A Health Belief Model-Based Motivational Interviewing for Medication Adherence and Treatment Success in Pulmonary Tuberculosis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Theory Used in the Motivational Interviewing Model
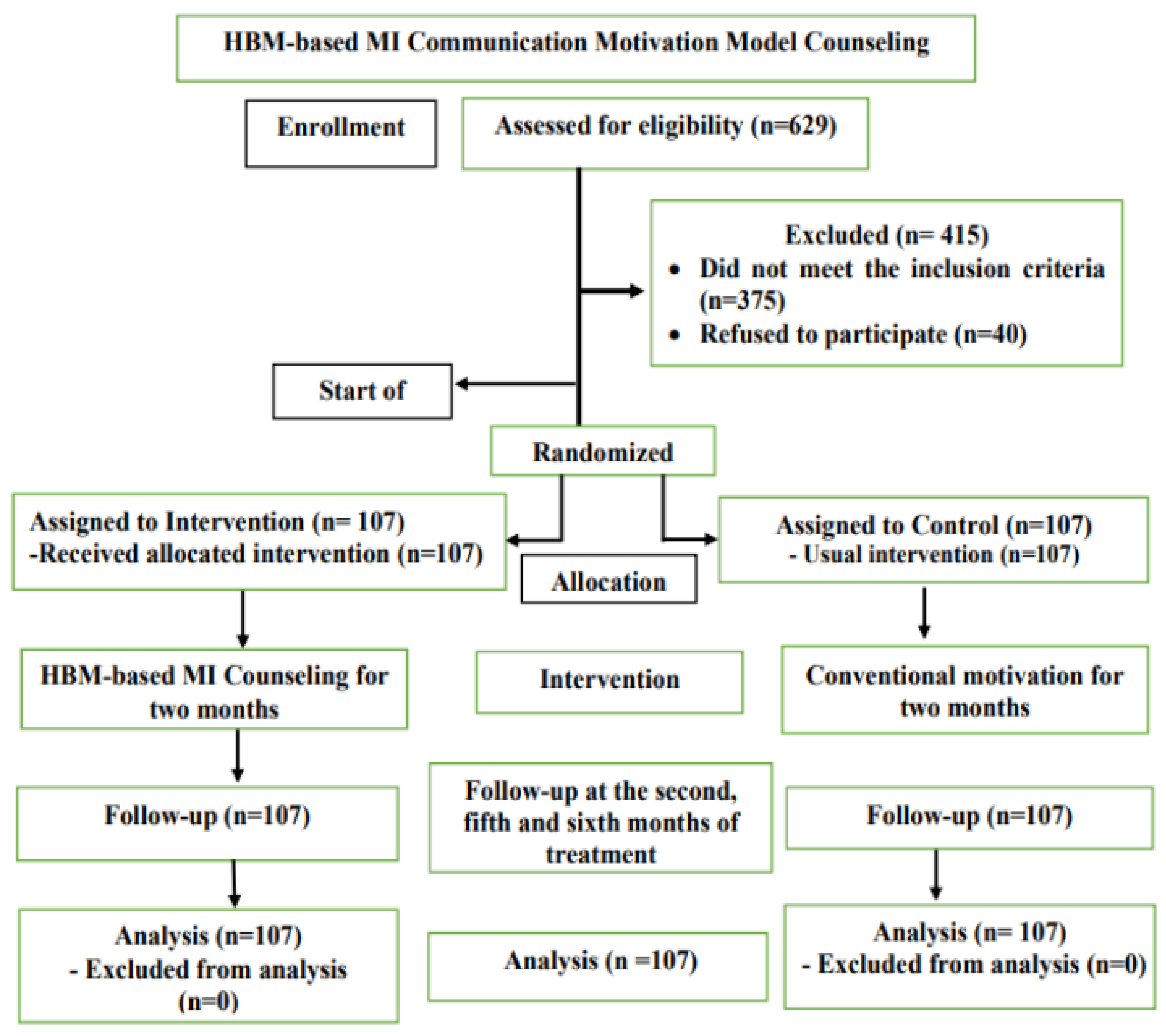
2.2. Study Design and Participants
2.3. Sampling and Data Collection
2.4. Primary Outcome
- 1.
- Improved medication adherence for 6 months in each counseling group. The results of the HBM-based MI intervention were compared with conventional counseling. Adherence to taking medication was measured by the percentage of pills taken. The number of unit doses taken by the patient in the second and sixth months of treatment was checked at the time of the visit to the community health center. This number was then compared with the total number of units the patient received to calculate the compliance ratio.
- 2.
- Treatment success was measured by bacteriological sputum examination, carried out after each phase of treatment. The examination was carried out following the standard reference for TB treatment, namely at the end of the intensive phase in the second month, and in the fifth and sixth months. Treatment was considered successful if the sputum was negative at the end of the treatment phase and at one of the previous examinations [11].
2.5. Secondary Results
2.6. Intervention Procedure
2.7. Statistical Analysis
2.8. Ethics Statement
3. Results
3.1. Primary Outcome
3.2. Secondary Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tola, H.H.; Shojaeizadeh, D.; Tol, A.; Garmaroudi, G.; Yekaninejad, M.S.; Kebede, A.; Ejeta, L.T.; Kassa, D.; Klinkenberg, E. Psychological and educational intervention to improve Tuberculosis treatment adherence in Ethiopia based on health belief model: A cluster randomized control trial. PLoS ONE 2016, 11, e0155147. [Google Scholar] [CrossRef]
- Indonesian Ministry of Health. Basic Health Research Year 2018; Agency of Health Dev Res Pusdatin: Jakarta, Indonesia, 2019. Available online: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274 (accessed on 10 December 2019).
- World Health Organization. Global Tuberculosis Report 2017; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/tb/publications/global_report/gtbr2017_main (accessed on 1 May 2020).
- Abraham, C.; Sheeran, P. The health belief model. In Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models; Conner, M., Norman, P., Eds.; Open University Press: Maidenhead, UK, 2015; pp. 30–69. Available online: https://www.cambridge.org/core/terms (accessed on 10 July 2020).
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Azizi, N.; Karimy, M.; Salahshour, V.N. Original Article Determinants of adherence to Tuberculosis treatment in Iranian patients: Application of health belief model. J. Infect. Dev. Ctries 2018, 12, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Orji, R.; Vassileva, J.; Mandryk, R. Towards an Effective Health Interventions Design: An Extension of the Health Belief Model. Online J. Public Health Inf. 2012, 4. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the Health Belief Model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Sastroasmoro, S.; Ismail, S. Fundamentals of Clinical Research Methodology, 3rd ed.; CV Sagung Seto: Jakarta, Indonesia, 2018. [Google Scholar]
- Lavsa, S.M.; Holzworth, A.; Ansani, N.T. Selection of a validated scale for measuring medication adherence. J. Am. Pharm. Assoc. 2011, 51, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Indonesian Ministry of Health. Regulation of The Minister of Health Number 67 Year 2016 Concerning Tuberculosis Control; Indonesian Ministry of Health: Pusdatin, Jakarta, 2016.
- Norcross, J.C.; Krebs, P.M.; Prochaska, J.O. Stages of change. J. Clin. Psychol. 2011, 67, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Hill, S.; Kavookjian, J.; Hill, S.; Kavookjian, J. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV Motivational interviewing as a behavioral intervention to increase HAART adherence in patients who are HIV-positive: A systematic review of the literature who are HIV-positive: A systema. AIDS Care 2013, 24, 37–41. [Google Scholar]
- Zomahoun, H.T.V.; Guenette, L.; Gregoire, J.; Lauzier, S.; Lawani, A.M.; Ferdynus, C.; Huiart, L.; Moisan, J. Effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases: A systematic review and meta-analysis. Int. J. Epidemiol. 2017, 46, 589–602. [Google Scholar] [CrossRef]
- Cook, P.F.; Bremer, R.W. Feasibility of motivational interviewing delivered by a glaucoma educator to improve medication adherence. Clin. Ophthalmol. 2010, 1091–1101. [Google Scholar] [CrossRef] [PubMed]
- Golin, C.E.; Anne, J.; Catherine, E.; Shilpa, A.G.; Groves, J. Longitudinal Effects of SafeTalk, a Motivational Interviewing-Based Program to Improve Safer Sex Practices Among People Living with HIV/AIDS. AIDS Behav. 2012, 65, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.J. A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior. Health Commun. 2010, 25, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Krukowski, R.A.; Di Lillo, V.; Ingle, K.; Harvey, J.R.; West, D.S. Design and Methods of a Synchronous Online Motivational Interviewing Intervention for Weight Management Corresponding Author. J. Patient Educ. Couns. 2015, 5, e69. [Google Scholar] [CrossRef]
- Brenes, G.A.; Ingram, C.W.; Danhauer, S.C. Benefits and Challenges of Conducting Psychotherapy by Telephone. Prof. Psychol. Res. Prect. 2011, 42, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Shabibi, P.; Sadegh Abedzadeh Zavareh, M.; Sayehmiri, K.; Qorbani, M.; Safari, O.; Rastegarimehr, B.; Mansourian, M. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electron. Phys. 2017, 9, 2008–5842. [Google Scholar] [CrossRef] [PubMed]
- Muture, B.N.; Keraka, M.N.; Kimuu, P.K.; Kabiru, E.W.; Ombeka, V.O.; Oguya, F. Factors associated with default from treatment among Tuberkulosis patients in nairobi province, Kenya: A case control study. BMC Public Health 2011, 11, 2–10. [Google Scholar] [CrossRef]
- Notoatmodjo, S. Promosi Kesehatan dan Ilmu Perilaku; Rineka Cipta: Jakarta, Indonesia, 2010. [Google Scholar]
- Vera Rahardjo, S.S.; Murti, B. Health Belief Model and Precede Proceed on the Risk Factors of Multidrug Resistant Tuberculosis in Surakarta, Central Java. J. Epidemiol. Public Health 2017, 2, 241–254. [Google Scholar] [CrossRef]
- Palacio, A.; Garay, D.; Langer, B.; Taylor, J.; Wood, B.A.; Tamariz, L. Motivational Interviewing Improves Medication Adherence: A Systematic Review and Meta-analysis. J. Gen. Intern. Med. 2016, 31, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.D.; Soucy, J.N.; Hadjistavropoulos, H.D. Mixed-method evaluation of an online motivational intervention as a pre-treatment to internet-delivered cognitive behaviour therapy: Immediate benefits and user feedback. Internet Interv. 2020, 20, 100311. [Google Scholar] [CrossRef] [PubMed]
- Hedegaard, U.; Hallas, J.; Kjeldsen, L.J. Multifaceted Intervention Including Motivational Interviewing to Support Medication Adherence after Stroke/Transient Ischemic Attack: A Randomized Trial. Cerebrovasc. Dis. Extra 2014, 4, 221–234. [Google Scholar] [CrossRef]
- Dombrowski, S.U.; Sniehotta, F.F.; Avenell, A.; Johnston, M.; MacLennan, G.; Araújo-Soares, V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: A systematic review. Health Psychol. Rev. 2012, 6, 7–32. [Google Scholar] [CrossRef]
- Kementerian Kesehatan Republik Indonesia. Infodatin Tuberkulosis, 2018; Ministry of Health: Jakarta, Indonesia, 2018. Available online: https://pusdatin.kemkes.go.id/article/view/18101500001/infodatin-tuberkulosis-2018.html (accessed on 10 June 2020).
- Holmes EA, F.; Hughes, D.A.; Morrison, V.L. Predicting adherence to medications using health psychology theories: A systematic review of 20 years of empirical research. Value Health 2014, 17, 863–876. [Google Scholar] [CrossRef] [PubMed]
- Jm, M.I.; Kredo, T.; Volmink, J. Patient education and counselling for promoting adherence to treatment for Tuberculosis. Cochrane Libr. 2012, 5, CD006591. [Google Scholar]
- Zein, R.A.; Suhariadi, F.; Hendriani, W. Estimating the effect of lay knowledge and prior contact with pulmonary TB patients, on health-belief model in a high-risk pulmonary TB transmission population. Psychol. Res. Behav. Manag. 2017, 10, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Chapman, H.J.; Veras-Estévez, B.A.; Pomeranz, J.L.; Pérez-Then, E.N.; Marcelino, B.; Lauzardo, M. The Role of Powerlessness Among Health Care Workers in Tuberculosis Infection Control. Qual. Health Res. 2017, 27, 2116–2127. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Intervention (n = 107) | Control (n = 107) | p-Value 1 | |
|---|---|---|---|---|
| 1. | Gender | |||
| Male | 64 (59.8) | 60 (56.1) | 0.580 | |
| Female | 43 (40.2) | 47 (43.9) | ||
| 2. | Marital status | |||
| Married | 89 (83.2) | 82 (76.6) | 0.087 | |
| Unmarried | 15 (14.0) | 14 (13.1) | ||
| Other | 3 (2.8) | 11 (10.3) | ||
| 3. | Education level | |||
| Elementary or less Medium to high | 56 (52.3) 51 (47.7) | 67 (62.6) 40 (37.4) | 0.128 | |
| 4. | Have occupation | |||
| No | 24 (22.4) | 32 (29.9) | 0.213 | |
| Yes | 83 (77.6) | 75 (70.1) | ||
| 5. | Age (y) | 42.3 ± 12 | 43 ± 10.9 | 0.412 2 |
| 6. | Income * | 2,310,280 ± 489,692 | 2,083,177 ± 100,000 | 0.000 2 |
| HBM-Based MI Communication Motivation Model | Intervention | Control | p-Value | |
|---|---|---|---|---|
| 1 | Adherence | |||
| Adherence | 103 (96.3) | 94 (87.9) | 0.023 1 | |
| Non-adherence | 4 (3.7) | 13 (12.1) | ||
| Mean difference in adherence | 115.65 | 99.35 | 0.037 2 | |
| 2 | Treatment success | |||
| Success | 103 (96.3) | 95 (88.8) | 0.038 1 | |
| No success | 4 (3.7) | 12 (11.2) | ||
| Variabel | Medication Adherence | Treatment Success | |||
|---|---|---|---|---|---|
| ARR * | p-Value * | ARR * | p-Value * | ||
| 1. | MI-HBM intervention | 4.51 | 0.018 | 3.81 | 0.038 |
| 2. | Good knowledge | 2.93 | 0.042 | 3.49 | 0.022 |
| 3. | Good family support | 0.63 | 0.507 | 0.708 | 0.618 |
| 4. | Good perception of health workers’ attitudes | 0.46 | 0.233 | 0.538 | 0.337 |
| Other Variables | Medication Adherence | Treatment Success | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adherence | Non Adherence | p-Value 1 | Success | Non Successful | p-Value 1 | ||||||||
| 1 | Age (y) | ||||||||||||
| 18–45 | 107 (92.2) | 9 (7.8) | 0.913 | 107 (92.2) | 9 (7.8) | 0.913 | |||||||
| 46–65 | 90 (91.8) | 8 (8.2) | 90 (91.8) | 8 (8.2) | |||||||||
| 2 | Education level | ||||||||||||
| Basic | 112 (91.1) | 11(8.9) | 0.530 | 113 (91.9) | 10 (8.1) | 0.673 | |||||||
| Medium to high | 85 (93.4) | 6 (6.6) | 85 (93.4) | 6 (6.6) | |||||||||
| 3 | Income | ||||||||||||
| Sufficient | 54 (93.1) | 4 (6.9) | 0.730 | 54 (93.1) | 4 (6.9) | 0.844 | |||||||
| Insufficient | 143 (91.7) | 13 (8.3) | 144 (92.3) | 12 (7.7) | |||||||||
| 4 | Knowledge of TBC | ||||||||||||
| Good | 138 (95.2) | 7 (4.80) | 0.015 | 139 (95.9) | 6 (4.1) | 0.007 | |||||||
| Poor | 59 (85.5) | 10 (14.5) | 59 (85.5) | 10 (14.5) | |||||||||
| 5 | Family support | ||||||||||||
| Good | 157 (91.8) | 14 (8.2) | 0.240 | 158 (92.4) | 13 (7.6) | 0.189 | |||||||
| Poor | 40 (93.0) | 3 (7.0) | 40 (93.0) | 3 (7.0) | |||||||||
| 6 | Perceptions of attitudes of health workers | ||||||||||||
| Good | 146 (91.8) | 13 (8.2) | 0.188 | 147 (92.5) | 12 (7.5) | 0.147 | |||||||
| Poor | 51(92.7) | 4 (7.3) | 51 (92.7) | 4 (7.3) | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parwati, N.M.; Bakta, I.M.; Januraga, P.P.; Wirawan, I.M.A. A Health Belief Model-Based Motivational Interviewing for Medication Adherence and Treatment Success in Pulmonary Tuberculosis Patients. Int. J. Environ. Res. Public Health 2021, 18, 13238. https://doi.org/10.3390/ijerph182413238
Parwati NM, Bakta IM, Januraga PP, Wirawan IMA. A Health Belief Model-Based Motivational Interviewing for Medication Adherence and Treatment Success in Pulmonary Tuberculosis Patients. International Journal of Environmental Research and Public Health. 2021; 18(24):13238. https://doi.org/10.3390/ijerph182413238
Chicago/Turabian StyleParwati, Ni Made, I Made Bakta, Pande Putu Januraga, and I Made Ady Wirawan. 2021. "A Health Belief Model-Based Motivational Interviewing for Medication Adherence and Treatment Success in Pulmonary Tuberculosis Patients" International Journal of Environmental Research and Public Health 18, no. 24: 13238. https://doi.org/10.3390/ijerph182413238
APA StyleParwati, N. M., Bakta, I. M., Januraga, P. P., & Wirawan, I. M. A. (2021). A Health Belief Model-Based Motivational Interviewing for Medication Adherence and Treatment Success in Pulmonary Tuberculosis Patients. International Journal of Environmental Research and Public Health, 18(24), 13238. https://doi.org/10.3390/ijerph182413238







