3. Results
3.1. Participant Characteristics
Of the 12 patient–parent pairs recruited for the telerehabilitation program, nine from four different groups completed the program and final interview. The three families that did not complete the program were either excluded (
n = 1 relapsed;
n = 1 did not meet technical requirements) or dropped out due to parents’ lack of interest (
n = 1). The characteristics of the 16 participants who completed the program (parents and children) are found in
Table 1.
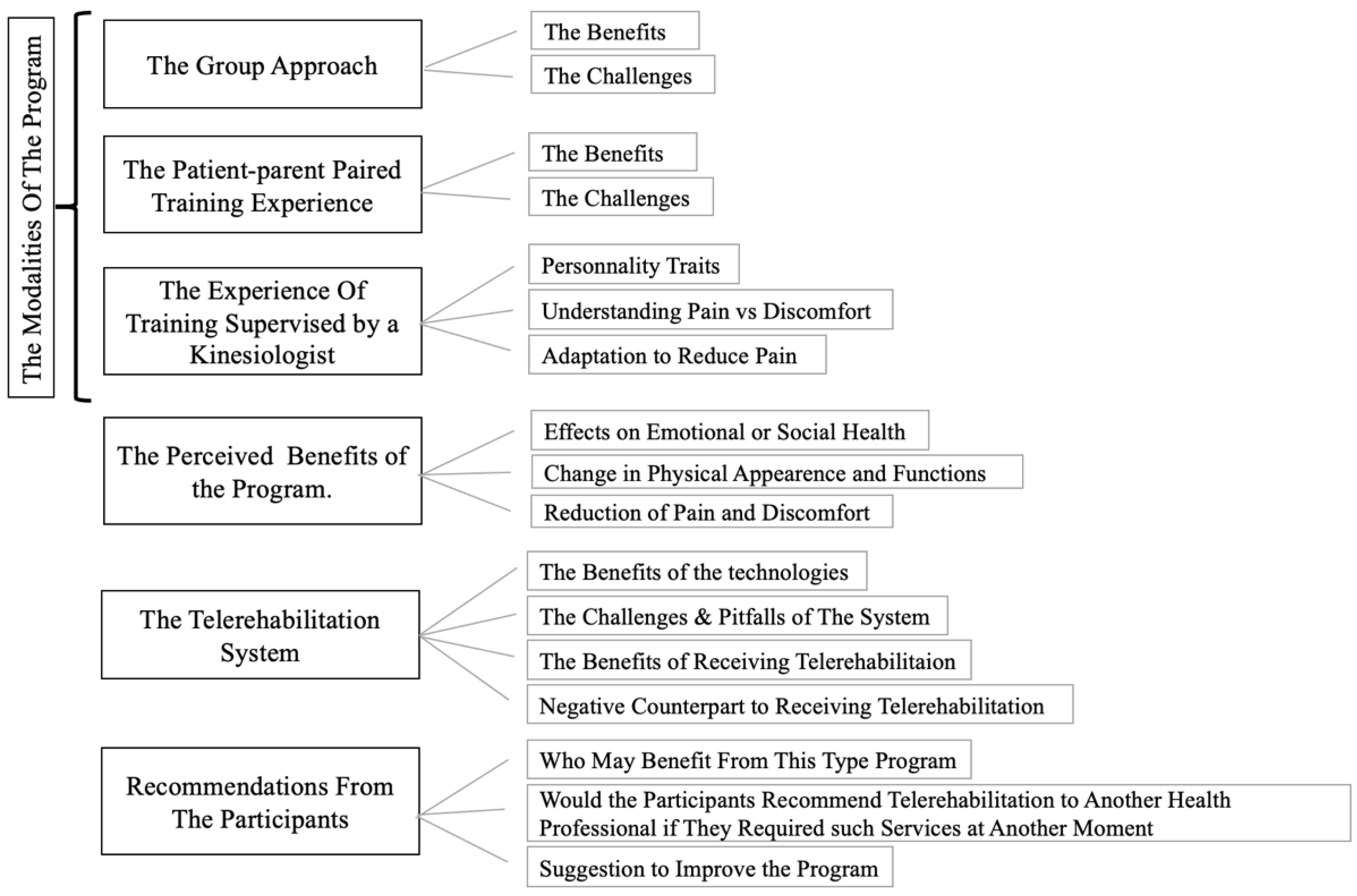
3.2. Overarching Themes
The interview results confirm that patient and parent experiences were influenced by the modalities of the program (i.e., group training, patient–parent pairing, and kinesiologist supervision), the perceived benefits of the intervention, and the telerehabilitation system itself. Participants also offered recommendations for other families and healthcare professionals considering such a program. The themes identified and confirmed by the authors are shown in
Figure 2.
3.3. The Group Approach
The role of the group approach in participants’ experience was widely positive. Participants reported few challenges. Only one parent reported a major challenge.
While only some parents mentioned the telerehabilitation program would have been impossible without the group approach, many patients mentioned that when the other families were unable to attend the session, they felt it was “a little boring” (Patient 06) or “monotonous” (Patient 12), suggesting it was less motivating. In fact, the group approach was identified as a motivating factor by all participants, parents and patients alike. The underlying motivational phenomena were mostly healthy competition and a collaborative atmosphere between families, in addition to feeling able to relate to each other. Patients reported “healthy competition, because when you’re next to someone, you’re always going to try to do like the person next to you (during in-person trainings). But now, it is in our home… (everyone feels comfortable) That’s it, everyone’s doing their work. When someone feels tired, others can go on, or stop, you don’t feel like you have to force or anything” (Parent 12). The second motivating phenomenon of the group approach was the collaborative atmosphere: “It was like teamwork” (Patient 09). It was reported that if “someone had a problem, we could give ideas, we could help each other” (Patient 11) and encourage each other: “It’s actually more than positive, because when (Patient 09) would see the other girl exercising, she would be like, ‘Yeah, let’s do this’! and they would high-five each other at the end” (Parent 09). Moreover, participants appreciated being able to relate to others about their health: “I wasn’t comparing myself, but I could see that I wasn’t the only one who wasn’t used to it. So that made me feel comfortable, I was not alone” (Parent 05). “There was a father who had a knee problem, and I have a shoulder problem” (Parent 12). “It was good because you could meet more people and could see others who had the disease, what it is like, and if they have the same booboos as you do, things like that” (Patient 04). They also mentioned shared challenges: “Because sometimes they’d say things to each other. Let’s say, if it’s advice, it can also apply to me too. Even if she (the kinesiologist, G.L.) isn’t talking to me, I can still listen to her” (Patient 10). “We are not alone in our living room doing this” (Parent 10).
The level of interaction varied between groups. Group 1 did not communicate very much with other families, while Groups 3 and 4 had patients that played together when hospitalized during treatments. “I like exercising with someone—another family I’ve met in the hospital. Before, it was kind of a hospital friend” (Patient 09). This may have elicited a higher level of interaction among both patients and parents. Participants in Group 4 did not know each other before the program, but became friends: “(today we) met for the first time (during the final evaluation), it’s like (we have) known each other for years” (Parent 12).
During the interviews, very few challenges were mentioned related to the group approach. Parents commented that families “were not always in sync” (Parent 10), which made the parent anxious to keep pace, although she added that the kinesiologist did not pressure them. Another parent mentioned not really hearing the other families “people were still discreet” (Parent 04). On the other hand, challenges regarding the group approach reported by patients included families disappearing from the screen, or not seeing everyone all the time; however, only one patient said this approach was distracting. Another patient reported that, at times, another participant looked like he did not want to be there.
The major challenge cited earlier referred to a parent experiencing discomfort overhearing an incident in another family: “We didn’t have to hear that” (Parent 11). The parent said, “We don’t all have the same values”, and concluded, “Afterwards, I don’t know if someone spoke to them or not, but it was less disturbing (the training), and more fun”.
3.4. The Patient–Parent Paired Training Experience
According to the parents, the patient–parent paired training was also beneficial. Limited challenges and no major challenges were cited by study participants.
The main benefits reported were the motivation it provided, the time spent together, the healthy competition, and the opportunity for parents to help their child. Motivation was mentioned by several participants: “It also helps motivate (Patient 06) because sometimes she doesn’t want to do it, sometimes she does. It depends on her mood” (Parent 06). Many patients or parents mentioned that training sessions were an opportunity to spend quality time together: “It’s rare that you have a lot of time together because, at school, you always have to hurry. When it comes to training, you are more relaxed” (Patient 04). Many parents found it to be a time to develop their relationship with their child: “We do it together. The exercises with the elastic band also created a bond because we watch each other and do it together. I think that it gave me a (sense of) complicity with my daughter (a desire) to do activities (together), and it really makes me see that training should not be seen as an overload of activity, but rather as a family moment” (Parent 05). One of the parents reported that his relationship with his son improved. The child “has ADHD with an opposition disorder, so there’s always parent–child conflict. (The program) allowed me (Parent 12) to spend time with him, and at the same time, to do something with him, (…) to get closer—well not to get closer, but (for him) to see someone other than the father who says stop doing that, or whatever” (Parent 12). Both parents and patients also appreciated that there was healthy competitiveness between them. This rivalry was perceived as motivating: If patients saw they were able to do one more repetition than their parent, it empowered them to continue. Moreover, patients appreciated the opportunity for their parent to assist them: “It helped (to do the training with my mother) because my mother, even if (the kinesiologist) didn’t say it, she (referring to the mother) could tell me things that I had to improve” (Patient 05). Parents recognized and valued the supportive role they played in their child’s experience: “(…) him just doing the exercises wouldn’t have worked. First, (he has to understand), and also there are exercises you (referring to Patient 07) needed a little help with and stuff—like holding the carrot (referring to assisted drop jump)—it went really well. And then, I also participated, and that makes me feel good, too” (Parent 07).
As indicated above, the pairing of parents and patients caused no critical issues; however, some challenges were raised, such as conflicts: “sometimes, if we quarrelled (…) everyone could hear us” (Patient 04). One family mentioned that a parent was less motivated, which reduced the motivation of the patient. Another child mentioned that sometimes the parent was anxious to finish quickly to continue doing housework. Differences in strength between partners was also reported twice as a possible limiting factor by two teenagers, which had an impact on the partner they chose to exercise with: One decided to exercise with her parents instead of her siblings; another chose his father instead of his mother as his exercise partner.
3.5. The Training Experience While Supervised by A Kinesiologist
When asked about their experience of training while supervised by a kinesiologist, participants unanimously said they felt the kinesiologist had a positive impact. All participants said that they received enough information to do the exercises correctly, and that the information was clear. Some mentioned that, if they misunderstood or an audio-video lag occurred, the kinesiologist took the time to explain and demonstrate the exercise again. This was greatly appreciated by participants, as expressed by one parent: “If (…) we didn’t understand, she would go down on the ground to demonstrate the exercise” (Parent 03). Participants expanded mainly on three elements regarding the kinesiologist: (a) the kinesiologist’s personality, which helped foster the therapeutic relationship; (b) their understanding and attention paid to pain and discomfort; and (c) their knowledge and ability to adapt the training to individual limitations.
The kinesiologist’s personality was the factor most often mentioned by study participants. Many parents used qualifiers such as attentive, knowledgeable, motivating and motivated, inclusive, accommodating, accessible or approachable, and open to questions. Additionally, almost all parents used at least one of the following adjectives, warm, kind, playful, positive, dynamic, or enthusiastic, when describing the kinesiologist’s personality. For their part, patients described the kinesiologist as friendly, nice, happy, funny, playful, motivating, and engaged. Patients appreciated the incorporation of games in the training “We do games, yes it’s going to be exercise, but in activities” (Patient 06). Some patients mentioned that the kinesiologist was a mix of serious and comical, or relaxed, that they were supportive, and that they provided constructive criticism. To describe their relationship with the kinesiologist, some made the following comparisons: “like my teacher” (Patient 11) or “a fourth cousin who you don’t know, but play well with” (Patient 12), illustrating the friendly therapeutic relationship that developed between the patient and trainer.
Furthermore, some parents and patients emphasized that they appreciated the opportunity to understand the nuance between pain and discomfort that the patients were experiencing. As seen in
Table 2, patients frequently reported pain throughout the program which demanded adaptation (varying among patients from 42% to 96% of sessions). The kinesiologist took the time in each instance to discuss and understand the pain or normal discomfort that the participant was feeling. On this topic, one parent interviewed said that, before the program, he did not know how to react when his son was complaining of pain, but he was now able to ask questions and help his son understand what he was experiencing: “Yes, he had pain in his feet, because it is normal after treatments. But now, we learned something:
‘is it pain or discomfort’? Sometimes, he does physical education at school, then he comes home, and he’s tired. And ‘
yes, you have done physical activities, so, of course, you are a little uncomfortable’. (…) Then he understood the difference” (Parent 07).
Lastly, the kinesiologist paid careful attention to pain, in order to adapt the exercises and training to participants’ individual condition and limitations. The ability to adapt the exercises and training to all participants was greatly appreciated by both parents and patients. “And really, it worked” (Patient 11), “I had back pain before, and she gave me tips to have less back pain” (Patient 04). Parents appreciated the adjustments for their children as it made the training “adapted to their needs” (Parent 04). But they also appreciated having access to the service for themselves: “because, even though we are parents, we have little booboos” (Parent 12), and “she always had a plan B and a plan C when someone was having pain; you know, like me. Sometimes I had pain in my knee, and I would tell her and (she would say:) Okay, do this exercise instead” (Parent 06). This allowed parents “to be active, without doing the same exercises” (Parent 12).
3.6. The Perception of Training Benefits
Although the program aimed to improve physical function, participants perceived benefits that extended beyond this outcome. The interviews and kinesiologist’s clinical notes revealed that participants recognized positive effects on emotional or social health, and changes in appearance and function. Some participants also reported less pain and discomfort as a result of the program.
The effects on emotional or social health were reported mainly by the parents on behalf of their children. Almost half the parents spoke of the effects of the program on their child’s self-esteem, ability to focus, general motivation, or socialization and communication skills. Two patients also mentioned this aspect during their interviews:
Patient 09, “It also helped me get less distracted”.
Interviewer, “Less distracted? Do you mean during the training, or just in general”?
Patient 09, “In general”.
Interviewer, “In general”?
Patient 09, “It helped me get less distracted, because I’m always distracted”.
The main changes in physical function cited by parents and patients alike were improved strength, increased endurance either during trainings or in everyday life, and increased energy or less fatigue. Participants mentioned, among other things, the ability to do exercises at the end of the program that they could not do at the beginning (such as push-ups or burpees), or being able to wear their backpack to school, walk to school, jog in a corridor, or pick up grocery bags more easily than before, with less tiredness or fatigue. “At first, he was really, in physical terms, he was really not at all in shape. I even met his physical education teacher at school, and he said, ‘Ah! (Patient 07) has improved. He is doing very well! Are you doing anything special’? I explained the program to him a bit. We were also able to start playing other sports, and he is good at them: We play badminton and soccer, and it’s going well. Before, I tell you, five minutes and he was ready to give up” (Parent 07). Another patient decided to take up a new sport: “Because I wasn’t there for a few years. Just after I finished chemo, and I wasn’t able… I was weak… I didn’t have enough energy, strength so—I felt like, during the training I did, I bounced back, so I want to take advantage of it to try to start karate again” (Patient 06). Parents also spoke of appearance. A third of parents reported changes in their child’s appearance, mainly patients looking thinner or having more muscle definition. One parent also reported that they, too, lost weight.
Some patients and parents saw a reduction in pain and discomfort as a result of the program. Two parents expressed a reduction in either chronic or acute knee pain due to the program exercises or movement corrections. Patients mentioned chronic pain such as headaches, and back, leg or foot pain, which they attributed to the lasting effects of ALL treatments. Patients did not report diminished frequency of headaches in daily life, however, some said that other types of pain decreased or disappeared: “All the pain went away while doing the exercises. I may still be in pain sometimes (referring to headaches), but the physical pain, doesn’t happen that much anymore” (Patient 10). Another patient reported disappearance of pain multiple times during the program: “I used to get up (in the morning), and there was a leg like, it just didn’t work. It was stiff, and it hurt. I had to find a (different) way to go down the stairs, or it hurt. But now, that has stopped” (Patient 11). Clinical notes confirmed that some patients reported specific sensations as pain at the beginning, and over the weeks reported it as discomfort or no longer reported it at all. This was most notably the case for Patient 07 and Patient 12.
3.7. The Telerehabilitation System
One of the main benefits of telerehabilitation technologies mentioned by the parents was that the system was adaptable. The families valued being able to use their own technologies. For example, a family that used their tablet mentioned, “it wasn’t distracting me from anything and, you know, if it had been a big screen, and I would have seen them (the other families) live, then I would have been uncomfortable. But the way it was set up, it was fine” (Parent 03). Another family said, “We really had a great set-up at home. I was able to take my laptop and put it (the video feed) on the television” (Parent 05). Furthermore, many patients and parents described the system technologies as user-friendly, which allowed patients in more than half the families to sometimes connect by themselves to the telerehabilitation sessions. A specific detail mentioned that facilitated the experience was that links for the training sessions were sent by email the day before the session: “It was easy. Well, we just had to click on a link (…) in an email. Because we had the codes, and we were given them as we went through the sessions” (Patient 12).
However, even if the technologies were generally easy to use for all families, when asked about minor or major challenges, most participants mentioned occasional video or audio malfunctions, “It happened from time to time, sporadically” (Parent 12). System difficulties were reported if other family members were using the Internet simultaneously, if the weather was poor, or sometimes if families were doing the training from somewhere other than at home. Some families said that issues occurred mostly in the early sessions, while they were adjusting their Internet consumption: “At home, the children all have devices that use the Internet. So, at the beginning, we weren’t sure. We didn’t really know how much consumption it was going to take. So, at the beginning, the first and second week we had a lot of, you know, lags, because the Internet was in great demand, because the children were already listening to videos with voices, and we had the camera live with the voice. Well, there was one point when the Internet jumped a bit there. (…) We had stopped the devices (for the other) children during the training; to dedicate the Internet just to that” (Parent 06). “No, nothing went wrong. But at first the camera froze a lot”. (Patient 09). Two other factors were mentioned as limiting by some parents. The first was the sound, “As soon as someone spoke, we couldn’t hear what was happening elsewhere (…) we could no longer hear what the instructor was saying. It was hard to manage sometimes. It was not all the time” (Parent 10). The second limiting factor was the watch, “Sometimes we forgot, it’s our fault, but we forgot to plug in the watch, and things like that” (Parent 04).
Overall, the telerehabilitation method of delivering the service was identified as beneficial by all participants, because the program did not require travel and could be done from the comfort of their home, allowing families to balance training with personal and professional activities. Some mentioned that it might not have been possible for them to participate if the program had been in-person: “We don’t waste 20 or 30 min to get there and come back. It sounds like nothing, but it’s still precious. Because if we had to go to (the hospital), (…) it’s not certain that we could have participated” (Parent 06). Others said that the telerehabilitation delivery was crucial in their decision to participate “Three evenings, it was going to be a little more difficult. (…) The fact that I knew I didn’t have to go out, that was one of the characteristics that made me say yes” (Parent 11). Patients also liked not having to come to the hospital for interventions: “Before the telehealth, I was like ‘Why don’t we go to the hospital? That would be better’. It would be weird to do it on the computer. But then I noticed it was better, because you can do it in your living room. You don’t have to be like, ‘Okay, it’s 6:30 a.m. I have to go to the hospital’. Because it takes an hour to get there, and it will be at 7:30 a.m. You can say like, ‘It’s 7:15. Okay, I’m going to turn on the television, and I’m going to start this’. There you go, you didn’t have to go to the hospital and do everything” (Patient 05). Doing the training at home was appreciated by all parents, but this subject was not addressed as much by patients. Parents mentioned that their children felt at ease doing their exercises, and that it was even more beneficial in winter that they did not need to leave the house. Moreover, they agreed on the convenience of the delivery method. Most parents mentioned that it helped to balance the training in the family’s everyday life: “In family life with children, it fits well, it makes it much easier. I don’t need to call a babysitter for the others while we go to his appointment. For family management, I think it’s something very useful” (Parent 10). As indicated in the kinesiologist’s notes, it was common for families to have the other parent involved in the training (n = 7), as well as siblings (n = 4), cousins (n = 1), grandparents (n = 2) or even friends (n = 2).
However, in some cases, the increased accessibility of the telerehabilitation method of delivery led to a sense of obligation, especially among the teenagers: “(I) felt a bit like I had to do it even though I didn’t feel like it sometimes. Then, like when I was in pain, I felt bad for not doing it” (Patient 03).
3.8. Recommendations and Suggestions from the Families
When asked if they would recommend the program to other patients and their families, all parents and patients agreed that they would, some even going so far as to propose that it become part of the ALL treatment protocols: “This should be a part of the treatment. It has (been) five years (since) she (Patient 09) got sick, she has (had) two years of chemotherapy. This type of program should be included in her treatment, as a follow-up with the hospital, because she would benefit a lot. (It would be) beneficial for all kids in her situation” (Parent 09). Similarly, most parents and patients also thought that the telerehabilitation delivery method could be useful not only for cancer survivors but for anyone interested in exercising. Some patients specifically mentioned that it would be ideal for populations with factors that limit travel or mobility. Others mentioned that if the person is able to do the training in person, it may not be needed.
Many parents agreed that they would propose the telerehabilitation method of delivery to another health or sport professional if they ever needed such rehabilitation services again, mainly due to the aforementioned general benefits of the telerehabilitation service delivery method: no travel time, being able to do it from the comfort of their own home, and the balance of training with personal and work life.
During the program, a few families said that they would have appreciated at least a few in-person training sessions to help correct movements that were more technically difficult for the patient and to get tactile feedback. Other suggestions from the families to the research team for improving the system or service were as follows:
Provide more material (such as yoga mats, or wider variety of weighted balls, and elastic bands).
Provide the system to families with fewer technologies at home, or with better quality cameras that could be controlled by the kinesiologist to focus on participants so that they would stay in the frame while in motion (Parent 06), or even to use a set of three cameras to see different angles.
For the kinesiologist to “have (real-time) access to the data from the training (to) watch” on the screen, to help motivate and set goals (Parent 10).
Have a more flexible schedule for families to do a different session if they couldn’t attend one earlier in the week. “Let us decide when our training is. (…) Sometimes, we might have an exam on Thursday, so we can’t do it on Wednesday evening because it takes too long and we couldn’t study” (Patient 04), or for families to select their preferred times without selecting the age group.
Offer a longer program to gain more benefits (“a full school year” (Patient 11) was proposed by two families).
Incorporate a wider variety of exercises, or exercises that each child likes, and more games.
Encourage families to include friends, siblings, and other family members to shift the focus and make it playful.
Offer the service earlier to help families plan their schedules ahead of time.
Offer the service to more families “As a part, included in the treatments” (Parent 09).
The hospital should better advertise the service to families, such as having the treating physician recommend the program to patients during the final months of treatments.
4. Discussion
Parents and patients were very satisfied with the program, as confirmed by the semi-structured interviews. All participants said they would recommend the program to other families in their situation. In addition, they all spoke in great detail of the benefits of the program and its modalities, and were less concerned by its challenges.
Factors that contributed to the high satisfaction identified in this study, i.e., primarily the method of delivery and the intervention modalities, may explain the high adherence rates recorded in this study (89% [
10]), and for some, may have contributed to the initial decision to participate. The current findings illustrate that the telerehabilitation method of delivering the rehabilitation service was critical in choosing to participate, played an important role in facilitating participants’ access to the program, and, subsequently, to their satisfaction with the program. Pairing, grouping, and supervision also positively influenced participants’ experience once they chose to enroll in the program. The frequency and quantity of benefits mentioned during the interviews concerning these aspects of the program far outweighed the challenges. Therefore, it would seem that the modalities of the telerehabilitation service (i.e., pairing, grouping, and supervision) impacted adherence to the program, while its accessibility contributed to the initial decision to participate.
The literature examining factors influencing ALL survivors to participate in, adhere to, and complete a rehabilitation or exercise program is limited. Nevertheless, the findings of the current study are consistent with the earlier study done by Wright et al. (2015). Both highlight that participants prefer to exercise at home rather than at a hospital or clinic [
6].
Furthermore, the current study parallels the findings of Kairy et al. (2013) in certain respects. The latter explored the patient perspective of adults who received an eight-week home-based telerehabilitation program following total knee arthroplasty [
11]. That study used a system similar to the current study, to provide supervised intervention to patients; however, their program was neither paired nor grouped. Although each study targeted very different populations, their findings are astonishingly similar, indicating that the aspects interviewees appreciated most were being able to receive the services at home, and their relationship with the physiotherapist. In both studies, participants reported that the physiotherapist and kinesiologist were capable of adequately evaluating patient’s technique, pain, and discomfort. Furthermore, patients in both studies mentioned that some in-person sessions might be useful to facilitate a clinical follow-up, such as physical correction. Lastly, in both studies, telerehabilitation was not viewed by patients as an impediment to their satisfaction with the program. However, the differences between the populations and modalities (i.e., paired and grouped trainings) may have influenced the perspective of the participants: Patients in the current study highlighted the playfulness of both the training regimen and their kinesiologist. Additionally, while in the study by Kairy et al. the patients preferred the telerehabilitation delivery method over in-person, due to saved preparation and travel time, they did not mention the advantages of better balancing of personal, family and work life, a factor raised repeatedly in the current study. The increased social interactions, due to the paired and grouped approach of the current study, may have imposed some challenges, but motivated participants to adhere to the program [
15].
To this extent, a study revealed that children with disabilities considered their participation in physiotherapies and occupational therapies meaningful when they were enjoying themselves, felt capable and autonomous in their activity, and when there was a social component to the activity [
16]. The modalities of the present study had an intrinsic social component. Participants took full advantage of the social involvement. The original “patient–parent paired” experience very often expanded to not just two but three participants, including other family members or friends. Furthermore, participants mentioned the perceived benefit of being able to do exercises or tasks that had once been difficult. This finding aligns with the essential role of capacity in creating a meaningful rehabilitation experience. Lastly, participants highlighted the importance of enjoyment in their experience of the current program. This enjoyment is noted, in their perspective, concerning the modalities: Patients appreciated the healthy competition between families, as well as with their parents. Enjoyment is also observed in their perspective of the kinesiologist’s personality. Both patients and parents described her as playful. It is also noted in their recommendations for future programs.
Early survivors of ALL are known to be a difficult population to recruit for exercise interventional study. Their adherence to such programs tends to be low, since they are less active than the general population. Furthermore, after ALL treatment completion, patients and their families may experience challenges related to family cohesion [
17] and the addition of school-related activities to the schedule [
18]. In these respects, the modalities of the current program were beneficial, since they reduced the burden on the family’s schedule by increasing the accessibility of the rehabilitation services. The social intra- and inter-family interactions might also provide a valuable tool to improve patient motivation to adhere to such rehabilitation programs.
Study Limitations
The main limitation of this study was the small sample size: Results from nine parent–patient pairs cannot be generalized to the entire population of early survivors of ALL. Furthermore, interviews were conducted only with participants who completed the program, and their perspectives may differ from participants excluded prior to intervention completion.
The current study used a hybrid approach (i.e., not all interactions with the kinesiologist were done remotely) that may have allowed the therapeutic relationship with the participants to develop, but it is impossible to infer whether this would be better than other telerehabilitation approaches, such as conducting all activities online. One of the main aspects appreciated by both parents and patients was supervision by the kinesiologist during the telerehabilitation training sessions. However, it is important to note that the therapeutic relationship fostered between participants and the kinesiologist was not created exclusively through the use of telerehabilitation. Participants met the kinesiologist twice before starting the program: once for the baseline evaluation in the hospital (three to four hours), and once for a home visit to help the families prepare the technologies and their training environment (45 to 90 min). Consequently, it is not possible to infer from the results of this study alone that a therapeutic relationship can be created through the use of telerehabilitation alone.
Moreover, regarding the benefits perceived by participants, it remains unclear if the decreased pain that patients reported was due to actual changes in the pain sensation (i.e., whether it decreased to discomfort or the sensation was no longer present), or was the result of the educational role of the kinesiologist in gaining a better understanding of the pain. Nonetheless, pain is a very important issue and was raised as limiting in this study. This finding raises the need to address pain in this population, using a multidisciplinary approach.