Leveraging HIV Care Infrastructures for Integrated Chronic Disease and Pandemic Management in Sub-Saharan Africa
Abstract
1. Introduction
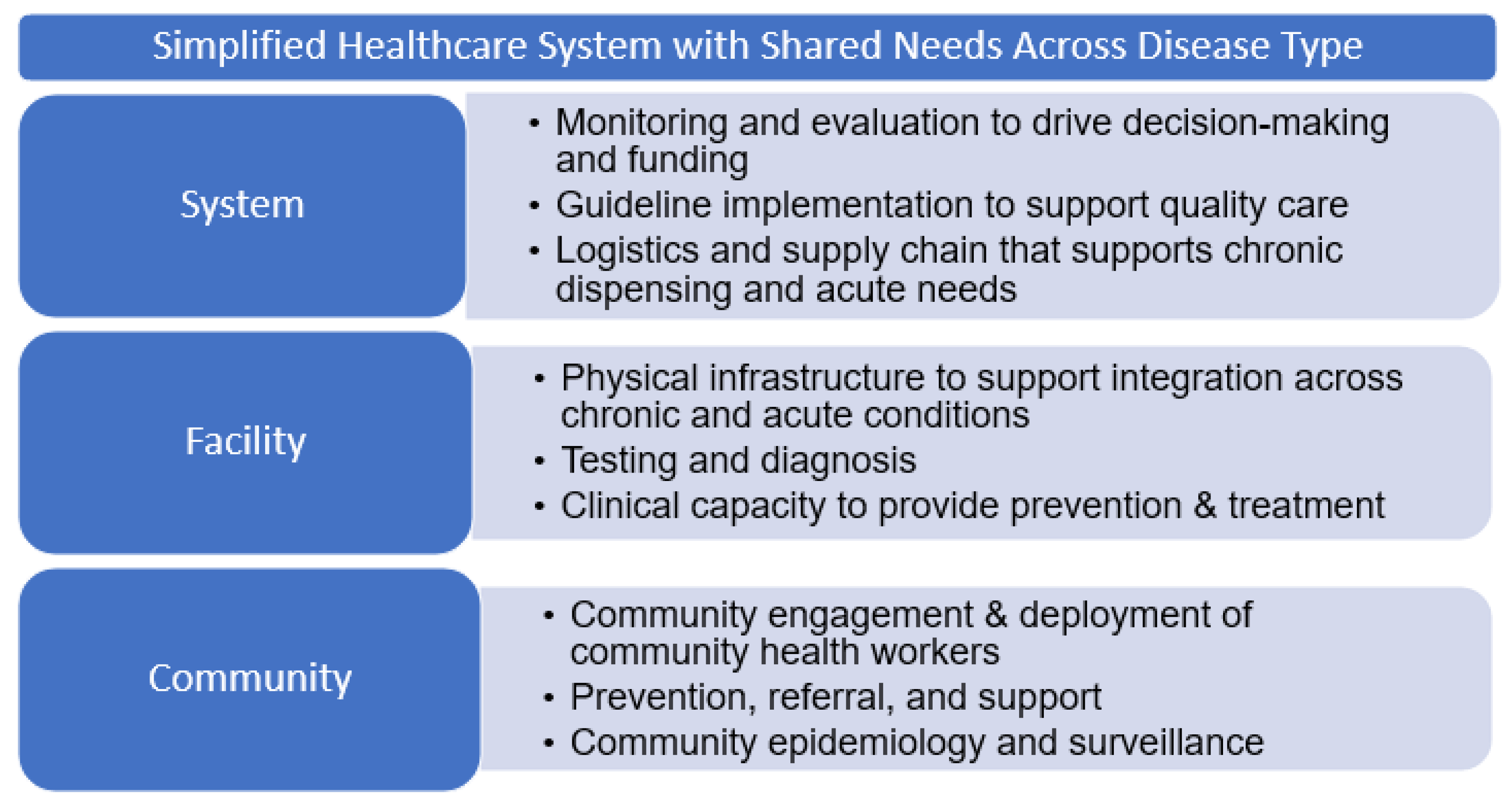
2. Integrated Service Delivery
3. A South African Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fosu, A.K. Growth, Inequality and Poverty in Sub-Saharan Africa: Recent Progress in a Global Context. Oxf. Dev. Stud. 2015, 43, 44–59. [Google Scholar] [CrossRef]
- Bicaba, Z.; Brixiová, Z.; Ncube, M. Can Extreme Poverty in Sub-Saharan Africa be Eliminated by 2030? J. Afr. Dev. 2017, 19, 93–110. [Google Scholar]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 2021, 1–18. [Google Scholar] [CrossRef]
- Ake, J.A.; Polyak, C.S.; Crowell, T.A.; Kiweewa, F.; Semwogerere, M.; Maganga, L.; Bahemana, E.; Maswai, J.; Langat, R.; Owuoth, J.; et al. Noninfectious Comorbidity in the African Cohort Study. Clin. Infect. Dis. 2018, 69, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Yaya, S.; Ekholuenetale, M.; Bishwajit, G. Differentials in prevalence and correlates of metabolic risk factors of non-communicable diseases among women in sub-Saharan Africa: Evidence from 33 countries. BMC Public Health 2018, 18, 1168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zeng, Q.; Cai, W.; Ruan, W. Trends of cervical cancer at global, regional, and national level: Data from the Global Burden of Disease study 2019. BMC Public Health 2021, 21, 894. [Google Scholar] [CrossRef]
- Anyigba, C.A.; Awandare, G.A.; Paemka, L. Breast cancer in sub-Saharan Africa: The current state and uncertain future. Exp. Biol. Med. 2021, 246, 1377–1387. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. UNAIDS Global AIDS Update 2021; UNAIDS: Geneva, Switzerland, 2021. [Google Scholar]
- Martial, N.T.; Mubarik, S.; Yu, C. Long-term trends of tuberculosis incidence and mortality in four central African countries. Sci. Rep. 2021, 11, 16624. [Google Scholar] [CrossRef] [PubMed]
- Osman, M.; Karat, A.S.; Khan, M.; Meehan, S.-A.; von Delft, A.; Brey, Z.; Charalambous, S.; Hesseling, A.C.; Naidoo, P.; Loveday, M. Health system determinants of tuberculosis mortality in South Africa: A causal loop model. BMC Health Serv. Res. 2021, 21, 388. [Google Scholar] [CrossRef]
- Lungu, P.; Kerkhoff, A.D.; Kasapo, C.C.; Mzyece, J.; Nyimbili, S.; Chimzizi, R.; Silumesii, A.; Kagujje, M.; Subbaraman, R.; Muyoyeta, M.; et al. Tuberculosis care cascade in Zambia—Identifying the gaps in order to improve outcomes: A population-based analysis. BMJ Open 2021, 11, e044867. [Google Scholar] [CrossRef] [PubMed]
- Weber, A.-C.; Bogler, L.; Vollmer, S.; Simen-Kapeu, A.; Ekpini, R.E.; Zagre, N.M. The wealth gradient in diarrhoea, acute respiratory infections, and malaria in childhood over time: A descriptive analysis using DHS and MICS from Western and Central Africa between 1995 and 2017. J. Glob. Health 2021, 11, 13009. [Google Scholar] [CrossRef] [PubMed]
- Africa CDC COVID-19 Dashboard [Database on the Internet]. African Union. 2021. Available online: https://africacdc.org/covid-19/ (accessed on 15 September 2021).
- Brault, M.A.; Spiegelman, D.; Abdool Karim, S.S.; Vermund, S.H. Integrating and Interpreting Findings from the Latest Treatment as Prevention Trials. Curr. HIV/AIDS Rep. 2020, 17, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Otieno, G.; Whiteside, Y.O.; Achia, T.; Kwaro, D.; Zielinski-Gutierrez, E.; Ojoo, S.; Sewe, M.; Musingila, P.; Akelo, V.; Obor, D.; et al. Decreased HIV-associated mortality rates during scale-up of antiretroviral therapy, 2011–2016. AIDS 2019, 33, 2423–2430. [Google Scholar] [CrossRef] [PubMed]
- Levitt, N.S.; Steyn, K.; Dave, J.; Bradshaw, D. Chronic noncommunicable diseases and HIV-AIDS on a collision course: Relevance for health care delivery, particularly in low-resource settings—Insights from South Africa. Am. J. Clin. Nutr. 2011, 94, 1690S–1696S. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard; World Health Organization: Geneva, Switzerland, 2021; Available online: https://covid19.who.int/ (accessed on 7 June 2021).
- Hatchett, R.; Berkley, S.; Ghebreyesus, T.; Fore, H. COVAX Joint Statement: Call to action to equip COVAX to deliver 2 billion doses in 2021. In World Health Organization News; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Patel, L.N.; Kozikott, S.; Ilboudo, R.; Kamateeka, M.; Lamorde, M.; Subah, M.; Tsiouris, F.; Vorndran, A.; Lee, C.T. Safer primary healthcare facilities are needed to protect healthcare workers and maintain essential services: Lessons learned from a multicountry COVID-19 emergency response initiative. BMJ Glob. Health 2021, 6, e005833. [Google Scholar] [CrossRef] [PubMed]
- Boggs, D.; Polack, S.; Kuper, H.; Foster, A. Shifting the focus to functioning: Essential for achieving Sustainable Development Goal 3, inclusive Universal Health Coverage and supporting COVID-19 survivors. Glob. Health Action 2021, 14, 1903214. [Google Scholar] [CrossRef]
- Gouda, H.N.; Charlson, F.; Sorsdahl, K.; Ahmadzada, S.; Ferrari, A.J.; Erskine, H.; Leung, J.; Santamauro, D.; Lund, C.; Aminde, L.N.; et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: Results from the Global Burden of Disease Study 2017. Lancet Glob. Health 2019, 7, e1375–e1387. [Google Scholar] [CrossRef]
- Kontis, V.; Cobb, L.K.; Mathers, C.D.; Frieden, T.R.; Ezzati, M.; Danaei, G. Three Public Health Interventions Could Save 94 Million Lives in 25 Years. Circulation 2019, 140, 715–725. [Google Scholar] [CrossRef]
- Hall, V.; Thomsen, R.W.; Henriksen, O.; Lohse, N. Diabetes in Sub Saharan Africa 1999–2011: Epidemiology and public health implications. a systematic review. BMC Public Health 2011, 11, 564. [Google Scholar] [CrossRef] [PubMed]
- WHO; World Economic Forum. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseaes in Low- and Middle-Income Countries; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Zarocostas, J. WHO lists “best buys” for cutting deaths from non-communicable disease. BMJ 2011, 342, d2648. [Google Scholar] [CrossRef]
- Abila, D.B.; Ainembabazi, P.; Wabinga, H. COVID-19 pandemic and the widening gap to access cancer services in Uganda. Pan Afr. Med. J. 2020, 35, 140. [Google Scholar] [CrossRef]
- Solanki, G.; Kelly, G.; Cornell, J.; Geffen, L.; Doherty, T. The need to incorporate the impact of population ageing into the post-COVID-19 policy and planning reset in Low and Middle Income Countries. Glob. Health Action 2021, 14, 1921351. [Google Scholar] [CrossRef] [PubMed]
- Bendavid, E. Past and Future Performance: PEPFAR in the Landscape of Foreign Aid for Health. Curr. HIV/AIDS Rep. 2016, 13, 256–262. [Google Scholar] [CrossRef] [PubMed]
- US Department of State. The United States President’s Emergency Plan for AIDS Relief (PEPFAR) 2019 Annual Report to Congress; US Department of State, Ed.; U.S. Department of State: Washington, DC, USA, 2019.
- Sturchio, J.L.; Cohen, G.M. How PEPFAR’s Public-Private Partnerships Achieved Ambitious Goals, From Improving Labs to Strengthening Supply Chains. Health Aff. 2012, 31, 1450–1458. [Google Scholar] [CrossRef]
- Porter, L.E.; Bouey, P.D.; Curtis, S.; Hochgesang, M.; Idele, P.; Jefferson, B.; Lemma, W.; Myrick, R.; Nuwagaba-Biribonwoha, H.; Prybylski, D.; et al. Beyond indicators: Advances in global HIV monitoring and evaluation during the PEPFAR era. J. Acquir. Immune Defic. Syndr. 2012, 60 (Suppl. 3), S120–S126. [Google Scholar] [CrossRef] [PubMed]
- Golin, R.; Godfrey, C.; Firth, J.; Lee, L.; Minior, T.; Phelps, B.R.; Raizes, E.G.; Ake, J.A.; Siberry, G.K. PEPFAR’s response to the convergence of the HIV and COVID-19 pandemics in Sub-Saharan Africa. J. Int. AIDS Soc. 2020, 23, e25587. [Google Scholar] [CrossRef]
- Goosby, E.; Von Zinkernagel, D.; Holmes, C.; Haroz, D.; Walsh, T. Raising the bar: PEPFAR and new paradigms for global health. J. Acquir. Immune Defic. Syndr. 2012, 60 (Suppl. 3), S158–S162. [Google Scholar] [CrossRef]
- Vogus, A.; Graff, K. PEPFAR Transitions to Country Ownership: Review of Past Donor Transitions and Application of Lessons Learned to the Eastern Caribbean. Glob. Health Sci. Pract. 2015, 3, 274–286. [Google Scholar] [CrossRef]
- Janssens, B.; Van Damme, W.; Raleigh, B.; Gupta, J.; Khem, S.; Ty, K.S.; Vun, M.C.; Ford, N.; Zachariah, R. Offering integrated care for HIV/AIDS, diabetes and hypertension within chronic disease clinics in Cambodia. Bull. World Health Organ. 2007, 85, 880–885. [Google Scholar] [CrossRef]
- Topp, S.M.; Chipukuma, J.M.; Giganti, M.; Mwango, L.K.; Chiko, L.M.; Tambatamba-Chapula, B.; Wamulume, C.S.; Reid, S. Strengthening Health Systems at Facility-Level: Feasibility of Integrating Antiretroviral Therapy into Primary Health Care Services in Lusaka, Zambia. PLoS ONE 2010, 5, e11522. [Google Scholar] [CrossRef]
- Njuguna, B.; Vorkoper, S.; Patel, P.; Reid, M.J.; Vedanthan, R.; Pfaff, C.; Park, P.H.; Fischer, L.; Laktabai, J.; Pastakia, S.D. Models of integration of HIV and noncommunicable disease care in sub-Saharan Africa: Lessons learned and evidence gaps. AIDS 2018, 32 (Suppl. 1), S33–S42. [Google Scholar] [CrossRef]
- Maitra, S.; Brault, M.A.; Schensul, S.L.; Schensul, J.J.; Nastasi, B.K.; Verma, R.K.; Burleson, J.A. An Approach to Mental Health in Low- and Middle-Income Countries: A Case Example from Urban India. Int. J. Ment. Health 2015, 44, 215–230. [Google Scholar] [CrossRef] [PubMed]
- Duffy, M.; Ojikutu, B.; Andrian, S.; Sohng, E.; Minior, T.; Hirschhorn, L.R. Non-communicable diseases and HIV care and treatment: Models of integrated service delivery. Trop. Med. Int. Health 2017, 22, 926–937. [Google Scholar] [CrossRef] [PubMed]
- Kintu, A.; Sando, D.; Okello, S.; Mutungi, G.; Guwatudde, D.; Menzies, N.A.; Danaei, G.; Verguet, S. Integrating care for non-communicable diseases into routine HIV services: Key considerations for policy design in sub-Saharan Africa. J. Int. AIDS Soc. 2020, 23, e25508. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, K.; Van Wyk, J. What the elderly experience and expect from primary care services in KwaZulu-Natal, South Africa. Afr. J. Prim. Health Care Fam. Med. 2019, 11, e1–e6. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, & Medicine. The Convergence of Infectious Diseases and Noncommunicable Diseases: Proceedings of a Workshop; Ogawa, V.A., Shah, C.M., Negussie, Y., Nicholson, A., Eds.; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar]
- Shenoi, S.V.; Moll, A.P.; Brooks, R.P.; Kyriakides, T.; Andrews, L.; Kompala, T.; Upadhya, D.; Altice, F.; Eksteen, F.J.; Friedland, G. Integrated Tuberculosis/Human Immunodeficiency Virus Community-Based Case Finding in Rural South Africa: Implications for Tuberculosis Control Efforts. Open Forum Infect. Dis. 2017, 4, ofx092. [Google Scholar] [CrossRef]
- Havlir, D.V.; Balzer, L.B.; Charlebois, E.D.; Clark, T.D.; Kwarisiima, D.; Ayieko, J.; Kabami, J.; Sang, N.; Liegler, T.; Chamie, G.; et al. HIV Testing and Treatment with the Use of a Community Health Approach in Rural Africa. N. Engl. J. Med. 2019, 381, 219–229. [Google Scholar] [CrossRef]
- Patel, M.R.; Mushavi, A.; Balachandra, S.; Shambira, G.; Nyakura, J.; Mugurungi, O.; Kilmarx, P.H.; Rivadeneira, E.; Dinh, T.-H. HIV-exposed uninfected infant morbidity and mortality within a nationally representative prospective cohort of mother-infant pairs in Zimbabwe. AIDS 2020, 34, 1339–1346. [Google Scholar] [CrossRef]
- Duffy, C.; Kenga, D.B.; Gebretsadik, T.; Maússe, F.E.; Manjate, A.; Zaqueu, E.; Fernando, H.F.; Green, A.F.; Sacarlal, J.; Moon, T.D. Multiple Concurrent Illnesses Associated with Anemia in HIV-Infected and HIV-Exposed Uninfected Children Aged 6–59 Months, Hospitalized in Mozambique. Am. J. Trop. Med. Hyg. 2020, 102, 605–612. [Google Scholar] [CrossRef]
- Slogrove, A.L.; Powis, K.M.; Johnson, L.F.; Stover, J.; Mahy, M. Estimates of the global population of children who are HIV-exposed and uninfected, 2000–2018: A modelling study. Lancet Glob. Health 2020, 8, e67–e75. [Google Scholar] [CrossRef]
- Carlucci, J.G.; Liu, Y.; Friedman, H.; E Pelayo, B.; Robelin, K.; Sheldon, E.K.; Clouse, K.; Vermund, S.H. Attrition of HIV-exposed infants from early infant diagnosis services in low- and middle-income countries: A systematic review and meta-analysis. J. Int. AIDS Soc. 2018, 21, e25209. [Google Scholar] [CrossRef] [PubMed]
- Sofeu, C.L.; Tejiokem, M.C.; Penda, C.I.; Protopopescu, C.; Ndongo, F.A.; Ndiang, S.T.; Guemkam, G.; Warszawski, J.; Faye, A.; Giorgi, R.; et al. Early treated HIV-infected children remain at risk of growth retardation during the first five years of life: Results from the ANRS-PEDIACAM cohort in Cameroon. PLoS ONE 2019, 14, e0219960. [Google Scholar] [CrossRef] [PubMed]
- Ntozini, R.; Chandna, J.; Evans, C.; Chasekwa, B.; Majo, F.D.; Kandawasvika, G.; Tavengwa, N.V.; Mutasa, B.; Mutasa, K.; Moulton, L.H.; et al. Early child development in children who are HIV-exposed uninfected compared to children who are HIV-unexposed: Observational sub-study of a cluster-randomized trial in rural Zimbabwe. J. Int. AIDS Soc. 2020, 23, e25456. [Google Scholar] [CrossRef]
- Crowell, C.S.; Williams, P.L.; Yildirim, C.; Van Dyke, R.B.; Smith, R.; Chadwick, E.G.; Seage, G.R.; Diperna, A.; Hazra, R. Safety of in-utero antiretroviral exposure: Neurologic outcomes in children who are HIV-exposed but uninfected. AIDS 2020, 34, 1377–1387. [Google Scholar] [CrossRef]
- Scrymgeour-Wedderburn, C.; Yeung, S.; Rehman, A.; Stadler, J.A.M.; Nhapi, R.T.; Barnett, W.; Myer, L.; Gibb, D.M.; Zar, H.; Stein, D.; et al. Neurodevelopment of HIV-exposed uninfected children in South Africa: Outcomes from an observational birth cohort study. Lancet Child Adolesc. Health 2019, 3, 803–813. [Google Scholar] [CrossRef]
- Goga, A.E.; Lombard, C.; Jackson, D.; Ramokolo, V.; Ngandu, N.K.; Sherman, G.; Puren, A.; Chirinda, W.; Bhardwaj, S.; Makhari, N.; et al. Impact of breastfeeding, maternal antiretroviral treatment and health service factors on 18-month vertical transmission of HIV and HIV-free survival: Results from a nationally representative HIV-exposed infant cohort, South Africa. J. Epidemiol. Community Health 2020, 74, 1069–1077. [Google Scholar] [CrossRef]
- Ramokolo, V.; Goga, A.E.; Slogrove, A.; Powis, K.M. Unmasking the vulnerabilities of uninfected children exposed to HIV. BMJ 2019, 366, l4479. [Google Scholar] [CrossRef]
- Le Roux, S.M.; Abrams, E.J.; Nguyen, K.; Myer, L. Clinical outcomes of HIV-exposed, HIV-uninfected children in sub-Saharan Africa. Trop. Med. Int. Health TM IH 2016, 21, 829–845. [Google Scholar] [CrossRef]
- Marotta, C.; Giaquinto, C.; Di Gennaro, F.; Chhaganlal, K.D.; Saracino, A.; Moiane, J.; Maringhini, G.; Pizzol, D.; Putoto, G.; Monno, L.; et al. Pathways of care for HIV infected children in Beira, Mozambique: Pre-post intervention study to assess impact of task shifting. BMC Public Health 2018, 18, 703. [Google Scholar] [CrossRef]
- Ajibola, G.; Bennett, K.; Powis, K.M.; Hughes, M.D.; Leidner, J.; Kgole, S.; Batlang, O.; Mmalane, M.; Makhema, J.; Lockman, S.; et al. Decreased diarrheal and respiratory disease in HIV exposed uninfected children following vaccination with rotavirus and pneumococcal conjugate vaccines. PLoS ONE 2020, 15, e0244100. [Google Scholar] [CrossRef] [PubMed]
- Rotheram-Borus, M.J.; Christodoulou, J.; Rezvan, P.H.; Comulada, W.S.; Gordon, S.; Skeen, S.; Stewart, J.; Almirol, E.; Tomlinson, M. Maternal HIV does not affect resiliency among uninfected/HIV exposed South African children from birth to 5 years of age. AIDS 2019, 33, S5–S16. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, M.; Rotheram-Borus, M.J.; Le Roux, I.M.; Youssef, M.; Nelson, S.H.; Scheffler, A.; Weiss, R.E.; O’Connor, M.; Worthman, C.M. Thirty-Six-Month Outcomes of a Generalist Paraprofessional Perinatal Home Visiting Intervention in South Africa on Maternal Health and Child Health and Development. Prev. Sci. 2016, 17, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Archary, M.; Fairlie, L.; Slogrove, A. Current perspectives on paediatric HIV management from the Mexico International Aids Society Conference, 2019. S. Afr. J. HIV Med. 2019, 20, 5. [Google Scholar] [CrossRef][Green Version]
- Mulenga, P.; Mutanga, J. Follow-up of children HIV exposed uninfected through routine child health services: Zambian perspective. In Proceedings of the 5th Workshop on Children and Adolescents HIV Exposed and Uninfected, Mexico City, Mexico, 21 July 2019; International AIDS Society: Geneva, Switzerland, 2019. [Google Scholar]
- Shiri, T.; Birungi, J.; Garrib, A.V.; Kivuyo, S.L.; Namakoola, I.; Mghamba, J.; Musinguzi, J.; Kimaro, G.; Mutungi, G.; Nyirenda, M.J.; et al. Patient and health provider costs of integrated HIV, diabetes and hypertension ambulatory health services in low-income settings—An empirical socio-economic cohort study in Tanzania and Uganda. BMC Med. 2021, 19, 230. [Google Scholar] [CrossRef] [PubMed]
- Moucheraud, C.; Hing, M.; Seleman, J.; Phiri, K.; Chibwana, F.; Kahn, D.; Schooley, A.; Moses, A.; Hoffman, R. Integrated care experiences and out-of-pocket expenditures: A cross-sectional survey of adults receiving treatment for HIV and hypertension in Malawi. BMJ Open 2020, 10, e032652. [Google Scholar] [CrossRef] [PubMed]
- McGuire, F.; Vijayasingham, L.; Vassall, A.; Small, R.; Webb, D.; Guthrie, T.; Remme, M. Financing intersectoral action for health: A systematic review of co-financing models. Glob. Health 2019, 15, 86. [Google Scholar] [CrossRef]
- Rosenberg, M.; Amisi, J.A.; Szkwarko, D.; Tran, D.N.; Genberg, B.; Luetke, M.; Kianersi, S.; Namae, J.; Laktabai, J.; Pastakia, S. The relationship between a microfinance-based healthcare delivery platform, health insurance coverage, health screenings, and disease management in rural Western Kenya. BMC Health Serv. Res. 2020, 20, 868. [Google Scholar] [CrossRef] [PubMed]
- Woo, Y.L.; Gravitt, P.; Khor, S.K.; Ng, C.W.; Saville, M. Accelerating action on cervical screening in lower- and middle-income countries (LMICs) post COVID-19 era. Prev. Med. 2021, 144, 106294. [Google Scholar] [CrossRef]
- Bernard, C.; Seydi, M.; Tanon, A.; Messou, E.; Minga, A.; Font, H.; Dabis, F. The International Epidemiological Database to evaluate Aids (IeDEA) West Africa Collaboration Barriers influencing task-shifting for the management of depression in people living with HIV: A study from West Africa IeDEA cohort collaboration. AIDS Care 2021, 33, 352–356. [Google Scholar] [CrossRef]
- Aifah, A.; Onakomaiya, D.; Iwelunmor, J.; Oladele, D.; Gbajabiamila, T.; Obiezu-Umeh, C.; Nwaozuru, U.; Musa, A.Z.; Ezechi, O.; Ogedegbe, G. Nurses’ perceptions on implementing a task-shifting/sharing strategy for hypertension management in patients with HIV in Nigeria: A group concept mapping study. Implement. Sci. Commun. 2020, 1, 58. [Google Scholar] [CrossRef]
- Nyamayaro, P.; Bere, T.; Magidson, J.F.; Simms, V.; O’Cleirigh, C.; Chibanda, D.; Abas, M. A Task-Shifting Problem-Solving Therapy Intervention for Depression and Barriers to Antiretroviral Therapy Adherence for People Living With HIV in Zimbabwe: Case Series. Cogn. Behav. Pract. 2020, 27, 84–92. [Google Scholar] [CrossRef]
- Udedi, M.; Stockton, M.A.; Kulisewa, K.; Hosseinipour, M.C.; Gaynes, B.N.; Mphonda, S.M.; Pence, B.W. The effectiveness of depression management for improving HIV care outcomes in Malawi: Protocol for a quasi-experimental study. BMC Public Health 2019, 19, 827. [Google Scholar] [CrossRef]
- Udedi, M.; Stockton, M.A.; Kulisewa, K.; Hosseinipour, M.C.; Gaynes, B.N.; Mphonda, S.M.; Mwagomba, B.M.; Mazenga, A.C.; Pence, B.W. Integrating depression management into HIV primary care in central Malawi: The implementation of a pilot capacity building program. BMC Health Serv. Res. 2018, 18, 593. [Google Scholar] [CrossRef]
- Dlamini-Simelane, T.; Moyer, E. Task shifting or shifting care practices? The impact of task shifting on patients’ experiences and health care arrangements in Swaziland. BMC Health Serv. Res. 2017, 17, 20. [Google Scholar] [CrossRef]
- Jobson, G.; Naidoo, N.; Matlakala, N.; Marincowitz, G.; Railton, J.; McIntyre, J.A.; Struthers, H.E.; Peters, R.P.H. Contextual factors affecting the integration of community health workers into the health system in Limpopo Province, South Africa. Int. Health 2019, 12, 281–286. [Google Scholar] [CrossRef]
- Kredo, T.; Adeniyi, F.B.; Bateganya, M.; Pienaar, E.D. Task shifting from doctors to non-doctors for initiation and maintenance of antiretroviral therapy. Cochrane Database Syst. Rev. 2014, 2014, CD007331. [Google Scholar] [CrossRef] [PubMed]
- Seidman, G.; Atun, R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum. Resour. Health 2017, 15, 29. [Google Scholar] [CrossRef]
- Kane, J.; Landes, M.; Carroll, C.; Nolen, A.; Sodhi, S. A systematic review of primary care models for non-communicable disease interventions in Sub-Saharan Africa. BMC Fam. Pract. 2017, 18, 46. [Google Scholar] [CrossRef] [PubMed]
- Lovero, K.L.; Lammie, S.L.; Van Zyl, A.; Paul, S.N.; Ngwepe, P.; Mootz, J.J.; Carlson, C.; Sweetland, A.C.; Shelton, R.C.; Wainberg, M.L.; et al. Mixed-methods evaluation of mental healthcare integration into tuberculosis and maternal-child healthcare services of four South African districts. BMC Health Serv. Res. 2019, 19, 83. [Google Scholar] [CrossRef]
- Limbani, F.; Thorogood, M.; Gómez-Olivé, F.X.; Kabudula, C.; Goudge, J. Task shifting to improve the provision of integrated chronic care: Realist evaluation of a lay health worker intervention in rural South Africa. BMJ Glob. Health 2019, 4, e001084. [Google Scholar] [CrossRef] [PubMed]
- Goudge, J.; Chirwa, T.; Eldridge, S.; Gómez-Olivé, F.X.F.; Kabudula, C.; Limbani, F.; Musenge, E.; Thorogood, M. Can lay health workers support the management of hypertension? Findings of a cluster randomised trial in South Africa. BMJ Glob. Health 2018, 3, e000577. [Google Scholar] [CrossRef] [PubMed]
- Ansbro, É.M.; Biringanine, M.; Caleo, G.; Prieto-Merino, D.; Sadique, Z.; Perel, P.; Jobanputra, K.; Roberts, B. Management of diabetes and associated costs in a complex humanitarian setting in the Democratic Republic of Congo: A retrospective cohort study. BMJ Open 2019, 9, e030176. [Google Scholar] [CrossRef] [PubMed]
- Osetinsky, B.; Mwangi, A.; Pastakia, S.; Wilson-Barthes, M.; Kimetto, J.; Rono, K.; Laktabai, J.; Galárraga, O. Layering and scaling up chronic non-communicable disease care on existing HIV care systems and acute care settings in Kenya: A cost and budget impact analysis. J. Int. AIDS Soc. 2020, 23, e25496. [Google Scholar] [CrossRef]
- Sam-Agudu, N.A.; Odiachi, A.; Bathnna, M.J.; Ekwueme, C.N.; Nwanne, G.; Iwu, E.N.; Cornelius, L.J. “They do not see us as one of them”: A qualitative exploration of mentor mothers’ working relationships with healthcare workers in rural North-Central Nigeria. Hum. Resour. Health 2018, 16, 47. [Google Scholar] [CrossRef]
- Rabkin, M.; de Pinho, H.; Michaels-Strasser, S.; Naitore, D.; Rawat, A.; Topp, S.M. Strengthening the health workforce to support integration of HIV and noncommunicable disease services in sub-Saharan Africa. AIDS 2018, 32, S47–S54. [Google Scholar] [CrossRef]
- Lawn, J.; Rohde, J.; Rifkin, S.; Were, M.; Paul, V.K.; Chopra, M. Alma-Ata 30 years on: Revolutionary, relevant, and time to revitalise. Lancet 2008, 372, 917–927. [Google Scholar] [CrossRef]
- Braveman, P.; Gruskin, S. Poverty, equity, human rights and health. Bull. World Health Organ. 2003, 81, 539–545. [Google Scholar]
- Narasimhan, M.; Askew, I.; Vermund, S.H. Advancing sexual and reproductive health and rights of young women at risk of HIV. Lancet Glob. Health 2016, 4, e684–e685. [Google Scholar] [CrossRef]
- South Africa National Department of Health (NDoH). Ideal Clinic Manual; Version 18; National Department of Health: Pretoria, South Africa, 2018. [Google Scholar]
- Matanje Mwagomba, B.L.; Ameh, S.; Bongomin, P.; Juma, P.A.; MacKenzie, R.K.; Kyobutungi, C.; Lukhele, N.; Mwangi, K.J.; Amberbir, A.; Klipstein-Grobusch, K.; et al. Opportunities and challenges for evidence-informed HIV-noncommunicable disease integrated care policies and programs: Lessons from Malawi, South Africa, Swaziland and Kenya. AIDS 2018, 32 (Suppl. 1), S21–S32. [Google Scholar] [CrossRef] [PubMed]
- Tollman, S. Community oriented primary care: Origins, evolution, applications. Soc. Sci. Med. 1991, 32, 633–642. [Google Scholar] [CrossRef]
- Connor, E.; Mullan, F. Community Oriented Primary Care: New Directions for Health Services Delivery; Conference Proceedings; National Academies: Washington, DC, USA, 1983. [Google Scholar]
- Hunter, J.R.; Chandran, T.M.; Asmall, S.; Tucker, J.-M.; Ravhengani, N.M.; Mokgalagadi, Y. The Ideal Clinic in South Africa: Progress and challenges in implementation. S. Afr. Health Rev. 2017, 2017, 111–123. [Google Scholar]
- Bresick, G.; von Pressentin, K.B.; Mash, R. Evaluating the performance of South African primary care: A cross-sectional descriptive survey. South Afr. Fam. Pract. 2019, 61, 109–116. [Google Scholar] [CrossRef]
- Massyn, N.; Barron, P.; Day, C.; Ndlovu, N.; Padarath, A. District Health Barometer 2018/19; Health Systems Trust: Durban, South Africa, 2020. [Google Scholar]
- Muthathi, I.S.; Rispel, L.C. Policy context, coherence and disjuncture in the implementation of the Ideal Clinic Realisation and Maintenance programme in the Gauteng and Mpumalanga provinces of South Africa. Health Res. Policy Syst. 2020, 18, 55. [Google Scholar] [CrossRef]
- Muthathi, I.S.; Levin, J.; Rispel, L.C. Decision space and participation of primary healthcare facility managers in the Ideal Clinic Realisation and Maintenance programme in two South African provinces. Health Policy Plan. 2020, 35, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Rawat, A.; Uebel, K.; Moore, D.; Cingl, L.; Yassi, A. Patient Responses on Quality of Care and Satisfaction with Staff After Integrated HIV Care in South African Primary Health Care Clinics. J. Assoc. Nurses AIDS Care 2018, 29, 698–711. [Google Scholar] [CrossRef] [PubMed]
- Ameh, S.; Klipstein-Grobusch, K.; D’Ambruoso, L.; Kahn, K.; Tollman, S.M.; Gómez-Olivé, F.X. Quality of integrated chronic disease care in rural South Africa: User and provider perspectives. Health Policy Plan. 2016, 32, 257–266. [Google Scholar] [CrossRef]
- Ameh, S.; D’Ambruoso, L.; Gómez-Olivé, F.X.; Kahn, K.; Tollman, S.; Klipstein-Grobusch, K. Paradox of HIV stigma in an integrated chronic disease care in rural South Africa: Viewpoints of service users and providers. PLoS ONE 2020, 15, e0236270. [Google Scholar] [CrossRef]
- Lebina, L.; Oni, T.; Alaba, O.A.; Kawonga, M. A mixed methods approach to exploring the moderating factors of implementation fidelity of the integrated chronic disease management model in South Africa. BMC Health Serv. Res. 2020, 20, 617. [Google Scholar] [CrossRef]
- Ameh, S.; Klipstein-Grobusch, K.; Musenge, E.; Kahn, K.; Tollman, S.; Gómez-Olivé, F.X. Effectiveness of an Integrated Approach to HIV and Hypertension Care in Rural South Africa: Controlled Interrupted Time-Series Analysis. JAIDS J. Acquir. Immune Defic. Syndr. 2017, 75, 472–479. [Google Scholar] [CrossRef]
- Uebel, K.E.; Lombard, C.; Joubert, G.; Fairall, L.R.; Bachmann, M.O.; Mollentze, W.F.; van Rensburg, D.; Wouters, E. Integration of HIV care into primary care in South Africa: Effect on survival of patients needing antiretroviral treatment. J. Acquir. Immune Defic. Syndr. 2013, 63, e94–e100. [Google Scholar] [CrossRef]
- Rawat, A.; Uebel, K.; Moore, D.; Yassi, A. Integrated HIV-Care into Primary Health Care Clinics and the Influence on Diabetes and Hypertension Care: An Interrupted Time Series Analysis in Free State, South Africa Over 4 Years. JAIDS J. Acquir. Immune Defic. Syndr. 2018, 77, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Haldane, V.; Legido-Quigley, H.; Chuah, F.L.H.; Sigfrid, L.; Murphy, G.A.V.; Ong, S.E.; Cervero-Liceras, F.; Watt, N.; Balabanova, D.; Hogarth, S.; et al. Integrating cardiovascular diseases, hypertension, and diabetes with HIV services: A systematic review. AIDS Care 2018, 30, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Lince-Deroche, N.; Leuner, R.; Kgowedi, S.; Moolla, A.; Madlala, S.; Manganye, P.; Xhosa, B.; Govathson, C.; Ndwanya, T.W.; Long, L. Voices from the front lines: A qualitative study of integration of HIV, tuberculosis, and primary healthcare services in Johannesburg, South Africa. PLoS ONE 2020, 15, e0230849. [Google Scholar] [CrossRef]
- Heller, D.J.; Balzer, L.B.; Kazi, D.; Charlebois, E.D.; Kwarisiima, D.; Mwangwa, F.; Jain, V.; Kotwani, P.; Chamie, G.; Cohen, C.R.; et al. Hypertension testing and treatment in Uganda and Kenya through the SEARCH study: An implementation fidelity and outcome evaluation. PLoS ONE 2020, 15, e0222801. [Google Scholar] [CrossRef]
- Kotwani, P.; Balzer, L.; Kwarisiima, D.; Clark, T.D.; Kabami, J.; Byonanebye, D.; Bainomujuni, B.; Black, D.; Chamie, G.; Jain, V.; et al. Evaluating linkage to care for hypertension after community-based screening in rural Uganda. Trop. Med. Int. Health 2014, 19, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Hyle, E.P.; Naidoo, K.; Su, A.E.; El-Sadr, W.M.; Freedberg, K.A. HIV, tuberculosis, and noncommunicable diseases: What is known about the costs, effects, and cost-effectiveness of integrated care? J. Acquir. Immune Defic. Syndr. 2014, 67 (Suppl. 1), S87–S95. [Google Scholar] [CrossRef]
- Ojo, T.; Lester, L.; Iwelunmor, J.; Gyamfi, J.; Obiezu-Umeh, C.; Onakomaiya, D.; Aifah, A.; Nagendra, S.; Opeyemi, J.; Oluwasanmi, M.; et al. Feasibility of integrated, multilevel care for cardiovascular diseases (CVD) and HIV in low- and middle-income countries (LMICs): A scoping review. PLoS ONE 2019, 14, e0212296. [Google Scholar] [CrossRef] [PubMed]
- Onywera, H.; Mwapagha, L.; Hsiao, N.-Y. The need for a balanced hospital-based care (HBC) and home- and community-based care (HCBC) approach for mitigating COVID-19 pandemic in sub-Saharan Africa. Pan Afr. Med. J. 2021, 38. [Google Scholar] [CrossRef]
- Anstey Watkins, J.; Griffiths, F.; Goudge, J. Community health workers’ efforts to build health system trust in marginalised communities: A qualitative study from South Africa. BMJ Open 2021, 11, e044065. [Google Scholar] [CrossRef]
- Bendavid, E.; Miller, G. The US Global Health Initiative: Informing policy with evidence. JAMA 2010, 304, 791–792. [Google Scholar] [CrossRef]
- Gostin, L.O.; Mok, E.A. The President’s Global Health Initiative. JAMA 2010, 304, 789–790. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, K.L.; Hlongwane, K.; Otwombe, K.; Dietrich, J.; Cheyip, M.; Khanyile, N.; Doherty, T.; Gray, G.E. Demographics and health profile on precursors of non-communicable diseases in adults testing for HIV in Soweto, South Africa: A cross-sectional study. BMJ Open 2019, 9, e030701. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, K.L.; Hlongwane, K.E.; Otwombe, K.; Dietrich, J.; Jaffer, M.; Cheyip, M.; Olivier, J.; Van Rooyen, H.; Wade, A.N.; Doherty, T.; et al. Does peer-navigated linkage to care work? A cross-sectional study of active linkage to care within an integrated non-communicable disease-HIV testing centre for adults in Soweto, South Africa. PLoS ONE 2020, 15, e0241014. [Google Scholar] [CrossRef] [PubMed]
- Mazhin, S.A.; Khankeh, H.; Farrokhi, M.; Aminizadeh, M.; Poursadeqiyan, M. Migration health crisis associated with climate change: A systematic review. J. Educ. Health Promot. 2020, 9, 97. [Google Scholar] [CrossRef]
- Lieber, M.; Chin-Hong, P.; Kelly, K.; Dandu, M.; Weiser, S.D. A systematic review and meta-analysis assessing the impact of droughts, flooding, and climate variability on malnutrition. Glob. Public Health 2020, 2020, 1–15. [Google Scholar] [CrossRef]
- Anenberg, S.C.; Haines, S.; Wang, E.; Nassikas, N.; Kinney, P.L. Synergistic health effects of air pollution, temperature, and pollen exposure: A systematic review of epidemiological evidence. Environ. Health 2020, 19, 130. [Google Scholar] [CrossRef]
- Chersich, M.F.; Pham, M.D.; Areal, A.; Haghighi, M.M.; Manyuchi, A.; Swift, C.P.; Wernecke, B.; Robinson, M.; Hetem, R.; Boeckmann, M.; et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: Systematic review and meta-analysis. BMJ 2020, 371, m3811. [Google Scholar] [CrossRef]
- Shea, E.; Perera, F.; Mills, D. Towards a fuller assessment of the economic benefits of reducing air pollution from fossil fuel combustion: Per-case monetary estimates for children’s health outcomes. Environ. Res. 2020, 182, 109019. [Google Scholar] [CrossRef]
- Tidman, R.; Abela-Ridder, B.; de Castañeda, R.R. The impact of climate change on neglected tropical diseases: A systematic review. Trans. R. Soc. Trop. Med. Hyg. 2021, 115, 147–168. [Google Scholar] [CrossRef]
- Cruz, J.; White, P.C.L.; Bell, A.; Coventry, P.A. Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK. Int. J. Environ. Res. Public Health 2020, 17, 8581. [Google Scholar] [CrossRef]
- Mellet, J.; Pepper, M.S. A COVID-19 Vaccine: Big Strides Come with Big Challenges. Vaccines 2021, 9, 39. [Google Scholar] [CrossRef]
- Nhamo, G.; Chikodzi, D.; Kunene, H.P.; Mashula, N. COVID-19 vaccines and treatments nationalism: Challenges for low-income countries and the attainment of the SDGs. Glob. Public Health 2021, 16, 319–339. [Google Scholar] [CrossRef]
- Members LCoC-VaTTF. Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet 2021, 397, 562–564. [Google Scholar] [CrossRef]
- Mejia, R.; Hotez, P.; Bottazzi, M.E. Global COVID-19 Efforts as the Platform to Achieving the Sustainable Development Goals. Curr. Trop. Med. Rep. 2020, 7, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, J.; Liu, Y.; Clouse, K.; Vermund, S.H. Attrition of HIV-positive children from HIV services in low and middle-income countries. AIDS 2019, 33, 2375–2386. [Google Scholar] [CrossRef]
- Audet, C.M.; Groh, K.; Moon, T.; Vermund, S.H.; Sidat, M. Poor-quality health services and lack of programme support leads to low uptake of HIV testing in rural Mozambique. Afr. J. AIDS Res. 2012, 11, 327–335. [Google Scholar] [CrossRef][Green Version]
- Bravo, M.P.; Peratikos, M.M.B.; Muicha, M.A.S.; Mahagaja, E.; Alvim, M.F.S.; Green, A.F.; Wester, C.W.; Vermund, S.H. Monitoring Pharmacy and Test Kit Stocks in Rural Mozambique: U.S. President’s Emergency Plan for AIDS Relief Surveillance to Help Prevent Ministry of Health Shortages. AIDS Res. Hum. Retrovir. 2020, 36, 415–426. [Google Scholar] [CrossRef]
- Ciampa, P.J.; Tique, J.; Jumá, N.; Sidat, M.; Moon, T.D.; Rothman, R.L.; Vermund, S.H. Addressing poor retention of infants exposed to HIV: A quality improvement study in rural Mozambique. J. Acquir. Immune Defic. Syndr. 2012, 60, e46–e52. [Google Scholar] [CrossRef]
- Aliyu, M.H.; Blevins, M.; Audet, C.M.; Kalish, M.; Gebi, U.I.; Onwujekwe, O.; Lindegren, M.L.; Shepherd, B.E.; Wester, C.W.; Vermund, S.H. Integrated prevention of mother-to-child HIV transmission services, antiretroviral therapy initiation, and maternal and infant retention in care in rural north-central Nigeria: A cluster-randomised controlled trial. Lancet HIV 2016, 3, e202–e211. [Google Scholar] [CrossRef]
- Audet, C.M.; Blevins, M.; Chire, Y.M.; Aliyu, M.; Vaz, L.M.E.; Antonio, E.; Alvim, F.; Bechtel, R.; Wester, C.W.; Vermund, S. Engagement of Men in Antenatal Care Services: Increased HIV Testing and Treatment Uptake in a Community Participatory Action Program in Mozambique. AIDS Behav. 2016, 20, 2090–2100. [Google Scholar] [CrossRef]
- Tankwanchi, A.B.; Ozden, C.; Vermund, S.H. Physician emigration from sub-Saharan Africa to the United States: Analysis of the 2011 AMA physician masterfile. PLoS Med. 2013, 10, e1001513. [Google Scholar] [CrossRef]
- Tankwanchi, A.S.; Hagopian, A.; Vermund, S.H. African Physician Migration to High-Income Nations: Diverse Motives to Emigrate (“We Are not Florence Nightingale”) or Stay in Africa (“There Is No Place Like Home”) Comment on “Doctor Retention: A Cross-sectional Study of How Ireland Has Been Losing the Battle”. Int. J. Health Policy Manag. 2020, 10, 660–663. [Google Scholar] [CrossRef]
- Tankwanchi, A.B.; Vermund, S.H.; Perkins, D.D. Has the WHO Global Code of Practice on the International Recruitment of Health Personnel been effective? Lancet Glob. Health 2014, 2, e390–e391. [Google Scholar] [CrossRef][Green Version]
| Elements of HIV Capacity-Building | Common Communicable Disease Needs | Common Non-Communicable Disease (NCD) Needs | Emerging and Pandemic Pathogen Needs |
|---|---|---|---|
| Health system strengthening |
|
|
|
| Clinical capacity for management of complex patients |
|
|
|
| Laboratories and point-of-care testing, diagnosis, monitoring |
|
|
|
| Community engagement and referral, local delivery of interventions |
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brault, M.A.; Vermund, S.H.; Aliyu, M.H.; Omer, S.B.; Clark, D.; Spiegelman, D. Leveraging HIV Care Infrastructures for Integrated Chronic Disease and Pandemic Management in Sub-Saharan Africa. Int. J. Environ. Res. Public Health 2021, 18, 10751. https://doi.org/10.3390/ijerph182010751
Brault MA, Vermund SH, Aliyu MH, Omer SB, Clark D, Spiegelman D. Leveraging HIV Care Infrastructures for Integrated Chronic Disease and Pandemic Management in Sub-Saharan Africa. International Journal of Environmental Research and Public Health. 2021; 18(20):10751. https://doi.org/10.3390/ijerph182010751
Chicago/Turabian StyleBrault, Marie A., Sten H. Vermund, Muktar H. Aliyu, Saad B. Omer, Dave Clark, and Donna Spiegelman. 2021. "Leveraging HIV Care Infrastructures for Integrated Chronic Disease and Pandemic Management in Sub-Saharan Africa" International Journal of Environmental Research and Public Health 18, no. 20: 10751. https://doi.org/10.3390/ijerph182010751
APA StyleBrault, M. A., Vermund, S. H., Aliyu, M. H., Omer, S. B., Clark, D., & Spiegelman, D. (2021). Leveraging HIV Care Infrastructures for Integrated Chronic Disease and Pandemic Management in Sub-Saharan Africa. International Journal of Environmental Research and Public Health, 18(20), 10751. https://doi.org/10.3390/ijerph182010751







