Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Statistical Models and Discovery of Association Rules
2.2.1. Rank—frequency Analysis
2.2.2. Discovery of Association Rules
- Support measures the co-occurrence frequency of X and Y in the patient dataset, i.e., the number of patients having both X and Y divided by the total number of patients, denoted as P(X, Y).
- Confidence measures the reliability of a rule—namely, the probability of seeing Y among patients with X, denoted as P(Y|X).
- Lift measures the significance of the support P(X, Y) of a rule by calculating the ratio between the observed co-occurrence frequency P(X, Y) and the expected co-occurrence frequency ) when X and Y are independent—namely, . If the ratio is close to 1, then little information is provided by this rule. If the ratio is greater than 1, then X and Y are positively correlated; otherwise, they are negatively correlated. Overall, this method is often used to measure the interest of a rule [42].
3. Results
3.1. Patient Statistics
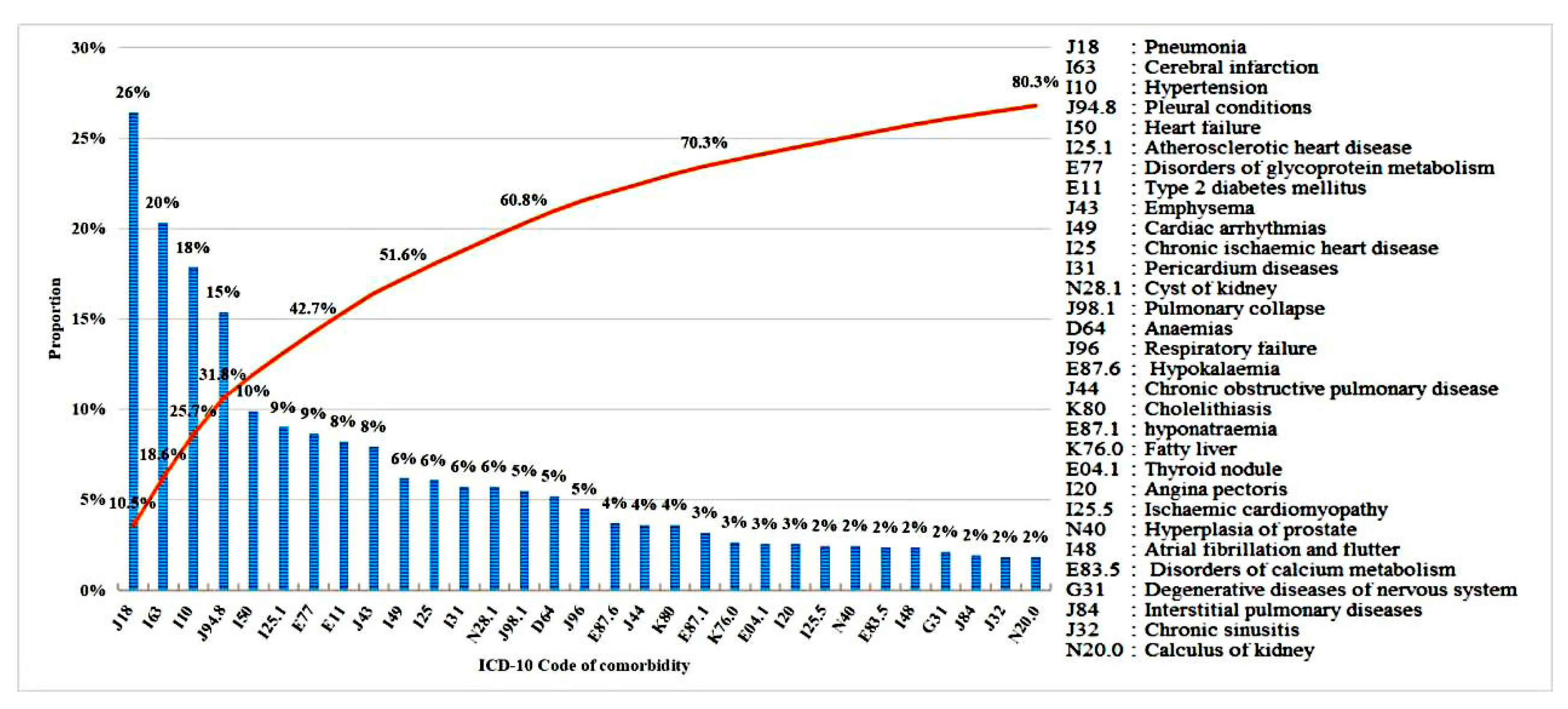
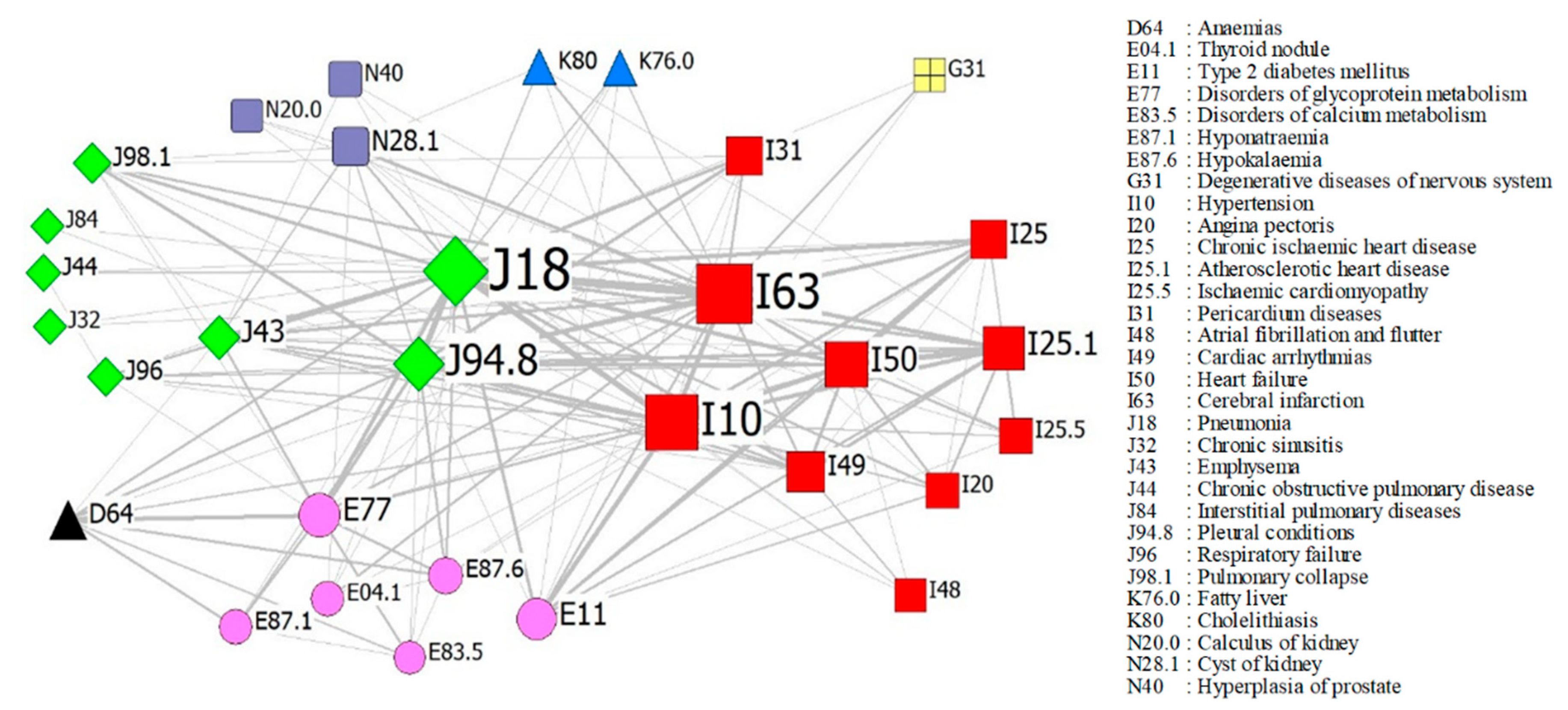
3.2. Network-Based Analysis
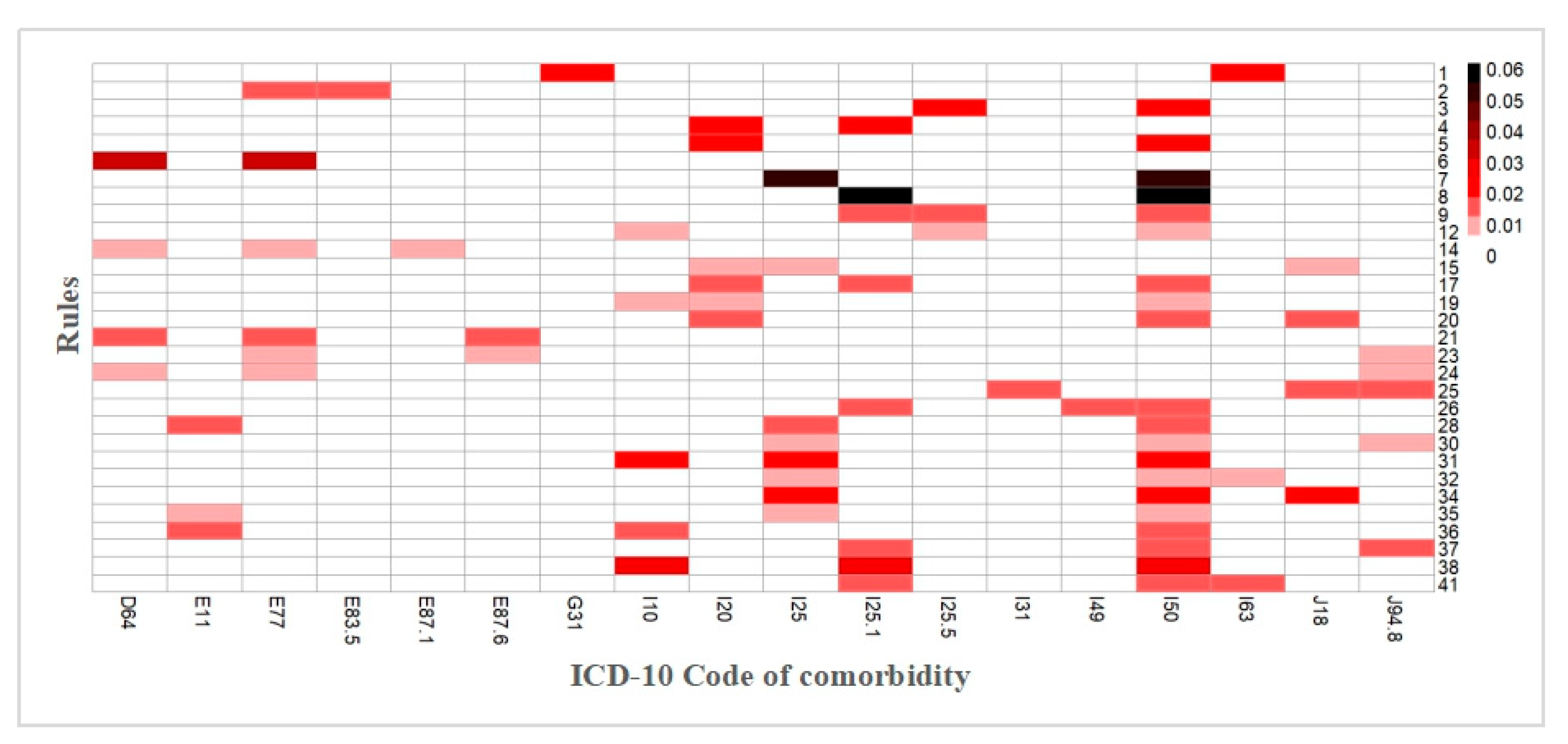
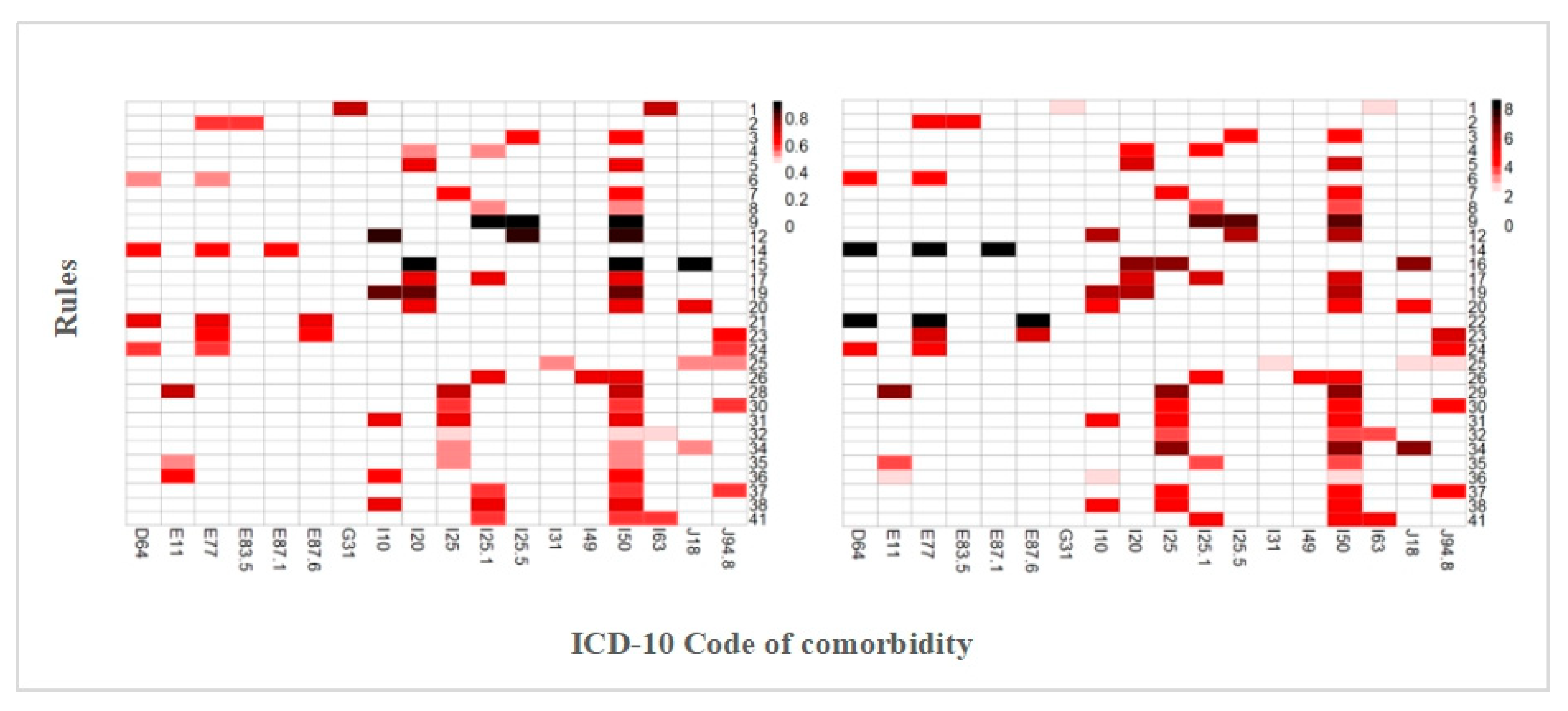
3.3. Derivation of the Association Rules
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef] [PubMed]
- Yancik, R.; Ries, L.A.G. Cancer and aging in America—Demographic and epidemiologic perspectives. Hematol. Oncol. Clin. N. Am. 2000, 14, 17–23. [Google Scholar] [CrossRef]
- Ritchie, C.S.; Kvale, E.; Fisch, M.J. Multimorbidity: An issue of growing importance for oncologists. J. Oncol. Pract. 2011, 7, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Mellemgaard, A.; Luechtenborg, M.; Iachina, M.; Jakobsen, E.; Green, A.; Krasnik, M.; Moller, H. Role of Comorbidity on Survival after Radiotherapy and Chemotherapy for Nonsurgically Treated Lung Cancer. J. Thorac. Oncol. 2015, 10, 272–279. [Google Scholar] [CrossRef]
- Ogle, K.S.; Swanson, G.M.; Woods, N.; Azzouz, F. Cancer and comorbidity—Redefining chronic diseases. Cancer 2000, 88, 653–663. [Google Scholar] [CrossRef]
- Marengoni, A.; Rizzuto, D.; Wang, H.X.; Winblad, B.; Fratiglioni, L. Patterns of Chronic Multimorbidity in the Elderly Population. J. Am. Geriatr. Soc. 2009, 57, 225–230. [Google Scholar] [CrossRef]
- Griffith, L.E.; Gilsing, A.; Mangin, D.; Patterson, C.; van den Heuvel, E.; Sohel, N.; St John, P.; van den Akker, M.; Raina, P. Multimorbidity Frameworks Impact Prevalence and Relationships with Patient-Important Outcomes. J. Am. Geriatr. Soc. 2019, 67, 1632–1640. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, C.C.; Zheng, J.Z.; Hou, L.H.; Xue, Y.Q.; Li, M.M. Prevalence and Related Factors of Comorbidity of Chronic Diseases among Elderly in Taiyuan, China. J. Am. Geriatr. Soc. 2019, 67, S663. [Google Scholar]
- Pengpid, S.; Peltzer, K. Multimorbidity in Chronic Conditions: Public Primary Care Patients in Four Greater Mekong Countries. Int. J. Environ. Res. Public Health 2017, 14, 1019. [Google Scholar] [CrossRef]
- Sanchez-Rodriguez, J.; Martinez-Almazan, E. Predictors of early readmissions in elderly patients with multimorbidity admitted to an intermediate care unit. J. Am. Geriatr. Soc. 2016, 64, S67–S68. [Google Scholar]
- Pes, G.M.; Licheri, G.; Soro, S.; Longo, N.P.; Salis, R.; Tomassini, G.; Niolu, C.; Errigo, A.; Dore, M.P. Overweight: A Protective Factor against Comorbidity in the Elderly. Int. J. Environ. Res. Public Health 2019, 16, 3656. [Google Scholar] [CrossRef] [PubMed]
- Olivares, D.E.V.; Chambi, F.R.V.; Chani, E.M.M.; Craig, W.J.; Pacheco, S.O.S.; Pacheco, F.J. Risk Factors for Chronic Diseases and Multimorbidity in a Primary Care Context of Central Argentina: A Web-Based Interactive and Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 251. [Google Scholar] [CrossRef] [PubMed]
- Bynum, J.P.W.; Chang, C.H.; Austin, A.; Carmichael, D.; Meara, E. Outcomes in Older Adults with Multimorbidity Associated with Predominant Provider of Care Specialty. J. Am. Geriatr. Soc. 2017, 65, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Joao Forjaz, M.; Rodriguez-Blazquez, C.; Guerrero-Fernandez de Alba, I.; Gimeno-Miguel, A.; Bliek-Bueno, K.; Prados-Torres, A.; Culig, J.; Jureviciene, E.; Maggini, M.; Maguire, P.; et al. Application of the JA-CHRODIS Integrated Multimorbidity Care Model (IMCM) to a Case Study of Diabetes and Mental Health. Int. J. Environ. Res. Public Health 2019, 16, 5151. [Google Scholar] [CrossRef]
- Palmer, K.; Carfi, A.; Angioletti, C.; Di Paola, A.; Navickas, R.; Dambrauskas, L.; Jureviciene, E.; Joao Forjaz, M.; Rodriguez-Blazquez, C.; Prados-Torres, A.; et al. A Methodological Approach for Implementing an Integrated Multimorbidity Care Model: Results from the Pre-Implementation Stage of Joint Action CHRODIS-PLUS. Int. J. Environ. Res. Public Health 2019, 16, 5044. [Google Scholar] [CrossRef]
- Cho, H.; Mariotto, A.B.; Mann, B.S.; Klabunde, C.N.; Feuer, E.J. Assessing non-cancer-related health status of US cancer patients: Other-cause survival and comorbidity prevalence. Am. J. Epidemiol. 2013, 178, 339–349. [Google Scholar] [CrossRef]
- Chang, Y.S.; Huang, J.S.; Yen, C.L.; Wang, C.H.; Lai, C.H.; Wu, T.H.; Lan, Y.J.; Chang, P.H.; Yeh, K.Y. The Charlson Comorbidity Index is an Independent Prognostic Factor for Treatment-Naive Hepatocellular Carcinoma Patients with Extrahepatic Metastases. Hepato-Gastroenterology 2015, 62, 1011–1015. [Google Scholar]
- Iachina, M.; Green, A.; Jakobsen, E. The direct and indirect impact of comorbidity on the survival of patients with non-small cell lung cancer: A combination of survival, staging and resection models with missing measurements in covariates. BMJ Open 2014, 4, e003846. [Google Scholar] [CrossRef]
- Wong, M.L.; McMurry, T.L.; Stukenborg, G.J.; Francescatti, A.B.; Amato-Martz, C.; Schumacher, J.R.; Chang, G.J.; Greenberg, C.C.; Winchester, D.P.; McKellar, D.P.; et al. Impact of age and comorbidity on treatment of non-small cell lung cancer recurrence following complete resection: A nationally representative cohort study. Lung Cancer 2016, 102, 108–117. [Google Scholar] [CrossRef]
- Williams, C.D.; Stechuchak, K.M.; Zullig, L.L.; Provenzale, D.; Kelley, M.J. Influence of comorbidity on racial differences in receipt of surgery among US veterans with early-stage non-small-cell lung cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 475–481. [Google Scholar] [CrossRef]
- Mu, X.M.; Wang, W.; Wu, F.Y.; Jiang, Y.Y.; Ma, L.L.; Feng, J. Comorbidity in Older Patients Hospitalized with Cancer in Northeast China based on Hospital Discharge Data. Int. J. Environ. Res. Public Health 2020, 17, 8028. [Google Scholar] [CrossRef] [PubMed]
- John, R.; Kerby, D.S.; Hennessy, C.H. Patterns and impact of comorbidity and multimorbidity among community-resident American Indian elders. Gerontologist 2003, 43, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, L.M.; Lepkowski, J.M.; Imanaka, Y. Comorbidity and its impact on disability. Milbank Q. 1989, 67, 450–484. [Google Scholar] [CrossRef] [PubMed]
- Goldstein-Piekarski, A.N.; Williams, L.M.; Humphreys, K. A trans-diagnostic review of anxiety disorder comorbidity and the impact of multiple exclusion criteria on studying clinical outcomes in anxiety disorders. Transl. Psychiatry 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Rendas-Baum, R. Health state utility for comorbid conditions: evaluating the impact of different estimation methods. Value Health 2018, 21, S322. [Google Scholar] [CrossRef]
- Rief, W.; Nanke, A.; Emmerich, J.; Bender, A.; Zech, T. Causal illness attributions in somatoforin disorders—Associations with comorbidity and illness behavior. J. Psychosom. Res. 2004, 57, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Schiotz, M.L.; Stockmarr, A.; Host, D.; Glumer, C.; Frolich, A. Social disparities in the prevalence of multimorbidity—A register-based population study. BMC Public Health 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.K.; Holden, L.; Sun, J. Identifying comorbidity patterns of health conditions via cluster analysis of pairwise concordance statistics. Stat. Med. 2012, 31, 3393–3405. [Google Scholar] [CrossRef]
- Nicholson, K.; Bauer, M.; Terry, A.; Fortin, M.; Williamson, T.; Thind, A. The Multimorbidity Cluster Analysis Tool: Identifying Combinations and Permutations of Multiple Chronic Diseases Using a Record-Level Computational Analysis. J. Innov. Health Inform. 2017, 24, 962. [Google Scholar] [CrossRef][Green Version]
- Pintelas, E.G.; Kotsilieris, T.; Livieris, I.E.; Pintelas, P. A review of machine learning prediction methods for anxiety disorders. In Proceedings of the 8th International Conference on Software Development and Technologies for Enhancing Accessibility and Fighting Info-exclusion, Thessaloniki, Greece, 20–22 June 2018; pp. 8–15. [Google Scholar] [CrossRef]
- Zandvakili, A.; Philip, N.S.; Jones, S.R.; Tyrka, A.R.; Greenberg, B.D.; Carpenter, L.L. Use of machine learning in predicting clinical response to transcranial magnetic stimulation in comorbid posttraumatic stress disorder and major depression: A resting state electroencephalography study. J. Affect. Disord. 2019, 252, 47–54. [Google Scholar] [CrossRef]
- Agrawal, R.; Imieliński, T.; Swami, A. Mining association rules between sets of items in large databases. In Proceedings of the 1993 ACM SIGMOD international conference on Management of data, Washington, DC, USA, 26–28 May 1993; pp. 207–216. [Google Scholar] [CrossRef]
- Cheng, C.W.; Chanani, N.; Venugopalan, J.; Maher, K.; Wang, M.D. icuARM-An ICU Clinical Decision Support System Using Association Rule Mining. IEEE J. Transl. Eng. Health Med. 2013, 1, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Nahar, J.; Imam, T.; Tickle, K.S.; Chen, Y.P.P. Association rule mining to detect factors which contribute to heart disease in males and females. Expert Syst. Appl. 2013, 40, 1086–1093. [Google Scholar] [CrossRef]
- Pattanaprateep, O.; McEvoy, M.; Attia, J.; Thakkinstian, A. Evaluation of rational nonsteroidal anti-inflammatory drugs and gastro-protective agents use; association rule data mining using outpatient prescription patterns. BMC Med. Inform. Decis. Mak. 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Tai, Y.M.; Chiu, H.W. Comorbidity study of ADHD: Applying association rule mining (ARM) to National Health Insurance Database of Taiwan. Int. J. Med. Inform. 2009, 78, E75–E83. [Google Scholar] [CrossRef]
- Kim, H.S.; Shin, A.M.; Kim, M.K.; Kim, Y.N. Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining. Korean J. Intern. Med. 2012, 27, 197–202. [Google Scholar] [CrossRef]
- Wang, C.H.; Lee, T.Y.; Hui, K.C.; Chung, M.H. Mental disorders and medical comorbidities: Association rule mining approach. Perspect. Psychiatr. Care 2019, 55, 517–526. [Google Scholar] [CrossRef]
- Chen, W.; Sun, K.; Zheng, R.; Zeng, H.; Zhang, S.; Xia, C.; Yang, Z.; Li, H.; Zou, X.; He, J. Cancer incidence and mortality in China, 2014. Chin. J. Cancer Res. 2018, 30, 1–12. [Google Scholar] [CrossRef]
- The Measures for the Administration of the Hospital Grade; National Health Commission of The People’s Republic of China: Beijing, China, 1989.
- Sanders, R. The pareto principle: Its use and abuse. J. Serv. Mark. 1987, 1, 37–40. [Google Scholar] [CrossRef]
- McNicholas, P.D.; Murphy, T.B.; O’Regan, M. Standardising the lift of an association rule. Comput. Stat. Data Anal. 2008, 52, 4712–4721. [Google Scholar] [CrossRef]
- Yao, S.S.; Cao, G.Y.; Han, L.; Chen, Z.S.; Huang, Z.T.; Gong, P.; Hu, Y.; Xu, B. Prevalence and Patterns of Multimorbidity in a Nationally Representative Sample of Older Chinese: Results From the China Health and Retirement Longitudinal Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 1974–1980. [Google Scholar] [CrossRef]
- Hu, X.; Huang, J.; Lv, Y.; Li, G.; Peng, X. Status of prevalence study on multimorbidity of chronic disease in China: Systematic review. Geriatr. Gerontol. Int. 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ruuskanen, O.; Lahti, E.; Jennings, L.C.; Murdoch, D.R. Viral pneumonia. Lancet 2011, 377, 1264–1275. [Google Scholar] [CrossRef]
- Poling, J.; Kelly, L.; Chan, C.; Fisman, D.; Ulanova, M. Hospital admission for community-acquired pneumonia in a First Nations population. Can. J. Rural Med. Off. J. Soc. Rural Physicians Can. 2014, 19, 135–141. [Google Scholar]
- Cangemi, R.; Calvieri, C.; Falcone, M.; Bucci, T.; Bertazzoni, G.; Scarpellini, M.G.; Barilla, F.; Taliani, G.; Violi, F. Relation of Cardiac Complications in the Early Phase of Community-Acquired Pneumonia to Long-Term Mortality and Cardiovascular Events. Am. J. Cardiol. 2015, 116, 647–651. [Google Scholar] [CrossRef]
- Islam, K.M.M.; Jiang, X.; Anggondowati, T.; Lin, G.; Ganti, A.K. Comorbidity and Survival in Lung Cancer Patients. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1079–1085. [Google Scholar] [CrossRef]
- Al-Kindi, S.G.; Oliveira, G.H. Prevalence of Preexisting Cardiovascular Disease in Patients with Different Types of Cancer: The Unmet Need for Onco-Cardiology. Mayo Clin. Proc. 2016, 91, 81–83. [Google Scholar] [CrossRef]
- Iachina, M.; Jakobsen, E.; Moller, H.; Luechtenborg, M.; Mellemgaard, A.; Krasnik, M.; Green, A. The Effect of Different Comorbidities on Survival of Non-small Cells Lung Cancer Patients. Lung 2015, 193, 291–297. [Google Scholar] [CrossRef]
- Wei, Y.F.; Wu, J.T.; Chen, J.Y.; Hsu, C.K.; Lee, H.S.; Hsu, Y.C. Chronic Kidney Disease Is Associated With Mortality Risk In Patients With Lung Cancer: A Nationwide Population-Based Cohort Study. Am. J. Respir. Crit. Care Med. 2016, 193. [Google Scholar] [CrossRef]
- Wei, Y.F.; Chen, J.Y.; Lee, H.S.; Wu, J.T.; Hsu, C.K.; Hsu, Y.C. Association of chronic kidney disease with mortality risk in patients with lung cancer: A nationwide Taiwan population-based cohort study. BMJ Open 2018, 8. [Google Scholar] [CrossRef]
- Wu, W.; Liao, H.; Ye, W.; Li, X.; Zhang, J.; Bu, J. Fatty liver is a risk factor for liver metastasis in Chinese patients with non-small cell lung cancer. Peerj 2019, 7. [Google Scholar] [CrossRef]
- Dominguez-Ventura, A.; Allen, M.S.; Cassivi, S.D.; Nichols, F.C., III; Deschamps, C.; Pairolero, P.C. Lung cancer in octogenarians: Factors affecting morbidity and mortality after pulmonary resection. Ann. Thorac. Surg. 2006, 82, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
- Kravchenko, J.; Berry, M.; Arbeev, K.; Lyerly, H.K.; Yashin, A.; Akushevich, I. Cardiovascular comorbidities and survival of lung cancer patients: Medicare data based analysis. Lung Cancer 2015, 88, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Shukuya, T.; Mori, K.; Kanemaru, R.; Honma, Y.; Nanjo, Y.; Muraki, K.; Shibayama, R.; Koyama, R.; Shimada, N.; et al. Cerebral infarction in advanced non-small cell lung cancer: A case control study. BMC Cancer 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; Han, Y.; Zhou, Y. Research progress of cancer related ischemic stroke. Chin. J. Cerebrovasc. Dis. 2018, 15, 206–211. [Google Scholar]
- Mancuso, A.; Migliorino, M.; De Santis, S.; Saponiero, A.; De Marinis, F. Correlation between anemia and functional/cognitive capacity in elderly lung cancer patients treated with chemotherapy. Ann. Oncol. 2006, 17, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Balducci, L. Anemia, fatigue and aging. Transfus. Clin. Biol. 2010, 17, 375–381. [Google Scholar] [CrossRef] [PubMed]
- McMahon, T.J.; Prybylowski, A.C. Anemia in the Patient with Chronic Lung Disease. In Management of Anemia: A Comprehensive Guide for Clinicians; Provenzano, R., Lerma, E.V., Szczech, L., Eds.; Springer: New York, NY, USA, 2018; pp. 143–155. [Google Scholar] [CrossRef]
- Li, Y.N.; Zhang, L.; Li, X.L.; Cui, D.J.; Zheng, H.D.; Yang, S.Y.; Yang, W.L. Glycoprotein nonmetastatic B as a prognostic indicator in small cell lung cancer. APMIS 2014, 122, 140–146. [Google Scholar] [CrossRef]
- Wang, L.H.; Yang, J.Y.; Yang, S.N.; Li, Y.; Ping, G.F.; Hou, Y.; Cui, W.; Wang, Z.Z.; Xiao, W.; Wu, C.F. Suppression of NF-κB signaling and P-glycoprotein function by gambogic acid Synergistically Potentiates Adriamycin -induced Apoptosis in Lung Cancer. Curr. Cancer Drug Targets 2014, 14, 91–103. [Google Scholar] [CrossRef]
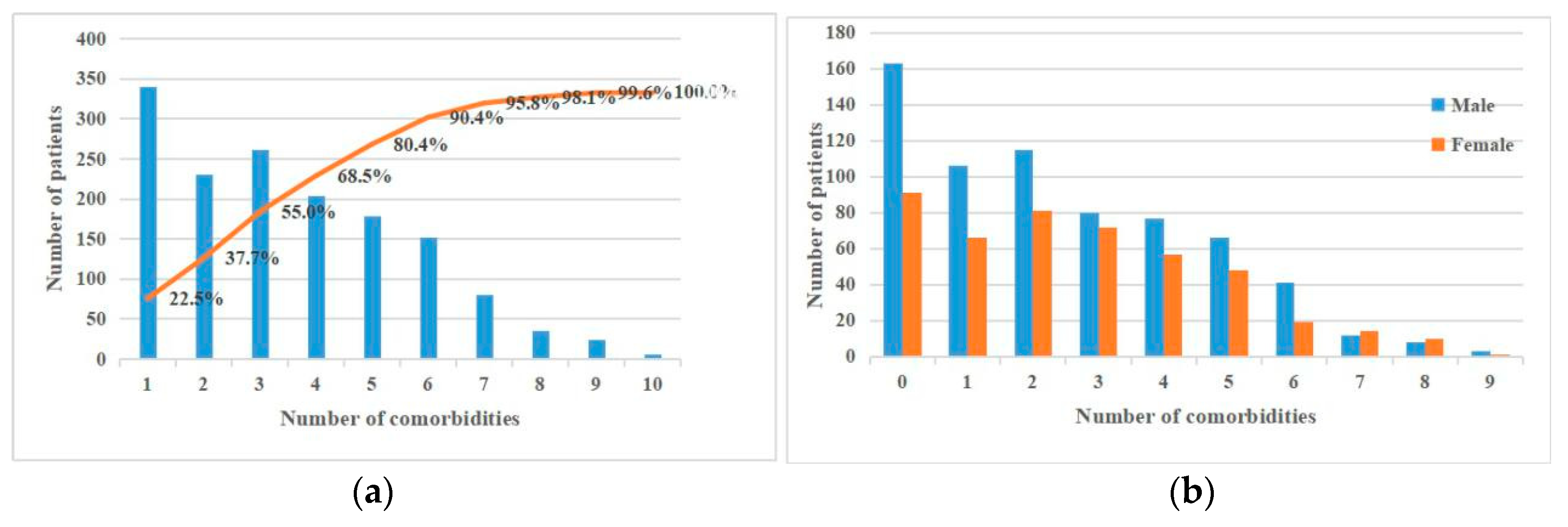

| Characteristics | N | Percentage (%) |
|---|---|---|
| Total | 1510 | 100 |
| Age(years) | ||
| 65–74 | 1124 | 74.4 |
| 75–84 | 329 | 21.8 |
| 85 + | 57 | 3.8 |
| Gender | ||
| Male | 909 | 60.2 |
| Female | 601 | 39.8 |
| Nationality | ||
| Han | 1416 | 93.8 |
| Korean | 68 | 4.5 |
| Other | 25 | 1.7 |
| Occupation | ||
| Farmers | 246 | 16.3 |
| Retired | 337 | 22.3 |
| Unemployed | 84 | 5.6 |
| Workers | 55 | 3.6 |
| Staff | 23 | 1.5 |
| Other | 33 | 2.2 |
| Unspecified | 732 | 48.5 |
| Marital status | ||
| Unmarried | 9 | 0.6 |
| Married | 1375 | 91.0 |
| Death of a spouse | 59 | 3.8 |
| Divorce | 11 | 0.7 |
| Other | 56 | 3.7 |
| No. of comorbidities | ||
| 0 | 339 | 22.5 |
| 1 | 230 | 15.2 |
| 2 | 262 | 17.3 |
| 3 | 203 | 13.5 |
| >3 | 496 | 31.5 |
| Disease | All Cases (n) | Single Comorbidity (%) | Multiple Comorbidities (%) |
|---|---|---|---|
| Pneumonia | 299 | 11.7 | 88.3 |
| Cerebral infarction | 230 | 10.9 | 89.1 |
| Hypertension | 202 | 8.4 | 91.6 |
| Pleural conditions | 174 | 11.5 | 88.5 |
| Heart failure | 112 | 0.0 | 100.0 |
| Atherosclerotic heart disease | 102 | 3.9 | 96.1 |
| Disorders of glycoprotein metabolism | 98 | 1.0 | 99.0 |
| Type 2 diabetes mellitus | 93 | 10.8 | 89.2 |
| Emphysema | 90 | 4.4 | 95.6 |
| Cardiac arrhythmias | 70 | 1.4 | 98.6 |
| Chronic ischemic heart disease | 69 | 0.0 | 100.0 |
| Pericardium diseases | 65 | 10.8 | 89.2 |
| Cyst of kidney | 65 | 1.5 | 98.5 |
| Pulmonary collapse | 62 | 4.8 | 95.2 |
| Anemia | 59 | 3.4 | 96.6 |
| Respiratory failure | 51 | 7.8 | 92.2 |
| Hypokalemia | 42 | 0.0 | 100.0 |
| Chronic obstructive pulmonary disease | 41 | 7.3 | 92.7 |
| Cholelithiasis | 41 | 2.4 | 97.6 |
| Hyponatremia | 36 | 5.6 | 94.4 |
| Fatty liver | 30 | 0.0 | 100.0 |
| Thyroid nodule | 29 | 3.4 | 96.6 |
| Angina pectoris | 29 | 0.0 | 100.0 |
| Ischemic cardiomyopathy | 28 | 3.6 | 96.4 |
| Hyperplasia of the prostate | 28 | 3.6 | 96.4 |
| Disorders of calcium metabolism | 27 | 0.0 | 100.0 |
| Atrial fibrillation and flutter | 27 | 3.7 | 96.3 |
| Degenerative diseases of the nervous system | 24 | 0.0 | 100.0 |
| Interstitial pulmonary diseases | 22 | 13.6 | 86.4 |
| Chronic sinusitis | 21 | 4.8 | 95.2 |
| Calculus of the kidney | 21 | 0.0 | 100.0 |
| No. | Rules | Sup | Con | Lift | ||
|---|---|---|---|---|---|---|
| 1 | (Degenerative diseases of the nervous system) | => | (Cerebral infarction) | 0.02 | 0.71 | 2.60 |
| 2 | (Disorders of calcium metabolism) | => | (Disorders of glycoprotein metabolism) | 0.02 | 0.56 | 4.78 |
| 3 | (Ischemic cardiomyopathy) | => | (Heart failure) | 0.02 | 0.61 | 4.58 |
| 4 | (Angina pectoris) | => | (Atherosclerotic heart disease) | 0.02 | 0.55 | 4.57 |
| 5 | (Angina pectoris) | => | (Heart failure) | 0.02 | 0.69 | 5.20 |
| 6 | (Anemias) | => | (Disorders of glycoprotein metabolism) | 0.04 | 0.53 | 4.53 |
| 7 | (Chronic ischemic heart disease) | => | (Heart failure) | 0.05 | 0.62 | 4.70 |
| 8 | (Atherosclerotic heart disease) | => | (Heart failure) | 0.06 * | 0.51 | 3.84 |
| 9 | (Atherosclerotic heart disease, Ischemic cardiomyopathy) | => | (Heart failure) | 0.01 | 0.92 | 6.96 |
| 10 | (Ischemic cardiomyopathy, Heart failure) | => | (Atherosclerotic heart disease) | 0.01 | 0.71 | 5.84 |
| 11 | (Ischemic cardiomyopathy, Heart failure) | => | (Hypertension) | 0.01 | 0.59 | 2.46 |
| 12 | (Hypertension, Ischemic cardiomyopathy) | => | (Heart failure) | 0.01 | 0.83 | 6.28 |
| 13 | (Anemias, Hyponatremia) | => | (Disorders of glycoprotein metabolism) | 0.01 | 0.60 | 5.17 |
| 14 | (Disorders of glycoprotein metabolism, Hyponatremia) | => | (Anemias) | 0.01 | 0.60 | 8.58 |
| 15 | (Angina pectoris, Chronic ischemic heart disease) | => | (Pneumonia) | 0.01 | 0.90 | 2.54 |
| 16 | (Angina pectoris, Pneumonia) | => | (Chronic ischemic heart disease) | 0.01 | 0.53 | 6.48 |
| 17 | (Angina pectoris, Atherosclerotic heart disease) | => | (Heart failure) | 0.01 | 0.69 | 5.18 |
| 18 | (Angina pectoris, Heart failure) | => | (Atherosclerotic heart disease) | 0.01 | 0.55 | 4.55 |
| 19 | (Hypertension, Angina pectoris) | => | (Heart failure) | 0.01 | 0.82 | 6.17 |
| 20 | (Angina pectoris, Pneumonia) | => | (Heart failure) | 0.01 | 0.65 | 4.88 |
| 21 | (Anemias, Hypokalemia) | => | (Disorders of glycoprotein metabolism) | 0.01 | 0.69 | 5.92 |
| 22 | (Disorders of glycoprotein metabolism, Hypokalemia) | => | (Anemias) | 0.01 | 0.58 | 8.28 |
| 23 | (Hypokalemia, Pleural conditions) | => | (Disorders of glycoprotein metabolism) | 0.01 | 0.64 | 5.54 |
| 24 | (Anemias, Pleural conditions) | => | (Disorders of glycoprotein metabolism) | 0.01 | 0.56 | 4.84 |
| 25 | (Pericardium diseases, Pneumonia) | => | (Pleural conditions) | 0.02 | 0.52 | 2.51 |
| 26 | (Atherosclerotic heart disease, Cardiac arrhythmias) | => | (Heart failure) | 0.02 | 0.67 | 5.02 |
| 27 | (Cardiac arrhythmias, Heart failure) | => | (Atherosclerotic heart disease) | 0.02 | 0.58 | 4.83 |
| 28 | (Type 2 diabetes mellitus, Chronic ischemic heart disease) | => | (Heart failure) | 0.01 | 0.73 | 5.53 |
| 29 | (Type 2 diabetes mellitus, Heart failure) | => | (Chronic ischemic heart disease) | 0.01 | 0.52 | 6.41 |
| 30 | (Chronic ischemic heart disease, Pleural conditions) | => | (Heart failure) | 0.01 | 0.59 | 4.43 |
| 31 | (Hypertension, Chronic ischemic heart disease) | => | (Heart failure) | 0.02 | 0.67 | 5.02 |
| 32 | (Chronic ischemic heart disease, Cerebral infarction) | => | (Heart failure) | 0.01 | 0.50 | 3.77 |
| 33 | (Chronic ischemic heart disease, Pneumonia) | => | (Heart failure) | 0.02 | 0.53 | 4.00 |
| 34 | (Heart failure, Pneumonia) | => | (Chronic ischemic heart disease) | 0.02 | 0.55 | 6.71 |
| 35 | (Type 2 diabetes mellitus, Atherosclerotic heart disease) | => | (Heart failure) | 0.01 | 0.53 | 3.99 |
| 36 | (Type 2 diabetes mellitus, Heart failure) | => | (Hypertension) | 0.02 | 0.62 | 2.59 |
| 37 | (Atherosclerotic heart disease, Pleural conditions) | => | (Heart failure) | 0.02 | 0.59 | 4.45 |
| 38 | (Hypertension, Atherosclerotic heart disease) | => | (Heart failure) | 0.03 | 0.67 | 5.02 |
| 39 | (Hypertension, Heart failure) | => | (Atherosclerotic heart disease) | 0.03 | 0.50 | 4.14 |
| 40 | (Atherosclerotic heart disease, Cerebral infarction) | => | (Heart failure) | 0.02 | 0.50 | 3.77 |
| 41 | (Heart failure, Cerebral infarction) | => | (Atherosclerotic heart disease) | 0.02 | 0.58 | 4.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, J.; Mu, X.-m.; Ma, L.-l.; Wang, W. Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records. Int. J. Environ. Res. Public Health 2020, 17, 9119. https://doi.org/10.3390/ijerph17239119
Feng J, Mu X-m, Ma L-l, Wang W. Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records. International Journal of Environmental Research and Public Health. 2020; 17(23):9119. https://doi.org/10.3390/ijerph17239119
Chicago/Turabian StyleFeng, Jia, Xiao-min Mu, Ling-ling Ma, and Wei Wang. 2020. "Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records" International Journal of Environmental Research and Public Health 17, no. 23: 9119. https://doi.org/10.3390/ijerph17239119
APA StyleFeng, J., Mu, X.-m., Ma, L.-l., & Wang, W. (2020). Comorbidity Patterns of Older Lung Cancer Patients in Northeast China: An Association Rules Analysis Based on Electronic Medical Records. International Journal of Environmental Research and Public Health, 17(23), 9119. https://doi.org/10.3390/ijerph17239119





