Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
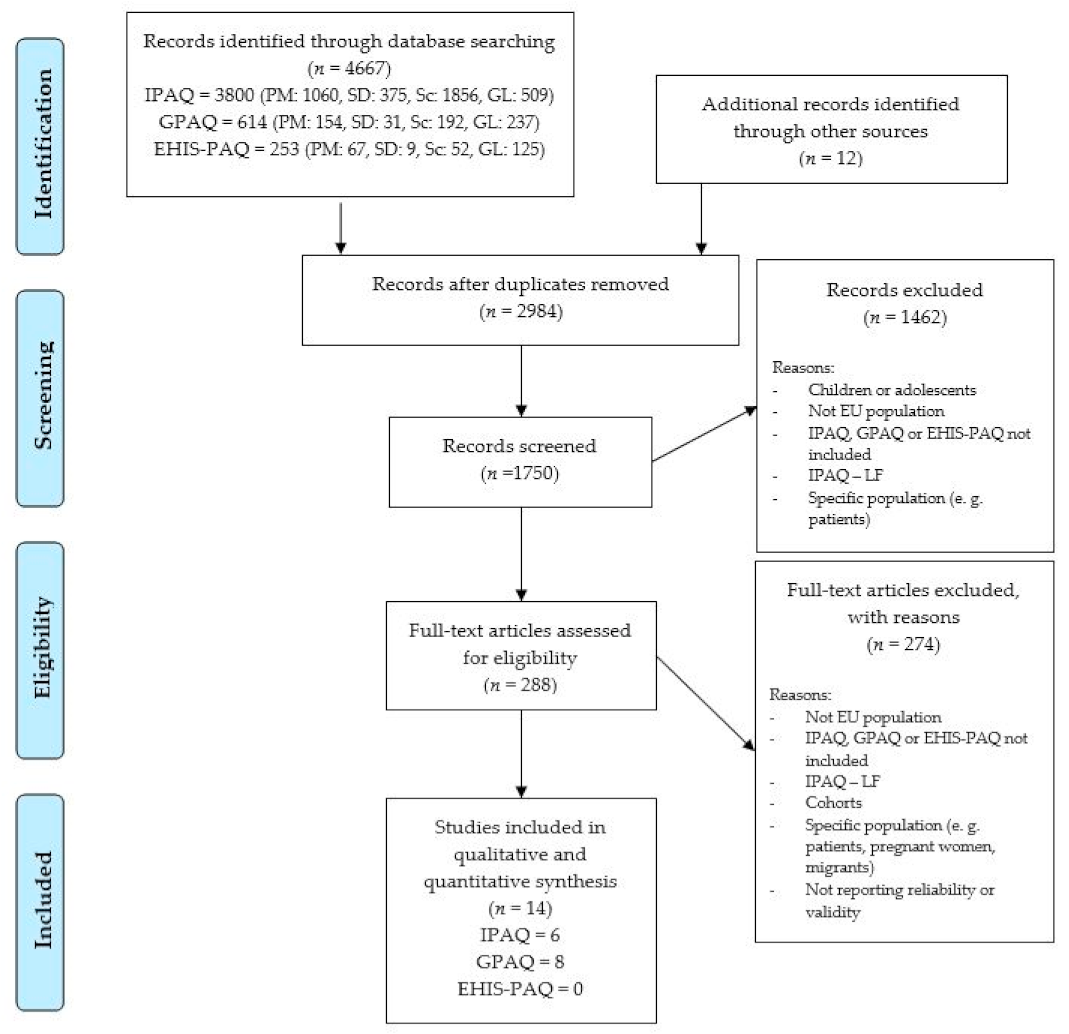
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Quality and Risk of Bias Assessment
2.4. Data Extraction and Statistical Analysis
2.5. Grading the Level of Evidence
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Panahi, S.; Tremblay, A. Sedentariness and health: Is sedentary behavior more than just physical inactivity? Front. Public Health 2018, 6, 258. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population-health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Bames, J.; Behrens, T.K.; Benden, M.E.; Biddle, S.; Bond, D.; Brassard, P.; Brown, H.; Carr, L.; Carson, V.; Chaput, J. Letter to the Editor: Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl. Physiol. Nutr. Metab. Appl. Nutr. Metab. 2012, 37, 540–542. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001512-8. [Google Scholar]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–17. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily sitting time and all-cause mortality: A meta-analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Alkandari, J.R.; Andersen, L.B.; Bauman, A.E.; Brownson, R.C.; et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Zhai, L.; Zhang, Y.; Zhang, D. Sedentary behaviour and the risk of depression: A meta-analysis. Br. J. Sports Med. 2015, 49, 705–709. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M.; Series, L.P.A.; Group, L.S.B.W. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Strath, S.J.; Kaminsky, L.A.; Ainsworth, B.E.; Ekelund, U.; Freedson, P.S.; Gary, R.A.; Richardson, C.R.; Smith, D.T.; Swartz, A.M. Guide to the assessment of physical activity: Clinical and research applications: A scientific statement from the American Heart Association. Circulation 2013, 128, 2259–2279. [Google Scholar] [CrossRef]
- Bowles, H.R. Measurement of active and sedentary behaviors: Closing the gaps in self-report methods. J. Phys. Act. Health 2012, 9, S1–S4. [Google Scholar] [CrossRef]
- Dall, P.M.; Coulter, E.H.; Fitzsimons, C.F.; Skelton, D.A.; Chastin, S.F.M. TAxonomy of Self-reported Sedentary behaviour Tools (TASST) framework for development, comparison and evaluation of self-report tools: Content analysis and systematic review. BMJ Open 2017, 7, e013844. [Google Scholar] [CrossRef]
- Healy, G.N.; Clark, B.K.; Winkler, E.A.H.; Gardiner, P.A.; Brown, W.J.; Matthews, C.E. Measurement of adults’ sedentary time in population-based studies. Am. J. Prev. Med. 2011, 41, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.; Ainsworth, B.E.; Sallis, J.F.; Hagströmer, M.; Craig, C.L.; Bull, F.C.; Pratt, M.; Venugopal, K.; Chau, J.; Sjöström, M. The descriptive epidemiology of sitting: A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Saelens, B.E. Assessment of physical activity by self-report: Status, limitations, and future directions. Res. Q. Exerc. Sport 2000, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Skender, S.; Ose, J.; Chang-Claude, J.; Paskow, M.; Brühmann, B.; Siegel, E.M.; Steindorf, K.; Ulrich, C.M. Accelerometry and physical activity questionnaires-a systematic review. BMC Public Health 2016, 16, 515. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Butler, G.; Garriguet, D.; Prince, S.A.; Roberts, K.C. Comparison of self-reported and accelerometer-measured physical activity in Canadian adults. Health Rep 2018, 29, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Bakker, E.A.; Hartman, Y.A.W.; Hopman, M.T.E.; Hopkins, N.D.; Graves, L.E.F.; Dunstan, D.W.; Healy, G.N.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Validity and reliability of subjective methods to assess sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–31. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Rosenberg, D.E.; Bull, F.C.; Marshall, A.L.; Sallis, J.F.; Bauman, A.E. Assessment of sedentary behavior with the International Physical Activity Questionnaire. J. Phys. Act. Health 2008, 5, S30–S44. [Google Scholar] [CrossRef]
- Trinh, O.T.H.; Do Nguyen, N.; Van Der Ploeg, H.P.; Dibley, M.J.; Bauman, A. Test-retest repeatability and relative validity of the Global Physical Activity Questionnaire in a developing country context. J. Phys. Act. Health 2009, 6, S46–S53. [Google Scholar] [CrossRef] [PubMed]
- Sember, V.; Meh, K.; Sorić, M.; Starc, G.; Rocha, P.; Jurak, G. Validity and Reliability of International Physical Activity Questionnaires for Adults across EU Countries: Systematic Review and Meta Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7161. [Google Scholar] [CrossRef]
- IPAQ Research Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. 2005. Available online: http//www.ipaq.ki.se/scoring.pdf (accessed on 16 April 2020).
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef]
- Riley, L.; Guthold, R.; Cowan, M.; Savin, S.; Bhatti, L.; Armstrong, T.; Bonita, R. The World Health Organization STEPwise approach to noncommunicable disease risk-factor surveillance: Methods, challenges, and opportunities. Am. J. Public Health 2016, 106, 74–78. [Google Scholar] [CrossRef]
- World Health Organization. Review of Physical Activity Surveillance Data Sources in European Union Member States; WHO Regional Office for Europe: Copenhagen, Denmark, 2011. [Google Scholar]
- Finger, J.D.; Tafforeau, J.; Gisle, L.; Oja, L.; Ziese, T.; Thelen, J.; Mensink, G.B.M.; Lange, C. Development of the European health interview survey-physical activity questionnaire (EHIS-PAQ) to monitor physical activity in the European Union. Arch. Public Health 2015, 73, 59. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- van Poppel, M.N.M.; Chinapaw, M.J.M.; Mokkink, L.B.; van Mechelen, W.; Terwee, C.B.; van Poppel, M.N.M.; van Mechelen, W.; Terwee, C.B. Physical activity questionnaires for youth. Sport. Med. 2010, 40, 539–563. [Google Scholar] [CrossRef]
- Ekelund, U.; Sepp, H.; Brage, S.; Becker, W.; Jakes, R.; Hennings, M.; Wareham, N.J. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr. 2006, 9, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Kalvenas, A.; Burlacu, I.; Abu-Omar, K. Reliability and validity of the International Physical Activity Questionnaire in Lithuania. Balt. J. Health Phys. Act. 2016, 8, 29–41. [Google Scholar] [CrossRef]
- Scholes, S.; Bridges, S.; Fat, L.N.; Mindell, J.S. Comparison of the physical activity and sedentary behaviour assessment questionnaire and the short-form international physical activity questionnaire: An analysis of health survey for England data. PLoS ONE 2016, 11, e0151647. [Google Scholar] [CrossRef]
- Rivière, F.; Widad, F.Z.; Speyer, E.; Erpelding, M.-L.; Escalon, H.; Vuillemin, A. Reliability and validity of the French version of the global physical activity questionnaire. J. Sport Health Sci. 2018, 7, 339–345. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Mokkink, L.B.; van Poppel, M.N.M.; Chinapaw, M.J.M.; van Mechelen, W.; de Vet, H.C.W. Qualitative attributes and measurement properties of physical activity questionnaires. Sport Med. 2010, 40, 525–537. [Google Scholar] [CrossRef] [PubMed]
- Sneck, S.; Viholainen, H.; Syväoja, H.; Kankaapää, A.; Hakonen, H.; Poikkeus, A.-M.; Tammelin, T. Effects of school-based physical activity on mathematics performance in children: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 109. [Google Scholar] [CrossRef]
- Sember, V.; Jurak, G.; Kovač, M.; Morrison, S.A.; Starc, G. Children’s physical activity, academic performance and cognitive functioning: A systematic review and meta-analysis. Front. Public Health 2020, 8, 307. [Google Scholar] [CrossRef]
- Green, S.; Higgins, J.P.T.; Alderson, P.; Clarke, M.; Mulrow, C.D.; Oxman, A.D. Chapter 1: Introduction. Cochrane Handb. Syst. Rev. Interv. Version 2011, 5, 11–102. [Google Scholar]
- Hunter, J.E.; Schmidt, F.L.; Le, H. Implications of direct and indirect range restriction for meta-analysis methods and findings. J. Appl. Psychol. 2006, 91, 594. [Google Scholar] [CrossRef]
- Teugels, J.L.; Vet, H. Observer reliability and agreement. Wiley StatsRef Stat. Ref. Online 2014. [Google Scholar] [CrossRef]
- Helmerhorst, H.H.J.F.; Brage, S.; Warren, J.; Besson, H.; Ekelund, U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 103. [Google Scholar] [CrossRef]
- Rudolf, K.; Lammer, F.; Stassen, G.; Froböse, I.; Schaller, A. Show cards of the Global Physical Activity Questionnaire (GPAQ)–do they impact validity? A crossover study. BMC Public Health 2020, 20, 223. [Google Scholar] [CrossRef]
- Kastelic, K.; Šarabon, N. Comparison of Self-Reported Sedentary Time on Weekdays with an Objective Measure (activPAL). Meas. Phys. Educ. Exerc. Sci. 2019, 23, 227–236. [Google Scholar] [CrossRef]
- Laeremans, M.; Dons, E.; Avila-Palencia, I.; Carrasco-Turigas, G.; Orjuela, J.P.; Anaya, E.; Brand, C.; Cole-Hunter, T.; de Nazelle, A.; Götschi, T. Physical activity and sedentary behaviour in daily life: A comparative analysis of the Global Physical Activity Questionnaire (GPAQ) and the SenseWear armband. PLoS ONE 2017, 12, e0177765. [Google Scholar] [CrossRef]
- Rütten, A.; Vuillemin, A.; Ooijendijk, W.T.M.; Schena, F.; Sjöström, M.; Stahl, T.; Vanden Auweele, Y.; Welshman, J.; Ziemainz, H. Physical activity monitoring in europe. The European Physical Activity Surveillance System (EUPASS) approach and indicator testing. Public Health Nutr. 2003, 6, 377–384. [Google Scholar] [CrossRef]
- De La Cámara, M.A.; Higueras-Fresnillo, S.; Cabanas-Sánchez, V.; Sadarangani, K.P.; Martinez-Gomez, D.; Veiga, Ó.L. Criterion validity of the sedentary behavior question from the global physical activity questionnaire in older adults. J. Phys. Act. Health 2020, 17, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Cleland, C.L.; Hunter, R.F.; Kee, F.; Cupples, M.E.; Sallis, J.F.; Tully, M.A. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health 2014, 14, 1255. [Google Scholar] [CrossRef]
- Novak, B.; Holler, P.; Jaunig, J.; Ruf, W.; van Poppel, M.N.M.; Sattler, M.C. Do we have to reduce the recall period? Validity of a daily physical activity questionnaire (PAQ24) in young active adults. BMC Public Health 2020, 20, 72. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Lameck, W.U. Sampling design, validity and reliability in general social survey. Int. J. Acad. Res. Bus. Soc. Sci. 2013, 3, 212–218. [Google Scholar] [CrossRef]
- González, K.; Fuentes, J.; Márquez, J.L. Physical inactivity, sedentary behavior and chronic diseases. Korean J. Fam. Med. 2017, 38, 111–115. [Google Scholar] [CrossRef]
- Tremblay, M.S. Introducing 24-hour movement guidelines for the early years: A new paradigm gaining momentum. J. Phys. Act. Health 2020, 17, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Wilkens, L.R.; Park, S.-Y.; Goodman, M.T.; Monroe, K.R.; Kolonel, L.N. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: The Multiethnic Cohort Study. Int. J. Epidemiol. 2013, 42, 1040–1056. [Google Scholar] [CrossRef] [PubMed]
- The Council of the European Union. Council Recommendation of 26 November 2013 on promoting health-enhancing physical activity across sectors. Off. J. Eur. Union 2013, 56, 1–5. [Google Scholar]
- European Commission. Report from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions on the Implementation of the Council Recommendation on Promoting Health-Enhancing Physical Activity across Sect; Publications Office of the European Union: Brussels, Belgium, 2019. [Google Scholar]
- World Health Organization. Physical Activity Strategy for the WHO European Region 2016–2025; WHO Regional Office for Europe: Copenhagen, Denmark, 2016; ISBN 978-92-890-5147-7. [Google Scholar]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-415-9997-9. [Google Scholar]
- Jinyuan, L.I.U.; Wan, T.; Guanqin, C.; Yin, L.U.; Changyong, F. Correlation and agreement: Overview and clarification of competing concepts and measures. Shanghai Arch. Psychiatry 2016, 28, 115–120. [Google Scholar] [CrossRef]
| Level of Evidence | Reliability | Concurrent Validity | Criterion Validity |
|---|---|---|---|
| 1 | Adequate time between test–retest and use of ICC, Kappa or Concordance reliability score > 0.70. | Comparison method to other PA questionnaires and concurrent validity score > 0.8. | Comparison method to accelerometers or doubly, calorimetry or doubly labelled water, criterion validity score > 0.8. |
| 2 | Inadequate time between test–retest and use of ICC, Kappa or Concordance reliability score < 0.70; adequate time between test-retest and use of Pearson or Spearman correlation < 0.7. | Comparison method to other PA questionnaires; 0.8 > concurrent validity score > 0.5. | Comparison method to accelerometers or doubly, calorimetry or doubly labelled water; 0.8 > validity score > 0.5. |
| 3 | Inadequate time between test–retest and use of Pearson or Spearman correlation < 0.70. | Comparison method to other PA questionnaires; concurrent validity score < 0.50. | Comparison method to accelerometers or doubly, calorimetry or doubly labelled water; criterion validity score < 0.50. |
| Positive (+) score | Studies with more than 50 participants and reliability of coefficients > 0.70. | Studies with more than 50 participants. | Studies with more than 50 participants. |
| Negative (−) score | Studies with less than 50 participants and reliability coefficients < 0.70. | Studies with less than 50 participants. | Studies with less than 50 participants. |
| Author (PA Questionnaire) Language Version | Country | Population ** | ||||
|---|---|---|---|---|---|---|
| Size | Age; (Range) | Gender (Male, Female) | Sample Description | Mode and Means of Administration | ||
| Bull et al. [25] (GPAQ), Portuguese | PT | 67 | 18–75 | 17 + 50 | Prevalence of young participants (18–44, n = 56). Convenient regional sample. | Interview. Unknown mode. |
| Cámara et al. [48] (GPAQ), Spanish | ES | 163 | 70 (67–75) | 67 + 96 | Older adults from IMPACT65+ study. | Interview. Face to face. |
| Cleland et al. [49] (GPAQ), English | UK | 22 | 46 | 8 + 14 | Random national sample. | Self-administered. Unknown mode. |
| Craig et al. [20] (IPAQ-SF), German, English, Finnish, Dutch, Portuguese, Swedish | Cross-national: AT, UK, FI, NL, PT, SE | 2115: | 47 | 77 + 123 | Specific populations. Convenient samples, but collectively, the participants represented a wide range of age, education, income, and activity levels. | Self-administered. Unknown modes. |
| 200 SE1; 50 SE2; | 41 | 22 + 28 | ||||
| 149 UK1 | 35 | 68 + 81 | ||||
| 101 UK2 | 41 | 38 + 63 | ||||
| 88 FI | 56 | 43 + 45 | ||||
| 196 PT | 35 | 96 + 100 | ||||
| 74 NL | 33 | 34 + 40 | ||||
| Ekelund et al. [31] (IPAQ-SF), Swedish | SE | 185 | 42 (20–69) | 93 + 92 | Workers and students. Convenient regional sample. | Telephone interview. |
| Kalvenas et al. [32] (IPAQ-SF), Lithuanian | LT | 92 # | 18–69 | reliability 29 + 63 validity 23 + 58 | Employees of university and private company. Convenient sample from urban area. | Self-administered. Unknown mode. |
| Kastelic et al. [5] (GPAQ), Slovenian | SI | 42 | M 39 F 50 | 37 + 5 | Crane operators and office workers. Convenient sample. | Interview. Unknown mode. |
| Laeremans et al. [46] (GPAQ), German, Spanish, English | Cross-national: B. ES, UK | 122: 41 B; 41 ES; 40 UK | 35 | 55 + 67 | Random regional sample. | Self-administered. Online. |
| Novak et al. [50] (GPAQ), German | AT | 50 | 25 | 39 + 11 | Students. Convenient sample. | Self-administered. Unknown mode. |
| Rivière et al. [34] (GPAQ), French | FR | 87 ### | 30 | 25 + 67 | Medical personnel and students. Convenient sample. | Interview and self-administered. Unknown mode. |
| Rosenberg et al. [21] (IPAQ-SF), English, Dutch | UK, NL | UK 146 (118) * NL 64 (30) * | UK 35.3 NL 32.7 | UK 65 + 78 NL 28 + 38 (UK 56 + 61 NL 11 + 19) * | Convenient sample. University staff and students. | Self-administered. Unknown mode. |
| Rudolf et al. [44] (GPAQ), German | DE | 54 | 28 | 23 + 31 | University students. Convenient sample. | Self- administered. Online. |
| Rütten et al. [47] (IPAQ-SF), German, Finnish, French, Italian, Dutch, Spanish, English | Cross-national: B, FI, FR, DE, I, NL, ES, UK | 951: 100 B; 127 FI; 91 FR; 223 DE; 98 I; 86 NL; 128 ES; 98 UK | >18 | Unknown | Random sample. | Interview. Face to face. |
| Scholes et al. [33] (IPAQ-SF), English | UK | 1252 | >16 | 548 + 704 | Multistage stratified probability sampling. | Self-administered. Pen and paper. |
| Reference (PA Questionnaire) | Study Pop. | Construct (Comparison PA Questionnaire or Device) | Results * | Rating |
|---|---|---|---|---|
| Craig et al. [20] (IPAQ-SF) | SE 1 | sitting | 0.50 | 3+ |
| UK1 | sitting | 0.86 | 2+ | |
| UK2 | sitting | 0.73 | 3+ | |
| FI | sitting | 0.94 | 2+ | |
| PT | sitting | 0.69 | 3+ | |
| SE 2 | sitting | 0.79 | 2+ | |
| NL | sitting | 0.95 | 2+ | |
| Kalvenas et al. [32] (IPAQ-SF) | LT | sitting (min/weekday/week) | 0.60 | 3+ |
| Riviere et al. [34] (GPAQ) | FR | sitting | 0.78 ICC = 0.80 | 2+ 1+ |
| Rosenberg et al. [21] (IPAQ-SF) | UK | total sitting (male) | 0.81 | 2+ |
| weekday sitting (male) | 0.79 | 2+ | ||
| weekend sitting (male) | 0.77 | 2+ | ||
| total sitting (female) | 0.63 | 3+ | ||
| weekday sitting (female) | 0.62 | 3+ | ||
| weekend sitting (female) | 0.71 | 2+ | ||
| total sitting (all) | 0.73 | 2+ | ||
| weekday sitting (all) | 0.70 | 2+ | ||
| weekend sitting (all) | 0.75 | 2+ | ||
| NL | total sitting (male) | 0.93 | 2− | |
| weekday sitting (male) | 0.94 | 2− | ||
| weekend sitting (male) | 0.90 | 2− | ||
| total sitting (female) | 0.94 | 2− | ||
| weekday sitting (female) | 0.96 | 2− | ||
| weekend sitting (female) | 0.92 | 2− | ||
| total sitting (all) | 0.95 | 2− | ||
| weekday sitting (all) | 0.96 | 2− | ||
| weekend sitting (all) | 0.91 | 2− | ||
| Rütten et al. [47] (IPAQ-SF) | B | sitting weekdays—total minutes | 0.52 | 3+ |
| sitting weekend-total minutes | 0.34 | 3+ | ||
| sitting sum MET | 0.42 | 3+ | ||
| FI | sitting weekdays—total minutes | 0.70 | 2+ | |
| sitting weekend-total minutes | 0.64 | 3+ | ||
| sitting sum MET | 0.58 | 3+ | ||
| FR | sitting weekdays—total minutes | 0.42 | 3+ | |
| sitting weekend-total minutes | 0.37 | 3+ | ||
| sitting sum MET | 0.42 | 3+ | ||
| DE | sitting weekdays—total minutes | 0.64 | 2+ | |
| sitting weekend-total minutes | 0.41 | 3+ | ||
| sitting sum MET | 0.52 | 3+ | ||
| I | sitting weekdays—total minutes | 0.73 | 2+ | |
| sitting weekend-total minutes | 0.33 | 3+ | ||
| sitting sum MET | 0.57 | 3+ | ||
| NL | sitting weekdays—total minutes | 0.63 | 3+ | |
| sitting weekend-total minutes | 0.45 | 3+ | ||
| sitting sum MET | 0.50 | 3+ | ||
| ES | sitting weekdays—total minutes | 0.62 | 3+ | |
| sitting weekend-total minutes | 0.43 | 3+ | ||
| sitting sum MET | 0.50 | 3+ | ||
| UK | sitting weekdays—total minutes | 0.55 | 3+ | |
| sitting weekend-total minutes | 0.44 | 3+ | ||
| sitting sum MET | 0.54 | 3+ | ||
| All nations | sitting weekdays—total minutes | 0.62 | 3+ | |
| sitting weekend-total minutes | 0.46 | 3+ | ||
| sitting sum MET | 0.53 | 3+ |
| Reference (PA Questionnaire) | Study Pop. | Method | Construct (Comparison PA Questionnaire or Device) | Results * | Rating |
|---|---|---|---|---|---|
| Bull et al. [25] (GPAQ) | PT | CCV | sitting (IPAQ-SF) | 0.56 | 2+ |
| Camara et al. [48] (GPAQ) | ES | CRV | Total sitting (IDEEA) | 0.11 | 3+ |
| sitting and reclining (IDEEA) | 0.21 | 3+ | |||
| SB (IDEEA) | 0.29 | 3+ | |||
| Cleland et al. [49] (GPAQ) | UK | CRV | sitting (ActiGraph GT3X) | 0.19 | 3− |
| Craig et al. [20] (IPAQ-SF) | SE1 | CCV | sitting 1st session (IPAQ L7T) | 0.57 | 2+ |
| sitting 2nd session (IPAQ L7T) | 0.91 | 1+ | |||
| UK2 | CRV | sitting (CSA motion detector MTI) | 0.25 | 3+ | |
| CCV | sitting 1st session (IPAQ L7S) | 0.82 | 1+ | ||
| sitting 2nd session (IPAQ L7S) | 0.84 | 1+ | |||
| FI | CRV | sitting (CSA motion detector MTI) | 0.46 | 3+ | |
| CCV | sitting 1st session (IPAQ LUS) | 0.96 | 1+ | ||
| sitting 2nd session (IPAQ LUS) | 0.96 | 1+ | |||
| sitting 1st session (IPAQ L7S) | 0.94 | 1+ | |||
| PT | CCV | sitting 1st session (IPAQ LUS) | 0.60 | 2+ | |
| sitting 2nd session (IPAQ LUS) | 0.42 | 3+ | |||
| SE 2 | CRV | sitting (CSA motion detector MTI) | 0.12 | 3+ | |
| CCV | sitting 1st session (IPAQ LUS) | 0.79 | 1+ | ||
| sitting 2nd session (IPAQ LUS) | 0.84 | 1+ | |||
| sitting (IPAQ L7S) | 0.89 | 1+ | |||
| NL | CRV | sitting (CSA motion detector MTI) | 0.22 | 3+ | |
| CCV | sitting 1st session (IPAQ L7T) | 0.91 | 1+ | ||
| sitting 2nd session (IPAQ L7T) | 0.97 | 1+ | |||
| Ekelund et al. [31] (IPAQ-SF) | SE | CRV | sitting(ActiGraph) | Pearson r = 0.16 | 3+ |
| Kalvenas et al. [32] (IPAQ-SF) | LT | CRV | sitting (ActiGraph GT3X) | 0.28 | 3+ |
| Kastelic et al. [45] (GPAQ) | SI | CRV | sitting (ActivPAL) | 0.32 ICC = 0.21 | 3− 3− |
| Laeremans et al. [46] (GPAQ) | B, ES, UK | CRV | sitting 1st session (Bodymedia Fit SenseWear) | 0.09 | 3− |
| sitting 2nd session (Bodymedia Fit SenseWear) | 0.25 | 3− | |||
| sitting 3rd session (Bodymedia Fit SenseWear) | 0.24 | 3− | |||
| Overall sitting (Bodymedia Fit SenseWear) | 0.12 | 3− | |||
| Novak et al. [50] (GPAQ) | AT | CCV | sitting (PAQ 24) | 0.74 | 2+ |
| Riviere et al. [34] (GPAQ) | FR | CRV | sitting (ActiGraph GT3X) | 0.42 | 3+ |
| CCV | sitting 1st session (IPAQ-LF) | 0.85 | 1+ | ||
| sitting 2nd session (IPAQ-LF) | 0.89 | 1+ | |||
| Rosenberg et al. [21] (IPAQ-SF) | UK | CRV | sitting (male, CSA 7164) | 0.24 | 3+ |
| sitting (female, CSA 7164) | 0.29 | 3+ | |||
| sitting (all, CSA 7164) | 0.20 | 3+ | |||
| NL | CRV | sitting (male, CSA 7164) | −0.48 | 3− | |
| sitting (female, CSA 7164) | 0.43 | 3− | |||
| sitting (all, CSA 7164) | 0.22 | 3− | |||
| Rudolf et al. [44] (GPAQ) | DE | CRV | sitting (ActiGraph GT3X and GPAQ +) | 0.32 | 3+ |
| sitting (ActiGraph GT3X and GPAQ) | 0.29 | 3+ | |||
| Scholes et al. [33] (IPAQ-SF) | UK | CCV | sitting (PASBAQ) male | Pearson r = 0.23 | 3+ |
| sitting (PASBAQ) female | Pearson r = 0.29 | 3+ |
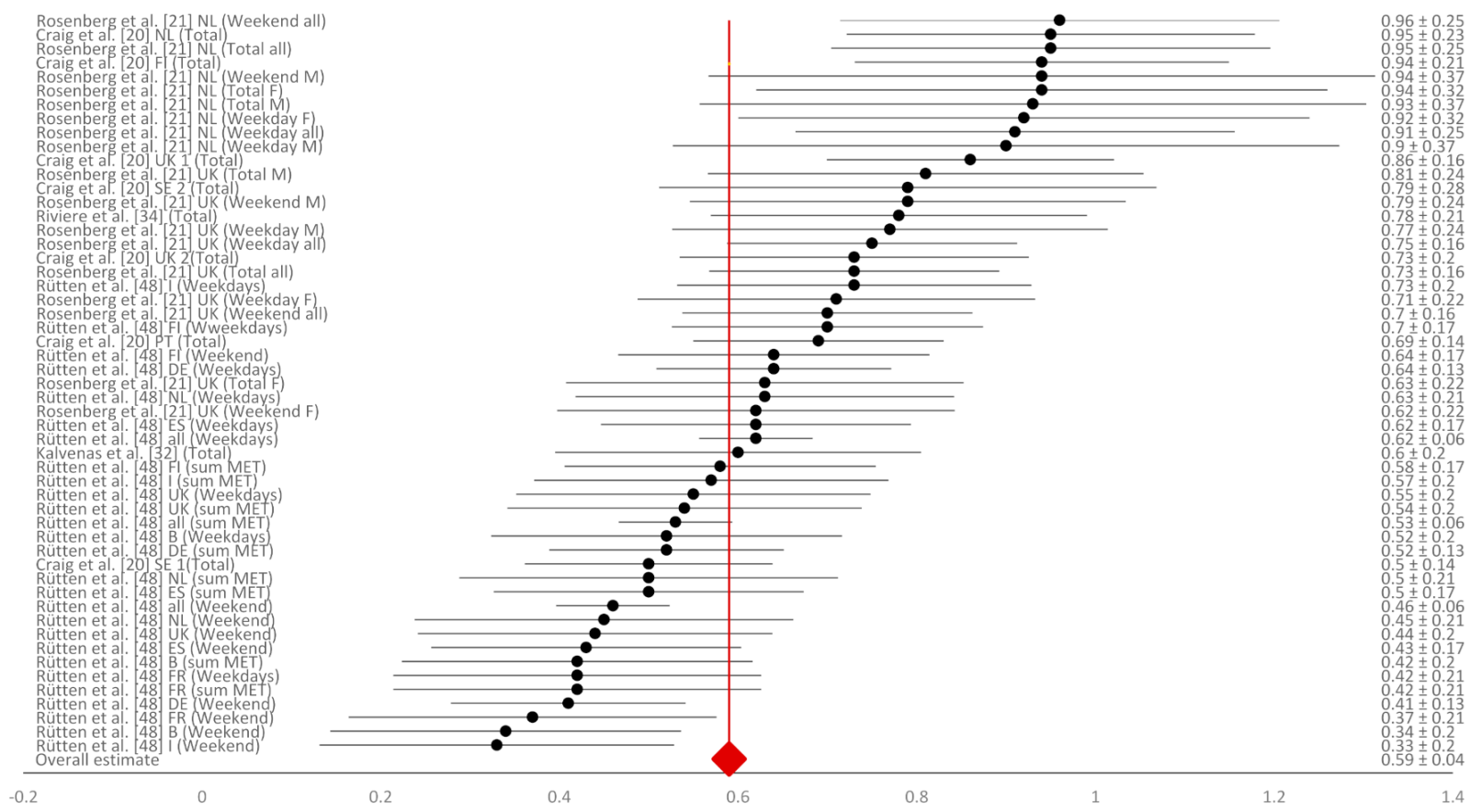
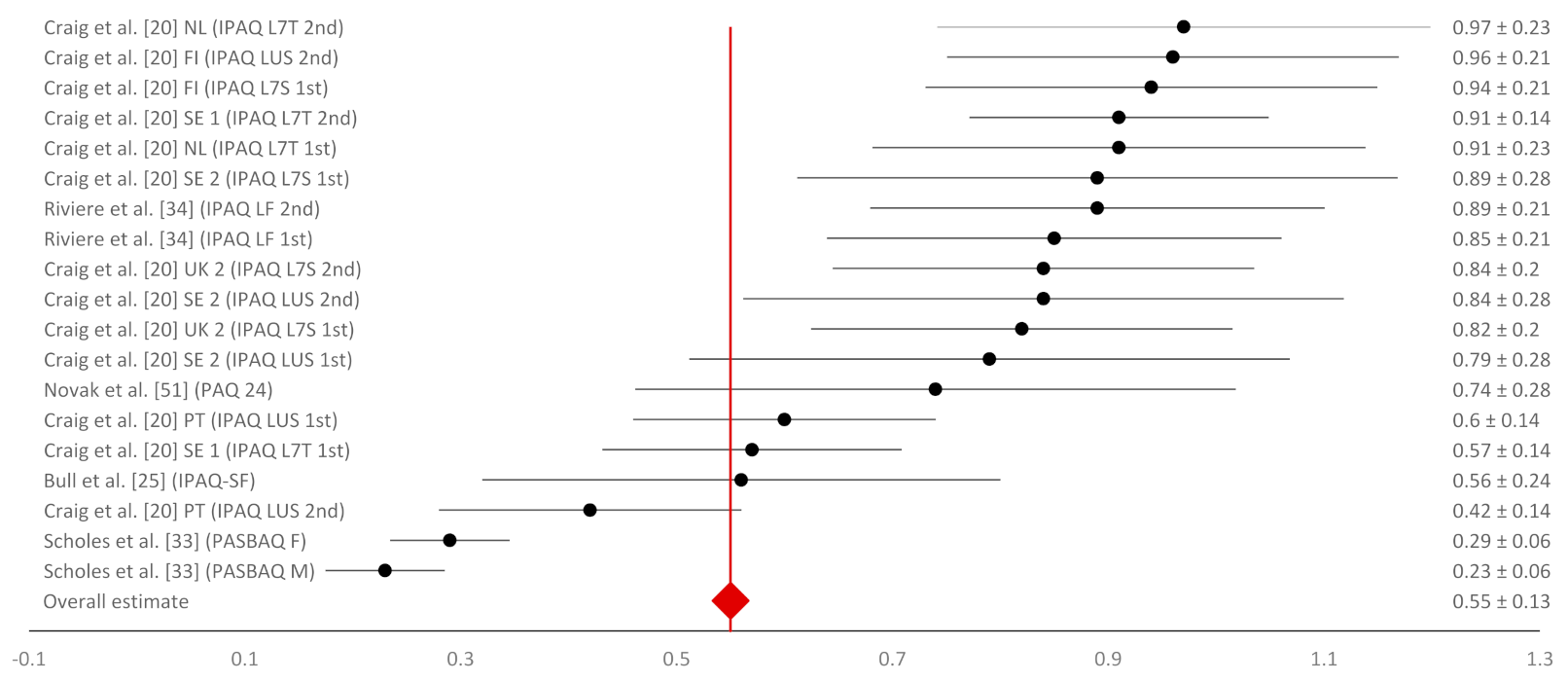
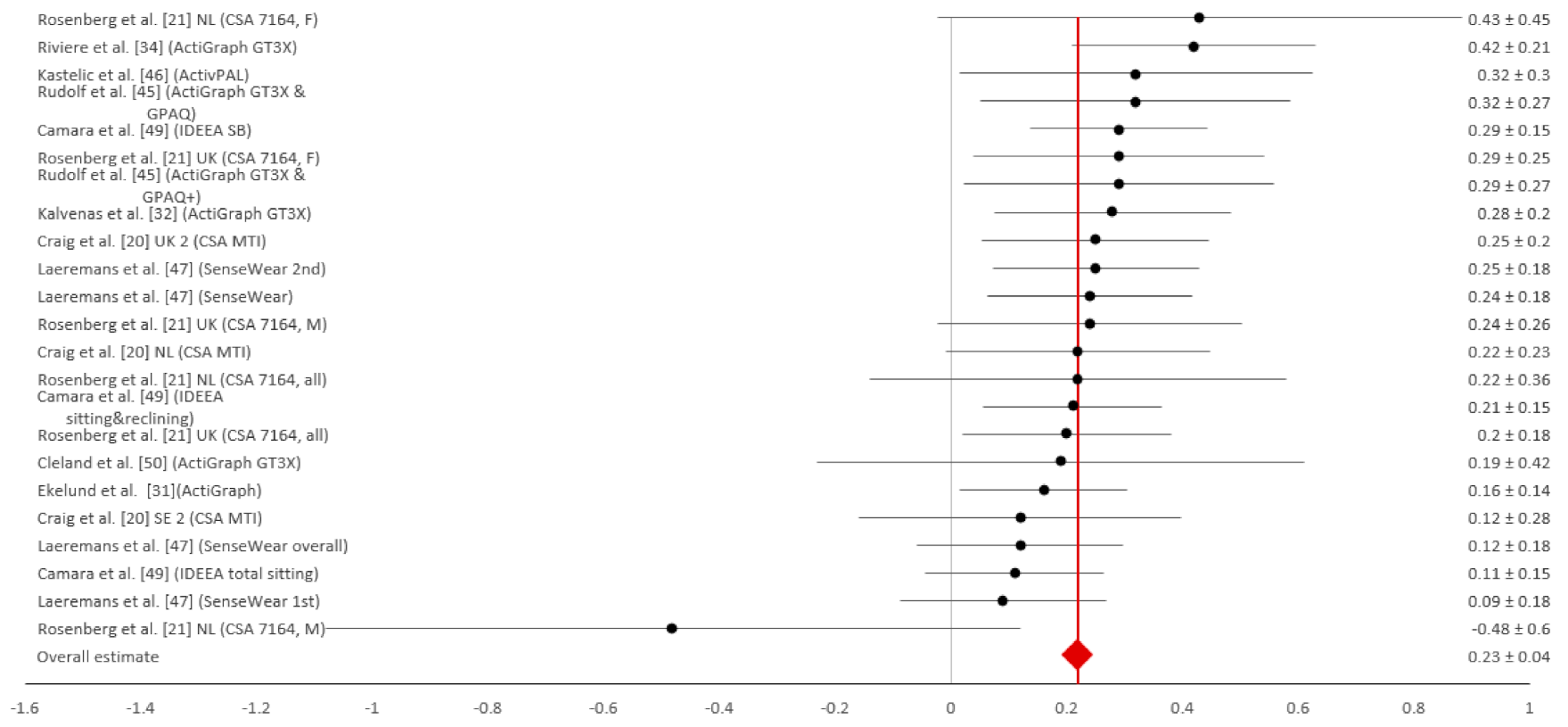
| Measurement Characteristic | Sample | Population Effect | Egger’s Bias Test | Heterogeneity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (k) | k | n | Unweighted Mean | Weighted Mean | 95% CI | 80% CRI | Bias | 95% CI | p | I2 (%) | Q | p | |
| Reliability | 5 [20,21,32,34,47] | 36 | 6719 | 0.66 | 0.59 | 0.55 to 0.63 | 0.42 to 0.66 | −0.98 | −3.22 to 1.24 | 0.38 | 86.29 | 386.63 | 0.00 |
| Concurrent validity | 5 [20,25,33,34,50] | 18 | 3074 | 0.72 | 0.55 | 0.42 to 0.68 | 0.20 to 0.90 | −3.90 | −11.26 to 3.46 | 0.31 | 96.47 | 481.49 | 0.00 |
| Criterion validity | 10 [20,21,31,32,34,44,45,46,48,49] | 24 | 2164 | 0.22 | 0.23 | 0.19 to 0.27 | 0.19 to 0.25 | 0.89 | −1.27 to 3.06 | 0.43 | 10.54 | 19.0 | 0.33 |
| Author (year) | Outcome | R | BC | BV | T | BM | VO | DA | RR | PC | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bull et al. (2009) [25] | GPAQ + | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 4/9 (0.44) |
| Cámara et al. 2020 [48] | GPAQ − | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 3/9 (0.33) |
| Cleland et al. (2014) [49] | GPAQ − | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7/9 (0.78) |
| Craig et al. (2003) [20] | IPAQ-SF *, + | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 2/9 (0.22) |
| Ekelund et al. (2005) [31] | IPAQ-SF − | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 3/9 (0.33) |
| Kalvenas et al. (2016) [32] | IPAQ-SF * | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 3/9 (0.33) |
| Kastelic et al. (2019) [45] | GPAQ − | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 3/9 (0.33) |
| Laeremans et a.l (2016) [46] | GPAQ − | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 3/9 (0.33) |
| Novak et al. (2020) [50] | GPAQ + | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 4/9 (0.44) |
| Rivière et al. (2016) [34] | GPAQ *, +, − | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 4/9 (0.44) |
| Rosenberger et al. (2008) [21] | IPAQ-SF * | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 3/9 (0.33) |
| Rudolf et al. (2020) [44] | GPAQ − | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 4/9 (0.44) |
| Rütten et al. (2003) [47] | IPAQ-SF * | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 6/9 (0.67) |
| Scholes et al. (2016) [33] | IPAQ-SF + | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 4/9 (0.44) |
| AVERAGE OF ALL STUDIES | 0.29 | 0.00 | 0.36 | 0.86 | 0.00 | 1.00 | 0.14 | 0.86 | 0.29 | 0.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meh, K.; Jurak, G.; Sorić, M.; Rocha, P.; Sember, V. Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4602. https://doi.org/10.3390/ijerph18094602
Meh K, Jurak G, Sorić M, Rocha P, Sember V. Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(9):4602. https://doi.org/10.3390/ijerph18094602
Chicago/Turabian StyleMeh, Kaja, Gregor Jurak, Maroje Sorić, Paulo Rocha, and Vedrana Sember. 2021. "Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 9: 4602. https://doi.org/10.3390/ijerph18094602
APA StyleMeh, K., Jurak, G., Sorić, M., Rocha, P., & Sember, V. (2021). Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(9), 4602. https://doi.org/10.3390/ijerph18094602







