Iodine Intake Estimated by 24 h Urine Collection in the Italian Adult Population: 2008–2012 Survey
Abstract
:1. Introduction
2. Materials and Methods
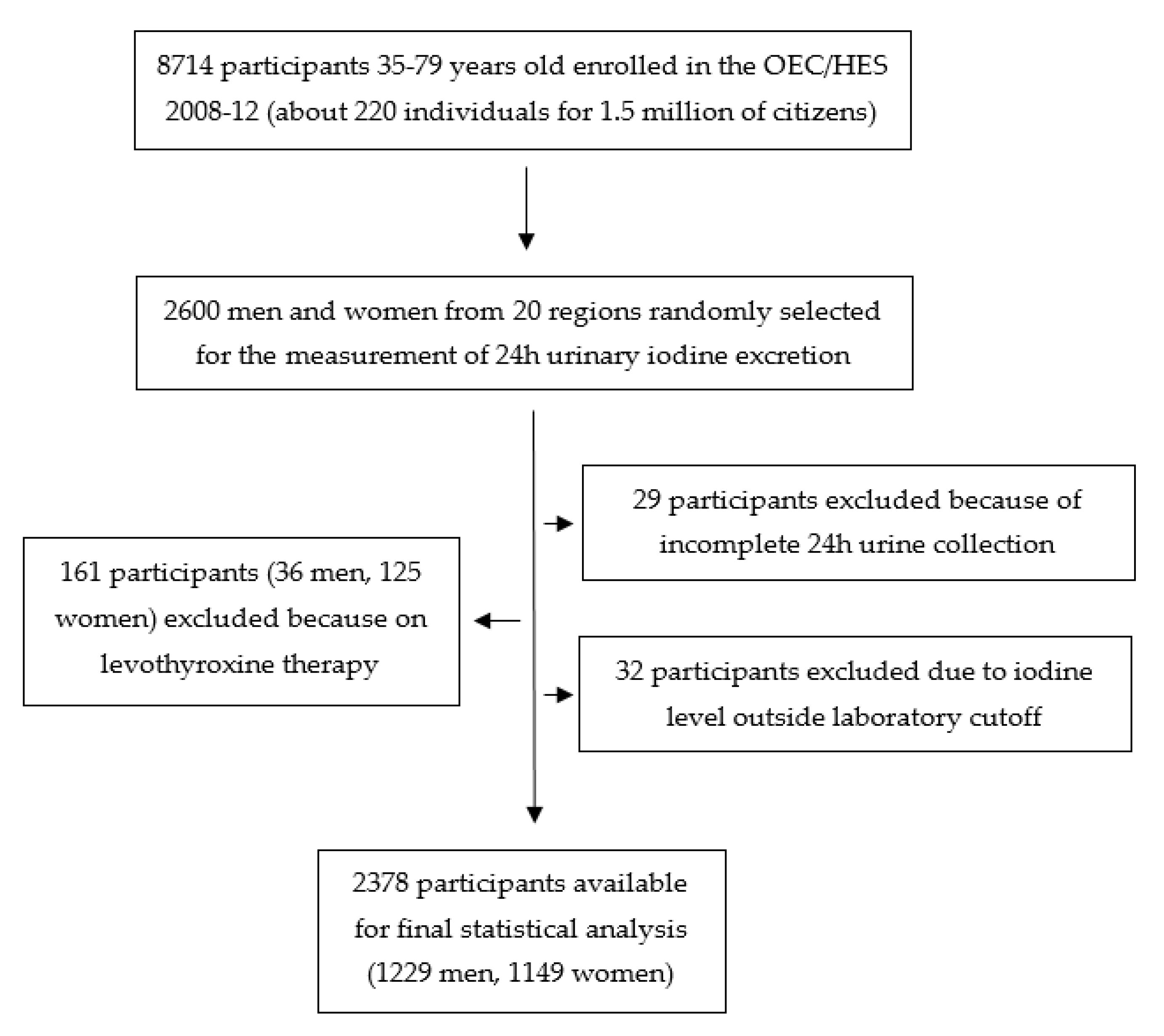
2.1. Study Population and Survey Protocol
2.2. Iodine Intake Assessment
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions and Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zimmermann, M.B. The effects of iodine deficiency in pregnancy and infancy. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. 1), 108–117. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Yen, P.M. Cellular Action of Thyroid Hormone (Updated 2018 June 20). In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Grossman, A., Hershman, J.M., Hofland, J., et al., Eds.; MDText.com Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK285568/ (accessed on 11 February 2021).
- Santiago-Fernandez, P.; Torres-Barahona, R.; Muela-Martínez, J.A.; Rojo-Martínez, G.; García-Fuentes, E.; Garriga, M.J.; Leòn, A.G.; Soriguer, F. Intelligence quotient and iodine intake: A cross-sectional study in children. J. Clin. Endocrinol. Metab. 2004, 89, 3851–3857. [Google Scholar] [CrossRef] [Green Version]
- Salarkin, N.; Mirmiran, P.; Azizi, F. Timing of the effect of iodine supplementation on intelligence quotient of schoolchildren. Int. J. Endocrinol. Metab. 2004, 2, 95–102. [Google Scholar]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- WHO. Urinary Iodine Concentrations for Determining Iodine Status Deficiency in Populations; Vitamin and Mineral Nutrition Information System; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/bitstream/handle/10665/85972/WHO_NMH_NHD_EPG_13.1_eng.pdf;jsessionid=BBB84CB1D7102320189EA52DFDCEF7B7?sequence=1 (accessed on 11 February 2021).
- Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; The National Academies Press: Washington, DC, USA, 2001; p. 264. [Google Scholar] [CrossRef] [Green Version]
- EFSA NDA Panel (EFSA Panel on Panel on Dietetic Products Nutrition and Allergies). Scientific Opinion on Dietary Reference Values for iodine. EFSA J. 2014, 12, 3660. Available online: https://efsa.onlinelibrary.wiley.com/doi/epdf/10.2903/j.efsa.2014.3660 (accessed on 11 February 2021).
- World Health Organization and Food and Agriculture Organization of the United Nations. Vitamin and Mineral Requirements in Human Nutrition: Report of a Joint FAO/WHO Expert Consultation, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004; Available online: https://apps.who.int/iris/bitstream/handle/10665/42716/9241546123.pdf (accessed on 11 February 2021).
- Vejbjerg, P.; Knudsen, N.; Perrild, H.; Laurberg, P.; Andersen, S.; Rasmussen, L.B.; Ovesen, L.; Jørgensen, T. Estimation of iodine intake from various urinary iodine measurements in population studies. Thyroid 2009, 19, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Remer, T.; Fonteyn, N.; Alexy, U.; Berkemeyer, S. Longitudinal examination of 24-h urinary iodine excretion in schoolchildren as a sensitive, hydration status-independent research tool for studying iodine status. Am. J. Clin. Nutr. 2006, 83, 639–646. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in populations: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef] [PubMed]
- The Iodine Global Network: 2019 Annual Report. Available online: https://www.ign.org/cm_data/2019_IGN_Annual_Report_051820.pdf (accessed on 11 February 2021).
- WHO Guideline: Fortification of Food-grade Salt with Iodine for the Prevention and Control of Iodine Deficiency Disorders; World Health Organization: Geneva, Switzerland, 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/136908/9789241507929_eng.pdf?ua=1 (accessed on 11 February 2021).
- WHO; UNICEF and ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination; World Health Organization: Geneva, Switzerland, 2007; Available online: https://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf (accessed on 11 February 2021).
- Olivieri, A.; Vitti, P.; Istituto Superiore di Sanità. Rapporti ISTISAN 14/6. Attività di monitoraggio del programma nazionale per la prevenzione dei disordini da carenza iodica. In Epidemiol. Sanità Pubblica; 2014; 6, pp. 1–113. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2375_allegato.pdf (accessed on 11 February 2021).
- D’Argenio, P.; Olivieri, A.; Rotondi, D.; Donfrancesco, C.; Giampaoli, S. La Raccomandazione “Meno Sale ma Iodato” è Realmente Condivisa dai Medici Italiani? Alcune Indicazioni Tratte da Un’indagine Online. Boll. Epidemiol. Naz. 2014, 27, 1–4. Available online: https://www.epicentro.iss.it/ben/2014/gennaio/1 (accessed on 11 February 2021).
- Giampaoli, S.; Palmieri, L.; Donfrancesco, C.; Lo Noce, C.; Pilotto, L.; Vanuzzo, D. Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey Research Group. Cardiovascular health in Italy. Ten-year surveillance of cardiovascular diseases and risk factors: Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey 1998–2012. Eur. J. Prev. Cardiol. 2015, 22 (Suppl. 1), 9–37. [Google Scholar]
- Donfrancesco, C.; Ippolito, R.; Lo Noce, C.; Palmieri, L.; Iacone, R.; Russo, O.; Vanuzzo, D.; Galletti, F.; Galeone, D.; Giampaoli, S.; et al. Excess dietary sodium and inadequate potassium intake in Italy: Results of the MINISAL study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 850–856. [Google Scholar] [CrossRef]
- Campanozzi, A.; Rutigliano, I.; Macchia, P.E.; De Filippo, G.; Barbato, A.; Iacone, R.; Russo, O.; D’Angelo, G.; Frigeri, M.; Pensabene, L.; et al. Iodine deficiency among Italian children and adolescents assessed through 24-hour urinary iodine excretion. Am. J. Clin. Nutr. 2019, 109, 1080–1087. [Google Scholar] [CrossRef]
- Olivieri, A.; Andò, S.; Bagnasco, M.; Meringolo, D.; Mian, C.; Moleti, M.; Puxeddu, E.; Regalbuto, C.; Taccaliti, A.; Tanda, M.L.; et al. The iodine nutritional status in the Italian population: Data from the Italian National Observatory for Monitoring Iodine Prophylaxis (OSNAMI) (period 2015–2019). Am. J. Clin. Nutr. 2019, 110, 1265–1266. [Google Scholar] [CrossRef]
- Aghini-Lombardi, F.; Antonangeli, L. Legislazione sulla iodoprofilassi in Italia [Iodine prophylaxis legislation in Italy]. Ann. Ist Super. Sanita. 1998, 34, 363–366. (In Italian) [Google Scholar] [PubMed]
- Vella, V. Goitre decline in Italy and contribution of the silent and active prophylaxis. Br. J. Nutr. 2005, 94, 818–824. [Google Scholar] [CrossRef] [Green Version]
- Censi, S.; Manso, J.; Barollo, S.; Mondin, A.; Bertazza, L.; De Marchi, M.; Mian, C. Changing Dietary Habits in Veneto Region over Two Decades: Still a Long Road to Go to Reach an Iodine-Sufficient Status. Nutrients 2020, 12, 2399. [Google Scholar] [CrossRef] [PubMed]
- Conte, L.; Comina, M.; Monti, E.; Sidoti, M.; Vannozzi, O.; Di Ciolo, L.; Lillo, F.; Giusti, M. Urinary Iodine Concentration in a Cohort of Adult Outpatients with Thyroid Diseases in Liguria 14 Years after the Law on Salt Iodization. Nutrients 2019, 12, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giordano, C.; Barone, I.; Marsico, S.; Bruno, R.; Bonofiglio, D.; Catalano, S.; Andò, S. Endemic Goiter and Iodine Prophylaxis in Calabria, a Region of Southern Italy: Past and Present. Nutrients 2019, 11, 2428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldini, E.; Virili, C.; D’Armiento, E.; Centanni, M.; Ulisse, S. Iodine Status in Schoolchildren and Pregnant Women of Lazio, a Central Region of Italy. Nutrients 2019, 11, 1647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Censi, S.; Watutantrige-Fernando, S.; Groccia, G.; Manso, J.; Plebani, M.; Faggian, D.; Mion, M.M.; Venturini, R.; Andrisani, A.; Casaro, A.; et al. The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area. Nutrients 2019, 11, 2639. [Google Scholar] [CrossRef] [Green Version]
- Watutantrige-Fernando, S.; Barollo, S.; Bertazza, L.; Cavedon, E.; Censi, S.; Manso, J.; Vianello, F. Efficacy of educational intervention to improve awareness of the importance of iodine, use of iodized salt, and dietary iodine intake in northeastern Italian schoolchildren. Nutrition 2018, 53, 134–139. [Google Scholar] [CrossRef]
- Olivieri, A.; Trimarchi, F.; Vitti, P. Global iodine nutrition 2020: Italy is an iodine sufficient country. J. Endocrinol. Investig. 2020, 43, 1671–1672. [Google Scholar] [CrossRef] [PubMed]
- Ittermann, T.; Albrecht, D.; Arohonka, P.; Bilek, R.; de Castro, J.J.; Dahl, L.; Nystrom, H.F.; Gaberscek, S.; Garcia-Fuentes, E.; Gheorghiu, M.L.; et al. Standardized Map of Iodine Status in Europe. Thyroid 2020, 30, 1346–1354. [Google Scholar] [CrossRef] [PubMed]
- Esche, J.; Thamm, M.; Remer, T. Contribution of iodized salt to total iodine and total salt intake in Germany. Eur. J. Nutr. 2020, 59, 3163–3169. [Google Scholar] [CrossRef] [PubMed]
- Dineva, M.; Rayman, M.P.; Bath, S.C. Iodine status of consumers of milk-alternative drinks versus cows’ milk: Data from the UK National Diet and Nutrition Survey. Br. J. Nutr. 2020, 30, 1–21. [Google Scholar] [CrossRef]
- Trofimiuk-Müldner, M.; Konopka, J.; Sokołowski, G.; Dubiel, A.; Kieć-Klimczak, M.; Kluczyński, Ł.; Motyka, M.; Rzepka, E.; Walczyk, J.; Sokołowska, M.; et al. Current iodine nutrition status in Poland (2017): Is the Polish model of obligatory iodine prophylaxis able to eliminate iodine deficiency in the population? Public Health Nutr. 2020, 23, 2467–2477. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Wu, Y.; Feng, X.X.; Ma, J.; Ma, Y.; Wang, H.; Zhang, J.; Yuan, J.; Lin, C.P.; Nowson, C.; et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): Cluster randomised controlled trial. BMJ 2015, 350, h770. [Google Scholar] [CrossRef] [Green Version]
- Aghini-Lombardi, F.; Antonangeli, L.; Vitti, P. Epidemiology of endemic goiter in Italy. Ann. Ist. Super. Sanita 1998, 34, 311–314. [Google Scholar]
- Donfrancesco, C.; Lo Noce, C.; Russo, O.; Minutoli, D.; Di Lonardo, A.; Profumo, E.; Buttari, B.; Iacone, R.; Vespasiano, F.; Vannucchi, S.; et al. Trend of salt intake measured by 24-h urine collection in the Italian adult population between the 2008 and 2018 CUORE Project surveys. NMCD 2020, 31, 814–826. [Google Scholar] [CrossRef]
- Leclercq, C.; Ferro-Luzzi, A. Total and Domestic Consumption of Salt and Their Determinants in Three Regions of Italy. Eur. J. Clin. Nutr. 1991, 45, 151–159. [Google Scholar]
- Iaccarino Idelson, P.; D’Elia, L.; Cairella, G.; Sabino, P.; Scalfi, L.; Fabbri, A.; Galletti, F.; Garbagnati, F.; Lionetti, L.; Paolella, G.; et al. Salt and Health: Survey on Knowledge and Salt Intake Related Behaviour in Italy. Nutrients 2020, 12, 279. [Google Scholar] [CrossRef] [Green Version]
- National Institute of Health Surveillance System PASSI—Progressi delle Aziende Sanitarie per la Salute in Italia. 2019. Available online: https://www.epicentro.iss.it/passi/dati/sale (accessed on 11 February 2021).
- Cappuccio, F.P.; Ji, C.; Donfrancesco, C.; Palmieri, L.; Ippolito, R.; Vanuzzo, D.; Giampaoli, S.; Strazzullo, P. Geographic and socioeconomic variation of sodium and potassium intake in Italy: Results from the MINISAL-GIRCSI programme. BMJ Open 2015, 5, e007467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perrine, C.G.; Cogswell, M.E.; Swanson, C.A.; Sullivan, K.M.; Chen, T.C.; Carriquiry, A.L.; Dodd, K.W.; Caldwell, K.L.; Wang, C.Y. Comparison of population iodine estimates from 24-hour urine and timed-spot urine samples. Thyroid 2014, 24, 748–757. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Wu, Y.; Lin, L.; Tan, L.; Shen, J.; Pearce, E.N.; Guo, X.; Wang, W.; Bian, J.; Jiang, W.; et al. 24-hour urine samples are more reproducible than spot urine samples for evaluation of iodine status in school-age children. J. Nutr. 2016, 146, 142–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernando, S.W.; Barollo, S.; Nacamulli, D.; Pozza, D.; Giachetti, M.; Frigato, F.; Redaelli, M.; Zagotto, G.; Girelli, M.E.; Mantero, F.; et al. Iodine status in schoolchildren living in northeast Italy: The importance of iodized-salt use and milk consumption. Eur. J. Clin. Nutr. 2013, 67, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Coccaro, C.; Tuccilli, C.; Prinzi, N.; D’Armiento, E.; Pepe, M.; Del Maestro, F.; Cacciola, G.; Forlini, B.; Verdolotti, S.; Bononi, M.; et al. Consumption of iodized salt may not represent a reliable indicator of iodine adequacy: Evidence from a cross-sectional study on schoolchildren living in an urban area of central Italy. Nutrition 2016, 32, 662–666. [Google Scholar] [CrossRef]
- Rasmussen, L.B.; Ovesen, L.; Christiansen, E. Day-to-day and within-day variation in urinary iodine excretion. Eur. J. Clin. Nutr. 1999, 53, 401–407. [Google Scholar] [CrossRef] [Green Version]
- König, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef]
| Basic Characteristics | Whole Population n = 2378 | Men n = 1229 (51.7%) | Women n = 1149 (48.3%) | p * |
|---|---|---|---|---|
| Age, y | 56 (46–67) | 56 (45–66) | 57 (46–67) | 0.247 |
| Weight, kg | 73.0 (62.8–83.0) | 79.2 (71.5–88.0) | 64.4 (57.6–74.2) | <0.001 |
| Height, cm | 164 (157–171) | 171.0 (165–176) | 158 (153–162) | <0.001 |
| BMI, Kg/m2 | 26.7 (24.0–30.2) | 27.1 (24.9–30.2) | 26.1 (23.0–30.2) | <0.001 |
| UIC, µg/L | 46 ** (23–88) | 55 ** (27–101) | 41 ** (20–72) | <0.001 |
| Urine volume, mL/24 h | 1900 (1500–2500) | 1900 (1450–2500) | 1950 (1500–2500) | 0.156 |
| DII, µg/d | 96 *** (51–165) | 111 *** (60–189) | 85 *** (43–140) | <0.001 |
| Whole Population | 35–44 y, n = 521 | 45–54 y, n = 570 | 55–64 y, n = 742 | 65–79 y, n = 545 |
|---|---|---|---|---|
| UIC, µg/L | 49 * (24–93) | 51 * (27–95) | 43 * (21–83) | 43 * (20–82) |
| DII, µg/d | 97 ** (52–160) | 106 ** (60–176) | 92 ** (49–164) | 90 ** (44–152) |
| Male participants | 35–44 y, n = 285 | 45–54 y, n = 291 | 55–64 y, n = 377 | 65–79 y, n = 276 |
| UIC, µg/L | 60 * (32–103) | 63 * (33–114) | 47 * (24–96) | 48 * (20–92) |
| DII, µg/d | 122 ** (65–192) | 127 ** (75–196) | 99 ** (56–183) | 95 ** (45–179) |
| Female participants | 35–44 y, n = 236 | 45–54 y, n = 279 | 55–64 y, n = 365 | 65–79 y, n = 269 |
| UIC, µg/L | 39 * (19–72) | 43 * (24–73) | 41 * (20–72) | 39 * (19–70) |
| DII, µg/d | 81 ** (39–128) | 91 ** (49–146) | 81 ** (41–144) | 84 ** (41–135) |
| Whole Population | BMI < 25 Kg/m2 | BMI 25–29.99 Kg/m2 | BMI ≥ 30 Kg/m2 |
| n = 806 | n = 950 | n = 622 | |
| UIC, µg/L | 43 * (23–77) | 46 * (22–87) | 53 * (25–98) |
| DII, µg/d | 90 ** (50–146) | 96 ** (48–167) | 106 ** (55–185) |
| Male Participants | BMI < 25 Kg/m2 | BMI 25–29.99 Kg/m2 | BMI ≥ 30 Kg/m2 |
| n = 329 | n = 575 | n = 325 | |
| UIC, µg/L | 49 * (25–89) | 50 * (26–100) | 68 * (30–110) |
| DII, µg/d | 100 ** (55–172) | 107 ** (60–188) | 125 ** (65–211) |
| Female Participants | BMI < 25 Kg/m2 | BMI 25–29.99 Kg/m2 | BMI ≥ 30 Kg/m2 |
| n = 477 | n = 375 | n = 297 | |
| UIC, µg/L | 40 * (21–67) | 39 * (18–71) | 44 * (22–82) |
| DII, µg/d | 84 ** (45–133) | 87 ** (39–141) | 83 ** (49–154) |
| Whole Population | Northern Italy | Central Italy | Southern Italy | p * |
| n = 1150 | n = 515 | n = 713 | ||
| UIC, µg/L | 45 ** (24–84) | 54 ** (26–91) | 43 ** (20–89) | 0.021 |
| DII, µg/d | 97 *** (55–158) | 109 *** (55–179) | 87 *** (44–165) | 0.002 |
| Male Participants | Northern Italy | Central Italy | Southern Italy | p * |
| n = 585 | n = 281 | n = 363 | ||
| UIC, µg/L | 51 ** (28–97) | 63 ** (31–114) | 47 ** (24–101) | 0.011 |
| DII, µg/d | 112 *** (62–185) | 131 *** (63–205) | 95 *** (52–181) | 0.005 |
| Female Participants | Northern Italy | Central Italy | Southern Italy | p * |
| n = 565 | n = 234 | n = 350 | ||
| UIC, µg/L | 42 ** (22–71) | 39 ** (21–70) | 40 ** (18–74) | 0.712 |
| DII, µg/d | 85 *** (48–141) | 89 *** (47–139) | 78 *** (38–137) | 0.209 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacone, R.; Iaccarino Idelson, P.; Formisano, P.; Russo, O.; Lo Noce, C.; Donfrancesco, C.; Macchia, P.E.; Palmieri, L.; Galeone, D.; di Lenarda, A.; et al. Iodine Intake Estimated by 24 h Urine Collection in the Italian Adult Population: 2008–2012 Survey. Nutrients 2021, 13, 1529. https://doi.org/10.3390/nu13051529
Iacone R, Iaccarino Idelson P, Formisano P, Russo O, Lo Noce C, Donfrancesco C, Macchia PE, Palmieri L, Galeone D, di Lenarda A, et al. Iodine Intake Estimated by 24 h Urine Collection in the Italian Adult Population: 2008–2012 Survey. Nutrients. 2021; 13(5):1529. https://doi.org/10.3390/nu13051529
Chicago/Turabian StyleIacone, Roberto, Paola Iaccarino Idelson, Pietro Formisano, Ornella Russo, Cinzia Lo Noce, Chiara Donfrancesco, Paolo Emidio Macchia, Luigi Palmieri, Daniela Galeone, Andrea di Lenarda, and et al. 2021. "Iodine Intake Estimated by 24 h Urine Collection in the Italian Adult Population: 2008–2012 Survey" Nutrients 13, no. 5: 1529. https://doi.org/10.3390/nu13051529






