Could Physical Therapy Interventions Be Adopted in the Management of Critically Ill Patients with COVID-19? A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Participants
2.1.2. Concept
2.1.3. Context
2.2. Information Sources
2.3. Literature Search
2.4. Charting Data
2.5. Data Items
2.6. Critical Appraisal of Individual Sources of Evidence
2.7. Synthesis of Results
3. Results
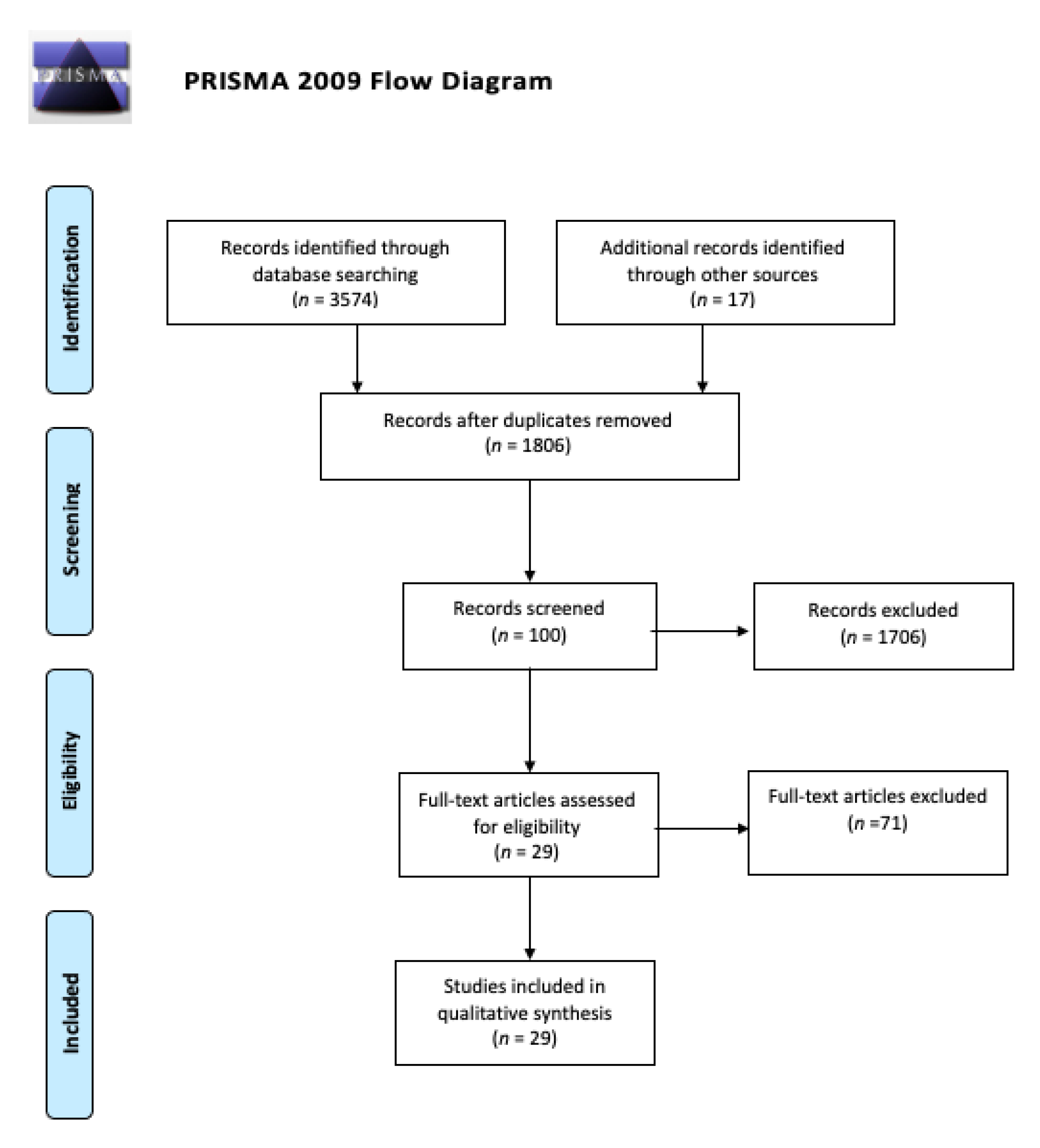
3.1. Study Selection
3.2. Relevant Data about Included Studies
3.3. ICU Environment in COVID-19
- Breathing frequency <24 respirations per minute (RPM)
- Resting heart rate <50% age-predicted maximal heart rate
- Body temperature <38 °C
- Blood pressure <20% variability recently
- PaO2/FIO2 >300, SpO2 >90%, and < 4% recent decrease in SpO2 (if not previous respiratory failure)
- A stable level of consciousness
- Electrocardiogram (ECG) normal (i.e., no evidence of myocardial infarction or arrhythmia)
3.4. Important Items before Applying Physical Therapy Interventions
3.5. Respiratory Physiotherapy
3.5.1. Non-Intubated and Extubated Patients
Active Cycle of Breathing Technique (ACBT)
Mechanical Insufflation–Exsufflation
Directed Cough or Manually Assisted Cough
Huff Coughing
Manual Hyperinflation (MHI)
Positive Expiratory Pressure Devices
Inspiratory Musculature Training (IMT)
3.5.2. Intubated Patients
Ventilator Hyperinflation (VHI)
Humidification
Aspiration
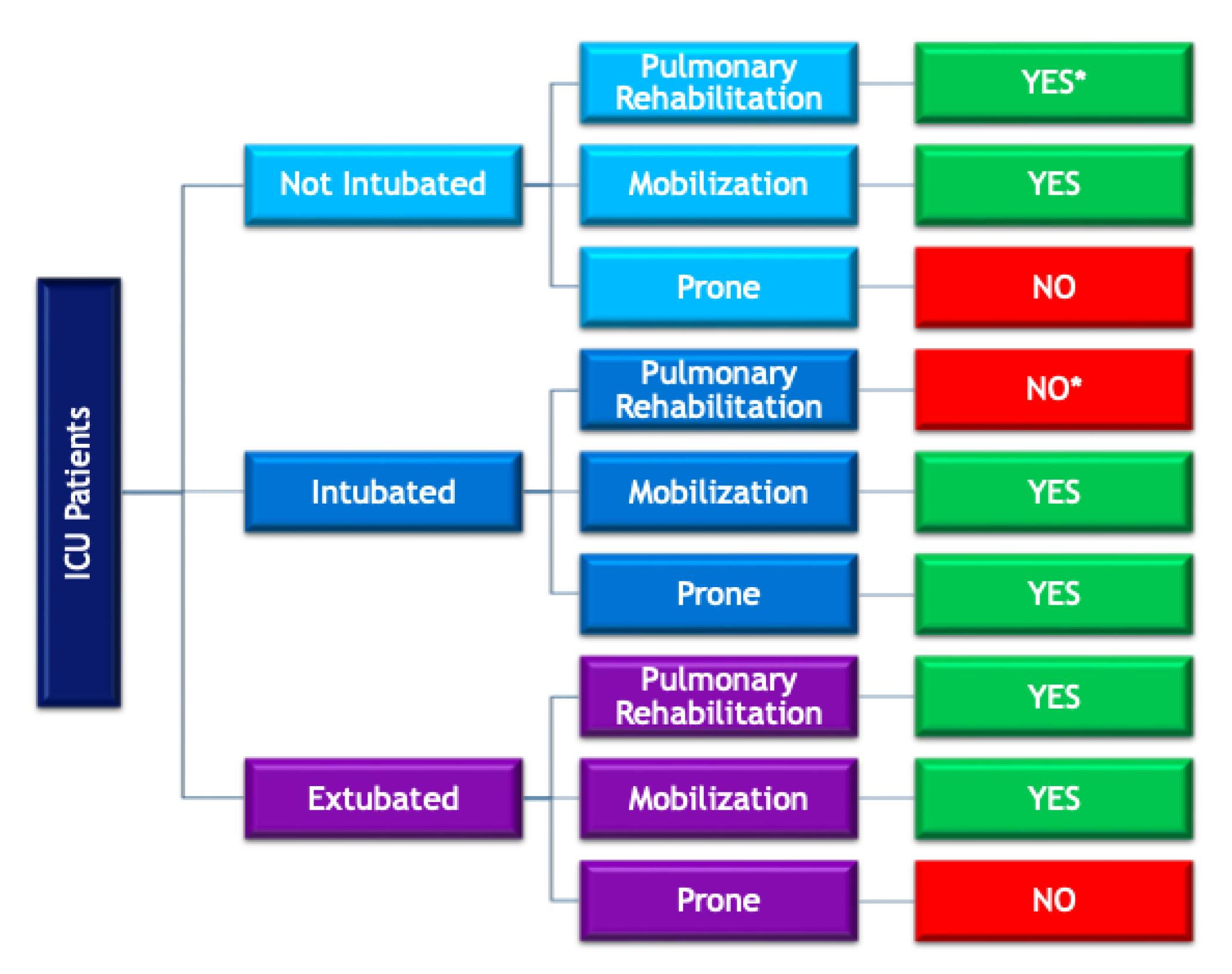
3.6. Positional Treatment
3.6.1. Non-Intubated and Extubated Patients
3.6.2. Intubated Patients
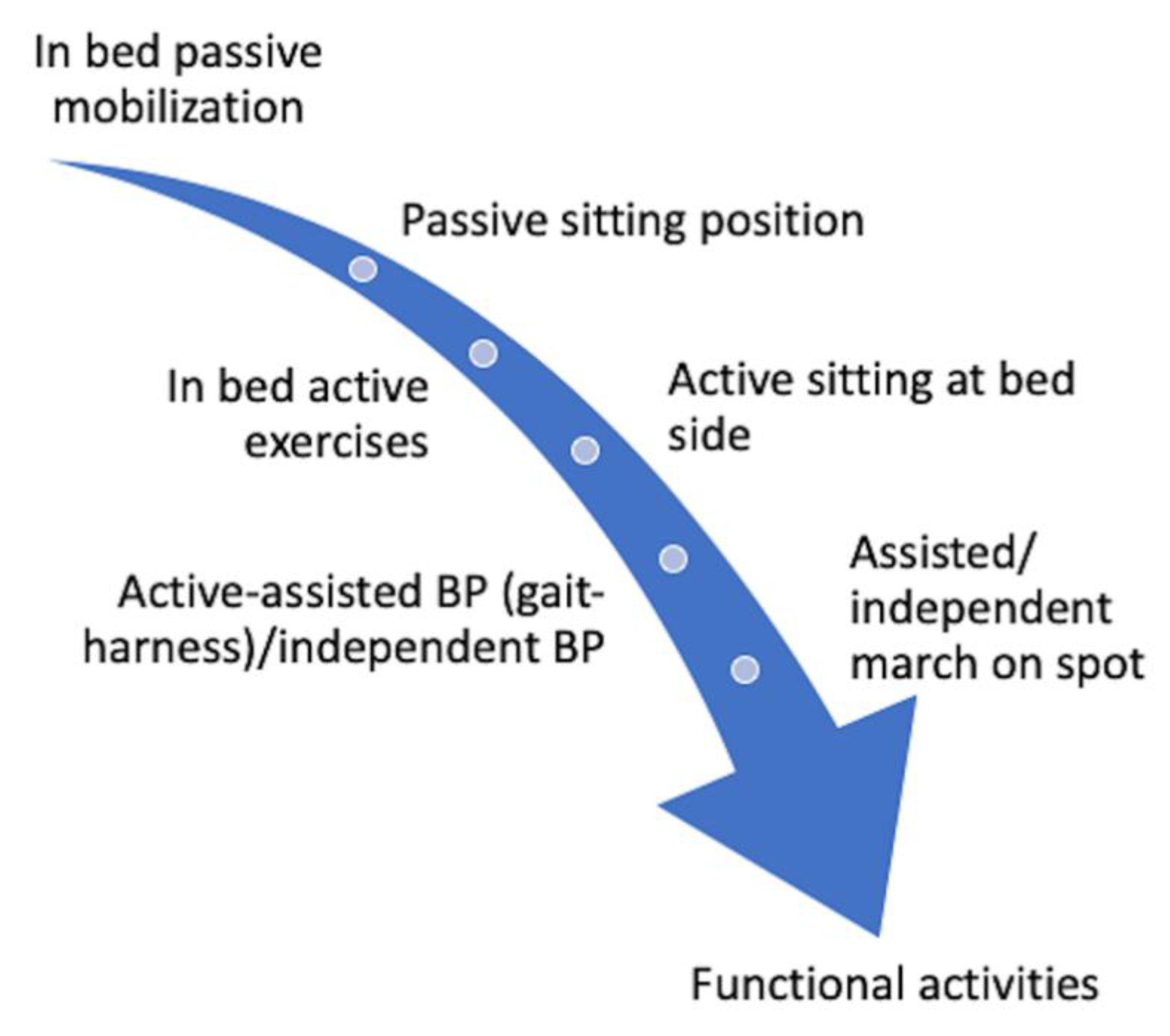
3.7. Mobilization and Exercise Therapy
3.7.1. Non-Intubated Patients
3.7.2. Intubated Patients
3.7.3. Extubated Patients
4. Discussion
4.1. Respiratory Physiotherapy
4.2. Positional Treatment
4.3. Mobilization and Exercise Therapy
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Munster, V.J.; Koopmans, M.; van Doremalen, N.; van Riel, D.; de Wit, E. A novel coronavirus emerging in China—Key questions for impact assessment. N. Engl. J. Med. 2020, 382, 692–694. [Google Scholar] [CrossRef]
- Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 2 February 2021).
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Guan, W.N.Z.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, S.C.D.; Du, B.; et al. Clinical characteristics of 2019 novel coronavirus infection in China. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.H.; Faraji, F.; Prajapati, D.P.; Boone, C.E.; DeConde, A.S. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int. Forum Allergy Rhinol. 2020. [Google Scholar] [CrossRef]
- Bartsch, S.M.; Ferguson, M.C.; McKinnell, J.A.; O’Shea, K.J.; Wedlock, P.T.; Siegmund, S.S.; Lee, B.Y. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff. 2020, 39, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 2020. [Google Scholar] [CrossRef]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, A.L.; Dean, C.N.; Fine, J.M.; Flanders, A.S.; et al. Diagnosis and treatment of adults with community-acquired pneumonia: An official clinical practice guideline of the American thoracic society and infectious diseases society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- Spain Goberment, Health Ministry. 2020. Available online: https://www.mscbs.gob.es/ (accessed on 19 August 2020).
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, N.M.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef] [PubMed]
- Pozuelo-Carrascosa, D.P.; Torres-Costoso, A.; Alvarez-Bueno, C.; Cavero-Redondo, I.; López Muñoz, P.; Martínez-Vizcaíno, V. Multimodality respiratory physiotherapy reduces mortality but may not prevent ventilator-associated pneumonia or reduce length of stay in the intensive care unit: A systematic review. J. Physiother. 2018, 64, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Tipping, C.J.; Harrold, M.; Holland, A.; Romero, L.; Nisbet, T.; Hodgson, C.L. The effects of active mobilisation and rehabilitation in ICU on mortality and function: A systematic review. Intensive Care Med. 2017, 43, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Kress, J.P.; Hall, J.B. ICU-acquired weakness and recovery from critical illness. N. Engl. J. Med. 2014, 370, 1626–1635. [Google Scholar] [CrossRef]
- Herridge, M.S.; Tansey, C.M.; Matté, A.; Tomlinson, G.; Diaz-Granados, N.; Cooper, A.; Guest, B.C.; Mazer, D.C.; Mehta, S.; Stewart, E.T.; et al. Functional disability 5 years after acute respiratory distress syndrome. N. Engl. J. Med. 2011, 364, 1293–1304. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, J.J.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, M.; Lanza, A.; Bellini, R.; Bellofiore, A.; Cecchetto, S.; Colombo, A.; D’Abrosca, F.; del Monaco, C.; Gaudielloet, G.; Paneronial, M.; et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: A Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch. Chest. Dis. 2020, 90. [Google Scholar] [CrossRef] [PubMed]
- Arbillaga, A.; Pardas, M.; Escudero, R.; Rodriguez, R.; Alcaraz, V.; Llanes, S.; Herrero, H.; Gimeno, E.; Rios, A. Fisioterapia Respiratoria en el Manejo del Paciente con COVID-19: Recomendaciones Generales. Area de Fisioterapia Respiratoria. Sociedad Española de Neumología y Cirugía Toracica (SEPAR). Available online: https://www.separ.es/node/1763 (accessed on 13 August 2020).
- Thomas, P.; Baldwin, C.; Bissett, B.; Boden, I.; Gosselink, R.; Granger, C.L.; Hodgson, C.L.; Jones, A.Y.M.; Kho, M.E.; Moses, R.; et al. Physiotherapy management for COVID-19 in the acute hospital setting. Recommendations to guide clinical practice, version 1.0. J. Physiother. 2020, 66, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, D.G.; Rennie, D.; Moher, D.; Becker, J.B.; Sipe, A.T.; Thacker, B.S.; et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Bassett, R.D.; Vollman, K.M.; Brandwene, L.; Murray, T. Integrating a multidisciplinary mobility programme into intensive care practice (IMMPTP): A multicentre collaborative. Intensive Crit. Care Nurs. 2012, 28, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Amidei, C.; Sole, M.L. Physiological responses to passive exercise in adults receiving mechanical ventilation. Am. J. Crit. Care 2013, 22, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Berney, S.C.; Rose, J.W.; Denehy, L.; Grangeret, C.L.; Ntoumenopoulosal, G.; Crothers, E.; Steel, B.; Clarke, S.; Skinner, E.H. Commencing out-of-bed rehabilitation in critical care—What influences clinical decision—Making? Arch. Phys. Med. Rehabil. 2019, 100, 261–269.e2. [Google Scholar] [CrossRef] [PubMed]
- Guia de Actos Fisioterápicos. Ilustre Colegio Profesional de Fisioterapeutas de Andalucía. Available online: https://www.colfisio.org/guia_de_actos_fisioterapicos/indice.html (accessed on 19 August 2020).
- Bissett, B.; Leditschke, I.A.; Green, M.; Marzano, V.; Collins, S.; van Haren, F. Inspiratory muscle training for intensive care patients: A multidisciplinary practical guide for clinicians. Aust. Crit. Care 2019, 32, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Guidance for Prone Positioning in Adult Critical Care. Intensive Care Society. Available online: https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf (accessed on 15 August 2020).
- Royal National Orthoapaedic Hospital NHS Trust (2020). Prone Positioning Plexopathy: Advice to Minimise Risk of Brachial Plexus Injury. Available online: https://www.rnoh.nhs.uk/application/files/6715/8834/4124/Proning_advice_and_pathway_for_COVID19_patients.pdf (accessed on 15 August 2020).
- Hodgson, C.L.; Capell, E.; Tipping, C.J. Early mobilization of patients in intensive care: Organization, communication and safety factors that influence translation into clinical practice. Crit. Care 2018, 22, 77. [Google Scholar] [CrossRef]
- Green, M.; Marzano, V.; Leditschke, I.A.; Mitchell, I.; Bissett, B. Mobilization of intensive care patients: A multidisciplinary practical guide for clinicians. J. Multidiscip Healthc. 2016, 9, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Engel, H.J.; Tatebe, S.; Alonzo, P.B.; Mustille, R.L.; Rivera, M.J. Physical therapist-established intensive care unit early mobilization program: Quality improvement project for critical care at the University of California San Francisco Medical Center. Phys. Ther. 2013, 93, 975–985. [Google Scholar] [CrossRef]
- Griffith, D.E.; Aksamit, T.; Brown-Elliott, B.A.; Catanzaro, A.; Daley, C.; Gordin, F.; Holland, S.M.; Horsburgh, R.; Huitt, G.; Iademarco, M.F.; et al. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respi. Crit. Care Med. 2007, 175, 367–416. [Google Scholar] [CrossRef] [PubMed]
- Medrinal, C.; Prieur, G.; Frenoy, É.; Quesada, R.A.; Poncet, A.; Bonnevie, T.; Gravier, F.-E.; Lamia, B.; Contal, O. Respiratory weakness after mechanical ventilation is associated with one-year mortality—A prospective study. Crit. Care 2016, 20, 231. [Google Scholar] [CrossRef] [PubMed]
- Elkins, M.; Dentice, R. Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: A systematic review. J. Physiother. 2015, 61, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Munshi, L.; del Sorbo, L.; Adhikari, N.K.J.; Hodgson, C.L.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Mancebo, J.; Pesenti, A.; Ranieri, V.M.; et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann. Am. Thorac. Soc. 2017, 14, S280–S288. [Google Scholar] [CrossRef] [PubMed]
- Nydahl, P.; Sricharoenchai, T.; Chandra, S.; Kundt, F.S.; Huang, M.; Fischill, M.; Needham, D.M. Safety of patient mobilization and rehabilitation in the intensive care unit. systematic review with meta-analysis. Ann. Am. Thorac. Soc. 2017, 14, 766–777. [Google Scholar] [CrossRef]
- Stiller, K. Safety issues that should be considered when mobilizing critically ill patients. Crit. Care Clin. 2007, 23, 35–53. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.H.; Shin, M.; Shin, Y.B. Pulmonary and physical rehabilitation in critically Ill patients. Acute Crit. Care 2019, 34. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Taccone, P.; Carlesso, E.; Marini, J.J. Prone position in acute respiratory distress syndrome: Rationale, indications, and limits. Am. J. Respir. Crit. Care Med. 2013, 188, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Ntoumenopoulos, G. Rehabilitation during mechanical ventilation: Review of the recent literature. Intensive Crit. Care Nurs. 2015, 31, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Messerole, E.; Peine, P.; Wittkopp, S.; Marini, J.J.; Albert, R.K. The pragmatics of prone positioning. Am. J. Respir. Crit. Care Med. 2002, 165, 1359–1363. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, C.L.; Stiller, K.; Needham, D.M.; Tipping, C.J.; Harrold, M.; Baldwin, C.E.; Bradley, S.; Berney, S.; Caruana, L.R.; Elliott, D.; et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit. Care 2014, 18, 658. [Google Scholar] [CrossRef] [PubMed]
- Burtin, C.; Clerckx, B.; Robbeets, C.; Patrick, F.; Daniel, L.; Thierry, T.; Greet, H.; Marc, D.; Rik, G. Early exercise in critically ill patients enhances short-term functional recovery. Crit. Care Med. 2009, 37, 2499–2505. [Google Scholar] [CrossRef]
- Denehy, L.; Skinner, E.H.; Edbrooke, L.; Haines, K.; Warrillow, S.; Hawthorne, G.; Gough, K.; Hoorn, S.V.; Morris, M.E.; Berney, S.; et al. Exercise rehabilitation for patients with critical illness: A randomized controlled trial with 12 months of follow-up. Crit. Care 2013, 17, R156. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.L.; Wang, L.Y.; Wu, C.P.; Wu, H.D.; Wu, Y.T. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys. Ther. 2006, 86, 1271–1281. [Google Scholar] [CrossRef]
- Porta, R.; Vitacca, M.; Gilè, L.S.; Enrico, C.; Luca, B.; Ercole, Z.; Nicolino, A. Supported arm training in patients recently weaned from mechanical ventilation. Chest 2005, 128, 2511–2520. [Google Scholar] [CrossRef] [PubMed]
- Engel, H.J.; Needham, D.M.; Morris, P.E.; Gropper, M.A. ICU early mobilization: From recommendation to implementation at three medical centers. Crit. Care Med. 2013, 41, S69–S80. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Ceña, D.; Fernández-de-Las-Peñas, C.; Palacios-Ceña, M.; de-la-Llave-Rincón, A.I.; Florencio, L.L. Working on the frontlines of the COVID-19 pandemic: A qualitative study of physical therapists’ experience in Spain. Phys. Ther. 2021, pzab025. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Joyner, M.; Lucia, A. Early mobilization in hospitalized patients with COVID-19. Ann. Phys. Rehabil. Med. 2020, 63, 384–385. [Google Scholar] [CrossRef]
- Villamil-Parra, W.A.; Hernández-Álvarez, E.D.; Moscoso-Loaiza, L.F. Efficacy of physical exercise in adult patients admitted to ICU: Systematic review and meta-analysis. Fisioterapia 2020, 42, 98–107. [Google Scholar]
- World Health Organisation. Infection Prevention and Control during Health Care Novel Coronavirus (nCoV) Infection is Suspected: Interim Guidance, 25 January 2020; License: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/330674 (accessed on 19 August 2020).
- Borg, K.; Stam, H. Covid-19 and Physical and rehabilitation medicine. J. Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Amatya, B. Medical rehabilitation in pandemics: Towards a new perspective. J. Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.C.; Park, D. How should rehabilitative departments of hospitals prepare for coronavirus disease 2019? Am. J. Phys. Med. Rehabil. 2020. [Google Scholar] [CrossRef] [PubMed]
- Roqué i Figuls, M.; Giné-Garriga, M.; Granados Rugeles, C.; Perrotta, C.; Vilaró, J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database Syst. Rev. 2016, 2, CD004873. [Google Scholar] [CrossRef] [PubMed]
- Dubb, R.; Nydahl, P.; Hermes, C.; Schwabbauer, N.; Toonstra, A.; Parker, A.M.; Kaltwasser, A.; Needham, D.M. Barriers and strategies for early mobilization of patients in intensive care units. Ann. Am. Thorac. Soc. 2016, 13, 724–730. [Google Scholar] [CrossRef]
- Dimitrov, S.; Hulteng, E.; Hong, S. Inflammation and exercise: Inhibition of monocytic intracellular TNF production by acute exercise via β2-adrenergic activation. Brain Behav. Immun. 2017, 61, 60–68. [Google Scholar] [CrossRef]
- Nieman, D.C.; Wentz, L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Morris, P.E.; Goad, A.; Thompson, C.; Karen, T.; Bethanyet, H.; Leah, P.; Amelia, R.; Laura, A.; Shirley, B.; Mary, S.; et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit. Care Med. 2008, 36, 2238–2243. [Google Scholar] [CrossRef] [PubMed]
- Svenningsen, H.; Langhorn, L.; Ågård, A.S.; Dreyer, P. Post-ICU symptoms, consequences, and follow-up: An integrative review. Nurs. Crit. Care 2017, 22, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Held, N.; Moss, M. Optimizing post-intensive care unit rehabilitation. Turk. Thorac. J. 2019, 20, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Jiandani, M.P.; Salagre, S.B.; Kazi, S.; Iyer, S.; Patil, P.; Khot, W.Y.; Patil, E.; Sopariwala, M. Preliminary observations and experiences of physiotherapy practice in acute care setup of COVID 19: A retrospective observational study. J. Assoc. Physicians India 2020, 68, 18–24. [Google Scholar]
- Wittmeier, K.; Parsons, J.; Webber, S.; Askin, N.; Salonga, A. Operational Considerations for Physical Therapy During COVID-19: A Rapid Review. Phys. Ther. 2020, 100, 1917–1929. [Google Scholar] [CrossRef] [PubMed]
- Smondack, P.; Gravier, F.É.; Prieur, G.; Repel, A.; Muir, J.F.; Cuvelier, A.; Combret, Y.; Medrinal, C.; Bonnevie, T. Physiotherapy and COVID-19. From intensive care unit to home care—An overview of international guidelines. Rev. Mal. Respir. 2020, 37, 811–822. [Google Scholar] [CrossRef] [PubMed]
| Author′s Name/Society | Year of Publication | Journal Name | Design | Condition of Interest | Intervention/Assessment 1 | Quality 2 |
|---|---|---|---|---|---|---|
| Li et al. [23] | 2020 | The New England Journal of Medicine | Descriptive study | COVID-19 3 | - | - |
| Guan et al. [4] | 2020 | medRxiv preprint | Descriptive study | COVID-19 | - | - |
| Spanish Government [9] | 2020 | - | Clinical Protocol | COVID-19 | - | - |
| Lazzeri et al. [16] | 2020 | Monaldi Archives for Chest Disease | Clinical Guideline | COVID-19 | - | - |
| SEPAR [17] | 2020 | - | Clinical Guideline | COVID-19 | - | - |
| Thomas et al. [18] | 2020 | Journal of Physiotherapy | Clinical Guideline | COVID-19 | - | - |
| Griffith et al. [34] | 2007 | American Journal of Respiratory and Critical Care Medicine | Statement | Nontuberculous mycobacterial disease | - | - |
| College of Physical Therapy from Andalucia (Spain) [27] | 2020 | - | Clinical Guideline | Respiratory Interventions | - | - |
| Medrinal et al. [35] | 2016 | Critical Care | Observational Cohort Study | Mechanically ventilated critically ill patients | Respiratory weakness | - |
| Bisset et al. [28] | 2019 | Australian Critical Care | Clinical Guideline | Mechanically ventilated critically ill patients | Inspiratory muscle training | - |
| Elkins et al. [36] | 2015 | Journal of Physiotherapy | Systematic review | Mechanically ventilated critically ill patients | Inspiratory muscle training | 9/13 |
| Munshi et al. [37] | 2017 | Annals of American Thoracic Society | Systematic review | ARDS 4 | Prone positioning | 13/16 |
| Gattinoni et al. [41] | 2013 | American Journal of Respiratory and Critical Care Medicine | Narrative Review | ARDS | Prone positioning | - |
| Messerole et al. [43] | 2002 | American Journal of Respiratory and Critical Care Medicine | Expert Commentary | ARDS | Prone positioning | - |
| Intensive Care Society [29] | 2019 | - | Clinical Guideline | Intensive care patients | Prone positioning | - |
| Hodgson et al. [31] | 2018 | Critical Care | Clinical Guideline | Intensive care patients | Mobilization | - |
| Green et al. [32] | 2016 | Journal of Multidisciplinary Healthcare | Clinical Guideline | Intensive care patients | Mobilization | - |
| Hodgson et al. [44] | 2014 | Critical Care | Expert Consensus | Mechanically ventilated critically ill patients | Mobilization | - |
| Bassett et al. [24] | 2012 | Intensive and Critical Care Nursing | Descriptive study | Intensive care patients | Mobilization | - |
| Amidei et al. [25] | 2013 | American Journal of Critical Care | Descriptive study | Mechanically ventilated critically ill patients | Mobilization | - |
| Burtin et al. [45] | 2009 | Critical Care Medicine | RCT 5 | Intensive care patients | Early exercise | 4/10 |
| Engel et al. [49] | 2013 | Critical Care Medicine | Comparative study | Intensive care patients | Mobilization | - |
| Nydahl et al. [38] | 2017 | Annals of American Thoracic Society | Systematic review | Intensive care patients | Mobilization | 14/16 |
| Ntoumenopoulos et al. [42] | 2015 | Intensive Critical Care Nursing | Narrative Review | Mechanically ventilated critically ill patients | Mobilization | - |
| Berney et al. [26] | 2019 | Archives of Physical Medicine and Rehabilitation | Descriptive study | Intensive care patients | Out-of-Bed exercise | - |
| Engel et al. [33] | 2013 | Physical Therapy | Clinical Guideline | Intensive care patients | Mobilization | - |
| Denehy et al. [46] | 2013 | Critical Care | RCT | Intensive care patients | Exercise | 7/10 |
| Chiang et al. [47] | 2006 | Physical Therapy | RCT | Mechanically ventilated critically ill patients | Exercise | 6/10 |
| Porta et al. [48] | 2005 | Chest | RCT | Recently weaned patients | Exercise | 5/10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernal-Utrera, C.; Anarte-Lazo, E.; Gonzalez-Gerez, J.J.; De-La-Barrera-Aranda, E.; Saavedra-Hernandez, M.; Rodriguez-Blanco, C. Could Physical Therapy Interventions Be Adopted in the Management of Critically Ill Patients with COVID-19? A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1627. https://doi.org/10.3390/ijerph18041627
Bernal-Utrera C, Anarte-Lazo E, Gonzalez-Gerez JJ, De-La-Barrera-Aranda E, Saavedra-Hernandez M, Rodriguez-Blanco C. Could Physical Therapy Interventions Be Adopted in the Management of Critically Ill Patients with COVID-19? A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(4):1627. https://doi.org/10.3390/ijerph18041627
Chicago/Turabian StyleBernal-Utrera, Carlos, Ernesto Anarte-Lazo, Juan Jose Gonzalez-Gerez, Elena De-La-Barrera-Aranda, Manuel Saavedra-Hernandez, and Cleofas Rodriguez-Blanco. 2021. "Could Physical Therapy Interventions Be Adopted in the Management of Critically Ill Patients with COVID-19? A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 4: 1627. https://doi.org/10.3390/ijerph18041627
APA StyleBernal-Utrera, C., Anarte-Lazo, E., Gonzalez-Gerez, J. J., De-La-Barrera-Aranda, E., Saavedra-Hernandez, M., & Rodriguez-Blanco, C. (2021). Could Physical Therapy Interventions Be Adopted in the Management of Critically Ill Patients with COVID-19? A Scoping Review. International Journal of Environmental Research and Public Health, 18(4), 1627. https://doi.org/10.3390/ijerph18041627








