Can Smart Home Technologies Help Older Adults Manage Their Chronic Condition? A Systematic Literature Review
Abstract
1. Introduction
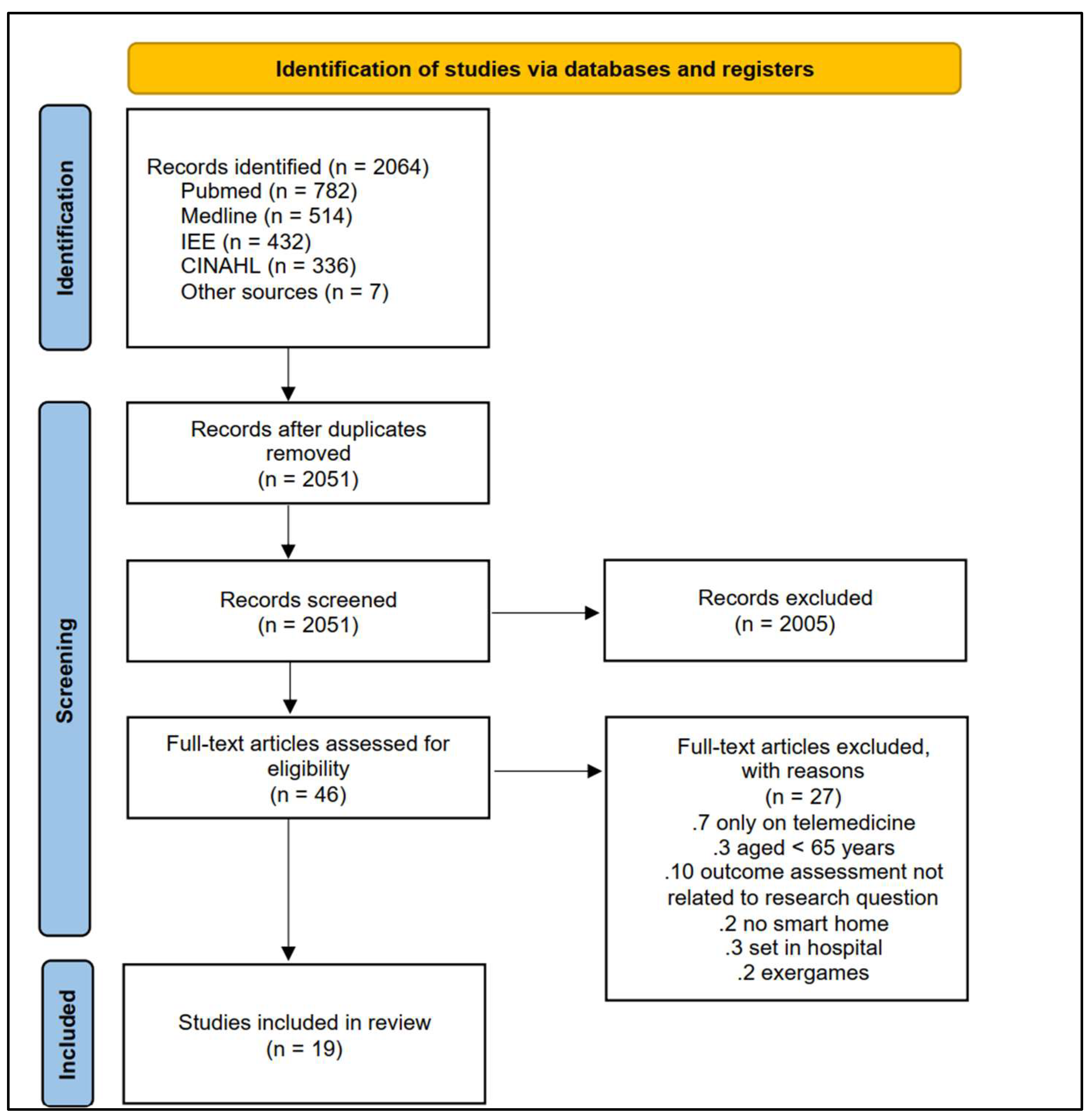
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection and Data Collection
2.3. Quality Assessment
2.4. Data Analysis
3. Results
3.1. Study Types and Patient Characteristics
3.2. Quality Assessment
3.3. Interventions Characteristics and Aims
3.4. Smart Homes
3.5. External Memory Aids
3.6. Hybrid Technology
3.7. Health Outcomes and Vital Signs
3.8. Medication Management
3.9. IADL and ADL
3.10. Mobility and Falls
3.11. Quality of Life
4. Discussion
4.1. What Are the Characteristics and Aims of Smart Home Technologies?
4.2. What Type of Health Outcomes Have Been Reported?
4.3. Recommendation for Further Research
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meulendijk, M.; Van De Wijngaert, L.; Brinkkemper, S.; Leenstra, H. AmI in good care? Developing design principles for ambient intelligent domotics for elderly. Inform. Health Soc. Care 2011, 36, 75–88. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- March, R. Delivering on the promise of personalized healthcare. Pers. Med. 2010, 7, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Boldy, D.; Grenade, L.; Lewin, G.; Karol, E.; Burton, E. Older people’s decisions regarding ‘ageing in place’: A Western Australian case study. Australas J. Ageing 2011, 30, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Vanleerberghe, P.; De Witte, N.; Claes, C.; Schalock, R.L.; Verte, D. The quality of life of older people aging in place: A literature review. Qual. Life Res. 2017, 26, 2899–2907. [Google Scholar] [CrossRef]
- Davey, J.A.; de Joux, V.; Nana, G.; Arcus, M. Accommodation Options for Older People in Aotearoa/New Zealand; Citeseer, The Pennsylvania State University: State College, PA, USA, 2004. [Google Scholar]
- Wang, S.; Bolling, K.; Mao, W.; Reichstadt, J.; Jeste, D.; Kim, H.-C.; Nebeker, C. Technology to Support Aging in Place: Older Adults’ Perspectives. Healthcare 2019, 7, 60. [Google Scholar] [CrossRef]
- Iecovich, E.; Rabin, B. Practices used in Israel by nurses who care during hospitalization for older patients with dementia or who are bedridden. Am. J. Alzheimers Dis. Other Demen. 2014, 29, 166–176. [Google Scholar] [CrossRef]
- Kim, Y.; Park, Y.; Choi, J. A study on the adoption of IoT smart home service: Using Value-based Adoption Model. Total Qual. Manag. Bus. Excell. 2017, 28, 1149–1165. [Google Scholar] [CrossRef]
- Dahmen, J.; Minor, B.; Cook, D.; Vo, T.; Schmitter-Edgecombe, M. Design of a smart home-driven digital memory notebook to support self-management of activities for older adults. Gerontechnology 2018, 17, 113–125. [Google Scholar] [CrossRef]
- Patel, K.K.; Patel, S.M.; Scholar, P. Internet of things-IOT: Definition, characteristics, architecture, enabling technologies, application & future challenges. Int. J. Eng. Sci. Comput. 2016, 6, 6122–6132. [Google Scholar]
- Lee, L.N.; Kim, M.J. A Critical Review of Smart Residential Environments for Older Adults with a Focus on Pleasurable Experience. Front. Psychol. 2019, 10, 3080. [Google Scholar] [CrossRef]
- Augusto, J.C.; Callaghan, V.; Cook, D.; Kameas, A.; Satoh, I. “Intelligent Environments: A manifesto”. Hum. -Cent. Comput. Inf. Sci. 2013, 3, 12. [Google Scholar] [CrossRef]
- Demiris, G.; Hensel, B.K. Technologies for an aging society: A systematic review of “smart home” applications. Yearb. Med. Inform. 2008, 17, 33–40. [Google Scholar]
- Turjamaa, R.; Pehkonen, A.; Kangasniemi, M. How smart homes are used to support older people: An integrative review. Int. J. Older People Nurs. 2019, 14, e12260. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Stroulia, E.; Nikolaidis, I.; Miguel-Cruz, A.; Rios Rincon, A. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inform. 2016, 91, 44–59. [Google Scholar] [CrossRef]
- Qian, K.; Zhang, Z.; Yamamoto, Y.; Schuller, B.W. Artificial intelligence internet of things for the elderly: From assisted living to health-care monitoring. IEEE Signal Process. Mag. 2021, 38, 78–88. [Google Scholar] [CrossRef]
- Ghorayeb, A.; Comber, R.; Gooberman-Hill, R. Older adults’ perspectives of smart home technology: Are we developing the technology that older people want? Int. J. Hum. Comput. Stud. 2021, 147, 102571. [Google Scholar] [CrossRef]
- Liu, P.; Li, G.; Jiang, S.; Liu, Y.; Leng, M.; Zhao, J.; Wang, S.; Meng, X.; Shang, B.; Chen, L.; et al. The effect of smart homes on older adults with chronic conditions: A systematic review and meta-analysis. Electronic 2019, 40, 1528–3984. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Sayers, A. Tips and tricks in performing a systematic review. Br. J. Gen. Pract. 2007, 57, 425. [Google Scholar] [CrossRef]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic Reviews of Effectiveness. In Joanna Briggs Institute Reviewer’s Manual; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Cavallo, F.; Aquilano, M.; Arvati, M. An ambient assisted living approach in designing domiciliary services combined with innovative technologies for patients with Alzheimer’s disease: A case study. Am. J. Alzheimers Dis. Other Demen. 2015, 30, 69–77. [Google Scholar] [CrossRef]
- Celler, B.G.; Sparks, R.; Nepal, S.; Alem, L.; Varnfield, M.; Li, J.; Jang-Jaccard, J.; McBride, S.J.; Jayasena, R. Design of a multi-site multi-state clinical trial of home monitoring of chronic disease in the community in Australia. BMC Public Health 2014, 14, 1270. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.; Campo, E.; Estève, D. Assessment of activity of elderly people using a home monitoring system. Int. J. Rehabil. Res. 2005, 28, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Dawadi, P.N.; Cook, D.J.; Schmitter-Edgecombe, M. Automated Cognitive Health Assessment from Smart Home-Based Behavior Data. IEEE J. Biomed. Health Inform. 2016, 20, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Fritz, R.L.; Dermody, G. A nurse-driven method for developing artificial intelligence in “smart” homes for aging-in-place. Nurs. Outlook 2019, 67, 140–153. [Google Scholar] [CrossRef]
- Goldberg, L.R.; Piette, J.D.; Walsh, M.N.; Frank, T.A.; Jaski, B.E.; Smith, A.L.; Rodriguez, R.; Mancini, D.M.; Hopton, L.A.; Orav, E.J.; et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: The Weight Monitoring in Heart Failure (WHARF) trial. Am. Heart J. 2003, 146, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Hayes, T.L.; Abendroth, F.; Adami, A.; Pavel, M.; Zitzelberger, T.A.; Kaye, J.A. Unobtrusive assessment of activity patterns associated with mild cognitive impairment. Alzheimers Dement 2008, 4, 395–405. [Google Scholar] [CrossRef]
- Jekel, K.; Damian, M.; Storf, H.; Hausner, L.; Frölich, L. Development of a proxy-free objective assessment tool of instrumental activities of daily living in mild cognitive impairment using smart home technologies. J. Alzheimers Dis. 2016, 52, 509–517. [Google Scholar] [CrossRef]
- Kuo, Y.H.; Chien, Y.K.; Wang, W.R.; Chen, C.H.; Chen, L.S.; Liu, C.K. Development of a home-based telehealthcare model for improving the effectiveness of the chronic care of stroke patients. Kaohsiung J. Med. Sci. 2012, 28, 38–43. [Google Scholar] [CrossRef]
- Lazarou, I.; Karakostas, A.; Stavropoulos, T.G.; Tsompanidis, T.; Meditskos, G.; Kompatsiaris, I.; Tsolaki, M. A Novel and Intelligent Home Monitoring System for Care Support of Elders with Cognitive Impairment. J. Alzheimers Dis. 2016, 54, 1561–1591. [Google Scholar] [CrossRef]
- Lazarou, I.; Stavropoulos, T.G.; Meditskos, G.; Andreadis, S.; Kompatsiaris, I.; Tsolaki, M. Long-Term Impact of Intelligent Monitoring Technology on People with Cognitive Impairment: An Observational Study. J. Alzheimers Dis. 2019, 70, 757–792. [Google Scholar] [CrossRef]
- Rawtaer, I.; Mahendran, R.; Kua, E.H.; Tan, H.P.; Tan, H.X.; Lee, T.-S.; Ng, T.P. Early detection of mild cognitive impairment with in-home sensors to monitor behavior patterns in community-dwelling senior citizens in Singapore: Cross-sectional feasibility study. JMIR 2020, 22, e16854. [Google Scholar] [CrossRef] [PubMed]
- Sacco, G.; Joumier, V.; Darmon, N.; Dechamps, A.; Derreumaux, A.; Lee, J.-H.; Piano, J.; Bordone, N.; Konig, A.; Teboul, B. Detection of activities of daily living impairment in Alzheimer’s disease and mild cognitive impairment using information and communication technology. Clin. Interv. Aging 2012, 7, 539. [Google Scholar] [CrossRef] [PubMed]
- Soran, O.Z.; Feldman, A.M.; Piña, I.L.; Lamas, G.A.; Kelsey, S.F.; Selzer, F.; Pilotte, J.; Lave, J.R. Cost of medical services in older patients with heart failure: Those receiving enhanced monitoring using a computer-based telephonic monitoring system compared with those in usual care: The heart failure home care trial. J. Card. Fail. 2010, 16, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Urwyler, P.; Stucki, R.; Rampa, L.; Muri, R.; Mosimann, U.P.; Nef, T. Cognitive impairment categorized in community-dwelling older adults with and without dementia using in-home sensors that recognise activities of daily living. Sci. Rep. 2017, 7, 42084. [Google Scholar] [CrossRef]
- Wakefield, B.J.; Koopman, R.J.; Keplinger, L.E.; Bomar, M.; Bernt, B.; Johanning, J.L.; Kruse, R.L.; Davis, J.W.; Wakefield, D.S.; Mehr, D.R. Effect of home telemonitoring on glycemic and blood pressure control in primary care clinic patients with diabetes. Telemed. e-Health 2014, 20, 199–205. [Google Scholar] [CrossRef]
- Yu, J.; An, N.; Hassan, T.; Kong, Q. A Pilot Study on a Smart Home for Elders Based on Continuous In-Home Unobtrusive Monitoring Technology. Herd 2019, 12, 206–219. [Google Scholar] [CrossRef]
- Alberdi, A.; Weakley, A.; Schmitter-Edgecombe, M.; Cook, D.J.; Aztiria, A.; Basarab, A.; Barrenechea, M. Smart Home-Based Prediction of Multidomain Symptoms Related to Alzheimer’s Disease. IEEE J. Biomed. Health Inf. 2018, 22, 1720–1731. [Google Scholar] [CrossRef]
- Glasziou, P.; Irwig, L.; Mant, D. Monitoring in chronic disease: A rational approach. BMJ 2005, 330, 644–648. [Google Scholar] [CrossRef]
- Chen, L.-K. Gerontechnology and artificial intelligence: Better care for older people. Arch. Gerontol. Geriatr. 2020, 91, 104252. [Google Scholar] [CrossRef]
- Arcelus, A.; Jones, M.H.; Goubran, R.; Knoefel, F. In Integration of Smart Home Technologies in a Health Monitoring System for the Elderly. In Proceedings of the 21st International Conference on Advanced Information Networking and Applications Workshops (AINAW’07), Niagara Falls, ON, Canada, 21–23 May 2007; pp. 820–825. [Google Scholar]
- Morris, M.E.; Adair, B.; Miller, K.; Ozanne, E.; Hansen, R.; Pearce, A.J.; Santamaria, N.; Viega, L.; Long, M.; Said, C.M. Smart-home technologies to assist older people to live well at home. J. Aging Sci. 2013, 1, 1–9. [Google Scholar]
- Lê, Q.; Nguyen, H.B.; Barnett, T. Smart homes for older people: Positive aging in a digital world. Future Internet 2012, 4, 607–617. [Google Scholar] [CrossRef]
- Demiris, G.; Hensel, B.K.; Skubic, M.; Rantz, M. Senior residents’ perceived need of and preferences for “smart home” sensor technologies. Int. J. Technol. Assess Health Care 2008, 24, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Mann, W.C.; Belchior, P.; Tomita, M.R.; Kemp, B.J. Older adults’ perception and use of PDAs, home automation system, and home health monitoring system. Top. Geriatr. Rehabil. 2007, 23, 35–46. [Google Scholar] [CrossRef]
- Alkhaldi, G.; Hamilton, F.L.; Lau, R.; Webster, R.; Michie, S.; Murray, E. The effectiveness of technology-based strategies to promote engagement with digital interventions: A systematic review protocol. JMIR Res. Protoc. 2015, 4, e47. [Google Scholar] [CrossRef]
- Gentry, T. Smart homes for people with neurological disability: State of the art. Electronic 2009, 25, 1878–6448. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, Z.; Dong, T. A Review of Wearable Technologies for Elderly Care that Can Accurately Track Indoor Position, Recognize Physical Activities and Monitor Vital Signs in Real Time. Sensors 2017, 17, 341. [Google Scholar] [CrossRef]
- Avgerinakis, K.; Briassouli, A.; Kompatsiaris, I. Recognition of Activities of Daily Living for Smart Home Environments. In Proceedings of the 2013 9th International Conference on Intelligent Environments, Athens, Greece, 16–17 July 2013; pp. 173–180. [Google Scholar]
- Hamm, J.; Money, A.G.; Atwal, A.; Paraskevopoulos, I. Fall prevention intervention technologies: A conceptual framework and survey of the state of the art. J. Biomed. Inform. 2016, 59, 319–345. [Google Scholar] [CrossRef]
- Keshini, Assistive technologies in reducing caregiver burden among informal caregivers of older adults: A systematic review. Disabil. Rehabil. Assist. Technol. 2016, 11, 353–360. [CrossRef]
- Martin, S.; Kelly, G.; Kernohan, W.G.; McCreight, B.; Nugent, C. Smart home technologies for health and social care support. Electronic 2008, 8, CD006412. [Google Scholar] [CrossRef]
- Majumder, S.; Aghayi, E.; Noferesti, M.; Memarzadeh-Tehran, H.; Mondal, T.; Pang, Z.; Deen, M.J. Smart Homes for Elderly Healthcare–Recent Advances and Research Challenges. Sensors 2017, 17, 2496. [Google Scholar] [CrossRef]
- Chung, J.; Demiris, G.; Thompson, H.J. Ethical considerations regarding the use of smart home technologies for older adults: An integrative review. Annu. Rev. Nurs. Res. 2016, 34, 155–181. [Google Scholar] [CrossRef] [PubMed]
- Courtney, K.L. Privacy and senior willingness to adopt smart home information technology in residential care facilities. Methods Inf. Med. 2008, 47, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Balta-Ozkan, N.; Davidson, R.; Bicket, M.; Whitmarsh, L. Social barriers to the adoption of smart homes. Energy Policy 2013, 63, 363–374. [Google Scholar] [CrossRef]
| Good Quality | Fair Quality | Poor Quality | |
|---|---|---|---|
| Cavallo et al., 2015 [23] | X | ||
| Celler et al., 2014 [24] | X | ||
| Chan et al., 2005 [25] | X | ||
| Dawadi et al., 2016 [26] | X | ||
| Fritz et al., 2019 [27] | X | ||
| Goldberg et al., 2003 [28] | X | ||
| Hayes et al., 2008 [29] | X | ||
| Jekel et al., 2016 [30] | X | ||
| Kuo et al., 2012 [31] | X | ||
| Lanzarou et al., 2016 [32] | X | ||
| Lanzarou et al., 2019 [33] | X | ||
| Rawtaer et al., 2020 [34] | X | ||
| Sacco et al., 2012 [35] | X | ||
| Soran et al., 2010 [36] | X | ||
| Urweyler et al., 2017 [37] | X | ||
| Wakefield et al., 2014 [38] | X | ||
| Yu et al., 2019 [39] | X |
| Article Year Country | Sample (n) | Disease | Type of Study | Characteristics of Technology | Aim | Smart Home Functionality | Health Outcomes |
|---|---|---|---|---|---|---|---|
| Alberdi et al., 2018 [40] Spain | 29 | Alzheimer disease | Iterative study | Environmental Sensor | To assess the possibility of detecting changes in psychological, cognitive, and behavioural symptoms of AD by making use of unobtrusively collected smart home behaviour data and machine learning techniques | Motion sensors | Sleep disorders, ADL, cognitive abilities, mobility |
| Cavallo et al., 2015 [23] Italy | 14 | Alzheimer disease | Case study | Environmental Sensor | To demonstrate the technical effectiveness and acceptability of an innovative domiciliary smart sensor system for providing domiciliary assistance to patients with AD which has been developed with an ambient assisted living approach | Smart sensor system | Exit/entrance monitoring and alerting, multimedia cognitive stimulation, supporting in taking drugs, control of gas and water electron valve, support in using phone |
| Celler et al., 2014 [24] Australia | 375 | COPD, Cardiovascular Disease, Diabetes, Asthma | Before After Control Intervention | Integration between Telemedicine and the use of devices | To demonstrate how telehealth services for chronic disease management in the community can be deployed nationally and to develop advanced modelling and data analytics tools to risk stratify patients daily to automatically identify exacerbations of their chronic conditions | Telemedcare monitoring unit | Blood sugar, SpO2, mortality, hospitalization, |
| Chan et al., 2004 [25] France | 4 | Dementia and Alzheimer Disease | Case study | Environmental Sensor | To show the detailed results obtained by the system for the differed assessment of night-time activities and the computation of correlation coefficients between data for in-bed rest-lessness and getting up, going out or visiting the toilet in individuals followed for several months | Ten infrared sensors on the ceiling, connected to a computer by means of a communication network in its wire version | Getting up, going out, going to bed, visiting the toilet, in bed restlessness |
| Dahamen et al., 2018 [10] USA | 17 | Dementia, memory difficulties | Iterative study | Exergames and Digital Interfaces | To introduce a real-time automated intervention that partners mobile apps with smart home-based activity learning using two primary mechanisms | Digital memory notebook mobile application composed of four main components: home, calendar, profile, and Notes. | ADL (Eat, work cook) |
| Dawadi et al., 2016 [26] USA | 67 | Dementia | Observational study | Environmental Sensor | (1) To provide automated task quality scoring from sensor data using machine learning techniques and (2) to automate cognitive health assessment by using machine learning algorithms to classify individuals as cognitively healthy, MCI, or dementia based on the collected sensor data | Motion sensors on the ceiling, door sensors on cabinets and doors, and item sensors | IADL |
| Fritz et al., 2019 [27] USA | 4 | Parkinson’s disease | Case series study | Environmental Sensor | To offer practical guidance to nurse investigators interested in multi-disciplinary research that includes assisting in the development of artificial intelligence algorithms for “smart” health management and aging-in-place | Five sensor types: infrared motion, contact, light, temperature, and humidity. The sensors are placed on the ceiling, walls, and doors. | Falls, medications, vital signs, timed up and go test |
| Goldberg et al., 2003 [28] USA | 280 | Heart failure with a left ventricular ejection fraction < or =35% | RCT | Integration between Telemedicine and the use of devices | To determine whether daily reporting of weight and symptoms in patients with advanced heart failure reduce rehospitalization and mortality rates despite aggressive guideline-driven heart failure care | AlertNet: a program with the DayLink monitor and an electronic scale | Hospital readmission rate, mortality, emergency room visitation rate, and quality of life |
| Hayes et al., 2008 [29] USA | 14 | Alzheimer disease | Quasi-experimental | Environmental sensors | To evaluate the use of continuous, long-term, and unobtrusive in-home monitoring to assess neurological function in healthy and cognitively impaired elders | Motion sensor and contact sensor | Walking speed, mobility |
| Jekel et al., 2016 [30] Germany | 21 | Dementia | Pilot study (quasi experimental) | Environmental sensors | To investigate the potential of a smart home environment for the assessment of IADL in MCI | Sensors and video cameras | IADL |
| Kuo et al., 2012 [31] Taiwan | 84 | Stroke | Case series study | Integration between Telemedicine and the use of devices | To present an IT-mediated health- care model as an extension of ordinary chronic care | A machine for measuring several physiological parameters (blood pressure, heart rate, blood sugar, and body temperature) is set up in each patient’s home. | Vital signs (Blood pressure, heart rate, blood sugar, body temperature) |
| Lazarou et al., 2016 [32] Grecee | 4 | Dementia, mild cognitive impairment | Case study | Environmental sensors | To propose a system for continuous and objective remote monitoring of problematic daily living activity areas and design personalized interventions based on system feedback and clinical observations for improving cognitive function and health-related quality of life | Wearable, sleep, object motion, presence, and utility usage sensor | ADL, cognitive functions, daily functionality |
| Lanzarou et al., 2019 [33] Grecee | 18 | Cognitive impairment and Alzheimer’s disease | Observational study | Environmental sensors | (1) To investigate whether the long-term use of sensor-based remote monitoring systems at home can be accepted and sustained (2) To validate the beneficial impact of its long-term use, taking into account the tailored system-driven interventions, among different groups of people with MCI and AD (3) To pilot, maintain, and evaluate the long-term effects (up to a year) of a personalized sensor-based system to support non-pharmacological interventions for people with cognitive impairment, both in preclinical and advanced stages | The Ambient and Wearable Sensors (ambient depth cameras, Plug sensors, tags, presence IRmotion sensor, sleep sensor | Cognitive Functions (memory, attention, etc.) sleep duration and behaviour, physical activity and ADL |
| Rawtaer et al., 2020 [34] Singapore | 49 | Mild Cognitive Impairment | Cross-sectional | Environmental sensors | To establish the feasibility and acceptability of utilizing sensors in the homes of senior citizens to detect changes in behaviours unobtrusively | PIR, bed sensor, a sensor-equipped medication box | Time spent away from home, television use, sleep duration |
| Sacco et al., 2012 [35] France | 35 | Alzheimer’s disease and mild cognitive impairment | Observational study | Video monitoring system | To assess IADL in AD and in MCI through the video monitoring system | Imaging and video processing enables the patients’ performances and actions in real-time and real-life situations to be captured and accurately evaluated | ADL |
| Soran et al., 2010 [36] USA | 315 | Heart failure | RCT | Integration between Telemedicine and the use of devices | To determine if a heart failure disease management program using a computer-based telephonic system for home monitoring, in addition to the targeted and consistent physician/patient education, coupled with assiduous efforts to use optimal medical therapy | Day link monitor: a home-based disease management program to monitor and detect early signs and symptoms of heart failure using telecommunication equipment. The system includes an electronic scale and an individualized symptoms response system linked via a standard phone line to a computerized database staffed by trained nurses | Hospital readmission |
| Urwyler et al., 2017 [37] Switzerland | 20 | Dementia | Observational study | Environmental sensors | (1) To investigate the extent of difference in ADL (both basic ADL and IADL) patterns between the healthy controls and dementia patients and to investigate if the difference in ADL can be used to classify the subjects into the two groups (2) To investigate the influence of the measurement duration on the classification performance | Wireless-unobtrusive sensors | ADL |
| Wakefield et al.,2014 [38] USA | 53 | Diabetes and Hypertension | RCT | Telemonitoring system + in-home devices | To evaluate the effectiveness of short-term targeted use of remote data transmission on treatment outcomes in patients with diabetes who had either out-of-range haemoglobin A1c (A1c) and/or blood pressure measurements | Electronic monitors and data were transferred to a secure Web site | Blood pressure and glucose blood |
| Yu et al., 2019 [39] China | 1 | Chronic diseases | Case study | Environmental sensors | To describe the development of a smart home for elders that uses unobtrusive sensor technology to assess older adults’ daily activities and assist their healthcare services | Wireless sensor networks that value humidity, temperature, electricity usage, closure of doors and windows | ADL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Facchinetti, G.; Petrucci, G.; Albanesi, B.; De Marinis, M.G.; Piredda, M. Can Smart Home Technologies Help Older Adults Manage Their Chronic Condition? A Systematic Literature Review. Int. J. Environ. Res. Public Health 2023, 20, 1205. https://doi.org/10.3390/ijerph20021205
Facchinetti G, Petrucci G, Albanesi B, De Marinis MG, Piredda M. Can Smart Home Technologies Help Older Adults Manage Their Chronic Condition? A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2023; 20(2):1205. https://doi.org/10.3390/ijerph20021205
Chicago/Turabian StyleFacchinetti, Gabriella, Giorgia Petrucci, Beatrice Albanesi, Maria Grazia De Marinis, and Michela Piredda. 2023. "Can Smart Home Technologies Help Older Adults Manage Their Chronic Condition? A Systematic Literature Review" International Journal of Environmental Research and Public Health 20, no. 2: 1205. https://doi.org/10.3390/ijerph20021205
APA StyleFacchinetti, G., Petrucci, G., Albanesi, B., De Marinis, M. G., & Piredda, M. (2023). Can Smart Home Technologies Help Older Adults Manage Their Chronic Condition? A Systematic Literature Review. International Journal of Environmental Research and Public Health, 20(2), 1205. https://doi.org/10.3390/ijerph20021205









