgomery, K.; Coakley, J.C.; Hodson, E.; Stormon, M.; et al. Population pharmacokinetics of mycophenolic acid in children and young people undergoing blood or marrow and solid organ transplantation. Br. J. Clin. Pharmacol. 2010, 70, 567–579. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Fakhoury, M.; Deschenes, G.; Roussey, G.; Brochard, K.; Niaudet, P.; Tsimaratos, M.; André, J.L.; Cloarec, S.; Cochat, P.; et al. Population pharmacokinetics and pharmacogenetics of mycophenolic acid following administration of mycophenolate mofetil in de novo pediatric renal-transplant patients. J. Clin. Pharmacol. 2010, 50, 1280–1291. [Google Scholar] [CrossRef] [PubMed]
- Payen, S.; Zhang, D.; Maisin, A.; Popon, M.; Bensman, A.; Bouissou, F.; Loirat, C.; Gomeni, R.; Bressolle, F.; Jacqz-Aigrain, E. Population pharmacokinetics of mycophenolic acid in kidney transplant pediatric and adolescent patients. Ther. Drug Monit. 2005, 27, 378–388. [Google Scholar] [CrossRef]
- Labriffe, M.; Vaidie, J.; Monchaud, C.; Debord, J.; Turlure, P.; Girault, S.; Marquet, P.; Woillard, J. Population pharmacokinetics and Bayesian estimators for intravenous mycophenolate mofetil in haematopoietic stem cell transplant patients. Br. J. Clin. Pharmacol. 2020, 86, 1550–1559. [Google Scholar] [CrossRef]
- Yoshimura, K.; Yano, I.; Yamamoto, T.; Kawanishi, M.; Isomoto, Y.; Yonezawa, A.; Kondo, T.; Takaori-Kondo, A.; Matsubara, K. Population pharmacokinetics and pharmacodynamics of mycophenolic acid using the prospective data in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transpl. 2018, 53, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Mager, D.E.; Sandmaier, B.M.; Storer, B.E.; Boeckh, M.J.; Bemer, M.J.; Phillips, B.R.; Risler, L.J.; McCune, J.S. Pharmacokinetic and pharmacodynamic analysis of inosine monophosphate dehydrogenase activity in hematopoietic cell transplantation recipients treated with mycophenolate mofetil. Biol. Blood Marrow Transpl. 2014, 20, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Frymoyer, A.; Verotta, D.; Jacobson, P.; Long-Boyle, J. Population pharmacokinetics of unbound mycophenolic acid in adult allogeneic haematopoietic cell transplantation: Effect of pharmacogenetic factors. Br. J. Clin. Pharmacol. 2013, 75, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Mager, D.E.; Bemer, M.J.; Salinger, D.H.; Vicini, P.; Sandmaier, B.M.; Nash, R.; McCune, J.S. A limited sampling schedule to estimate mycophenolic Acid area under the concentration-time curve in hematopoietic cell transplantation recipients. J. Clin. Pharmacol. 2012, 52, 1654–1664. [Google Scholar] [CrossRef] [PubMed]
- Saint-Marcoux, F.; Royer, B.; Debord, J.; Larosa, F.; Legrand, F.; Deconinck, E.; Kantelip, J.-P.; Marquet, P. Pharmacokinetic modelling and development of Bayesian estimators for therapeutic drug monitoring of mycophenolate mofetil in reduced-intensity haematopoietic stem cell transplantation. Clin. Pharmacokinet. 2009, 48, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.; Wichart, J.; Hamiwka, L.; Kiang, T.K.L. Significant Effects of Renal Function on Mycophenolic Acid Total Clearance in Pediatric Kidney Transplant Recipients with Population Pharmacokinetic Modeling. Clin. Pharmacokinet. 2023, 62, 1289–1303. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Mager, D.E.; Sandmaier, B.M.; Maloney, D.G.; Bemer, M.J.; McCune, J.S. Population pharmacokinetics and dose optimization of mycophenolic acid in HCT recipients receiving oral mycophenolate mofetil. J. Clin. Pharmacol. 2013, 53, 393–402. [Google Scholar] [CrossRef]
- Jacobson, P.; Huang, J.; Rydholm, N.; Tran, M.; Defor, T.; Tolar, J.; Orchard, P.J. Higher mycophenolate dose requirements in children undergoing hematopoietic cell transplant (HCT). J. Clin. Pharmacol. 2008, 48, 485–494. [Google Scholar] [CrossRef]
- Staatz, C.E.; Tett, S.E. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin. Pharmacokinet. 2007, 46, 13–58. [Google Scholar] [CrossRef]
- Zhang, D.; Renbarger, J.L.; Chow, D.S. Pharmacokinetic Variability of Mycophenolic Acid in Pediatric and Adult Patients with Hematopoietic Stem Cell Transplantation. J. Clin. Pharmacol. 2016, 56, 1378–1386. [Google Scholar] [CrossRef]
- Zhang, D.; Chow, D.S. Clinical Pharmacokinetics of Mycophenolic Acid in Hematopoietic Stem Cell Transplantation Recipients. Eur. J. Drug Metab. Pharmacokinet. 2017, 42, 183–189. [Google Scholar] [CrossRef] [PubMed]
- van Hest, R.M.; Doorduijn, J.K.; de Winter, B.C.; Cornelissen, J.J.; Vulto, A.G.; Oellerich, M.; Löwenberg, B.; A A Mathot, R.; Armstrong, V.W.; van Gelder, T. Pharmacokinetics of mycophenolate mofetil in hematopoietic stem cell transplant recipients. Ther. Drug Monit. 2007, 29, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Haentzschel, I.; Freiberg-Richter, J.; Platzbecker, U.; Kiani, A.; Schetelig, J.; Illmer, T.; Ehninger, G.; Schleyer, E.; Bornhäuser, M. Targeting mycophenolate mofetil for graft-versus-host disease prophylaxis after allogeneic blood stem cell transplantation. Bone Marrow Transpl. 2008, 42, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Resztak, M.; Sobiak, J.; Czyrski, A. Recent Advances in Therapeutic Drug Monitoring of Voriconazole, Mycophenolic Acid, and Vancomycin: A Literature Review of Pediatric Studies. Pharmaceutics 2021, 13, 1991. [Google Scholar] [CrossRef] [PubMed]
- Kum, C.D.; Lee, M.J.; Park, J.E. Successful engraftment after infusion of multiple low doses of CD34+ cells from a poorly matched sibling donor in a patient with severe aplastic anemia. Yeungnam Univ. J. Med. 2019, 36, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Ham, J.Y.; Jung, H.Y.; Choi, J.Y.; Park, S.H.; Kim, Y.L.; Kim, H.K.; Huh, S.; Kim, C.-D.; Won, D.I.; Song, K.E.; et al. Usefulness of mycophenolic acid monitoring with PETINIA for prediction of adverse events in kidney transplant recipients. Scand. J. Clin. Lab. Investig. 2016, 76, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Vergara Chozas, J.M.; Saez-Benito Godino, A.; Zopeque Garcia, N.; Garcia Pinteno, S.; Joumady, I.; Carrasco Garcia, C.; Gil, F.V. Analytical validation of a homogeneous immunoassay for determination of mycophenolic acid in human plasma. Transpl. Proc. 2012, 44, 2669–2672. [Google Scholar] [CrossRef] [PubMed]
- Funatogawa, T.; Narita, Y.; Tamura, A.; Mii, K.; Sugitani, Y.; Uchida, T. Use of mycophenolate mofetil in patients with pediatric and adult primary nephrotic syndrome: Information from a Japanese hospital claims database. Clin. Exp. Nephrol. 2022, 26, 1005–1013. [Google Scholar] [CrossRef]
- Genentech USA, Inc. Cellcept (Mycophenolate Mofetil) [Package Insert]; Genentech USA, Inc.: South San Francisco, CA, USA, 2022. [Google Scholar]
- Rong, Y.; Jun, H.; Kiang, T.K.L. Population pharmacokinetics of mycophenolic acid in paediatric patients. Br. J. Clin. Pharmacol. 2021, 87, 1730–1757. [Google Scholar] [CrossRef]
- Doesch, A.O.; Mueller, S.; Konstandin, M.; Celik, S.; Erbel, C.; Kristen, A.; Frankenstein, L.; Koch, A.; Ehlermann, P.; Zugck, C.; et al. Proton pump inhibitor co-medication reduces active drug exposure in heart transplant recipients receiving mycophenolate mofetil. Transpl. Proc. 2010, 42, 4243–4246. [Google Scholar] [CrossRef]
- Chaudhry, H.M.; Bruce, A.J.; Wolf, R.C.; Litzow, M.R.; Hogan, W.J.; Patnaik, M.S.; Kremers, W.K.; Phillips, G.L.; Hashmi, S.K. The Incidence and Severity of Oral Mucositis among Allogeneic Hematopoietic Stem Cell Transplantation Patients: A Systematic Review. Biol. Blood Marrow Transpl. 2016, 22, 605–616. [Google Scholar] [CrossRef] [PubMed]
- Borrows, R.; Chusney, G.; Loucaidou, M.; James, A.; Van Tromp, J.; Cairns, T.; Griffith, M.; Hakim, N.; McLean, A.; Palmer, A.; et al. The magnitude and time course of changes in mycophenolic acid 12-hour predose levels during antibiotic therapy in mycophenolate mofetil-based renal transplantation. Ther. Drug Monit. 2007, 29, 122–126. [Google Scholar] [CrossRef] [PubMed]
- McCune, J.S.; Jacobson, P.; Wiseman, A.; Militano, O. Optimizing drug therapy in pediatric SCT: Focus on pharmacokinetics. Bone Marrow Transpl. 2015, 50, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Mathew, B.S.; Fleming, D.H.; Prasanna, S.; Basu, G.; Chandy, S.J.; John, G.T. Mycophenolic acid estimation by pooled sampling: A novel strategy. Ther. Drug Monit. 2010, 32, 141–144. [Google Scholar] [CrossRef]
- Kiang, T.K.; Ensom, M.H. Therapeutic drug monitoring of mycophenolate in adult solid organ transplant patients: An update. Expert Opin. Drug Metab. Toxicol. 2016, 12, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Fukuda, T.; Cox, S.; de Vries, M.T.; Hooper, D.K.; Goebel, J.; Vinks, A.A. Population pharmacokinetic-pharmacodynamic modelling of mycophenolic acid in paediatric renal transplant recipients in the early post-transplant period. Br. J. Clin. Pharmacol. 2014, 78, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Uchiyama, K.; Saito, Y.; Takekuma, Y.; Sugita, J.; Teshima, T.; Sugawara, M. Pharmacokinetics of mycophenolic acid after haplo-hematopoietic stem cell transplantation in Japanese recipients. J. Oncol. Pharm. Pract. 2022, 28, 31–38. [Google Scholar] [CrossRef]



| Characteristics | Values |
|---|---|
| Male gender, n (%) | 12 (60.0) |
| Age, years, median (range) | 9.7 (1.7–15.6) |
| 1 ≤ age < 12, n (%) | 14 (70.0) |
| 12 ≤ age < 18, n (%) | 6 (30.0) |
| Body weight, kg, median (range) | 31.2 (9.9–51.0) |
| Height, cm, median (range) | 136.0 (83.6–176.9) |
| BSA, m2, median (range) | 1.12 (0.49–1.60) |
| Diagnosis for HSCT, n (%) | |
| AA | 2 (10.0) |
| ALL | 7 (35.0) |
| AML | 5 (25.0) |
| Congenital neutropenia | 1 (5.0) |
| HLH | 1 (5.0) |
| Krabbe disease | 1 (5.0) |
| NHL | 2 (10.0) |
| T-MDS | 1 (5.0) |
| Conditioning regimen, n (%) | |
| BuFluATG | 1 (5.0) |
| BuFluCy | 15 (75.0) |
| BuFludaVPATG | 1 (5.0) |
| FluMelATG | 1 (5.0) |
| TBI FluCyATG | 2 (10.0) |
| Donor source, n (%) | |
| Haploidentical family donor/matched unrelated donor | 16 (80.0)/4 (20.0) |
| ABO match, n (%) | |
| Compatible/incompatible | 16 (80.0)/4 (20.0) |
| Patients with previous or concomitant tacrolimus on the day of blood sampling, n (%) | 20 (100.0) |
| Previous tacrolimus history, n (%) | 4 (20.0) |
| Concomitant tacrolimus, n (%) | 16 (80.0) |
| Time post-HSCT, days, median (range) * | 31 (20–181) |
| Duration of MMF, days, median (range) * | 23 (16–123) |
| MMF first use, n (%) | |
| aGVHD prophylaxis/treatment | 16 (80.0)/4 (20.0) |
| MMF dose, mg/day, median (range) | 1100 (380–2000) |
| MMF dose normalized by body weight, mg/kg/dose, median (range) | 17.9 (16.1–19.8) |
| MMF formulation, n (%) | |
| Capsule/suspension | 6 (30.0)/14 (70.0) |
| Laboratory values * | |
| SCr, mg/dL, median (range) | 0.42 (0.32–0.72) |
| eGFR, mL/min/1.73 m2, median (range) | 112.6 (86.3–165.3) |
| AST, IU/L, median (range) | 48.5 (26–93) |
| ALT, IU/L, median (range) | 52 (16–251) |
| T.bil, mg/dL, median (range) | 0.5 (0.4–2.0) |
| Alb, g/dL, median (range) | 3.8 (3.3–4.2) |
| Comedication, n (%) * | |
| Ciprofloxacin | 15 (75.0) |
| Esomeprazole | 4 (20.0) |
| Famotidine | 4 (20.0) |
| Itraconazole | 2 (10.0) |
| Lansoprazole | 3 (15.0) |
| Voriconazole | 1 (5.0) |
| Pharmacokinetic Parameters | MPA PK Parameter Estimates (Mean ± Standard Deviation) (n = 20) |
|---|---|
| Cmax (mg/L) | 8.50 ± 4.76 |
| AUC0–6 (mg·h/L) | 22.37 ± 13.50 |
| AUC0–inf (mg·h/L) | 27.69 ± 15.94 |
| Vd/F (L) | 69.04 ± 59.58 |
| CL/F (L/h) | 23.43 ± 15.69 |
| Pharmacokinetic Parameters | MPA PK Parameter Estimates * | p-Value | |
|---|---|---|---|
| aGVHD Patients (n = 7) | Non-aGVHD Patients (n = 9) | ||
| Cmax (mg/L) | 5.18 ± 1.09 | 10.93 ± 5.21 | 0.016 |
| Tmax (h) | 1.29 ± 0.49 | 1.44 ± 0.53 | 0.606 |
| AUC0–6 (mg·h/L) | 13.26 ± 5.35 | 28.20 ± 16.64 | 0.023 |
| AUC0–inf (mg·h/L) | 14.78 ± 6.41 | 35.16 ± 18.86 | 0.016 |
| Vd/F (L) | 74.55 ± 48.10 | 54.89 ± 59.13 | 0.210 |
| CL/F (L/h) | 32.69 ± 21.45 | 18.01 ± 9.50 | 0.114 |
| Parameter | Structural Model (n = 20) | Final Model (n = 20) | Bootstrap (n = 1000) | ||
|---|---|---|---|---|---|
| Estimate | RSE % | Estimate | RSE % | Median (95% CI *) | |
| Fixed effects | |||||
| ka (h−1) | 6.53 | 20 | 5.18 | 21 | 5.22 (1.83–7.04) |
| Vd/F (L) | 77.7 | 19 | 89.8 | 16 | 85.13 (60.65–121.45) |
| CL/F (L/h) | 16.5 | 18 | 16.6 | 17 | 17.14 (12.03–23.60) |
| BSA on Vd/F | - | - | 0.854 | 24 | 0.839 (0.32–1.20) |
| Random effects | |||||
| Inter-individual variability (IIV) | |||||
| IIV Vd/F, %CV | 49.48 | 68 | 37.71 | 69 | 35.16 (9.83–62.03) |
| IIV CL/F, %CV | 84.51 | 33 | 89.96 | 33 | 86.72 (43.83–126.39) |
| Residual error | |||||
| Proportional error | 0.675 | 9 | 0.660 | 9 | 0.656 (0.547–0.763) |
| Additive error | 0.110 | 24 | 0.111 | 17 | 0.109 (0.083–0.327) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.J.; Hong, K.T.; Han, N.; Kim, I.-W.; Oh, J.M.; Kang, H.J. Body Surface Area-Based Dosing of Mycophenolate Mofetil in Pediatric Hematopoietic Stem Cell Transplant Recipients: A Prospective Population Pharmacokinetic Study. Pharmaceutics 2023, 15, 2741. https://doi.org/10.3390/pharmaceutics15122741
Park HJ, Hong KT, Han N, Kim I-W, Oh JM, Kang HJ. Body Surface Area-Based Dosing of Mycophenolate Mofetil in Pediatric Hematopoietic Stem Cell Transplant Recipients: A Prospective Population Pharmacokinetic Study. Pharmaceutics. 2023; 15(12):2741. https://doi.org/10.3390/pharmaceutics15122741
Chicago/Turabian StylePark, Hyun Jin, Kyung Taek Hong, Nayoung Han, In-Wha Kim, Jung Mi Oh, and Hyoung Jin Kang. 2023. "Body Surface Area-Based Dosing of Mycophenolate Mofetil in Pediatric Hematopoietic Stem Cell Transplant Recipients: A Prospective Population Pharmacokinetic Study" Pharmaceutics 15, no. 12: 2741. https://doi.org/10.3390/pharmaceutics15122741





