Nutritional Status in Peritoneal Dialysis: Nutritional Guidelines, Adequacy and the Management of Malnutrition
Abstract
:1. Introduction
2. Epidemiology
3. Significance of Nutritional Status in PD
4. Biochemical and Clinical Markers of Malnutrition
5. Adequacy in Peritoneal Dialysis
6. Complications of Malnutrition in PD Patients
7. Nutritional Recommendations for Pediatric Patients Treated with Peritoneal Dialysis
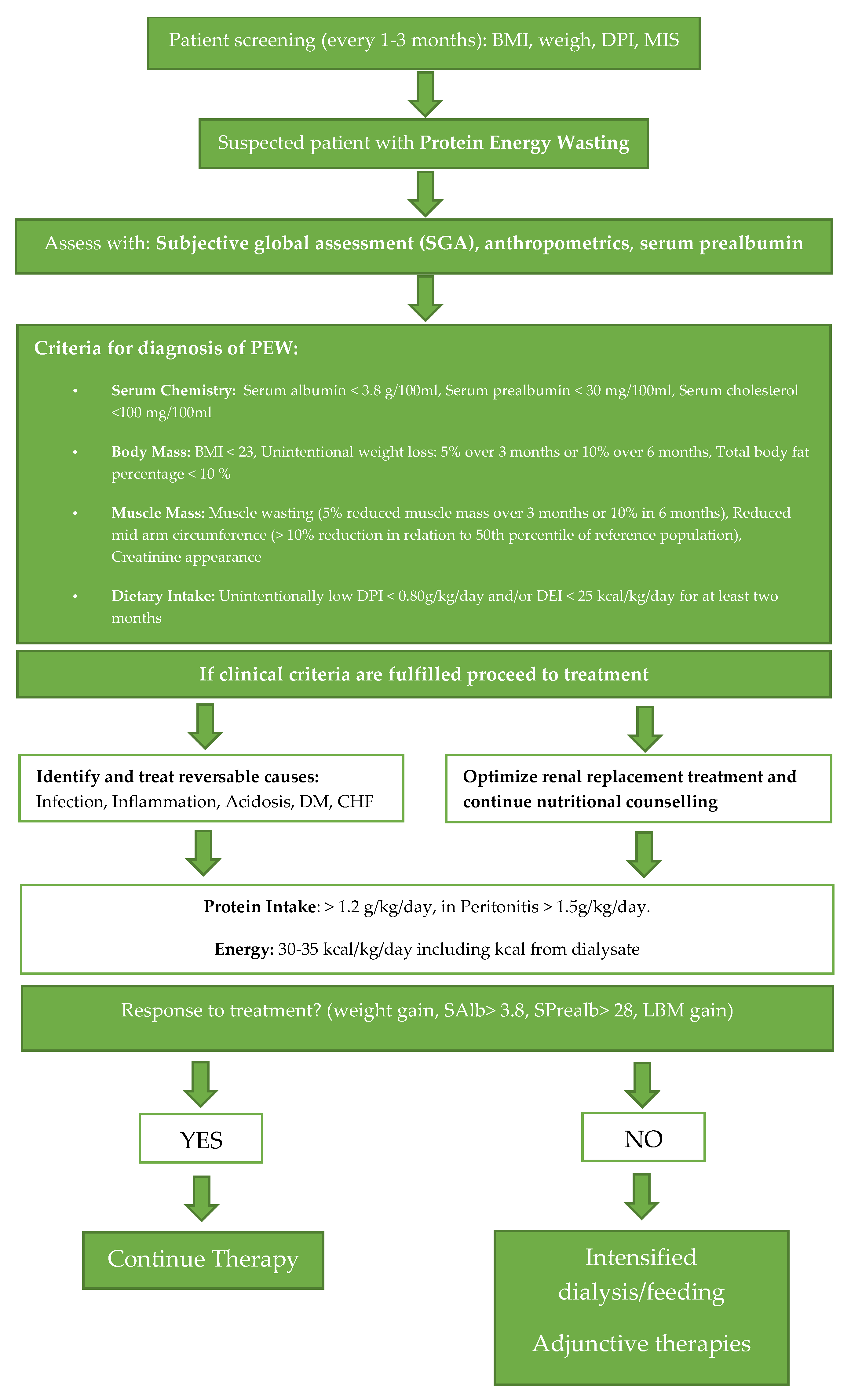
8. Nutritional Guidelines for PD Patients
9. Adjuvant Therapies
10. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Satirapoj, B.; Limwannata, P.; Kleebchaiyaphum, C.; Prapakorn, J.; Yatinan, U.; Chotsriluecha, S.; Supasyndh, O. Nutritional status among peritoneal dialysis patients after oral supplement with ONCE dialyze formula. Int. J. Nephrol. Renov. Dis. 2017, 10, 145–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piraino, B. Recommendations for dietary protein intake in CAPD patients. Adv. Perit. Dial. 1996, 12, 275–279. [Google Scholar] [PubMed]
- Kovesdy, C.P.; Kopple, J.D.; Kalantar-Zadeh, K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: Reconciling low protein intake with nutritional therapy. Am. J. Clin. Nutr. 2013, 97, 1163–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zha, Y.; Qian, Q. Protein Nutrition and Malnutrition in CKD and ESRD. Nutrients 2017, 9, 208. [Google Scholar] [CrossRef] [PubMed]
- Li, P.K.; Chow, K.M.; Van de Luijtgaarden, M.W.; Johnson, D.W.; Jager, K.J.; Mehrotra, R.; Naicker, S.; Pecoits-Filho, R.; Yu, X.Q.; Lameire, N. Changes in the worldwide epidemiology of peritoneal dialysis. Nat. Rev. Nephrol. 2017, 13, 90–103. [Google Scholar] [CrossRef] [PubMed]
- Lameire, N.; Van Biesen, W. Epidemiology of peritoneal dialysis: A story of believers and nonbelievers. Nat. Rev. Nephrol. 2010, 6, 75–82. [Google Scholar] [CrossRef]
- Polycystic Kidney Disease Foundation, Nutrition-Recommendations. Available online: https://pkdcure.org/living-with-pkd/nutrition/ (accessed on 14 March 2020).
- Council on Renal Nutrition, Nutrition and Peritoneal Dialysis. Available online: https://www.kidney.org/atoz/content/nutripd (accessed on 14 March 2020).
- Blake, P.G.; Bargman, J.M.; Brimble, K.S.; Davison, S.N.; Hirsch, D.; McCormick, B.B.; Suri, R.S.; Taylor, P.; Zalunardo, N.; Tonelli, M.; et al. Clinical Practice Guidelines and Recommendations on Peritoneal Dialysis Adequacy 2011. Perit. Dial. Int. 2011, 31, 218–239. [Google Scholar] [CrossRef]
- Ponton-Vazquez, C.; Vasquez-Garibay, E.M.; Hurtado-Lopez, E.F.; de la Torre Serrano, A.; Garcia, G.P.; Romero-Velarde, E. Dietary Intake, Nutritional Status, and Body Composition in Children With End-Stage Kidney Disease on Hemodialysis or Peritoneal Dialysis. J. Ren. Nutr. 2017, 27, 207–215. [Google Scholar] [CrossRef]
- Thuc, L.T.M.; Dung, N.Q.; Ha, V.N.; Tam, N.D.; Nga, N.T.H. Actual Diet and Nutritional Deficiencies Status in Children on Peritoneal Dialysis at the Vietnam National Hospital of Pediatrics. Saudi J. Kidney Dis. Transplant. 2019, 30, 924–931. [Google Scholar] [CrossRef]
- Martin-del-Campo, F.; Batis-Ruvalcaba, C.; Gonzalez-Espinoza, L.; Rojas-Campos, E.; Angel, J.R.; Ruiz, N.; Gonzalez, J.; Pazarin, L.; Cueto-Manzano, A.M. Dietary micronutrient intake in peritoneal dialysis patients: Relationship with nutrition and inflammation status. Perit. Dial. Int. 2012, 32, 183–191. [Google Scholar] [CrossRef] [Green Version]
- Johansson, L. Nutrition in Older Adults on Peritoneal Dialysis. Perit. Dial. Int. 2015, 35, 655–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kendrick, J.; Teitelbaum, I. Strategies for improving long-term survival in peritoneal dialysis patients. Clin. J. Am. Soc. Nephrol. 2010, 5, 1123–1131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Lopez, E.; Lindholm, B.; Davies, S. An update on peritoneal dialysis solutions. Nat. Rev. Nephrol. 2012, 8, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Choi, S.R.; Song, Y.S.; Yoon, S.Y.; Lee, S.Y.; Han, D.S. New insight of amino acid-based dialysis solutions. Kidney Int. Suppl. 2006, 70, S110–S114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tjiong, H.L.; Swart, R.; van den Berg, J.W.; Fieren, M.W. Amino Acid-based peritoneal dialysis solutions for malnutrition: New perspectives. Perit. Dial. Int. 2009, 29, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Tjiong, H.L.; Rietveld, T.; Wattimena, J.L.; van den Berg, J.W.; Kahriman, D.; van der Steen, J.; Hop, W.C.; Swart, R.; Fieren, M.W. Peritoneal dialysis with solutions containing amino acids plus glucose promotes protein synthesis during oral feeding. Clin. J. Am. Soc. Nephrol. 2007, 2, 74–80. [Google Scholar] [CrossRef] [Green Version]
- Kopple, J.D.; Bernard, D.; Messana, J.; Swartz, R.; Bergstrom, J.; Lindholm, B.; Lim, V.; Brunori, G.; Leiserowitz, M.; Bier, D.M.; et al. Treatment of malnourished CAPD patients with an amino acid based dialysate. Kidney Int. 1995, 47, 1148–1157. [Google Scholar] [CrossRef] [Green Version]
- Brulez, H.F.; van Guldener, C.; Donker, A.J.; ter Wee, P.M. The impact of an amino acid-based peritoneal dialysis fluid on plasma total homocysteine levels, lipid profile and body fat mass. Nephrol. Dial. Transplant. 1999, 14, 154–159. [Google Scholar] [CrossRef] [Green Version]
- Schmicker, R. Nutritional treatment of hemodialysis and peritoneal dialysis patients. Artif. Organs. 1995, 19, 837–841. [Google Scholar] [CrossRef]
- Davies, S.J.; Phillips, L.; Griffiths, A.M.; Russell, L.H.; Naish, P.F.; Russell, G.I. What really happens to people on long-term peritoneal dialysis? Kidney Int. 1998, 54, 2207–2217. [Google Scholar] [CrossRef] [Green Version]
- Burkart, J.M. Effect of peritoneal dialysis prescription and peritoneal membrane transport characteristics on nutritional status. Perit. Dial. Int. 1995, 15, S20–S35. [Google Scholar] [CrossRef]
- Han, S.H.; Han, D.S. Nutrition in patients on peritoneal dialysis. Nat. Rev. Nephrol. 2012, 8, 163–175. [Google Scholar] [CrossRef]
- Mehrotra, R. Nutritional issues in peritoneal dialysis patients: How do they differ from that of patients undergoing hemodialysis? J. Ren. Nutr. 2013, 23, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.C.; Bufarah, M.N.B.; Ponce, D.; Balbi, A. Longitudinal changes in nutritional parameters and resting energy expenditure in end-stage renal disease. J. Bras. Nefrol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Wang, T.; Wang, H.Y. The impact of new comorbidities on nutritional status in continuous ambulatory peritoneal dialysis patients. Blood Purif. 2006, 24, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Tennankore, K.K.; Bargman, J.M. Nutrition and the kidney: Recommendations for peritoneal dialysis. Adv. Chronic Kidney Dis. 2013, 20, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Szeto, C.C.; Wong, T.Y.; Chow, K.M.; Leung, C.B.; Li, P.K. Oral sodium bicarbonate for the treatment of metabolic acidosis in peritoneal dialysis patients: A randomized placebo-control trial. J. Am. Soc. Nephrol. 2003, 14, 2119–2126. [Google Scholar] [CrossRef] [Green Version]
- de Brito-Ashurst, I.; Varagunam, M.; Raftery, M.J.; Yaqoob, M.M. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J. Am. Soc. Nephrol. 2009, 20, 2075–2084. [Google Scholar] [CrossRef] [Green Version]
- Tian, X.K.; Shan, Y.S.; Zhe, X.W.; Cheng, L.T.; Wang, T. Metabolic acidosis in peritoneal dialysis patients: The role of residual renal function. Blood Purif. 2005, 23, 459–465. [Google Scholar] [CrossRef]
- Szeto, C.C.; Chow, K.M. Metabolic acidosis and malnutrition in dialysis patients. Semin. Dial. 2004, 17, 371–375. [Google Scholar] [CrossRef]
- Vanholder, R.; Glorieux, G.; Lameire, N. The other side of the coin: Impact of toxin generation and nutrition on the uremic syndrome. Semin. Dial. 2002, 15, 311–314. [Google Scholar] [CrossRef]
- Dhondt, A.; Vanholder, R.; Van Biesen, W.; Lameire, N. The removal of uremic toxins. Kidney Int. Suppl. 2000, 76, S47–S59. [Google Scholar] [CrossRef] [Green Version]
- Ondrussek-Sekac, M.; Navas-Carrillo, D.; Orenes-Pinero, E. Intestinal microbiota alterations in chronic kidney disease and the influence of dietary components. Crit. Rev. Food Sci. Nutr. 2020, 1–13. [Google Scholar] [CrossRef]
- Kirsch, R.; Frith, L.; Black, E.; Hoffenberg, R. Regulation of albumin synthesis and catabolism by alteration of dietary protein. Nature 1968, 217, 578–579. [Google Scholar] [CrossRef]
- Bharadwaj, S.; Ginoya, S.; Tandon, P.; Gohel, T.D.; Guirguis, J.; Vallabh, H.; Jevenn, A.; Hanouneh, I. Malnutrition: Laboratory markers vs nutritional assessment. Gastroenterol. Rep. 2016, 4, 272–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabrerizo, S.; Cuadras, D.; Gomez-Busto, F.; Artaza-Artabe, I.; Marin-Ciancas, F.; Malafarina, V. Serum albumin and health in older people: Review and meta analysis. Maturitas 2015, 81, 17–27. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pupim, L.B. Assessment of Protien and Energy Nutritional Status. In Nutritional Managment of Renal Disease; Academic Press: Cambridge, MA, USA, 2013; pp. 137–158. [Google Scholar] [CrossRef]
- Ikizler, T.A. The use and misuse of serum albumin as a nutritional marker in kidney disease. Clin. J. Am. Soc. Nephrol. 2012, 7, 1375–1377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiber, A.L.; Kalantar-Zadeh, K.; Secker, D.; McCarthy, M.; Sehgal, A.; McCann, L. Subjective Global Assessment in chronic kidney disease: A review. J. Ren. Nutr. 2004, 14, 191–200. [Google Scholar] [CrossRef]
- Yun, T.; Ko, Y.E.; Kim, S.J.; Kang, D.H.; Choi, K.B.; Oh, H.J.; Ryu, D.R. The additional benefit of weighted subjective global assessment (SGA) for the predictability of mortality in incident peritoneal dialysis patients: A prospective study. Medicine 2017, 96, e8421. [Google Scholar] [CrossRef] [PubMed]
- Tapiawala, S.; Vora, H.; Patel, Z.; Badve, S.; Shah, B. Subjective global assessment of nutritional status of patients with chronic renal insufficiency and end stage renal disease on dialysis. J. Assoc. Physicians India 2006, 54, 923–926. [Google Scholar] [PubMed]
- Lopes, A.A. The malnutrition-inflammation score: A valid nutritional tool to assess mortality risk in kidney transplant patients. Am. J. Kidney Dis. 2011, 58, 7–9. [Google Scholar] [CrossRef]
- Bigogno, F.G.; Fetter, R.L.; Avesani, C.M. Applicability of subjective global assessment and malnutrition inflammation score in the assessment of nutritional status on chronic kidney disease. J. Bras. Nefrol. 2014, 36, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Kopple, J.D. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am. J. Kidney Dis. 2001, 37, S66–S70. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, K.; Schwermer, K.; Kawka, A.; Klysz, P.; Baum, E.; Kaluzna, M.; Sikorska, D.; Scigacz, A.; Lindholm, B.; Pawlaczyk, K.; et al. Dialysis vintage stratified comparison of body composition, hydration and nutritional state in peritoneal dialysis and hemodialysis patients. Arch. Med. Sci. 2018, 14, 807–817. [Google Scholar] [CrossRef] [Green Version]
- Akbulut, G.; Sanlier, N.; Inal, S.; Tek, N.A.; Onec, K.; Erten, Y. Daily dietary energy and macronutrient intake and anthropometric measurements of the peritoneal dialysis patients. Ren. Fail. 2013, 35, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Edefonti, A.; Picca, M.; Damiani, B.; Garavaglia, R.; Loi, S.; Ardissino, G.; Marra, G.; Ghio, L. Prevalence of malnutrition assessed by bioimpedance analysis and anthropometry in children on peritoneal dialysis. Perit. Dial. Int. 2001, 21, 172–179. [Google Scholar] [CrossRef]
- Vanholder, R.C.; Ringoir, S.M. Adequacy of dialysis: A critical analysis. Kidney Int. 1992, 42, 540–558. [Google Scholar] [CrossRef] [Green Version]
- Owen, W.F., Jr.; Lew, N.L.; Liu, Y.; Lowrie, E.G.; Lazarus, J.M. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N. Engl. J. Med. 1993, 329, 1001–1006. [Google Scholar] [CrossRef]
- Lew, S.Q. Maintaining Peritoneal Dialysis Adequacy: The Process of Incremental Prescription. Adv. Perit. Dial. 2018, 34, 10–14. [Google Scholar]
- Rocco, M.; Soucie, J.M.; Pastan, S.; McClellan, W.M. Peritoneal dialysis adequacy and risk of death. Kidney Int. 2000, 58, 446–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hemayati, R.; Lesanpezeshki, M.; Seifi, S. Association of dialysis adequacy with nutritional and inflammatory status in patients with chronic kidney failure. Saudi J. Kidney Dis. Transplant. 2015, 26, 1154–1160. [Google Scholar] [CrossRef] [PubMed]
- Bieber, S.; Mehrotra, R. Peritoneal Dialysis Access Associated Infections. Adv. Chronic Kidney Dis. 2019, 26, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Naeeni, A.E.; Poostiyan, N.; Teimouri, Z.; Mortazavi, M.; Soghrati, M.; Poostiyan, E.; Paknahad, Z. Assessment of Severity of Malnutrition in Peritoneal Dialysis Patients via Malnutrition: Inflammatory Score. Adv. Biomed. Res. 2017, 6, 128. [Google Scholar] [CrossRef]
- Jadeja, Y.P.; Kher, V. Protein energy wasting in chronic kidney disease: An update with focus on nutritional interventions to improve outcomes. Indian J. Endocrinol. Metab. 2012, 16, 246–251. [Google Scholar] [CrossRef]
- van Diepen, A.T.; Jassal, S.V. A qualitative systematic review of the literature supporting a causal relationship between exit-site infection and subsequent peritonitis in patients with end-stage renal disease treated with peritoneal dialysis. Perit. Dial. Int. 2013, 33, 604–610. [Google Scholar] [CrossRef] [Green Version]
- van Diepen, A.T.; Tomlinson, G.A.; Jassal, S.V. The association between exit site infection and subsequent peritonitis among peritoneal dialysis patients. Clin. J. Am. Soc. Nephrol. 2012, 7, 1266–1271. [Google Scholar] [CrossRef] [Green Version]
- Kerschbaum, J.; Konig, P.; Rudnicki, M. Risk factors associated with peritoneal-dialysis-related peritonitis. Int. J. Nephrol. 2012, 2012, 483250. [Google Scholar] [CrossRef] [Green Version]
- Ma, X.; Shi, Y.; Tao, M.; Jiang, X.; Wang, Y.; Zang, X.; Fang, L.; Jiang, W.; Du, L.; Jin, D.; et al. Analysis of risk factors and outcome in peritoneal dialysis patients with early-onset peritonitis: A multicentre, retrospective cohort study. BMJ Open 2020, 10, e029949. [Google Scholar] [CrossRef] [Green Version]
- Ozturk, S.; Soyluk, O.; Karakaya, D.; Yazici, H.; Caliskan, Y.K.; Yildiz, A.; Bozfakioglu, S. Is decline in serum albumin an ominous sign for subsequent peritonitis in peritoneal dialysis patients? Adv. Perit. Dial. 2009, 25, 172–177. [Google Scholar]
- Prasad, N.; Gupta, A.; Sharma, R.K.; Sinha, A.; Kumar, R. Impact of nutritional status on peritonitis in CAPD patients. Perit. Dial. Int. 2007, 27, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Katona, P.; Katona-Apte, J. The interaction between nutrition and infection. Clin. Infect. Dis. 2008, 46, 1582–1588. [Google Scholar] [CrossRef]
- McCarthy, D.O.; Kluger, M.J.; Vander, A.J. Suppression of food intake during infection: Is interleukin-1 involved? Am. J. Clin. Nutr. 1985, 42, 1179–1182. [Google Scholar] [CrossRef] [PubMed]
- Tonbul, H.Z.; Demir, M.; Altintepe, L.; Guney, I.; Yeter, E.; Turk, S.; Yeksan, M.; Yildiz, A. Malnutrition-inflammation-atherosclerosis (MIA) syndrome components in hemodialysis and peritoneal dialysis patients. Ren. Fail. 2006, 28, 287–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahab, I.; Nolph, K.D. MIA syndrome in peritoneal dialysis: Prevention and treatment. Contrib. Nephrol. 2006, 150, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Maraj, M.; Kusnierz-Cabala, B.; Dumnicka, P.; Gala-Bladzinska, A.; Gawlik, K.; Pawlica-Gosiewska, D.; Zabek-Adamska, A.; Mazur-Laskowska, M.; Ceranowicz, P.; Kuzniewski, M. Malnutrition, Inflammation, Atherosclerosis Syndrome (MIA) and Diet Recommendations among End-Stage Renal Disease Patients Treated with Maintenance Hemodialysis. Nutrients 2018, 10, 69. [Google Scholar] [CrossRef] [Green Version]
- Altieri, P.; Sau, G.; Cao, R.; Barracca, A.; Menneas, A.; Micchittu, B.; Cabiddu, G.; Esposito, P.; Pani, A. Immunosuppressive treatment in dialysis patients. Nephrol. Dial. Transplant. 2002, 17 (Suppl. S8), 2–9. [Google Scholar] [CrossRef] [Green Version]
- Hurley, K.M.; Yousafzai, A.K.; Lopez-Boo, F. Early Child Development and Nutrition: A Review of the Benefits and Challenges of Implementing Integrated Interventions. Adv. Nutr. 2016, 7, 357–363. [Google Scholar] [CrossRef] [Green Version]
- Silverstein, D.M. Growth and Nutrition in Pediatric Chronic Kidney Disease. Front. Pediatr. 2018, 6, 205. [Google Scholar] [CrossRef] [Green Version]
- Paglialonga, F.; Edefonti, A. Nutrition assessment and management in children on peritoneal dialysis. Pediatr. Nephrol. 2009, 24, 721–730. [Google Scholar] [CrossRef] [Green Version]
- Nutrition for Your Child on Peritoneal Dialysis. Available online: https://www.niddk.nih.gov/health-information/kidney-disease/children/caring-child-kidney-disease/nutrition-chronic-kidney-disease#nutrition (accessed on 18 April 2020).
- Nutrition for Your Child on Peritoneal Dialysis. Available online: https://www.seattlechildrens.org/pdf/PE105.pdf (accessed on 18 April 2020).
- Nguyen, L.; Levitt, R.; Mak, R.H. Practical Nutrition Management of Children with Chronic Kidney Disease. Clin. Med. Insights Urol. 2016, 9. [Google Scholar] [CrossRef]
- Foundation, N.K. KDOQI Clinical Practice Guideline for Nutrition in Children with CKD:2008 Update. Am. J. Kidney Dis. 2009, 53, S11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canepa, A.; Carrea, A.; Caridi, G.; Dertenois, L.; Minniti, G.; Cerone, R.; Canini, S.; Calevo, M.G.; Perfumo, F. Homocysteine, folate, vitamin B12 levels, and C677T MTHFR mutation in children with renal failure. Pediatr. Nephrol. 2003, 18, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, A.; Keles, F.; Ozdemir, G.; Kosger, P.; Ucar, B.; Alatas, O.; Kilic, Z. Homocysteine levels in normotensive children of hypertensive parents. Anatol. J. Cardiol. 2015, 15, 1008–1013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locatelli, F.; Fouque, D.; Heimburger, O.; Drueke, T.B.; Cannata-Andia, J.B.; Horl, W.H.; Ritz, E. Nutritional status in dialysis patients: A European consensus. Nephrol. Dial. Transplant. 2002, 17, 563–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ketteler, M.; Block, G.A.; Evenepoel, P.; Fukagawa, M.; Herzog, C.A.; McCann, L.; Moe, S.M.; Shroff, R.; Tonelli, M.A.; Toussaint, N.D.; et al. Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: What’s changed and why it matters. Kidney Int. 2017, 92, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Wheeler, D.C.; Winkelmayer, W.C. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar]
- Ikizler, T.A.; Cano, N.J.; Franch, H.; Fouque, D.; Himmelfarb, J.; Kalantar-Zadeh, K.; Kuhlmann, M.K.; Stenvinkel, P.; TerWee, P.; Teta, D.; et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: A consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013, 84, 1096–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amalia, R.I.; Davenport, A. Estimated dietary sodium intake in peritoneal dialysis patients using food frequency questionnaires and total urinary and peritoneal sodium losses and assessment of extracellular volumes. Eur. J. Clin. Nutr. 2019, 73, 105–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cases, A.; Cigarran-Guldris, S.; Mas, S.; Gonzalez-Parra, E. Vegetable-Based Diets for Chronic Kidney Disease? It Is Time to Reconsider. Nutrients 2019, 11, 1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cupisti, A.; D’Alessandro, C.; Finato, V.; Del Corso, C.; Catania, B.; Caselli, G.M.; Egidi, M.F. Assessment of physical activity, capacity and nutritional status in elderly peritoneal dialysis patients. BMC Nephrol. 2017, 18, 180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguilera, A.; Cirugeda, A.; Amair, R.; Sansone, G.; Alegre, L.; Codoceo, R.; Bajo, M.A.; del Peso, G.; Diez, J.J.; Sanchez-Tomero, J.A.; et al. Ghrelin plasma levels and appetite in peritoneal dialysis patients. Adv. Perit. Dial. 2004, 20, 194–199. [Google Scholar] [PubMed]
- Cummings, D.E.; Purnell, J.Q.; Frayo, R.S.; Schmidova, K.; Wisse, B.E.; Weigle, D.S. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 2001, 50, 1714–1719. [Google Scholar] [CrossRef] [Green Version]
- Yeh, S.S.; Marandi, M.; Thode, H.C., Jr.; Levine, D.M.; Parker, T.; Dixon, T.; Schuster, M.W. Report of a pilot, double-blind, placebo-controlled study of megestrol acetate in elderly dialysis patients with cachexia. J. Ren. Nutr. 2010, 20, 52–62. [Google Scholar] [CrossRef]
- Evans, W.J. Editorial: Megestrol acetate use for weight gain should be carefully considered. J. Clin. Endocrinol. Metab. 2007, 92, 420–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Protein | Calcium | Phosphorus | Sodium | Potassium | |
|---|---|---|---|---|---|
| PDK | 1.2–1.4 g/kg | 1000 mg | ≥1200 mg | 2000–3000 mg | None |
| KDIGO | None | 1000–1200 mg | <4000 mg | None | |
| Europe | ≥1.2 g/kg | None | |||
| Canada | None | ||||
| Society | Recommendation |
|---|---|
| KDIGO [7,8] | Restriction of dietary calcium binders in all stages of chronic kidney disease without limitations |
| Phytate consumption: anti-oxidant and anti-cancer properties, ability to hinder nutrient absorption | |
| Importance of minimizing hyperphosphatemia in patients through the ingestion of food additives to an upper tolerable limit of 4000 mg (3000 in those >70 years of age) | |
| Lack of data which associates dietary restrictions to improved outcomes in patients with stage G3A-G4 chronic renal disease | |
| PKD Foundation [7] | Maintaining blood calcium levels between 8.4 and 9.5 mg/dL |
| Phosphorus in the diet may be restricted if blood levels reach greater than 5.0 mg/dL | |
| National Kidney Foundation [8] | Phosphorus in the diet may be restricted if blood levels reach greater than 5.0 mg/dL |
| Canadian Guidelines [9] | Reduce levels of sodium, phosphorus and fluids |
| Increase intake of potassium and protein | |
| Patient’s following a potassium restricted diet should limit their intake to 2000 milligrams per day, in constant to the standard recommendation of 3500 to 4500 milligrams daily for healthy patients |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiebalo, T.; Holotka, J.; Habura, I.; Pawlaczyk, K. Nutritional Status in Peritoneal Dialysis: Nutritional Guidelines, Adequacy and the Management of Malnutrition. Nutrients 2020, 12, 1715. https://doi.org/10.3390/nu12061715
Kiebalo T, Holotka J, Habura I, Pawlaczyk K. Nutritional Status in Peritoneal Dialysis: Nutritional Guidelines, Adequacy and the Management of Malnutrition. Nutrients. 2020; 12(6):1715. https://doi.org/10.3390/nu12061715
Chicago/Turabian StyleKiebalo, Thomas, Jacqueline Holotka, Ireneusz Habura, and Krzysztof Pawlaczyk. 2020. "Nutritional Status in Peritoneal Dialysis: Nutritional Guidelines, Adequacy and the Management of Malnutrition" Nutrients 12, no. 6: 1715. https://doi.org/10.3390/nu12061715





