The Moderating Effects of the Families Improving Together (FIT) for Weight Loss Intervention and Parenting Factors on Family Mealtime in Overweight and Obese African American Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. FIT Trial Study Design
2.3. FIT Motivational and Family Weight Loss (M + FWL) Intervention
2.4. Comprehensive Health Education (CHE) Comparison Program
2.5. Measures
2.5.1. Demographic Information
2.5.2. Adolescent and Parent BMI
2.5.3. Adolescent Perceptions of Parenting Style (Responsiveness and Demandingness)
2.5.4. Adolescent-Reported Parental Feeding Practices
2.6. Outcome Measures
Family Mealtime
2.7. Analysis Plan
3. Results
3.1. Participant Characteristics
3.2. Bivariate Correlations
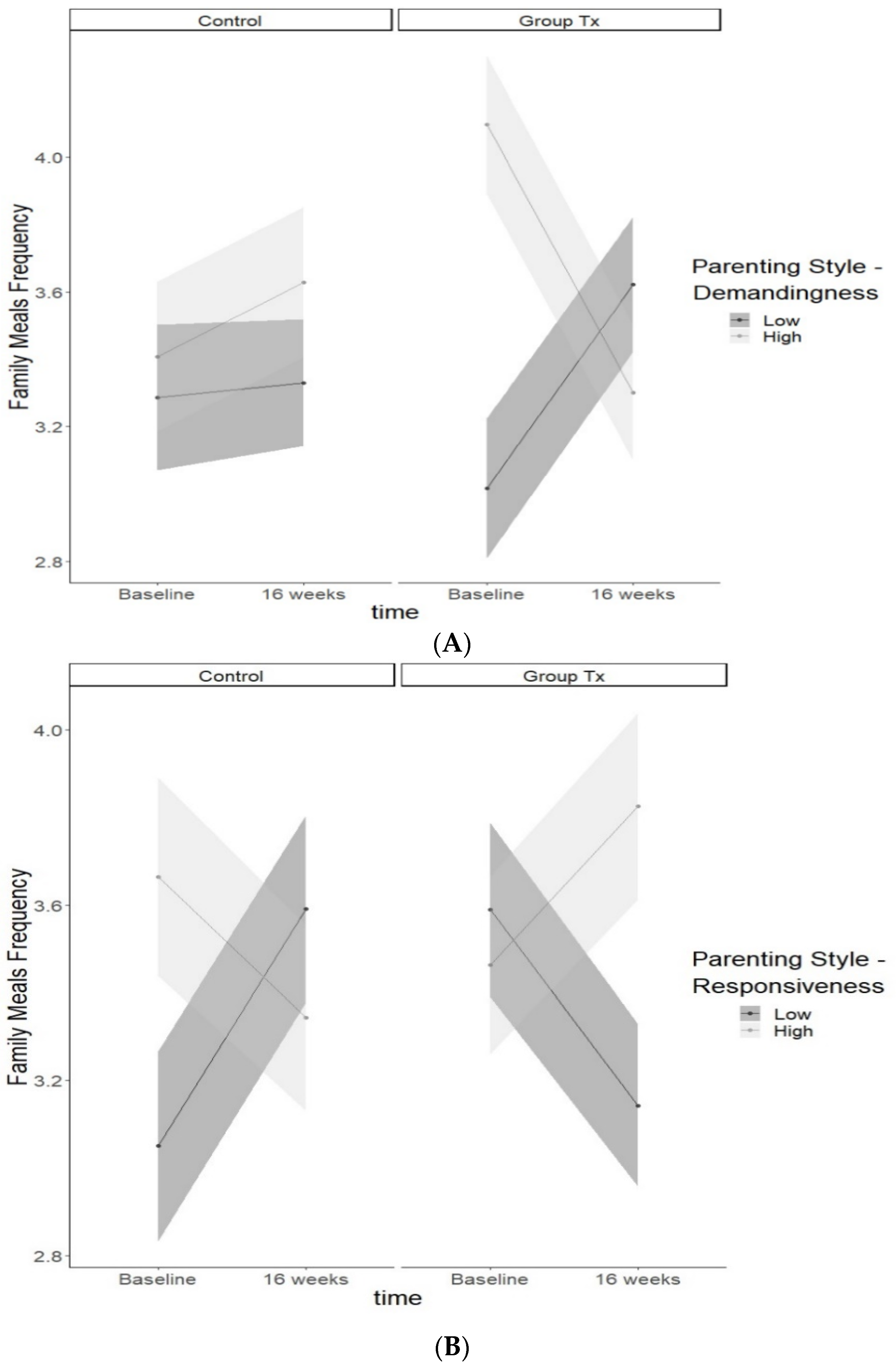
3.3. Parenting Style
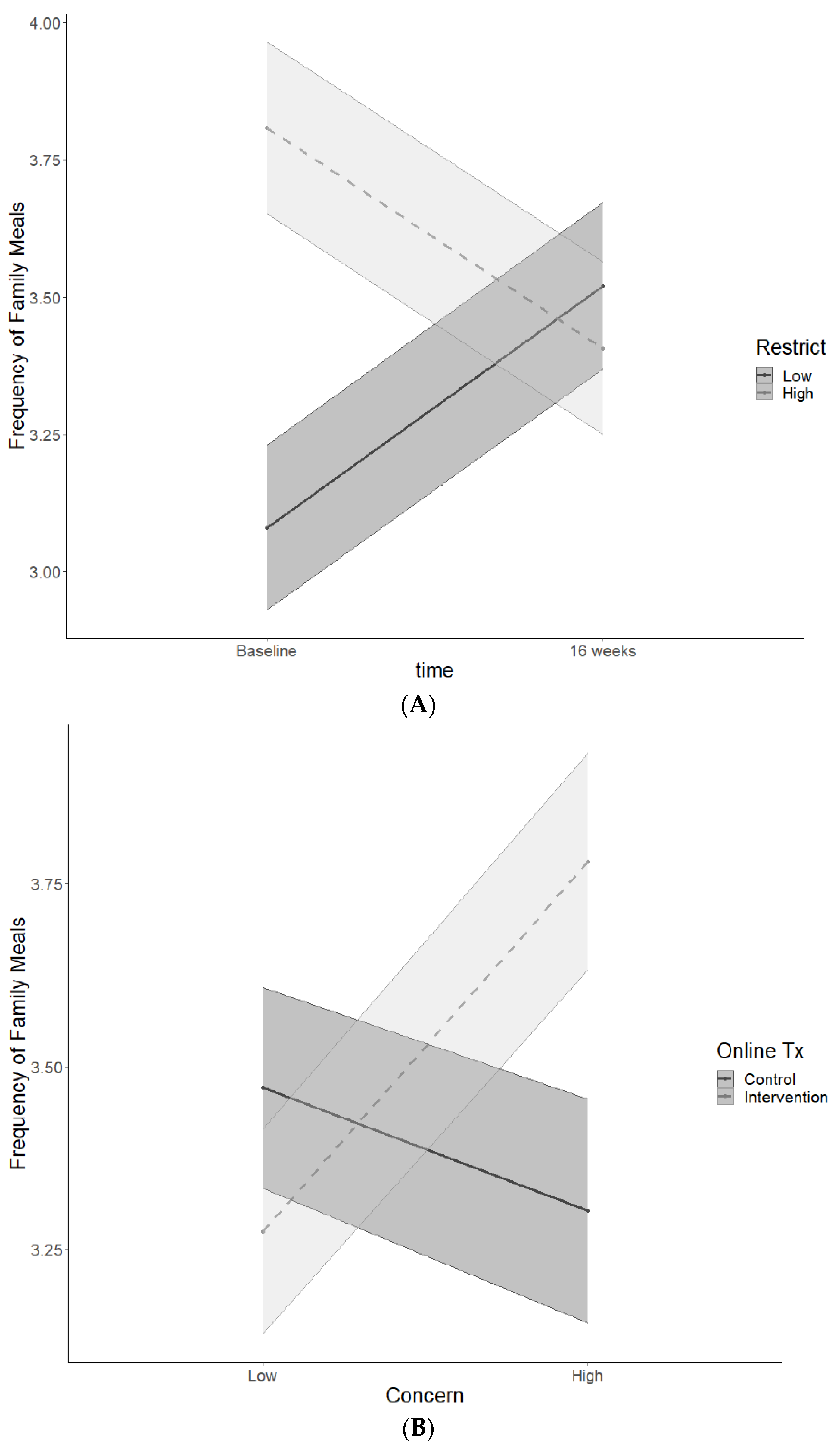
3.4. Parenting Feeding Practices
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ogden, C.L.; Carroll, M.D.; Lawman, H.G.; Fryar, C.D.; Kruszon-Moran, D.; Kit, B.K.; Flegal, K.M. Trends in Obesity Prevalence among Children and Adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016, 315, 2292–2299. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity among Adults. CDC 2020, 360, 1–8. [Google Scholar]
- Pi-Sunyer, F.X. The Obesity Epidemic: Pathophysiology and Consequences of Obesity. Obes. Res. 2002, 10 (Suppl. S2), 97S–104S. [Google Scholar] [CrossRef]
- Bell, C.N.; Kerr, J.; Young, J.L. Associations between Obesity, Obesogenic Environments, and Structural Racism Vary by County-Level Racial Composition. Int. J. Environ. Res. Public Health 2019, 16, 861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neumark-Sztainer, D.; Hannan, P.J.; Story, M.; Croll, J.; Perry, C. Family Meal Patterns: Associations with Sociodemographic Characteristics and Improved Dietary Intake among Adolescents. J. Am. Diet. Assoc. 2003, 103, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Hammons, A.J.; Fiese, B.H. Is Frequency of Shared Family Meals Related to the Nutritional Health of Children and Adolescents? Pediatrics 2011, 127, 1565–1574. [Google Scholar] [CrossRef] [Green Version]
- Berge, J.M.; Wall, M.; Larson, N.; Loth, K.A.; Neumark-Sztainer, D. Family Functioning: Associations with Weight Status, Eating Behaviors, and Physical Activity in Adolescents. J. Adolesc. Health 2013, 52, 351–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broderick, C.B. Understanding Family Process: Basics of Family Systems Theory; SAGE Publications: Thousand Oaks, CA, USA, 1993. [Google Scholar]
- Kitzman-Ulrich, H.; Wilson, D.K.; George, S.M.S.; Lawman, H.; Segal, M.; Fairchild, A. The Integration of a Family Systems Approach for Understanding Youth Obesity, Physical Activity, and Dietary Programs. Clin. Child Fam. Psychol. Rev. 2010, 13, 231–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, D.K.; Sweeney, A.M.; Kitzman-Ulrich, H.; Gause, H.; George, S.M.S. Promoting Social Nurturance and Positive Social Environments to Reduce Obesity in High-Risk Youth. Clin. Child Fam. Psychol. Rev. 2017, 20, 64–77. [Google Scholar] [CrossRef] [Green Version]
- Maccoby, E.E.; Martin, J. Socialization in the Context of the Family: Parent-Child Interaction. In Handbook of Child Psychology: {Vol}.~4. {Socialization}, Personality, and Social Development; Wiley: New York, NY, USA, 1983. [Google Scholar]
- Lytle, L.A.; Varnell, S.; Murray, D.M.; Story, M.; Perry, C.; Birnbaum, A.S.; Kubik, M.Y. Predicting Adolescents’ Intake of Fruits and Vegetables. J. Nutr. Educ. Behav. 2003, 35, 170–175. [Google Scholar] [CrossRef]
- Alsharairi, N.A.; Somerset, S.M. Associations between Parenting Styles and Children’s Fruit and Vegetable Intake. Ecol. Food Nutr. 2015, 54, 93–113. [Google Scholar] [CrossRef] [PubMed]
- Kröller, K.; Jahnke, D.; Warschburger, P. Are Maternal Weight, Eating and Feeding Practices Associated with Emotional Eating in Childhood? Appetite 2013, 65, 25–30. [Google Scholar] [CrossRef]
- LeCroy, M.N.; Siega-Riz, A.M.; Albrecht, S.S.; Ward, D.S.; Cai, J.; Perreira, K.M.; Isasi, C.R.; Mossavar-Rahmani, Y.; Gallo, L.C.; Castañeda, S.F.; et al. Association of Food Parenting Practice Patterns with Obesogenic Dietary Intake in Hispanic/Latino Youth: Results from the Hispanic Community Children’s Health Study/Study of Latino Youth (SOL Youth). Appetite 2019, 140, 277–287. [Google Scholar] [CrossRef]
- Wilson, D.K.; Kitzman-Ulrich, H.; Resnicow, K.; Van Horn, M.L.; George, S.M.S.; Siceloff, E.R.; Alia, K.A.; McDaniel, T.; Heatley, V.S.; Huffman, L.; et al. An Overview of the Families Improving Together (FIT) for Weight Loss Randomized Controlled Trial in African American Families. Contemp. Clin. Trials 2015, 42, 145–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryan, R.M.; Deci, E.L.; Grolnick, W.S.; La Guardia, J.G. The Significance of Autonomy and Autonomy Support in Psychological Development and Psychopathology. In Developmental Psychopathology, 2nd ed.; Wiley: New York, NY, USA, 2015; Volume 1. [Google Scholar] [CrossRef]
- Mâsse, L.C.; Watts, A.W.; Barr, S.I.; Tu, A.W.; Panagiotopoulos, C.; Geller, J.; Chanoine, J.P. Individual and Household Predictors of Adolescents’ Adherence to a Web-Based Intervention. Ann. Behav. Med. 2015, 49, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Haines, J.; Rifas-Shiman, S.L.; Horton, N.J.; Kleinman, K.; Bauer, K.W.; Davison, K.K.; Walton, K.; Austin, S.B.; Field, A.E.; Gillman, M.W. Family Functioning and Quality of Parent-Adolescent Relationship: Cross-Sectional Associations with Adolescent Weight-Related Behaviors and Weight Status. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- West, F.; Sanders, M.R.; Cleghorn, G.J.; Davies, P.S.W. Randomised Clinical Trial of a Family-Based Lifestyle Intervention for Childhood Obesity Involving Parents as the Exclusive Agents of Change. Behav. Res. Ther. 2010, 48, 1170–1179. [Google Scholar] [CrossRef]
- Rhee, K.E.; Jelalian, E.; Boutelle, K.; Dickstein, S.; Seifer, R.; Wing, R. Warm Parenting Associated with Decreasing or Stable Child BMI during Treatment. Child. Obes. 2016, 12, 94–102. [Google Scholar] [CrossRef] [Green Version]
- Dallacker, M.; Hertwig, R.; Mata, J. The Frequency of Family Meals and Nutritional Health in Children: A Meta-Analysis. Obes Rev. 2018, 19, 638–653. [Google Scholar] [CrossRef]
- Lee, S.Y.; Ha, S.A.; Seo, J.S.; Sohn, C.M.; Park, H.R.; Kim, K.W. Eating Habits and Eating Behaviors by Family Dinner Frequency in the Lower-Grade Elementary School Students. Nutr. Res. Pract. 2014, 8, 679–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mamun, A.A.; Lawlor, D.A.; O’Callaghan, M.J.; Williams, G.M.; Najman, J.M. Positive Maternal Attitude to the Family Eating Together Decreases the Risk of Adolescent Overweight. Obes. Res. 2005, 13, 1422–1430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huffman, L.E.; Wilson, D.K.; Kitzman-Ulrich, H.; Lyerly, J.E.; Gause, H.M.; Resnicow, K. Associations between Culturally Relevant Recruitment Strategies and Participant Interest, Enrollment and Generalizability in a Weight-Loss Intervention for African American Families. Ethn. Dis. 2016, 26, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.K.; Sweeney, A.M.; Law, L.H.; Kitzman-Ulrich, H.; Resnicow, K. Web-Based Program Exposure and Retention in the Families Improving Together for Weight Loss Trial. Ann. Behav. Med. 2019, 53, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Law, L.H.; Wilson, D.K.; St George, S.M.; Kitzman, H.; Kipp, C.J. Families Improving Together (FIT) for Weight Loss: A Resource for Translation of a Positive Climate-Based Intervention into Community Settings. Transl. Behav. Med. 2019, 10, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Alia, K.A.; Wilson, D.K.; McDaniel, T.; George, S.M.S.; Kitzman-Ulrich, H.; Smith, K.; Heatley, V.S.; Wise, C. Development of an Innovative Process Evaluation Approach for the Families Improving Together (FIT) for Weight Loss Trial in African American Adolescents. Eval. Program Plann. 2015, 49, 106–116. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Cliffs, NJ, USA, 1986; Volume 16:2–xiii, p. 617. [Google Scholar]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC Growth Charts: United States Advance Data from Vital and Health Statistics; National Center for Health Statistics: Hyattsville, MD, USA, 2000; pp. 1–27.
- Jackson, C.; Henriksen, L.; Foshee, V.A. The Authoritative Parenting Index: Predicting Health Risk Behaviors among Children and Adolescents. Heal. Educ. Behav. 1998, 25, 319–337. [Google Scholar] [CrossRef]
- Huffman, L.E.; Wilson, D.K.; Van Horn, M.L.; Pate, R.R. Associations between Parenting Factors, Motivation, and Physical Activity in Overweight African American Adolescents. Ann. Behav. Med. 2018, 52, 93–105. [Google Scholar] [CrossRef]
- Birch, L.L.; Fisher, J.O.; Grimm-Thomas, K.; Markey, C.N.; Sawyer, R.; Johnson, S.L. Confirmatory Factor Analysis of the Child Feeding Questionnaire: A Measure of Parental Attitudes, Beliefs and Practices about Child Feeding and Obesity Proneness. Appetite 2001, 36, 201–210. [Google Scholar] [CrossRef]
- Farrow, C.V. Do Parental Feeding Practices Moderate the Relationships between Impulsivity and Eating in Children? Eat. Behav. 2012, 13, 150–153. [Google Scholar] [CrossRef] [Green Version]
- Kaur, H.; Li, C.; Nazir, N.; Choi, W.S.; Resnicow, K.; Birch, L.L.; Ahluwalia, J.S. Confirmatory Factor Analysis of the Child-Feeding Questionnaire among Parents of Adolescents. Appetite 2006, 47, 36–45. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Larson, N.I.; Fulkerson, J.A.; Eisenberg, M.E.; Story, M. Family Meals and Adolescents: What Have We Learned from Project EAT (Eating Among Teens)? Public Health Nutr. 2010, 13, 1113–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schafer, J.L. Analysis of Incomplete Multivariate Data; Chapman & Hall/CRC: Washington, DC, USA, 1997. [Google Scholar] [CrossRef]
- Enders, C.K. Analyzing Longitudinal Data With Missing Values. Rehabil. Psychol. 2011, 56, 267–288. [Google Scholar] [CrossRef]
- Sleddens, E.F.C.; Gerards, S.M.P.L.; Thijs, C.; De Vries, N.K.; Kremers, S.P.J. General Parenting, Childhood Overweight and Obesity-Inducing Behaviors: A Review. Int. J. Pediatr. Obes. 2011, 6, e12–e27. [Google Scholar] [CrossRef] [PubMed]
- Loncar, H.; Wilson, D.K.; Sweeney, A.M.; Quattlebaum, M.; Zarrett, N. Associations of Parenting Factors and Weight Related Outcomes in African American Adolescents with Overweight and Obesity. J. Behav. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wrotniak, B.H.; Epstein, L.H.; Paluch, R.A.; Roemmich, J.N. The Relationship between Parent and Child Self-Reported Adherence and Weight Loss. Obes. Res. 2005, 13, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; McKenzie, S.J.; Valoski, A.; Klein, K.R.; Wing, R.R. Effects of Mastery Criteria and Contingent Reinforcement for Family-Based Child Weight Control. Addict. Behav. 1994, 19, 135–145. [Google Scholar] [CrossRef]
- Monaghan, M.; Horn, I.B.; Alvarez, V.; Cogen, F.R.; Streisand, R. Authoritative Parenting, Parenting Stress, and Self-Care in Pre-Adolescents with Type 1 Diabetes. J. Clin. Psychol. Med. Settings 2012, 19, 255–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinberg, L.; Lamborn, S.D.; Darling, N.; Mounts, N.S.; Dornbusch, S.M. Over-Time Changes in Adjustment and Competence among Adolescents from Authoritative, Authoritarian, Indulgent, and Neglectful Families. Child Dev. 1994, 65, 754–770. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.A.; Story, M.; Mellin, A.; Leffert, N.; Neumark-Sztainer, D.; French, S.A. Family Dinner Meal Frequency and Adolescent Development: Relationships with Developmental Assets and High-Risk Behaviors. J. Adolesc. Health 2006, 39, 337–345. [Google Scholar] [CrossRef]
- Tamis-LeMonda, C.S.; Briggs, R.D.; McClowry, S.G.; Snow, D.L. Challenges to the Study of African American Parenting: Conceptualization, Sampling, Research Approaches, Measurement, and Design. Parenting 2008, 8, 319–358. [Google Scholar] [CrossRef]
- Hennessy, E.; Hughes, S.O.; Goldberg, J.P.; Hyatt, R.R.; Economos, C.D. Parent Behavior and Child Weight Status among a Diverse Group of Underserved Rural Families. Appetite 2010, 54, 369–377. [Google Scholar] [CrossRef]
- Lane, S.P.; Bluestone, C.; Burke, C.T. Trajectories of BMI from Early Childhood through Early Adolescence: SES and Psychosocial Predictors. Br. J. Health Psychol. 2013, 18, 66–82. [Google Scholar] [CrossRef]
- Fuemmeler, B.F.; Yang, C.; Costanzo, P.; Hoyle, R.H.; Siegler, I.C.; Williams, R.B.; Østbye, T. Parenting Styles and Body Mass Index Trajectories from Adolescence to Adulthood. Health Psychol. 2012, 31, 441–449. [Google Scholar] [CrossRef] [Green Version]
- Baumrind, D. An Exploratory Study of Socialization Effects on Black Children: Some Black-White Comparisons. Child Dev. 1972, 43, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.E. The Relationship Between Family Environment and Parenting Style: A Preliminary Study of African American Families. J. Black Psychol. 1995, 21, 408–423. [Google Scholar] [CrossRef]
- LeCuyer, E.A.; Swanson, D.P.; Cole, R.; Kitzman, H. Effect of African- and European-American Maternal Attitudes and Limit-Setting Strategies on Children’s Self-Regulation. Res. Nurs. Health 2011, 34, 468–482. [Google Scholar] [CrossRef]
- Burton, E.T.; Wilder, T.; Beech, B.M.; Bruce, M.A. Caregiver Feeding Practices and Weight Status among African American Adolescents: The Jackson Heart KIDS Pilot Study. Eat. Behav. 2017, 27, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.; Wall, M.; Choi, C.W.; Bucchianeri, M.; Quick, V.; Larson, N.; Neumark-Sztainer, D. Family Meals and Disordered Eating in Adolescents: Are the Benefits the Same for Everyone? Int. J. Eat. Disord. 2015, 48, 100–110. [Google Scholar] [CrossRef]
| Adolescent sex (n, % female) | 153 (63.5%) |
| Adolescent Age (years) M (SD) | 12.8 (1.75) |
| Average Adolescent BMI % | 96.63% |
| Parent sex (n, % female) | 231 (96%) |
| Parent Age (years) (M, SD) | 43.2 (8.65) |
| Parent BMI (kg/m2) (M, SD) | 37.75 (8.79) |
| Married (n, %) | 83 (34.4%) |
| Parent Education (n, %) | |
| 9 To 11 Years | 6 (2.5%) |
| 12 Years | 33 (13.7%) |
| Some College | 100 (41.5%) |
| 4 Year College | 47 (19.5%) |
| Professional | 55 (22.8%) |
| Parent Annual Household Income (n, %) | |
| Less than $10,000 | 36 (14.9%) |
| $10,000–$24,000 | 50 (20.3%) |
| $25,000–$39,000 | 66 (27.4%) |
| $40,000–$54,000 | 32 (13.3%) |
| $55,000–$69,000 | 21 (8.7%) |
| $70,000–$84,000 | 12 (5%) |
| $85,000 or greater | 24 (10%) |
| Frequency of Family Meals-baseline, M(SD) | 3.46 (1.62) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adolescent Age | − | −0.12 | −0.22 * | −0.06 | −0.03 | −0.07 | −0.21 * | −0.12 | −0.08 | 0.02 | −0.06 | −0.12 | −0.20 * | −0.15 * |
| 2. Adolescent zBMI | − | 0.08 | −0.08 | −0.03 | 0.17 * | 0.12 | 0.02 | −0.03 | −0.05 | 0.04 | 0.04 | −0.06 | −0.14 * | |
| 3. Family Meals (BL) | − | 0.15 * | 0.24 * | 0.12 | 0.24 * | 0.05 | 0.26 * | 0.03 | 0.14 * | 0.09 | 0.08 | 0.02 | ||
| 4. Responsiveness (BL) | − | 0.48 * | 0.28 * | 0.22 * | 0.01 | 0.12 | 0.38 * | 0.16 * | 0.13 * | −0.03 | 0 | |||
| 5. Demandingness (BL) | − | 0.29 * | 0.19 * | 0.1 | 0.05 | 0.2 * | 0.3 * | 0.16 * | −0.03 | 0.07 | ||||
| 6. Concern (BL) | − | 0.36 * | 0.15 * | 0.02 | 0.08 | 0.13 * | 0.36 * | 0.06 | 0.14 * | |||||
| 7. Restrict (BL) | − | 0.41 * | 0.07 | 0.06 | 0.08 | 0.25 * | 0.22 * | 0.11 | ||||||
| 8. Pressure (BL) | − | 0.03 | −0.05 | −0.14 * | 0.01 | 0.11 | 0.24 * | |||||||
| 9. Family Meals (16 w) | − | 0.06 | −0.08 | 0.05 | −0.02 | −0.08 | ||||||||
| 10. Responsiveness (16 w) | − | 0.47 * | 0.19 * | 0 | −0.09 | |||||||||
| 11. Demandingness (16 w) | − | 0.31 * | 0.09 | −0.01 | ||||||||||
| 12. Concern (16 w) | − | 0.3 * | 0.22 * | |||||||||||
| 13. Restrict (16 w) | − | 0.47 * | ||||||||||||
| 14. Pressure (16 w) | − |
| Estimate | SE | p | FMI | |
|---|---|---|---|---|
| Fixed Effects | ||||
| Intercept | 4.849 | 0.697 | <0.001 | 0.118 |
| Time | −0.097 | 0.277 | 0.726 | 0.212 |
| Group Treatment (tx) | 0.189 | 0.200 | 0.344 | 0.001 |
| Online Treatment (tx) | −0.019 | 0.199 | 0.922 | 0.001 |
| Adolescent Age | −0.137 | 0.045 | 0.002 | 0.175 |
| Adolescent Sex | 0.075 | 0.157 | 0.634 | 0.113 |
| Adolescent zBMI | 0.115 | 0.157 | 0.462 | 0.160 |
| Family income | 0.047 | 0.160 | 0.771 | 0.148 |
| Parenting Style—Responsiveness | 0.289 | 0.220 | 0.188 | 0.002 |
| Parenting Style—Demandingness | 0.201 | 0.187 | 0.282 | 0.002 |
| Time: Responsiveness | −0.530 | 0.321 | 0.099 | 0.131 |
| Group tx: Responsiveness | −0.380 | 0.234 | 0.105 | 0.002 |
| Time: Group tx | −0.143 | 0.316 | 0.651 | 0.190 |
| Time: Demandingness | −0.068 | 0.307 | 0.824 | 0.222 |
| Group tx: Demandingness | 0.503 | 0.240 | 0.036 | 0.003 |
| Online tx: Responsiveness | 0.065 | 0.231 | 0.777 | 0.001 |
| Time: Online tx | 0.140 | 0.306 | 0.647 | 0.136 |
| Online tx: Demandingness | −0.317 | 0.240 | 0.187 | 0.002 |
| Time: Group tx: Responsiveness | 0.852 | 0.358 | 0.018 | 0.196 |
| Time: Group tx: Demandingness | −0.947 | 0.364 | 0.010 | 0.217 |
| Time: Online tx: Responsiveness | 0.056 | 0.345 | 0.871 | 0.159 |
| Time: Online tx: Demandingness | 0.405 | 0.351 | 0.249 | 0.164 |
| Random Effects | ||||
| Intercept | 0.000 | |||
| Group | 0.000 | |||
| Residual | 1.534 |
| Estimate | SE | p | FMI | |
|---|---|---|---|---|
| Fixed Effects | ||||
| Intercept | 4.853 | 0.732 | <0.001 | 0.162 |
| Time | −0.109 | 0.269 | 0.685 | 0.164 |
| Group Treatment (tx) | 0.097 | 0.204 | 0.636 | 0.002 |
| Online Treatment (tx) | 0.046 | 0.203 | 0.822 | 0.002 |
| Adolescent Age | −0.123 | 0.047 | 0.009 | 0.203 |
| Adolescent Sex | 0.08 | 0.165 | 0.629 | 0.169 |
| Adolescent zBMI | 0.043 | 0.161 | 0.792 | 0.167 |
| Family income | −0.032 | 0.159 | 0.84 | 0.118 |
| Feeding Practice—Restrict | 0.499 | 0.191 | 0.009 | 0.002 |
| Feeding Practice—Concern | −0.168 | 0.199 | 0.400 | 0.007 |
| Feeding Practice—Pressure to Eat | 0.053 | 0.193 | 0.784 | 0.002 |
| Time: Restrict | −0.68 | 0.332 | 0.042 | 0.307 |
| Group tx: Restrict | 0.004 | 0.242 | 0.986 | 0.001 |
| Time: Group tx | −0.071 | 0.319 | 0.825 | 0.192 |
| Online tx: Restrict | −0.284 | 0.241 | 0.239 | 0.00 |
| Time: Online tx | 0.075 | 0.306 | 0.807 | 0.12 |
| Time: Concern | 0.209 | 0.313 | 0.505 | 0.258 |
| Group tx: Concern | −0.091 | 0.223 | 0.685 | 0.002 |
| Online tx: Concern | 0.542 | 0.223 | 0.015 | 0.001 |
| Time: Pressure | −0.11 | 0.308 | 0.721 | 0.236 |
| Group tx: Pressure | −0.122 | 0.221 | 0.583 | 0.001 |
| Online tx: Pressure | −0.161 | 0.222 | 0.468 | 0.001 |
| Time: Group tx: Restrict | 0.248 | 0.367 | 0.500 | 0.151 |
| Time: Online tx: Restrict | 0.172 | 0.37 | 0.643 | 0.163 |
| Time: Group tx: Concern | −0.131 | 0.33 | 0.692 | 0.141 |
| Time: Online tx: Concern | −0.179 | 0.337 | 0.594 | 0.178 |
| Time: Group tx: Pressure | 0.06 | 0.373 | 0.872 | 0.289 |
| Time: Online tx: Pressure | 0.199 | 0.34 | 0.558 | 0.129 |
| Random Effects | ||||
| Intercept | 0.000 | |||
| Group | 0.000 | |||
| Residual | 1.540 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, D.K.; Sweeney, A.M.; Quattlebaum, M.; Loncar, H.; Kipp, C.; Brown, A. The Moderating Effects of the Families Improving Together (FIT) for Weight Loss Intervention and Parenting Factors on Family Mealtime in Overweight and Obese African American Adolescents. Nutrients 2021, 13, 1745. https://doi.org/10.3390/nu13061745
Wilson DK, Sweeney AM, Quattlebaum M, Loncar H, Kipp C, Brown A. The Moderating Effects of the Families Improving Together (FIT) for Weight Loss Intervention and Parenting Factors on Family Mealtime in Overweight and Obese African American Adolescents. Nutrients. 2021; 13(6):1745. https://doi.org/10.3390/nu13061745
Chicago/Turabian StyleWilson, Dawn K., Allison M. Sweeney, Mary Quattlebaum, Haylee Loncar, Colby Kipp, and Asia Brown. 2021. "The Moderating Effects of the Families Improving Together (FIT) for Weight Loss Intervention and Parenting Factors on Family Mealtime in Overweight and Obese African American Adolescents" Nutrients 13, no. 6: 1745. https://doi.org/10.3390/nu13061745








