Abstract
Background: Neighborhoods are critical to understanding how environments influence health outcomes. Prolonged environmental stressors, such as a lack of green spaces and neighborhood socioeconomic disadvantage, have been associated with higher allostatic load levels. Since allostatic load levels experienced earlier in life have stronger associations with mortality risk, neighborhoods may be uniquely suited to monitor and mitigate the impacts of environmental stressors. Researchers often study allostatic load in neighborhoods by utilizing administrative boundaries within publicly accessible databases as proxies for neighborhoods. Methods: This systematic review of reviews aims to identify commonly used biomarkers in the measurement of allostatic load, compare measurement approaches, inventory databases to study allostatic load, and spotlight considerations referenced in the literature where allostatic load is studied in neighborhoods. The review was conducted using the search term “allostatic load” in the MEDLINE, CINAHL, and PsychINFO databases. The search results were filtered to include reviews. Results: The search returned 499 articles after deduplication. Overall, 18 synthesis reviews met the inclusion criteria and were retained for extraction. The synthesis reviews analyzed represented 238 studies published from 1995 to 2020. The original ten biomarkers were most often used to measure allostatic load. More recently, body mass index and C-reactive protein have additionally been frequently used to measure allostatic load burden. Conclusions: The scientific contributions of this study are that we have identified a clear gap in geographic considerations when studying allostatic load. The implication of this study is that we have highlighted geographic concepts when conducting neighborhood-level research using administrative databases as a neighborhood proxy and outlined emerging future trends that can enable future study of allostatic load in the neighborhood context.
1. Introduction
Neighborhoods are a setting of research interest for studies that seek to understand how environmental stressors influence future health outcomes. Neighborhoods are where we grow, live, work, and play [1,2]. Since the impacts of allostatic load on all-cause and cardiac-specific mortality are more strongly associated with allostatic load levels experienced earlier in life [3], neighborhoods may be uniquely suited to address the long-term health risks associated with high allostatic load levels. Perceived neighborhood quality [4,5] with increased neighborhood green spaces [6,7], decreased neighborhood disorder [8], and neighborhood socioeconomic advantage [9,10] have all been associated with normal allostatic load. Researchers often study allostatic load in the neighborhood context by utilizing administrative boundaries within publicly accessible databases as proxies for neighborhoods, which may not reflect the actual realities of the people who live in those neighborhoods [11,12].
Allostatic load conceptualizes the biosocial mechanisms of the prolonged activation of the acute stress response [13]. Allostatic load has been conceptually well-established in scientific literature as reflecting the overall wear-and-tear on the body from environmental stresses, and it is considered a precursor of chronic disease development [14,15,16,17]. An initial battery of 10 biomarkers was reported in the seminal work to quantify allostatic load and has since been utilized in research as a cumulative indicator of overall stress adaptation [15,16]. The initial allostatic load battery is composed of four primary mediators (representing biochemical changes in the neuroendocrine system as the stress response is initiated) and six secondary mediators (representing structural remodeling of receptors sites of the cardiovascular, immune, and metabolic systems due to long-term activation of the stress response). The original primary mediators included cortisol, noradrenaline (norepinephrine), adrenaline (epinephrine), and dehydroepiandrosterone (DHEA). These mediators are responsible for triggering the hypothalamic–pituitary–adrenal axis and the sympathetic–adrenal medullary axis cascades of the stress response or are an outcome of the primary cascades. Secondary mediators measure the symptom manifestations of a prolonged stress response. The original six secondary mediators include systolic blood pressure (SBP), diastolic blood pressure (DBP), waist-to-hip ratio (WHR), high-density lipoprotein (HDL), total cholesterol (TC), and glycosylated hemoglobin (HgbA1C) [15,16].
Throughout the initial decades of allostatic load being used in research to conceptualize overall stress burden, the use of biomarkers intended to represent allostatic load became much more varied from study to study [18,19]. In addition, the concept started to be explored as a measure of episodic trauma and not cumulative wear-and-tear over the life-course [20]. Additionally, the utility of allostatic load in settings outside of the initial setting of longevity studies also became prominent [6,21,22,23].
Social epidemiologists started to explore allostatic load as a potential conceptualization of how place-based determinants of health impact the life course of health [24]. Similarly, spatial epidemiologists wanted to better understand how allostatic load interplays with the neighborhood context to determine health. Although the focus on the allostatic load in the neighborhood context is increasing in the literature and doctoral dissertations, a more standardized approach to measuring allostatic load, especially when studying neighborhoods, is needed to compare studies and appraise the overall inferences in the body of literature [25,26].
Aims
This systematic review conceptualizes the allostatic load as a precursor to chronic disease development. This study aims to determine which biomarkers are frequently used in research to measure allostatic load and to provide researchers with database tools to examine allostatic load and the geographic considerations for studying allostatic load in the neighborhood context. To address these aims, this systematic review focuses on evaluating systematic reviews in published, peer-reviewed health sciences literature.
2. Materials and Methods
The design of this study is a systematic review of reviews (also termed an “umbrella review”). The search strategy for this approach focuses on the identification and examination of systematic reviews, meta-analyses, and other forms of synthesized literature. A systematic review of reviews serves as an accepted and valuable method to gain a clear understanding of the specific aspects of a broad topic area [27].
The inclusion criteria for this study were that each included article was a meta-analysis, systematic review, or high-quality synthesis review. Other inclusion criteria included the following: English language, publication in a peer-reviewed journal, human subjects, and use of biomarkers to measure allostatic load. Animal studies were excluded.
Since the first two of the three aims were focused on the measurement of allostatic load as a general concept, we did not limit the search terms by geography. Using the search term “allostatic load,” a search was conducted on 6 July 2021, in the following databases: MEDLINE (through PubMed), CINAHL (through EBSCOhost), and PsychINFO (through the American Psychological Association). The results were filtered by the inclusion criteria described above and limited to reviews published between 2003 and 2021. We knew from previous searches that the first synthesis review was published in 2003 and the search was conducted in 2021. The search results were imported into Covidence [28], a software program for systematic reviews, and independently screened by investigators for the inclusion criteria. Two investigators (S.B., J.M.G.) independently reviewed the articles to assess if the inclusion criteria were met. The articles included in the study are hereafter referred to as synthesis reviews.
The following information was extracted from each synthesis review: the review type, the number of studies reviewed, the purpose of the study, the population addressed, and whether potential conflicts of interest were addressed. Additional information extracted from each synthesis article included biomarkers used to determine the biomarker frequency, the measurement approach for allostatic load, and the databases used in the study. Each database identified in the synthesis reviews was searched to determine whether neighborhood measures were available in each database. This systematic review was not registered. All the study procedures adhered to the PRISMA 2020 Statement Checklist.
Quality Appraisal
Protocols to eliminate selection bias are essential in systematic reviews seeking to inform practice [29,30]. The AMSTAR-2 was used as the quality appraisal tool in this study [30]. This tool, designed to aid in the critical appraisal of systematic reviews that synthesize healthcare studies, is validated with reviews that include randomized control and non-randomized control trials that evaluate health, such as observational studies [31].
Cohen’s Kappa was utilized to determine interrater reliability. Covidence™ software (Veritas Health Innovation Ltd., Melbourne, Australia) was utilized to calculate Cohen’s Kappa. We reconciled any discrepancies in the quality appraisals of the AMSTAR-2 scoring through consensus. To determine the overall quality of the synthesis reviews, we calculated the total scores using the AMSTAR-2 tool. The responses “Yes,” “Partial,” and “No,” were assigned numeric values, so “Yes” = 1, “Partial” = 0.5, and “No” = 0 (maximum possible score: 16). Synthesis reviews with AMSTAR-2 scores within the interquartile range were considered “average” quality, while those with scores below and above the interquartile range were classified as “weak” and “strong,” respectively.
3. Results
The initial search returned 571 articles with 72 duplications (Figure 1). Two investigators independently screened the title and abstract of 499 articles and full-text reviews of 45 articles. Overall, 18 synthesis reviews met the inclusion and exclusion criteria and were extracted for analysis. These synthesis reviews represent 238 studies published from 1995 to 2020. All 238 individual studies were cross-referenced across the synthesis review to remove duplicates. There were cases where individual studies were included in multiple synthesis reviews; however, the biomarkers of the 238 individual studies were only accounted for once in the analysis.
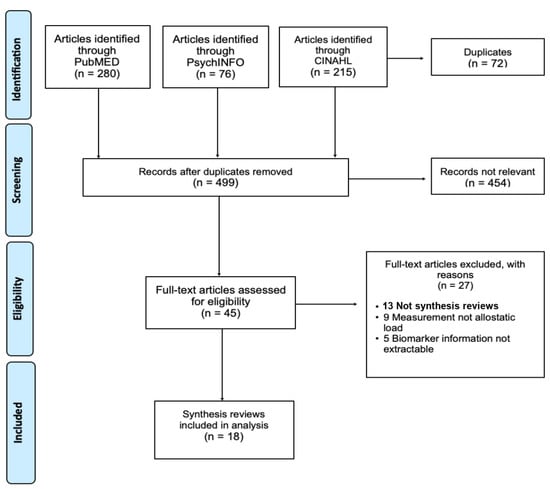
Figure 1.
PRISMA Algorithm for the systematic literature search for “allostatic load” conducted on 6 July 2021.
3.1. Interrater Reliability
Cohen’s Kappa was used to determine the agreement between the two independent reviewers for the relevance screening of the articles using the title/abstract and full-text review to assess whether the inclusion criteria were met. There was moderate agreement between the reviewers for the title/abstract screening phase (Cohen’s κ = 0.533) and almost perfect agreement for the full-text reviews (κ = 0.82). We resolved discrepancies in the rating through discussion and consensus.
3.2. Characteristics of the Included Reviews
Ten out of eighteen synthesis reviews self-identified as systematic reviews (n = 8) or systematic reviews combined with meta-analyses (n = 2). Other article types included as synthesis reviews were literature reviews (n = 3), perspective reviews (n = 3), a scoping review (n = 1), and a narrative review (n = 1). We analyzed the individual studies described in each synthesis review (range: 6 to 61 studies, mean: 19, median: 23.3). Potential conflicts of interest were explicitly addressed in 66.6% of the synthesis reviews by explicitly stating no conflicts of interest exist or including a statement of the conflicts of interest with an explanation. In total, 33.3% of the synthesis reviews did not acknowledge a conflict of interest in any way within the text of the manuscript. The purpose and description of the population of each synthesis review are summarized in Table 1. Only one of the synthesis reviews included any geographic considerations for studying allostatic load.
3.3. Quality of Research and Potential Bias
We used AMSTAR-2 to individually appraise each of the 18 synthesis reviews (Table 1). The AMSTAR-2 scores of the synthesis reviews ranged from 1.5 to 12.5, with a mean of 5.9 (standard deviation: 3.0, interquartile range: 9.0–3.0). Two-thirds (66.6%) of the synthesis reviews were classified as average (scores within the interquartile range), while 22.2% and 11.1% were classified as weak and strong, respectively. The synthesis reviews classified as weak failed to account for bias in the inclusion and exclusion protocols, did not include how bias was addressed, or explicitly stated potential conflicts of interest. The reviews rated as strong explicitly used pre-stated protocols for the inclusion criteria, provided a robust description of the role of bias in selecting individual studies, and included a quality appraisal of the individual studies reviewed.
To mitigate potential bias for this umbrella review, we developed a formal protocol with defined inclusion and exclusion criteria prior to conducting our search. We used two independent reviewers for a title/abstract screen and full-text review. All conflicts of interest were disclosed.
3.4. Biomarker Frequency
The most frequently utilized primary mediator was cortisol (n = 134). Cortisol was used in 56.3% of the 238 studies represented in the 18 synthesis reviews (Figure 2). Epinephrine was used in 39.9% (n = 95) and norepinephrine in 39.4% (n = 94) of the individual studies represented in our analysis. Dehydroepiandrosterone was used in 34.0% (n = 81) of the extracted studies. The final two primary mediators that were used in relatively few studies over the years, but were not part of the original biomarkers, were heart-rate variability (n = 20, 8.4%) and dopamine (n = 11, 4.6%).
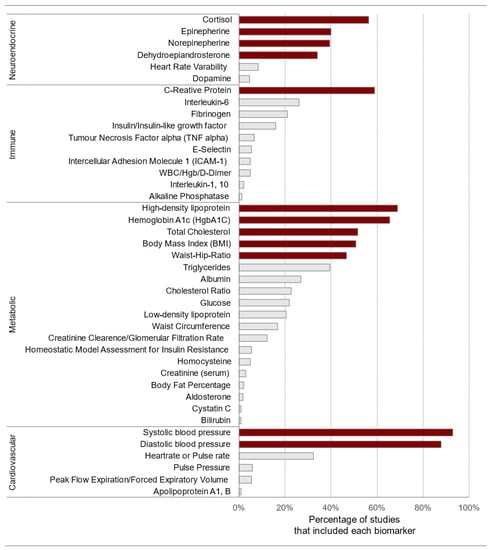
Figure 2.
Biomarker use frequency extracted from 18 synthesis reviews identified through a systematic literature search for “allostatic load” conducted on 6 July 2021. The darker shaded biomarkers are the original 10, body mass index, and C-reactive protein. Note: HgbA1C = glycosylated hemoglobin; white blood cell count (WBC), hemoglobin (Hgb).
The most frequently used secondary mediators included cardiovascular biomarkers of systolic blood pressure (n = 221, 92.8%) and diastolic blood pressure (n = 209, 87.8%). The lesser-used cardiovascular biomarkers that appeared in the literature were heart rate/pulse rate (n = 77, 32.3%), pulse pressure (n = 14, 5.8%), peak flow expiratory (n = 13, 5.4%), and apolipoprotein A1, B (n = 2, 0.8%). Among the metabolic system biomarkers, the most frequently used were high-density lipoprotein (n = 164, 68.9%), glycosylated hemoglobin (n = 156, 66.6%), total cholesterol (n = 123, 51.6%), body mass index (n = 121, 50.8%), and waist-to-hip ratio (n = 111, 46.6%). C-reactive protein (n = 140, 58.8%), interleukin-6 (n = 62, 26.0%), and fibrinogen (n = 50, 21.0%) were the most frequently used immune system biomarkers. In addition to these metabolic and immune biomarkers, there were 14 more metabolic biomarkers with a frequency of usage ranging from 39.4% to 0.8% and 7 additional immune biomarkers with a frequency of usage ranging from 15.9% to 1.2%.
Traditionally, two primary approaches have been used to calculate allostatic load scores. A frequently used method to calculate allostatic load is to evenly weigh all the biomarkers in a composite measure representing the sum of the measured biomarkers, whereby each is coded as “0” for normal/low findings or “1” for high findings (per nationally established ranges). High allostatic loads are determined by summing the score. High allostatic load risk is determined when three or more biomarkers are in high-risk ranges [11,18]. The most frequently used method of calculation is some variation of the original calculation of using extreme quantiles, such as the 10/90th percentile, per biomarker to determine the acceptable range. There is no consistent quantile cut-off; the researchers of individual studies describe the percentiles for all the biomarkers and justify the cut-off defined by the research team [18,19,32,33]. A third method used is to use z-scores; however, this calculation method is used far less frequently than the two primary methods. A wide variation persists among the studies included in the synthesis reviews if calculation methods were examined and discussed.

Table 1.
Characteristics of the analyzed articles extracted from 18 synthesis article reviews identified through a systematic literature search for “allostatic load” conducted on 6 July 2021.
Table 1.
Characteristics of the analyzed articles extracted from 18 synthesis article reviews identified through a systematic literature search for “allostatic load” conducted on 6 July 2021.
| References | Review Type | Number of Studies | AMSTAR2 Quality | Purpose of Review | Population Addressed | Conflicts of Interest Addressed |
|---|---|---|---|---|---|---|
| Szanton et al., 2005 [34] | Systematic review | 10 [15,35,36,37,38,39,40,41,42,43] | Average | Examine and synthesize the literature on allostatic load as a construct to understand and qualify health disparities. | Target population is unspecified. | Yes |
| Dowd et al., 2009 [44] | Systematic review | 7 [35,36,42,45,46,47,48] | Average | Review of the existing literature on socioeconomic status and cortisol, as well as allostatic load. | Target population is unspecified. | Yes |
| Juster et al., 2010 [49] | Literature review | 59 [15,16,35,36,37,39,40,41,42,43,45,46,47,48,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89] | Average | Review of the existing literature on the theoretical and empirical work that exists on allostatic load. | Target population is unspecified. | No |
| Beckie, 2012 [90] | Systematic review | 58 [15,16,35,36,37,38,39,40,41,42,43,45,46,48,49,53,58,59,60,61,62,63,64,67,68,69,74,75,77,78,82,83,84,85,86,87,88,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110] | Average | Review of the existing literature to synthesize the state of the science on allostatic load over the life span. | Target population variable and specified by study. | Yes |
| Mauss et al., 2015 [111] | Systematic review | 16 [40,67,73,74,75,78,82,84,104,112,113,114,115,116] | Average | Examine and synthesize literature on allostatic load measurement, operational measures, and biomarkers used in measurement. | Target population is workers, context specified by studies. | No |
| Duong et al., 2017 [18] | Perspective review | 20 [48,54,58,80,87,93,95,100,117,118,119,120,121,122,123,124,125,126,127,128] | Weak | Review of the calculation of allostatic load studies that used NHANES data 1988 and 2010. | Target population variable and specified by study. | Yes |
| Johnson et al., 2017 [19] | Literature review | 26 [35,36,73,81,87,89,94,101,113,114,120,122,128,129,130,131,132,133,134,135,136,137,138,139,140,141] | Average | Review of the biomarkers and methods used to analyze the association between allostatic load and socioeconomic position. | Target population is unspecified. | No |
| Rosemberg et al., 2017 [142] | Perspective review | 12 [40,66,67,76,78,84,96,108,143,144,145] | Weak | Elucidate and synthesize the historical development of the allostatic load and its use in nursing research. | Two stress-vulnerable populations, workers, and women of childbearing age. | No |
| Wiley et al., 2017 [32] | Systematic review | 24 [36,38,40,41,50,53,72,76,103,106,113,133,141,146,147,148,149,150,151,152,153,154,155,156] | Average | Explore and synthesize the literature on allostatic load and with psychological/social resources. | Target population is unspecified. | Yes |
| Ribeiro et al., 2018 [11] | Scoping review | 14 [9,87,94,130,145,147,157,158,159,160,161,162,163,164] | Average | Explore and synthesize the literature on allostatic load and neighborhood socioeconomic deprivation. | Target population is unspecified. | Yes |
| Larrabee Sonderland et al., 2019 [165] | Systematic review | 20 [38,41,47,53,72,76,103,133,141,147,152,153,155,156,166,167,168,169,170,171] | Average | Review of the relationship between everyday stress, social connectedness, and allostatic load. | Target population variable and specified by study. | Yes |
| D’Amico et al., 2020 [33] | Systematic review and meta-analysis | 18 [15,16,37,59,63,98,118,172,173,174,175,176,177,178,179,180,181,182] | Strong | Investigate the association between allostatic load and standardized cognitive test among adults. | The target population is 18 and older. | Yes |
| Ketheesan et al., 2020 [183] | Narrative review | 6 [184,185,186,187,188,189] | Weak | Explore and synthesize the literature on allostatic load and mental health disparities observed between indigenous and non-indigenous Australians. | Target population is indigenous Australians, age unspecified. | No |
| Kerr et al., 2020 [190] | Systematic review | 61 [38,40,54,57,60,66,67,73,78,82,86,92,100,102,103,106,112,113,117,135,137,146,148,149,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227] | Average | To assess sex differences in allostatic load and identify allostatic load associations that are specific to women. | Target population is women, ages specified by study. | Yes |
| Misiak, 2020 [228] | Perspective review | 9 [202,215,229,230,231,232,233,234,235] | Weak | Explore and synthesize the literature on allostatic load and psychotic disorders. | People diagnosed with a psychotic disorder; characteristics specified by study. | No |
| Suvarna et al., 2020 [236] | Systematic review | 24 [9,46,83,92,101,117,128,140,161,214,237,238,239,240,241,242,243,244,245,246,247,248,249,250] | Average | Examine and synthesize the literature on allostatic load and health-related behaviors. | Target population variable and specified by study. | Yes |
| Mathew et al., 2021 [251] | Systematic review and meta-analysis | 12 [109,121,124,211,252,253,254,255,256,257,258,259] | Strong | Explore and synthesize the literature on allostatic load and cancer. | People diagnosed with cancer; characteristics specified by study. | Yes |
| Whelan et al., 2021 [260] | Literature review | 24 [81,120,122,136,146,147,149,151,152,161,187,197,261,262,263,264,265,266,267,268,269,270,271,272] | Average | Identify and synthesize the literature on variations of allostatic load measurement and cancer. | Target population is adolescents. | Yes |
3.5. Database Inventory
Multiple studies that were reviewed used secondary databases to determine allostatic load. We extracted those databases from the individual studies included in the synthesis reviews and inventoried them. A full description of each database, including the web address and the allostatic biomarkers the researcher can access in the database, is presented in Supplemental Material Table S1. The United States databases identified in the review were the Multi-Ethnic Study of Atherosclerosis (MESA) [273,274,275], the Community Child Health Research Network (CCHN) [276,277], Midlife in the United States (MIDUS) [278], the Jackson Heart Study [279], and the National Archive of Computerized Data on Aging (NACDA) [280]. The databases that provide georeferenced biomarker data include the National Health and Nutrition Examination Survey (NHANES) [281], and the Health and Retirement Study (HRS) [282].
4. Discussion
This study aimed to identify the frequency of biomarkers used to measure allostatic load in the published literature. Unsurprisingly, the findings demonstrated that the original ten biomarkers were most often used to measure allostatic load. More recently, body mass index and C-reactive protein biomarkers have started being used to reflect metabolic pathways and inflammation.
A detailed account of how allostatic load was calculated by each of the individual studies reviewed within the synthesis review was provided in 13 of the 18 synthesis reviews included in this study. One comment, “The 21 studies calculated ALS (allostatic load score) in 18 different ways using 26 different biomarkers” fairly characterized the findings from all the synthesis reviews that examined allostatic load calculations. There is wide variation in how allostatic load is calculated; however, we have summarized the most frequently used methods found for each of the synthesis reviews (noted in Supplemental Materials Table S1).
4.1. Geographic Consideration in Neighborhood Research
A secondary aim of this systematic review was to spotlight geographic considerations for researchers conducting research at the neighborhood level. There was a marked gap in the literature regarding geographic considerations when studying allostatic load. Only one synthesis review, by Ribeiro et al., addressed geographic considerations from all the synthesis reviews included in this study.
There are four common biases to be aware of when using administrative databases to study neighborhoods, two of which are noted in the literature reviewed [11]. Administrative proxies include census data and areal-level public and private databases. First, ecological fallacies arise when inferences about the characteristics of one scale form the conclusions at a different scale (e.g., inferences about an individual based on neighborhood characteristics). Three criteria must be satisfied to establish an ecological fallacy: (a) the findings must result from the use of population data, (b) the results must be inferred to the individual level, and (c) there must be individual data that contradict the findings [283].
Second, the observations attributed to the neighborhood defined by administrative boundaries may differ from the actual neighborhood attributes. This difference is called the Modifiable Areal Unit Problem (MAUP). The MAUP is especially significant when using choropleths and should be addressed in the literature [284].
Third, a bias that can be created is the Uncertain Geographic Context Problem (UGCoP). This is the acknowledgement that using geographic (neighborhood) exposure context is not fully understood by the researcher. The amount of time individuals have lived in the studied neighborhood, the ground realities, and the amount of time individuals are exposed to environments that are not their neighborhood all need to be considered when interpreting neighborhood findings [11].
One last consideration for neighborhood researchers to be aware of was not found in our review but is nonetheless an important concept for neighborhood researchers. Tobler’s first law of geography states, “everything is related to everything else, but near things are more related than distant things” [285]. Spatial autocorrelation/dependence refers to the degree of autocorrelation that must be accounted for statistically. Assessing and adjusting for spatial dependence requires understanding the nature of clustering and dispersion patterns [286].
Several barriers to accessing georeferenced biomarker data exist. For example, restricted data-center application processes may require a time horizon of multiple months (this is the case for NHANES). The fees for accessing restricted data may also limit researchers’ ability to conduct geographic analyses using these data sources. For example, accessing NHANES via the Restricted Data Center requires a minimum application cost of USD 3000.
Additionally, the All of Us database [287], a racially, ethnically, and regionally diverse national database, is relatively new (initial release in 2018). This may explain why it was not identified in our analysis. Nonetheless, we included All of Us in our inventory as an additional tool for allostatic load researchers (noted in Supplemental Materials Table S2).
4.2. Future Trends in Allostatic Load Measurement
There is a movement within the allostatic load measurement community to operationalize allostatic load measurement for clinical application [288]. “Clinimetrics” represents the science of clinically applicable metrics [289]. Allostatic load clinimetrics can hold utility in both the primary care setting and the neighborhood context [290]. An example of a potential clinimetrics measurement would be the development of a clinical tool that explores the associations between Adverse Childhood Experience (ACE) scores and the development of high allostatic load [22,291]. Studies that examine both clinimetrics criteria and biomarkers present an exciting new realm of allostatic load inquiry.
Another horizon in allostatic load research is studying whether even weighting of biomarkers is the best method of allostatic load calculation. Are some biomarkers more predictive of overall wear-and-tear than others? A recent study that used the item response theory explored biomarker weighting using 2015–2016 NHANES data. The study concluded that body mass index and C-reactive protein were the most informative biomarkers [292].
The last horizon in allostatic load research is validity testing, which aims to use streamlined composites using fewer biomarkers. One recent study established that 5 biomarkers are highly associated with the allostatic load composite of the original 10 biomarkers [293]. The five streamlined biomarkers are diastolic blood pressure, glycosylated hemoglobin, low-density lipoprotein, waist circumference, and the heart-rate variability measure of the root mean square of the successive difference between normal heartbeats. This could be valuable for future research, as heart-rate variability is a biomarker that can be obtained from wearable devices. This reduces the laboratory testing to glycosylated hemoglobin and low-density lipoprotein.
4.3. Limitations
The primary limitation of this systematic review of reviews was choosing the AMSTAR-2 as our quality-appraisal tool. The AMSTAR-2 is designed to appraise systematic reviews of healthcare interventions. Many of the studies included in the synthesis reviews were observational studies and did include an intervention. However, we used the AMSTAR-2 because it fit most of the study designs and is a reputable/rigorous tool for appraising the quality of review literature.
5. Conclusions
This systematic review of reviews summarizes the current state of the art of measuring allostatic load. We identify the most frequently used biomarkers and present standardized practices for calculating allostatic load.
We include the historical perspective of allostatic load biomarkers and calculation variations and highlight crucial conceptual neighborhood considerations for studying allostatic load in neighborhood contexts. The inventory of public databases that include commonly used biomarkers is intended to facilitate future research on allostatic load.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijerph192417006/s1, Table S1: Allostatic Load Calculation Methods extracted from 18 synthesis reviews identified through a systematic literature search for “allostatic load” conducted on 6 July 2021; Table S2: Database inventory extracted from 18 synthesis reviews identified through a systematic literature search for “allostatic load” conducted on 6 July 2021.
Author Contributions
Conceptualization, S.B. and J.M.G.; methodology, S.B. and J.M.G.; formal analysis, S.B.; writing—original draft preparation, S.B.; writing—review and editing, J.M.G. and J.P.; visualization, S.B. and J.M.G.; supervision, J.M.G. and J.P. All authors have read and agreed to the published version of the manuscript.
Funding
The dissemination of this research was partly funded by a Carl M. Hansen Foundation Scholarship, awarded to Shawna Beese in 2022.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Shawna Beese’s PhD dissertation committee, including Gail Oneal (co-chair) and Kevin Murphy.
Conflicts of Interest
This manuscript was prepared as partial fulfillment of the PhD dissertation of the first author, Shawna Beese.
References
- Braveman, P.; Gottlieb, L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014, 129 (Suppl. S2), 19–31. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, E. Environmental justice: An interview with Robert Bullard. Earth First J. 1999, 19, 8. [Google Scholar]
- Parker, H.W.; Abreu, A.M.; Sullivan, M.C.; Vadiveloo, M.K. Allostatic Load and Mortality: A Systematic Review and Meta-Analysis. Am. J. Prev. Med. 2022, 63, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Buschmann, R.N.; Prochaska, J.D.; Cutchin, M.P.; Peek, M.K. Stress and health behaviors as potential mediators of the relationship between neighborhood quality and allostatic load. Ann. Epidemiol. 2018, 28, 356–361. [Google Scholar] [CrossRef]
- Carbone, J.T. Neighborhood perceptions and allostatic load: Evidence from Midlife in the United States study. Health Place. 2020, 61, 102263. [Google Scholar] [CrossRef]
- Egorov, A.I.; Griffin, S.M.; Converse, R.R.; Styles, J.N.; Sams, E.A.; Wilson, A.; Jackson, L.E.; Wade, T.J. Vegetated land cover near residence is associated with reduced allostatic load and improved biomarkers of neuroendocrine, metabolic and immune functions. Environ. Res. 2017, 158, 508–521. [Google Scholar] [CrossRef]
- Egorov, A.I.; Griffin, S.M.; Converse, R.R.; Styles, J.N.; Klein, E.; Scott, J.; Sams, E.A.; Hudgens, E.E.; Wade, T.J. Greater tree cover near residence is associated with reduced allostatic load in residents of central North Carolina. Environ. Res. 2020, 186, 109435. [Google Scholar] [CrossRef]
- Carbone, J.T. The mediating effect of allostatic load on the relationship between neighborhood perceptions and depression. SSM Popul. Health 2020, 11, 100638. [Google Scholar] [CrossRef]
- Robinette, J.W.; Charles, S.T.; Almeida, D.M.; Gruenewald, T.L. Neighborhood features and physiological risk: An examination of allostatic load. Health Place 2016, 41, 110–118. [Google Scholar] [CrossRef]
- Rodriguez, J.M.; Karlamangla, A.S.; Gruenewald, T.L.; Miller-Martinez, D.; Merkin, S.S.; Seeman, T.E. Social stratification and allostatic load: Shapes of health differences in the MIDUS study in the United States. J. Biosoc. Sci. 2019, 51, 627–644. [Google Scholar] [CrossRef]
- Ribeiro, A.; Amaro, J.; Lisi, C.; Fraga, S. Neighborhood Socioeconomic Deprivation and Allostatic Load: A Scoping Review. Int. J. Environ. Res. Public Health 2018, 15, 1092. [Google Scholar] [CrossRef] [PubMed]
- Diez, J.; Cebrecos, A.; Galán, I.; Pérez-Freixo, H.; Franco, M.; Bilal, U. Assessing the Retail Food Environment in Madrid: An Evaluation of Administrative Data against Ground Truthing. Int. J. Environ. Res. Public Health 2019, 16, 3538. [Google Scholar] [CrossRef]
- McEwen, B.S.; Stellar, E. Stress and the individual. Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Stress and Hippocampal Plasticity. Annu. Rev. Neurosci. 1999, 22, 105–122. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; Singer, B.H.; Rowe, J.W.; Horwitz, R.I.; McEwen, B.S. Price of adaptation—Allostatic load and its health consequences. MacArthur studies of successful aging. Arch. Intern. Med. 1997, 157, 2259–2268. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; McEwen, B.S.; Rowe, J.W.; Singer, B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA 2001, 98, 4770–4775. [Google Scholar] [CrossRef]
- McEwen, B.S.; Lasley, E.N. The End of Stress as We Know It; Joseph Henry Press: Washington, DC, USA, 2002. [Google Scholar]
- Duong, M.T.; Bingham, B.A.; Aldana, P.C.; Chung, S.T.; Sumner, A.E. Variation in the Calculation of Allostatic Load Score: 21 Examples from NHANES. J. Racial Ethn. Health Disparities 2017, 4, 455–461. [Google Scholar] [CrossRef]
- Johnson, S.C.; Cavallaro, F.L.; Leon, D.A. A systematic review of allostatic load in relation to socioeconomic position: Poor fidelity and major inconsistencies in biomarkers employed. Soc. Sci. Med. 2017, 192, 66–73. [Google Scholar] [CrossRef]
- Casavant, S.G.; Cong, X.; Fitch, R.H.; Moore, J.; Rosenkrantz, T.; Starkweather, A. Allostatic Load and Biomarkers of Stress in the Preterm Infant: An Integrative Review. Biol. Res. Nurs. 2019, 21, 210–223. [Google Scholar] [CrossRef]
- Castagné, R.; Garès, V.; Karimi, M.; Chadeau-Hyam, M.; Vineis, P.; Delpierre, C.; Kelly-Irving, M.; Lifepath Consortium. Allostatic load and subsequent all-cause mortality: Which biological markers drive the relationship? Findings from a UK birth cohort. Eur. J. Epidemiol. 2018, 33, 441–458. [Google Scholar] [CrossRef]
- Finlay, S.; Roth, C.; Zimsen, T.; Bridson, T.L.; Sarnyai, Z.; McDermott, B. Adverse childhood experiences and allostatic load: A systematic review. Neurosci. Biobehav. Rev. 2022, 136, 104605. [Google Scholar] [CrossRef] [PubMed]
- Prior, L. Allostatic Load and Exposure Histories of Disadvantage. Int. J. Environ. Res. Public Health 2021, 18, 7222. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N. Epidemiology and the People’s Health: Theory and Context; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health: Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef]
- Duncan, D.T.; Kawachi, I. (Eds.) Neighborhoods and Health, 2nd ed.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. 2021. Available online: https://www.Covidence.Org (accessed on 6 July 2021).
- Shea, B.J.; Bouter, L.; Peterson, J.; Boers, M.; Andersson, N.; Ortiz, Z.; Ramsay, T.; Bai, A.; Shukla, V.K.; Grimshaw, J. External Validation of a Measurement Tool to Assess Systematic Reviews (AMSTAR). PLoS ONE 2007, 2, e1350. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Ma, L.L.; Wang, Y.Y.; Yang, Z.H.; Huang, D.; Weng, H.; Zeng, X.T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- Wiley, J.F.; Bei, B.; Bower, J.E.; Stanton, A.L. Relationship of Psychosocial Resources With Allostatic Load: A Systematic Review. Psychosom. Med. 2017, 79, 283–292. [Google Scholar] [CrossRef]
- D’Amico, D.; Amestoy, M.E.; Fiocco, A.J. The association between allostatic load and cognitive function: A systematic and meta-analytic review. Psychoneuroendocrinology 2020, 121, 104849. [Google Scholar] [CrossRef]
- Szanton, S.L.; Gill, J.M.; Allen, J.K. Allostatic Load: A Mechanism of Socioeconomic Health Disparities? Biol. Res. Nurs. 2005, 7, 7–15. [Google Scholar] [CrossRef]
- Kubzansky, L.D.; Kawachi, I.; Sparrow, D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: Any help from the concept of allostatic load? Ann. Behav. Med. Publ. Soc. Behav. Med. 1999, 21, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Singer, B.; Ryff, C.D. Hierarchies of life histories and associated health risks. Ann. N. Y. Acad. Sci. 1999, 896, 96–115. [Google Scholar] [CrossRef] [PubMed]
- Karlamangla, A.S.; Singer, B.H.; McEwen, B.S.; Rowe, J.W.; Seeman, T.E. Allostatic load as a predictor of functional decline. MacArthur studies of successful aging. J. Clin. Epidemiol. 2002, 55, 696–710. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; Singer, B.H.; Ryff, C.D.; Dienberg Love, G.; Levy-Storms, L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom. Med. 2002, 64, 395–406. [Google Scholar] [CrossRef]
- Crimmins, E.M.; Johnston, M.; Hayward, M.; Seeman, T. Age differences in allostatic load: An index of physiological dysregulation. Exp. Gerontol. 2003, 38, 731–734. [Google Scholar] [CrossRef]
- Schnorpfeil, P.; Noll, A.; Schulze, R.; Ehlert, U.; Frey, K.; Fischer, J.E. Allostatic load and work conditions. Soc. Sci. Med. 2003, 57, 647–656. [Google Scholar] [CrossRef]
- Weinstein, M.; Goldman, N.; Hedley, A.; Yu-Hsuan, L.; Seeman, T. Social linkages to biological markers of health among the elderly. J. Biosoc. Sci. 2003, 35, 433–453. [Google Scholar] [CrossRef]
- E Seeman, T.; Crimmins, E.; Huang, M.-H.; Singer, B.; Bucur, A.; Gruenewald, T.; Berkman, L.F.; Reuben, D.B. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc. Sci. Med. 2004, 58, 1985–1997. [Google Scholar] [CrossRef]
- Seplaki, C.L.; Goldman, N.; Weinstein, M.; Lin, Y.H. How are biomarkers related to physical and mental well-being? J. Gerontol. Biol. Sci. Med. Sci. 2004, 59, 201–217. [Google Scholar] [CrossRef]
- Dowd, J.B.; Simanek, A.M.; Aiello, A.E. Socio-economic status, cortisol and allostatic load: A review of the literature. Int. J. Epidemiol. 2009, 38, 1297–1309. [Google Scholar] [CrossRef]
- Dowd, J.B.; Goldman, N. Do biomarkers of stress mediate the relation between socioeconomic status and health? J. Epidemiol. Community Health 2006, 60, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Wagle, N.; Goldman, N.; Weinstein, M.; Seeman, T.E. The associations between socioeconomic status, allostatic load and measures of health in older Taiwanese persons: Taiwan social environment and biomarkers of aging study. J. Biosoc. Sci. 2007, 39, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Gersten, O. Neuroendocrine biomarkers, social relations, and the cumulative costs of stress in Taiwan. Soc. Sci. Med. 2008, 66, 507–519. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.; Merkin, S.S.; Crimmins, E.; Koretz, B.; Charette, S.; Karlamangla, A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994). Soc. Sci. Med. 2008, 66, 72–87. [Google Scholar] [CrossRef] [PubMed]
- Juster, R.P.; McEwen, B.S.; Lupien, S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010, 35, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev. Psychol. 2003, 39, 924–933. [Google Scholar] [CrossRef]
- Von Känel, R.; Dimsdale, J.E.; Patterson, T.L.; Grant, I. Acute procoagulant stress response as a dynamic measure of allostatic load in Alzheimer caregivers. Ann. Behav. Med. Publ. Soc. Behav. Med. 2003, 26, 42–48. [Google Scholar] [CrossRef]
- Hellhammer, J.; Schlotz, W.; Stone, A.A.; Pirke, K.M.; Hellhammer, D. Allostatic load, perceived stress, and health: A prospective study in two age groups. Ann. N. Y. Acad. Sci. 2004, 1032, 8–13. [Google Scholar] [CrossRef]
- Seeman, T.; Glei, D.; Goldman, N.; Weinstein, M.; Singer, B.; Lin, Y.H. Social relationships and allostatic load in Taiwanese elderly and near elderly. Soc. Sci. Med. 2004, 59, 2245–2257. [Google Scholar] [CrossRef]
- Allsworth, J.E.; Weitzen, S.; Boardman, L.A. Early age at menarche and allostatic load: Data from the Third National Health and Nutrition Examination Survey. Ann. Epidemiol. 2005, 15, 438–444. [Google Scholar] [CrossRef]
- Goldman, N.; Glei, D.A.; Seplaki, C.; Liu, I.W.; Weinstein, M. Perceived stress and physiological dysregulation in older adults. Stress Amst. Neth. 2005, 8, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; McEwen, B.S.; Huang, B.; Dolan, L.M.; Adler, N.E. Social inequalities in biomarkers of cardiovascular risk in adolescence. Psychosom. Med. 2005, 67, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, M.L.; Kaprio, J.; Pulkkinen, L. Allostatic Load of Men and Women in Early Middle Age. J. Individ. Differ. 2005, 26, 20–28. [Google Scholar] [CrossRef]
- Geronimus, A.T.; Hicken, M.; Keene, D.; Bound, J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health 2006, 96, 826–833. [Google Scholar] [CrossRef]
- Seplaki, C.L.; Goldman, N.; Weinstein, M.; Lin, Y.H. Measurement of cumulative physiological dysregulation in an older population. Demography 2006, 43, 165–183. [Google Scholar] [CrossRef]
- Glover, D.A.; Stuber, M.; Poland, R.E. Allostatic load in women with and without PTSD symptoms. Psychiatry 2006, 69, 191–203. [Google Scholar] [CrossRef][Green Version]
- Goertzel, B.N.; Pennachin, C.; de Souza Coelho, L.; Maloney, E.M.; Jones, J.F.; Gurbaxani, B. Allostatic load is associated with symptoms in chronic fatigue syndrome patients. Pharmacogenomics 2006, 7, 485–494. [Google Scholar] [CrossRef]
- Goldman, N.; Turra, C.M.; Glei, D.A.; Seplaki, C.L.; Lin, Y.H.; Weinstein, M. Predicting mortality from clinical and nonclinical biomarkers. J. Gerontol. Biol. Sci. Med. Sci. 2006, 61, 1070–1074. [Google Scholar] [CrossRef]
- Goldman, N.; Turra, C.M.; Glei, D.A.; Lin, Y.H.; Weinstein, M. Physiological dysregulation and changes in health in an older population. Exp. Gerontol. 2006, 41, 862–870. [Google Scholar] [CrossRef]
- Gruenewald, T.L.; Seeman, T.E.; Ryff, C.D.; Karlamangla, A.S.; Singer, B.H. Combinations of biomarkers predictive of later life mortality. Proc. Natl. Acad. Sci. USA 2006, 103, 14158–14163. [Google Scholar] [CrossRef]
- Karlamangla, A.S.; Singer, B.H.; Seeman, T.E. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom. Med. 2006, 68, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Lindfors, P.; Lundberg, O.; Lundberg, U. Allostatic load and clinical risk as related to sense of coherence in middle-aged women. Psychosom. Med. 2006, 68, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Von Thiele, U.; Lindfors, P.; Lundberg, U. Self-rated recovery from work stress and allostatic load in women. J. Psychosom. Res. 2006, 61, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.S.; Bond, M.J.; Hecker, J.R. Environmental stress, psychological stress and allostatic load. Psychol. Health Med. 2007, 12, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Crews, D.E. Composite estimates of physiological stress, age, and diabetes in American Samoans. Am. J. Phys. Anthropol. 2007, 133, 1028–1034. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, E.M.; Kim, J.K.; Alley, D.E.; Karlamangla, A.; Seeman, T. Hispanic paradox in biological risk profiles. Am. J. Public Health 2007, 97, 1305–1310. [Google Scholar] [CrossRef]
- Evans, G.W.; Kim, P.; Ting, A.H.; Tesher, H.B.; Shannis, D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev. Psychol. 2007, 43, 341–351. [Google Scholar] [CrossRef]
- Glei, D.A.; Goldman, N.; Chuang, Y.L.; Weinstein, M. Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosom. Med. 2007, 69, 769–776. [Google Scholar] [CrossRef]
- Johansson, G.; Huang, Q.; Lindfors, P. A life-span perspective on women’s careers, health, and well-being. Soc. Sci. Med. 2007, 65, 685–697. [Google Scholar] [CrossRef]
- Langelaan, S.; Bakker, A.B.; Schaufeli, W.B.; van Rhenen, W.; van Doornen, L.J.P. Is burnout related to allostatic load? Int. J. Behav. Med. 2007, 14, 213–221. [Google Scholar] [CrossRef]
- Li, W.; Zhang, J.Q.; Sun, J.; Ke, J.H.; Dong, Z.Y.; Wang, S. Job stress related to glyco-lipid allostatic load, adiponectin and visfatin. Stress Health 2007, 23, 257–266. [Google Scholar] [CrossRef]
- Maselko, J.; Kubzansky, L.; Kawachi, I.; Seeman, T.; Berkman, L. Religious service attendance and allostatic load among high-functioning elderly. Psychosom. Med. 2007, 69, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.M.; Reiber, G.; Kohler, T.; Boyko, E.J. Peripheral arterial disease in a multiethnic national sample: The role of conventional risk factors and allostatic load. Ethn. Dis. 2007, 17, 669–675. [Google Scholar] [PubMed]
- Sun, J.; Wang, S.; Zhang, J.Q.; Li, W. Assessing the cumulative effects of stress: The association between job stress and allostatic load in a large sample of Chinese employees. Work Stress. 2007, 21, 333–347. [Google Scholar] [CrossRef]
- Gersten, O. The path traveled and the path ahead for the allostatic framework: A rejoinder on the framework’s importance and the need for further work related to theory, data, and measurement. Soc. Sci. Med. 2008, 66, 531–535. [Google Scholar] [CrossRef]
- Sabbah, W.; Watt, R.G.; Sheiham, A.; Tsakos, G. Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: Evidence from the Third National Health and Nutrition Examination Survey. J. Epidemiol. Community Health 2008, 62, 415–420. [Google Scholar] [CrossRef]
- Worthman, C.M.; Panter-Brick, C. Homeless street children in Nepal: Use of allostatic load to assess the burden of childhood adversity. Dev. Psychopathol. 2008, 20, 233–255. [Google Scholar] [CrossRef]
- Bellingrath, S.; Weigl, T.; Kudielka, B.M. Chronic work stress and exhaustion is associated with higher allostastic load in female school teachers. Stress Amst. Neth. 2009, 12, 37–48. [Google Scholar] [CrossRef]
- Crimmins, E.M.; Kim, J.K.; Seeman, T.E. Poverty and biological risk: The earlier “aging” of the poor. J. Gerontol. Biol. Sci. Med. Sci. 2009, 64, 286–292. [Google Scholar] [CrossRef]
- Hasson, D.; Von Thiele Schwarz, U.; Lindfors, P. Self-rated health and allostatic load in women working in two occupational sectors. J. Health Psychol. 2009, 14, 568–577. [Google Scholar] [CrossRef]
- Maloney, E.M.; Boneva, R.; Nater, U.M.; Reeves, W.C. Chronic fatigue syndrome and high allostatic load: Results from a population-based case-control study in Georgia. Psychosom. Med. 2009, 71, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.K.; Maloney, E.M.; Falkenberg, V.R.; Dimulescu, I.; Rajeevan, M.S. An angiotensin-1 converting enzyme polymorphism is associated with allostatic load mediated by C-reactive protein, interleukin-6 and cortisol. Psychoneuroendocrinology 2009, 34, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Merkin, S.S.; Basurto-Dávila, R.; Karlamangla, A.; Bird, C.E.; Lurie, N.; Escarce, J.; Seeman, T. Neighborhoods and Cumulative Biological Risk Profiles by Race/Ethnicity in a National Sample of U.S. Adults: NHANES III. Ann. Epidemiol. 2009, 19, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Szanton, S.L.; Allen, J.K.; Seplaki, C.L.; Bandeen-Roche, K.; Fried, L.P. Allostatic load and frailty in the women’s health and aging studies. Biol. Res. Nurs. 2009, 10, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; Schamberg, M.A. Childhood poverty, chronic stress, and adult working memory. Proc. Natl. Acad. Sci. USA 2009, 106, 6545–6549. [Google Scholar] [CrossRef]
- Beckie, T.M. A Systematic Review of Allostatic Load, Health, and Health Disparities. Biol. Res. Nurs. 2012, 14, 311–346. [Google Scholar] [CrossRef]
- Gruenewald, T.L.; Seeman, T.E.; Karlamangla, A.S.; Sarkisian, C.A. Allostatic load and frailty in older adults. J. Am. Geriatr. Soc. 2009, 57, 1525–1531. [Google Scholar] [CrossRef]
- Hampson, S.E.; Goldberg, L.R.; Vogt, T.M.; Hillier, T.A.; Dubanoski, J.P. Using physiological dysregulation to assess global health status: Associations with self-rated health and health behaviors. J. Health Psychol. 2009, 14, 232–241. [Google Scholar] [CrossRef][Green Version]
- Kaestner, R.; Pearson, J.A.; Keene, D.; Geronimus, A.T. Stress, Allostatic Load and Health of Mexican Immigrants. Soc. Sci. Q. 2009, 90, 1089–1111. [Google Scholar] [CrossRef]
- E Bird, C.; Seeman, T.; Escarce, J.J.; Basurto-Dávila, R.; Finch, B.K.; Dubowitz, T.; Heron, M.; Hale, L.; Merkin, S.S.; Weden, M.; et al. Neighbourhood socioeconomic status and biological “wear and tear” in a nationally representative sample of US adults. J. Epidemiol. Community Health 2010, 64, 860–865. [Google Scholar] [CrossRef]
- Borrell, L.N.; Dallo, F.J.; Nguyen, N. Racial/ethnic disparities in all-cause mortality in U.S. adults: The effect of allostatic load. Public Health Rep. 2010, 125, 810–816. [Google Scholar] [CrossRef] [PubMed]
- De Castro, A.B.; Voss, J.G.; Ruppin, A.; Dominguez, C.F.; Seixas, N.S. Stressors among Latino day laborers. A pilot study examining allostatic load. AAOHN J. 2010, 58, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Peek, M.K.; Cutchin, M.P.; Salinas, J.J.; Sheffield, K.M.; Eschbach, K.; Stowe, R.P.; Goodwin, J.S. Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: Effects of ethnicity, nativity, and acculturation. Am. J. Public Health 2010, 100, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Rigney, T. Allostatic load and delirium in the hospitalized older adult. Nurs. Res. 2010, 59, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.; Gruenewald, T.; Karlamangla, A.; Sidney, S.; Liu, K.; McEwen, B.; Schwartz, J. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am. J. Hum. Biol. 2010, 22, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Chyu, L.; Upchurch, D.M. Racial and ethnic patterns of allostatic load among adult women in the United States: Findings from the National Health and Nutrition Examination Survey 1999–2004. J. Womens Health 2011, 20, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.C.; Jiménez, J.A.; Shivpuri, S.; Espinosa de los Monteros, K.; Mills, P.J. Domains of chronic stress, lifestyle factors, and allostatic load in middle-aged Mexican-American women. Ann. Behav. Med. Publ. Soc. Behav. Med. 2011, 41, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, P.E.; Janlert, U.; Theorell, T.; Westerlund, H.; Hammarström, A. Socioeconomic status over the life course and allostatic load in adulthood: Results from the Northern Swedish Cohort. J. Epidemiol. Community Health 2011, 65, 986–992. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Lavelle, L.A.; Berntson, G.G.; Cacioppo, J.T. Mediators of the relationship between socioeconomic status and allostatic load in the Chicago Health, Aging, and Social Relations Study (CHASRS). Psychophysiology 2011, 48, 1134–1145. [Google Scholar] [CrossRef]
- Juster, R.-P.; Marin, M.-F.; Sindi, S.; Nair, N.V.; Ng, Y.K.; Pruessner, J.C.; Lupien, S.J. Allostatic load associations to acute, 3-year and 6-year prospective depressive symptoms in healthy older adults. Physiol. Behav. 2011, 104, 360–364. [Google Scholar] [CrossRef]
- Mair, C.A.; Cutchin, M.P.; Kristen Peek, M. Allostatic load in an environmental riskscape: The role of stressors and gender. Health Place 2011, 17, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Roepke, S.K.; Mausbach, B.; Patterson, T.L.; von Känel, R.; Ancoli-Israel, S.; Harmell, A.L.; Dimsdale, J.E.; Aschbacher, K.; Mills, P.J.; Ziegler, M.G.; et al. Effects of Alzheimer caregiving on allostatic load. J. Health Psychol. 2011, 16, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Kozloski, M. Sex differences in age trajectories of physiological dysregulation: Inflammation, metabolic syndrome, and allostatic load. J. Gerontol. Biol. Sci. Med. Sci. 2011, 66, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, P.E.; Janlert, U.; Theorell, T.; Westerlund, H.; Hammarström, A. Social and material adversity from adolescence to adulthood and allostatic load in middle-aged women and men: Results from the Northern Swedish Cohort. Ann. Behav. Med. Publ. Soc. Behav. Med. 2012, 43, 117–128. [Google Scholar] [CrossRef]
- Mattei, J.; Demissie, S.; Falcon, L.M.; Ordovas, J.M.; Tucker, K. Allostatic load is associated with chronic conditions in the Boston Puerto Rican Health Study. Soc. Sci. Med. 2010, 70, 1988–1996. [Google Scholar] [CrossRef]
- Carlsson, A.C.; Nixon Andreasson, A.; Wändell, P.E. Poor self-rated health is not associated with a high total allostatic load in type 2 diabetic patients--but high blood pressure is. Diabetes Metab. 2011, 37, 446–451. [Google Scholar] [CrossRef]
- Mauss, D.; Li, J.; Schmidt, B.; Angerer, P.; Jarczok, M.N. Measuring allostatic load in the workforce: A systematic review. Ind. Health 2015, 53, 5–20. [Google Scholar] [CrossRef]
- Juster, R.P.; Lupien, S. A sex- and gender-based analysis of allostatic load and physical complaints. Gend. Med. 2012, 9, 511–523. [Google Scholar] [CrossRef]
- Juster, R.P.; Moskowitz, D.S.; Lavoie, J.; D’Antono, B. Sex-specific interaction effects of age, occupational status, and workplace stress on psychiatric symptoms and allostatic load among healthy Montreal workers. Stress Amst. Neth. 2013, 16, 616–629. [Google Scholar] [CrossRef]
- Lipowicz, A.; Szklarska, A.; Malina, R.M. Allostatic load and socioeconomic status in Polish adult men. J. Biosoc. Sci. 2014, 46, 155–167. [Google Scholar] [CrossRef]
- Näswall, K.; Lindfors, P.; Sverke, M. Job insecurity as a predictor of physiological indicators of health in healthy working women: An extension of previous research. Stress Health 2012, 28, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.C.; Kudielka, B.M.; von Känel, R.; Siegrist, J.; Thayer, J.F.; Fischer, J.E. Bone-marrow derived progenitor cells are associated with psychosocial determinants of health after controlling for classical biological and behavioral cardiovascular risk factors. Brain Behav. Immun. 2009, 23, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Redline, S.; Shields, A.E.; Williams, D.R.; Williams, M.A. Associations of allostatic load with sleep apnea, insomnia, short sleep duration, and other sleep disturbances: Findings from the National Health and Nutrition Examination Survey 2005 to 2008. Ann. Epidemiol. 2014, 24, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Kobrosly, R.W.; Seplaki, C.L.; Jones, C.M.; van Wijngaarden, E. Physiologic dysfunction scores and cognitive function test performance in U.S. adults. Psychosom. Med. 2012, 74, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Sanders, A.E.; By, K. Role of allostatic load in sociodemographic patterns of pain prevalence in the U.S. population. J. Pain. 2012, 13, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Theall, K.P.; Drury, S.S.; Shirtcliff, E.A. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. Am. J. Epidemiol. 2012, 176 (Suppl. S7), S164–S174. [Google Scholar] [CrossRef] [PubMed]
- Parente, V.; Hale, L.; Palermo, T. Association between breast cancer and allostatic load by race: National Health and Nutrition Examination Survey 1999–2008. Psychooncology 2013, 22, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Rainisch, B.K.W.; Upchurch, D.M. Sociodemographic correlates of allostatic load among a national sample of adolescents: Findings from the National Health and Nutrition Examination Survey, 1999–2008. J. Adolesc. Health Publ. Soc. Adolesc. Med. 2013, 53, 506–511. [Google Scholar] [CrossRef]
- Zota, A.R.; Shenassa, E.D.; Morello-Frosch, R. Allostatic load amplifies the effect of blood lead levels on elevated blood pressure among middle-aged U.S. adults: A cross-sectional study. Environ. Health Glob. Access. Sci. Source 2013, 12, 64. [Google Scholar] [CrossRef]
- Levine, M.E.; Crimmins, E.M. A comparison of methods for assessing mortality risk. Am. J. Hum. Biol. 2014, 26, 768–776. [Google Scholar] [CrossRef]
- Doamekpor, L.A.; Dinwiddie, G.Y. Allostatic load in foreign-born and US-born blacks: Evidence from the 2001–2010 National Health and Nutrition Examination Survey. Am. J. Public Health 2015, 105, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Frei, R.; Haile, S.R.; Mutsch, M.; Rohrmann, S. Relationship of Serum Vitamin D Concentrations and Allostatic Load as a Measure of Cumulative Biological Risk among the US Population: A Cross-Sectional Study. PLoS ONE 2015, 10, e0139217. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, N.; Park, C.G.; Eldeirawi, K. Relationship of serum carotenoid concentrations with allostatic load as a measure of chronic stress among middle-aged adults in the USA. Public Health Nutr. 2015, 18, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Upchurch, D.M.; Rainisch, B.W.; Chyu, L. Greater Leisure Time Physical Activity Is Associated with Lower Allostatic Load in White, Black, and Mexican American Midlife Women: Findings from the National Health and Nutrition Examination Survey, 1999 through 2004. Womens Health Issues 2015, 25, 680–687. [Google Scholar] [CrossRef]
- Hickson, D.A.; Roux, A.V.D.; Gebreab, S.Y.; Wyatt, S.B.; Dubbert, P.M.; Sarpong, D.F.; Sims, M.; Taylor, H.A. Social patterning of cumulative biological risk by education and income among African Americans. Am. J. Public Health 2012, 102, 1362–1369. [Google Scholar] [CrossRef]
- Gustafsson, P.E.; San Sebastian, M.; Janlert, U.; Theorell, T.; Westerlund, H.; Hammarström, A. Life-Course Accumulation of Neighborhood Disadvantage and Allostatic Load: Empirical Integration of Three Social Determinants of Health Frameworks. Am. J. Public Health 2014, 104, 904–910. [Google Scholar] [CrossRef]
- Hansen, M.; Lund, R.; Bruunsgaard, H.; Rod, N.H.; Garde, A.H.; Molbo, D.; Avlund, K. Social gradient in allostatic load among Danish men and women in late midlife. J. Aging Health 2014, 26, 72–87. [Google Scholar] [CrossRef]
- Robertson, T.; Popham, F.; Benzeval, M. Socioeconomic position across the lifecourse & allostatic load: Data from the West of Scotland Twenty-07 cohort study. BMC Public Health 2014, 14, 184. [Google Scholar] [CrossRef]
- Seeman, M.; Stein Merkin, S.; Karlamangla, A.; Koretz, B.; Seeman, T. Social status and biological dysregulation: The “status syndrome” and allostatic load. Soc. Sci. Med. 2014, 118, 143–151. [Google Scholar] [CrossRef]
- Upchurch, D.M.; Stein, J.; Greendale, G.A.; Chyu, L.; Tseng, C.-H.; Huang, M.-H.; Lewis, T.T.; Kravitz, H.M.; Seeman, T. A Longitudinal Investigation of Race, Socioeconomic Status, and Psychosocial Mediators of Allostatic Load in Midlife Women: Findings From the Study of Women’s Health Across the Nation. Psychosom. Med. 2015, 77, 402–412. [Google Scholar] [CrossRef]
- Barboza Solís, C.; Fantin, R.; Kelly-Irving, M.; Delpierre, C. Physiological wear-and-tear and later subjective health in mid-life: Findings from the 1958 British birth cohort. Psychoneuroendocrinology 2016, 74, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.; Miller, G.E.; Yu, T.; Brody, G.H. The Great Recession and health risks in African American youth. Brain Behav. Immun. 2016, 53, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Gale, C.R.; Booth, T.; Starr, J.M.; Deary, I.J. Intelligence and socioeconomic position in childhood in relation to frailty and cumulative allostatic load in later life: The Lothian Birth Cohort 1936. J. Epidemiol. Community Health 2016, 70, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, N.R.; South, S.C.; Krueger, R.F. Does education lower allostatic load? A co-twin control study. Brain Behav. Immun. 2016, 56, 221–229. [Google Scholar] [CrossRef]
- Robertson, T.; Watts, E. The importance of age, sex and place in understanding socioeconomic inequalities in allostatic load: Evidence from the Scottish Health Survey (2008–2011). BMC Public Health 2016, 16, 126. [Google Scholar] [CrossRef]
- Robertson, T.; Benzeval, M.; Whitley, E.; Popham, F. The role of material, psychosocial and behavioral factors in mediating the association between socioeconomic position and allostatic load (measured by cardiovascular, metabolic and inflammatory markers). Brain Behav. Immun. 2015, 45, 41–49. [Google Scholar] [CrossRef]
- Gruenewald, T.L.; Karlamangla, A.S.; Hu, P.; Stein-Merkin, S.; Crandall, C.; Koretz, B.; Seeman, T.E. History of socioeconomic disadvantage and allostatic load in later life. Soc. Sci. Med. 2012, 74, 75–83. [Google Scholar] [CrossRef]
- Rosemberg, M.A.S.; Li, Y.; Seng, J. Allostatic load: A useful concept for advancing nursing research. J. Clin. Nurs. 2017, 26, 5191–5205. [Google Scholar] [CrossRef]
- Morrison, S.; Shenassa, E.D.; Mendola, P.; Wu, T.; Schoendorf, K. Allostatic load may not be associated with chronic stress in pregnant women, NHANES 1999–2006. Ann. Epidemiol. 2013, 23, 294–297. [Google Scholar] [CrossRef]
- Wallace, M.E.; Harville, E.W. Allostatic load and birth outcomes among white and black women in New Orleans. Matern. Child Health J. 2013, 17, 1025–1029. [Google Scholar] [CrossRef]
- Wallace, M.; Harville, E.; Theall, K.; Webber, L.; Chen, W.; Berenson, G. Preconception biomarkers of allostatic load and racial disparities in adverse birth outcomes: The Bogalusa Heart Study. Paediatr. Perinat Epidemiol. 2013, 27, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Brody, G.H.; Yu, T.; Chen, E.; Miller, G.E.; Kogan, S.M.; Beach, S.R.H. Is resilience only skin deep? rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychol. Sci. 2013, 24, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Brody, G.H.; Lei, M.K.; Chen, E.; Miller, G.E. Neighborhood poverty and allostatic load in African American youth. Pediatrics 2014, 134, e1362–e1368. [Google Scholar] [CrossRef]
- Song, J.; Mailick, M.R.; Ryff, C.D.; Coe, C.L.; Greenberg, J.S.; Hong, J. Allostatic load in parents of children with developmental disorders: Moderating influence of positive affect. J. Health Psychol. 2014, 19, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Dich, N.; Hansen, M.; Avlund, K.; Lund, R.; Mortensen, E.L.; Bruunsgaard, H.; Rod, N.H. Early life adversity potentiates the effects of later life stress on cumulative physiological dysregulation. Anxiety Stress Coping 2015, 28, 372–390. [Google Scholar] [CrossRef]
- Chen, E.; Miller, G.E.; Lachman, M.E.; Gruenewald, T.L.; Seeman, T.E. Protective factors for adults from low-childhood socioeconomic circumstances: The benefits of shift-and-persist for allostatic load. Psychosom. Med. 2012, 74, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; Fuller-Rowell, T.E. Childhood poverty, chronic stress, and young adult working memory: The protective role of self-regulatory capacity. Dev. Sci. 2013, 16, 688–696. [Google Scholar] [CrossRef]
- Brody, G.H.; Lei, M.K.; Chae, D.H.; Yu, T.; Kogan, S.M.; Beach, S.R.H. Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Dev. 2014, 85, 989–1002. [Google Scholar] [CrossRef]
- Brooks, K.P.; Gruenewald, T.; Karlamangla, A.; Hu, P.; Koretz, B.; Seeman, T.E. Social relationships and allostatic load in the MIDUS study. Health Psychol. 2014, 33, 1373–1381. [Google Scholar] [CrossRef]
- Seeman, T.E.; Gruenewald, T.L.; Cohen, S.; Williams, D.R.; Matthews, K.A. Social relationships and their biological correlates: Coronary Artery Risk Development in Young Adults (CARDIA) study. Psychoneuroendocrinology 2014, 43, 126–138. [Google Scholar] [CrossRef]
- Friedman, E.M.; Karlamangla, A.S.; Gruenewald, T.L.; Koretz, B.; Seeman, T.E. Early life adversity and adult biological risk profiles. Psychosom. Med. 2015, 77, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Falcón, L.M.; Gao, X.; Tucker, K.L.; Mattei, J. A Healthy Lifestyle Score Is Associated with Cardiometabolic and Neuroendocrine Risk Factors among Puerto Rican Adults. J. Nutr. 2015, 145, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.J.; Mentz, G.; Lachance, L.; Johnson, J.; Gaines, C.; Israel, B.A. Associations Between Socioeconomic Status and Allostatic Load: Effects of Neighborhood Poverty and Tests of Mediating Pathways. Am. J. Public Health 2012, 102, 1706–1714. [Google Scholar] [CrossRef] [PubMed]
- King, K.E.; Morenoff, J.D.; House, J.S. Neighborhood context and social disparities in cumulative biological risk factors. Psychosom. Med. 2011, 73, 572–579. [Google Scholar] [CrossRef]
- Schulz, A.J.; Mentz, G.; Lachance, L.; Zenk, S.N.; Johnson, J.; Stokes, C.; Mandell, R. Do observed or perceived characteristics of the neighborhood environment mediate associations between neighborhood poverty and cumulative biological risk? Health Place 2013, 24, 147–156. [Google Scholar] [CrossRef]
- Slopen, N.; Non, A.; Williams, D.R.; Roberts, A.L.; Albert, M.A. Childhood adversity, adult neighborhood context, and cumulative biological risk for chronic diseases in adulthood. Psychosom. Med. 2014, 76, 481–489. [Google Scholar] [CrossRef]
- Chen, E.; Miller, G.E.; Brody, G.H.; Lei, M. Neighborhood Poverty, College Attendance, and Diverging Profiles of Substance Use and Allostatic Load in Rural African American Youth. Clin. Psychol. Sci. J. Assoc. Psychol. Sci. 2015, 3, 675–685. [Google Scholar] [CrossRef]
- Jiménez, M.P.; Osypuk, T.L.; Arevalo, S.; Tucker, K.L.; Falcon, L.M. Neighborhood socioeconomic context and change in allostatic load among older Puerto Ricans: The Boston Puerto Rican health study. Health Place 2015, 33, 1–8. [Google Scholar] [CrossRef]
- Barber, S.; Hickson, D.A.; Kawachi, I.; Subramanian, S.V.; Earls, F. Neighborhood Disadvantage and Cumulative Biological Risk Among a Socioeconomically Diverse Sample of African American Adults: An Examination in the Jackson Heart Study. J. Racial. Ethn. Health Disparities 2016, 3, 444–456. [Google Scholar] [CrossRef]
- Barber, S.; Hickson, D.A.; Kawachi, I.; Subramanian, S.V.; Earls, F. Double-jeopardy: The joint impact of neighborhood disadvantage and low social cohesion on cumulative risk of disease among African American men and women in the Jackson Heart Study. Soc. Sci. Med. 2016, 153, 107–115. [Google Scholar] [CrossRef]
- Larrabee Sonderlund, A.; Thilsing, T.; Sondergaard, J. Should social disconnectedness be included in primary-care screening for cardiometabolic disease? A systematic review of the relationship between everyday stress, social connectedness, and allostatic load. PLoS ONE 2019, 14, e0226717. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.C.; McClintock, M.K.; Kozloski, M.; Li, T. Social isolation and adult mortality: The role of chronic inflammation and sex differences. J. Health Soc. Behav. 2013, 54, 183–203. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.C.; Li, T.; Frenk, S.M. Social network ties and inflammation in U.S. adults with cancer. Biodemography Soc. Biol. 2014, 60, 21–37. [Google Scholar] [CrossRef] [PubMed]
- McClure, H.H.; Josh Snodgrass, J.; Martinez, C.R., Jr.; Squires, E.C.; Jiménez, R.A.; Isiordia, L.E.; Mark Eddy, J.; McDade, T.W.; Small, J. Stress, Place, and Allostatic Load Among Mexican Immigrant Farmworkers in Oregon. J. Immigr. Minor. Health 2015, 17, 1518–1525. [Google Scholar] [CrossRef]
- Yang, Y.C.; Boen, C.; Mullan Harris, K. Social relationships and hypertension in late life: Evidence from a nationally representative longitudinal study of older adults. J. Aging Health 2015, 27, 403–431. [Google Scholar] [CrossRef]
- Miller, G.E.; Cohen, S.; Ritchey, A.K. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid-resistance model. Health Psychol. 2002, 21, 531–541. [Google Scholar] [CrossRef]
- Rosal, M.C.; King, J.; Ma, Y.; Reed, G.W. Stress, social support, and cortisol: Inverse associations? Behav. Med. 2004, 30, 11–21. [Google Scholar] [CrossRef]
- Seplaki, C.L.; Goldman, N.; Glei, D.; Weinstein, M. A comparative analysis of measurement approaches for physiological dysregulation in an older population. Exp. Gerontol. 2005, 40, 438–449. [Google Scholar] [CrossRef]
- Wong, A. Allostatic Load and Cognitive Functioning: A Preliminary Analysis. Fuller Theological Seminary. 2012. Available online: https://www.proquest.com/openview/eaafe9a657500020a48ea2a5a6f2bb9b/1?pq-origsite=gscholar&cbl=18750 (accessed on 12 December 2022).
- Forrester, S. Cognitive Function Across Self-Identified Ethno-Racial Groups: The Role of Discrimination, Allostatic Load, and Health Behaviors. Johns Hopkins University. 2016. Available online: https://jscholarship.library.jhu.edu/bitstream/handle/1774.2/40802/FORRESTER-DISSERTATION-2017.pdf?sequence=1 (accessed on 12 December 2022).
- Crook, Z.; Booth, T.; Cox, S.R.; Corley, J.; Dykiert, D.; Redmond, P.; Pattie, A.; Taylor, A.M.; Harris, S.E.; Starr, J.M.; et al. Apolipoprotein E genotype does not moderate the associations of depressive symptoms, neuroticism and allostatic load with cognitive ability and cognitive aging in the Lothian Birth Cohort 1936. PLoS ONE 2018, 13, e0192604. [Google Scholar] [CrossRef]
- De Robert, S.C. impact of allostatic Load on cognitive Level, Memory and Left Ventricular Mass. Argent J. Cardiol. 2019, 87, 40–46. [Google Scholar]
- Schmitz, N.; Deschênes, S.S.; Burns, R.J.; Danna, S.; Franco, O.; Ikram, M.A.; Kivimaki, M.; Singh-Manoux, A.; Tiemeier, H. Cardiometabolic dysregulation and cognitive decline: Potential role of depressive symptoms. Br. J. Psychiatry J. Ment. Sci. 2018, 212, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Narbutas, J.; Van Egroo, M.; Chylinski, D.; González, P.V.; Jimenez, C.G.; Besson, G.; Ghaemmaghami, P.; Hammad, G.; Muto, V.; Schmidt, C.; et al. Cognitive efficiency in late midlife is linked to lifestyle characteristics and allostatic load. Aging 2019, 11, 7169–7186. [Google Scholar] [CrossRef] [PubMed]
- Oi, K.; Haas, S. Cardiometabolic Risk and Cognitive Decline: The Role of Socioeconomic Status in Childhood and Adulthood. J. Health Soc. Behav. 2019, 60, 326–343. [Google Scholar] [CrossRef] [PubMed]
- Ottino-González, J.; Jurado, M.; García-García, I.; Caldú, X.; Prats-Soteras, X.; Tor, E.; Sender-Palacios, M.; Garolera, M. Allostatic load and executive functions in overweight adults. Psychoneuroendocrinology 2019, 106, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Karlamangla, A.S.; Miller-Martinez, D.; Lachman, M.E.; Tun, P.A.; Koretz, B.K.; Seeman, T.E. Biological correlates of adult cognition: Midlife in the United States (MIDUS). Neurobiol. Aging 2014, 35, 387–394. [Google Scholar] [CrossRef]
- Booth, T.; Royle, N.A.; Corley, J.; Gow, A.J.; Hernández, M.D.C.V.; Maniega, S.M.; Ritchie, S.J.; Bastin, M.E.; Starr, J.M.; Wardlaw, J.M.; et al. Association of allostatic load with brain structure and cognitive ability in later life. Neurobiol. Aging 2015, 36, 1390–1399. [Google Scholar] [CrossRef]
- Ketheesan, S.; Rinaudo, M.; Berger, M.; Wenitong, M.; Juster, R.P.; McEwen, B.S.; Sarnyai, Z. Stress, allostatic load and mental health in Indigenous Australians. Stress 2020, 23, 509–518. [Google Scholar] [CrossRef]
- Schmitt, L.H.; Harrison, G.A.; Spargo, R.M.; Pollard, T.; Ungpakorn, G. Patterns of cortisol and adrenaline variation in Australian aboriginal communities of the Kimberley region. J. Biosoc. Sci. 1995, 27, 107–116. [Google Scholar] [CrossRef]
- Schmitt, L.H.; Harrison, G.A.; Spargo, R.M. Variation in epinephrine and cortisol excretion rates associated with behavior in an Australian Aboriginal community. Am. J. Phys. Anthropol. 1998, 106, 249–253. [Google Scholar] [CrossRef]
- Berger, M.; Leicht, A.; Slatcher, A.; Kraeuter, A.-K.; Ketheesan, S.; Larkins, S.; Sarnyai, Z. Cortisol Awakening Response and Acute Stress Reactivity in First Nations People. Sci. Rep. 2017, 7, 41760. [Google Scholar] [CrossRef]
- Berger, M.; Taylor, S.; Harriss, L.; Campbell, S.; Thompson, F.; Jones, S.; Sushames, A.; Amminger, G.P.; Sarnyai, Z.; McDermott, R. Hair cortisol, allostatic load, and depressive symptoms in Australian Aboriginal and Torres Strait Islander people. Stress Amst. Neth. 2019, 22, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Davison, B.; Singh, G.R.; McFarlane, J. Hair cortisol and cortisone as markers of stress in Indigenous and non-Indigenous young adults. Stress Amst. Neth. 2019, 22, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Davison, B.; Singh, G.R.; Oguoma, V.M.; McFarlane, J. Fingernail cortisol as a marker of chronic stress exposure in Indigenous and non-Indigenous young adults. Stress Amst. Neth. 2020, 23, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Kerr, P.; Kheloui, S.; Rossi, M.; Désilets, M.; Juster, R.P. Allostatic load and women’s brain health: A systematic review. Front. Neuroendocrinol. 2020, 59, 100858. [Google Scholar] [CrossRef] [PubMed]
- Mellner, C.; Krantz, G.; Lundberg, U. Medically unexplained symptoms in women as related to physiological stress responses. Stress Health 2005, 21, 45–52. [Google Scholar] [CrossRef]
- Westerlund, H.; Gustafsson, P.E.; Theorell, T.; Janlert, U.; Hammarström, A. Social adversity in adolescence increases the physiological vulnerability to job strain in adulthood: A prospective population-based study. PLoS ONE 2012, 7, e35967. [Google Scholar] [CrossRef]
- Glei, D.A.; Goldman, N.; Shkolnikov, V.; Jdanov, D.; Shkolnikova, M.; Vaupel, J.; Weinstein, M. Perceived stress and biological risk: Is the link stronger in Russians than in Taiwanese and Americans? Stress Amst. Neth. 2013, 16, 411–420. [Google Scholar] [CrossRef]
- Glei, D.A.; Goldman, N.; Wu, C.H.; Weinstein, M. Does exposure to stressors predict changes in physiological dysregulation? Ann. Behav. Med. Publ. Soc. Behav. Med. 2013, 46, 121–126. [Google Scholar] [CrossRef][Green Version]
- Juster, R.P.; Smith, N.G.; Ouellet, É.; Sindi, S.; Lupien, S.J. Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosom. Med. 2013, 75, 103–116. [Google Scholar] [CrossRef]
- Sjörs, A.; Jansson, P.A.; Eriksson, J.W.; Jonsdottir, I.H. Increased insulin secretion and decreased glucose concentrations, but not allostatic load, are associated with stress-related exhaustion in a clinical patient population. Stress Amst. Neth. 2013, 16, 24–33. [Google Scholar] [CrossRef]
- Dich, N.; Doan, S.N.; Evans, G.W. Children’s Emotionality Moderates the Association Between Maternal Responsiveness and Allostatic Load: Investigation Into Differential Susceptibility. Child Dev. 2015, 86, 936–944. [Google Scholar] [CrossRef]
- Dich, N.; Lange, T.; Head, J.; Rod, N.H. Work stress, caregiving, and allostatic load: Prospective results from the Whitehall II cohort study. Psychosom. Med. 2015, 77, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Gale, C.R.; Batty, G.D.; Cooper, S.-A.; Deary, I.J.; Der, G.; McEwen, B.S.; Cavanagh, J. Reaction time in adolescence, cumulative allostatic load, and symptoms of anxiety and depression in adulthood: The West of Scotland Twenty-07 Study. Psychosom. Med. 2015, 77, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Horan, J.M.; Widom, C.S. From Childhood Maltreatment to Allostatic Load in Adulthood: The Role of Social Support. Child Maltreat. 2015, 20, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Mauss, D.; Jarczok, M.N.; Fischer, J.E. A streamlined approach for assessing the Allostatic Load Index in industrial employees. Stress Amst. Neth. 2015, 18, 475–483. [Google Scholar] [CrossRef]
- Nugent, K.L.; Chiappelli, J.; Rowland, L.M.; Hong, L.E. Cumulative stress pathophysiology in schizophrenia as indexed by allostatic load. Psychoneuroendocrinology 2015, 60, 120–129. [Google Scholar] [CrossRef]
- Tomasdottir, M.O.; Sigurdsson, J.A.; Petursson, H.; Kirkengen, A.L.; Krokstad, S.; McEwen, B.; Hetlevik, I.; Getz, L. Self Reported Childhood Difficulties, Adult Multimorbidity and Allostatic Load. A Cross-Sectional Analysis of the Norwegian HUNT Study. PLoS ONE 2015, 10, e0130591. [Google Scholar] [CrossRef]
- Beckie, T.M.; Duffy, A.; Groer, M.W. The Relationship between Allostatic Load and Psychosocial Characteristics among Women Veterans. Womens Health Issues 2016, 26, 555–563. [Google Scholar] [CrossRef]
- Juster, R.-P.; Pruessner, J.C.; Desrochers, A.B.; Bourdon, O.; Durand, N.; Wan, N.; Tourjman, V.; Kouassi, E.; Lesage, A.; Lupien, S.J. Sex and Gender Roles in Relation to Mental Health and Allostatic Load. Psychosom. Med. 2016, 78, 788–804. [Google Scholar] [CrossRef]
- Stapleton, L.R.T.; Schetter, C.D.; Dooley, L.N.; Guardino, C.M.; Huynh, J.; Paek, C.; Clark-Kauffman, E.; Schafer, P.; Woolard, R.; Lanzi, R.G.; et al. The Community Child Health Network Life Stress Interview: A brief chronic stress measure for community health research. Anxiety Stress Coping 2016, 29, 352–366. [Google Scholar] [CrossRef]
- Turner, R.J.; Thomas, C.S.; Brown, T.H. Childhood adversity and adult health: Evaluating intervening mechanisms. Soc. Sci. Med. 2016, 156, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, R.H.; Hansen, Å.M.; Nielsen, M.L.; Blønd, M.; Netterstrøm, B. Changes in Allostatic Load during workplace reorganization. J. Psychosom. Res. 2017, 103, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.Y.; Kuha, J.; Murphy, M. Multidimensional predictors of physical frailty in older people: Identifying how and for whom they exert their effects. Biogerontology 2017, 18, 237–252. [Google Scholar] [CrossRef] [PubMed]
- Hux, V.J.; Roberts, J.M.; Okun, M.L. Allostatic load in early pregnancy is associated with poor sleep quality. Sleep Med. 2017, 33, 85–90. [Google Scholar] [CrossRef]
- Ye, Z.J.; Qiu, H.Z.; Liang, M.Z.; Liu, M.L.; Li, P.F.; Chen, P.; Sun, Z.; Yu, Y.L.; Ni Wang, S.; Zhang, Z.; et al. Effect of a mentor-based, supportive-expressive program, Be Resilient to Breast Cancer, on survival in metastatic breast cancer: A randomised, controlled intervention trial. Br. J. Cancer. 2017, 117, 1486–1494. [Google Scholar] [CrossRef]
- Bey, G.S.; Jesdale, B.M.; Ulbricht, C.M.; Mick, E.O.; Person, S.D. Allostatic Load Biomarker Associations with Depressive Symptoms Vary among US Black and White Women and Men. Healthcare 2018, 6, 105. [Google Scholar] [CrossRef]
- Bey, G.S.; Waring, M.E.; Jesdale, B.M.; Person, S.D. Gendered race modification of the association between chronic stress and depression among Black and White U.S. adults. Am. J. Orthopsychiatry 2018, 88, 151–160. [Google Scholar] [CrossRef]
- Rodriquez, E.J.; Livaudais-Toman, J.; Gregorich, S.E.; Jackson, J.S.; Nápoles, A.M.; Pérez-Stable, E.J. Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults, 2005-2012 NHANES. Prev. Med. 2018, 110, 9–15. [Google Scholar] [CrossRef]
- Savransky, A.; Chiappelli, J.; Fisseha, F.; Wisner, K.M.; Xiaoming, D.; Mirmomen, S.M.; Jones, A.D.; Adhikari, B.M.; Bruce, H.A.; Rowland, L.M.; et al. Elevated allostatic load early in the course of schizophrenia. Transl. Psychiatry 2018, 8, 246. [Google Scholar] [CrossRef]
- Schenk, H.M.; Jeronimus, B.F.; van der Krieke, L.; Bos, E.H.; de Jonge, P.; Rosmalen, J.G.M. Associations of Positive Affect and Negative Affect With Allostatic Load: A Lifelines Cohort Study. Psychosom. Med. 2018, 80, 160–166. [Google Scholar] [CrossRef]
- Soltani, H.; Keim, N.L.; Laugero, K.D. Diet Quality for Sodium and Vegetables Mediate Effects of Whole Food Diets on 8-Week Changes in Stress Load. Nutrients 2018, 10, 1606. [Google Scholar] [CrossRef] [PubMed]
- Tampubolon, G.; Maharani, A. Trajectories of allostatic load among older Americans and Britons: Longitudinal cohort studies. BMC Geriatr. 2018, 18, 255. [Google Scholar] [CrossRef] [PubMed]
- Adynski, H.; Zimmer, C.; Thorp, J.; Santos, H.P. Predictors of psychological distress in low-income mothers over the first postpartum year. Res. Nurs. Health 2019, 42, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Boneva, R.S.; Lin, J.-M.S.; Wieser, F.; Nater, U.M.; Ditzen, B.; Taylor, R.N.; Unger, E.R. Endometriosis as a Comorbid Condition in Chronic Fatigue Syndrome (CFS): Secondary Analysis of Data From a CFS Case-Control Study. Front. Pediatr. 2019, 7, 195. [Google Scholar] [CrossRef]
- Chiu, C.J.; Lin, Y.C. Spousal health and older adults’ biomarker change over six years: Investigation of gender differences. Arch. Gerontol. Geriatr. 2019, 83, 44–49. [Google Scholar] [CrossRef]
- Christensen, D.S.; Flensborg-Madsen, T.; Garde, E.; Hansen, Å.M.; Mortensen, E.L. Big Five personality traits and allostatic load in midlife. Psychol. Health 2019, 34, 1011–1028. [Google Scholar] [CrossRef]
- Ellis, E.M.; Prather, A.A.; Grenen, E.G.; Ferrer, R.A. Direct and indirect associations of cognitive reappraisal and suppression with disease biomarkers. Psychol. Health 2019, 34, 336–354. [Google Scholar] [CrossRef]
- Gillespie, S.L.; Anderson, C.M.; Zhao, S.; Tan, Y.; Kline, D.; Brock, G.; Odei, J.; O’Brien, E.; Sims, M.; Lazarus, S.A.; et al. Allostatic load in the association of depressive symptoms with incident coronary heart disease: The Jackson Heart Study. Psychoneuroendocrinology 2019, 109, 104369. [Google Scholar] [CrossRef]
- Rosemberg, M.A.S.; Li, Y.; McConnell, D.S.; McCullagh, M.C.; Seng, J.S. Stressors, allostatic load, and health outcomes among women hotel housekeepers: A pilot study. J. Occup. Environ. Hyg. 2019, 16, 206–217. [Google Scholar] [CrossRef]
- Rodriquez, E.J.; Sabado-Liwag, M.D.; Pérez-Stable, E.J.; Lee, A.; Haan, M.N.; Gregorich, S.E.; Jackson, J.S.; Nápoles, A.M. Allostatic Load, Unhealthy Behaviors, and Depressive Symptoms by Birthplace Among Older Adults in the Sacramento Area Latino Study on Aging (SALSA). J. Aging Health 2020, 32, 851–860. [Google Scholar] [CrossRef]
- Groër, M.W.; Kostas-Polston, E.A.; Dillahunt-Aspillaga, C.; Beckie, T.M.; Johnson-Mallard, V.; Duffy, A.; Evans, M.E. Allostatic Perspectives in Women Veterans With a History of Childhood Sexual Assault. Biol. Res. Nurs. 2016, 18, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Misiak, B. Stress, Allostatic Load, and Psychosis: One Step Forward in Research But Where to Go Next? Front. Psychiatry 2020, 10, 937. [Google Scholar] [CrossRef] [PubMed]
- Chiappelli, J.; Kochunov, P.; Savransky, A.; Fisseha, F.; Wisner, K.; Du, X.; Rowland, L.M.; Hong, L.E. Allostatic load and reduced cortical thickness in schizophrenia. Psychoneuroendocrinology 2017, 77, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Savransky, A.; Chiappelli, J.; Rowland, L.; Wisner, K.; Shukla, D.K.; Kochunov, P.; Hong, L.E. Fornix Structural Connectivity and Allostatic Load: Empirical Evidence From Schizophrenia Patients and Healthy Controls. Psychosom. Med. 2017, 79, 770–776. [Google Scholar] [CrossRef]
- Berger, M.; Juster, R.-P.; Westphal, S.; Amminger, G.P.; Bogerts, B.; Schiltz, K.; Bahn, S.; Steiner, J.; Sarnyai, Z. Allostatic load is associated with psychotic symptoms and decreases with antipsychotic treatment in patients with schizophrenia and first-episode psychosis. Psychoneuroendocrinology 2018, 90, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Lavoie, S.; McGorry, P.D.; Nelson, B.; Markulev, C.; Yuen, H.-P.; Schaefer, M.; Sarnyai, Z.; Amminger, G.P. Relationship between allostatic load and clinical outcomes in youth at ultra-high risk for psychosis in the NEURAPRO study. Schizophr. Res. 2020, 226, 38–43. [Google Scholar] [CrossRef]
- Misiak, B.; Kotowicz, K.; Loska, O.; Stramecki, F.; Beszłej, J.A.; Samochowiec, J.; Jabłoński, M.; Podwalski, P.; Waszczuk, K.; Wroński, M.; et al. Decreased use of active coping styles contributes to elevated allostatic load index in first-episode psychosis. Psychoneuroendocrinology 2018, 96, 166–172. [Google Scholar] [CrossRef]
- Misiak, B.; Kotowicz, K.; Loska, O.; Stramecki, F.; Beszłej, J.A.; Samochowiec, J.; Samochowiec, A.; Jabłoński, M.; Podwalski, P.; Waszczuk, K.; et al. Elevated allostatic load index is associated with working memory deficits in first-episode psychosis. Schizophr. Res. 2019, 204, 439–441. [Google Scholar] [CrossRef]
- Piotrowski, P.; Kotowicz, K.; Rymaszewska, J.; Beszłej, J.A.; Plichta, P.; Samochowiec, J.; Kalinowska, S.; Trześniowska-Drukała, B.; Misiak, B. Allostatic load index and its clinical correlates at various stages of psychosis. Schizophr. Res. 2019, 210, 73–80. [Google Scholar] [CrossRef]
- Suvarna, B.; Suvarna, A.; Phillips, R.; Juster, R.P.; McDermott, B.; Sarnyai, Z. Health risk behaviours and allostatic load: A systematic review. Neurosci. Biobehav. Rev. 2020, 108, 694–711. [Google Scholar] [CrossRef] [PubMed]
- Duru, O.K.; Harawa, N.T.; Kermah, D.; Norris, K.C. Allostatic Load Burden and Racial Disparities in Mortality. J. Natl. Med. Assoc. 2012, 104, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Mattei, J.; Noel, S.E.; Tucker, K.L. A meat, processed meat, and French fries dietary pattern is associated with high allostatic load in Puerto Rican older adults. J. Am. Diet Assoc. 2011, 111, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Mattei, J.; Bhupathiraju, S.; Tucker, K.L. Higher adherence to a diet score based on American Heart Association recommendations is associated with lower odds of allostatic load and metabolic syndrome in Puerto Rican adults. J. Nutr. 2013, 143, 1753–1759. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.J.; Dich, N.; Lange, T.; Jennum, P.; Hansen, M.; Lund, R.; Rod, N.H. Impaired sleep and allostatic load: Cross-sectional results from the Danish Copenhagen Aging and Midlife Biobank. Sleep Med. 2014, 15, 1571–1578. [Google Scholar] [CrossRef] [PubMed]
- Doan, S.N.; Dich, N.; Evans, G.W. Childhood cumulative risk and later allostatic load: Mediating role of substance use. Health Psychol. 2014, 33, 1402–1409. [Google Scholar] [CrossRef]
- Carroll, J.E.; Irwin, M.R.; Stein Merkin, S.; Seeman, T.E. Sleep and multisystem biological risk: A population-based study. PLoS ONE 2015, 10, e0118467. [Google Scholar] [CrossRef]
- Gay, J.L.; Salinas, J.J.; Buchner, D.M.; Mirza, S.; Kohl, H.W.; Fisher-Hoch, S.P.; McCormick, J.B. Meeting physical activity guidelines is associated with lower allostatic load and inflammation in Mexican Americans. J. Immigr. Minor Health 2015, 17, 574–581. [Google Scholar] [CrossRef]
- Bingham, B.A.; Duong, M.T.; Ricks, M.; Mabundo, L.S.; Baker, R.L.J.; Utumatwishima, J.N.; Udahogora, M.; Berrigan, D.; Sumner, A.E. The Association between Stress Measured by Allostatic Load Score and Physiologic Dysregulation in African Immigrants: The Africans in America Study. Front. Public Health 2016, 4, 265. [Google Scholar] [CrossRef]
- Kusano, Y.; Crews, D.E.; Iwamoto, A.; Sone, Y.; Aoyagi, K.; Maeda, T.; Leahy, R. Allostatic load differs by sex and diet, but not age in older Japanese from the Goto Islands. Ann. Hum. Biol. 2016, 43, 34–41. [Google Scholar] [CrossRef]
- Petrovic, D.; Pivin, E.; Ponte, B.; Dhayat, N.; Pruijm, M.; Ehret, G.; Ackermann, D.; Guessous, I.; Younes, S.E.; Pechère-Bertschi, A.; et al. Sociodemographic, behavioral and genetic determinants of allostatic load in a Swiss population-based study. Psychoneuroendocrinology 2016, 67, 76–85. [Google Scholar] [CrossRef]
- Vadiveloo, M.; Mattei, J. Perceived Weight Discrimination and 10-Year Risk of Allostatic Load Among US Adults. Ann. Behav. Med. Publ. Soc. Behav. Med. 2017, 51, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.R.; Jee, S.H.; Pikhart, H. Role of allostatic load and health behaviours in explaining socioeconomic disparities in mortality: A structural equation modelling approach. J. Epidemiol. Community Health 2018, 72, 545–551. [Google Scholar] [CrossRef] [PubMed]
- McClain, A.C.; Xiao, R.S.; Gao, X.; Tucker, K.L.; Falcon, L.M.; Mattei, J. Food Insecurity and Odds of High Allostatic Load in Puerto Rican Adults: The Role of Participation in the Supplemental Nutrition Assistance Program During 5 Years of Follow-Up. Psychosom. Med. 2018, 80, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Van Draanen, J.; Prelip, M.; Upchurch, D.M. Consumption of fast food, sugar-sweetened beverages, artificially-sweetened beverages and allostatic load among young adults. Prev. Med. Rep. 2018, 10, 212–217. [Google Scholar] [CrossRef]
- Mathew, A.; Doorenbos, A.Z.; Li, H.; Jang, M.K.; Park, C.G.; Bronas, U.G. Allostatic Load in Cancer: A Systematic Review and Mini Meta-Analysis. Biol. Res. Nurs. 2021, 23, 341–361. [Google Scholar] [CrossRef]
- Robertson, T.; Beveridge, G.; Bromley, C. Allostatic load as a predictor of all-cause and cause-specific mortality in the general population: Evidence from the Scottish Health Survey. PLoS ONE 2017, 12, e0183297. [Google Scholar] [CrossRef]
- Hwang, A.-C.; Peng, L.-N.; Wen, Y.-W.; Tsai, Y.-W.; Chang, L.-C.; Chiou, S.-T.; Chen, L.-K. Predicting all-cause and cause-specific mortality by static and dynamic measurements of allostatic load: A 10-year population-based cohort study in Taiwan. J. Am. Med. Dir. Assoc. 2014, 15, 490–496. [Google Scholar] [CrossRef]
- Santacroce, S.J.; Crandell, J.B. Feasibility and preliminary findings from a pilot study of allostatic load in adolescent-young adult childhood cancer survivors and their siblings. J. Pediatr. Oncol. Nurs. 2014, 31, 122–134. [Google Scholar] [CrossRef]
- Ruini, C.; Offidani, E.; Vescovelli, F. Life Stressors, Allostatic Overload, and Their Impact on Posttraumatic Growth. J. Loss Trauma. 2015, 20, 109–122. [Google Scholar] [CrossRef]
- Beydoun, H.A.; Huang, S.; Beydoun, M.A.; Hossain, S.; Zonderman, A.B. Mediating-Moderating Effect of Allostatic Load on the Association between Dietary Approaches to Stop Hypertension Diet and All-Cause and Cause-Specific Mortality: 2001–2010 National Health and Nutrition Examination Surveys. Nutrients 2019, 11, 2311. [Google Scholar] [CrossRef]
- Acheampong, T.; Jiang, L.; Ziogas, A.; Odegaard, A.O. Multi-Systemic Biological Risk and Cancer Mortality: The NHANES III Study. Sci. Rep. 2020, 10, 5047. [Google Scholar] [CrossRef] [PubMed]
- Hughes Halbert, C.; Jefferson, M.; Ambrose, L.; Caulder, S.; Savage, S.J. Resiliency and Allostatic Load among Veterans at Risk for Adverse Prostate Cancer Outcomes. Ethn. Dis. 2020, 30 (Suppl. S1), 177–184. [Google Scholar] [CrossRef] [PubMed]
- Xing, C.Y.; Doose, M.; Qin, B.; Lin, Y.; Plascak, J.J.; Omene, C.; He, C.; Demissie, K.; Hong, C.-C.; Bandera, E.V.; et al. Prediagnostic Allostatic Load as a Predictor of Poorly Differentiated and Larger Sized Breast Cancers among Black Women in the Women’s Circle of Health Follow-Up Study. Cancer Epidemiol. Biomark. Prev. 2020, 29, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Whelan, E.; O’Shea, J.; Hunt, E.; Dockray, S. Evaluating measures of allostatic load in adolescents: A systematic review. Psychoneuroendocrinology 2021, 131, 105324. [Google Scholar] [CrossRef] [PubMed]
- Doan, S.N.; Evans, G.W. Maternal responsiveness moderates the relationship between allostatic load and working memory. Dev. Psychopathol. 2011, 23, 873–880. [Google Scholar] [CrossRef]
- Skinner, M.L.; Shirtcliff, E.A.; Haggerty, K.P.; Coe, C.L.; Catalano, R.F. Allostasis model facilitates understanding race differences in the diurnal cortisol rhythm. Dev. Psychopathol. 2011, 23, 1167–1186. [Google Scholar] [CrossRef]
- Brody, G.H.; Yu, T.; Chen, Y.-F.; Kogan, S.M.; Evans, G.W.; Windle, M.; Gerrard, M.; Gibbons, F.X.; Simons, R.L.; Philibert, R.A. Supportive family environments, genes that confer sensitivity, and allostatic load among rural African American emerging adults: A prospective analysis. J. Fam. Psychol. 2013, 27, 22–29. [Google Scholar] [CrossRef]
- Brody, G.H.; Yu, T.; Chen, Y.-F.; Kogan, S.M.; Evans, G.W.; Beach, S.R.H.; Windle, M.; Simons, R.L.; Gerrard, M.; Gibbons, F.X.; et al. Cumulative socioeconomic status risk, allostatic load, and adjustment: A prospective latent profile analysis with contextual and genetic protective factors. Dev. Psychol. 2013, 49, 913–927. [Google Scholar] [CrossRef]
- Wolpert, C. The Relation of Chronic Stress during Middle Childhood to Allostatic Load in Adolescence; The University of North Carolina: Chapel Hill, NC, USA, 2014. [Google Scholar]
- Augustine, L.F.; Nair, K.M.; Rao, S.F.; Rao, M.V.V.; Ravinder, P.; Laxmaiah, A. Exploring the bio-behavioural link between stress, allostatic load & micronutrient status: A cross-sectional study among adolescent boys. Indian J. Med. Res. 2016, 144, 378–384. [Google Scholar] [CrossRef]
- Doan, S.N.; Dich, N.; Evans, G.W. Stress of stoicism: Low emotionality and high control lead to increases in allostatic load. Appl. Dev. Sci. 2016, 20, 310–317. [Google Scholar] [CrossRef]
- Harding, S.; Silva, M.J.; Molaodi, O.R.; E Enayat, Z.; Cassidy, A.; Karamanos, A.; Read, U.M.; Cruickshank, J.K. Longitudinal study of cardiometabolic risk from early adolescence to early adulthood in an ethnically diverse cohort. BMJ Open 2016, 6, e013221. [Google Scholar] [CrossRef] [PubMed]
- Dich, N.; Doan, S.N.; Evans, G.W. In risky environments, emotional children have more behavioral problems but lower allostatic load. Health Psychol. 2017, 36, 468–476. [Google Scholar] [CrossRef] [PubMed]
- King, A.L.; Garnier-Villarreal, M.; Simanek, A.M.; Johnson, N.L. Testing allostatic load factor structures among adolescents: A structural equation modeling approach. Am. J. Hum. Biol. 2019, 31, e23242. [Google Scholar] [CrossRef] [PubMed]
- King, L.S.; Humphreys, K.L.; Camacho, M.C.; Gotlib, I.H. A person-centered approach to the assessment of early life stress: Associations with the volume of stress-sensitive brain regions in early adolescence. Dev. Psychopathol. 2019, 31, 643–655. [Google Scholar] [CrossRef]
- Tian, Y.; Ming, H.; Huang, S.; Zhang, H. Discrimination Increases the Association Between Parental and Adolescent Allostatic Load in Chinese Rural-to-Urban Migrants. J. Adolesc. Health 2020, 66, 499–505. [Google Scholar] [CrossRef]
- Bild, D.E. Multi-Ethnic Study of Atherosclerosis: Objectives and Design. Am. J. Epidemiol. 2002, 156, 871–881. [Google Scholar] [CrossRef]
- Burke, G.; Lima, J.; Wong, N.D.; Narula, J. The Multiethnic Study of Atherosclerosis. Glob. Heart 2016, 11, 267. [Google Scholar] [CrossRef]
- Olson, J.L.; Bild, D.E.; Kronmal, R.A.; Burke, G.L. Legacy of MESA. Glob. Heart 2016, 11, 269. [Google Scholar] [CrossRef]
- Schetter, C.D.; Schafer, P.; Lanzi, R.G.; Clark-Kauffman, E.; Raju, T.N.K.; Hillemeier, M.M.; Community Child Health Network. Shedding Light on the Mechanisms Underlying Health Disparities Through Community Participatory Methods: The Stress Pathway. Perspect. Psychol. Sci. 2013, 8, 613–633. [Google Scholar] [CrossRef] [PubMed]
- Schetter, C.D.; Dolbier, C. Resilience in the Context of Chronic Stress and Health in Adults: Resilience, Chronic Stress and Health. Soc. Personal Psychol. Compass 2011, 5, 634–652. [Google Scholar] [CrossRef]
- Radler, B.T. The Midlife in the United States (MIDUS) Series: A National Longitudinal Study of Health and Well-being. Open Health Data 2014, 2, e3. [Google Scholar] [CrossRef]
- Wyatt, S.B.; Diekelmann, N.; Henderson, F.; E Andrew, M.; Billingsley, G.; Felder, S.H.; Fuqua, S.; Jackson, P.B. A community-driven model of research participation: The Jackson Heart Study Participant Recruitment and Retention Study. Ethn. Dis. 2003, 13, 438–455. [Google Scholar] [PubMed]
- About Us: National Archive of Computerized Data on Aging (NACDA). Available online: https://www.icpsr.umich.edu/web/pages/NACDA/index.html (accessed on 12 December 2022).
- Curtin, L.R.; Mohadjer, L.K.; Dohrmann, S.M.; Montaquila, J.M.; Kruszan-Moran, D.; Mirel, L.B.; Carroll, M.D.; Hirsch, R.; Schober, S.; Johnson, C.L. The National Health and Nutrition Examination Survey: Sample Design, 1999–2006. Vital. Health Stat. 2012, 155, 1–39. [Google Scholar]
- Sonnega, A.; Faul, J.D.; Ofstedal, M.B.; Langa, K.M.; Phillips, J.W.R.; Weir, D.R. Cohort Profile: The Health and Retirement Study (HRS). Int. J. Epidemiol. 2014, 43, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Idrovo, A.J. Three Criteria for Ecological Fallacy. Environ. Health Perspect. 2011, 119, A332. [Google Scholar] [CrossRef]
- Buzzelli, M. Modifiable Areal Unit Problem. In International Encyclopedia of Human Geography; Elsevier: Amsterdam, The Netherlands, 2020; pp. 169–173. [Google Scholar] [CrossRef]
- Kanankege, K.S.T.; Alvarez, J.; Zhang, L.; Perez, A.M. An Introductory Framework for Choosing Spatiotemporal Analytical Tools in Population-Level Eco-Epidemiological Research. Front. Vet. Sci. 2020, 7, 339. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, W.F.; Delmerico, A.M. Geographic information systems. Wiley Interdiscip. Rev. Comput. Stat. 2009, 1, 167–186. [Google Scholar] [CrossRef]
- Denny, J.C.; Rutter, J.L.; Goldstein, D.B.; Philippakis, A.; Smoller, J.W.; Jenkins, G.; Dishman, E.; All of Us Research Program Investigators. The “All of Us” Research Program. N. Engl. J. Med. 2019, 381, 668–676. [Google Scholar] [CrossRef]
- Rosemberg, M.A.S.; Granner, J.; Li, Y.; Seng, J.S. A scoping review of interventions targeting allostatic load. Stress 2020, 23, 519–528. [Google Scholar] [CrossRef]
- Fava, G.A.; Guidi, J.; Semprini, F.; Tomba, E.; Sonino, N. Clinical Assessment of Allostatic Load and Clinimetric Criteria. Psychother. Psychosom. 2010, 79, 280–284. [Google Scholar] [CrossRef]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother. Psychosom. 2021, 90, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Misiak, B.; Stańczykiewicz, B.; Pawlak, A.; Szewczuk-Bogusławska, M.; Samochowiec, J.; Samochowiec, A.; Tyburski, E.; Juster, R.-P. Adverse childhood experiences and low socioeconomic status with respect to allostatic load in adulthood: A systematic review. Psychoneuroendocrinology 2022, 136, 105602. [Google Scholar] [CrossRef]
- Liu, S.H.; Juster, R.P.; Dams-O’Connor, K.; Spicer, J. Allostatic load scoring using item response theory. Compr. Psychoneuroendocrinol. 2021, 5, 100025. [Google Scholar] [CrossRef] [PubMed]
- Mauss, D.; Jarczok, M.N. The streamlined allostatic load index is associated with perceived stress in life—Findings from the MIDUS study. Stress 2021, 24, 404–412. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).