Transition to Multidisciplinary Pediatric Telerehabilitation during the COVID-19 Pandemic: Strategy Development and Implementation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development of Guidelines for Telerehabilitation Practice
2.2. Evaluation of Telerehabilitation Sessions
2.3. Data Analysis
3. Results
3.1. Development of Guidelines for Telerehabilitation Practice
3.2. Evaluation of Telerehabilitation Sessions—Clinicians and Families
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.-M.; Divatia, J.V.; Shrestha, B.R.; Arabi, Y.M.; Ng, J.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1680. [Google Scholar] [CrossRef]
- Telemedicine and Telehealth|HealthIT.gov. Available online: https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth (accessed on 18 April 2020).
- Dart, E.H.; Whipple, H.M.; Pasqua, J.L.; Furlow, C.M. Chapter 13—Legal, Regulatory, and Ethical Issues in Telehealth Technology. In Computer-Assisted and Web-Based Innovations in Psychology, Special Education, and Health; Luiselli, J.K., Fischer, A.J., Eds.; Academic Press: San Diego, CA, USA, 2016; pp. 339–363. [Google Scholar]
- Patel, P.D.; Cobb, J.; Wright, D.; Turer, R.W.; Jordan, T.; Humphrey, A.; Kepner, A.L.; Smith, G.; Rosenbloom, S.T. Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: Barriers, solutions, results. J. Am. Med. Inform. Assoc. 2020, 27, 1116–1120. [Google Scholar] [CrossRef] [PubMed]
- Appleby, E.; Gill, S.T.; Hayes, L.K.; Walker, T.L.; Walsh, M.; Kumar, S. Effectiveness of telerehabilitation in the management of adults with stroke: A systematic review. PLoS ONE 2019, 14, e0225150. [Google Scholar] [CrossRef] [Green Version]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 2020, CD010255. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Yamabayashi, C.; Syed, N.; Kirkham, A.; Camp, P.G. Exercise Telemonitoring and Telerehabilitation Compared with Traditional Cardiac and Pulmonary Rehabilitation: A Systematic Review and Meta-Analysis. Physiother. Can. 2016, 68, 242–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef]
- Jiang, S.; Xiang, J.; Gao, X.; Guo, K.; Liu, B. The comparison of telerehabilitation and face-to-face rehabilitation after total knee arthroplasty: A systematic review and meta-analysis. J. Telemed. Telecare 2018, 24, 257–262. [Google Scholar] [CrossRef]
- Van Egmond, M.A.; van der Schaaf, M.; Vredeveld, T.; Vollenbroek-Hutten, M.M.R.; van Berge Henegouwen, M.I.; Klinkenbijl, J.H.G.; Engelbert, R.H.H. Effectiveness of physiotherapy with telerehabilitation in surgical patients: A systematic review and meta-analysis. Physiotherapy 2018, 104, 277–298. [Google Scholar] [CrossRef]
- Standing, C.; Standing, S.; McDermott, M.-L.; Gururajan, R.; Mavi, N.K. The Paradoxes of Telehealth: A Review of the Literature 2000-2015. Syst. Res. Behav. Sci. 2018, 35, 90–101. [Google Scholar] [CrossRef]
- Wade, V.; Soar, J.; Gray, L.C. Uptake of telehealth services funded by Medicare in Australia. Aust. Health Rev. 2014, 38, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Brewster, L.; Mountain, G.; Wessels, B.; Kelly, C.; Hawley, M. Factors affecting front line staff acceptance of telehealth technologies: A mixed-method systematic review. J. Adv. Nurs. 2014, 70, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Wade, V.; Eliott, J.A.; Hiller, J.E. Clinician Acceptance is the Key Factor for Sustainable Telehealth Services. Qual. Health Res. 2014, 24, 682–694. [Google Scholar] [CrossRef] [PubMed]
- Van Houwelingen, C.T.M.; Moerman, A.H.; Ettema, R.G.A.; Kort, H.S.; Ten Cate, O. Competencies required for nursing telehealth activities: A Delphi-study. Nurse Educ. Today 2016, 39, 50–62. [Google Scholar] [CrossRef] [Green Version]
- Ingersoll, B.; Wainer, A.L.; Berger, N.I.; Pickard, K.E.; Bonter, N. Comparison of a Self-Directed and Therapist-Assisted Telehealth Parent-Mediated Intervention for Children with ASD: A Pilot RCT. J. Autism Dev. Disord. 2016, 46, 2275–2284. [Google Scholar] [CrossRef]
- Kuravackel, G.M.; Ruble, L.A.; Reese, R.J.; Ables, A.P.; Rodgers, A.D.; Toland, M.D. COMPASS for Hope: Evaluating the Effectiveness of a Parent Training and Support Program for Children with ASD. J. Autism Dev. Disord. 2018, 48, 404–416. [Google Scholar] [CrossRef] [PubMed]
- Pickard, K.E.; Wainer, A.L.; Bailey, K.M.; Ingersoll, B.R. A mixed-method evaluation of the feasibility and acceptability of a telehealth-based parent-mediated intervention for children with autism spectrum disorder. Autism 2016, 20, 845–855. [Google Scholar] [CrossRef]
- Camden, C.; Pratte, G.; Fallon, F.; Couture, M.; Berbari, J.; Tousignant, M. Diversity of practices in telerehabilitation for children with disabilities and effective intervention characteristics: Results from a systematic review. Disabil. Rehabil. 2019, 1–13. [Google Scholar] [CrossRef]
- Geller, S.M.; Greenberg, L.S.; Watson, J.C. Therapist and client perceptions of therapeutic presence: The development of a measure. Psychother. Res. 2010, 20, 599–610. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage: London, UK, 2013. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007. [Google Scholar]
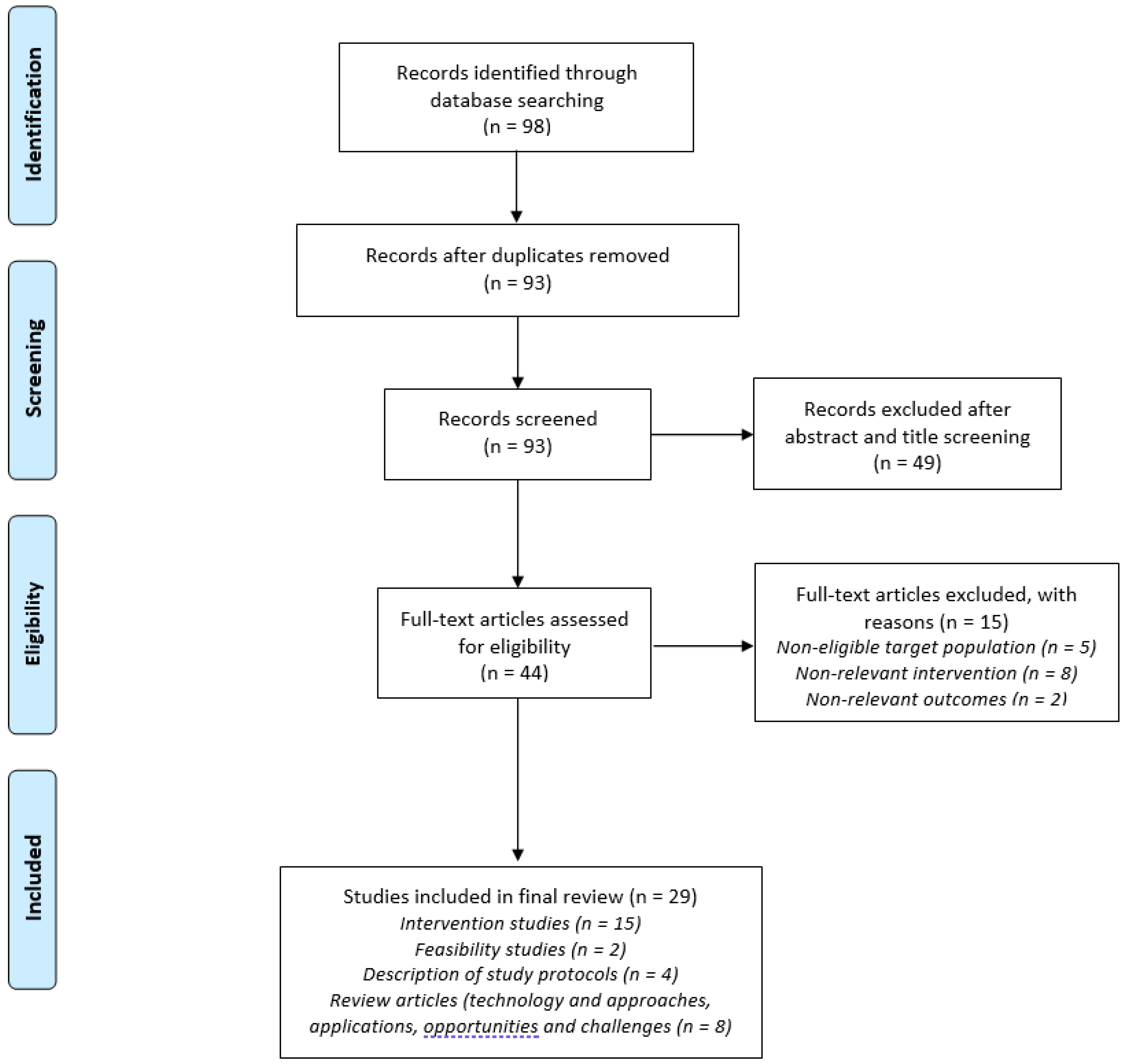
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Camden, C.; Silva, M. Pediatric Teleheath: Opportunities Created by the COVID-19 and Suggestions to Sustain Its Use to Support Families of Children with Disabilities. Phys. Occup. Ther. Pediatr. 2020, 41, 1–17. [Google Scholar] [CrossRef]
- Wind, T.R.; Rijkeboer, M.; Andersson, G.; Riper, H. The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet Interv. 2020, 20, 100317. [Google Scholar] [CrossRef] [PubMed]
- Barney, A.; Buckelew, S.; Mesheriakova, V.; Raymond-Flesch, M. The COVID-19 Pandemic and Rapid Implementation of Adolescent and Young Adult Telemedicine: Challenges and Opportunities for Innovation. J. Adolesc. Health 2020, 67, 164–171. [Google Scholar] [CrossRef]
- Berger, T. The therapeutic alliance in internet interventions: A narrative review and suggestions for future research. Psychother. Res. 2017, 27, 511–524. [Google Scholar] [CrossRef]
- Bexelius, A.; Carlberg, E.B.; Löwing, K. Quality of goal setting in pediatric rehabilitation-A SMART approach. Child Care Health Dev. 2018, 44, 850–856. [Google Scholar] [CrossRef]
- Topooco, N.; Riper, H.; Araya, R.; Berking, M.; Brunn, M.; Chevreul, K.; Cieslak, R.; Ebert, D.D.; Etchmendy, E.; Herrero, R.; et al. E-COMPARED consortium Attitudes towards digital treatment for depression: A European stakeholder survey. Internet Interv. 2017, 8, 1–9. [Google Scholar] [CrossRef]
- Heeren, A. Commentary: The Impact of Digital Technology on Psychological Treatments and Their Dissemination. Front. Psychol. 2018, 9, 1571. [Google Scholar] [CrossRef]
- Antón, D.; Berges, I.; Bermúdez, J.; Goñi, A.; Illarramendi, A. A Telerehabilitation System for the Selection, Evaluation and Remote Management of Therapies. Sensors 2018, 18, 1459. [Google Scholar] [CrossRef] [Green Version]
- Kizony, R.; Weiss, P.L.; Elion, O.; Harel, S.; Baum-Cohen, I.; Krasovsky, T.; Feldman, Y.; Shani, M. Development and validation of tele-health system for stroke rehabilitation. Int. J. Disabil. Hum. Dev. 2014, 13, 361–368. [Google Scholar] [CrossRef]
- Caprì, T.; Nucita, A.; Iannizzotto, G.; Stasolla, F.; Romano, A.; Semino, M.; Giannatiempo, S.; Canegallo, V.; Fabio, R.A. Telerehabilitation for Improving Adaptive Skills of Children and Young Adults with Multiple Disabilities: A Systematic Review. Rev. J. Autism Dev. Disord. 2020, 1–9. [Google Scholar] [CrossRef]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy During the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys. Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Rabatin, A.E.; Lynch, M.E.; Severson, M.C.; Brandenburg, J.E.; Driscoll, S.W. Pediatric telerehabilitation medicine: Making your virtual visits efficient, effective and fun. J. Pediatr. Rehabil. Med. 2020, 13, 355–370. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. Retrieved March 2020, 27, 2020. [Google Scholar]
| Topic | Description | Notes to Clinicians |
|---|---|---|
| Goals of telerehabilitation |
|
|
| Preliminary discussion of therapeutic principles (clinician + parent) | A preliminary talk should include:
|
|
| Content of session |
|
|
| Assessment |
|
|
| Score [1,2,3,4,5] Mean ± SD | Rotated Component Coefficients | ||||
|---|---|---|---|---|---|
| Item | Component 1 | Component 2 | Component 3 | Communalities | |
| 1. I was able to grade levels of difficulty in the session according to the child’s capabilities | 3.38 ± 1.25 | 0.939 | −0.026 | 0.023 | 0.883 |
| 2. Feedback to the child was efficiently transferred | 2.92 ± 1.02 | 0.911 | 0.123 | −0.017 | 0.845 |
| 3. I was focused during the session | 4.29 ± 0.99 | 0.837 | 0.040 | 0.030 | 0.703 |
| 4. Home environment conditions were suitable for the activities | 3.29 ± 1.12 | 0.791 | 0.106 | 0.009 | 0.638 |
| 5. The child was distracted (inversed score) | 2.96 ± 1.43 | 0.709 | 0.515 | 0.102 | 0.778 |
| 6. I could evaluate the status of the child | 2.82 ± 1.05 | 0.680 | 0.100 | −0.092 | 0.481 |
| 7. The child cooperated during the session | 3.79 ± 1.22 | 0.623 | 0.356 | .390 | 0.666 |
| 8. This telerehabilitation session assists the child | 3.67 ± 0.96 | 0.615 | 0.540 | −0.044 | 0.672 |
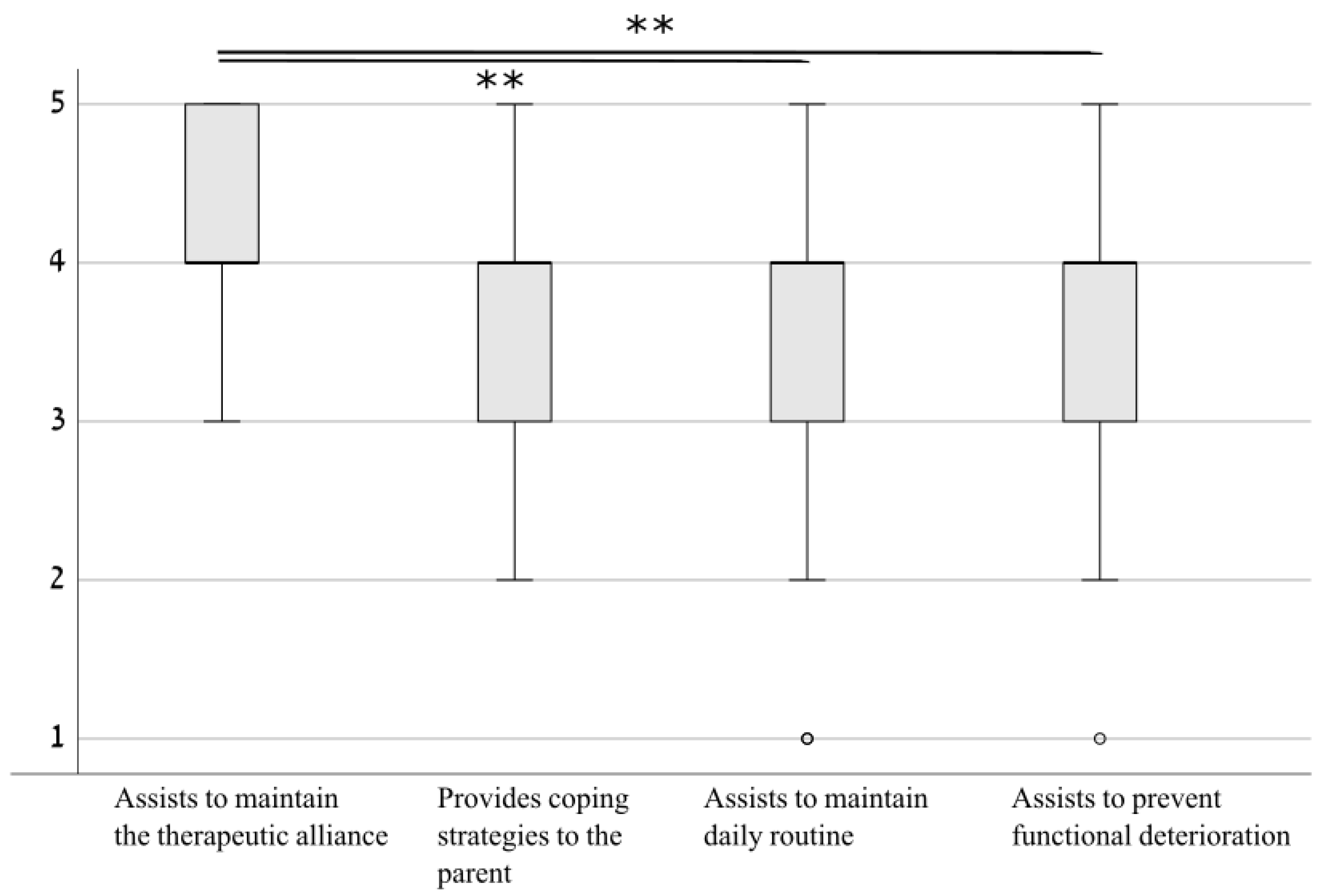
| 9. This telerehabilitation session assists in preventing functional deterioration | 3.79 ± 0.83 | 0.040 | 0.916 | 0.141 | 0.860 |
| 10. This telerehabilitation session assists in maintaining daily routine | 3.54 ± 1.02 | 0.009 | 0.906 | −0.033 | 0.822 |
| 11. This telerehabilitation session assists in maintaining therapeutic alliance | 4.17 ± 0.64 | 0.404 | 0.530 | 0.272 | 0.518 |
| 12. This telerehabilitation session provides coping strategies to the parent | 3.92 ± 0.72 | −0.140 | −0.029 | 0.850 | 0.742 |
| 13. The parent cooperated during the session | 4.71 ± 0.55 | 0.145 | 0.506 | 0.619 | 0.660 |
| Item | Mean (SD) | 95% Confidence Interval (CI) for the Mean |
|---|---|---|
| My therapist was fully there in the moment with me. | 6.8 (0.38) | 6.71–6.96 |
| My therapist’s responses were really in tune with what I was experiencing in the moment. | 6.75 (0.6) | 6.55–6.95 |
| My therapist seemed distracted (*reversed). | 6.67 (1.17) | 6.27–7.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krasovsky, T.; Silberg, T.; Barak, S.; Eisenstein, E.; Erez, N.; Feldman, I.; Guttman, D.; Liber, P.; Patael, S.Z.; Sarna, H.; et al. Transition to Multidisciplinary Pediatric Telerehabilitation during the COVID-19 Pandemic: Strategy Development and Implementation. Int. J. Environ. Res. Public Health 2021, 18, 1484. https://doi.org/10.3390/ijerph18041484
Krasovsky T, Silberg T, Barak S, Eisenstein E, Erez N, Feldman I, Guttman D, Liber P, Patael SZ, Sarna H, et al. Transition to Multidisciplinary Pediatric Telerehabilitation during the COVID-19 Pandemic: Strategy Development and Implementation. International Journal of Environmental Research and Public Health. 2021; 18(4):1484. https://doi.org/10.3390/ijerph18041484
Chicago/Turabian StyleKrasovsky, Tal, Tamar Silberg, Sharon Barak, Etzyona Eisenstein, Neta Erez, Irit Feldman, Dafna Guttman, Pnina Liber, Smadar Zohar Patael, Hadar Sarna, and et al. 2021. "Transition to Multidisciplinary Pediatric Telerehabilitation during the COVID-19 Pandemic: Strategy Development and Implementation" International Journal of Environmental Research and Public Health 18, no. 4: 1484. https://doi.org/10.3390/ijerph18041484
APA StyleKrasovsky, T., Silberg, T., Barak, S., Eisenstein, E., Erez, N., Feldman, I., Guttman, D., Liber, P., Patael, S. Z., Sarna, H., Sadeh, Y., Steinberg, P., & Landa, J. (2021). Transition to Multidisciplinary Pediatric Telerehabilitation during the COVID-19 Pandemic: Strategy Development and Implementation. International Journal of Environmental Research and Public Health, 18(4), 1484. https://doi.org/10.3390/ijerph18041484







