Effects of a Multi-Professional Intervention on Mental Health of Middle-Aged Overweight Survivors of COVID-19: A Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
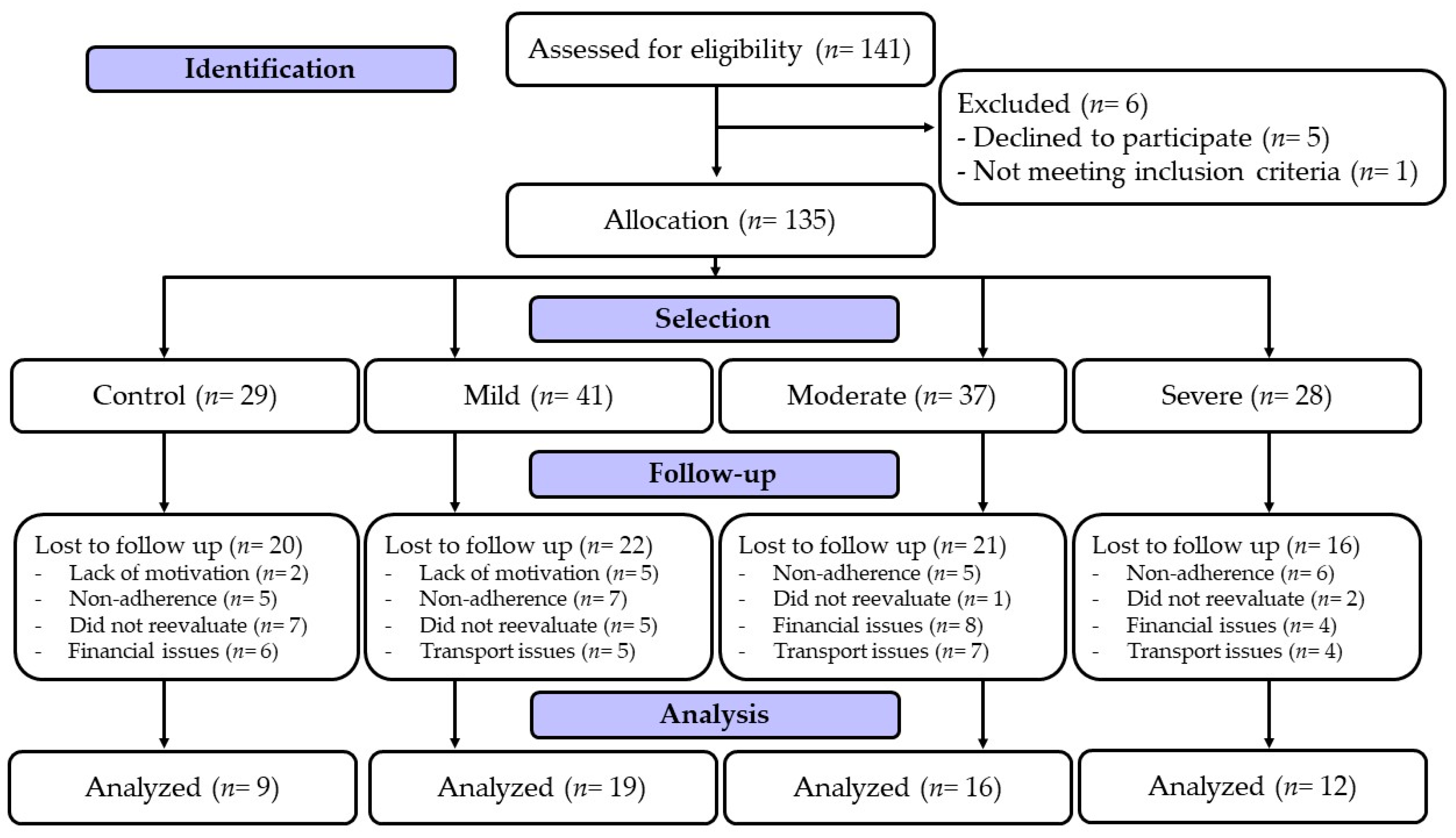
2.1. Study Design
2.2. Participants
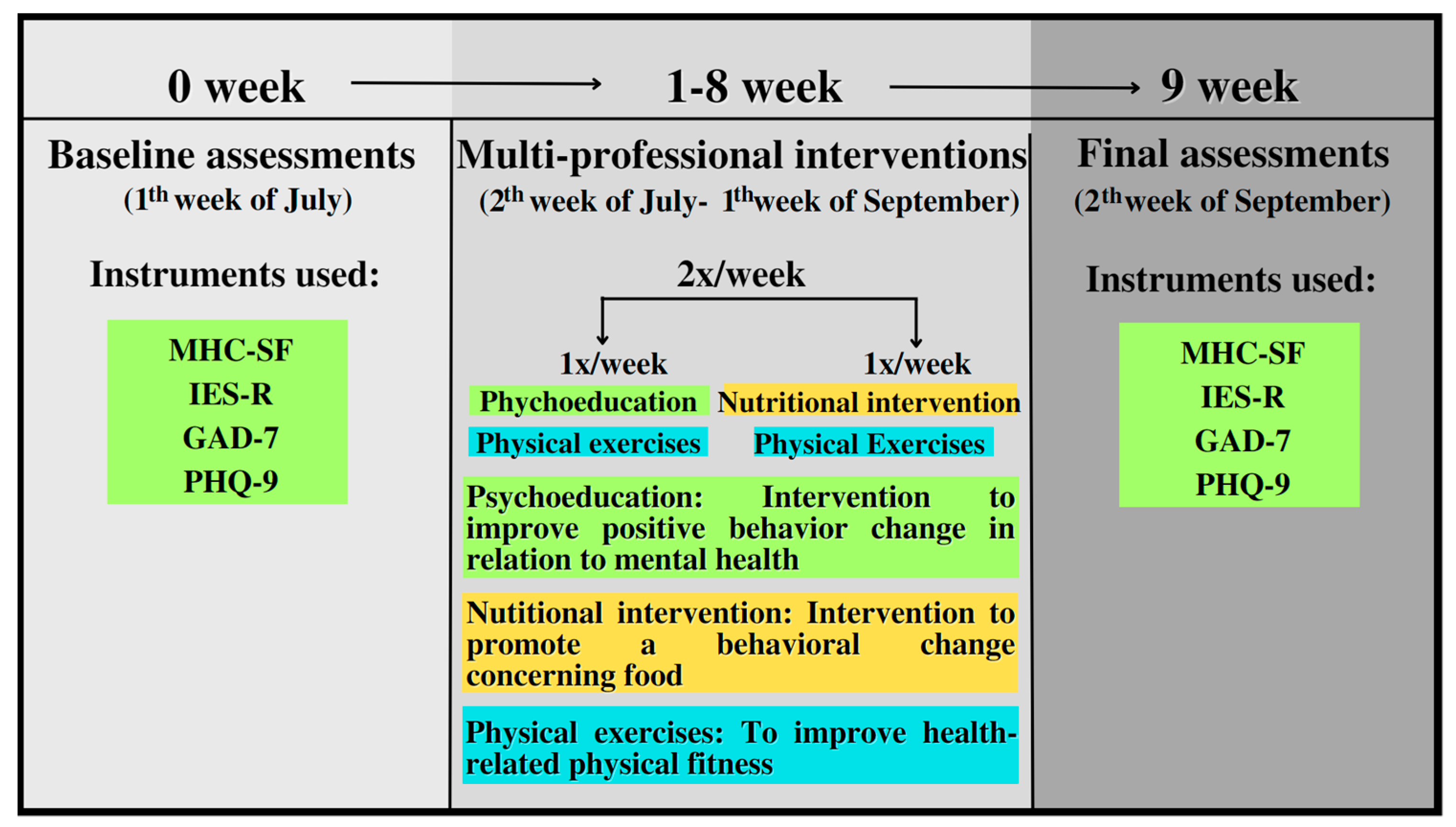
2.3. Procedures
2.3.1. Mental Health Continuum–Short Form (MHC-SF)
2.3.2. Impact of Event Scale-Revised (IES-R)
2.3.3. Generalized Anxiety Disorder–(GAD-7)
2.3.4. Patient Health Questionnaire-9–(PHQ-9)
2.4. Compositions of Interventions
2.4.1. Physical Exercise
2.4.2. Nutritional Intervention
2.4.3. Psychoeducation
2.5. Statistical Analysis
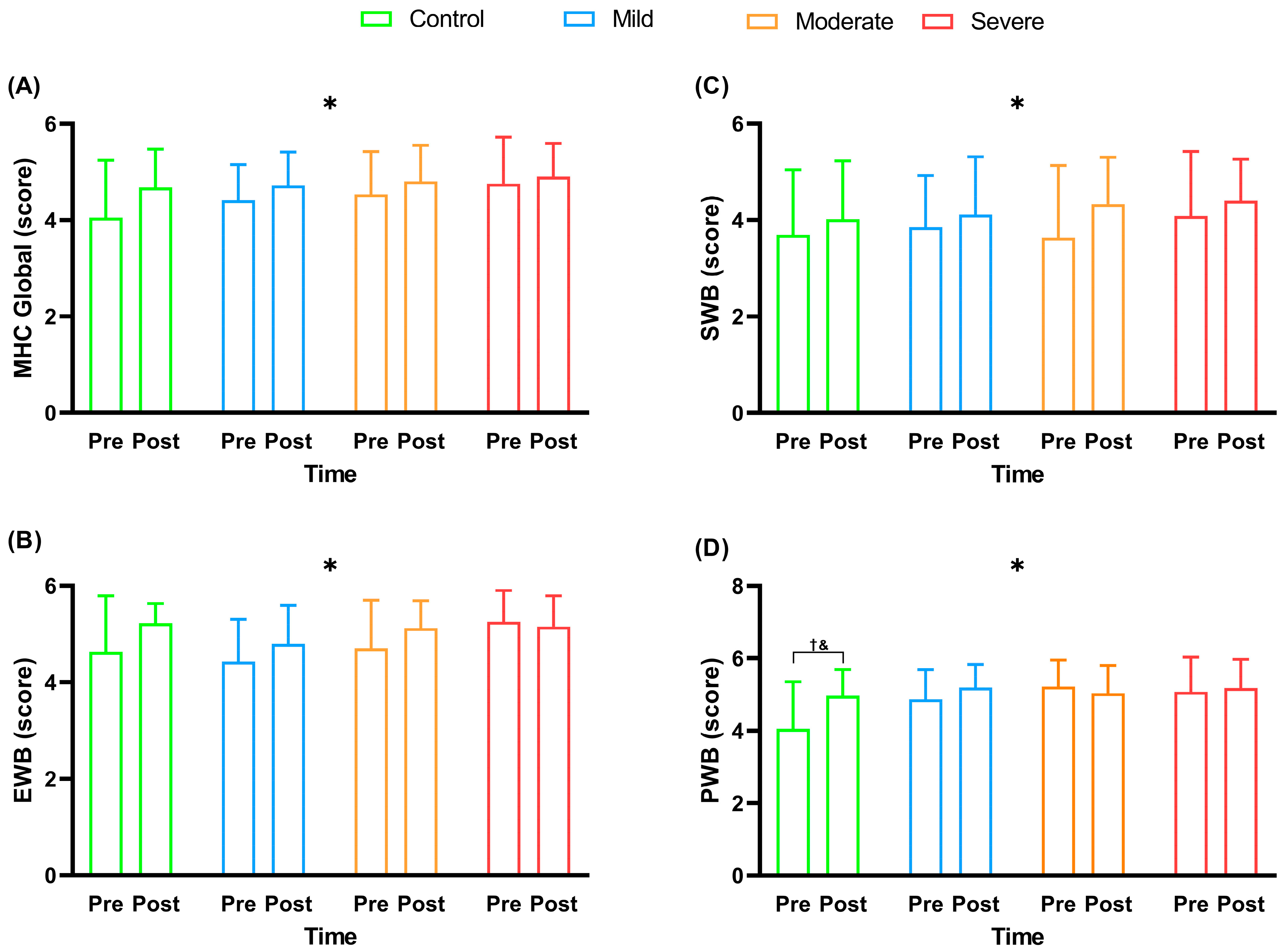
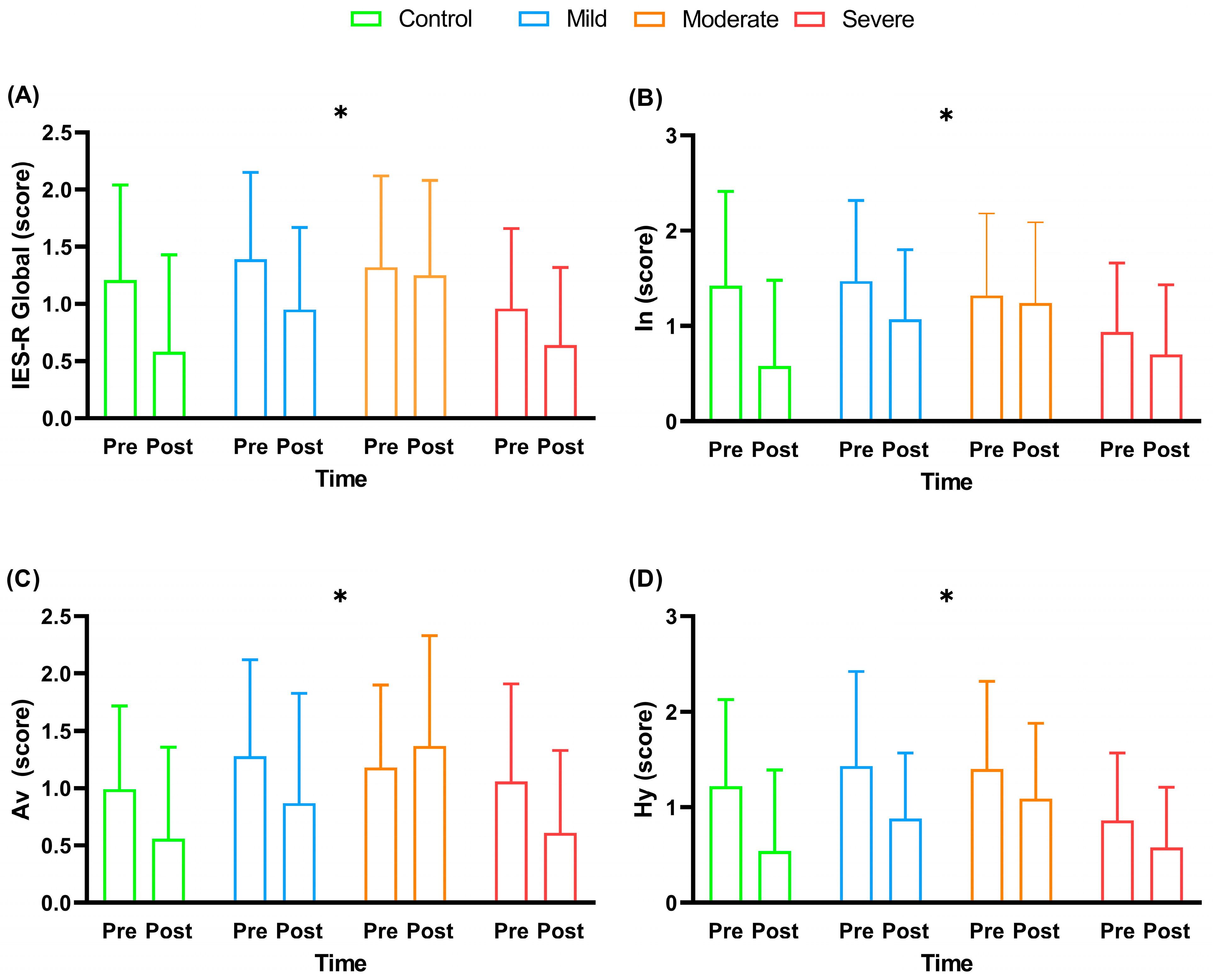
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Huang, E.; Zuo, Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 2021, 1486, 90–111. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Ba, W.G.T.F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Guzmán-Muñoz, E.; Concha-Cisternas, Y.; Oñate-Barahona, A.; Lira-Cea, C.; Cigarroa-Cuevas, I.; Méndez-Rebolledo, G.; Castillo-Retamal, M.; Valdés-Badilla, P.; Zapata-Lamana, R. Factores asociados a una baja calidad de vida en adultos chilenos durante la cuarentena por COVID-19. Rev. Med. Chil. 2020, 148, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Lemos, M.M.; Cavalini, G.R.; Henrique, C.R.P.; Perli, V.A.S.; Marchiori, G.D.M.; Marchiori, L.L.D.M.; Sordi, A.F.; de Moraes, S.M.F.; Ramos, S.D.P.; Valdés-Badilla, P.; et al. Body composition and cardiorespiratory fitness in overweight or obese people post COVID-19: A comparative study. Front. Physiol. 2022, 13, 949351. [Google Scholar] [CrossRef] [PubMed]
- Jaywant, A.; Bueno-Castellano, C.; Oberlin, L.E.; Vanderlind, W.M.; Wilkins, V.M.; Cherestal, S.; Boas, S.J.; Kanellopoulos, D. Psychological interventions on the front lines: A roadmap for the development of a behavioral treatment program to mitigate the mental health burden faced by COVID-19 survivors. Prof. Psychol. Res. Pract. 2022, 53, 80–89. [Google Scholar] [CrossRef]
- Lemes, C.B.; Neto, J.O. Aplicações da psicoeducação no contexto da saúde. Temas Psicol. 2017, 25, 17–28. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; for the CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010, 7, e1000251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic Report; WHO Consultation on Obesity: Geneva, Switzerland, 2000. [Google Scholar]
- de Paula, J.J.; Costa, D.S.; de Miranda, D.M.; Romano-Silva, M.A. Brazilian version of the Cognitive Failures Questionnaire (CFQ): Cross-cultural adaptation and evidence of validity and reliability. Rev. Bras. Psiquiatr. 2018, 40, 312–315. [Google Scholar] [CrossRef] [Green Version]
- Lamers, S.M.; Westerhof, G.J.; Bohlmeijer, E.T.; Klooster, P.T.; Keyes, C.L. Evaluating the psychometric properties of the mental health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 2011, 67, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Machado, W.D.L.; Bandeira, D.R. Positive Mental Health Scale: Validation of the Mental Health Continuum—Short Form. Psico-Usf 2015, 20, 259–274. [Google Scholar] [CrossRef] [Green Version]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Caiuby, A.V.S.; Lacerda, S.S.; Quintana, M.I.; Torii, T.S.; Andreoli, S.B. Adaptação transcultural da versão brasileira da Escala do Impacto do Evento—Revisada (IES-R). Cad. Saude Publica 2012, 28, 597–603. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000; Volume 1. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Moreno, A.L.; DeSousa, D.A.; Souza, A.M.F.L.P.; Manfro, G.G.; Salum, G.A.; Koller, S.H.; Osório, F.L.; Crippa, J.A.S. Factor Structure, Reliability, and Item Parameters of the Brazilian-Portuguese Version of the GAD-7 Questionnaire. Temas Psicol. 2016, 24, 367–376. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Santos, I.S.; Tavares, B.F.; Munhoz, T.N.; De Almeida, L.S.P.; Da Silva, N.T.B.; Tams, B.D.; Patella, A.; Matijasevich, A. Sensibilidade e especificidade do Patient Health Questionnaire-9 (PHQ-9) entre adultos da população geral. Cad. Saude Publica 2013, 29, 1533–1543. [Google Scholar] [CrossRef] [PubMed]
- Jimeno-Almazán, A.; Franco-López, F.; Buendía-Romero, Á.; Martínez-Cava, A.; Sánchez-Agar, J.A.; Martínez, B.J.S.; Courel-Ibáñez, J.; Pallarés, J.G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand. J. Med. Sci. Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Brasil Ministério da Saude. Guia Alimentar para a População Brasileira Guia Alimentar para a População Brasileira, 2°; Brasil Ministério da Saude: Brasília, Brazil, 2014.
- Authier, J. The Psychoeducation Model: Definition, Contemporary Roots and Content. Can. J. Couns. Psychother. 1977, 12, 15–22. [Google Scholar]
- Beck, J.S. Terapia Cognitivo-Componamental: Teoria e Prática, 2°; Artmed: Porrto Alegre, Portugal, 2013. [Google Scholar]
- McCrorie, A.; Donnelly, C.; McGlade, K. Infographics: Healthcare Communication for the Digital Age. Ulst. Med. J. 2016, 85, 71–75. [Google Scholar]
- De Oliveira, D.A.; Lessa, R.S.; Ribeiro, S.C.S.; De Vasconcelos, P.F. The Visual Practice: The Infographic as a Facilitating Tool for Learning in Medical School. Rev. Bras. Educ. Med. 2020, 44, 4. [Google Scholar] [CrossRef]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Arantes, D.J.; Picasso, R.; da Silva, E.A. Grupos psicoeducativos com familiares dos usuários de um Centro de Atenção Psicossocial. Pesqui. Prát. Psicossociais 2019, 14, 1–15. [Google Scholar]
- Bhattacharjee, D.; Rai, A.K.; Singh, N.K.; Kumar, P.; Munda, S.K.; Das, B. Psychoeducation: A Measure to Strengthen Psychiatric Treatment. Delhi Psychiatry J. 2011, 14, 33–39. [Google Scholar]
- Bolognese, M.A.; Franco, C.B.; Ferrari, A.; Bennemann, R.M.; Lopes, S.M.A.; Bertolini, S.M.M.G.; Júnior, N.N.; Branco, B.H.M. Group Nutrition Counseling or Individualized Prescription for Women With Obesity? A Clinical Trial. Front. Public Health 2020, 8, 127. [Google Scholar] [CrossRef]
- Golińska, P.; Cieślak, M.; Hubert, O.; Bidzan, M. Mental Health and the Symptoms of PTSD in People with Depression and Anxiety Disorders during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5542. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Hamatani, S.; Shimizu, E.; Käll, A.; Andersson, G. Impact of post-COVID conditions on mental health: A cross-sectional study in Japan and Sweden. BMC Psychiatry 2022, 22, 237. [Google Scholar] [CrossRef]
- Anjum, S.; Ullah, R.; Rana, M.S.; Khan, H.A.; Memon, F.S.; Ahmed, Y.; Jabeen, S.; Faryal, R. COVID-19 Pandemic: A Serious Threat for Public Mental Health Globally. Psychiatr. Danub. 2020, 32, 245–250. [Google Scholar] [CrossRef]
- Khoramipour, K.; Basereh, A.; Hekmatikar, A.A.; Castell, L.; Ruhee, R.T.; Suzuki, K. Physical activity and nutrition guidelines to help with the fight against COVID-19. J. Sports Sci. 2021, 39, 101–107. [Google Scholar] [CrossRef]
- Guo, K.; Zhang, X.; Bai, S.; Minhat, H.S.; Nazan, A.I.N.M.; Feng, J.; Li, X.; Luo, G.; Zhang, X.; Feng, J.; et al. Assessing social support impact on depression, anxiety, and stress among undergraduate students in Shaanxi province during the COVID-19 pandemic of China. PLoS ONE 2021, 16, e0253891. [Google Scholar] [CrossRef]
- Styra, R.; Hawryluck, L.; Mc Geer, A.; Dimas, M.; Sheen, J.; Giacobbe, P.; Dattani, N.; Lorello, G.; Rac, V.E.; Francis, T.; et al. Surviving SARS and living through COVID-19: Healthcare worker mental health outcomes and insights for coping. PLoS ONE 2021, 16, e0258893. [Google Scholar] [CrossRef]
- van Agteren, J.; Iasiello, M.; Lo, L.; Bartholomaeus, J.; Kopsaftis, Z.; Carey, M.; Kyrios, M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 2021, 5, 631–652. [Google Scholar] [CrossRef] [PubMed]
- Egan, K.P. Supporting Mental Health and Well-being Among Student-Athletes. Clin. Sports Med. 2019, 38, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hawkley, L.C.; Crawford, L.E.; Ernst, J.M.; Burleson, M.H.; Kowalewski, R.B.; Malarkey, W.B.; Van Cauter, E.; Berntson, G.G. Loneliness and Health: Potential Mechanisms. Psychosom. Med. 2002, 64, 407–417. [Google Scholar] [CrossRef]
- Smith, K.J.; Gavey, S.; Riddell, N.E.; Kontari, P.; Victor, C. The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2020, 112, 519–541. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.Y.K.; Townson, A.T.; Kapur, M.; Ferreira, A.F.; Nunn, R.; Galante, J.; Phillips, V.; Gentry, S.; Usher-Smith, J.A. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLoS ONE 2021, 16, e0247139. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-Arimi, S. Physical and mental health complications post-COVID-19: Scoping review. J. Psychosom. Res. 2021, 147, 110525. [Google Scholar] [CrossRef]
- Dinas, P.C.; Koutedakis, Y.; Flouris, A.D. Effects of exercise and physical activity on depression. Ir. J. Med. Sci. 2011, 180, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, M.; Gonzaga, A.P.; Modesto, S.E.F.; Cobelo, A.W. Grupo psicoeducativo multifamiliar no tratamento dos transtornos alimentares na adolescência. Psicol. Estud. 2010, 15, 217–223. [Google Scholar] [CrossRef]
- Desai, A.D.; Lavelle, M.; Boursiquot, B.C.; Wan, E.Y. Long-term complications of COVID-19. Am. J. Physiol. -Cell Physiol. 2022, 322, C1–C11. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.C.D.S.; Menon, V.; Phadke, R.; Dapke, K.; Miranda, A.V.; Ahmad, S.; Essar, M.Y.; Hashim, H.T. Mental health in the post COVID-19 era: Future perspectives. Einstein 2022, 20. [Google Scholar] [CrossRef]
- Vlake, J.H.; Wesselius, S.; van Genderen, M.E.; van Bommel, J.; Klerk, B.B.-D.; Wils, E.-J. Psychological distress and health-related quality of life in patients after hospitalization during the COVID-19 pandemic: A single-center, observational study. PLoS ONE 2021, 16, e0255774. [Google Scholar] [CrossRef]

| Control (n = 9) | Mild (n = 19) | Moderate (n = 16) | Severe (n = 12) | |
|---|---|---|---|---|
| Age (years) | 45.44 ± 11.98 | 49.47 ± 13.46 | 46.63 ± 12.80 | 48.25 ± 10.29 |
| Male | 8 (88.89) | 11 (57.89) | 8 (50.00) | 10 (83.33) |
| Female | 1 (11.11) | 8 (42.11) | 8 (50.00) | 2 (16.67) |
| BMI (kg/m2) | 30.22 ± 5.22 | 28.05 ± 3.78 | 34.59 ± 6.83 | 32.40 ± 4.89 |
| Infirmary (d) | - | - | 10 (5.00–14.00) | 14.00 (11.50–18.00) |
| ICU (d) | - | - | - | 12.00 (4.00–29.00) |
| Civil status | ||||
| Single | 3 (37.50) | 4 (22.22) | 2 (12.50) | 0 (0.00) |
| Stable union | 5 (62.50) | 11 (61.11) | 12 (75.00) | 11 (91.67) |
| Divorced | 0 (0.00) | 1 (5.56) | 1 (6.25) | 1 (8.33) |
| Widower | 0 (0.00) | 2 (11.11) | 1 (6.25) | 0 (0.00) |
| Education | ||||
| Postgraduate | 4 (50.00) | 7 (38.89) | 3 (18.75) | 4 (33.33) |
| University education | 4 (50.00) | 5 (27.78) | 8 (50.00) | 3 (25.00) |
| High school | 0 (0.00) | 5 (27.78) | 4 (25.00) | 4 (33.33) |
| Others * | 0 (0.00) | 1 (5.56) | 1 (6.25) | 1 (8.33) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryal, J.J.; Perli, V.A.S.; Marques, D.C.d.S.; Sordi, A.F.; Marques, M.G.d.S.; Camilo, M.L.; Milani, R.G.; Mota, J.; Valdés-Badilla, P.; Magnani Branco, B.H. Effects of a Multi-Professional Intervention on Mental Health of Middle-Aged Overweight Survivors of COVID-19: A Clinical Trial. Int. J. Environ. Res. Public Health 2023, 20, 4132. https://doi.org/10.3390/ijerph20054132
Ryal JJ, Perli VAS, Marques DCdS, Sordi AF, Marques MGdS, Camilo ML, Milani RG, Mota J, Valdés-Badilla P, Magnani Branco BH. Effects of a Multi-Professional Intervention on Mental Health of Middle-Aged Overweight Survivors of COVID-19: A Clinical Trial. International Journal of Environmental Research and Public Health. 2023; 20(5):4132. https://doi.org/10.3390/ijerph20054132
Chicago/Turabian StyleRyal, Joed Jacinto, Victor Augusto Santos Perli, Déborah Cristina de Souza Marques, Ana Flávia Sordi, Marilene Ghiraldi de Souza Marques, Maria Luiza Camilo, Rute Grossi Milani, Jorge Mota, Pablo Valdés-Badilla, and Braulio Henrique Magnani Branco. 2023. "Effects of a Multi-Professional Intervention on Mental Health of Middle-Aged Overweight Survivors of COVID-19: A Clinical Trial" International Journal of Environmental Research and Public Health 20, no. 5: 4132. https://doi.org/10.3390/ijerph20054132
APA StyleRyal, J. J., Perli, V. A. S., Marques, D. C. d. S., Sordi, A. F., Marques, M. G. d. S., Camilo, M. L., Milani, R. G., Mota, J., Valdés-Badilla, P., & Magnani Branco, B. H. (2023). Effects of a Multi-Professional Intervention on Mental Health of Middle-Aged Overweight Survivors of COVID-19: A Clinical Trial. International Journal of Environmental Research and Public Health, 20(5), 4132. https://doi.org/10.3390/ijerph20054132








