Clinical Profiles, Survival, and Lung Function Outcomes in ANCA-Associated Interstitial Lung Disease: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Survival and Functional Outcomes
2.3. Statistical Analysis
3. Results
3.1. Baseline Clinical Characteristics of the ILD-ANCA Population
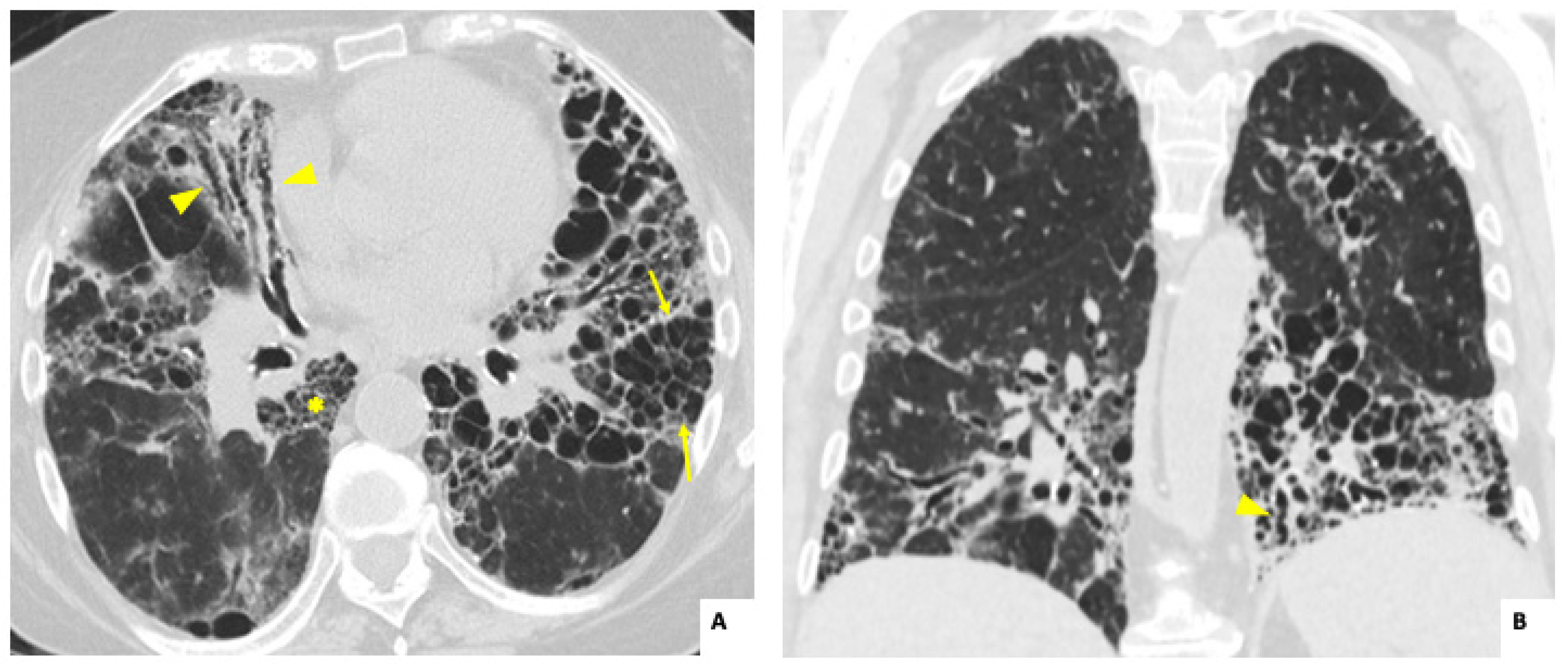
3.2. Radiological and Lung Function Findings
3.3. Treatment Administered
3.4. Pulmonary Function Outcomes During Follow-Up
3.5. Survival and Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allard-Chamard, H.; Liang, P. Antineutrophil Cytoplasmic Antibodies Testing and Interpretation. Clin. Lab. Med. 2019, 39, 539–552. [Google Scholar] [CrossRef]
- Jennette, J.C.; Falk, R.J. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 2013, 65, 1–11. [Google Scholar] [CrossRef]
- Thompson, G.E.; Specks, U. Update on the Management of Respiratory Manifestations of the Antineutrophil Cytoplasmic Antibodies-Associated Vasculitides. Clin. Chest Med. 2019, 40, 573–582. [Google Scholar] [CrossRef]
- Kadura, S.; Raghu, G. Antineutrophil cytoplasmic antibody-associated interstitial lung disease: A review. Eur. Respir. Rev. 2021, 30, 210123. [Google Scholar] [CrossRef]
- Shen, H.C.; Bui, K.A. Comparison of Interstitial Lung Disease Between Antineutrophil Cytoplasmic Antibodies Positive and Negative Patients: A Retrospective Cohort Study. ACR Open Rheumatol. 2024, 6, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Kagiyama, N.; Takayanagi, N. Antineutrophil cytoplasmic antibody-positive conversion and microscopic polyangiitis development in patients with idiopathic pulmonary fibrosis. BMJ Open Respir. Res. 2015, 2, e000058. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, J.; Yoshizawa, S. Acute exacerbation in antineutrophil cytoplasmic antibody-associated interstitial lung disease: Clinical features and risk factors. Respir. Med. 2022, 203, 106992. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Peng, M. Clinical features and long-term outcomes of interstitial lung disease with anti-neutrophil cytoplasmic antibody. BMC Pulm. Med. 2021, 21, 88. [Google Scholar] [CrossRef] [PubMed]
- Sebastiani, M.; Manfredi, A. Epidemiology and management of interstitial lung disease in ANCA-associated vasculitis. Clin. Exp. Rheumatol. 2020, 38 (Suppl. S124), 221–231. [Google Scholar] [PubMed]
- Doliner, B.; Rodriguez, K. Interstitial lung disease in ANCA-associated vasculitis: Associated factors, radiographic features and mortality. Rheumatology 2023, 62, 716–725. [Google Scholar] [CrossRef]
- Raghu, G.; Remy-Jardin, M. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2018, 198, e44–e68. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Antoniou, K.M. “ERS/ATS Task Force on Undifferentiated Forms of CTD-ILD”. An official European Respiratory Society/American Thoracic Society research statement: Interstitial pneumonia with autoimmune features. Eur. Respir. J. 2015, 46, 976–987. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Chai, D. Patterns of lung diseases predict survival in patients with MPO-ANCA-associated vasculitis: A single-center retrospective study. Clin. Rheumatol. 2022, 41, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Maillet, T.; Goletto, T. Usual interstitial pneumonia in ANCA-associated vasculitis: A poor prognostic factor. J. Autoimmun. 2020, 106, 102338. [Google Scholar] [CrossRef]
- Zhou, P.; Li, Z. Pulmonary involvement of ANCA-associated vasculitis in adult Chinese patients. BMC Pulm. Med. 2022, 22, 35. [Google Scholar] [CrossRef]
- Comarmond, C.; Crestani, B. Pulmonary fibrosis in antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitis: A series of 49 patients and review of the literature. Medicine 2014, 93, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, T.; Faguer, S. HRCT imaging of pulmonary involvement in granulomatosis with polyangiitis and microscopic polyangiitis at disease onset and during follow-up. Semin. Arthritis Rheum. 2023, 63, 152307. [Google Scholar] [CrossRef]
- Takakuwa, Y.; Yamasaki, Y. Long-term survival, causes of death, and prognostic factors for mortality in patients with microscopic polyangiitis and those with anti-neutrophil cytoplasmic antibody-positive interstitial lung disease: A single-center retrospective study. Int. J. Rheum. Dis. 2023, 26, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.W.; Pyo, J.Y. Incidence and Patterns of Interstitial Lung Disease and Their Clinical Impact on Mortality in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis: Korean Single-Centre Observational Study. J. Immunol. Res. 2022, 2022, 2499404. [Google Scholar] [CrossRef]
- Manfredi, A.; Cassone, G. Interstitial lung disease in microscopic polyangiitis and granulomatosis with polyangiitis: Demographic, clinical, serological and radiological features of an Italian cohort from the Italian Society for Rheumatology. Clin. Exp. Rheumatol. 2023, 41, 821–828. [Google Scholar] [CrossRef]
- Yildirim Dogan, H.G.; Yildirim, F. Pulmonary involvement in antineutrophil cytoplasmic antibody-associated vasculitides: A single center experience from Turkey. Int. J. Rheum. Dis. 2023, 26, 1495–1503. [Google Scholar] [CrossRef] [PubMed]
- Sada, K.E.; Yamamura, M. Research Committee on Intractable Vasculitides, the Ministry of Health, Labour and Welfare of Japan. Classification and characteristics of Japanese patients with antineutrophil cytoplasmic antibody-associated vasculitis in a nationwide, prospective, inception cohort study. Arthritis Res. Ther. 2014, 16, R101. [Google Scholar] [CrossRef]
- Matsuda, S.; Kotani, T. Evaluation of poor prognostic factors of respiratory related death in microscopic polyangiitis complicated by interstitial lung disease. Sci. Rep. 2021, 11, 1490. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Zhang, Y. Clinical significance of acute exacerbation in interstitial lung disease with antineutrophil cytoplasmic antibody: An indicator of poor prognosis. Ther. Adv. Respir. Dis. 2022, 16, 17534666221140974. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.Y.; Ventura, I.B. Prevalence and Clinical Significance of Antineutrophil Cytoplasmic Antibodies in North American Patients with Idiopathic Pulmonary Fibrosis. Chest 2019, 156, 715–723. [Google Scholar] [CrossRef]
- Hozumi, H.; Oyama, Y. Clinical significance of myeloperoxidase-anti-neutrophil cytoplasmic antibody in idiopathic interstitial pneumonias. PLoS ONE 2018, 13, e0199659. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, S.; Suzuki, A. Outcomes and prognosis of progressive pulmonary fibrosis in patients with antineutrophil cytoplasmic antibody-positive interstitial lung disease. Sci. Rep. 2023, 13, 17616. [Google Scholar] [CrossRef] [PubMed]
- Nozu, T.; Kondo, M. A comparison of the clinical features of ANCA-positive and ANCA-negative idiopathic pulmonary fibrosis patients. Respiration 2009, 77, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kim, H.C. Progression to ANCA-associated vasculitis in patients with idiopathic interstitial pneumonia and positive ANCA. Semin. Arthritis Rheum. 2024, 68, 152484. [Google Scholar] [CrossRef]
- Yamakawa, H.; Sato, S. Prognostic value of radiological findings indeterminate for UIP pattern and anterior upper lobe honeycomb-like lesion in chronic fibrosing interstitial lung disease associated with MPO-ANCA. BMC Pulm. Med. 2021, 21, 346. [Google Scholar] [CrossRef] [PubMed]
- Guilpain, P.; Chéreau, C. The oxidation induced by antimyeloperoxidase antibodies triggers fibrosis in microscopic polyangiitis. Eur. Respir. J. 2011, 37, 1503–1513. [Google Scholar] [CrossRef] [PubMed]
- Hirayama, K.; Kobayashi, M. Pulmonary involvements of anti-neutrophil cytoplasmic autoantibody-associated renal vasculitis in Japan. Nephrol. Dial. Transplant. 2015, 30 (Suppl. S1), i83–i93. [Google Scholar] [CrossRef] [PubMed]
- Fan, M.; Li, P. Development of a novel predictive model for interstitial lung disease in ANCA-associated vasculitis prognostications within the Chinese population. Medicine 2024, 103, e37048. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Yamaguchi, A. Interstitial lung disease with myeloperoxidase antineutrophil cytoplasmic antibody-associated vasculitis in elderly patients. Rheumatol. Int. 2021, 41, 1641–1650. [Google Scholar] [CrossRef] [PubMed]
- Hosoda, C.; Baba, T.; Hagiwara, E.; Ito, H.; Matsuo, N.; Kitamura, H.; Iwasawa, T.; Okudela, K.; Takemura, T.; Ogura, T. Clinical features of usual interstitial pneumonia with anti-neutrophil cytoplasmic antibody in comparison with idiopathic pulmonary fibrosis. Respirology 2016, 21, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Yamakawa, H.; Toyoda, Y. Anti-Inflammatory and/or Anti-Fibrotic Treatment of MPO-ANCA-Positive Interstitial Lung Disease: A Short Review. J. Clin. Med. 2022, 11, 3835. [Google Scholar] [CrossRef] [PubMed]


| Baseline Characteristics | All Patients (n = 23) | Isolated ANCA-ILD (n = 13) | AAV-ILD (n = 10; 5 MPA, 3 GPA, 2 EGPA) | p-Value |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Female, n (%) | 16 (69.6) | 8 (61.5) | 8 (80) | 0.96 |
| Males, n (%) | 7 (30.4) | 5 (38.4) | 2 (30) | 0.40 |
| Smoker, n (%) | 3 (13) | 2 (15.3) | 1 (10) | 0.068 |
| Former smoker, n (%) | 10 (43.5) | 4 (30.7) | 6 (60) | 0.76 |
| Obesity (BMI > 30), n (%) | 5 (21.7) | 4 (30.7) | 1 (10) | 0.339 |
| Age at diagnosis, mean ± SD | 70.5 ± 9 | 70.7 ± 10.7 | 71.2 ± 6.9 | 0.38 |
| Presence of other lung diseases | ||||
| Asthma, n (%) | 3 (13) | 1 (7.7) | 2 (20) | 0.068 |
| COPD, n (%) | 6 (26) | 5 (38.5) | 1 (10) | 0.05 |
| OSA, n (%) | 2 (8.6) | 2 (15.4) | 0 (0) | 0.092 |
| ANCA pattern | ||||
| P-ANCA, n (%) | 10 (43.5) | 4 (30.7) | 6 (60) | 0.22 |
| C-ANCA, n (%) | 13 (56.5) | 9 (69.2) | 4 (40) | 0.22 |
| Anti-MPO, n (%) | 13 (56.5) | 5 (38.4) | 8 (80) | 0.046 |
| Anti-PR3, n (%) | 4 (17.4) | 3 (23) | 1 (10) | 0.924 |
| Other autoantibodies | ||||
| Rheumatoid factor, n (%) | 6 (26) | 5 (38.4) | 1 (10) | 0.179 |
| Anti-CCP, n (%) | 1 (4.3) | 1 (7.7) | 0 (0) | 0.06 |
| ANA (>1/160), n (%) | 8 (34.7) | 6 (46.1) | 2 (20) | 0.05 |
| Anti-ENA, n (%) | 4 (17.4) | 4 (30.7) | 0 (0) | 0.05 |
| Respiratory manifestations (dyspnea or cough), n (%) | 15 (65.2) | 7 (53.8) | 8 (80) | 0.673 |
| PFTs values | ||||
| % FVC, mean ± SD (n = 20; 9 AAV) | 83.5 ± 26 | 81 ± 27 | 87 ± 26 | 0.68 |
| % FEV1, median ± SD (n = 20; 9 AAV) | 85.2 ± 26 | 80 ± 25 | 92 ± 29 | 0.16 |
| % DLCO, median ± SD (n = 17; 9 AAV) | 66.1 ± 19 | 66 ± 21 | 65 ± 17 | 0.44 |
| Hypoxemia *, n (%) | 5 (21.7) | 3 (23) | 2 (20) | 0.85 |
| Abnormal PFT **, (n = 20; 9 AAV) | 14 (70) | 10 (76.9) | 4 (40) | 0.161 |
| Radiological features in HRCT | ||||
| Nodules, n (%) | 2 (8.7) | 2 (15.3) | 0 (0) | 0.092 |
| Lung consolidation, n (%) | 8 (34.8) | 2 (15.3) | 6 (60) | 0.039 |
| Ground glass opacities, n (%) | 17 (73.9) | 9 (69.2) | 8 (80) | 0.66 |
| Traction bronchiectasis, n (%) | 19 (82.6) | 13 (100) | 6 (60) | 0.024 |
| Reticulation, n (%) | 15 (65.2) | 10 (76.9) | 5 (50) | 0.179 |
| Honeycomb, n (%) | 8 (34.8) | 5 (38.4) | 3 (30) | 0.673 |
| Radiological pattern in HRCT | ||||
| UIP, n (%) | 12 (52.2) | 9 (69.2) | 3 (30) | 0.161 |
| NSIP, n (%) | 6 (26) | 1 (7.7) | 5 (50) | 0.022 |
| Fibrotic NSIP, n (%) | 5 (21.7) | 4 (30.7) | 1 (10) | 0.09 |
| OP, n (%) | 5 (21.7) | 3 (23) | 2 (20) | 0.673 |
| C-reactive protein, mean ± SD | 2.3 ± 3.2 | 0.48 ± 0.3 | 4.8 ± 3.6 | 0.001 |
| Variables Analyzed During Follow-Up | All Patients (n = 23 Patients) | Isolated ANCA-ILD (n = 13 Patients) | AAV-ILD (n = 10 Patients: 5 MPA, 3 GPA, 2 EGPA) | p-Value |
|---|---|---|---|---|
| ILD follow-up period (months), median (IQR) | 36 (24–68) | 36 (24–47) | 35.5 (24–86) | 0.77 |
| Deterioration of PFT during follow up *, n (%) | 15 (65.2) | 8 (61.5) | 7 (70) | 0.673 |
| %FVC, median (IQR) | ||||
| 6 months (n = 16; 8 AAV) | 80.5 (73.5–100.5) | 90 (77–100.5) | 75 (67.5–104) | 0.115 |
| 12 months (n = 17; 8 AAV) | 75 (68–106) | 78 (73–106) | 69 (64–104) | 0.027 |
| 24 months (n = 14; 5 AAV) | 84 (69–102) | 81 (61–102) | 87 (71–102) | 0.43 |
| %DLCO, median (IQR) | ||||
| 6 months (n = 14; 7 AAV) | 72.6 (46–81) | 72 (52.6–93) | 73.2 (45.9–79) | 0.554 |
| 12 months (n = 14; 7 AAV) | 45.5 (30–67) | 47 (44–83) | 44 (29–53) | 0.712 |
| 24 months (n = 11; 3 AAV) | 47 (35–73) | 47 (36–75) | 69 (26–73) | 0.076 |
| Hypoxemia during follow-up ** | 12 (52.2) | 7 (53.8) | 5 (50) | 0.855 |
| Radiological progression in HRCT, n (%) | 15 (65.2) | 9 (69.2) | 6 (60) | 0.685 |
| RP-ILD, n (%) | 8 (34.8) | 3 (23) | 5 (50) | 0.673 |
| Death rate, n (%) | 10 (43.5) | 5 (38.4) | 5 (50) | 0.58 |
| Incidence mortality rate & (95% CI) | 11.7 (6.3–22) | 11.5 (4.8–27) | 11.9 (4.9–28) | 0.48 |
| Cause of death | ||||
| ILD, n (%) | 8 (34.8) | 5 (38.4) | 3 (30) | 0.673 |
| Infection, n (%) | 1 (4.3) | 0 (0) | 1 (10) | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valero-Martínez, C.; Valenzuela, C.; Baldivieso Achá, J.P.; Martínez-Besteiro, E.; Quiroga-Colina, P.; Alfranca, A.; Vicente-Rabaneda, E.F.; Muñiz, S.H.; Castañeda, S.; García-Vicuña, R. Clinical Profiles, Survival, and Lung Function Outcomes in ANCA-Associated Interstitial Lung Disease: An Observational Study. J. Clin. Med. 2025, 14, 229. https://doi.org/10.3390/jcm14010229
Valero-Martínez C, Valenzuela C, Baldivieso Achá JP, Martínez-Besteiro E, Quiroga-Colina P, Alfranca A, Vicente-Rabaneda EF, Muñiz SH, Castañeda S, García-Vicuña R. Clinical Profiles, Survival, and Lung Function Outcomes in ANCA-Associated Interstitial Lung Disease: An Observational Study. Journal of Clinical Medicine. 2025; 14(1):229. https://doi.org/10.3390/jcm14010229
Chicago/Turabian StyleValero-Martínez, Cristina, Claudia Valenzuela, Juan Pablo Baldivieso Achá, Elisa Martínez-Besteiro, Patricia Quiroga-Colina, Arantzazu Alfranca, Esther F. Vicente-Rabaneda, Susana Hernández Muñiz, Santos Castañeda, and Rosario García-Vicuña. 2025. "Clinical Profiles, Survival, and Lung Function Outcomes in ANCA-Associated Interstitial Lung Disease: An Observational Study" Journal of Clinical Medicine 14, no. 1: 229. https://doi.org/10.3390/jcm14010229
APA StyleValero-Martínez, C., Valenzuela, C., Baldivieso Achá, J. P., Martínez-Besteiro, E., Quiroga-Colina, P., Alfranca, A., Vicente-Rabaneda, E. F., Muñiz, S. H., Castañeda, S., & García-Vicuña, R. (2025). Clinical Profiles, Survival, and Lung Function Outcomes in ANCA-Associated Interstitial Lung Disease: An Observational Study. Journal of Clinical Medicine, 14(1), 229. https://doi.org/10.3390/jcm14010229







