The Impact of Meaningful Use and Electronic Health Records on Hospital Patient Safety
Abstract
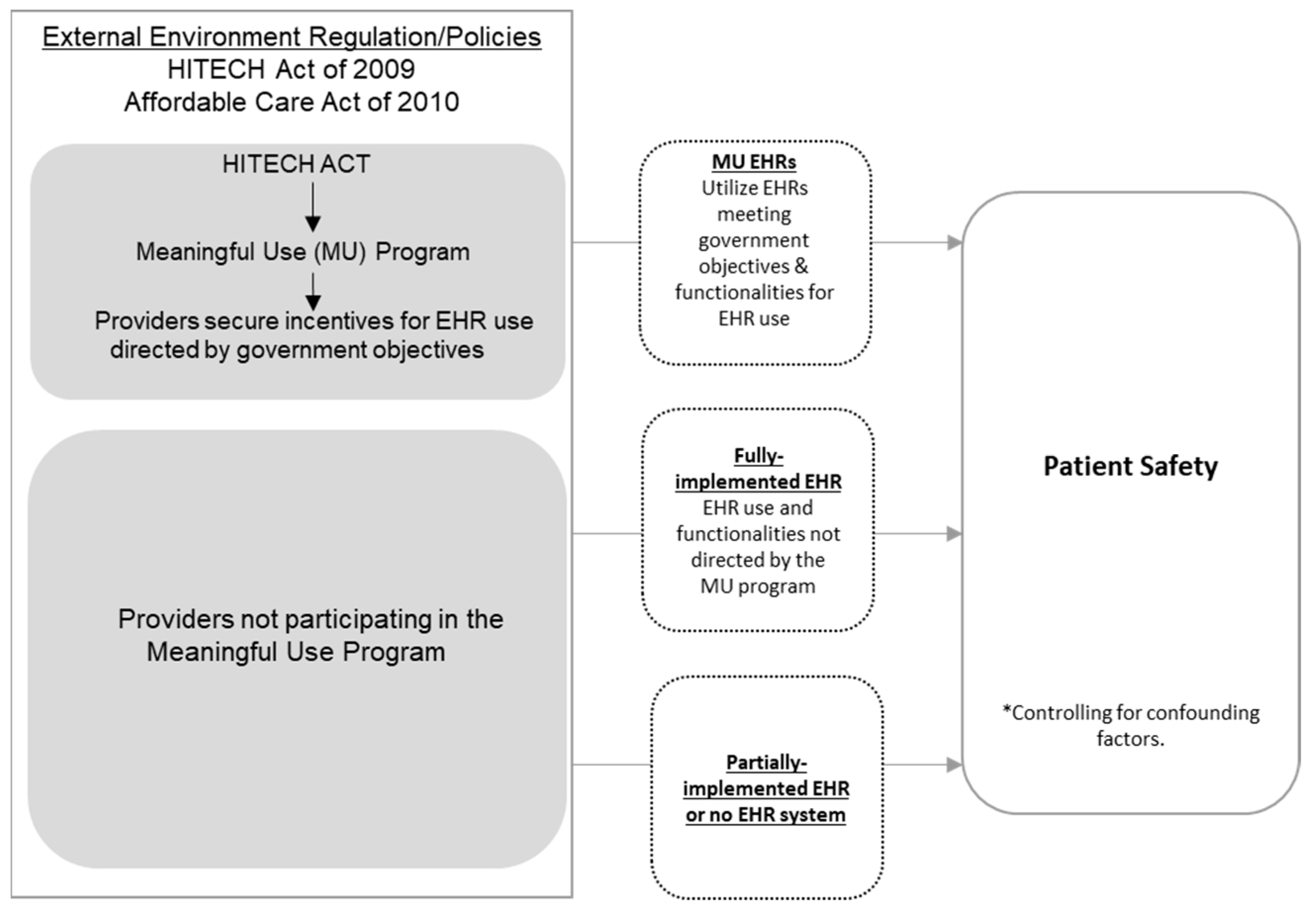
1. Introduction
2. Methods
2.1. Data
2.2. Calculating PSIs
2.3. Analytical Approach
3. Results
3.1. Hospital Characteristics
3.2. Impact of EHR Use on Patient Safety
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- HITECH. Act of 2009, Pub. L. 111-5, 123 Stat.227 (Feb. 17, 2009) [Public Law]. Available online: https://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf (accessed on 27 September 2022).
- Jamoom, E.; Patel, V.; King, J.; Furukawa, M. National perceptions of ehr adoption: Barriers, impacts, and federal policies. In Proceedings of the National conference on health statistics, Washington, DC, USA, 6–8 August 2012. [Google Scholar]
- Duffy, R.L.; Yiu, S.S.; Molokhia, E.; Walker, R.; Perkins, R.A. Effects of electronic prescribing on the clinical practice of a family medicine residency. Fam Med. 2010, 42, 358–363. [Google Scholar] [PubMed]
- Kern, L.M.; Barrón, Y.; Dhopeshwarkar, R.V.; Edwards, A.; Kaushal, R. Electronic health records and ambulatory quality of care. J. Gen. Intern. Med. 2013, 28, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Bell, B.; Thornton, K. From promise to reality achieving the value of an EHR. Healthc. Financ. Manag. 2011, 65, 51–57. [Google Scholar]
- Holt, T.A.; Thorogood, M.; Griffiths, F.; Munday, S.; Friede, T.; Stables, D. Automated electronic reminders to facilitate primary cardiovasculardisease prevention: Randomised controlled trial. Br. J. Gen. Pract. 2010, 60, e137–e143. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.; Johnson, J.; Steck, J. The economic effect of implementing an EMR in an outpatient clinical setting. J. Healthc. Inf. Manag. 2003, 18, 46–51. [Google Scholar]
- Jones, S.S.; Rudin, R.S.; Perry, T.; Shekelle, P.G. Health information technology: An updated systematic review with a focus on meaningful use. Ann. Intern. Med. 2014, 160, 48–54. [Google Scholar] [CrossRef]
- Verdon, D.R. Medical Economics EHR survey probes physician angst about adoption, use of technology: 2014 EHR Survey. Med. Econ. 2014. Available online: http://medicaleconomics.modernmedicine.com/medical-economics/content/tags/ehr/slideshow-medical-economics-ehr-survey-probes-physician-angst-abo (accessed on 1 March 2022).
- Adler-Milstein, J.; Salzberg, C.; Franz, C.; Orav, E.J.; Bates, D.W. The Impact of Electronic Health Records on Ambulatory Costs Among Medicaid Beneficiaries. Medicare Medicaid Res. Rev. 2013, 3. [Google Scholar] [CrossRef][Green Version]
- Murphy, Z.R.; Wang, J.; Boland, M.V. Association of Electronic Health Record Use Above Meaningful Use Thresholds With Hospital Quality and Safety Outcomes. JAMA Netw. Open 2020, 3, e2012529. [Google Scholar] [CrossRef] [PubMed]
- Center for Medicare and Medicaid Services (CMS). Hospital Value Based Purchasing (HVBP) Program FY 2018–2026 Measures. Available online: https://qualitynet.cms.gov/inpatient/hvbp/measures (accessed on 1 March 2022).
- Himmelstein, D.U.; Wright, A.; Woolhandler, S. Hospital computing and the costs and quality of care: A national study. Am. J. Med. 2010, 123, 40–46. [Google Scholar] [CrossRef]
- Jones, S.S.; Heaton, P.; Friedberg, M.W.; Schneider, E.C. Today’s ‘meaningful use’ standard for medication orders by hospitals may save few lives; later stages may do more. Health Aff. 2011, 30, 2005–2012. [Google Scholar] [CrossRef] [PubMed]
- Appari, A.; Johnson, E.M.; Anthony, D.L. Information technology and hospital patient safety: A cross-sectional study of US acute care hospitals. Am. J. Manag. Care 2014, 20, eSP39–eSP47. [Google Scholar] [PubMed]
- DesRoches, C.M.; Charles, D.; Furukawa, M.F.; Joshi, M.S.; Kralovec, P.; Mostashari, F.; Worzala, C.; Jha, A.K. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff. 2013, 32, 1478–1485. [Google Scholar] [CrossRef] [PubMed]
- Geppert, J.; Rhoda, D.; Morara, M. Quality Indicator Empirical Methods; Rockville, M.D., Ed.; Agency for Healthcare Research and Quality: North Bethesda, MD, USA, 2013. Available online: http://www.qualityindicators.ahrq.gov/Downloads/Resources/Publications/2013/Empirical_Methods_r.pdf. (accessed on 1 March 2022).
- Singer, S.; Lin, S.; Falwell, A.; Gaba, D.; Baker, L. Relationship of safety climate and safety performance in hospitals. Health Serv. Res. 2009, 44, 399–421. [Google Scholar] [CrossRef]
- Gardner, W.; Mulvey, E.P.; Shaw, E.C. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull. 1995, 118, 392. [Google Scholar] [CrossRef]
- Patient Protection and Affordable Care Act of 2010, Pub. L. 111-148, 124 Stat.119 (Mar. 23, 2010) [Public Law]. Available online: https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf (accessed on 27 September 2022).
- Heit, J.A.; O’Fallon, W.M.; Petterson, T.M.; Lohse, C.M.; Silverstein, M.D.; Mohr, D.N.; Melton, L.J. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: A population-based study. Arch Intern. Med. 2002, 162, 1245–1248. [Google Scholar]
- Heit, J.A.; Silverstein, M.D.; Mohr, D.N.; Petterson, T.M.; O’Fallon, W.M.; Melton, L.J. Predictors of survival after deep vein thrombosis and pulmonary embolism: A population-based, cohort study. Arch. Intern. Med. 1999, 159, 445–453. [Google Scholar] [CrossRef]
- Bergqvist, D.; Jendteg, S.; Johansen, L.; Persson, U.; Odegaard, K. Cost of long-term complications of deep venous thrombosis of the lower extremities: An analysis of a defined patient population in Sweden. Ann. Intern. Med. 1997, 126, 454–457. [Google Scholar] [CrossRef]
- Goldhaber, S.Z.; Bounameaux, H. Pulmonary embolism and deep vein thrombosis. Lancet 2012, 379, 1835–1846. [Google Scholar]
- Trudel, M.C.; Marsan, J.; Paré, G.; Raymond, L.; de Guinea, A.O.; Maillet, É.; Micheneau, T. Ceiling effect in EMR system assimilation: A multiple case study in primary care family practices. BMC Med. Inform. Decis. Mak. 2017, 17, 46. [Google Scholar] [CrossRef]
- Arozullah, A.M.; Khuri, S.F.; Henderson, W.G.; Daley, J. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann. Intern. Med. 2001, 135, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Scanlon, M.C.; Harris, J.M.; Levy, F.; Sedman, A. Evaluation of the Agency for Healthcare Research and Quality Pediatric Quality Indicators. Pediatrics 2008, 121, e1723–e1731. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, V.A.; Cornell, J.E.; Smetana, G.W. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 596–608. [Google Scholar] [CrossRef]
- Utter, G.H.; Cuny, J.; Sama, P.; Silver, M.R.; Zrelak, P.A.; Baron, R.; Drösler, S.E.; Romano, P.S. Detection of postoperative respiratory failure: How predictive is the Agency for Healthcare Research and Quality’s Patient Safety Indicator? J. Am. Coll. Surg. 2010, 211, 347–354. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality (AHRQ). Patient Safety Quality Indicators Composite Measure Workgroup; Agency for Healthcare Research and Quality: North Bethesda, MD, USA, 2008. Available online: https://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/PSI_Composite_Development.pdf (accessed on 1 March 2022).
- Henry, J.; Pylypchuk, Y.; Searcy, T.; Patel, V. Adoption of Electronic Health Record Systems among U.S. Non-Federal Acute Care Hospitals: 2008–2015; ONC Data Brief, no.35; Office of the National Coordinator for Health Information Technology: Washington, DC, USA, 2016.
| Total Sample n (%) (n = 349) | Partially Implemented or No HER n (%) (n = 32) | Full-EHR without MU n (%) (n = 30) | EHR that Attests to MU n (%) (n = 287) | p-Value | |
|---|---|---|---|---|---|
| Hospital Characteristics | |||||
| Number of staffed beds Mean (SD) <100 100–299 300–399 400–499 500 and greater | 292.2 (17.2) 97 (27.8) 135 (38.7) 36 (10.3) 20 (5.7) 60 (17.5) | 237.8 (73.5) 15 (46.9) 11 (34.4) 2 (6.25) 0 4 (12.5) | 217.8 (79.2) 17 (56.7) 7 (23.3) 3 (10.0) 1 (3.3) 2 (6.7) | 306.1 (17.4) 65 (22.7) 117 (40.8) 31 (10.8) 19 (6.6) 55 (19.2) | 0.218 0.002 |
| N (%) for profit | 30 (8.6) | 4 (12.5) | 2 (6.7) | 24 (8.4) | 0.676 |
| Teaching status Non-teaching Minor teaching Major teaching | 199 (57.0) 110 (31.5) 40 (11.5) | 21 (65.6) 8 (25.0) 3 (9.4) | 19 (63.3) 7 (23.3) 4 (13.3) | 159 (55.4) 95 (33.1) 33 (11.5) | 0.687 |
| Location | |||||
| State Florida Nebraska New York Washington | 122 (35.0) 38 (10.9) 130 (37.3) 59 (16.9) | 6 (18.8) 10 (31.3) 11 (34.4) 5 (15.6) | 9 (30.0) 6 (20.0) 5 (16.7) 10 (33.3) | 107 (37.3) 22 (7.7) 114 (39.7) 44 (15.3) | <0.001 |
| Rurality Rural Metropolitan | 88 (25.2) 261 (74.8) | 12 (37.5) 20 (62.5) | 9 (30.0) 21 (70.0) | 67 (23.3) 220 (76.7) | 0.177 |
| Nurse attendance | |||||
| Nurse to bed ratio Mean (SD) | 1.73 (0.03) | 2.02 (0.38) | 1.84 (0.22) | 1.81 (0.05) | 0.577 |
| Partially Implemented or No EHR Mean (SD) | Full-EHR not Receiving MU Mean (SD) | EHR that Attests to MU Mean (SD) | p-Value | |
|---|---|---|---|---|
| Death Related PSI | ||||
| Death Rate in Low-Mortality Diagnosis Related Groups (DRGs) | 1.04 (0.82) | 0.10 (0.06) | 0.34 (0.04) | 0.022 |
| Death Rate among Surgical Inpatients with Serious Treatable Complications | 89.21 (15.65) | 109.43 (16.42) | 124.83 (5.64) | 0.222 |
| Non-Death Related PSI | ||||
| Iatrogenic Pneumothorax Rate (collapsed lung due to medical treatment) | 0.28 (0.16) | 0.19 (0.05) | 8.69 (8.40) | 0.897 |
| Postoperative Physiologic and Metabolic Derangement Rate | 2.20 (1.84) | 0.10 (0.04) | 0.49 (0.06) | 0.004 |
| Postoperative Respiratory Failure Rate (breathing failure after surgery) | 7.54 (4.12) | 9.25 (3.48) | 8.21 (0.39) | 0.810 |
| Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate (serious blood clots after surgery) | 9.21 (4.84) | 7.52 (4.03) | 4.11 (0.19) | 0.007 |
| Postoperative Sepsis Rate | 9.44 (3.06) | 19.34 (6.97) | 8.70 (0.71) | 0.004 |
| Postoperative Wound Dehiscence Rate (wounds split open after surgery) | 5.90 (4.74) | 0.59 (0.24) | 1.45 (0.22) | 0.006 |
| PSI-90 Composite Score * | 0.99 (0.03) | 0.99 (0.03) | 0.95 (0.01) | 0.407 |
| Coefficient | Confidence Interval | p-Value | |
|---|---|---|---|
| Death Related PSI | |||
| Death Rate in Low-Mortality DRGs | |||
| Full-EHR not receiving MU | −2.91 | −4.31 to −1.51 | <0.001 |
| EHR that attests to MU | −0.93 | −2.00 to 0.13 | 0.086 |
| Death Rate among Surgical Inpatients with Serious Treatable Complications | |||
| Full-EHR not receiving MU | 0.12 | −0.37 to 0.60 | 0.641 |
| EHR that attests to MU | 0.16 | −0.22 to 0.53 | 0.410 |
| Non-Death Related PSI | |||
| Iatrogenic Pneumothorax Rate (collapsed lung due to medical treatment) | |||
| Full-EHR not receiving MU | −0.42 | −2.29 to 1.44 | 0.658 |
| EHR that attests to MU | −0.33 | −1.72 to 1.07 | 0.647 |
| Postoperative Physiologic and Metabolic Derangement Rate | |||
| Full-EHR not receiving MU | −2.42 | −4.35 to −0.49 | 0.014 |
| EHR that attests to MU | −1.99 | −3.27 to −0.71 | 0.002 |
| Postoperative Respiratory Failure Rate (breathing failure after surgery) | |||
| Full-EHR not receiving MU | 0.68 | −0.01 to 1.31 | 0.053 |
| EHR that attests to MU | 0.47 | −0.05 to 0.99 | 0.077 |
| Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate (serious blood clots after surgery) | |||
| Full-EHR not receiving MU | −0.13 | −0.91 to 0.65 | 0.744 |
| EHR that attests to MU | −0.89 | −1.44 to −0.34 | 0.001 |
| Postoperative Sepsis Rate | |||
| Full-EHR not receiving MU | 0.63 | −0.31 to 1.56 | 0.188 |
| EHR that attests to MU | −0.17 | −0.86 to 0.52 | 0.634 |
| Postoperative Wound Dehiscence Rate (wounds split open after surgery) | |||
| Full-EHR not receiving MU | −1.93 | −3.43 to −0.43 | 0.011 |
| EHR that attests to MU | −0.86 | −2.02 to 0.31 | 0.152 |
| PSI-90 Composite Score | |||
| Full-EHR not receiving MU | −0.02 | −0.15 to 0.10 | 0.701 |
| EHR that attests to MU | −0.07 | −0.16 to 0.02 | 0.122 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trout, K.E.; Chen, L.-W.; Wilson, F.A.; Tak, H.J.; Palm, D. The Impact of Meaningful Use and Electronic Health Records on Hospital Patient Safety. Int. J. Environ. Res. Public Health 2022, 19, 12525. https://doi.org/10.3390/ijerph191912525
Trout KE, Chen L-W, Wilson FA, Tak HJ, Palm D. The Impact of Meaningful Use and Electronic Health Records on Hospital Patient Safety. International Journal of Environmental Research and Public Health. 2022; 19(19):12525. https://doi.org/10.3390/ijerph191912525
Chicago/Turabian StyleTrout, Kate E., Li-Wu Chen, Fernando A. Wilson, Hyo Jung Tak, and David Palm. 2022. "The Impact of Meaningful Use and Electronic Health Records on Hospital Patient Safety" International Journal of Environmental Research and Public Health 19, no. 19: 12525. https://doi.org/10.3390/ijerph191912525
APA StyleTrout, K. E., Chen, L.-W., Wilson, F. A., Tak, H. J., & Palm, D. (2022). The Impact of Meaningful Use and Electronic Health Records on Hospital Patient Safety. International Journal of Environmental Research and Public Health, 19(19), 12525. https://doi.org/10.3390/ijerph191912525






